Gastrointestinal Functions q Introduction q Mouth digestion q























- Slides: 90
Gastrointestinal Functions
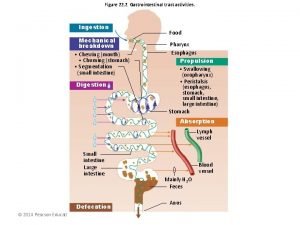
q Introduction q Mouth digestion q Stomach digestion q Small intestinal digestion q Large intestinal digestion q Absorption

Section 1 Introduction n Physiological characteristics of digestive smooth muscle n Secretion of digestive gland n Neural control of digestive tract § Gastrointestinal hormones
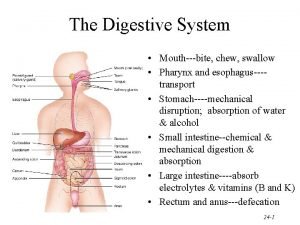
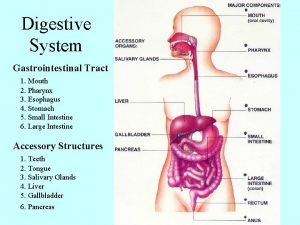
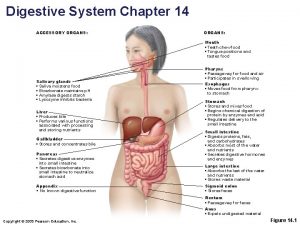
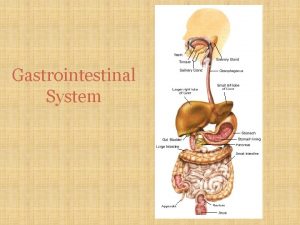
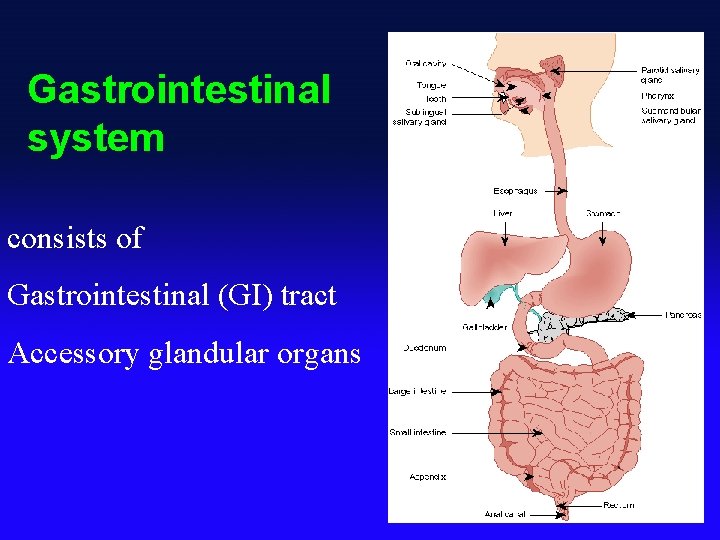
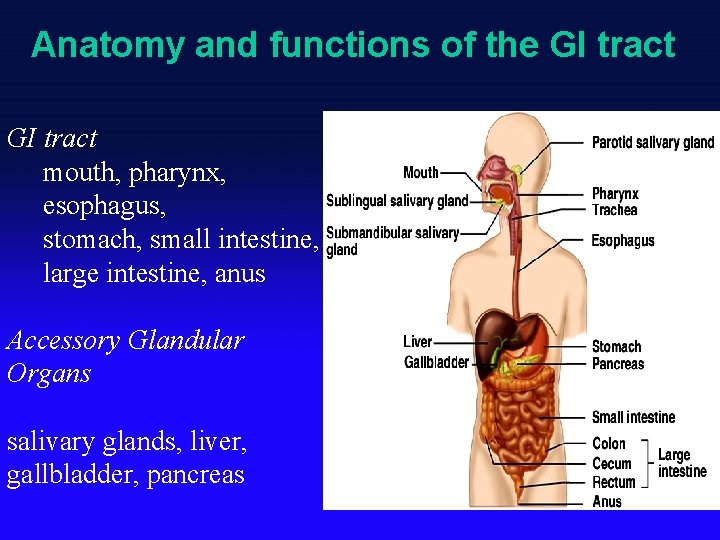
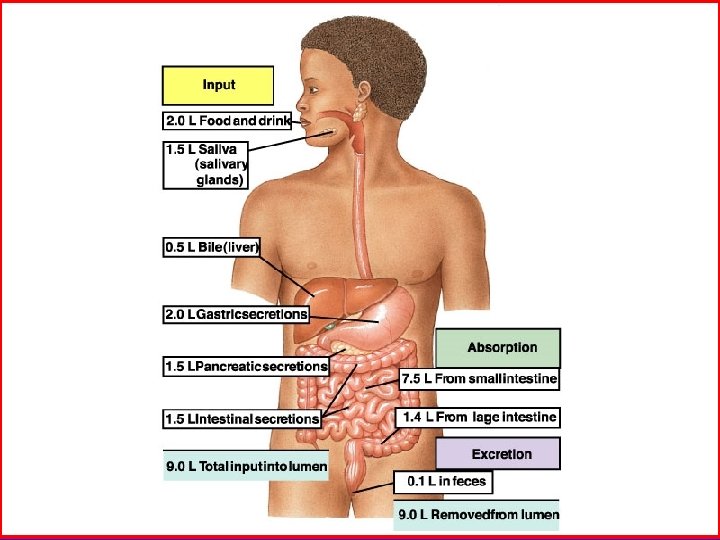
Gastrointestinal system consists of Gastrointestinal (GI) tract Accessory glandular organs
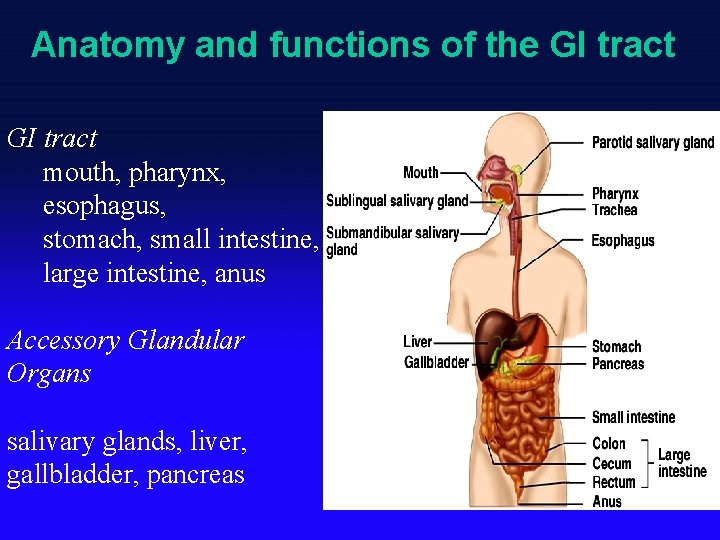
Anatomy and functions of the GI tract mouth, pharynx, esophagus, stomach, small intestine, large intestine, anus Accessory Glandular Organs salivary glands, liver, gallbladder, pancreas

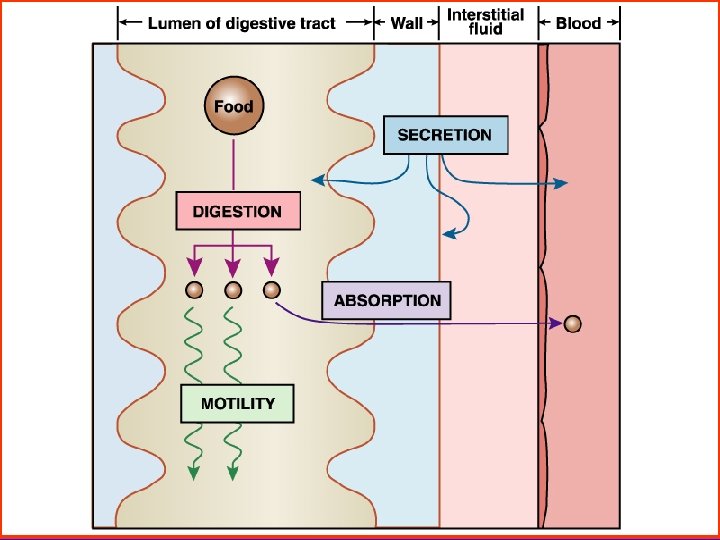
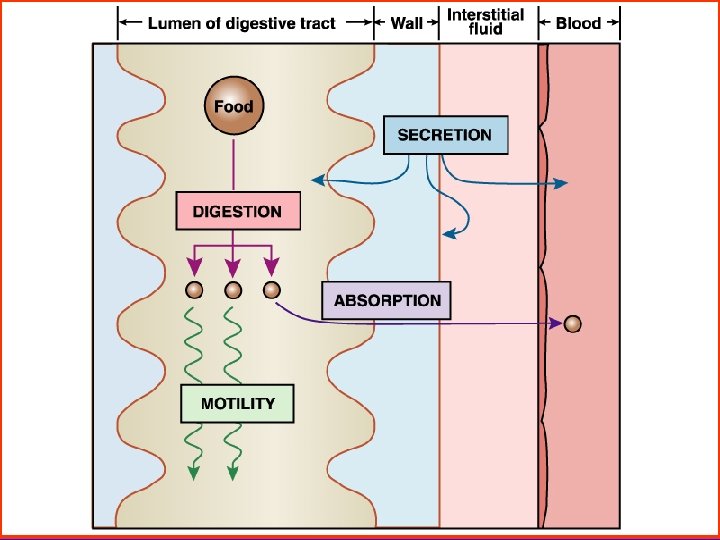
1. Definition - Digestion It shows the large molecular substances were changed into the small molecular substances. - Absorption It indicates the small molecular substances were absorbed to blood & lymph. 2. Digestive modes - Mechanical digestion: by smooth muscles of digestive tracts - Chemical digestion: by digestive enzyme
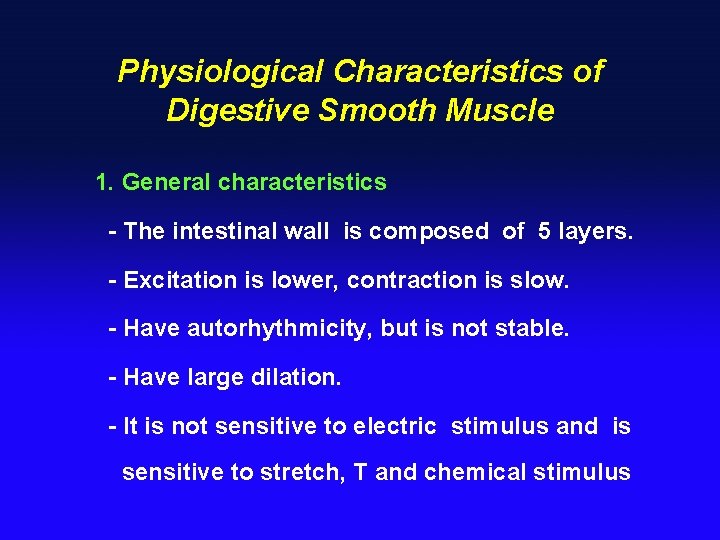
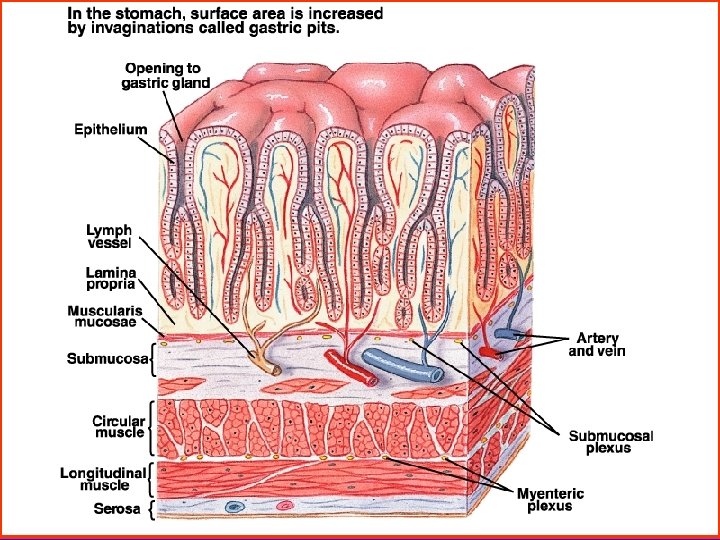
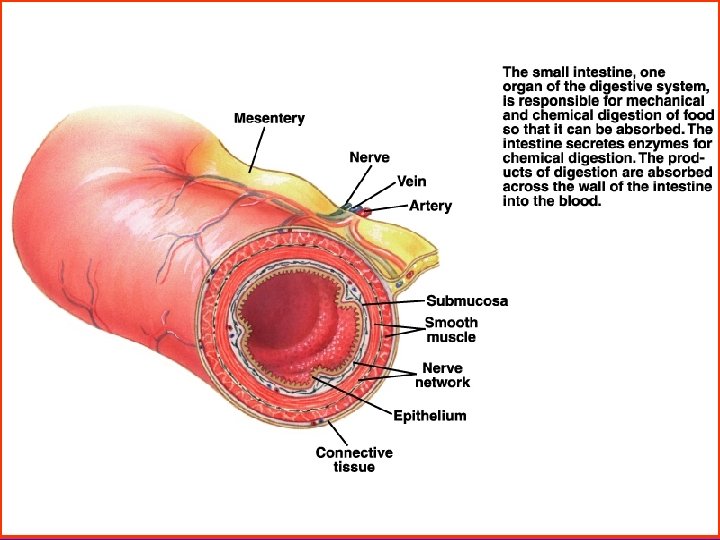
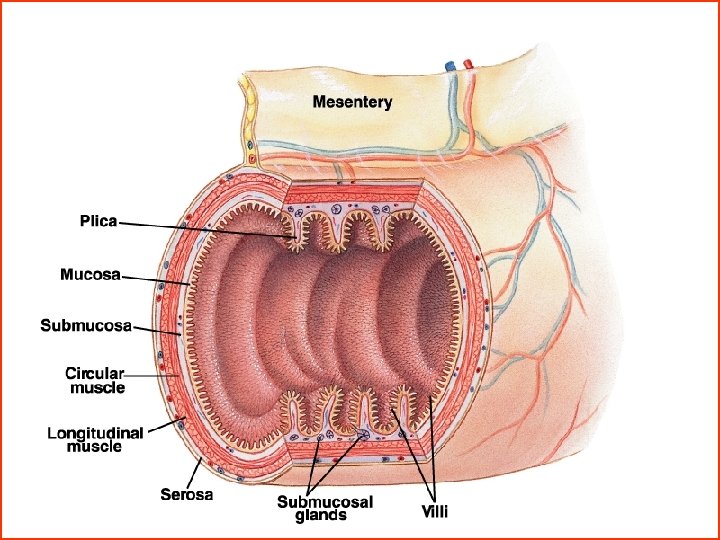
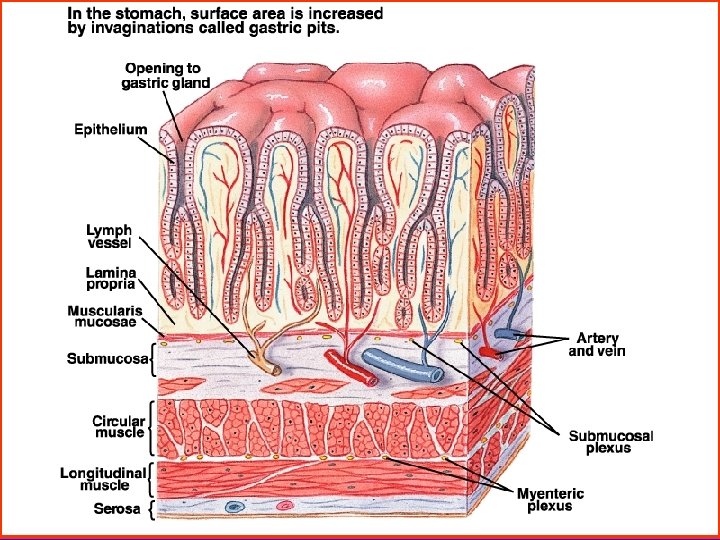
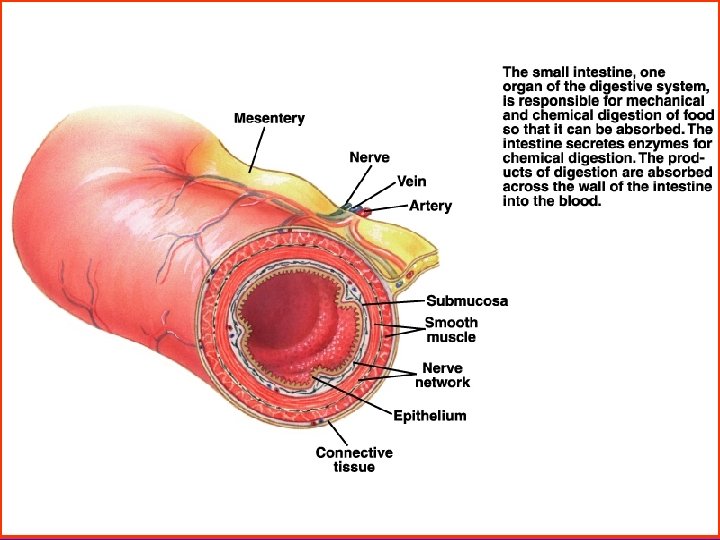
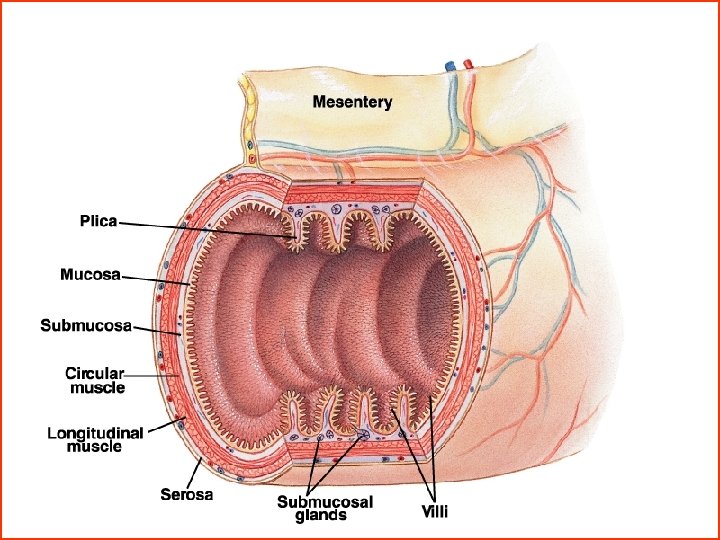
Physiological Characteristics of Digestive Smooth Muscle 1. General characteristics - The intestinal wall is composed of 5 layers. - Excitation is lower, contraction is slow. - Have autorhythmicity, but is not stable. - Have large dilation. - It is not sensitive to electric stimulus and is sensitive to stretch, T and chemical stimulus
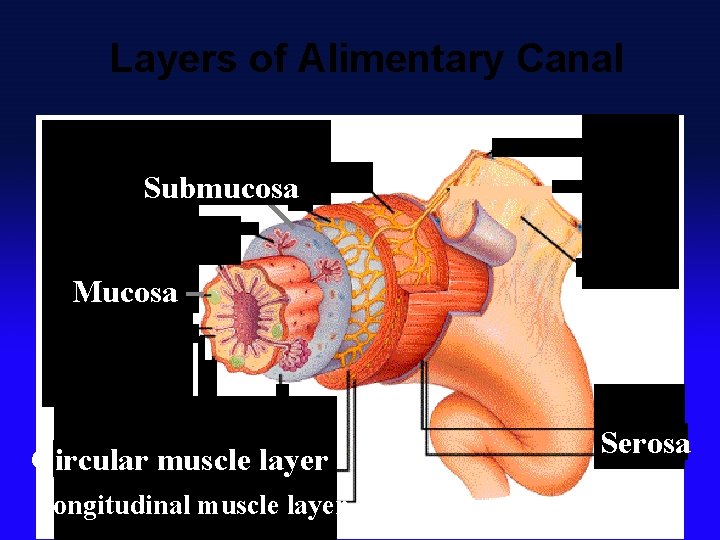
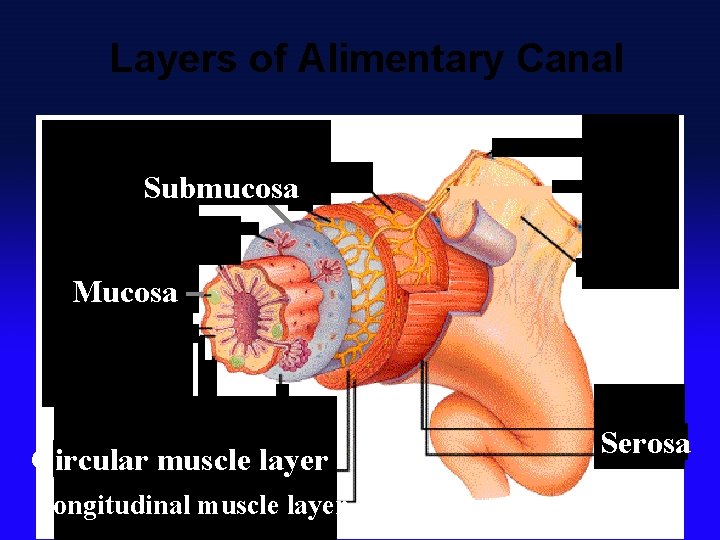
Layers of Alimentary Canal Submucosa Mucosa Circular muscle layer Longitudinal muscle layer Serosa
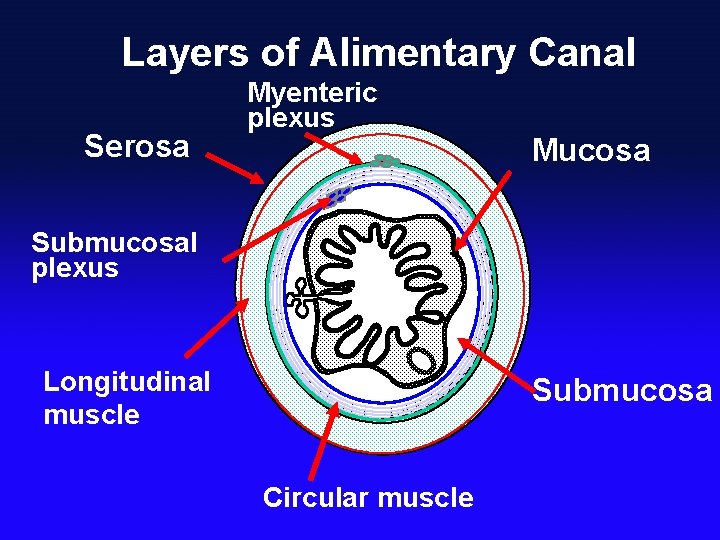
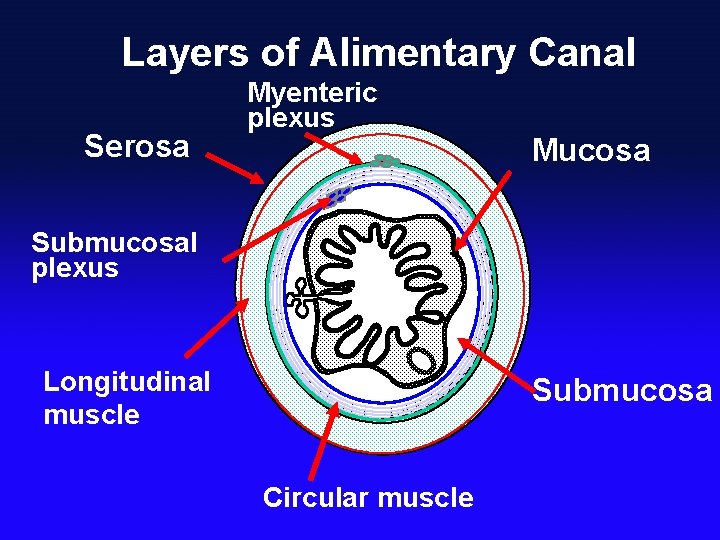
Layers of Alimentary Canal Serosa Myenteric plexus Mucosa Submucosal plexus Longitudinal muscle Submucosa Circular muscle
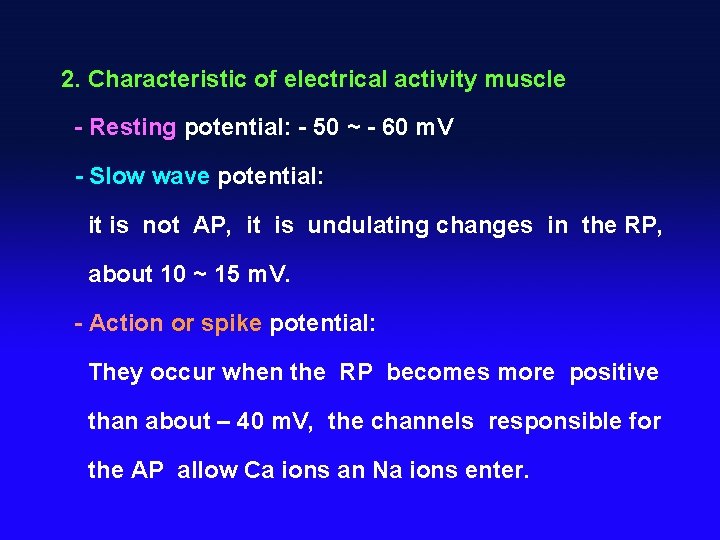
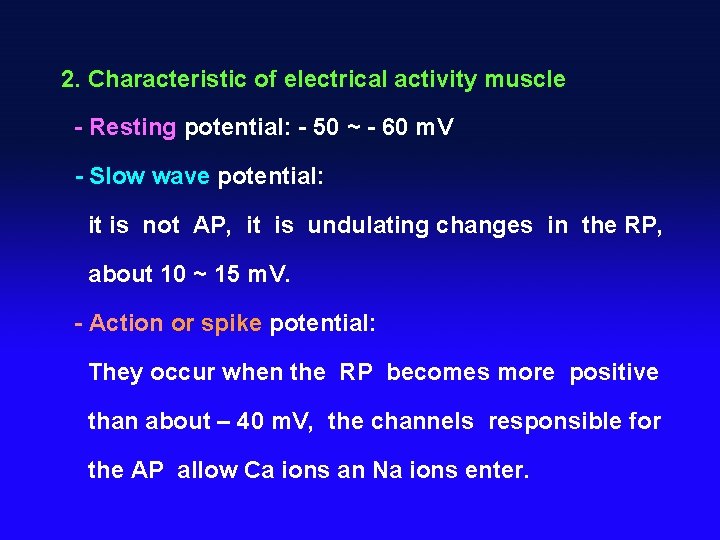
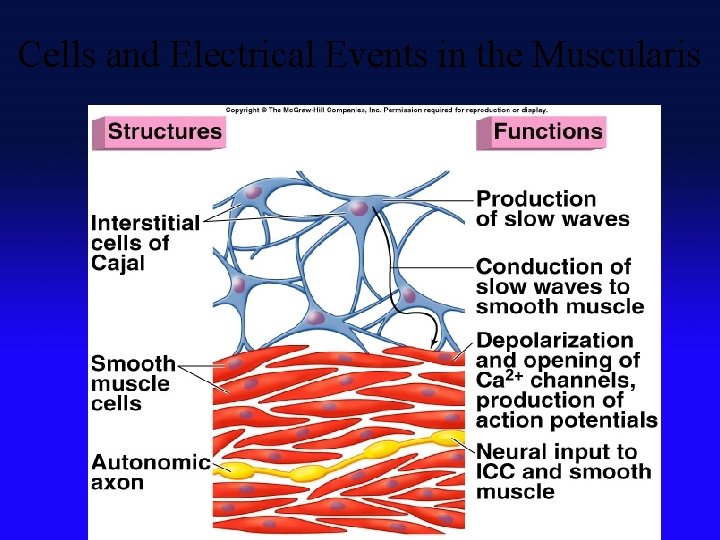
2. Characteristic of electrical activity muscle - Resting potential: - 50 ~ - 60 m. V - Slow wave potential: it is not AP, it is undulating changes in the RP, about 10 ~ 15 m. V. - Action or spike potential: They occur when the RP becomes more positive than about – 40 m. V, the channels responsible for the AP allow Ca ions an Na ions enter.
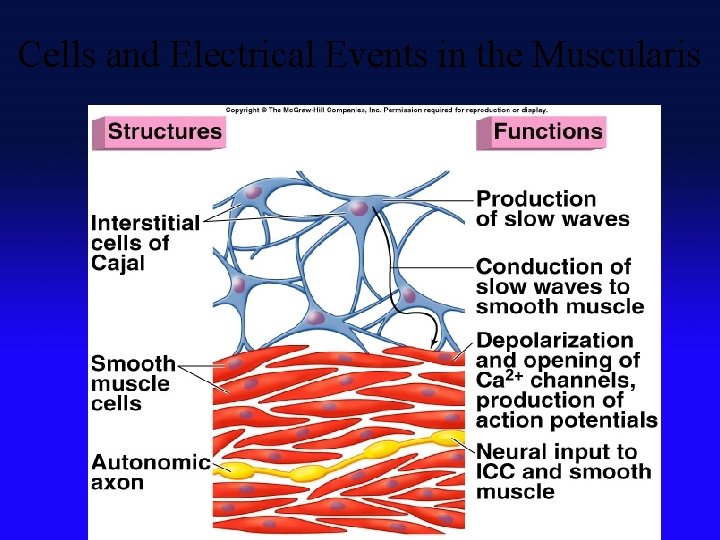
Cells and Electrical Events in the Muscularis Insert fig. 18. 16


