Gastrointestinal Intubations Module 5 Gastrostomy Surgical creation of
Gastrointestinal Intubations Module 5
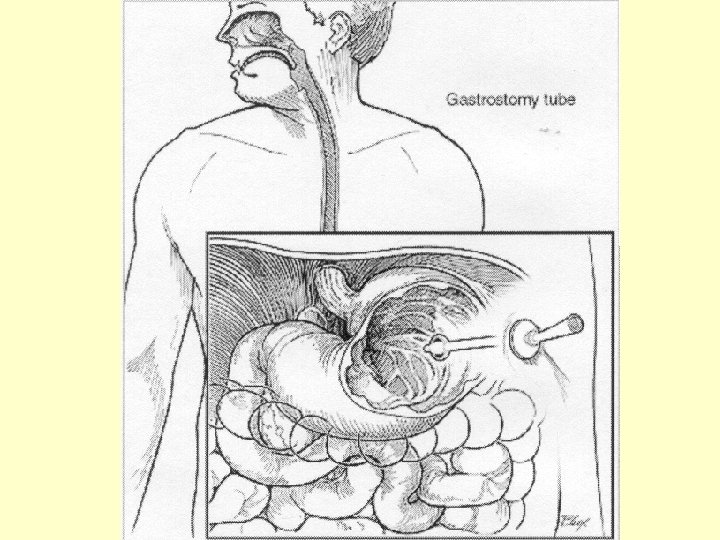
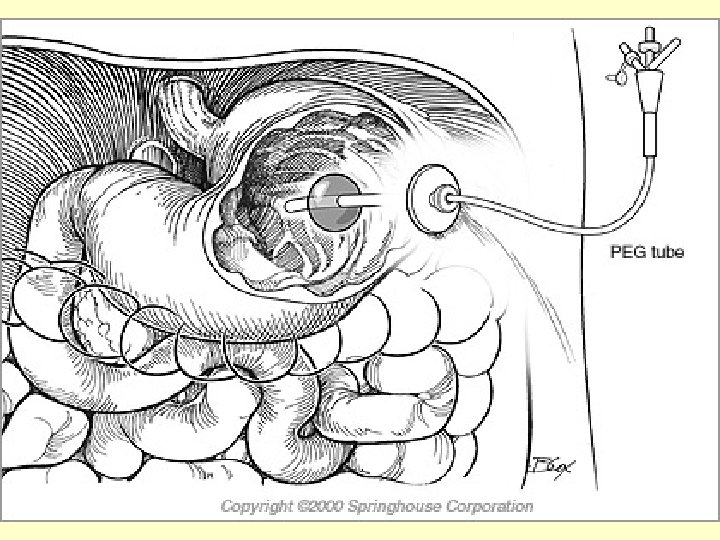
Gastrostomy • Surgical creation of a gastric fistula through the abdominal wall, necessary in some cases of cicatricial stricture of the esophagus for the purpose of introducing food into the stomach. Percutaneous endoscopic gastrostomy (PEG) • A feeding ostomy. PEG tubes are inserted through the esophagus into the stomach with the aid of an endoscope and then pulled through a stab wound made in the abdominal wall. Nasogastric • the nostril to the nasopharynx and to the stomach
Ileus • failure of appropriate forward movement of bowel contents. It may be secondary to either mechanical obstruction of the bowel or a disturbance in neural stimulation (adynamic ileus). Paralytic ileus • paralysis of the gut due to peritoneal contamination by pus (from a perforated appendix) or acid (from a perforated ulcer); • Underlying condition must be treated appropriately • Can also follow spinal cord injuries, pneumonia, and other general conditions. May occur after any abdominal surgery & can be a anticholinergic side effect of certain psychotropic drugs. • Usually temporary, with distention & symptoms of acute obstruction
Gastrointestinal Tubes • Can be inserted via – Nose – Stomach • Many types can be inserted by nurses, but some of the larger, longer or multiple lumen tubes must be inserted by physicians or nurses with advanced training
