Gas exchange Airway no gas exchange CO 2









- Slides: 43

Gas exchange Airway no gas exchange CO 2 flow O 2
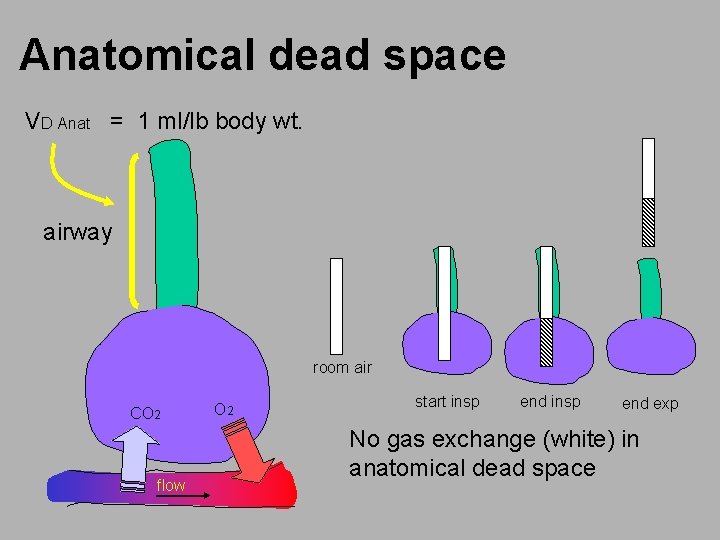
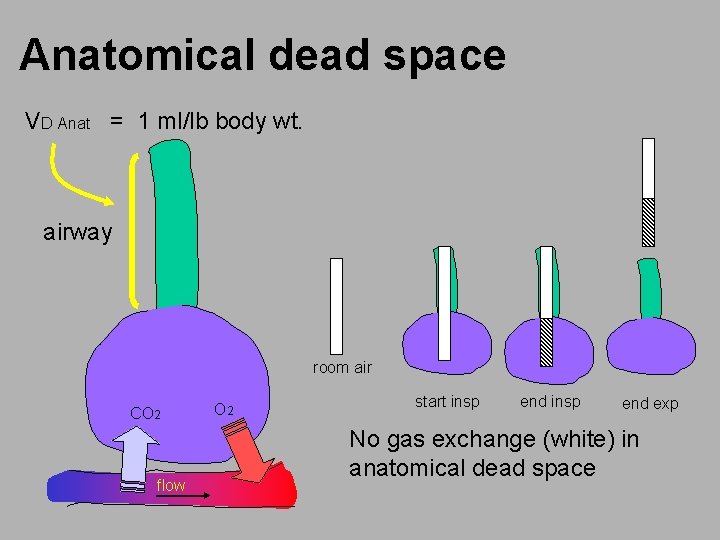
Anatomical dead space VD Anat = 1 ml/lb body wt. airway room air CO 2 flow O 2 start insp end exp No gas exchange (white) in anatomical dead space
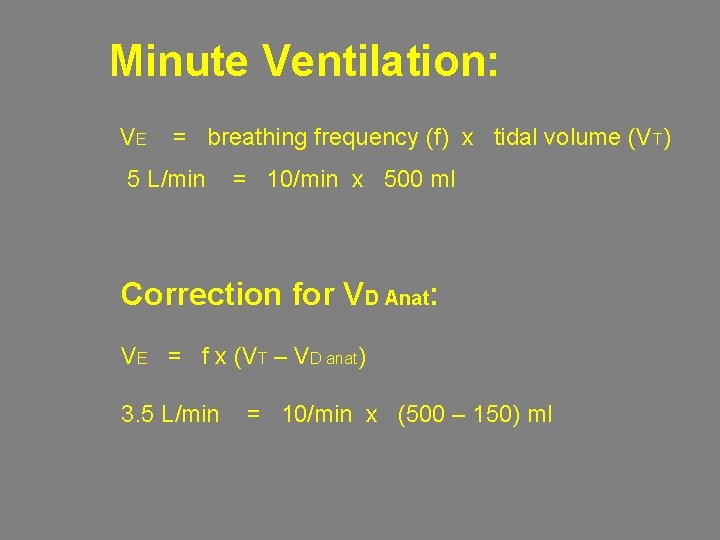
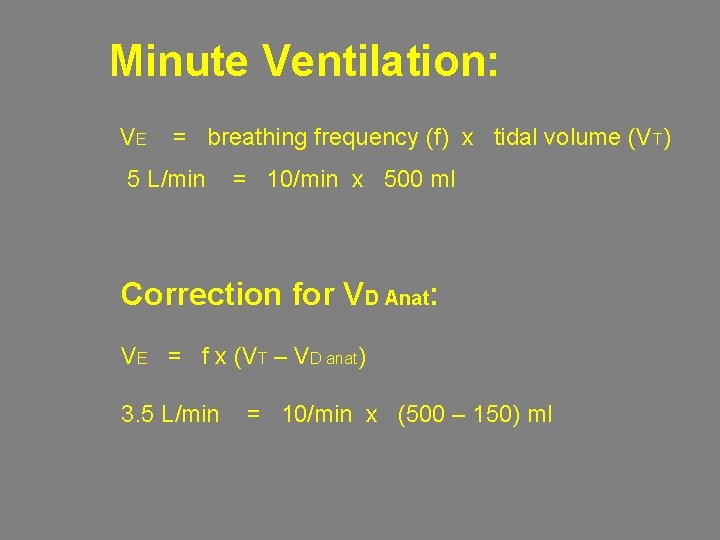
Minute Ventilation: VE = breathing frequency (f) x tidal volume (VT) 5 L/min = 10/min x 500 ml Correction for VD Anat: VE = f x (VT – VD anat) 3. 5 L/min = 10/min x (500 – 150) ml
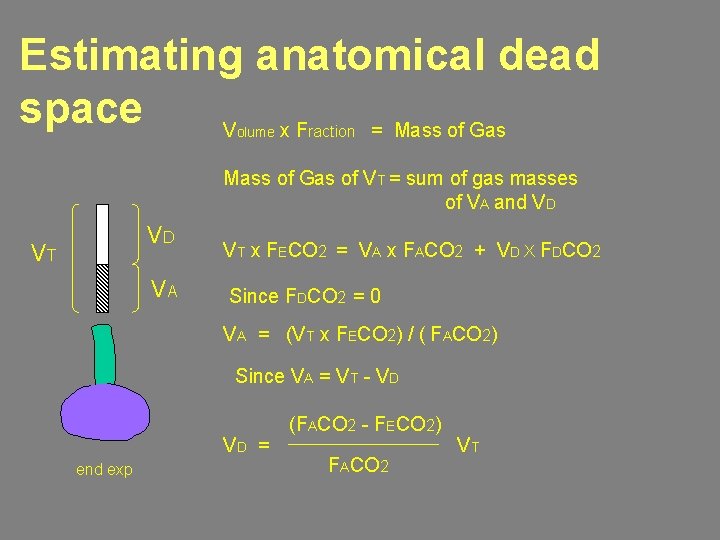
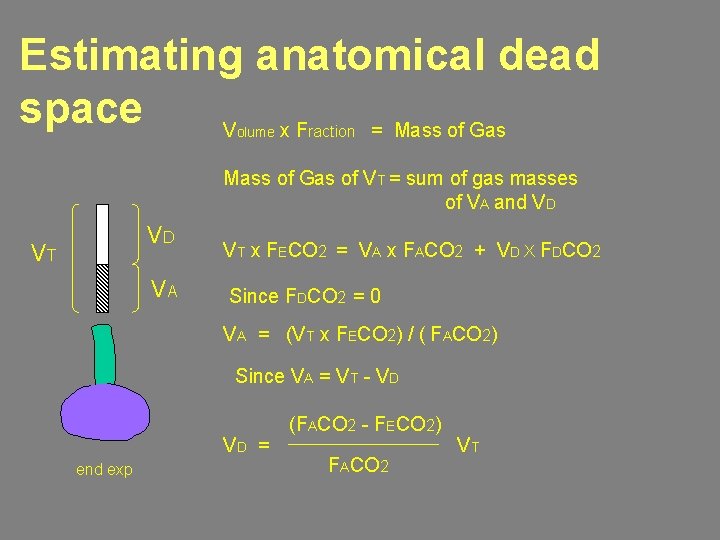
Estimating anatomical dead space V x. F = Mass of Gas olume raction Mass of Gas of VT = sum of gas masses of VA and VD VD VT VA VT x FECO 2 = VA x FACO 2 + VD X FDCO 2 Since FDCO 2 = 0 VA = (VT x FECO 2) / ( FACO 2) Since VA = VT - VD VD = end exp (FACO 2 - FECO 2) FACO 2 VT
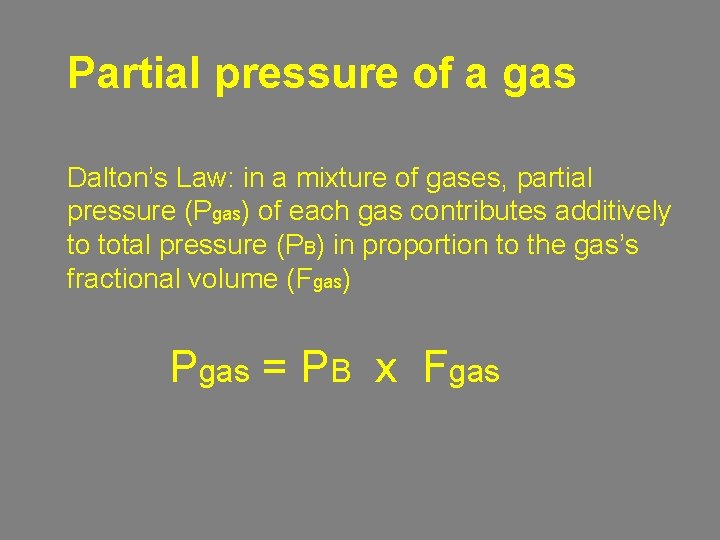
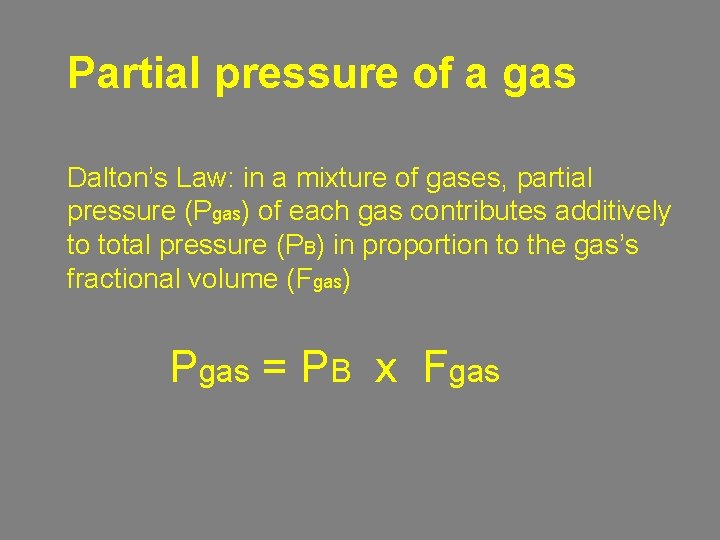
