Gastroparesis Edy E Soffer M D Keck School

- Slides: 43
Gastroparesis Edy E Soffer, M. D. Keck School of Medicine, University of Southern California
Objectives • Epidemiology • Physiology of gastric motor function / pathophysiology • Evaluation • Treatment options
Definition Symptoms of gastric retention, evidence of delayed gastric emptying, in the absence of obstruction
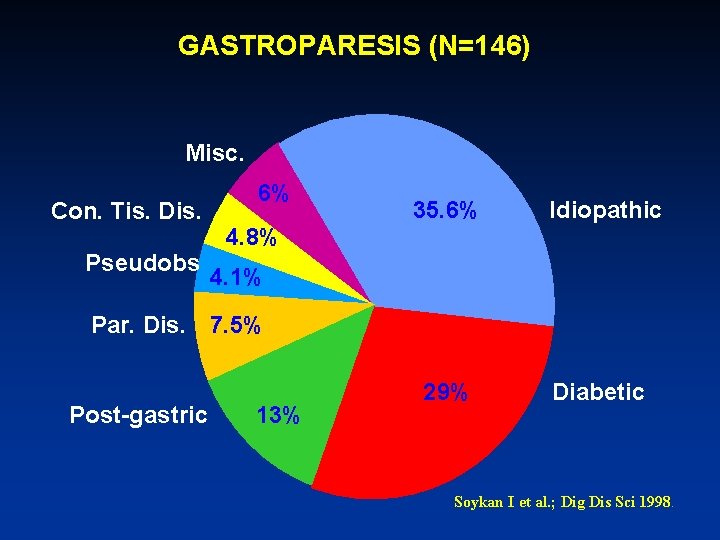
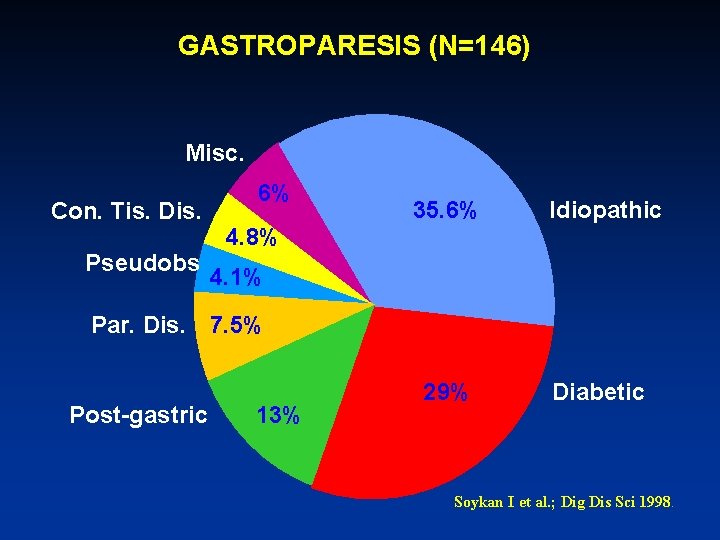
GASTROPARESIS (N=146) Misc. Con. Tis. Dis. Pseudobs 6% 35. 6% 4. 8% Idiopathic 4. 1% Par. Dis. 7. 5% Post-gastric 13% 29% Diabetic Soykan I et al. ; Dig Dis Sci 1998.

ICC’s Vagus,
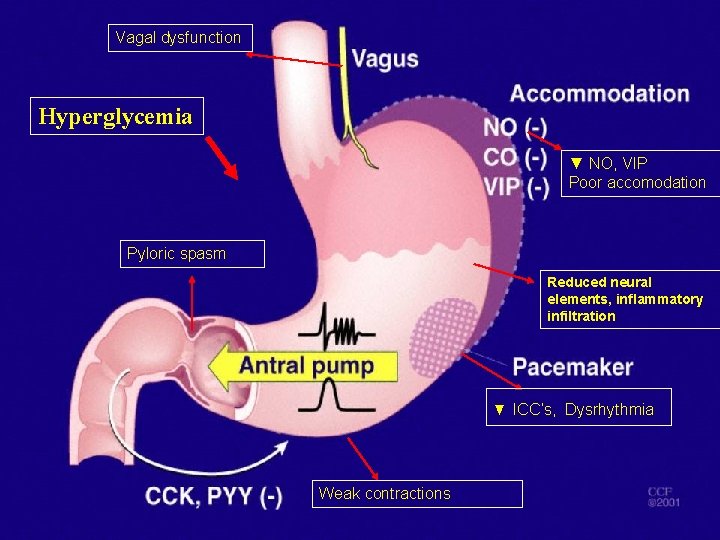
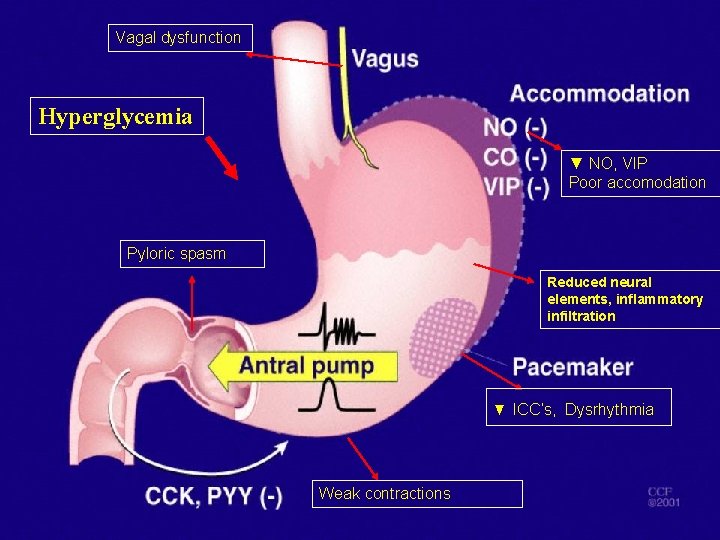
Vagal dysfunction Hyperglycemia ▼ NO, VIP Poor accomodation Pyloric spasm Reduced neural elements, inflammatory infiltration ▼ ICC’s, Dysrhythmia Weak contractions
Gastroparesis: Symptoms Early satiety, nausea and vomiting, bloating, abdominal pain, weight loss
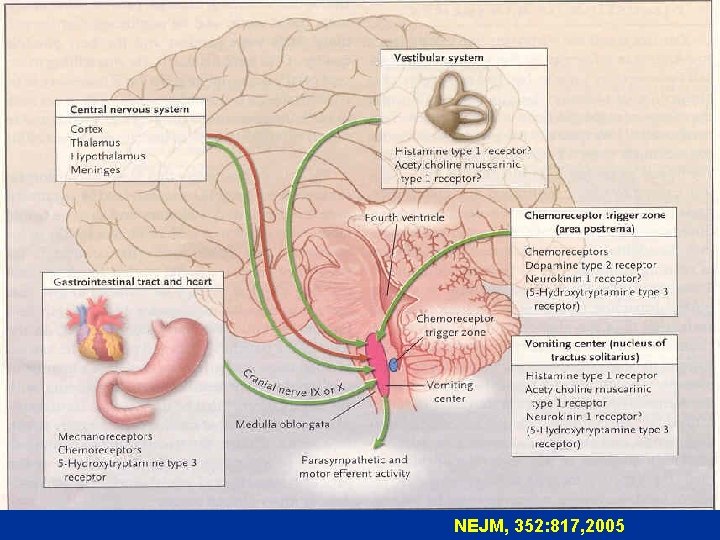
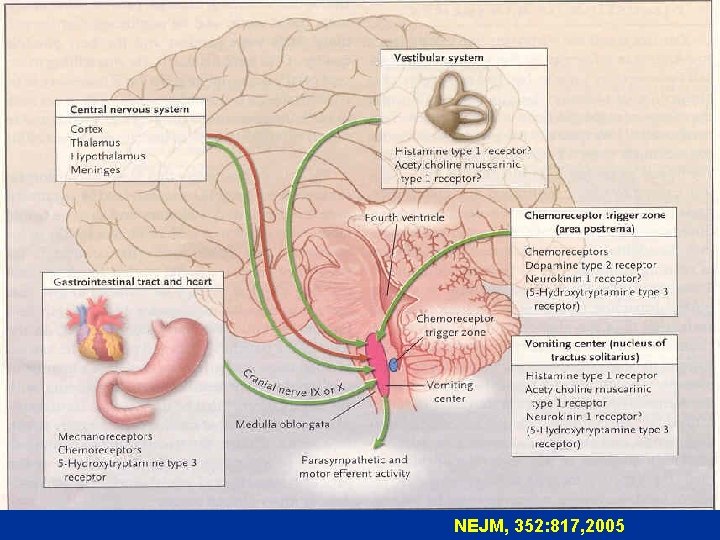
NEJM, 352: 817, 2005
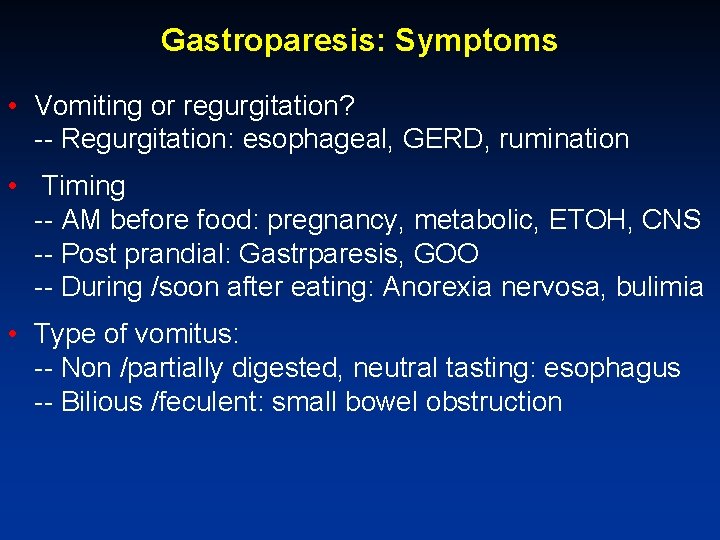
