Gallstone disease Pathogenesis and clinical presentations Allan Kwok














- Slides: 58
Gallstone disease: Pathogenesis and clinical presentations Allan Kwok SET 4 Liverpool Hospital
� Approximately 12% of men and 24% of women of all ages have gallstones � 80% are asymptomatic � 2 -3% of patients progress per year to symptomatic disease � 1% of patients with gallstones develop acute complications � Approximately 12% of patients undergoing cholecystectomy found to have CBD stones
Constituents of bile �Lipid component ◦ Bile acids (70%) ◦ Phospholipids (25%) ◦ Cholesterol (5%) �Mucoproteins ◦ Act as a barrier between epithelium and concentrated bile acids ◦ However, also serve as a nidus for cholesterol nucleation
Types of gallstones �Cholesterol �Black pigment �Brown pigment �Mixed (usually contain >50% cholesterol) �Approximately 10 -20% have adequate calcification to render stones radioopaque
Bile acids �Primary bile acids include chenodeoxycholic acid and cholic acid �Conjugated to glycine (75%) or taurine (25%) in the liver before being transported into the bile cannaliculus �Bile acids, phospholipids and cholesterol form vesicles which increase solubility of cholesterol in bile
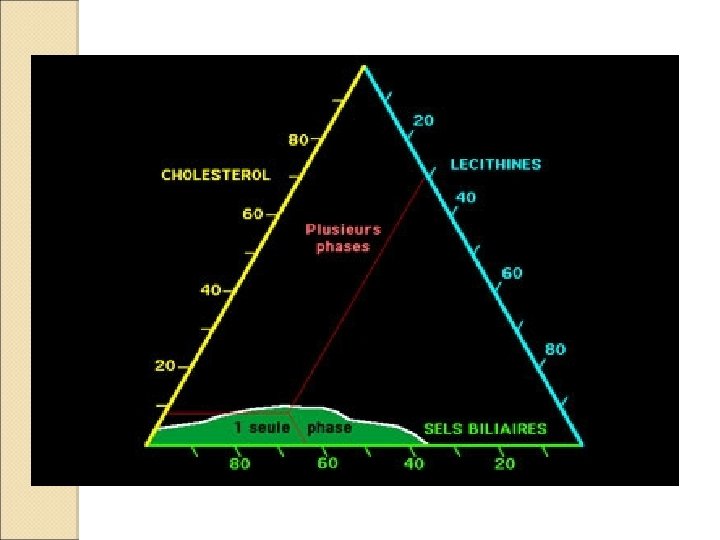
Cholesterol stone formation � Cholesterol is most soluble when bile acid concentration >50% � When biliary cholesterol concentration increases, the vesicles form multilamellar vesicles or micelles. These have a lower solubility coefficient for cholesterol and crystals form on their surfaces � Mucoproteins promote a pro-nucleation state and encourage further crystals to precipitate � Gallbladder stasis leads to concentration of bile and also contributes to poorer cholesterol solubility
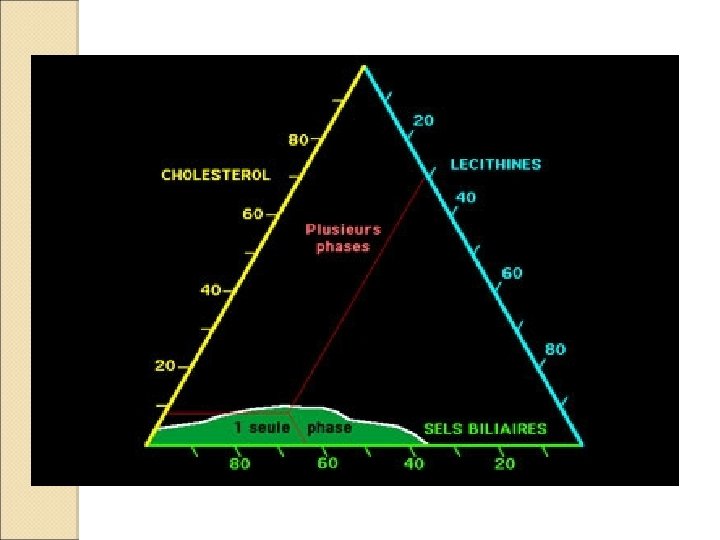

Cholesterol stone formation �There is a small zone where cholesterol will exist in a ‘metastable supersaturated zone’ �Outside of this, crystals of cholesterol will eventually precipitate