Secretion of Digestive Gland 1. Component: Water, digestive enzyme, mucus and antibody ets. 2. Function: - digest food - provide p. H, - dilute food - protect mucosa of digestive tract.
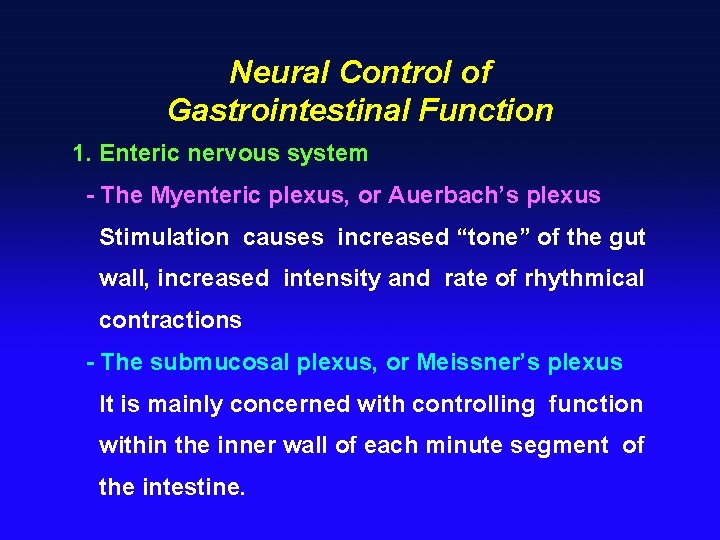
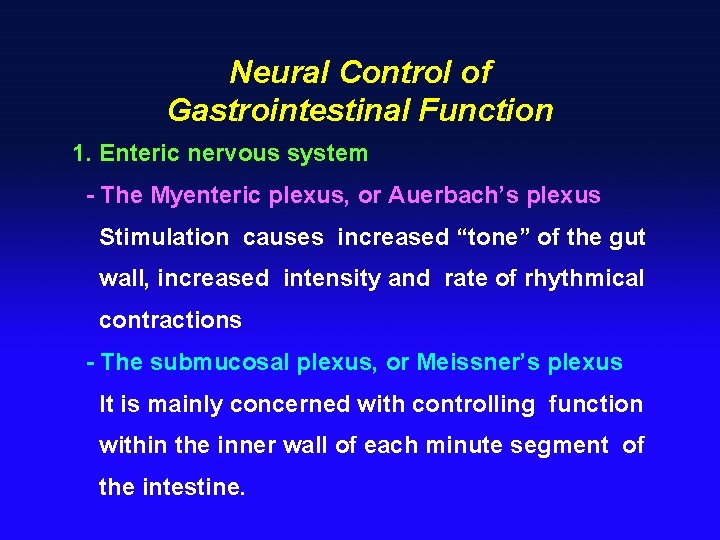
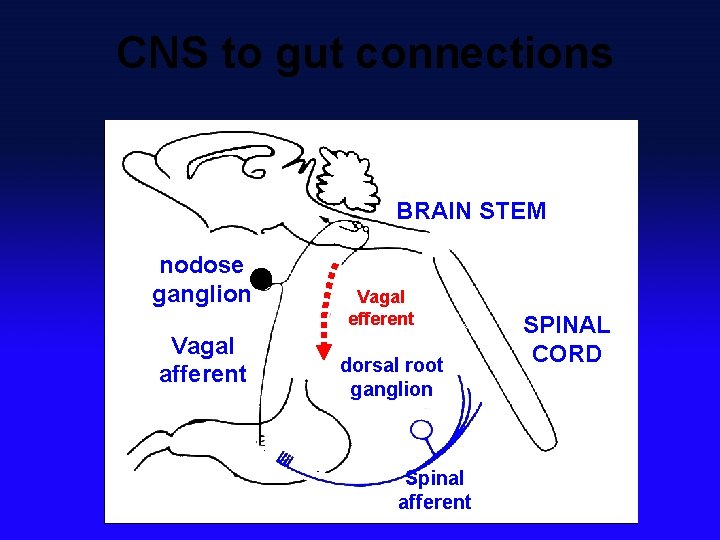
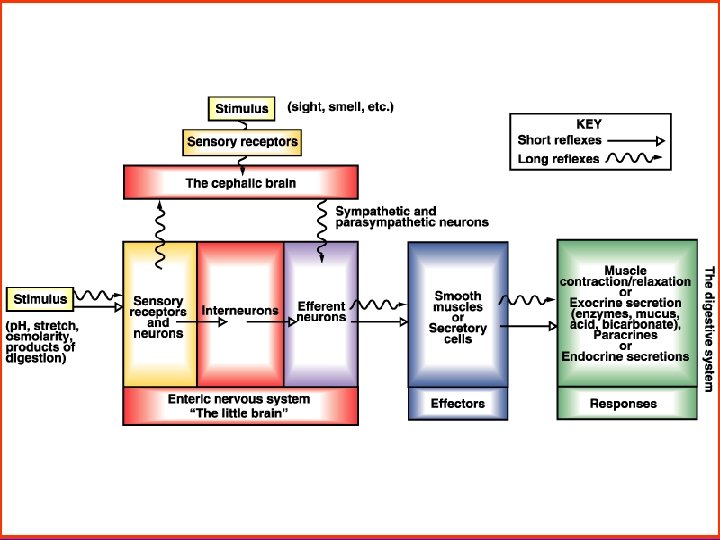
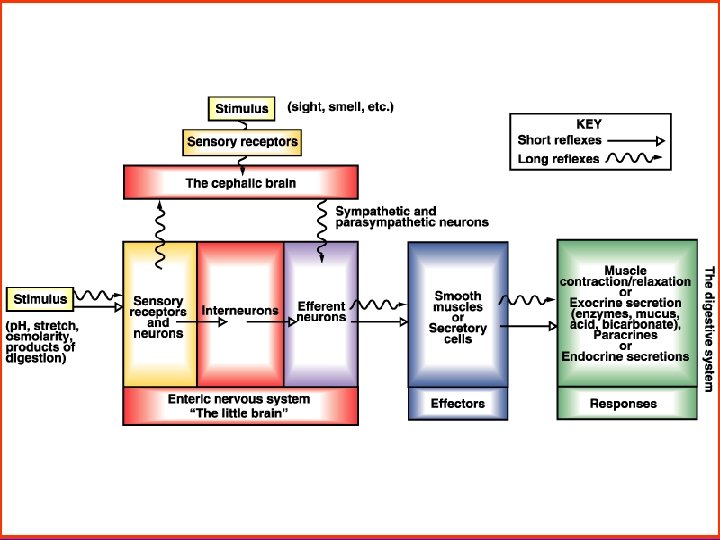
Neural Control of Gastrointestinal Function 1. Enteric nervous system - The Myenteric plexus, or Auerbach’s plexus Stimulation causes increased “tone” of the gut wall, increased intensity and rate of rhythmical contractions - The submucosal plexus, or Meissner’s plexus It is mainly concerned with controlling function within the inner wall of each minute segment of the intestine.
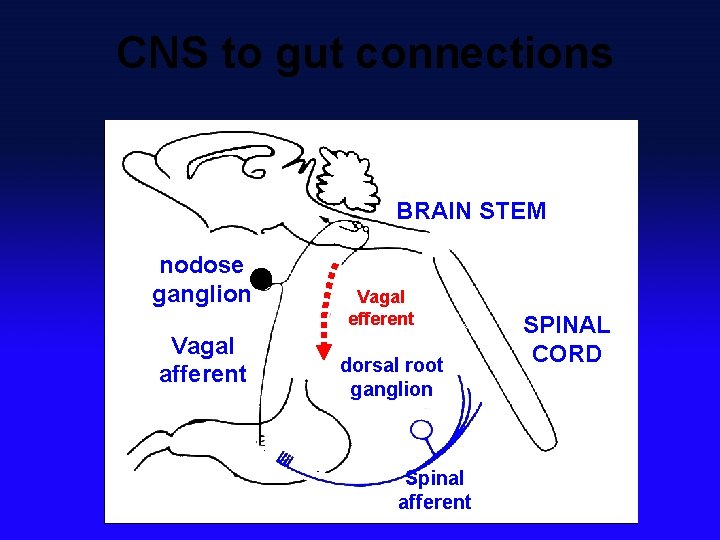
CNS to gut connections BRAIN STEM nodose ganglion Vagal afferent Vagal efferent dorsal root ganglion Spinal afferent SPINAL CORD
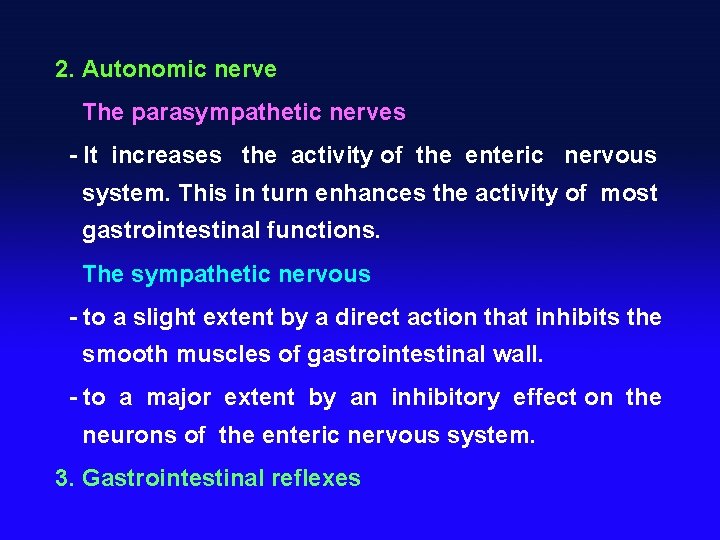
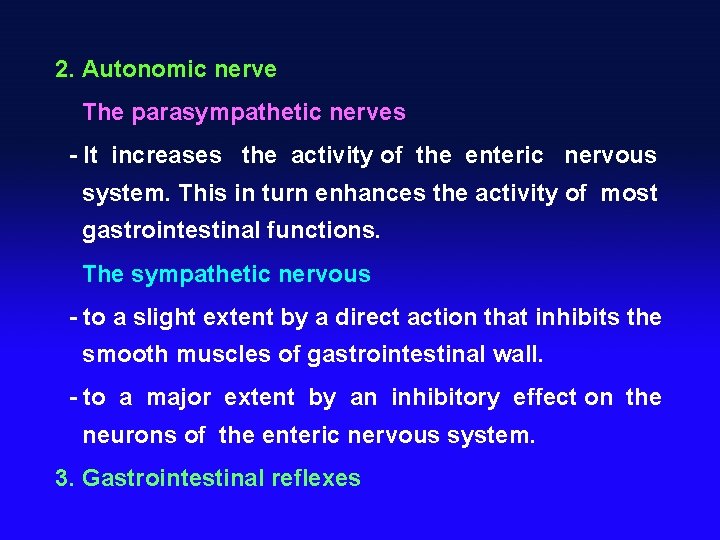
2. Autonomic nerve The parasympathetic nerves - It increases the activity of the enteric nervous system. This in turn enhances the activity of most gastrointestinal functions. The sympathetic nervous - to a slight extent by a direct action that inhibits the smooth muscles of gastrointestinal wall. - to a major extent by an inhibitory effect on the neurons of the enteric nervous system. 3. Gastrointestinal reflexes
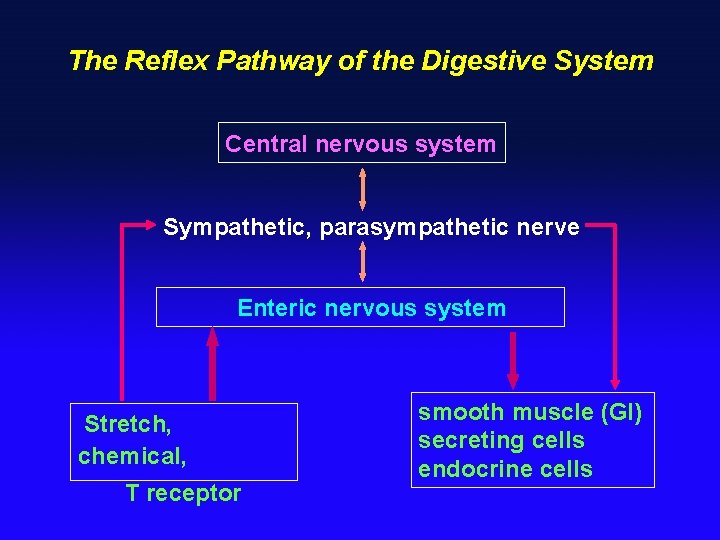
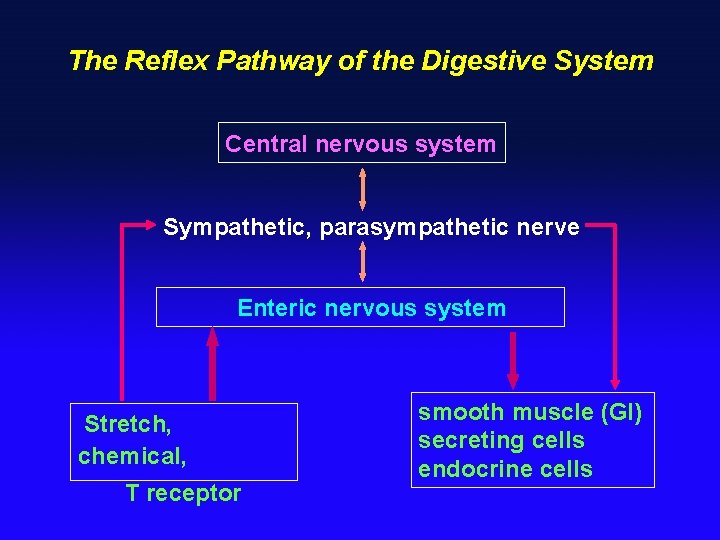
The Reflex Pathway of the Digestive System Central nervous system Sympathetic, parasympathetic nerve Enteric nervous system Stretch, chemical, T receptor smooth muscle (GI) secreting cells endocrine cells
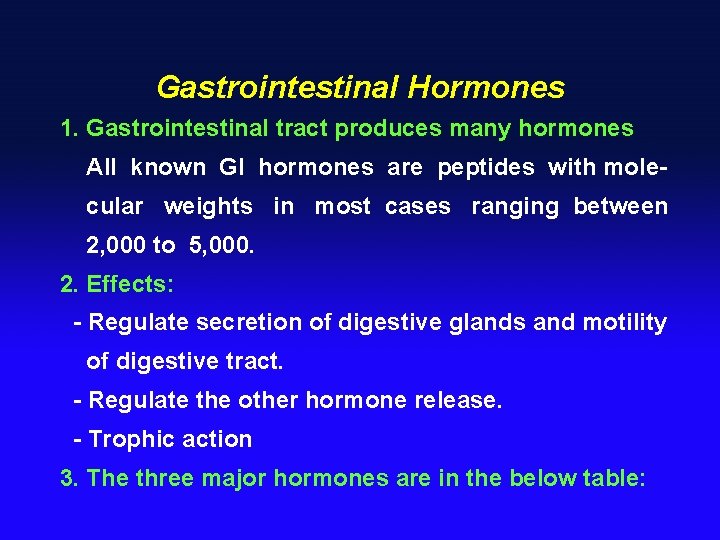
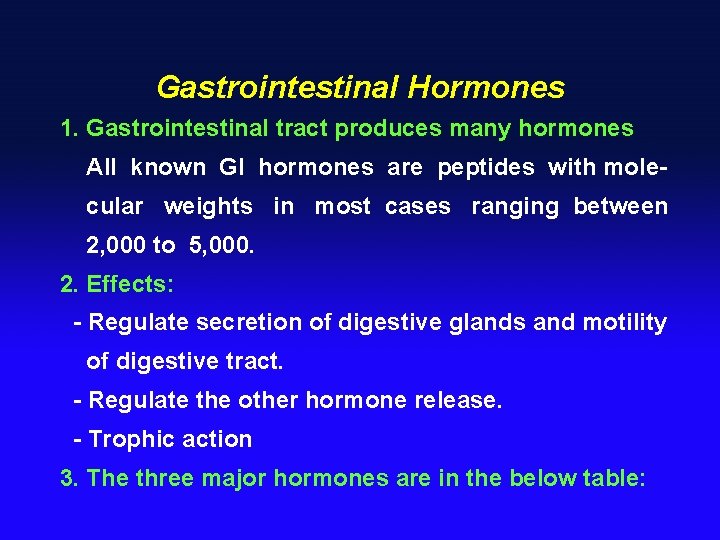
Gastrointestinal Hormones 1. Gastrointestinal tract produces many hormones All known GI hormones are peptides with molecular weights in most cases ranging between 2, 000 to 5, 000. 2. Effects: - Regulate secretion of digestive glands and motility of digestive tract. - Regulate the other hormone release. - Trophic action 3. The three major hormones are in the below table:
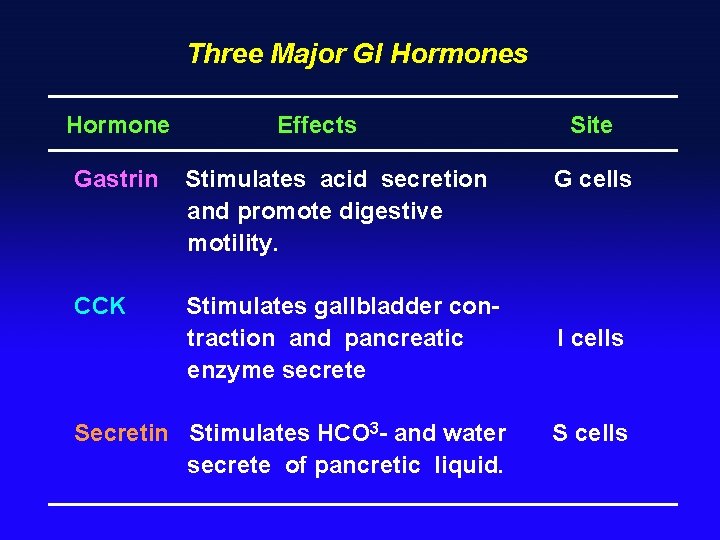
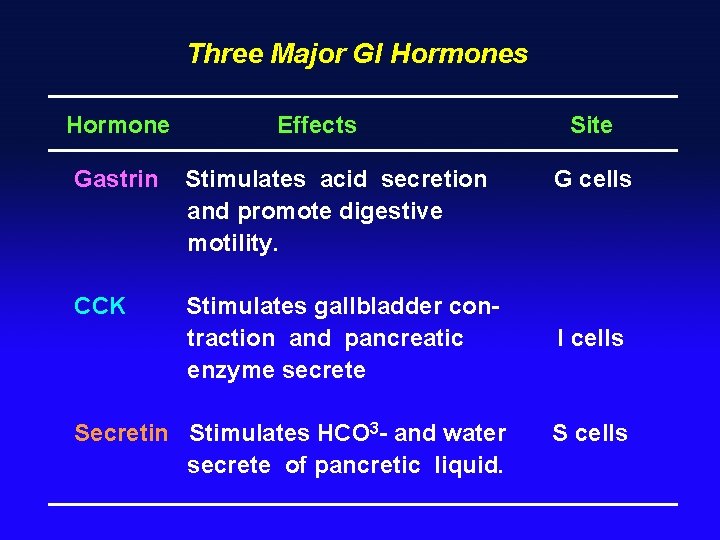
Three Major GI Hormones Hormone Effects Gastrin Stimulates acid secretion and promote digestive motility. CCK Stimulates gallbladder contraction and pancreatic enzyme secrete Secretin Stimulates HCO 3 - and water secrete of pancretic liquid. Site G cells I cells S cells
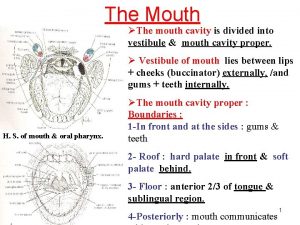
Section 2 Mouth and Esophagus § Saliva & function § Digestion of food in mouth
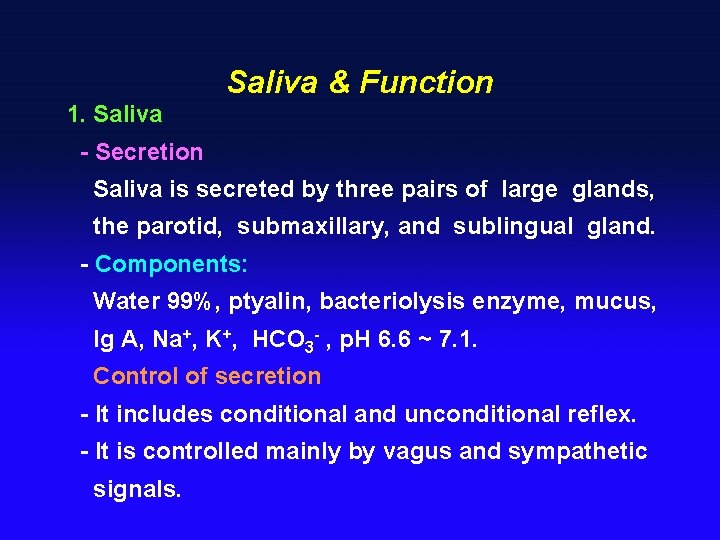
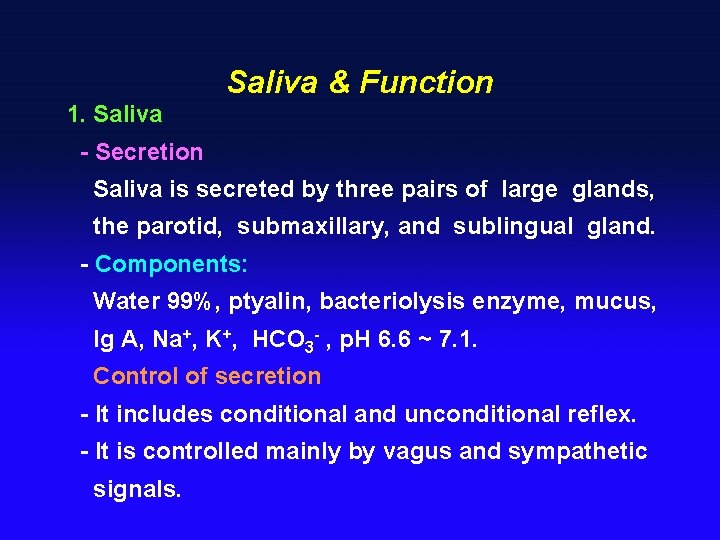
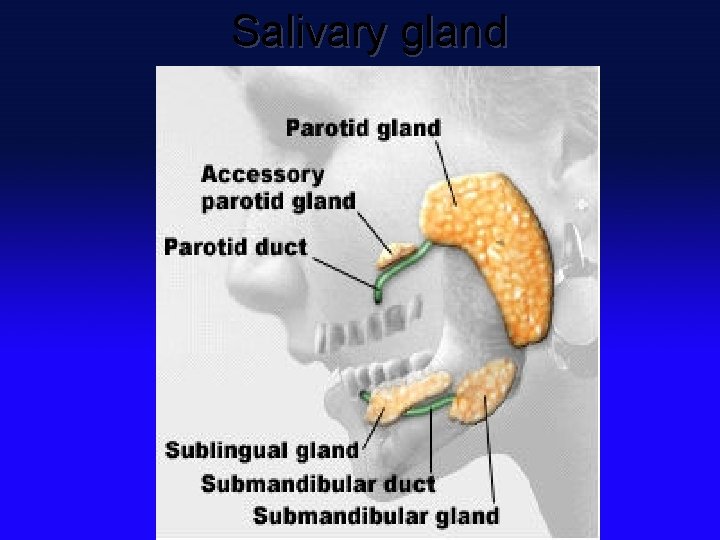
Saliva & Function 1. Saliva - Secretion Saliva is secreted by three pairs of large glands, the parotid, submaxillary, and sublingual gland. - Components: Water 99%, ptyalin, bacteriolysis enzyme, mucus, Ig A, Na+, K+, HCO 3 - , p. H 6. 6 ~ 7. 1. Control of secretion - It includes conditional and unconditional reflex. - It is controlled mainly by vagus and sympathetic signals.
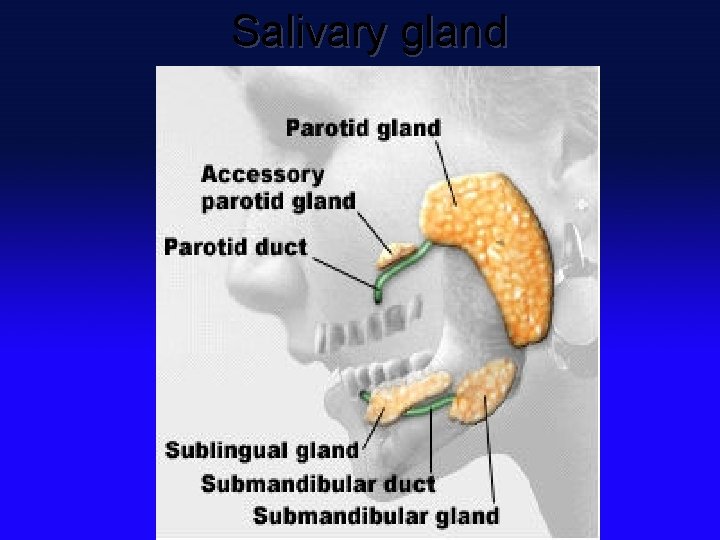
Salivary gland
2. Functions of saliva - The serous secretion contains ptyalin ( an αamylase ), which is an enzyme for digesting starch. - Mucous secretion contains mucus for surface protection and lubrication. - Solubilizes dry food - Keep oral hygiene: bacteriolysis enzyme, Ig A.
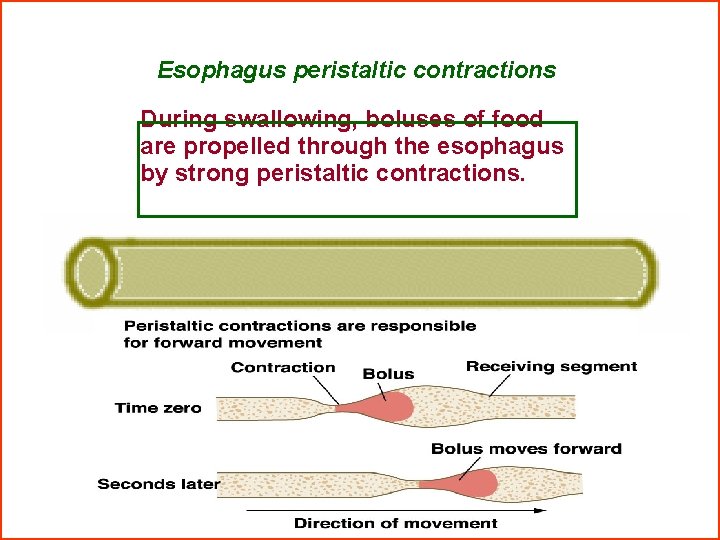
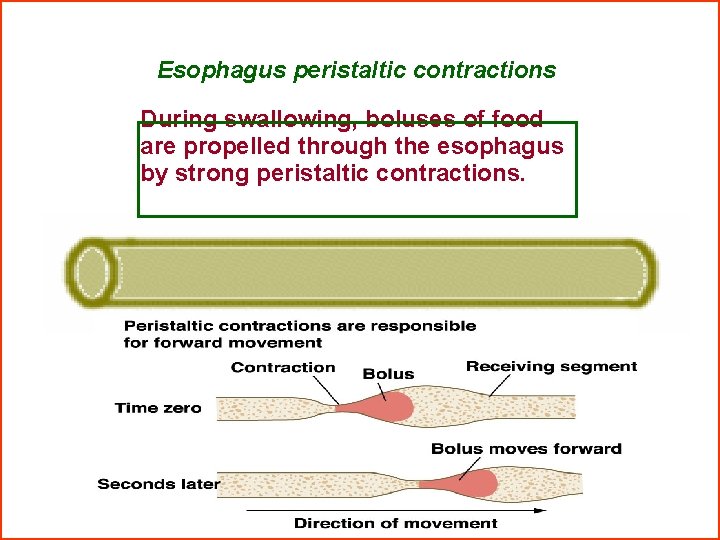
Esophagus peristaltic contractions During swallowing, boluses of food are propelled through the esophagus by strong peristaltic contractions.
Section 3 Gastric Digestion § Functional structure of the stomach § Gastric secretion § Regulation of gastric secretion § Motor functions of the stomach
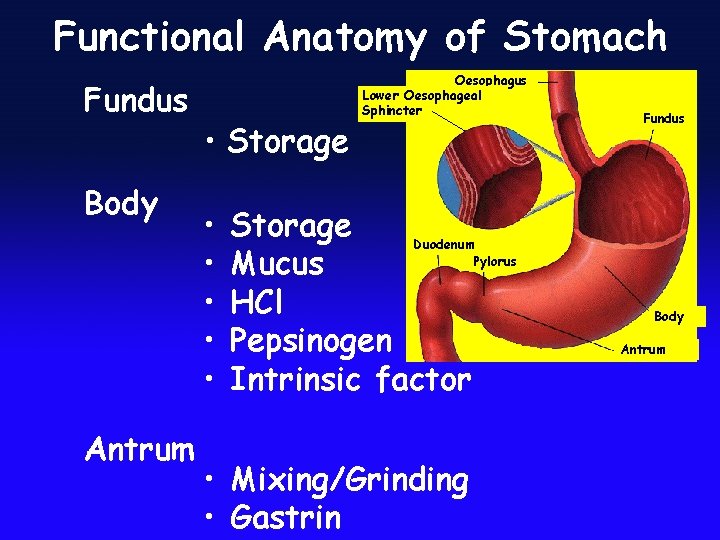
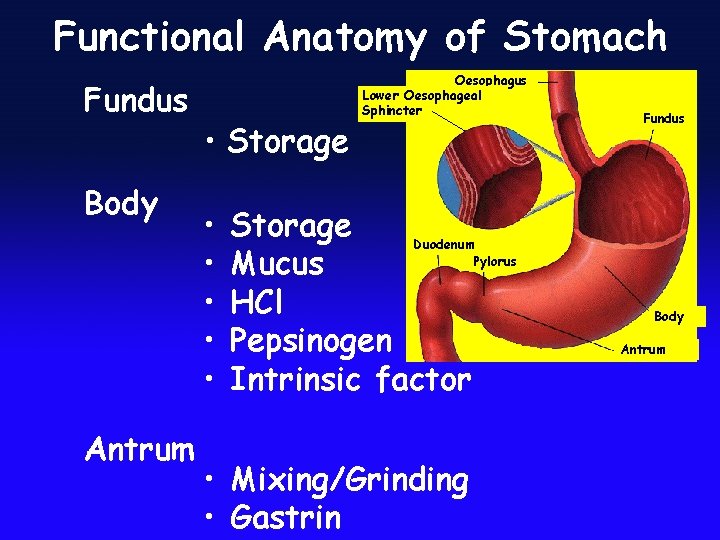
Functional Anatomy of Stomach Fundus Body Antrum • Storage • • • Oesophagus Lower Oesophageal Sphincter Storage Duodenum Pylorus Mucus HCl Pepsinogen Intrinsic factor • Mixing/Grinding • Gastrin Fundus Body Antrum
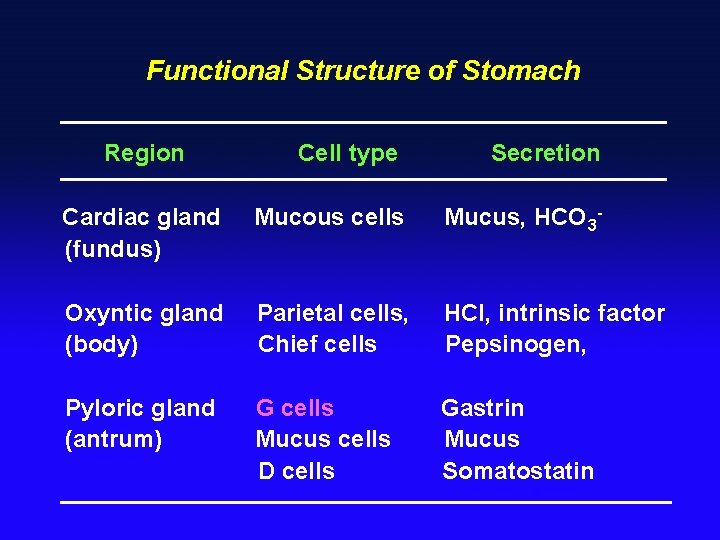
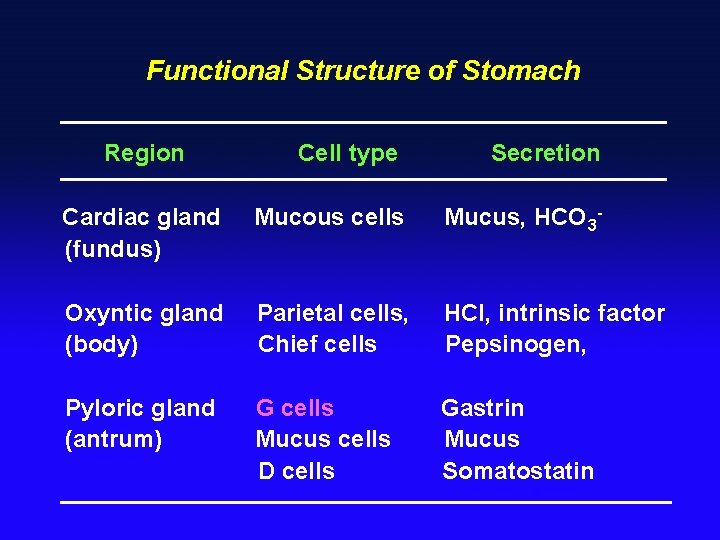
Functional Structure of Stomach Region Cell type Secretion Cardiac gland (fundus) Mucous cells Mucus, HCO 3 - Oxyntic gland (body) Parietal cells, Chief cells HCl, intrinsic factor Pepsinogen, Pyloric gland (antrum) G cells Mucus cells D cells Gastrin Mucus Somatostatin

