Gastro for finals OSCE edition Abdo exam Intro
Gastro for finals OSCE edition
Abdo exam • Intro
Abdo exam • Intro • General inspection – patient & bedspace – Cachexia, icterus, pallor, discomfort, vomit bowels, catheter
Abdo exam • Intro • General inspection – patient & bedspace • Hands – Clubbing, erythema, Dupuytren’s contracture, leukonychia, koilonychia, xanthomata, flap
Abdo exam • • Intro General inspection – patient & bedspace Hands Head/neck – Conjunctival pallor, icteric sclera, xanthelasma, angular stomatitis, glossitis – Lymph nodes – Virchow’s
Abdo exam • • • Intro General inspection – patient & bedspace Hands Head/neck Close inspection – Chest: spider naevi, gynaecomastia, lack of axillary hair, acanthosis nigricans – Abdomen: distension, scars, striae, hernias, caput medusae, Cullen’s sign, Grey-Turner’s sign, stomas
Abdo exam • • • Intro General inspection – patient & bedspace Hands Head/neck Close inspection Palpation – Superficial & deep in 9 regions – Liver & spleen with respiration – Ballot kidneys – AAA
Abdo exam • • Intro General inspection – patient & bedspace Hands Head/neck Close inspection Palpation Percussion – Liver & spleen – Shifting dullness – bladder
Abdo exam • • Intro General inspection – patient & bedspace Hands Head/neck Close inspection Palpation Percussion Auscultation – Bowel sounds – Bruits
Abdo exam • • • Intro General inspection – patient & bedspace Hands Head/neck Close inspection Palpation Percussion Auscultation Complete exam – Peripheral oedema – Hernial orifices, PR, ext genitalia
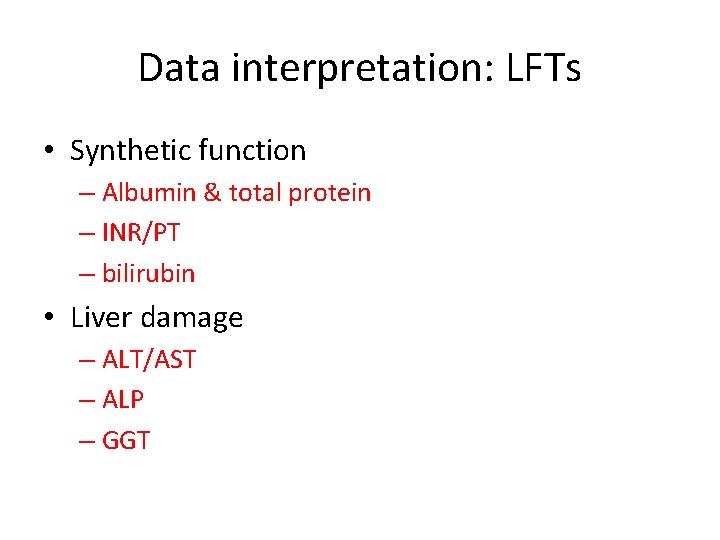
Data interpretation: LFTs • Synthetic function – Albumin & total protein – INR/PT – bilirubin • Liver damage – ALT/AST – ALP – GGT
