Genera Bacillus Corynebacterium Listeria Legionella Genera Mycobacterium Chapter
Genera Bacillus Corynebacterium Listeria Legionella Genera Mycobacterium Chapter 11, 12, 23 2013/14/15
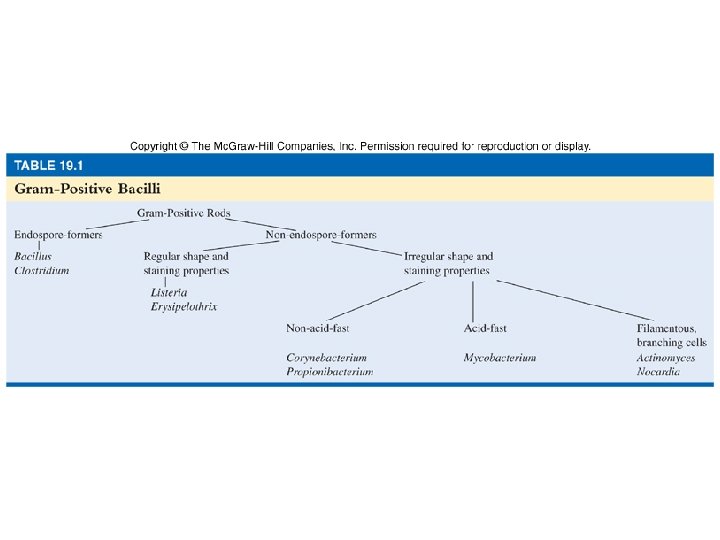
Spore-forming Bacilli Genus Bacillus - aerobes Genus Clostridium - anaerobes
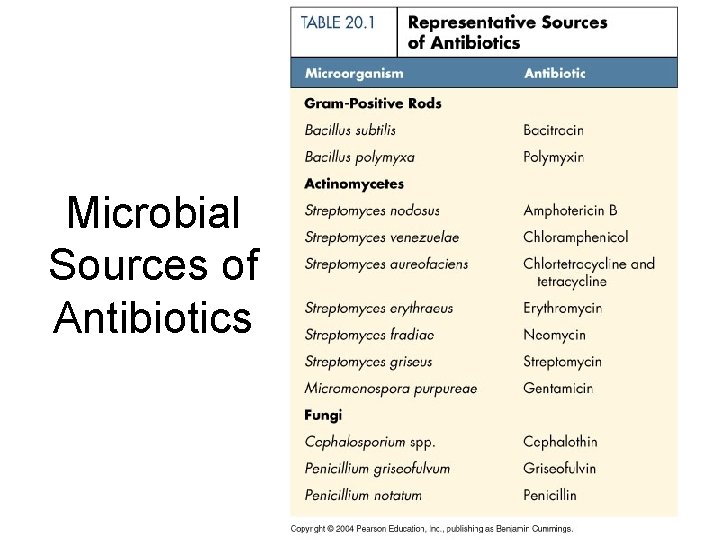
Microbial Sources of Antibiotics
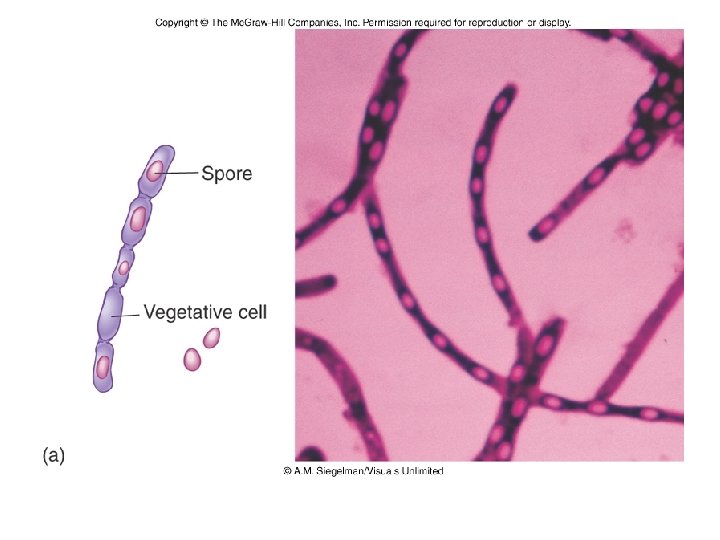
General Characteristics of the Genus Bacillus • gram-positive large aerobic, endosporeforming, motile rods • mostly saprophytic in soil, water, air • catalase positive • source of antibiotics • 2 species of medical importance: – Bacillus anthracis – Bacillus cereus
General Characteristics of the Genus Bacillus • typical rods with square ends, long chains • spores located in the center of bacilli • B. anthracis without hemolysis on BA, with round colonies with “cut glass” • B. cereus with hemolysis • Spores can be sterilized by autoclaving
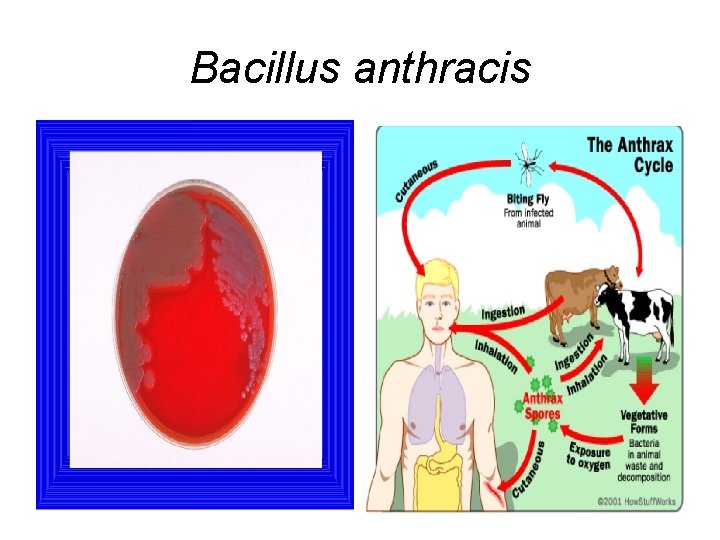
Bacillus anthracis
Bacillus anthracis • Large, block-shaped rods • Central spores that develop under all conditions except in the living body • Virulence factors – polypeptide capsule and exotoxins • 3 types of anthrax: – cutaneous – spores enter through skin, black sore-eschar; least dangerous – pulmonary –inhalation of spores – gastrointestinal – ingested spores
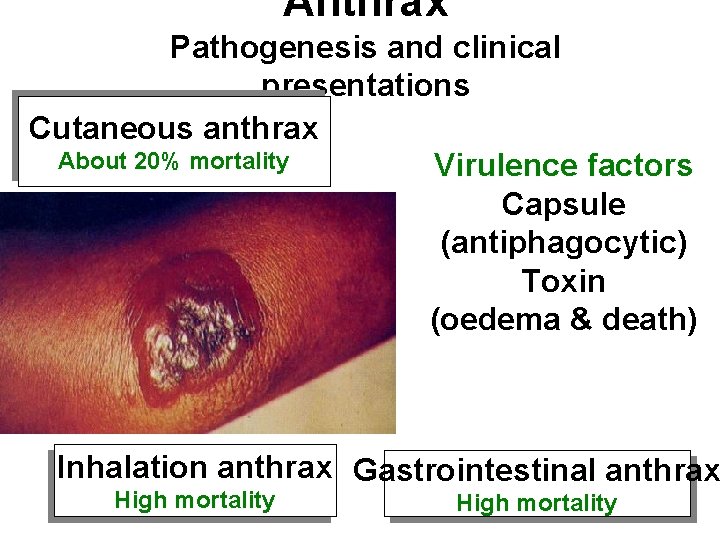
Anthrax Pathogenesis and clinical presentations Cutaneous anthrax About 20% mortality Virulence factors Capsule (antiphagocytic) Toxin (oedema & death) Inhalation anthrax Gastrointestinal anthrax High mortality

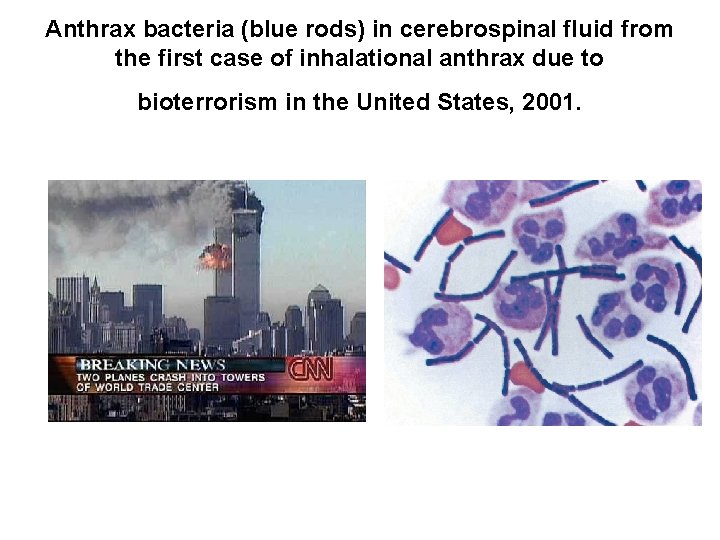
Anthrax bacteria (blue rods) in cerebrospinal fluid from the first case of inhalational anthrax due to bioterrorism in the United States, 2001.
