GASTROINTESTINAL SYSTEM PROCEDURES PYRAMID POINTS Common types of
- Slides: 57
GASTROINTESTINAL SYSTEM PROCEDURES
PYRAMID POINTS • Common types of tubes used in the clinical setting • Assessment points related to the specific type of tube • Procedures for insertion of a particular tube • Standard (universal) precautions • Handling infectious materials
PYRAMID POINTS • Verifying correct placement and procedures for administering medications or feedings, if appropriate • Interventions related to the care of the client • Interventions associated with complications or emergencies that may occur • Client/family education regarding care at home
NASOGASTRIC (NG) TUBES • DESCRIPTION – Short tubes used to intubate the stomach – Inserted from the nose to the stomach
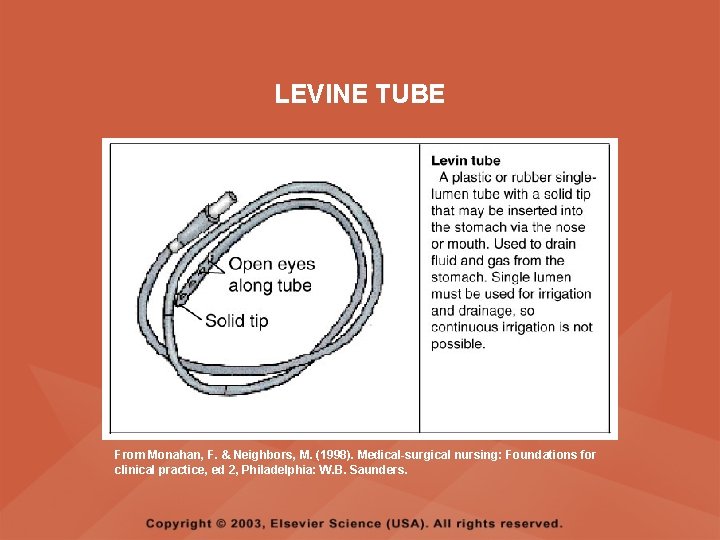
NASOGASTRIC (NG) TUBES • LEVINE – Single-lumen nasogastric tube – Used to remove gastric contents via intermittent suction or to provide tube feedings
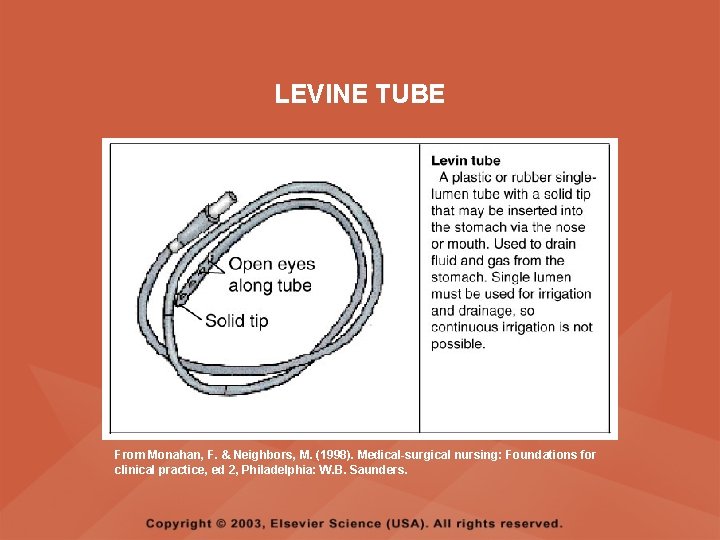
LEVINE TUBE From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
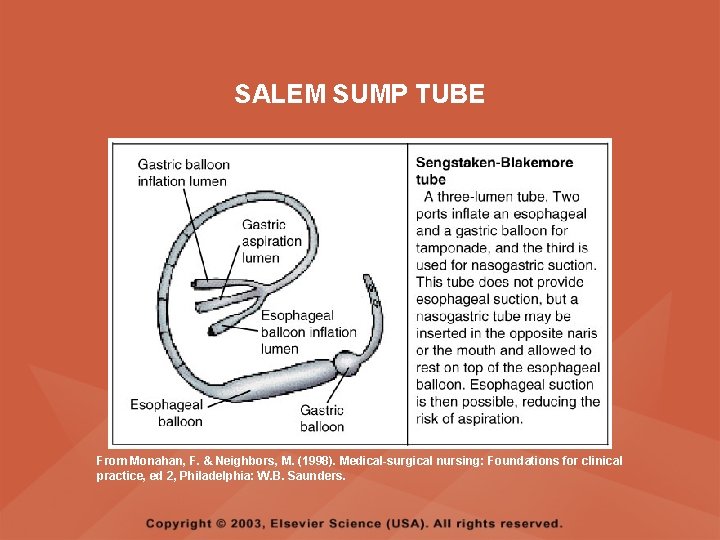
NASOGASTRIC (NG) TUBES • SALEM SUMP – Double-lumen nasogastric tube with an air vent – Used for decompression with continuous suction – Air vent is not to be clamped and is to be kept above the level of the stomach – If leakage occurs through the air vent, instill 30 ml of air into the air vent and irrigate the main lumen with normal saline (NS)
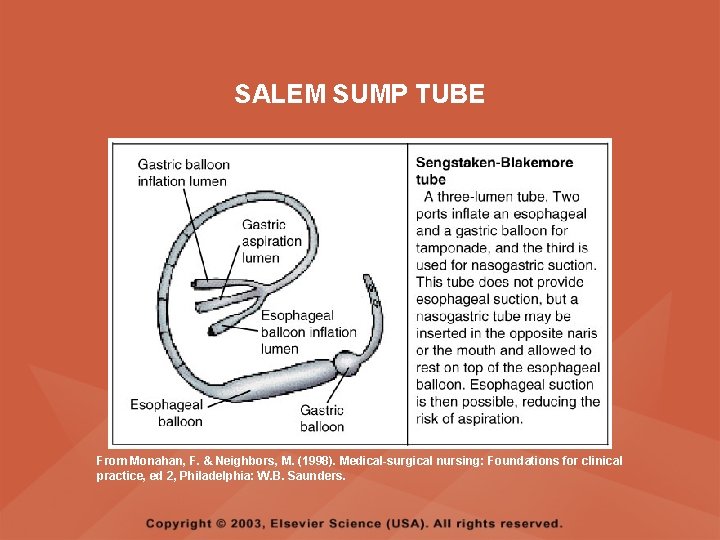
SALEM SUMP TUBE From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
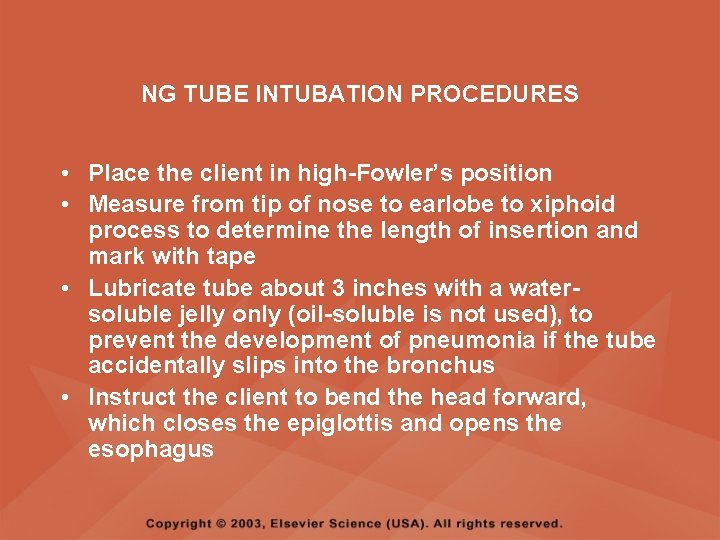