• Improper tube placement can lead to serious complications: –Esophagotracheal fistula –Gastric ulceration –Esophageal or gastric perforation –Aspiration pneumonia
GI tubes • May be inserted for the purpose of – Instilling liquid foods or other substances – Establish a means for suctioning stomach contents to prevent gastric distention, nausea & vomiting – To obtain stomach contents for lab work – To lavage stomach in cases of poisoning or overdoses – Gastric decompression (to remove gas and or fluid)
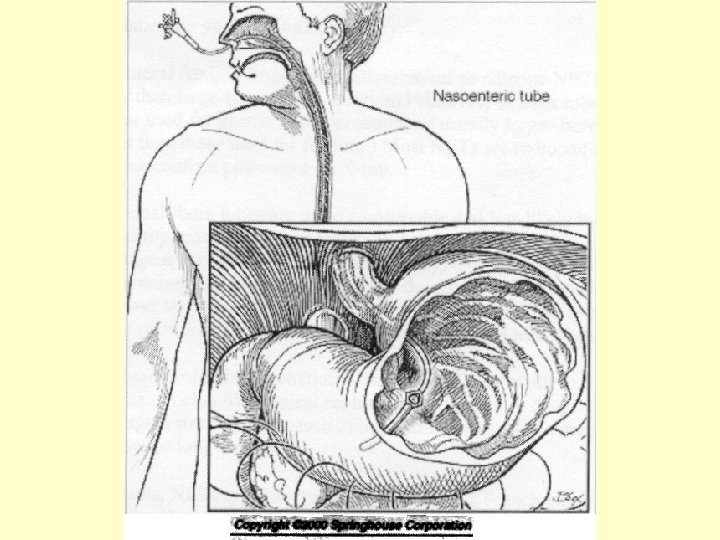
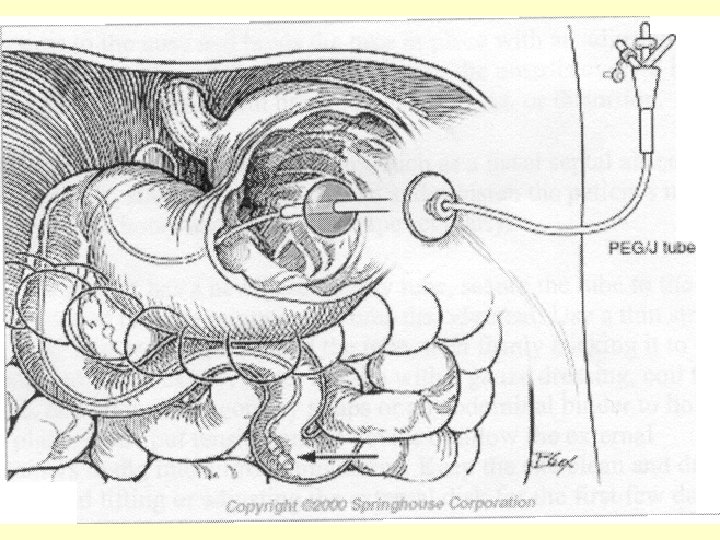
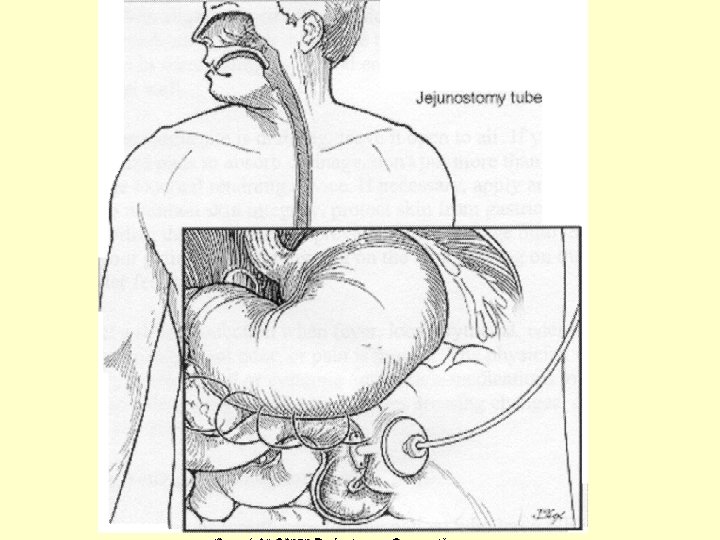
Enteral Access devices • Access can be achieved via various routes – Nasogastric = inserted thru 1 of nostrils down nasopharnyx to alimentary tract (may also go mouth down but causes gagging++ and discomfort, more often in premies) – Nasoenteric inserted same as Nasogastric but extends down into upper small intestine (used with those with high risk of aspiration) – Gastrostomy, Jejunostomy = for longer term and placed via placement thru abd wall into stomach (gastrostomy) or into jujumen (Jejunostomy)
• Nasoenteric tube (NET) is generally indicated for short-term therapy (< 6 wks) • More permanent enterostomal devices for nutrition, such as a gastrostomy or jejunostomy tube, is appropriate for therapy expected to last a month to 6 weeks or more.