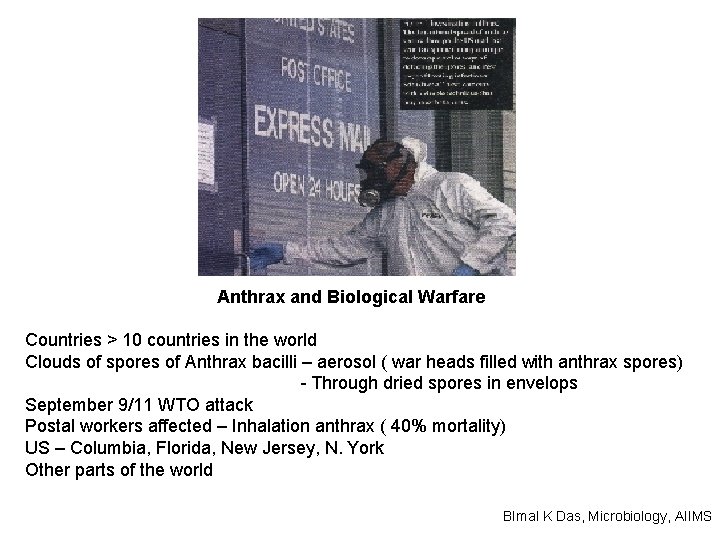
Anthrax and Biological Warfare Countries > 10 countries in the world Clouds of spores of Anthrax bacilli – aerosol ( war heads filled with anthrax spores) - Through dried spores in envelops September 9/11 WTO attack Postal workers affected – Inhalation anthrax ( 40% mortality) US – Columbia, Florida, New Jersey, N. York Other parts of the world BImal K Das, Microbiology, AIIMS

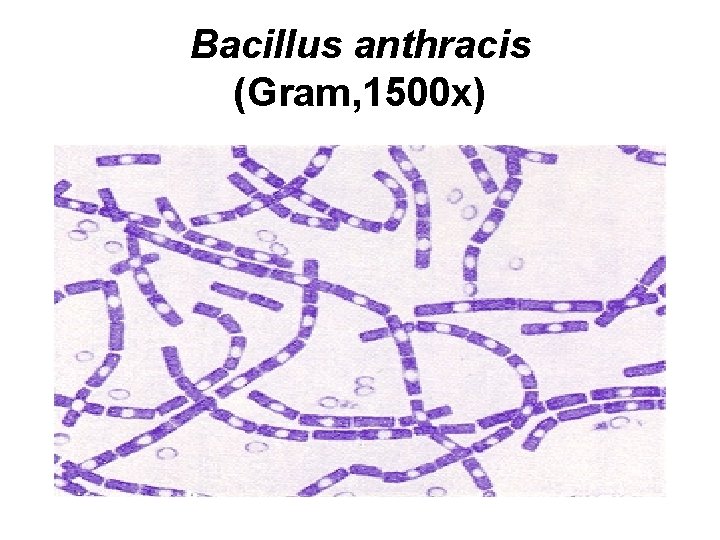
Bacillus anthracis (Gram, 1500 x)
Bacillus anthracis virulence factors • In the human body capsula made from poly-D-glutamic acid – antiphagocytic • • Antrax toxin: three proteins protective antigen PA (binding) edema factor EF (adenylat cyclase) lethal factor LF • Genes for both factors on plasmids
Infections • Incidentally by contact with infected animals or their products • Cutaneous – entry of spores in skin • Gastrointestinal – by mucous membrane • Inhalation – lung anthrax (woolsorters) • Spores germinate in the tissue, get capsule and clinical presentation
Anthrax - Diagnosis • Specimen – Aspirate or swab from cutaneous lesion – Sputum – Blood culture (sepsis) – allways! • Microbiology – Gram stain (Medusa head, curled hair) – Culture BA – Identification of isolate by molecular tests (PCR)
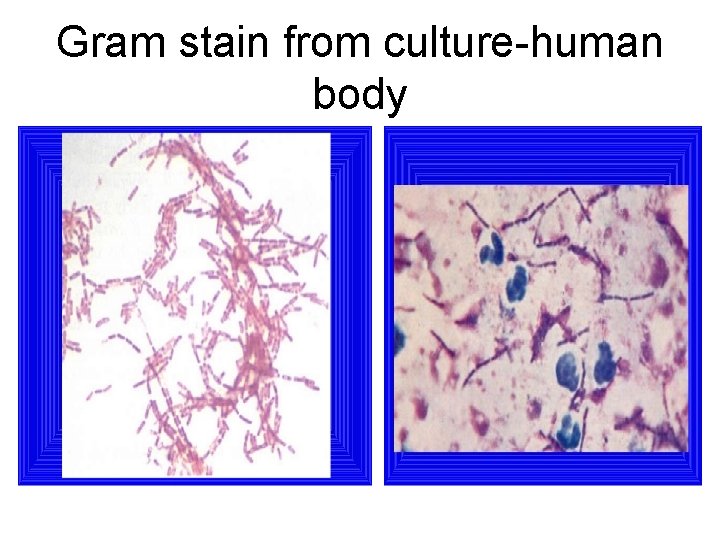
Gram stain from culture-human body
Bacillus cereus • Large, motile, saprophytic bacillus • Cause food poisoning in two forms, emetic and diarrheal type • Cause eye infections in trauma • Resistant to penicillins and cephalosporins
Bacillus cereus • Two forms of food poisoning • Pre formed heat and acid stable toxin (emetic syndrome) • Heat labile enterotoxin (diarrhoeal disease) • Lab diagnosis – demonstation of large number of bacilli in food
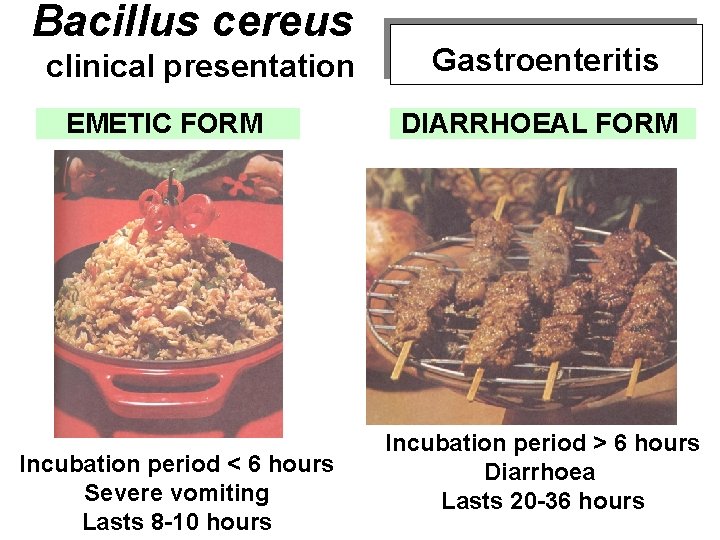
Bacillus cereus clinical presentation EMETIC FORM Incubation period < 6 hours Severe vomiting Lasts 8 -10 hours Gastroenteritis DIARRHOEAL FORM Incubation period > 6 hours Diarrhoea Lasts 20 -36 hours

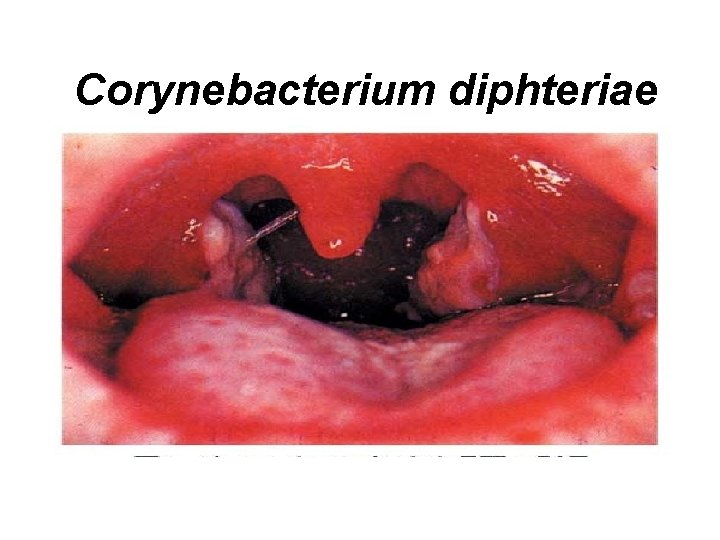
Corynebacterium diphteriae
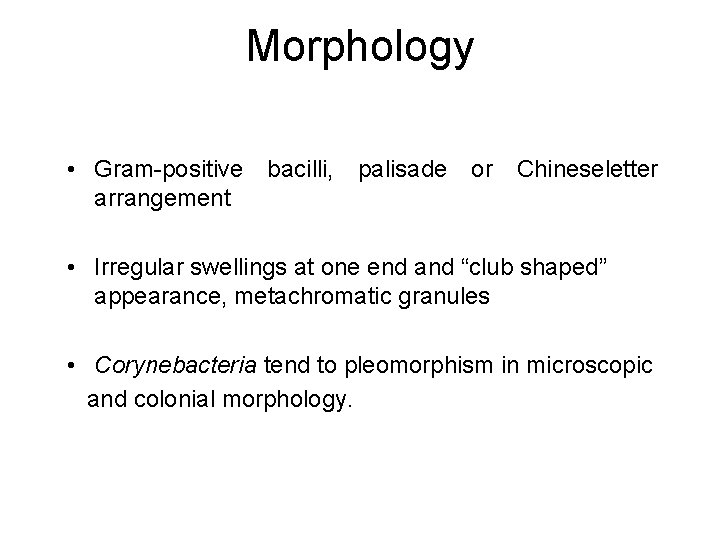
Morphology • Gram-positive bacilli, palisade or Chineseletter arrangement • Irregular swellings at one end and “club shaped” appearance, metachromatic granules • Corynebacteria tend to pleomorphism in microscopic and colonial morphology.
