Gender Disparity in Treatment of Coronary Artery Disease



- Slides: 19
Gender Disparity in Treatment of Coronary Artery Disease? Alexandra Lansky, M. D, FACC, FESC, FSCAI 1
DISCLOSURES Alexandra J. Lansky, MD I have no real or apparent conflicts of interest to report.
Overview Gender based statistics for cardiovascular mortality and morbidity Gender gaps in management and outcomes of stable coronary artery disease (CAD) Gender gaps in management and outcomes of ACS Gender gaps in management and outcomes of STEMI Conclusions 3
Gender-based Statistics for Cardiovascular Mortality and Morbidity Gender Gap in Management and Outcomes of Women with Coronary Artery Disease 4 © 2009 Abbott Laboratories 4
Why Should We Care About Women’s Cardiovascular Health? CAD is not just a “man’s disease” 1 52% of US population is female 2 Life expectancy of US females expected to be 81 years by 2010 2 Post menopausal women are at greater risk of CAD and today 33 M women are over 55 years of age 2 More difficult to diagnose coronary artery disease (CAD) in women 1 1. Adapted from American Heart Association, the Nurse’s Health Study. WISE and Acute Coronary Syndromes Without Chest Pain: Insights from GRACE 2. AHA Heart and stroke Stas update 2009 5

Heart Disease is the No. 1 Killer of American Women • CVD : the #1 killer in women – – – One third of all deaths in women due to CVD One woman dies of heart disease every minute CVD kills more women than men every year (since 1984) More women die of heart disease each year than all types of cancer plus other