Gastroesophageal Reflux in Children By Karla Au Yeung

Gastroesophageal Reflux in Children By Karla Au Yeung LTC, MC, USA 21 November 2007
Definition • Gastroesophageal Reflux: – Involuntary retrograde movement of stomach contents into the esophagus – Regurgitation is when the stomach contents pass the lower and upper esophageal sphincters – Vomiting is expulsion of refluxed gastric contents into the oral pharynx • Gastroesophageal Reflux Disease: – Symptoms of tissue damage caused by GER – Extraintestinal symptoms
“A picture is worth a 1000 words. . . ” From: PE Hyman, Pediat GI Problems, vol 4 of Gastroenterology and Hepatology, Current Medicine, Philadelphia, 1997
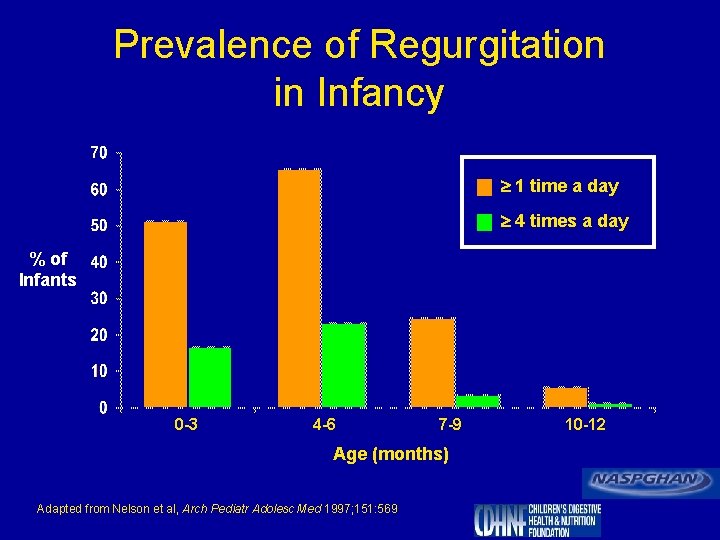
Prevalence of Regurgitation in Infancy 1 time a day 4 times a day % of Infants 0 -3 4 -6 7 -9 Age (months) Adapted from Nelson et al, Arch Pediatr Adolesc Med 1997; 151: 569 10 -12
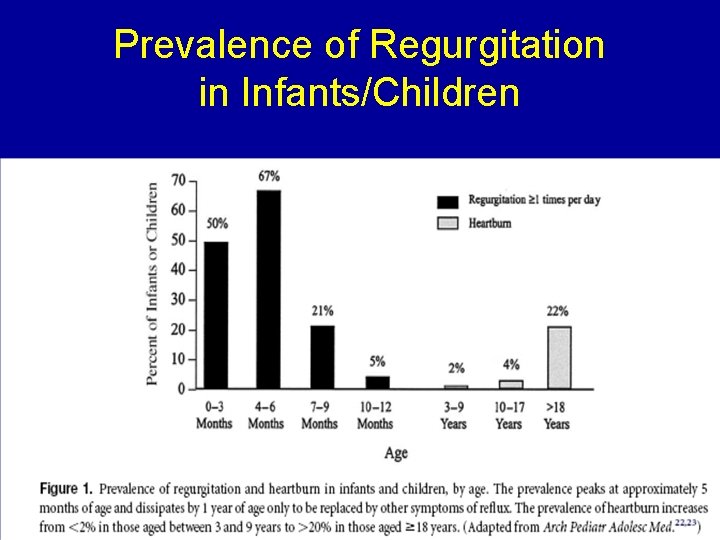
Prevalence of Regurgitation in Infants/Children
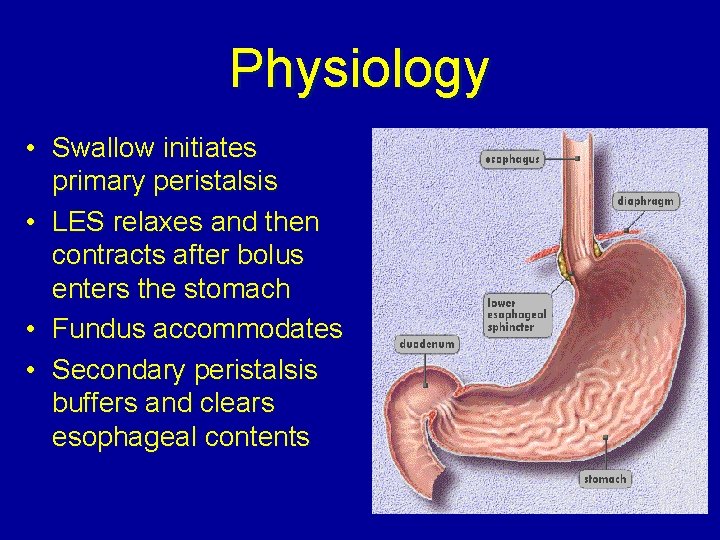
Physiology • Swallow initiates primary peristalsis • LES relaxes and then contracts after bolus enters the stomach • Fundus accommodates • Secondary peristalsis buffers and clears esophageal contents
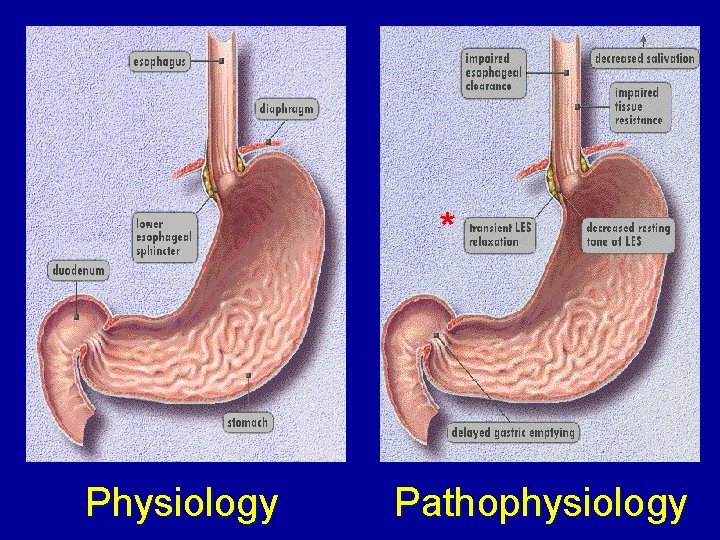
* Physiology Pathophysiology
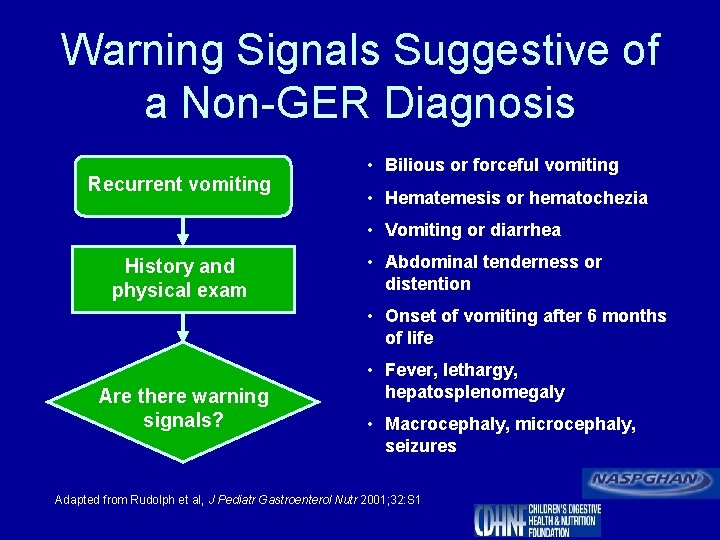
Warning Signals Suggestive of a Non-GER Diagnosis Recurrent vomiting • Bilious or forceful vomiting • Hematemesis or hematochezia • Vomiting or diarrhea History and physical exam • Abdominal tenderness or distention • Onset of vomiting after 6 months of life Are there warning signals? • Fever, lethargy, hepatosplenomegaly • Macrocephaly, microcephaly, seizures Adapted from Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1
