Fundamentals of Anatomy Physiology Eleventh Edition Chapter 26











































- Slides: 150
Fundamentals of Anatomy & Physiology Eleventh Edition Chapter 26 The Urinary System Lecture Presentation by Deborah A. Hutchinson Seattle University © 2018 Pearson Education, Inc.
Introduction to the Urinary System § Urinary system – Removes most metabolic wastes produced by body’s cells – Kidneys remove metabolic wastes from circulation • Produce urine 2 © 2018 Pearson Education, Inc.

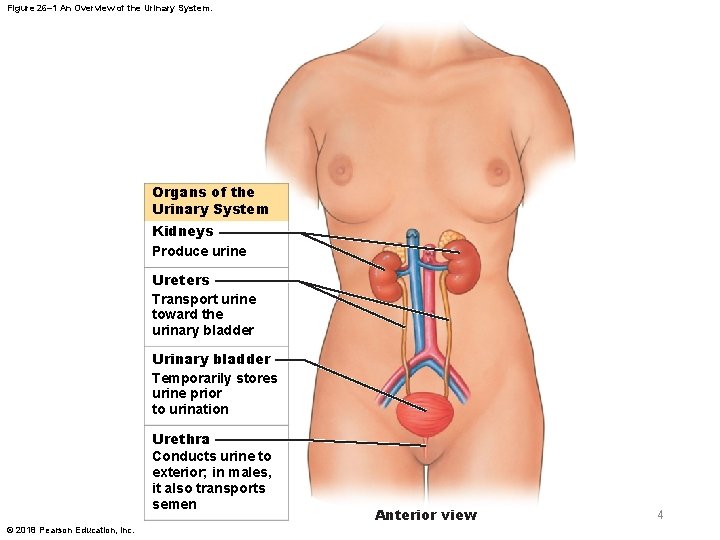
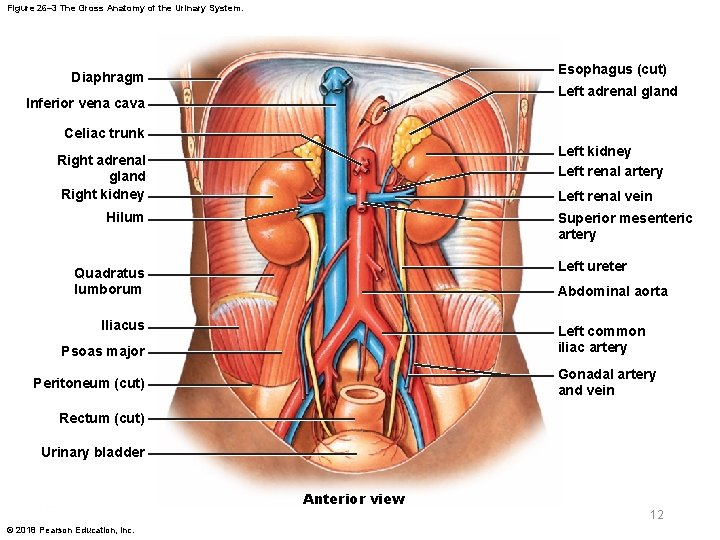
26 -1 Organs and Functions of Urinary System § Organs of urinary system – Kidneys—paired organs that produce urine – Urinary tract—eliminates urine • Ureters (paired tubes) • Urinary bladder (muscular sac) • Urethra (exit tube) – Urination or micturition—process of eliminating urine • Contraction of muscular urinary bladder forces urine through urethra, and out of body 3 © 2018 Pearson Education, Inc.
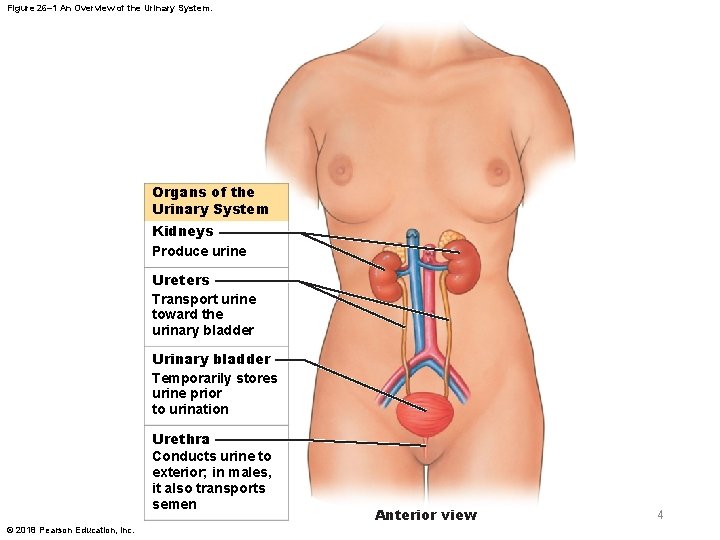
Figure 26– 1 An Overview of the Urinary System. Organs of the Urinary System Kidneys Produce urine Ureters Transport urine toward the urinary bladder Urinary bladder Temporarily stores urine prior to urination Urethra Conducts urine to exterior; in males, it also transports semen © 2018 Pearson Education, Inc. Anterior view 4

26 -1 Organs and Functions of Urinary System § Three functions of urinary system – Excretion • Removal of metabolic wastes from body fluids – Elimination • Discharge of wastes from body – Homeostatic regulation • Of volume and solute concentration of blood 5 © 2018 Pearson Education, Inc.

26 -1 Organs and Functions of Urinary System § Homeostatic functions of urinary system – Regulating blood volume and blood pressure • By adjusting volume of water lost in urine • Releasing erythropoietin and renin – Regulating plasma ion concentrations • By controlling quantities of sodium, potassium, chloride, and other ions lost in urine • Calcium ion level controlled through synthesis of calcitriol 6 © 2018 Pearson Education, Inc.
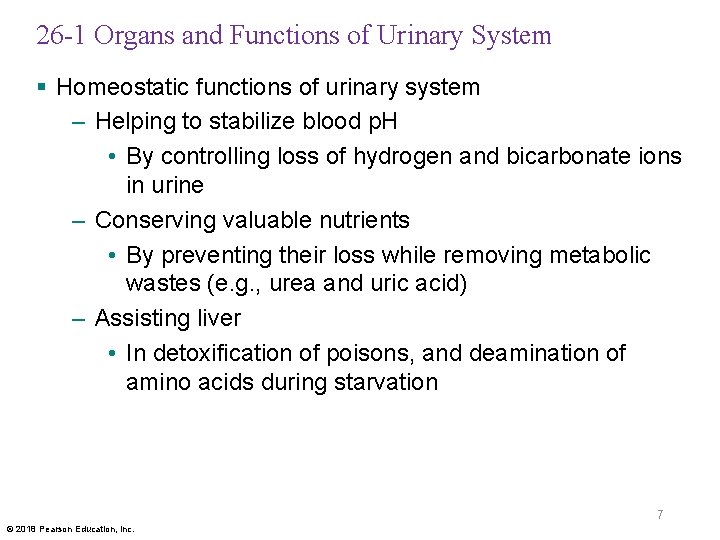
26 -1 Organs and Functions of Urinary System § Homeostatic functions of urinary system – Helping to stabilize blood p. H • By controlling loss of hydrogen and bicarbonate ions in urine – Conserving valuable nutrients • By preventing their loss while removing metabolic wastes (e. g. , urea and uric acid) – Assisting liver • In detoxification of poisons, and deamination of amino acids during starvation 7 © 2018 Pearson Education, Inc.
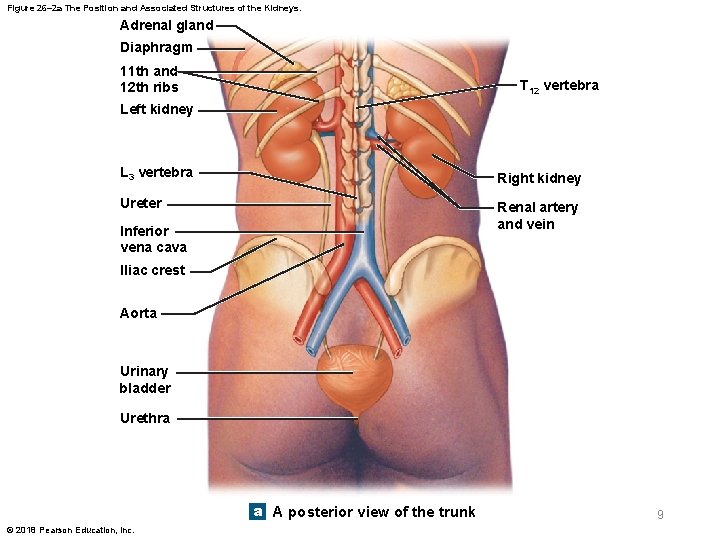
26 -2 The Kidneys and Nephrons § Kidneys – Located on either side of vertebral column – Left kidney is slightly superior to right kidney – Superior surface is capped by adrenal gland – Position is maintained by • Overlying peritoneum • Contact with adjacent visceral organs • Supporting connective tissues 8 © 2018 Pearson Education, Inc.
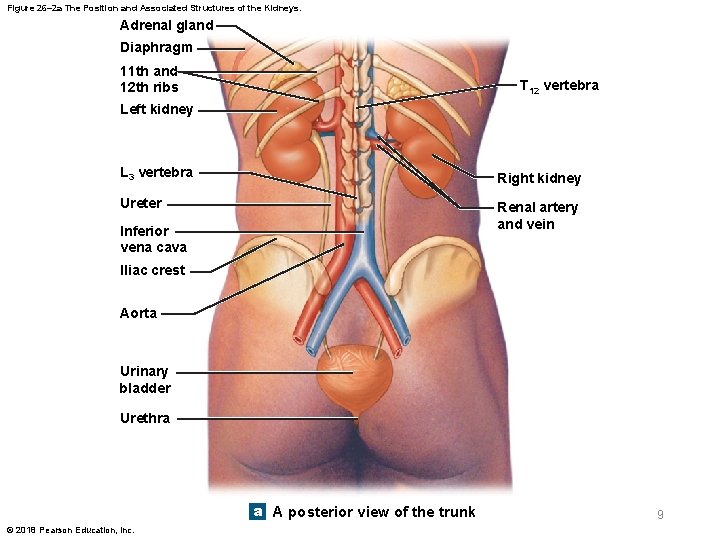
Figure 26– 2 a The Position and Associated Structures of the Kidneys. Adrenal gland Diaphragm 11 th and 12 th ribs T 12 vertebra Left kidney L 3 vertebra Right kidney Ureter Renal artery and vein Inferior vena cava Iliac crest Aorta Urinary bladder Urethra a A posterior view of the trunk © 2018 Pearson Education, Inc. 9
26 -2 The Kidneys and Nephrons § Kidneys are protected and stabilized by 3 layers 1. Fibrous capsule • A layer of collagen fibers • Covers outer surface of entire organ 2. Perinephric fat • A thick layer of adipose tissue • Surrounds fibrous capsule 3. Renal fascia • A dense, fibrous outer layer • Anchors kidney to surrounding structures 10 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Typical adult kidney – About 10 cm long, 5. 5 cm wide, and 3 cm thick – Weighs about 150 g § Hilum – Prominent medial indentation – Point of entry for renal artery and renal nerves – Point of exit for renal vein and ureter 11 © 2018 Pearson Education, Inc.
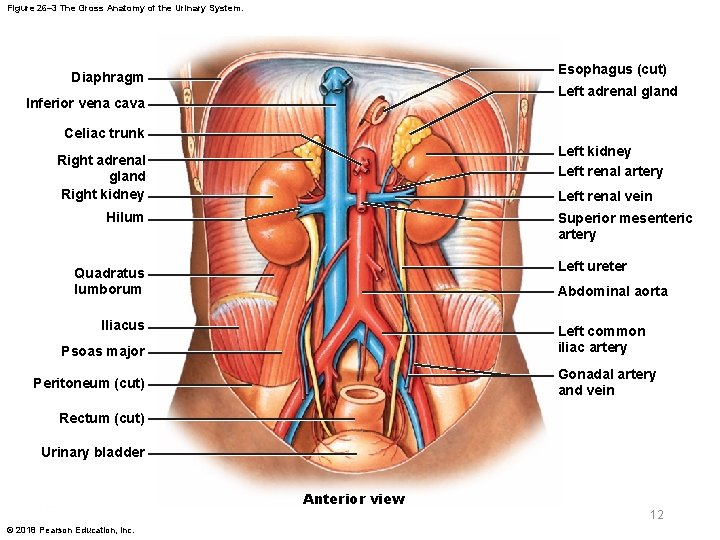
Figure 26– 3 The Gross Anatomy of the Urinary System. Esophagus (cut) Diaphragm Left adrenal gland Inferior vena cava Celiac trunk Left kidney Left renal artery Right adrenal gland Right kidney Left renal vein Hilum Superior mesenteric artery Left ureter Quadratus lumborum Abdominal aorta Iliacus Left common iliac artery Psoas major Gonadal artery and vein Peritoneum (cut) Rectum (cut) Urinary bladder Anterior view 12 © 2018 Pearson Education, Inc.