Partial pressure of a gas Dalton’s Law: in a mixture of gases, partial pressure (Pgas) of each gas contributes additively to total pressure (PB) in proportion to the gas’s fractional volume (Fgas) Pgas = PB x Fgas
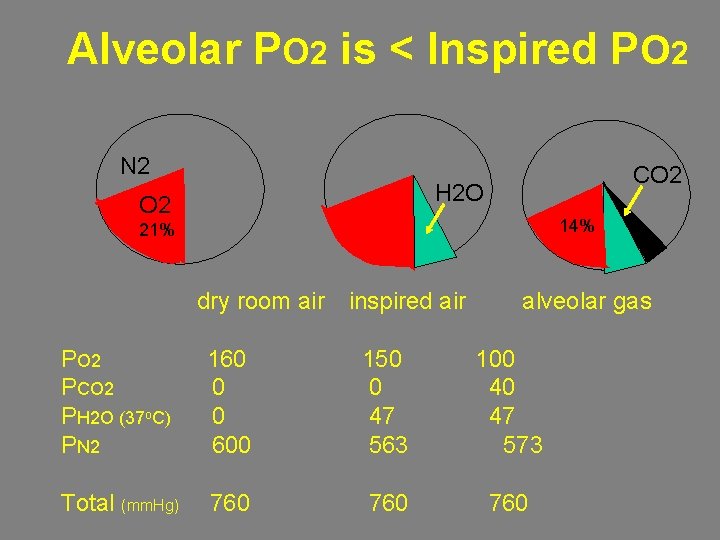
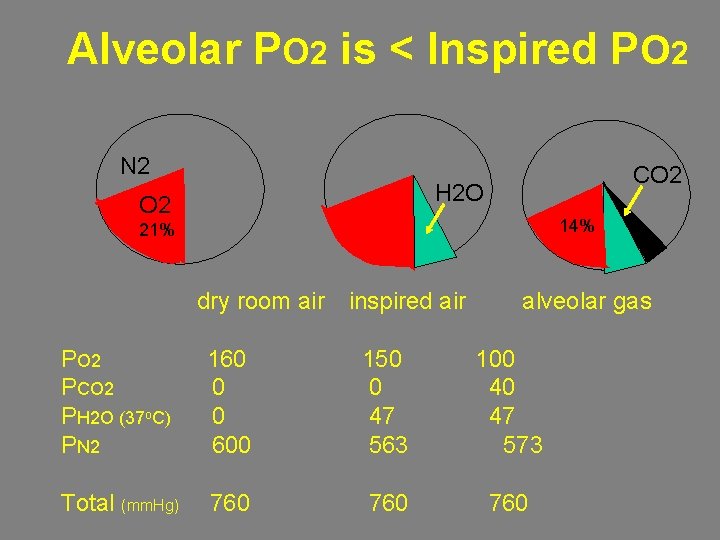
Alveolar PO 2 is < Inspired PO 2 N 2 CO 2 H 2 O O 2 14% 21% dry room air inspired air alveolar gas PO 2 PCO 2 PH 2 O (37 o. C) PN 2 160 0 0 600 150 0 47 563 100 40 47 573 Total (mm. Hg) 760 760
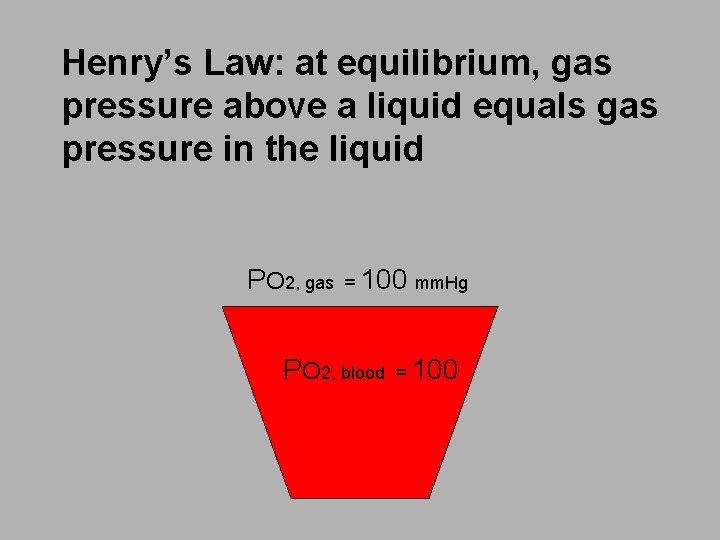
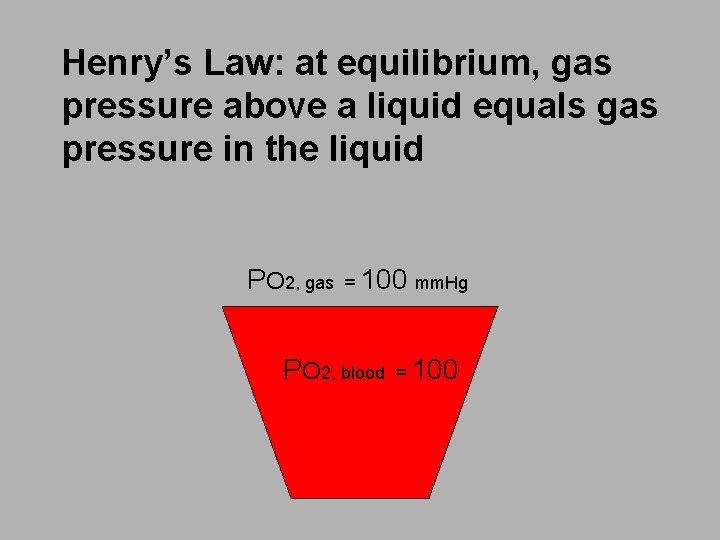
Henry’s Law: at equilibrium, gas pressure above a liquid equals gas pressure in the liquid PO 2, gas = 100 mm. Hg PO 2, blood = 100
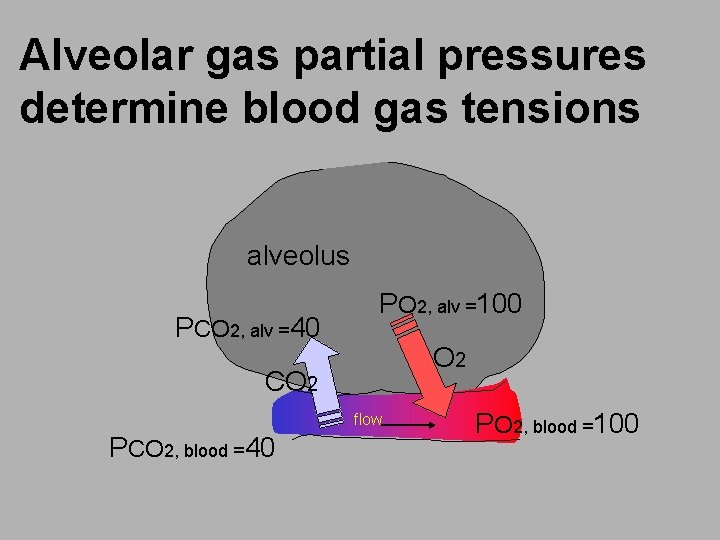
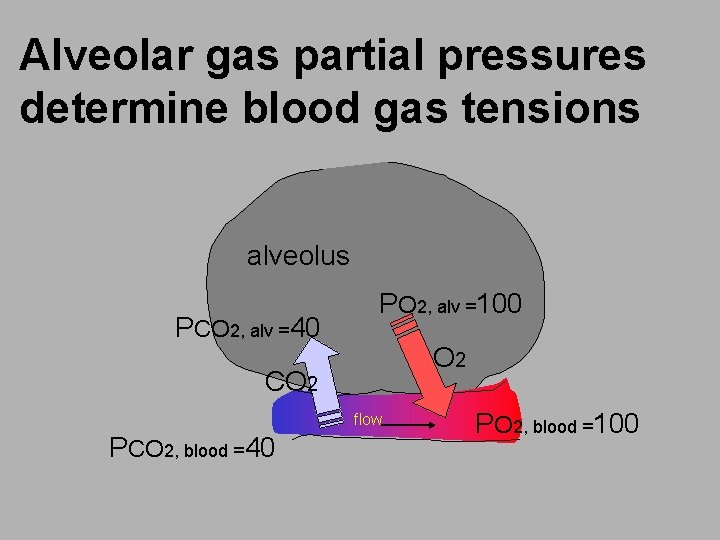
Alveolar gas partial pressures determine blood gas tensions alveolus PCO 2, alv =40 PO 2, alv =100 O 2 CO 2 flow PCO 2, blood =40 PO 2, blood =100
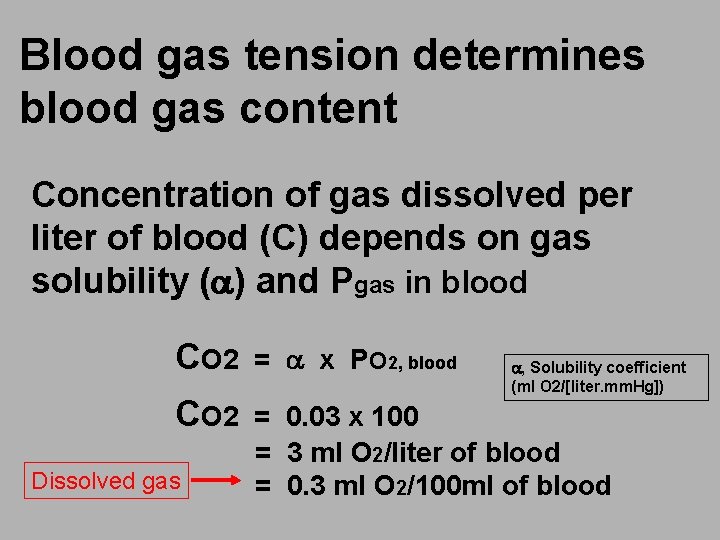
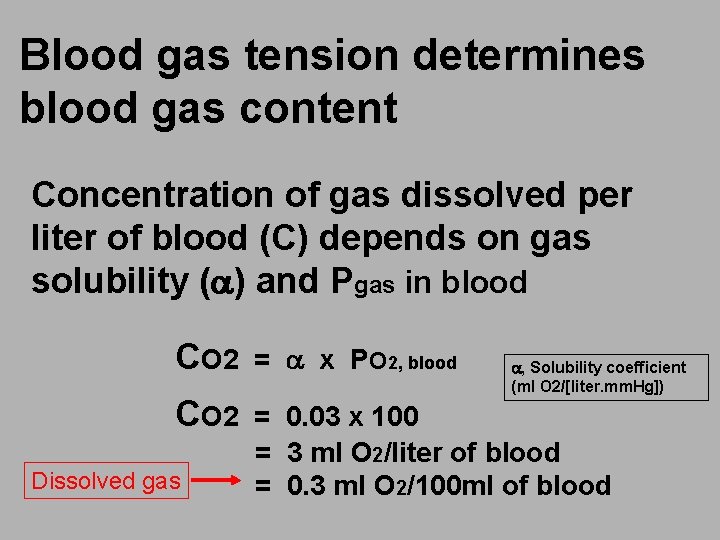
