GASTRIC SECRETIONS 1 Dr Somia Iqbal STOMACH FUNDUS
GASTRIC SECRETIONS 1 Dr. Somia Iqbal
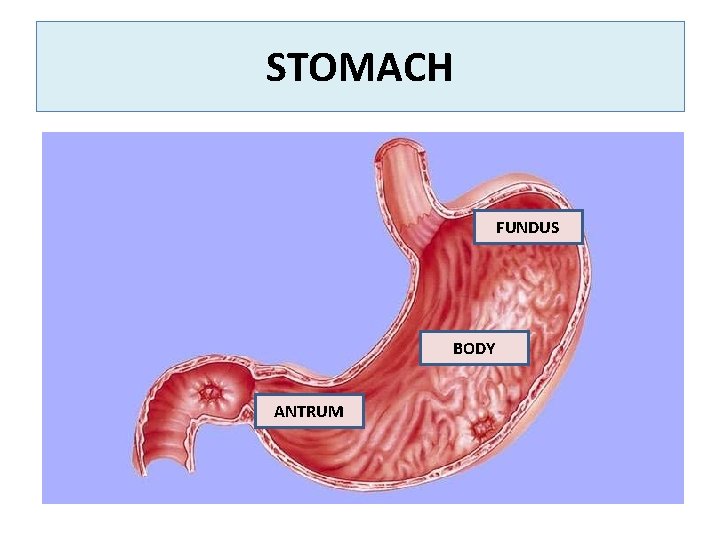
STOMACH FUNDUS BODY ANTRUM
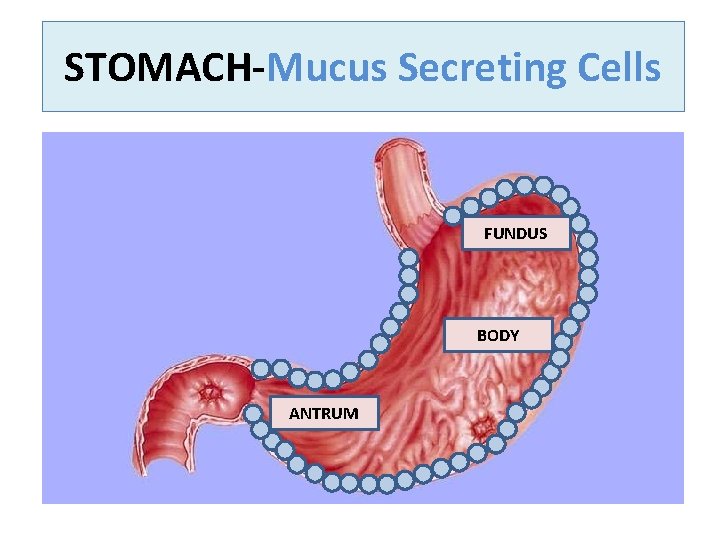
STOMACH Mucus Secreting Cells FUNDUS BODY ANTRUM
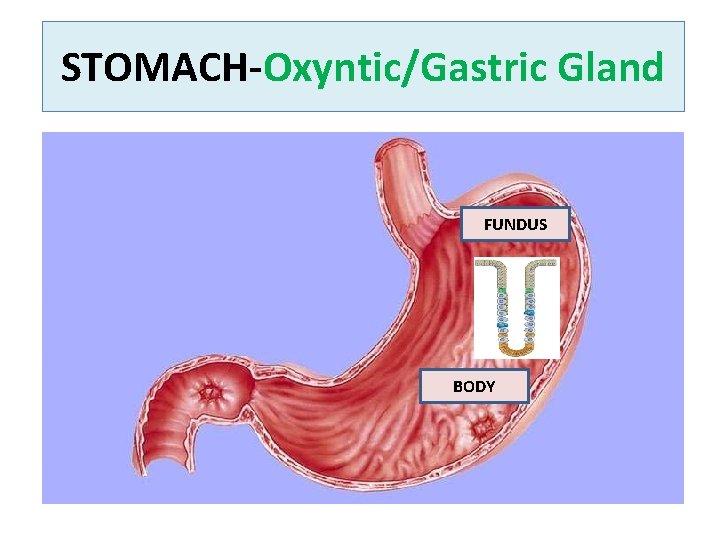
STOMACH Oxyntic/Gastric Gland FUNDUS BODY
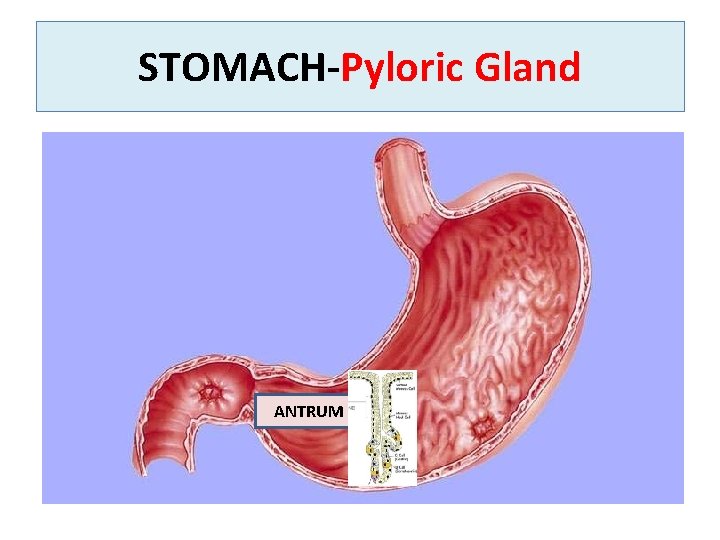
STOMACH Pyloric Gland ANTRUM

• • • MUCOUS SECRETING CELLS OXYNTIC/GASTRIC GLAND Line the entire surface of stomach