Gastric outlet obstruction secondary to duodenal stricture due
Gastric outlet obstruction secondary to duodenal stricture due to unusual cause By Dr SL Chung, Dr Shamas Zaman Stoke Mandeville Hospital, Aylesbury
Clinical Presentation • 58 year old gentleman, presented with fever and sweats. Required hospital admission for intermittent epigastric pain/discomfort, vomiting and nausea. He reported weight loss of approximately 20 kg in 2 -3 months. • Symptoms started shortly after travel to Pakistan.
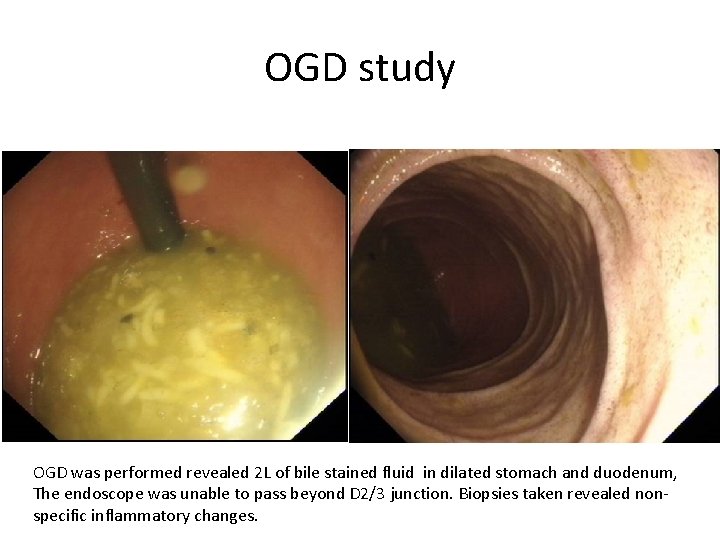
OGD study OGD was performed revealed 2 L of bile stained fluid in dilated stomach and duodenum, The endoscope was unable to pass beyond D 2/3 junction. Biopsies taken revealed nonspecific inflammatory changes.

Barium Meal Barium meal confirmed hold up of contrast till D 3/4 with delay in transit
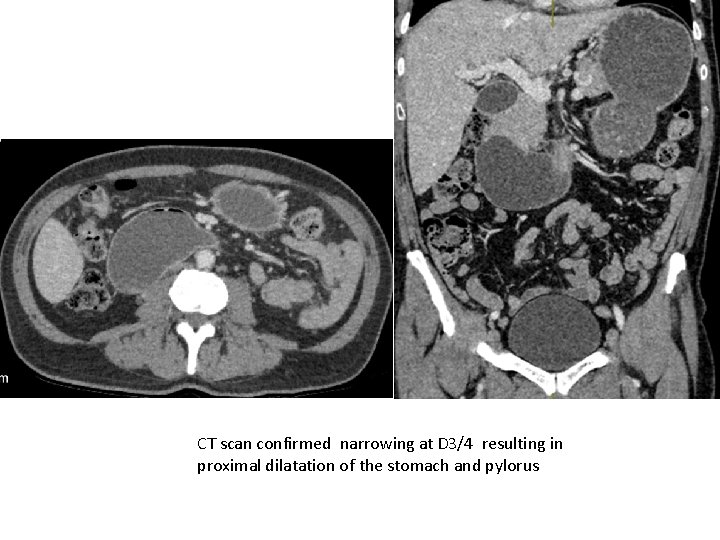
CT scan confirmed narrowing at D 3/4 resulting in proximal dilatation of the stomach and pylorus
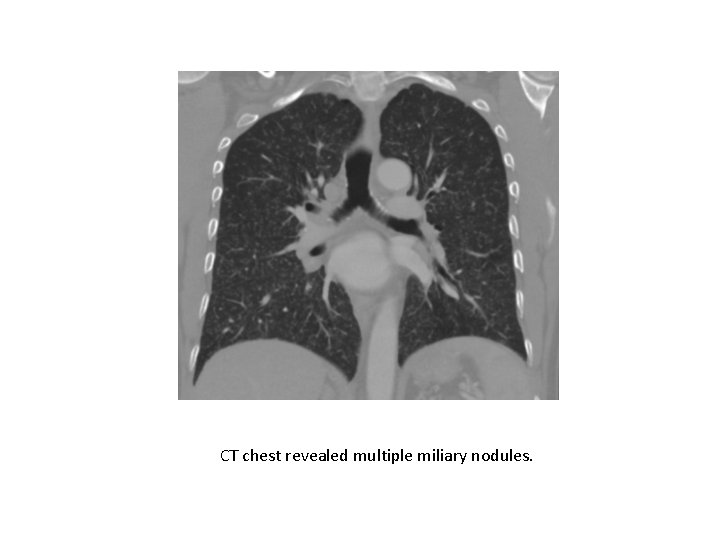
CT chest revealed multiple miliary nodules.
