GCA Masquerading as Altered Mental Status and Diarrhea
- Slides: 1
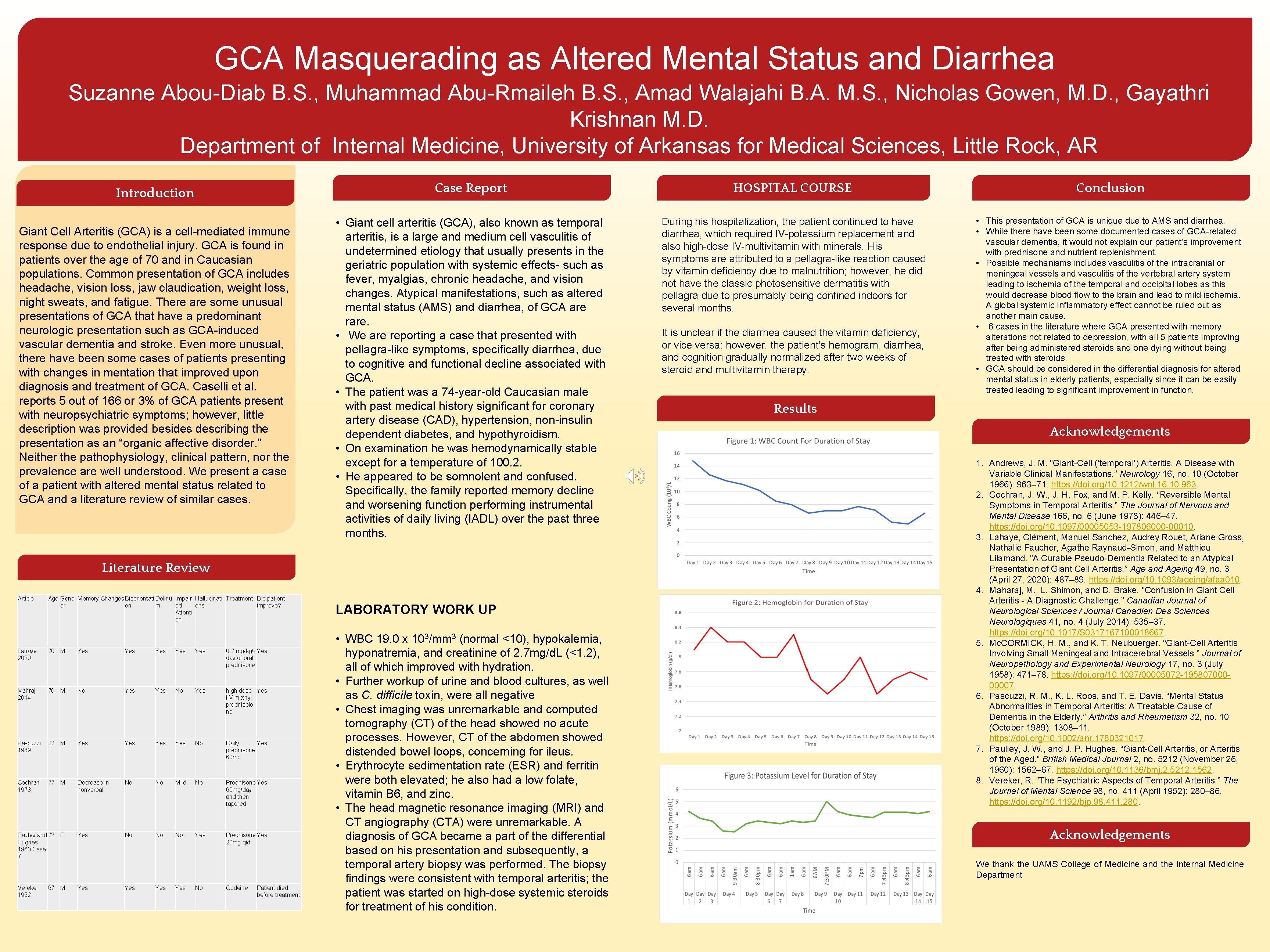
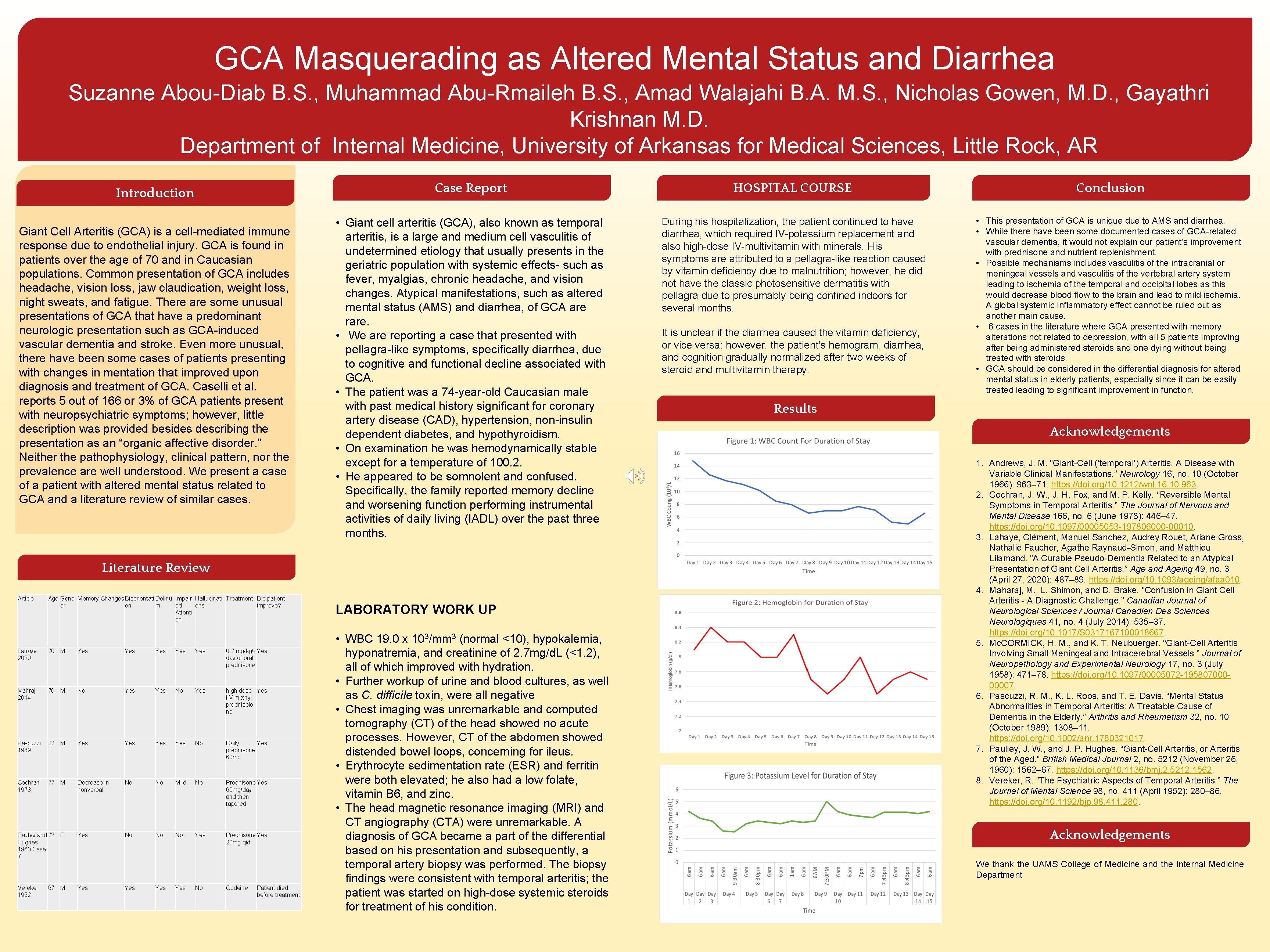
GCA Masquerading as Altered Mental Status and Diarrhea Suzanne Abou-Diab B. S. , Muhammad Abu-Rmaileh B. S. , Amad Walajahi B. A. M. S. , Nicholas Gowen, M. D. , Gayathri Krishnan M. D. Department of Internal Medicine, University of Arkansas for Medical Sciences, Little Rock, AR Introduction Giant Cell Arteritis (GCA) is a cell-mediated immune response due to endothelial injury. GCA is found in patients over the age of 70 and in Caucasian populations. Common presentation of GCA includes headache, vision loss, jaw claudication, weight loss, night sweats, and fatigue. There are some unusual presentations of GCA that have a predominant neurologic presentation such as GCA-induced vascular dementia and stroke. Even more unusual, there have been some cases of patients presenting with changes in mentation that improved upon diagnosis and treatment of GCA. Caselli et al. reports 5 out of 166 or 3% of GCA patients present with neuropsychiatric symptoms; however, little description was provided besides describing the presentation as an “organic affective disorder. ” Neither the pathophysiology, clinical pattern, nor the prevalence are well understood. We present a case of a patient with altered mental status related to GCA and a literature review of similar cases. Case Report HOSPITAL COURSE Conclusion • Giant cell arteritis (GCA), also known as temporal arteritis, is a large and medium cell vasculitis of undetermined etiology that usually presents in the geriatric population with systemic effects- such as fever, myalgias, chronic headache, and vision changes. Atypical manifestations, such as altered mental status (AMS) and diarrhea, of GCA are rare. • We are reporting a case that presented with pellagra-like symptoms, specifically