PYLORIC GLAND In mucosa of antral portion of stomach In mucosa of fundus and body of stomach
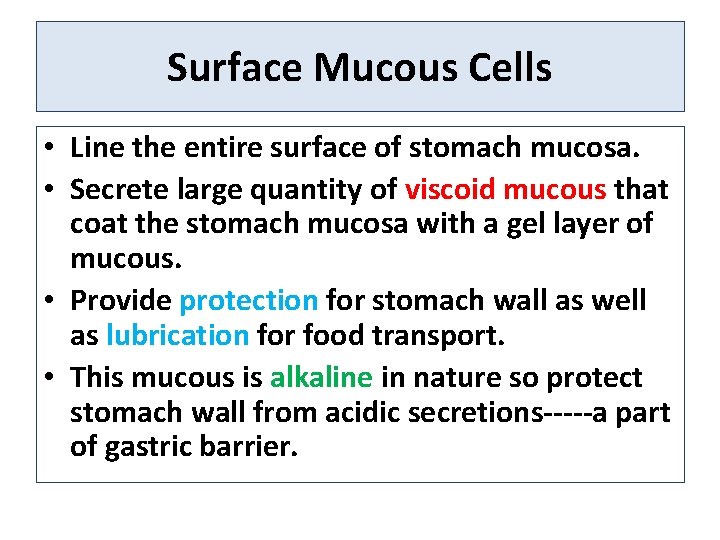
Surface Mucous Cells • Line the entire surface of stomach mucosa. • Secrete large quantity of viscoid mucous that coat the stomach mucosa with a gel layer of mucous. • Provide protection for stomach wall as well as lubrication for food transport. • This mucous is alkaline in nature so protect stomach wall from acidic secretions a part of gastric barrier.