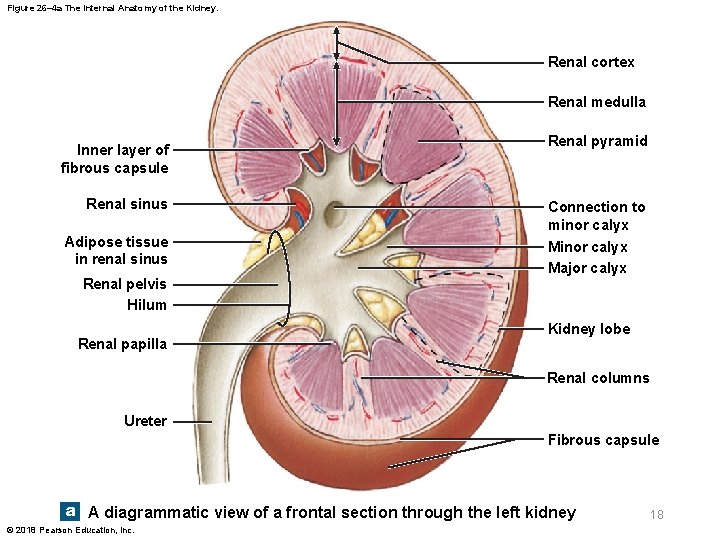
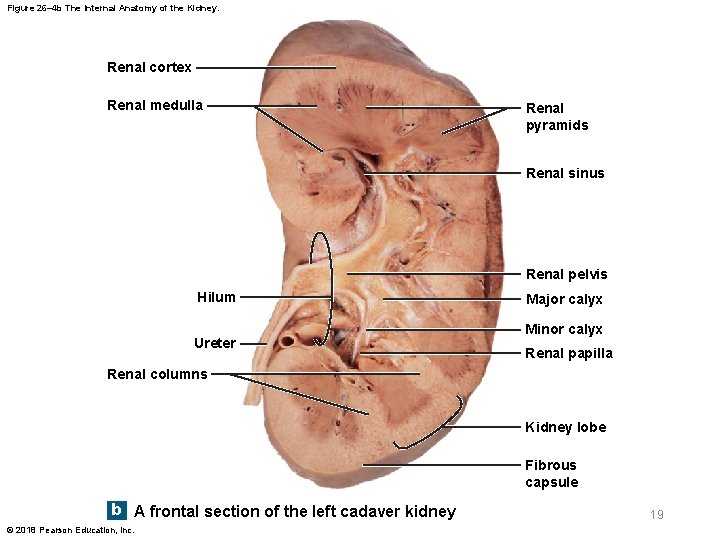
26 -2 The Kidneys and Nephrons § Renal sinus – Internal cavity within kidney – Lined by fibrous capsule • Bound to outer surfaces of structures in renal sinus • Stabilizes positions of ureter, renal blood vessels, and nerves 13 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Renal cortex – Superficial region of kidney in contact with fibrous capsule – Reddish-brown and granular § Renal pyramids – 6 to 18 triangular structures in renal medulla • Base of each pyramid abuts cortex • Tip (renal papilla) projects into renal sinus 14 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Renal columns – Bands of cortical tissue that separate adjacent renal pyramids – Extend into medulla – Have distinct granular texture 15 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Kidney lobe – Consists of • A renal pyramid • Overlying area of renal cortex • Adjacent tissues of renal columns – Produces urine 16 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Ducts within each renal papilla – Discharge urine into a minor calyx, a cup-shaped drain § Major calyx – Formed by four or five minor calyces § Renal pelvis – Large, funnel-shaped chamber – Formed by two or three major calyces – Fills most of renal sinus – Connected to ureter, which drains kidney 17 © 2018 Pearson Education, Inc.
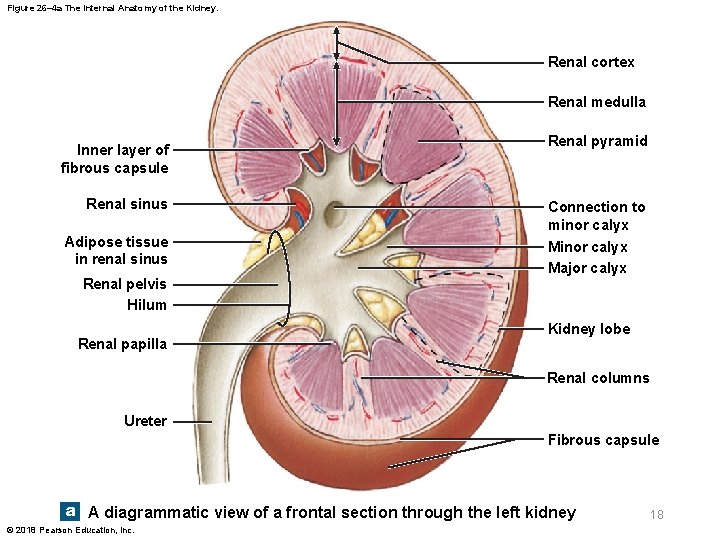
Figure 26– 4 a The Internal Anatomy of the Kidney. Renal cortex Renal medulla Inner layer of fibrous capsule Renal sinus Adipose tissue in renal sinus Renal pelvis Hilum Renal papilla Renal pyramid Connection to minor calyx Major calyx Kidney lobe Renal columns Ureter Fibrous capsule a A diagrammatic view of a frontal section through the left kidney © 2018 Pearson Education, Inc. 18
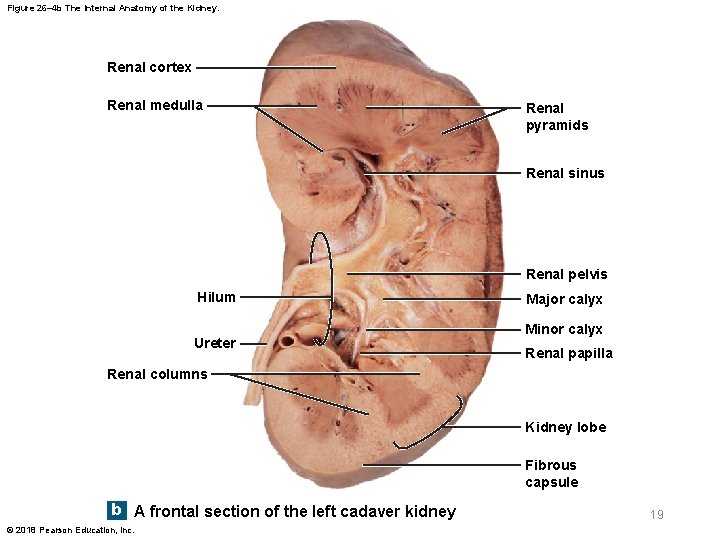
Figure 26– 4 b The Internal Anatomy of the Kidney. Renal cortex Renal medulla Renal pyramids Renal sinus Renal pelvis Hilum Ureter Major calyx Minor calyx Renal papilla Renal columns Kidney lobe Fibrous capsule b A frontal section of the left cadaver kidney © 2018 Pearson Education, Inc. 19
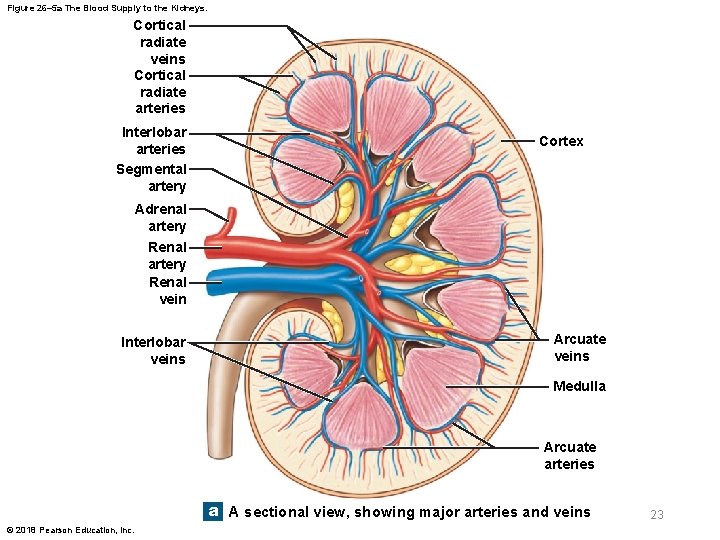
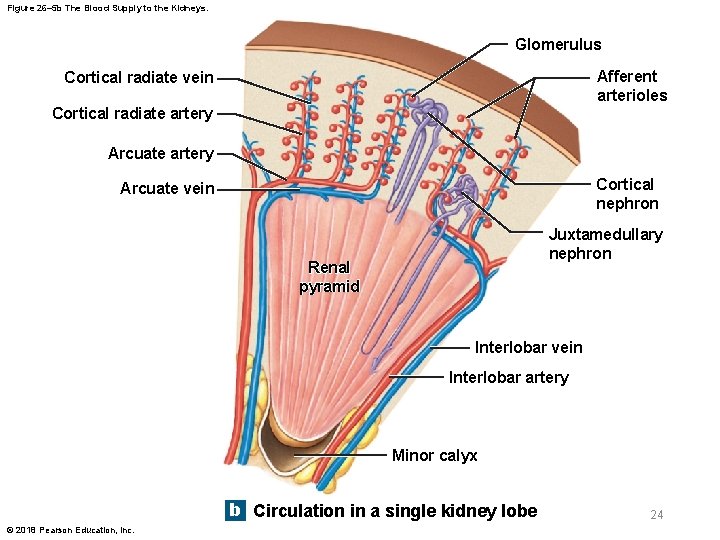
26 -2 The Kidneys and Nephrons § Blood supply to kidneys – Kidneys receive 20– 25 percent of total cardiac output – About 1200 m. L of blood flow through kidneys each minute – Each kidney receives blood through a renal artery 20 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Segmental arteries – Receive blood from renal artery – Divide into interlobar arteries • Radiate outward through renal columns between renal pyramids – Interlobar arteries supply blood to arcuate arteries • Arch along boundary between cortex and medulla of kidney 21 © 2018 Pearson Education, Inc.
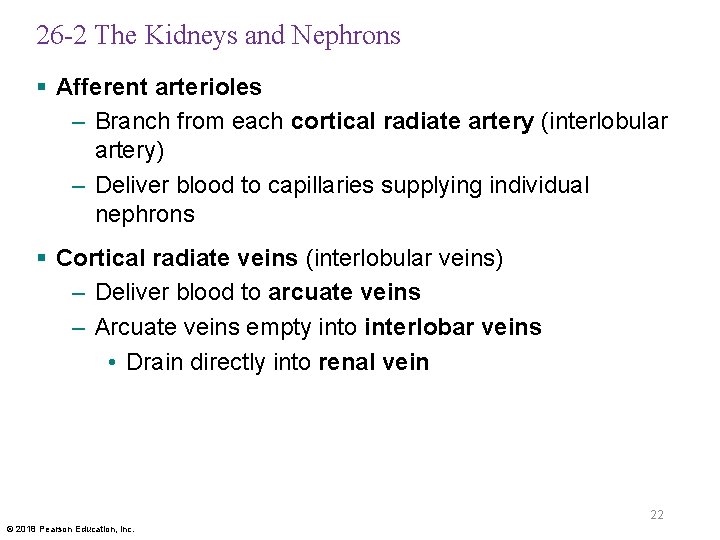
26 -2 The Kidneys and Nephrons § Afferent arterioles – Branch from each cortical radiate artery (interlobular artery) – Deliver blood to capillaries supplying individual nephrons § Cortical radiate veins (interlobular veins) – Deliver blood to arcuate veins – Arcuate veins empty into interlobar veins • Drain directly into renal vein 22 © 2018 Pearson Education, Inc.
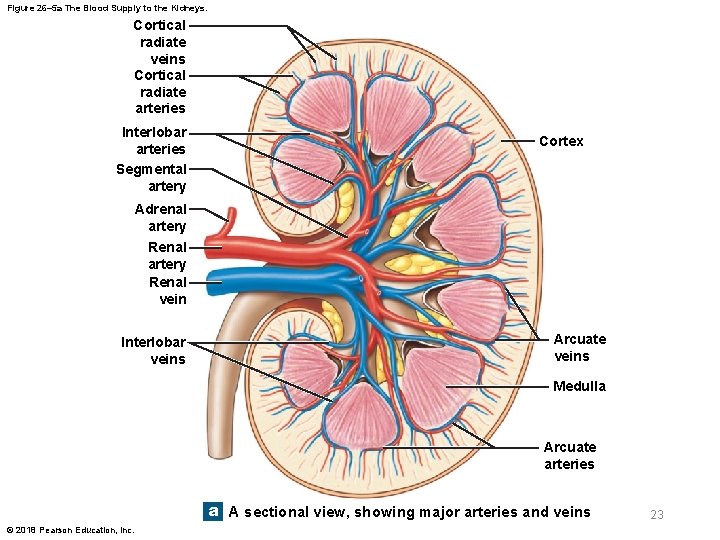
Figure 26– 5 a The Blood Supply to the Kidneys. Cortical radiate veins Cortical radiate arteries Interlobar arteries Segmental artery Cortex Adrenal artery Renal vein Interlobar veins Arcuate veins Medulla Arcuate arteries a A sectional view, showing major arteries and veins © 2018 Pearson Education, Inc. 23
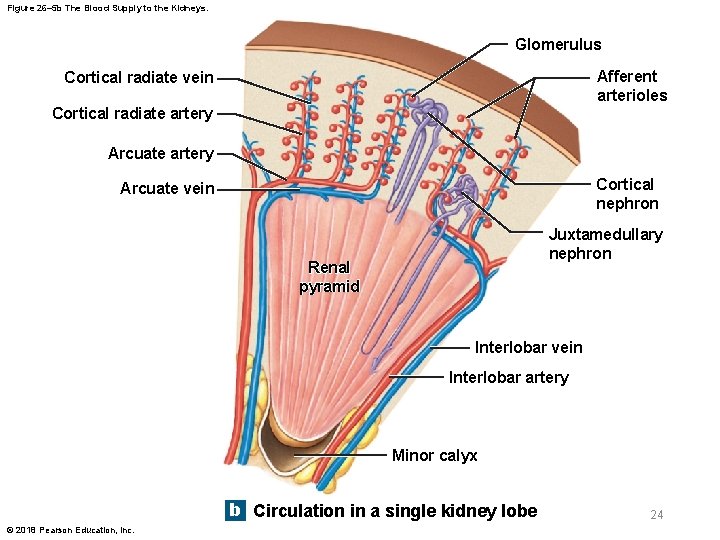
Figure 26– 5 b The Blood Supply to the Kidneys. Glomerulus Afferent arterioles Cortical radiate vein Cortical radiate artery Arcuate artery Cortical nephron Arcuate vein Juxtamedullary nephron Renal pyramid Interlobar vein Interlobar artery Minor calyx b Circulation in a single kidney lobe © 2018 Pearson Education, Inc. 24