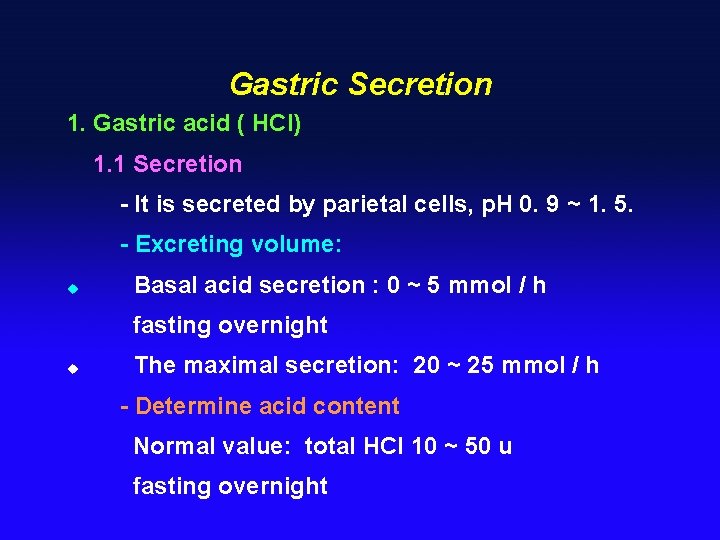
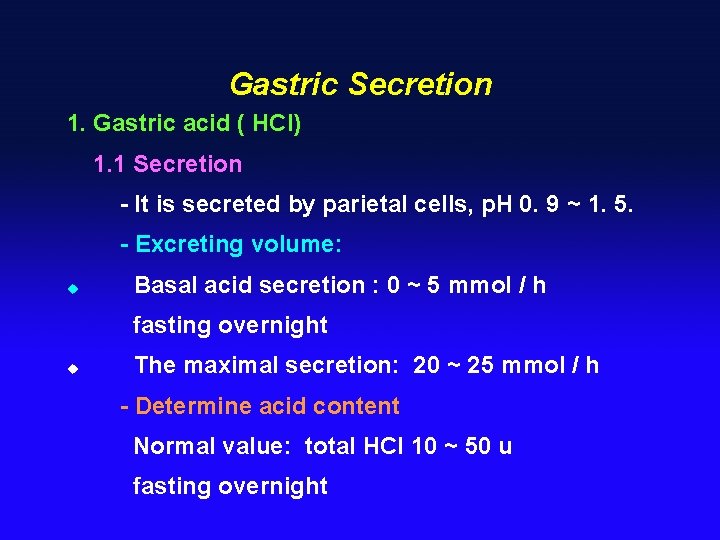
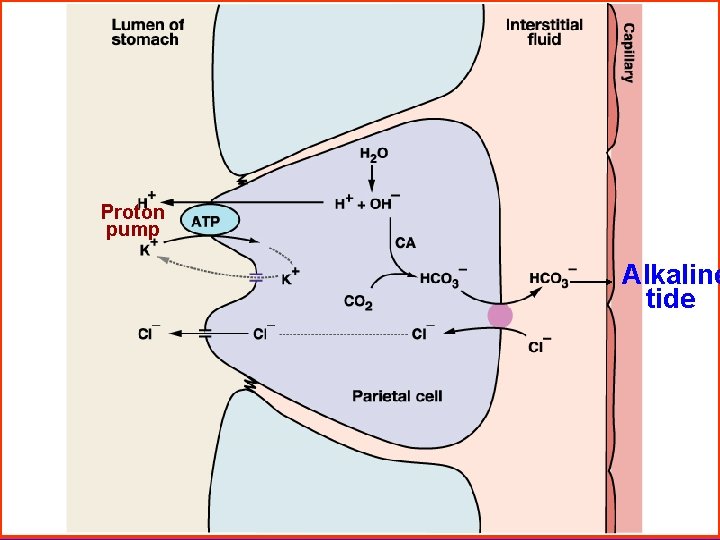
Gastric Secretion 1. Gastric acid ( HCl) 1. 1 Secretion - It is secreted by parietal cells, p. H 0. 9 ~ 1. 5. - Excreting volume: u Basal acid secretion : 0 ~ 5 mmol / h fasting overnight u The maximal secretion: 20 ~ 25 mmol / h - Determine acid content Normal value: total HCl 10 ~ 50 u fasting overnight
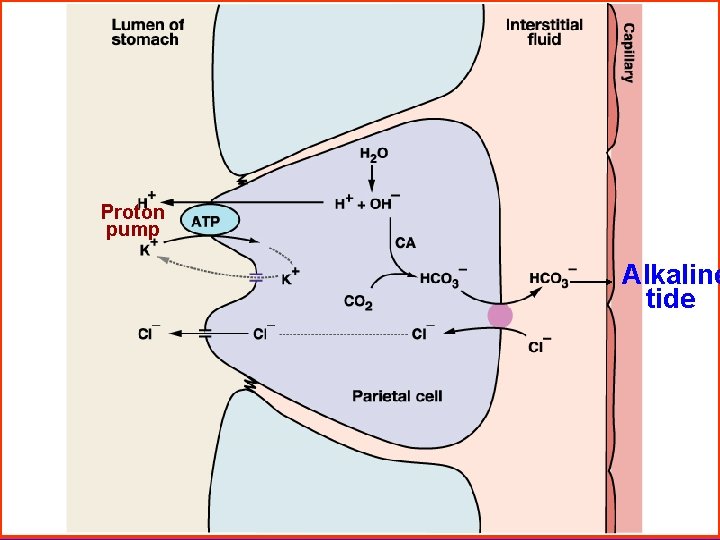
Proton pump Alkaline tide
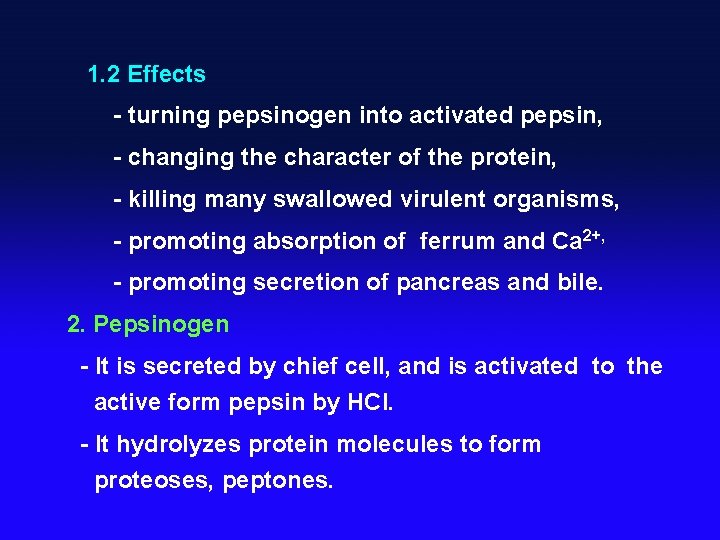
1. 2 Effects - turning pepsinogen into activated pepsin, - changing the character of the protein, - killing many swallowed virulent organisms, - promoting absorption of ferrum and Ca 2+, - promoting secretion of pancreas and bile. 2. Pepsinogen - It is secreted by chief cell, and is activated to the active form pepsin by HCl. - It hydrolyzes protein molecules to form proteoses, peptones.
3. Intrinsic factor - It is a glucoprotein secreted by the parietal cell. - It is essential to absorption of vitamin B 12 in the ileum. 4. Mucus - The surface epithelial cells of the stomach secrete a viscous mucus, they also secrete HCO 3 -. - It is widely believed that mucus and bicarbonate form a mucus bicarbonate barrier. - The mucus bicabonate barrier serves an important role in protecting the epithelium from acid - pepsin and other chemical insults.

