GASTROINTESTINAL INFECTIONS FOOD POISONING AND SALMONELLOSIS Prof Dr







- Slides: 29
GASTROINTESTINAL INFECTIONS FOOD POISONING AND SALMONELLOSIS Prof. Dr. A. Çağrı BÜKE Yeditepe University Medical Faculty Department of Infectious Diseases 1
Ç. BÜKE Gastrointestinal Infections Gastrointestinal infections • Gastrointestinal infections have a range of clinical manifestations and can result from infection with viruses, bacteria, protozoa, or parasites • Symptoms of gastroenteritis relate to – infection at the mucosal surface, – direct microbial invasion of the gut, and/or – the effect of microbial toxins on gastrointestinal mucosal cells or on the central or enteric nervous systems 2
Ç. BÜKE Gastrointestinal Infections Source of gastrointestinal infections • Enteric pathogens are frequently transmitted through contaminated food or water, and • Some pathogens with low infectious doses may spread from person to person • These pathogens may cause outbreaks of local and international significance and are among the leading causes of childhood morbidity and mortality, particularly in the developing world • There were 1. 4 million deaths due to diarrheal diseases in 2010 and most of them was children younger than the age of 5 years 3
Ç. BÜKE Gastrointestinal Infections Gastrointestinal • 38 -year old male • Abdominal tenderness, diarrhea, weakness, fatigue • Complaints have since two days • What to do next ? • + Fever ? • He has only complain of vomiting ? 4