diarrhea, due to cognitive and functional decline associated with GCA. • The patient was a 74 -year-old Caucasian male with past medical history significant for coronary artery disease (CAD), hypertension, non-insulin dependent diabetes, and hypothyroidism. • On examination he was hemodynamically stable except for a temperature of 100. 2. • He appeared to be somnolent and confused. Specifically, the family reported memory decline and worsening function performing instrumental activities of daily living (IADL) over the past three months. During his hospitalization, the patient continued to have diarrhea, which required IV-potassium replacement and also high-dose IV-multivitamin with minerals. His symptoms are attributed to a pellagra-like reaction caused by vitamin deficiency due to malnutrition; however, he did not have the classic photosensitive dermatitis with pellagra due to presumably being confined indoors for several months. • This presentation of GCA is unique due to AMS and diarrhea. • While there have been some documented cases of GCA-related vascular dementia, it would not explain our patient’s improvement with prednisone and nutrient replenishment. • Possible mechanisms includes vasculitis of the intracranial or meningeal vessels and vasculitis of the vertebral artery system leading to ischemia of the temporal and occipital lobes as this would decrease blood flow to the brain and lead to mild ischemia. A global systemic inflammatory effect cannot be ruled out as another main cause. • 6 cases in the literature where GCA presented with memory alterations not related to depression, with all 5 patients improving after being administered steroids and one dying without being treated with steroids. • GCA should be considered in the differential diagnosis for altered mental status in elderly patients, especially since it can be easily treated leading to significant improvement in function. Literature Review Article Age Gend Memory Changes Disorientati Deliriu Impair Hallucinati Treatment Did patient er on m ed ons improve? Attenti on Lahaye 2020 70 M Yes Yes Yes 0. 