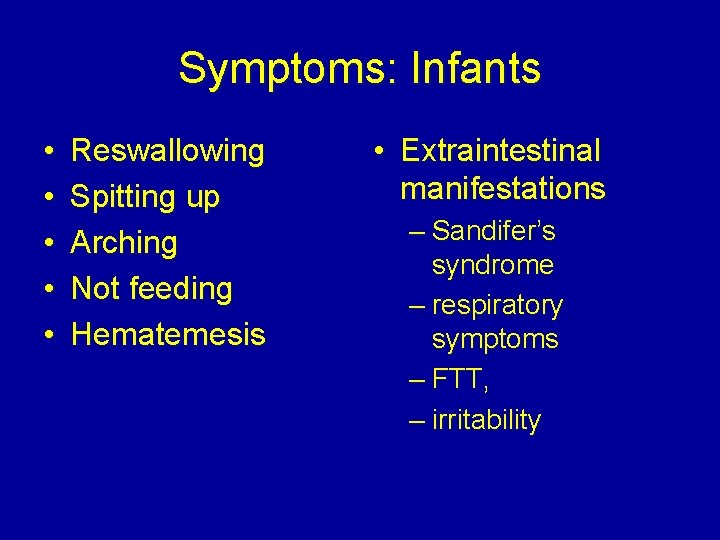
Symptoms: Infants • • • Reswallowing Spitting up Arching Not feeding Hematemesis • Extraintestinal manifestations – Sandifer’s syndrome – respiratory symptoms – FTT, – irritability
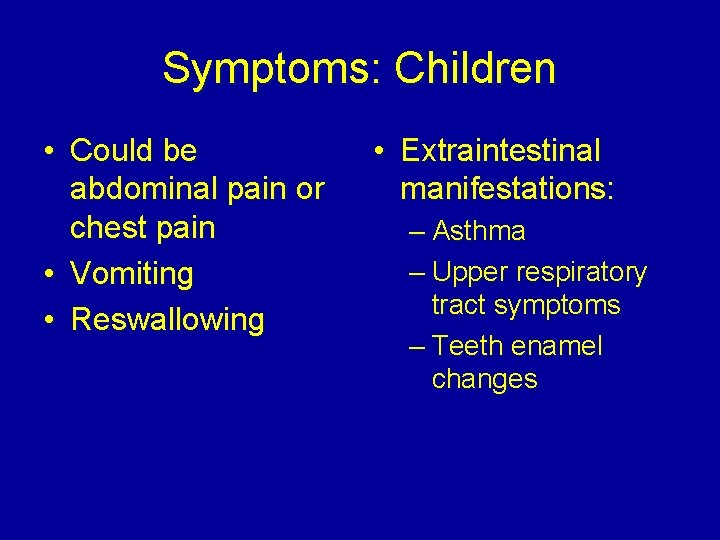
Symptoms: Children • Could be abdominal pain or chest pain • Vomiting • Reswallowing • Extraintestinal manifestations: – Asthma – Upper respiratory tract symptoms – Teeth enamel changes
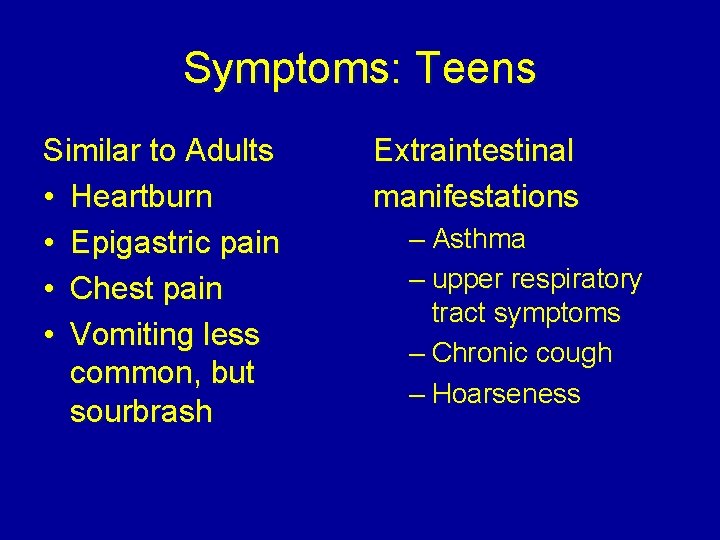
Symptoms: Teens Similar to Adults • Heartburn • Epigastric pain • Chest pain • Vomiting less common, but sourbrash Extraintestinal manifestations – Asthma – upper respiratory tract symptoms – Chronic cough – Hoarseness
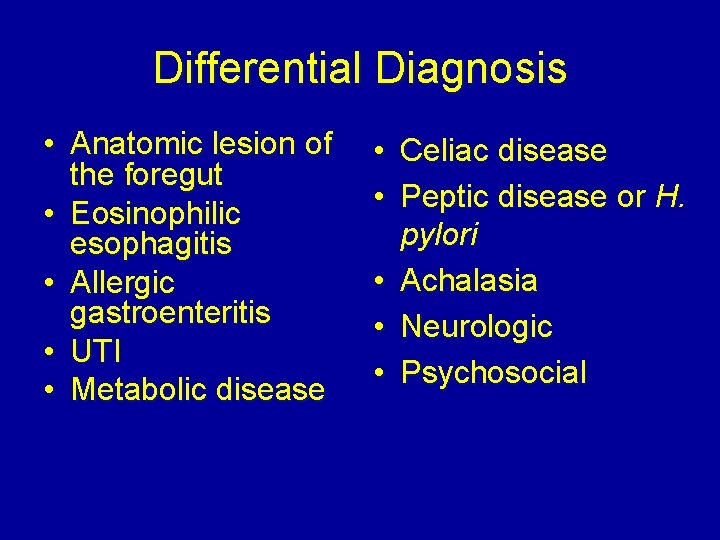
Differential Diagnosis • Anatomic lesion of the foregut • Eosinophilic esophagitis • Allergic gastroenteritis • UTI • Metabolic disease • Celiac disease • Peptic disease or H. pylori • Achalasia • Neurologic • Psychosocial
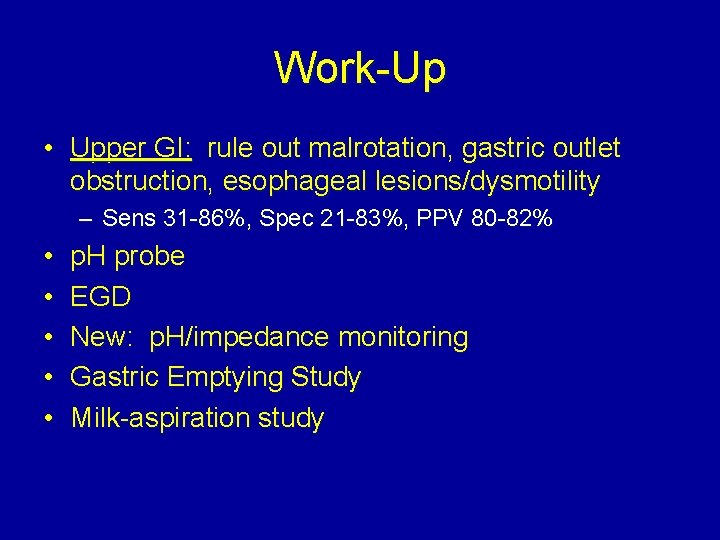
Work-Up • Upper GI: rule out malrotation, gastric outlet obstruction, esophageal lesions/dysmotility – Sens 31 -86%, Spec 21 -83%, PPV 80 -82% • • • p. H probe EGD New: p. H/impedance monitoring Gastric Emptying Study Milk-aspiration study

Upper GI Series
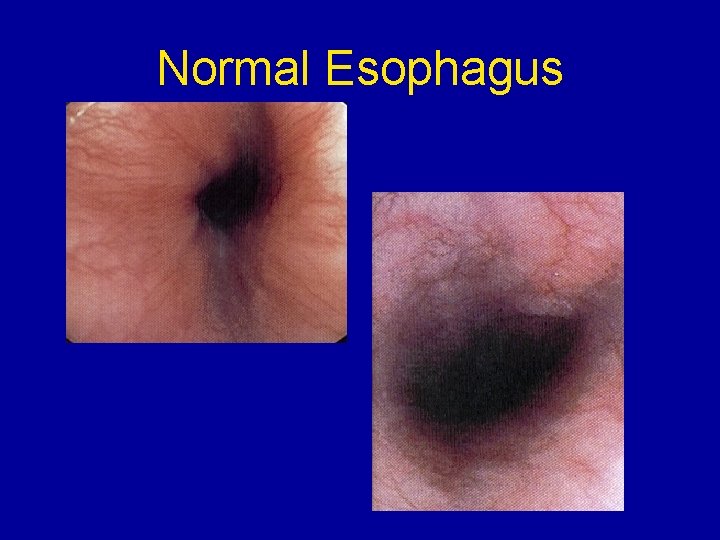
Normal Esophagus
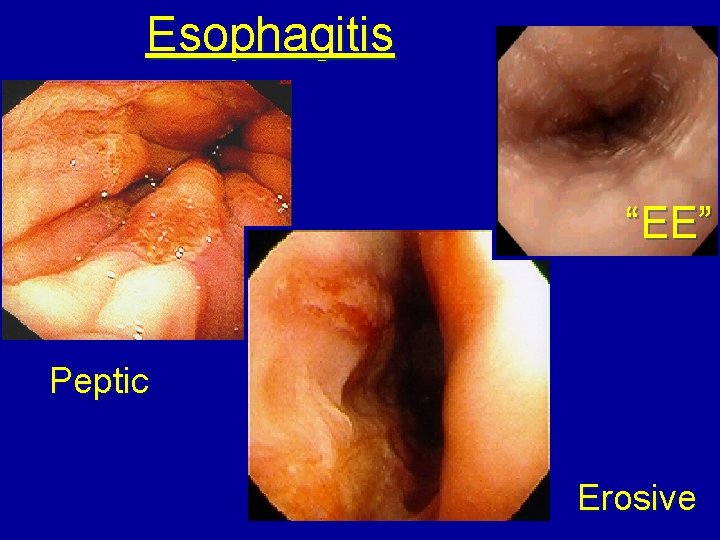
Esophagitis “EE” Peptic Erosive
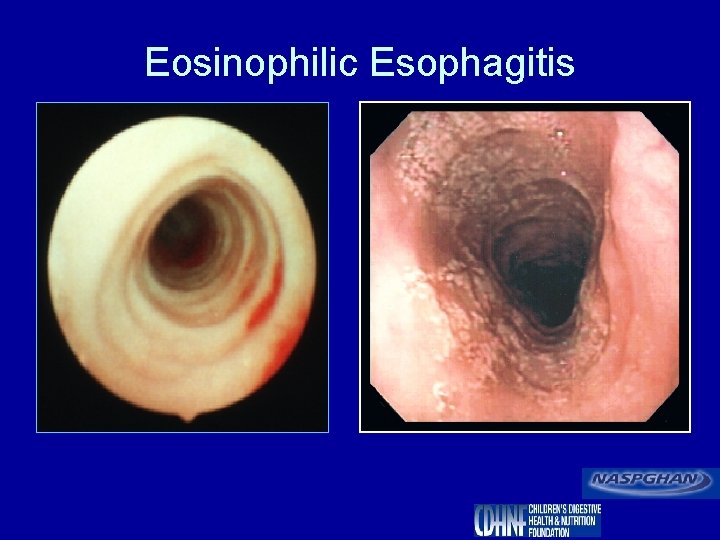
Eosinophilic Esophagitis

Treatment: Alternatives to Medication • • • Formula changes for infants Small Frequent Feeds Rice Cereal Added to Feeds Positioning Rumination – Treat anxiety, Hypnosis, Biofeedback • Weight loss, avoid certain dietary items