Black pigment stones (calcium bilirubinate) � Contain less than 20% cholesterol by weight � Generally smaller and dark in colour � More common in haemolytic conditions and patients with cirrhosis ◦ Haemolytic anaemia ◦ Thalassaemia ◦ Hypersplenism � Are caused by an increase in haem breakdown +/inability of the liver to conjugate bilirubin ◦ Haem -> biliverdin -> bilirubin ◦ Bilirubin is normally conjugated to glucuronic acid
Black pigment stones (calcium bilirubinate) � In haemolytic conditions, bilirubin concentrations are higher � In cirrhotic patients, the liver is unable to synthesise / conjugate adequately � Conjugated bilirubin is quite water-soluble � However, unconjugated bilirubin forms insoluble precipitates, especially with calcium, and is secreted into bile in higher-than-normal concentrations in these disease states � Usually form in the gallbladder
Brown pigment stones � Uncommon (5%) in Western society � Associated with biliary stasis and bacterial infection ◦ E. coli, Bacteroides, Ascaris � Bacteria release glucuronidase, which unconjugates bilirubin ◦ They also hydrolyse lecithin to release fatty acids � Bind calcium to form soft ‘brown’ pigment stones � Often form in bile ducts de novo
Risk factors for gallstone formation � Age ◦ Risk is x 4 between the ages of 40 -69 compared with younger subjects ◦ Due to increased cholesterol content in bile � Sex ◦ Higher prevalance in women, up to x 3 between ages of 30 -39 � Pregnancies / hormones ◦ Related to frequency and number of pregnancies ◦ New biliary sludge may form in up to 30% of women ◦ Oestrogens promote cholesterol hypersecretion in bile and reduce bile acid synthesis ◦ Progesterones promote stasis and impair contractility ◦ These changes reverse 1 -2 months after giving birth with resolution of sludge in up to 60% of cases
Risk factors for gallstone formation �Oral contraceptives and HRT ◦ As above ◦ Also found to apply to men receiving oestrogen therapy for prostate cancer, compared to those who elected for orchiectomy (small study) �Obesity ◦ Enhanced cholesterol synthesis and secretion
Risk factors for gallstone formation �Gallbladder ◦ ◦ ◦ stasis Fasting states Rapid weight loss TPN use / ICU admission Major trauma Somatostatin Due to excessive reabsorption of water with resultant cholesterol supersaturation �Rapid weight loss ◦ Increases bile calcium concentration ◦ Increases bile mucin concentration
