Fundamentals of Anatomy Physiology Eleventh Edition Chapter 5

















- Slides: 90
Fundamentals of Anatomy & Physiology Eleventh Edition Chapter 5 The Integumentary System Lecture Presentation by Deborah A. Hutchinson Seattle University © 2018 Pearson Education, Inc.

Learning Outcomes 5 -1 Describe the main structural features of the epidermis, and explain the functional significance of each. 5 -2 Describe the structures and functions of the dermis. 5 -3 Describe the structures and functions of the subcutaneous layer. 5 -4 Explain what accounts for individual differences in skin color, and discuss the response of melanocytes to sunlight exposure. 5 -5 Describe the interaction between sunlight and vitamin D 3 production. 5 -6 Describe the mechanisms that produce hair, and explain the structural basis for hair texture and color. 2 © 2018 Pearson Education, Inc.
Learning Outcomes 5 -7 Discuss the various kinds of glands in the skin, and list the secretions of those glands. 5 -8 Describe the anatomical structures of nails, and explain how they are formed. 5 -9 Explain how the skin responds to injury and repairs itself. 5 -10 Summarize the effects of aging on the skin. 3 © 2018 Pearson Education, Inc.
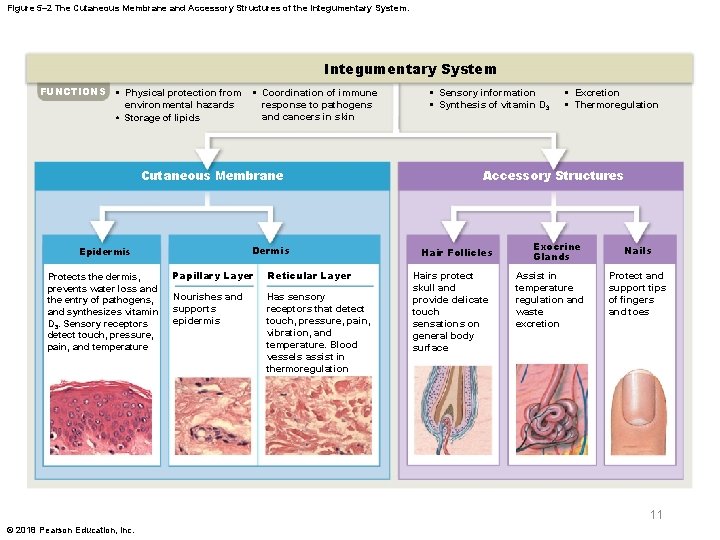
The Integumentary System § Integumentary system (integument) – Largest system of the body • Sixteen percent of body weight • 1. 5 to 2 m 2 of surface area • Two major parts – Cutaneous membrane (skin) – Accessory structures 4 © 2018 Pearson Education, Inc.
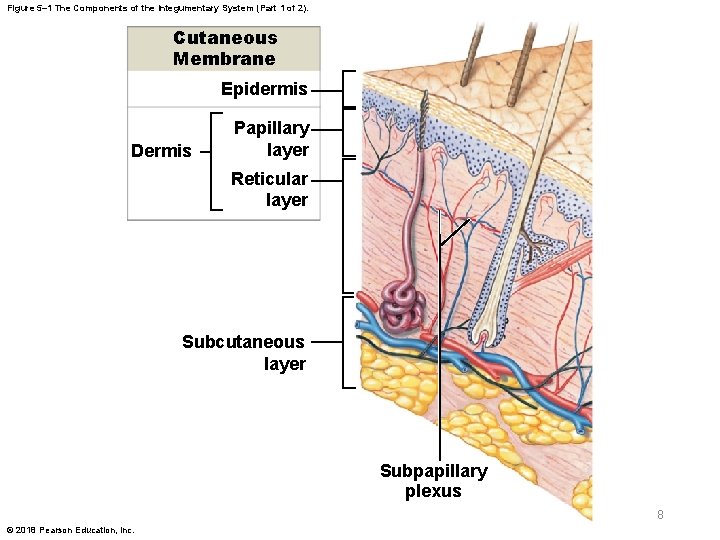
The Integumentary System § Components of the cutaneous membrane – Outer epidermis • Superficial epithelium – Inner dermis • Connective tissues 5 © 2018 Pearson Education, Inc.
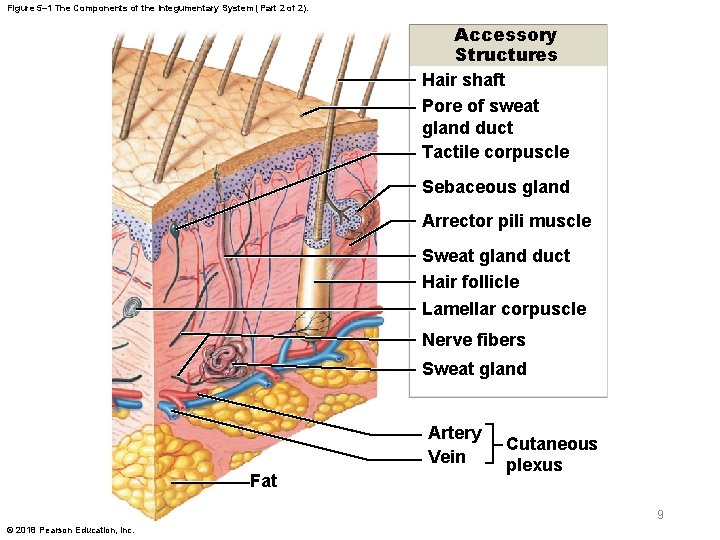
The Integumentary System § Accessory structures – Originate in the dermis – Extend through the epidermis to skin surface • Hair and hair follicles • Exocrine glands • Nails 6 © 2018 Pearson Education, Inc.
The Integumentary System § The integument contains blood vessels and sensory receptors § Subcutaneous layer (hypodermis) – Loose connective tissue – Below the dermis 7 © 2018 Pearson Education, Inc.
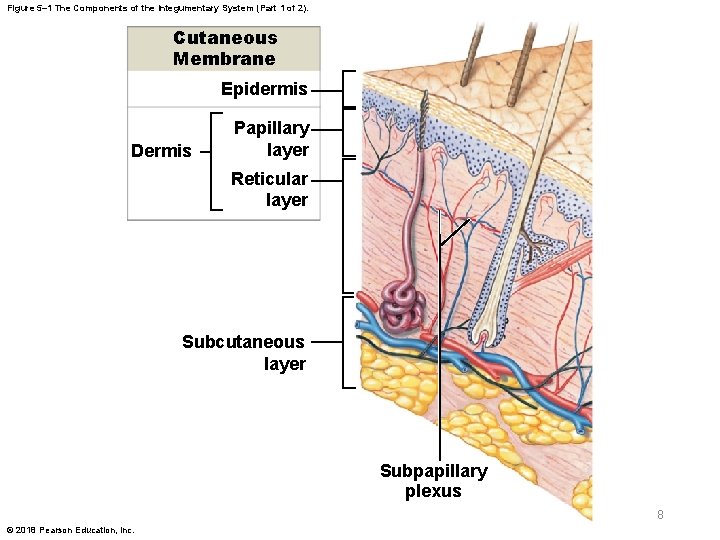
Figure 5– 1 The Components of the Integumentary System (Part 1 of 2). Cutaneous Membrane Epidermis Dermis Papillary layer Reticular layer Subcutaneous layer Subpapillary plexus 8 © 2018 Pearson Education, Inc.
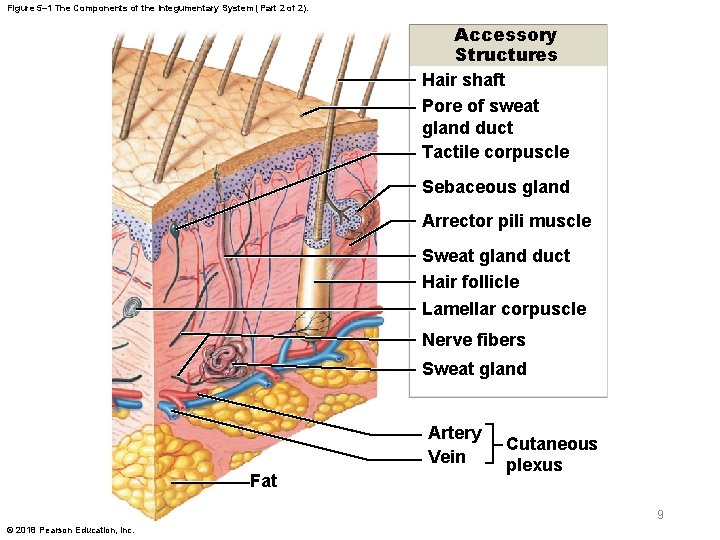
Figure 5– 1 The Components of the Integumentary System (Part 2 of 2). Accessory Structures Hair shaft Pore of sweat gland duct Tactile corpuscle Sebaceous gland Arrector pili muscle Sweat gland duct Hair follicle Lamellar corpuscle Nerve fibers Sweat gland Artery Vein Fat Cutaneous plexus 9 © 2018 Pearson Education, Inc.
The Integumentary System § Functions of the integument – Protection of underlying tissues and organs – Excretion of salts, water, and organic wastes – Maintenance of normal body temperature – Production of melanin – Production of keratin – Synthesis of vitamin D 3 – Storage of lipids – Detection of touch, pressure, pain, etc. – Coordination of the immune response 10 © 2018 Pearson Education, Inc.
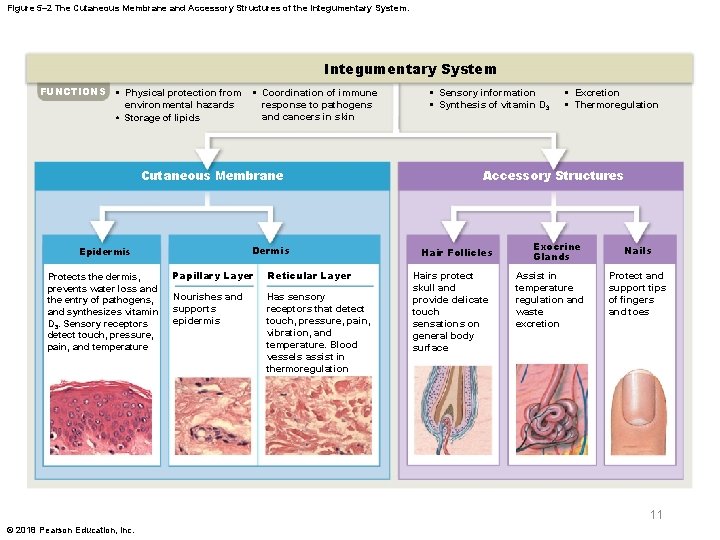
Figure 5– 2 The Cutaneous Membrane and Accessory Structures of the Integumentary System FUNCTIONS • Physical protection from environmental hazards • Storage of lipids • Coordination of immune response to pathogens and cancers in skin Cutaneous Membrane Dermis Epidermis Protects the dermis, prevents water loss and the entry of pathogens, and synthesizes vitamin D 3. Sensory receptors detect touch, pressure, pain, and temperature Papillary Layer Reticular Layer Nourishes and supports epidermis Has sensory receptors that detect touch, pressure, pain, vibration, and temperature. Blood vessels assist in thermoregulation • Sensory information • Synthesis of vitamin D 3 • Excretion • Thermoregulation Accessory Structures Hair Follicles Hairs protect skull and provide delicate touch sensations on general body surface Exocrine Glands Assist in temperature regulation and waste excretion Nails Protect and support tips of fingers and toes 11 © 2018 Pearson Education, Inc.
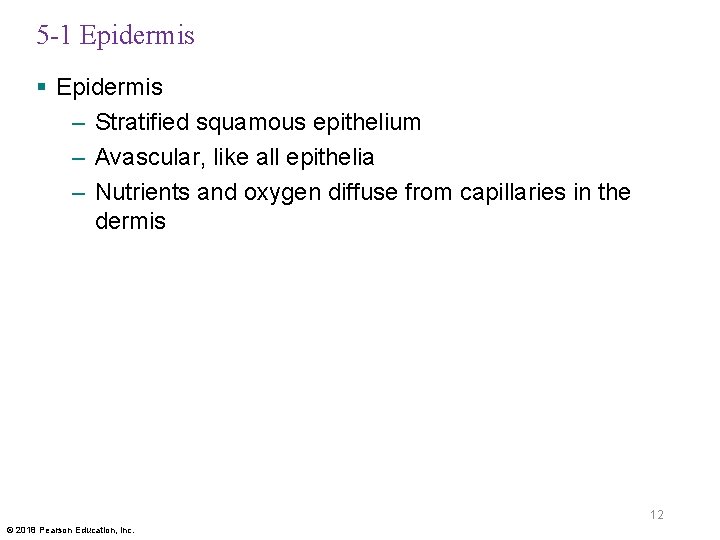
5 -1 Epidermis § Epidermis – Stratified squamous epithelium – Avascular, like all epithelia – Nutrients and oxygen diffuse from capillaries in the dermis 12 © 2018 Pearson Education, Inc.
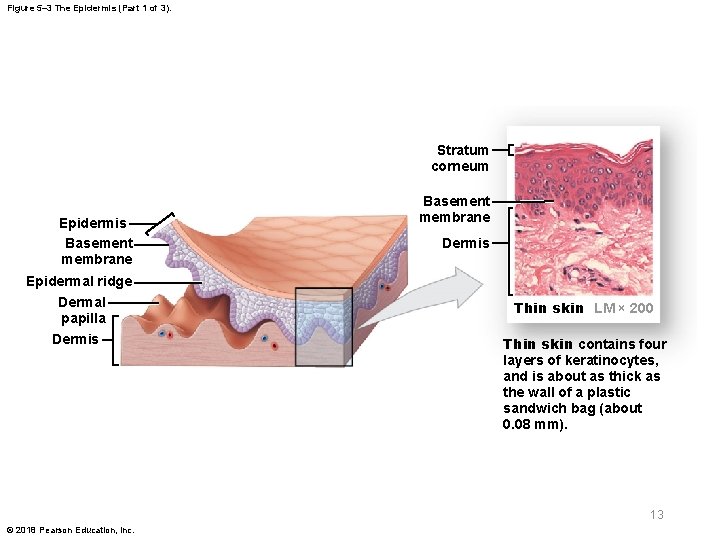
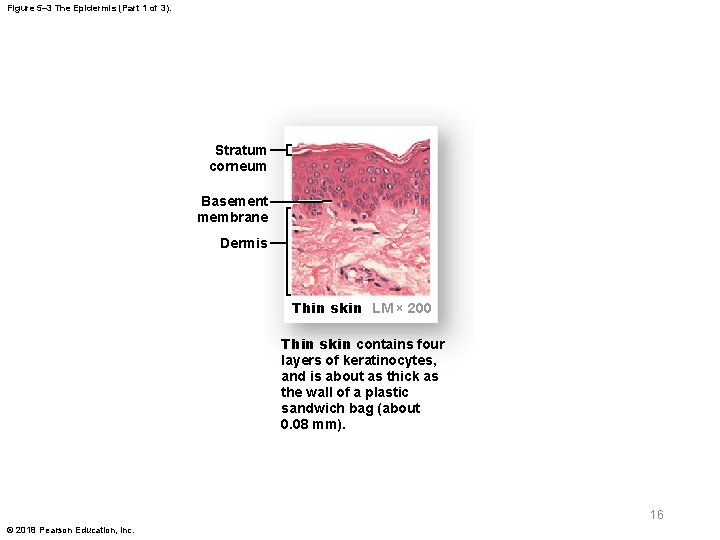
Figure 5– 3 The Epidermis (Part 1 of 3). Stratum corneum Epidermis Basement membrane Epidermal ridge Dermal papilla Dermis Basement membrane Dermis Thin skin LM × 200 Thin skin contains four layers of keratinocytes, and is about as thick as the wall of a plastic sandwich bag (about 0. 08 mm). 13 © 2018 Pearson Education, Inc.
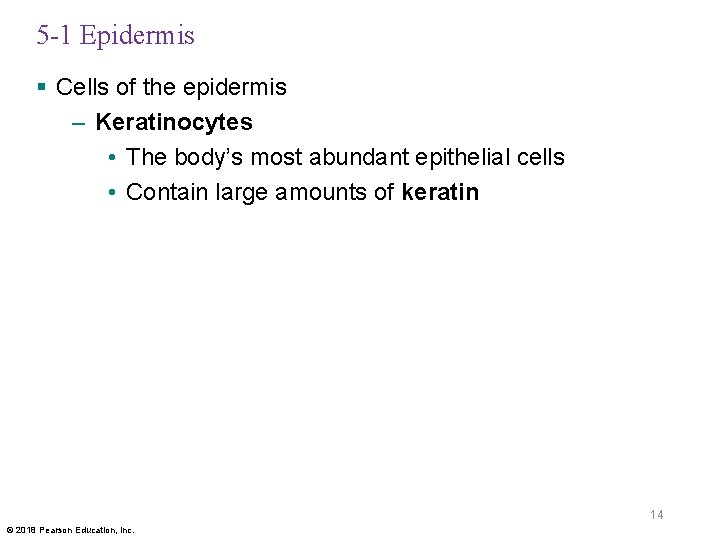
5 -1 Epidermis § Cells of the epidermis – Keratinocytes • The body’s most abundant epithelial cells • Contain large amounts of keratin 14 © 2018 Pearson Education, Inc.