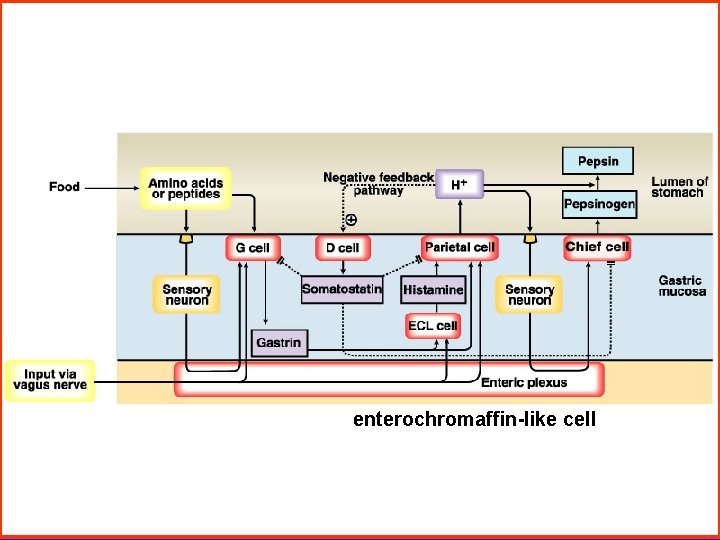
Regulation of Gastric Secretion 1. Stimulating factor of gastric secretion - Ach It excites secretion of gastric secretion. - Gastrin G cells secrete gastrin which stimulates pariatal cells strongly and peptic cells to a lesser extent. - Histamine( enterochromaffin like cell) It can enhances acid secretion by stimulating parietal cells.
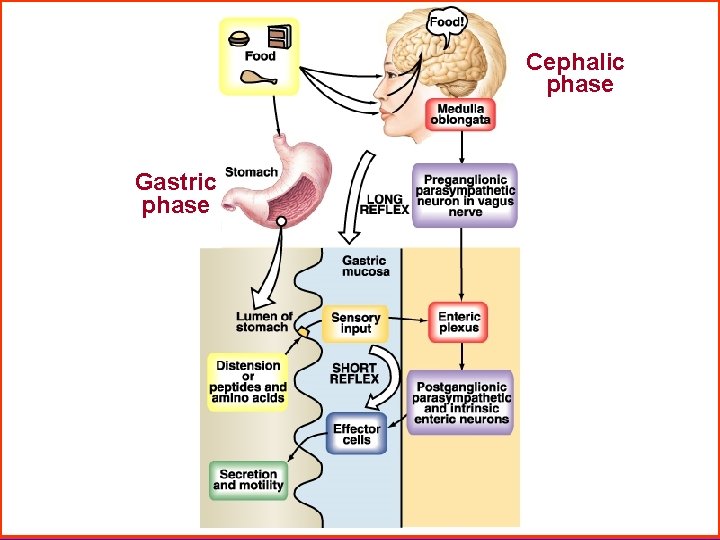
2. There are three phases of gastric secretion Cephalic phase - It is 30% of all gastric juice, HCl and pepsinogen are higher. - Vagus directly stimulates parietal cells and G cell releasing gastrin. Gastric phase - It is 60 % of all gastic juice, HCl is high but pepsinogen is lower than cephalic’. Intestinal phase - It is 10%, HCl and pepsinogen are low.
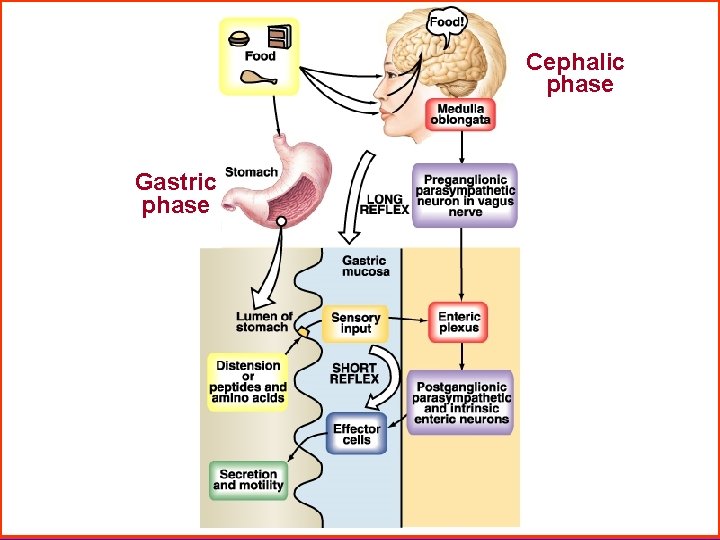
Cephalic phase Gastric phase