Risk factors for gallstone formation �Cirrhosis ◦ ◦ Overall prevalance approaches 30% Higher incidence with Childs B and C disease High unconjugated bilirubin levels High circulating oestrogen levels (aromatase) �Impaired enterohepatic circulation ◦ Small bowel resection ◦ Crohn’s disease ◦ Reduced levels of bile acid content in bile, leading to poor cholesterol solubility
Risk factors for gallstone formation �Drugs ◦ Ceftriaxone (biliary excretion, forms a complex with calcium and precipitates) ◦ Clofibrate (impairs bile acid formation, leading to supersaturation) �Physical inactivity / sedentary lifestyle
Risk factors for gallstone formation �Increased bilirubin ◦ ◦ circulating unconjugated Haemolytic states Cirrhosis Hypersplenism High-turnover haematological disease �Genetic factors / ethnicity ◦ Pima Native Americans have incidence of up to 75% ◦ Chilean ◦ Mexican
Gallstone formation – in summary �Imbalance of bile content ◦ Cholesterol supersaturation ◦ Too much unconjugated bilirubin ◦ Inadequate bile salt content �Gall bladder stasis

Protective factors �Statins �Aspirin �Vitamin C (but only for women!) �Coffee (>3 cups per day), but decaffeinated coffee not protective �Diet rich in unsaturated fats (monoand poly-)
CLINICAL FEATURES

Presentation � Depends ◦ ◦ ◦ biliary colic cholecystitis choledocholithiasis cholangitis pancreatitis � Biliary ◦ ◦ ◦ on the site of gallstone impaction / obstruction colic RUQ pain nausea vomiting post-prandial usually unaffected by movement and lasts only for several hours
Presentation �Cholecystitis may present with all the above, plus ◦ Fever ◦ Positive Murphy’s sign ◦ Elevated WCC, CRP ◦ May be mild derangements in ALT/AST, but unusual to have elevated bilirubin or ALP in uncomplicated cholecystitis
Presentation �Cholangitis ◦ Charcot’s triad (pain, fever, jaundice) ◦ obstructive LFTs ◦ French neurologist (1825 -1893) ◦ ‘founder of modern neurology’ ◦ taught Sigmund Freud, Joseph Babinski, George Gilles de la Tourette among others
Presentation �Choledocholithiasis ◦ RUQ pain, nausea, vomiting ◦ traditionally believed that CBD does not produce colicky pain, as it has no smooth muscle ◦ however, may be associated with spasm of Sphincter of Oddi ◦ steatorrhoea ◦ pruritis
