Gastrointestinal bleeding General Principles of GIBleeding can occur

Gastrointestinal bleeding
General Principles of GI-Bleeding can occur anywhere, from the oral mucosa to the anus. The ligament of Treitz sepparates “upper” from “lower”. Overt presentation varies: Hematemesis (upper), melena (upper > lower), maroon stools (lower > upper), bright red blood per rectum – BRBPR (lower >> upper). Stool colour ≠ upper vs. lower. ALL patients with a presentation of severe GI bleeding should immediately be treated with fluids and worked up for anemia/ coagulation problems ALL patient with Hx of liver disease, alcoholism, or patients with hematemesis should also get IV octreotide Hx will always give you a hint to the likely diagnosis
Emergency Treatment of GI Bleeding (Volume)Resuscitation is always the first step in GI bleeding! Severe GI Bleeding: Immediate NS bolus Hematemesis is always severe Ongoing bloody diarrhea is always severe Low blood pressure or orthostasis is always severe Patient has hematemesis or Hx of liver disease/ Eto. H: IV octreotide Labs: EKG, CBC, PT/PTT, type+ crossmatch Low haemoglobin (<10): Administer PRBCs Low platelets (<50): Platelet transfusion Elevated PT or PTT: Administer FFP
Laboratory Hemoglobin: In early stage doesn’t show volume loss Microcytic, hypochromic in chronic bleeding Urea: High in GI bleeding unrelated to the value of creatinine (bacterial metabolism of proteins in blood) FE, ferritin low in chronic bleed
Upper GI Bleeding Peptic Ulcer disease (gnawing pain, NSAID use, etc. ) Gastritis (gnawing pain, NSAID, alcohol, tobacco, etc. ) Mallory-Weiss tear (retching, sudden bleed) Gastroesophageal varices (alcoholism, liver disease) Gastric or esophageal cancer (refractory GERD, alcohol, tob. ) Esophagitis (odynophagia) Rarely: Aortoenteric fistula (hx of recent AAA surgical repair)
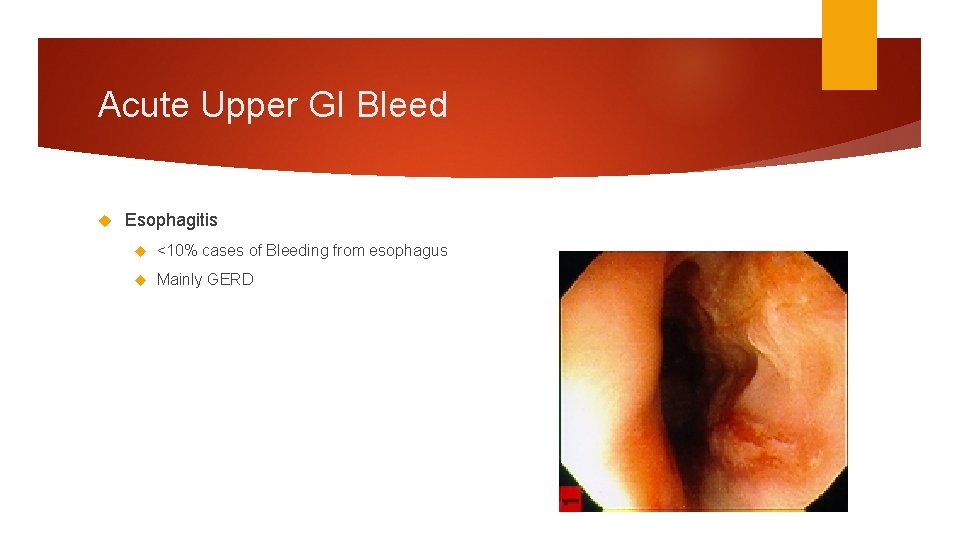
Acute Upper GI Bleed Esophagitis <10% cases of Bleeding from esophagus Mainly GERD