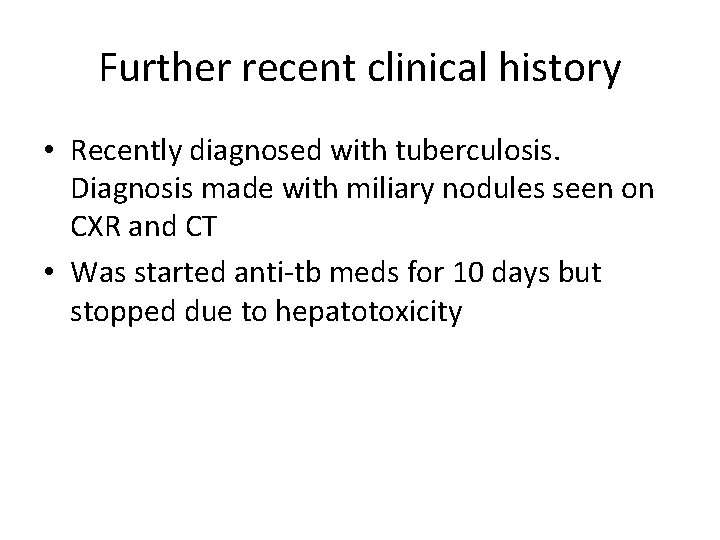
Further recent clinical history • Recently diagnosed with tuberculosis. Diagnosis made with miliary nodules seen on CXR and CT • Was started anti-tb meds for 10 days but stopped due to hepatotoxicity
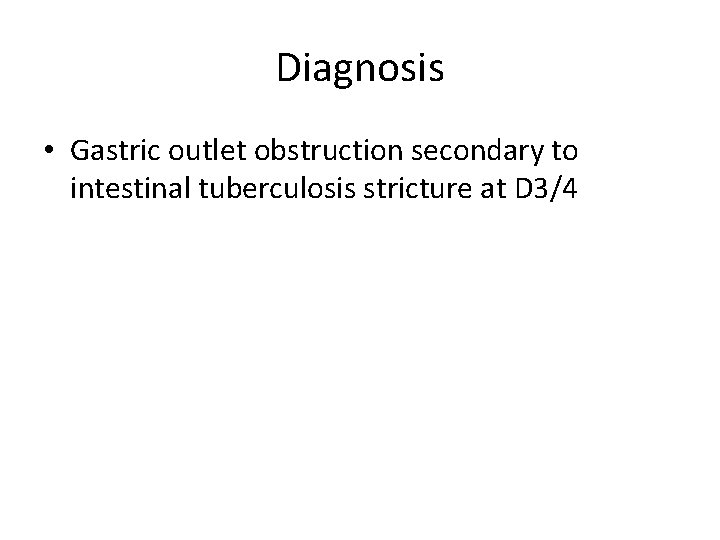
Diagnosis • Gastric outlet obstruction secondary to intestinal tuberculosis stricture at D 3/4
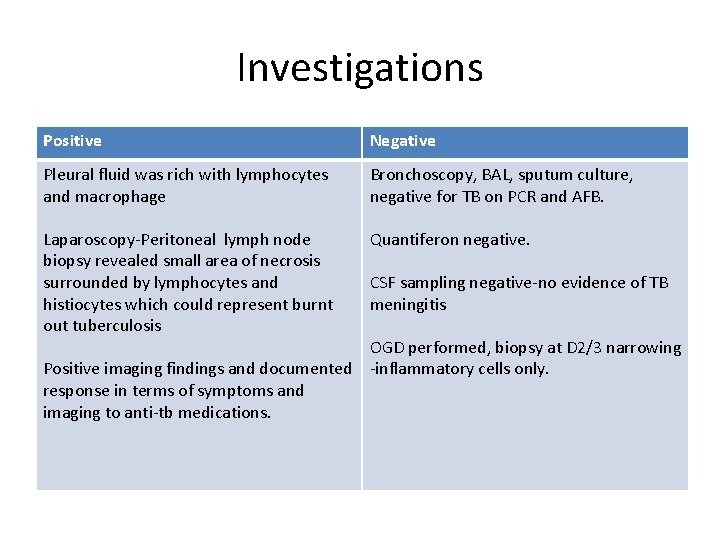
Investigations Positive Negative Pleural fluid was rich with lymphocytes and macrophage Bronchoscopy, BAL, sputum culture, negative for TB on PCR and AFB. Laparoscopy-Peritoneal lymph node biopsy revealed small area of necrosis surrounded by lymphocytes and histiocytes which could represent burnt out tuberculosis Quantiferon negative. CSF sampling negative-no evidence of TB meningitis OGD performed, biopsy at D 2/3 narrowing Positive imaging findings and documented -inflammatory cells only. response in terms of symptoms and imaging to anti-tb medications.