Synthetic function • Albumin 35 -52 g/l – Accounts for >50% plasma proteins – Manufactured in liver from amino-acids – Helps regulate osmotic pressure – Low in diarrhoea, liver disease, malnutrition, infection
Synthetic function • Clotting factors – Prothrombin time specific to extrinsic pathway – If prolonged (in absence anticoagulants/vit k deficiency) can = liver damage • Bilirubin 0 -21 umol/l – Conjugated in the liver – Might not cause jaundice if <60 umol/l – Correlate with colour stools/urine
Hepatobiliary enzymes • ALT 0 -33 iu/l – Hepatocyte cytoplasm • AST – Hepatocyte cytoplasm, hepatocyte mitochondria, skeletal & cardiac muscle • ALT>AST : chronic liver disease • AST>ALT: cirrhosis & acute alcoholic hepatitis
Hepatobiliary enzymes • ALP 35 -104 iu/l – Canalicular surface of hepatocyte & bone, intestine, placenta • GGT 6 -42 iu/l – Canalicular surface of hepatocyte – Alcohol • Both raised: highly suggestive of cholestasis • Isolated raised ALP: suspect bone/other • ALT or ALP raised more? ? Hepatocellular vs cholestatic pattern
Isolated jaundice • Haemolysis – Blood film, reticulocytes, LDH, haptoglobins • Gilbert’s syndrome – Inability to conjugate bilirubin – Intermittent jaundice precipitated by stress/illness/exercise
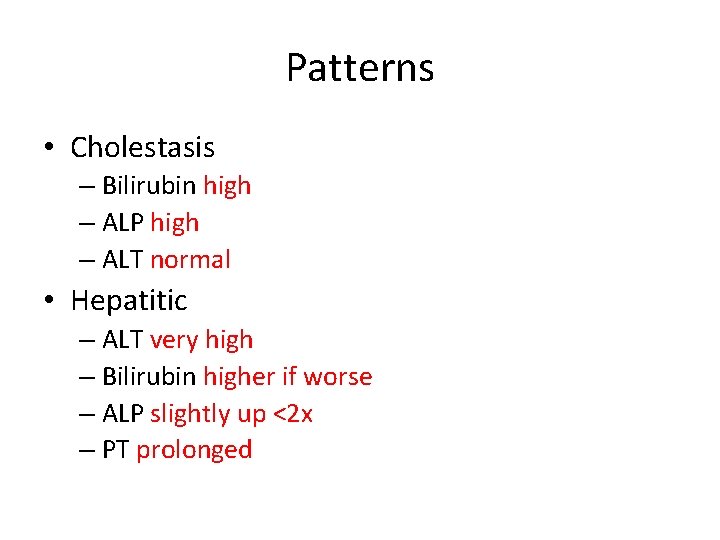
Patterns • Cholestasis – Bilirubin high – ALP high – ALT normal • Hepatitic – ALT very high – Bilirubin higher if worse – ALP slightly up <2 x – PT prolonged
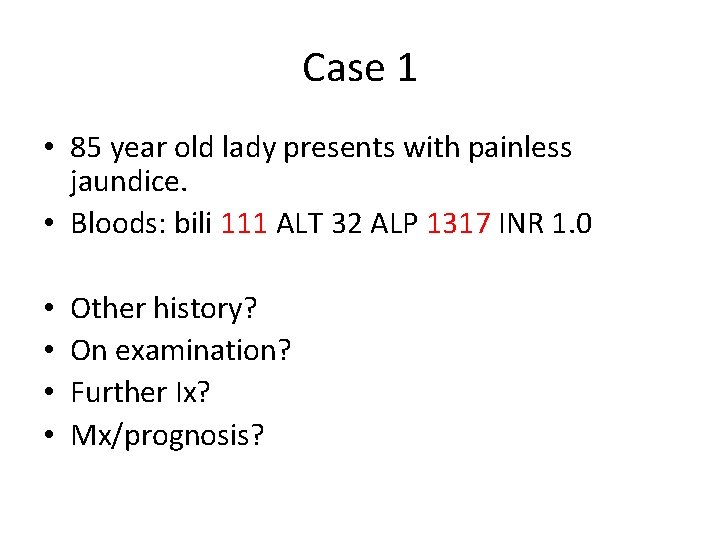
Case 1 • 85 year old lady presents with painless jaundice. • Bloods: bili 111 ALT 32 ALP 1317 INR 1. 0 • • Other history? On examination? Further Ix? Mx/prognosis?
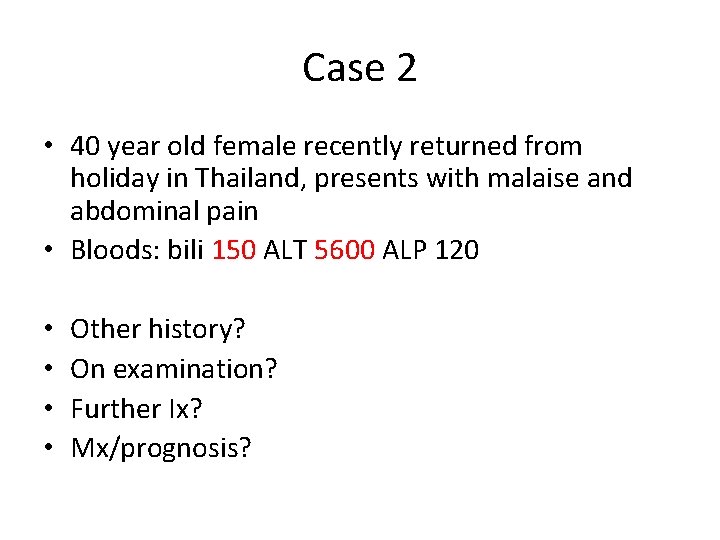
Case 2 • 40 year old female recently returned from holiday in Thailand, presents with malaise and abdominal pain • Bloods: bili 150 ALT 5600 ALP 120 • • Other history? On examination? Further Ix? Mx/prognosis?