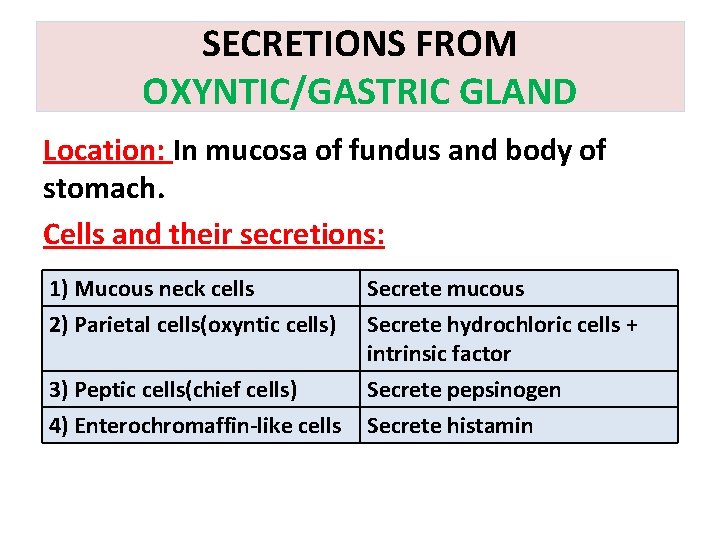
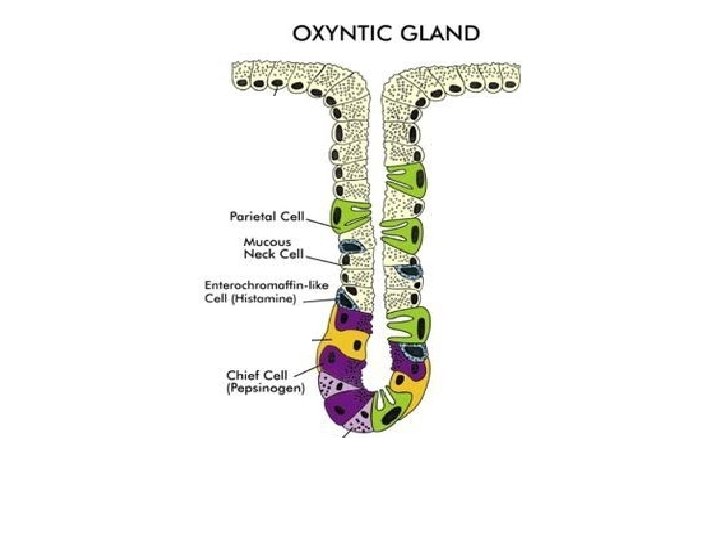
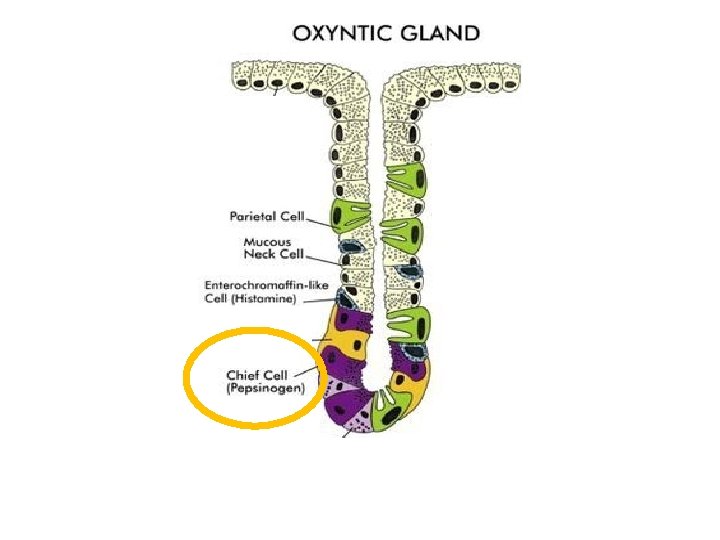
SECRETIONS FROM OXYNTIC/GASTRIC GLAND Location: In mucosa of fundus and body of stomach. Cells and their secretions: 1) Mucous neck cells 2) Parietal cells(oxyntic cells) Secrete mucous Secrete hydrochloric cells + intrinsic factor 3) Peptic cells(chief cells) 4) Enterochromaffin like cells Secrete pepsinogen Secrete histamin

PARIETAL CELLS
HCL
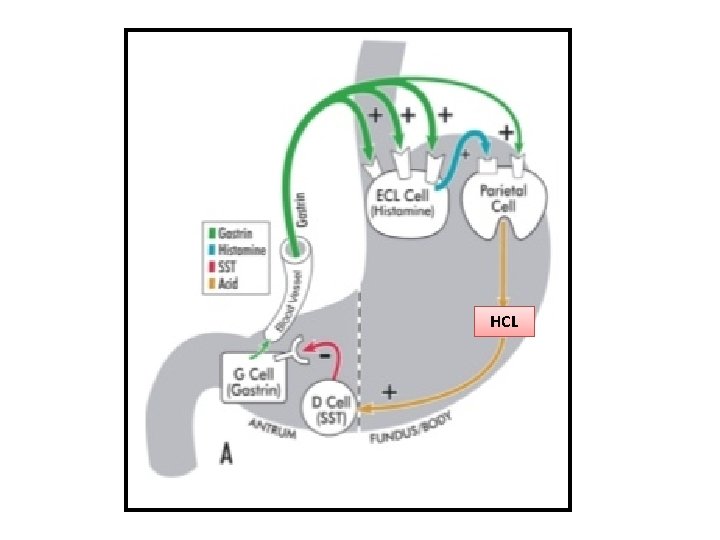
SECRETION OF HYDROCHLORIC ACID STIMULI FOR SECRETION: 1. Parasympathetic stimulation→ release of Acetylcholine 2. Gastrin 3. Histamine
HCL
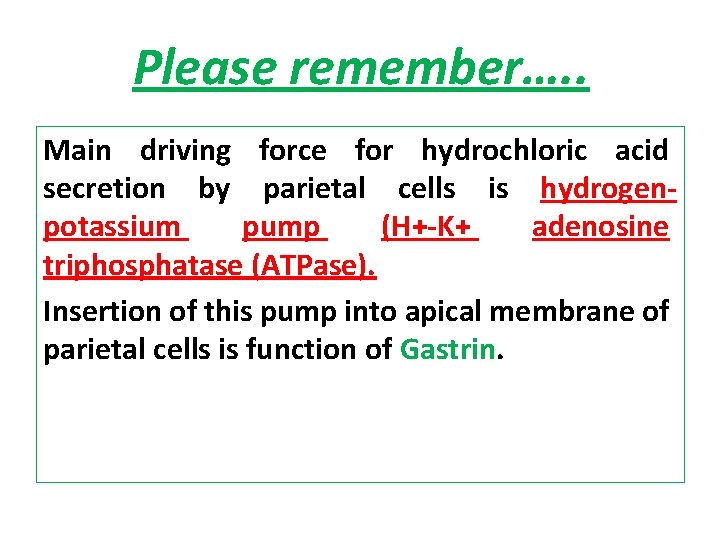
Please remember…. . Main driving force for hydrochloric acid secretion by parietal cells is hydrogen potassium pump (H+ K+ adenosine triphosphatase (ATPase). Insertion of this pump into apical membrane of parietal cells is function of Gastrin.