5 -1 Epidermis § Two types of skin – Thin skin • Covers most of the body • Has four layers of keratinocytes – Thick skin • Covers the palms of the hands and soles of the feet • Has five layers of keratinocytes 15 © 2018 Pearson Education, Inc.
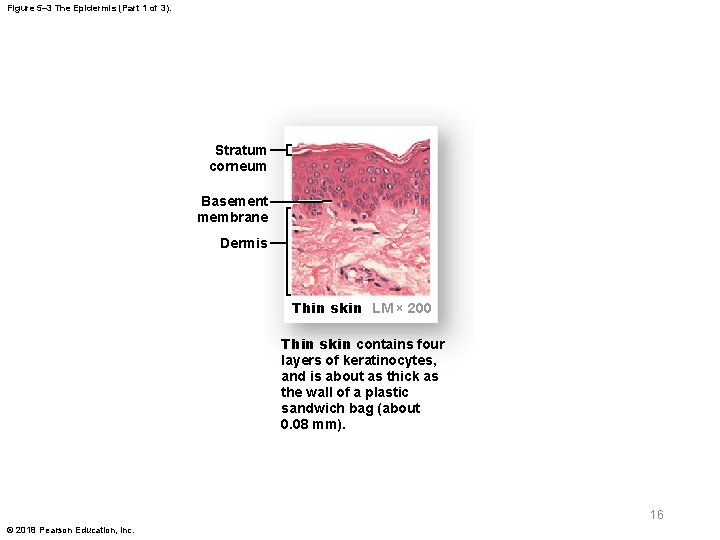
Figure 5– 3 The Epidermis (Part 1 of 3). Stratum corneum Basement membrane Dermis Thin skin LM × 200 Thin skin contains four layers of keratinocytes, and is about as thick as the wall of a plastic sandwich bag (about 0. 08 mm). 16 © 2018 Pearson Education, Inc.

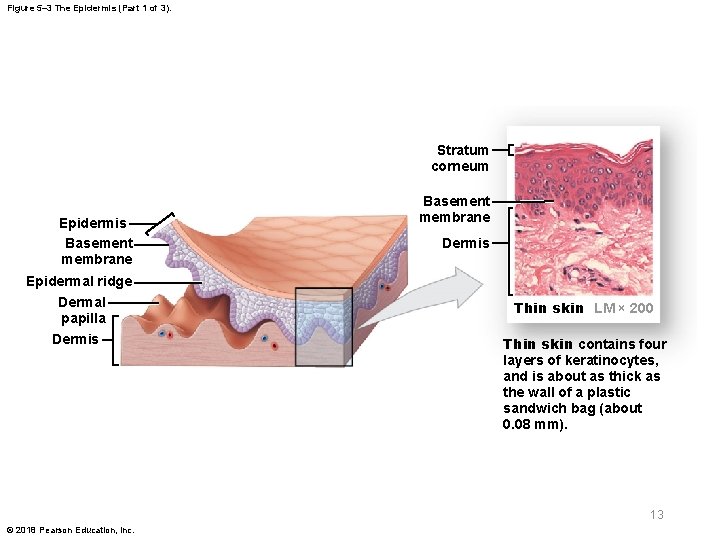
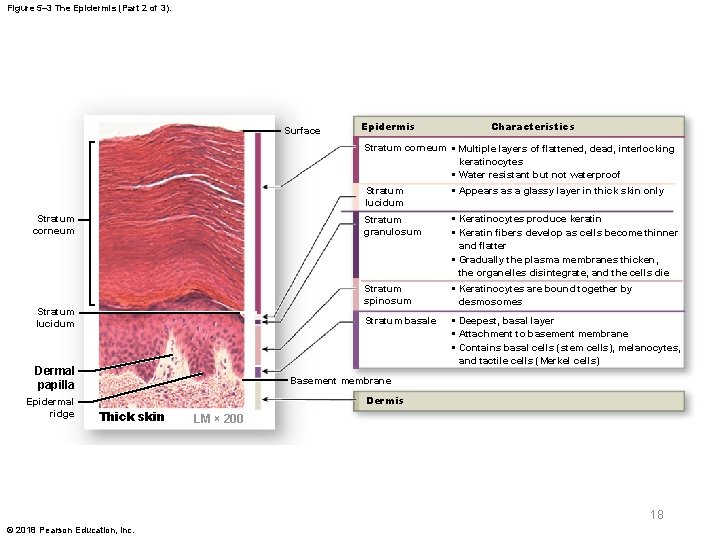
5 -1 Epidermis § Five strata (layers) of keratinocytes in thick skin – From basement membrane to free surface • Stratum basale • Stratum spinosum • Stratum granulosum • Stratum lucidum • Stratum corneum 17 © 2018 Pearson Education, Inc.
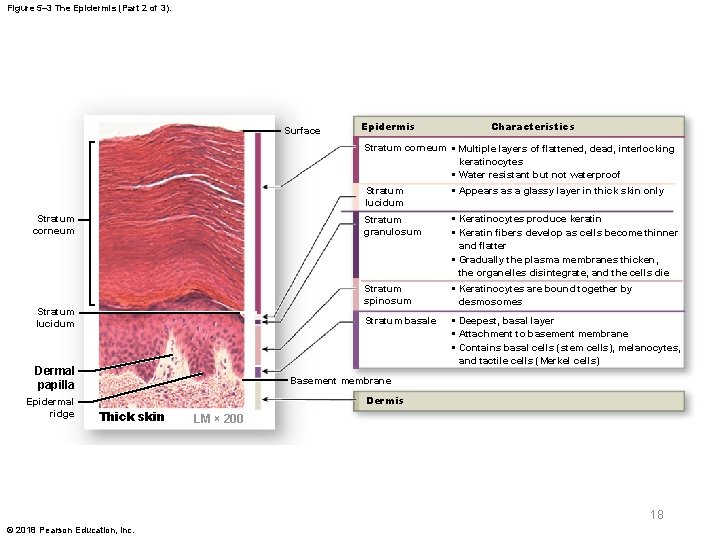
Figure 5– 3 The Epidermis (Part 2 of 3). Surface Epidermis Characteristics Stratum corneum • Multiple layers of flattened, dead, interlocking keratinocytes • Water resistant but not waterproof Stratum corneum Stratum lucidum Dermal papilla Epidermal ridge Stratum lucidum • Appears as a glassy layer in thick skin only Stratum granulosum • Keratinocytes produce keratin • Keratin fibers develop as cells become thinner and flatter • Gradually the plasma membranes thicken, the organelles disintegrate, and the cells die Stratum spinosum • Keratinocytes are bound together by desmosomes Stratum basale • Deepest, basal layer • Attachment to basement membrane • Contains basal cells (stem cells), melanocytes, and tactile cells (Merkel cells) Basement membrane Dermis Thick skin LM × 200 18 © 2018 Pearson Education, Inc.
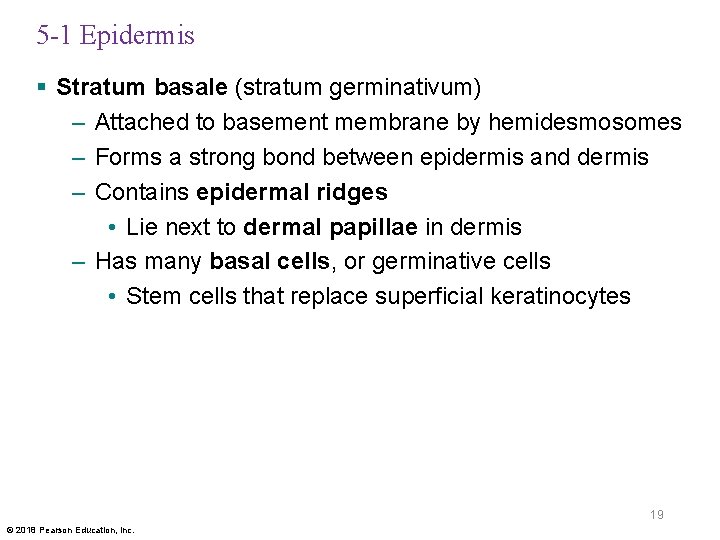
5 -1 Epidermis § Stratum basale (stratum germinativum) – Attached to basement membrane by hemidesmosomes – Forms a strong bond between epidermis and dermis – Contains epidermal ridges • Lie next to dermal papillae in dermis – Has many basal cells, or germinative cells • Stem cells that replace superficial keratinocytes 19 © 2018 Pearson Education, Inc.

Figure 5– 3 The Epidermis (Part 3 of 3). Pores of sweat gland ducts Epidermal ridge Thick skin SEM × 20 20 © 2018 Pearson Education, Inc.
5 -1 Epidermis § Specialized structures of stratum basale – Tactile discs • Tactile (Merkel) cells with sensory nerve endings • Found in hairless skin • Respond to touch – Melanocytes • Contain the pigment melanin 21 © 2018 Pearson Education, Inc.

5 -1 Epidermis § Stratum spinosum—the “spiny layer” – Eight to ten layers of keratinocytes bound by desmosomes – Cells appear spiny in histological sections – Produced by division of cells in stratum basale, some of which continue dividing – Contains dendritic (Langerhans) cells, which are active in immune response 22 © 2018 Pearson Education, Inc.
5 -1 Epidermis § Stratum granulosum—the “granular layer” – Three to five layers of keratinocytes – Produced from cells of stratum spinosum – Most cells stop dividing and produce • Keratin • Keratohyalin – Forms dense granules – Promotes cellular dehydration and cross-linking of keratin fibers – After production of proteins, cells die 23 © 2018 Pearson Education, Inc.
5 -1 Epidermis § Stratum lucidum—the “clear layer” – Found only in thick skin – Covers stratum granulosum 24 © 2018 Pearson Education, Inc.

5 -1 Epidermis § Stratum corneum—the “horny layer” – Exposed surface of skin – Water resistant – 15 to 30 layers of keratinized cells • Keratinization is the formation of protective layers of cells filled with keratin – New cells move from stratum basale to stratum corneum in 7 to 10 days – Exposed cells are shed after two weeks 25 © 2018 Pearson Education, Inc.
5 -1 Epidermis § Water is lost from skin in two ways – Insensible perspiration • Water diffuses across stratum corneum and evaporates from skin • 500 m. L per day • Rate increases if stratum corneum is damaged (e. g. , from burns) – Sensible perspiration • Water excreted by sweat glands 26 © 2018 Pearson Education, Inc.
5 -1 Epidermis § Epidermal growth factor (EGF) – A peptide growth factor – Produced by salivary glands and duodenum – Used in laboratories to grow skin grafts § Functions of EGF – Promotes division of basal cells – Accelerates keratin production – Stimulates epidermal repair – Stimulates glandular secretion 27 © 2018 Pearson Education, Inc.
5 -2 The Dermis § Dermis – Located between epidermis and subcutaneous layer – Anchors epidermal accessory structures (e. g. , hair follicles and sweat glands) – Two components • Outer papillary layer • Deeper reticular layer 28 © 2018 Pearson Education, Inc.
5 -2 The Dermis § Papillary layer – Consists of areolar tissue – Contains capillaries, lymphatic vessels, and sensory neurons – Named for dermal papillae that project between epidermal ridges – Becomes inflamed in dermatitis • Caused by infection, radiation, mechanical irritation, or chemicals (e. g. , poison ivy) • May produce itching or pain 29 © 2018 Pearson Education, Inc.
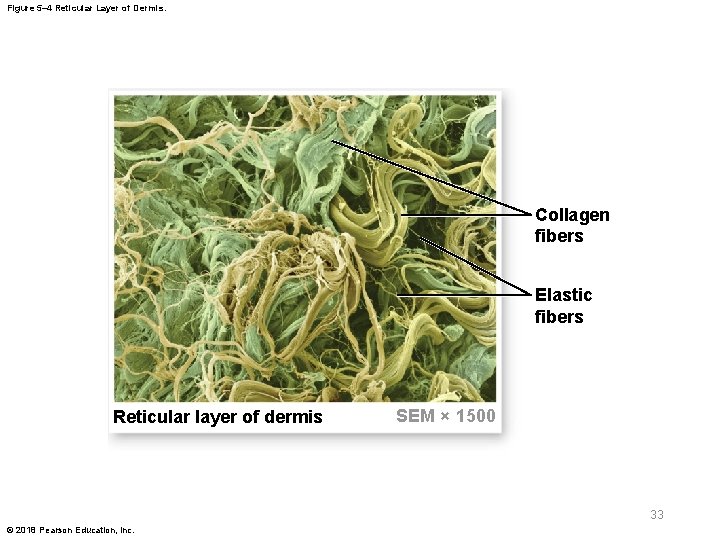
5 -2 The Dermis § Reticular layer – Consists of dense irregular connective tissue – Contains collagen and elastic fibers – The dermis contains all cells of connective tissue proper 30 © 2018 Pearson Education, Inc.
5 -2 The Dermis § Dermal strength and elasticity – Collagen fibers • Very strong, resist stretching • Easily bent or twisted • Limit flexibility to prevent tissue damage – Elastic fibers • Permit stretching and then recoil to original length • Provide flexibility – Fibers and water provide flexibility and resilience • Known as skin turgor 31 © 2018 Pearson Education, Inc.
5 -2 The Dermis § Skin damage – Loss of skin turgor is caused by • Dehydration (reversible) • Aging • Hormones • UV radiation – Excessive distortion of skin from pregnancy or weight gain may cause stretch marks 32 © 2018 Pearson Education, Inc.
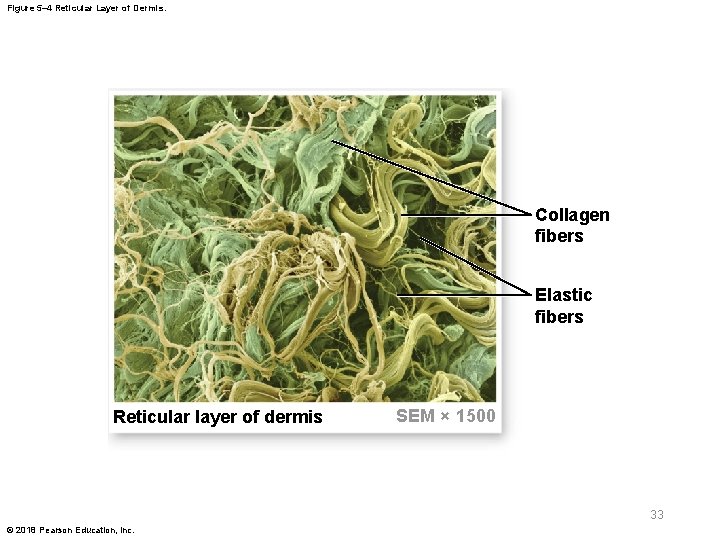
Figure 5– 4 Reticular Layer of Dermis. Collagen fibers Elastic fibers Reticular layer of dermis SEM × 1500 33 © 2018 Pearson Education, Inc.