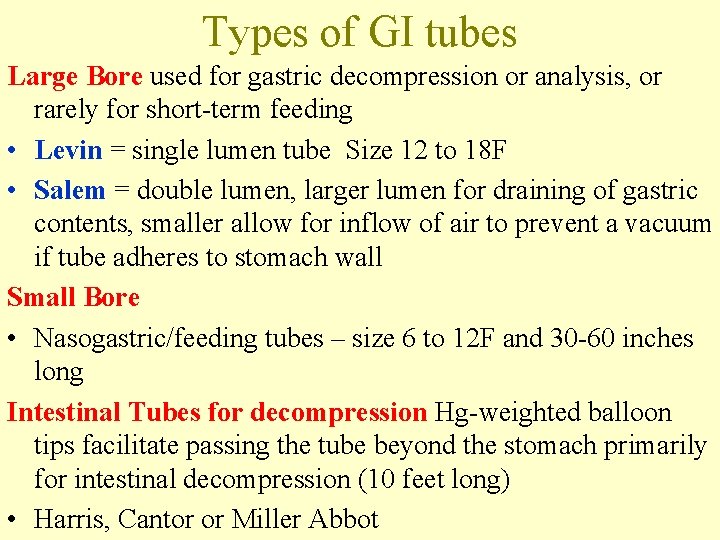
Types of GI tubes Large Bore used for gastric decompression or analysis, or rarely for short-term feeding • Levin = single lumen tube Size 12 to 18 F • Salem = double lumen, larger lumen for draining of gastric contents, smaller allow for inflow of air to prevent a vacuum if tube adheres to stomach wall Small Bore • Nasogastric/feeding tubes – size 6 to 12 F and 30 -60 inches long Intestinal Tubes for decompression Hg-weighted balloon tips facilitate passing the tube beyond the stomach primarily for intestinal decompression (10 feet long) • Harris, Cantor or Miller Abbot
Smaller diameter • Smaller diameter tubes – Clog easier esp with thick feeds or when meds are tabs that have been crushed – Can also be dislodged by vomiting or coughing – Can become knotted or kinked in GI tract – If not flushed before and after, easily become clogged requiring a change of tube – More difficult to check residual volumes
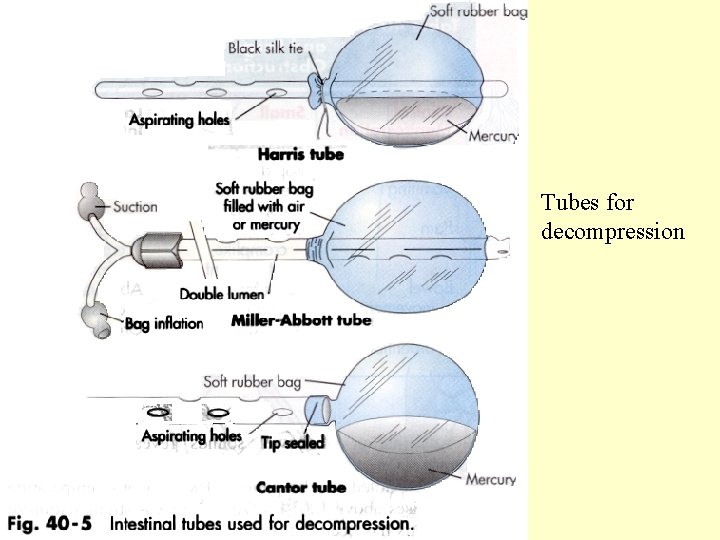
Tubes for decompression
• Tubes made of polyurethane or silicone – Radiopaque so position visible by x-ray • Tubes made of rubber or polyvinyl chloride stiffen with time
Procedures • • Inserting a NG tube – Kozier p. 1149 Removing NG tube – Kozier p. 1152 Managing GI suction – Kozier p. 872 Administering tube feed via NG tube – Kozier p. 1156 • Administering feed via gastrostomy or jejunostomy feed – Kozier p. 1158
Purposes of NG tubes • Decompression (remove fluids & gas from stomach) • Prevent or relieve N&V after surgery (by the decompression) • To determine amt of pressure & motor activity in GI tract • Irrigate stomach (lavage) after poisoning • Treat mechanical obstruction • Administer meds & nutrition • Obtain specimens (when pyloric or intestinal obstruction suspected)
NG tubes • Used with –Pts with intact gag & cough reflexes –Pts with adequate gastric emptying –Short term use