MECHANISM OF HCL SECRETION
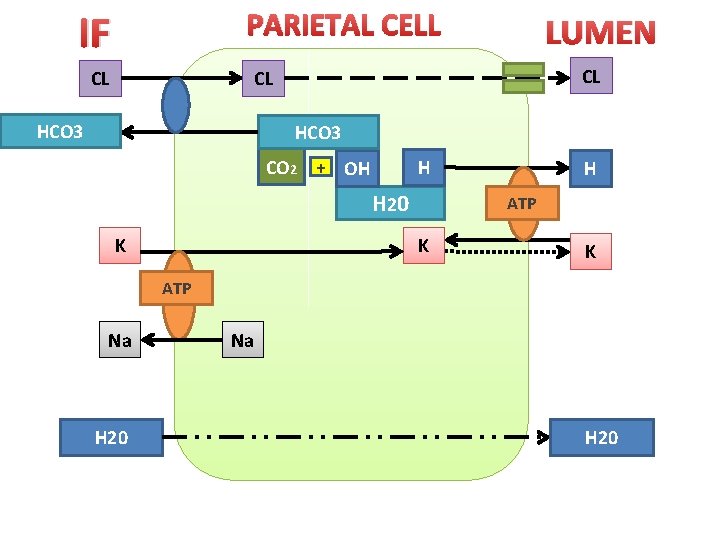
PARIETAL CELL IF CL LUMEN CL CL HCO 3 CO 2 + OH H H 20 K H ATP K K ATP Na H 20
1: Water dissociate into OH and H ion, in the cytoplasm of parietal cell. 2: Hydrogen is actively secreted into the canaliculi in exchange of k (this process is catalyzed by H K atpase. 3: k normally enter into cell by NA K atpase pump present on basolateral (extracellular side of member) which then leak into lumen but then recycled back. 4: OH combine with C 02 and form carbonic acid in the presence of carbonic anhydrase enzyme and transported into extracellular fluid in exchange of chloride ion. 5: This chloride ion leak into lumen of canaliculi by leak cannels. 6: Water pass into canaliculi from ECF by process of osmosis as canaliculi has more ions.