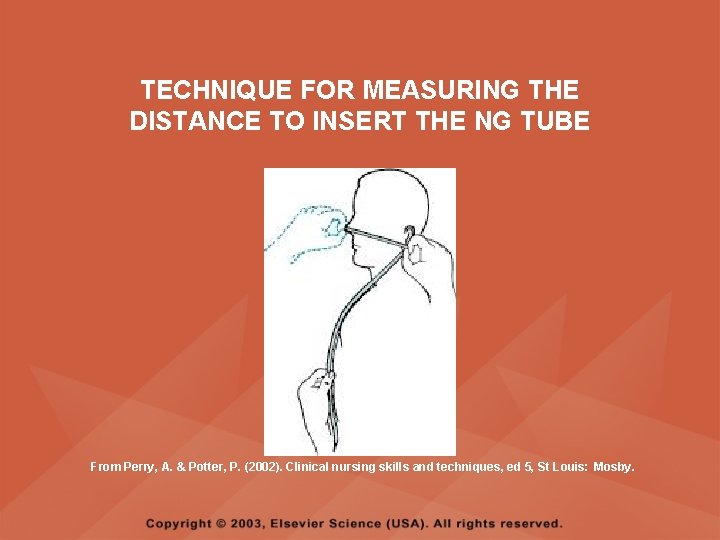
NG TUBE INTUBATION PROCEDURES • Place the client in high-Fowler’s position • Measure from tip of nose to earlobe to xiphoid process to determine the length of insertion and mark with tape • Lubricate tube about 3 inches with a watersoluble jelly only (oil-soluble is not used), to prevent the development of pneumonia if the tube accidentally slips into the bronchus • Instruct the client to bend the head forward, which closes the epiglottis and opens the esophagus
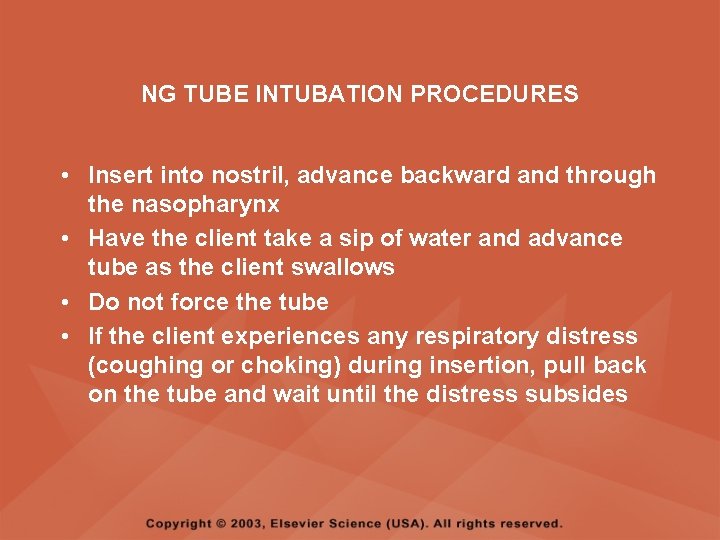
NG TUBE INTUBATION PROCEDURES • Insert into nostril, advance backward and through the nasopharynx • Have the client take a sip of water and advance tube as the client swallows • Do not force the tube • If the client experiences any respiratory distress (coughing or choking) during insertion, pull back on the tube and wait until the distress subsides
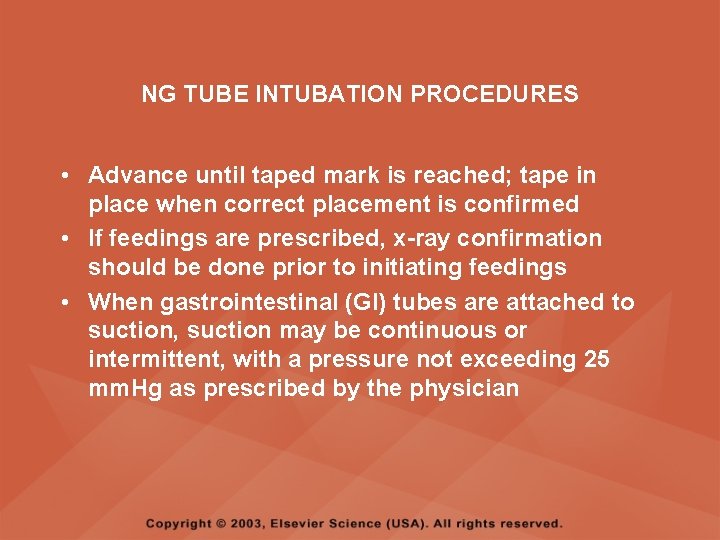
NG TUBE INTUBATION PROCEDURES • Advance until taped mark is reached; tape in place when correct placement is confirmed • If feedings are prescribed, x-ray confirmation should be done prior to initiating feedings • When gastrointestinal (GI) tubes are attached to suction, suction may be continuous or intermittent, with a pressure not exceeding 25 mm. Hg as prescribed by the physician
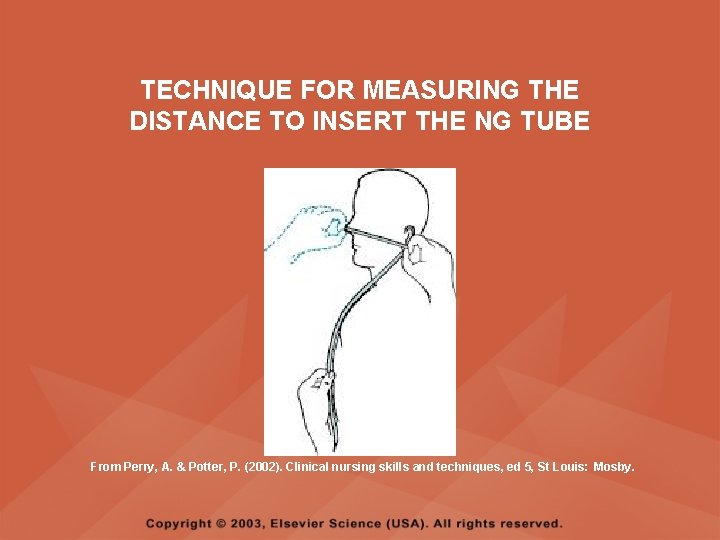
TECHNIQUE FOR MEASURING THE DISTANCE TO INSERT THE NG TUBE From Perry, A. & Potter, P. (2002). Clinical nursing skills and techniques, ed 5, St Louis: Mosby.
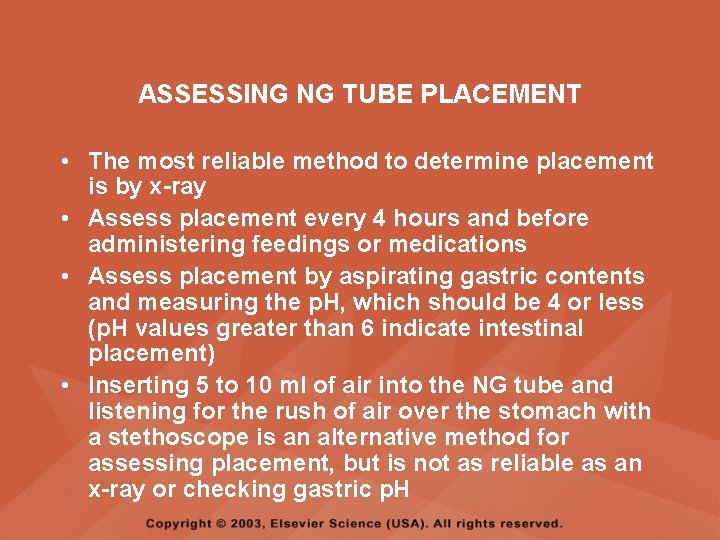
