Fungi Systemic Mycoses Alfred Lewin References http www
- Slides: 34
Fungi & Systemic Mycoses Alfred Lewin References http: //www. doctorfungus. org/ Schaechter et al. Mechanisms of Microbial Disease Kobayashi et al. Medical Microbiology
Pizza Mushrooms • • Domain Eukarya Kingdom Fungi Phylum Basidiomycota Class Hymenomycetes Order Agricales Family Agricaceae Genus Agricarus Species bisporus
Characteristics of fungi A. eukaryotic, non- vascular organisms B. reproduce by means of spores, usually wind-disseminated C. both sexual (meiotic) and asexual (mitotic) spores may be produced, depending on the species and conditions D. typically not motile, although a few (e. g. Chytrids) have a motile phase. E. like plants, fungi have an alternation of generations
More Characteristics of Fungi F. vegetative body may be unicellular (yeasts) or composed of microscopic threads called hyphae G. cell walls similar in structure to plants’ but differ in chemical composition-fungi cell walls are composed of mostly of chitin-plant cell walls are composed mostly of cellulose (plus lignin in secondary walls) H. cytoplasmic ultrastructure broadly similar to plants cells, but differ significantly in kinds of organelles and their structures.
Even more fungal facts I. fungi are heterotrophic ( “other feeding, ” must feed on preformed organic material), not autotrophic ( “self feeding, ” make their own food by photosynthesis). - Unlike animals (also heterotrophic), which ingest then digest, fungi digest then ingest. -Fungi produce exoenzymes to accomplish this. J. Most fungi store their food as glycogen (like animals). Plants store food as starch
Final Fun Facts on Fungi K. Fungal cell membranes have a unique sterol, ergosterol, which replaces cholesterol found in mammalian cell membranes L. Tubule protein—production of a different type in microtubules formed during nuclear division. M. Chitin biosynthesis occurs in fungi. N. Most fungi have very small nuclei, with little repetitive DNA. O. Mitosis is generally accomplished without dissolution of the nuclear envelope.