Figure 26– 5 c The Blood Supply to the Kidneys. Renal vein Renal artery Segmental artery Interlobar vein Interlobar artery Arcuate vein Arcuate artery Cortical radiate vein Cortical radiate artery Venule Afferent arteriole NEPHRON Peritubular Glomerulus capillaries Efferent arteriole c A flowchart of renal circulation © 2018 Pearson Education, Inc. 25

26 -2 The Kidneys and Nephrons § Renal nerves – Innervate kidneys and ureters – Enter each kidney at hilum – Follow branches of renal arteries to individual nephrons § Sympathetic innervation – Adjusts rate of urine formation • By changing blood flow at nephron – Influences urine composition • By stimulating release of renin 26 © 2018 Pearson Education, Inc.
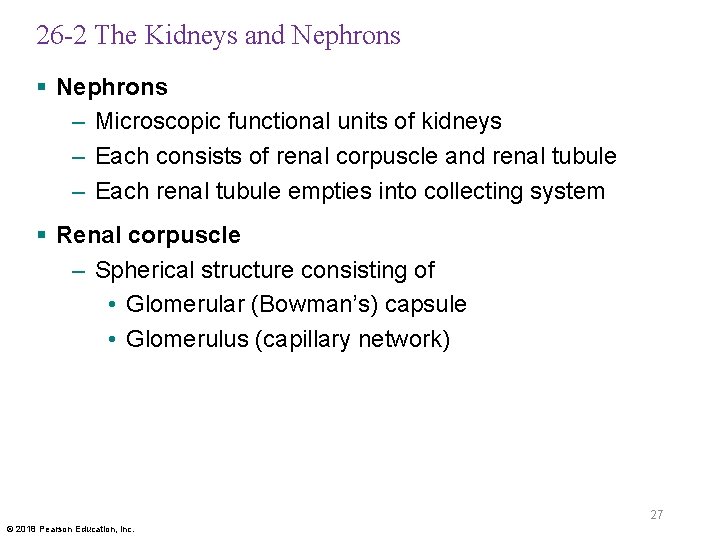
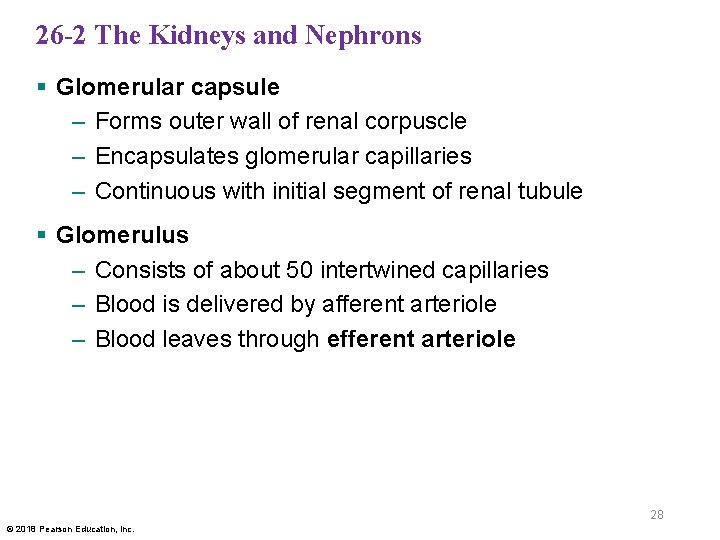
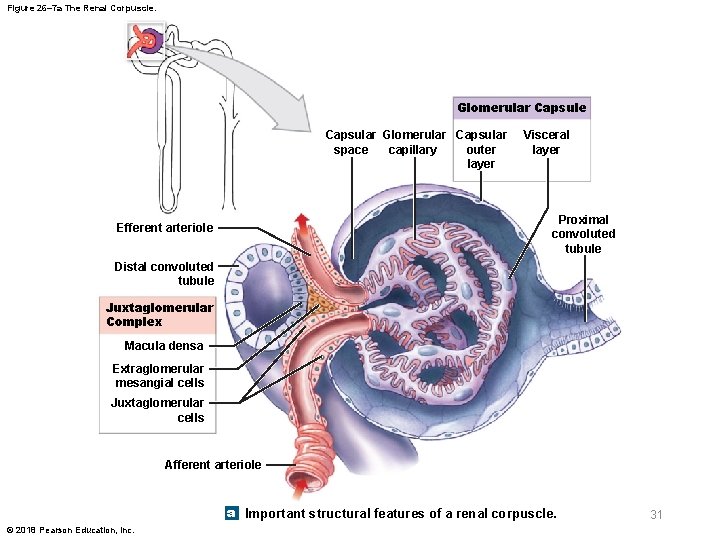
26 -2 The Kidneys and Nephrons § Nephrons – Microscopic functional units of kidneys – Each consists of renal corpuscle and renal tubule – Each renal tubule empties into collecting system § Renal corpuscle – Spherical structure consisting of • Glomerular (Bowman’s) capsule • Glomerulus (capillary network) 27 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Glomerular capsule – Forms outer wall of renal corpuscle – Encapsulates glomerular capillaries – Continuous with initial segment of renal tubule § Glomerulus – Consists of about 50 intertwined capillaries – Blood is delivered by afferent arteriole – Blood leaves through efferent arteriole 28 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Glomerular capsule – Capsular outer layer • Simple squamous epithelium – Visceral layer • Covers glomerular capillaries – Capsular space • Separates two layers 29 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Podocytes – Large cells of visceral layer – Have complex foot processes (pedicels) that wrap around glomerular capillaries – Filtration slits • Narrow (6– 9 nm wide) gaps between adjacent foot processes 30 © 2018 Pearson Education, Inc.
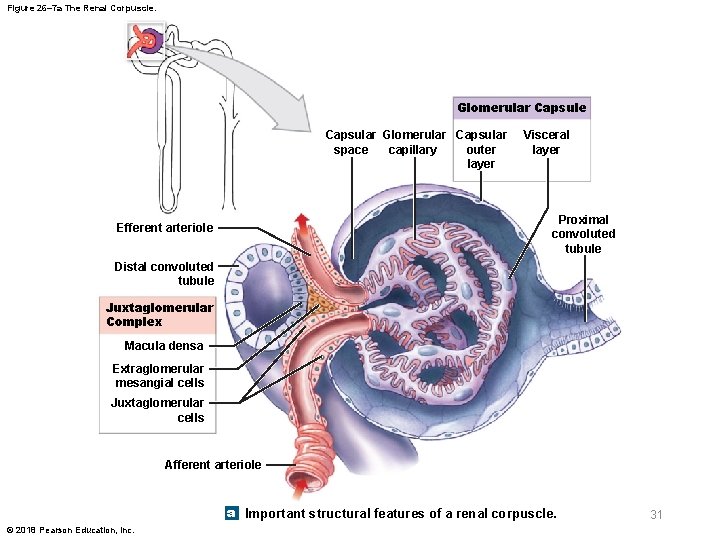
Figure 26– 7 a The Renal Corpuscle. Glomerular Capsule Capsular Glomerular Capsular outer space capillary layer Visceral layer Proximal convoluted tubule Efferent arteriole Distal convoluted tubule Juxtaglomerular Complex Macula densa Extraglomerular mesangial cells Juxtaglomerular cells Afferent arteriole a Important structural features of a renal corpuscle. © 2018 Pearson Education, Inc. 31

26 -2 The Kidneys and Nephrons § Filtration membrane – Consists of • Fenestrated endothelium • Basement membrane • Foot processes of podocytes – During filtration in renal corpuscle • Blood pressure forces water and small solutes across membrane into capsular space • Larger solutes (e. g. , plasma proteins) do not pass • Solution produced is essentially protein-free filtrate 32 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Renal tubule – Two convoluted segments • Proximal convoluted tubule (PCT) • Distal convoluted tubule (DCT) – Segments are separated by nephron loop (loop of Henle) • U-shaped tube • Extends at least partially into medulla 33 © 2018 Pearson Education, Inc.