Ç. BÜKE Gastrointestinal Infections Gastrointestinal infections • Most gastrointestinal infections due to common bacterial and viral causes are self-limited, with symptoms resolving in a normal host usually within 7 days; • Specific microbiologic diagnosis is not necessary unless the disease is more severe or is part of an outbreak 5
Ç. BÜKE Gastrointestinal Infections Gastrointestinal infections • The term gastroenteritis is applied to syndromes of diarrhea or vomiting • Diarrhea is commonly defined as three or more loose stools in a 24 -hour period; • it is considered acute when the duration is 14 days or less and • Persistent when the duration is 14 days or longer • The term gastro-enterocolitis defines a serious condition of the gastrointestinal tract (GIT) manifested by inflammation of the stomach, small intestine and colon. 6
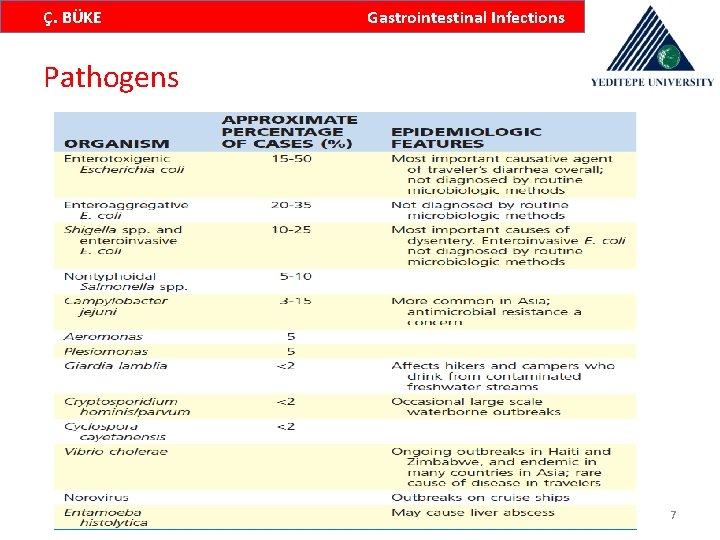
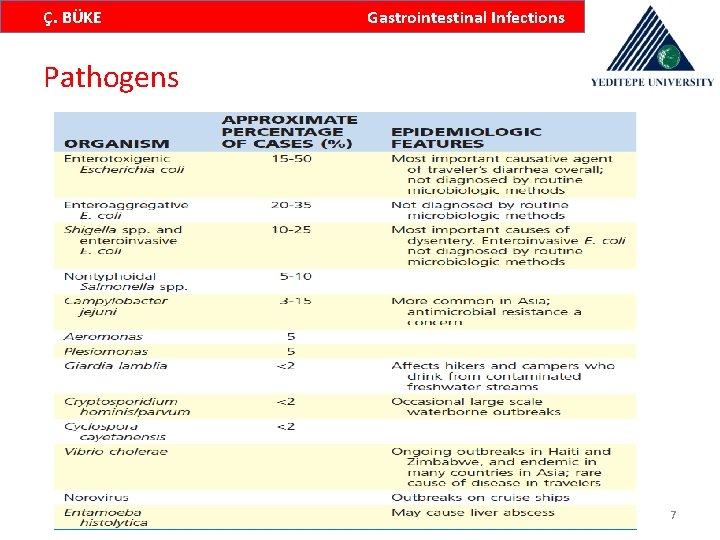
Ç. BÜKE Gastrointestinal Infections Pathogens 7
Ç. BÜKE Gastrointestinal Infections Risk factors for GIs Host factors • Age • Gastric acidity • Intestinal motiliyt • Intestinal microbiome • Immunocompromise • Genetic determinants (variant in the IL-8 promoter is associated with an increased risk for severe infection with C. difficile and enteroaggregative E. coli) • Malnutrition 8
Ç. BÜKE Gastrointestinal Infections Risk factors for GIs Microbial factors • Inoculum size – Some organisms have a very low ID 50, because they are resistant to killing by gastric acid – These organisms include; E. coli and Shigella, the cyst forms of certain parasites, including Cryptosporidium, G. lamblia, and