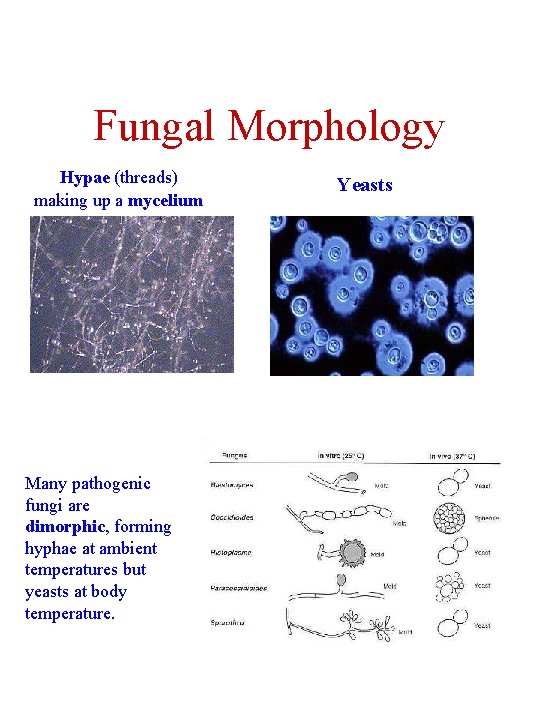
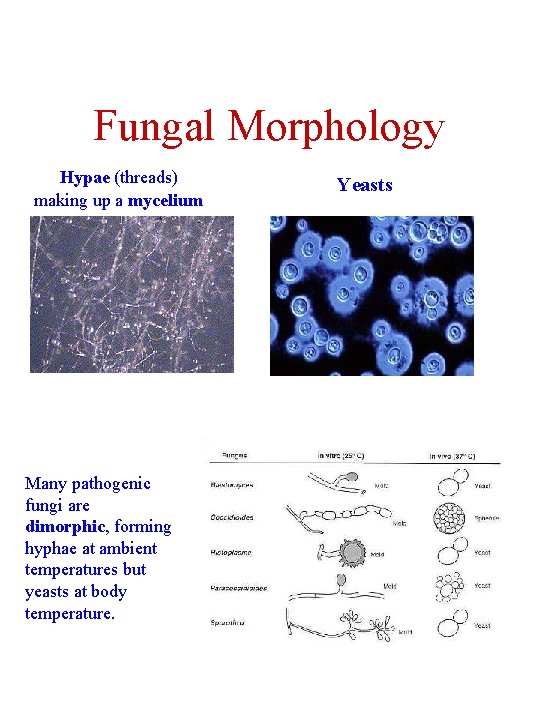
Fungal Morphology Hypae (threads) making up a mycelium Many pathogenic fungi are dimorphic, forming hyphae at ambient temperatures but yeasts at body temperature. Yeasts
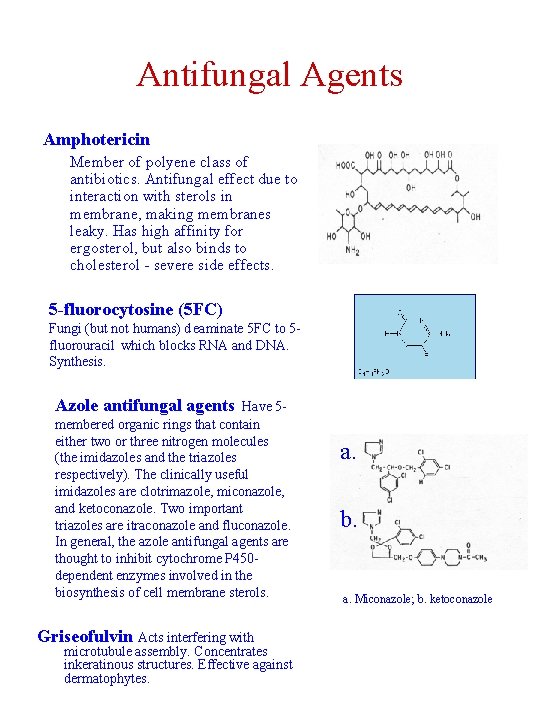
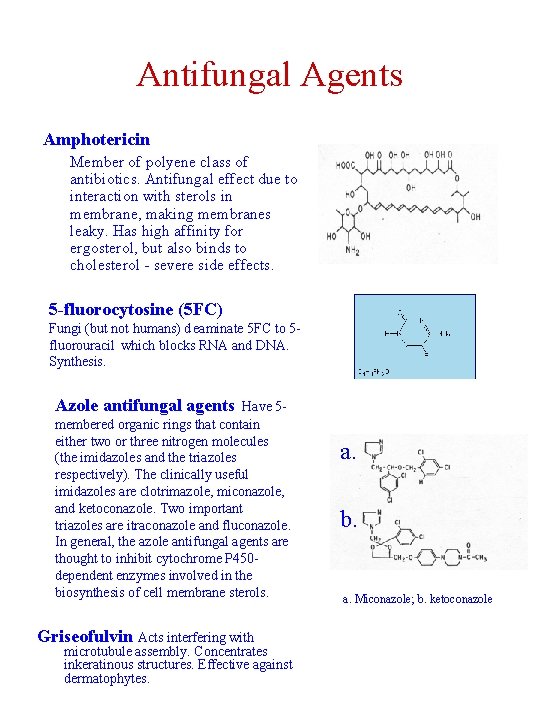
Antifungal Agents Amphotericin Member of polyene class of antibiotics. Antifungal effect due to interaction with sterols in membrane, making membranes leaky. Has high affinity for ergosterol, but also binds to cholesterol - severe side effects. 5 -fluorocytosine (5 FC) Fungi (but not humans) d eaminate 5 FC to 5 fluorouracil which blocks RNA and DNA. Synthesis. Azole antifungal agents Have 5 membered organic rings that contain either two or three nitrogen molecules (the imidazoles and the triazoles respectively). The clinically useful imidazoles are clotrimazole, miconazole, and ketoconazole. Two important triazoles are itraconazole and fluconazole. In general, the azole antifungal agents are thought to inhibit cytochrome P 450 dependent enzymes involved in the biosynthesis of cell membrane sterols. Griseofulvin Acts interfering with microtubule assembly. Concentrates inkeratinous structures. Effective against dermatophytes. a. b. a. Miconazole; b. ketoconazole
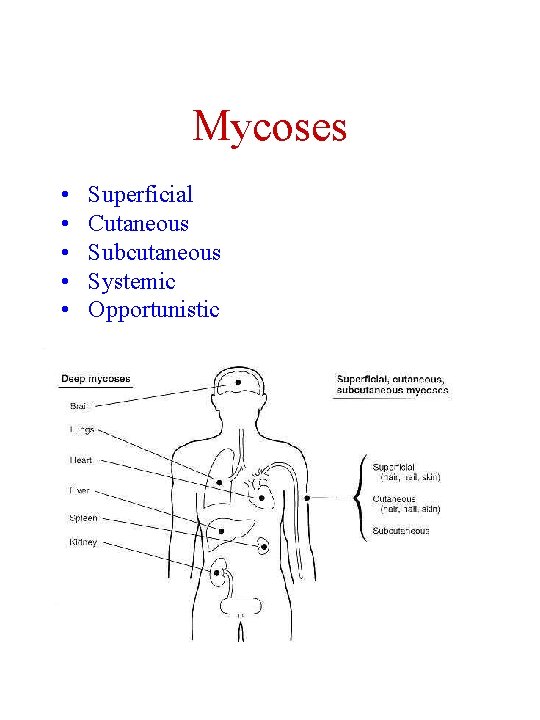
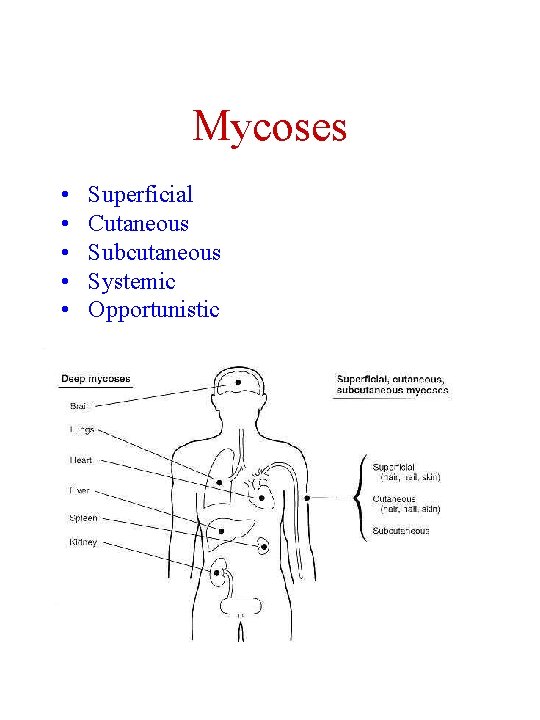
Mycoses • • • Superficial Cutaneous Subcutaneous Systemic Opportunistic
Superficial Mycoses • Pityriasis versicolor--pigmented lesions on torso • Tinea nigra--gray to black macular lesions often on palms • Black piedra--dark gritty deposits on hair • White piedra--soft whitish granules along hair shaft • All are diagnosed by microscopy and are easily treated by topical preparations.
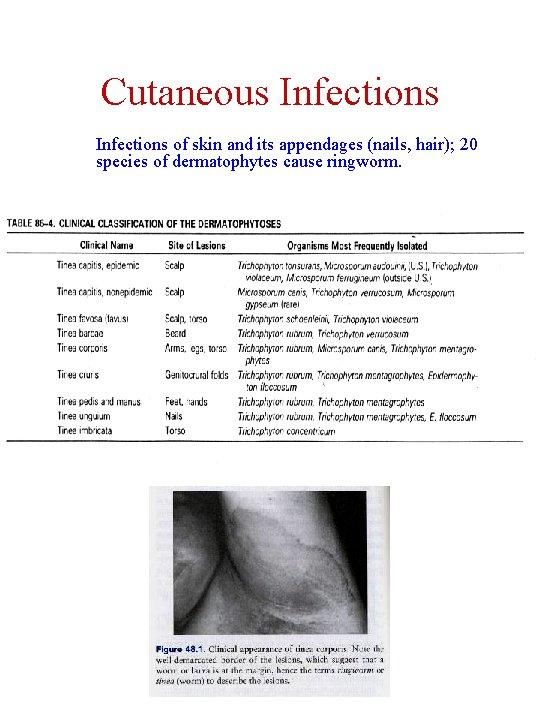
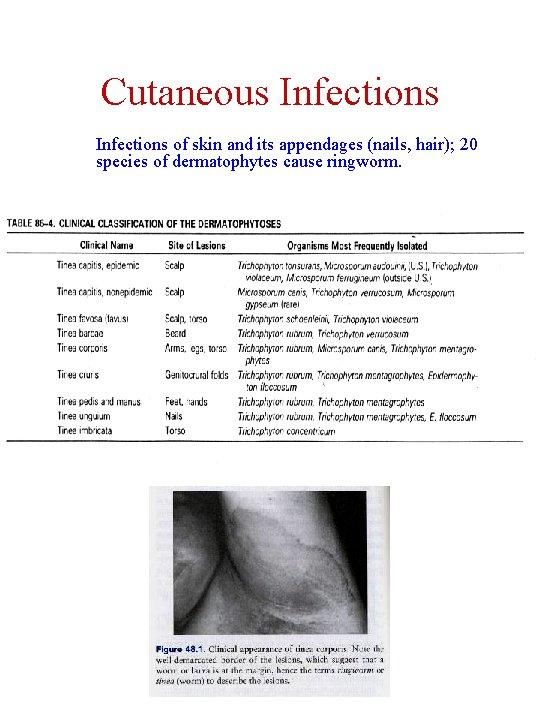
Cutaneous Infections of skin and its appendages (nails, hair); 20 species of dermatophytes cause ringworm.