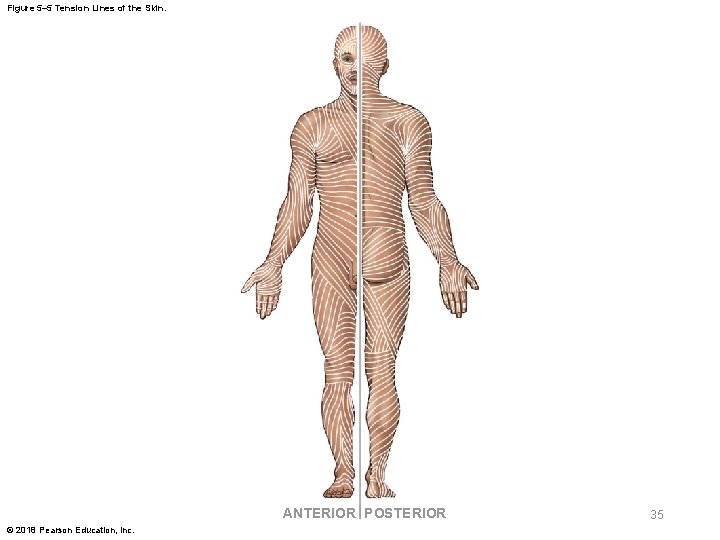
5 -2 The Dermis § Tension lines (cleavage lines) – Produced by parallel bundles of collagen and elastic fibers in the dermis – Resist forces applied to skin – A cut made parallel to a tension line remains shut, heals well • A cut at a right angle pulls open and scars 34 © 2018 Pearson Education, Inc.
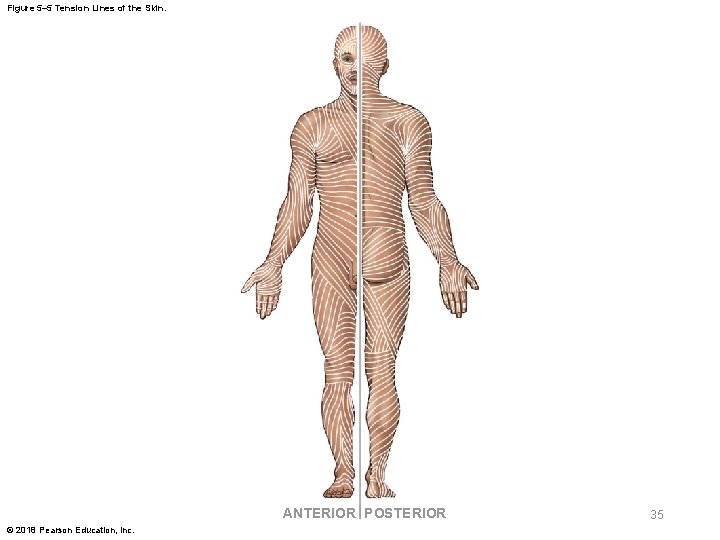
Figure 5– 5 Tension Lines of the Skin. ANTERIOR POSTERIOR © 2018 Pearson Education, Inc. 35
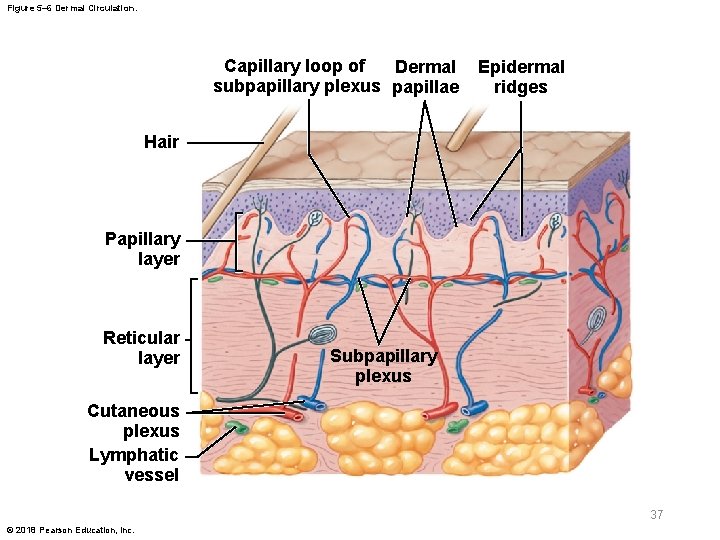
5 -2 The Dermis § Dermal blood supply – Cutaneous plexus • Deep network of arteries along the reticular layer – Subpapillary plexus • Network of small arteries in papillary layer • Capillaries drain into small veins that lead to larger veins in subcutaneous layer – Contusion (bruise) • Caused by damage to blood vessels in dermis 36 © 2018 Pearson Education, Inc.
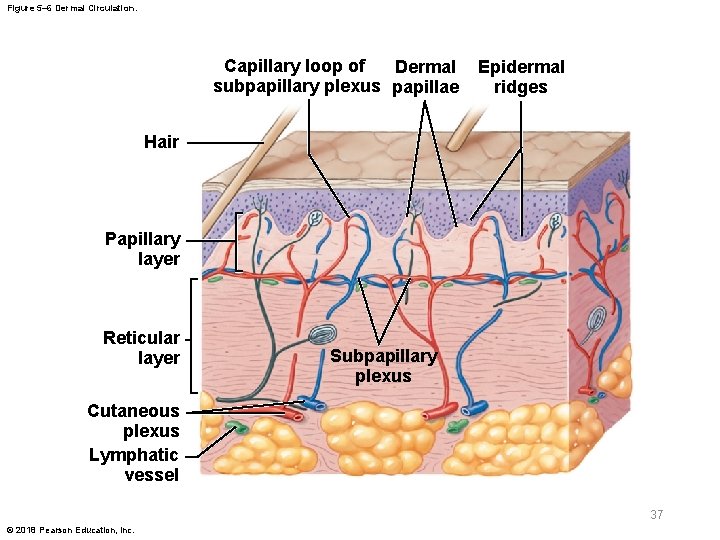
Figure 5– 6 Dermal Circulation. Capillary loop of Dermal subpapillary plexus papillae Epidermal ridges Hair Papillary layer Reticular layer Subpapillary plexus Cutaneous plexus Lymphatic vessel 37 © 2018 Pearson Education, Inc.
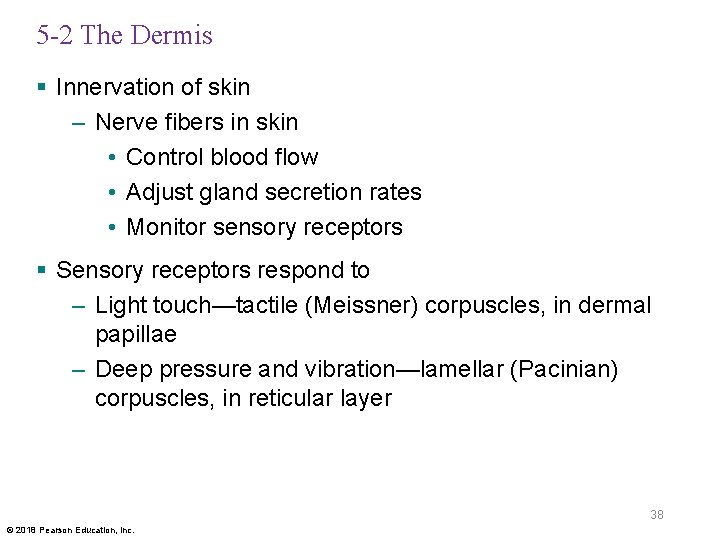
5 -2 The Dermis § Innervation of skin – Nerve fibers in skin • Control blood flow • Adjust gland secretion rates • Monitor sensory receptors § Sensory receptors respond to – Light touch—tactile (Meissner) corpuscles, in dermal papillae – Deep pressure and vibration—lamellar (Pacinian) corpuscles, in reticular layer 38 © 2018 Pearson Education, Inc.
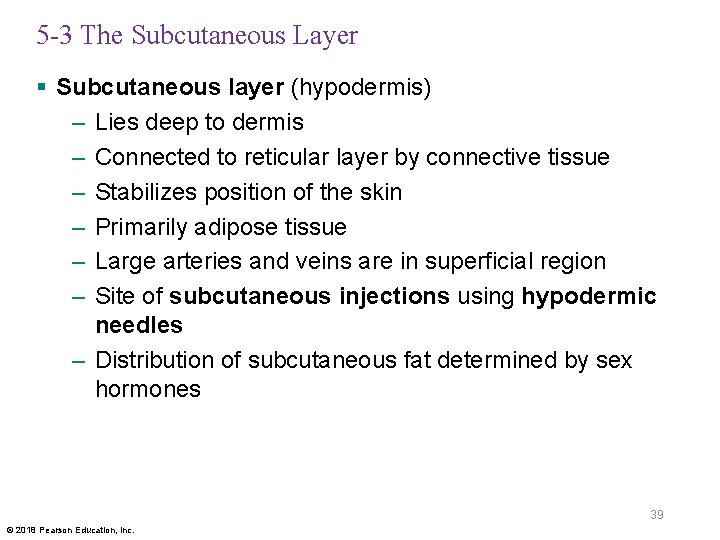
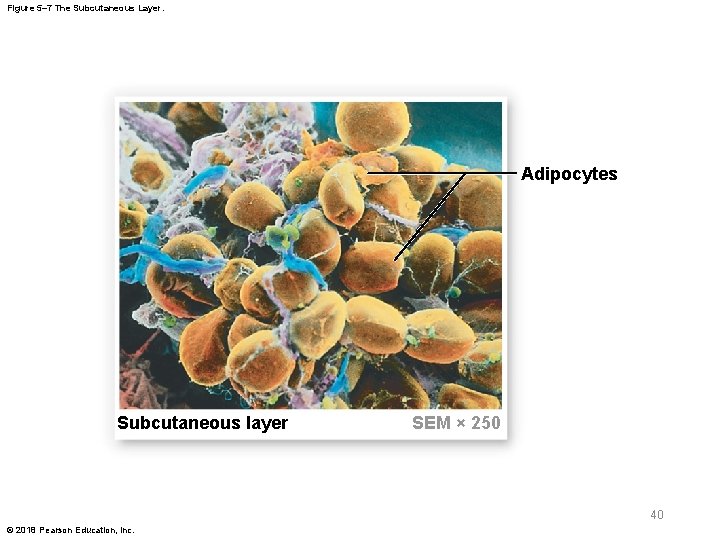
5 -3 The Subcutaneous Layer § Subcutaneous layer (hypodermis) – Lies deep to dermis – Connected to reticular layer by connective tissue – Stabilizes position of the skin – Primarily adipose tissue – Large arteries and veins are in superficial region – Site of subcutaneous injections using hypodermic needles – Distribution of subcutaneous fat determined by sex hormones 39 © 2018 Pearson Education, Inc.
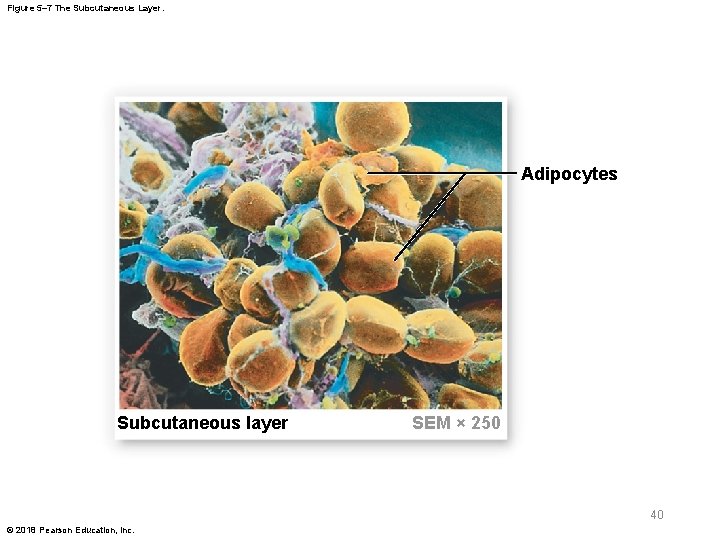
Figure 5– 7 The Subcutaneous Layer. Adipocytes Subcutaneous layer SEM × 250 40 © 2018 Pearson Education, Inc.
5 -4 Skin Color § Skin color is influenced by two pigments in the epidermis – Melanin – Carotene 41 © 2018 Pearson Education, Inc.
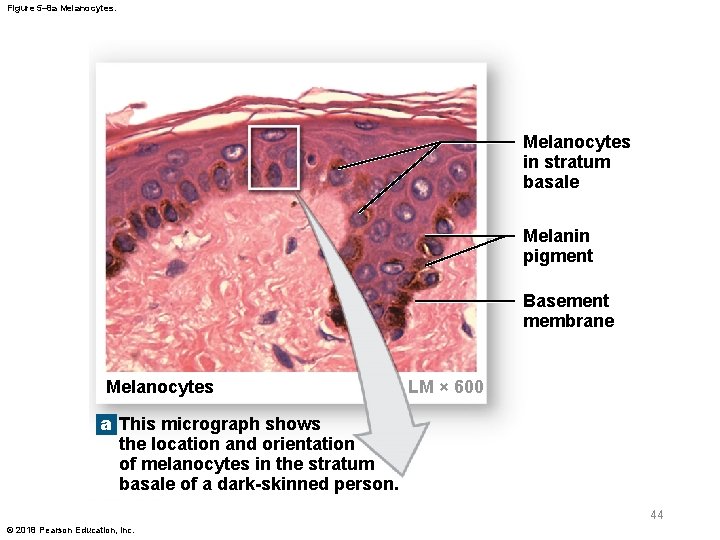
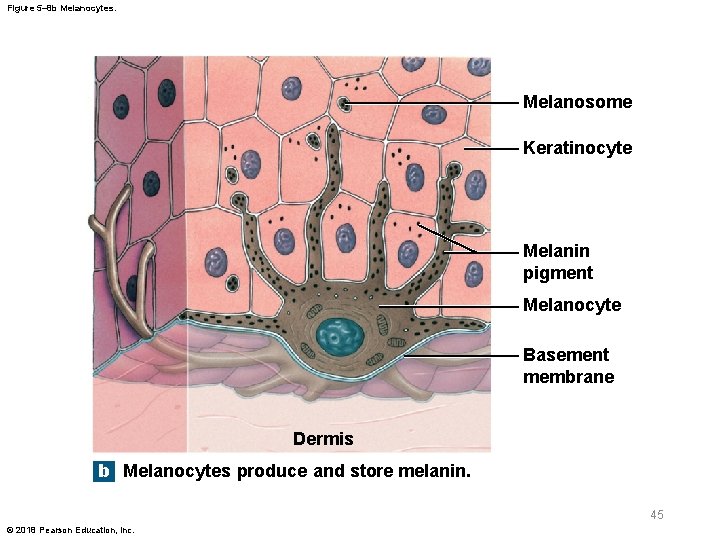
5 -4 Skin Color § Melanin – Red-yellow or brown-black pigment – Produced by melanocytes – Stored in intracellular vesicles (melanosomes) • Transferred to keratinocytes • Dark-skinned people have large, numerous melanosomes – Protects skin from ultraviolet (UV) radiation • Small amounts of UV radiation are beneficial • Too much can damage DNA and cause cancer 42 © 2018 Pearson Education, Inc.
5 -4 Skin Color § Carotene – Orange-yellow pigment – Found in orange vegetables – Accumulates in epidermal cells, deep dermis, and subcutaneous layer – Can be converted to vitamin A, required for • Maintenance of epithelia • Synthesis of photoreceptor pigments in eye 43 © 2018 Pearson Education, Inc.
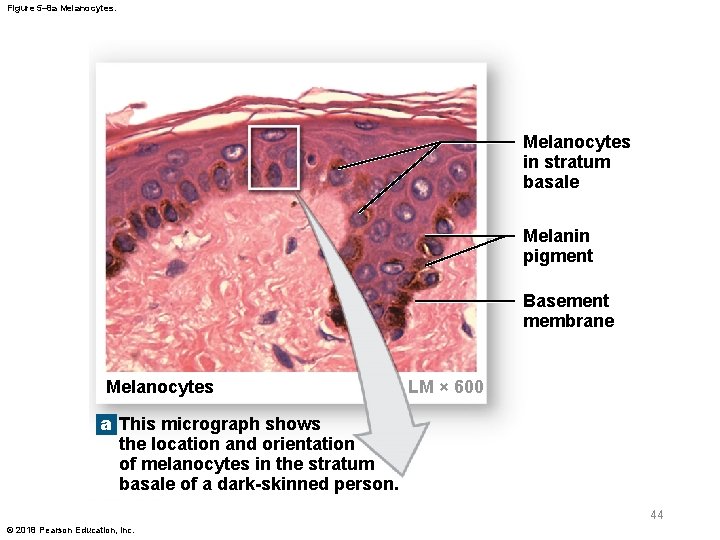
Figure 5– 8 a Melanocytes in stratum basale Melanin pigment Basement membrane Melanocytes LM × 600 a This micrograph shows the location and orientation of melanocytes in the stratum basale of a dark-skinned person. 44 © 2018 Pearson Education, Inc.
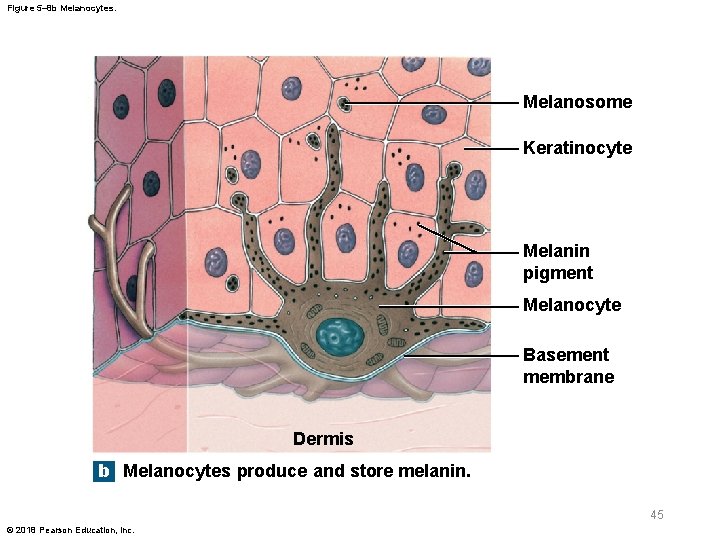
Figure 5– 8 b Melanocytes. Melanosome Keratinocyte Melanin pigment Melanocyte Basement membrane Dermis b Melanocytes produce and store melanin. 45 © 2018 Pearson Education, Inc.
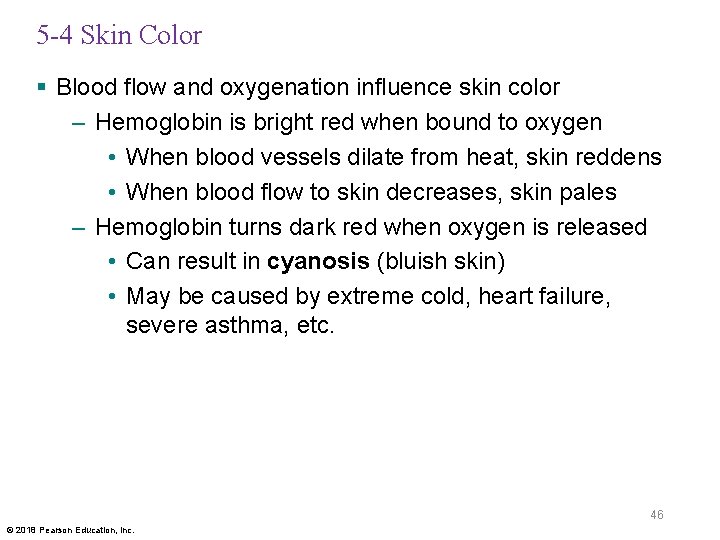
5 -4 Skin Color § Blood flow and oxygenation influence skin color – Hemoglobin is bright red when bound to oxygen • When blood vessels dilate from heat, skin reddens • When blood flow to skin decreases, skin pales – Hemoglobin turns dark red when oxygen is released • Can result in cyanosis (bluish skin) • May be caused by extreme cold, heart failure, severe asthma, etc. 46 © 2018 Pearson Education, Inc.
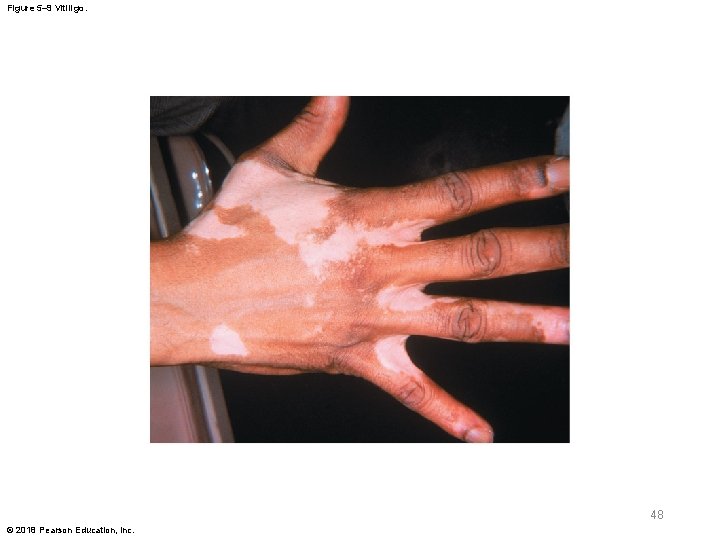
5 -4 Skin Color § Illness and skin color – Jaundice • Buildup of bile produced by liver • Skin and whites of eyes may turn yellow – Pituitary tumor • Excess MSH increases production of melanin – Addison’s disease • Causes pituitary gland to release excess ACTH, which has an effect similar to MSH – Vitiligo • Loss of melanocytes causing loss of color 47 © 2018 Pearson Education, Inc.
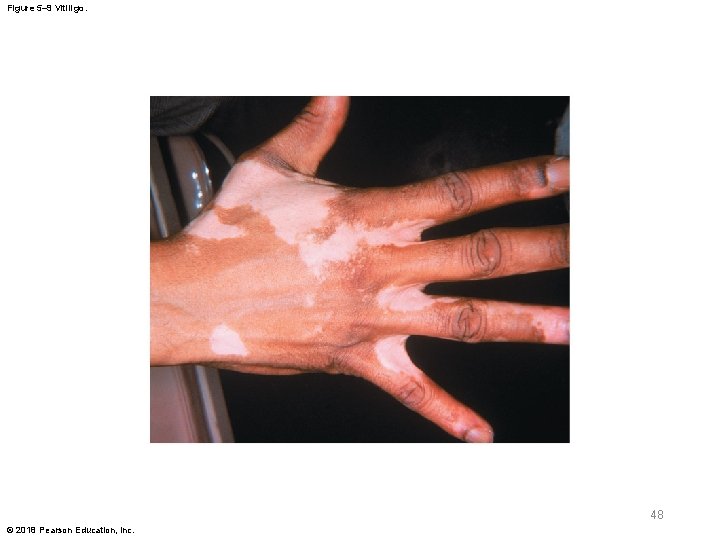
Figure 5– 9 Vitiligo. 48 © 2018 Pearson Education, Inc.
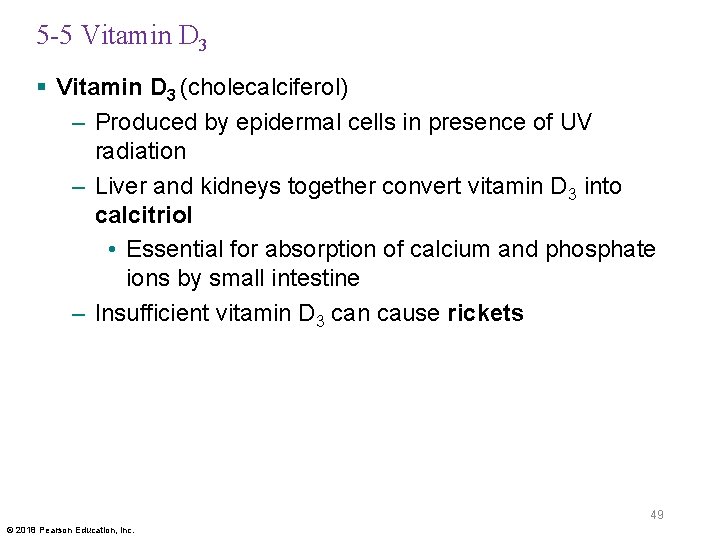
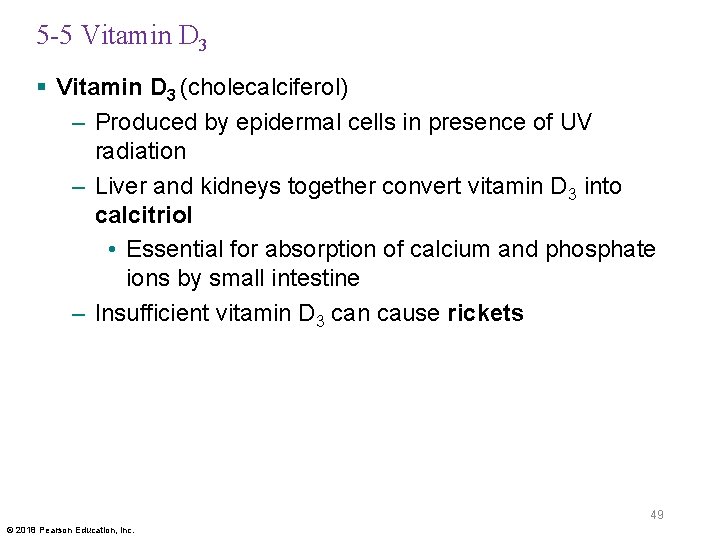
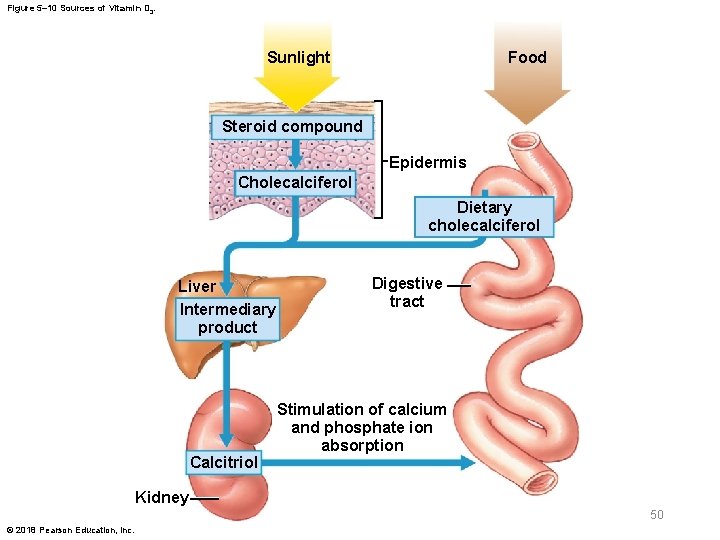
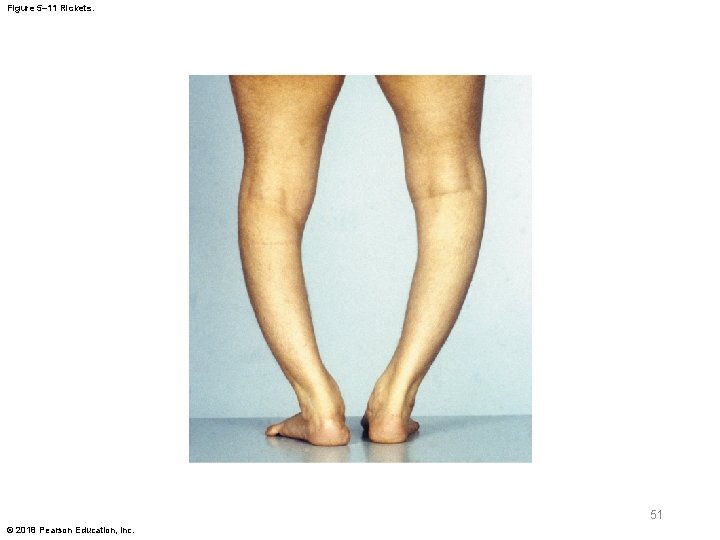
5 -5 Vitamin D 3 § Vitamin D 3 (cholecalciferol) – Produced by epidermal cells in presence of UV radiation – Liver and kidneys together convert vitamin D 3 into calcitriol • Essential for absorption of calcium and phosphate ions by small intestine – Insufficient vitamin D 3 can cause rickets 49 © 2018 Pearson Education, Inc.
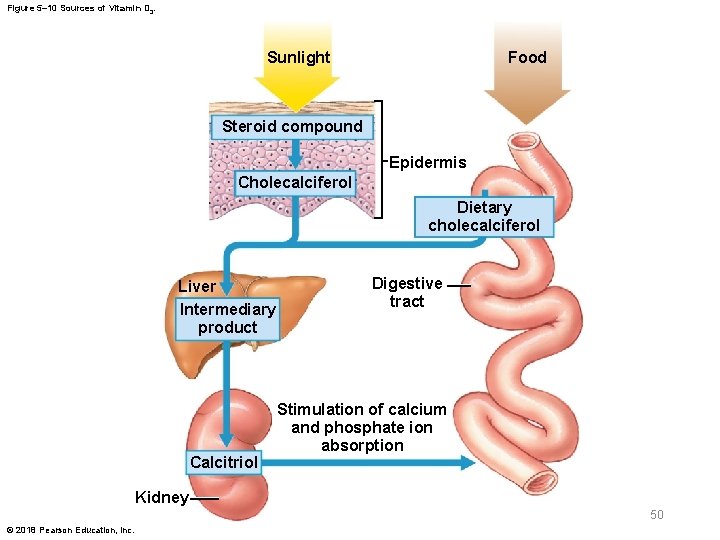
Figure 5– 10 Sources of Vitamin D 3. Food Sunlight Steroid compound Epidermis Cholecalciferol Dietary cholecalciferol Liver Intermediary product Calcitriol Digestive tract Stimulation of calcium and phosphate ion absorption Kidney 50 © 2018 Pearson Education, Inc.
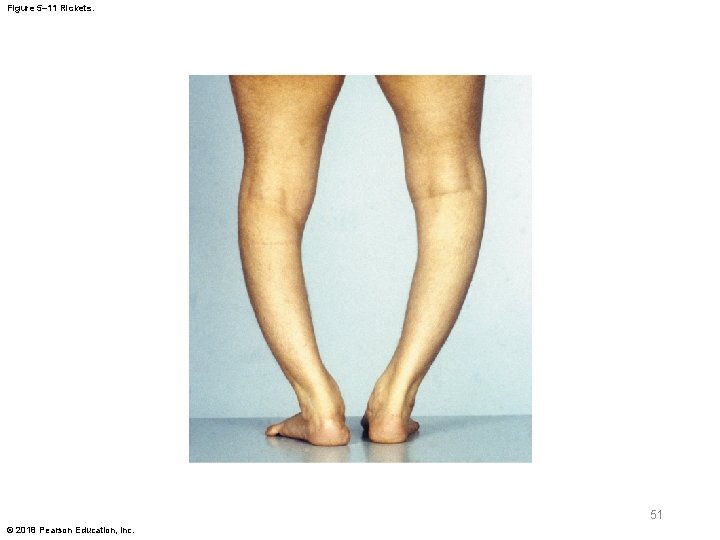
Figure 5– 11 Rickets. 51 © 2018 Pearson Education, Inc.
5 -6 Hair § Accessory structures of the integument – Hair, hair follicles, sebaceous and sweat glands, and nails – Derived from embryonic epidermis – Located in dermis, but project to skin surface 52 © 2018 Pearson Education, Inc.
5 -6 Hair § Hairs cover almost all of the body, except – Palms of hands, sides of fingers – Sides and soles of feet, sides of toes – Lips – Portions of external genitalia § Functions of hair – Protect and insulate – Guard openings from particles and insects – Serve as sensory receptors 53 © 2018 Pearson Education, Inc.
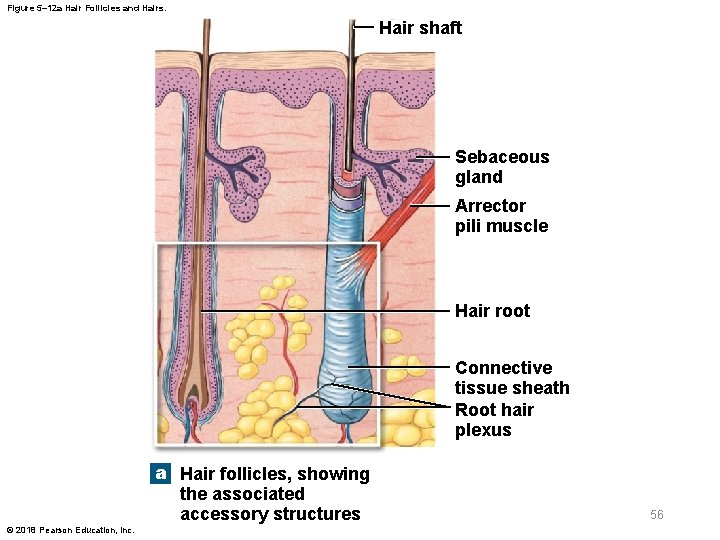
5 -6 Hair § Hair follicles – Extend deep into dermis – Produce nonliving hairs – Wrapped in a dense connective tissue sheath – Base is surrounded by sensory nerves (root hair plexus) – Arrector pili muscle • Involuntary smooth muscle • Contraction causes hairs to stand up • Produces “goose bumps” 54 © 2018 Pearson Education, Inc.
5 -6 Hair § Regions of the hair – Hair root • Portion that anchors it into skin – Hair shaft • Upper part of the hair 55 © 2018 Pearson Education, Inc.
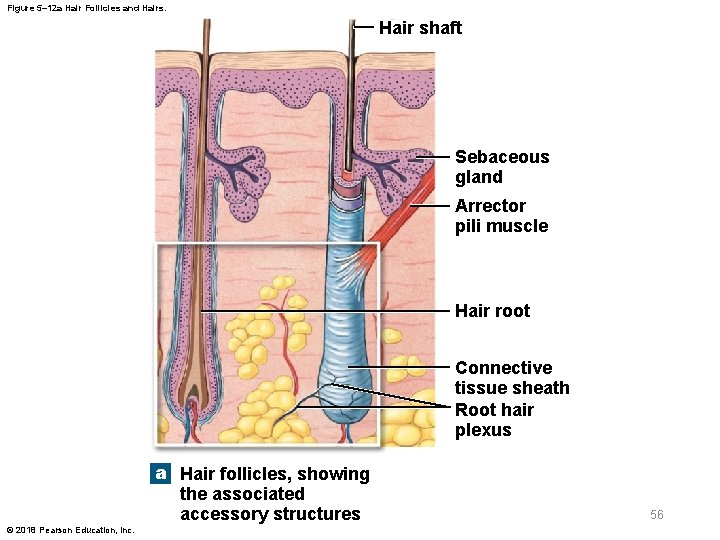
Figure 5– 12 a Hair Follicles and Hairs. Hair shaft Sebaceous gland Arrector pili muscle Hair root Connective tissue sheath Root hair plexus a Hair follicles, showing the associated accessory structures © 2018 Pearson Education, Inc. 56