26 -2 The Kidneys and Nephrons § Renal tubule – While traveling along tubule, the tubular fluid (filtrate) gradually changes in composition • Due to substances being reabsorbed or secreted in various segments of nephron 34 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Proximal convoluted tubule (PCT) – First segment of renal tubule – Entrance to PCT lies opposite of connection of afferent and efferent arterioles with glomerulus – Simple cuboidal epithelium • Microvilli on apical surfaces – Primary function is reabsorption of ions 35 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Nephron loop – Descending limb • Fluid flows toward renal pelvis – Ascending limb • Fluid flows toward renal cortex – Segments of limbs have thick or thin epithelia • Descending thin limb (DTL) • Ascending thin limb (ATL) • Thick ascending limb (TAL) 36 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Distal convoluted tubule (DCT) – Third segment of renal tubule – Initial portion passes between afferent and efferent arterioles – Smaller luminal diameter than PCT – Epithelial cells lack microvilli – Primary function is to reabsorb water and selected ions • Actively secretes undesirable substances 37 © 2018 Pearson Education, Inc.
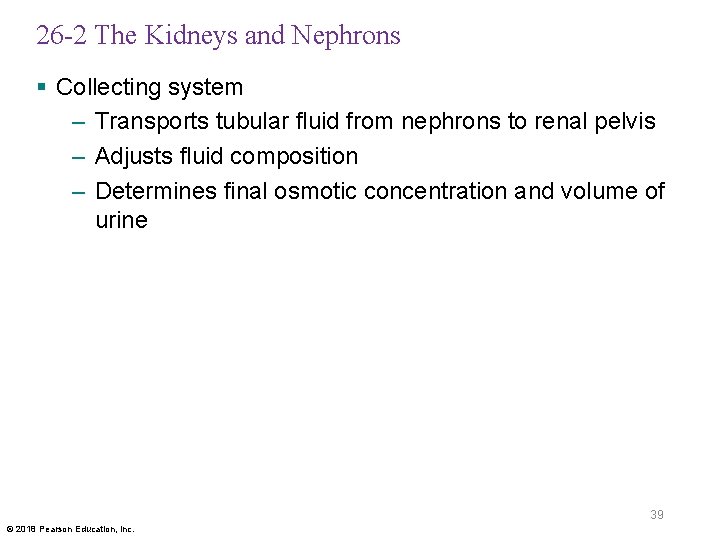
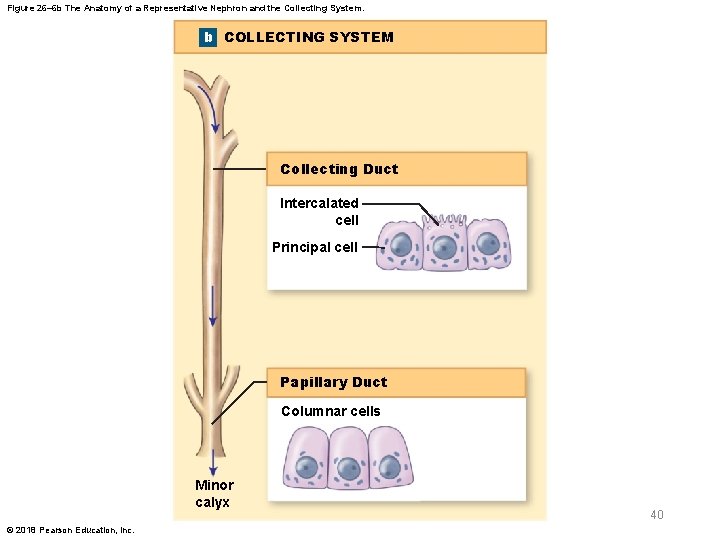
26 -2 The Kidneys and Nephrons § Collecting system – A series of tubes that carries tubular fluid away from nephrons – Collecting ducts • Receive fluid from many nephrons – Each collecting duct • Begins in cortex • Descends into medulla • Carries fluid to papillary duct, which drains into a minor calyx 38 © 2018 Pearson Education, Inc.
26 -2 The Kidneys and Nephrons § Collecting system – Transports tubular fluid from nephrons to renal pelvis – Adjusts fluid composition – Determines final osmotic concentration and volume of urine 39 © 2018 Pearson Education, Inc.
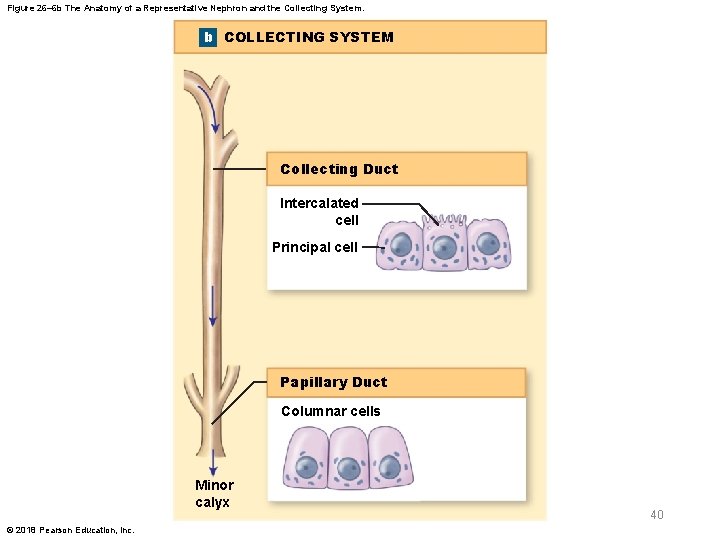
Figure 26– 6 b The Anatomy of a Representative Nephron and the Collecting System. b COLLECTING SYSTEM Collecting Duct Intercalated cell Principal cell Papillary Duct Columnar cells Minor calyx © 2018 Pearson Education, Inc. 40
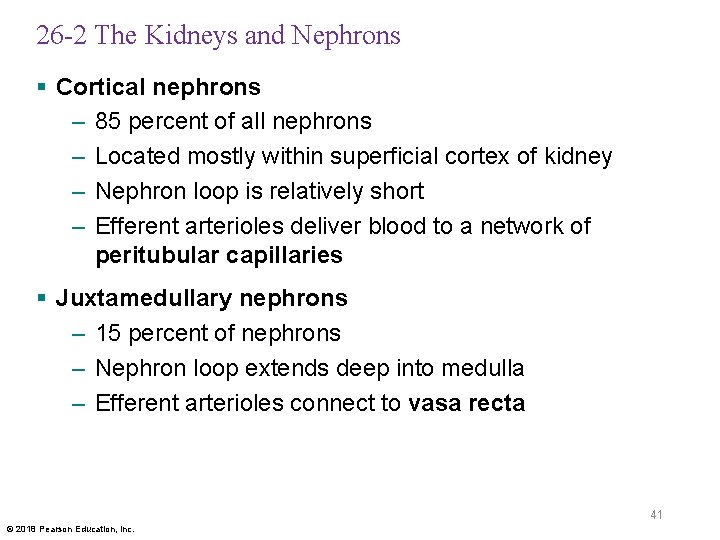
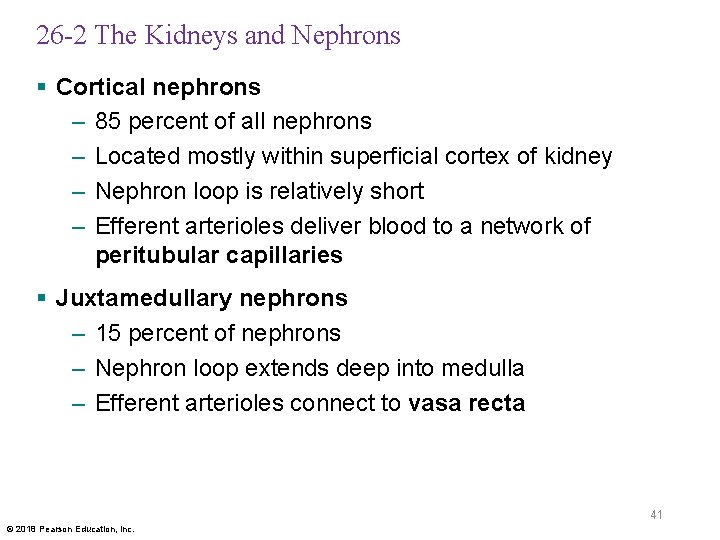
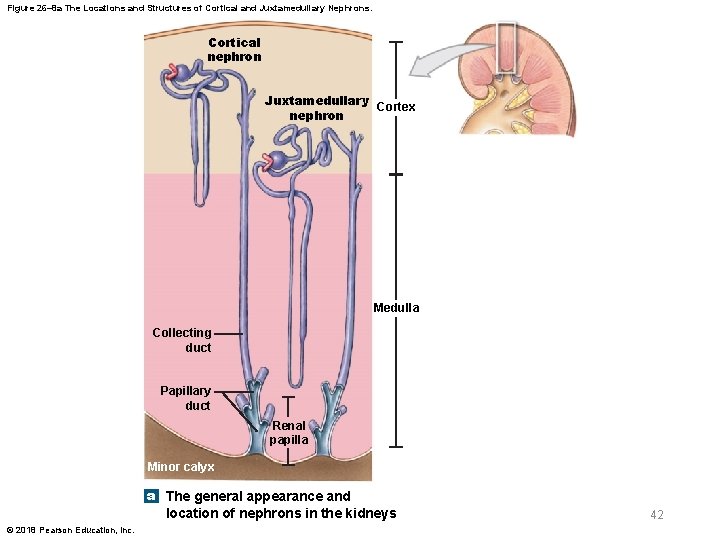
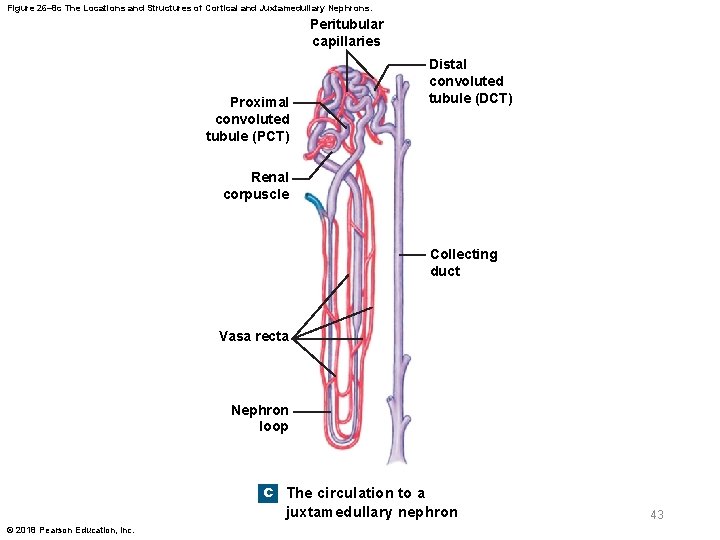
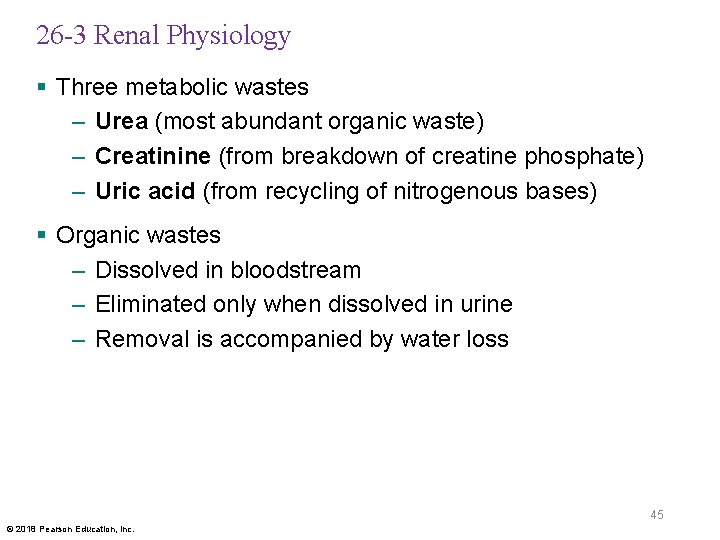
26 -2 The Kidneys and Nephrons § Cortical nephrons – 85 percent of all nephrons – Located mostly within superficial cortex of kidney – Nephron loop is relatively short – Efferent arterioles deliver blood to a network of peritubular capillaries § Juxtamedullary nephrons – 15 percent of nephrons – Nephron loop extends deep into medulla – Efferent arterioles connect to vasa recta 41 © 2018 Pearson Education, Inc.
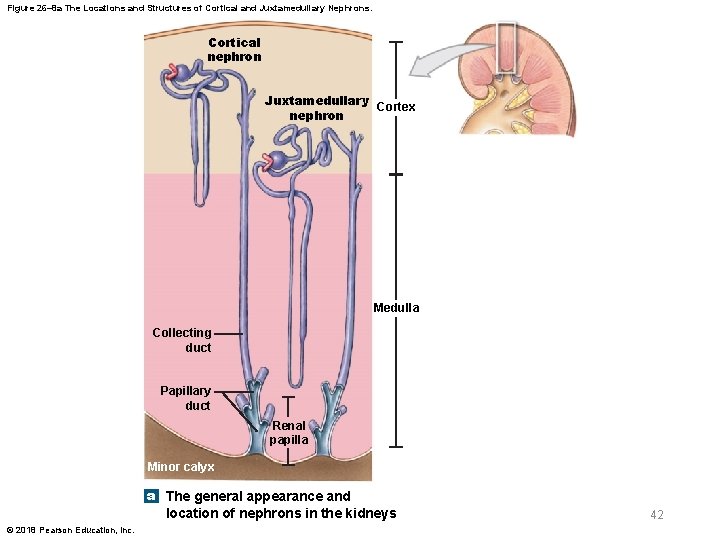
Figure 26– 8 a The Locations and Structures of Cortical and Juxtamedullary Nephrons. Cortical nephron Juxtamedullary Cortex nephron Medulla Collecting duct Papillary duct Renal papilla Minor calyx a The general appearance and location of nephrons in the kidneys © 2018 Pearson Education, Inc. 42
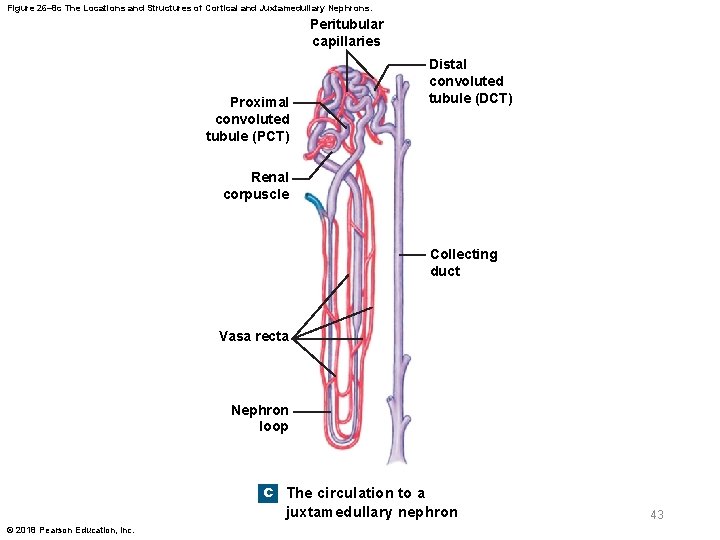
Figure 26– 8 c The Locations and Structures of Cortical and Juxtamedullary Nephrons. Peritubular capillaries Proximal convoluted tubule (PCT) Distal convoluted tubule (DCT) Renal corpuscle Collecting duct Vasa recta Nephron loop c The circulation to a juxtamedullary nephron © 2018 Pearson Education, Inc. 43

26 -3 Renal Physiology § Goal of urine production is to maintain homeostasis – By regulating volume and composition of blood – Involves excretion of metabolic wastes 44 © 2018 Pearson Education, Inc.
26 -3 Renal Physiology § Three metabolic wastes – Urea (most abundant organic waste) – Creatinine (from breakdown of creatine phosphate) – Uric acid (from recycling of nitrogenous bases) § Organic wastes – Dissolved in bloodstream – Eliminated only when dissolved in urine – Removal is accompanied by water loss 45 © 2018 Pearson Education, Inc.
26 -3 Renal Physiology § Kidneys – Usually produce concentrated urine • 1200 m. Osm/L (four times the osmotic concentration of plasma) § Kidney functions – Concentrating filtrate • Failure leads to fatal dehydration within hours – Reabsorption and retention of valuable materials • Example: sugars and amino acids 46 © 2018 Pearson Education, Inc.
26 -3 Renal Physiology § Basic processes of urine formation – Filtration • Blood pressure forces water and solutes across walls of glomerular capillaries – Reabsorption • Movement of water and solutes from filtrate to peritubular fluid – Secretion • Transport of solutes from peritubular fluid to tubular fluid 47 © 2018 Pearson Education, Inc.