E. histolytica, and norovirus – The ID 50 of these pathogens may be as low as 10 to 100 organisms, cysts, or viral particles; such low infectious doses may facilitate direct person-to-person spread and influence the epidemiology of these infections 9

Ç. BÜKE Gastrointestinal Infections Risk factors for GIs Microbial factors • Inoculum size – Most agents that infect the gastrointestinal tract have an intermediate ID 50, generally in the range of 103 to 108 microorganisms – Other organisms, such as Yersinia, have a higher ID 50, such as 109 or more • Adherence/Attachment • Invasions – Salmonella, Shigella, Yersinia, Campylobacter, EIEC, Entemoeba histolytica, V. parahaemolyticus 10
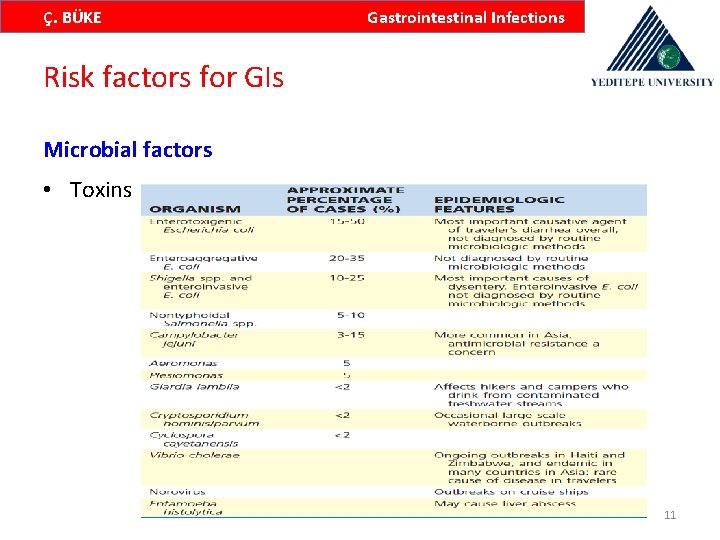
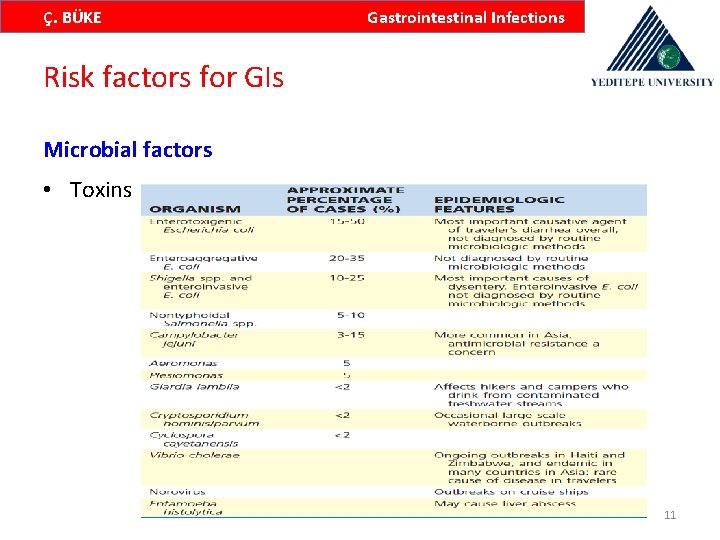
Ç. BÜKE Gastrointestinal Infections Risk factors for GIs Microbial factors • Toxins 11

Ç. BÜKE Gastrointestinal Infections Signs and symptoms of GIs 12
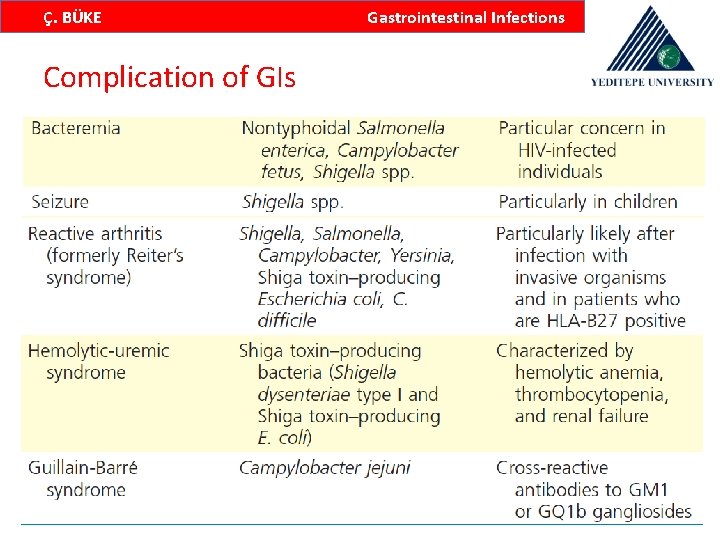
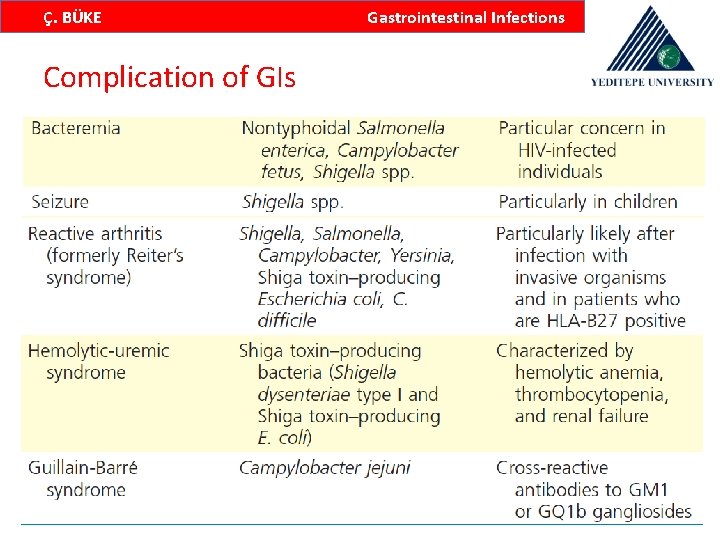
Ç. BÜKE Gastrointestinal Infections Complication of GIs 13
Ç. BÜKE Gastrointestinal Infections Diagnosis • The history should focus on recent travel, specific items in the diet, animal and other epidemiologic exposures, recent and current medications, and underlying medical conditions, particularly immunosuppressive conditions • The nature of the symptoms (vomiting, type of diarrhea watery, mucus, or blood and the presence of fever or other systemic symptoms) should also be explored 14
