Gastrointestinal associated lymphoid tissue GALT Anatomy of immune

- Slides: 40
Gastrointestinal associated lymphoid tissue (GALT)
Anatomy of immune system
primary or central lymphoid organs bone marrow B cells thymus T cells secondary or peripheral lymphoid organs lymph nodes spleen cutaneous immune system mucosal immune system
Mucosal associated lymphoid tissue Mucosal (MALT) gastrointestinal associated lymphoid tissue bronchopulmonary associated lymphoid tissue genitourinary associated lymphoid tissue
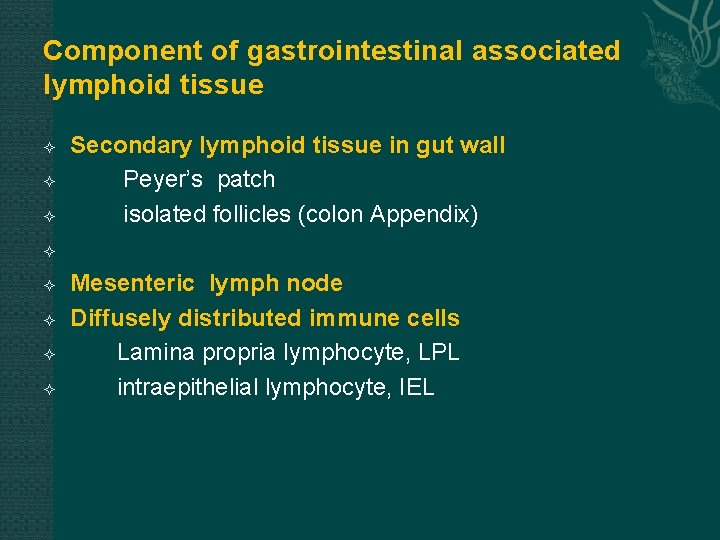
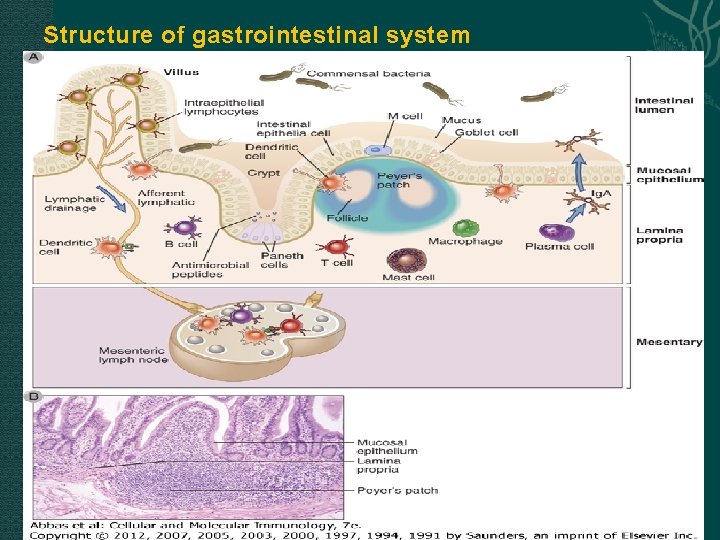
Component of gastrointestinal associated lymphoid tissue Secondary lymphoid tissue in gut wall Peyer’s patch isolated follicles (colon Appendix) Mesenteric lymph node Diffusely distributed immune cells Lamina propria lymphocyte, LPL intraepithelial lymphocyte, IEL
Immunity of gastrointestinal system