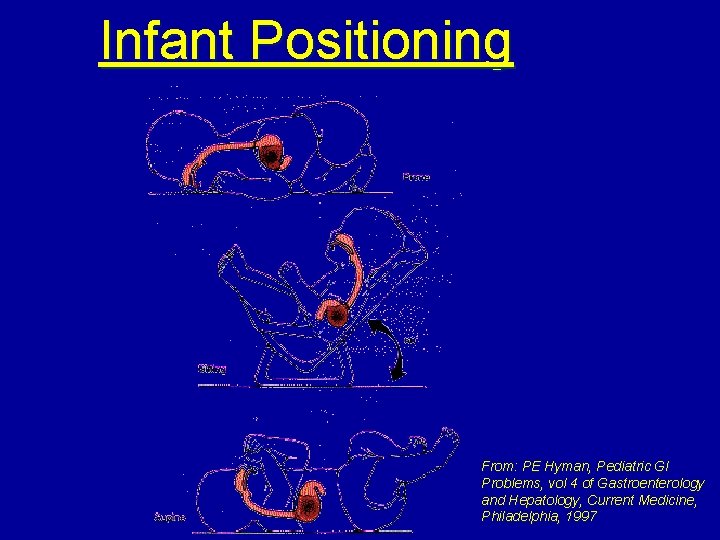
Infant Positioning From: PE Hyman, Pediatric GI Problems, vol 4 of Gastroenterology and Hepatology, Current Medicine, Philadelphia, 1997
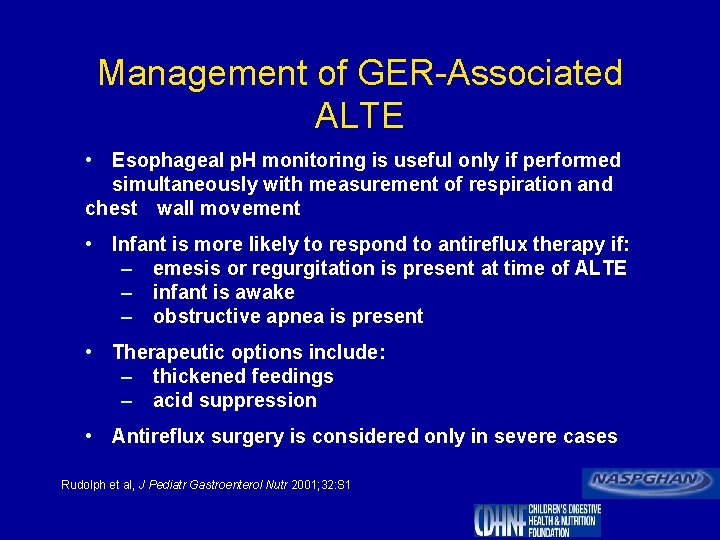
Management of GER-Associated ALTE • Esophageal p. H monitoring is useful only if performed simultaneously with measurement of respiration and chest wall movement • Infant is more likely to respond to antireflux therapy if: – emesis or regurgitation is present at time of ALTE – infant is awake – obstructive apnea is present • Therapeutic options include: – thickened feedings – acid suppression • Antireflux surgery is considered only in severe cases Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1
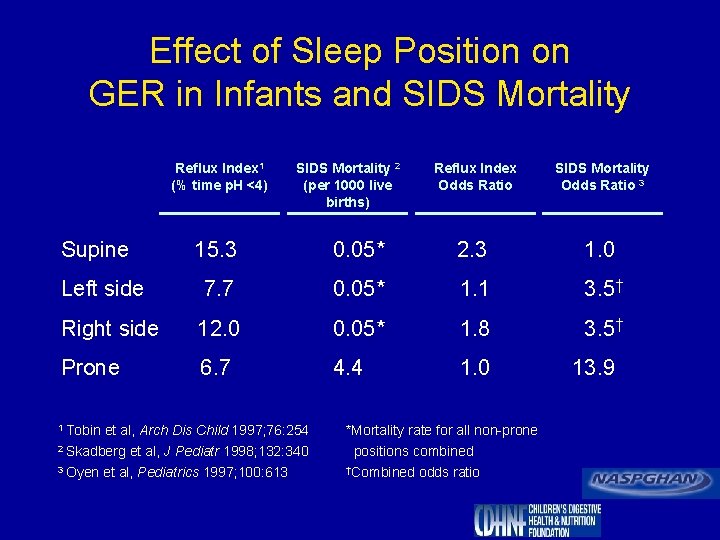
Effect of Sleep Position on GER in Infants and SIDS Mortality Reflux Index 1 (% time p. H <4) Supine SIDS Mortality 2 (per 1000 live births) Reflux Index Odds Ratio SIDS Mortality Odds Ratio 3 15. 3 0. 05* 2. 3 1. 0 Left side 7. 7 0. 05* 1. 1 3. 5† Right side 12. 0 0. 05* 1. 8 3. 5† Prone 6. 7 4. 4 1. 0 1 Tobin et al, Arch Dis Child 1997; 76: 254 2 Skadberg 3 Oyen et al, J Pediatr 1998; 132: 340 et al, Pediatrics 1997; 100: 613 *Mortality rate for all non-prone positions combined †Combined odds ratio 13. 9
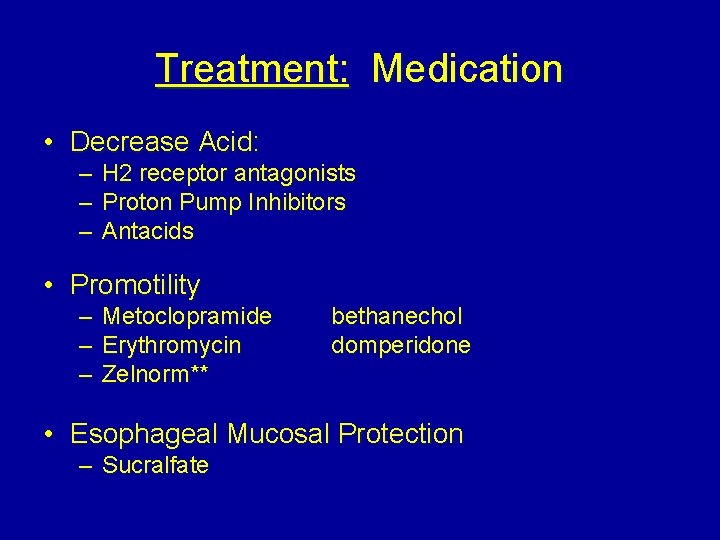
Treatment: Medication • Decrease Acid: – H 2 receptor antagonists – Proton Pump Inhibitors – Antacids • Promotility – – – Metoclopramide Erythromycin Zelnorm** bethanechol domperidone • Esophageal Mucosal Protection – Sucralfate
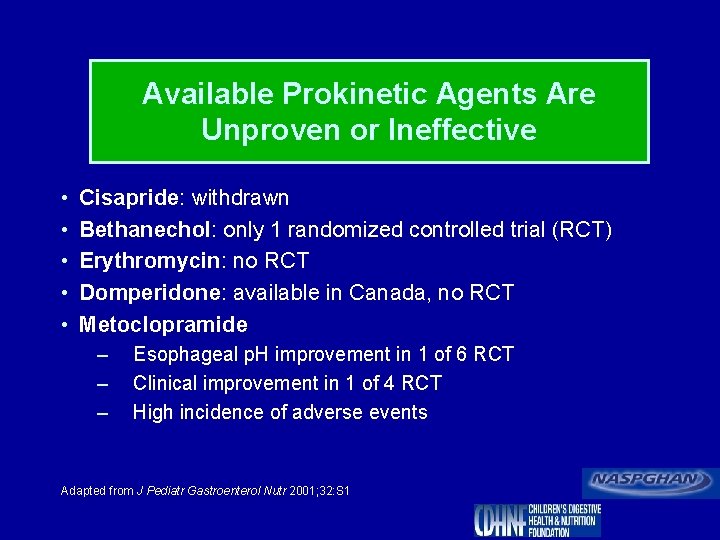