Blood gas tension determines blood gas content Concentration of gas dissolved per liter of blood (C) depends on gas solubility (a) and Pgas in blood CO 2 = a x PO 2, blood CO 2 = 0. 03 x 100 = 3 ml O 2/liter of blood = 0. 3 ml O 2/100 ml of blood Dissolved gas a, Solubility coefficient (ml O 2/[liter. mm. Hg])

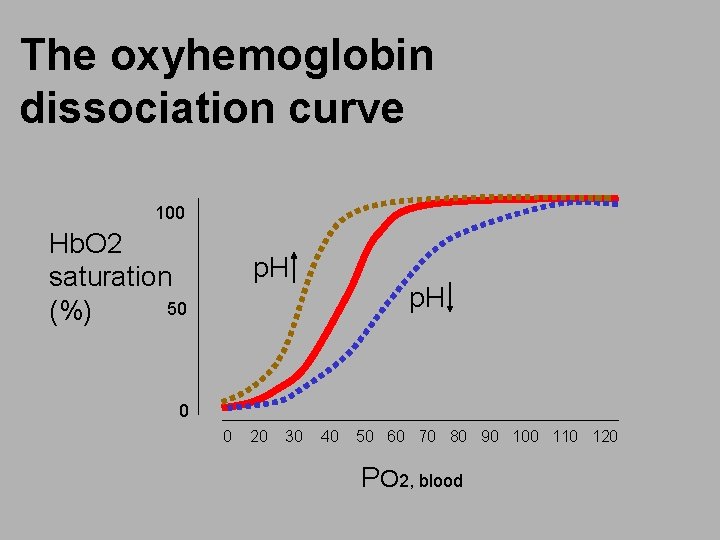
The oxyhemoglobin dissociation curve 100 Hb. O 2 saturation 50 (%) 0 0 20 30 40 50 60 70 80 90 100 110 120 PO 2, blood

The O 2 carrying capacity of blood = Hgb-bound O 2 + dissolved O 2 PO 2, alv PO 2, blood dissolved O 2 in blood Hgb. O 2 saturation = 1. 34 ml at 100% O 2 content in 1 liter of blood at PO 2, blood of 100 mm. Hg = (Hgb. O 2 sat [%] x 1. 34 x [Hgb]) + (. 03 x PO 2, blood) = (0. 98 x 1. 34 x 150 [g/l]) + 3 = 200 ml O 2/liter of blood
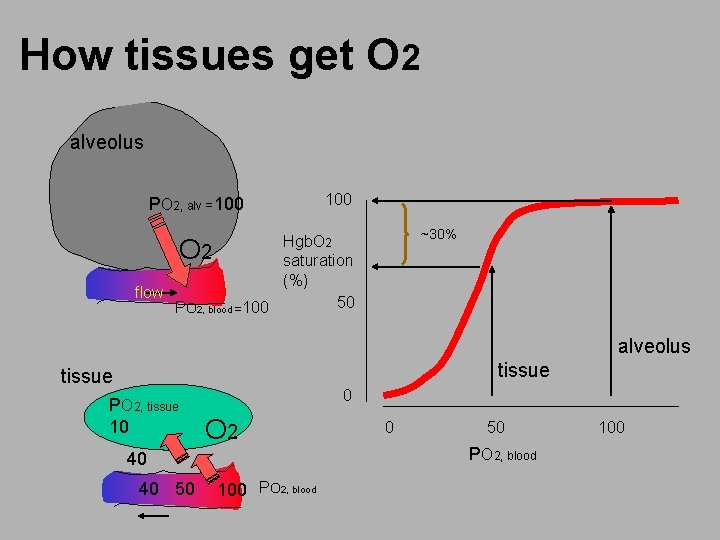
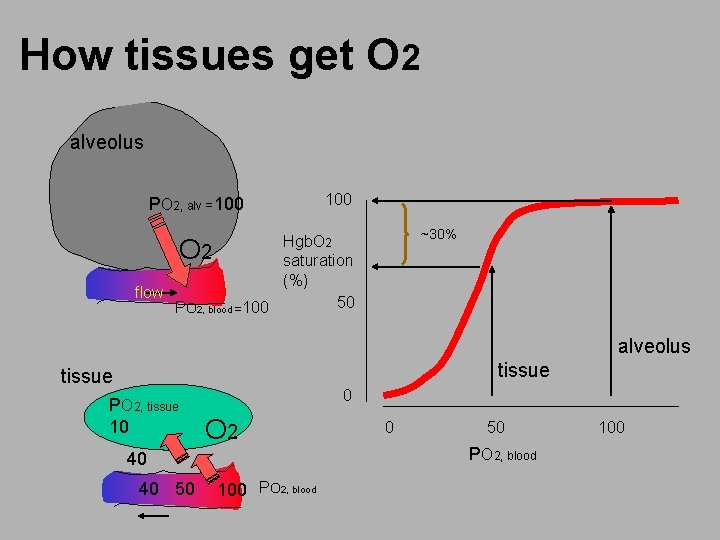
How tissues get O 2 alveolus PO 2, alv =100 ~30% Hgb. O 2 2 saturation (%) flow 50 PO 2, blood =100 O alveolus tissue PO 2, tissue 10 0 O 2 40 40 50 100 PO 2, blood 0 50 PO 2, blood 100