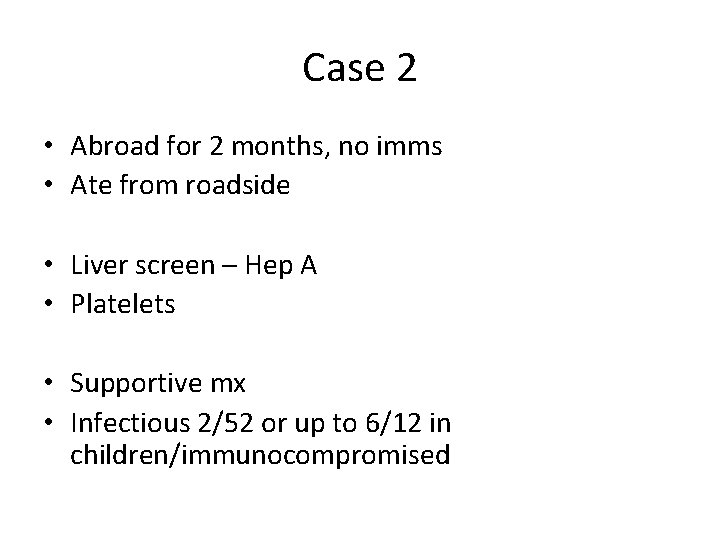
Case 2 • Abroad for 2 months, no imms • Ate from roadside • Liver screen – Hep A • Platelets • Supportive mx • Infectious 2/52 or up to 6/12 in children/immunocompromised
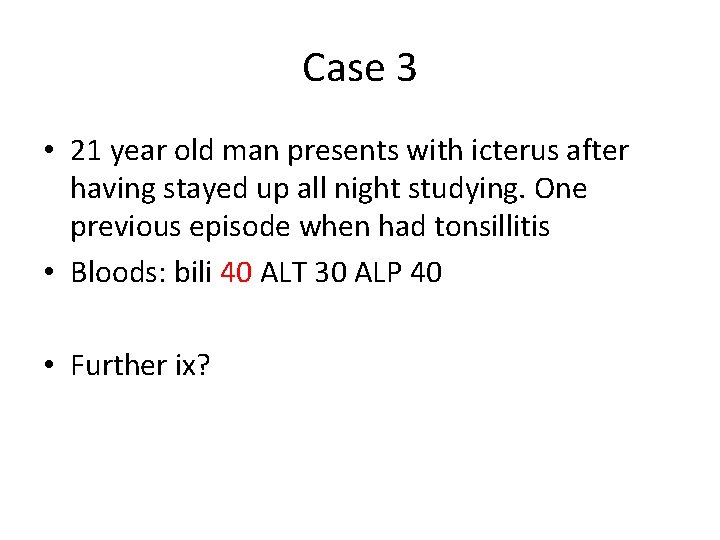
Case 3 • 21 year old man presents with icterus after having stayed up all night studying. One previous episode when had tonsillitis • Bloods: bili 40 ALT 30 ALP 40 • Further ix?
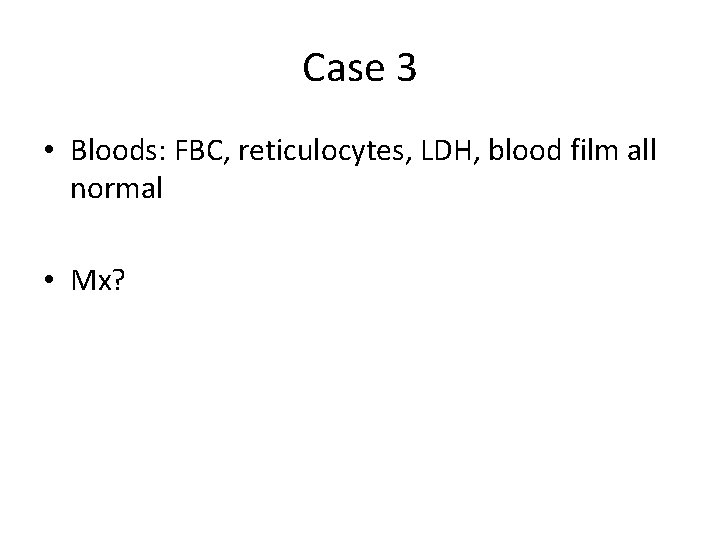
Case 3 • Bloods: FBC, reticulocytes, LDH, blood film all normal • Mx?
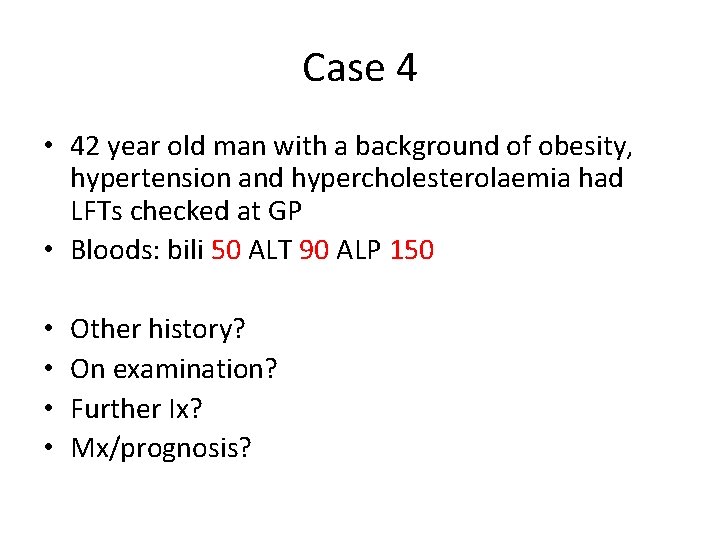
Case 4 • 42 year old man with a background of obesity, hypertension and hypercholesterolaemia had LFTs checked at GP • Bloods: bili 50 ALT 90 ALP 150 • • Other history? On examination? Further Ix? Mx/prognosis?
