General anesthetics General anaesthetics General anesthesia is a

- Slides: 34
General anesthetics
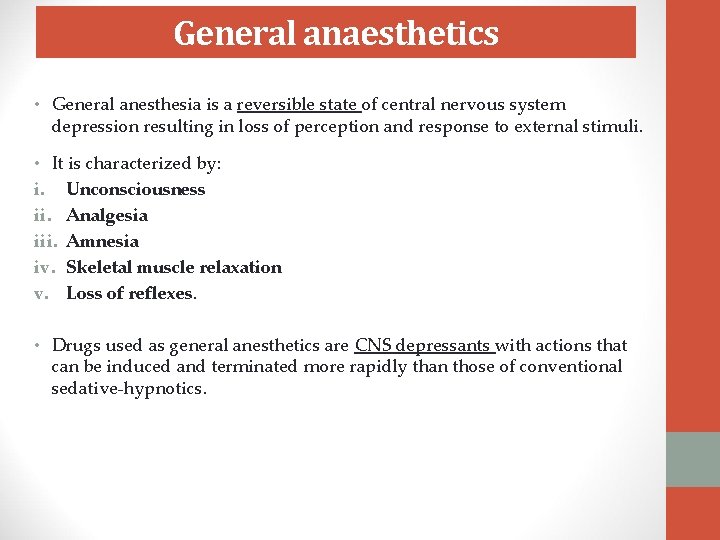
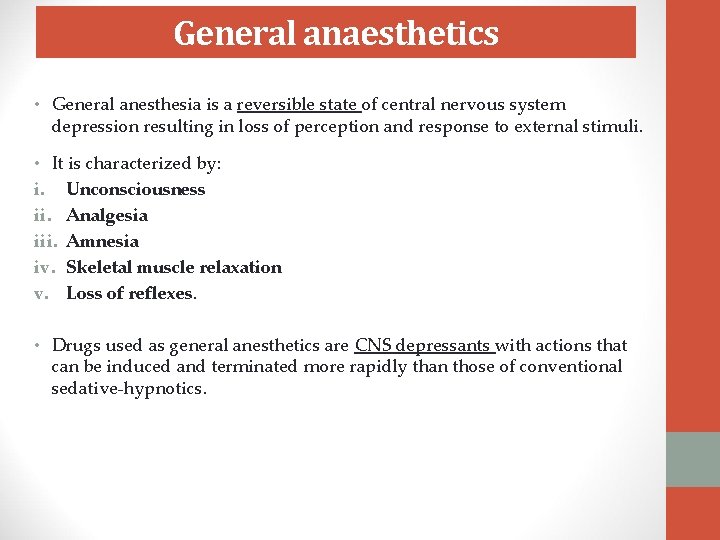
General anaesthetics • General anesthesia is a reversible state of central nervous system depression resulting in loss of perception and response to external stimuli. • It is characterized by: i. Unconsciousness ii. Analgesia iii. Amnesia iv. Skeletal muscle relaxation v. Loss of reflexes. • Drugs used as general anesthetics are CNS depressants with actions that can be induced and terminated more rapidly than those of conventional sedative-hypnotics.
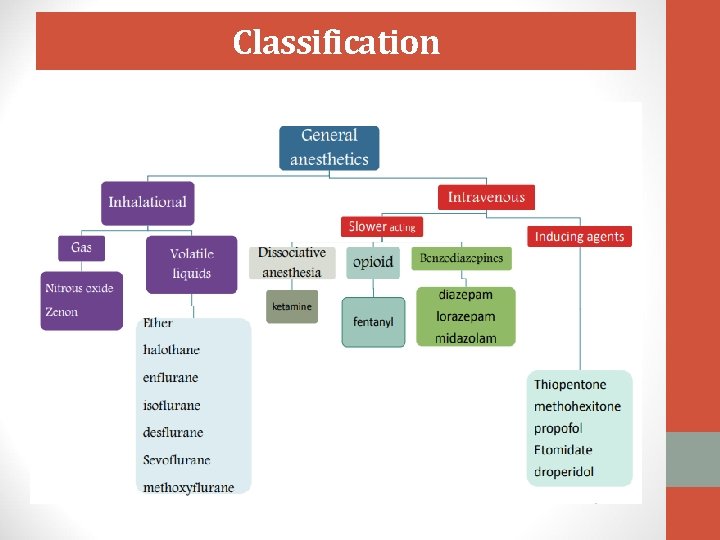
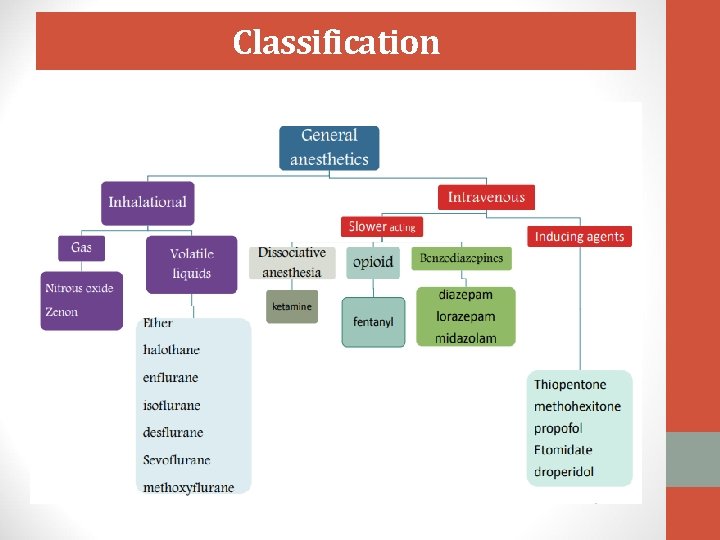
Classification
Factors in selection of anaesthesia • Drugs are chosen to provide safe and efficient anesthesia based on: 1. The type of the surgical or diagnostic procedure 2. Patient characteristics such as organ function, medical conditions, and concurrent medications e. g. ischemic heart disease, hypertension, bronchial asthma. Status of organ systems i. Cardiovascular: Although the hypotensive effect of most anesthetics is sometimes desirable, reduced perfusion pressure could cause ischemic injury of tissues. ii. Respiratory system: All inhaled anesthetics depress the respiratory system. Interestingly, they are bronchodilators. iii. Liver and kidney: The release of fluoride, bromide, and other metabolic products of the halogenated hydrocarbons can affect these organs, especially with repeated anesthetic administration over a short period of time.