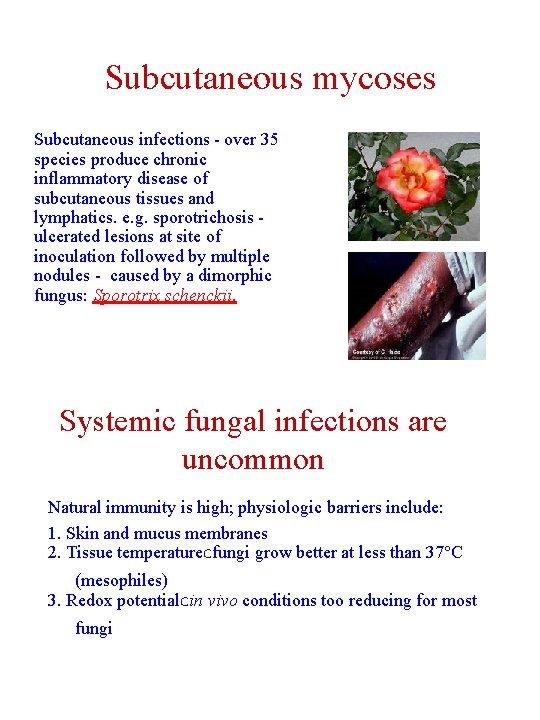
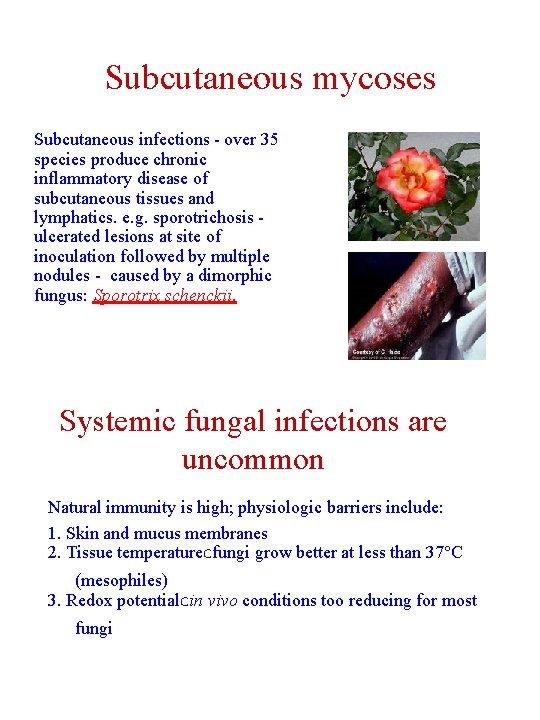
Subcutaneous mycoses Subcutaneous infections - over 35 species produce chronic inflammatory disease of subcutaneous tissues and lymphatics. e. g. sporotrichosis - ulcerated lesions at site of inoculation followed by multiple nodules - caused by a dimorphic fungus: Sporotrix schenckii. Systemic fungal infections are uncommon Natural immunity is high; physiologic barriers include: 1. Skin and mucus membranes 2. Tissue temperature. Cfungi grow better at less than 37°C (mesophiles) 3. Redox potential. Cin vivo conditions too reducing for most fungi
Infection requires a large inoculum and is affected by the resistance of the host • infection often occurs in endemic areas • • most infections are asymptomatic or self-limiting in immune-compromised hosts, infections are more often fatal (distinction between infection and disease) Systemic fungal disease is most often associated with three organisms (in U. S. ) 1. Coccidioides immitis 2. Histoplasma capsulatum 3. Blastomyces dermatitidis Normally found in soil, these organisms infect via inhilation.
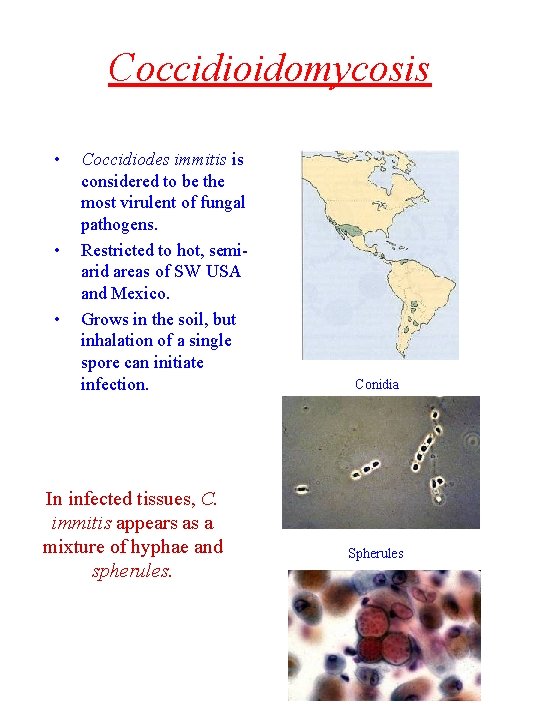
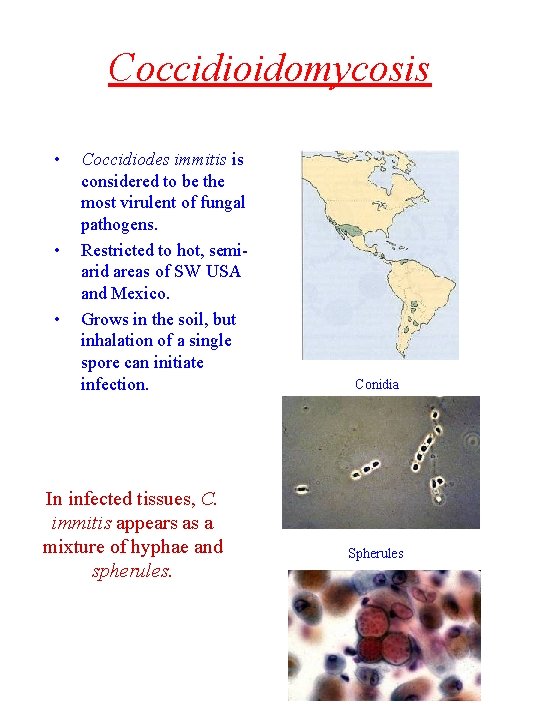
Coccidioidomycosis • • • Coccidiodes immitis is considered to be the most virulent of fungal pathogens. Restricted to hot, semiarid areas of SW USA and Mexico. Grows in the soil, but inhalation of a single spore can initiate infection. In infected tissues, C. immitis appears as a mixture of hyphae and spherules. Conidia Spherules
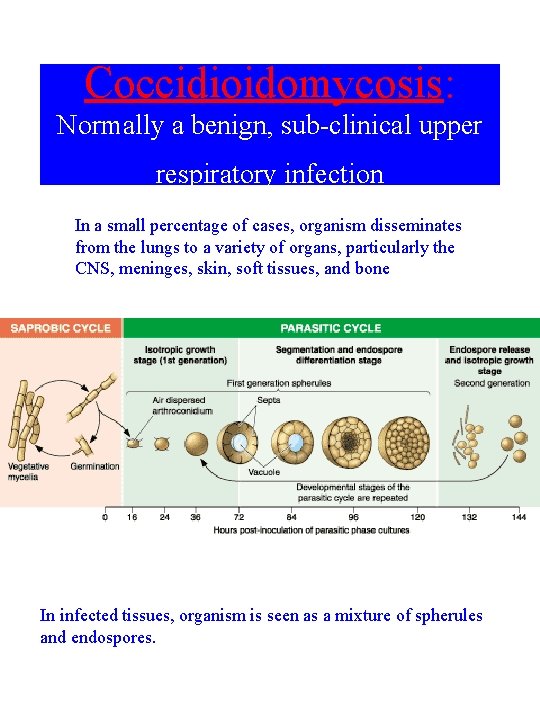
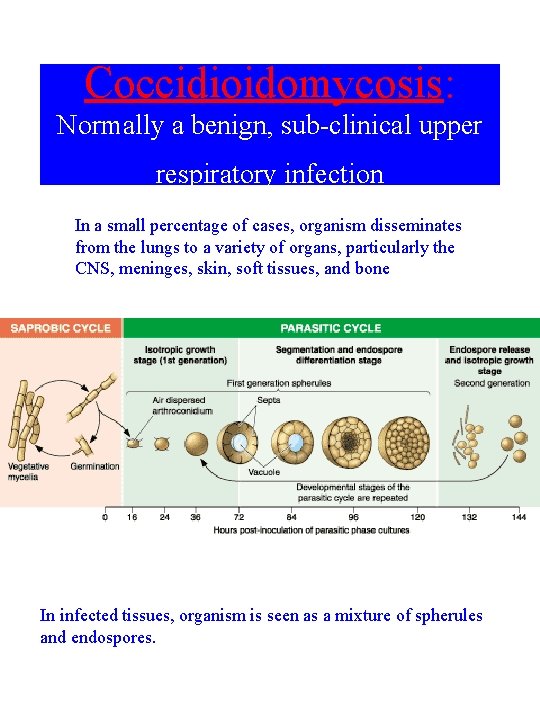
Coccidioidomycosis: Normally a benign, sub-clinical upper respiratory infection In a small percentage of cases, organism disseminates from the lungs to a variety of organs, particularly the CNS, meninges, skin, soft tissues, and bone In infected tissues, organism is seen as a mixture of spherules and endospores.