two remarkable properties of gastrointestinal tract the combined mucosa of the small and large bowel has a total surface area of more than 200 m 2 It is estimated that more than 500 different species of bacteria, amounting to approximately 1014 cells, live in the mammalian gut commensal organisms noncommensal pathogenic organisms
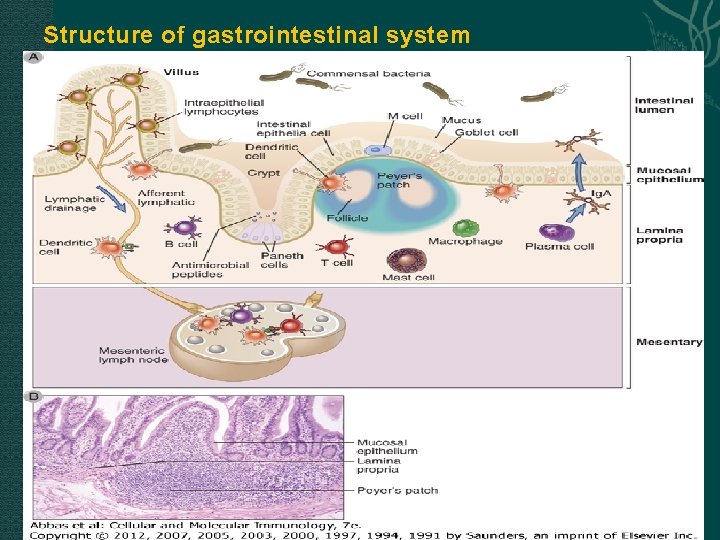
Structure of gastrointestinal system
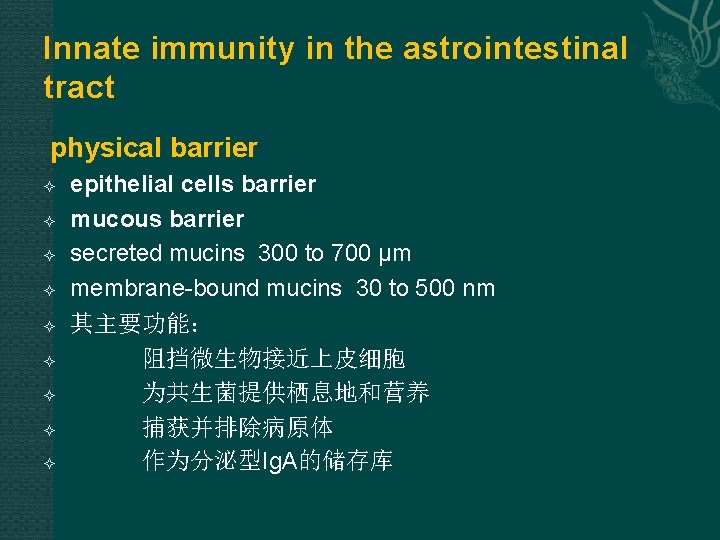
Innate immunity in the astrointestinal tract physical barrier epithelial cells barrier mucous barrier secreted mucins 300 to 700 μm membrane-bound mucins 30 to 500 nm 其主要功能: 阻挡微生物接近上皮细胞 为共生菌提供栖息地和营养 捕获并排除病原体 作为分泌型Ig. A的储存库
chemical barrier 转铁蛋白 溶菌酶 Defensin α-defensins(small bowel Paneth cells ) β-defensins (colonabsorptive epithelial cells)
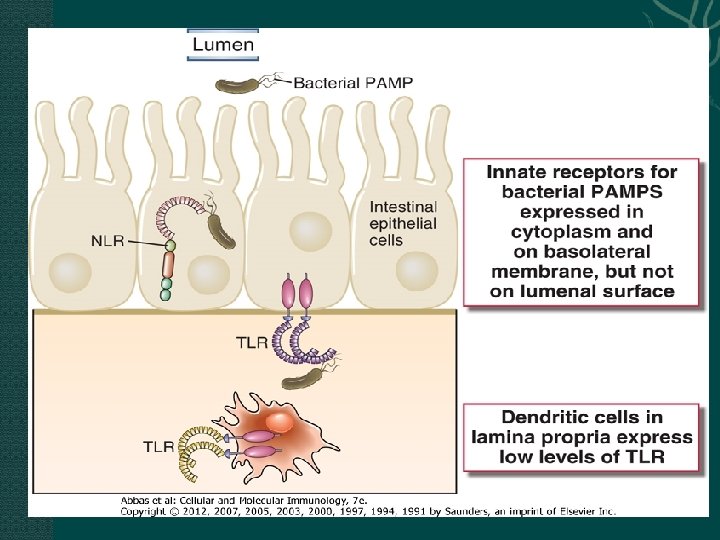
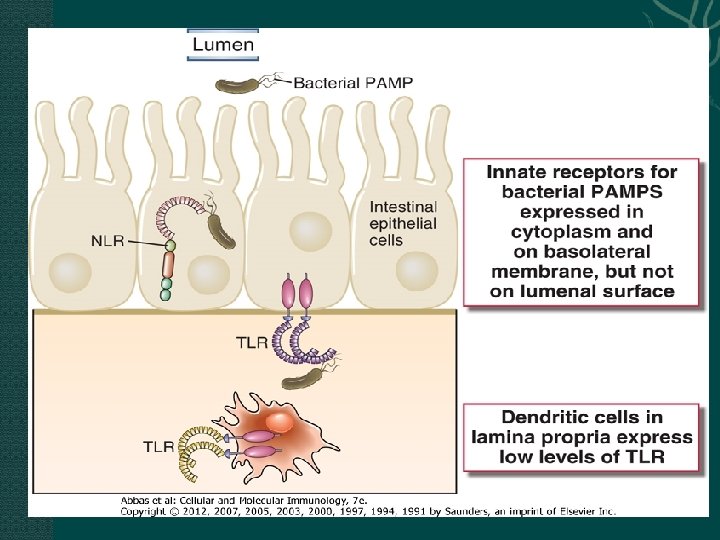