iv. Pregnancy: Effects on fetal organogenesis are a major concern in early pregnancy. • Nitrous oxide can cause aplastic anemia in the unborn child. • Oral clefts have occurred in the fetuses of women who have received benzodiazepines. • Diazepam causes temporary hypotonia and altered thermoregulation in the newborn if used during labour. v. Nervous system: The existence of neurologic disorders (e. g. , epilepsy) influences the selection of anesthetic
Pre-anesthetic medications • Some drugs are given prior to anesthesia. These pre-anesthetic medications serve to i. Calm the patient, relieve pain ii. Protect against undesirable effects of the subsequently administered anesthetics or the surgical procedure. iii. Facilitate smooth induction of anesthesia iv. Lower the required dose of anesthetic Preanaesthetic medicines include: i. Benzodiazepines - midazolam or diazepam: For anxiolysis and amnesia. ii. Barbiturates - pentobarbital: For sedation iii. Antihistamines -Diphenhydramine: Prevention of allergic reactions iv. H 2 receptor blocker- famotidine, ranitidine: Reduce gastric acidity v. Antiemetics- ondansetron: Prevents aspiration of stomach contents and post surgical vomiting vi. Acetaminophen, celecoxib or opioids (fentanyl) for analgesia vii. Anticholinergics- glycopyrrolate, scopolamine: For amnesia, reduction of bronchial and salivary secretions, reduce any tendency to bronchospasm, prevent bradycardia and hypotension
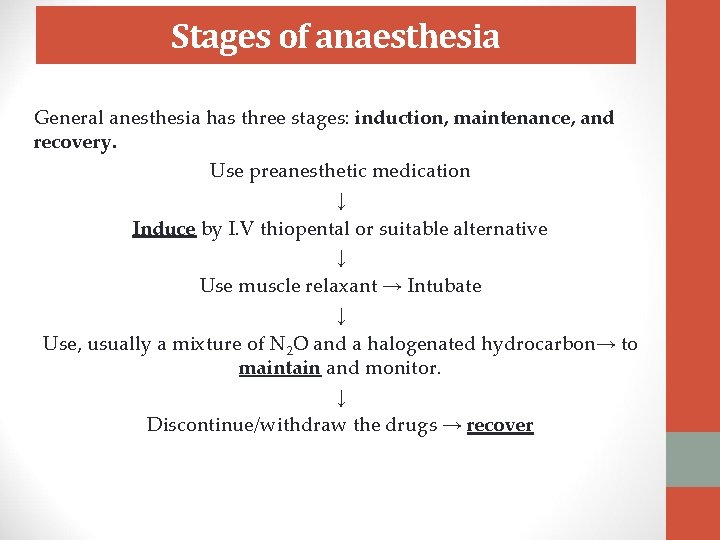
Stages of anaesthesia General anesthesia has three stages: induction, maintenance, and recovery. Use preanesthetic medication ↓ Induce by I. V thiopental or suitable alternative ↓ Use muscle relaxant → Intubate ↓ Use, usually a mixture of N 2 O and a halogenated hydrocarbon→ to maintain and monitor. ↓ Discontinue/withdraw the drugs → recover
Depths of anaesthesia • Guedel (1920) described four sequential stages with ether anaesthesia: A. Stage 1: Analgesia • The patient has decreased awareness of pain, sometimes with amnesia. Consciousness may be impaired but is not lost. B. Stage 2: Delirium • The patient appears to be delirious and excited. Amnesia occurs, reflexes are enhanced, and respiration is typically irregular; retching and incontinence may occur. C. Stage 3: Surgical Anesthesia • The patient is unconscious and has no pain reflexes; respiration is very regular, and blood pressure is maintained. D. Stage 4: Medullary Depression • The patient develops severe respiratory and cardiovascular depression that requires mechanical and pharmacologic support.