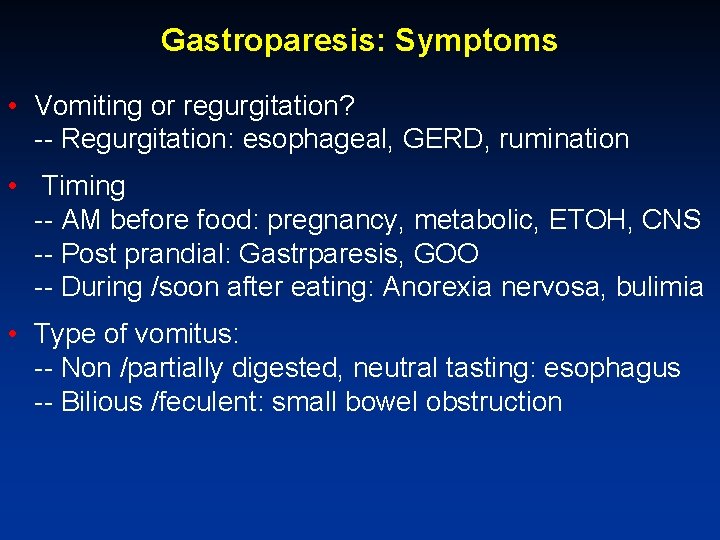
Gastroparesis: Symptoms • Vomiting or regurgitation? -- Regurgitation: esophageal, GERD, rumination • Timing -- AM before food: pregnancy, metabolic, ETOH, CNS -- Post prandial: Gastrparesis, GOO -- During /soon after eating: Anorexia nervosa, bulimia • Type of vomitus: -- Non /partially digested, neutral tasting: esophagus -- Bilious /feculent: small bowel obstruction
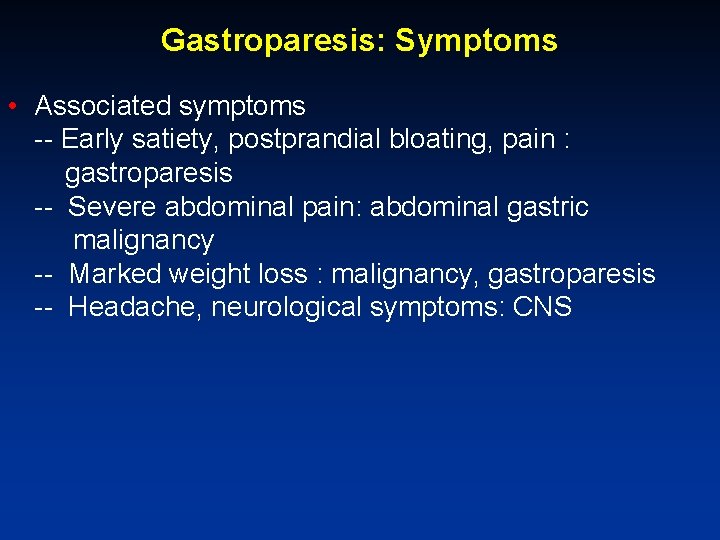
Gastroparesis: Symptoms • Associated symptoms -- Early satiety, postprandial bloating, pain : gastroparesis -- Severe abdominal pain: abdominal gastric malignancy -- Marked weight loss : malignancy, gastroparesis -- Headache, neurological symptoms: CNS
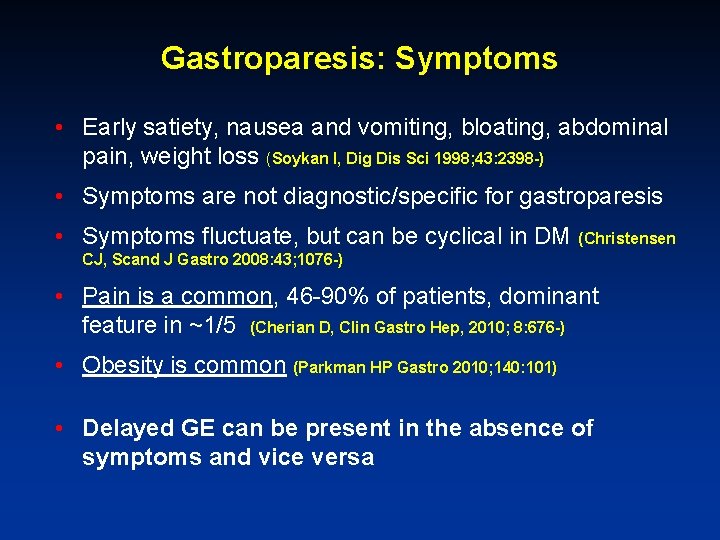
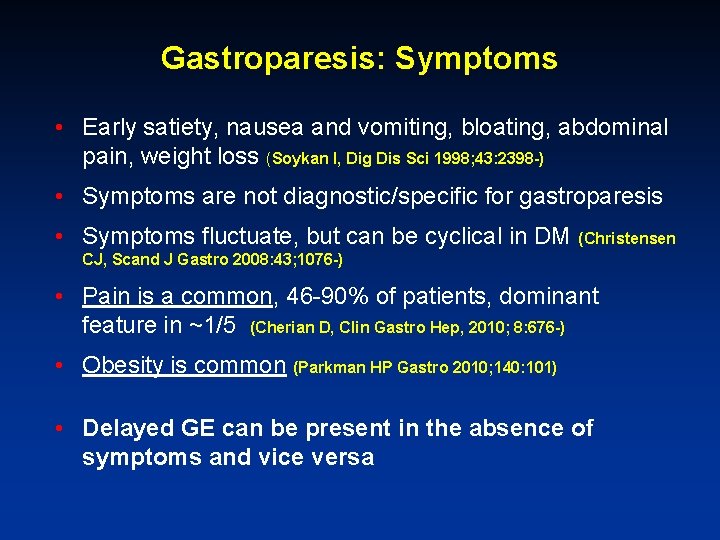
Gastroparesis: Symptoms • Early satiety, nausea and vomiting, bloating, abdominal pain, weight loss (Soykan I, Dig Dis Sci 1998; 43: 2398 -) • Symptoms are not diagnostic/specific for gastroparesis • Symptoms fluctuate, but can be cyclical in DM (Christensen CJ, Scand J Gastro 2008: 43; 1076 -) • Pain is a common, 46 -90% of patients, dominant