Available Prokinetic Agents Are Unproven or Ineffective • • • Cisapride: withdrawn Bethanechol: only 1 randomized controlled trial (RCT) Erythromycin: no RCT Domperidone: available in Canada, no RCT Metoclopramide – – – Esophageal p. H improvement in 1 of 6 RCT Clinical improvement in 1 of 4 RCT High incidence of adverse events Adapted from J Pediatr Gastroenterol Nutr 2001; 32: S 1
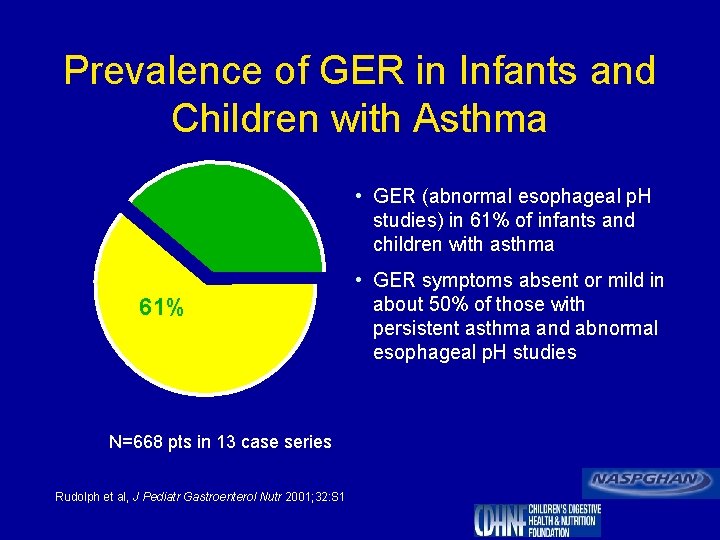
Prevalence of GER in Infants and Children with Asthma • GER (abnormal esophageal p. H studies) in 61% of infants and children with asthma 61% N=668 pts in 13 case series Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1 • GER symptoms absent or mild in about 50% of those with persistent asthma and abnormal esophageal p. H studies
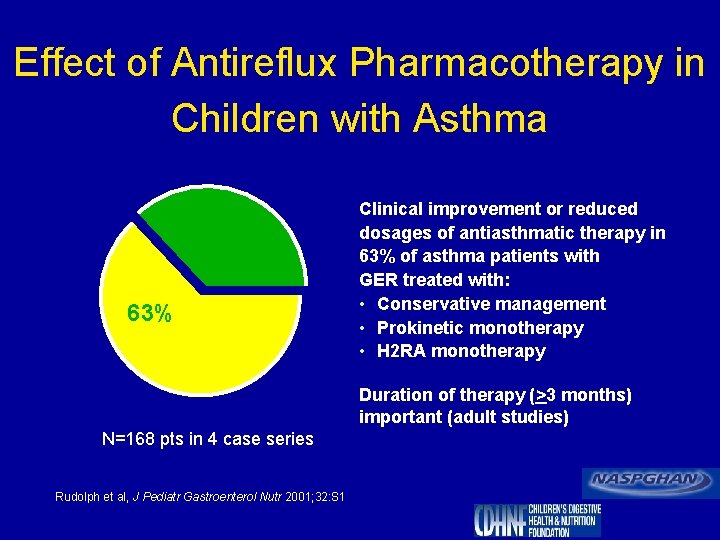
Effect of Antireflux Pharmacotherapy in Children with Asthma 63% Clinical improvement or reduced dosages of antiasthmatic therapy in 63% of asthma patients with GER treated with: • Conservative management • Prokinetic monotherapy • H 2 RA monotherapy Duration of therapy (>3 months) important (adult studies) N=168 pts in 4 case series Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1
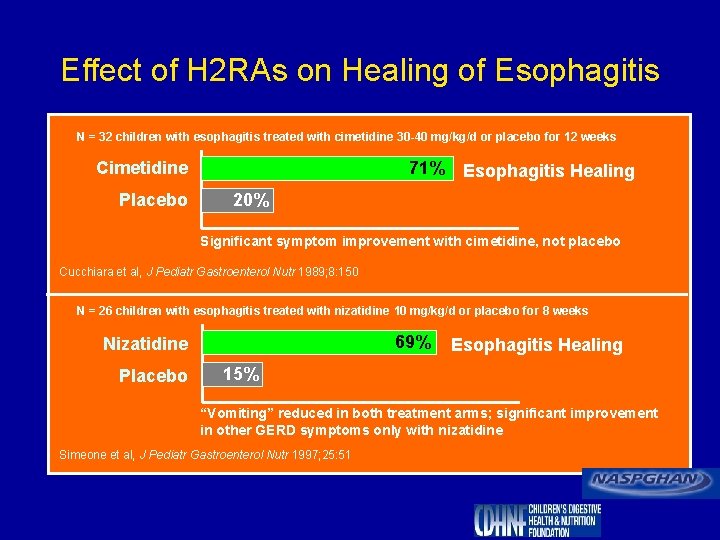
Effect of H 2 RAs on Healing of Esophagitis N = 32 children with esophagitis treated with cimetidine 30 -40 mg/kg/d or placebo for 12 weeks Cimetidine Placebo 71% Esophagitis Healing 20% Significant symptom improvement with cimetidine, not placebo Cucchiara et al, J Pediatr Gastroenterol Nutr 1989; 8: 150 N = 26 children with esophagitis treated with nizatidine 10 mg/kg/d or placebo for 8 weeks 69% Nizatidine Placebo Esophagitis Healing 15% “Vomiting” reduced in both treatment arms; significant improvement in other GERD symptoms only with nizatidine Simeone et al, J Pediatr Gastroenterol Nutr 1997; 25: 51