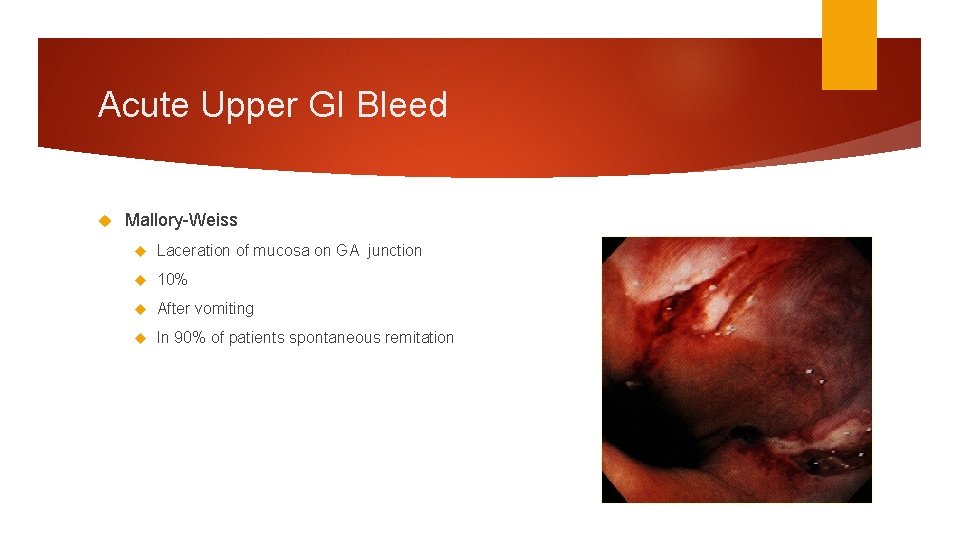
Acute Upper GI Bleed Mallory-Weiss Laceration of mucosa on GA junction 10% After vomiting In 90% of patients spontaneous remitation
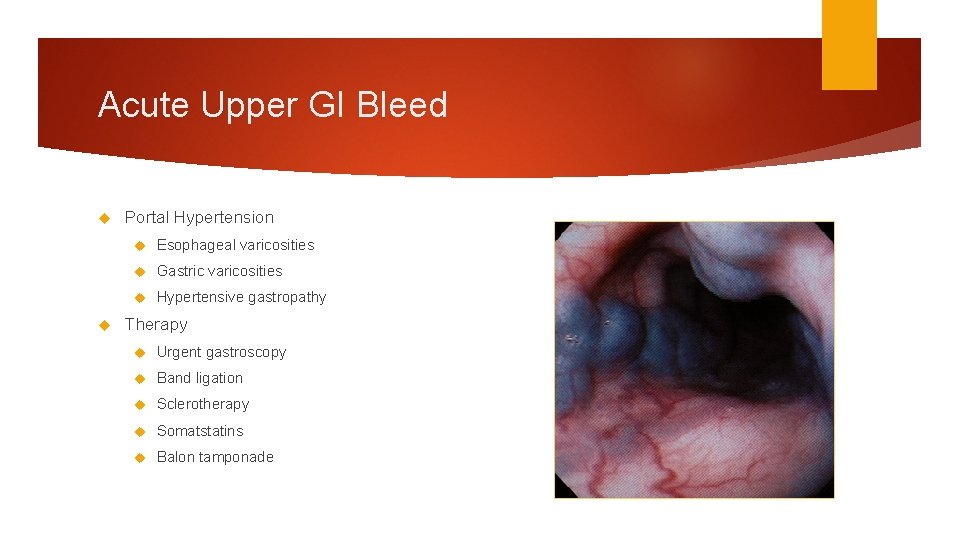
Acute Upper GI Bleed Portal Hypertension Esophageal varicosities Gastric varicosities Hypertensive gastropathy Therapy Urgent gastroscopy Band ligation Sclerotherapy Somatstatins Balon tamponade
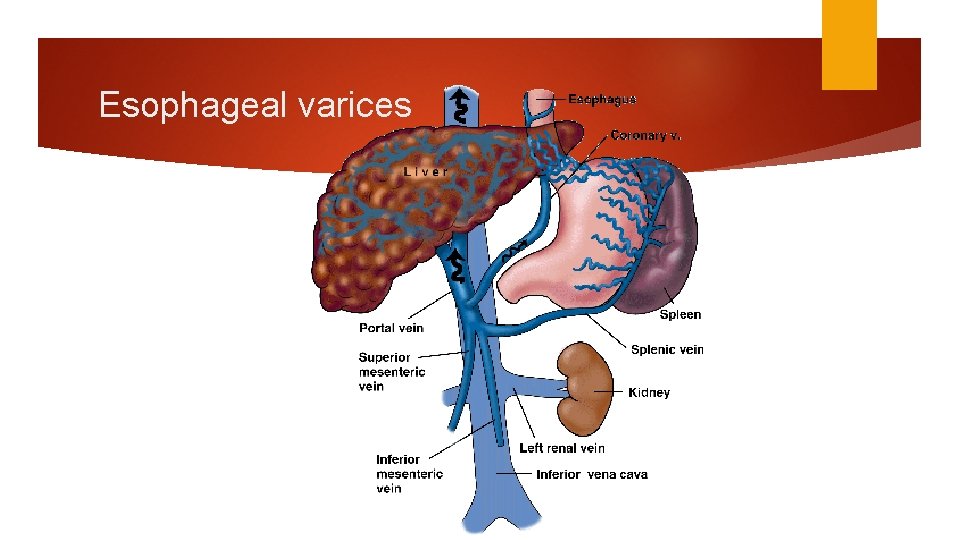
Esophageal varices
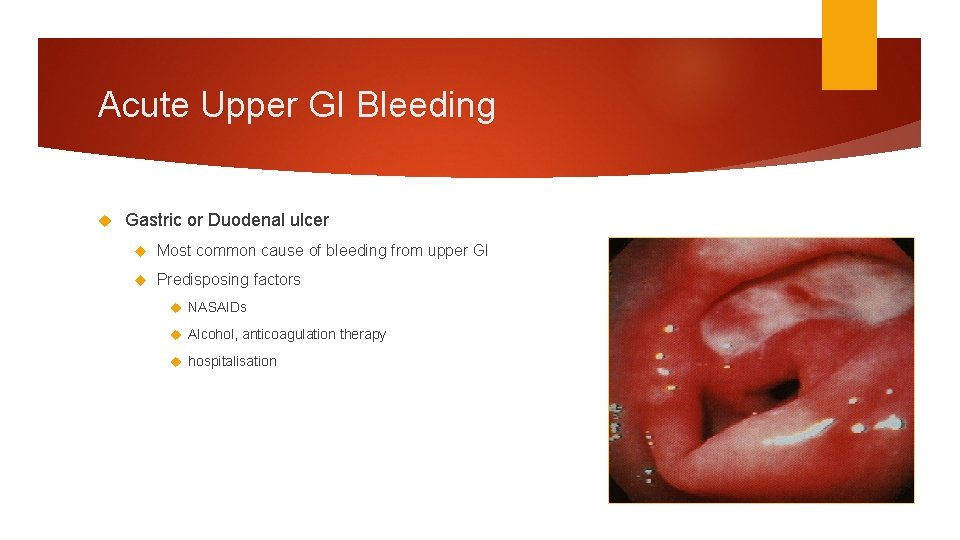
Acute Upper GI Bleeding Gastric or Duodenal ulcer Most common cause of bleeding from upper GI Predisposing factors NASAIDs Alcohol, anticoagulation therapy hospitalisation
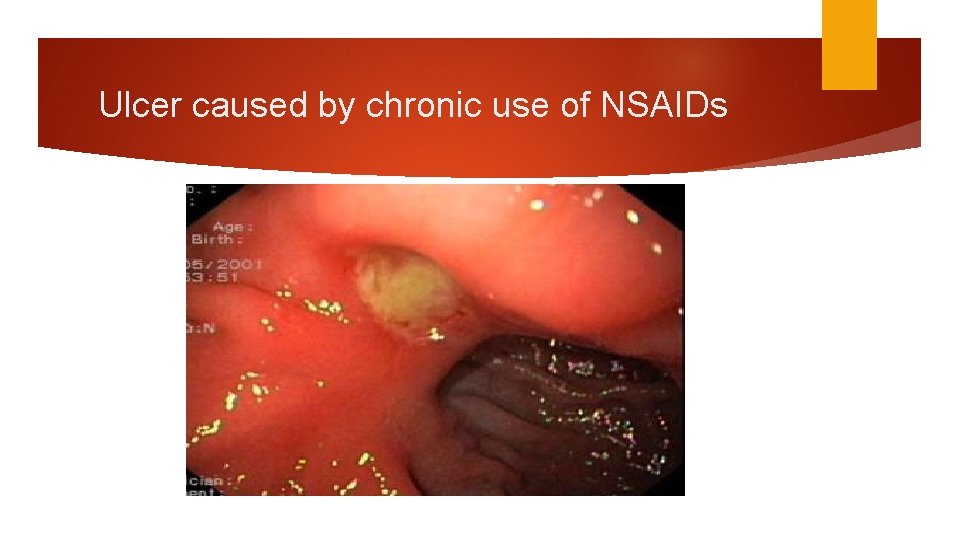
Ulcer caused by chronic use of NSAIDs
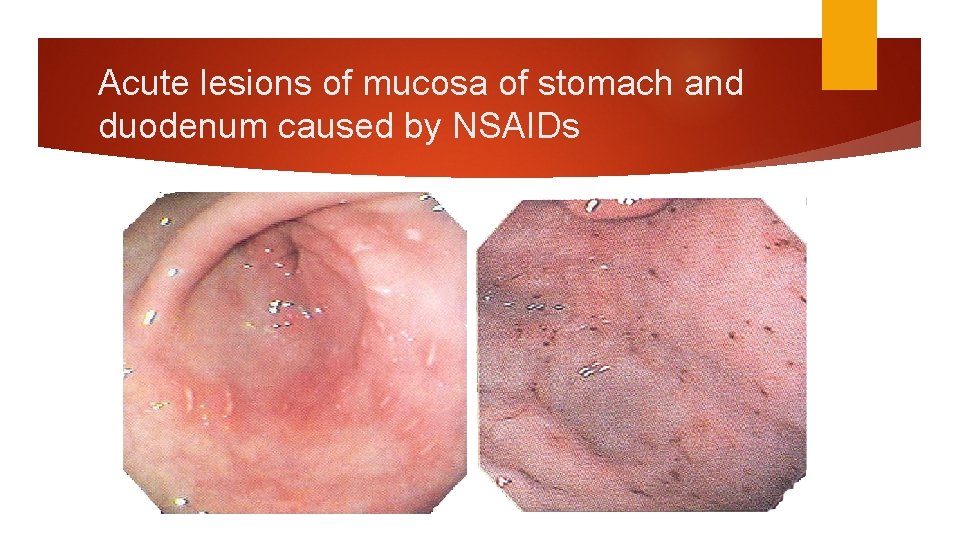
Acute lesions of mucosa of stomach and duodenum caused by NSAIDs
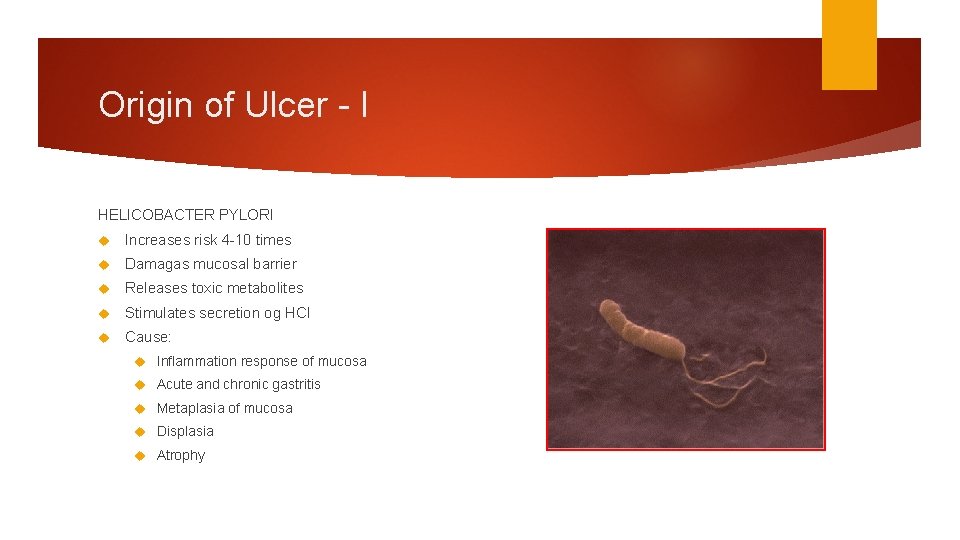