ASSESSING NG TUBE PLACEMENT • The most reliable method to determine placement is by x-ray • Assess placement every 4 hours and before administering feedings or medications • Assess placement by aspirating gastric contents and measuring the p. H, which should be 4 or less (p. H values greater than 6 indicate intestinal placement) • Inserting 5 to 10 ml of air into the NG tube and listening for the rush of air over the stomach with a stethoscope is an alternative method for assessing placement, but is not as reliable as an x-ray or checking gastric p. H
ASSESSING RESIDUAL VOLUMES • Check residual volumes every 4 hours, before each feeding, and before giving medications • Aspirate all stomach contents (residual) and measure amount • Reinstill residual feeding to prevent excessive fluid and electrolyte losses unless the residual volume appears abnormal
IRRIGATING A NG TUBE • Performed every 4 hours to check the patency of the tube • Assess placement before irrigating • Gently instill 30 to 50 ml of water or normal saline (NS) (depending on agency policy) with an irrigation syringe • Pull back on the syringe plunger to withdraw the fluid to check patency; repeat if tube remains sluggish
REMOVAL OF AN NG TUBE • Ask the client to take a deep breath and hold • Remove the tube slowly and evenly over the course of 3 to 6 seconds (coil the tube around the hand as it is being removed)
GI TUBE FEEDINGS • TUBES – Nasogastric – Nasoduodenal or nasojejunal – Gastrostomy – Jejunostomy
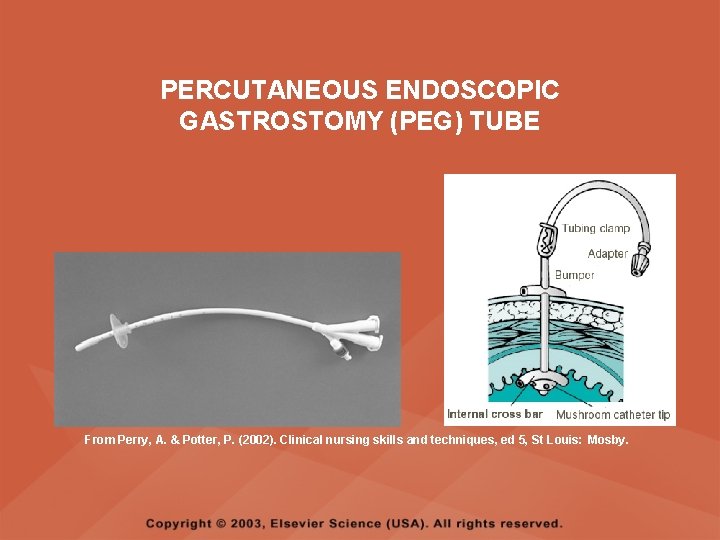
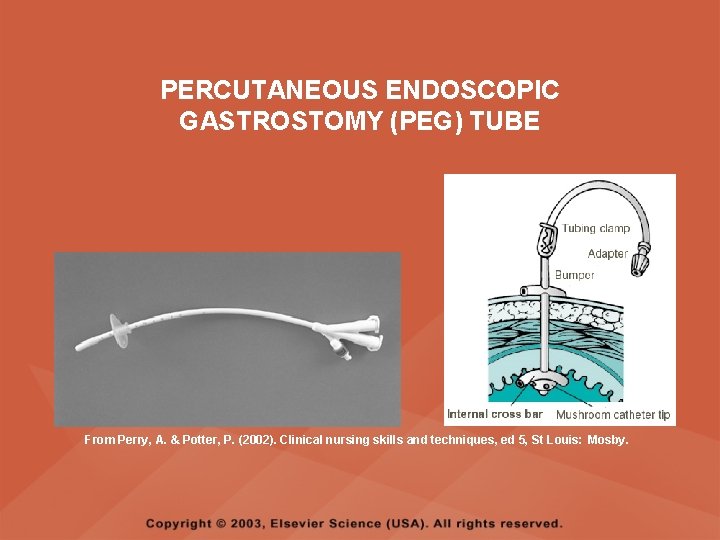
PERCUTANEOUS ENDOSCOPIC GASTROSTOMY (PEG) TUBE From Perry, A. & Potter, P. (2002). Clinical nursing skills and techniques, ed 5, St Louis: Mosby.