Ç. BÜKE Gastrointestinal Infections Diagnosis • A directed physical examination is important and should focus on; – Vital signs (particularly fever and orthostasis) – Volume status – Abdominal tenderness – Complications outside the gastrointestinal tract, and – Sensorium 15
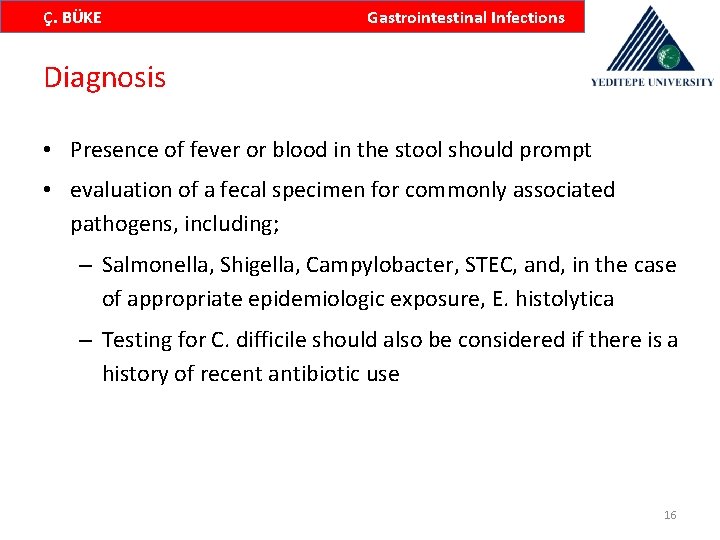
Ç. BÜKE Gastrointestinal Infections Diagnosis • Presence of fever or blood in the stool should prompt • evaluation of a fecal specimen for commonly associated pathogens, including; – Salmonella, Shigella, Campylobacter, STEC, and, in the case of appropriate epidemiologic exposure, E. histolytica – Testing for C. difficile should also be considered if there is a history of recent antibiotic use 16
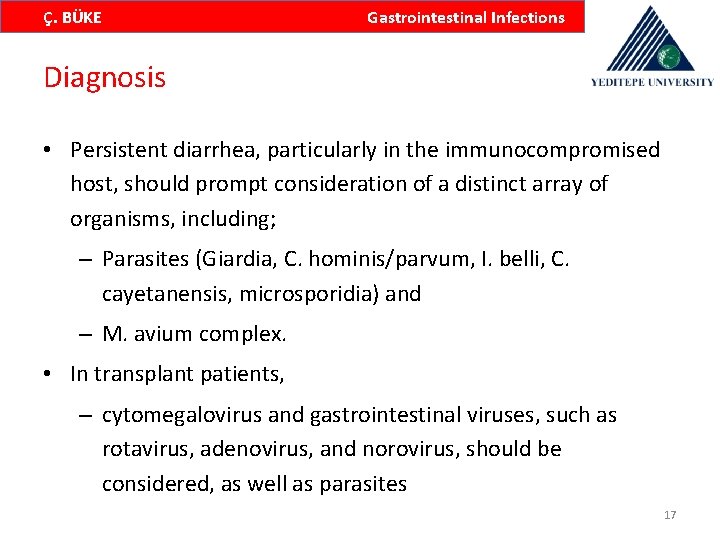
Ç. BÜKE Gastrointestinal Infections Diagnosis • Persistent diarrhea, particularly in the immunocompromised host, should prompt consideration of a distinct array of organisms, including; – Parasites (Giardia, C. hominis/parvum, I. belli, C. cayetanensis, microsporidia) and – M. avium complex. • In transplant patients, – cytomegalovirus and gastrointestinal viruses, such as rotavirus, adenovirus, and norovirus, should be considered, as well as parasites 17
Ç. BÜKE Gastrointestinal Infections Definitive diagnosis • Stool culture • Blood culture • Antigen test 18
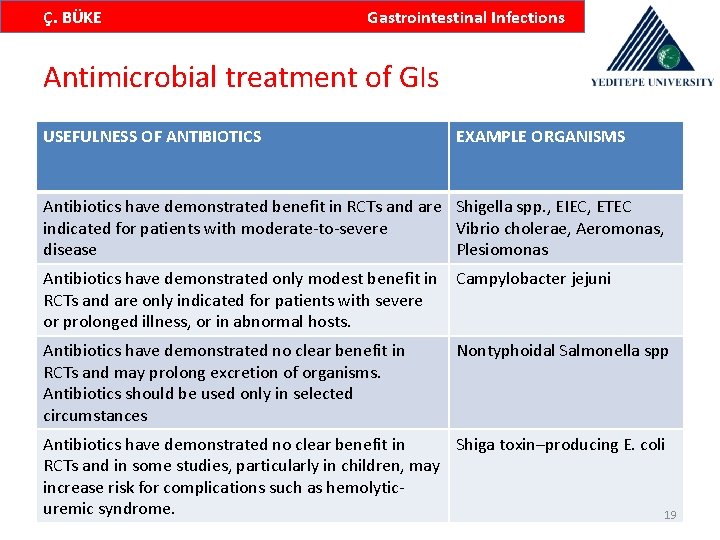
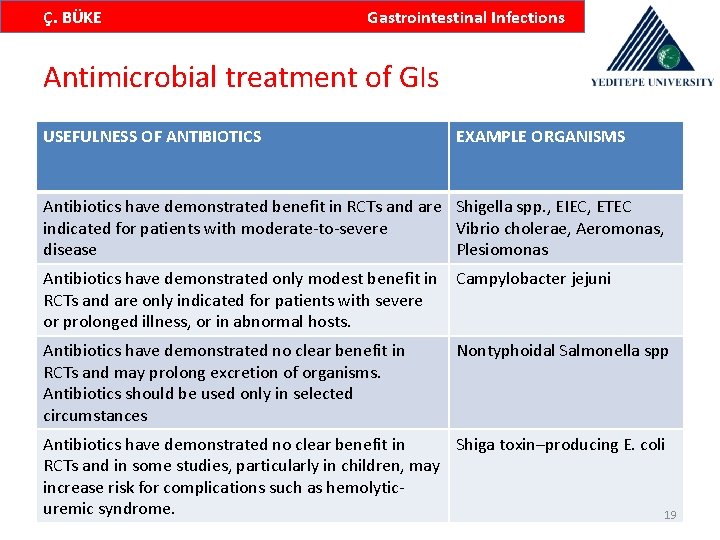