7 mg/kg/- Yes day of oral prednisone Mahraj 2014 70 M No Yes high dose Yes i. IV methyl prednisolo ne Pascuzzi 1989 72 M Yes Yes No Daily Yes prednisone 60 mg Cochran 1978 77 M Decrease in nonverbal No No Mild No Prednisone Yes 60 mg/day and then tapered Pauley and 72 F Hughes 1960 Case 7 Yes No No No Yes Prednisone Yes 20 mg qid Vereker 1952 Yes 67 M Yes Yes No Codeine Patient died before treatment LABORATORY WORK UP • WBC 19. 0 x 103/mm 3 (normal <10), hypokalemia, hyponatremia, and creatinine of 2. 7 mg/d. L (<1. 2), all of which improved with hydration. • Further workup of urine and blood cultures, as well as C. difficile toxin, were all negative • Chest imaging was unremarkable and computed tomography (CT) of the head showed no acute processes. However, CT of the abdomen showed distended bowel loops, concerning for ileus. • Erythrocyte sedimentation rate (ESR) and ferritin were both elevated; he also had a low folate, vitamin B 6, and zinc. • The head magnetic resonance imaging (MRI) and CT angiography (CTA) were unremarkable. A diagnosis of GCA became a part of the differential based on his presentation and subsequently, a temporal artery biopsy was performed. The biopsy findings were consistent with temporal arteritis; the patient was started on high-dose systemic steroids for treatment of his condition. It is unclear if the diarrhea caused the vitamin deficiency, or vice versa; however, the patient’s hemogram, diarrhea, and cognition gradually normalized after two weeks of steroid and multivitamin therapy. Results Acknowledgements 1. Andrews, J. M. “Giant-Cell (‘temporal’) Arteritis. A Disease with Variable Clinical Manifestations. ” Neurology 16, no. 10 (October 1966): 963– 71. https: //doi. org/10. 