Risk factors for disseminated coccidioidomycosis 1. Race: Filipinos > African American> Caucasian 2. Age: Extremes more susceptible 3. Sex: Males more susceptible 4. Pregnancy 5. Immunosuppression Diagnosis 1. 2. 3. 4. Suppurative or granulatomas inflammation Spherule or endospores seen on pathology Culture of microorganisms Complement fixation assay (in cerebrospinal fluid) Treatment Amphotericin B, Fluconazole
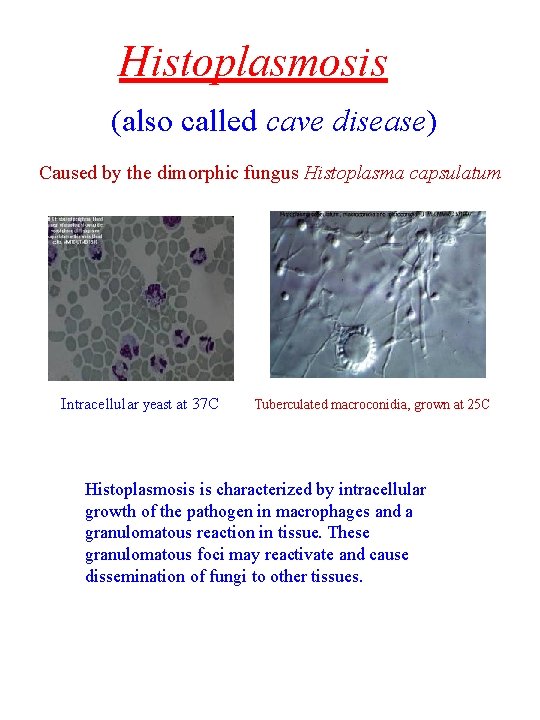
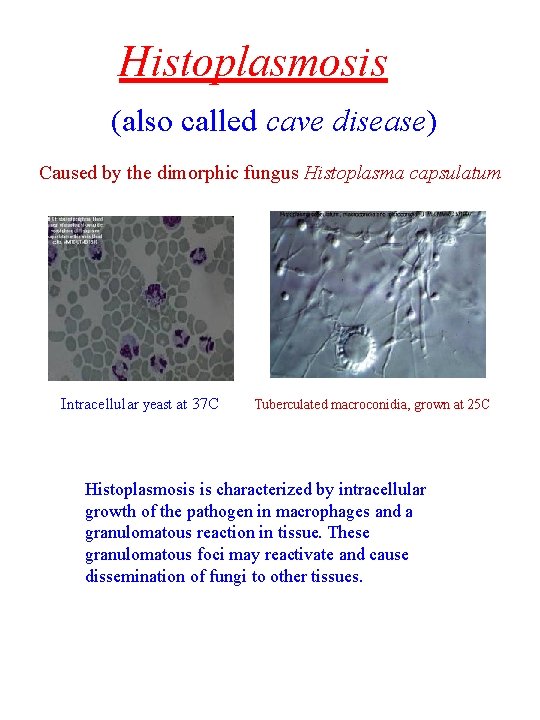
Histoplasmosis (also called cave disease) Caused by the dimorphic fungus Histoplasma capsulatum Intracellular yeast at 37 C Tuberculated macroconidia, grown at 25 C Histoplasmosis is characterized by intracellular growth of the pathogen in macrophages and a granulomatous reaction in tissue. These granulomatous foci may reactivate and cause dissemination of fungi to other tissues.
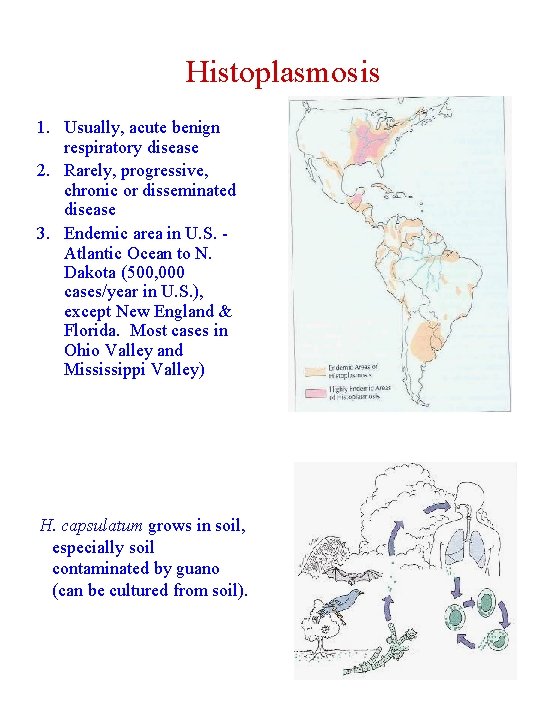
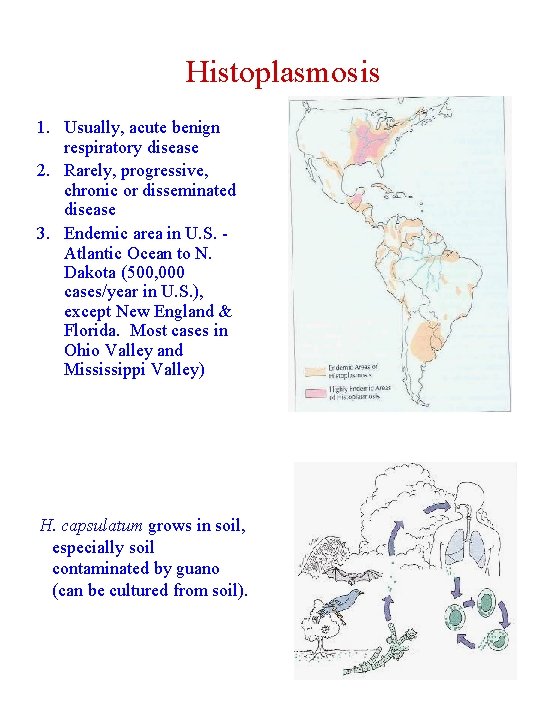
Histoplasmosis 1. Usually, acute benign respiratory disease 2. Rarely, progressive, chronic or disseminated disease 3. Endemic area in U. S. Atlantic Ocean to N. Dakota (500, 000 cases/year in U. S. ), except New England & Florida. Most cases in Ohio Valley and Mississippi Valley) H. capsulatum grows in soil, especially soil contaminated by guano (can be cultured from soil).