diseases combined Heart disease deaths are 11 times higher than breast cancer deaths • Poorer outcomes in women following a myocardial Infarction – Women are more likely to die within a year of myocardial infarction than their – – male counterparts Of women who survive myocardial infarction nearly half will be disabled by heart failure within six years Older age at onset and lack of awareness may contribute to poorer outcomes than men 1. AHA Heart and Stroke statistical 2009 update 6
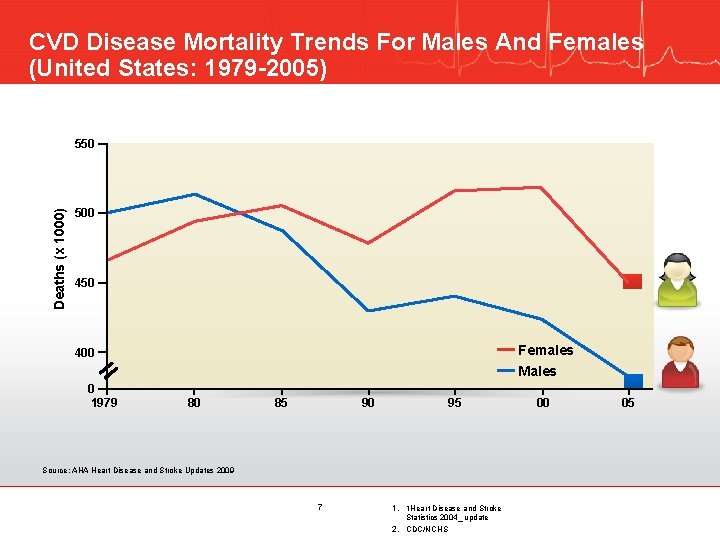
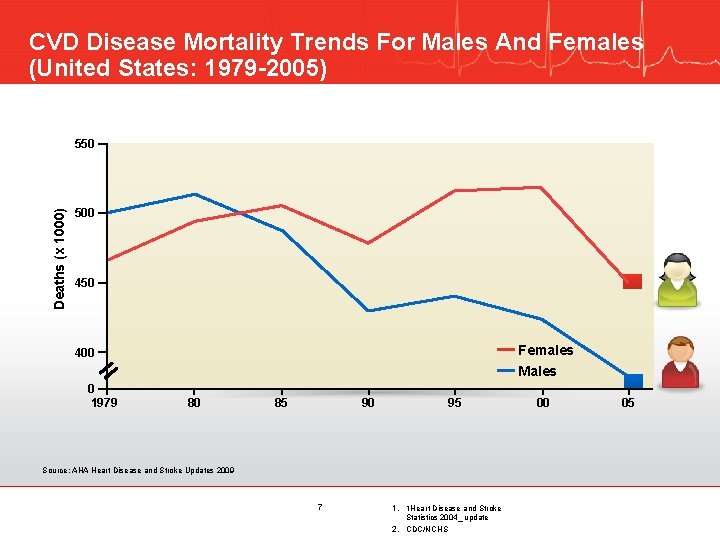
CVD Disease Mortality Trends For Males And Females (United States: 1979 -2005) Deaths (x 1000) 550 500 450 Females Males 400 0 1979 80 85 95 90 Source: AHA Heart Disease and Stroke Updates 2009 7 1. 1 Heart Disease and Stroke Statistics 2004_ update 2. CDC/NCHS 00 05
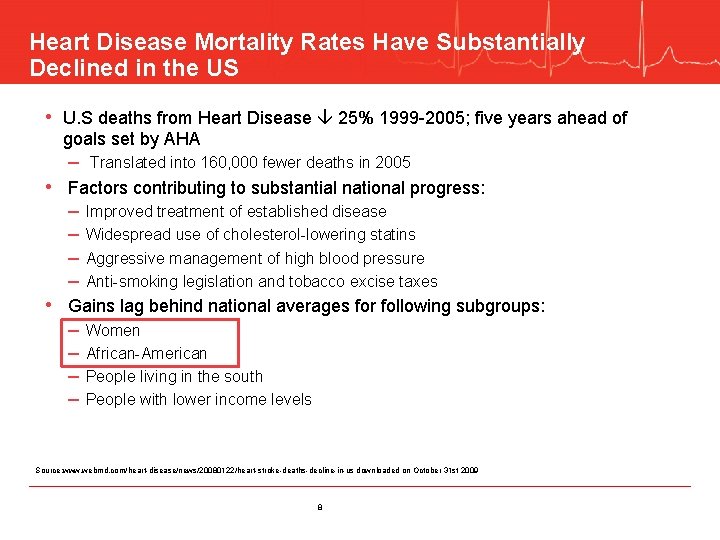
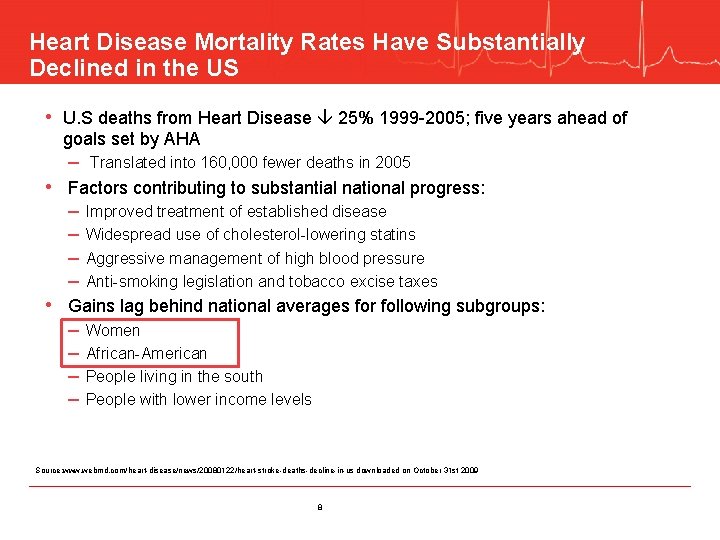
Heart Disease Mortality Rates Have Substantially Declined in the US • U. S deaths from Heart Disease 25% 1999 -2005; five years ahead of goals set by AHA – Translated into 160, 000 fewer deaths in 2005 • Factors contributing to substantial national progress: – – Improved treatment of established disease Widespread use of cholesterol-lowering statins Aggressive management of high blood pressure Anti-smoking legislation and tobacco excise taxes • Gains lag behind national averages for following subgroups: – – Women African-American People living in the south People with lower income levels Source: www. webmd. com/heart-disease/news/20080122/heart-stroke-deaths-decline-in-us downloaded on October 31 st 2009 8