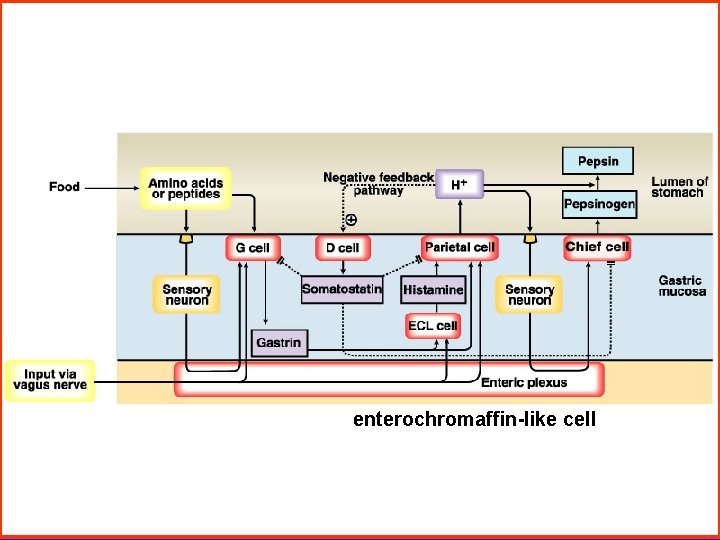
enterochromaffin-like cell
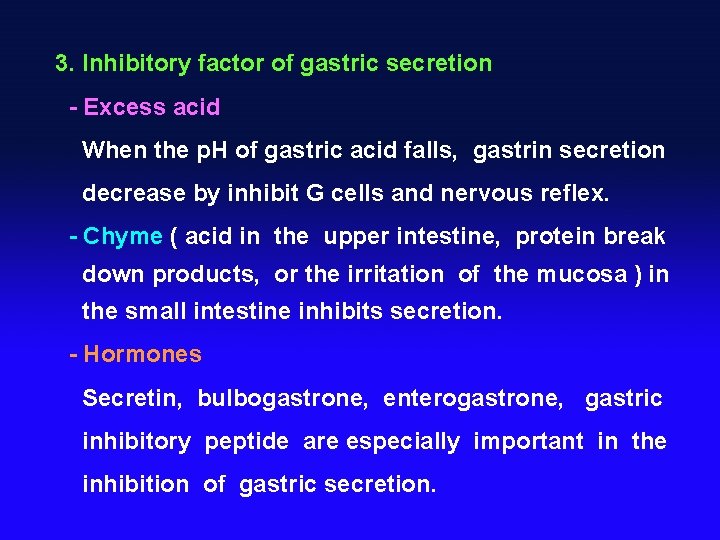
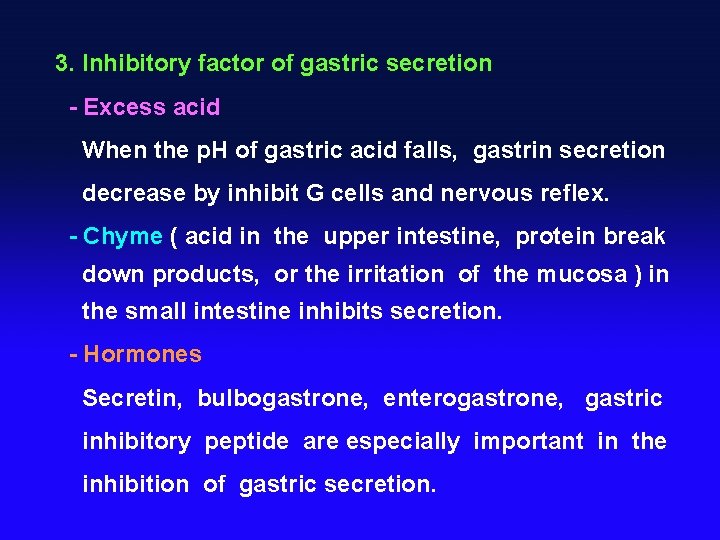
3. Inhibitory factor of gastric secretion - Excess acid When the p. H of gastric acid falls, gastrin secretion decrease by inhibit G cells and nervous reflex. - Chyme ( acid in the upper intestine, protein break down products, or the irritation of the mucosa ) in the small intestine inhibits secretion. - Hormones Secretin, bulbogastrone, enterogastrone, gastric inhibitory peptide are especially important in the inhibition of gastric secretion.
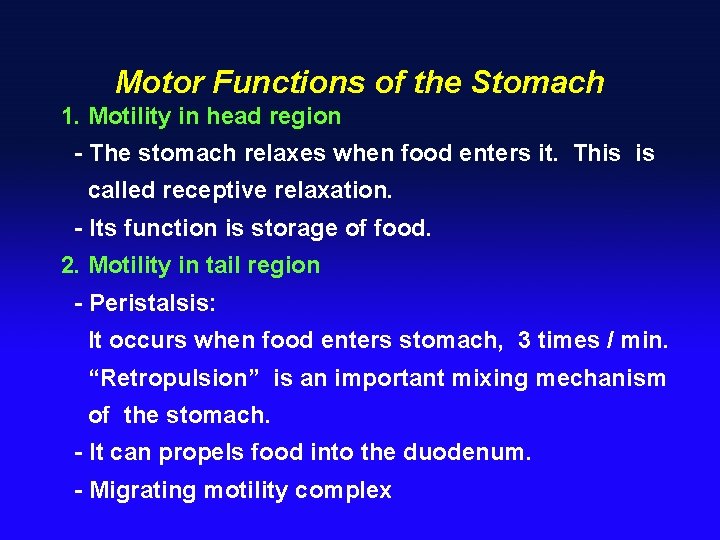
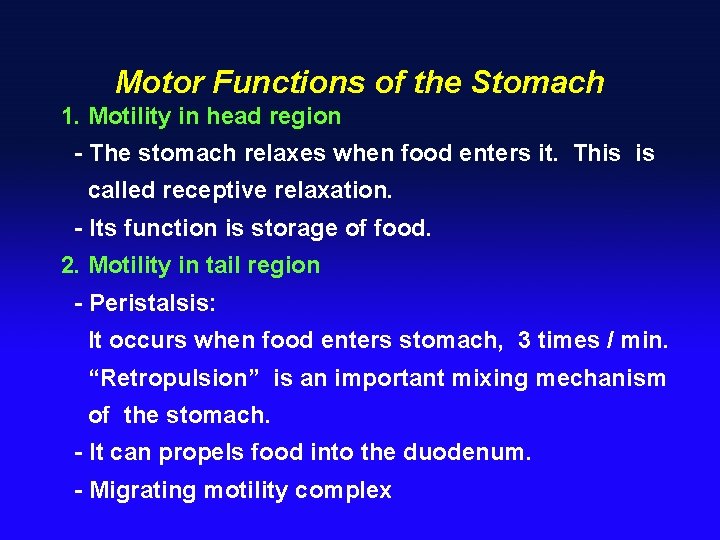
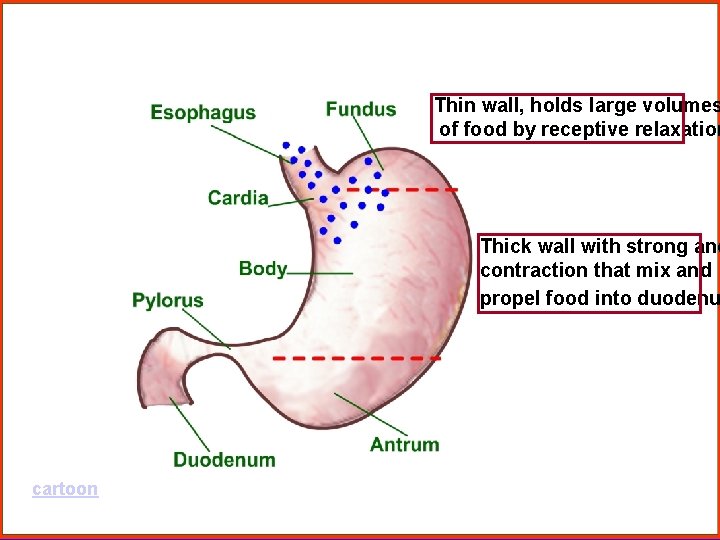
Motor Functions of the Stomach 1. Motility in head region - The stomach relaxes when food enters it. This is called receptive relaxation. - Its function is storage of food. 2. Motility in tail region - Peristalsis: It occurs when food enters stomach, 3 times / min. “Retropulsion” is an important mixing mechanism of the stomach. - It can propels food into the duodenum. - Migrating motility complex
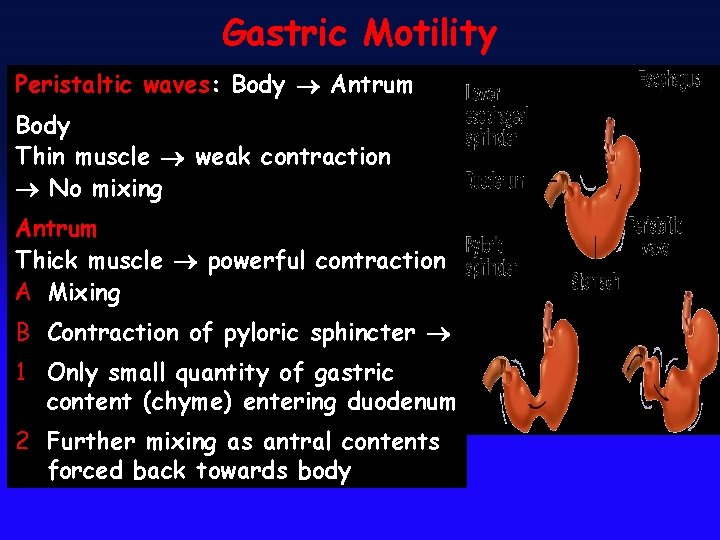
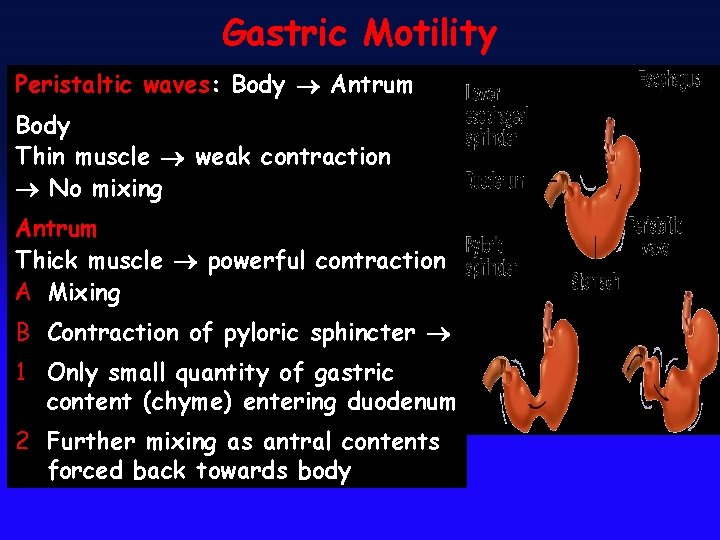
Gastric Motility Peristaltic waves: Body Antrum Body Thin muscle weak contraction No mixing Antrum Thick muscle powerful contraction A Mixing B Contraction of pyloric sphincter 1 Only small quantity of gastric content (chyme) entering duodenum 2 Further mixing as antral contents forced back towards body
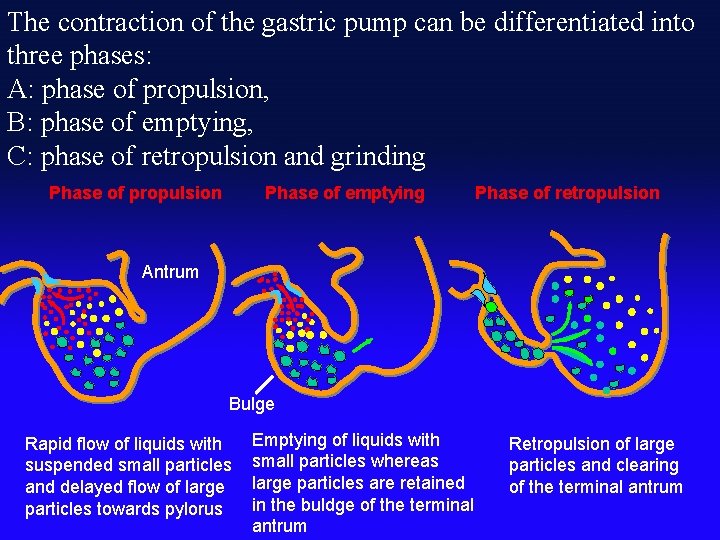
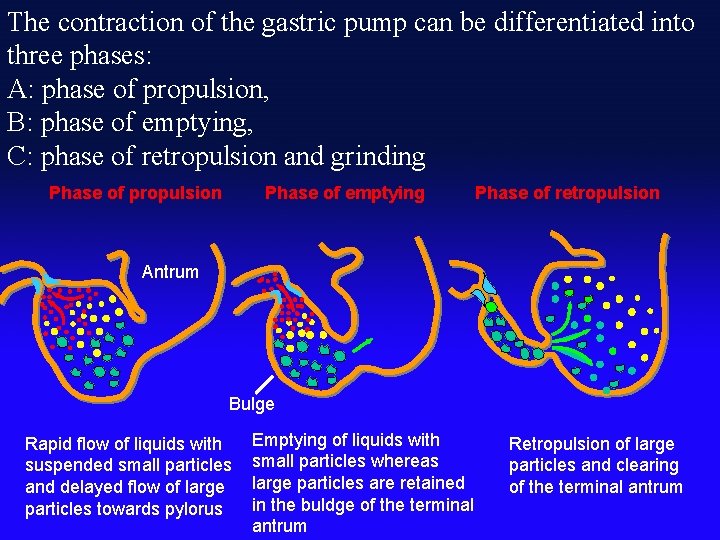
The contraction of the gastric pump can be differentiated into three phases: A: phase of propulsion, B: phase of emptying, C: phase of retropulsion and grinding Phase of propulsion Phase of emptying Phase of retropulsion Antrum Bulge Rapid flow of liquids with suspended small particles and delayed flow of large particles towards pylorus Emptying of liquids with small particles whereas large particles are retained in the buldge of the terminal antrum Retropulsion of large particles and clearing of the terminal antrum
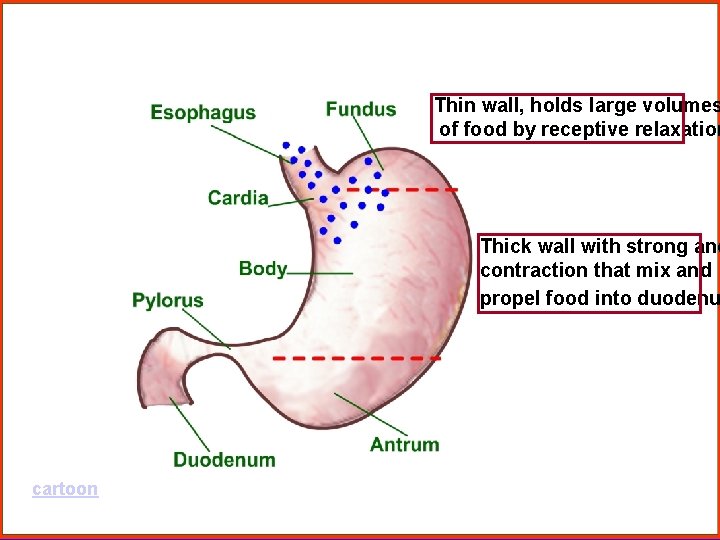
Thin wall, holds large volumes of food by receptive relaxation Thick wall with strong and contraction that mix and propel food into duodenu cartoon
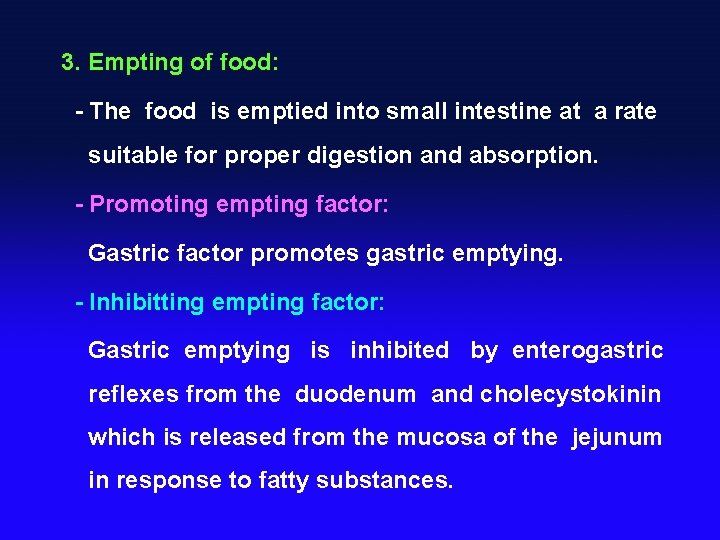
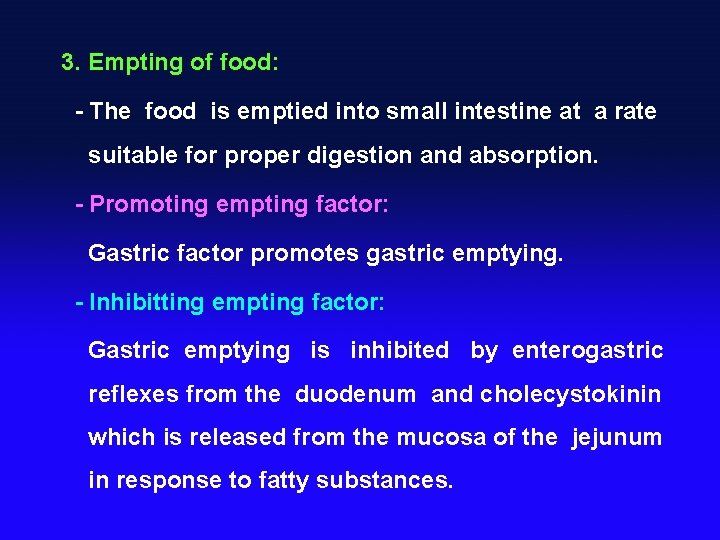
3. Empting of food: - The food is emptied into small intestine at a rate suitable for proper digestion and absorption. - Promoting empting factor: Gastric factor promotes gastric emptying. - Inhibitting empting factor: Gastric emptying is inhibited by enterogastric reflexes from the duodenum and cholecystokinin which is released from the mucosa of the jejunum in response to fatty substances.