Acute cholecystitis �A syndrome encompassing acute inflammation of the gallbladder usually in association with RUQ pain, fever and leucocystosis �Usually �May due to gall stones be acalculous (up to 10%, usually in critically unwell patients)
Acute cholecystitis � Experimental animal models have shown either mechanical or chemical irritation of gall bladder mucosa is the inciting event in development of cholecystitis, in conjunction with cystic duct obstruction (which alone does not seem to be adequate) � Inflammatory and F 1α � Bacterial process mediated by prostaglandins E 2 infection of bile is not a pre-requisite ◦ Healthy control subjects generally have sterile bile on fluid culture ◦ In one study, up to 40% of patients with gallstones (but not necessarily cholecystitis) have positive bile cultures ◦ Similar rates of positive culture in those with acute cholecystitis ◦ E. coli, Klebsiella, Enterococcus, Enterobacter

Chronic cholecystitis �A term used to describe histopathological findings of chronic inflammatory cell infiltrate in the wall of the gallbladder, invariably in association with long-standing mechanical irritation from stones leading to thickening and fibrosis

Differential diagnoses �Biliary colic �Hepatitis �Choledocholithiasis �Cholangitis �Pancreatitis �Pyelonephritis �Right lower lobe pneumonia �Peptic ulcer disease �Colitis �Appendicitis �…
Imaging investigations �FBC �LFT ◦ Bilirubin (conjugated, unconjugated) ◦ 60% of patients with CBD stones will have derangement of at least one LFT ◦ However, elevation of LFTs does not necessarily imply CBD stones �Lipase / amylase
Investigations � US ◦ 85 -95% sensitivity, 99% specificity for detection of gallstones ◦ 88% sensitivity, 80% specificity for cholecystitis ◦ Wall oedema, pericholecystic fluid � CT ◦ Poor sensitivity as stones may be isodense to bile � HIDA / DISIDA ◦ Tc-labelled hepatic iminodiacetic acid (or di-isopropyl) ◦ IV injection, biliary excretion ◦ Positive if gallbladder, CBD, duodenum not visualised after 60 minutes ◦ 97% sensitivity, 90% specificity ◦ False positives: sphincterotomy, TPN, severe liver disease ◦ Modification with morphine administration to encourage Sof. O contraction