Gender Gaps in Management of Coronary Artery Disease (CAD)
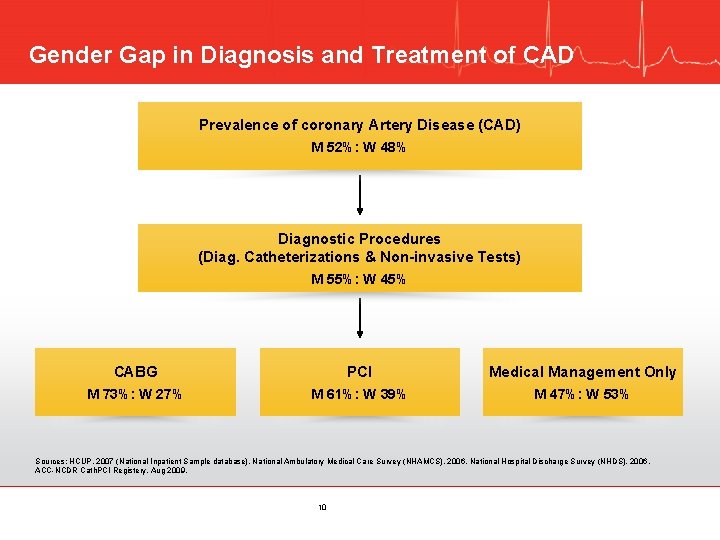
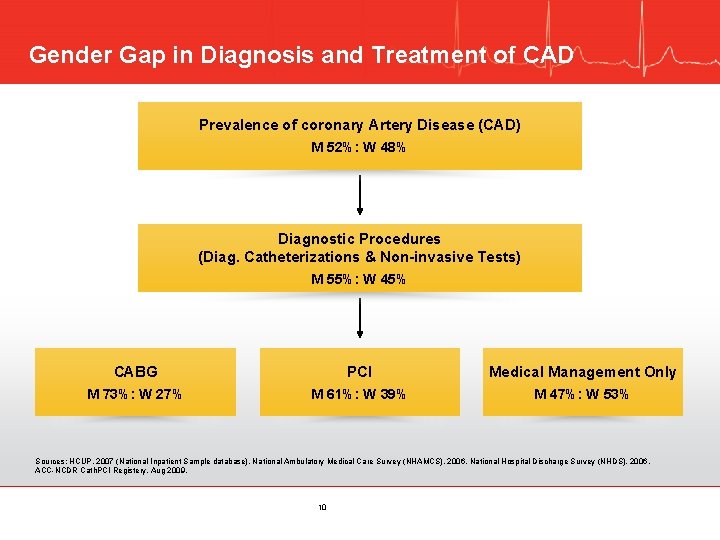
Gender Gap in Diagnosis and Treatment of CAD Prevalence of coronary Artery Disease (CAD) M 52%: W 48% Diagnostic Procedures (Diag. Catheterizations & Non-invasive Tests) M 55%: W 45% CABG PCI Medical Management Only M 73%: W 27% M 61%: W 39% M 47%: W 53% Sources: HCUP, 2007 (National Inpatient Sample database). National Ambulatory Medical Care Survey (NHAMCS), 2006. National Hospital Discharge Survey (NHDS), 2006. ACC-NCDR Cath. PCI Registery, Aug 2009. 10
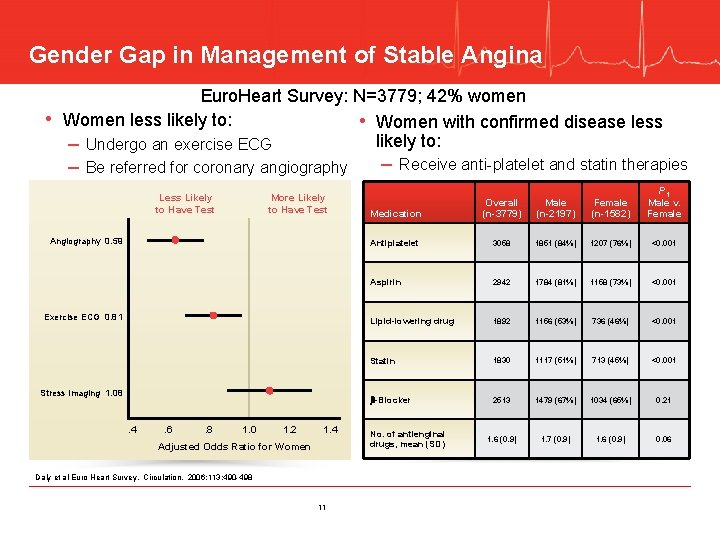
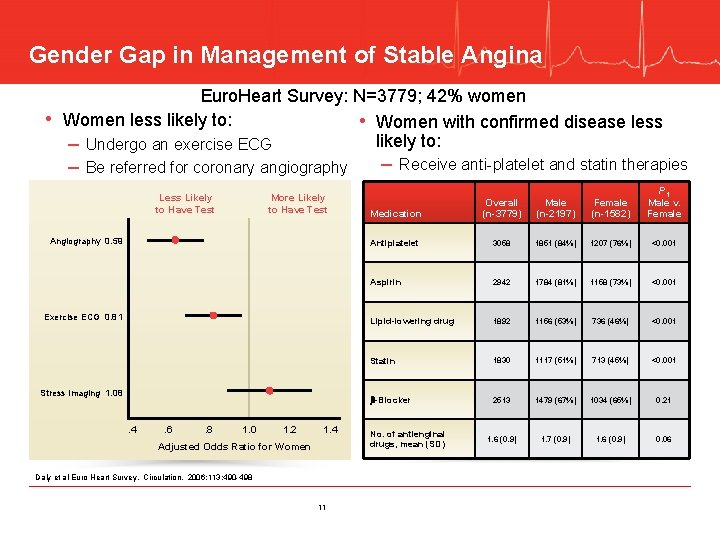
Gender Gap in Management of Stable Angina • Euro. Heart Survey: N=3779; 42% women Women less likely to: • Women with confirmed disease less likely to: – Undergo an exercise ECG – Be referred for coronary angiography Less Likely to Have Test More Likely to Have Test Angiography 0. 59 Exercise ECG 0. 81 Stress Imaging 1. 08 . 4 . 6 . 8 1. 0 1. 2 1. 4 Adjusted Odds Ratio for Women Daly et al Euro Heart Survey. Circulation. 2006: 113: 490 -498 11 – Receive anti-platelet and statin therapies Medication Overall (n-3779) Male (n-2197) Female (n-1582) P 1 Male v. Female Antiplatelet 3058 1851 (84%) 1207 (76%) <0. 001 Aspirin 2942 1784 (81%) 1158 (73%) <0. 001 Lipid-lowering drug 1892 1156 (53%) 736 (46%) <0. 001 Statin 1830 1117 (51%) 713 (45%) <0. 001 -Blocker 2513 1479 (67%) 1034 (65%) 0. 21 1. 6 (0. 9) 1. 7 (0. 9) 1. 6 (0. 9) 0. 06 No. of antienginal drugs, mean (SD)