Inserting a NG tube • If rubber tube used, place on ice for 5 -10 mins to stiffen tube • Make sure guide wire if present is secured in position • Measure distance (NEX) • Use only water soluble lubricant (muko) not Vaseline to lubricate tube • Have pt sit upright, head back • Once tube at throat (gag) have client tilt head forward and swallow • NEVER, EVER FORCE A TUBE DOWN
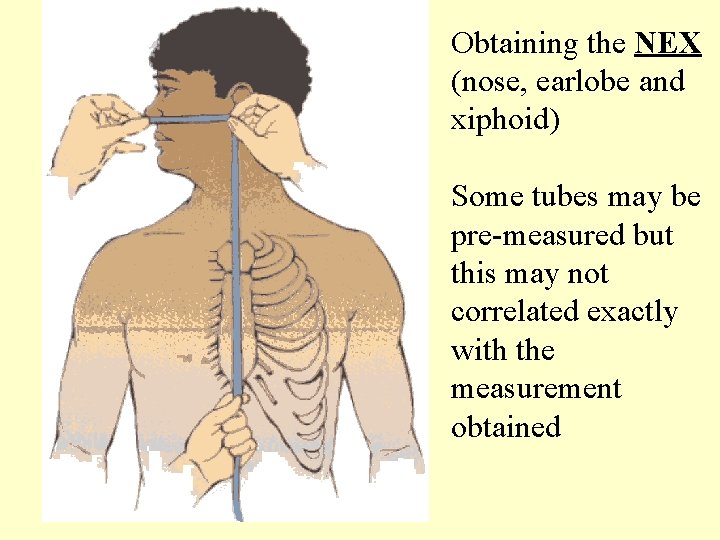
Obtaining the NEX (nose, earlobe and xiphoid) Some tubes may be pre-measured but this may not correlated exactly with the measurement obtained
TO CONFIRM PLACEMENT OF NG • • Placement most reliably confirmed by x-ray Can also aspirate for stomach contents or auscultate air insufflation 1. Aspirate for stomach contents = attach syringe to tube and apply gentle pressure. If contents return, tube is in place 2. Air insufflation = attach syringe, place stethoscope over pt’s epigastric region. Inject about 15 -20 ml of air and listen for “whoosh” 3. Ask pt to talk = if cannot talk, tube may be coiled in throat or passed through vocal cords
Methods to assess tube position • Test gastric aspirate for p. H (1 – 4 – 6 {if pt on meds for gastric acid control}) – Intestine aspirates at p. H 6 & > – Resp aspirates at 7 & > – p. H readings of 6+ indicate need for x-ray confirmation
Pt with NG tube • Will require – Inspect nose for discharge and irritation – Clean nostril and tube with moist qtips – Apply water soluble lubricant to nostril if area dry, crusted – Frequent mouth care (q 2 h) as client will be NPO
NG problem solving • Pain or vomiting after insertion = indicates tube is obstructed or incorrectly placed • Not draining = may be obstructed or needs to repositioned then checked again for placement • If pt displaying signs of distress (gasping, coughing, cyanotic) remove tube immediately