Mechanism of action of anesthetic drugs • No specific receptor has been identified. The fact that chemically unrelated compounds produce anesthesia argues against the existence of a single receptor. • The focus is NOW on proteins comprising ion channels: i. GABAA receptors, Glycine receptors: Sole targets for benzodiazepines and also I. V anaesthetics such as thiopental, propofol and etomidate ii. NMDA glutamate receptors (N 2 O and ketamine): iii. Nicotinic receptors: Blocks the excitatory postsynaptic current of the nicotinic receptors, inducing skeletal muscle paralysis (atracurium, pancuronium, vecuronium).
Inhalation anaesthetics • Inhaled gases are used primarily for maintenance of anesthesia. • Depth of anesthesia can be rapidly altered by changing the inhaled concentration • They have very narrow therapeutic index. • No antagonists exist. • Modern inhalation anesthetics are nonflammable, non-explosive agents. • There have decrease cerebrovascular resistance, resulting in increased perfusion of the brain • Cause bronchodilation, and decrease both spontaneous ventilation and hypoxic pulmonary vasoconstriction (increased pulmonary vascular resistance in poorly aerated regions of the lungs, redirecting blood flow to more oxygenated regions). • Movement of these agents from the lungs to various body compartments depends upon their solubility in blood and tissues, as well as on blood flow. These factors play a role in induction and recovery.
Minimum alveolar concentration (MAC) • The MAC is defined as the concentration of inhaled anesthetic required to produce immobility in 50% of subjects in response to surgical (pain) stimulus. • It is a measurement of the potency (ED 50) of the anesthetic and can be used to compare potency of anesthetics • It is expressed as the percentage of gas in a mixture required to achieve that effect. The smaller the MAC, the more potent the anesthetic is. • The more lipid soluble, the lower the concentration needed to produce anesthesia and, thus, the higher the potency. • Hyperthermia, drugs that increase CNS catecholamines, and chronic ethanol abuse are factors that can increase MAC • Increased age, hypothermia, pregnancy, sepsis, acute intoxication, concurrent IV anesthetics, and α 2 -adrenergic receptor agonists (e. g. , clonidine, dexmedetomidine), decrease MAC.
Halothane § It is the prototype inhalation anaesthetic § It is potent, and has rapid induction and recovery § It is neither flammable nor explosive, possess a sweet smell and is a non irritant § Does not augment bronchial and salivary secretions. § There’s low incidence of post operative nausea and vomiting. § It relaxes both skeletal and uterine muscle, and can be used in obstetrics when uterine relaxation is indicated. § It is not hepatotoxic in pediatric patient, and combined with its pleasant odor, this makes it suitable in children for inhalation induction.
Halothane (continued) Limitations in the use of halothane include: 1. It is a weak analgesic (thus is usually co-administerd with N 2 O, opioids) 2. It is a strong respiratory depressant 3. It is a strong cardiovascular depressant; halothane is vagomimetic and cause atropine-sensitive bradycardia. 4. Causes cardiac arrhythmias 5. Has hypotensive effect 6. It is associated with a risk of hepatotoxicity on repeated exposure. It undergoes oxidative metabolism in the liver to produce tissue-toxic hydrocarbons (e. g. , trifluroethanol and bromide ion). 7. Can cause malignant hyperthermia
Nitrous oxide (N 2 O) “laughing gas” • It is a potent analgesic but a weak general anesthetic. It is therefore not used on its own as an anaesthetic, but is very often used as an adjunct to volatile anaesthetics, allowing them to be used at lower concentrations • Has rapid onset and recovery • Does not depress respiration, and no muscle relaxation. • No effect on CVS or on increasing cerebral blood flow • It’s used clinically in dental surgery, obstetrics, postoperative physiotherapy, refractory pain in terminal illness, and maintenance of anesthesia. • The least hepatotoxic and not teratogenic. . Thus is used to reduce pain during childbirth
Enflurane • It is an halogenated hydrocarbon less potent than halothane, but produces rapid induction and recovery • ~2% metabolized to fluoride ion, which is excreted by the kidney • Has some analgesic activity • It differs from halothane in that it produces fewer arrhythmias, less sensitization of the heart to catecholamines and greater potentiation of muscle relaxant due to more potent “curare-like” effect. • However, it produces CNS excitation at twice the MAC and can induce seizure
Isoflurane • A very stable halogenated hydrocarbon molecule that undergoes little metabolism • Not tissue toxic • Does not induce cardiac arrhythmias • Does not sensitize the heart to the action of catecholamines • Produces concentration-dependent hypotension due to peripheral vasodilation • It also dilates the coronary vasculature, increasing coronary blood flow and oxygen consumption by the myocardium, this property make it beneficial in patients with ischemic heart disease.