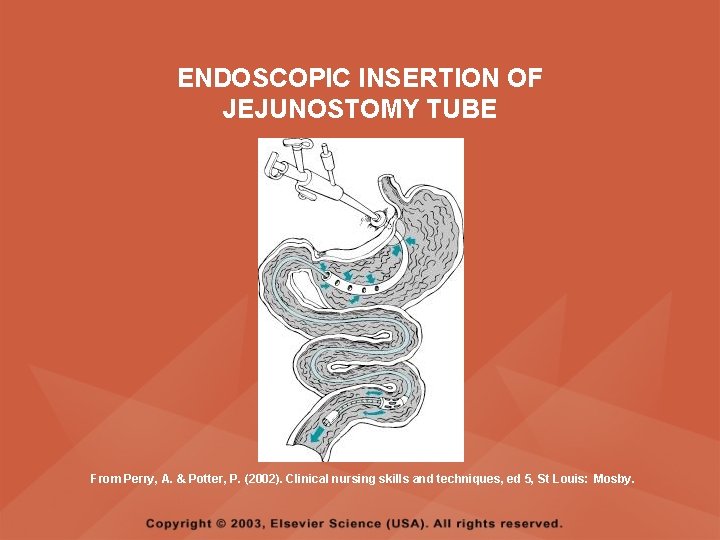
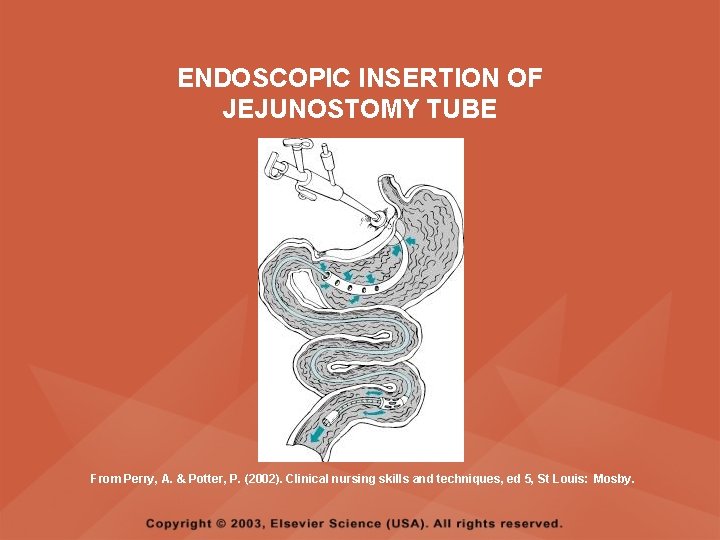
ENDOSCOPIC INSERTION OF JEJUNOSTOMY TUBE From Perry, A. & Potter, P. (2002). Clinical nursing skills and techniques, ed 5, St Louis: Mosby.
GI TUBE FEEDINGS • TYPES OF FEEDINGS – Bolus – Continuous – Cyclical
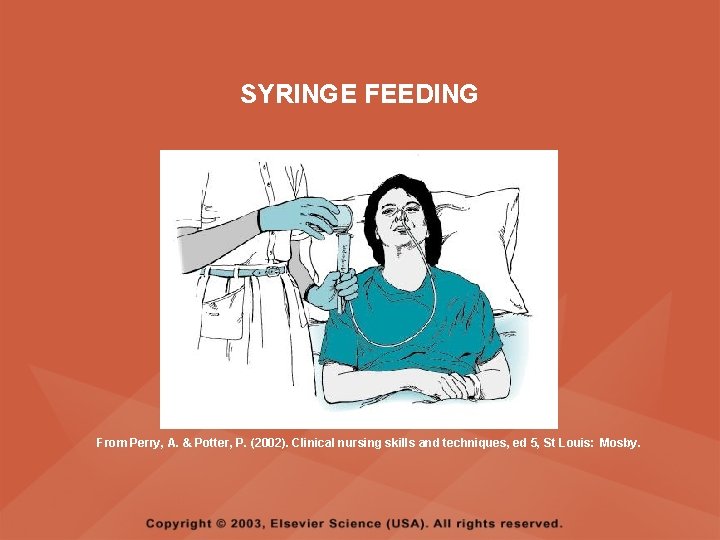
GI TUBE FEEDINGS • BOLUS – Resembles normal meal feeding patterns – Can be administered via a syringe or via an intermittent feeding – With an intermittent feeding, approximately 300 to 400 ml of formula is administered over a 30 to 60 -minute period every 3 to 6 hours
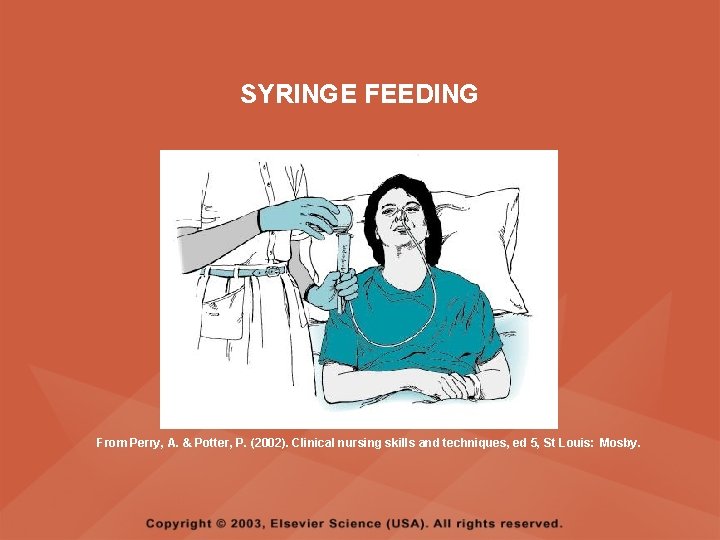
SYRINGE FEEDING From Perry, A. & Potter, P. (2002). Clinical nursing skills and techniques, ed 5, St Louis: Mosby.