biological barrier commensal organisms 作用:阻止病原体在�道的定居 与病原体�争空�和�养 �生抗菌物�(如蛋白�毒素) TLRs and NLRs 的表达�黏膜固有免疫的影响 DCs and macrophages in the lamina propria of the gut inhibit inflammation IL-10 transforming growth factor-β (TGF-β)
Adaptive Immunity in the Gastrointestinal Tract features of gastrointestinal adaptiveimmunity The major form of adaptive immunity in the gut is humoral immunity The dominant protective cell-mediated immune response consists of TH 17 effector cells The adaptive immune system in the gut must continuously suppress potential immune responses to food antigens and commensal microbial antigens
The Functional Anatomy of the Adaptive Immune System in the Gastrointestinal Tract
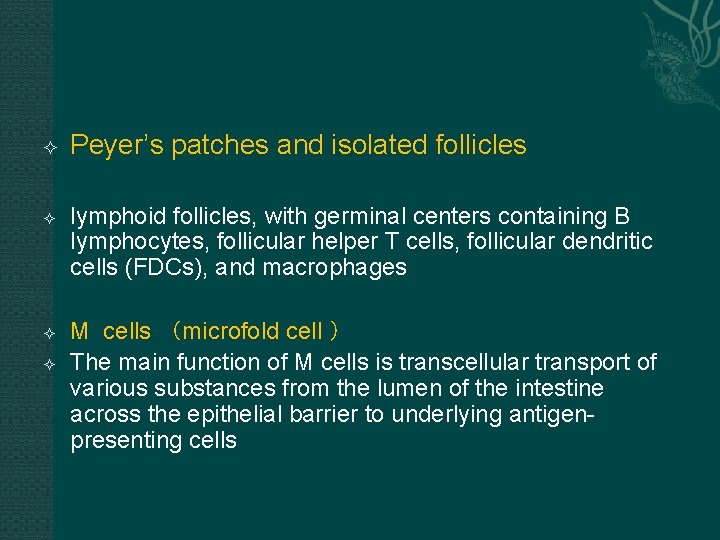
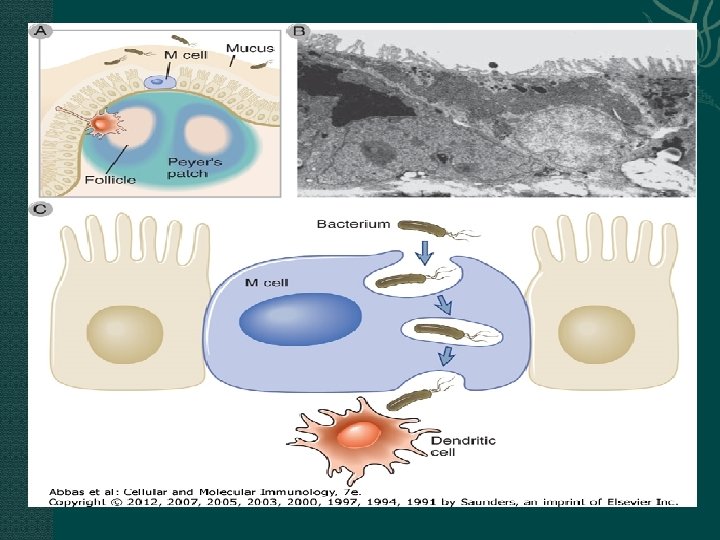
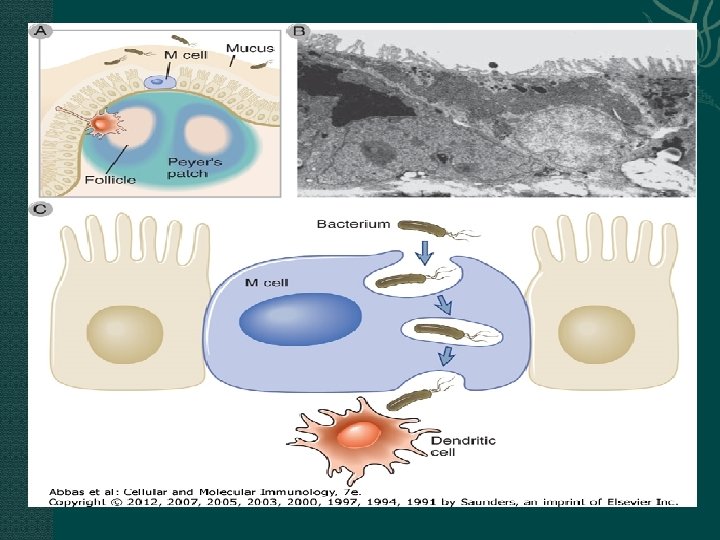
Peyer’s patches and isolated follicles lymphoid follicles, with germinal centers containing B lymphocytes, follicular helper T cells, follicular dendritic cells (FDCs), and macrophages M cells (microfold cell ) The main function of M cells is transcellular transport of various substances from the lumen of the intestine across the epithelial barrier to underlying antigenpresenting cells
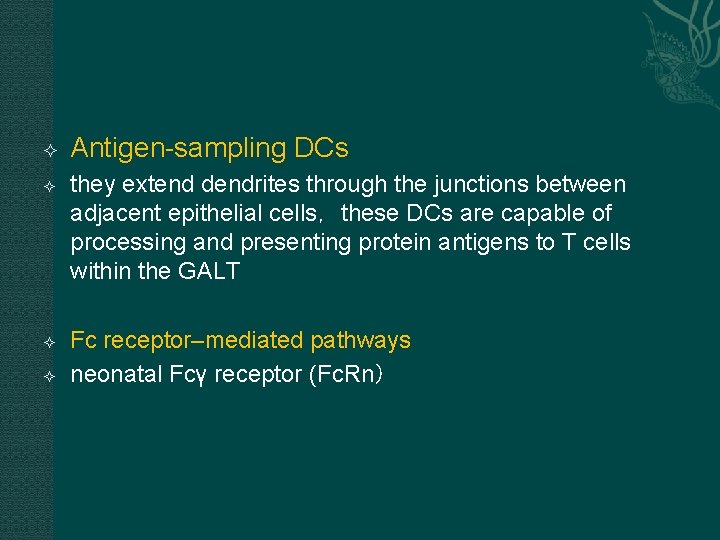
Antigen-sampling DCs they extend dendrites through the junctions between adjacent epithelial cells,these DCs are capable of processing and presenting protein antigens to T cells within the GALT Fc receptor–mediated pathways neonatal Fcγ receptor (Fc. Rn)
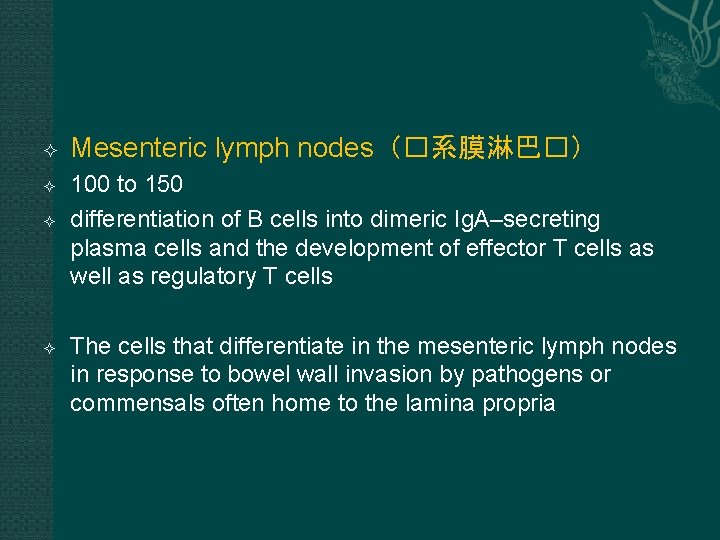
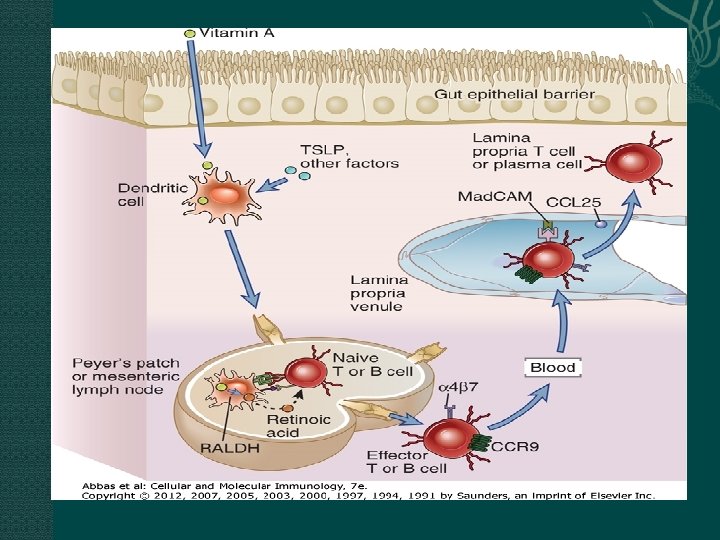
Mesenteric lymph nodes(�系膜淋巴�) 100 to 150 differentiation of B cells into dimeric Ig. A–secreting plasma cells and the development of effector T cells as well as regulatory T cells The cells that differentiate in the mesenteric lymph nodes in response to bowel wall invasion by pathogens or commensals often home to the lamina propria