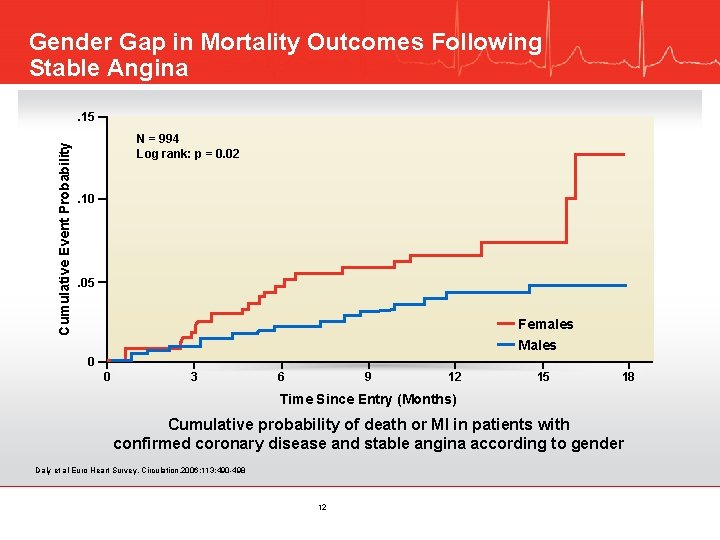
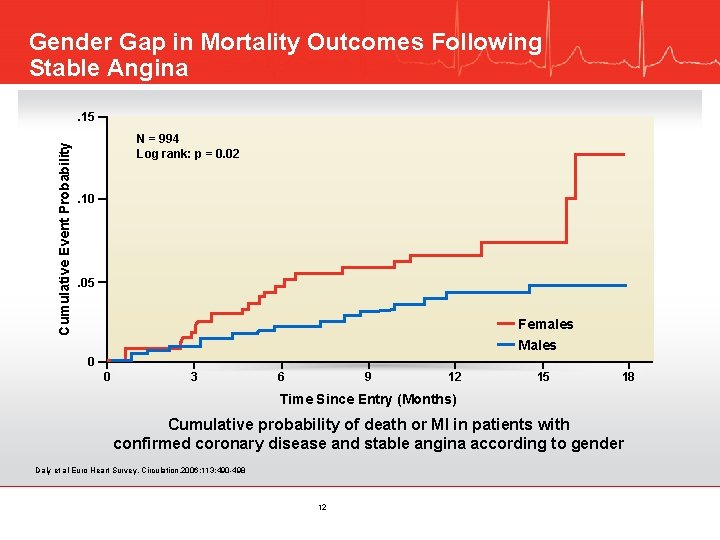
Gender Gap in Mortality Outcomes Following Stable Angina Cumulative Event Probability . 15 N = 994 Log rank: p = 0. 02 . 10 . 05 Females Males 0 0 3 6 9 12 15 18 Time Since Entry (Months) Cumulative probability of death or MI in patients with confirmed coronary disease and stable angina according to gender Daly et al Euro Heart Survey. Circulation. 2006: 113: 490 -498 12
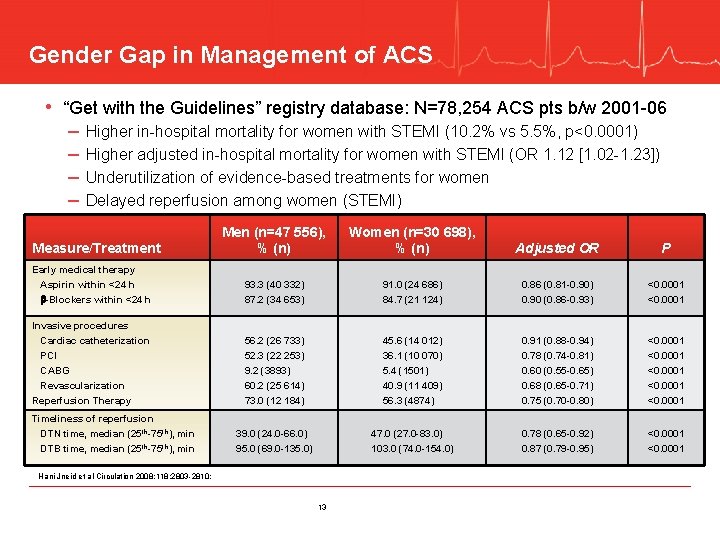
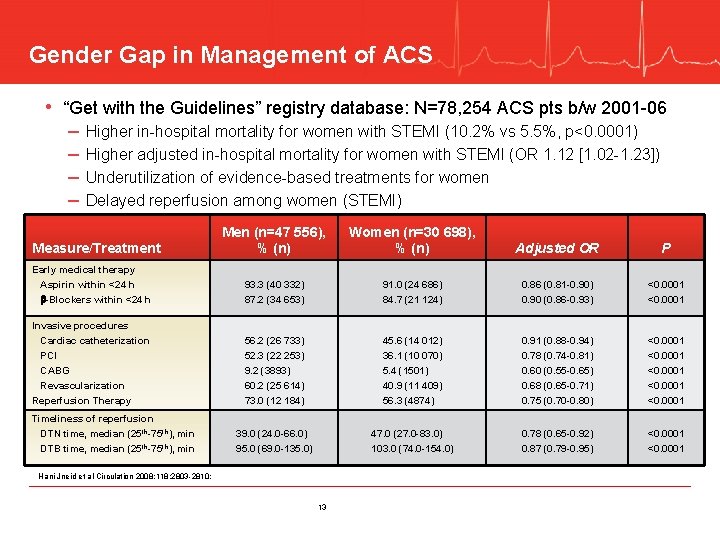
Gender Gap in Management of ACS • “Get with the Guidelines” registry database: N=78, 254 ACS pts b/w 2001 -06 – – Higher in-hospital mortality for women with STEMI (10. 2% vs 5. 5%, p<0. 0001) Higher adjusted in-hospital mortality for women with STEMI (OR 1. 12 [1. 02 -1. 23]) Underutilization of evidence-based treatments for women Delayed reperfusion among women (STEMI) Men (n=47 556), % (n) Women (n=30 698), % (n) Adjusted OR P Early medical therapy Aspirin within <24 h -Blockers within <24 h 93. 3 (40 332) 87. 2 (34 653) 91. 0 (24 686) 84. 7 (21 124) 0. 86 (0. 81 -0. 90) 0. 90 (0. 86 -0. 93) <0. 0001 Invasive procedures Cardiac catheterization PCI CABG Revascularization Reperfusion Therapy 56. 2 (26 733) 52. 3 (22 253) 9. 2 (3893) 60. 2 (25 614) 73. 0 (12 184) 45. 6 (14 012) 36. 1 (10 070) 5. 4 (1501) 40. 9 (11 409) 56. 3 (4874) 0. 91 (0. 88 -0. 94) 0. 78 (0. 74 -0. 81) 0. 60 (0. 55 -0. 65) 0. 68 (0. 65 -0. 71) 0. 75 (0. 70 -0. 80) <0. 0001 39. 