Imaging investigations �MRCP ◦ Less sensitive than US for detection of GB wall oedema ◦ More sensitive than US for detection of cystic duct and CBD stones (95%) �Oral cholecystography ◦ Largely abandoned in clinical practice ◦ Takes days to perform ◦ Relies on functional gallbladder to concentrate contrast medium

Complications �Emphysematous ◦ ◦ cholecystitis Clostridium welchii E. coli Klebsiella Pseudomonas �Gangrene (up to 20% if left untreated) �Perforation �Cholangitis (Charcot’s triad) �Pancreatitis �Mirizzi syndrome �Cholecystoenteric fistula / gallstone ileus
Mirizzi’s Syndrome � Extrahepatic cholelithiasis � Occurs � Type II obstruction in association with in around 1 in 200 ◦ Stone impacted in cystic duct causes direct pressure or oedema to CHD ◦ Will usually require conversion to open cholecystectomy ◦ Erosion of stone into CHD ◦ Will usually require hepatojejunostomy
Mirizzi �Pablo Luis Mirizzi (1893 -1964) �Cardoba, �Also Argentina introduced use of the intraoperative cholangiogram


TREATMENT
Treatment of asymptomatic gallstones �No evidence to support interventional treatment � 2% of incidentally-discovered gallstones become symptomatic per year
Treatment of symptomatic gallstones – non interventional �Acute ◦ Antibiotics (lower rates of wound infection but no difference re: development of GB empyema) ◦ Anti-inflammatories �Dissolution ◦ ◦ therapy Chenodeoxycholic acid Ursodeoxycholic acid (UDCA) Takes 6 -12 months to have benefit Requires smaller stones (larger surface area), radiolucency (lack of calcium matrix) ◦ High recurrence rate upon cessation of therapy (30% at 3 years)

Treatment of symptomatic gallstones – non interventional �Lithotripsy ◦ Similar technique to ESWL for renal stones ◦ Poorer results, however, ◦ Seldom used nowadays
Treatment - interventional �Cholecystectomy ◦ ◦ ◦ Open / mini-laparotomy Laparoscopic Needlescopic Single-incision NOTES (Subtotal) �Timing ◦ Higher rates of hospital re-presentation (38% -v 4%) for those managed conservatively and discharged without cholecystectomy