Nurses responsibility • Assess gastric contents – Color – Consistency – Odor – Amount • Irrigate tube before and after meds/feeds • Check GI function by auscultation for bowel sounds
Key Elements in insertion of NG • Minimize discomfort by positioning pt appropriately, lubricating tip and informing pt what to expect • NEVER force the tube against resistance • Confirm placement of the tube • Secure the tube to the pt’s nose or nose and cheek
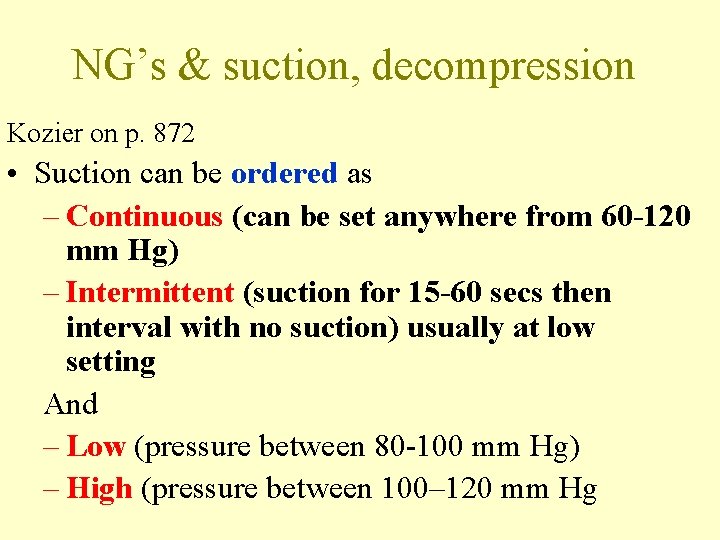
NG’s & suction, decompression Kozier on p. 872 • Suction can be ordered as – Continuous (can be set anywhere from 60 -120 mm Hg) – Intermittent (suction for 15 -60 secs then interval with no suction) usually at low setting And – Low (pressure between 80 -100 mm Hg) – High (pressure between 100– 120 mm Hg
• Can be connected to – Wall suction – Portable suction – By gravity • Before initiating, 1 st confirm tube in place • Intermittent – usually with single lumen • Continuous – usually with double lumen (Salem)
NG’s & suction, decompression… • Low continuous suction or high intermittent pressure = Salem sump tube (ie has double lumen. – Larger lumen for draining of gastric contents, smaller allow for inflow of air to prevent a vacuum if tube adheres to stomach wall • If Levin tube used, low intermittent suction recommended
Key Elements to Remove NG • Turn off suction, disconnect tube from suction • Clamp tubing before removal • Wear gloves • Withdraw tube while pt holds his breath

Part B: Enteral Feeding & Meds • Oral feeding is preferred & most effective method but there alternates for po nutrition including: 1. Enteral (thru GI system) and can be via • NG tubes • Gastrostomy or jejunostomy tubes 2. Parenteral (IV) • Alternates may deliver total or supplemental nutrition over short or long term