Ç. BÜKE Gastrointestinal Infections Antimicrobial treatment of GIs USEFULNESS OF ANTIBIOTICS EXAMPLE ORGANISMS Antibiotics have demonstrated benefit in RCTs and are Shigella spp. , EIEC, ETEC indicated for patients with moderate-to-severe Vibrio cholerae, Aeromonas, disease Plesiomonas Antibiotics have demonstrated only modest benefit in RCTs and are only indicated for patients with severe or prolonged illness, or in abnormal hosts. Campylobacter jejuni Antibiotics have demonstrated no clear benefit in RCTs and may prolong excretion of organisms. Antibiotics should be used only in selected circumstances Nontyphoidal Salmonella spp Antibiotics have demonstrated no clear benefit in Shiga toxin–producing E. coli RCTs and in some studies, particularly in children, may increase risk for complications such as hemolyticuremic syndrome. 19
Ç. BÜKE Gastrointestinal Infections Rehydration therapy for GIs • Rehydration is the mainstay of treatment of gastrointestinal infection. In the vast majority of cases, dehydration can be effectively treated with oral rehydration salts (ORS). 131 A reduced osmolarity ORS solution, containing 75 m. Eq/L of sodium and 75 mmol/L of glucose • Adults with severe dehydration should receive intravenous fluids. Lactated Ringer’s solution or lactated Ringer’s solution with 5% dextrose are preferred, but normal saline can also be used 20

Ç. BÜKE Gastrointestinal Infections Antimicrobial therapy for GIs • Antimicrobial therapy for patients with nontyphoidal Salmonella infection has no significant effect on the length of illness and may prolong carriage of the organism in the stool Antibiotics should given only for patients; – Severe illness – In patients older than age 50 (who are at