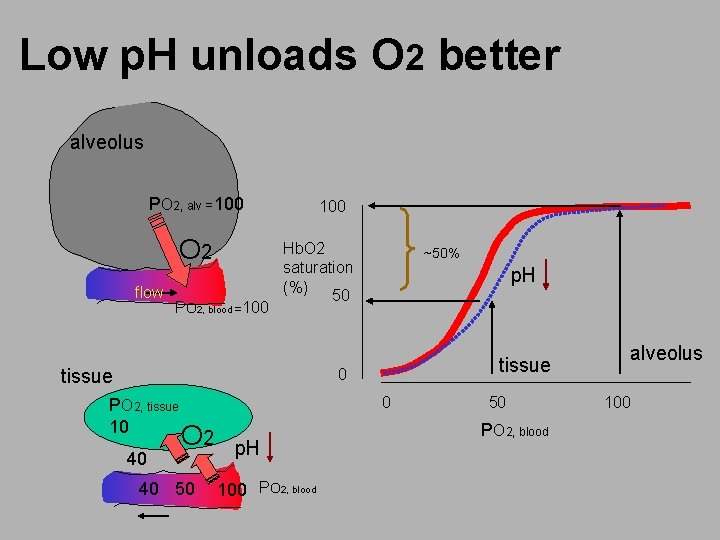
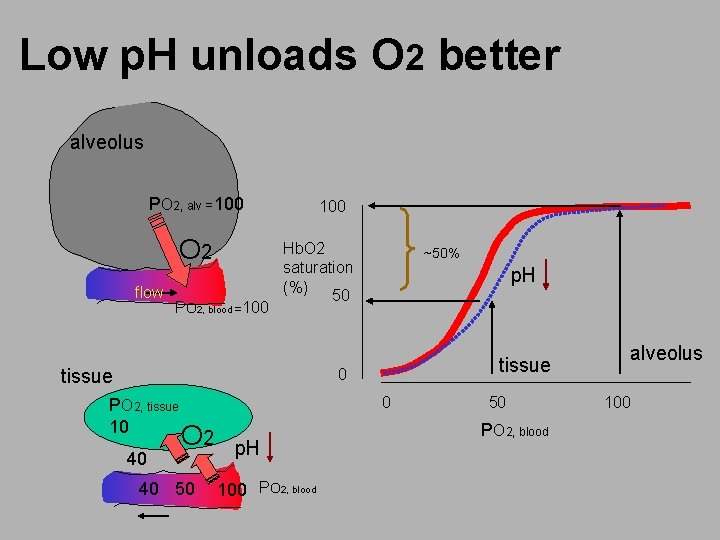
Low p. H unloads O 2 better alveolus PO 2, alv =100 O 2 flow PO 2, blood =100 Hb. O 2 saturation (%) 50 tissue ~50% p. H tissue 0 PO 2, tissue 10 40 0 O 2 40 50 p. H 100 PO 2, blood 50 PO 2, blood alveolus 100
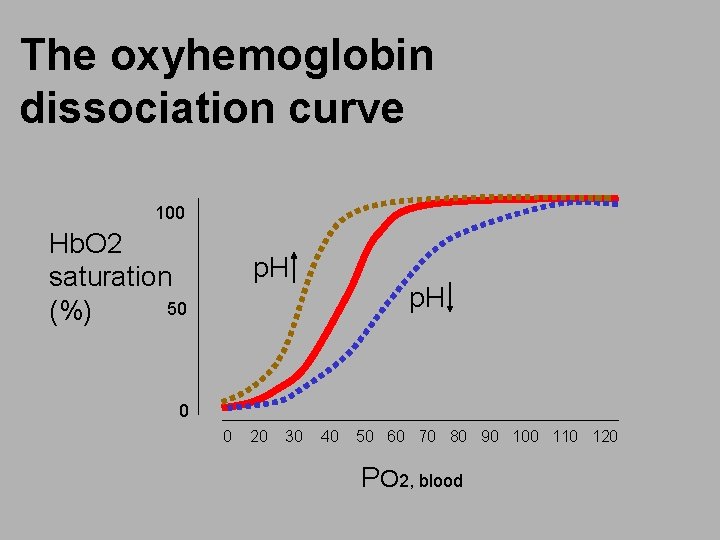
The oxyhemoglobin dissociation curve 100 Hb. O 2 saturation 50 (%) p. H 0 0 20 30 40 50 60 70 80 90 100 110 120 PO 2, blood

The pulmonary circulation O 2 CO 2 Pulmonary capillaries Pulmonary artery Pulmonary vein LA RV tissue

PVR is <<< SVR PVR = (Ppa – Pla) / CO CO 2 = 2 units O 2 Pulmonary capillaries Ppa = 20 Pla = 10 LA Pra = 0 RV CO = 5 Note: pressures are ‘mean’ and in cm. H 2 O. CO is 5 L/min. Pao = 200 tissue SVR = (Pao – Pra) / CO = 40 units
The lung has low vascular resistance
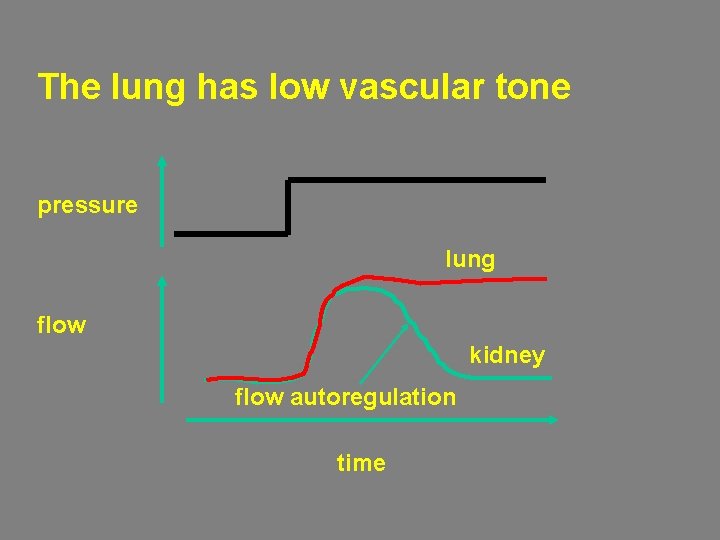
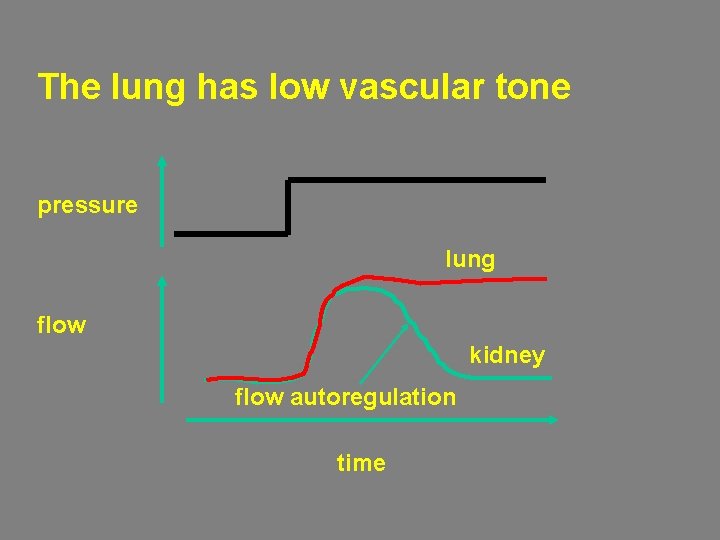
The lung has low vascular tone pressure lung flow kidney flow autoregulation time

Systemic capillaries
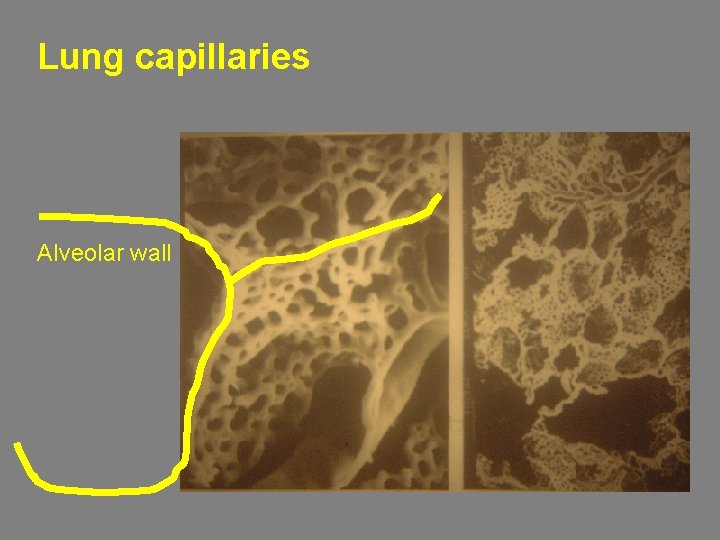