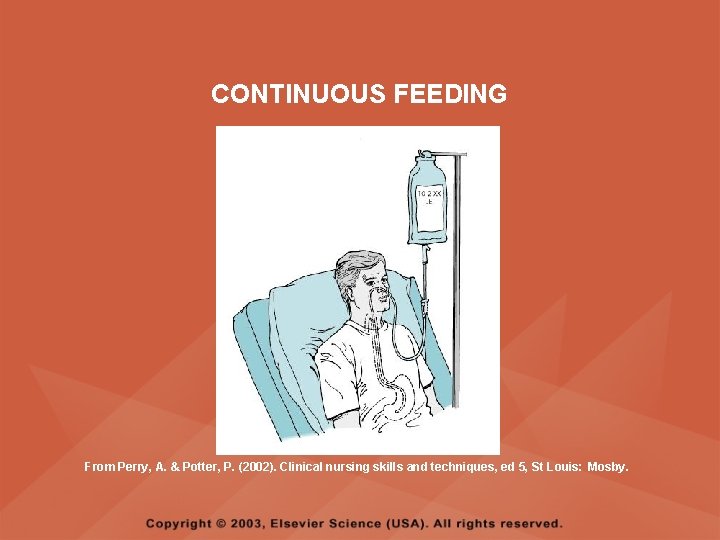
GI TUBE FEEDINGS • CONTINUOUS – Administered continuously for 24 hours – An infusion pump regulates the flow • CYCLICAL – Administered either in the daytime or nighttime for 8 to 16 hours – An infusion pump regulates the flow – Feedings at night allow for more freedom during the day
CONTINUOUS FEEDING From Perry, A. & Potter, P. (2002). Clinical nursing skills and techniques, ed 5, St Louis: Mosby.
ADMINISTERING GI TUBE FEEDINGS • Position the client in high-Fowler’s and on the right side if comatose • Warm feeding to room temperature to prevent diarrhea and cramps • Aspirate all stomach contents (residual), measure the amount, and return the contents to the stomach to prevent electrolyte imbalances • Check physician’s order and agency policy regarding residual amounts; usually if the residual is less than 100 to 150 ml, feeding is administered; if greater than 150 ml, hold the feeding
ADMINISTERING GI TUBE FEEDINGS • Assess tube placement by aspirating gastric contents and measuring the p. H (should be 4 or less) • Assess bowel sounds; hold feeding and notify the physician if bowel sounds are absent • Use a feeding pump for continuous or cyclical feedings • For bolus feeding, leave the client in a high. Fowler’s position for 30 minutes after feeding • For a continuous or cyclical feedings, keep the client in a semi-Fowler’s position at all times
PRECAUTIONS: GI TUBE FEEDINGS • Change the feeding container and tubing every 24 hours • Do not hang more solution than will be required for a 4 -hour period to prevent bacterial growth • Check the expiration date on the formula prior to administering • Shake the formula well prior to inserting into container
PRECAUTIONS: GI TUBE FEEDINGS • Always assess placement of the tube prior to feeding • Always assess bowel sounds; do not administer any feedings if bowel sounds are absent • If an obstruction occurs, try flushing with water, saline, cranberry juice, ginger ale, or cola, if not contraindicated, after checking placement
PRECAUTIONS: GI TUBE FEEDINGS • Add a drop of methyline blue to the feeding, particularly with clients who have endotracheal or tracheal tubes; suspect tracheoesophageal fistula when blue gastric contents appear in tracheal excretion and if this is noted, notify the physician immediately • Administer feeding at prescribed rate, or via gravity flow (intermittent, bolus feedings) with a 60 -ml syringe with the plunger removed • Gently flush with 30 to 50 ml of water or normal saline (depending on agency policy) with the irrigation syringe after the feeding