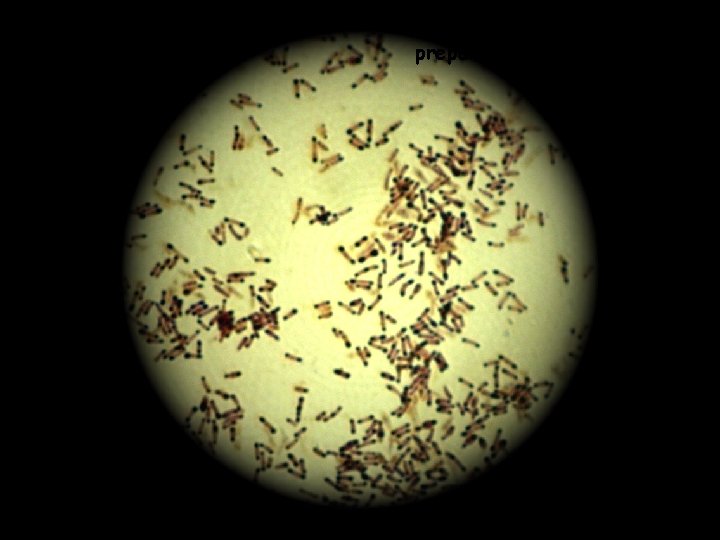
Corynebacterium diphtheriae preparat po Lubinskom
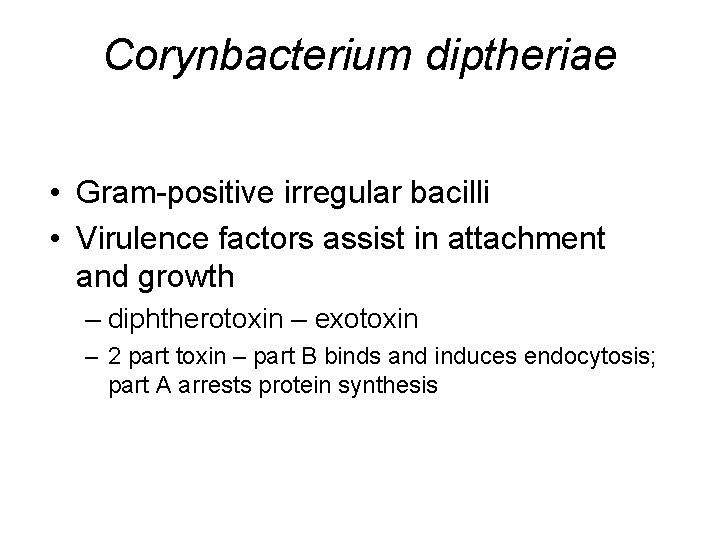
Corynbacterium diptheriae • Gram-positive irregular bacilli • Virulence factors assist in attachment and growth – diphtherotoxin – exotoxin – 2 part toxin – part B binds and induces endocytosis; part A arrests protein synthesis
Corynebacterium diphtheriae Normal flora of nasopharynx in about 10% Diphtheria caused ONLY when infected by lysogenic bacteriophage Diptheroids – Normal flora of skin – Usual contaminants of samples – Can cause disease in ‘compromised’ host C. ulcerans, C. haemolyticum, C. jeikeium
Corynbacterium diptheriae • Reservoir of healthy carriers; potential for diphtheria is always present • Causes localized inflammation (pseudomembrane, greyish white exudate ) and generalized toxaemia • Acquired via respiratory droplets from carriers or actively infected individuals
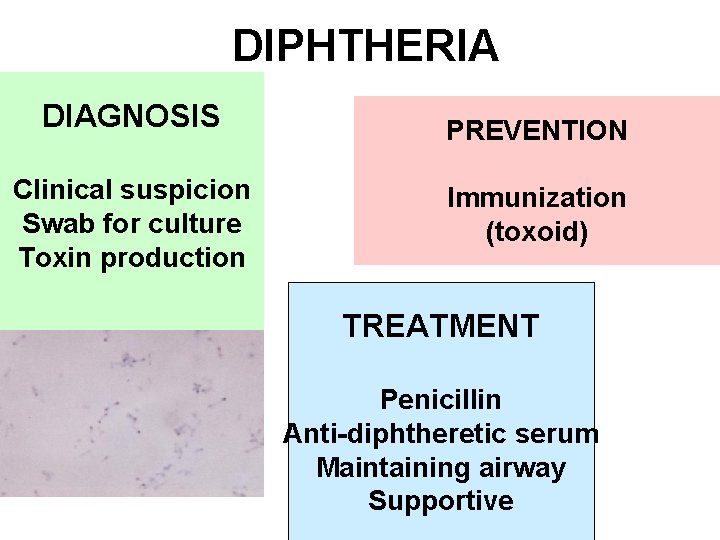
DIPHTHERIA DIAGNOSIS Clinical suspicion Swab for culture Toxin production PREVENTION Immunization (toxoid) TREATMENT Penicillin Anti-diphtheretic serum Maintaining airway Supportive
Effect of toxins 1. Local: pseudomembrane may extend to larynx and cause obstruction 2. General: Toxaemia and acts on the myocardium and on motor nerves and adrenals, complications like myocarditis /polyneuropathy
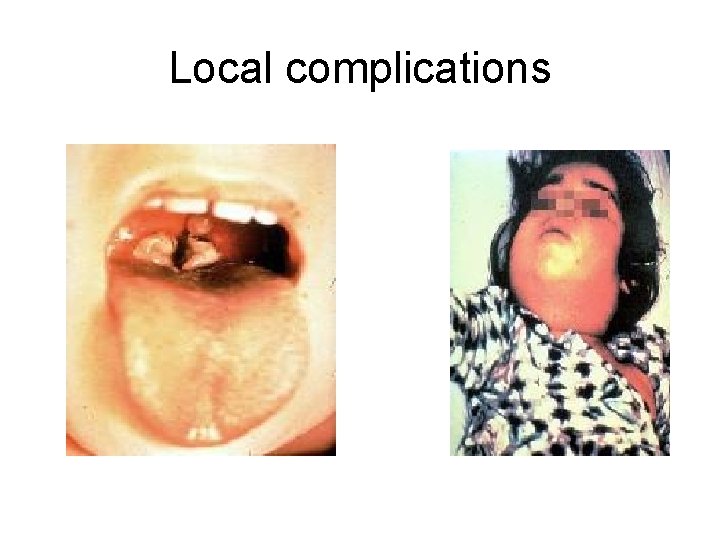
Local complications
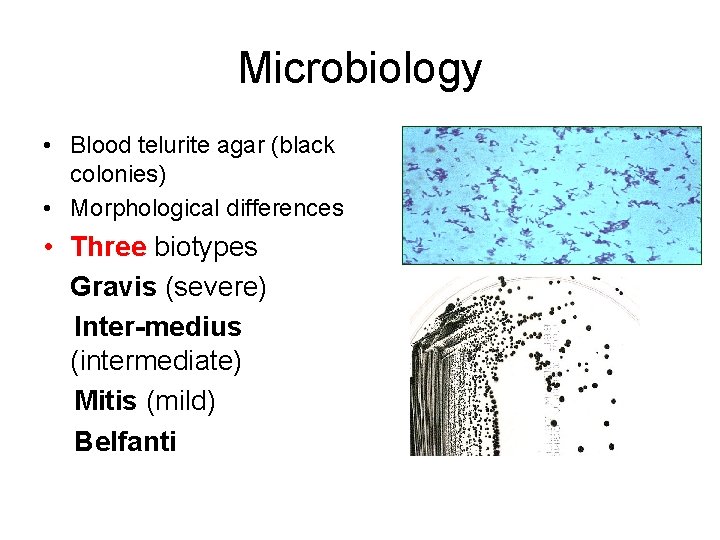
Microbiology • Blood telurite agar (black colonies) • Morphological differences • Three biotypes Gravis (severe) Inter-medius (intermediate) Mitis (mild) Belfanti
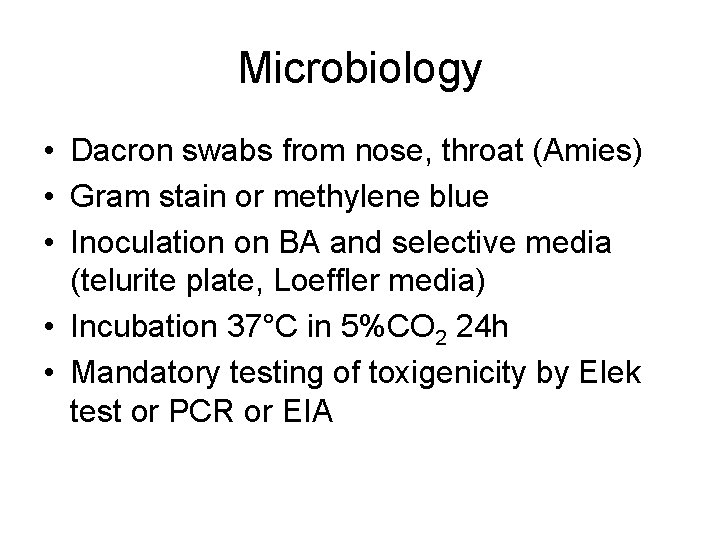
Microbiology • Dacron swabs from nose, throat (Amies) • Gram stain or methylene blue • Inoculation on BA and selective media (telurite plate, Loeffler media) • Incubation 37°C in 5%CO 2 24 h • Mandatory testing of toxigenicity by Elek test or PCR or EIA
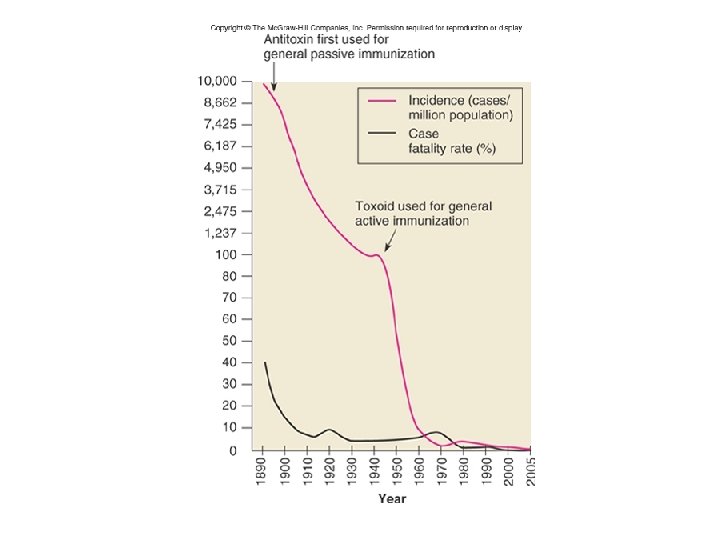
Treatment and prevention • Penicillin or erythromycin • Antitoxin in the case of clinical suspicion • Active immunisation in childhood with diphtheria toxoid (mostly in combinatiom with tetanus toxoid and pertussis -DPT)