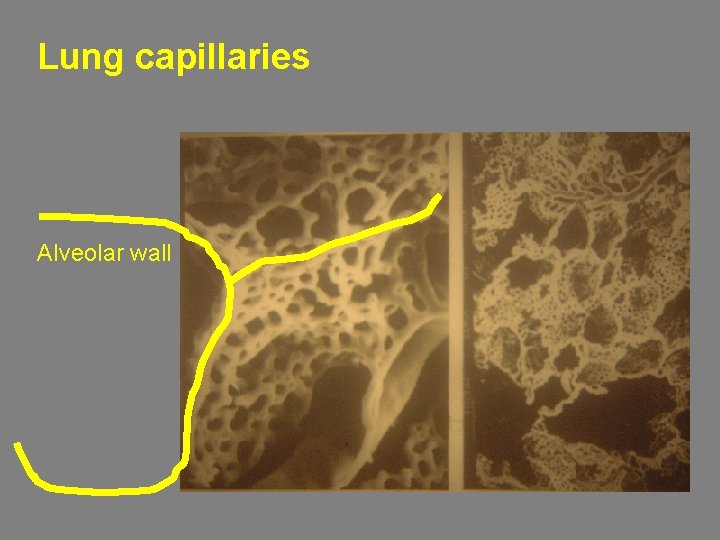
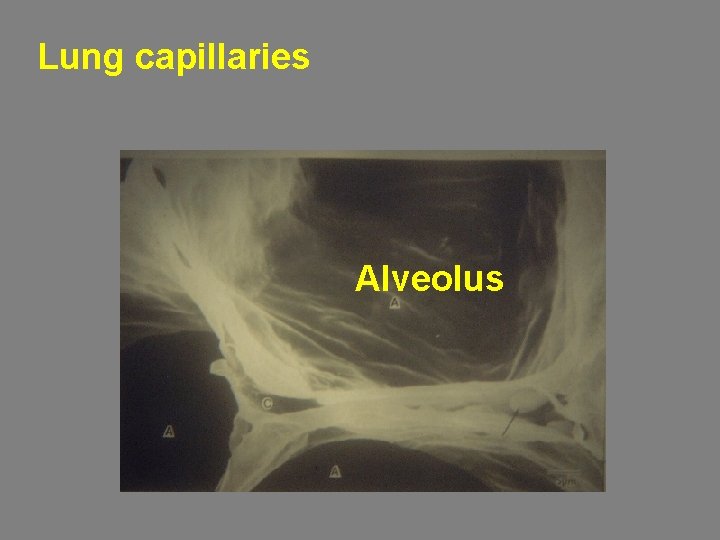
Lung capillaries Alveolar wall
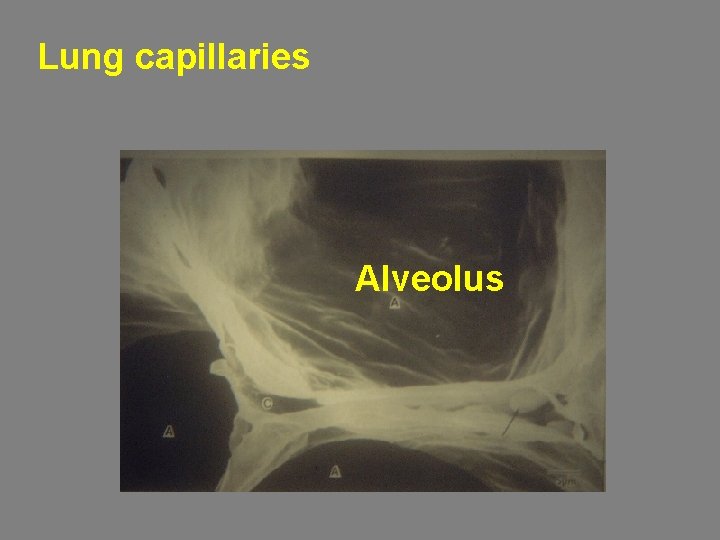
Lung capillaries Alveolus
The lung’s low vascular resistance is due to 1. Low vascular tone 2. Large capillary compliance
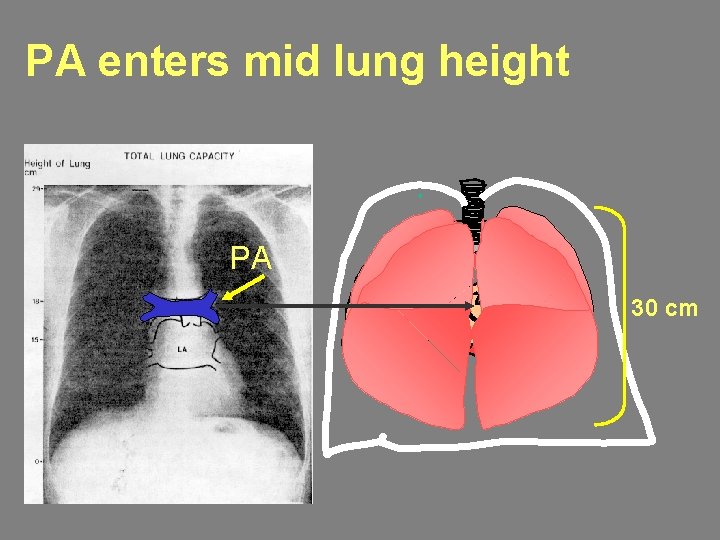
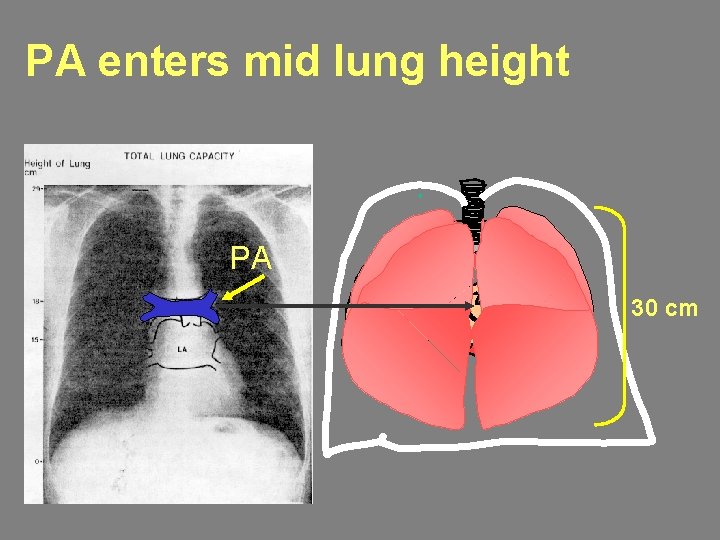
PA enters mid lung height PA 30 cm
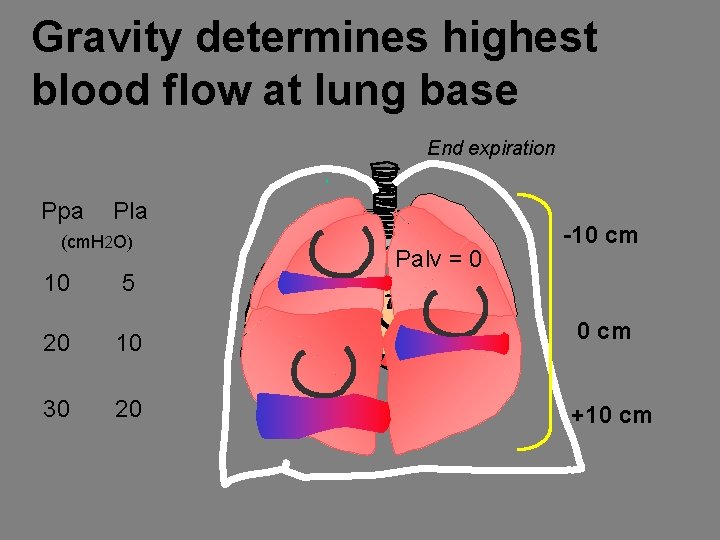
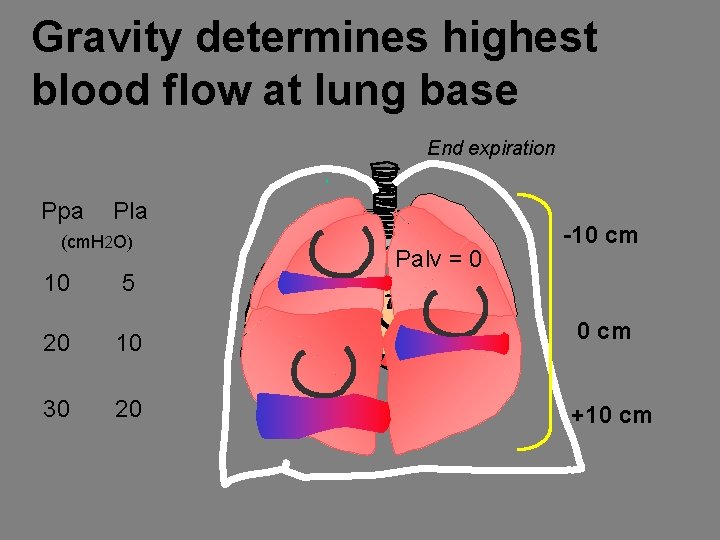
Gravity determines highest blood flow at lung base End expiration Ppa Pla (cm. H 2 O) Palv = 0 -10 cm 10 5 20 10 0 cm 30 20 +10 cm
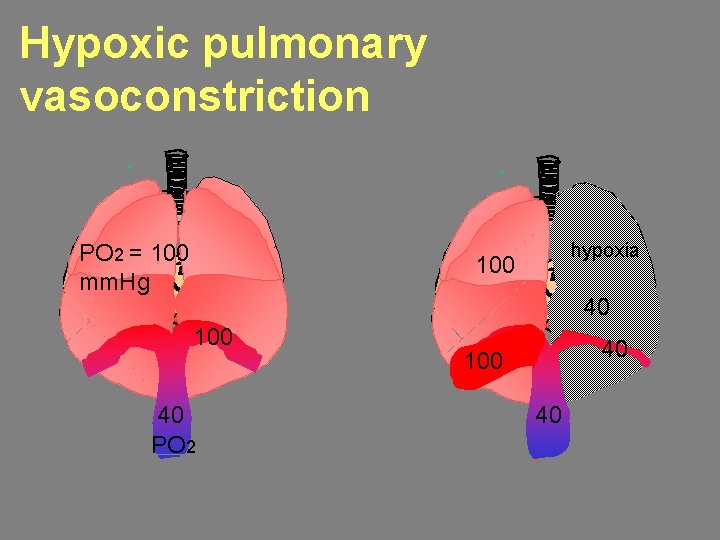
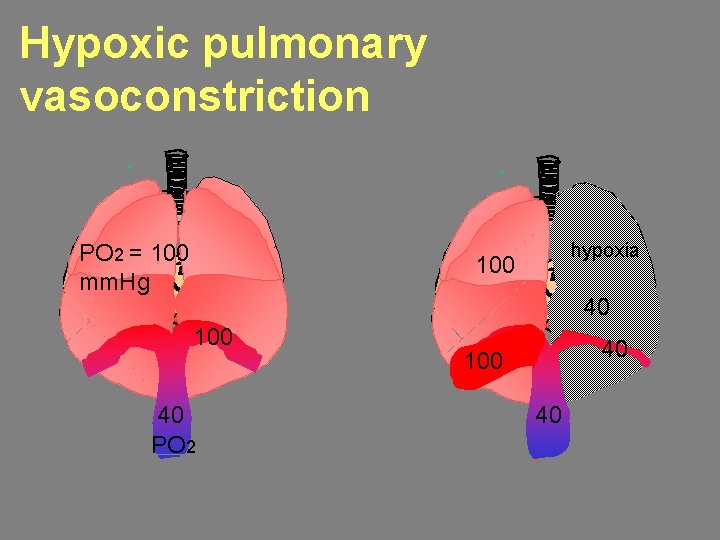
Hypoxic pulmonary vasoconstriction PO 2 = 100 mm. Hg hypoxia 100 40 PO 2 40 100 40
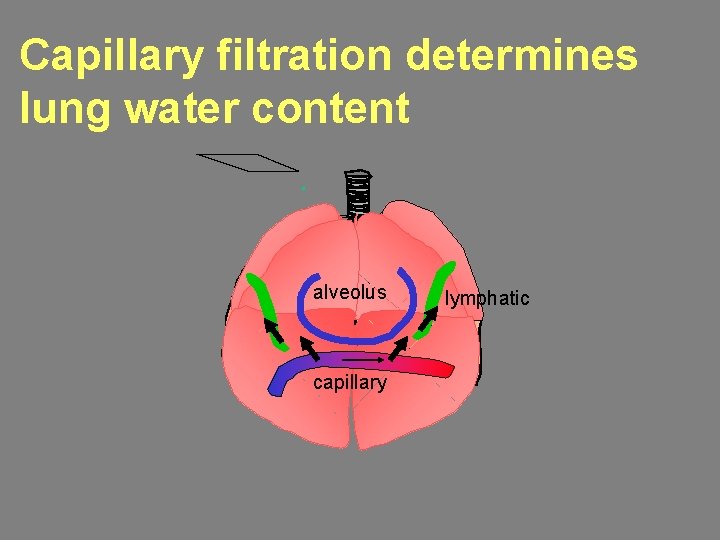
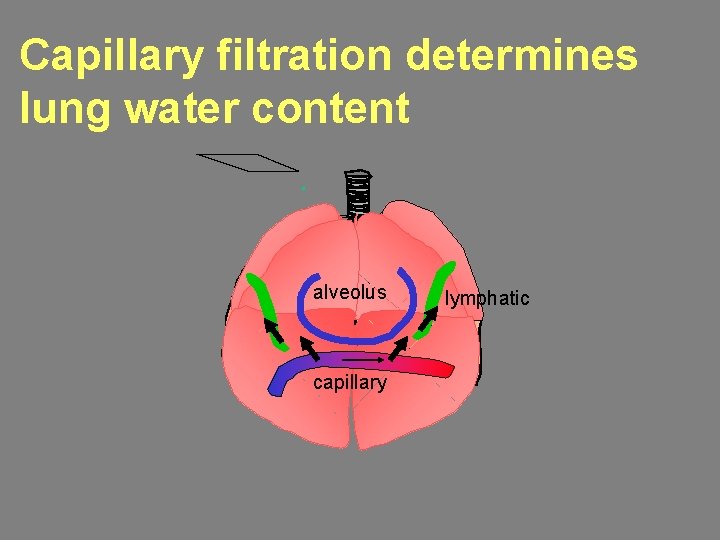
Capillary filtration determines lung water content alveolus capillary lymphatic