Figure 5– 12 b Hair Follicles and Hairs. Hair Structure The cuticle, although The medulla, or core, The cortex contains thick of the hair contains a layers of hard keratin, which thin, is very tough, and it contains hard keratin. flexible soft keratin. give the hair its stiffness. Follicle Structure The internal root sheath surrounds the hair root and the deeper portion of the shaft. The cells of this sheath disintegrate quickly, and this layer does not extend the entire length of the hair follicle. The external root sheath extends from the skin surface to the hair matrix. The glassy membrane is a thickened, clear layer wrapped in the dense connective tissue sheath of the follicle as a whole. b Cross section through a hair follicle and a hair, near the junction between the hair root and hair shaft © 2018 Pearson Education, Inc. Connective tissue sheath 57
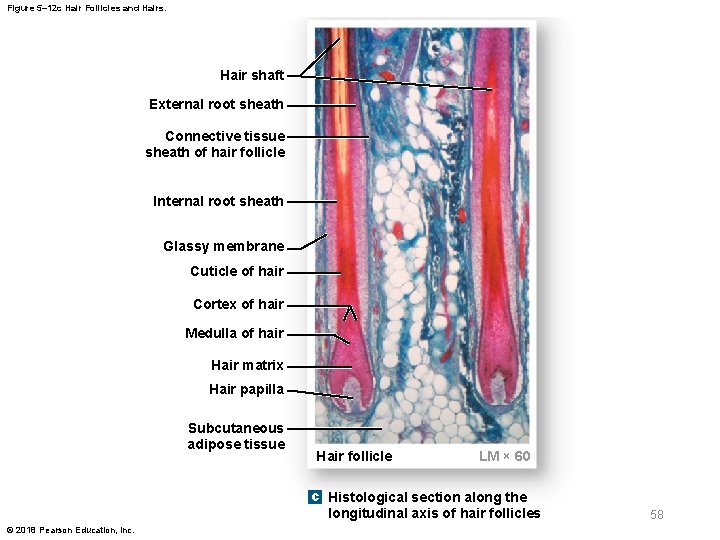
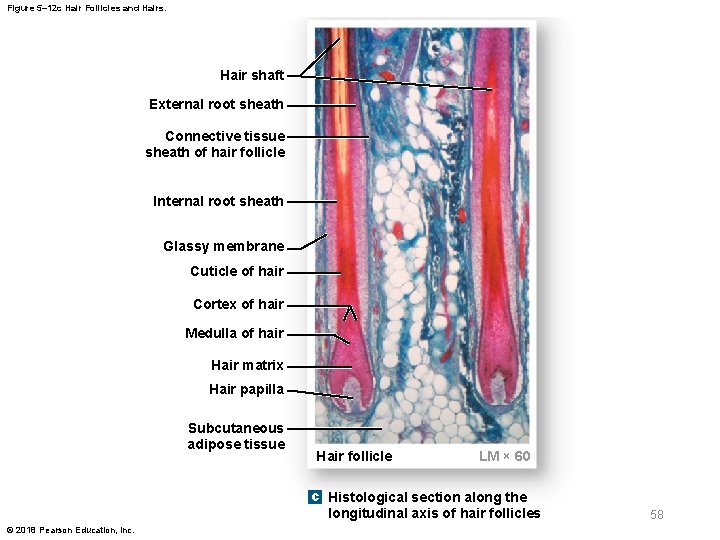
Figure 5– 12 c Hair Follicles and Hairs. Hair shaft External root sheath Connective tissue sheath of hair follicle Internal root sheath Glassy membrane Cuticle of hair Cortex of hair Medulla of hair Hair matrix Hair papilla Subcutaneous adipose tissue Hair follicle LM × 60 c Histological section along the longitudinal axis of hair follicles © 2018 Pearson Education, Inc. 58