Listeria monocytogenes
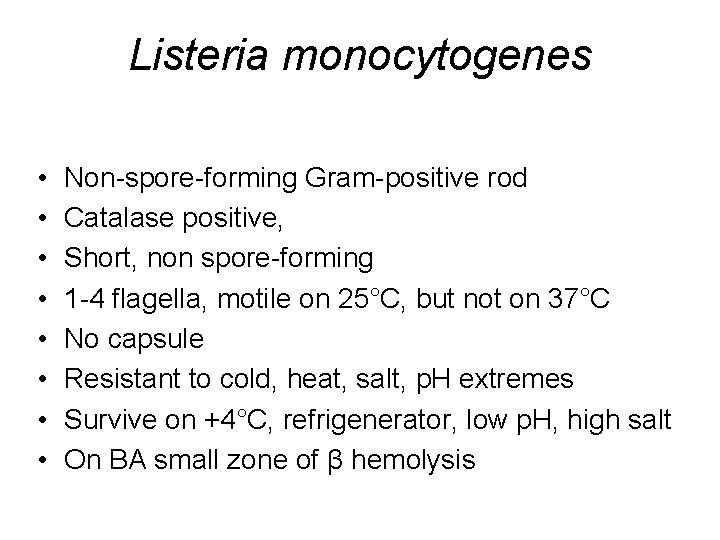
Listeria monocytogenes • • Non-spore-forming Gram-positive rod Catalase positive, Short, non spore-forming 1 -4 flagella, motile on 25°C, but not on 37°C No capsule Resistant to cold, heat, salt, p. H extremes Survive on +4°C, refrigenerator, low p. H, high salt On BA small zone of β hemolysis
Virulence factors • Adhesine proteins • Cell wall surface proteins called internalins A and B (binding to E-cadherin) • Produce listeriolysin O inside phagolysosome – disolve and escape to another cell
Epidemiology and Pathology • Primary reservoir is soil and water; animal intestines • Can contaminate foods and grow during refrigeration • Listeriosis - most cases associated with dairy products, poultry, and meat • Often mild or subclinical in normal adults • Immunocompromised patients, fetuses and neonates; affects brain and meninges – 20% death rate
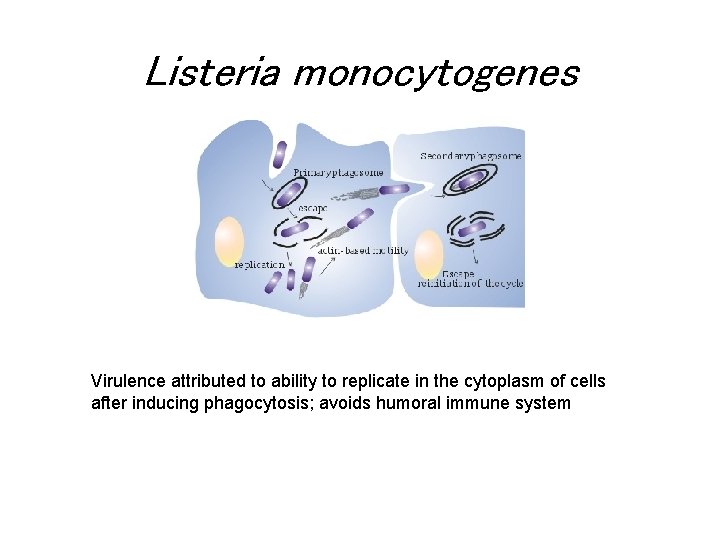
Listeria monocytogenes Virulence attributed to ability to replicate in the cytoplasm of cells after inducing phagocytosis; avoids humoral immune system
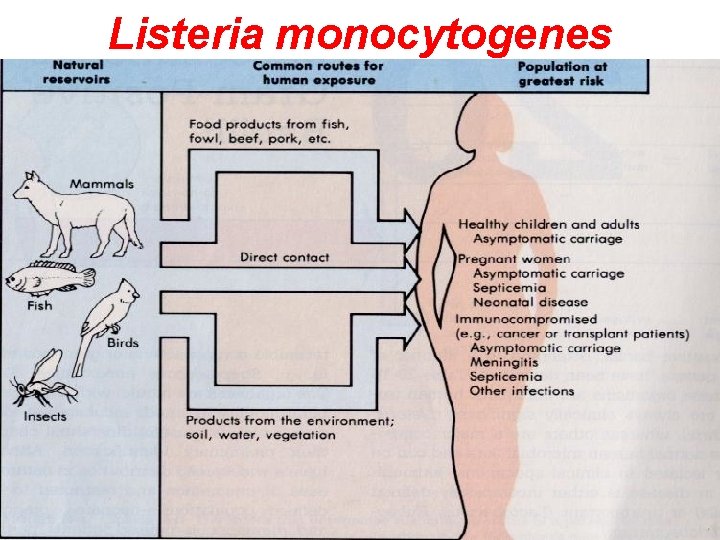
Listeria monocytogenes
Listeria monocytogenes • Treatment • ampicillin + genta /3 weeks » dd: R to cephalosporins or fluoroquinolones • Preventing measures (washing, cooking)

Legionella
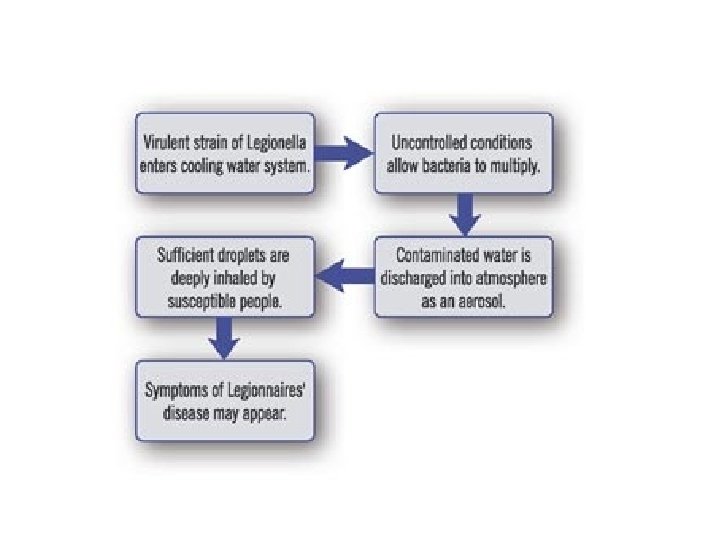
How big a risk?
Legionellae • Discovered after Legionnaires’ Conference in Philadelphia in 1976 • convention was the first major outbreak – > 200 cases of pneumonia – > 30 died • Legionnaires’ disease: severe form of pneumonia
What is Legionella? » A naturally occurring bacterium • Found in most water systems • Often present in mains water • Easily colonises most domestic water systems – hot and cold
LEGIONELLAE • • • Facultative intracellular pathogen Gram negative rod Requires specialized media to grow Stains poorly with gram stain Transmitted via contaminated aerosols No person transmission