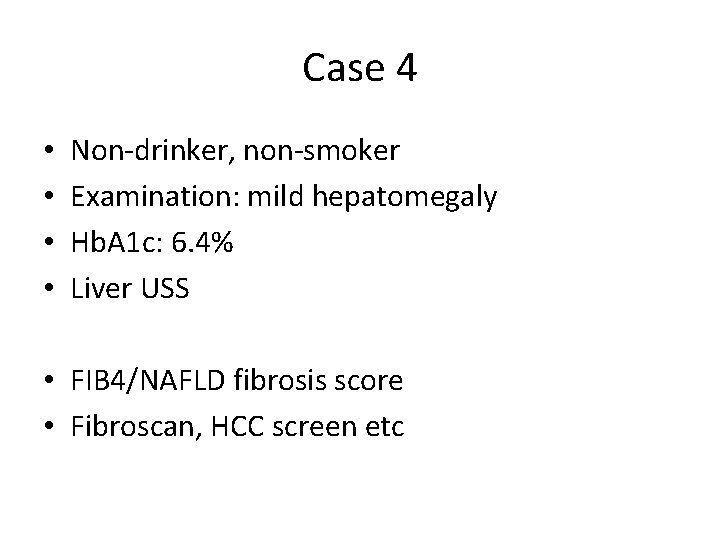
Case 4 • • Non-drinker, non-smoker Examination: mild hepatomegaly Hb. A 1 c: 6. 4% Liver USS • FIB 4/NAFLD fibrosis score • Fibroscan, HCC screen etc
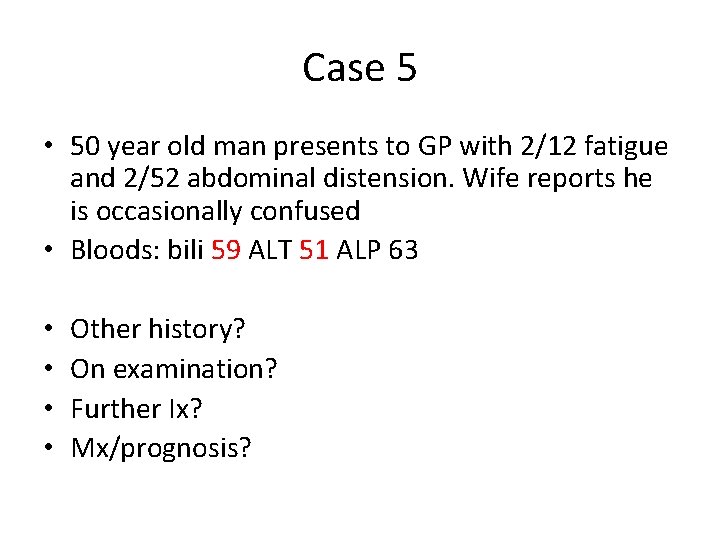
Case 5 • 50 year old man presents to GP with 2/12 fatigue and 2/52 abdominal distension. Wife reports he is occasionally confused • Bloods: bili 59 ALT 51 ALP 63 • • Other history? On examination? Further Ix? Mx/prognosis?
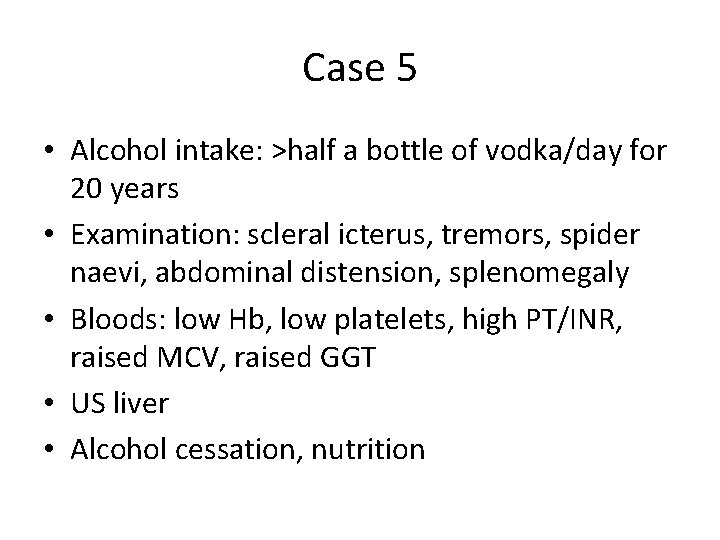
Case 5 • Alcohol intake: >half a bottle of vodka/day for 20 years • Examination: scleral icterus, tremors, spider naevi, abdominal distension, splenomegaly • Bloods: low Hb, low platelets, high PT/INR, raised MCV, raised GGT • US liver • Alcohol cessation, nutrition
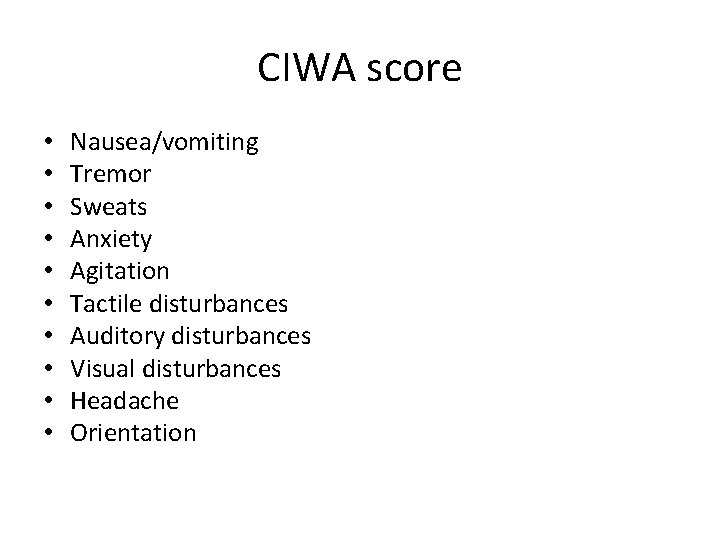