COMPLICATIONS OF NG TUBE FEEDINGS • • Aspiration Vomiting Diarrhea Clogged tube
PREVENTING ASPIRATION • Verify tube placement • Do not administer feeding if residual is greater than 150 ml • Keep the head of the bed elevated • If aspiration occurs, suction as needed, assess respiratory rate, auscultate lung sounds, monitor temperature for aspiration pneumonia, and prepare to obtain chest radiograph
PREVENTING VOMITING • Administer feedings slowly, and for bolus feedings, make the feeding last for 30 minutes • Do not allow feeding to run dry • Do not allow air to enter the tubing • Administer feeding at room temperature • Elevate the head of the bed • Administer antiemetics as prescribed • If client vomits, place in side-lying position
PREVENTING DIARRHEA • Use fiber-containing feedings • Administer feeding slowly and at room temperature
PREVENTING A CLOGGED TUBE • Use liquid forms of medication, if possible • Flush the tube with 30 to 50 ml of water or NS (depending on agency policy) before and after medication administration and before and after bolus feeding • Flush with water every 4 hours for continuous feeding
MEDICATIONS VIA A GI TUBE • Crush medications or use elixir forms of medications; assure that the medication ordered can be crushed or that the capsule can be opened • Dissolve crushed medication or capsule contents in 5 to 10 ml of water • Check placement and residual prior to instilling medications
MEDICATIONS VIA A GI TUBE • Draw up the medication into a catheter tip syringe, clear excess air, and insert medication into the tube • Flush with 30 to 50 ml of water or NS (depending on agency policy) • Clamp the tube for 30 to 60 minutes (depending on medication and agency policy)
INTESTINAL TUBES • DESCRIPTION – Passed nasally into the small intestine – Used to decompress the bowel or to remove intestinal contents – Enters the small intestine through the pyloric sphincter because of the weight of a small bag of mercury at the end
TYPES OF INTESTINAL TUBES • Cantor and Harris tube • Miller-Abbott tube
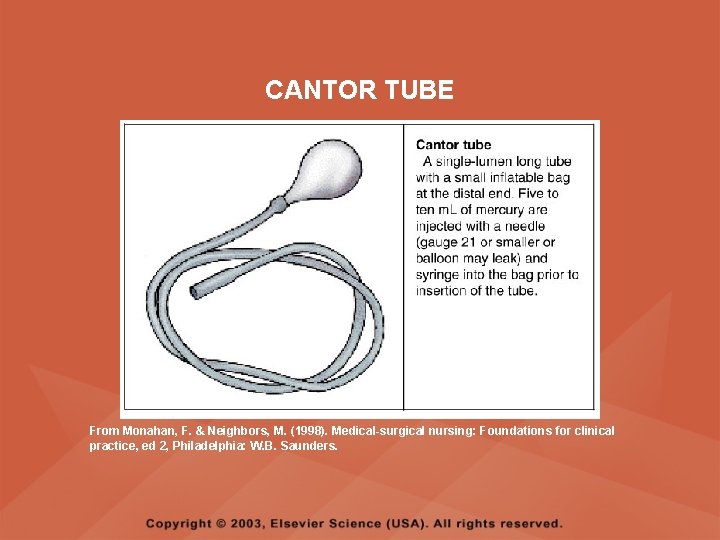
CANTOR AND HARRIS TUBE • Single-lumen tube with a reservoir for 5 to 10 ml of mercury located at its tip, below the level of the drainage holes • Mercury is inserted before the tube is passed through the nose, making the procedure uncomfortable • The Harris tube is also used for lavage and suction
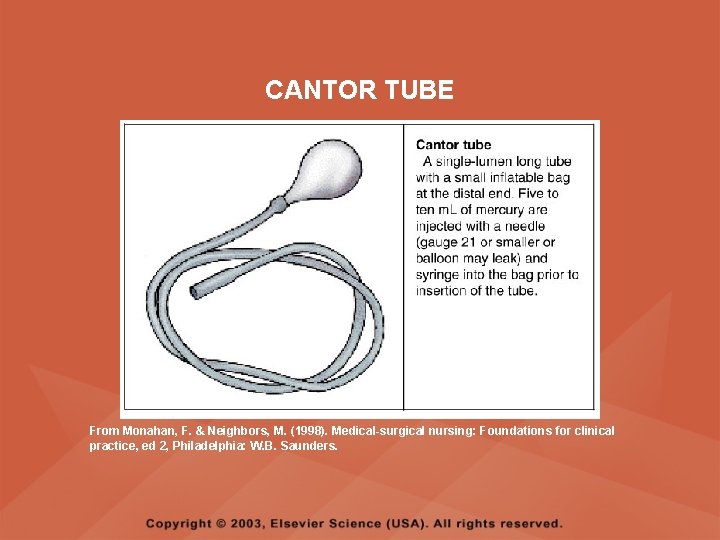
CANTOR TUBE From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
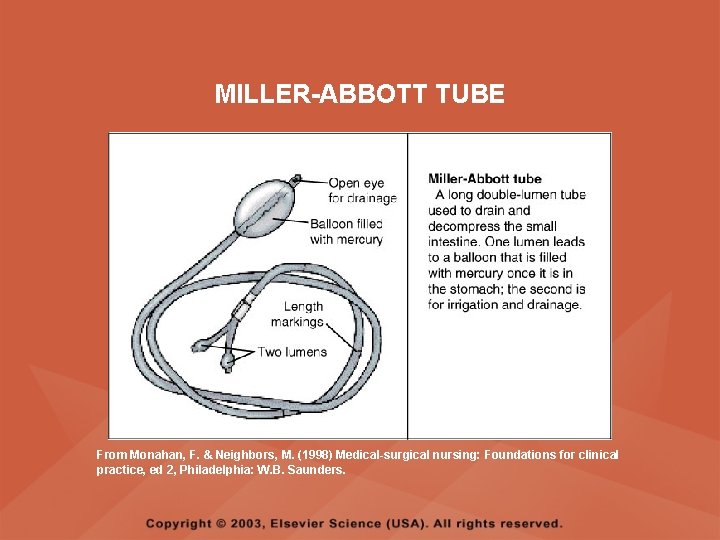
MILLER-ABBOTT TUBE • A double-lumen tube • One lumen is for the instillation of mercury once the tube is in the stomach, and the other is for irrigation or drainage