More Histoplasmosis 90% of histoplasmosis cases are clinically insignificant 1. Disseminated histoplasmosis is diagnosed frequently in patients with AIDS living in the central U. S. 2. It is often the initial manifestation of immunodeficiency. 3. In these cases, the organism spreads via blood from the lung to involve bone marrow, liver, spleen, or skin (see calcified granulomas). 4. Spread can also be associated with underlying lung disease (e. g. , emphysema). Diagnosis • Histology and culture • Skin test for histoplasmin [the major hyphal antigen] is not useful, because most people are positive in endemic area. • In HIV-infected patients with disseminated histoplasmosis, histo. antigen detection in serum and urine is at least 50%, and 90% sensitive, respectively.
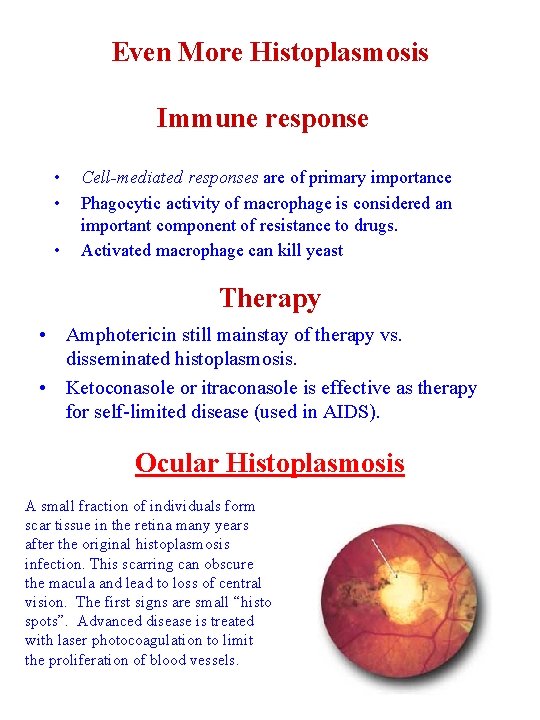
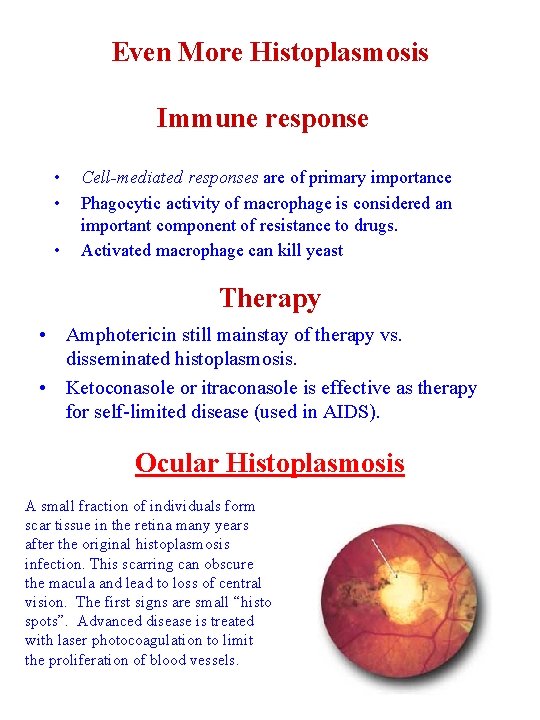
Even More Histoplasmosis Immune response • • • Cell-mediated responses are of primary importance Phagocytic activity of macrophage is considered an important component of resistance to drugs. Activated macrophage can kill yeast Therapy • Amphotericin still mainstay of therapy vs. disseminated histoplasmosis. • Ketoconasole or itraconasole is effective as therapy for self-limited disease (used in AIDS). Ocular Histoplasmosis A small fraction of individuals form scar tissue in the retina many years after the original histoplasmosis infection. This scarring can obscure the macula and lead to loss of central vision. The first signs are small “histo spots”. Advanced disease is treated with laser photocoagulation to limit the proliferation of blood vessels.
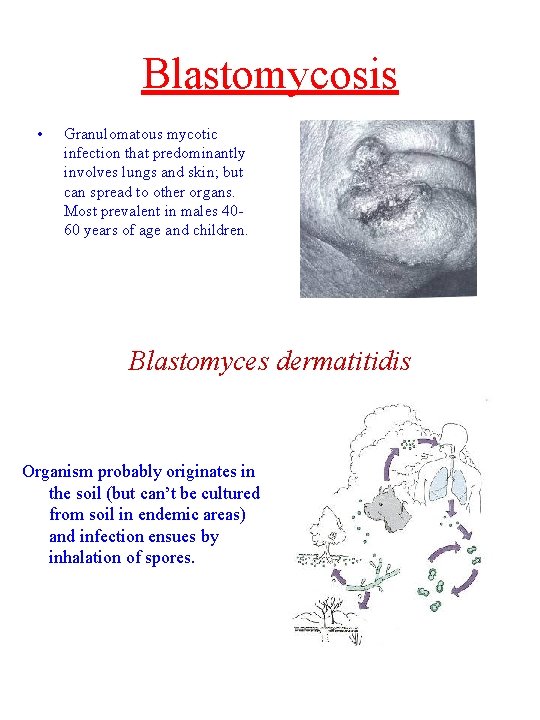
Blastomycosis • Granulomatous mycotic infection that predominantly involves lungs and skin; but can spread to other organs. Most prevalent in males 4060 years of age and children. Blastomyces dermatitidis Organism probably originates in the soil (but can’t be cultured from soil in endemic areas) and infection ensues by inhalation of spores.