Origin of Ulcer - I HELICOBACTER PYLORI Increases risk 4 -10 times Damagas mucosal barrier Releases toxic metabolites Stimulates secretion og HCl Cause: Inflammation response of mucosa Acute and chronic gastritis Metaplasia of mucosa Displasia Atrophy
Origin Of Ulcer - II Non Steroidal Anti Inflammatory Drugs (NSAIDs) NSAIDs interact with metabolism of prostaglandin Most often prescribed medication in world Huge number of indication Antiinflammatory Analgetic 75% of patients don’t know of possibility of GIT complications “silent epidemic”
Mechanism of NSAIDs Inhibition of cyclooxygenase (COX-1, COX-2) and release of prostaglandin Prostaglandin: Stimulation of secetion of bicarbonates Incresae in perfusion of mucosa Faster cellular proliferation Stimulation of production of c. AMP Stabiilization of cellular lysosomes and membrane Stimulation of active surface phospholipids
Origin Of Ulcer - III Stress Burns Injury of CNS (cushing) Sepsis Politrauma Repiratory insufficiency Coagulopathy Shock Liver failure Kidney failure Multiorgan failure
Further Treatment of Upper GI Bleed Patients with a Hx of PUD or gastritis should be given a IV or PO proton pump inhibitor (omeprazole, pantoprazole, etc. ) Pts with refractory hematemesis: Endoscopy Variceal band ligation is TOC if active variceal bleed found Sclerotherapy Pts with hematemesis refractory to endoscopic band ligation: Transjugular intrahepatic portosystemic shunting (TIPS) Pts diagnosed with esophageal varices should be on daily propranolol
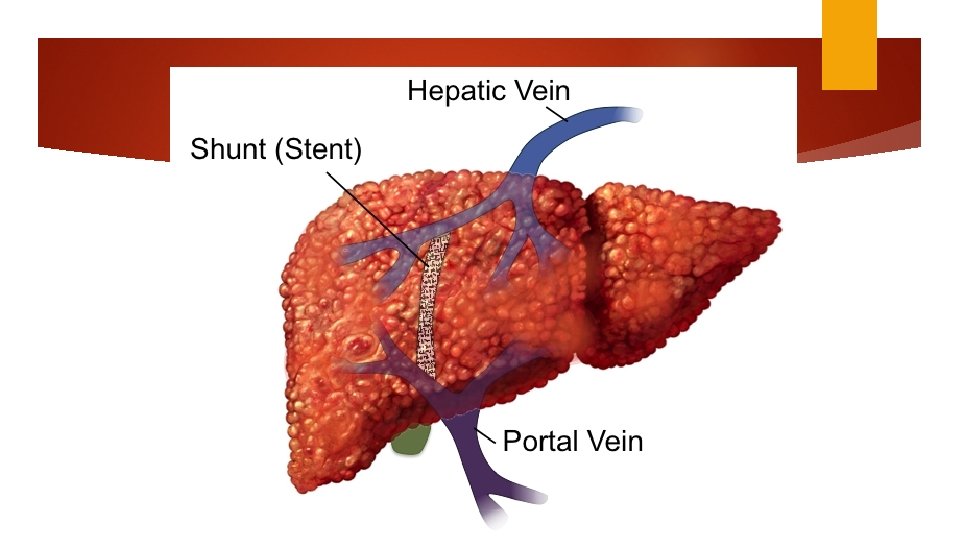
TIPS
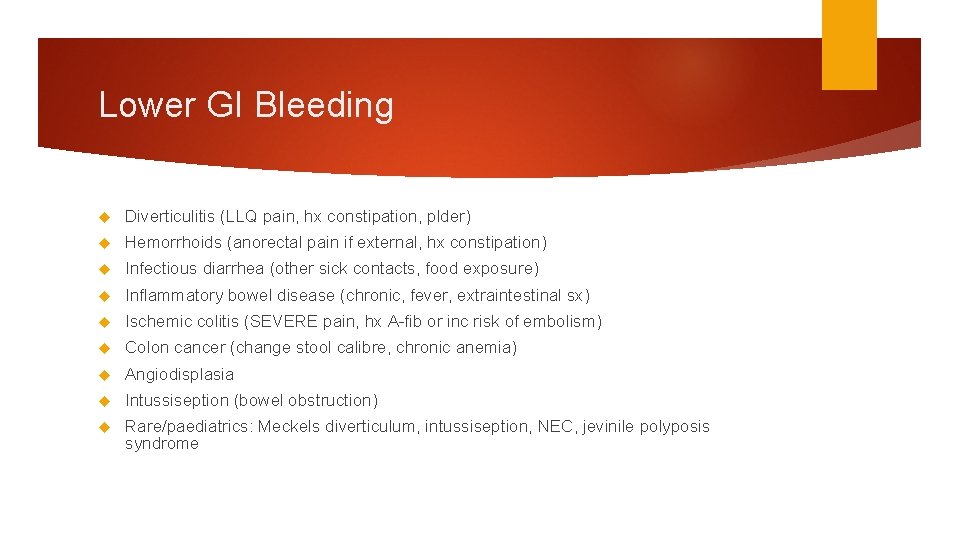
Lower GI Bleeding Diverticulitis (LLQ pain, hx constipation, plder) Hemorrhoids (anorectal pain if external, hx constipation) Infectious diarrhea (other sick contacts, food exposure) Inflammatory bowel disease (chronic, fever, extraintestinal sx) Ischemic colitis (SEVERE pain, hx A-fib or inc risk of embolism) Colon cancer (change stool calibre, chronic