The Starling equation describes capillary filtration FR = Lp x S [ (Pc – Pi) – s (Pc – Pi) ] FR S Pc Pi alveolus Pi Pc filtration rate capillary surface area capillary pressure interstitial pressure s reflection coefficient Pc plasma colloid osmotic pressure Pi interstitial colloid osmotic pressure
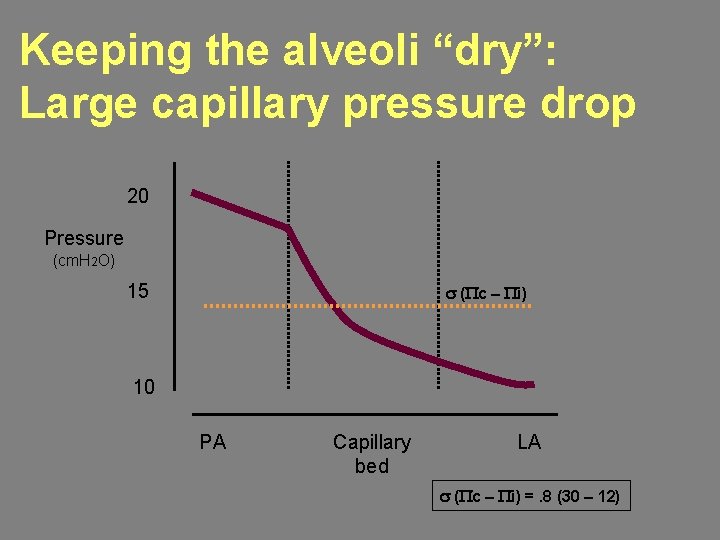
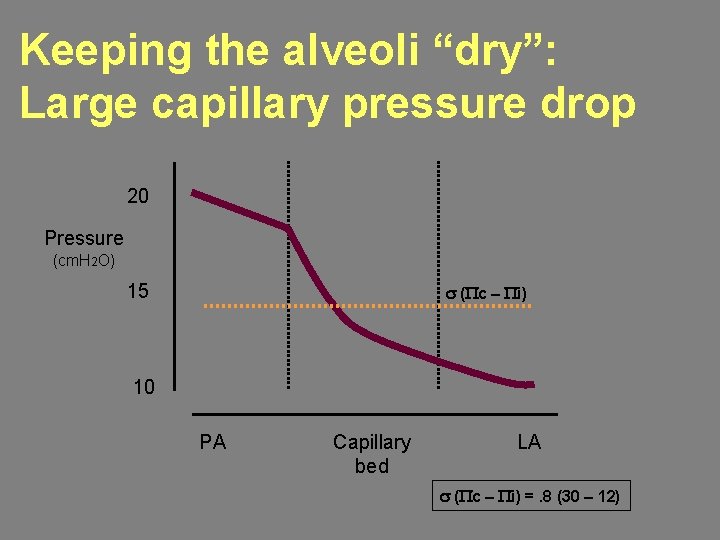
Keeping the alveoli “dry”: Large capillary pressure drop 20 Pressure (cm. H 2 O) 15 s (Pc – Pi) 10 PA Capillary bed LA s (Pc – Pi) =. 8 (30 – 12)
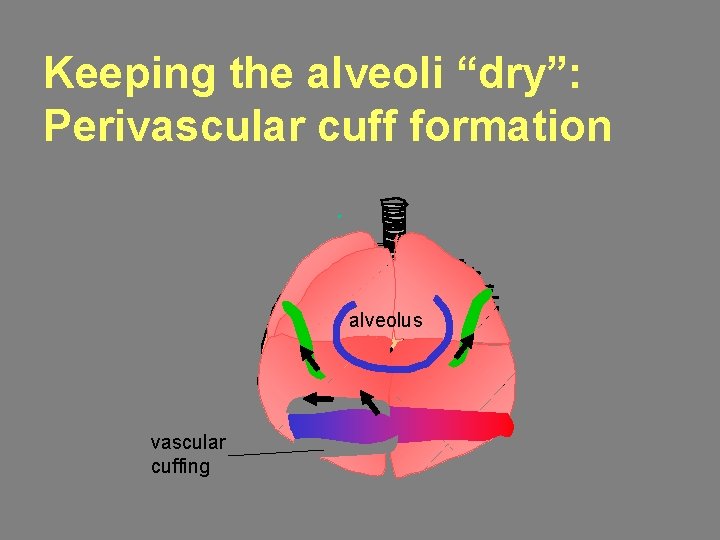
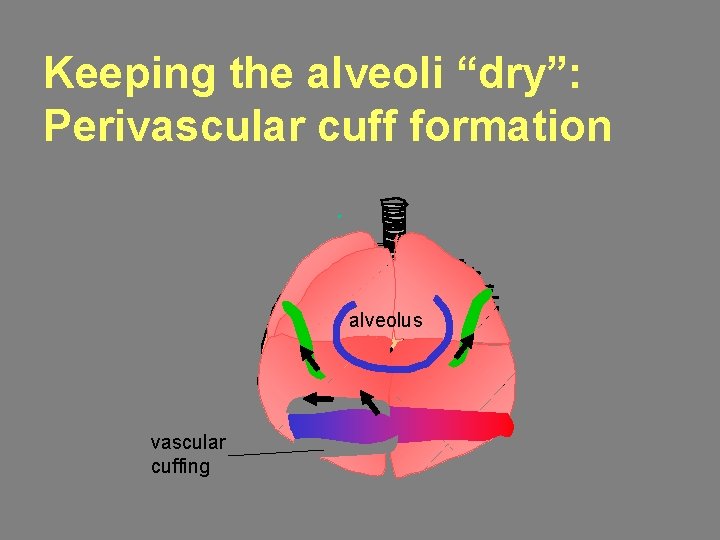
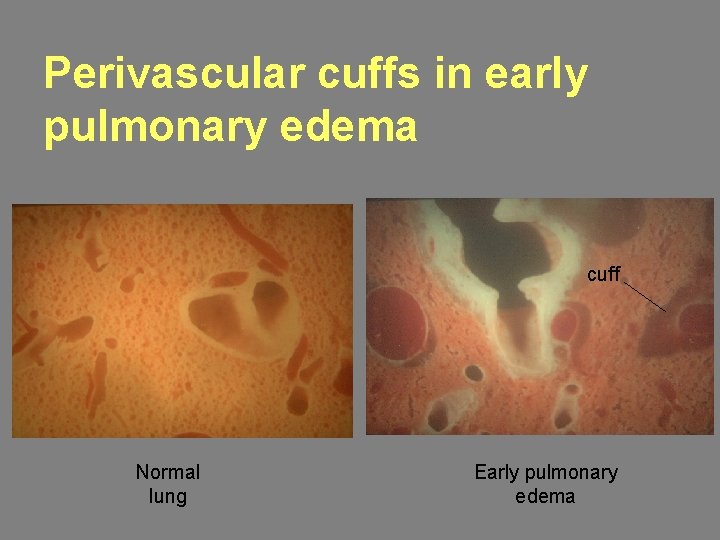
Keeping the alveoli “dry”: Perivascular cuff formation alveolus vascular cuffing
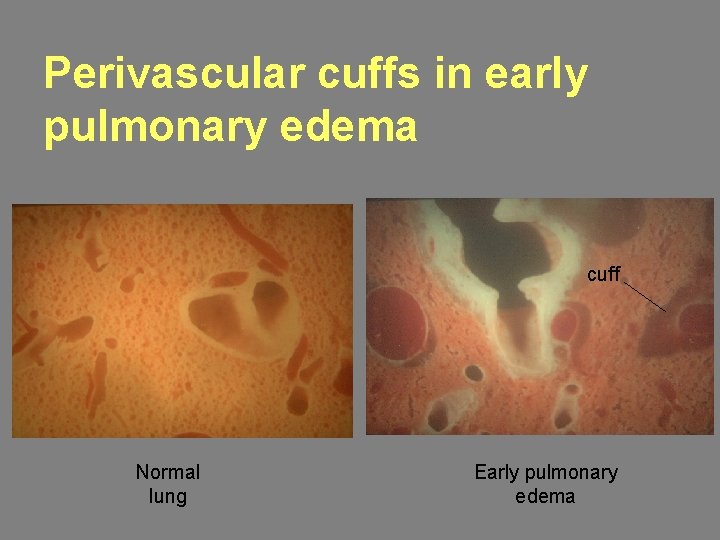
Perivascular cuffs in early pulmonary edema cuff Normal lung Early pulmonary edema
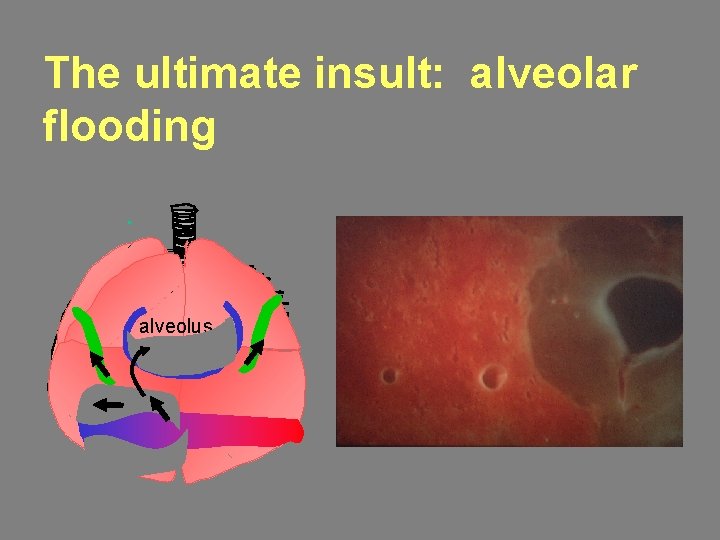
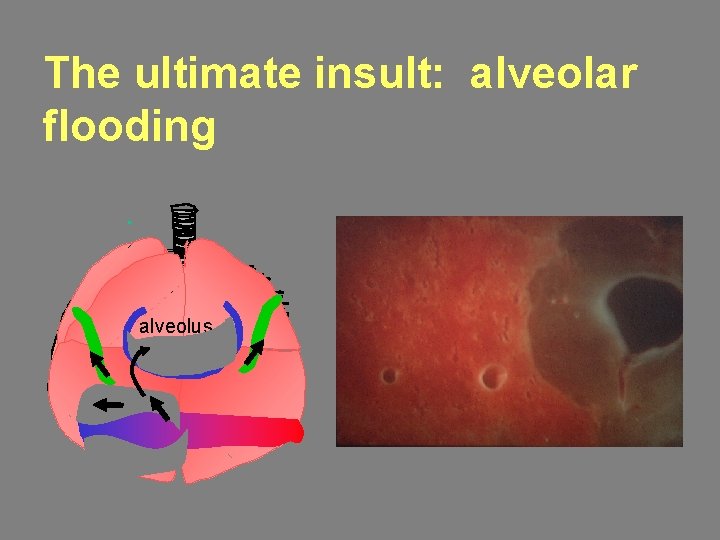
The ultimate insult: alveolar flooding alveolus
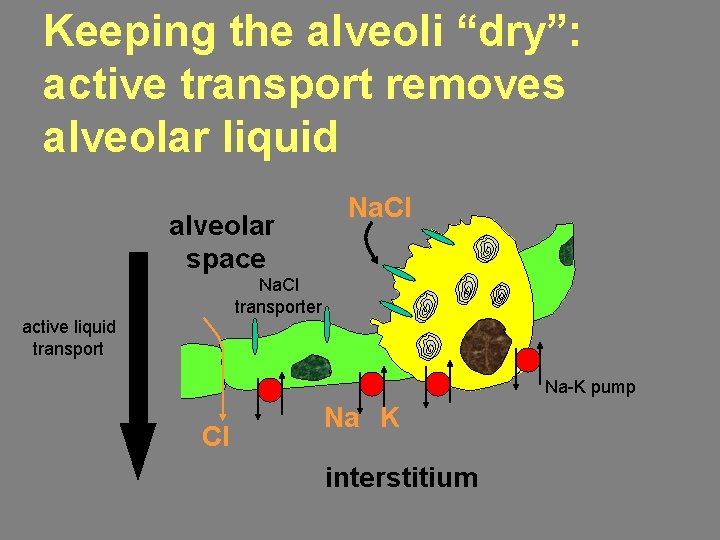
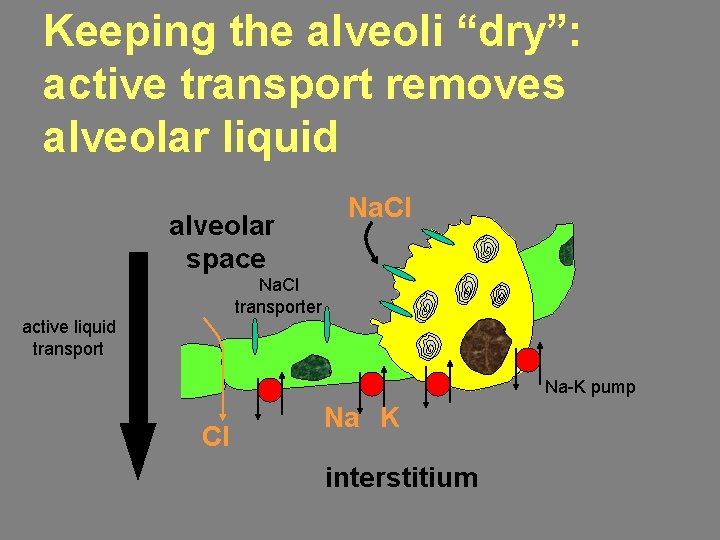