risk for a mycotic aneurysm from bacteremic seeding of preexisting atherosclerotic plaque), – In infants younger than 12 months of age (who are at risk for Salmonella meningitis) – In individuals with cardiac or joint prostheses at risk for bacteremic seeding – In pregnant women near term, and in the immunocompromised 21
Ç. BÜKE Gastrointestinal Infections Antimicrobial therapy for GIs • Multidrug-resistance has been identified in nontyphoidal Salmonella, Shigella spp. , and V. cholerae • If antimicrobial treatment is indicated for a diarrheal disease, the choice of agent should be based on recent local susceptibility testing 22
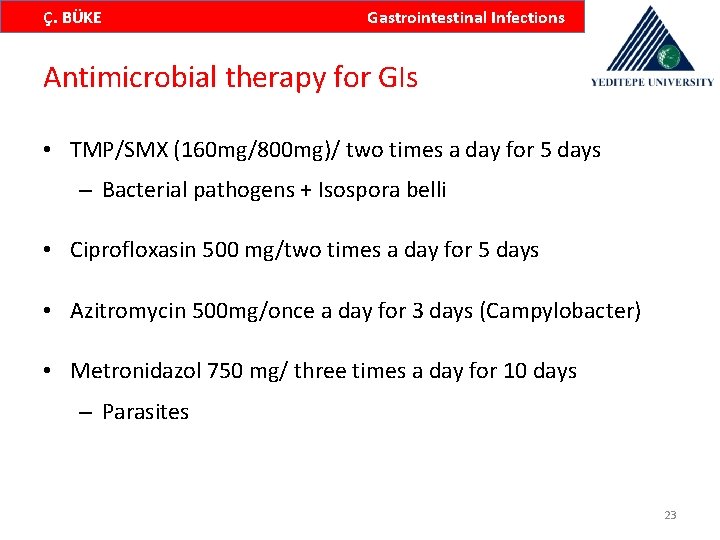
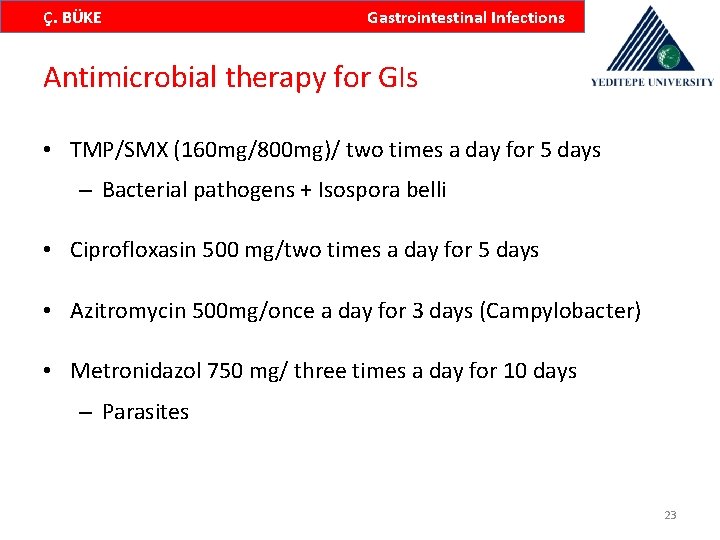
Ç. BÜKE Gastrointestinal Infections Antimicrobial therapy for GIs • TMP/SMX (160 mg/800 mg)/ two times a day for 5 days – Bacterial pathogens + Isospora belli • Ciprofloxasin 500 mg/two times a day for 5 days • Azitromycin 500 mg/once a day for 3 days (Campylobacter) • Metronidazol 750 mg/ three times a day for 10 days – Parasites 23

Ç. BÜKE Gastrointestinal Infections 24
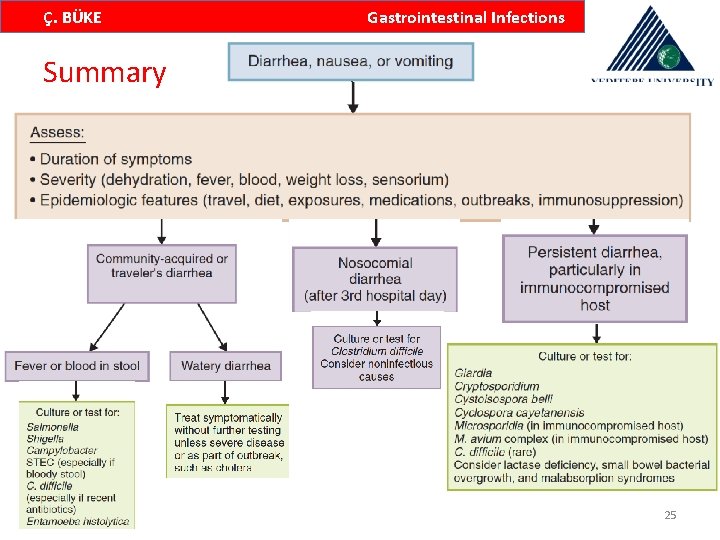
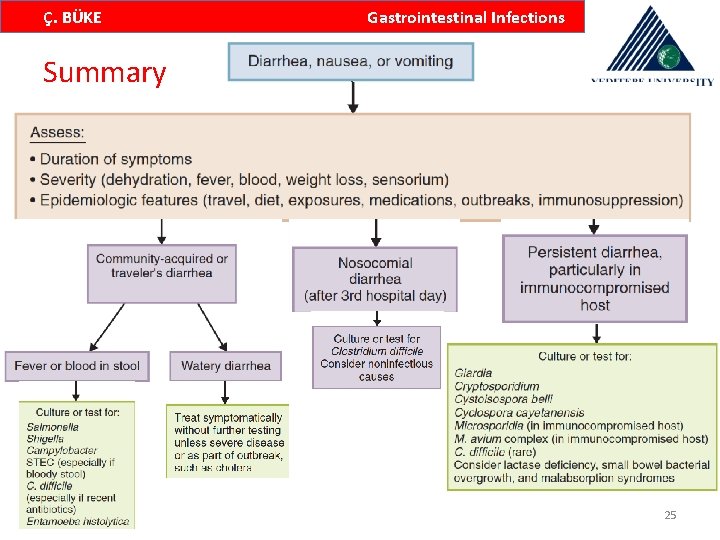
Ç. BÜKE Gastrointestinal Infections Summary 25

Ç. BÜKE Gastrointestinal Infections 26

Ç. BÜKE Gastrointestinal Infections 27
Ç. BÜKE Antibiotics Thank you for your attention 28

Ç. BÜKE Gastrointestinal Infections 29
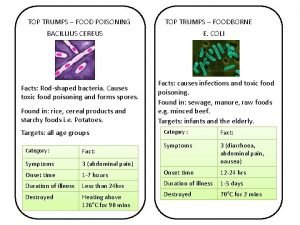
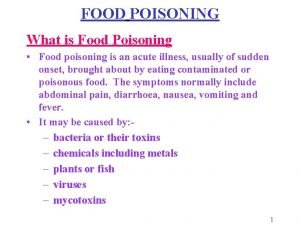
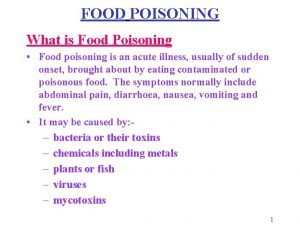
 Food top trumps