CIWA score • • • Nausea/vomiting Tremor Sweats Anxiety Agitation Tactile disturbances Auditory disturbances Visual disturbances Headache Orientation
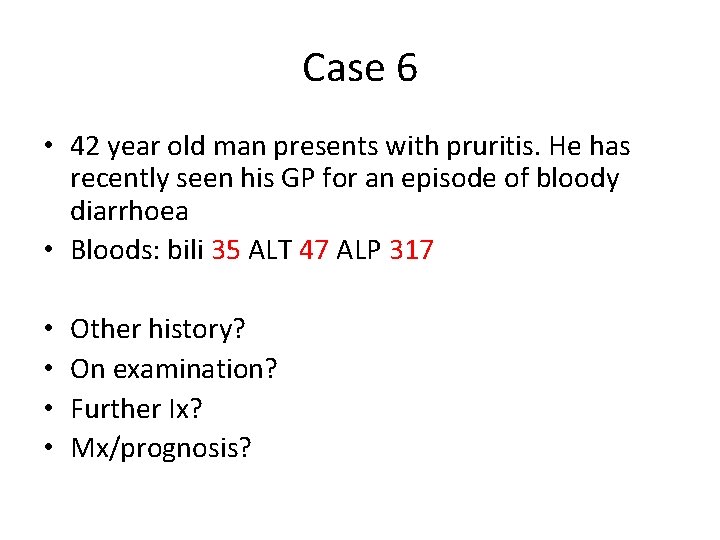
Case 6 • 42 year old man presents with pruritis. He has recently seen his GP for an episode of bloody diarrhoea • Bloods: bili 35 ALT 47 ALP 317 • • Other history? On examination? Further Ix? Mx/prognosis?
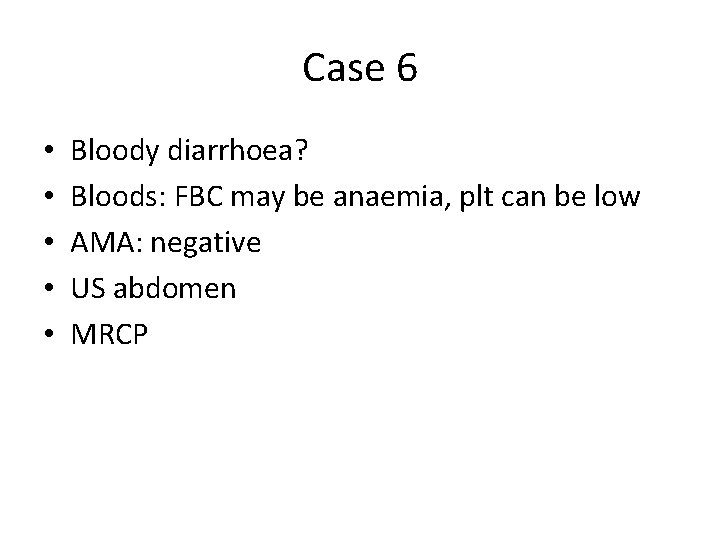
Case 6 • • • Bloody diarrhoea? Bloods: FBC may be anaemia, plt can be low AMA: negative US abdomen MRCP
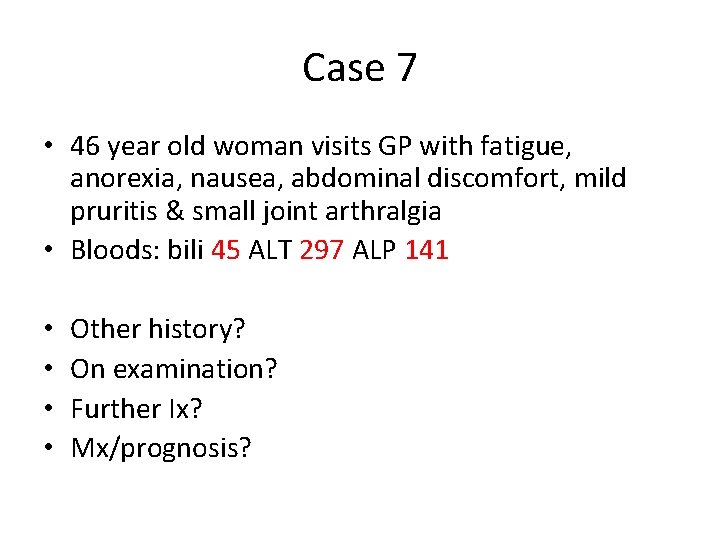
Case 7 • 46 year old woman visits GP with fatigue, anorexia, nausea, abdominal discomfort, mild pruritis & small joint arthralgia • Bloods: bili 45 ALT 297 ALP 141 • • Other history? On examination? Further Ix? Mx/prognosis?