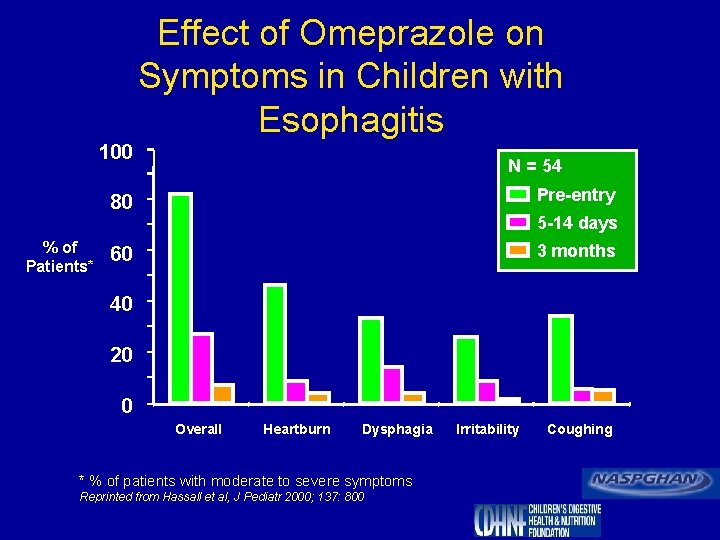
Effect of Omeprazole on Symptoms in Children with Esophagitis 100 % of Patients* N = 54 80 Pre-entry 60 3 months 5 -14 days 40 20 0 Overall Heartburn Dysphagia * % of patients with moderate to severe symptoms Reprinted from Hassall et al, J Pediatr 2000; 137: 800 Irritability Coughing
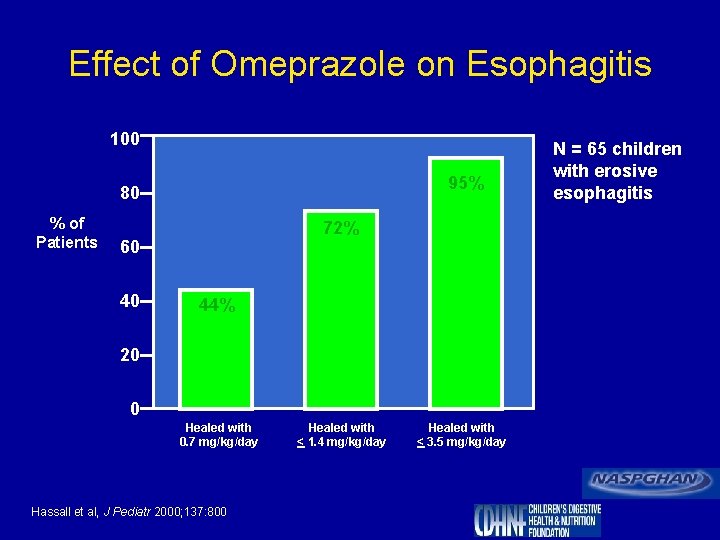
Effect of Omeprazole on Esophagitis 100 95% 80 % of Patients 72% 60 40 44% 20 0 Healed with 0. 7 mg/kg/day Hassall et al, J Pediatr 2000; 137: 800 Healed with < 1. 4 mg/kg/day Healed with < 3. 5 mg/kg/day N = 65 children with erosive esophagitis
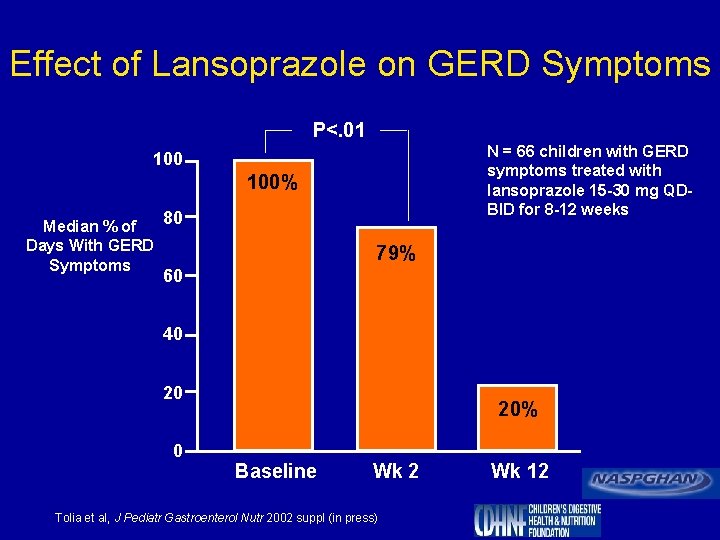
Effect of Lansoprazole on GERD Symptoms P<. 01 N = 66 children with GERD symptoms treated with lansoprazole 15 -30 mg QDBID for 8 -12 weeks 100% Median % of Days With GERD Symptoms 80 79% 60 40 20% Baseline Wk 2 Wk 12 Tolia et al, J Pediatr Gastroenterol Nutr 2002 suppl (in press)
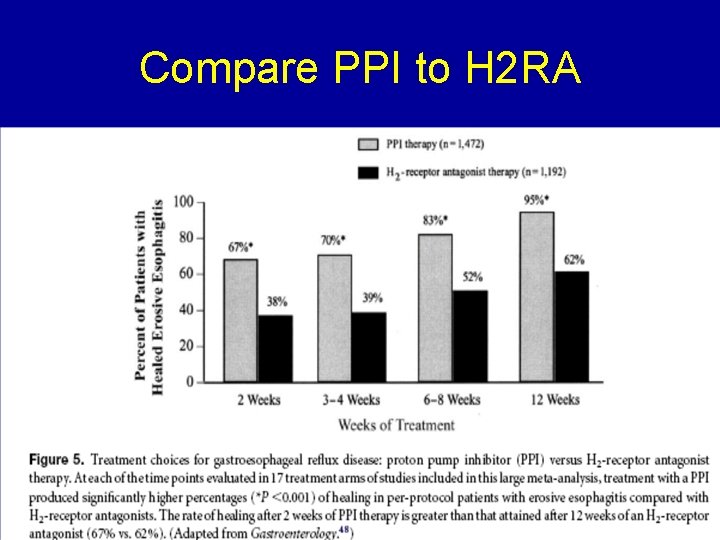
Compare PPI to H 2 RA
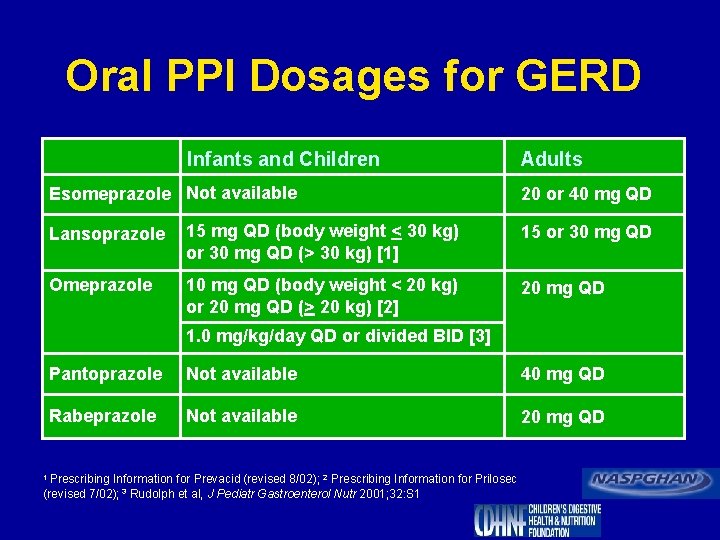
Oral PPI Dosages for GERD Infants and Children Esomeprazole Not available Adults 20 or 40 mg QD Lansoprazole 15 mg QD (body weight < 30 kg) or 30 mg QD (> 30 kg) [1] 15 or 30 mg QD Omeprazole 10 mg QD (body weight < 20 kg) or 20 mg QD (> 20 kg) [2] 20 mg QD 1. 0 mg/kg/day QD or divided BID [3] Pantoprazole Not available 40 mg QD Rabeprazole Not available 20 mg QD 1 Prescribing Information for Prevacid (revised 8/02); 2 Prescribing Information for Prilosec (revised 7/02); 3 Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1