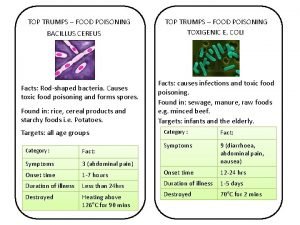
Food top trumps B. cereus food poisoning
B. cereus food poisoning Drug intoxication icd-10
Drug intoxication icd-10 Food poisoning onset
Food poisoning onset Symptoms of food poisoning
Symptoms of food poisoning Food poisoning cause
Food poisoning cause Food poisoning cause
Food poisoning cause Common factors that can lead to food poisoning
Common factors that can lead to food poisoning Sheila tarrant
Sheila tarrant Hangover or food poisoning
Hangover or food poisoning Lesson plan on food poisoning
Lesson plan on food poisoning Overall appearance
Overall appearance Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Johnson and johnson botnet infections
Johnson and johnson botnet infections Bone and joint infections
Bone and joint infections Methotrexate and yeast infections
Methotrexate and yeast infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Embriologia del sistema gastrointestinal
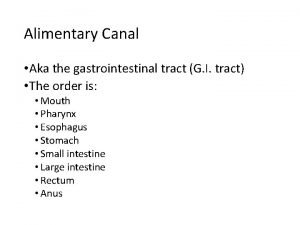
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Gastrointestinal tract
Gastrointestinal tract Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Gastrointestinal hormones
Gastrointestinal hormones Dr sigit djuniawan
Dr sigit djuniawan Lesão corto contusa
Lesão corto contusa Gastrointestinal sistem hormonları
Gastrointestinal sistem hormonları Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nutrition focused physical examination
Nutrition focused physical examination Derivatives of foregut
Derivatives of foregut Composition of stomach
Composition of stomach