0 (24. 0 -66. 0) 95. 0 (69. 0 -135. 0) 47. 0 (27. 0 -83. 0) 103. 0 (74. 0 -154. 0) 0. 78 (0. 65 -0. 92) 0. 87 (0. 79 -0. 95) <0. 0001 Measure/Treatment Timeliness of reperfusion DTN time, median (25 th-75 th), min DTB time, median (25 th-75 th), min Hani Jneid et al Circulation 2008; 118; 2803 -2810; 13
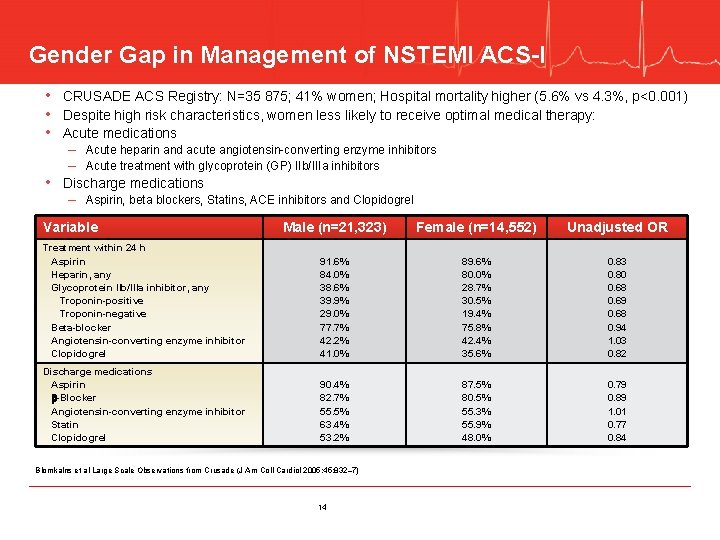
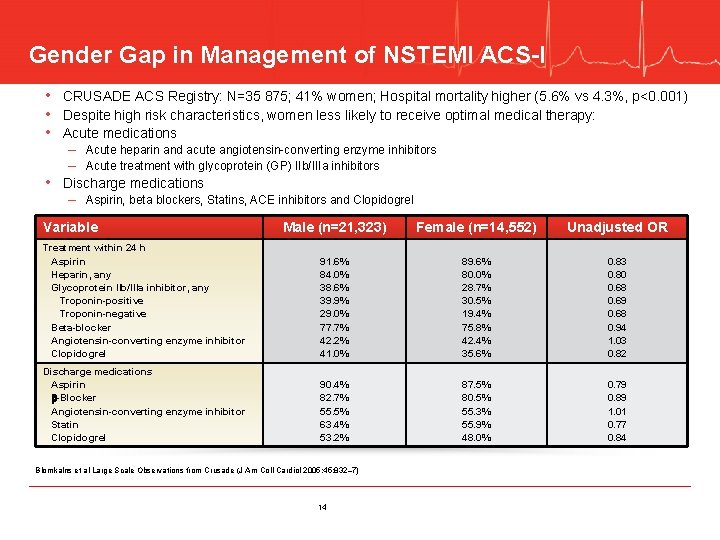
Gender Gap in Management of NSTEMI ACS-I • CRUSADE ACS Registry: N=35 875; 41% women; Hospital mortality higher (5. 6% vs 4. 3%, p<0. 001) • Despite high risk characteristics, women less likely to receive optimal medical therapy: • Acute medications – Acute heparin and acute angiotensin-converting enzyme inhibitors – Acute treatment with glycoprotein (GP) IIb/IIIa inhibitors • Discharge medications – Aspirin, beta blockers, Statins, ACE inhibitors and Clopidogrel Variable Male (n=21, 323) Female (n=14, 552) Unadjusted OR Treatment within 24 h Aspirin Heparin, any Glycoprotein IIb/IIIa inhibitor, any Troponin-positive Troponin-negative Beta-blocker Angiotensin-converting enzyme inhibitor Clopidogrel 91. 6% 84. 0% 38. 6% 39. 9% 29. 0% 77. 7% 42. 2% 41. 0% 89. 6% 80. 0% 28. 7% 30. 5% 19. 4% 75. 8% 42. 4% 35. 6% 0. 83 0. 80 0. 68 0. 69 0. 68 0. 94 1. 03 0. 82 Discharge medications Aspirin -Blocker Angiotensin-converting enzyme inhibitor Statin Clopidogrel 90. 4% 82. 7% 55. 5% 63. 4% 53. 2% 87. 5% 80. 5% 55. 3% 55. 9% 48. 0% 0. 79 0. 89 1. 01 0. 77 0. 84 Blomkalns et al Large Scale Observations from Crusade (J Am Coll Cardiol 2005; 45: 832– 7) 14