Species of Clinical Importance • Legionella – One genus – 50 species – ½ of species implicated in human disease • Legionella pneumophila – Causes ~ 90% of all cases of legionellosis – Majority of all confirmed cases are caused by serogroups 1 -6 • Legionella micdade – Most common after L. pneumophila
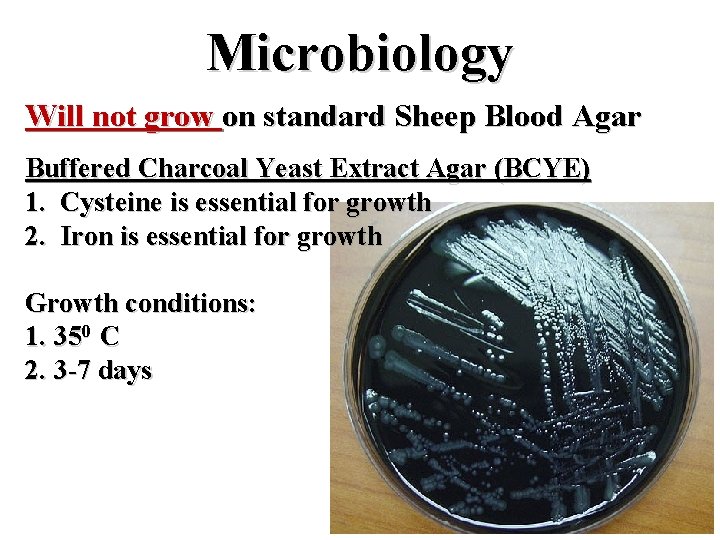
Microbiology Will not grow on standard Sheep Blood Agar Buffered Charcoal Yeast Extract Agar (BCYE) 1. Cysteine is essential for growth 2. Iron is essential for growth Growth conditions: 1. 350 C 2. 3 -7 days
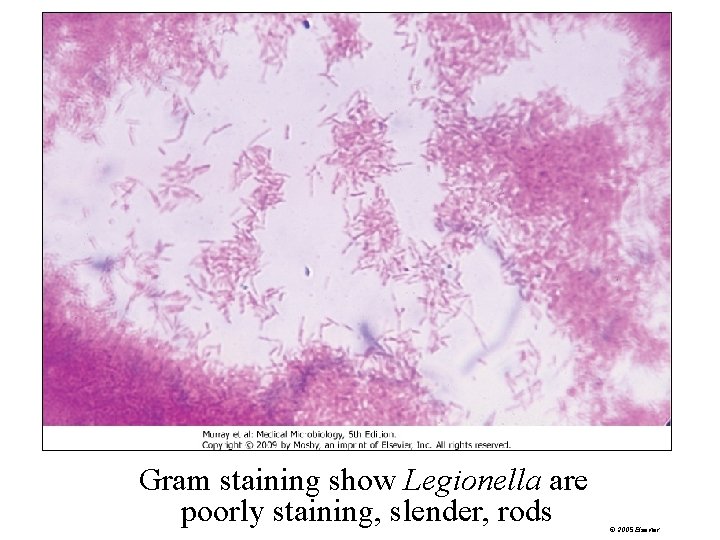
Gram staining show Legionella are poorly staining, slender, rods © 2005 Elsevier
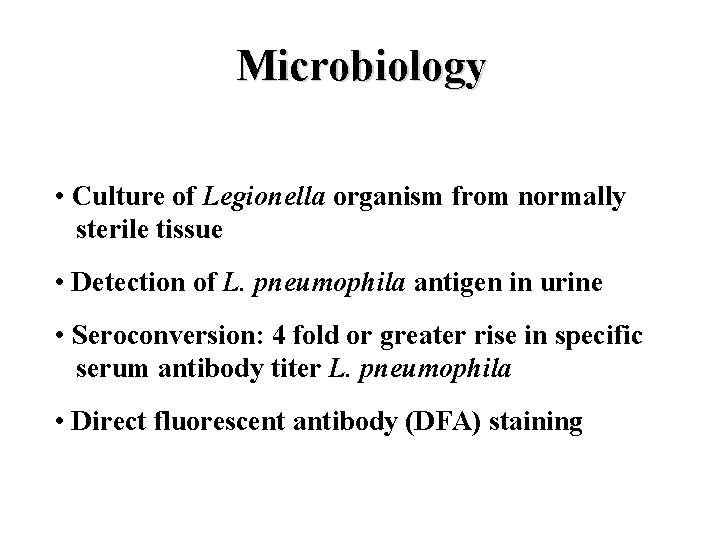
Microbiology • Culture of Legionella organism from normally sterile tissue • Detection of L. pneumophila antigen in urine • Seroconversion: 4 fold or greater rise in specific serum antibody titer L. pneumophila • Direct fluorescent antibody (DFA) staining
Legionnaires disease. Public Health • Disease - Worldwide sporadic epidemic community-acquired pneumonia nosocomial infections • Exposure - Water-based aerosols Air conditioning cooling towers Whirlpool spas sauna or mister • Survival – Environment Amoebae biofilms 54
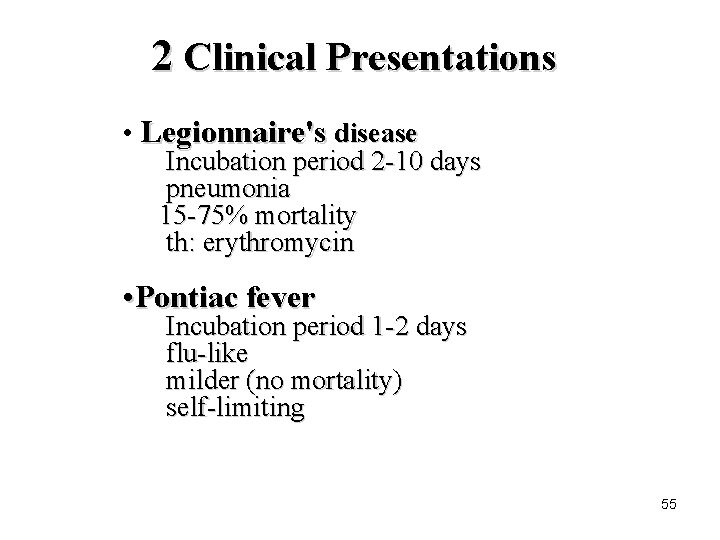
2 Clinical Presentations • Legionnaire's disease Incubation period 2 -10 days pneumonia 15 -75% mortality th: erythromycin • Pontiac fever Incubation period 1 -2 days flu-like milder (no mortality) self-limiting 55
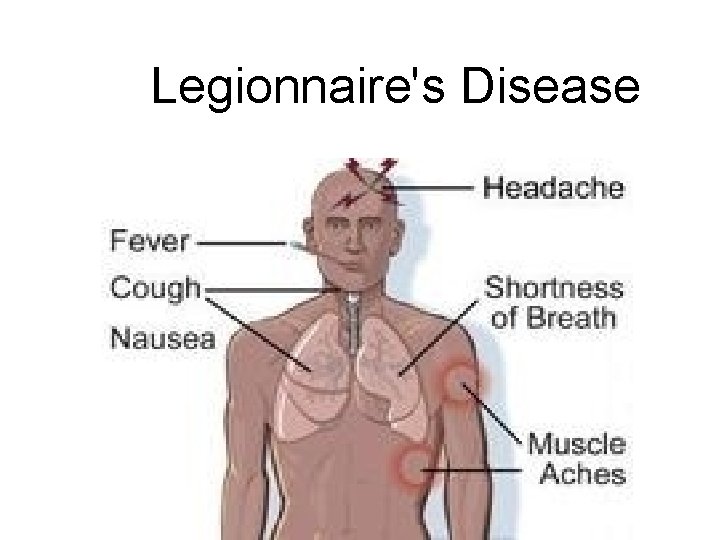
Legionnaire's Disease
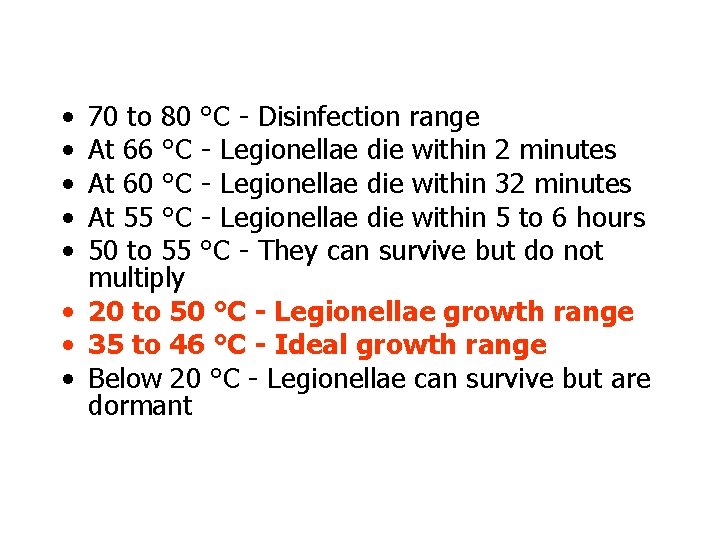
• • • 70 to 80 °C - Disinfection range At 66 °C - Legionellae die within 2 minutes At 60 °C - Legionellae die within 32 minutes At 55 °C - Legionellae die within 5 to 6 hours 50 to 55 °C - They can survive but do not multiply • 20 to 50 °C - Legionellae growth range • 35 to 46 °C - Ideal growth range • Below 20 °C - Legionellae can survive but are dormant
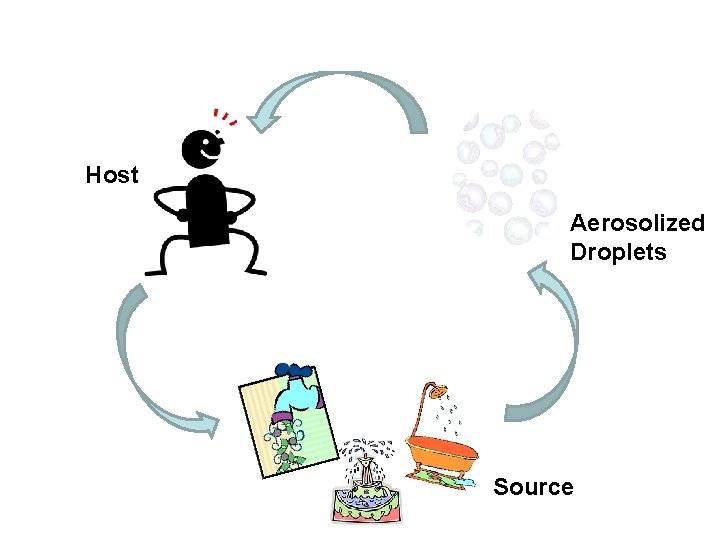
Host Aerosolized Droplets Source
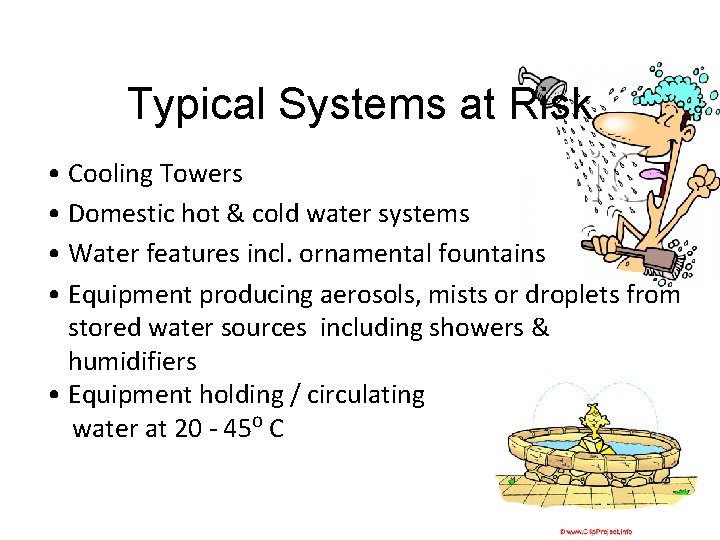