feature in ~1/5 (Cherian D, Clin Gastro Hep, 2010; 8: 676 -) • Obesity is common (Parkman HP Gastro 2010; 140: 101) • Delayed GE can be present in the absence of symptoms and vice versa
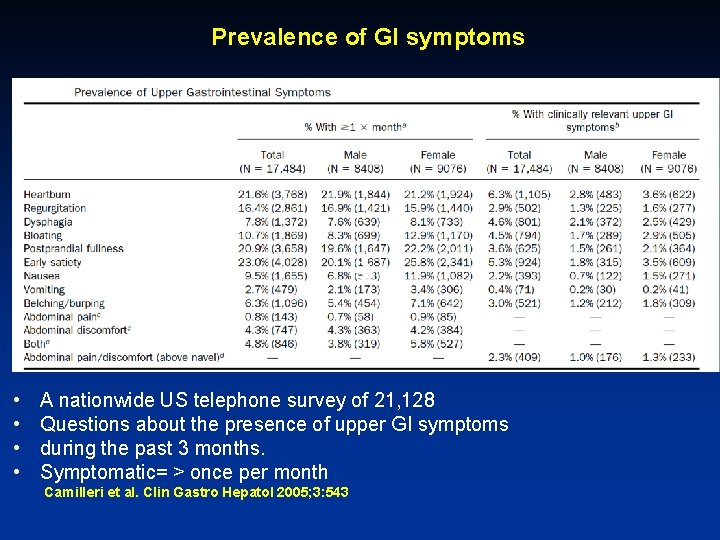
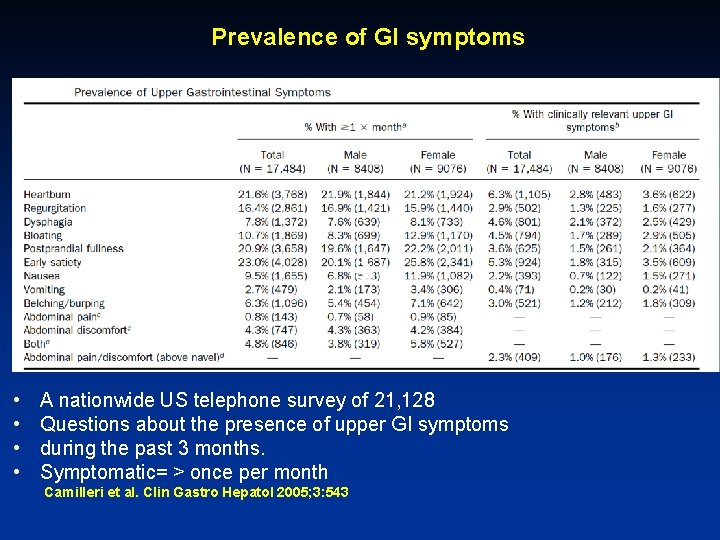
Prevalence of GI symptoms • • A nationwide US telephone survey of 21, 128 Questions about the presence of upper GI symptoms during the past 3 months. Symptomatic= > once per month Camilleri et al. Clin Gastro Hepatol 2005; 3: 543
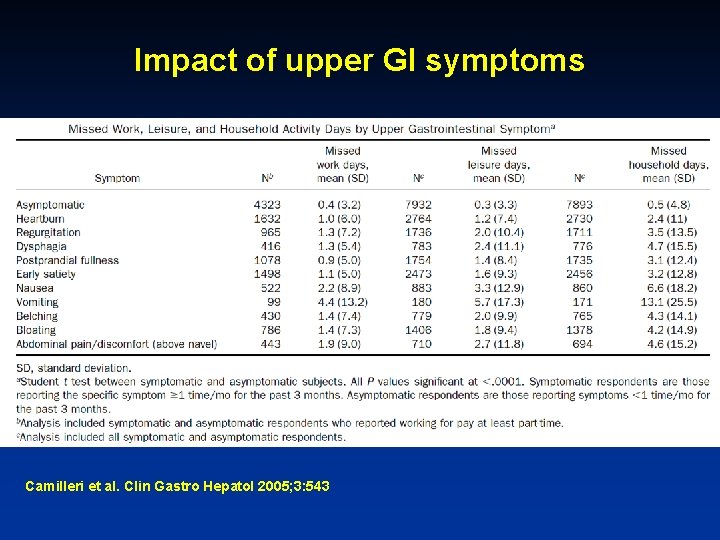
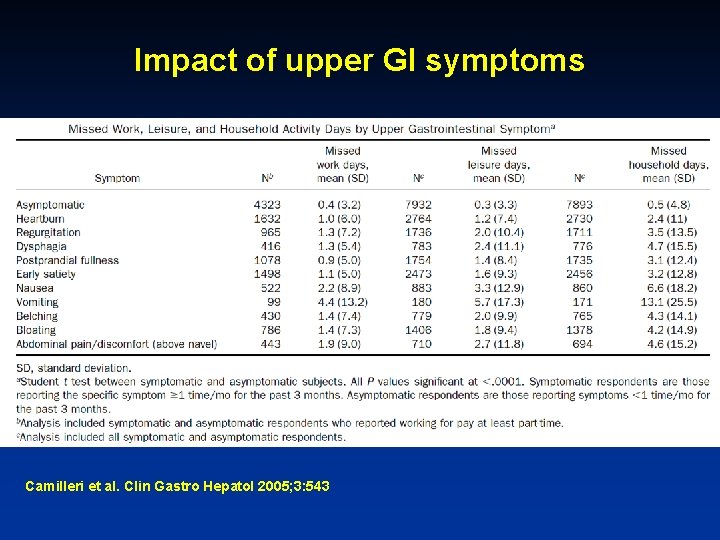
Impact of upper GI symptoms Camilleri et al. Clin Gastro Hepatol 2005; 3: 543
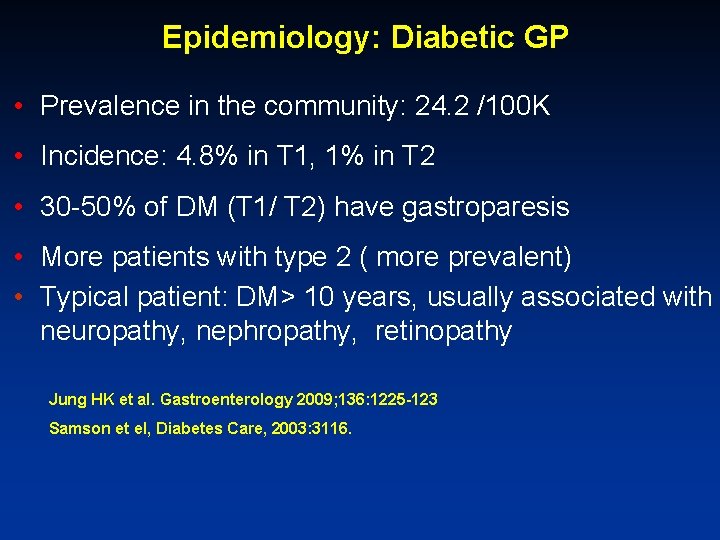
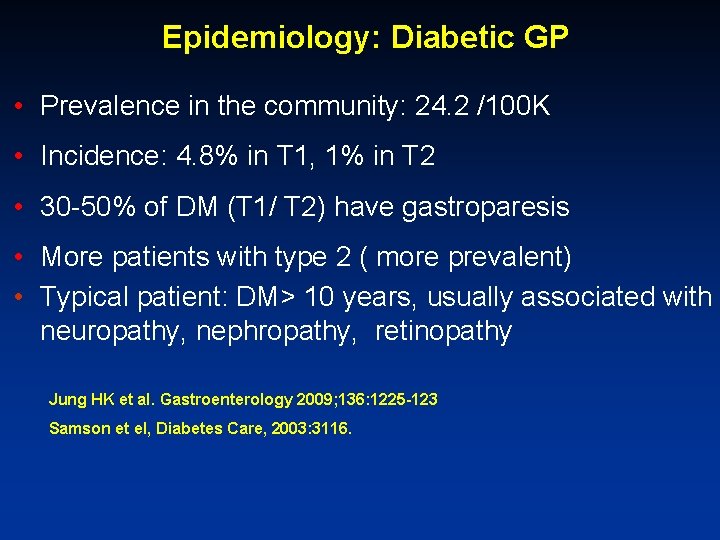
Epidemiology: Diabetic GP • Prevalence in the community: 24. 2 /100 K • Incidence: 4. 8% in T 1, 1% in T 2 • 30 -50% of DM (T 1/ T 2) have gastroparesis • More patients with type 2 ( more prevalent) • Typical patient: DM> 10 years, usually associated with neuropathy, nephropathy, retinopathy Jung HK et al. Gastroenterology 2009; 136: 1225 -123 Samson et el, Diabetes Care, 2003: 3116.