Figure 5– 12 d Hair Follicles and Hairs. Connective tissue sheath of hair follicle Glassy membrane External root sheath Internal root sheath Cuticle of hair Cortex of hair Medulla of hair Hair matrix Hair papilla Hair bulb d Diagrammatic view of the base of a hair follicle © 2018 Pearson Education, Inc. Subcutaneous adipose tissue 59

5 -6 Hair § Hair structure – Medulla • Central core – Cortex • Intermediate layer – Cuticle • Surface layer 60 © 2018 Pearson Education, Inc.
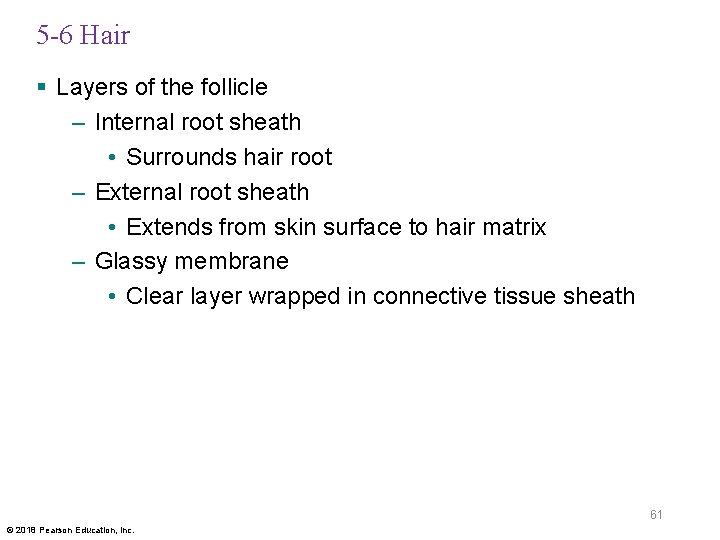
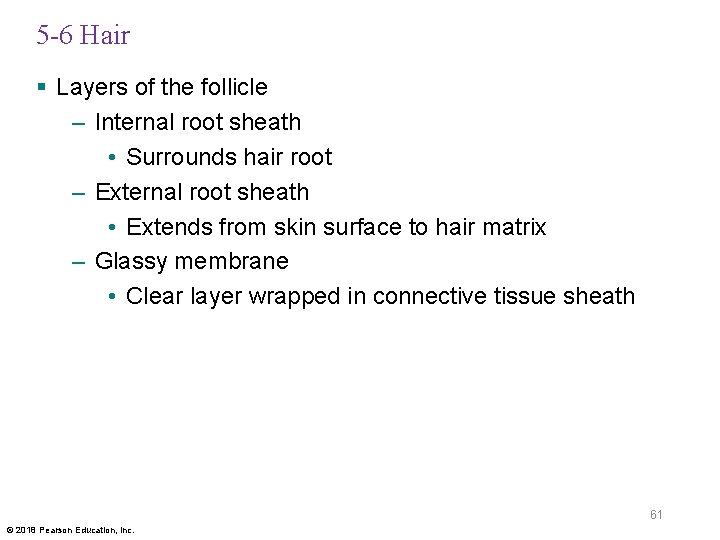
5 -6 Hair § Layers of the follicle – Internal root sheath • Surrounds hair root – External root sheath • Extends from skin surface to hair matrix – Glassy membrane • Clear layer wrapped in connective tissue sheath 61 © 2018 Pearson Education, Inc.
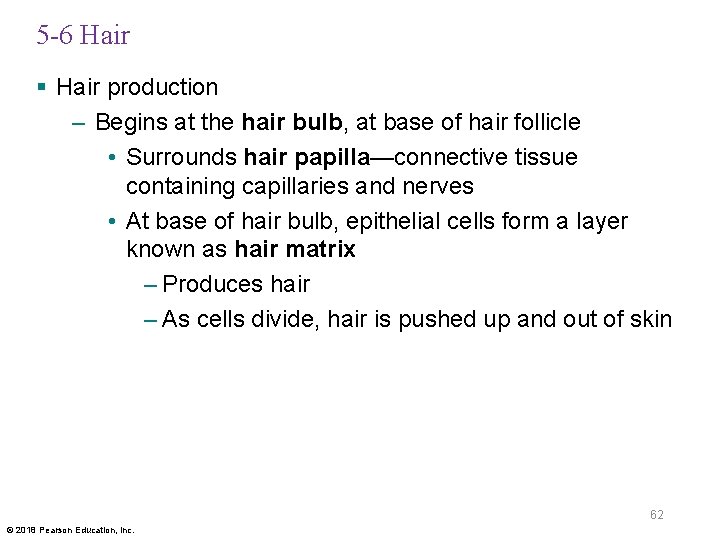
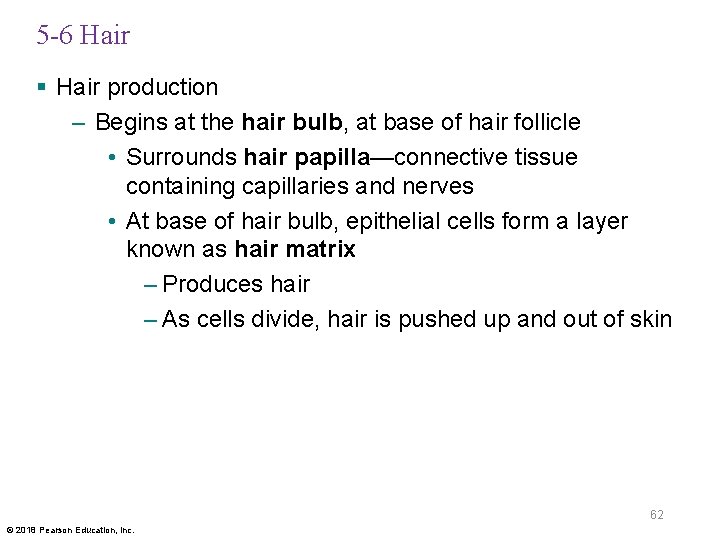
5 -6 Hair § Hair production – Begins at the hair bulb, at base of hair follicle • Surrounds hair papilla—connective tissue containing capillaries and nerves • At base of hair bulb, epithelial cells form a layer known as hair matrix – Produces hair – As cells divide, hair is pushed up and out of skin 62 © 2018 Pearson Education, Inc.
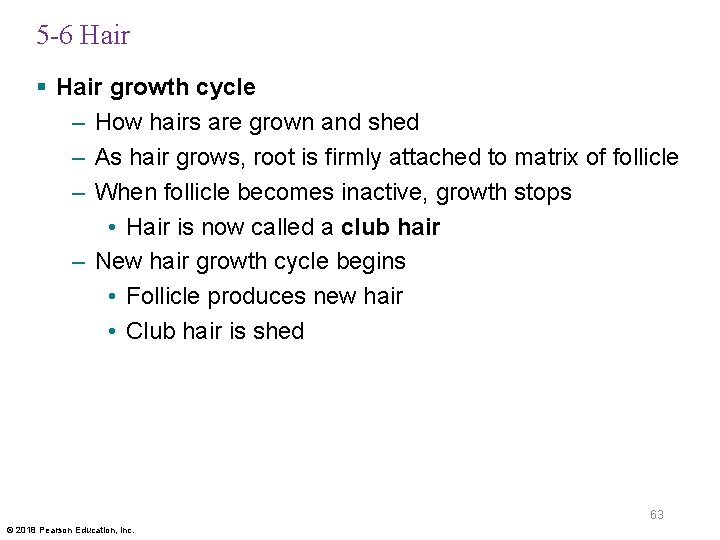
5 -6 Hair § Hair growth cycle – How hairs are grown and shed – As hair grows, root is firmly attached to matrix of follicle – When follicle becomes inactive, growth stops • Hair is now called a club hair – New hair growth cycle begins • Follicle produces new hair • Club hair is shed 63 © 2018 Pearson Education, Inc.
5 -6 Hair § Types of hairs – Vellus hairs • Soft, fine hairs that cover most of body surface – Terminal hairs • Heavy, pigmented hairs • On head, eyebrows, and eyelashes • Other parts of body after puberty § Hair color – Produced by melanocytes at hair matrix – Determined by genes 64 © 2018 Pearson Education, Inc.
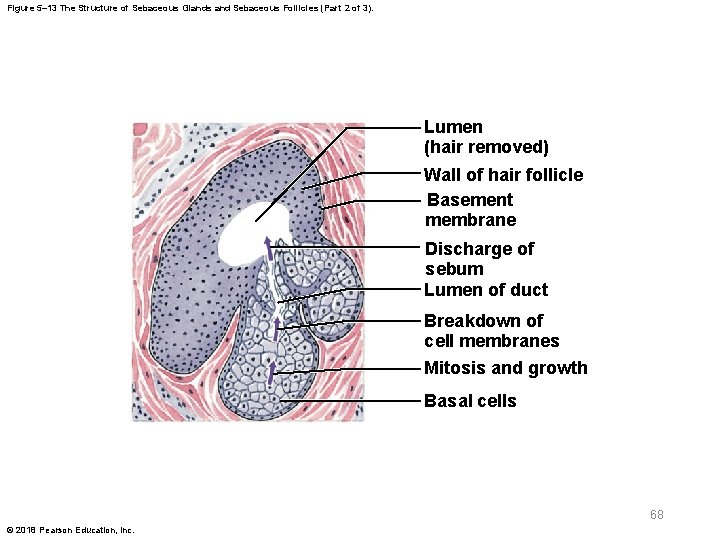
5 -7 Sebaceous and Sweat Glands § Exocrine glands in skin – Sebaceous glands (oil glands) • Holocrine glands • Discharge lipid secretion (sebum) into hair follicles – Lubricates and protects hair shaft – Inhibits growth of bacteria – Sweat glands • Apocrine sweat glands • Eccrine sweat glands 65 © 2018 Pearson Education, Inc.