Other inhalation anesthetics • Diethylether (ether): a volatile anesthetic, is practically obsolete because: it is explosive and highly inflammable when mixed with oxygen; its use entails prolonged induction and recovery; it causes post-operative nausea and vomiting; it stimulates salivary and bronchial secretions; and it stimulates the vagus to cause bradycardia. • Other more or less obsolete inhalation anestheticd ethylchloride, vinyl ether, cyclopropane, and chloroform. are • These agents cause serious severe cardiovascular side effects such as cardiac dysrrthmias by sensitizing the cardiac muscle to circulating cathecholamines which the agents themselves may release from the adrenal medulla. • Chloroform is toxic to the liver.
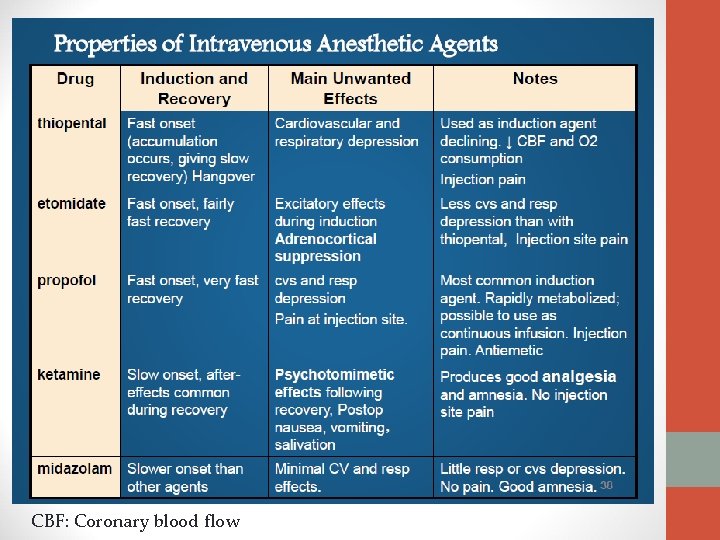
Intravenous anaesthetics • Intravenous anesthetics are usually used for induction. • They are usually given to induce rapid anesthesia which is then maintained by another anesthetic or are used for operations of brief duration. • They include: • Barbiturates • Propofol • Ketamine • Etomidate
Barbiturates • Thiopental, methohexital • They are potent anesthetics but a weak analgesics • High lipid solubility; quickly enter the CNS and depress function, often in less than one minute, and redistribution occur very rapidly as well to other body tissues, including skeletal muscle and ultimately adipose tissue (which serve as a reservoir). • Thiopental has minor effects on the CVS but it may cause severe hypotension in hypovolemic or shock patient • All barbiturates can cause apnea (temporary cessation of breathing, especially during sleep), coughing, chest wall spasm, laryngospasm, and bronchospasm
Propofol • Propofol, a phenol derivative, is an i. v sedative-hypnotic used in the induction and or maintenance of anesthesia. • Onset is smooth and rapid (40 seconds) • It is occasionally accompanied by excitatory phenomena, such as muscle twitching, spontaneous movement, or hiccups. • It decreases BP without depressing the myocardium, it also reduce intracranial pressure. • It is widely used and has replaced thiopental as the first choice for anesthesia induction and sedation, because it produces a euphoric feeling in the patient and does not cause post anesthetic nausea and vomiting. • Has poor analgesia.
Etomidate • Is used to induce anesthesia, it is a hypnotic agent but lacks analgesic activity. • Induction is rapid and short acting • It is only used for patients with coronary artery disease or cardiovascular dysfunction because it has no effect on heart and circulation • Adverse effects: a decrease in plasma cortisol and aldosterone levels which can persist for up to eight hours. This is due to inhibition of 11 B-hydroxylase
Ketamine • Ketamine (phencyclidine derivative) is a short-acting anesthetic which induces a dissociated state in which the patient is conscious but trancelike state (catalepsy). The patient is dissociated or uncoupled from sensory, motor, memory and emotional functions in the brain but cardiac function is not affected and there is minimal respiratory depression. They are rigid with their eyes open and staring like they are in a trance. • This dissociative anesthesia provides sedation, amnesia, and immobility. • Ketamine stimulates central sympathetic outflow, causing stimulation of the heart with increased blood pressure and cardiac output. • It is also a potent bronchodilator. Therefore, it is beneficial in patients with hypovolemic or cardiogenic shock and in asthmatics. Conversely, it is contraindicated in hypertensive or stroke patients. • Ketamine is used mainly in children and elderly adults for short procedures. • It is not widely used, because it increases cerebral blood flow and may induce hallucinations, particularly in young adults.
Adjuvants (BDZs & Opioids) Benzodiazepine (midazolam, lorazepam and diazepam): • Are used in conjunction with anesthetics to sedate the patient. Opioids (fentanyl and sufentanil) • Are used together with anesthetics. They provide analgesic but not good amnesic actions. • They are administered either I. V, epidurally, or intrathecally • All cause hypotension, respiratory depression and muscle rigidity as well as post anesthetic nausea and vomiting • They are antagonized by naloxone.