Treatment - interventional �Cholecystostomy ◦ Percutaneous ◦ Laparoscopic ◦ For high-risk patients with late presentation ◦ Too unwell to tolerate general anaesthetic or prolonged procedures ◦ May not necessarily obviate the need for surgery, e. g. mural gangrene
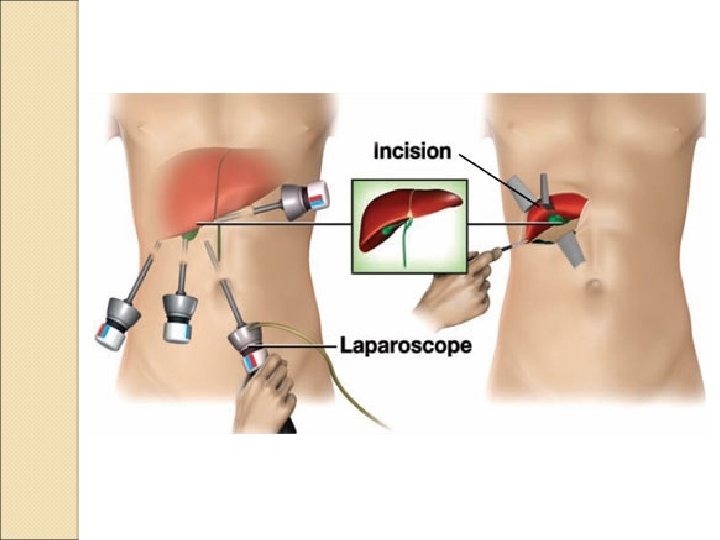
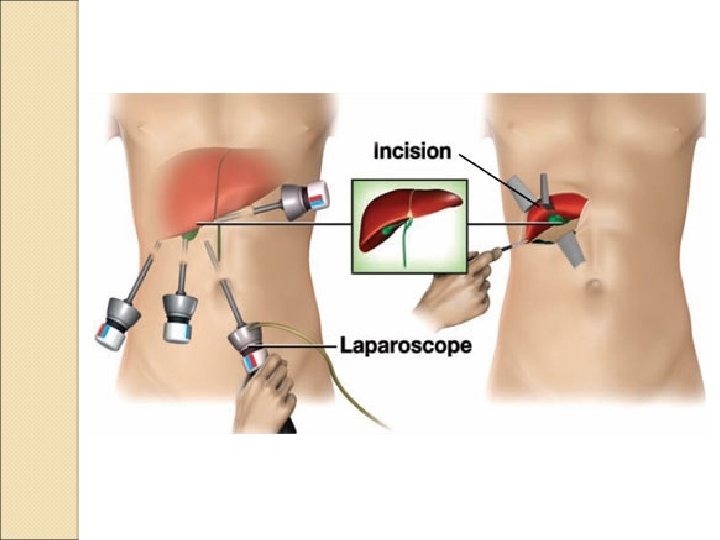
Laparoscopic cholecystectomy �Contraindications (relative) ◦ Haemodynamic compromise / unstable ◦ Significant upper abdominal surgery ◦ Anaesthetic concerns (pneumoperitoneum) �Positioning ◦ American (supine) ◦ French (lithotomy)
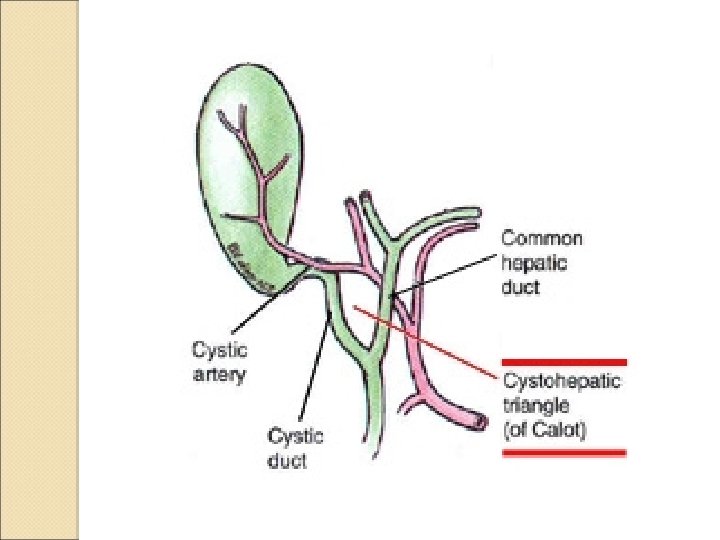
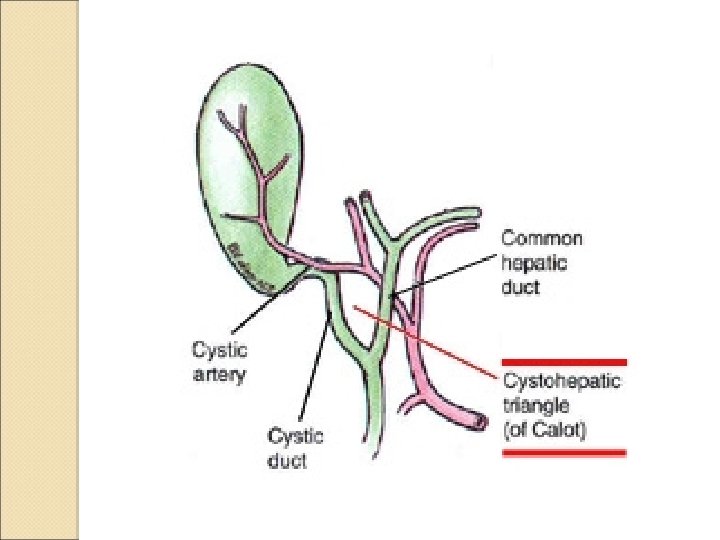
Critical view of safety �Described by Strasburg in 1995 �Mandates three conditions ◦ Calot’s triangle be cleared of fat and fibrous tissue ◦ Lower part of GB should be freed from cystic plate ◦ Two (and only two) structures should be seen to enter the GB �Beware anatomical variations ◦ Right hepatic artery mistaken for cystic a. ◦ Anomalous origins of cystic a. ◦ Anomalous ductal anatomy

Operative risks �Bleeding �Duodenal injury �Vascular injury / compromise �Bile leak / bile duct injury ◦ 0. 1% in open cholecystectomy ◦ 0. 3% in laparoscopic cholecystectomy ◦ Routine use of IOC conferred a protective effect against CBD injury
Intra-operative cholangiogram �A study of 1, 500, 000 cholecystectomies in WA found lower rates of CBD injury when IOC was performed (Fletcher et al. ) �Confirms anatomy of biliary tree prior to division of ducts (recoverable injury) �Also identifies residual CBD stones
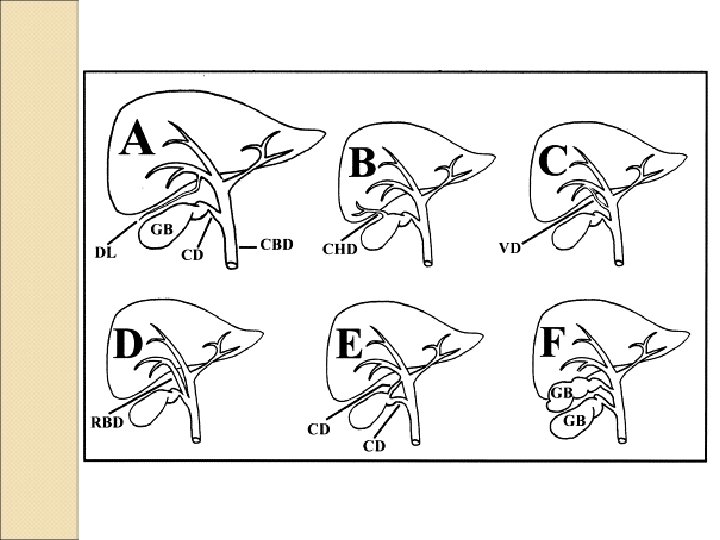
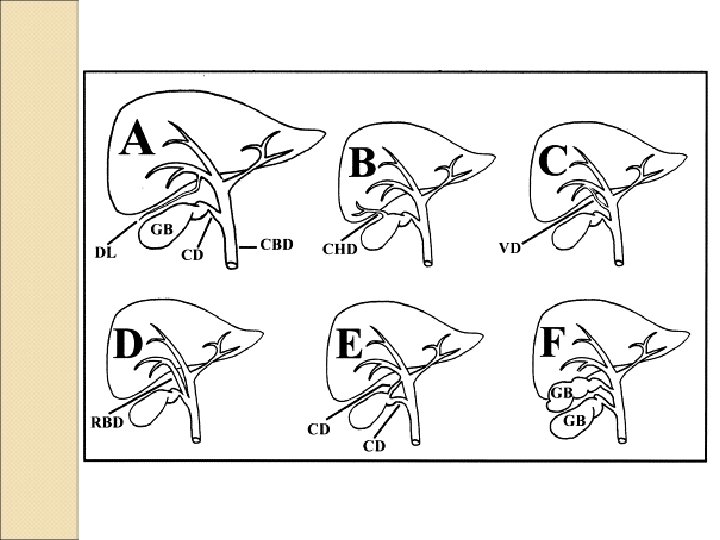
‘Typical’ bile duct injury �CBD is misidentified as the cystic duct and ligated / divided �Gall bladder is pulled to the right and the CHD is misidentified as an’ accessory’ cystic duct. Ligated and divided �Results in excision of most of the extrahepatic biliary tree

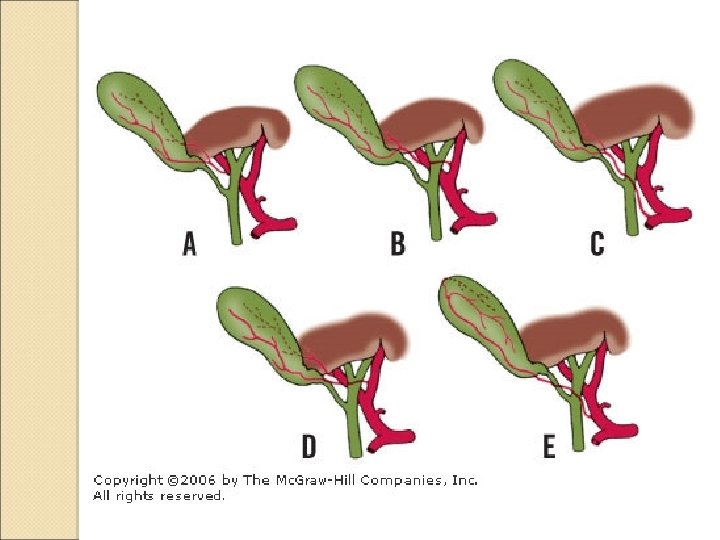
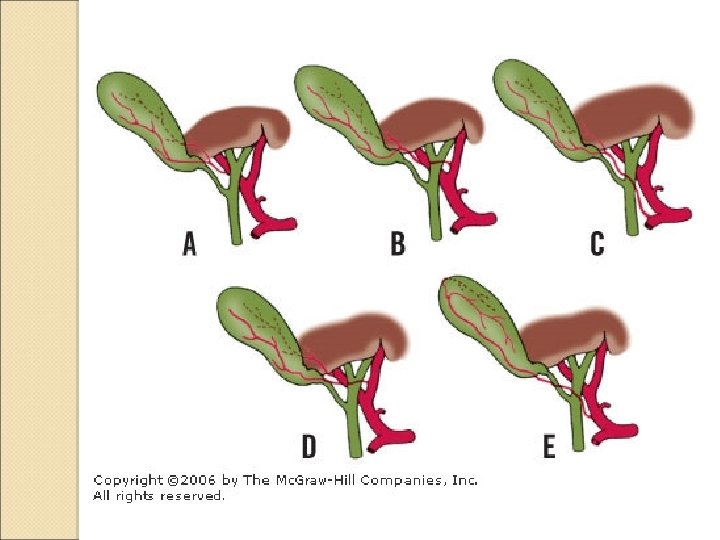
Other types of bile duct injury �Strasberg classification, from A to E ◦ A: cystic duct stump leak ◦ B: aberrant right hepatic duct occlusion ◦ C: aberrant right hepatic duct division without ligation ◦ D: lateral CBD injury ◦ E: related to the CHD confluence (further subdivided into 1 -5)