Typical Systems at Risk • Cooling Towers • Domestic hot & cold water systems • Water features incl. ornamental fountains • Equipment producing aerosols, mists or droplets from stored water sources including showers & humidifiers • Equipment holding / circulating water at 20 - 45⁰ C
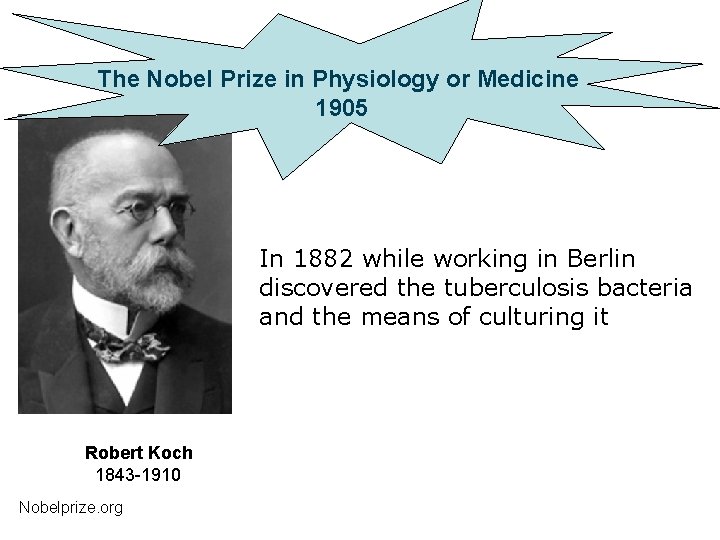
The Nobel Prize in Physiology or Medicine 1905 In 1882 while working in Berlin discovered the tuberculosis bacteria and the means of culturing it Robert Koch 1843 -1910 Nobelprize. org
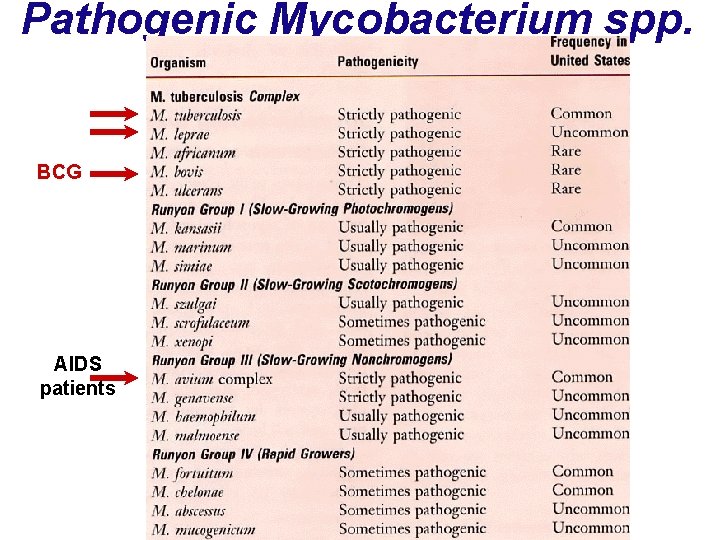
Pathogenic Mycobacterium spp. BCG AIDS patients
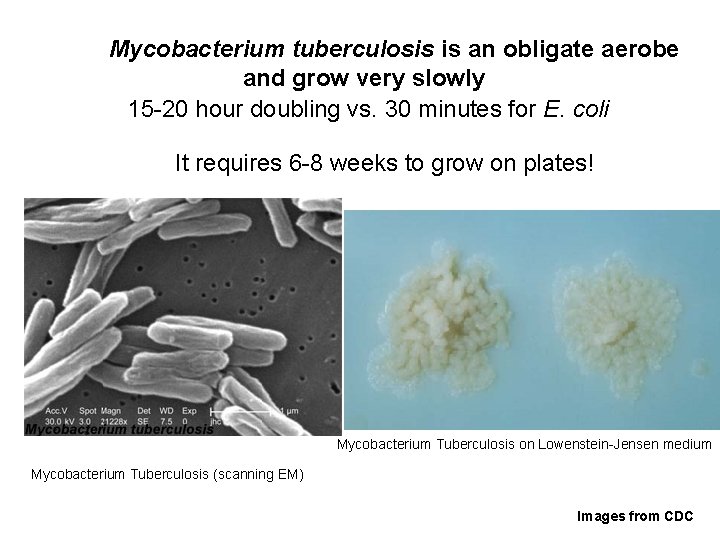
Mycobacterium tuberculosis is an obligate aerobe and grow very slowly 15 -20 hour doubling vs. 30 minutes for E. coli It requires 6 -8 weeks to grow on plates! Mycobacterium Tuberculosis on Lowenstein-Jensen medium Mycobacterium Tuberculosis (scanning EM) Images from CDC
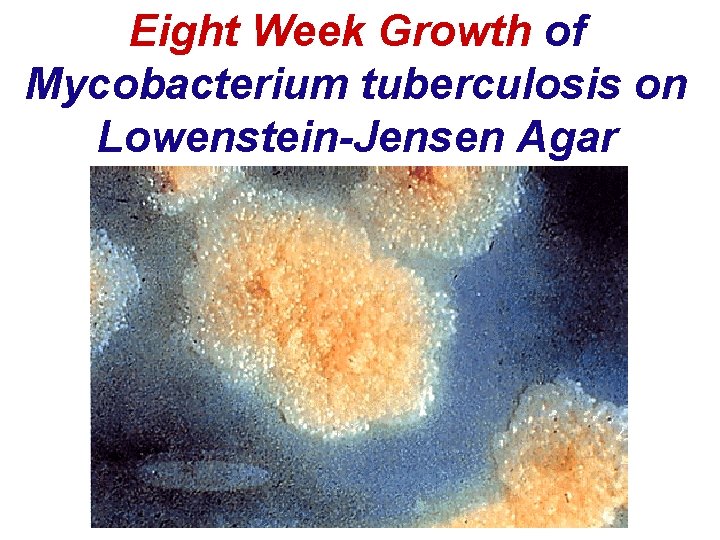
Eight Week Growth of Mycobacterium tuberculosis on Lowenstein-Jensen Agar
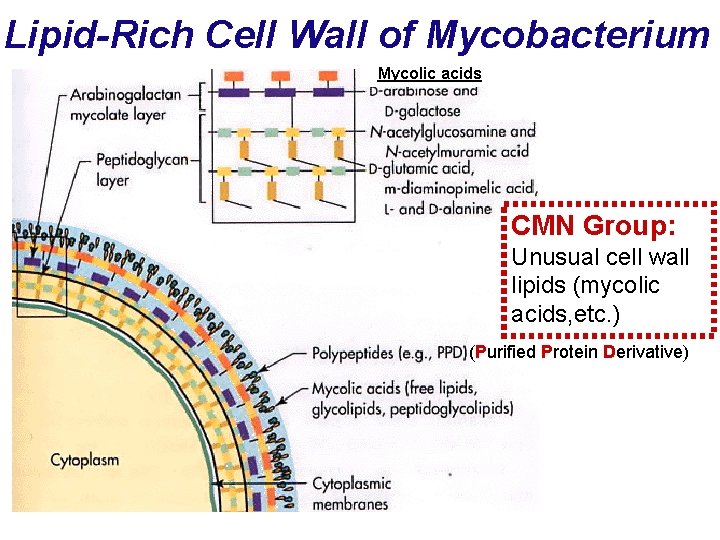
Lipid-Rich Cell Wall of Mycobacterium Mycolic acids CMN Group: Unusual cell wall lipids (mycolic acids, etc. ) (Purified Protein Derivative)
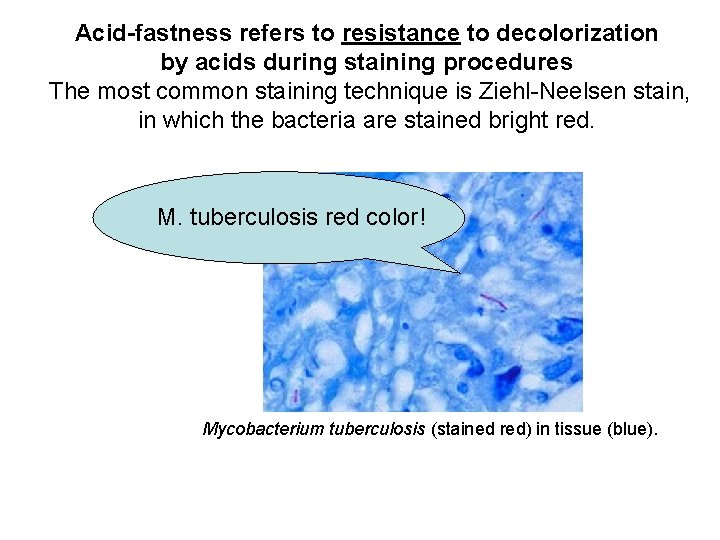
Acid-fastness refers to resistance to decolorization by acids during staining procedures The most common staining technique is Ziehl-Neelsen stain, in which the bacteria are stained bright red. M. tuberculosis red color! Mycobacterium tuberculosis (stained red) in tissue (blue).
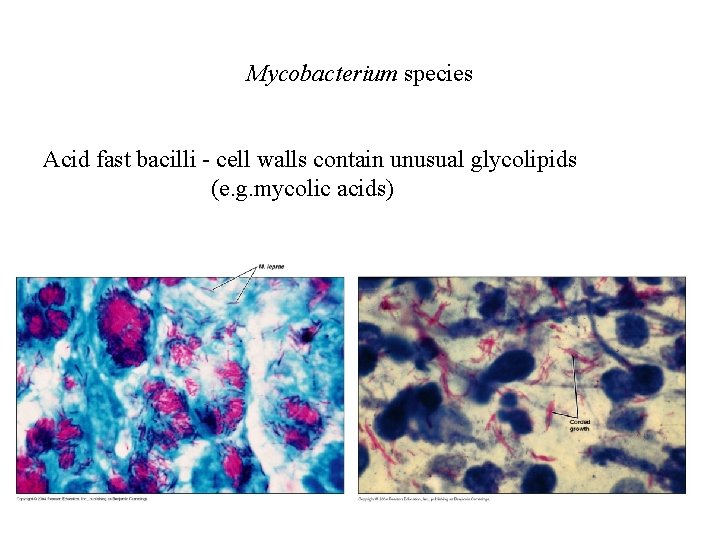
Mycobacterium species Acid fast bacilli - cell walls contain unusual glycolipids (e. g. mycolic acids)
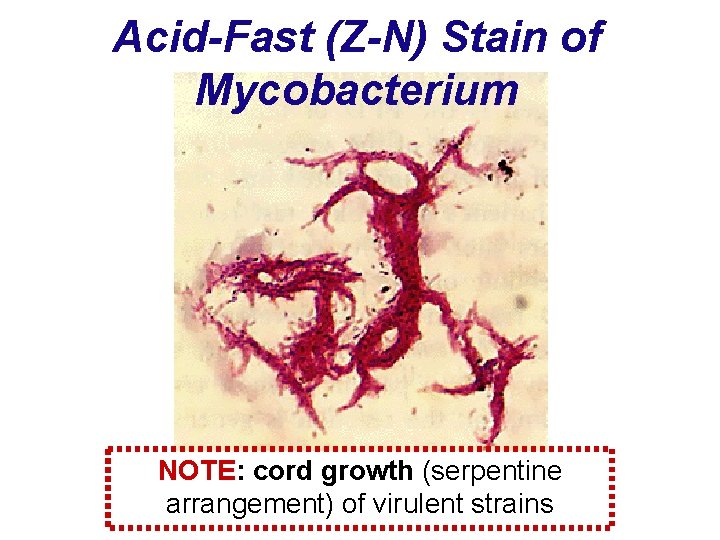
Acid-Fast (Z-N) Stain of Mycobacterium NOTE: cord growth (serpentine arrangement) of virulent strains
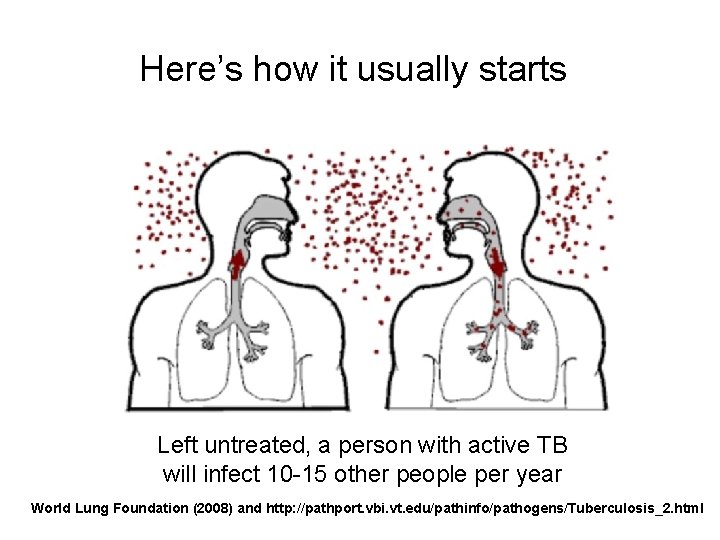
Here’s how it usually starts Left untreated, a person with active TB will infect 10 -15 other people per year World Lung Foundation (2008) and http: //pathport. vbi. vt. edu/pathinfo/pathogens/Tuberculosis_2. html
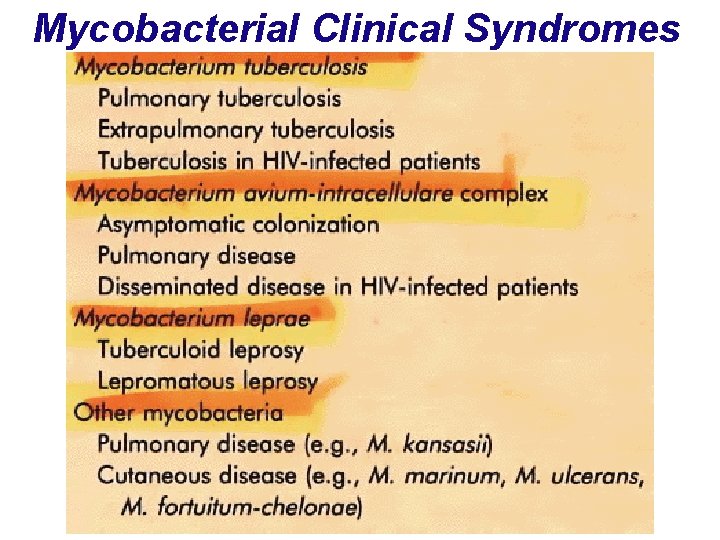