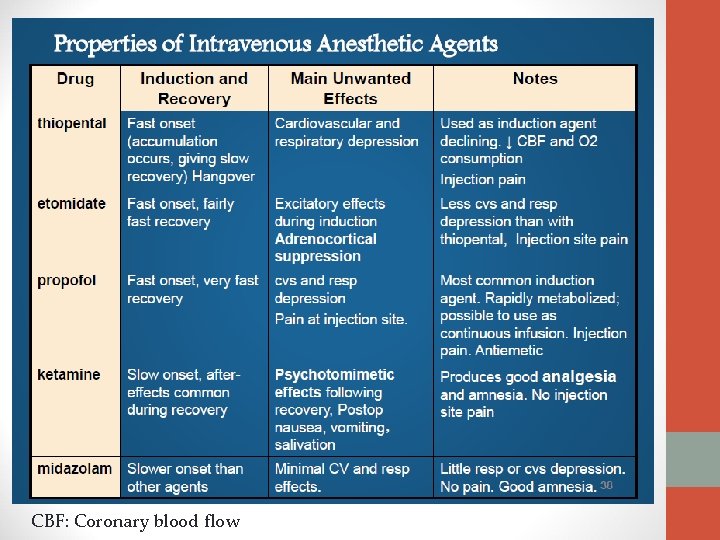
CBF: Coronary blood flow

Local anesthetics
Definition • Local anesthesia is defined as a loss of sensation in a circumscribed area of the body, caused by depression of excitation in nerve endings or an inhibition of the conduction process in peripheral nerves. • A local anaesthetic can be defined as a drug which reversibly prevents transmission of the nerve impulse in the region to which it is applied, without affecting consciousness. • When it is used on specific nerve pathways (nerve block), effects such as analgesia and paralysis can be achieved without any structural damage to neurons.
Characteristics of local anaesthetics 1. 2. 3. 4. 5. It should not be irritating to tissue to which it is applied It should not cause any permanent alteration of nerve structure Its systemic toxicity should be low Time of onset of anesthesia should be short It should be effective regardless of whether it is injected into the tissue or applied locally to mucous membrane. 6. The duration of action should be long enough to permit the completion of procedure (yet not so long as to require an extended recovery). 7. It should have the potency sufficient to give complete anesthesia without the use of harmful concentration solutions. 8. It should be free from producing allergic reactions. 9. It should be stable in solution and relatively undergo biotransformation in the body. 10. It should be either sterile or be capable of being sterilized by heat without deterioration.