FINAL SECRETION FROM CANALICULI Final secretion from canaliculi contain: • Water, • Hydrochloric acid (160 mmol/L), • Potassium chloride and • Small amount of sodium chloride. PH 0. 8

INTRINSIC FACTOR
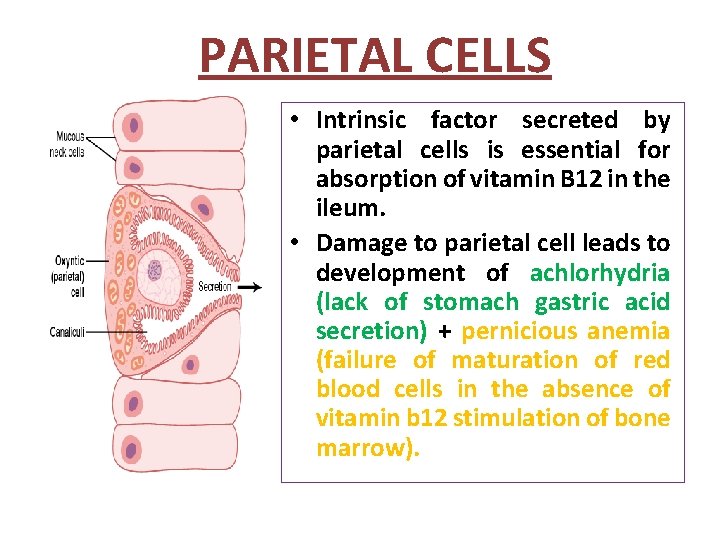
PARIETAL CELLS • Intrinsic factor secreted by parietal cells is essential for absorption of vitamin B 12 in the ileum. • Damage to parietal cell leads to development of achlorhydria (lack of stomach gastric acid secretion) + pernicious anemia (failure of maturation of red blood cells in the absence of vitamin b 12 stimulation of bone marrow).
PEPSINOGEN
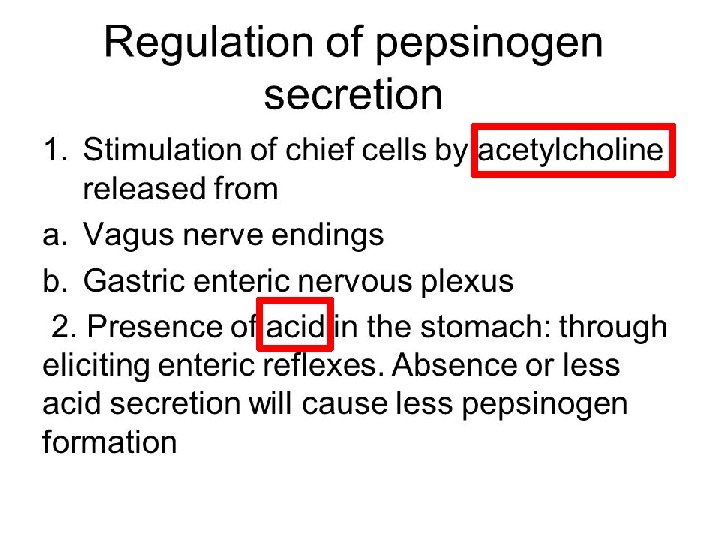
PEPSINOGEN • Secreted by mucous and chief (peptic) cells of oxyntic (gastric) gland. • When secreted has no digestive activity. • When come in contact with hydrochloric acid, it is activated and form active pepsin. • Pepsin functions as proteolytic enzyme in a highly acidic medium (PH 1. 8 to 3. 5) but above the p. H of 5, it has no proteolytic activity and become inactivate. • Required for protein digestion.