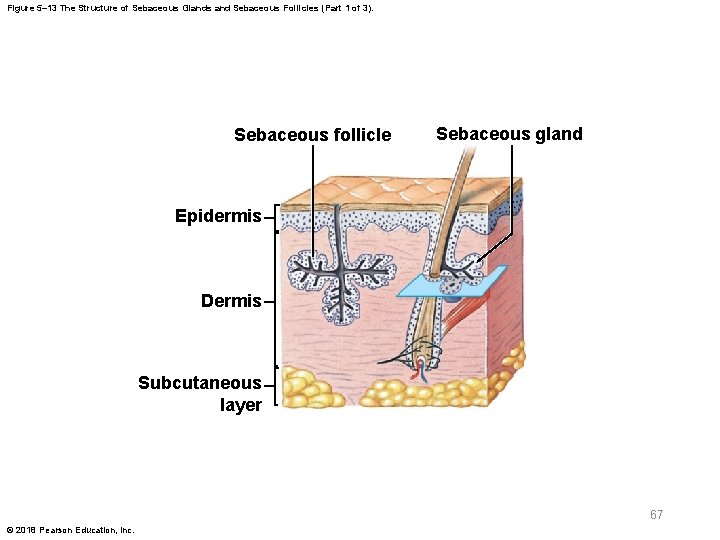
5 -7 Sebaceous and Sweat Glands § Types of sebaceous glands – Simple branched alveolar glands • Associated with hair follicles – Sebaceous follicles • Large sebaceous glands not associated with hair • Discharge sebum directly onto skin surface • Located on face, back, chest, nipples, external genitalia 66 © 2018 Pearson Education, Inc.
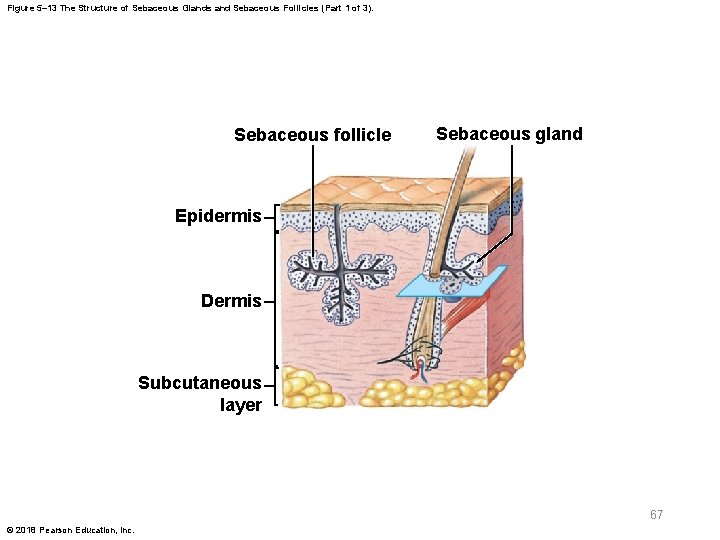
Figure 5– 13 The Structure of Sebaceous Glands and Sebaceous Follicles (Part 1 of 3). Sebaceous follicle Sebaceous gland Epidermis Dermis Subcutaneous layer 67 © 2018 Pearson Education, Inc.
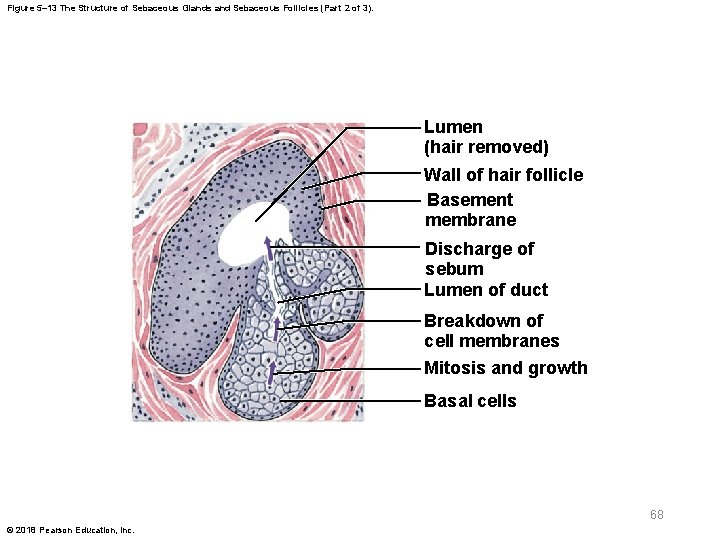
Figure 5– 13 The Structure of Sebaceous Glands and Sebaceous Follicles (Part 2 of 3). Lumen (hair removed) Wall of hair follicle Basement membrane Discharge of sebum Lumen of duct Breakdown of cell membranes Mitosis and growth Basal cells 68 © 2018 Pearson Education, Inc.
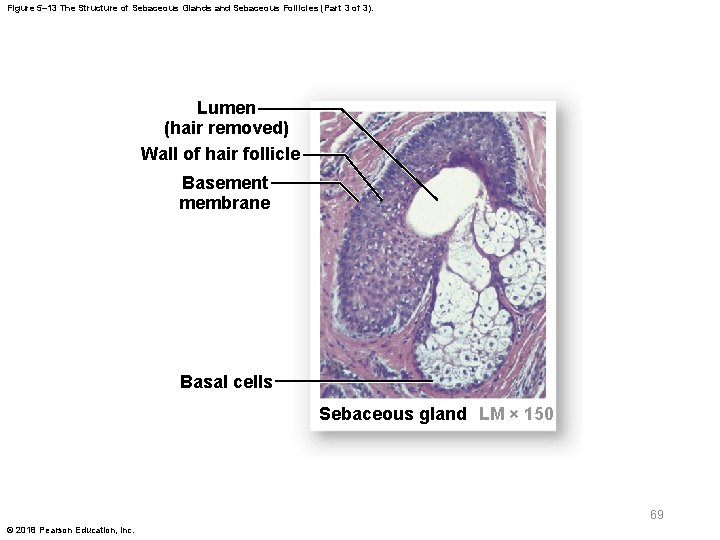
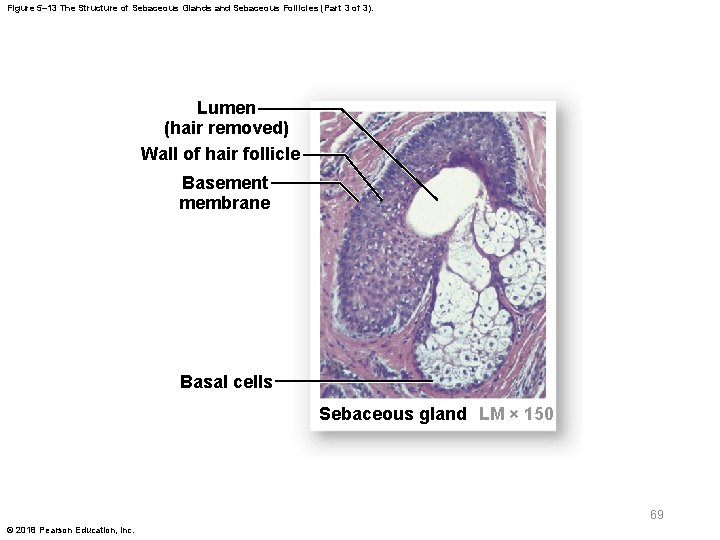
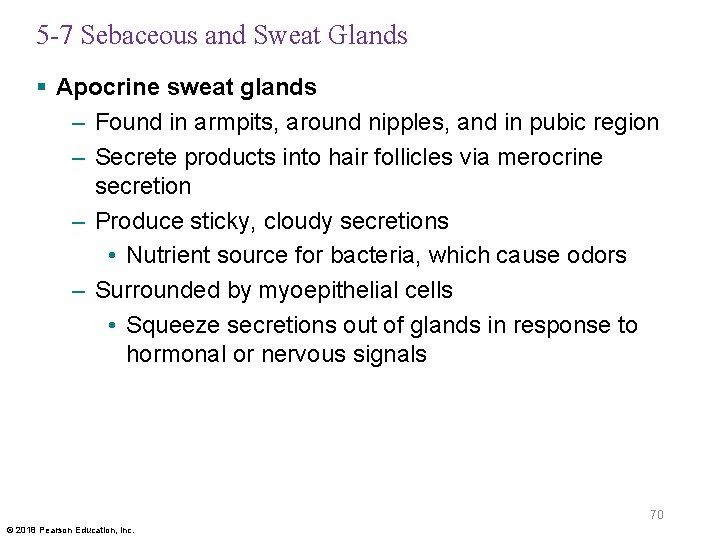
Figure 5– 13 The Structure of Sebaceous Glands and Sebaceous Follicles (Part 3 of 3). Lumen (hair removed) Wall of hair follicle Basement membrane Basal cells Sebaceous gland LM × 150 69 © 2018 Pearson Education, Inc.
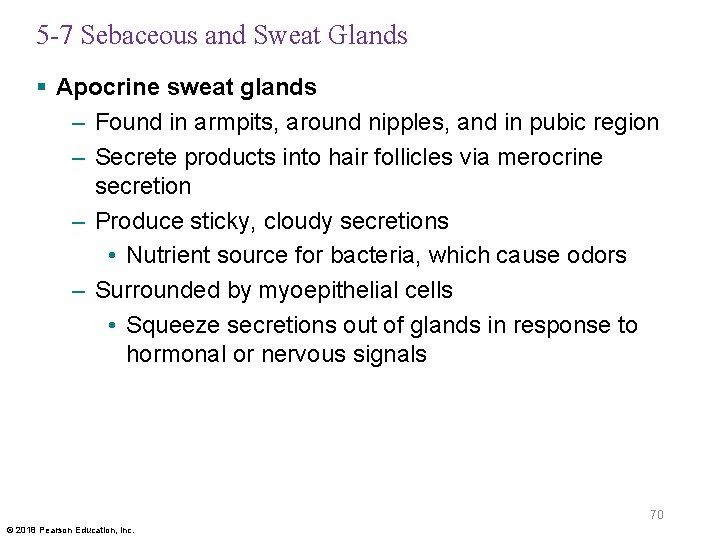
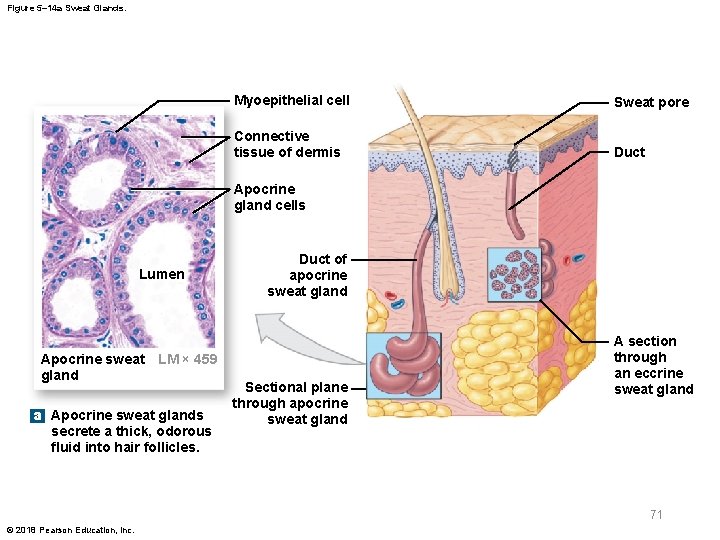
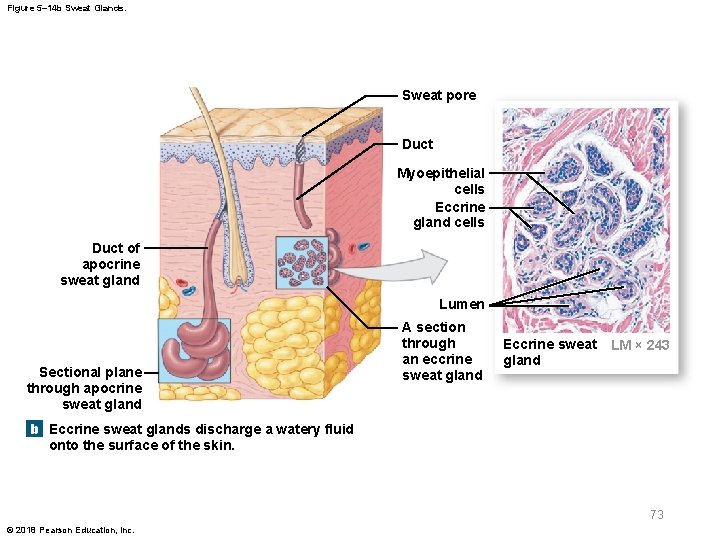
5 -7 Sebaceous and Sweat Glands § Apocrine sweat glands – Found in armpits, around nipples, and in pubic region – Secrete products into hair follicles via merocrine secretion – Produce sticky, cloudy secretions • Nutrient source for bacteria, which cause odors – Surrounded by myoepithelial cells • Squeeze secretions out of glands in response to hormonal or nervous signals 70 © 2018 Pearson Education, Inc.
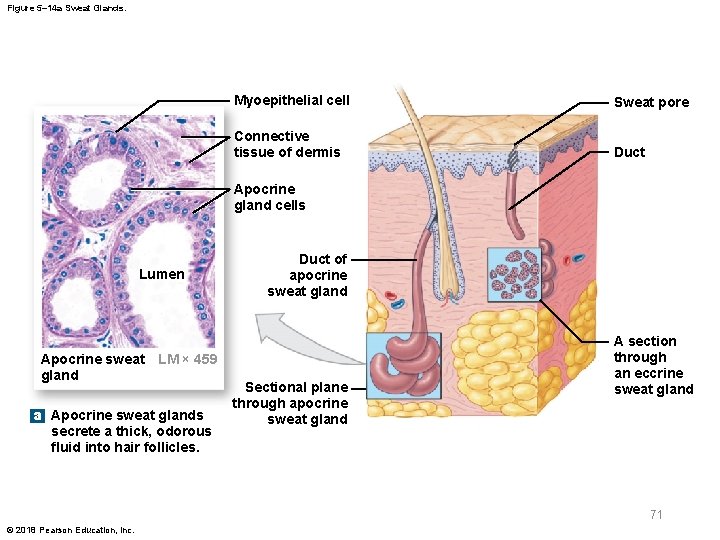
Figure 5– 14 a Sweat Glands. Myoepithelial cell Sweat pore Connective tissue of dermis Duct Apocrine gland cells Lumen Apocrine sweat LM × 459 gland a Apocrine sweat glands secrete a thick, odorous fluid into hair follicles. Duct of apocrine sweat gland Sectional plane through apocrine sweat gland A section through an eccrine sweat gland 71 © 2018 Pearson Education, Inc.
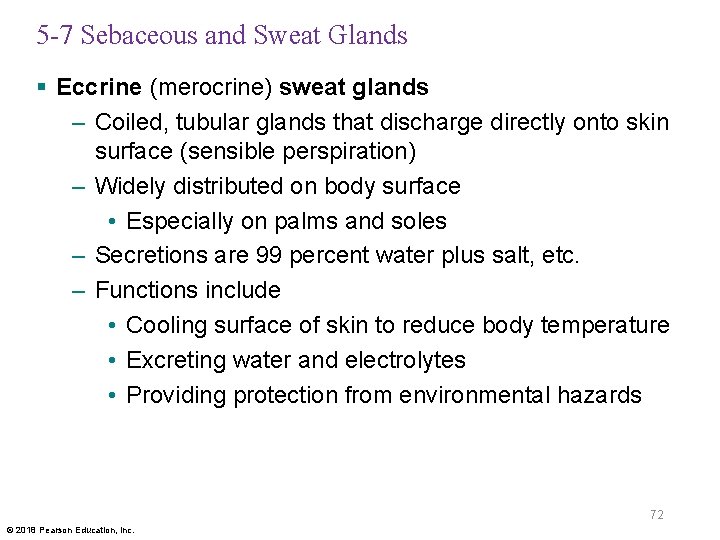
5 -7 Sebaceous and Sweat Glands § Eccrine (merocrine) sweat glands – Coiled, tubular glands that discharge directly onto skin surface (sensible perspiration) – Widely distributed on body surface • Especially on palms and soles – Secretions are 99 percent water plus salt, etc. – Functions include • Cooling surface of skin to reduce body temperature • Excreting water and electrolytes • Providing protection from environmental hazards 72 © 2018 Pearson Education, Inc.
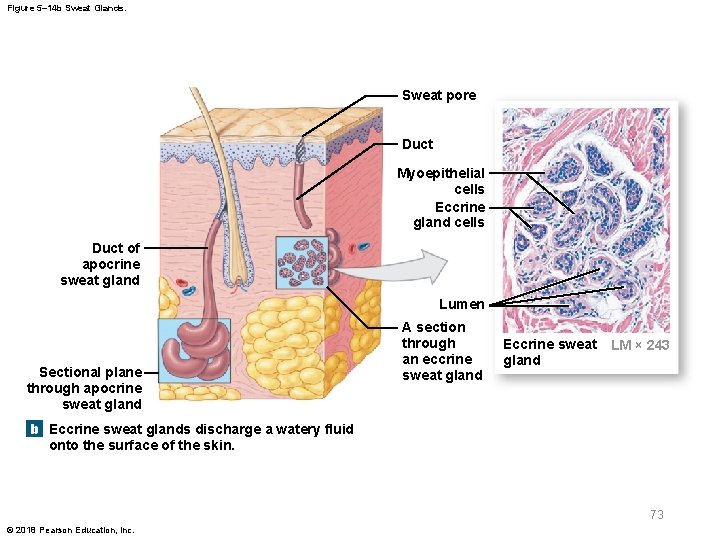
Figure 5– 14 b Sweat Glands. Sweat pore Duct Myoepithelial cells Eccrine gland cells Duct of apocrine sweat gland Lumen Sectional plane through apocrine sweat gland A section through an eccrine sweat gland Eccrine sweat gland LM × 243 b Eccrine sweat glands discharge a watery fluid onto the surface of the skin. 73 © 2018 Pearson Education, Inc.