Keeping the alveoli “dry”: active transport removes alveolar liquid alveolar space Na. Cl transporter active liquid transport Na-K pump Cl Na K interstitium
SUMMARY Features of the pulmonary circulation designed for efficient gas exchange: 1. Accommodate the cardiac output * low vascular tone * high capillary compliance
SUMMARY Features of the pulmonary circulation designed for efficient gas exchange: 2. Keep filtration low near alveoli * low Pc * vascular interstitial sump
SUMMARY Features of the pulmonary circulation designed for efficient gas exchange: 3. Keep liquid out of the alveoli * active transport * high resistance epithelium
Control of Breathing Central neurons determine minute ventilation (VE) by regulating tidal volume (VT) and breathing frequency (f). VE = V T x f
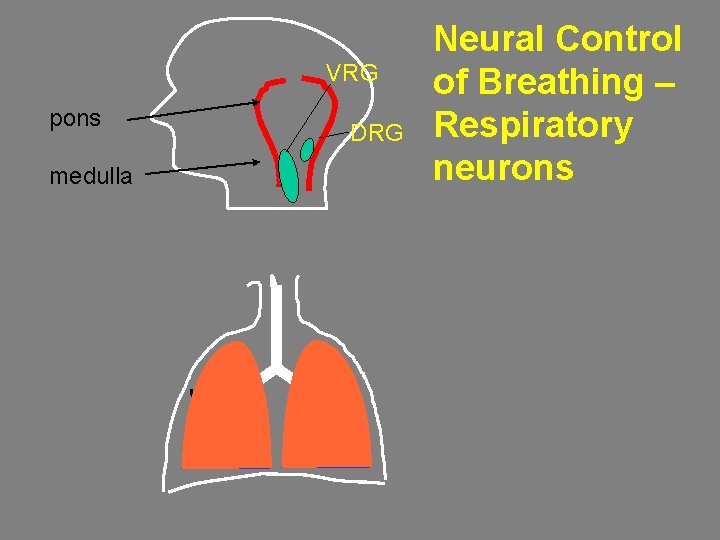
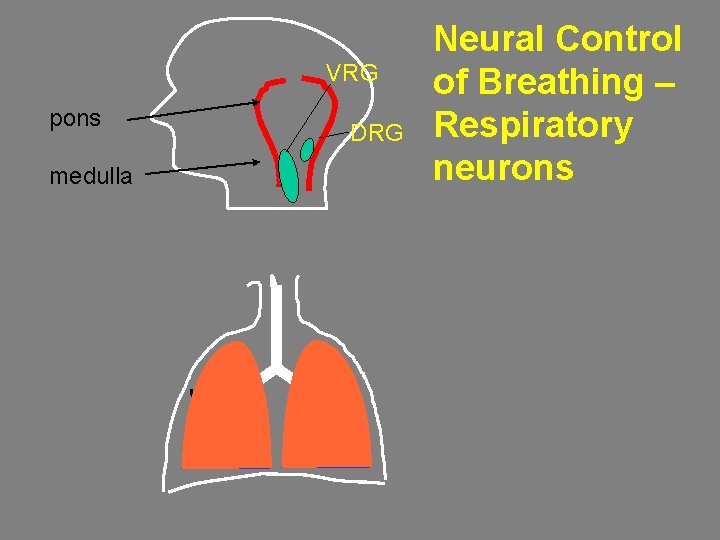
VRG pons medulla DRG Neural Control of Breathing – Respiratory neurons
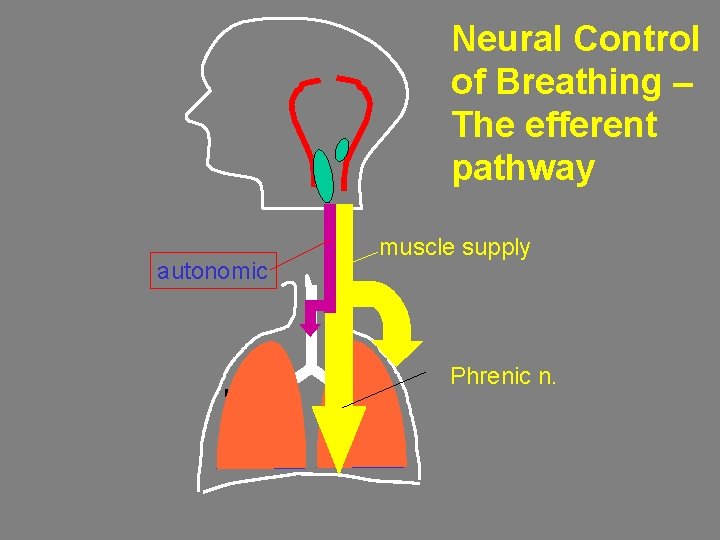
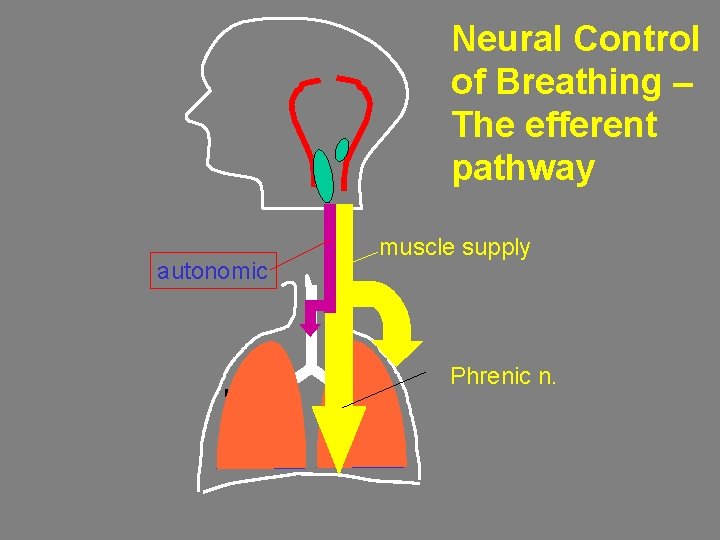
Neural Control of Breathing – The efferent pathway autonomic muscle supply Phrenic n.