Figure 26– 9 An Overview of Urine Formation. Proximal Convoluted Tubule Distal Convoluted Tubule • Reabsorption of water, ions, and all organic nutrients • Secretion of ions, acids, drugs, toxins • Variable reabsorption of water, sodium ions, and calcium ions (under hormonal control) Renal Corpuscle • Production of filtrate Glomerulus Collecting Duct Glomerular capsule Collecting duct Nephron Loop Descending thin limb • Further reabsorption of water • Variable reabsorption of water and reabsorption or secretion of sodium, potassium, hydrogen, and bicarbonate ions Thick ascending limb • Reabsorption of sodium and chloride ions KEY Papillary Duct Filtration occurs exclusively in the renal corpuscle, across the filtration membrane. Water reabsorption occurs primarily along the PCT and the descending thin limb of the nephron loop, but also to a variable degree in the DCT and collecting system. Variable water reabsorption occurs in the DCT and collecting system. • Delivery of urine to minor calyx Urine storage and elimination Solute reabsorption occurs along the PCT, the thick ascending limb of the nephron loop, the DCT, and the collecting system. Variable solute reabsorption or secretion occurs at the PCT, the DCT, and the collecting system. © 2018 Pearson Education, Inc. 48

Table 26– 2 Normal Laboratory Values for Solutes in Plasma and Urine 49 © 2018 Pearson Education, Inc.
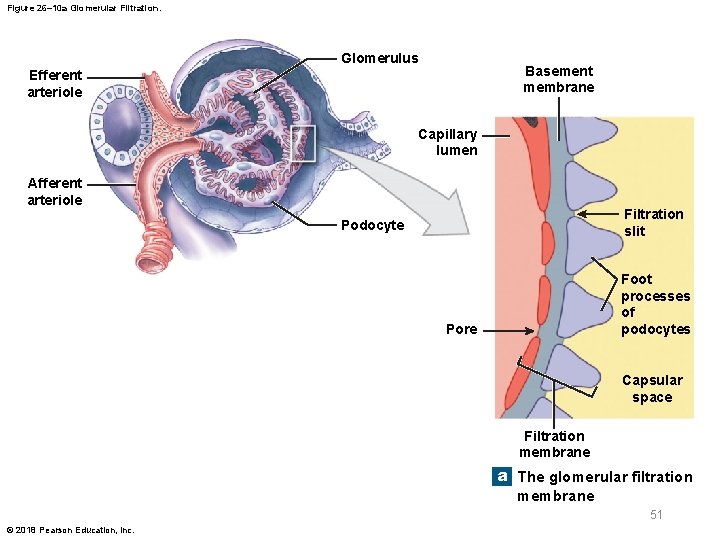
26 -4 Glomerular Filtration § Glomerular filtration – Driven by hydrostatic pressure – Involves passage across a filtration membrane • Small solute molecules pass through • Larger solutes and materials are restricted – Three components of membrane • Fenestrated endothelium • Basement membrane • Foot processes of podocytes 50 © 2018 Pearson Education, Inc.
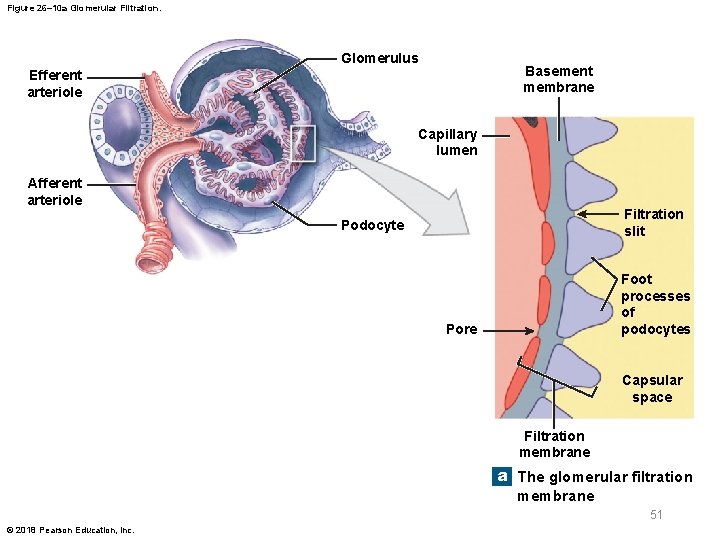
Figure 26– 10 a Glomerular Filtration. Glomerulus Basement membrane Efferent arteriole Capillary lumen Afferent arteriole Filtration slit Podocyte Foot processes of podocytes Pore Capsular space Filtration membrane a The glomerular filtration membrane 51 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Glomerular capillaries – Fenestrated endothelium with small pores – Prevent passage of blood cells – Allow diffusion of solutes, including plasma proteins § Basement membrane – More selective – Allows passage of only small plasma proteins, nutrients, and ions 52 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Filtration pressures – Glomerular filtration is governed by balance between • Hydrostatic pressure (fluid pressure) • Colloid osmotic pressure (of materials in solution) on each side of capillary walls 53 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Glomerular hydrostatic pressure (GHP) – Blood pressure in glomerular capillaries – Blood leaving glomerular capillaries • Flows into efferent arteriole with luminal diameter smaller than that of afferent arteriole – GHP is higher than hydrostatic pressure in peripheral capillaries – Tends to push water and solutes • Out of bloodstream • Into filtrate 54 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Capsular hydrostatic pressure (Cs. HP) – Opposes glomerular hydrostatic pressure – Pushes water and solutes • Out of filtrate • Into bloodstream – Results from resistance to flow along nephron and conducting system 55 © 2018 Pearson Education, Inc.

26 -4 Glomerular Filtration § Net hydrostatic pressure (NHP) – Difference between glomerular hydrostatic pressure and capsular hydrostatic pressure – GHP – Cs. HP = NHP • 50 mm Hg – 15 mm Hg = 35 mm Hg 56 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Colloid osmotic pressure – Pressure due to materials in solution – Blood colloid osmotic pressure (BCOP) • Osmotic pressure resulting from suspended proteins in blood 57 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Net filtration pressure (NFP) – Average pressure forcing water and dissolved substances • Out of glomerular capillaries • Into capsular spaces – Difference between net hydrostatic pressure and blood colloid osmotic pressure in glomerulus – NHP – BCOP = NFP • 35 mm Hg – 25 mm Hg = 10 mm Hg 58 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Glomerular filtration rate (GFR) – Amount of filtrate kidneys produce each minute – Averages 125 m. L/min – About 10 percent of fluid delivered to kidneys • Leaves bloodstream • Enters capsular spaces – Glomeruli generate about 180 liters of filtrate per day • Approximately 70 times total plasma volume – Net filtration pressure determines GFR 59 © 2018 Pearson Education, Inc.

26 -4 Glomerular Filtration § Regulation of GFR – Three interacting levels of control 1. Autoregulation (local level) 2. Hormonal regulation (initiated by kidneys) 3. Autonomic regulation (by sympathetic division of ANS) 60 © 2018 Pearson Education, Inc.

26 -4 Glomerular Filtration § Autoregulation of GFR – Maintains adequate GFR despite changes in local blood pressure and blood flow – Involves changing luminal diameters of • Afferent arterioles • Efferent arterioles • Glomerular capillaries 61 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Hormonal regulation of GFR – Renin-angiotensin-aldosterone system (RAAS) – Natriuretic peptides 62 © 2018 Pearson Education, Inc.

26 -4 Glomerular Filtration § Renin-angiotensin-aldosterone system (RAAS) – Three stimuli cause juxtaglomerular complex (JGC) to release renin • Decrease in blood pressure at glomerulus due to decrease in blood volume, decrease in systemic pressures, or blockage in renal artery or its branches • Stimulation of juxtaglomerular cells by sympathetic innervation • Decrease in osmotic concentration of tubular fluid at macula densa 63 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § RAAS – Renin converts inactive angiotensinogen to inactive angiotensin I – Angiotensin I is converted to angiotensin II by angiotensin-converting enzyme (ACE) • Primarily in capillaries of lungs 64 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Effects of angiotensin II – Contraction of vascular smooth muscle in peripheral capillary beds – Increased aldosterone secretion by adrenal glands • Increases Na+ retention – Increased arterial pressures – Stimulation of thirst centers – Increased production of ADH – Overall effect: increase in systemic blood pressure and blood volume and restoration of normal GFR 65 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Hormonal regulation of GFR – Increased blood volume • Automatically increases GFR to promote fluid loss • If increase in blood volume is severe, hormonal factors further increase GFR 66 © 2018 Pearson Education, Inc.

26 -4 Glomerular Filtration § Natriuretic peptides – Released by heart in response to stretched walls due to increased blood volume or pressure – Atrial natriuretic peptide (ANP) is released by atria – Trigger dilation of afferent glomerular arterioles and constriction of efferent glomerular arterioles – Increase glomerular pressures and increase GFR – ANP also decreases sodium reabsorption – Net result is increased urine production and decreased blood volume and pressure 67 © 2018 Pearson Education, Inc.
26 -4 Glomerular Filtration § Autonomic regulation of GFR – Mostly consists of sympathetic postganglionic fibers – Sympathetic activation • Constricts afferent glomerular arterioles • Decreases GFR • Slows filtrate production – Sympathetic activation can override local regulatory mechanisms that act to stabilize GFR 68 © 2018 Pearson Education, Inc.

26 -5 Reabsorption and Secretion § Filtration at renal corpuscle – Passive – Solutes entering capsular space include • Metabolic wastes and excess ions • Glucose, free fatty acids, amino acids, and vitamins § Useful materials are reabsorbed – In renal tubules and collecting system 69 © 2018 Pearson Education, Inc.

26 -5 Reabsorption and Secretion § Three functions of renal tubule – Reabsorbing useful organic nutrients in filtrate – Reabsorbing more than 90 percent of water in filtrate – Secreting any wastes that did not enter filtrate at glomerulus 70 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Principles of reabsorption and secretion – Reabsorption • Recovers useful materials from tubular fluid and returns them to blood • 99 percent of filtrate is reabsorbed in renal tubules – Secretion • Adds substances from blood to tubular fluid – Reabsorption and secretion • Occur in every segment of renal tubule and in collecting system 71 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption and secretion by kidneys involve – Diffusion – Osmosis – Leak channels (channel-mediated diffusion) – Carrier-mediated transport 72 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Types of carrier-mediated transport – Facilitated diffusion – Active transport – Countertransport 73 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Characteristics of carrier-mediated transport – A specific substrate binds to a carrier protein that facilitates movement across membrane – A given carrier protein typically works in one direction only – Distribution of carrier proteins can vary in different regions of cell surface – The membrane of a single tubular cell contains many types of carrier proteins 74 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Renal threshold – Plasma concentration at which a specific compound or ion begins to appear in urine – Varies with substance involved – If plasma glucose is higher than 180 mg/d. L, glucose appears in urine (glucosuria) – Renal threshold for amino acids is 65 mg/d. L • After a protein-rich meal, amino acids commonly appear in urine (aminoaciduria) 75 © 2018 Pearson Education, Inc.

Table 26– 3 Tubular Reabsorption and Secretion 76 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption and secretion at PCT – PCT cells normally reabsorb 60– 70 percent of filtrate volume produced in renal corpuscle – Reabsorbed materials enter peritubular fluid • And diffuse into peritubular capillaries 77 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Functions of PCT – Reabsorption of organic nutrients – Active reabsorption of ions – Reabsorption of water – Passive reabsorption of ions – Secretion 78 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Sodium ion reabsorption – Important in every PCT process – Sodium ions enter tubular cells by • Diffusion through sodium ion leak channels • Sodium ion–linked cotransport of organic solutes • Countertransport for hydrogen ions 79 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption and secretion along nephron loop – 60– 70 percent of filtrate volume is reabsorbed before tubular fluid reaches nephron loop – Nephron loop reabsorbs • About one-half of remaining water • Two-thirds of remaining sodium and chloride ions 80 © 2018 Pearson Education, Inc.

26 -5 Reabsorption and Secretion § Descending limb of nephron loop – Freely permeable to water but not to solutes – Descending thin limb reabsorbs sodium and chloride ions from tubular fluid § Ascending limb of nephron loop – Impermeable to water – Passively and actively removes sodium and chloride ions from tubular fluid – Very long in juxtamedullary nephrons, creating high solute concentrations in peritubular fluid 81 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption and secretion at DCT – Only 15– 20 percent of initial filtrate volume reaches DCT – Concentrations of electrolytes and metabolic wastes in arriving tubular fluid no longer resemble those in blood plasma 82 © 2018 Pearson Education, Inc.

26 -5 Reabsorption and Secretion § Three processes at DCT – Active secretion of ions, acids, drugs, and toxins into tubule – Selective reabsorption of sodium and calcium ions from tubular fluid – Selective reabsorption of water • Assists in concentrating tubular fluid 83 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption at DCT – Tubular cells actively transport Na+ and Cl– out of tubular fluid – Along distal regions • Tubular cells contain ion pumps that reabsorb Na+ in exchange for another cation (usually K+) 84 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Aldosterone – Hormone produced by adrenal cortex – Stimulates synthesis and incorporation of Na+ pumps and channels • In plasma membranes along DCT and collecting duct – Reduces Na+ lost in urine 85 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Hypokalemia – Dangerous reduction in plasma K+ concentration – Produced by prolonged aldosterone stimulation § Atrial natriuretic peptide (ANP) – Opposes secretion of aldosterone • And its actions on DCT and collecting system § Parathyroid hormone – Regulates calcium ion reabsorption at DCT 86 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Secretion at DCT – Blood entering peritubular capillaries • Contains undesirable substances that did not cross filtration membrane at glomerulus – Rate of K+ and H+ secretion rises or falls according to concentrations in peritubular fluid • Higher concentrations lead to higher rates of secretion 87 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Potassium ion secretion – Tubular cells exchange Na+ in tubular fluid • For excess K+ in body fluids – Potassium ions diffuse into lumen of DCT through K+ leak channels • At apical surfaces of tubular cells 88 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Hydrogen ion secretion – Hydrogen ions generated by dissociation of carbonic acid • Are secreted by sodium ion–linked countertransport • In exchange for Na+ in tubular fluid – Bicarbonate ions diffuse into bloodstream • Help prevent changes in plasma p. H 89 © 2018 Pearson Education, Inc.