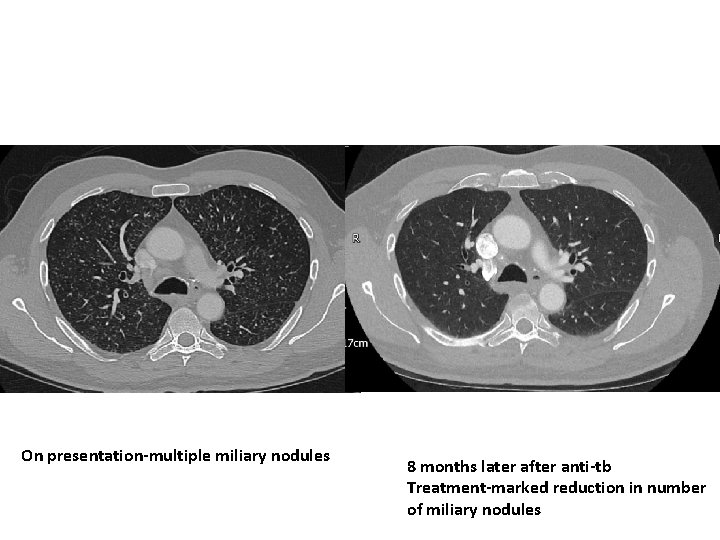
On presentation-multiple miliary nodules 8 months later after anti-tb Treatment-marked reduction in number of miliary nodules
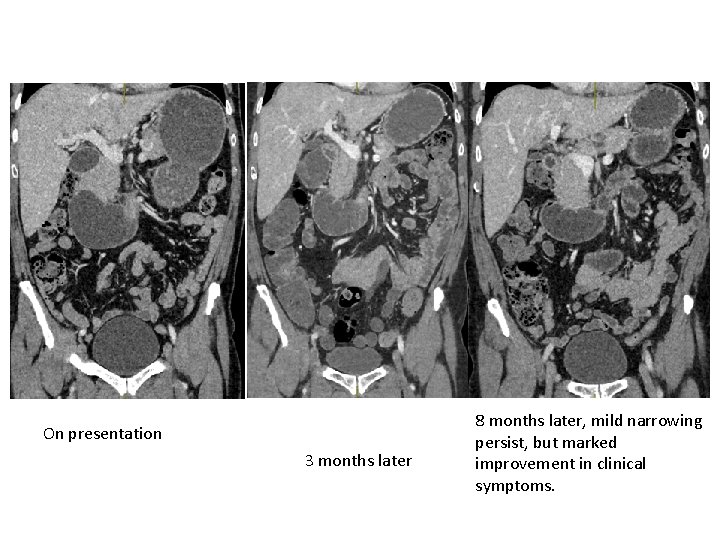
On presentation 3 months later 8 months later, mild narrowing persist, but marked improvement in clinical symptoms.
Discussion and learning points Pathophysiology • GI tuberculosis usually involves the ileocaecal junction but there have been cases reported involving the small bowel. • Intestinal tuberculosis has usually one of the three main forms i. e. ulcerative, hypertrophic or ulcerohypertrophic, and fibrous stricturing form. • Duodenal tuberculosis is rare and only a handful of case reports.
Clinical findings • • Signs of upper GI obstruction; Epigastric pain, vomiting, nausea, weight loss Diagnosis for duodenal tuberculosis is difficult. High index of suspicion supported by radiological investigation, exploratory laparotomy and histopathological examination of the tissue can only lead to a definitive diagnosis of this rare condition.
Imaging findings • The radiological features of duodenal tuberculosis are non-specific. • On barium studies, patients were found to have either one or a combination of mucosal ulcerations, luminal narrowing, extrinsic compression and proximal dilatations • Endoscopy may not be diagnostic and biopsies may only show nonspecific inflammation
References • https: //www. ncbi. nlm. nih. gov/pubmed/2400 9058 • https: //www. ncbi. nlm. nih. gov/pmc/articles/P MC 3024477/
- Slides: 15