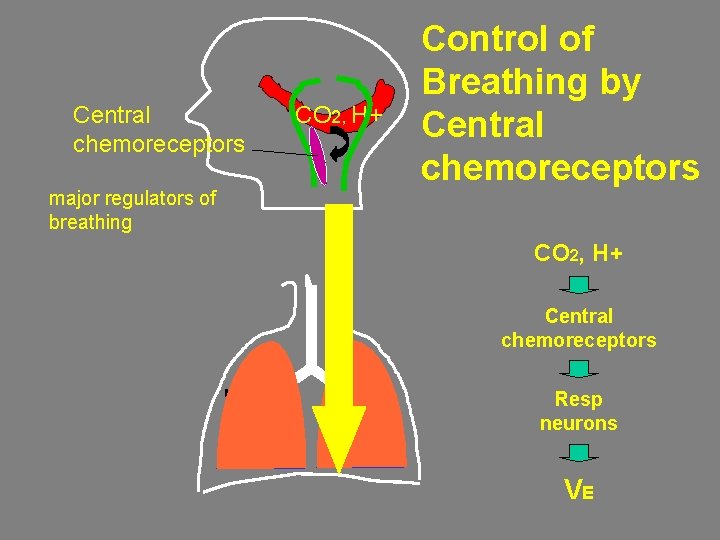
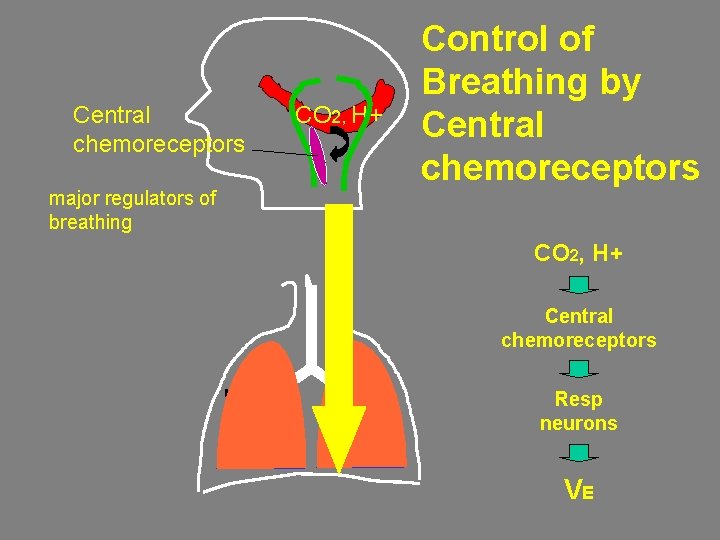
Central chemoreceptors major regulators of breathing CO 2, H+ Control of Breathing by Central chemoreceptors CO 2, H+ Central chemoreceptors Resp neurons VE
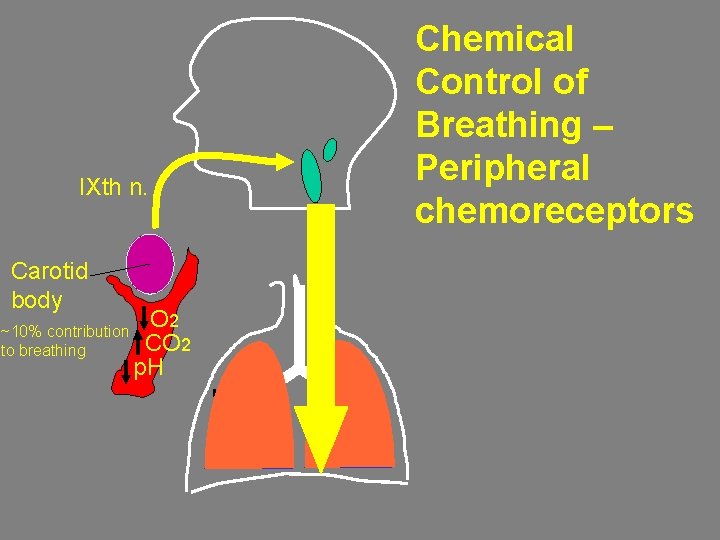
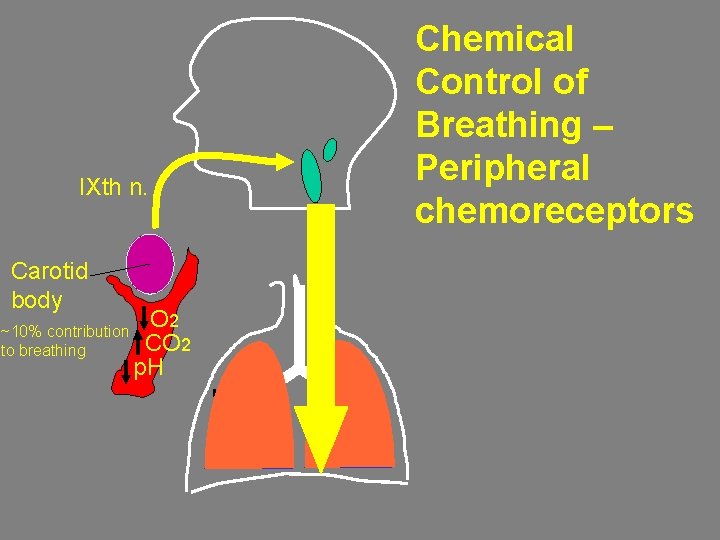
IXth n. Carotid body ~10% contribution to breathing O 2 CO 2 p. H Chemical Control of Breathing – Peripheral chemoreceptors

CO 2 drives ventilation 50 hypercapnia VE (L/min) 5 quiet breathing 35 40 45 CO 2 tension in blood (mm Hg)

Hypoxia is a weak ventilatory stimulus 50 blood p. O 2 = 50 mm. Hg VE blood p. O 2 = 100 mm. Hg (L/min) 5 35 40 45 CO 2 tension in blood (mm Hg)
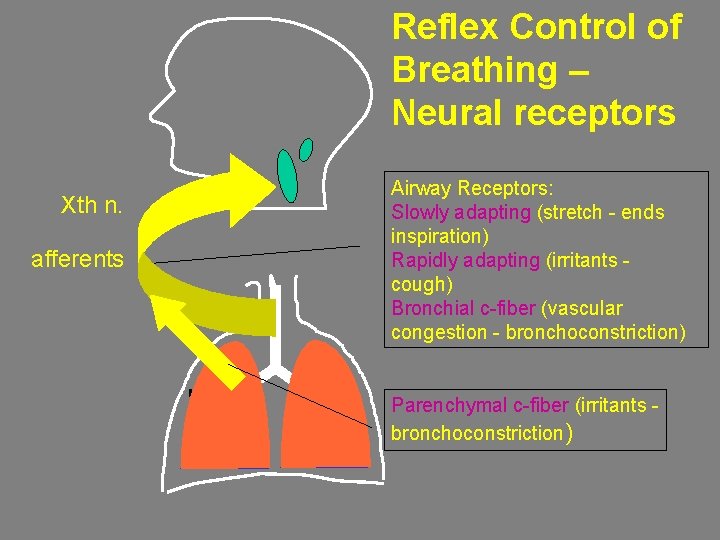
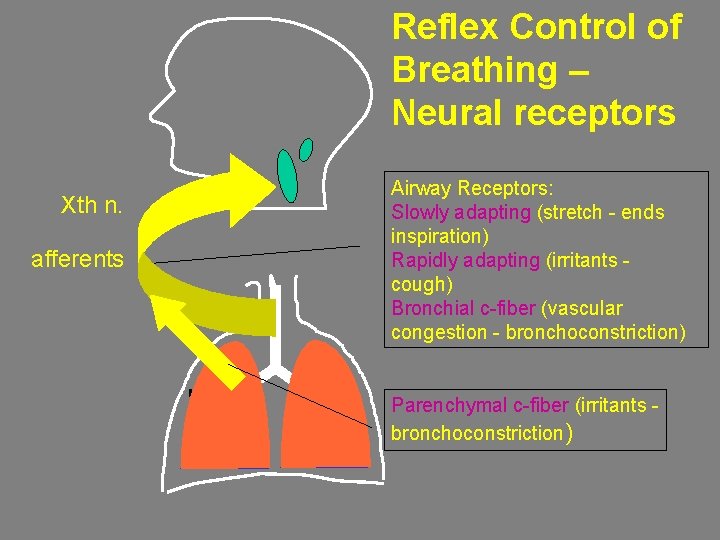
Reflex Control of Breathing – Neural receptors Xth n. afferents Airway Receptors: Slowly adapting (stretch - ends inspiration) Rapidly adapting (irritants cough) Bronchial c-fiber (vascular congestion - bronchoconstriction) Parenchymal c-fiber (irritants bronchoconstriction)
 Laryngoscopy view grades
Laryngoscopy view grades Gas exchange key events in gas exchange
Gas exchange key events in gas exchange Tatalaksana acls
Tatalaksana acls Aprv waveform
Aprv waveform Occepital
Occepital Stepwise airway management
Stepwise airway management Types of alveoli
Types of alveoli Norwich terrier upper airway syndrome
Norwich terrier upper airway syndrome Airway management ladder
Airway management ladder Cormack lehane grading
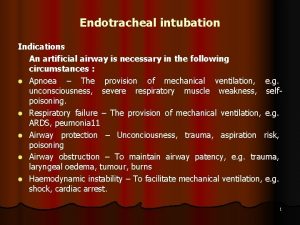
Cormack lehane grading Indications for artificial airway
Indications for artificial airway Asp medical
Asp medical Classroom.cloud
Classroom.cloud Nasopharyngeal airway
Nasopharyngeal airway Mean airway pressure
Mean airway pressure Airway abcde
Airway abcde Mechanism of respiratory system
Mechanism of respiratory system Intubating lma
Intubating lma Tracheostomy stoma
Tracheostomy stoma Open a casualty's airway
Open a casualty's airway Moans airway
Moans airway Airway anatomy intubation
Airway anatomy intubation Nasofaringeal
Nasofaringeal Chapter 9 airway management
Chapter 9 airway management Airway numaraları
Airway numaraları Cricothyroidotomy
Cricothyroidotomy Constricted airway
Constricted airway Nasopharyngeal airway
Nasopharyngeal airway Asa airway
Asa airway Krikotiroid membran
Krikotiroid membran Airway breathing c
Airway breathing c Ztechnique
Ztechnique Respiratory airway secretary
Respiratory airway secretary Mean airway pressure formula
Mean airway pressure formula Ehbo abcde
Ehbo abcde Asa airway fire algorithm
Asa airway fire algorithm Seeking consensual validation
Seeking consensual validation Sigh breaths on jet ventilator
Sigh breaths on jet ventilator Three emergency action steps
Three emergency action steps Lemon law anesthesie
Lemon law anesthesie Upper respiratory labeled
Upper respiratory labeled Retroglottic airway
Retroglottic airway Definitive airways
Definitive airways Hypoventilasi
Hypoventilasi