26 -5 Reabsorption and Secretion § Hydrogen ion secretion – Acidifies tubular fluid – Elevates blood p. H – Accelerates when blood p. H falls § p. H of blood decreases in – Metabolic acidosis (lactic acidosis) • Can develop after exhaustive muscle activity – Ketoacidosis • Can develop in starvation or diabetes mellitus 90 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Control of blood p. H – Accomplished by H+ removal and bicarbonate ion production at kidneys • Aldosterone stimulates H+ secretion • Prolonged aldosterone stimulation cause alkalosis • Abnormally high blood p. H 91 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § In response to acidosis – PCT and DCT deaminate amino acids • Ties up H+ and yields ammonium ions (NH 4+) and bicarbonate ions (HCO 3–) – Ammonium ions are pumped into tubular fluid – Bicarbonate ions enter bloodstream via peritubular fluid – Benefits of tubular deamination • Provides carbon chains for catabolism • Generates bicarbonate ions to buffer plasma 92 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption and secretion in collecting system – Collecting ducts • Receive tubular fluid from many nephrons • Carry it toward renal sinus – Hormones regulate water and solute loss • Aldosterone controls sodium ion pumps – Actions are opposed by ANP • ADH controls permeability to water – Secretion is suppressed by ANP 93 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Reabsorption in collecting system – Sodium ion reabsorption • Na+ exchanged for K+ – Bicarbonate ion reabsorption • HCO 3– exchanged for Cl– – Urea reabsorption • By diffusion 94 © 2018 Pearson Education, Inc.
26 -5 Reabsorption and Secretion § Secretion in collecting system – Controls p. H of body fluids – Low p. H in peritubular fluid • Carrier proteins pump H+ into tubular fluid and reabsorb bicarbonate ions – High p. H in peritubular fluid (uncommon) • Collecting system secretes bicarbonate ions and pumps H+ into peritubular fluid 95 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Descending thin limb – Permeable to water – Relatively impermeable to solutes § Thick ascending limb – Relatively impermeable to water and solutes – Contains active transport mechanisms • Pump Na+ and Cl− from tubular fluid into peritubular fluid of medulla 96 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Overview of countercurrent multiplication – Na+ and Cl− are pumped out of thick ascending limb • Elevates osmotic concentration in peritubular fluid around descending thin limb – Water flows out of descending thin limb into peritubular fluid • Increasing solute concentration of tubular fluid in descending thin limb 97 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Overview of countercurrent multiplication – A concentrated solution arrives in thick ascending limb • Accelerates transport of Na+ and Cl− into peritubular fluid – Solute pumping out of thick ascending limb • Increases solute concentration in tubular fluid in descending thin limb • Accelerates solute pumping in thick ascending limb 98 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Medullary osmotic gradient – Concentration gradient created in peritubular fluid of medulla – Active transport at apical surface of thick ascending limb • Moves Na+, K+, and Cl– out of tubular fluid – Uses Na+–K+/2 Cl− transporter • Each cycle of pump carries 1 sodium, 1 potassium, and 2 chloride ions into tubular cell 99 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Medullary osmotic gradient – Cotransport carriers pump K+ and Cl– into peritubular fluid • K+ is removed by sodium–potassium exchange pump • And diffuses back into lumen of tubule through K+ leak channels – Net result is that Na+ and Cl– enter peritubular fluid of medulla, raising osmotic concentration • Water moves out of descending thin limb • Osmotic concentration of tubular fluid increases 100 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Thick ascending limb – Has a highly effective pumping mechanism • Almost two-thirds of Na+ and Cl− are pumped out of tubular fluid – Fluid arriving at DCT has an osmotic concentration of 100 m. Osm/L • One-third the concentration of peritubular fluid of renal cortex 101 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Thick ascending limb – Rate of ion transport is proportional to an ion’s concentration in tubular fluid – More Na+ and Cl− are pumped into medulla at start of thick ascending limb • Where their concentrations are highest – Regional difference in rate of ion transport • Creates osmotic gradient in medulla 102 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Medullary osmotic gradient – Maximum solute concentration of peritubular fluid near turn of nephron loop is about 1200 m. Osm/L • Na+ and Cl− pumped out of thick ascending limb make up about two-thirds of that (750 m. Osm/L) • Remainder from urea 103 © 2018 Pearson Education, Inc.

26 -6 Countercurrent Multiplication § Role of urea – Thick ascending limb, DCT, and collecting ducts are impermeable to urea – As water is reabsorbed, concentration of urea in tubular fluid rises – Tubular fluid reaching papillary duct contains urea at about 450 m. Osm/L – Papillary ducts are permeable to urea • Thus, urea concentration in deepest parts of medulla averages 450 m. Osm/L 104 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Regulation of urine volume and concentration – Through control of water reabsorption – Water is reabsorbed by osmosis in • Proximal convoluted tubule • Descending limb of nephron loop – Water permeabilities of these regions cannot be adjusted 105 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Water reabsorption – Occurs when osmotic concentration of peritubular fluid exceeds that of tubular fluid – Ascending limb of nephron loop is impermeable to water – In distal convoluted tubule and collecting system • 1– 2 percent of water volume in original filtrate is recovered during sodium ion reabsorption 106 © 2018 Pearson Education, Inc.

26 -6 Countercurrent Multiplication § Obligatory water reabsorption – Water movement that cannot be prevented – Usually recovers 85 percent of filtrate volume § Facultative water reabsorption – Controls volume of water reabsorbed along DCT and collecting system • 15 percent of filtrate volume (27 liters/day) • These segments are relatively impermeable to water except in presence of ADH 107 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § ADH – Hormone that causes insertion of aquaporins (special water channels) in apical cell membranes – Increases rate of osmotic water movement – Higher levels of ADH increase • Number of water channels • Water permeability of DCT and collecting system – Without ADH • All fluid reaching DCT is lost in urine • Large amounts of dilute urine are produced 108 © 2018 Pearson Education, Inc.

26 -6 Countercurrent Multiplication § Hypothalamus – Continuously secretes low levels of ADH • Thus, DCT and collecting system are always permeable to water § A healthy adult produces 1200 m. L of urine per day (about 0. 6 percent of filtrate volume) – With osmotic concentration of 855– 1335 m. Osm/L 109 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Vasa recta returns reabsorbed solutes and water to general circulation – Without disrupting medullary osmotic gradient – Process is called countercurrent exchange – As blood in vasa recta descends into medulla, it increases in osmotic concentration • Some solutes absorbed in descending portion do not diffuse out in ascending portion • More water moves into ascending portion than is moved out of descending portion 110 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Summary of renal function – Step 1: glomerulus • Filtrate produced at renal corpuscle has same osmotic concentration as plasma (300 m. Osm/L) • Lacks plasma proteins – Step 2: proximal convoluted tubule (PCT) • Active removal of ions and organic nutrients • Produces osmotic water flow out of tubular fluid • Keeps solutions inside and outside tubule isotonic • 60– 70 percent of filtrate volume is absorbed here 111 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Summary of renal function – Step 3: PCT and descending limb • Water moves into peritubular fluid • Compulsory reabsorption of water results in small volume of highly concentrated tubular fluid – Step 4: thick ascending limb • Tubular cells actively transport Na+ and Cl– out • Urea accounts for higher proportion of total solute concentration at end of nephron loop 112 © 2018 Pearson Education, Inc.

26 -6 Countercurrent Multiplication § Summary of renal function – Step 5: DCT and collecting system • Further adjustments in composition of tubular fluid • Solute concentration is adjusted through active transport (reabsorption or secretion) – Step 6: DCT and collecting system • Final adjustments in volume and solute concentration of tubular fluid • ADH levels determine final urine volume and concentration 113 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Summary of renal function – Step 7: vasa recta • Absorbs solutes and water reabsorbed by nephron loop and collecting ducts • Maintains concentration gradient of medulla – Step 8: papillary duct • Permeable to urea, where its concentration is about 450 m. Osm/L • Same value as in deepest parts of medulla 114 © 2018 Pearson Education, Inc.

26 -6 Countercurrent Multiplication § Composition of urine – Reflects filtration, reabsorption, and secretion activities of nephrons – Some substances (such as urea) are neither actively excreted nor reabsorbed – Organic nutrients are completely reabsorbed • Other compounds missed by filtration (e. g. , creatinine) are actively secreted into tubular fluid 115 © 2018 Pearson Education, Inc.

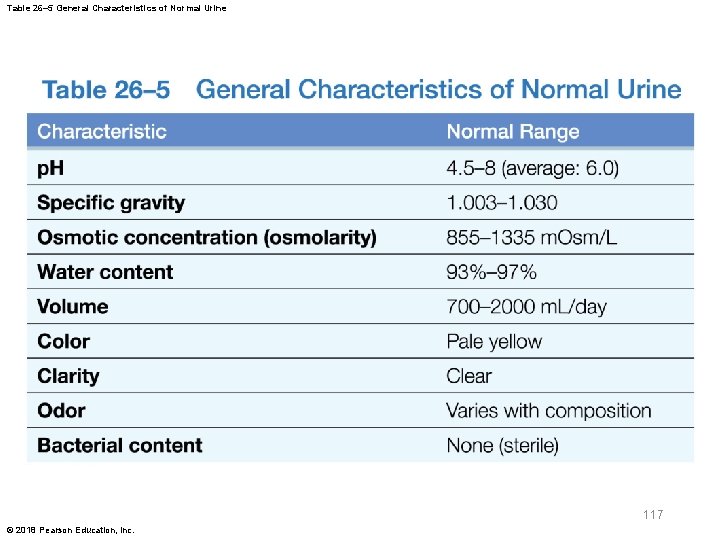
26 -6 Countercurrent Multiplication § Normal urine – Clear, sterile liquid – Concentration of substances • Depends on osmotic movement of water across walls of tubules and collecting ducts – Yellow color is due to urobilin (pigment) • Generated in kidneys from urobilinogens – Urinalysis (analysis of a urine sample) • Important diagnostic tool 116 © 2018 Pearson Education, Inc.
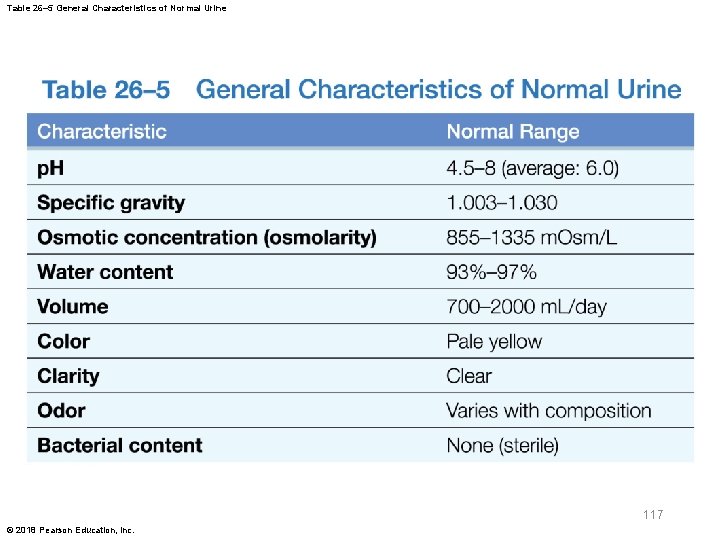
Table 26– 5 General Characteristics of Normal Urine 117 © 2018 Pearson Education, Inc.
26 -6 Countercurrent Multiplication § Creatinine clearance – Compares creatinine level in urine with that in blood – Used to estimate GFR – A more accurate GFR can be obtained using inulin • A carbohydrate that is not metabolized § BUN (blood urea nitrogen) test – Measures amount of urea in blood • Should be low 118 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Filtrate modification and urine production – End when fluid enters renal pelvis § Urine transport, storage, and elimination – Take place in urinary tract • Ureters, urinary bladder, urethra § Pyelogram – Image of urinary system – Obtained by taking an X-ray after radiopaque dye has been administered intravenously 119 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Minor and major calyces, renal pelvis, ureters, urinary bladder, and proximal portion of urethra – Lined by transitional epithelium – Undergo cycles of distention and relaxation without damage 120 © 2018 Pearson Education, Inc.
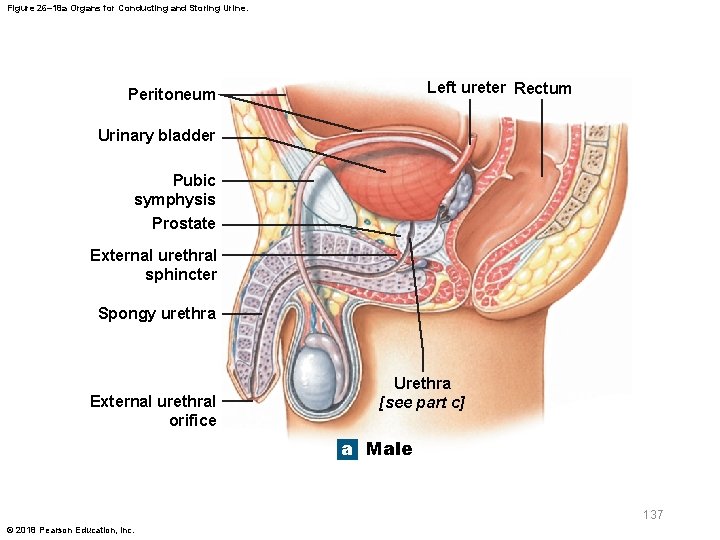
26 -7 Urine Transport, Storage, Elimination § Ureters – Pair of muscular tubes – Extend from kidneys to urinary bladder – Begin at renal pelvis and pass over psoas major – Retroperitoneal – Penetrate posterior wall of urinary bladder at oblique angle – Ureteric orifices are slit-like rather than rounded • Helps prevent backflow of urine when urinary bladder contracts 121 © 2018 Pearson Education, Inc.