Section 4 Digestion of the Small Intestine § Pancreatic secretion § Bile secretion n Secretion of the small intestine § Movement of the small intestine

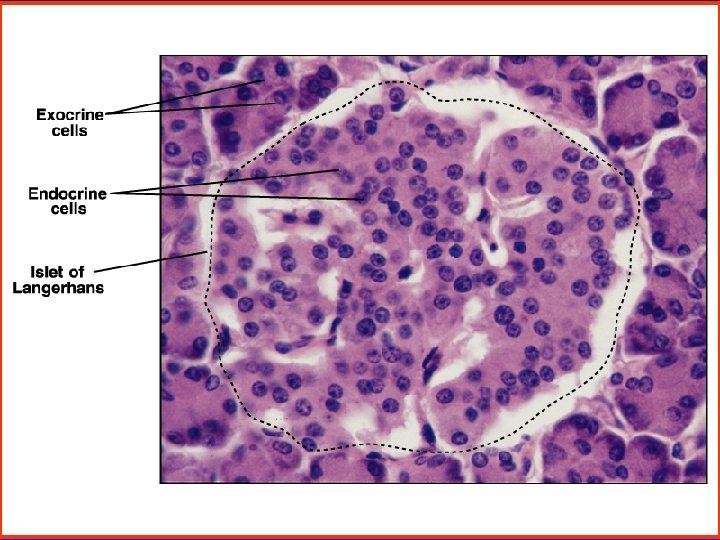
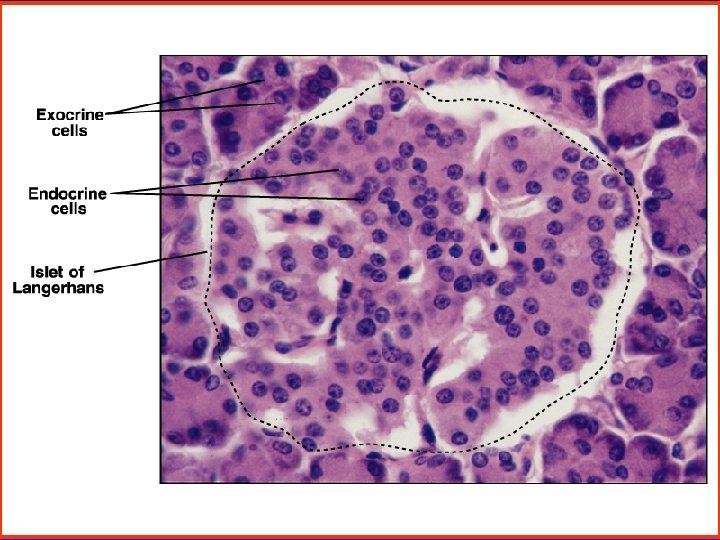
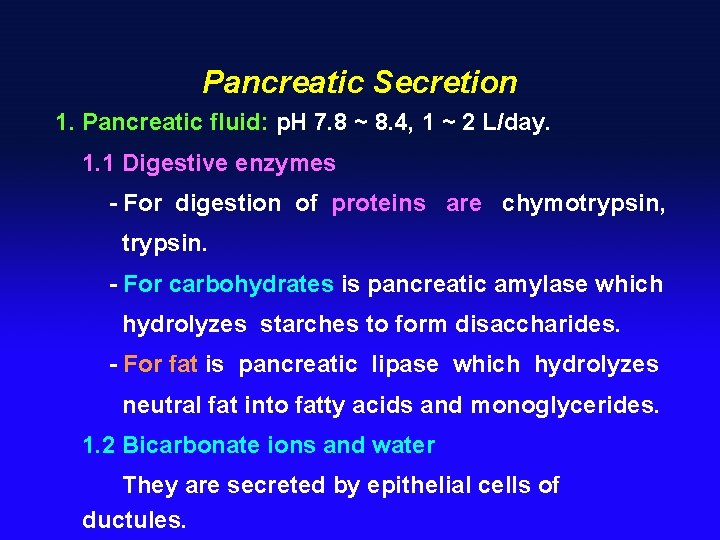
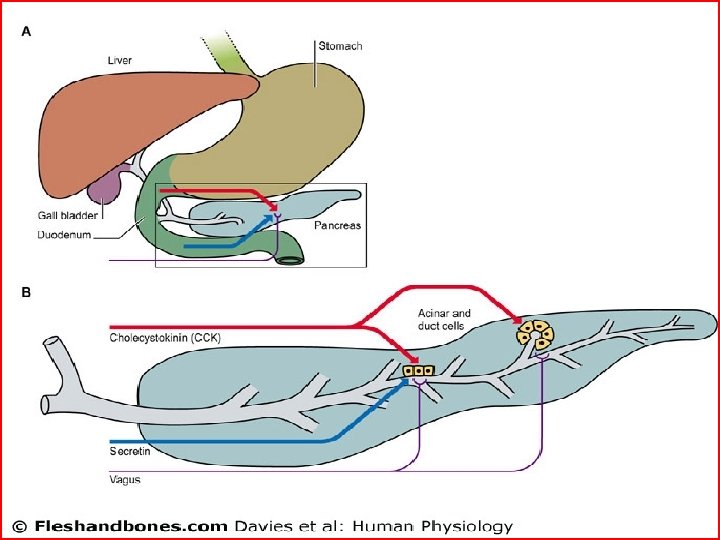
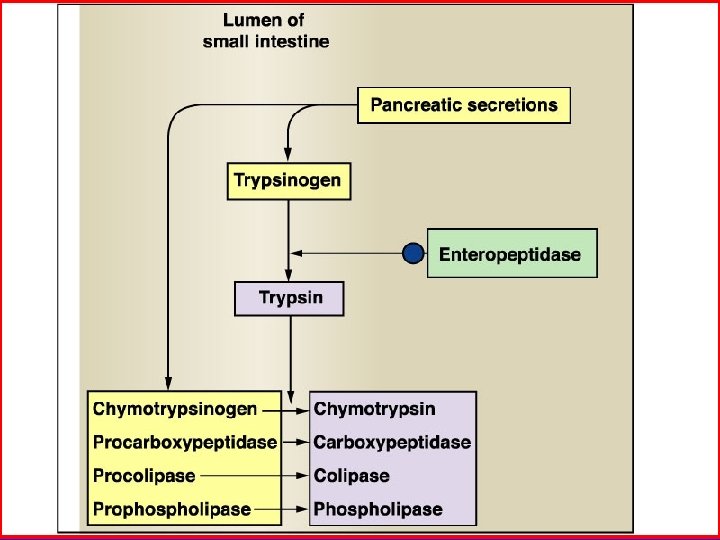
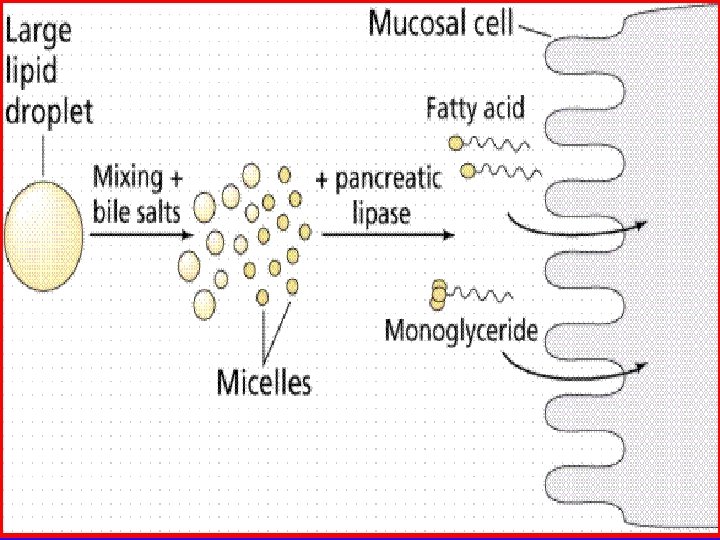
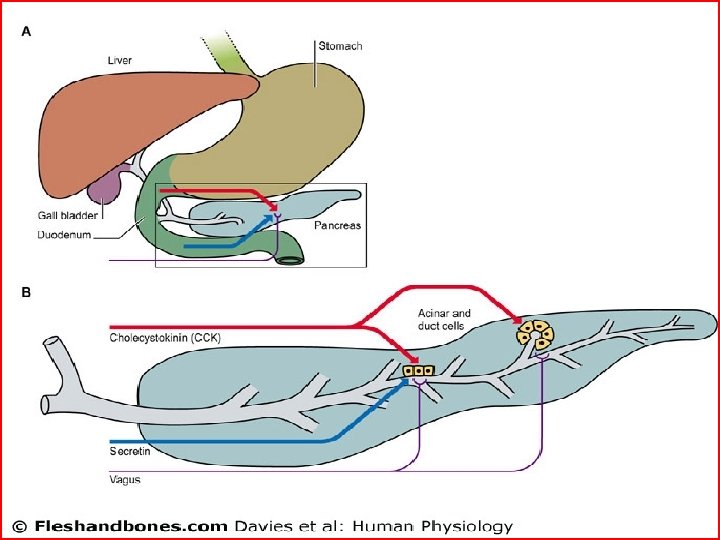
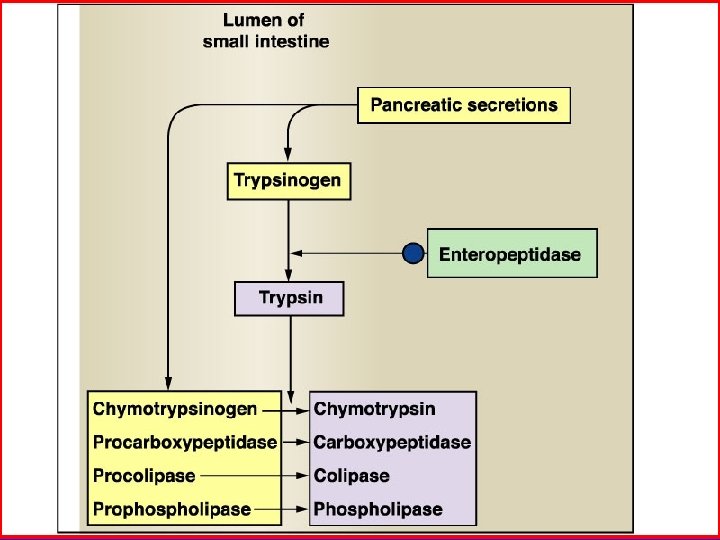
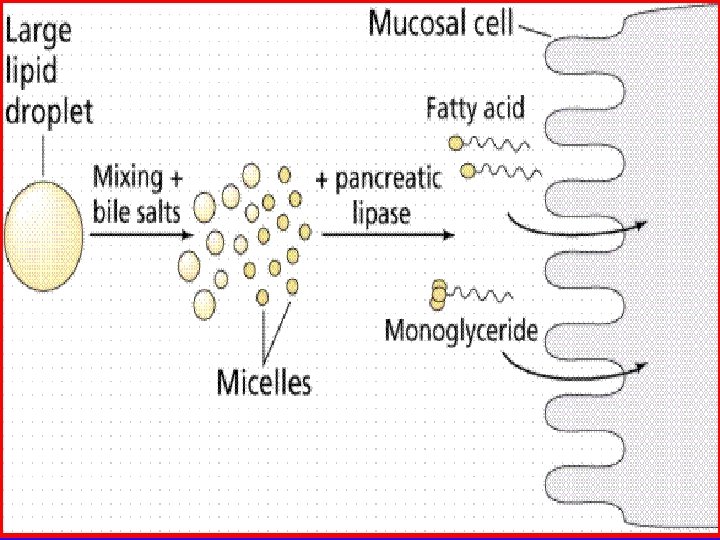
Pancreatic Secretion 1. Pancreatic fluid: p. H 7. 8 ~ 8. 4, 1 ~ 2 L/day. 1. 1 Digestive enzymes - For digestion of proteins are chymotrypsin, trypsin. - For carbohydrates is pancreatic amylase which hydrolyzes starches to form disaccharides. - For fat is pancreatic lipase which hydrolyzes neutral fat into fatty acids and monoglycerides. 1. 2 Bicarbonate ions and water They are secreted by epithelial cells of ductules.

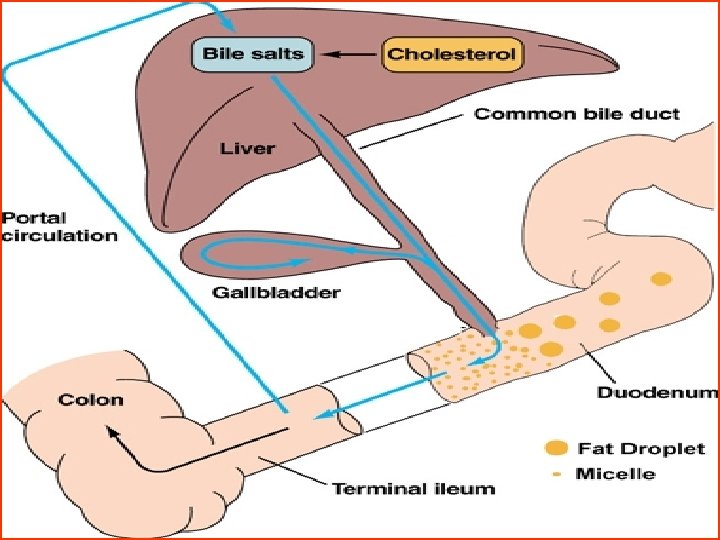
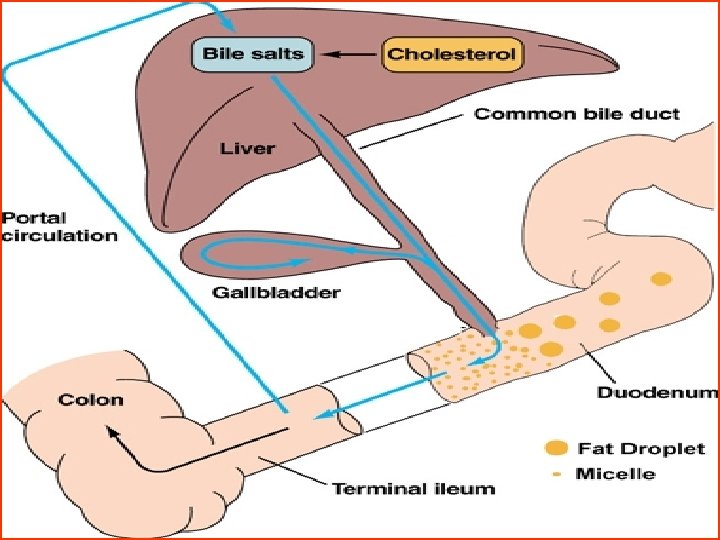
Bile Secretion 1. Components: Bile acids, cholesterol, bile salt, lecithin, bilirubin, electroytes. Bile contains no digestive enzyme. 2. Secretion: - Bile synthesized in the liver and is acidic as it flows through the bile ducts, is alkalescent in gallbladder. - Bile is concentrated about fivefold to tenfold in the gallbladder.

3. Action of bile salts: - promotes fat digestion (fat droplet) - help to emulsify the large fat particles into minute particles that can be attacked by the lipase enzyme. - promotes fat , fatsoluble vitamins absorption. 4. Regulation of bile: - Fatty foods that enter the duodenum cause CCK to be released from the local glands. - CCK cause rhythmical contractions of the gallbladder and simultaneous relaxation of the sphincter of Oddi.

Movements of the Small Intestine 1. Motility patterns - Segment contraction It promotes mixing of the solid food particles with the secretions of the small intestine. - Peristalsis Chyme is propelled through the small intestine by peristaltic waves at a velocity of 0. 5 to 2. 0 cm/s. 2. Regulation - Nervous signals are caused by the chyme into the duodenum but also by a gastroenteric reflex. - Hormonal signals: Gastrin, CCK enhance; secretin inhibits.



Secretion of the Large Intestine 1. Secretion: p. H 8. 3 -8. 4 - Most of the secretion in large intestine is mucus. - Mucus protects the intestinal wall against friction and bacterial activity, provides the adherent medium for fecal matter and barrier to keep acids from attacking the intestinal wall. 2. Bacterias action It can synthesize vitamine B ( B 1, B 2, B 12 ), K and folacin by ferment and decay of bacterias.