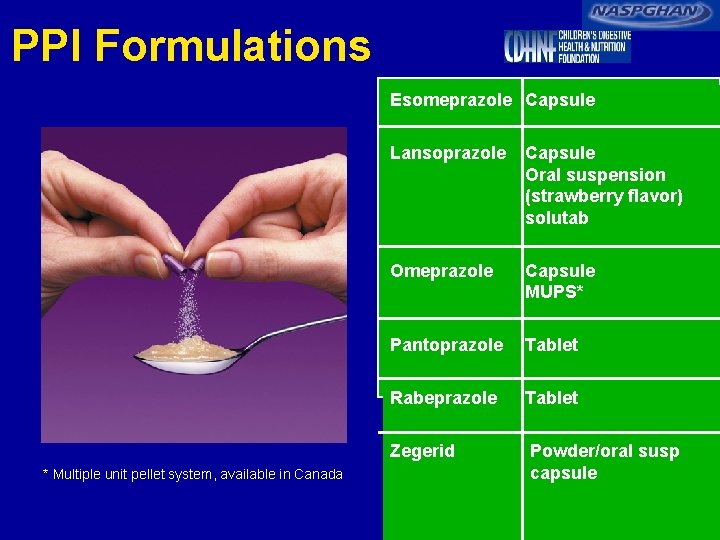
PPI Formulations Esomeprazole Capsule * Multiple unit pellet system, available in Canada Lansoprazole Capsule Oral suspension (strawberry flavor) solutab Omeprazole Capsule MUPS* Pantoprazole Tablet Rabeprazole Tablet Zegerid Powder/oral susp capsule
PPI Formulations
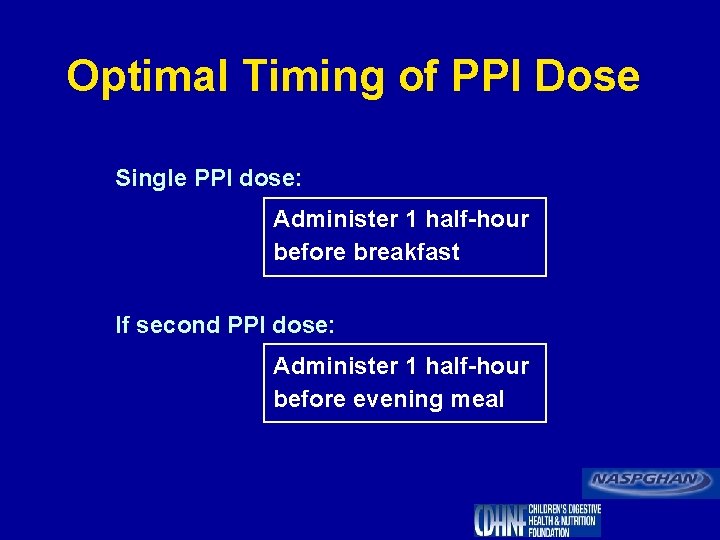
Optimal Timing of PPI Dose Single PPI dose: Administer 1 half-hour before breakfast If second PPI dose: Administer 1 half-hour before evening meal
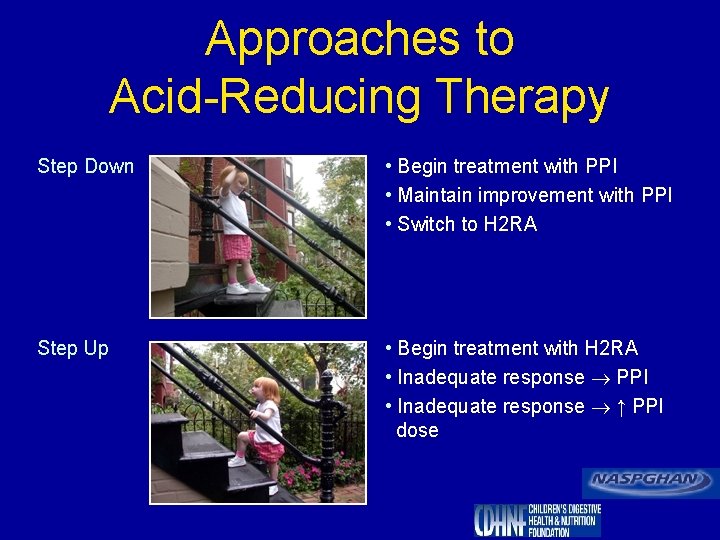
Approaches to Acid-Reducing Therapy Step Down • Begin treatment with PPI • Maintain improvement with PPI • Switch to H 2 RA Step Up • Begin treatment with H 2 RA • Inadequate response PPI • Inadequate response ↑ PPI dose
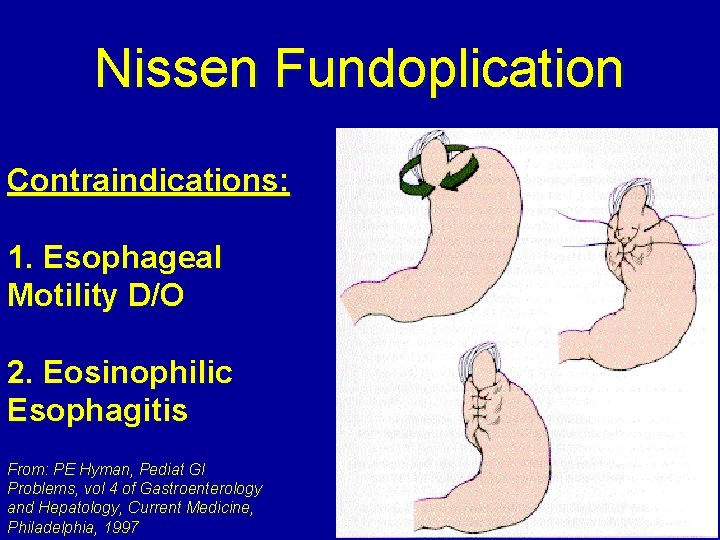
Nissen Fundoplication Contraindications: 1. Esophageal Motility D/O 2. Eosinophilic Esophagitis From: PE Hyman, Pediat GI Problems, vol 4 of Gastroenterology and Hepatology, Current Medicine, Philadelphia, 1997
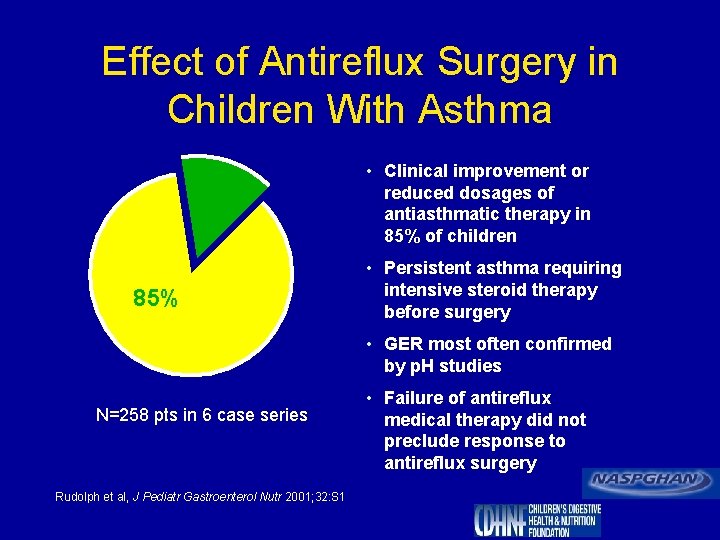
Effect of Antireflux Surgery in Children With Asthma • Clinical improvement or reduced dosages of antiasthmatic therapy in 85% of children 85% • Persistent asthma requiring intensive steroid therapy before surgery • GER most often confirmed by p. H studies N=258 pts in 6 case series Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1 • Failure of antireflux medical therapy did not preclude response to antireflux surgery
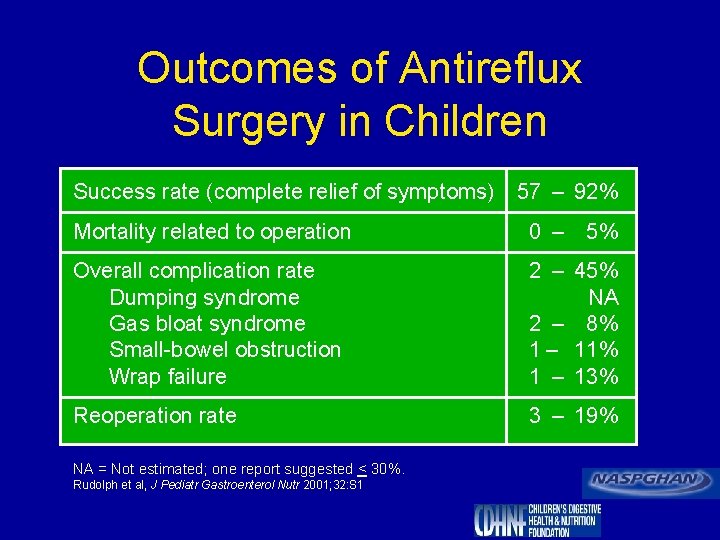