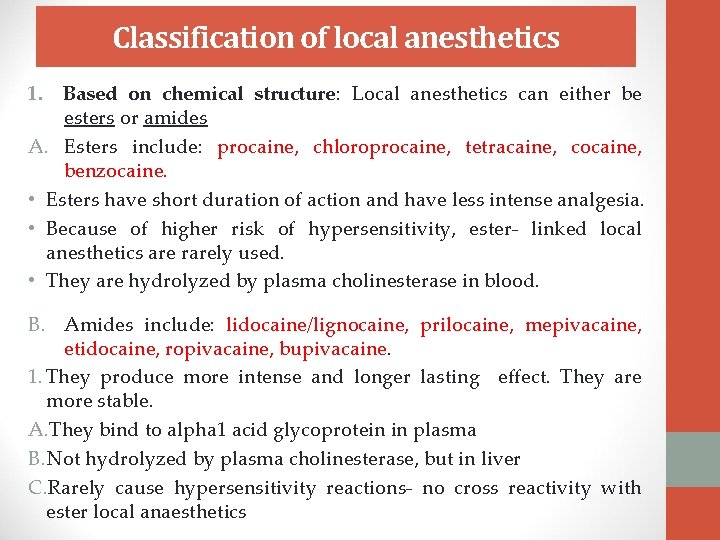
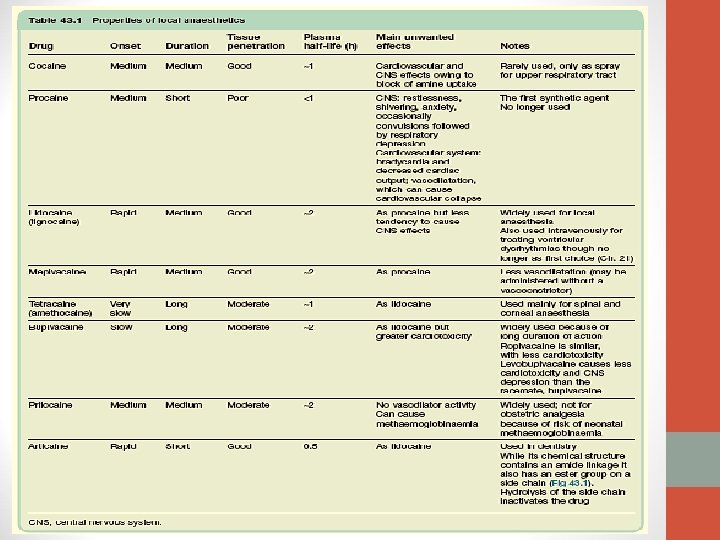
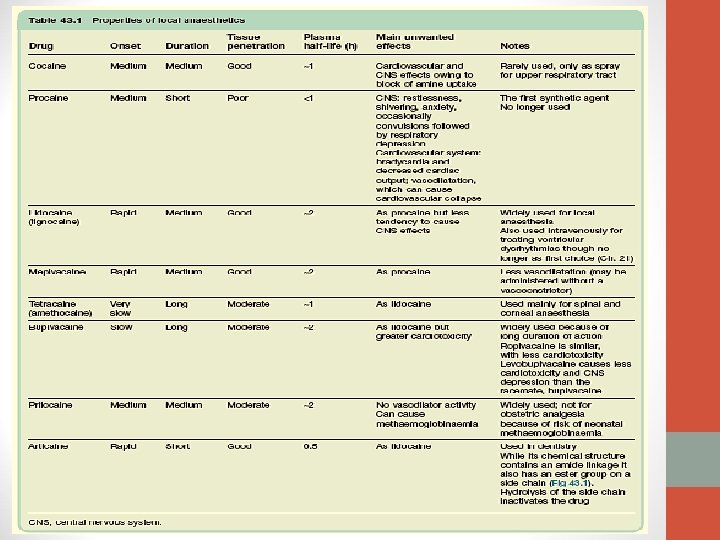
Classification of local anesthetics 1. Based on chemical structure: Local anesthetics can either be esters or amides A. Esters include: procaine, chloroprocaine, tetracaine, cocaine, benzocaine. • Esters have short duration of action and have less intense analgesia. • Because of higher risk of hypersensitivity, ester- linked local anesthetics are rarely used. • They are hydrolyzed by plasma cholinesterase in blood. B. Amides include: lidocaine/lignocaine, prilocaine, mepivacaine, etidocaine, ropivacaine, bupivacaine. 1. They produce more intense and longer lasting effect. They are more stable. A. They bind to alpha 1 acid glycoprotein in plasma B. Not hydrolyzed by plasma cholinesterase, but in liver C. Rarely cause hypersensitivity reactions- no cross reactivity with ester local anaesthetics
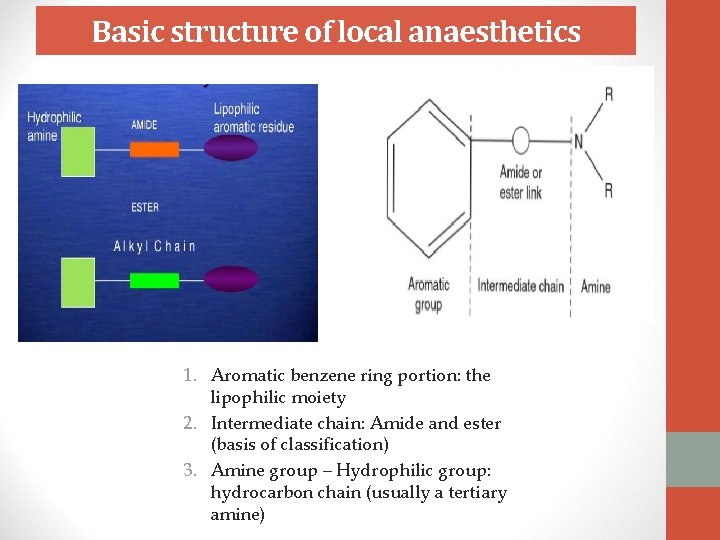
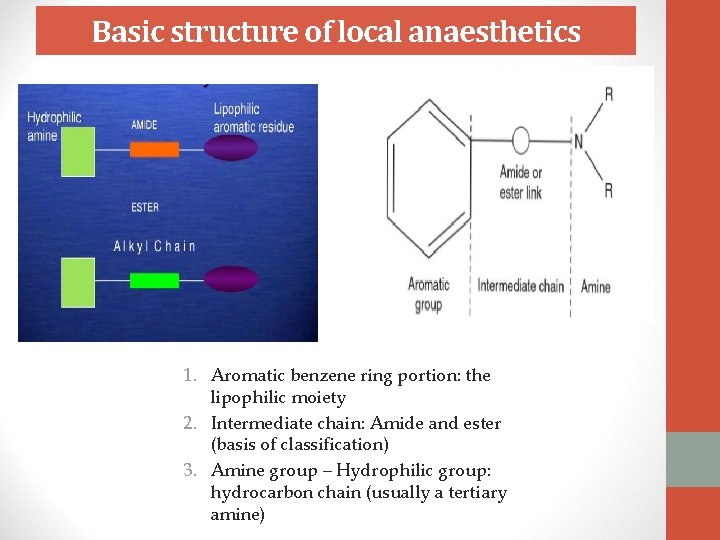
Basic structure of local anaesthetics 1. Aromatic benzene ring portion: the lipophilic moiety 2. Intermediate chain: Amide and ester (basis of classification) 3. Amine group – Hydrophilic group: hydrocarbon chain (usually a tertiary amine)