Mycobacterial Clinical Syndromes
TB Spread by aerosols Symptoms include : fever coughing (often with blood) weight loss malaise (loss of energy) progressive lung damage
Progression of TB Healthy individual exposed to low dose activated macrophages stop infection Individuals unable to mount a rapid response bacteria multiply in lung macrophages
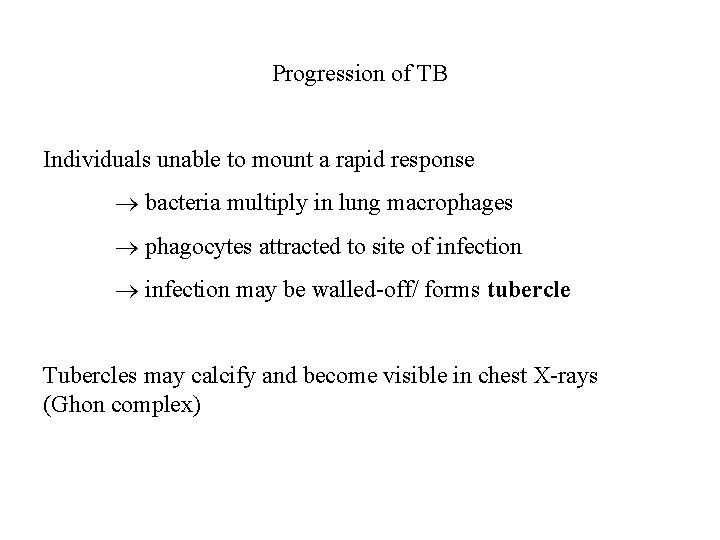
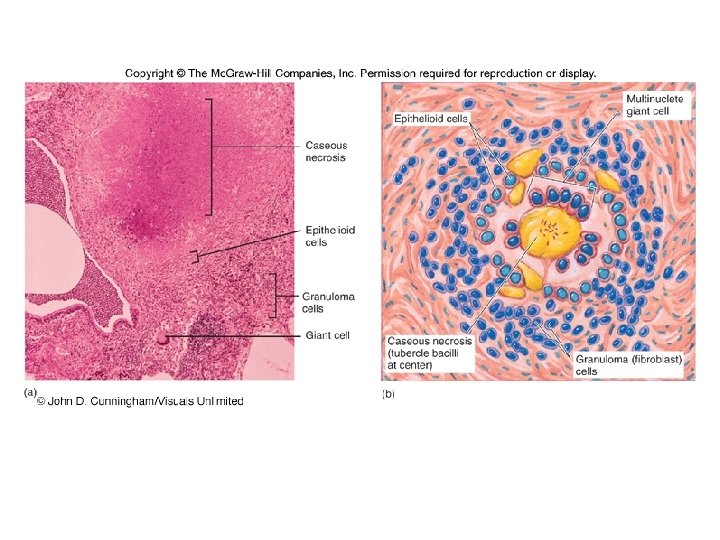
Progression of TB Individuals unable to mount a rapid response bacteria multiply in lung macrophages phagocytes attracted to site of infection may be walled-off/ forms tubercle Tubercles may calcify and become visible in chest X-rays (Ghon complex)
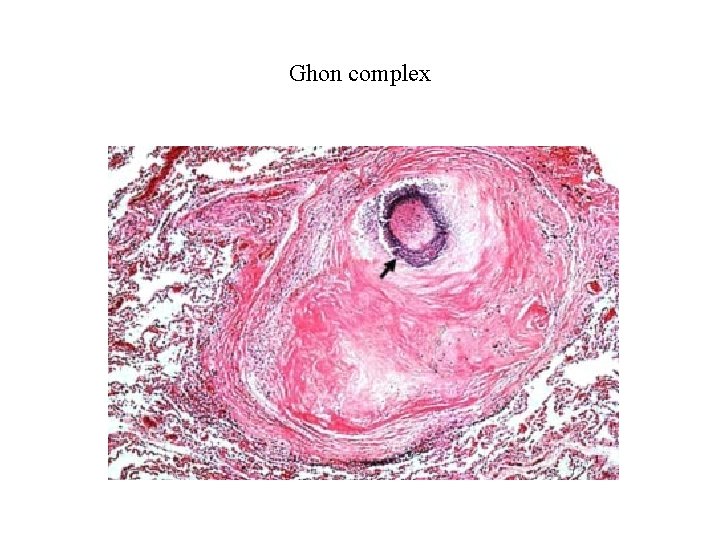
Ghon complex
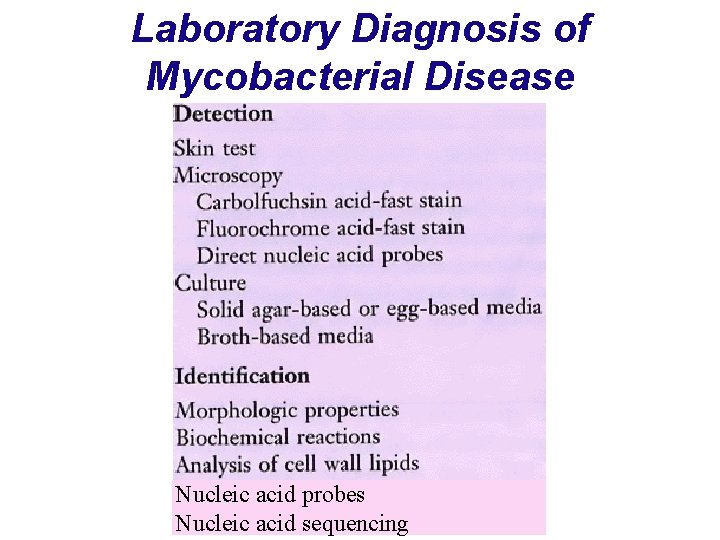
Laboratory Diagnosis of Mycobacterial Disease Nucleic acid probes Nucleic acid sequencing
Diagnosis 1. In vivo or tuberculin skin testing (TB test) Mantoux test – local intradermal injection of purified protein derivative (PPD); look for red wheal to form in 48 -72 hours- induration; established guidelines to indicate interpretation of result based on size of wheal and specific population factors Detect M. tuberculosis complex
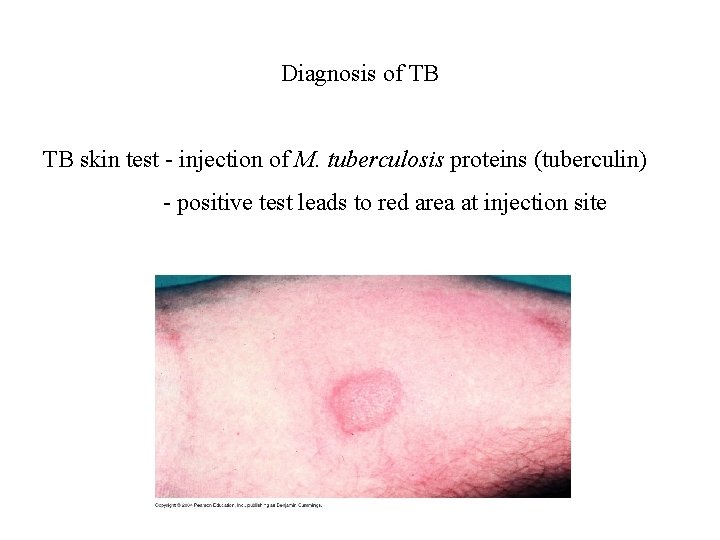
Diagnosis of TB TB skin test - injection of M. tuberculosis proteins (tuberculin) - positive test leads to red area at injection site
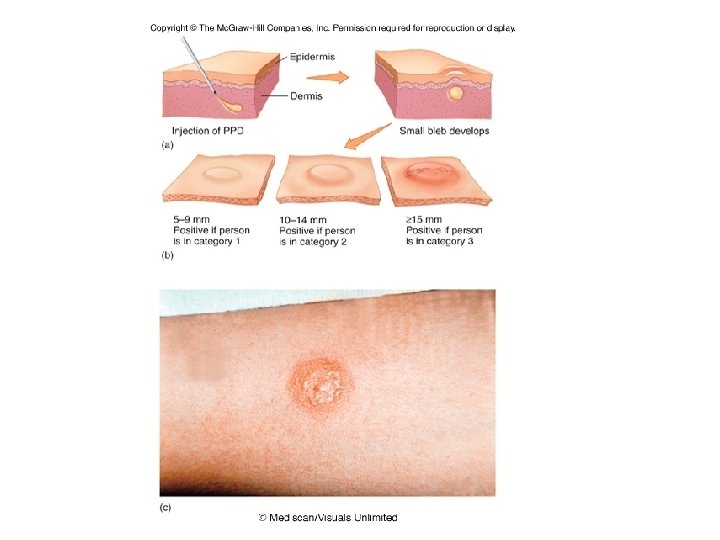
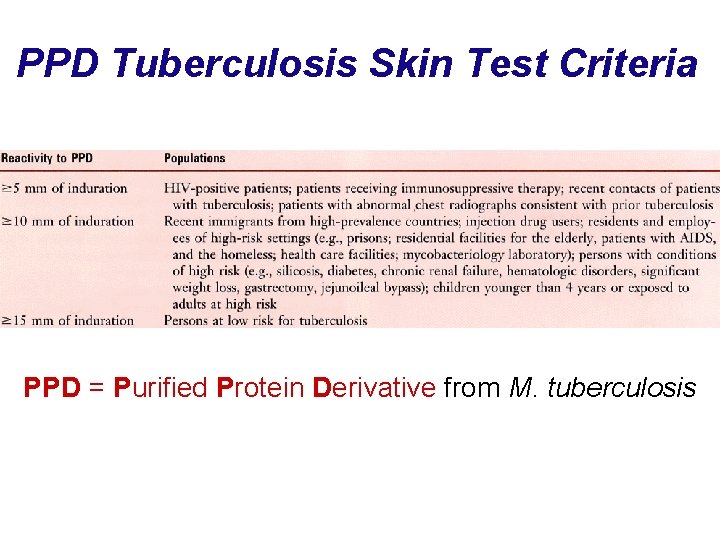
PPD Tuberculosis Skin Test Criteria PPD = Purified Protein Derivative from M. tuberculosis
IGRA – interferon gamma release assay • When tuberculin test is equivocal, screen • In vitro measure release of interferon-gamma (IFN-g) from blood as host response to M. tuberculosis • Detect specific M. tuberculosis antigens (ESAT and CFP)
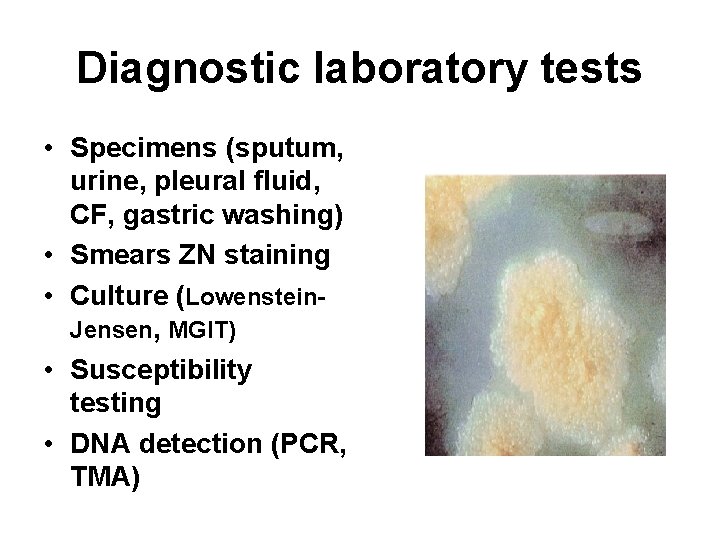
Diagnostic laboratory tests • Specimens (sputum, urine, pleural fluid, CF, gastric washing) • Smears ZN staining • Culture (Lowenstein. Jensen, MGIT) • Susceptibility testing • DNA detection (PCR, TMA)