CBD stones found at operation � Approximately 12% � ERCP ◦ Post-operative ◦ Intra-operative � Transcystic time) CBD exploration (successful ~65% of the � Choledochotomy ◦ ◦ ◦ Laparoscopic or open Requires CBD to be >8 mm Often required if multiple large stones remain After failed transcystic exploration After failed ERCP (or not available)

CBD stones found at operation �Choledochotomy can be followed by either antegrade stent placement and primary closure, or T-tube insertion �Trans-duodenal stent allows post-operative biliary drainage and may facilitate subsequent ERCP �T-tube placement has the added advantage of providing access for further choledochoscopy without the need for reoperation ◦ Lower complication rate than ERCP ◦ However, ERCP becoming increasingly accessible and avoids morbidity of T-tube care
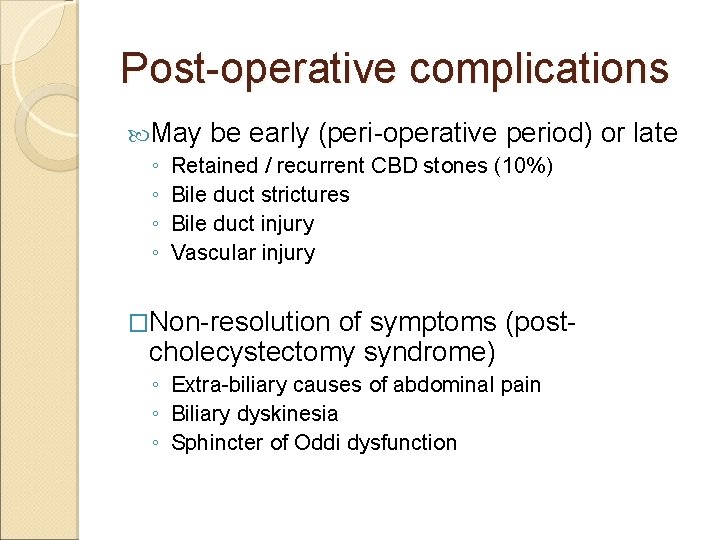
Post-operative complications May be early (peri-operative period) ◦ Retained / recurrent CBD stones (10%) ◦ Bile duct strictures ◦ Bile duct injury ◦ Vascular injury �Non-resolution of symptoms (postcholecystectomy syndrome) ◦ Extra-biliary causes of abdominal pain ◦ Biliary dyskinesia ◦ Sphincter of Oddi dysfunction or late
 Post cholecystectomy syndrome treatment
Post cholecystectomy syndrome treatment Biliary colic treatment
Biliary colic treatment Communicable disease and non communicable disease
Communicable disease and non communicable disease Oncocytoma salivary gland
Oncocytoma salivary gland Uremia pathogenesis
Uremia pathogenesis Cholecystitis
Cholecystitis Cholecystitis pathogenesis
Cholecystitis pathogenesis Bacterial pathogenesis
Bacterial pathogenesis Cholecystitis pathophysiology
Cholecystitis pathophysiology Bacterial pathogenesis
Bacterial pathogenesis Tetanus pathogenesis
Tetanus pathogenesis Jaundice pathogenesis
Jaundice pathogenesis Pathogenesis dengue fever
Pathogenesis dengue fever Rabies pathogenesis
Rabies pathogenesis Pathogenesis steps
Pathogenesis steps Pathogenesis game
Pathogenesis game Left parasternal heave
Left parasternal heave Cirrhosis pathogenesis