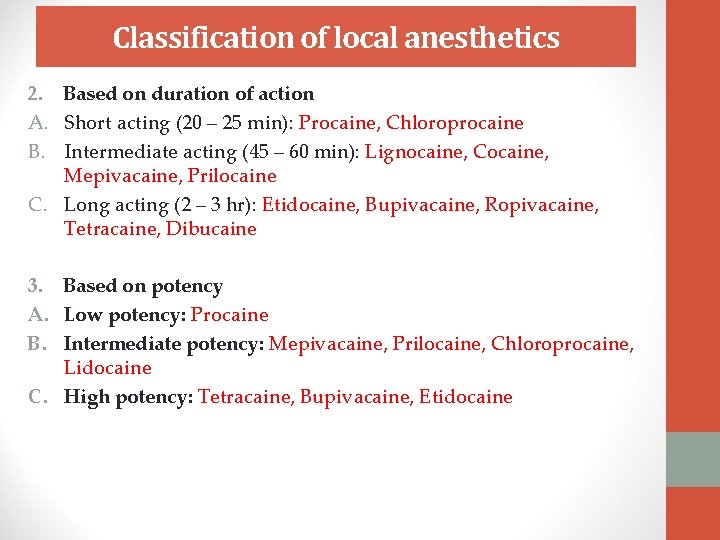
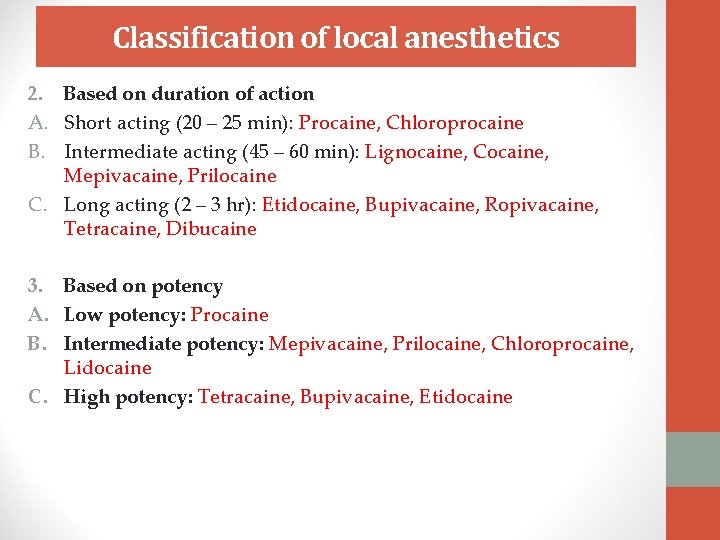
Classification of local anesthetics 2. Based on duration of action A. Short acting (20 – 25 min): Procaine, Chloroprocaine B. Intermediate acting (45 – 60 min): Lignocaine, Cocaine, Mepivacaine, Prilocaine C. Long acting (2 – 3 hr): Etidocaine, Bupivacaine, Ropivacaine, Tetracaine, Dibucaine 3. Based on potency A. Low potency: Procaine B. Intermediate potency: Mepivacaine, Prilocaine, Chloroprocaine, Lidocaine C. High potency: Tetracaine, Bupivacaine, Etidocaine
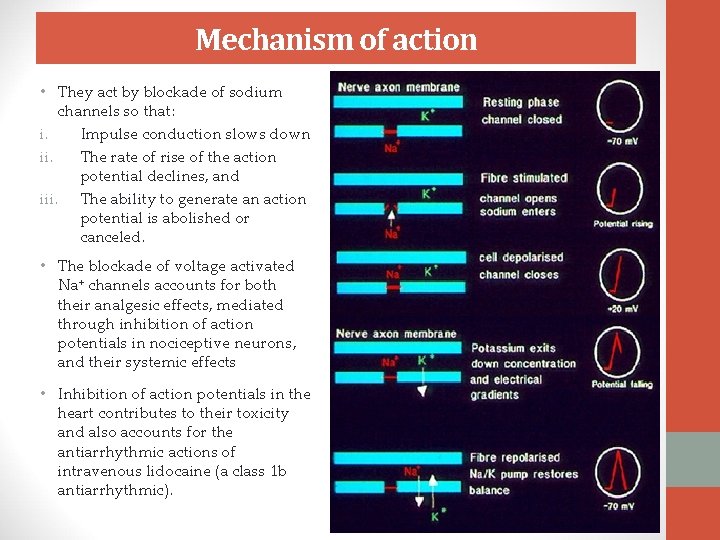
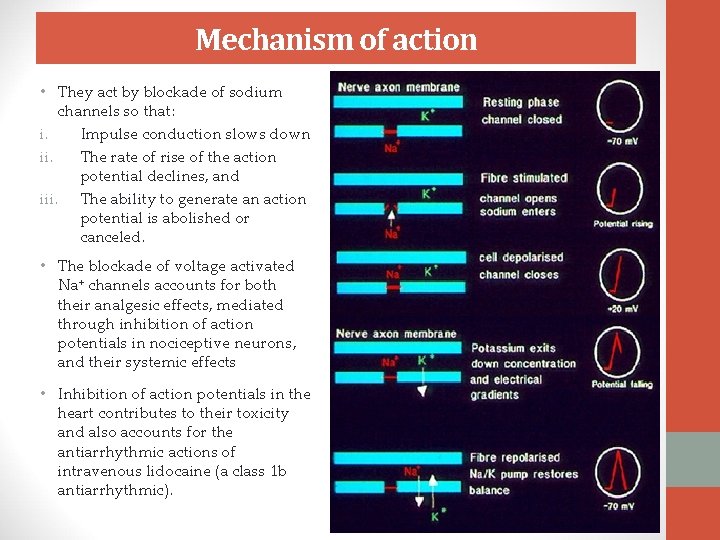
Mechanism of action • They act by blockade of sodium channels so that: i. Impulse conduction slows down ii. The rate of rise of the action potential declines, and iii. The ability to generate an action potential is abolished or canceled. • The blockade of voltage activated Na+ channels accounts for both their analgesic effects, mediated through inhibition of action potentials in nociceptive neurons, and their systemic effects • Inhibition of action potentials in the heart contributes to their toxicity and also accounts for the antiarrhythmic actions of intravenous lidocaine (a class 1 b antiarrhythmic).