anemia) Angiodisplasia Intussiseption (bowel obstruction) Rare/paediatrics: Meckels diverticulum, intussiseption, NEC, jevinile polyposis syndrome
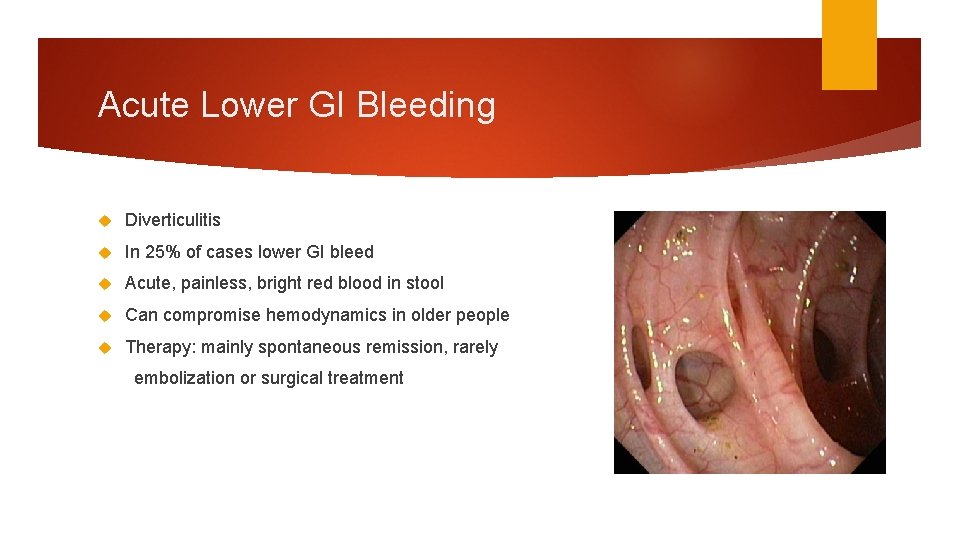
Acute Lower GI Bleeding Diverticulitis In 25% of cases lower GI bleed Acute, painless, bright red blood in stool Can compromise hemodynamics in older people Therapy: mainly spontaneous remission, rarely embolization or surgical treatment
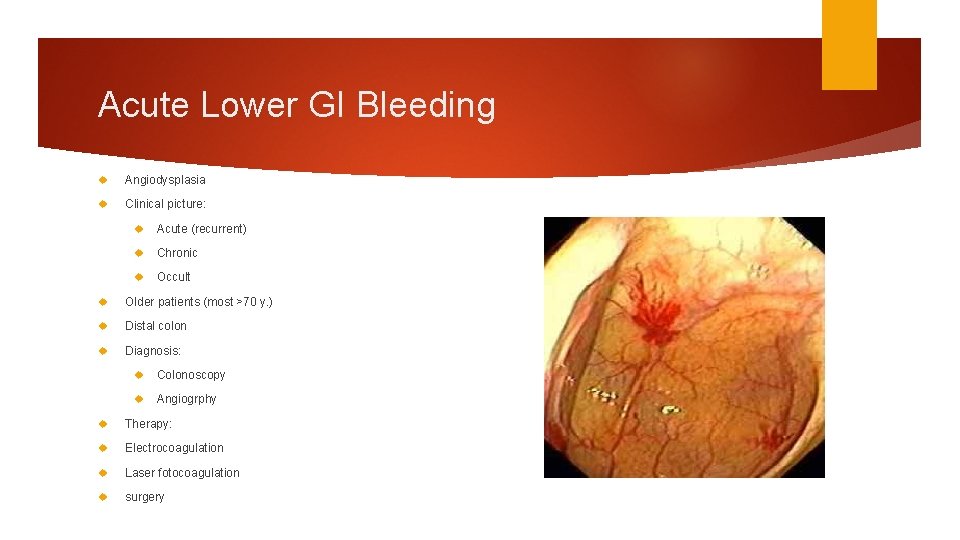
Acute Lower GI Bleeding Angiodysplasia Clinical picture: Acute (recurrent) Chronic Occult Older patients (most >70 y. ) Distal colon Diagnosis: Colonoscopy Angiogrphy Therapy: Electrocoagulation Laser fotocoagulation surgery
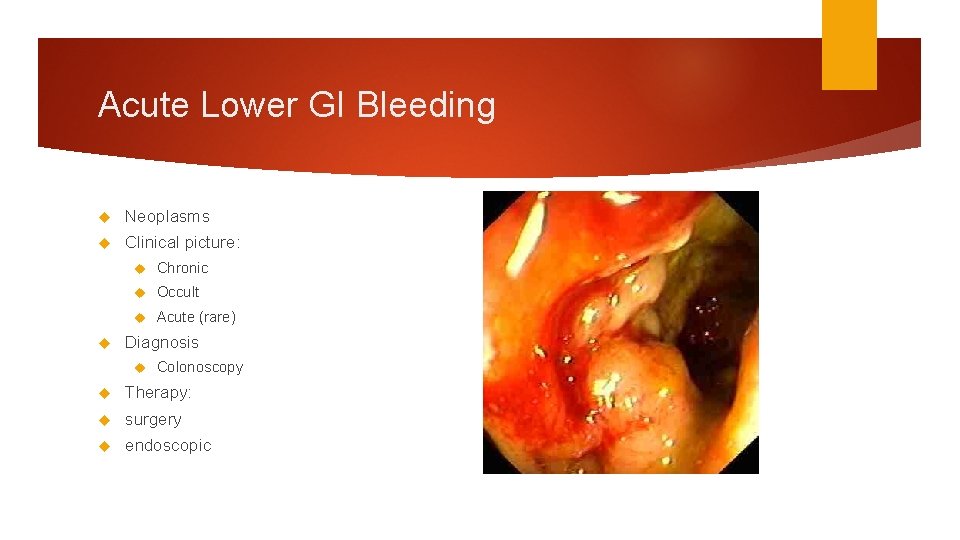
Acute Lower GI Bleeding Neoplasms Clinical picture: Chronic Occult Acute (rare) Diagnosis Colonoscopy Therapy: surgery endoscopic
Acute Lower GI Bleeding Homorrhoids Most common cause Clinical picture: Occasional fresh blood in stool after defecation Constipation makes bleeding stronger Rarely cause of anemia Only diagnose bleeding from Hemorrhoids after elimination of other causes Diagnosis: sigmoidoscopy (>50 y. colonoscopy)
Further treatment of lower GI Bleed When the patient is stable, endoscopy is the next appropriate diagnostic step Endoscopy is diagnostic in 85% of cases Tagged RBC scan be used in patients wher endoscopy is unsuccessful in diagnosis Capsule endoscopy is a last ditch diagnostic test for determining site of GI Bleed (visualizes small intestine)
Recap Severe GI Bleed (hematemesis, ongoing, BP changes): administer fluids! Patients with alcoholism, liver disease, or hematemesis should be given IV octreotide CBC and PT/PTT will help you dictate further resuscitative care. Shoud get EKG too Endoscopy is most accurate test for etiology For varices: octreotide endoscopic band ligation TIPS All patients with varices should be discharged on propranolol
- Slides: 25