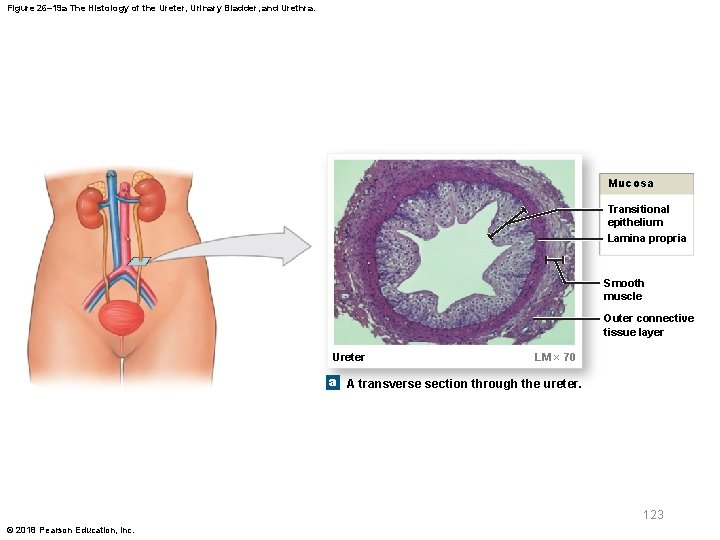
26 -7 Urine Transport, Storage, Elimination § Wall of each ureter has three layers – Inner mucosa • Transitional epithelium and lamina propria – Middle muscular layer • Longitudinal and circular bands of smooth muscle – Outer connective tissue layer • Continuous with fibrous capsule and peritoneum 122 © 2018 Pearson Education, Inc.
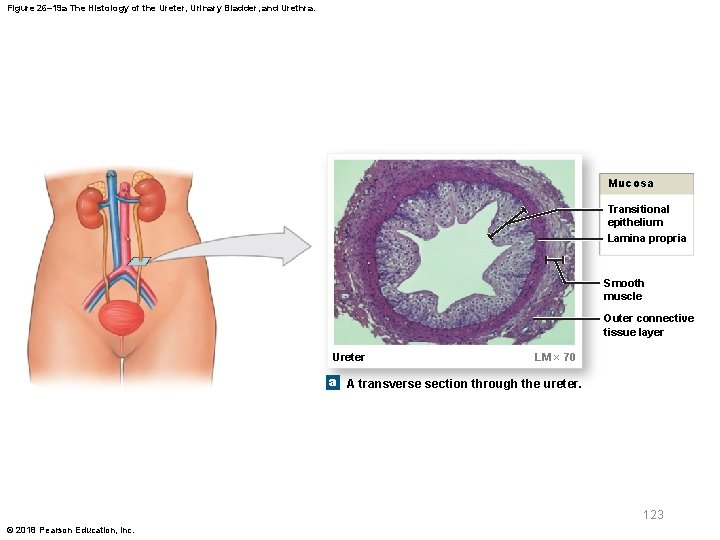
Figure 26– 19 a The Histology of the Ureter, Urinary Bladder, and Urethra. Mucosa Transitional epithelium Lamina propria Smooth muscle Outer connective tissue layer Ureter LM × 70 a A transverse section through the ureter. 123 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Peristaltic contractions – Occur about every 30 seconds – Begin at renal pelvis – Sweep along ureter – Forcing urine toward urinary bladder § Urinary bladder – Hollow, muscular organ – Serves as temporary storage for urine – Full bladder can contain 1 liter of urine 124 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Bladder position – Stabilized by several peritoneal folds – Posterior, inferior, and anterior surfaces • Lie outside peritoneal cavity – Ligamentous bands • Anchor urinary bladder to pelvic and pubic bones 125 © 2018 Pearson Education, Inc.

Figure 26– 18 a Organs for Conducting and Storing Urine. Left ureter Rectum Peritoneum Urinary bladder Pubic symphysis Prostate External urethral sphincter Spongy urethra External urethral orifice Urethra [see part c] a Male 126 © 2018 Pearson Education, Inc.

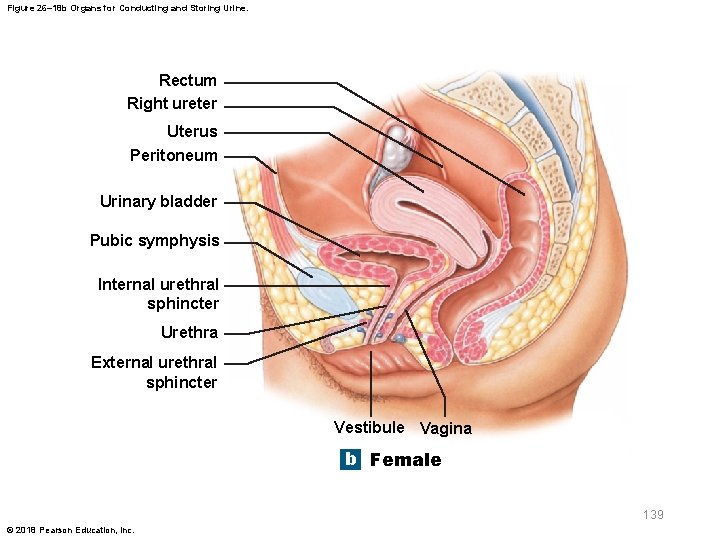
Figure 26– 18 b Organs for Conducting and Storing Urine. Rectum Right ureter Uterus Peritoneum Urinary bladder Pubic symphysis Internal urethral sphincter Urethra External urethral sphincter Vestibule Vagina b Female 127 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Umbilical ligaments of bladder – Median umbilical ligament • Extends from anterior, superior border • Toward umbilicus (navel) – Lateral umbilical ligaments • Pass along sides of bladder to umbilicus • Vestiges of two umbilical arteries 128 © 2018 Pearson Education, Inc.

Figure 26– 18 c Organs for Conducting and Storing Urine. Median umbilical ligament Ureter Lateral umbilical ligament Detrusor Rugae Ureteric orifices Internal urethral sphincter External urethral sphincter Center of trigone Neck of urinary bladder Prostate Prostatic urethra Membranous urethra c Urinary bladder in male 129 © 2018 Pearson Education, Inc.

26 -7 Urine Transport, Storage, Elimination § Mucosa – Lines urinary bladder – Has folds (rugae) that disappear as bladder fills § Trigone of urinary bladder – Triangular area bounded by • Openings of ureters • Entrance to urethra – Acts as a funnel • Channels urine into urethra when bladder contracts 130 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Urethral entrance – Lies at apex of trigone • At most inferior point in urinary bladder § Neck of urinary bladder – Region surrounding urethral opening – Contains a muscular internal urethral sphincter • Provides involuntary control of urine discharge 131 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Urinary bladder innervation – Postganglionic fibers • From ganglia in hypogastric plexus – Parasympathetic fibers • From intramural ganglia controlled by pelvic nerves 132 © 2018 Pearson Education, Inc.

26 -7 Urine Transport, Storage, Elimination § Wall of urinary bladder contains mucosa, submucosa, and muscular layers – Muscular layer consists of detrusor muscle • Internal and external layers of longitudinal smooth muscle separated by a layer of circular muscle 133 © 2018 Pearson Education, Inc.