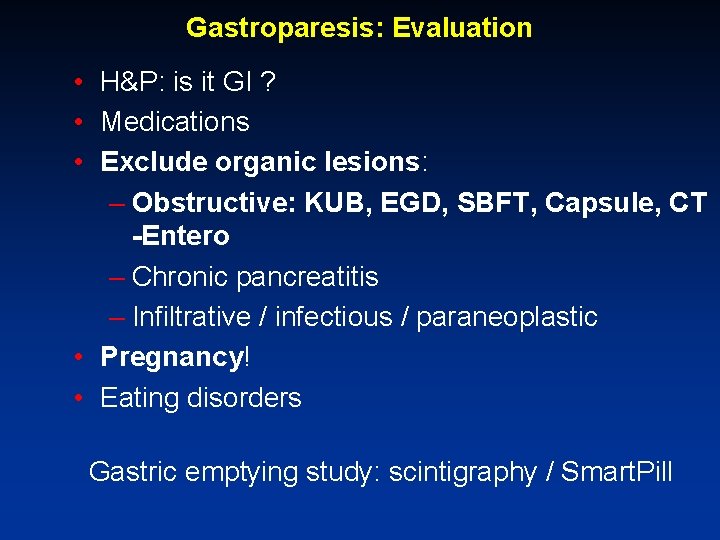
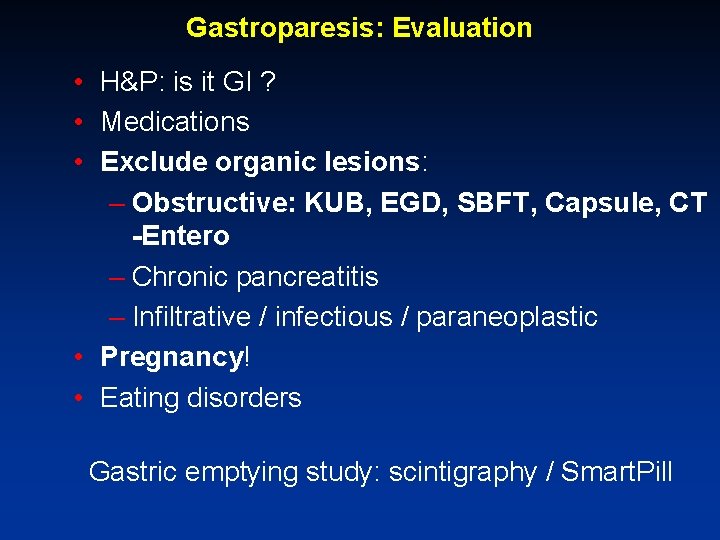
Gastroparesis: Evaluation • H&P: is it GI ? • Medications • Exclude organic lesions: – Obstructive: KUB, EGD, SBFT, Capsule, CT -Entero – Chronic pancreatitis – Infiltrative / infectious / paraneoplastic • Pregnancy! • Eating disorders Gastric emptying study: scintigraphy / Smart. Pill
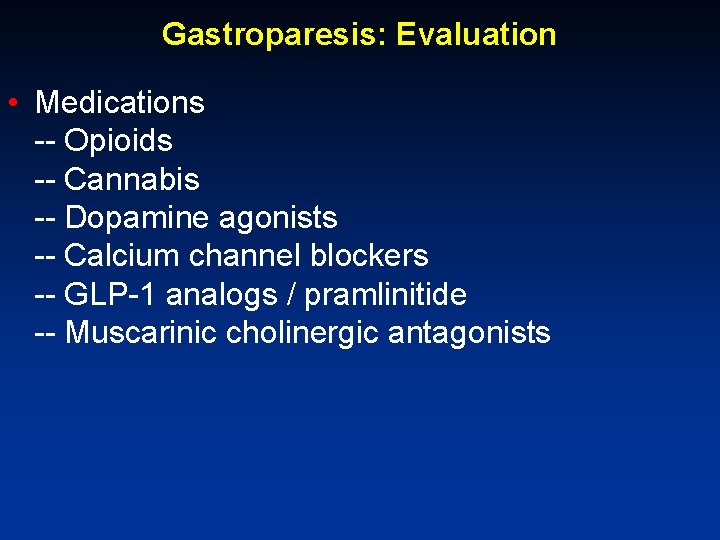
Gastroparesis: Evaluation • Medications -- Opioids -- Cannabis -- Dopamine agonists -- Calcium channel blockers -- GLP-1 analogs / pramlinitide -- Muscarinic cholinergic antagonists
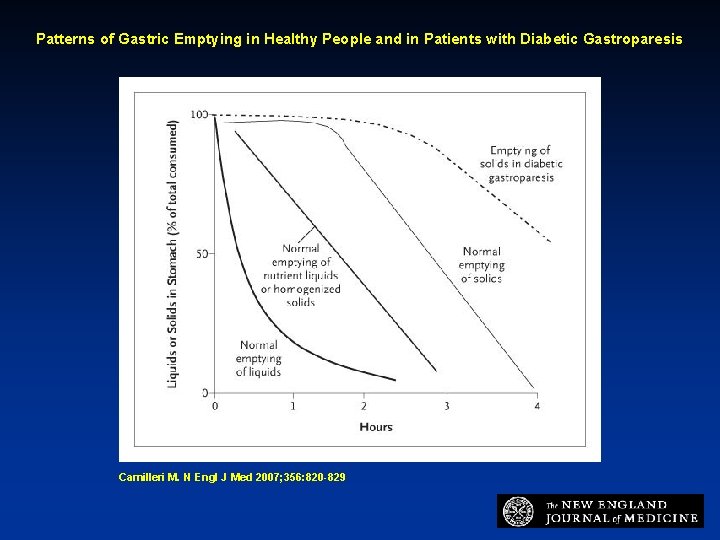
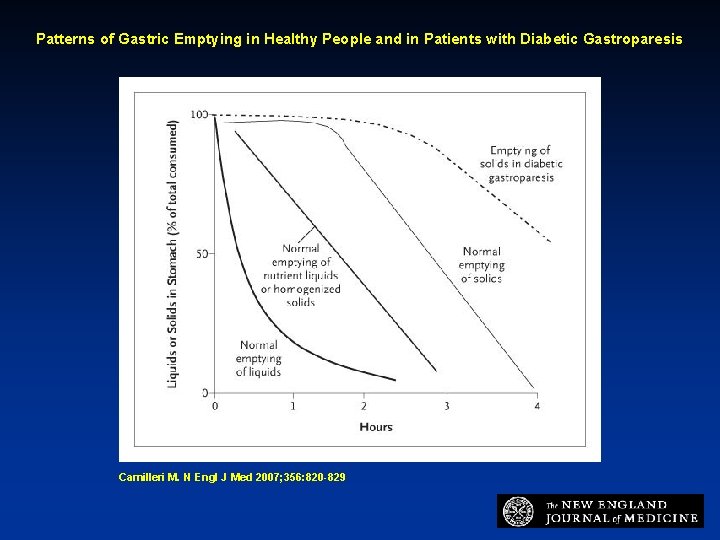
Patterns of Gastric Emptying in Healthy People and in Patients with Diabetic Gastroparesis Camilleri M. N Engl J Med 2007; 356: 820 -829
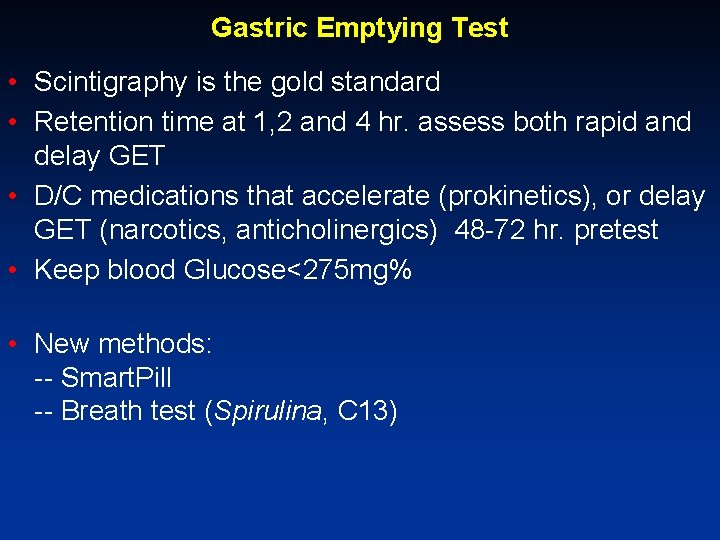
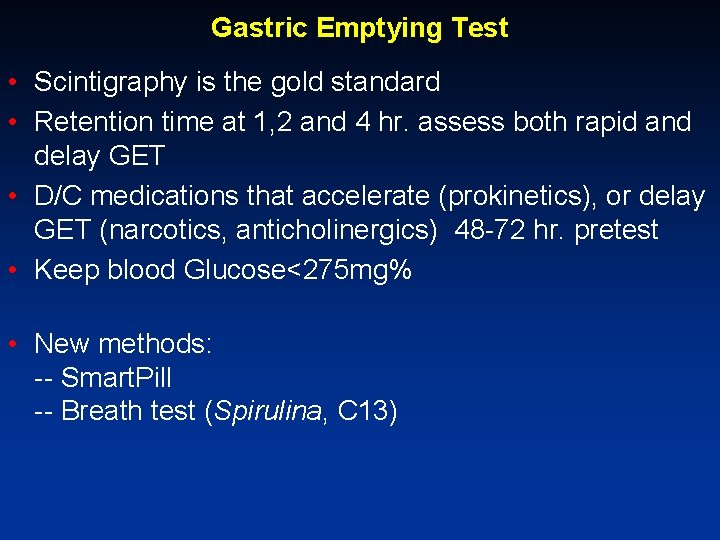
Gastric Emptying Test • Scintigraphy is the gold standard • Retention time at 1, 2 and 4 hr. assess both rapid and delay GET • D/C medications that accelerate (prokinetics), or delay GET (narcotics, anticholinergics) 48 -72 hr. pretest • Keep blood Glucose<275 mg% • New methods: -- Smart. Pill -- Breath test (Spirulina, C 13)
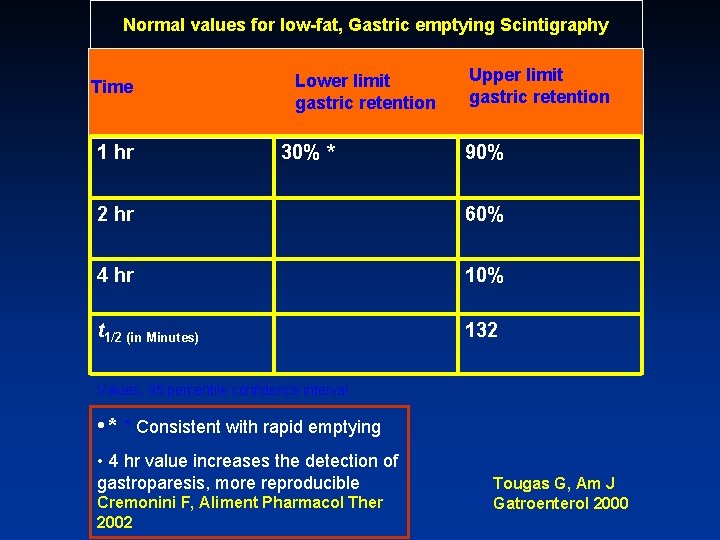
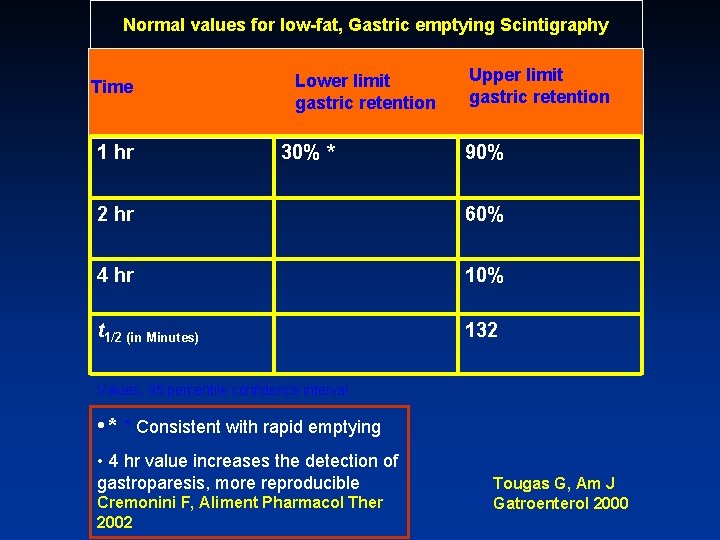
Normal values for low-fat, Gastric emptying Scintigraphy Time 1 hr Lower limit gastric retention 30% * Upper limit gastric retention 90% 2 hr 60% 4 hr 10% t 1/2 (in Minutes) 132 Values, 95 percentile confidence interval • * * Consistent with rapid emptying • 4 hr value increases the detection of gastroparesis, more reproducible Cremonini F, Aliment Pharmacol Ther 2002 Tougas G, Am J Gatroenterol 2000
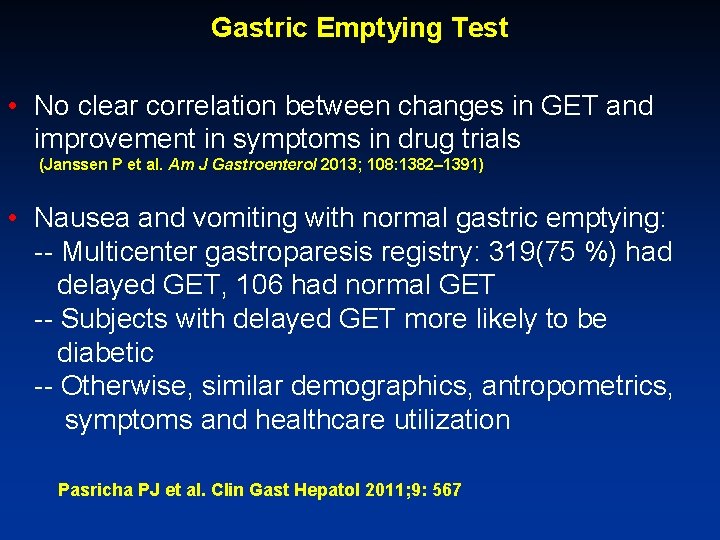
Gastric Emptying Test • No clear correlation between changes in GET and improvement in symptoms in drug trials (Janssen P et al. Am J Gastroenterol 2013; 108: 1382– 1391) • Nausea and vomiting with normal gastric emptying: -- Multicenter gastroparesis registry: 319(75 %) had delayed GET, 106 had normal GET -- Subjects with delayed GET more likely to be diabetic -- Otherwise, similar demographics, antropometrics, symptoms and healthcare utilization Pasricha PJ et al. Clin Gast Hepatol 2011; 9: 567