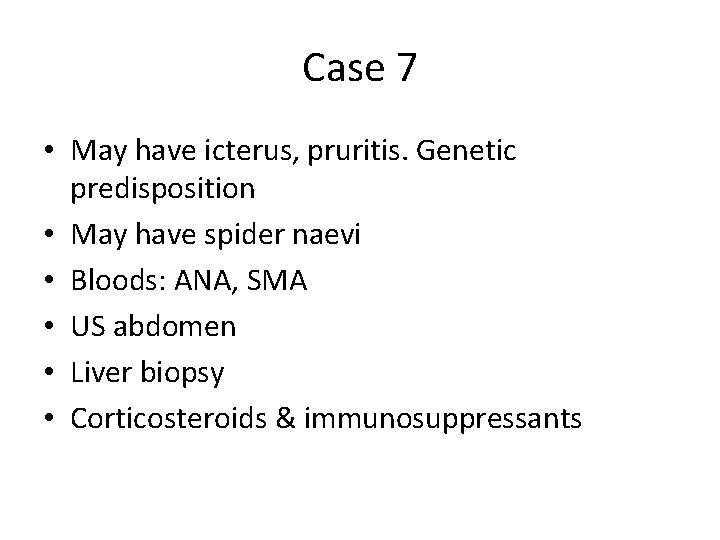
Case 7 • May have icterus, pruritis. Genetic predisposition • May have spider naevi • Bloods: ANA, SMA • US abdomen • Liver biopsy • Corticosteroids & immunosuppressants
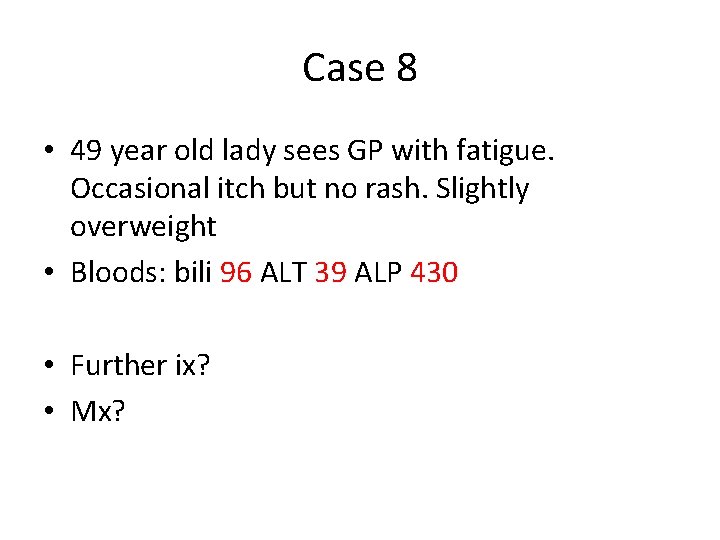
Case 8 • 49 year old lady sees GP with fatigue. Occasional itch but no rash. Slightly overweight • Bloods: bili 96 ALT 39 ALP 430 • Further ix? • Mx?
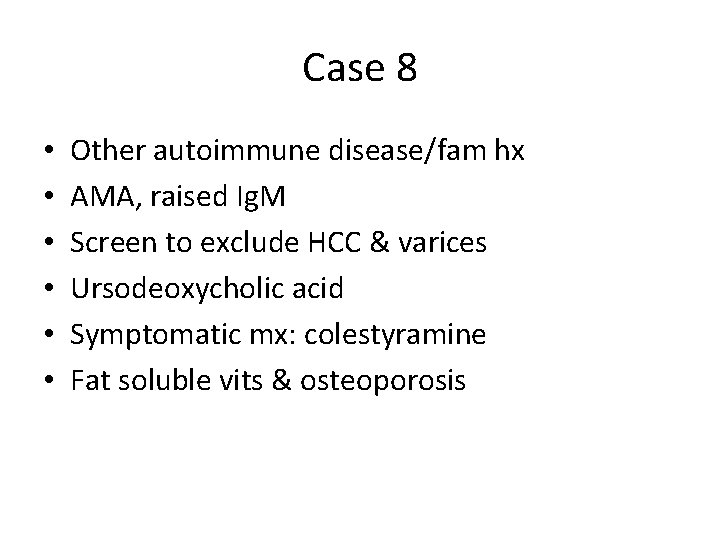
Case 8 • • • Other autoimmune disease/fam hx AMA, raised Ig. M Screen to exclude HCC & varices Ursodeoxycholic acid Symptomatic mx: colestyramine Fat soluble vits & osteoporosis
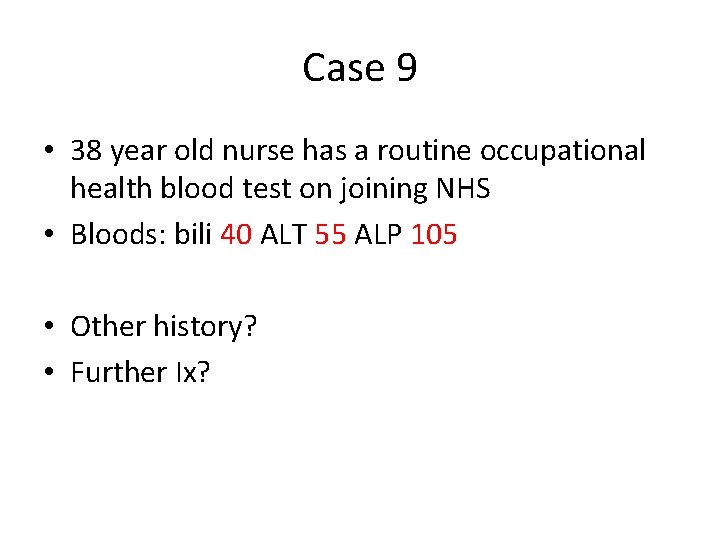
Case 9 • 38 year old nurse has a routine occupational health blood test on joining NHS • Bloods: bili 40 ALT 55 ALP 105 • Other history? • Further Ix?