Gender Gap in Management of NSTEMI ACS-II • Despite high risk characteristics: • Women less likely to receive invasive procedures such as: – Cardiac Catheterization, PCI and CABG • Women experience greater delays in receiving diagnostic catheterization and PCI Variable Male (n=21, 323) Female (n=14, 552) Unadjusted OR Non-invasive stress testing 11. 7% 13. 2% 1. 10 Diagnostic catheterization 71. 1% 60. 1% 0. 70 Catheterization 24 h of arrival 48. 7% 42. 1% 0. 69 Percutaneous coronary intervention (PCI) PCI 24 h of arrival 40. 4% 51. 9% 31. 4% 44. 3% 0. 73 0. 64 Coronary artery bypass grafting 14. 0% 9. 0% 0. 62 Blomkalns et al Large Scale Observations from Crusade (J Am Coll Cardiol 2005; 45: 832– 7) 15
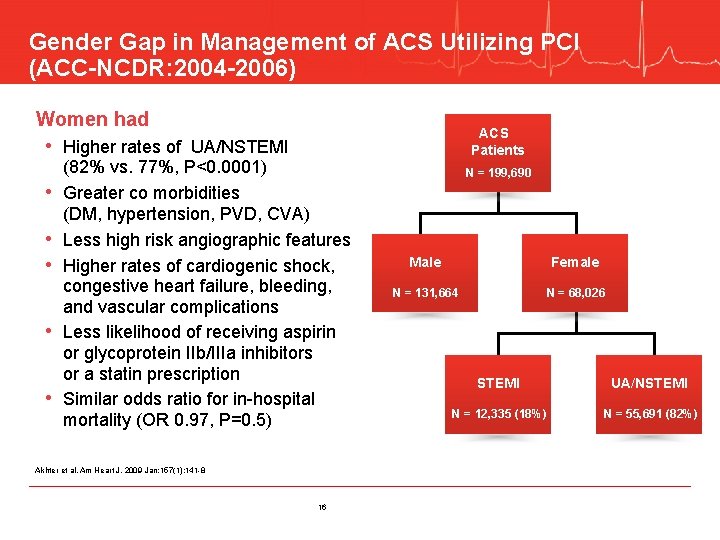
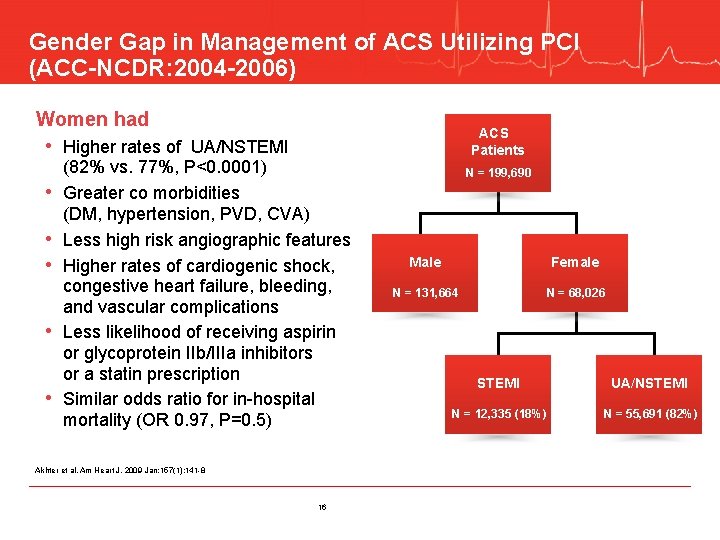
Gender Gap in Management of ACS Utilizing PCI (ACC-NCDR: 2004 -2006) Women had ACS Patients • Higher rates of UA/NSTEMI • • • (82% vs. 77%, P<0. 0001) Greater co morbidities (DM, hypertension, PVD, CVA) Less high risk angiographic features Higher rates of cardiogenic shock, congestive heart failure, bleeding, and vascular complications Less likelihood of receiving aspirin or glycoprotein IIb/IIIa inhibitors or a statin prescription Similar odds ratio for in-hospital mortality (OR 0. 97, P=0. 5) Akhter et al. Am Heart J. 2009 Jan; 157(1): 141 -8 16 N = 199, 690 Male Female N = 131, 664 N = 68, 026 STEMI UA/NSTEMI N = 12, 335 (18%) N = 55, 691 (82%)
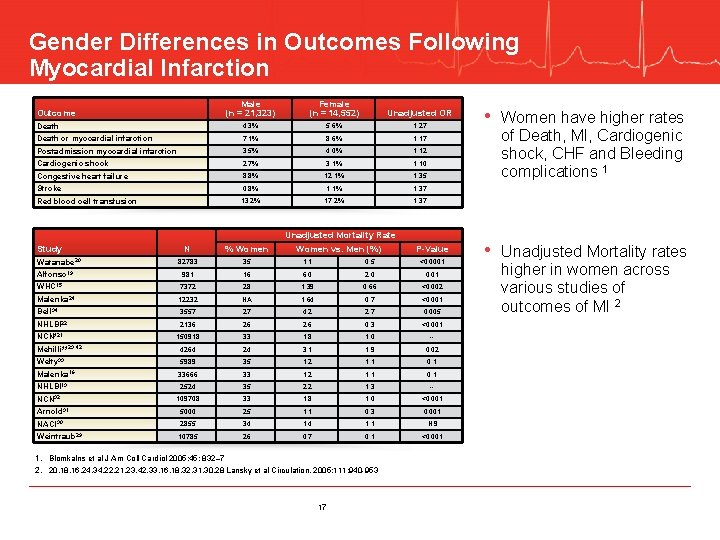
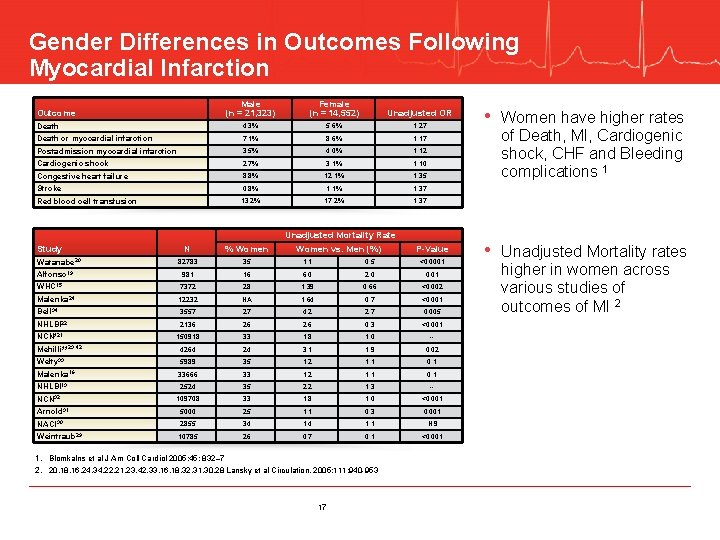