Outcomes of Antireflux Surgery in Children Success rate (complete relief of symptoms) 57 – 92% Mortality related to operation 0 – Overall complication rate Dumping syndrome Gas bloat syndrome Small-bowel obstruction Wrap failure 2 – 45% NA 2 – 8% 1 – 11% 1 – 13% Reoperation rate 3 – 19% NA = Not estimated; one report suggested < 30%. Rudolph et al, J Pediatr Gastroenterol Nutr 2001; 32: S 1 5%
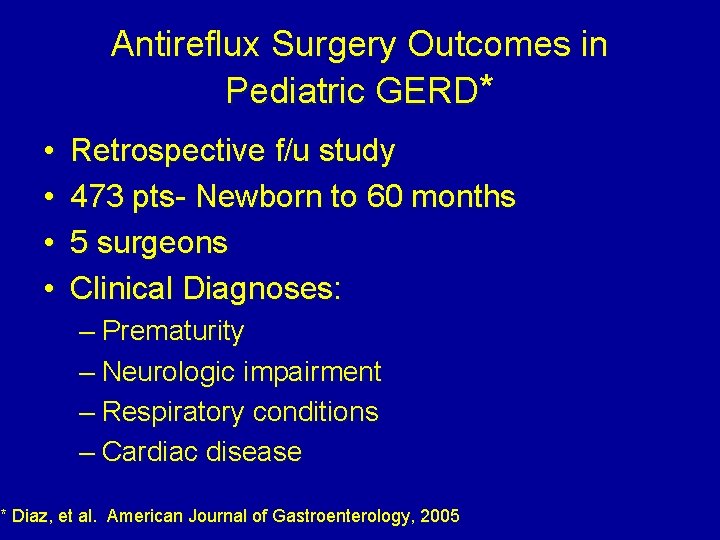
Antireflux Surgery Outcomes in Pediatric GERD* • • Retrospective f/u study 473 pts- Newborn to 60 months 5 surgeons Clinical Diagnoses: – Prematurity – Neurologic impairment – Respiratory conditions – Cardiac disease * Diaz, et al. American Journal of Gastroenterology, 2005
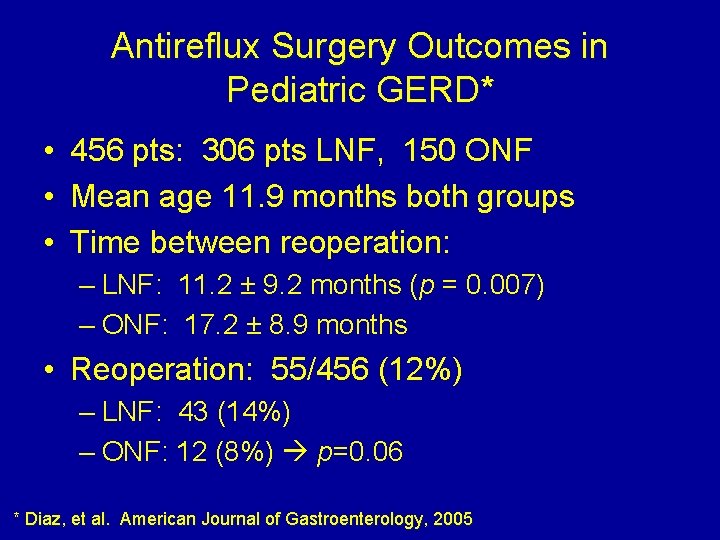
Antireflux Surgery Outcomes in Pediatric GERD* • 456 pts: 306 pts LNF, 150 ONF • Mean age 11. 9 months both groups • Time between reoperation: – LNF: 11. 2 ± 9. 2 months (p = 0. 007) – ONF: 17. 2 ± 8. 9 months • Reoperation: 55/456 (12%) – LNF: 43 (14%) – ONF: 12 (8%) p=0. 06 * Diaz, et al. American Journal of Gastroenterology, 2005
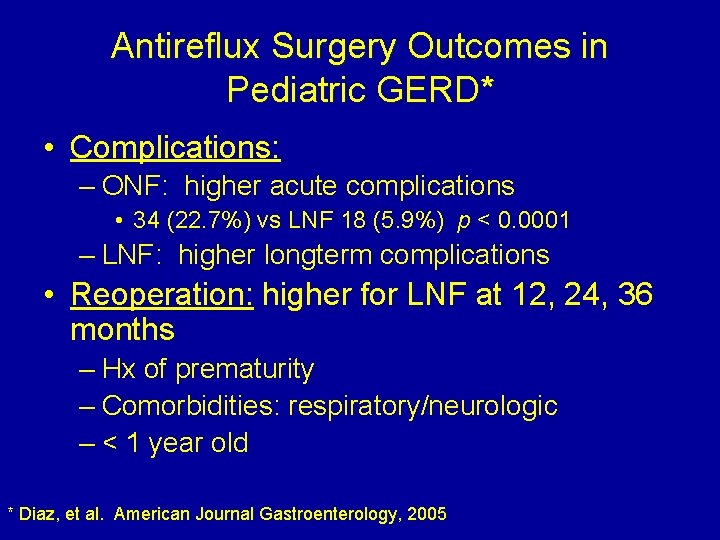
Antireflux Surgery Outcomes in Pediatric GERD* • Complications: – ONF: higher acute complications • 34 (22. 7%) vs LNF 18 (5. 9%) p < 0. 0001 – LNF: higher longterm complications • Reoperation: higher for LNF at 12, 24, 36 months – Hx of prematurity – Comorbidities: respiratory/neurologic – < 1 year old * Diaz, et al. American Journal Gastroenterology, 2005
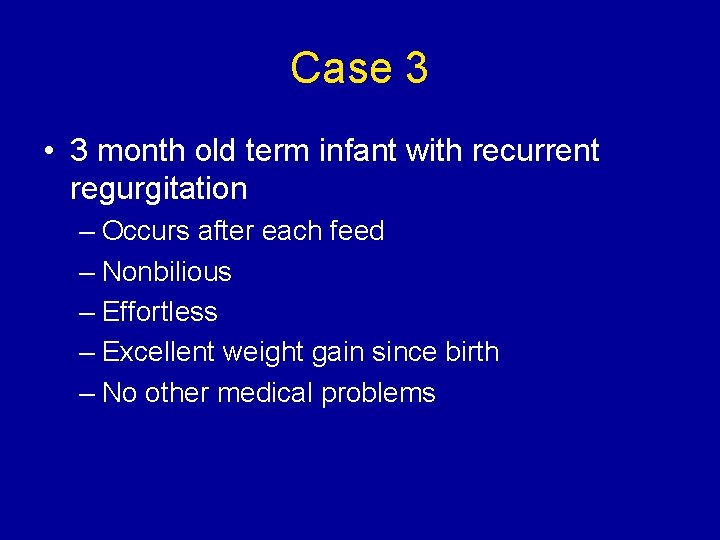
Case 3 • 3 month old term infant with recurrent regurgitation – Occurs after each feed – Nonbilious – Effortless – Excellent weight gain since birth – No other medical problems
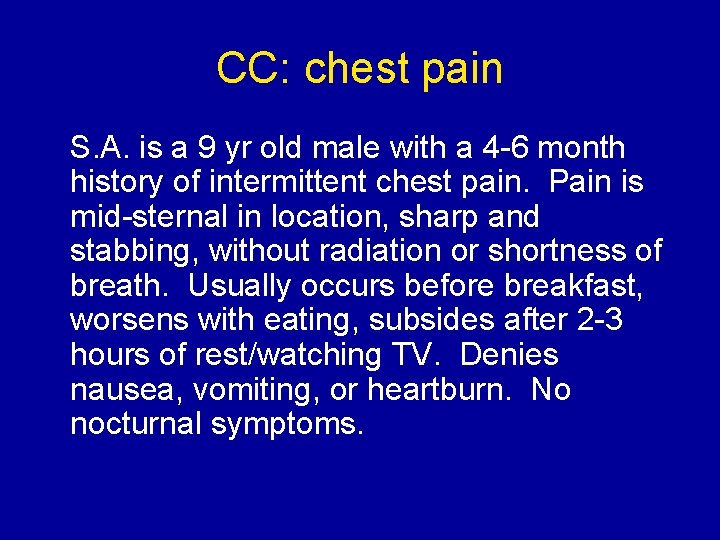