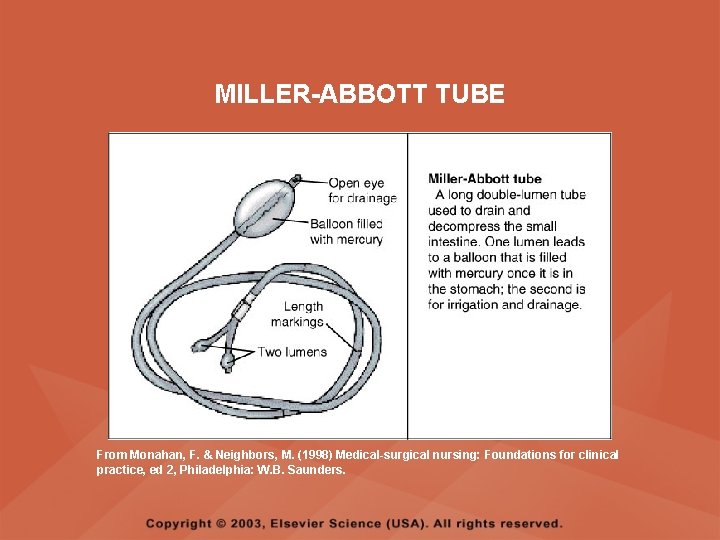
MILLER-ABBOTT TUBE From Monahan, F. & Neighbors, M. (1998) Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
INTESTINAL TUBES • IMPLEMENTATION – Assess physician’s orders and agency policy for advancement and removal of tube – Position client on the right side to facilitate passage of the mercury weights within the tube through the pylorus of the stomach and into the small intestine – Do not secure the tube to the face with tape until it has reached final placement (may take several hours) in the intestines – X-ray is performed to verify desired placement
INTESTINAL TUBES • IMPLEMENTATION – Monitor drainage from the tube – If the tube becomes blocked, notify the physician; a small amount of air injected into the lumen may be prescribed to clear the tube – Assess the abdomen and measure abdominal girth
INTESTINAL TUBES • IMPLEMENTATION – To remove the tube, the mercury and air are removed from the balloon portion of the tube with a 5 -ml syringe; the tube is gradually removed (6 inches every hour) as prescribed by the physician – Dispose the mercury in the appropriate manner as per agency policy
ESOPHAGEAL AND GASTRIC TUBES • DESCRIPTION – Used to apply pressure against esophageal veins to control bleeding – Not used if the client has ulceration or necrosis of the esophagus or had previous esophageal surgery
ESOPHAGEAL AND GASTRIC TUBES • TYPES – Sengstaken-Blakemore tube – Minnesota tube
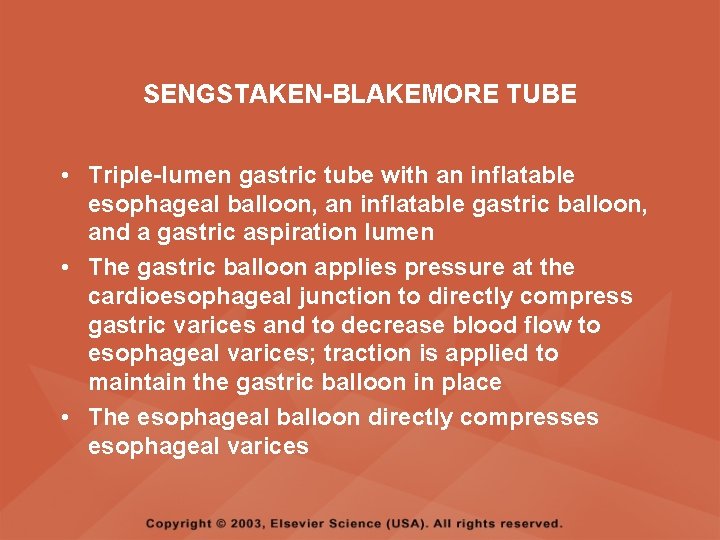
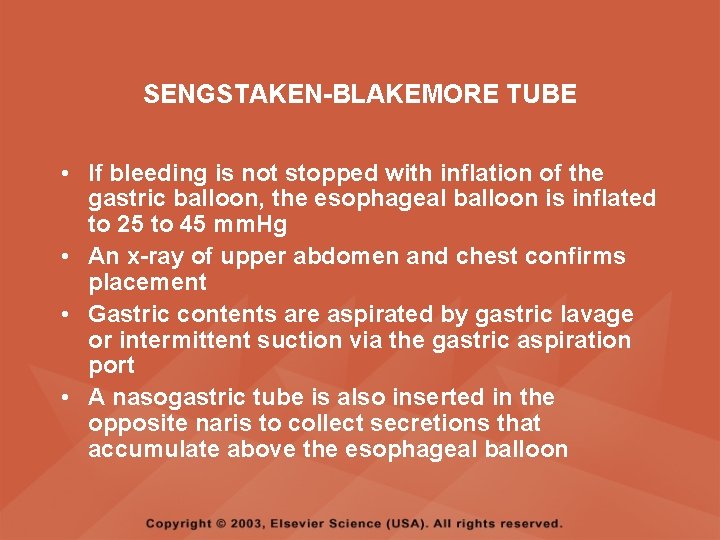
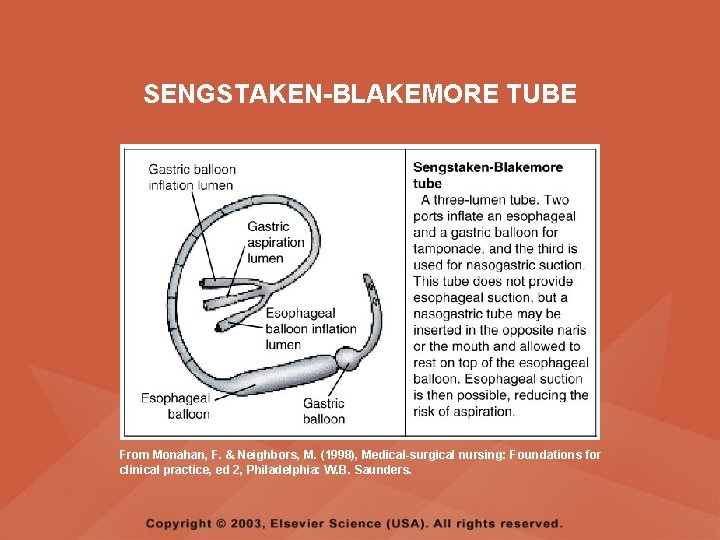
SENGSTAKEN-BLAKEMORE TUBE • Triple-lumen gastric tube with an inflatable esophageal balloon, an inflatable gastric balloon, and a gastric aspiration lumen • The gastric balloon applies pressure at the cardioesophageal junction to directly compress gastric varices and to decrease blood flow to esophageal varices; traction is applied to maintain the gastric balloon in place • The esophageal balloon directly compresses esophageal varices
SENGSTAKEN-BLAKEMORE TUBE • If bleeding is not stopped with inflation of the gastric balloon, the esophageal balloon is inflated to 25 to 45 mm. Hg • An x-ray of upper abdomen and chest confirms placement • Gastric contents are aspirated by gastric lavage or intermittent suction via the gastric aspiration port • A nasogastric tube is also inserted in the opposite naris to collect secretions that accumulate above the esophageal balloon
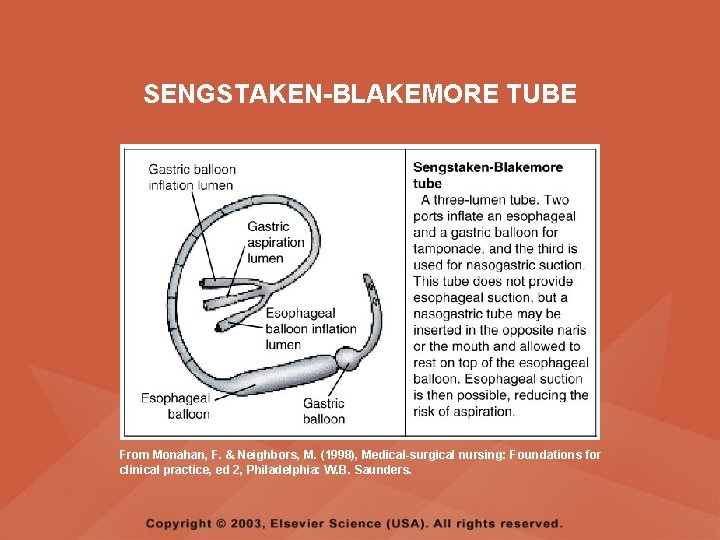
SENGSTAKEN-BLAKEMORE TUBE From Monahan, F. & Neighbors, M. (1998), Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.