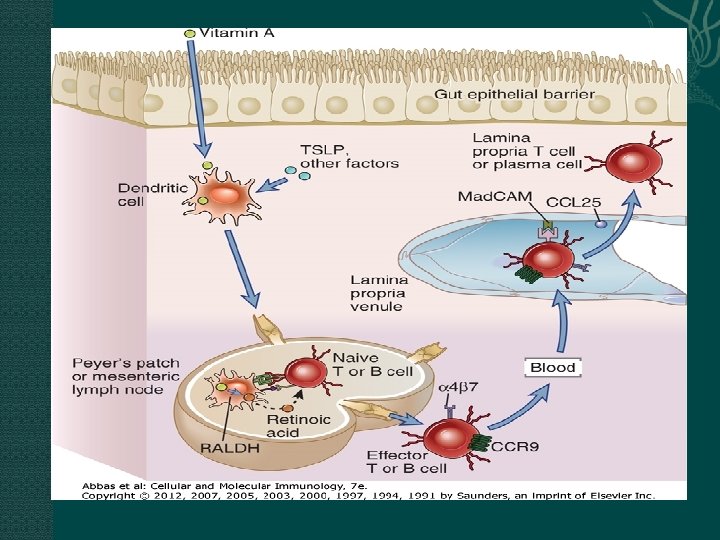
gut-homing of Ig. A-producing cells and effector T cells Effector lymphocytes that are generated in the GALT and mesenteric lymph nodes are imprinted with selective integrin- and chemokine receptor–dependent gut-homing properties, and they circulate from the blood back into the lamina propria of the gut

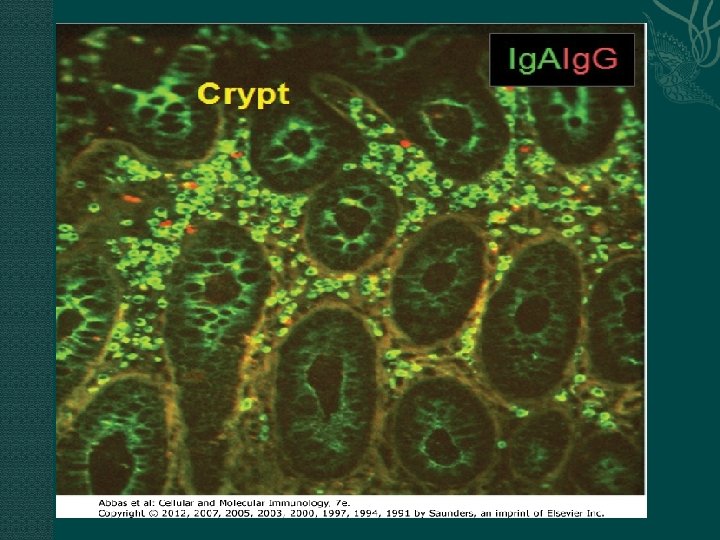
Humoral Immunity in the Gastrointestinal Tract production of secretory Ig. A in the GALT secretory immunity:Within the lumen, Ig. A, Ig. G, and Ig. M antibodies bind to microbes and toxins and neutralize them by preventing their binding to receptors on host cells. Ig. A is produced in larger amounts than any other antibody isotype 2 g of Ig. A per day
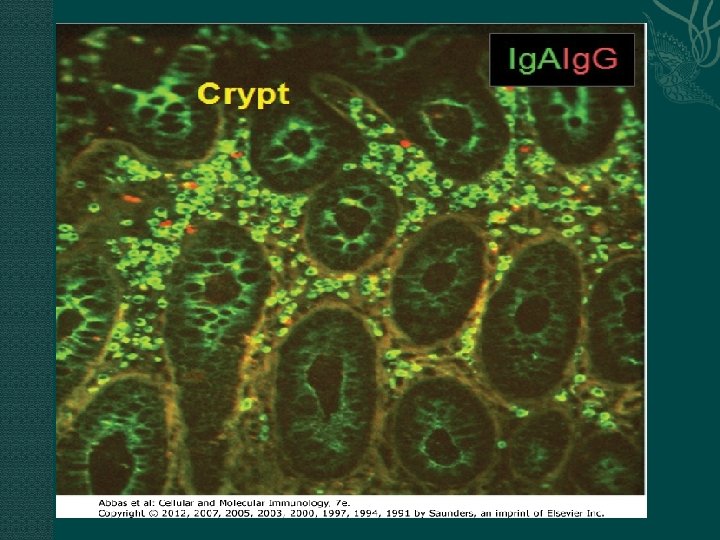
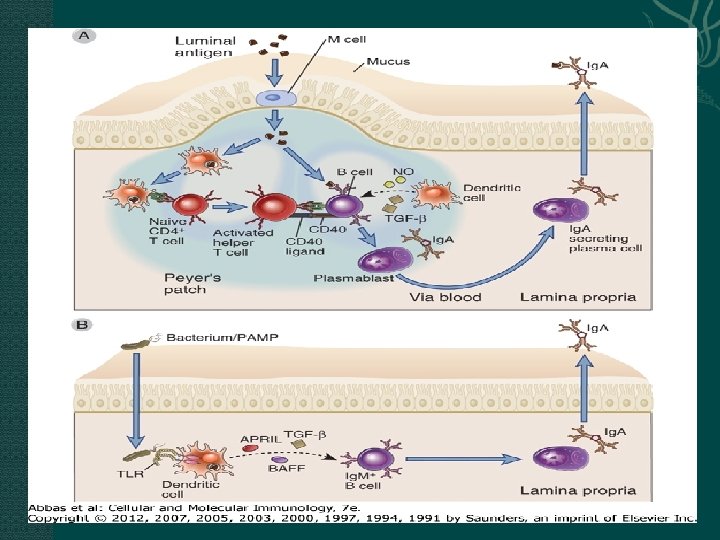
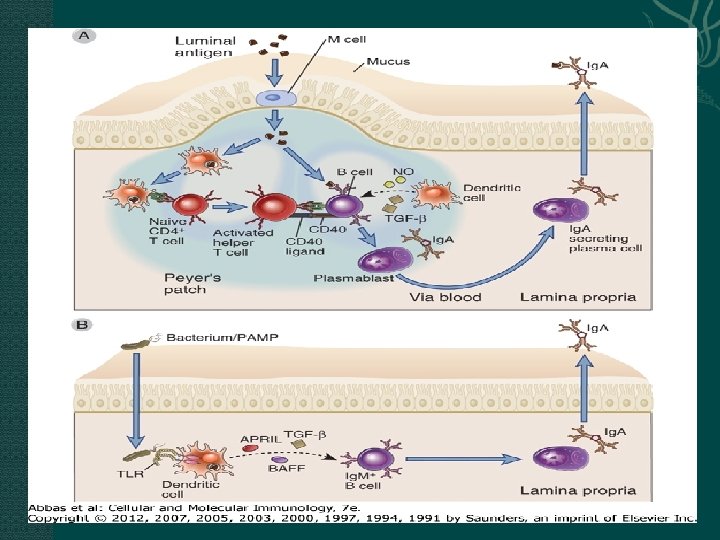