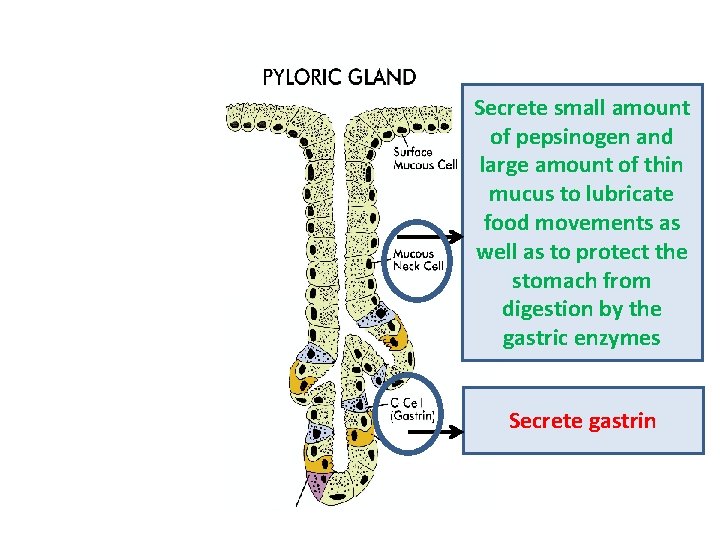
Secrete small amount of pepsinogen and large amount of thin mucus to lubricate food movements as well as to protect the stomach from digestion by the gastric enzymes Secrete gastrin
PHASES OF GASTRIC SECRETIONS Gastric secretions occur in three stages: 1. A cephalic phase 2. A gastric phase 3. An intestinal phase 4. Inter digestive phase
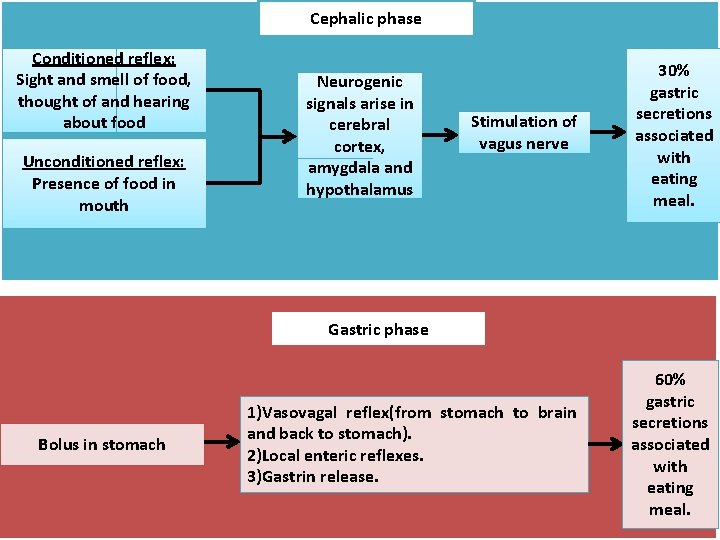
Cephalic phase Conditioned reflex: Sight and smell of food, thought of and hearing about food Unconditioned reflex: Presence of food in mouth Stimulation of vagus nerve 30% gastric secretions associated with eating meal. 1)Vasovagal reflex(from stomach to brain and back to stomach). 2)Local enteric reflexes. 3)Gastrin release. 60% gastric secretions associated with eating meal. Neurogenic signals arise in cerebral cortex, amygdala and hypothalamus Gastric phase Bolus in stomach
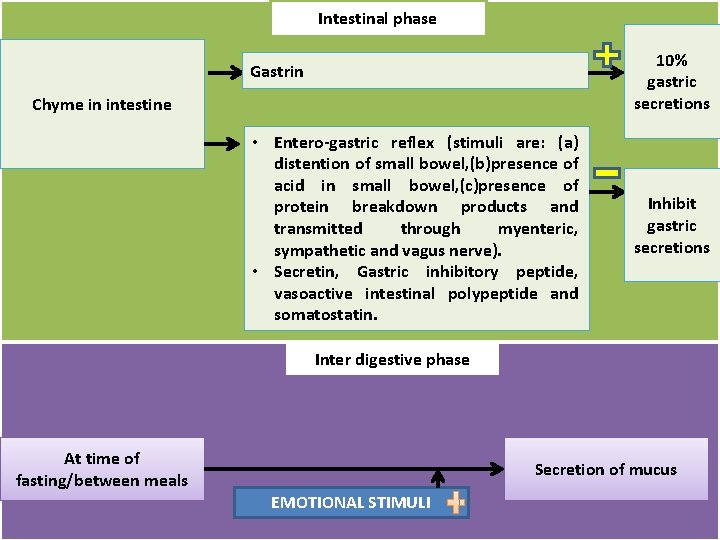
Intestinal phase 10% gastric secretions Gastrin Chyme in intestine • Entero gastric reflex (stimuli are: (a) distention of small bowel, (b)presence of acid in small bowel, (c)presence of protein breakdown products and transmitted through myenteric, sympathetic and vagus nerve). • Secretin, Gastric inhibitory peptide, vasoactive intestinal polypeptide and somatostatin. Inhibit gastric secretions Inter digestive phase At time of fasting/between meals Secretion of mucus EMOTIONAL STIMULI
GASTRITIS • Gastritis is an inflammation of the protective lining of the stomach. • Inflammation can be 1. Superficial (not very harmful) or 2. Deep (can lead to atrophy of gastric mucosa, in many long term cases).