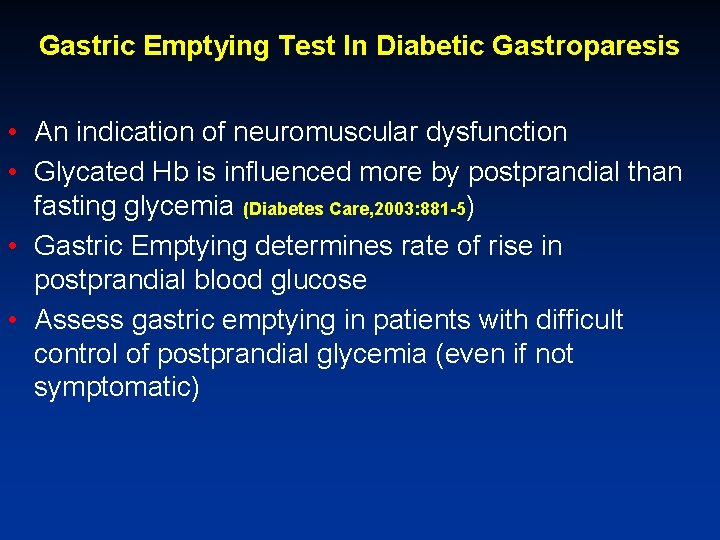
Gastric Emptying Test In Diabetic Gastroparesis • An indication of neuromuscular dysfunction • Glycated Hb is influenced more by postprandial than fasting glycemia (Diabetes Care, 2003: 881 -5) • Gastric Emptying determines rate of rise in postprandial blood glucose • Assess gastric emptying in patients with difficult control of postprandial glycemia (even if not symptomatic)
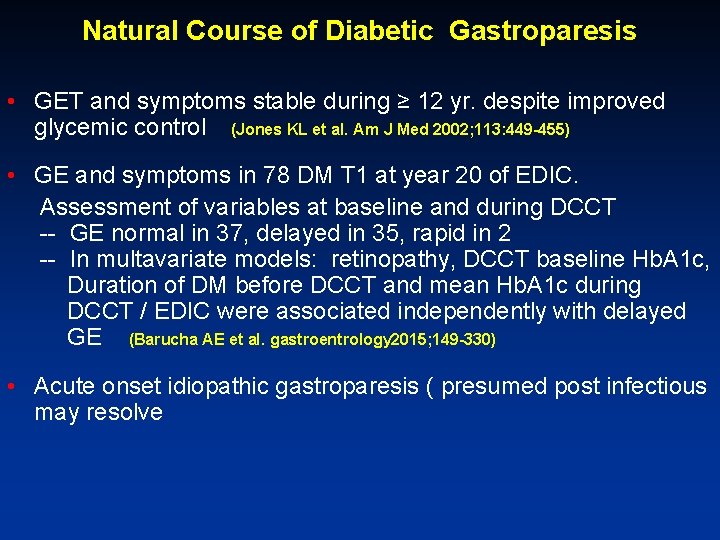
Natural Course of Diabetic Gastroparesis • GET and symptoms stable during ≥ 12 yr. despite improved glycemic control (Jones KL et al. Am J Med 2002; 113: 449 -455) • GE and symptoms in 78 DM T 1 at year 20 of EDIC. Assessment of variables at baseline and during DCCT -- GE normal in 37, delayed in 35, rapid in 2 -- In multavariate models: retinopathy, DCCT baseline Hb. A 1 c, Duration of DM before DCCT and mean Hb. A 1 c during DCCT / EDIC were associated independently with delayed GE (Barucha AE et al. gastroentrology 2015; 149 -330) • Acute onset idiopathic gastroparesis ( presumed post infectious may resolve
Treatment Principles • Improve nutritional and hydration • Relieve GI symptoms (QOL, functionality, hospitalization) • Optimize glycemic control
Management of Gastroparesis • Dietary modification, Glucose control • Medications: antiemetics, promotility • Pain control • Nutritional support: enteral, TPN • Surgical / endoscopic interventions
Management of Gastroparesis: Diet • Small frequent meals • Low fat (liquid fat) • Mechanically soft pureed liquid • Low residue • Supplementation: vitamins
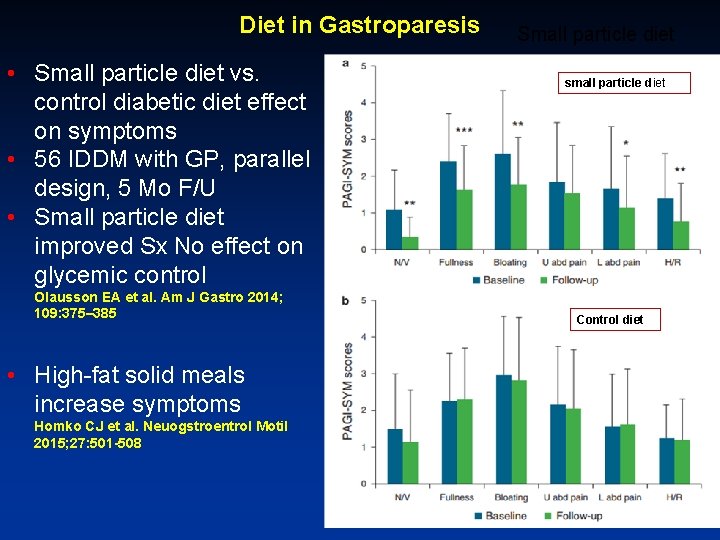
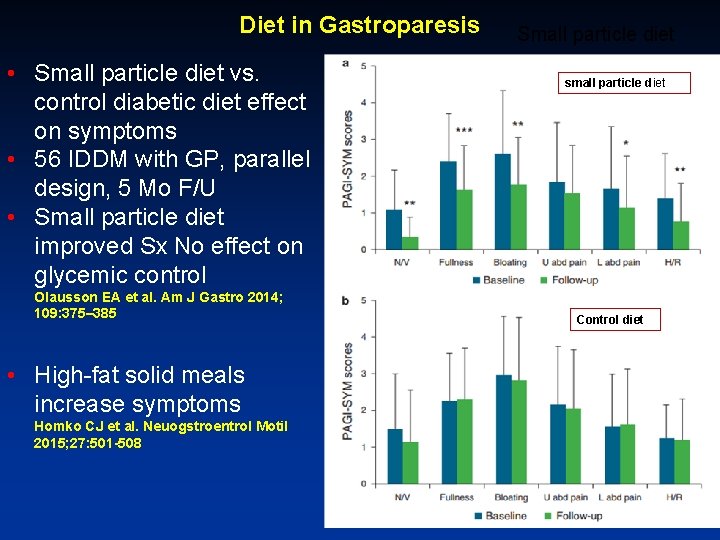
Diet in Gastroparesis • Small particle diet vs. control diabetic diet effect on symptoms • 56 IDDM with GP, parallel design, 5 Mo F/U • Small particle diet improved Sx No effect on glycemic control Olausson EA et al. Am J Gastro 2014; 109: 375– 385 • High-fat solid meals increase symptoms Homko CJ et al. Neuogstroentrol Motil 2015; 27: 501 -508 Small particle diet small particle diet Control diet