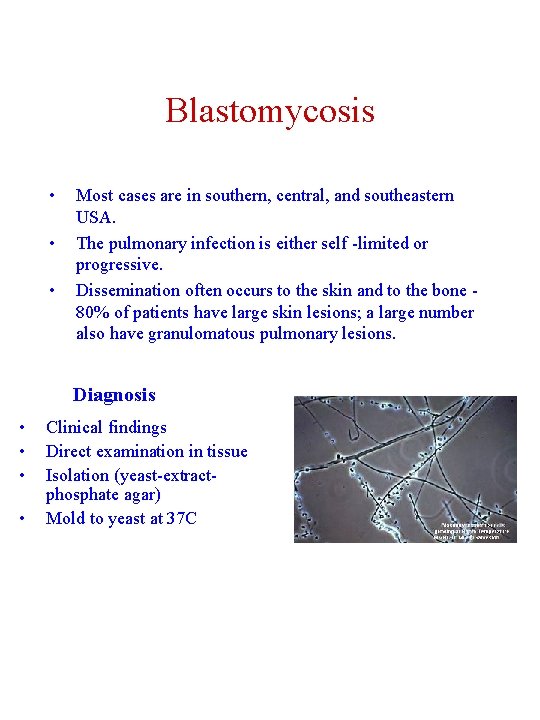
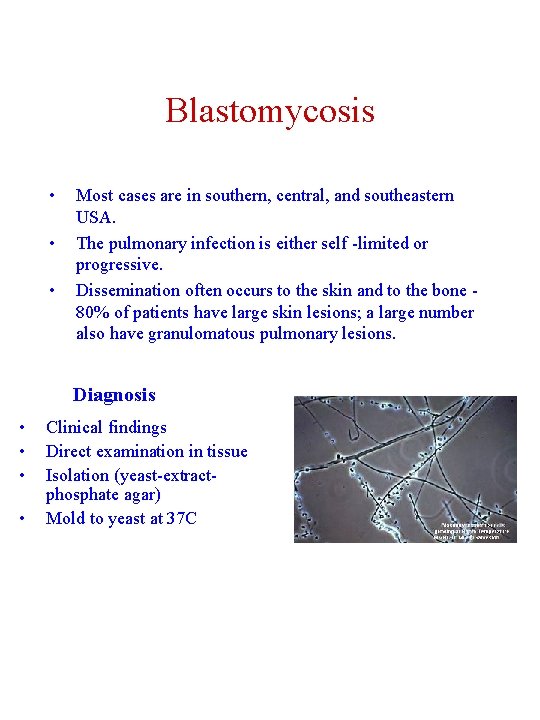
Blastomycosis • • • Most cases are in southern, central, and southeastern USA. The pulmonary infection is either self -limited or progressive. Dissemination often occurs to the skin and to the bone - 80% of patients have large skin lesions; a large number also have granulomatous pulmonary lesions. Diagnosis • • Clinical findings Direct examination in tissue Isolation (yeast-extractphosphate agar) Mold to yeast at 37 C
Therapy • Amphotericin B is the drug of choice for rapidly progressive blastomycosis • Ketoconazole for less severe cases Immune response 1. Alveolar macrophage provide a modest first line of defense. 2. PMNs (stimulated) also kill Blastomyces cells (by oxidative mechanisms). 3. Conidia are more sensitive to killing by PMNs because yeast are too big. 4. Cell-mediated immunity of great importance
Opportunistic Mycoses Opportunistic mycoses are fungal infections that do not normally cause disease in healthy people, but do cause disease in people with weakened immune defenses (immunocompromised people). Weakened immune function may occur due to inherited immunodeficiency diseases, drugs that suppress the immune system (cancer chemotherapy, corticosteroids, drugs to prevent organ transplant rejection), radiation therapy, infections (e. g. , HIV), cancer, diabetes, advanced age and malnutrition. The most common infections are: Candidiasis Aspergillosis Cryptococcosis Zygomycosis Pneumocystis carinii
Cryptococcus neoformans • Primary infection in lungs • Cryptococcal meningitis is most common disseminated manifestation • Can spread to skin, bone and prostate Organism is ubiquitous and infections occur worldwide C. neoformans recovered in large amounts in pigeon poop Does not cause disease in birds
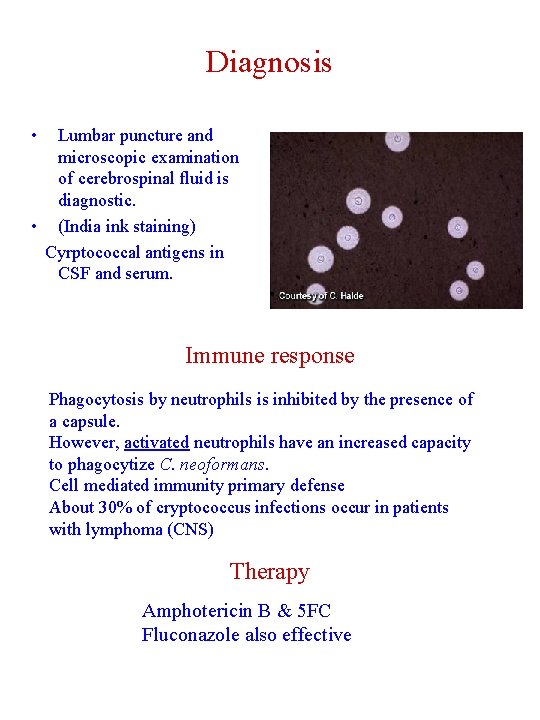
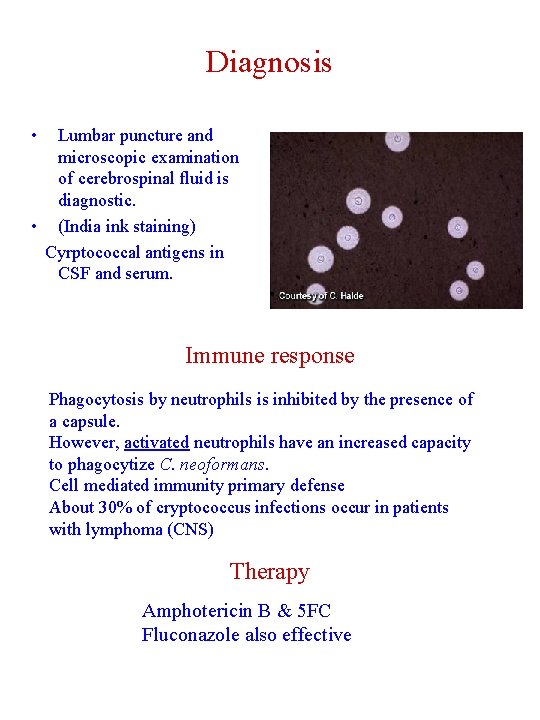
Diagnosis • Lumbar puncture and microscopic examination of cerebrospinal fluid is diagnostic. • (India ink staining) Cyrptococcal antigens in CSF and serum. Immune response Phagocytosis by neutrophils is inhibited by the presence of a capsule. However, activated neutrophils have an increased capacity to phagocytize C. neoformans. Cell mediated immunity primary defense About 30% of cryptococcus infections occur in patients with lymphoma (CNS) Therapy Amphotericin B & 5 FC Fluconazole also effective
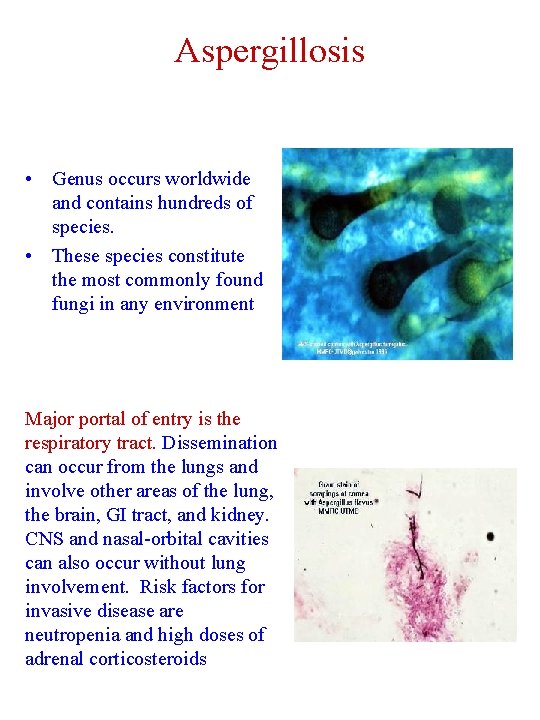