Case 9 • Trained abroad, ? immunised • Has had a needlestick injury 5 months ago
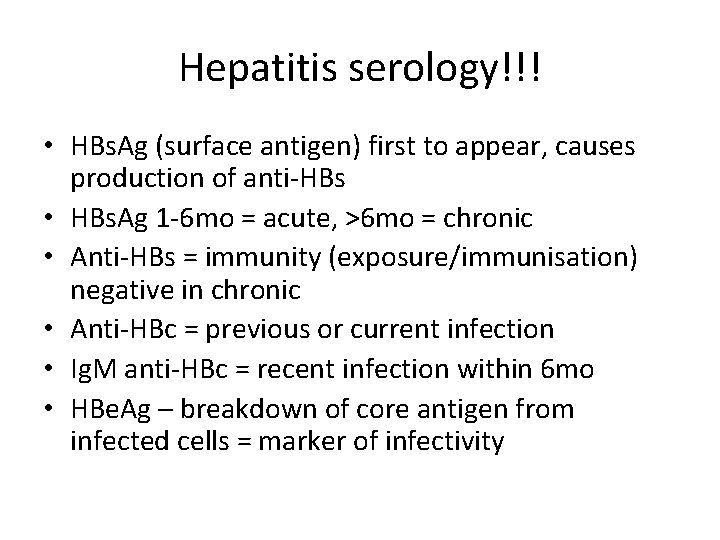
Hepatitis serology!!! • HBs. Ag (surface antigen) first to appear, causes production of anti-HBs • HBs. Ag 1 -6 mo = acute, >6 mo = chronic • Anti-HBs = immunity (exposure/immunisation) negative in chronic • Anti-HBc = previous or current infection • Ig. M anti-HBc = recent infection within 6 mo • HBe. Ag – breakdown of core antigen from infected cells = marker of infectivity
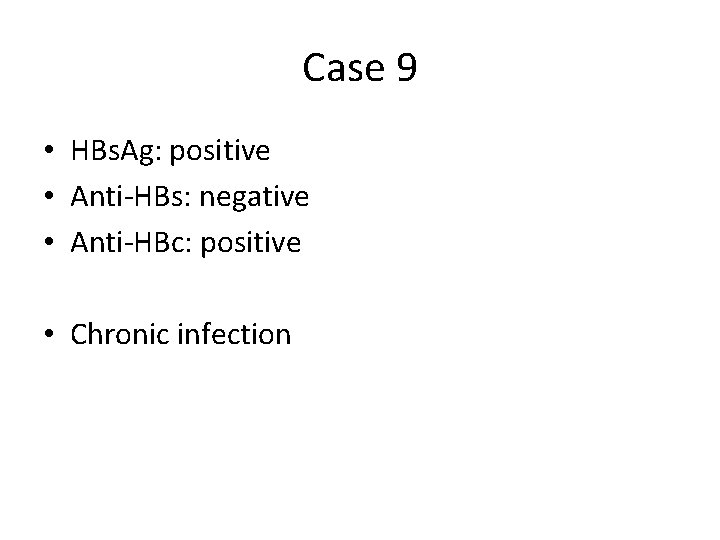
Case 9 • HBs. Ag: positive • Anti-HBs: negative • Anti-HBc: positive • Chronic infection
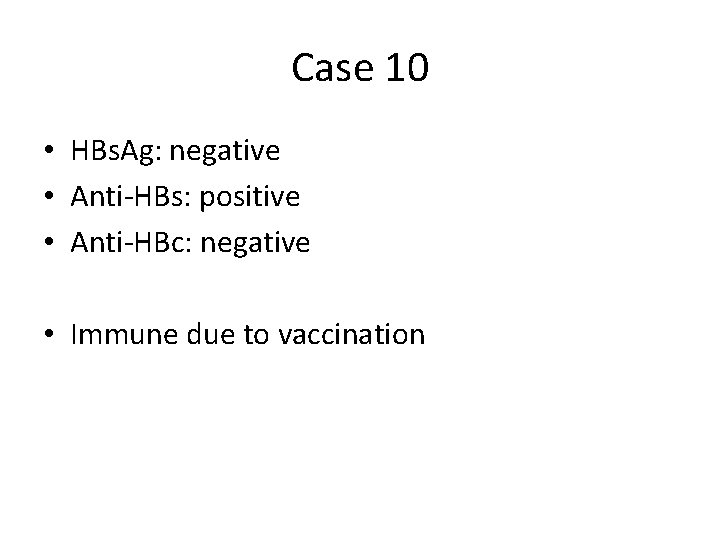
Case 10 • HBs. Ag: negative • Anti-HBs: positive • Anti-HBc: negative • Immune due to vaccination