5 -7 Sebaceous and Sweat Glands § Other integumentary glands – Mammary glands • Produce milk – Ceruminous glands • Produce cerumen (earwax) – Prevents foreign particles from reaching the eardrum 74 © 2018 Pearson Education, Inc.

5 -7 Sebaceous and Sweat Glands § Control of glands – Autonomic nervous system (ANS) • Controls sebaceous and apocrine sweat glands • Affects glands throughout body at once – Eccrine sweat glands • Controlled precisely; sweating may occur locally – Thermoregulation • The main function of sensible perspiration • Eccrine sweat glands work with cardiovascular system to regulate body temperature 75 © 2018 Pearson Education, Inc.
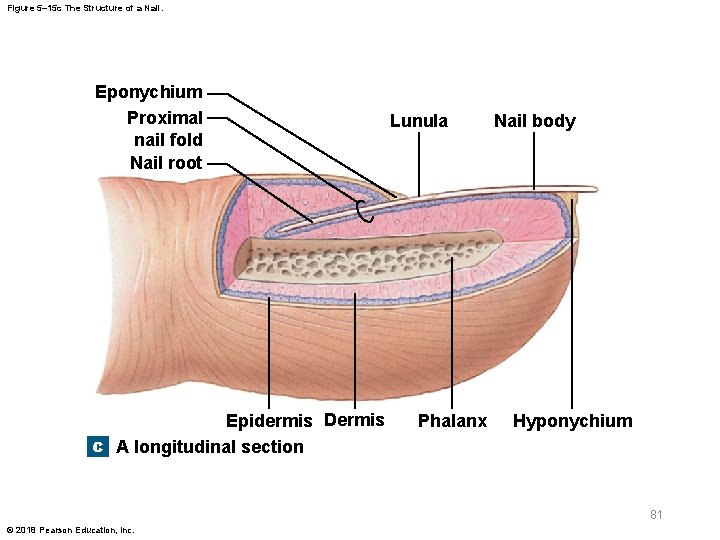
5 -8 Nails § Nails – Protect tips of fingers and toes – Made of dead cells packed with keratin – Metabolic disorders can change nail structure • Example: pitted nails may result from psoriasis 76 © 2018 Pearson Education, Inc.

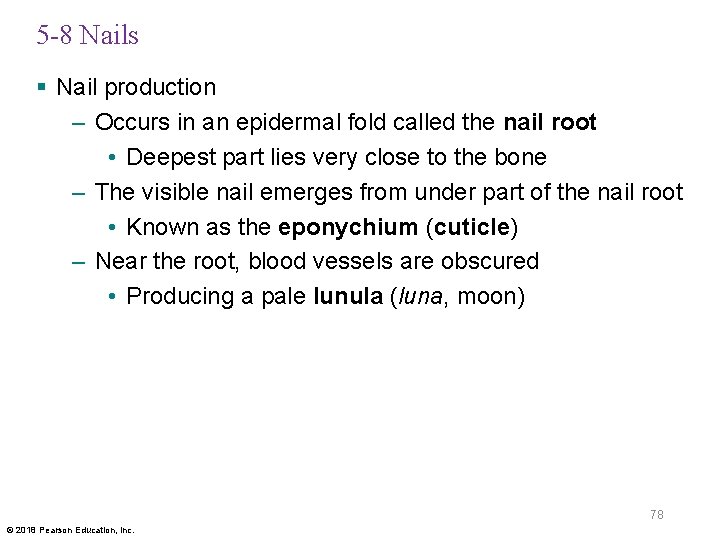
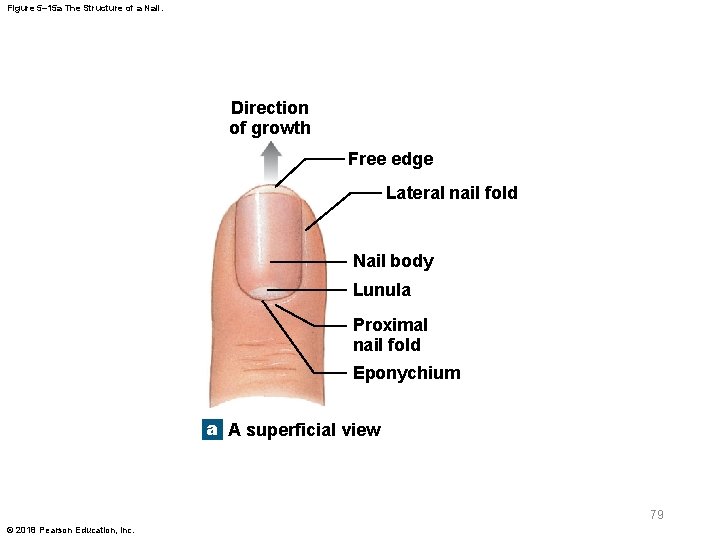
5 -8 Nails § Structure of a nail – Nail body • Visible portion of the nail • Covers the nail bed – Sides of nails • Lie in lateral nail grooves • Surrounded by lateral nail folds – Skin beneath the distal free edge of the nail is the hyponychium (onyx, nail) 77 © 2018 Pearson Education, Inc.
5 -8 Nails § Nail production – Occurs in an epidermal fold called the nail root • Deepest part lies very close to the bone – The visible nail emerges from under part of the nail root • Known as the eponychium (cuticle) – Near the root, blood vessels are obscured • Producing a pale lunula (luna, moon) 78 © 2018 Pearson Education, Inc.
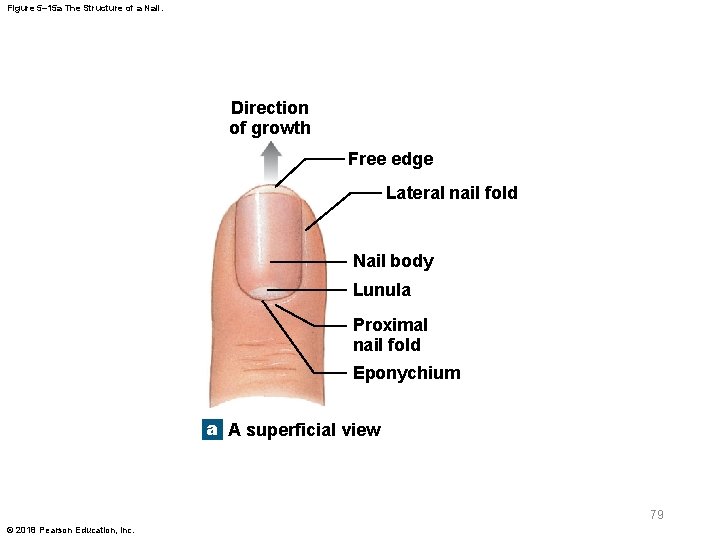
Figure 5– 15 a The Structure of a Nail. Direction of growth Free edge Lateral nail fold Nail body Lunula Proximal nail fold Eponychium a A superficial view 79 © 2018 Pearson Education, Inc.

Figure 5– 15 b The Structure of a Nail. Lateral nail Nail groove body Lateral nail fold Nail bed Phalanx (bone of fingertip) b A cross-sectional view 80 © 2018 Pearson Education, Inc.
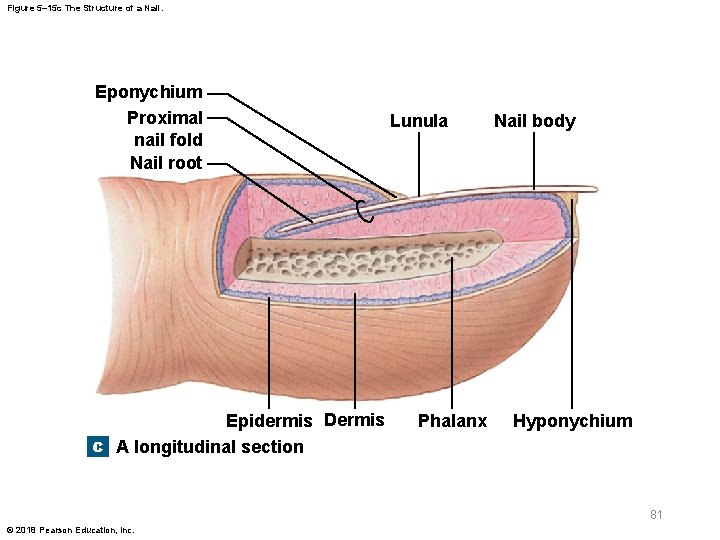
Figure 5– 15 c The Structure of a Nail. Eponychium Proximal nail fold Nail root Epidermis Dermis c A longitudinal section Lunula Phalanx Nail body Hyponychium 81 © 2018 Pearson Education, Inc.
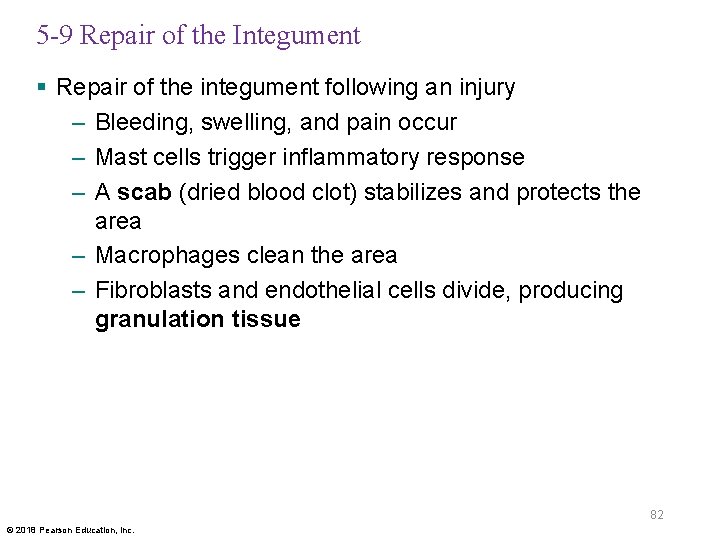
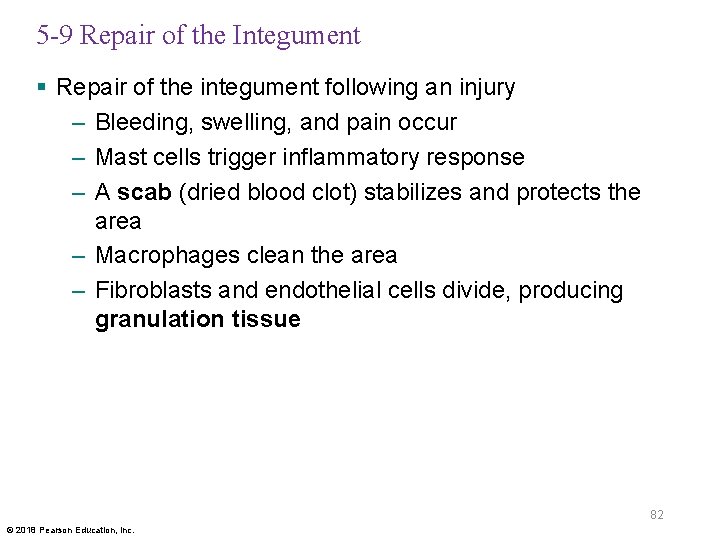
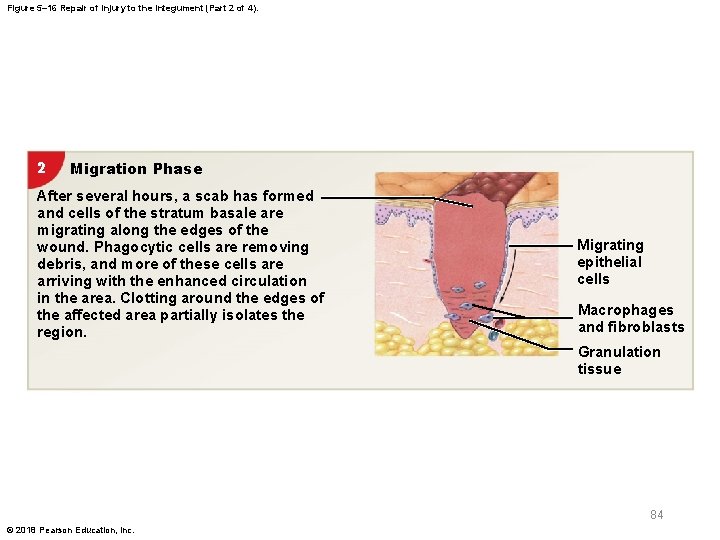
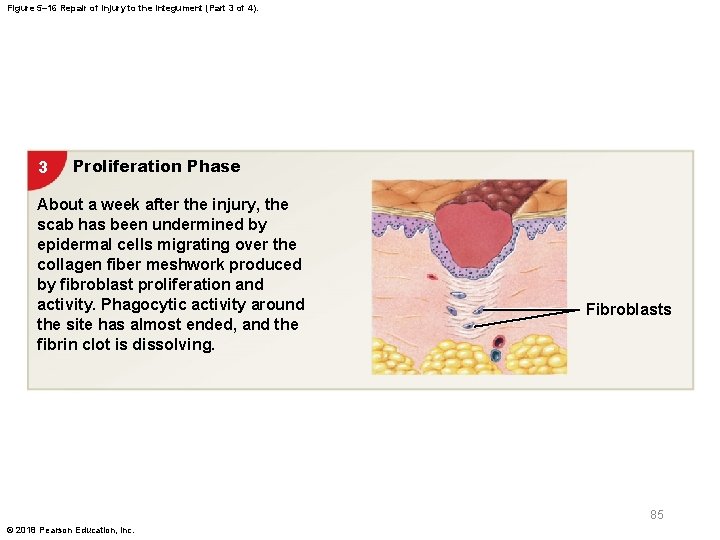
5 -9 Repair of the Integument § Repair of the integument following an injury – Bleeding, swelling, and pain occur – Mast cells trigger inflammatory response – A scab (dried blood clot) stabilizes and protects the area – Macrophages clean the area – Fibroblasts and endothelial cells divide, producing granulation tissue 82 © 2018 Pearson Education, Inc.