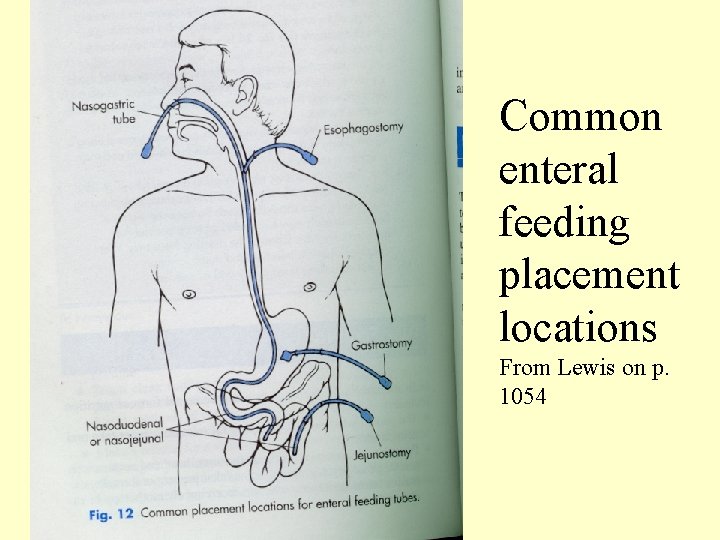
Common enteral feeding placement locations From Lewis on p. 1054
NG tubes for feeds • Until recently, large bore rubber or plastic feeding tubes were used for NG feeds. Problems with tubes (irritation, pharnygitis etc) led to development of more pliable, small bore feeding tubes • Now the are 8 -12 Fr (36 -43”long) • Have weights to assist introduction but also keep in place • Problem with smaller tubes is the difficulty to verify placement (difficult to aspirate & insufflating with air unreliable as get false positives – can sometimes hear the gurgle even if the tube is in the esophagus or lung)
Enteral Feeding & Meds • • Short term – less than 6 wks – A NG or nasointestinal tube appropriate Advantages of NG feeds: 1. Allows stomach to be used as natural reservoir (so regulates amt of food/liquid released into small intestine) 2. Presence of gastric juice may decrease risk of infection • Disadvantages of NG feeds 1. Potential aspiration into lungs 2. Uncomfortable 3. Pt’s with dysfunctional gag reflux or those unable to be in Fowler’s position not candidates
Enteral Feeding & Meds • Nasointestinal Tubes – inserted via nostril to upper portion of small intestine – Advantage: minimal risk for aspiration – Disadvantage: may develop dumping syndrome as food direct in ‘bolus’ into intestine (as pyloric valve in stomach cannot slow or regulate transit of food into intestine) • Volume of feed results in – Distention of intestine – Hypoglycemic reaction – Results in gas, bloating, crampy pain, weakness & dizziness
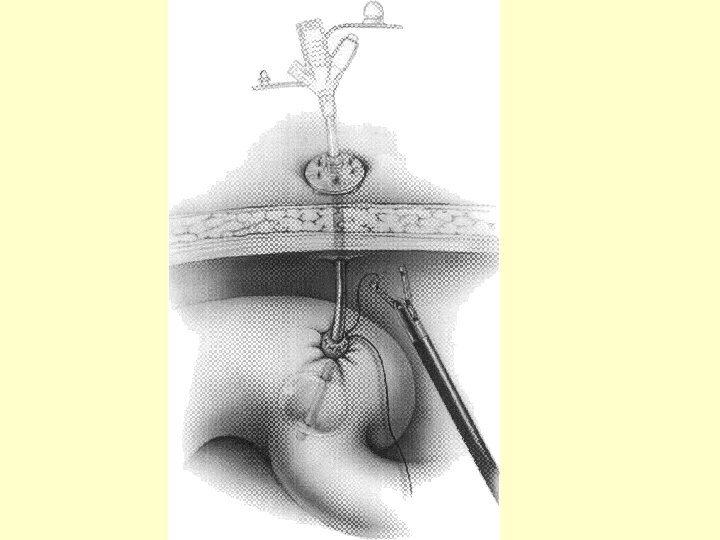
Enteral Feeding & Meds • Long Term Support accomplished by creating a an opening into: – Gastrostomy (opening into stomach) – Jejunostomy (opening into jejunum) • Methods of feeding includes: – PEG (Percutaneous endoscopic gastrostomy) – Surgical or laproscopically placed gastrostomy tube