Section 6 Absorption in the Gastrointestinal Tract n The site of the absorption n Absorption of foods
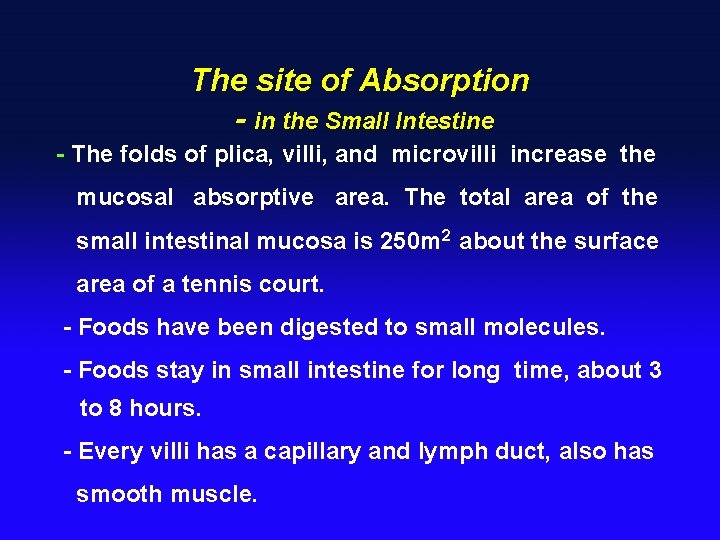
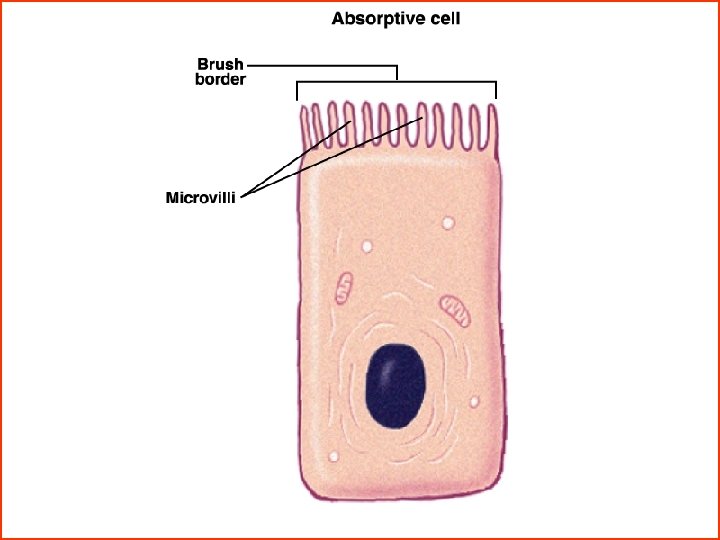
The site of Absorption - in the Small Intestine - The folds of plica, villi, and microvilli increase the mucosal absorptive area. The total area of the small intestinal mucosa is 250 m 2 about the surface area of a tennis court. - Foods have been digested to small molecules. - Foods stay in small intestine for long time, about 3 to 8 hours. - Every villi has a capillary and lymph duct, also has smooth muscle.


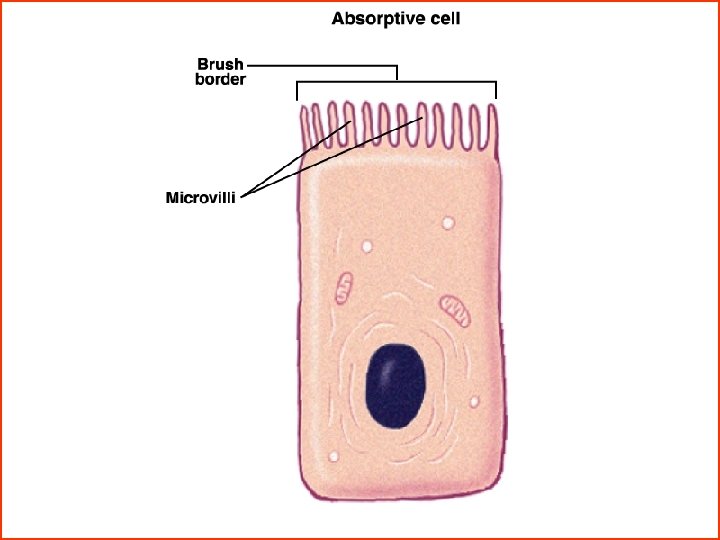
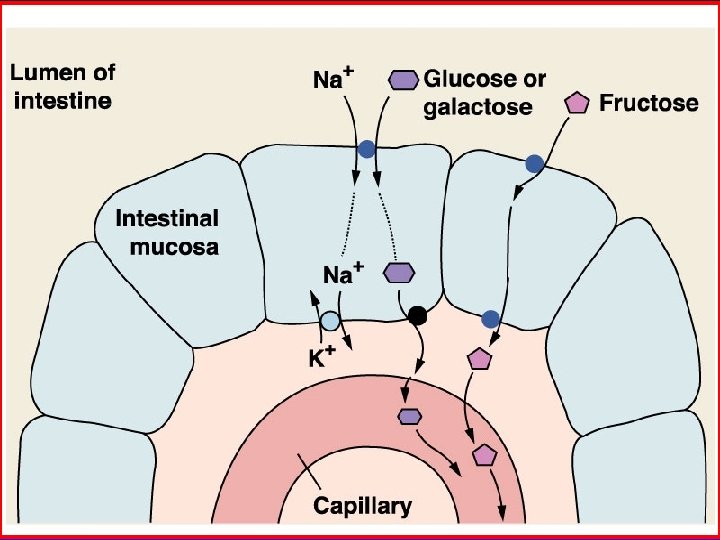
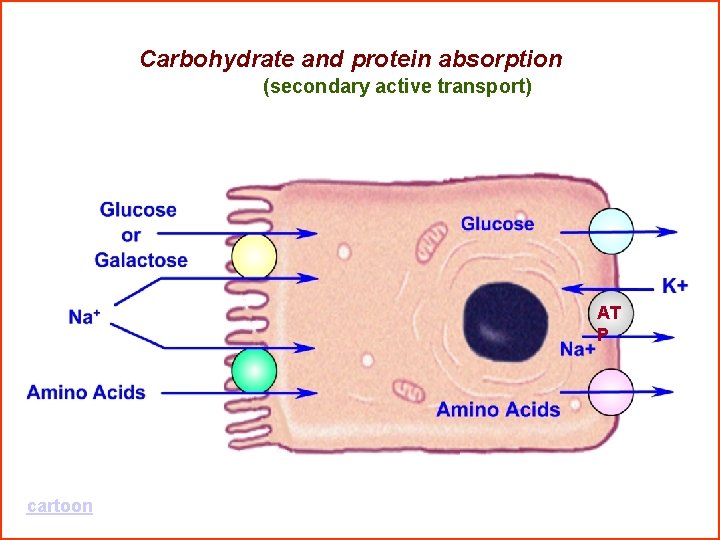
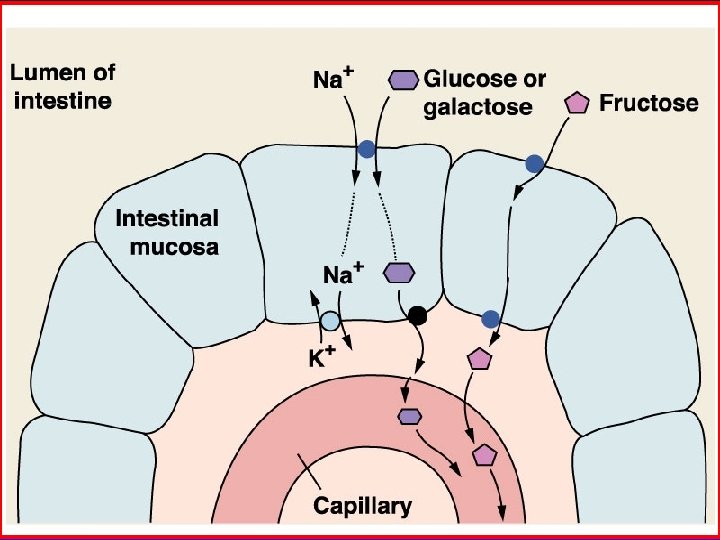
Absorption of Foods 1. Absorption of carbohydrates - Essentially all carbohydrates are absorbed in the form of monosaccharides. The most abundant of the absorbed monosaccharides is glucose which is absorbed to blood. - Glucose is transported by a sodium co-transport mechanism. - It is secondary active transport.
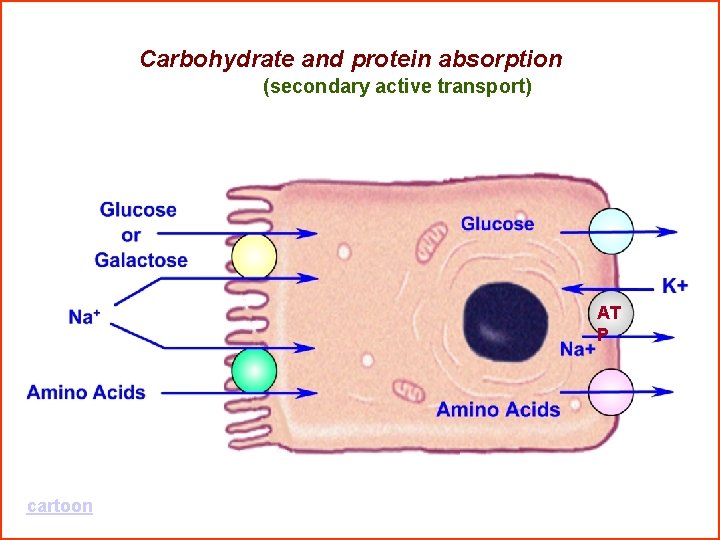
Carbohydrate and protein absorption (secondary active transport) AT P cartoon
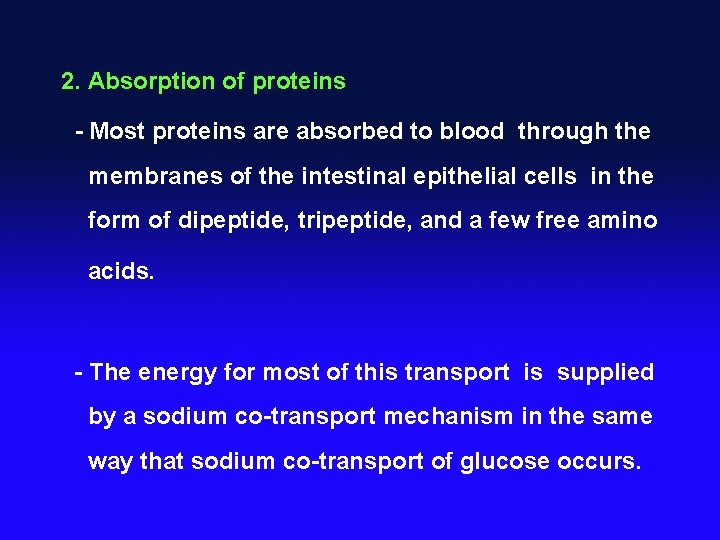
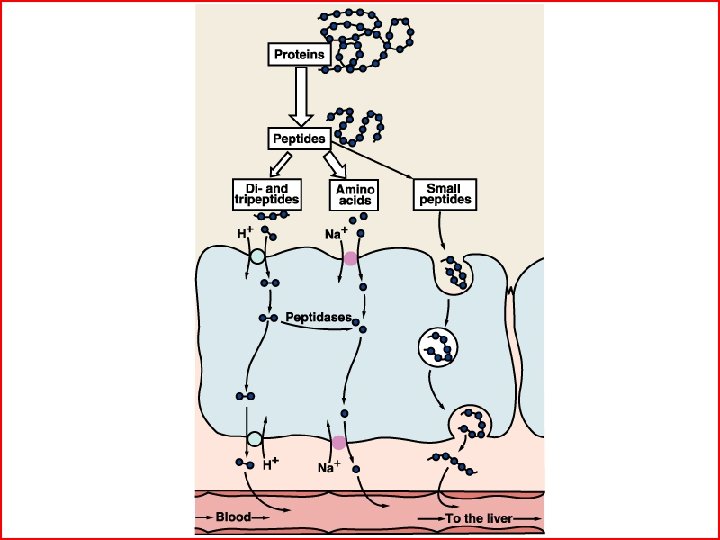
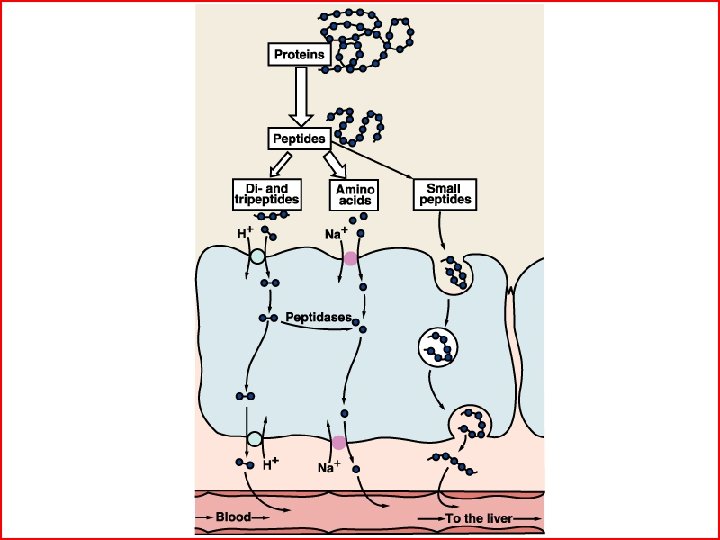
2. Absorption of proteins - Most proteins are absorbed to blood through the membranes of the intestinal epithelial cells in the form of dipeptide, tripeptide, and a few free amino acids. - The energy for most of this transport is supplied by a sodium co-transport mechanism in the same way that sodium co-transport of glucose occurs.
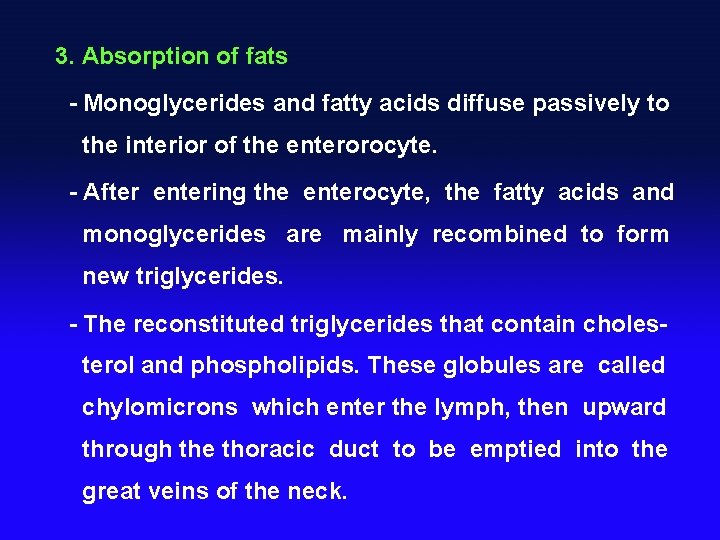
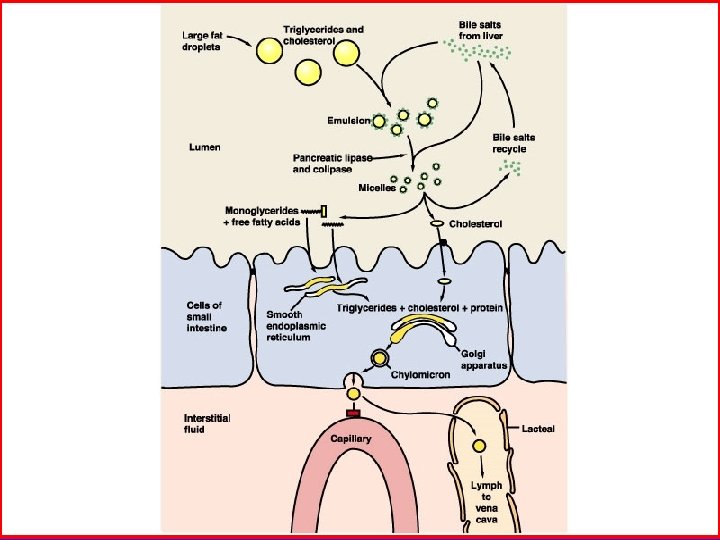
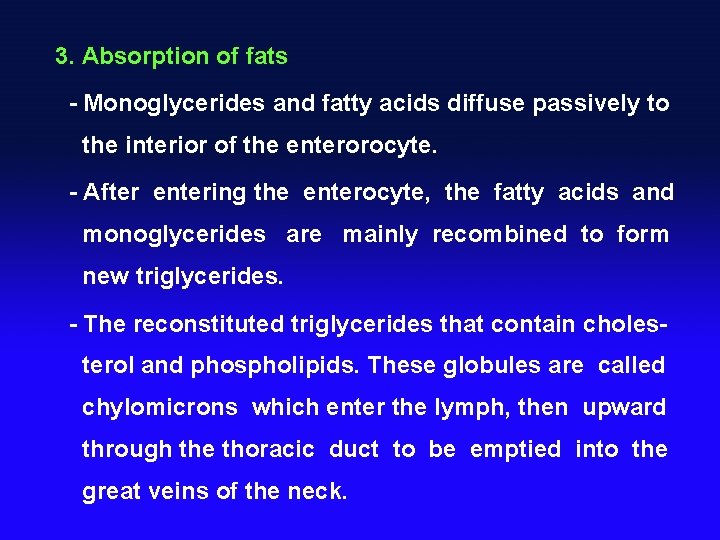
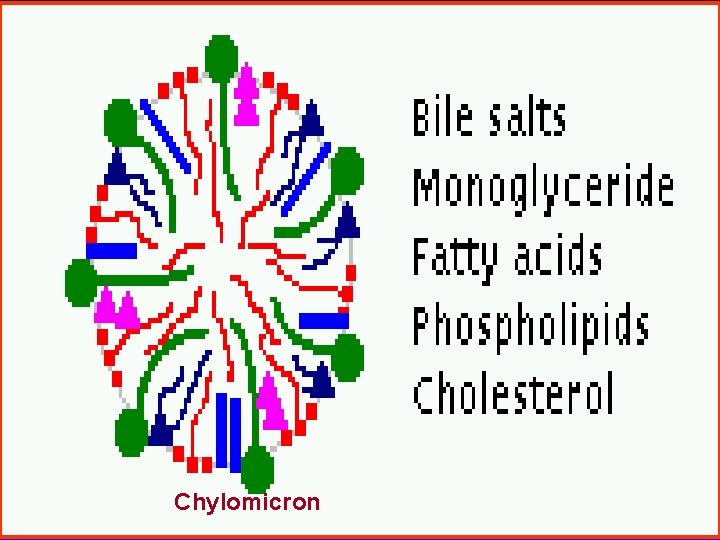
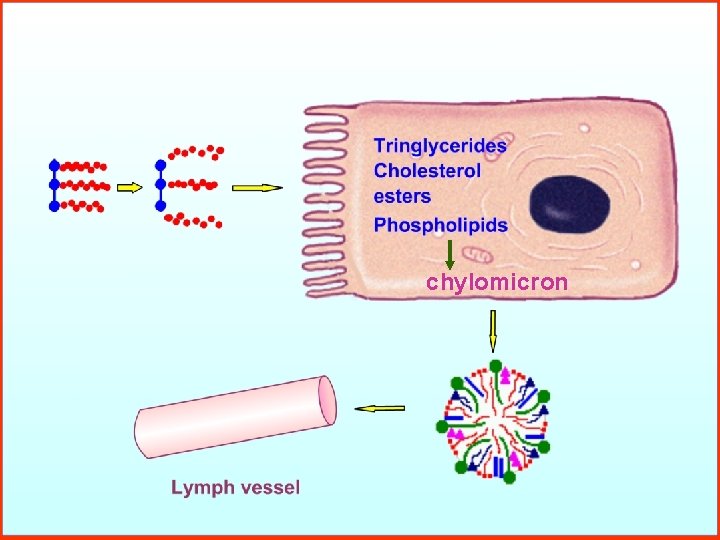
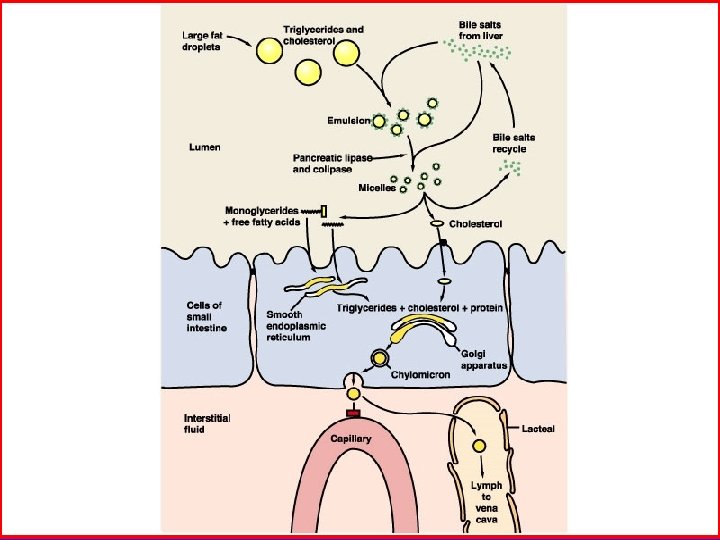
3. Absorption of fats - Monoglycerides and fatty acids diffuse passively to the interior of the enterorocyte. - After entering the enterocyte, the fatty acids and monoglycerides are mainly recombined to form new triglycerides. - The reconstituted triglycerides that contain cholesterol and phospholipids. These globules are called chylomicrons which enter the lymph, then upward through the thoracic duct to be emptied into the great veins of the neck.