Diagnosis 1. X rays 2. Direct identification of acid-fast bacilli in specimen 3. Cultural isolation and biochemical testing

“GOLD STANDARD” Culture (Lowenstein-Jensen, MGIT)
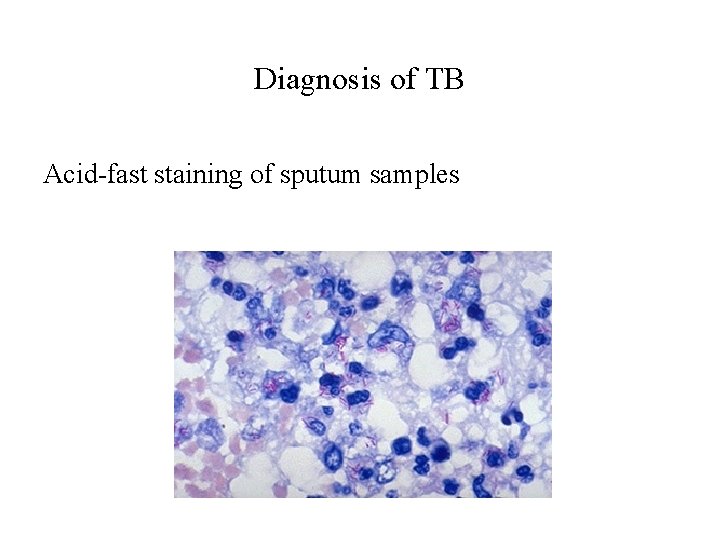
Diagnosis of TB Acid-fast staining of sputum samples
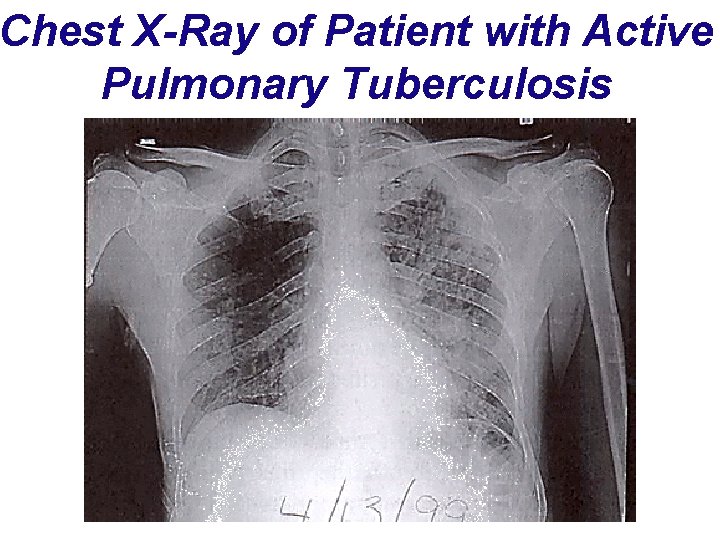
Chest X-Ray of Patient with Active Pulmonary Tuberculosis
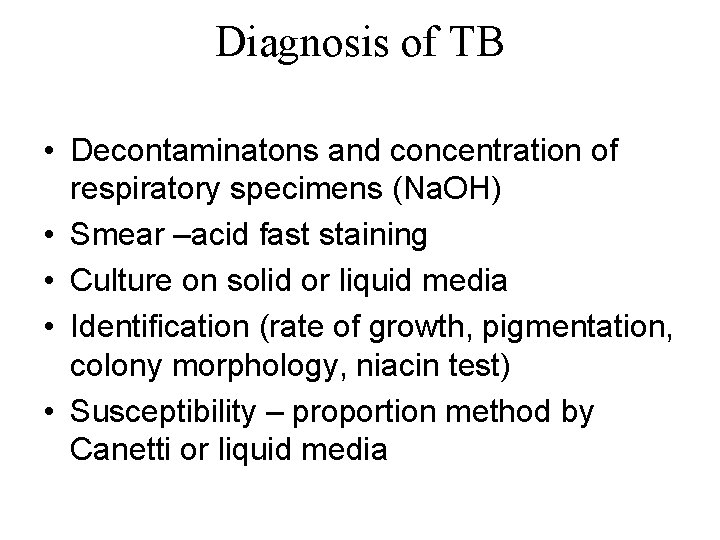
Diagnosis of TB • Decontaminatons and concentration of respiratory specimens (Na. OH) • Smear –acid fast staining • Culture on solid or liquid media • Identification (rate of growth, pigmentation, colony morphology, niacin test) • Susceptibility – proportion method by Canetti or liquid media
Treatment of TB – susceptibility test Streptomycin - first antibiotic used against M. tuberculosis - withdrow from use Ethambutol – always in combination, rapidly increase of resistance Rifampin - used to treat TB for bacterial meningitis - resistant mutants arise readily - used in combination with other drugs
M. tuberculosis specific drugs Isoniazid - isonicotinic acid hydrazide or INH - must be converted into the active form by a bacterial enzyme (catalase-peroxidase) - inhibits the formation of mycolic acid - resistance occurs by inactivation of catalaseperoxidase or by mutation of enzyme in mycolic acid synthesis pathway
M. tuberculosis specific drugs Pyrazinamide - bacterial enzyme (PZase) converts it to pyrazinoic acid (active form) - target of the drug is unknown - uptake increases under acidic conditions (vacuoles of phagocytes) - targets bacteria inside phagocytic cells - lowered activity of PZase results in resistance
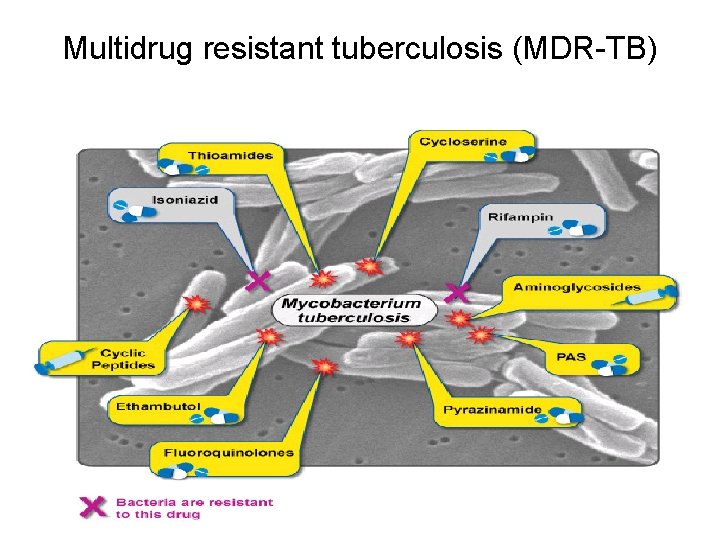
Multidrug resistant tuberculosis (MDR-TB)
Mycobacterium aviumintracellulaire Complex (MAC)
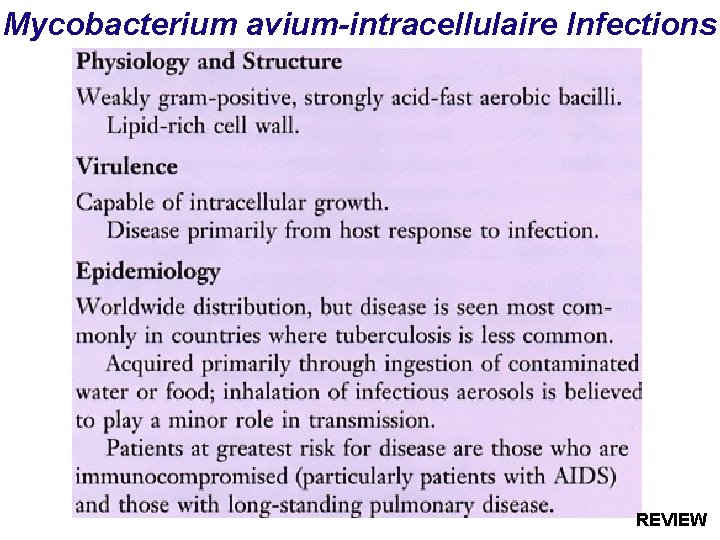
Mycobacterium avium-intracellulaire Infections REVIEW
Mycobacterium avium-intracellulaire Infections REVIEW
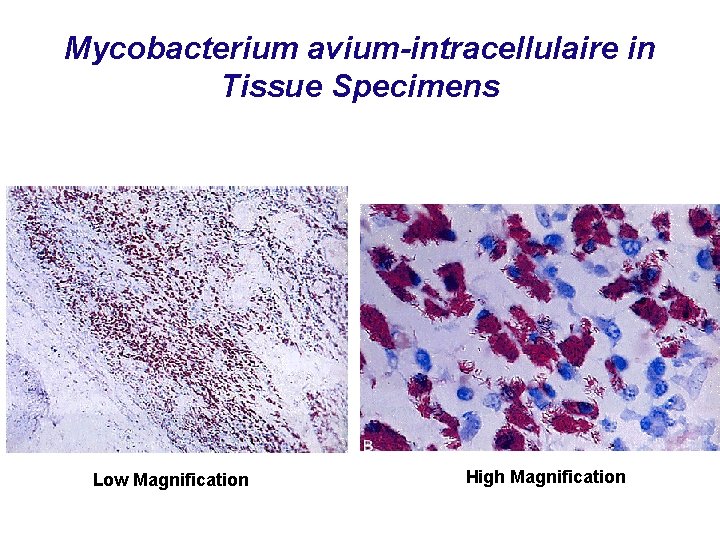
Mycobacterium avium-intracellulaire in Tissue Specimens Low Magnification High Magnification

Good luck • ivanagoicbar@net. hr • igoic@kbsplit. hr
- Slides: 96