Gender Differences in Outcomes Following Myocardial Infarction Male (n = 21, 323) Female (n = 14, 552) Unadjusted OR Death 4. 3% 5. 6% 1. 27 Death or myocardial infarction 7. 1% 8. 6% 1. 17 Postadmission myocardial infarction 3. 5% 4. 0% 1. 12 Cardiogenic shock 2. 7% 3. 1% 1. 10 Congestive heart failure 8. 8% 12. 1% 1. 35 Stroke 0. 8% 1. 1% 1. 37 Red blood cell transfusion 13. 2% 17. 2% 1. 37 Outcome Study Watanabe 20 Alfonso 19 Unadjusted Mortality Rate Women vs. Men (%) of Death, MI, Cardiogenic shock, CHF and Bleeding complications 1 N % Women P-Value 82783 35 1. 1 0. 5 <0. 0001 981 16 6. 0 2. 0 0. 01 WHC 15 7372 28 1. 39 0. 66 <0. 002 Malenka 24 12232 NA 1. 64 0. 7 <0. 001 Bell 34 3557 27 4. 2 2. 7 0. 005 NHLBI 22 2136 26 2. 6 0. 3 <0. 001 NCN*21 150918 33 1. 8 1. 0 -- 4264 24 3. 1 1. 9 0. 02 Welty 33 5989 35 1. 2 1. 1 0. 1 Malenka 16 33666 33 1. 2 1. 1 0. 1 NHLBI 13 2524 35 2. 2 1. 3 -- 109708 33 1. 8 1. 0 <0. 001 Arnold 31 5000 25 1. 1 0. 3 0. 001 NACI 30 2855 34 1. 1 NS Weintraub 29 10785 26 0. 7 0. 1 <0. 001 Mehilli**23, 42 NCN 32 1. Blomkalns et al J Am Coll Cardiol 2005; 45: 832– 7 2. 20, 18, 16, 24, 34, 22, 21, 23, 42, 33, 16, 18, 32, 31, 30, 28 Lansky et al Circulation. 2005; 111: 940 -953 17 • Women have higher rates • Unadjusted Mortality rates higher in women across various studies of outcomes of MI 2
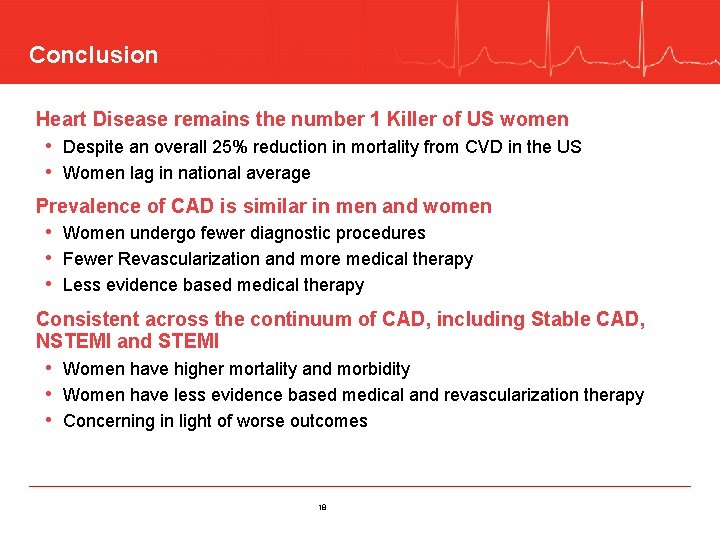
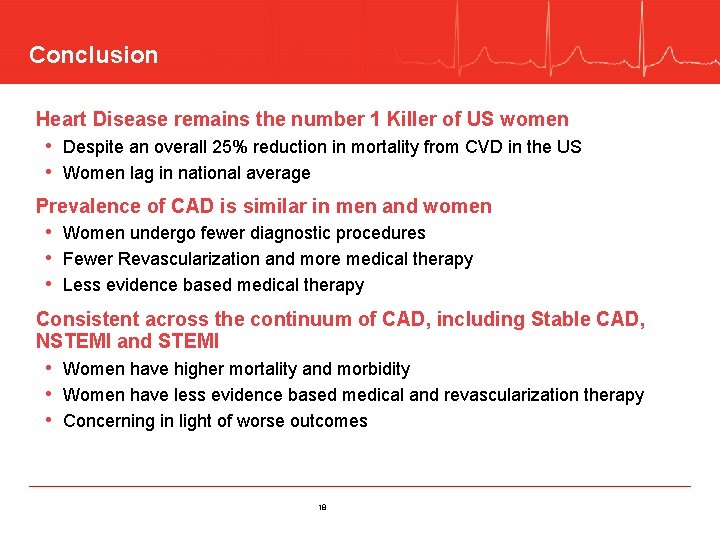