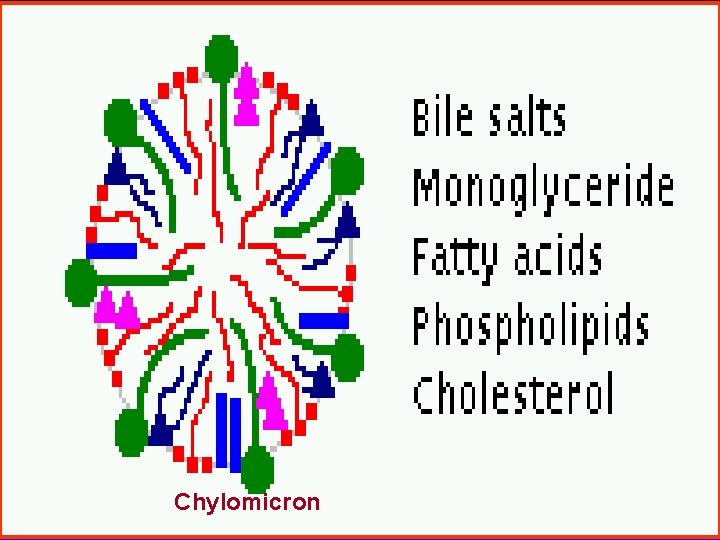
Chylomicron

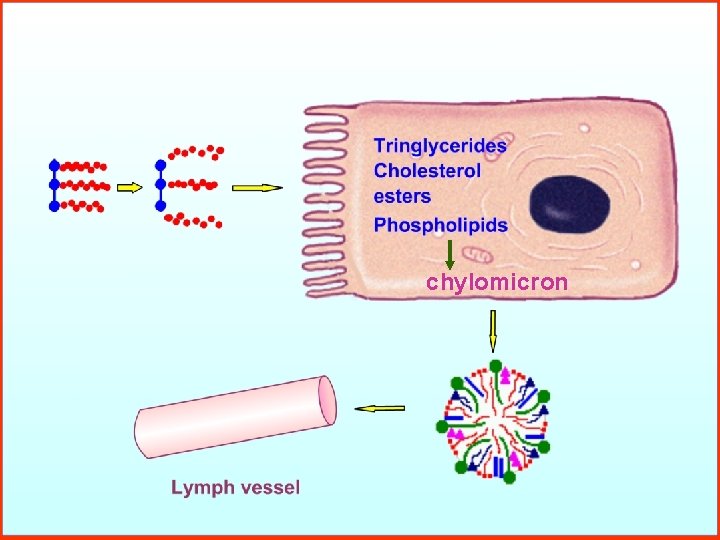
chylomicron

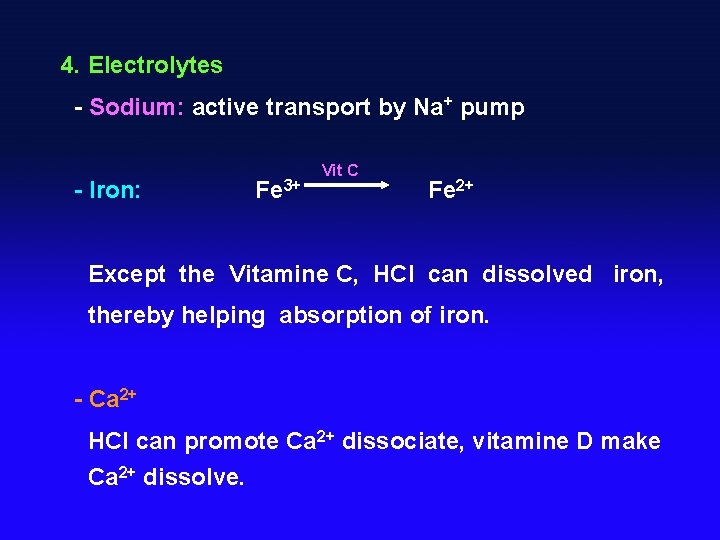
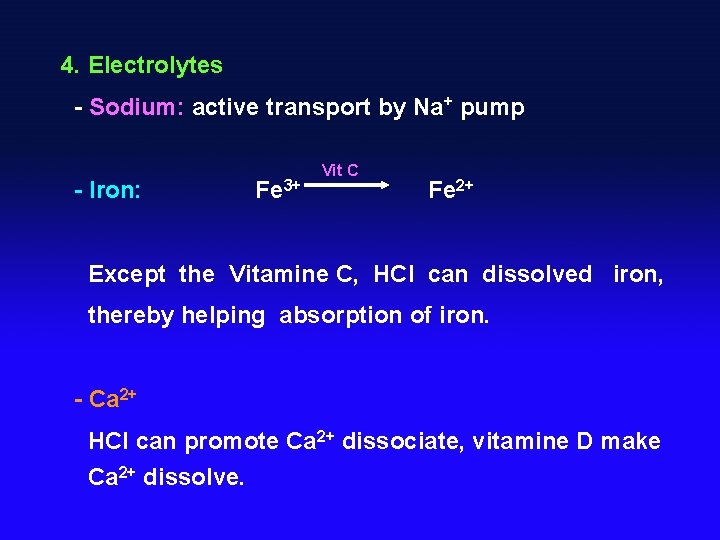
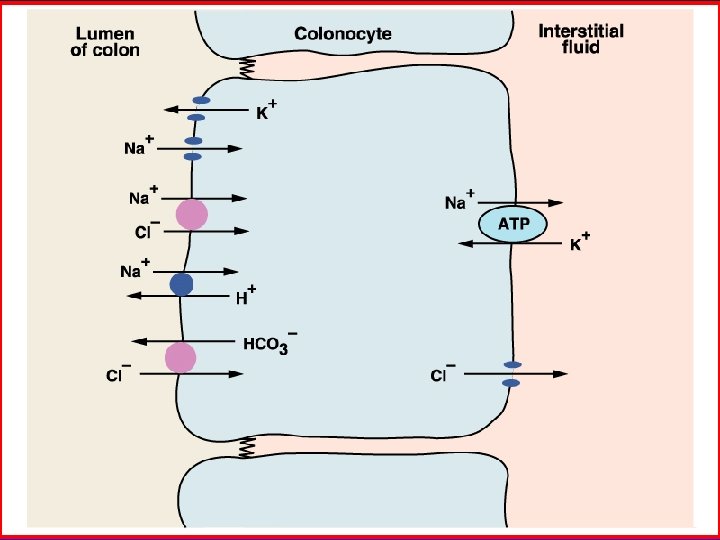
4. Electrolytes - Sodium: active transport by Na+ pump - Iron: Fe 3+ Vit C Fe 2+ Except the Vitamine C, HCl can dissolved iron, thereby helping absorption of iron. - Ca 2+ HCl can promote Ca 2+ dissociate, vitamine D make Ca 2+ dissolve.
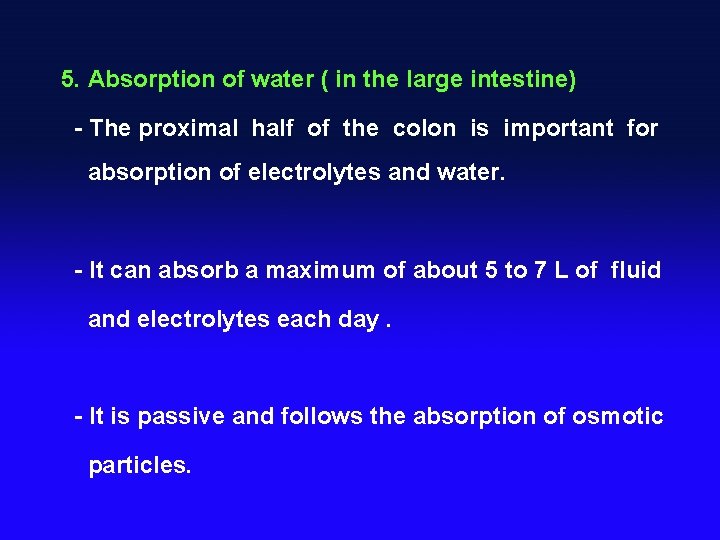
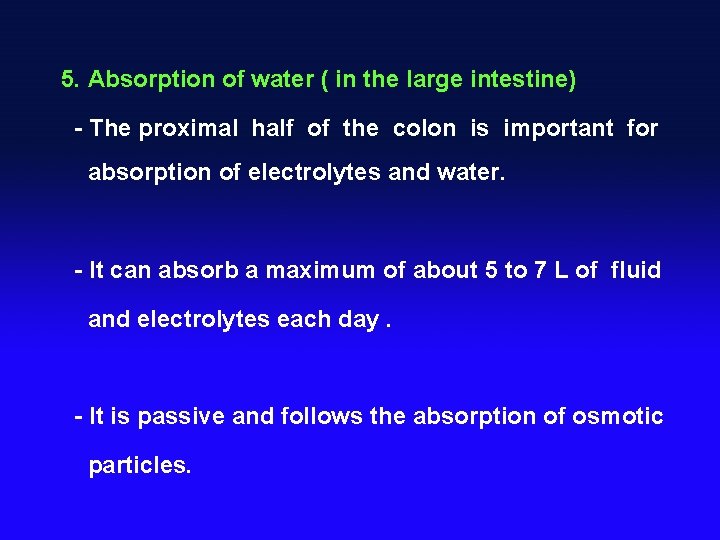
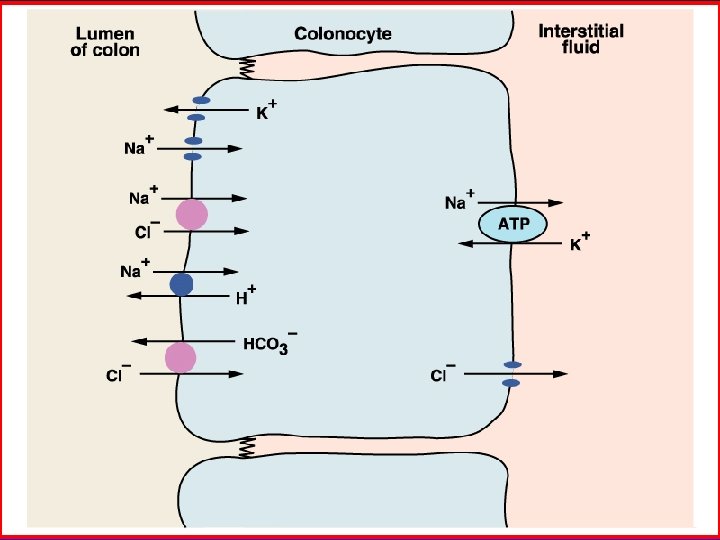
5. Absorption of water ( in the large intestine) - The proximal half of the colon is important for absorption of electrolytes and water. - It can absorb a maximum of about 5 to 7 L of fluid and electrolytes each day. - It is passive and follows the absorption of osmotic particles.

 Digestion in mouth
Digestion in mouth Digestion begins in the mouth
Digestion begins in the mouth Where does digestion begin? *
Where does digestion begin? * Carbohydrate digestion begins in the
Carbohydrate digestion begins in the Main functions of the digestive system
Main functions of the digestive system Digestion begins in the
Digestion begins in the Mechanical digestion and chemical digestion venn diagram
Mechanical digestion and chemical digestion venn diagram Embriologia del sistema gastrointestinal
Embriologia del sistema gastrointestinal Gastrointestinal tract
Gastrointestinal tract Gastrointestinal tract
Gastrointestinal tract Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 15 the gastrointestinal system
Chapter 15 the gastrointestinal system Gastrointestinal hormones
Gastrointestinal hormones Dr sigit djuniawan
Dr sigit djuniawan Equimosis colores
Equimosis colores Pankreatik polipeptid
Pankreatik polipeptid Gastrointestinal medical terminology breakdown
Gastrointestinal medical terminology breakdown Nutrition focused physical examination
Nutrition focused physical examination Proctodeum
Proctodeum Gastrointestinal tract
Gastrointestinal tract Motilidad gastrointestinal
Motilidad gastrointestinal Gastinoma
Gastinoma órgãos da barriga feminino
órgãos da barriga feminino Rins anatomia
Rins anatomia Functional constipation vs hirschsprung
Functional constipation vs hirschsprung Sublingual ilaç uygulaması
Sublingual ilaç uygulaması Gastrointestinal structure
Gastrointestinal structure Peristalsis and segmentation
Peristalsis and segmentation Why does metformin cause gastrointestinal problems
Why does metformin cause gastrointestinal problems Digestive system
Digestive system Hirschsprung disease nursing management
Hirschsprung disease nursing management Borborygmi
Borborygmi Absolute value functions as piecewise functions
Absolute value functions as piecewise functions How to solve evaluating functions
How to solve evaluating functions Evaluating functions and operations on functions
Evaluating functions and operations on functions How does a waterfall form
How does a waterfall form Unsegmented pseudocoelomate animal
Unsegmented pseudocoelomate animal Incisal papilla
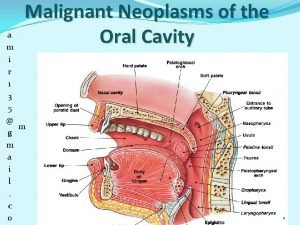
Incisal papilla Parietal layer and visceral layer
Parietal layer and visceral layer Mouth esophagus stomach intestines
Mouth esophagus stomach intestines Heart disease
Heart disease John kirby mouth
John kirby mouth Is kudlung an idiophone
Is kudlung an idiophone Make the moor thank me love me and reward me
Make the moor thank me love me and reward me Mouth preparation adalah
Mouth preparation adalah Mandibulate type mouth parts are seen in
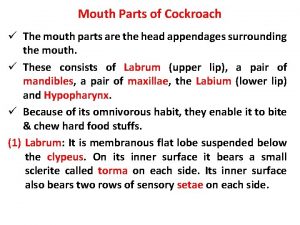
Mandibulate type mouth parts are seen in Mouth parts of cockroach
Mouth parts of cockroach A new way to measure word-of-mouth marketing
A new way to measure word-of-mouth marketing Bell mouth gate
Bell mouth gate Jawless fish characteristics
Jawless fish characteristics Mouth of bay
Mouth of bay Job 41
Job 41 Mouth parts
Mouth parts Frog mouth dissection
Frog mouth dissection Ribbon fish teeth
Ribbon fish teeth What is a mouth morpheme
What is a mouth morpheme Are sand dollars poisonous
Are sand dollars poisonous Large intestine histology
Large intestine histology Major and accessory organs of the digestive system
Major and accessory organs of the digestive system Properties of inlay wax
Properties of inlay wax Mouth parts name
Mouth parts name Mouth assessment normal findings
Mouth assessment normal findings Oral cavity landmarks
Oral cavity landmarks Pathway of food from mouth to anus
Pathway of food from mouth to anus Square breathing gif
Square breathing gif Pathway of food from mouth to anus
Pathway of food from mouth to anus Nacirema horace miner
Nacirema horace miner Be careful little mouth what you say
Be careful little mouth what you say Physiology of pharynx
Physiology of pharynx X ray mastoid towne's view cholesteatoma
X ray mastoid towne's view cholesteatoma How valuable is word of mouth
How valuable is word of mouth Paranasal sinus development
Paranasal sinus development Nacirema
Nacirema Vhoof
Vhoof Hand over mouth exercise
Hand over mouth exercise All star somebody once told me
All star somebody once told me Skew flap below knee amputation
Skew flap below knee amputation Floor of mouth cancer
Floor of mouth cancer Ideal properties of inlay wax
Ideal properties of inlay wax Wedge principle of elevators
Wedge principle of elevators We were given two ears but only one mouth
We were given two ears but only one mouth Mouth
Mouth Bad mouth betty
Bad mouth betty Copyright
Copyright Knuckle cruncher
Knuckle cruncher What can run but never walks has a mouth
What can run but never walks has a mouth Las partes de la boca
Las partes de la boca Journey of a sandwich through the digestive system
Journey of a sandwich through the digestive system Chemical digestion
Chemical digestion Indications of relining and rebasing
Indications of relining and rebasing Be transformed by the renewing of your mind meaning
Be transformed by the renewing of your mind meaning