Aspergillosis • Genus occurs worldwide and contains hundreds of species. • These species constitute the most commonly found fungi in any environment Major portal of entry is the respiratory tract. Dissemination can occur from the lungs and involve other areas of the lung, the brain, GI tract, and kidney. CNS and nasal-orbital cavities can also occur without lung involvement. Risk factors for invasive disease are neutropenia and high doses of adrenal corticosteroids
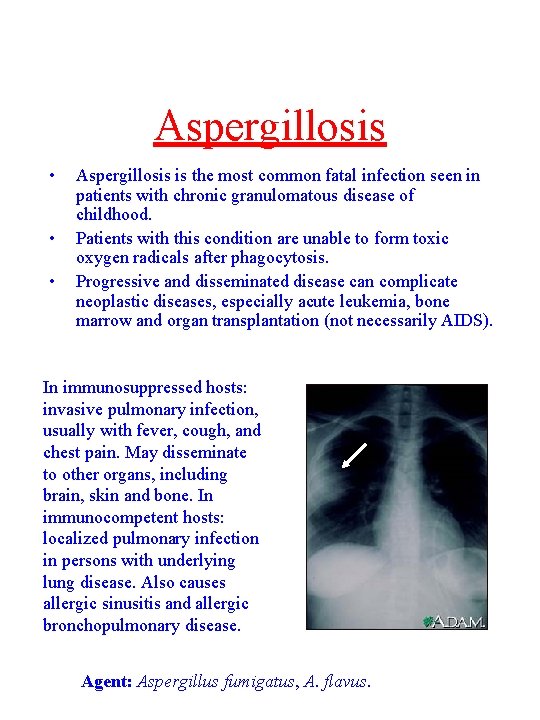
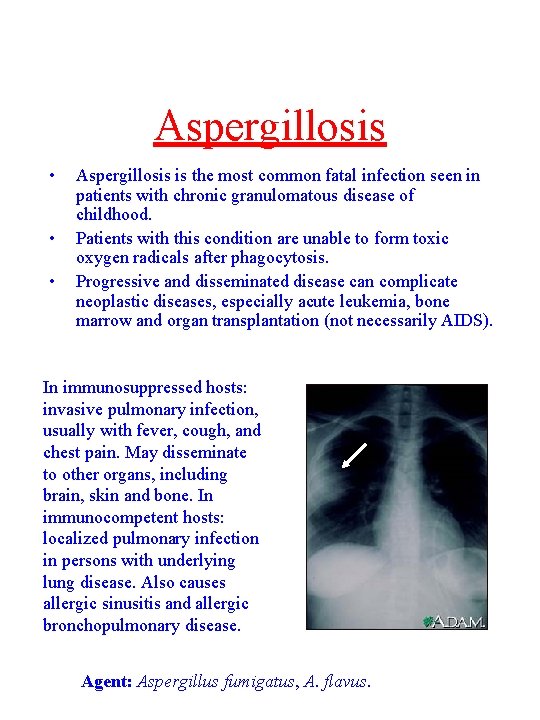
Aspergillosis • • • Aspergillosis is the most common fatal infection seen in patients with chronic granulomatous disease of childhood. Patients with this condition are unable to form toxic oxygen radicals after phagocytosis. Progressive and disseminated disease can complicate neoplastic diseases, especially acute leukemia, bone marrow and organ transplantation (not necessarily AIDS). In immunosuppressed hosts: invasive pulmonary infection, usually with fever, cough, and chest pain. May disseminate to other organs, including brain, skin and bone. In immunocompetent hosts: localized pulmonary infection in persons with underlying lung disease. Also causes allergic sinusitis and allergic bronchopulmonary disease. Agent: Aspergillus fumigatus, A. flavus.
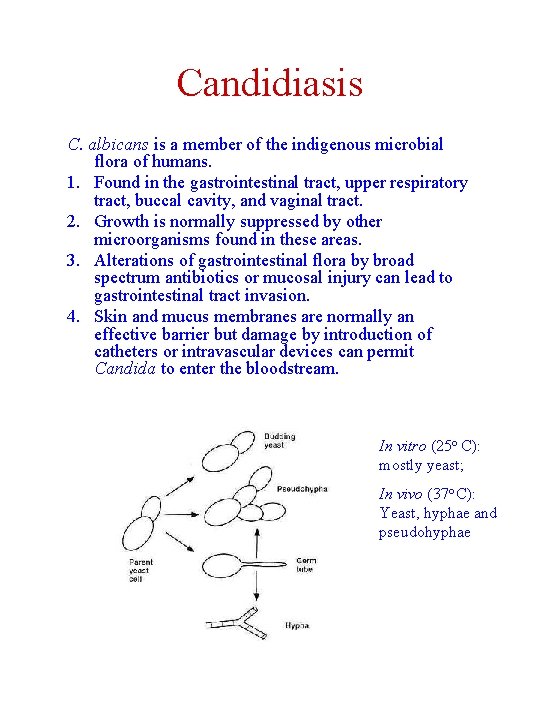
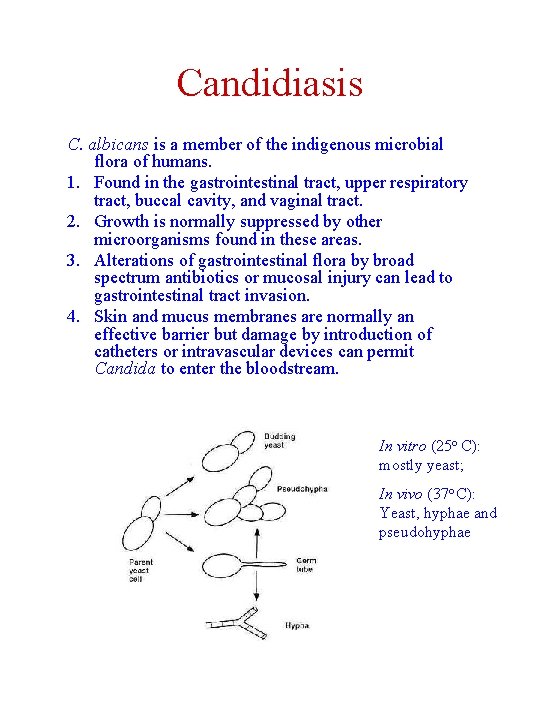
Candidiasis C. albicans is a member of the indigenous microbial flora of humans. 1. Found in the gastrointestinal tract, upper respiratory tract, buccal cavity, and vaginal tract. 2. Growth is normally suppressed by other microorganisms found in these areas. 3. Alterations of gastrointestinal flora by broad spectrum antibiotics or mucosal injury can lead to gastrointestinal tract invasion. 4. Skin and mucus membranes are normally an effective barrier but damage by introduction of catheters or intravascular devices can permit Candida to enter the bloodstream. In vitro (25 o C): mostly yeast; In vivo (37 o C): Yeast, hyphae and pseudohyphae
Candidiasis Vaginal candidiasis is the most common clinical infection. Local factors such as p. H and glucose concentration (under hormonal control) are of prime importance in the occurrence of vaginal candidiasis. In mouth: normal saliva reduces adhesion (lactoferrin is also protective). Immune Response Hyphae are too big for phagocytosis but are damaged by PMNs and by extracellular mechanisms (myeloperoxidase and b- glucuronidase). Cytokine activated lymphocytes can inhibit growth of C. albicans. Resistance to invasive infection by Candida is mediated by phagocytes, complement and antibody, though cell-mediated immunity plays a major role. Patients with defects in phagocytosis function and myeloperoxidase deficiency are at risk for disseminated (even fatal) Candidiasis.