Drug Therapy in Gastroparesis: Promotility / Antiemetics • Dopamine antagonists: metoclopramide, domperidone • Erythromycin /Azithromycin • Phenothiazines / antihistamines • Serotonin 3 antagonists • Cannabinoid • New agents- relamorin: ghrelin receptor agonist. -- A 4 weeks phase II double-blind, placebo control in 204 T 2 DM patients with gastroparesis. -- Improved GET vomiting and gastroparesis Sx in those with baseline vomiting Lembo A et al. Gastroenterology 2016; 151: 87– 96
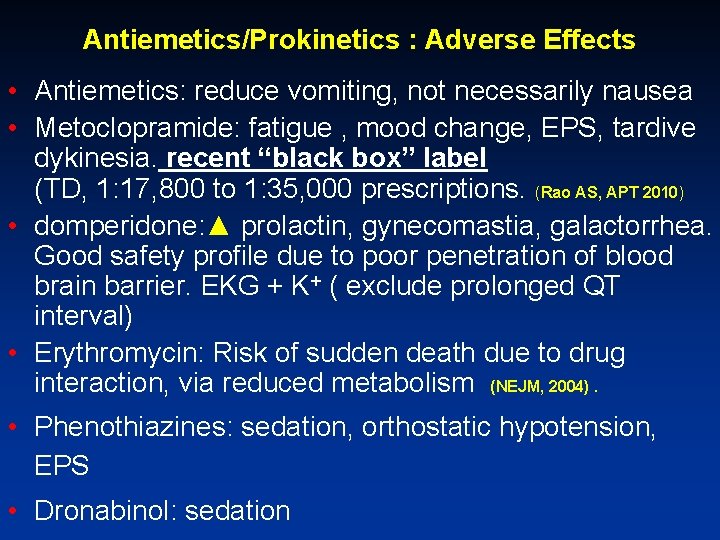
Antiemetics/Prokinetics : Adverse Effects • Antiemetics: reduce vomiting, not necessarily nausea • Metoclopramide: fatigue , mood change, EPS, tardive dykinesia. recent “black box” label (TD, 1: 17, 800 to 1: 35, 000 prescriptions. (Rao AS, APT 2010) • domperidone: ▲ prolactin, gynecomastia, galactorrhea. Good safety profile due to poor penetration of blood brain barrier. EKG + K+ ( exclude prolonged QT interval) • Erythromycin: Risk of sudden death due to drug interaction, via reduced metabolism (NEJM, 2004). • Phenothiazines: sedation, orthostatic hypotension, EPS • Dronabinol: sedation
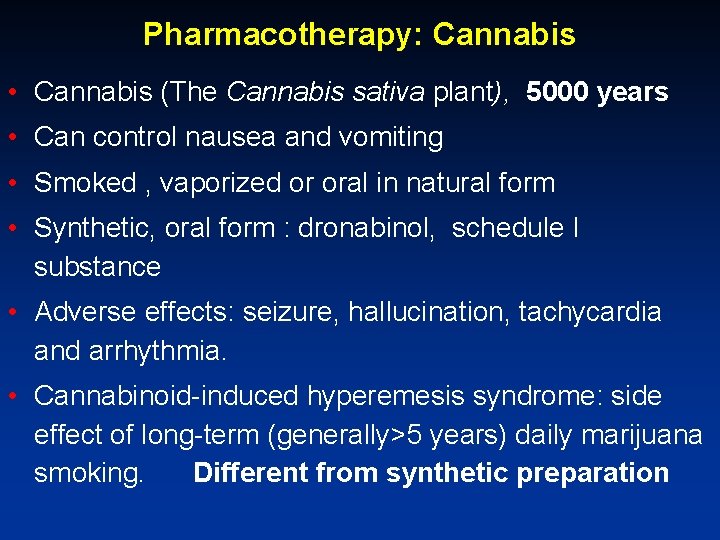
Pharmacotherapy: Cannabis • Cannabis (The Cannabis sativa plant), 5000 years • Can control nausea and vomiting • Smoked , vaporized or oral in natural form • Synthetic, oral form : dronabinol, schedule I substance • Adverse effects: seizure, hallucination, tachycardia and arrhythmia. • Cannabinoid-induced hyperemesis syndrome: side effect of long-term (generally>5 years) daily marijuana smoking. Different from synthetic preparation
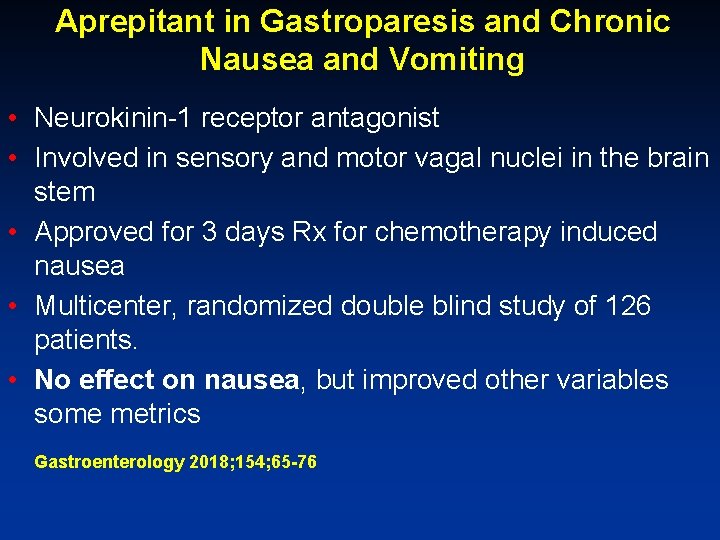
Aprepitant in Gastroparesis and Chronic Nausea and Vomiting • Neurokinin-1 receptor antagonist • Involved in sensory and motor vagal nuclei in the brain stem • Approved for 3 days Rx for chemotherapy induced nausea • Multicenter, randomized double blind study of 126 patients. • No effect on nausea, but improved other variables some metrics Gastroenterology 2018; 154; 65 -76
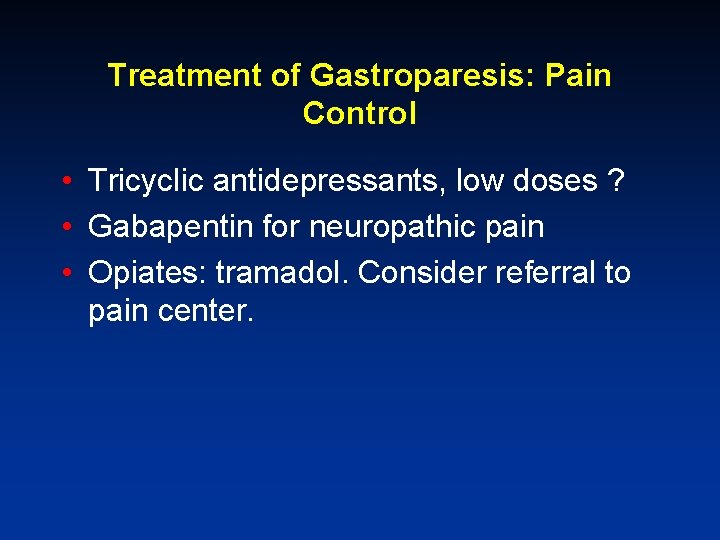