Figure 5– 16 Repair of Injury to the Integument (Part 1 of 4). 1 Inflammation Phase Bleeding occurs at the site of injury immediately after the injury, and mast cells in the region trigger an inflammatory response. Epidermis Dermis Mast cells 83 © 2018 Pearson Education, Inc.
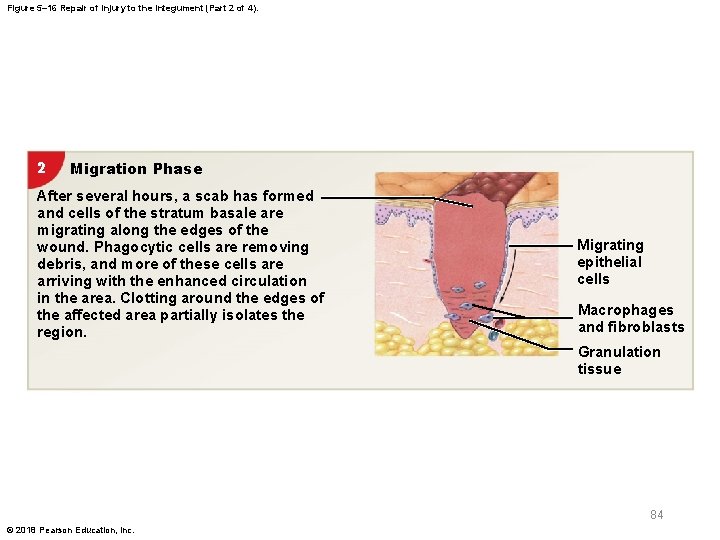
Figure 5– 16 Repair of Injury to the Integument (Part 2 of 4). 2 Migration Phase After several hours, a scab has formed and cells of the stratum basale are migrating along the edges of the wound. Phagocytic cells are removing debris, and more of these cells are arriving with the enhanced circulation in the area. Clotting around the edges of the affected area partially isolates the region. Migrating epithelial cells Macrophages and fibroblasts Granulation tissue 84 © 2018 Pearson Education, Inc.
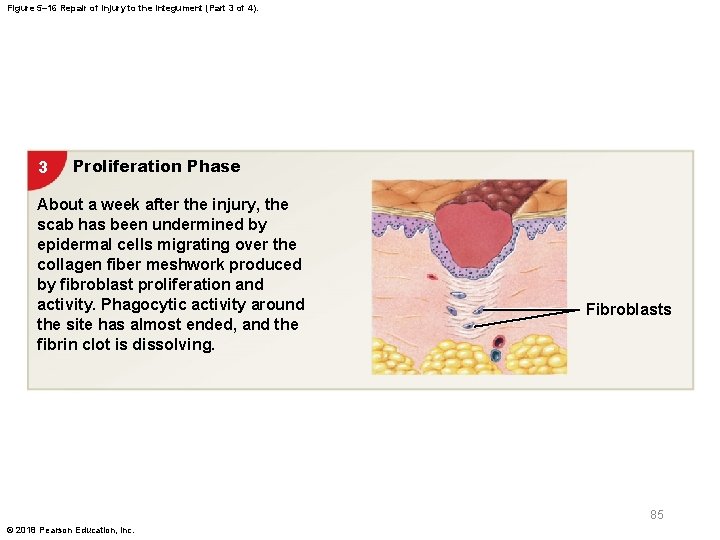
Figure 5– 16 Repair of Injury to the Integument (Part 3 of 4). 3 Proliferation Phase About a week after the injury, the scab has been undermined by epidermal cells migrating over the collagen fiber meshwork produced by fibroblast proliferation and activity. Phagocytic activity around the site has almost ended, and the fibrin clot is dissolving. Fibroblasts 85 © 2018 Pearson Education, Inc.
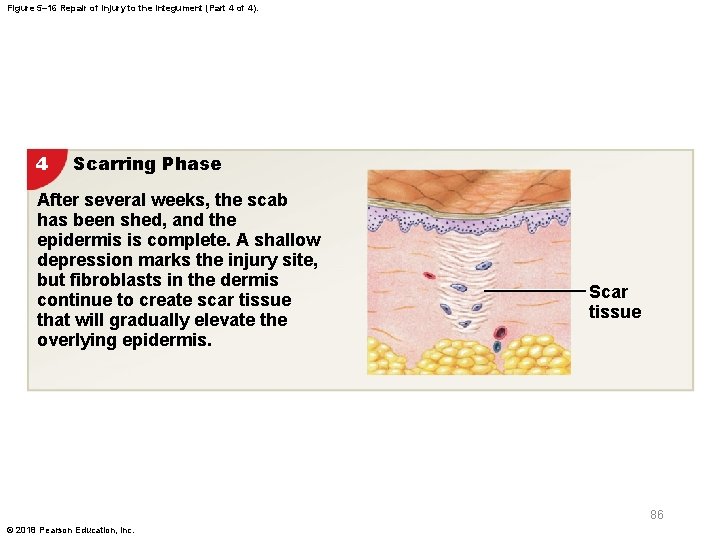
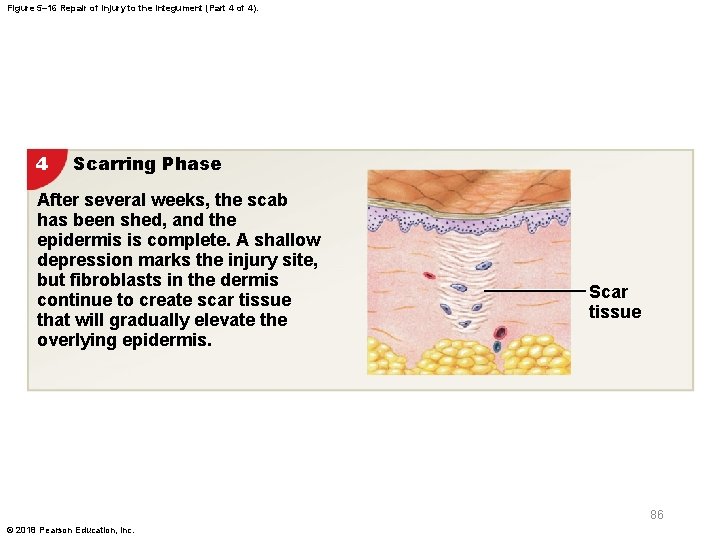
Figure 5– 16 Repair of Injury to the Integument (Part 4 of 4). 4 Scarring Phase After several weeks, the scab has been shed, and the epidermis is complete. A shallow depression marks the injury site, but fibroblasts in the dermis continue to create scar tissue that will gradually elevate the overlying epidermis. Scar tissue 86 © 2018 Pearson Education, Inc.
5 -9 Repair of the Integument § Repair of the integument following an injury – Clot begins to dissolve – Number of capillaries declines – Noncellular scar tissue is produced • A raised keloid may form 87 © 2018 Pearson Education, Inc.

Figure 5– 17 A Keloid. 88 © 2018 Pearson Education, Inc.
5 -10 Aging and the Integumentary System § Effects of aging on skin – Epidermis thins – Number of dendritic cells decreases – Vitamin D 3 production declines – Melanocyte and glandular activities decline – Blood supply to dermis is reduced – Function of hair follicles declines – Dermis thins and elastic fiber network shrinks – Sex-specific hair and body fat distribution fades – Repair rate slows 89 © 2018 Pearson Education, Inc.
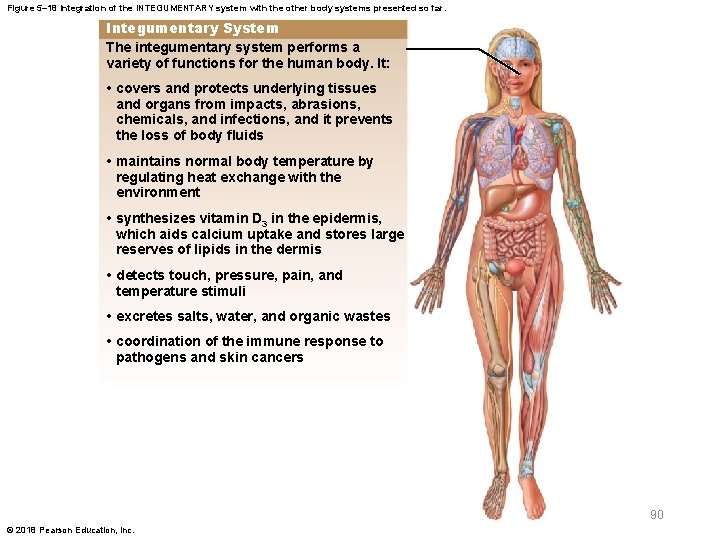
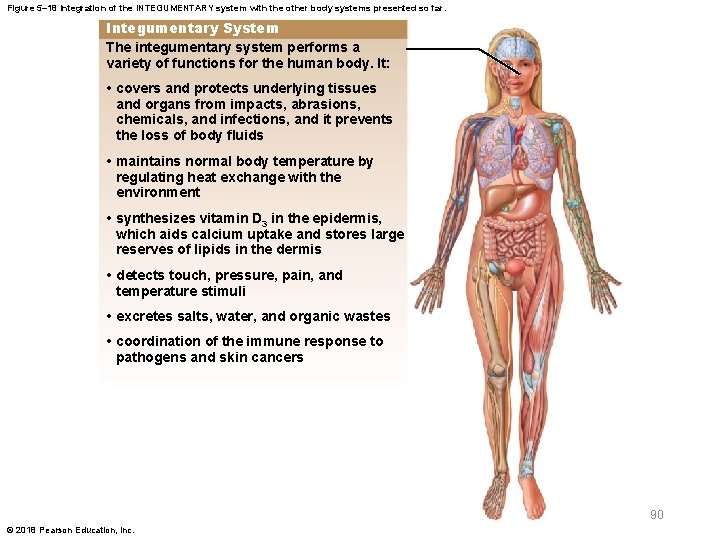
Figure 5– 18 Integration of the INTEGUMENTARY system with the other body systems presented so far. Integumentary System The integumentary system performs a variety of functions for the human body. It: • covers and protects underlying tissues and organs from impacts, abrasions, chemicals, and infections, and it prevents the loss of body fluids • maintains normal body temperature by regulating heat exchange with the environment • synthesizes vitamin D 3 in the epidermis, which aids calcium uptake and stores large reserves of lipids in the dermis • detects touch, pressure, pain, and temperature stimuli • excretes salts, water, and organic wastes • coordination of the immune response to pathogens and skin cancers 90 © 2018 Pearson Education, Inc.
 Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Eleventh edition management
Eleventh edition management Management eleventh edition
Management eleventh edition Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Paratubular cyst
Paratubular cyst Chapter 14 anatomy and physiology
Chapter 14 anatomy and physiology Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Heat and cold
Heat and cold Anatomy and physiology coloring workbook chapter 14
Anatomy and physiology coloring workbook chapter 14 Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Necessary life functions anatomy and physiology
Necessary life functions anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Gi tract histology
Gi tract histology Distal and proximal
Distal and proximal Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Male vs female skeleton pelvis
Male vs female skeleton pelvis Chapter 6 general anatomy and physiology
Chapter 6 general anatomy and physiology Cranial cephalic
Cranial cephalic Chadha committee
Chadha committee Eleventh 5 year plan
Eleventh 5 year plan Thfive
Thfive For his eleventh birthday elvis presley
For his eleventh birthday elvis presley Physiology of sport and exercise 5th edition
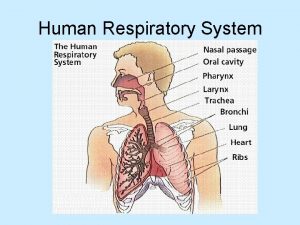
Physiology of sport and exercise 5th edition Upper respiratory system
Upper respiratory system Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Structure anatomy and physiology in agriculture
Structure anatomy and physiology in agriculture Anatomy and physiology of bone
Anatomy and physiology of bone Duodenal ulcer anatomy
Duodenal ulcer anatomy Liver anatomy and physiology
Liver anatomy and physiology Difference between anatomy and physiology
Difference between anatomy and physiology Epigastric vs hypogastric
Epigastric vs hypogastric Anatomy and physiology of rbc
Anatomy and physiology of rbc Http://anatomy and physiology
Http://anatomy and physiology Physiology of appendicitis
Physiology of appendicitis Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Agriscience unit 26 self evaluation answers
Agriscience unit 26 self evaluation answers Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Physiology of stomach ppt
Physiology of stomach ppt Anatomy and physiology of diabetes
Anatomy and physiology of diabetes Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Anatomy and physiology
Anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Human physiology exam 1
Human physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Anatomy and physiology of the foot
Anatomy and physiology of the foot Skin cancer
Skin cancer Pse4u
Pse4u Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Body landmarks diagram
Body landmarks diagram Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 10-1 blood
Figure 10-1 blood Anatomy histology
Anatomy histology Anatomy and physiology of eye
Anatomy and physiology of eye Principles of anatomy and physiology tortora
Principles of anatomy and physiology tortora Irn.org anatomy and physiology
Irn.org anatomy and physiology Anatomy and physiology body parts
Anatomy and physiology body parts Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition Figure 14-1 digestive system
Figure 14-1 digestive system Anatomy and physiology of the retina
Anatomy and physiology of the retina Animal tissue
Animal tissue Anatomy and physiology of meningitis ppt
Anatomy and physiology of meningitis ppt Jeopardy anatomy and physiology game
Jeopardy anatomy and physiology game What is homeostasis
What is homeostasis Anatomy and physiology
Anatomy and physiology Respiratory system
Respiratory system Physiology trivia
Physiology trivia