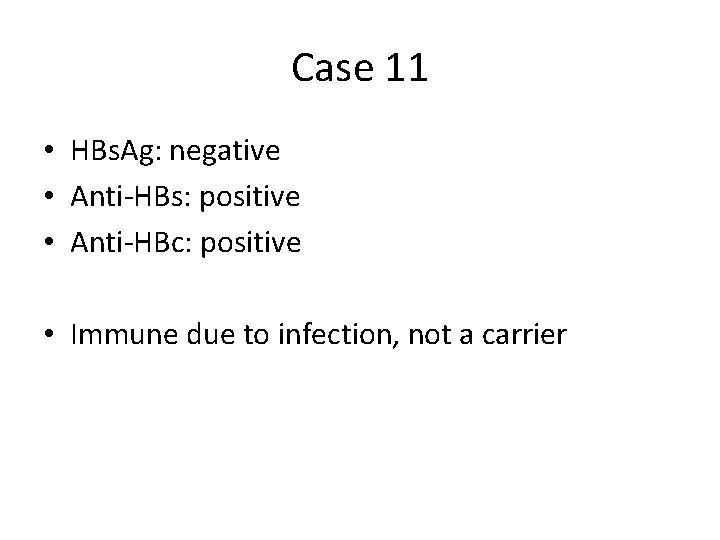
Case 11 • HBs. Ag: negative • Anti-HBs: positive • Anti-HBc: positive • Immune due to infection, not a carrier
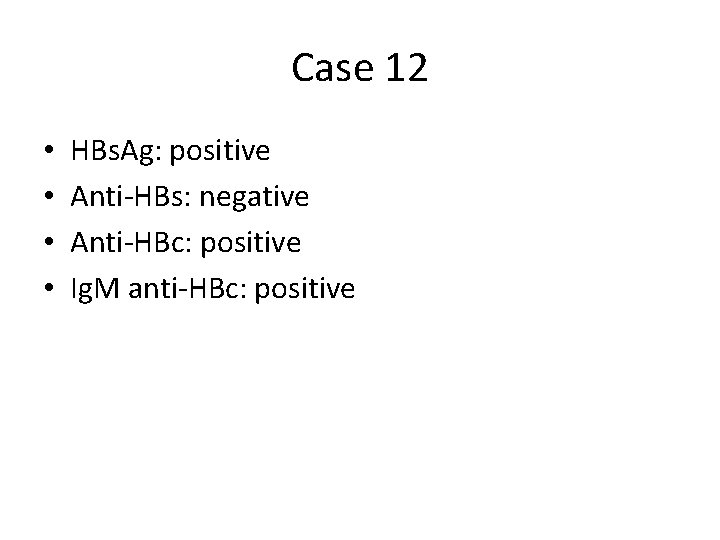
Case 12 • • HBs. Ag: positive Anti-HBs: negative Anti-HBc: positive Ig. M anti-HBc: positive
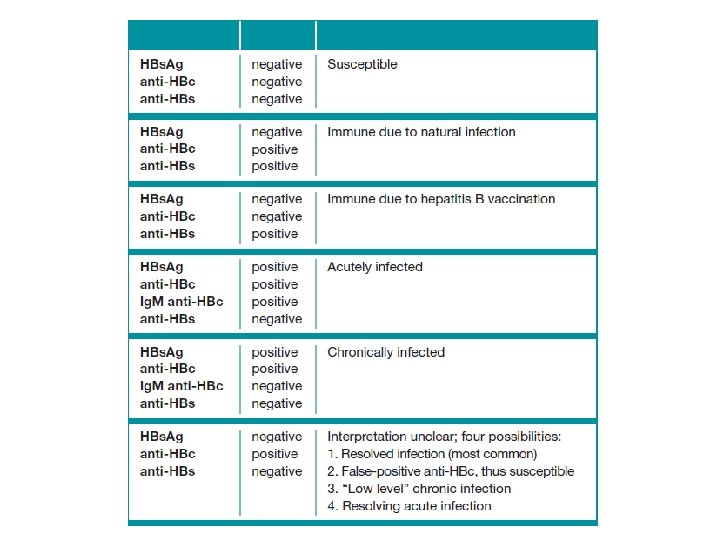
Case 13 • 63 year old man presents with abdominal distension worsening over several months & dark stools. PSHx abdominal surgery requiring blood transfusion in 80 s • Bloods: bili 30 ALT 79 ALP 80
Case 13 • Occasional alcohol use • Spider naevi, gynaecomastia, caput medsuae, ascites • Positive HCV antibodies • Antivirals • Assessment fibrosis & HCC screening
- Slides: 43