What causes gastritis? /pathophysiology Damage to stomach lining (gastric barrier) allows digestive juices to damage and inflame it , causing gastritis. Gastric mucosa has two main features: (1)it is lined with highly resistant mucous cells that secrete viscid and adherent mucus and (2) it has tight junctions between the adjacent epithelial cells. Together they form gastric barrier.
• In gastritis, the permeability of the barrier is greatly increased. • The hydrogen ions do then diffuse into the stomach epithelium, creating a vicious circle of progressive stomach mucosal damage and atrophy. • It also makes the mucosa susceptible to digestion by the peptic digestive enzymes, thus frequently resulting in a gastric ulcer.
Cause And Risk Factors The most common cause is helicobacter pylori. It’s a bacterium that infects the lining of the stomach. Other risk factors include: 1. NSAIDs 2. Tobacco, 3. Increase age, 4. Stress 5. Autoimmune disorders
Complications • Chronic gastritis can lead to gastric atrophy and loss of stomach secretions. • Achlorhydria (means simply that the stomach fails to secrete hydrochloric acid). • When acid is not secreted, pepsin also usually is not secreted. • Gastric atrophy may cause pernicious anemia(no intrinsic factor no vitamin B 12 absorption RBCs fail to mature)
PEPTIC ULCER A peptic ulcer is an excoriated area of stomach or intestinal mucosa caused by the digestive action of gastric juice or upper small intestinal secretions.