Treatment of Gastroparesis: Pain Control • Tricyclic antidepressants, low doses ? • Gabapentin for neuropathic pain • Opiates: tramadol. Consider referral to pain center.
Pain Control: Psychotropic Drugs • Randomized study: nortriptyline vs. placebo in patients with idiopathic gastroparesis: no difference in outcome. Parkman et al. JAMA 2013; 310: 2640 - • Randomized study: amitriptyline (TCA) vs. ecitalopram (SSRI) vs. placebo in patients with dyspepsia: -- TCA but not SSRI improved pain, but not dyspeptic symptoms (modest gain, borderline significance) -- Beneficial effect seen in normal gastric emptying only. Tally NJ et al. Gastroenterology 2015; 149: 340
Management of Gastroparesis: Medications • Adequate dosing (strength, frequency) • Adequate mode of delivery (ODT, patch, liquid, suppository, J-tube) • Combination therapy
Management of Gastroparesis: Alternative Nutrition Enteral: Jejunostomy-tube feeding: • Simple to operate, cheap, Improves nutritional status, glucose control, reduces hospitalizations Jones MP, Am J Gastro 2003 TPN: expensive, risky, difficult to operate
Enteral Nutrition in Gastroparesis • • • Trial of naso-jejunal feeding while NPO Method: PEG-J, dual G&J, jejunostomy Formula: polymeric (Glucerna). High caloric (11/2 -2 Kcals/ml), ensure hydration Use pump or gravity drip Nocturnal, continuous,
Surgical / Endoscopic interventions in Gastroparesis • Gastric resection in post surgical gastroparesis • Feeding tubes (jejunostomy) • Implantation of gastric neurostimulator • • Gastric resection in non surgical gastroparesis? Pyloroplasty Pyloric stenting G-POEM
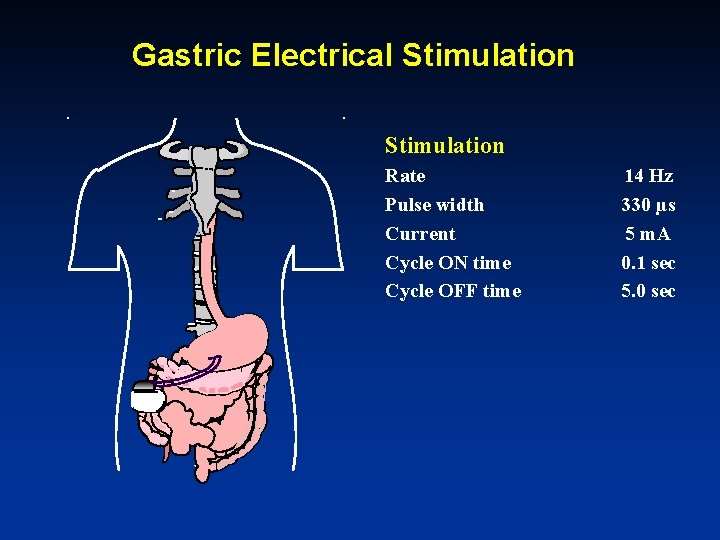
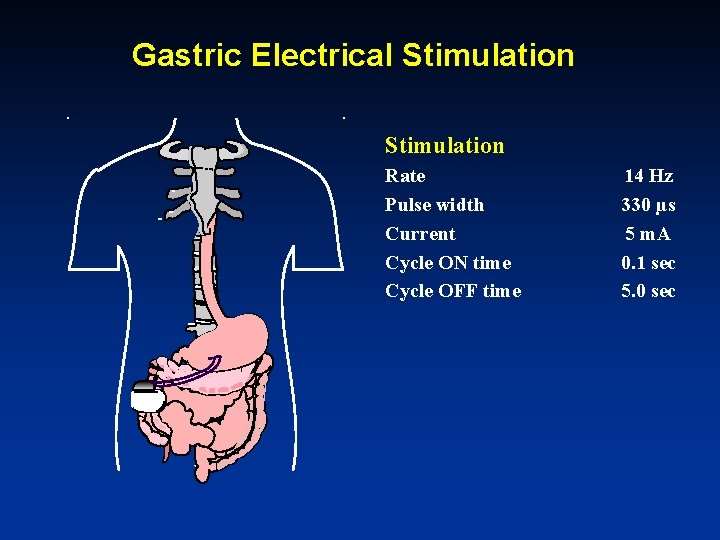
Gastric Electrical Stimulation Rate Pulse width Current Cycle ON time Cycle OFF time 14 Hz 330 µs 5 m. A 0. 1 sec 5. 0 sec