Cirrhosis pathogenesis Histoplasma capsulatum pathogenesis
Histoplasma capsulatum pathogenesis Nursing management of pyelonephritis
Nursing management of pyelonephritis Pathogenesis of hemolytic anemia
Pathogenesis of hemolytic anemia Mechanism of ischemic stroke
Mechanism of ischemic stroke Pathogenesis of tuberculosis
Pathogenesis of tuberculosis Wui san kwok
Wui san kwok Angela kwok
Angela kwok Jackie kwok
Jackie kwok Veronica kwok
Veronica kwok Christine mascolo harvard
Christine mascolo harvard Disguises by jean fong kwok
Disguises by jean fong kwok Nathan kwok
Nathan kwok Disguises by jean fong kwok
Disguises by jean fong kwok Hwu webmail
Hwu webmail Kwok wing tsoi
Kwok wing tsoi -is not one of the purposes for giving oral presentations.
-is not one of the purposes for giving oral presentations. Best and worst powerpoint presentations
Best and worst powerpoint presentations Worst powerpoint slides
Worst powerpoint slides Craft of scientific presentations
Craft of scientific presentations Titles for mental health presentations
Titles for mental health presentations Advantages of multimedia presentation
Advantages of multimedia presentation Slidetodoc
Slidetodoc Ventajas y desventajas de corel presentations
Ventajas y desventajas de corel presentations What is verbal support
What is verbal support Tok presentations
Tok presentations Anna ritchie allan
Anna ritchie allan Ria seminar system
Ria seminar system Boardworks ltd
Boardworks ltd Scqa pyramid principle
Scqa pyramid principle Internet presentations
Internet presentations The most dangerous game ppt
The most dangerous game ppt Note card for presentation
Note card for presentation The end pictures for presentations
The end pictures for presentations Useful phrases for presentations
Useful phrases for presentations Efficient elements powerpoint
Efficient elements powerpoint You exec
You exec Research project title
Research project title Catchy titles for presentations
Catchy titles for presentations Electricity merit badge powerpoint
Electricity merit badge powerpoint Customer service presentations
Customer service presentations Cisco 3750 stacking
Cisco 3750 stacking