Conclusion Heart Disease remains the number 1 Killer of US women • Despite an overall 25% reduction in mortality from CVD in the US • Women lag in national average Prevalence of CAD is similar in men and women • Women undergo fewer diagnostic procedures • Fewer Revascularization and more medical therapy • Less evidence based medical therapy Consistent across the continuum of CAD, including Stable CAD, NSTEMI and STEMI • Women have higher mortality and morbidity • Women have less evidence based medical and revascularization therapy • Concerning in light of worse outcomes 18
THANK YOU 19
 Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Coronary artery disease
Coronary artery disease Annulus of vieussens
Annulus of vieussens Where is the pulmonary semilunar valve located
Where is the pulmonary semilunar valve located Coronary heart disease
Coronary heart disease Origin of sma
Origin of sma Strategic gender needs and practical gender needs
Strategic gender needs and practical gender needs Uncrossed disparity
Uncrossed disparity Health disparity definition
Health disparity definition Monocular depth cues of interposition
Monocular depth cues of interposition Gerakan sakadik adalah
Gerakan sakadik adalah Phi phenomenon psychology definition
Phi phenomenon psychology definition Health disparities meaning
Health disparities meaning Retinal disparity definition psychology
Retinal disparity definition psychology Binocular disparity depth perception
Binocular disparity depth perception Metrical depth cues
Metrical depth cues Color constancy ap psychology
Color constancy ap psychology Depth from disparity
Depth from disparity Depth perception ap psychology
Depth perception ap psychology Heart disease symptoms
Heart disease symptoms