GES for Gastroparesis • Improvement in QOL, nutrition, reduces health care costs (Cutts TF, Neurogastromotil, 2005; 17: 35 -) • Improved glucose control (Lin Z, Diabetes care 2004) • Open label studies reported good clinical response (Soffer E, APT 2009) • Adequate double blind, sham control studies are lacking (Abell, Gastro 2003. Mc. Callum, CGH 2010, Gastro abstract 2010) • “Current evidence on the efficacy and safety of gastric electrical stimulation for gastroparesis is adequate to support the use of this procedure with normal arrangements for clinical governance, consent and audit”. (The National Institute for Health and Care Excellence UK (NICE) 2014)
Gastric Electrical Stimulation: Current Status/Indications • HDE status, requires IRB • Diabetic and idiopathic gastroparesis • Chronic, not responsive to available therapy, particularly when alternative nutrition required
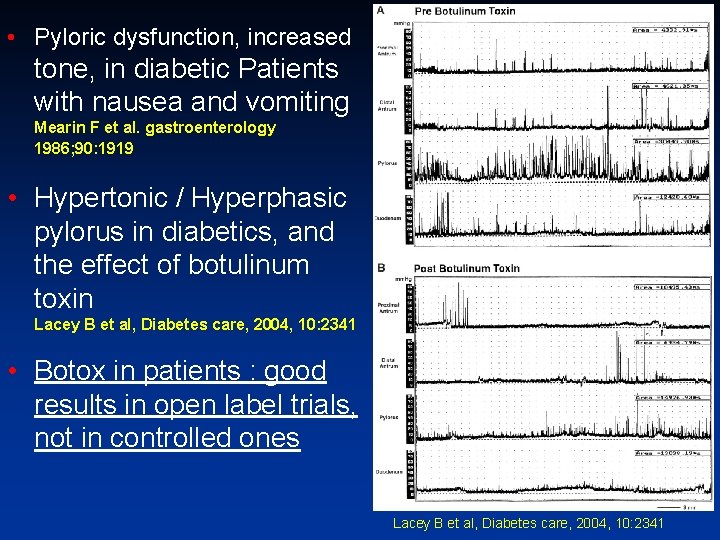
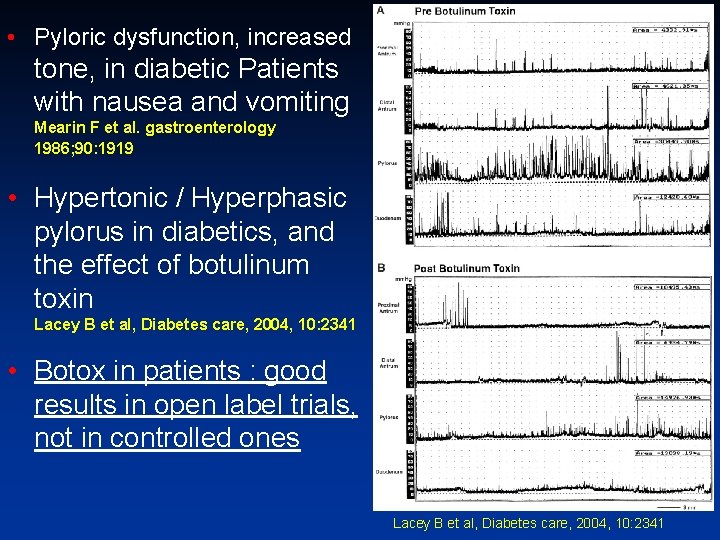
• Pyloric dysfunction, increased tone, in diabetic Patients with nausea and vomiting Mearin F et al. gastroenterology 1986; 90: 1919 • Hypertonic / Hyperphasic pylorus in diabetics, and the effect of botulinum toxin Lacey B et al, Diabetes care, 2004, 10: 2341 • Botox in patients : good results in open label trials, not in controlled ones Lacey B et al, Diabetes care, 2004, 10: 2341
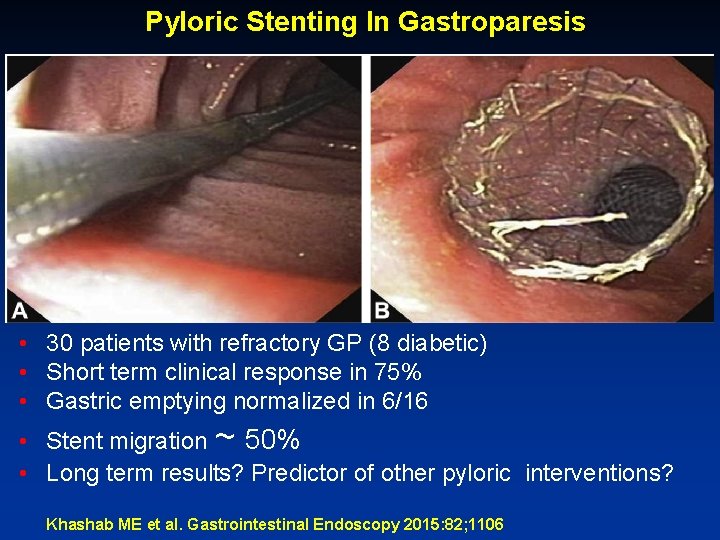
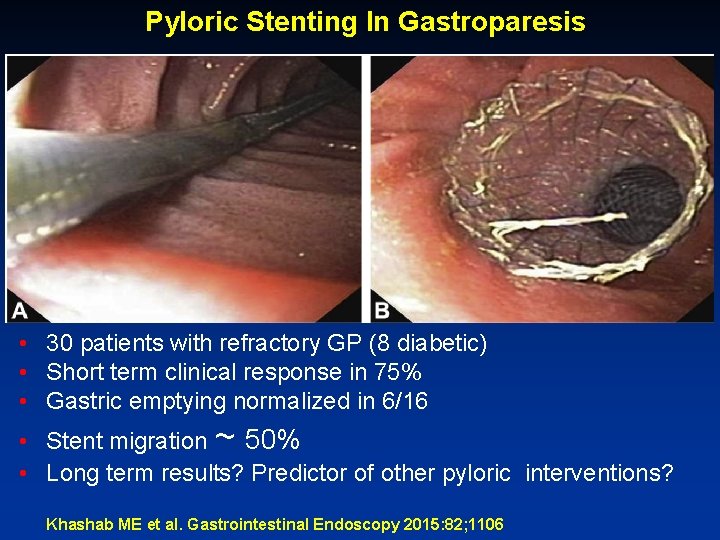
Pyloric Stenting In Gastroparesis • 30 patients with refractory GP (8 diabetic) • Short term clinical response in 75% • Gastric emptying normalized in 6/16 • Stent migration ~ 50% • Long term results? Predictor of other pyloric interventions? Khashab ME et al. Gastrointestinal Endoscopy 2015: 82; 1106
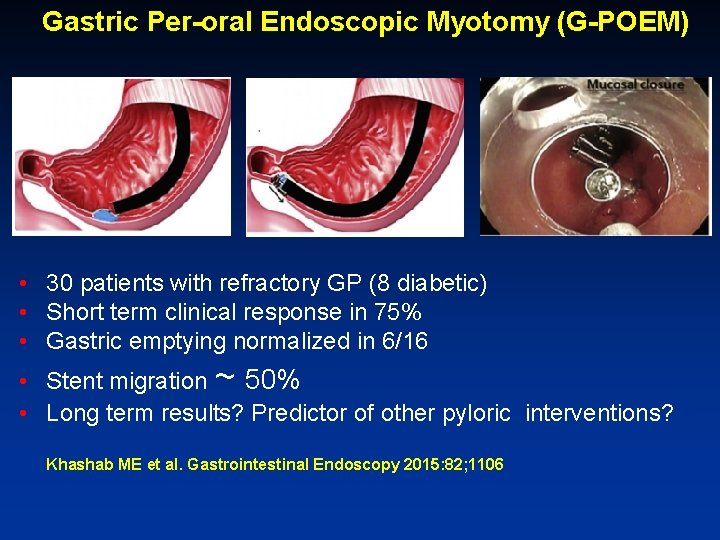
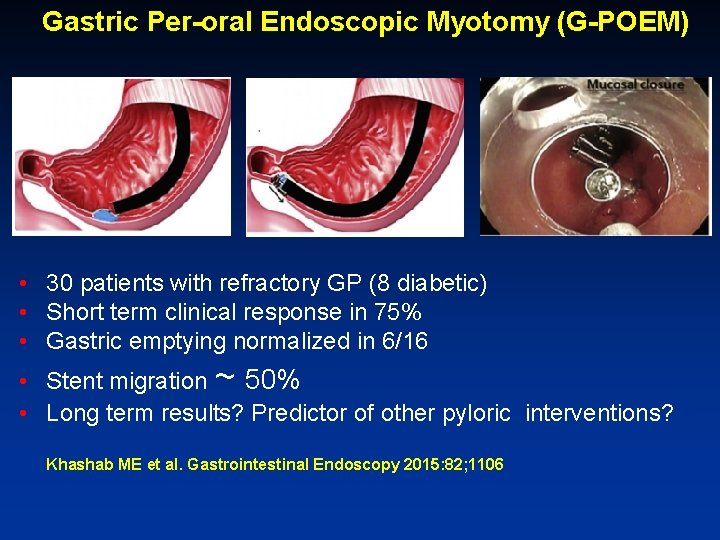
Gastric Per-oral Endoscopic Myotomy (G-POEM) • 30 patients with refractory GP (8 diabetic) • Short term clinical response in 75% • Gastric emptying normalized in 6/16 • Stent migration ~ 50% • Long term results? Predictor of other pyloric interventions? Khashab ME et al. Gastrointestinal Endoscopy 2015: 82; 1106
Take Home message • Make appropriate diagnosis : Is gastroparesis the true source of symptoms in your patient ? • Medications: dose, preparation • Secure nutrition • Electrical stimulation: select carefully • Ablative surgery: select carefully • Pyloric interventions?