• More & more PEG’s are popular as can be safely inserted & removed at bedside or in OPD To insert requires (by a physician) – local anesthesia, – passage of endoscope into stomach, – a small incision or stab wound thru the skin of the abdomen – pushing a cannula thru the incision – insertion of guide wire thru cannula – introduction & placement of PEG

Lewis, p. 1054
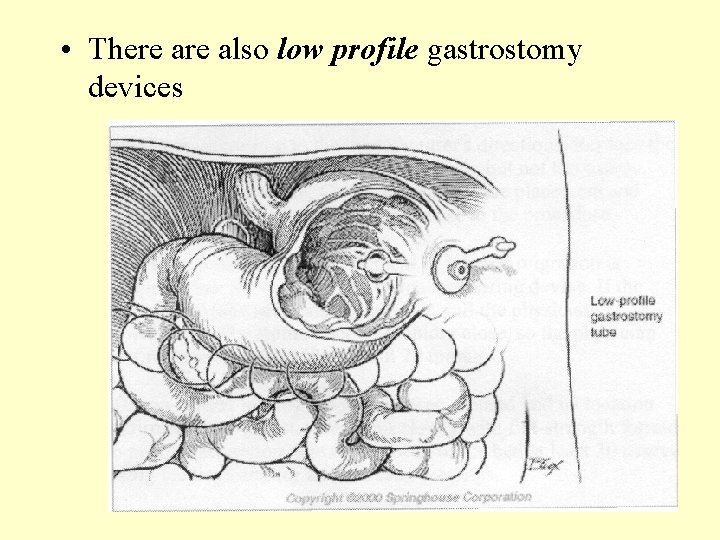
• There also low profile gastrostomy devices

Before feeds with PEG’s or NG • NG’s or NI’s placement should be confirmed: – After insertion – Before beginning meds or feeds – At regular interval during a continuous feed –Esp important with the smaller bore tubes (ie. 6 -12 FR)
• With NG’s and New PEG’s anticipate: – Measuring of residual before each feed – Measuring residual done to evaluate absorption of last feed (ie. Is there undigested formula from a previous feed) If residual is more than last infusion or 150 ml, hold feeding for 1 hour and recheck. For continuous feeds, check residual q 4 -6 hours
• Assess bowel sounds prior to each feeding or for continuous feeds, q 4 -8 h • Monitor for abdominal distention (would indicate intolerance to previous feed) • Monitor for diarrhea, constipation or flatulence (lack of bulk may cause constipation. Hypertonic or concentration of formula may cause diarrhea or flatulence)
Nursing care • Elevate head at least 30 degrees during feed and 1 hr following • Tube must be flushed before and after feeds, med admin or aspiration for patency • Delivery sets must be changed q 1224 hrs or according to policy
Nursing care • Opened cans must be stored according to manufacturer’s directions • Clean skin and stoma area at least daily, should be qshift • Mouth care q 2 -4 hours
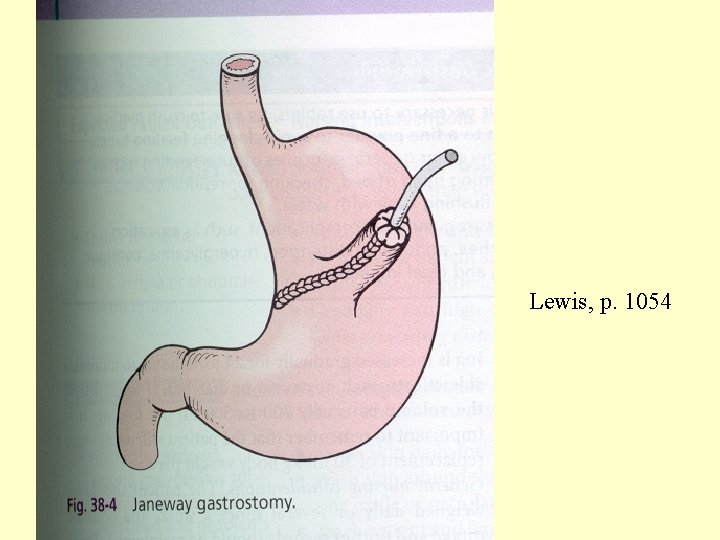
Lewis, p. 1054
- Slides: 48