Ig. A isotype switching in B cells in GALT and mesenteric lymph nodes T-dependent mechanisms T-independent mechanisms
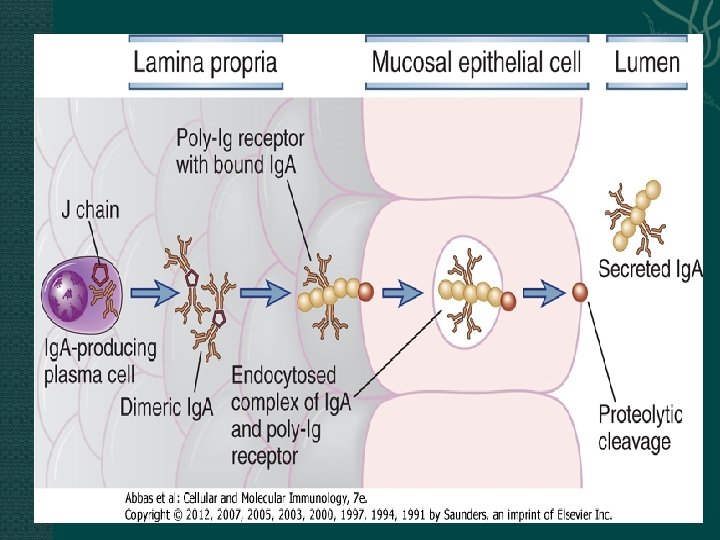
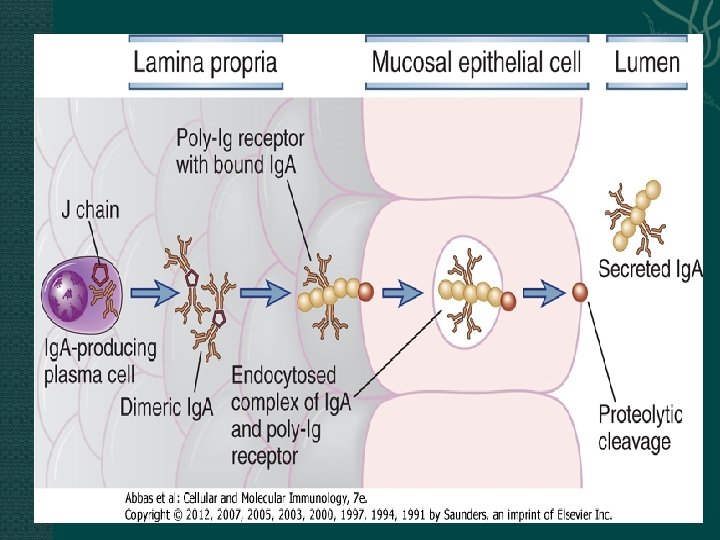
Secreted Ig. A is transported through epithelial cells into the intestinal lumen by an Ig. A/Ig. M-specific Fc receptor called the poly-Ig receptor
Transport of Ig. M and Ig. G Ig. M Poly-Ig. R Ig. G neonatal Fc receptor (Fc. Rn) bidirectional transport
T Cell–Mediated Immunity in the Gastrointestinal Tract T cells are found within the gut epithelial layer, scattered throughout the lamina propria and submucosa, and within Peyer’s patches and other organized collections of follicles
most of the intraepithelial T cells are CD 8+ cells Lamina propria T cells are mostly CD 4+, and most have the phenotype of activated effector or memory T cells within Peyer’s patches and in other follicles adjacent to the intestinal epithelium include CD 4+ helper T cells and regulatory T cells