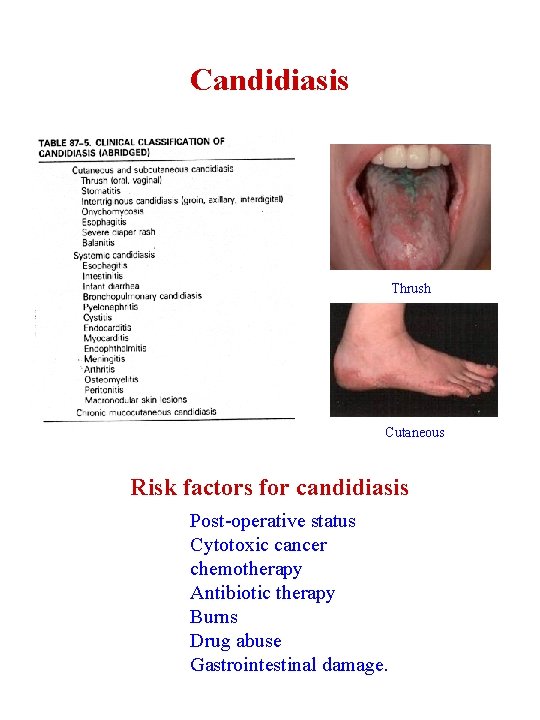
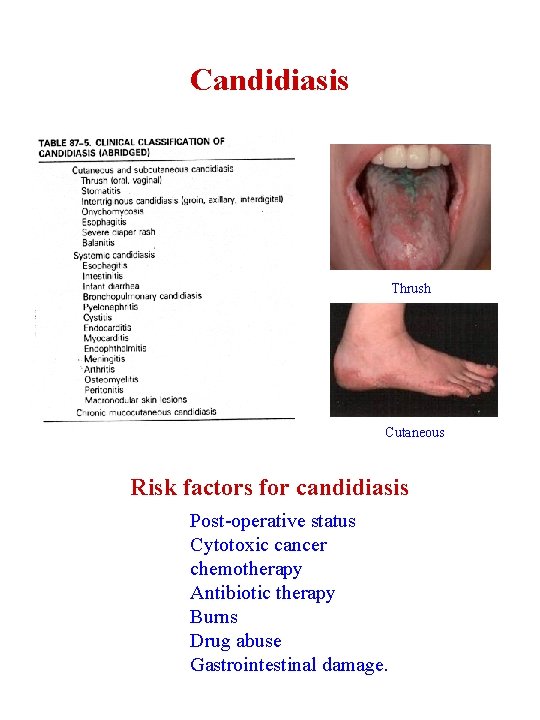
Candidiasis Thrush Cutaneous Risk factors for candidiasis Post-operative status Cytotoxic cancer chemotherapy Antibiotic therapy Burns Drug abuse Gastrointestinal damage.
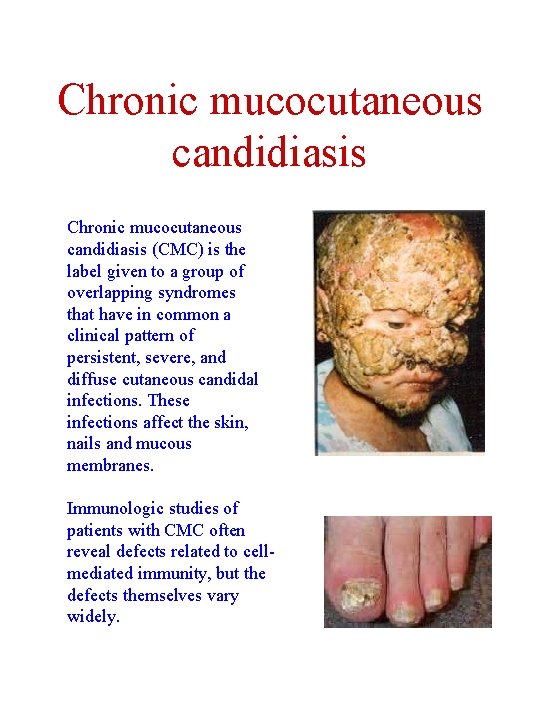
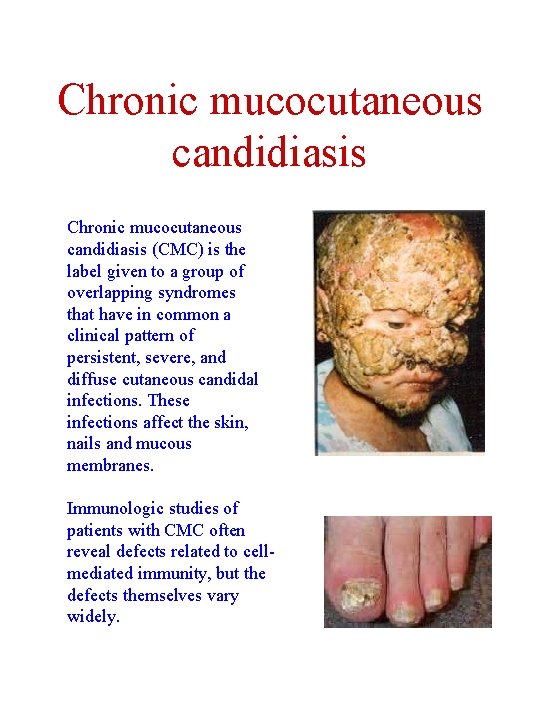
Chronic mucocutaneous candidiasis (CMC) is the label given to a group of overlapping syndromes that have in common a clinical pattern of persistent, severe, and diffuse cutaneous candidal infections. These infections affect the skin, nails and mucous membranes. Immunologic studies of patients with CMC often reveal defects related to cellmediated immunity, but the defects themselves vary widely.
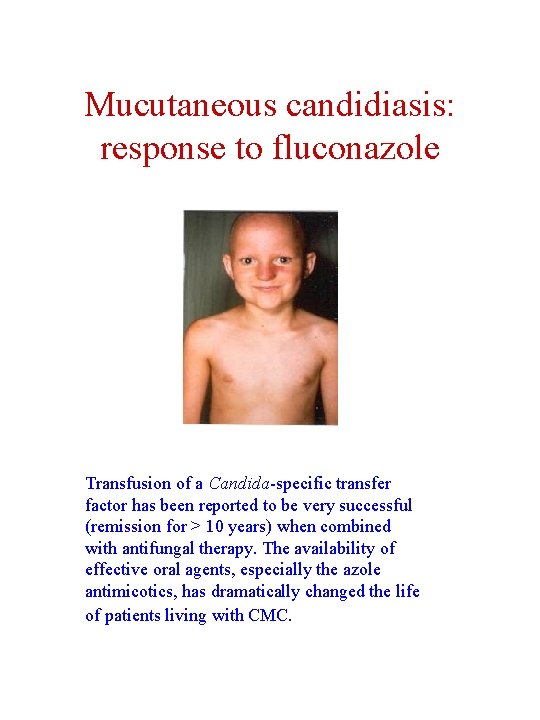
Mucutaneous candidiasis: response to fluconazole Transfusion of a Candida-specific transfer factor has been reported to be very successful (remission for > 10 years) when combined with antifungal therapy. The availability of effective oral agents, especially the azole antimicotics, has dramatically changed the life of patients living with CMC.
Environmental species kill neutropenic patients. • Zygomycosis due to Rhizopus, Rhizomucor, Absidia, Mucor species, or other members of the class of Zygomycetes, also causes invasive sinopulmonary infections. An especially life-threatening form of zygomycosis (also known as mucormycosis), is known as the rhinocerebral syndrome, which occurs in diabetics with ketoacidosis. In addition to diabetic ketoacidosis, neutropenia and corticosteroids are other major risk factors for zygomycosis. • Phaeohyphomycosis is an infection by brown to black pigmented fungi of the cutaneous, superficial, and deep tissues, especially brain. These infections are uncommon, life-threatening, and occur in various immunocompromised states. • Hyalohyphomycosis is an opportunistic fungal infection caused by any of a variety of normally saprophytic fungi with hyaline hyphal elements. For example, Fusarium spp. infect neutropenic patients to cause pneumonia, fungemia, and disseminated infection with cutaneous lesions.