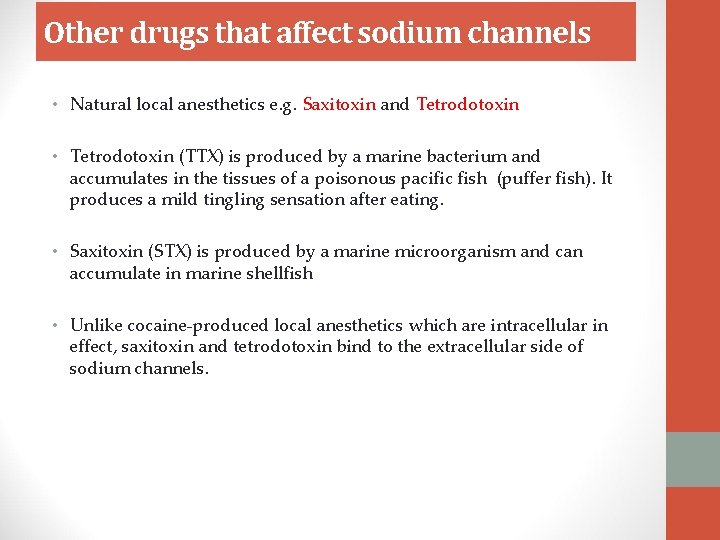
Other drugs that affect sodium channels • Natural local anesthetics e. g. Saxitoxin and Tetrodotoxin • Tetrodotoxin (TTX) is produced by a marine bacterium and accumulates in the tissues of a poisonous pacific fish (puffer fish). It produces a mild tingling sensation after eating. • Saxitoxin (STX) is produced by a marine microorganism and can accumulate in marine shellfish • Unlike cocaine-produced local anesthetics which are intracellular in effect, saxitoxin and tetrodotoxin bind to the extracellular side of sodium channels.
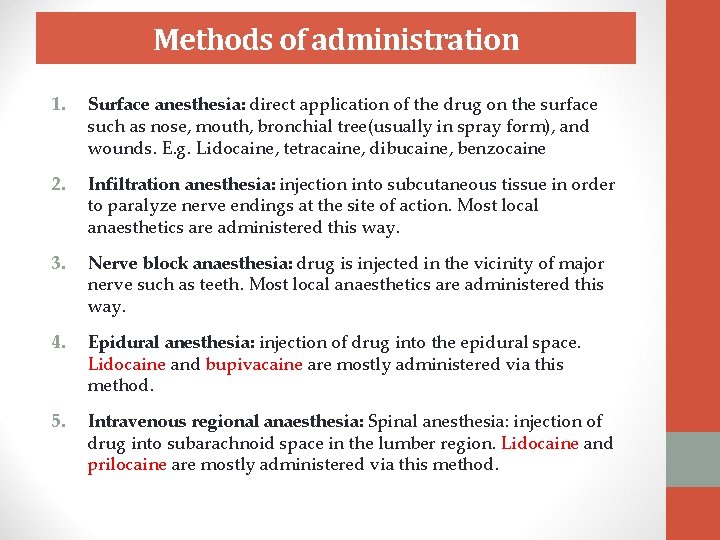
Methods of administration 1. Surface anesthesia: direct application of the drug on the surface such as nose, mouth, bronchial tree(usually in spray form), and wounds. E. g. Lidocaine, tetracaine, dibucaine, benzocaine 2. Infiltration anesthesia: injection into subcutaneous tissue in order to paralyze nerve endings at the site of action. Most local anaesthetics are administered this way. 3. Nerve block anaesthesia: drug is injected in the vicinity of major nerve such as teeth. Most local anaesthetics are administered this way. 4. Epidural anesthesia: injection of drug into the epidural space. Lidocaine and bupivacaine are mostly administered via this method. 5. Intravenous regional anaesthesia: Spinal anesthesia: injection of drug into subarachnoid space in the lumber region. Lidocaine and prilocaine are mostly administered via this method.