MINNESOTA TUBE • Four-lumen gastric tube • A modified Sengstaken-Blakemore tube with an additional lumen for aspirating esophagopharyngeal secretions
ESOPHAGEAL AND GASTRIC TUBES • IMPLEMENTATION – Check patency and integrity of all balloons prior to insertion – Label each lumen – Place the client in the upright or Fowler’s position for insertion – Prepare for x-ray immediately after insertion to verify placement – Maintain head elevation once the tube is in place
ESOPHAGEAL AND GASTRIC TUBES • IMPLEMENTATION – Double-clamp the balloon ports to prevent air leaks – Keep scissors at the bedside at all times; monitor for respiratory distress and if it occurs, cut tubes to deflate balloons – Release esophageal pressure as prescribed and per agency policy to prevent ulceration or necrosis of the esophagus
ESOPHAGEAL AND GASTRIC TUBES • IMPLEMENTATION – Monitor for increased bloody drainage, which may indicate persistent bleeding – Monitor for signs of esophageal rupture, which includes a drop in blood pressure, increased heart rate, or back and upper abdominal pain – Esophageal rupture is an emergency and must be reported to the physician immediately
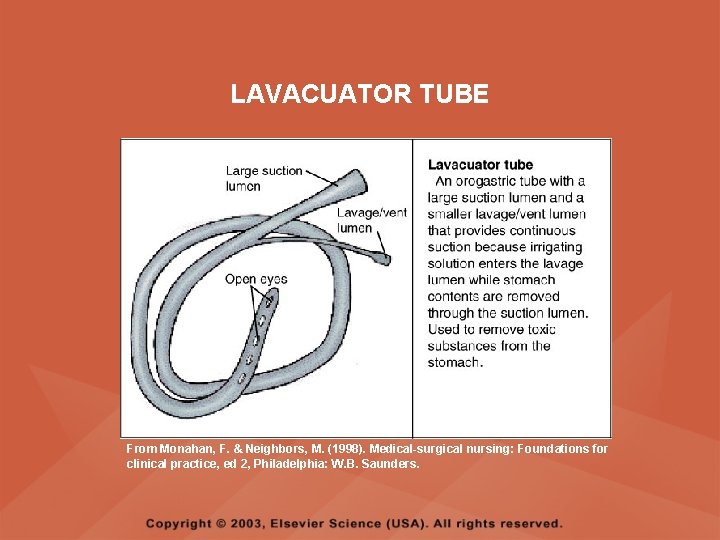
LAVAGE TUBES • DESCRIPTION – Used to remove toxic substances from the stomach
LAVAGE TUBES • LAVACUATOR – An orogastric tube with a large suction lumen and a smaller lavage/vent lumen that provides continuous suction – Irrigation solution enters the lavage lumen while stomach contents are removed through the suction lumen • EWALD’S – Reusable single-lumen large tube used for rapid one-time irrigation and evacuation
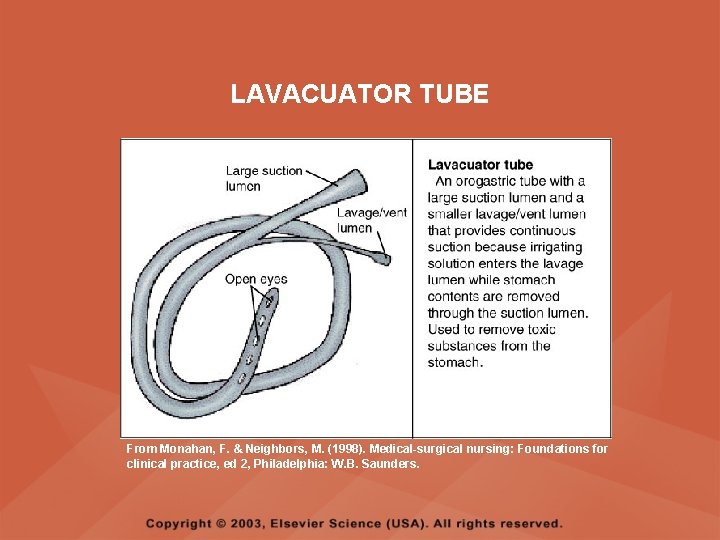
LAVACUATOR TUBE From Monahan, F. & Neighbors, M. (1998). Medical-surgical nursing: Foundations for clinical practice, ed 2, Philadelphia: W. B. Saunders.