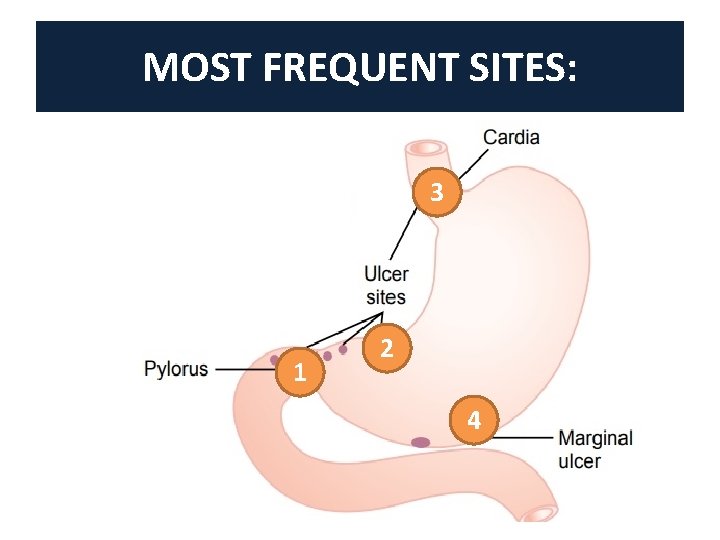
MOST FREQUENT SITES: 3 1 2 4
PATHOPHYSIOLOGY Main basic cause is imbalance between; • The rate of secretion of gastric juice and • The degree of protection afforded by (1) the gastroduodenal mucosal barrier and (2) the neutralization of the gastric acid by duodenal juices.
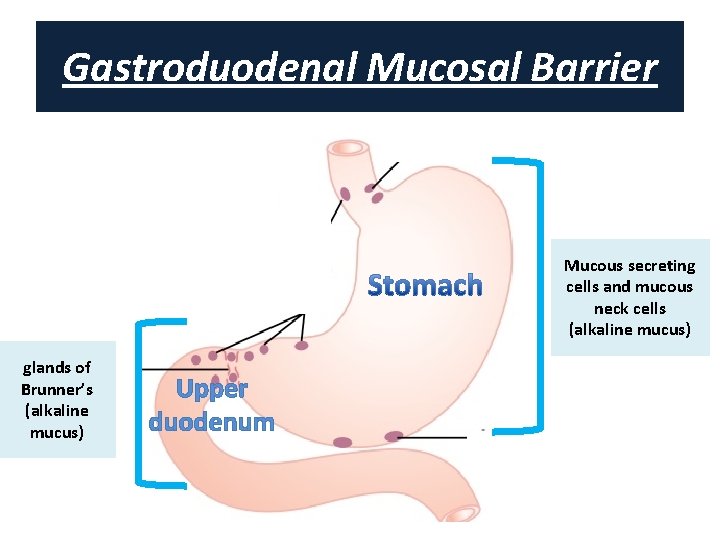
Gastroduodenal Mucosal Barrier Mucous secreting cells and mucous neck cells (alkaline mucus) glands of Brunner’s (alkaline mucus) Upper duodenum
Neutralization Of The Gastric Acid By Duodenal Juices 1. Bicarbonate ions secretions from the pancreas, Brunner’s glands of duodenum and gall bladder(bile)→neutralize the hydrochloric acid of the gastric juice, thus also inactivating pepsin and preventing digestion of the mucosa. 2. When excess acid enters the duodenum, it inhibits gastric secretion both by nervous reflexes and by hormonal feedback system, further ensure neutralization.
: : : Therefore, a peptic ulcer can be caused in either of two ways: (1) excess secretion of acid and pepsin by the gastric mucosa or (2) diminished ability of the gastroduodenal mucosal barrier to protect against the digestive properties of the stomach acid–pepsin secretion.
Main Cause Of Peptic Ulcer • Helicobacter pylori (75% of cases). • The bacteria penetrate the mucosal barrier by its physical capability to burrow through the barrier and by releasing ammonium that liquefies the barrier and stimulates the secretion of hydrochloric acid. • As a result, the strong acidic juices of the stomach penetrate into the underlying epithelium and literally digest the gastrointestinal wall, thus leading to peptic ulceration.
Other Causes Of Peptic Ulcer • Smoking, presumably because of increased nervous stimulation of the stomach secretory glands; • Alcohol, because it tends to break down the mucosal barrier; and • Aspirin and other nonsteroidal anti inflammatory drugs that also have a strong propensity for breaking down this barrier.
Treatment Of Peptic Ulcers 1. Use of antibiotics along with other agents to kill infectious bacteria and 2. Administration of an acid suppressant drug, especially ranitidine, an antihistaminic that blocks the stimulatory effect of histamine on gastric gland histamine 2 receptors, thus reducing gastric acid secretion by 70 to 80 percent.
- Slides: 42