CC: chest pain S. A. is a 9 yr old male with a 4 -6 month history of intermittent chest pain. Pain is mid-sternal in location, sharp and stabbing, without radiation or shortness of breath. Usually occurs before breakfast, worsens with eating, subsides after 2 -3 hours of rest/watching TV. Denies nausea, vomiting, or heartburn. No nocturnal symptoms.
PMH and PE • PMH: history of isolated episode of “heart racing” at age 8; normal EKG, echocardiogram, Holter • Social history: adopted from Latvia at age 6; lives with adopted parents, sibling; well-adjusted • Prior evaluation: – Pulmonary function testing: normal – Barium swallow/UGI: ? thickened duodenal folds • PE: unremarkable, with normal growth, abdominal exam, and rectal exam, with hemoccult-negative stool
Laboratory studies • CBC: WBC=5. 7, Plts=291 K, Hgb/Hct=14. 0/40. 1 • ESR=5 • Chemistries: normal electrolytes, total protein and albumin, liver-associated enzymes, amylase and lipase • Helicobacter pylori Ig. G = 1. 78 (positive)
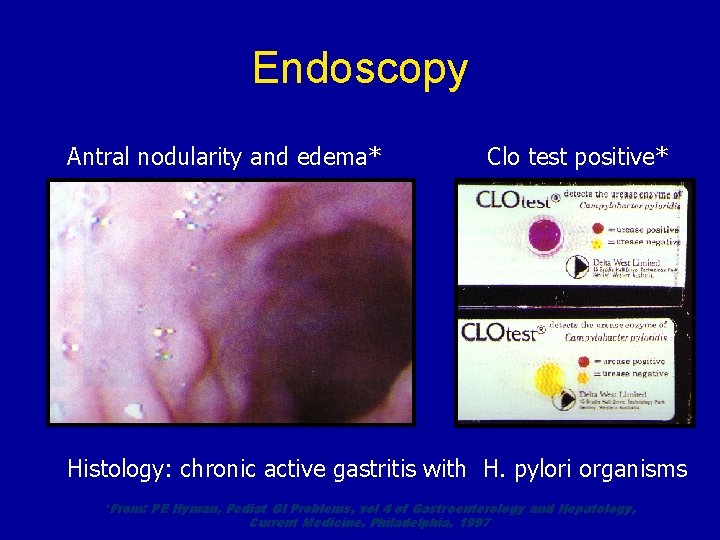
Endoscopy Antral nodularity and edema* Clo test positive* Histology: chronic active gastritis with H. pylori organisms *From: PE Hyman, Pediat GI Problems, vol 4 of Gastroenterology and Hepatology, Current Medicine, Philadelphia, 1997
Summary Points Ø GER is common in infants, but should “outgrow” it by 24 months of age Ø Eosinophilic esophagitis can mimic GERD in the infant/toddler, but presents as dysphagia in older children Ø Remember 3 facets of normal UGI
Summary Points ØTreatment with H 2 RA and PPI are both safe in children ØNo good motility agents ØPathologic reflux if the following occur: Øpast age 2 yrs, FTT, respiratory disease, dysphagia or odynophagia
- Slides: 49