1212/wnl. 16. 10. 963. 2. Cochran, J. W. , J. H. Fox, and M. P. Kelly. “Reversible Mental Symptoms in Temporal Arteritis. ” The Journal of Nervous and Mental Disease 166, no. 6 (June 1978): 446– 47. https: //doi. org/10. 1097/00005053 -197806000 -00010. 3. Lahaye, Clément, Manuel Sanchez, Audrey Rouet, Ariane Gross, Nathalie Faucher, Agathe Raynaud-Simon, and Matthieu Lilamand. “A Curable Pseudo-Dementia Related to an Atypical Presentation of Giant Cell Arteritis. ” Age and Ageing 49, no. 3 (April 27, 2020): 487– 89. https: //doi. org/10. 1093/ageing/afaa 010. 4. Maharaj, M. , L. Shimon, and D. Brake. “Confusion in Giant Cell Arteritis - A Diagnostic Challenge. ” Canadian Journal of Neurological Sciences / Journal Canadien Des Sciences Neurologiques 41, no. 4 (July 2014): 535– 37. https: //doi. org/10. 1017/S 0317167100018667. 5. Mc. CORMICK, H. M. , and K. T. Neubuerger. “Giant-Cell Arteritis Involving Small Meningeal and Intracerebral Vessels. ” Journal of Neuropathology and Experimental Neurology 17, no. 3 (July 1958): 471– 78. https: //doi. org/10. 1097/00005072 -19580700000007. 6. Pascuzzi, R. M. , K. L. Roos, and T. E. Davis. “Mental Status Abnormalities in Temporal Arteritis: A Treatable Cause of Dementia in the Elderly. ” Arthritis and Rheumatism 32, no. 10 (October 1989): 1308– 11. https: //doi. org/10. 1002/anr. 1780321017. 7. Paulley, J. W. , and J. P. Hughes. “Giant-Cell Arteritis, or Arteritis of the Aged. ” British Medical Journal 2, no. 5212 (November 26, 1960): 1562– 67. https: //doi. org/10. 1136/bmj. 2. 5212. 1562. 8. Vereker, R. “The Psychiatric Aspects of Temporal Arteritis. ” The Journal of Mental Science 98, no. 411 (April 1952): 280– 86. https: //doi. org/10. 1192/bjp. 98. 411. 280. Acknowledgements We thank the UAMS College of Medicine and the Internal Medicine Department