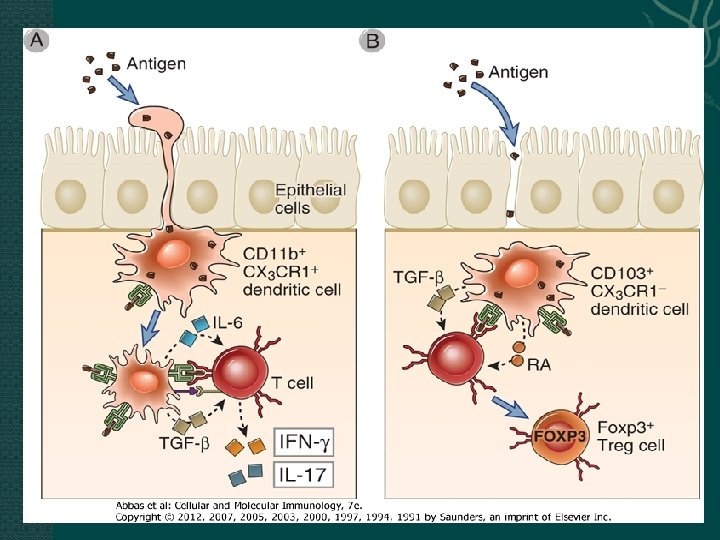
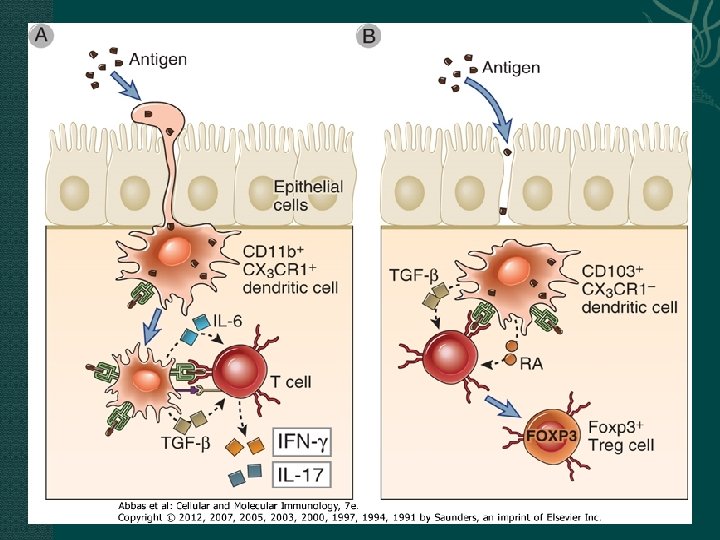
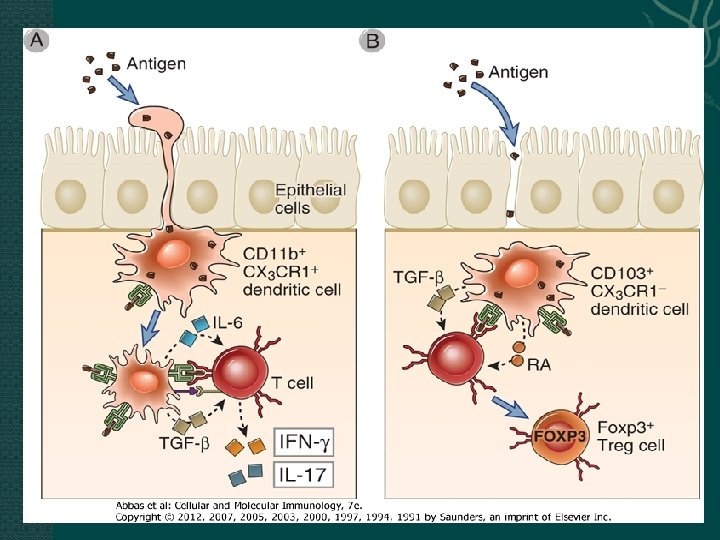
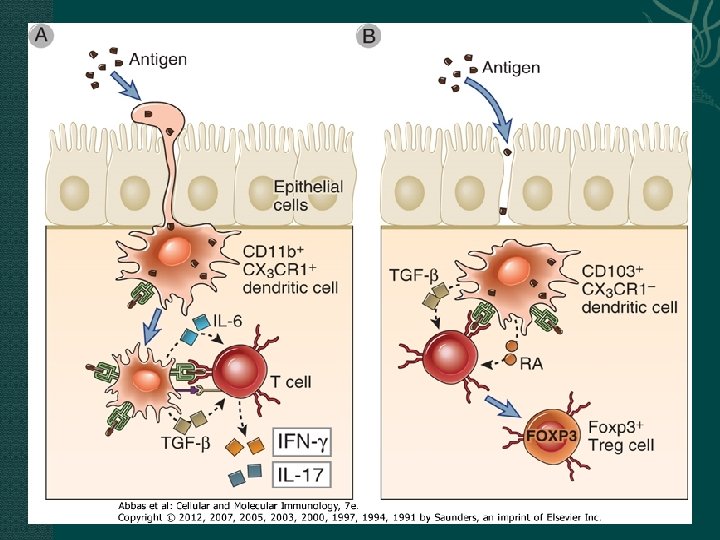
DCs of gastrointestinal immune system effector DCs CD 11 b+CX 3 CR 1+ induce T cells into IFN-γ– or IL-17–producing effector cells regulatory DCs CD 103+CX 3 CR 1− induce the differentiation of naive T cells into Fox. P 3+ regulatory T cells
TH 17 cells produce IL-17 and IL-22 which induce the expression of proteins important for barrier function, such as mucins and β-defensins TH 2 responses which are effective in eliminating the worms in intestinal helminthic infections because the TH 2 cytokines IL-4 and IL-13 cooperate in enhancing fluid and mucus secretions and inducing smooth muscle contraction and bowel motility
Regulation of Immunity in the Gastrointestinal Tract by Regulatory T Cells and Cytokines Fox. P 3+ Treg are thought to suppress immune responses by several mechanisms. Of these, the dominant mechanism in the gut seems to be production of the immunosuppressive cytokine IL-10.
cytokines maintaining homeostasis in the gut immune system TGF-β, IL-10, and IL-2 The uncontrolled inflammation observed in the gut in the absence of these cytokines or their receptors is most likely caused by innate and adaptive immune responses to commensal gut flora
Oral Tolerance Oral tolerance is systemic adaptive immune tolerance to antigens that are ingested or otherwise administered orally and is a potential way of treating diseases in which unwanted immune responses occur, such as autoimmunity
The physiologic role of oral tolerance is speculated to be the prevention of potentially harmful immune responses to food proteins and commensal bacteria 其可能的机制: 口服高�量抗原�致特异性 T�胞凋亡或失能,巨噬�胞 在吞噬凋亡�胞�程中�生 TGF-β,诱导Treg�生 口服低�量抗原����性 T�胞