Figure 26– 19 b The Histology of the Ureter, Urinary Bladder, and Urethra. Mucosa Transitional epithelium Lamina propria Submucosa Detrusor Visceral peritoneum Urinary bladder LM × 36 b The wall of the urinary bladder. 134 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Urethra – Transports urine from neck of urinary bladder • To exterior of body – Lamina propria is thick and elastic – Mucosa has longitudinal folds – Mucus-secreting cells lie in epithelial pockets 135 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Male urethra – Extends from neck of urinary bladder to tip of penis (18 – 20 cm) – Prostatic urethra passes through center of prostate – Membranous urethra includes short segment that penetrates deep transverse perineal muscle – Spongy urethra extends from distal border of deep transverse perineal muscle • To external urethral orifice at tip of penis 136 © 2018 Pearson Education, Inc.
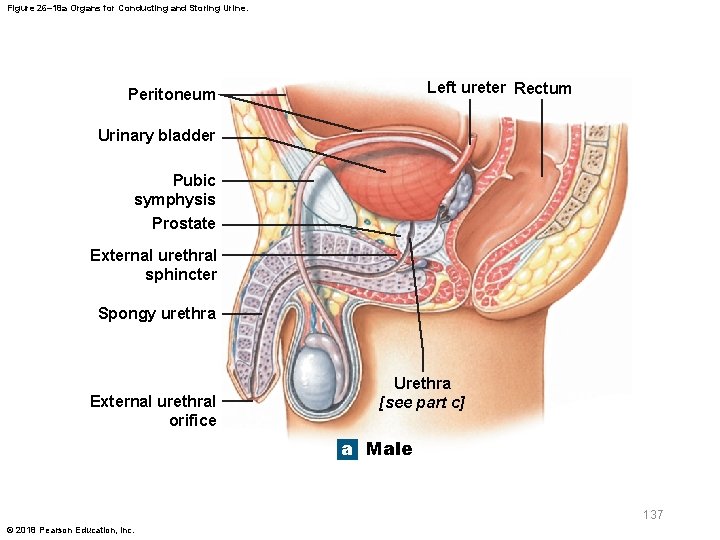
Figure 26– 18 a Organs for Conducting and Storing Urine. Left ureter Rectum Peritoneum Urinary bladder Pubic symphysis Prostate External urethral sphincter Spongy urethra External urethral orifice Urethra [see part c] a Male 137 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Female urethra – Very short (3– 5 cm) – Extends from bladder to vestibule – External urethral orifice is near anterior wall of vagina 138 © 2018 Pearson Education, Inc.
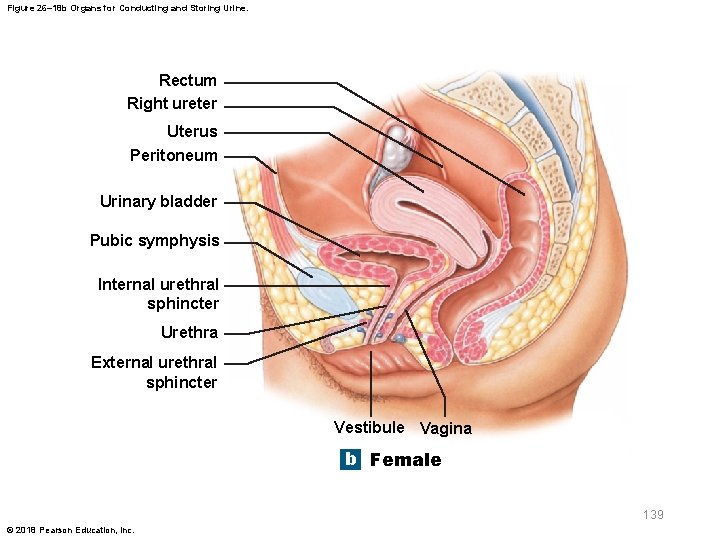
Figure 26– 18 b Organs for Conducting and Storing Urine. Rectum Right ureter Uterus Peritoneum Urinary bladder Pubic symphysis Internal urethral sphincter Urethra External urethral sphincter Vestibule Vagina b Female 139 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § External urethral sphincter – In both sexes – Circular band of skeletal muscle – Acts as a valve – Under voluntary control • Via perineal branch of pudendal nerve – Has resting muscle tone – Voluntary relaxation permits urination 140 © 2018 Pearson Education, Inc.
26 -7 Urine Transport, Storage, Elimination § Male urethra – Epithelial mucous glands • May form tubules that extend into lamina propria – Connective tissues of lamina propria • Anchor urethra to surrounding structures § Female urethra – Lamina propria contains extensive network of veins – Entire complex is surrounded by concentric layers of smooth muscle 141 © 2018 Pearson Education, Inc.
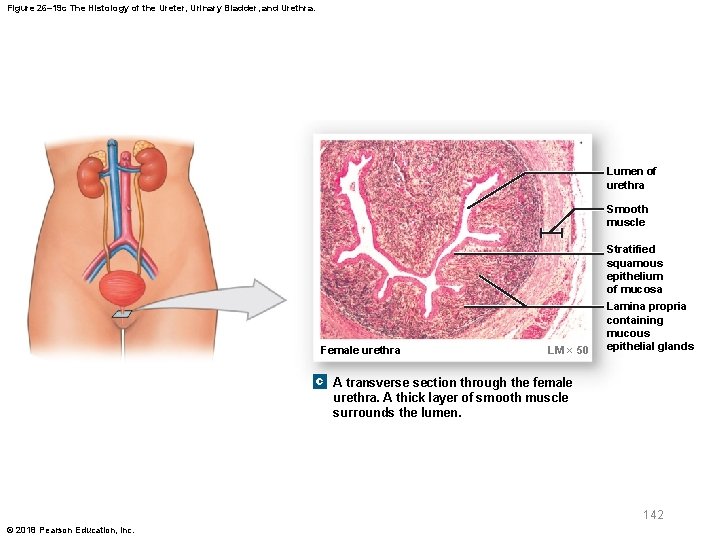
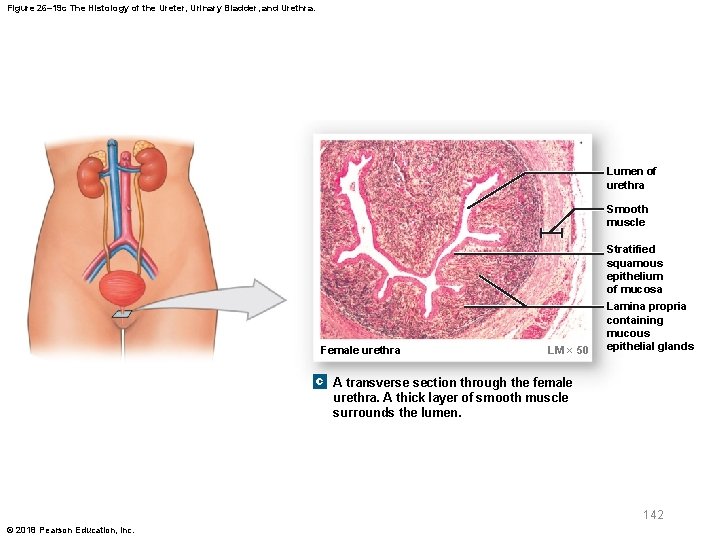
Figure 26– 19 c The Histology of the Ureter, Urinary Bladder, and Urethra. Lumen of urethra Smooth muscle Stratified squamous epithelium of mucosa Female urethra LM × 50 Lamina propria containing mucous epithelial glands c A transverse section through the female urethra. A thick layer of smooth muscle surrounds the lumen. 142 © 2018 Pearson Education, Inc.
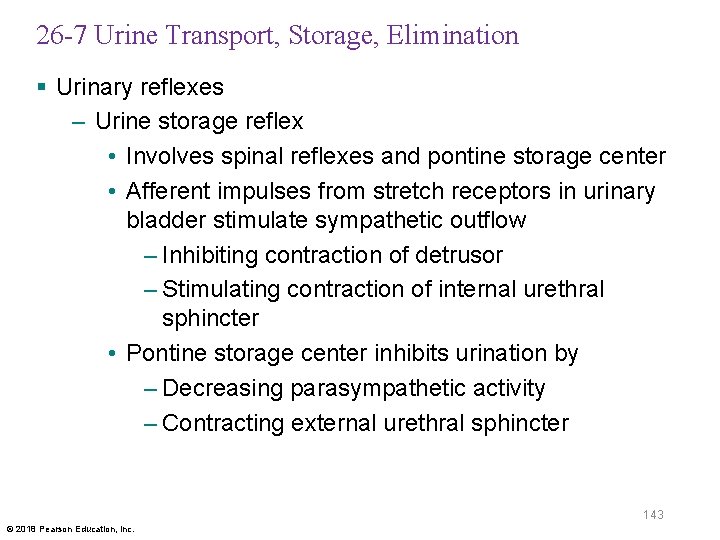
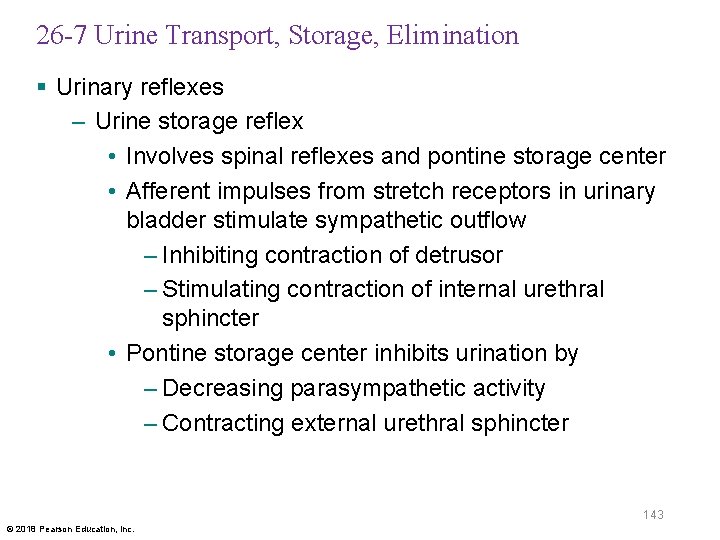
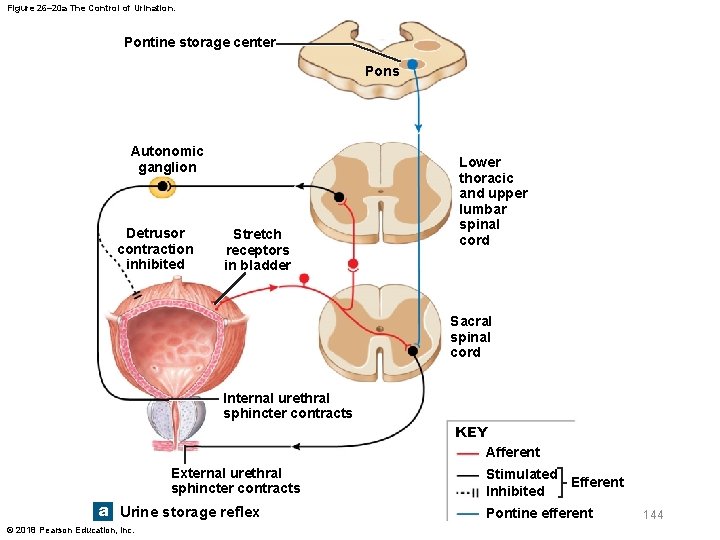
26 -7 Urine Transport, Storage, Elimination § Urinary reflexes – Urine storage reflex • Involves spinal reflexes and pontine storage center • Afferent impulses from stretch receptors in urinary bladder stimulate sympathetic outflow – Inhibiting contraction of detrusor – Stimulating contraction of internal urethral sphincter • Pontine storage center inhibits urination by – Decreasing parasympathetic activity – Contracting external urethral sphincter 143 © 2018 Pearson Education, Inc.
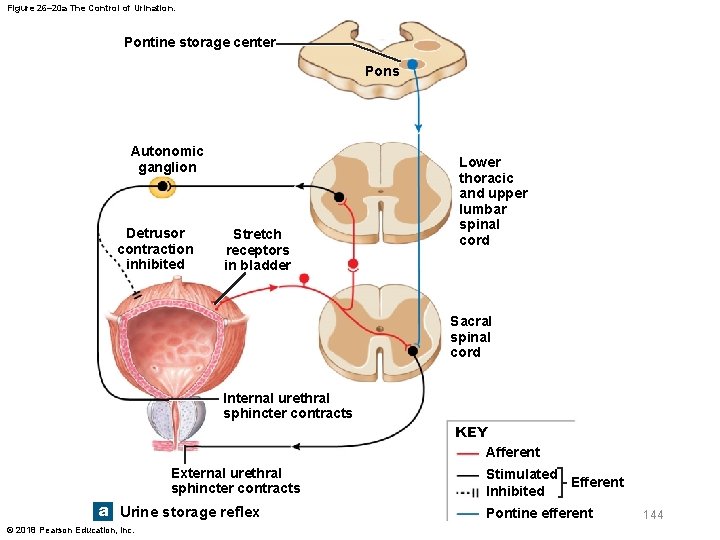
Figure 26– 20 a The Control of Urination. Pontine storage center Pons Autonomic ganglion Detrusor contraction inhibited Stretch receptors in bladder Lower thoracic and upper lumbar spinal cord Sacral spinal cord Internal urethral sphincter contracts KEY Afferent External urethral sphincter contracts a Urine storage reflex © 2018 Pearson Education, Inc. Stimulated Efferent Inhibited Pontine efferent 144
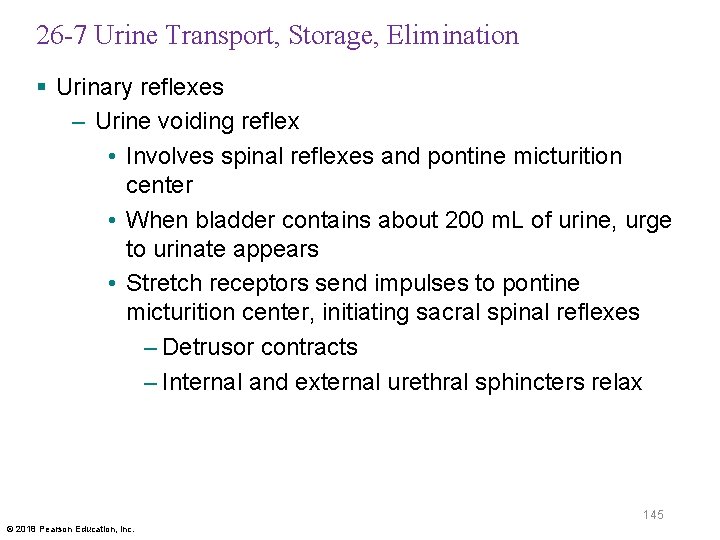
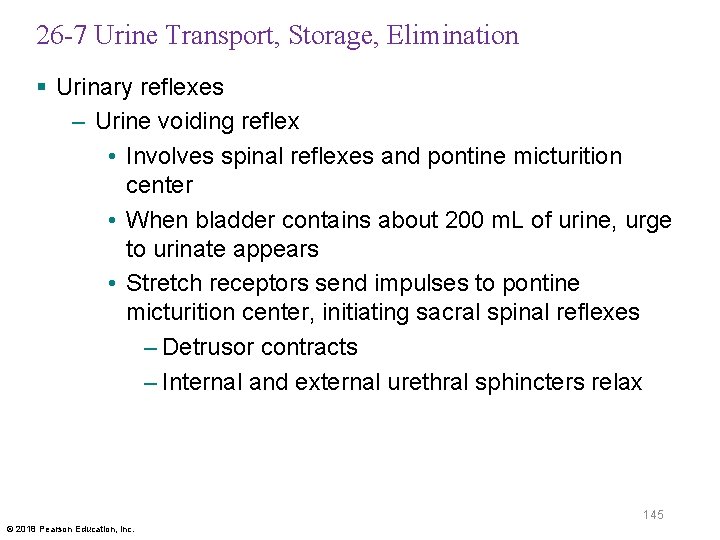
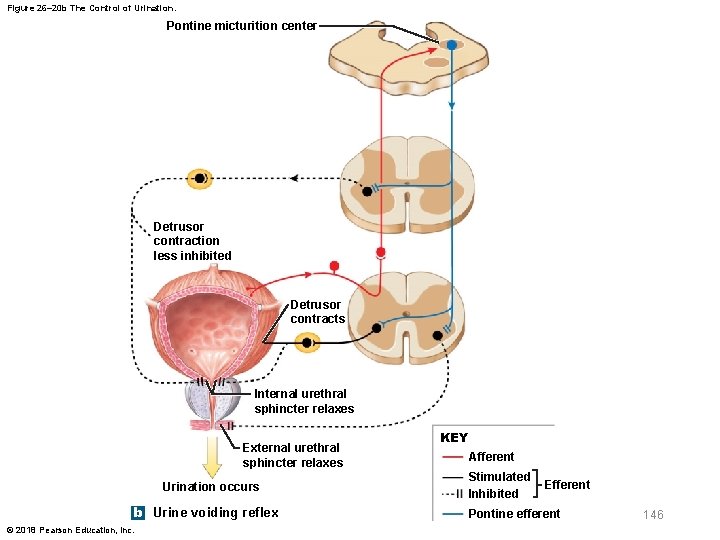
26 -7 Urine Transport, Storage, Elimination § Urinary reflexes – Urine voiding reflex • Involves spinal reflexes and pontine micturition center • When bladder contains about 200 m. L of urine, urge to urinate appears • Stretch receptors send impulses to pontine micturition center, initiating sacral spinal reflexes – Detrusor contracts – Internal and external urethral sphincters relax 145 © 2018 Pearson Education, Inc.
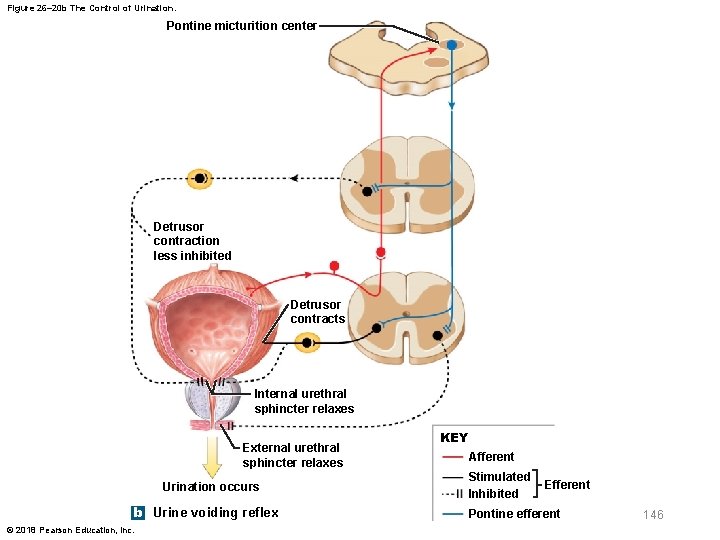
Figure 26– 20 b The Control of Urination. Pontine micturition center Detrusor contraction less inhibited Detrusor contracts Internal urethral sphincter relaxes External urethral sphincter relaxes Urination occurs b Urine voiding reflex © 2018 Pearson Education, Inc. KEY Afferent Stimulated Inhibited Efferent Pontine efferent 146
26 -7 Urine Transport, Storage, Elimination § Infants – Lack voluntary control over urination – Necessary corticospinal connections are not yet established § Incontinence – Inability to control urination voluntarily – May be caused by trauma to internal or external urethral sphincter 147 © 2018 Pearson Education, Inc.

26 -8 Effects of Aging on the Urinary System § Age-related changes – Nephrolithiasis (formation of calculi) – Decrease in number of functional nephrons – Reduction in GFR – Reduced sensitivity to ADH – Problems with urinary reflexes • External sphincter loses muscle tone • Control of urination can be lost due to a stroke, Alzheimer’s disease, and other CNS problems • In males, urinary retention may develop 148 © 2018 Pearson Education, Inc.
26 -9 Waste Excretion § Excretory system – Includes systems with excretory functions that affect composition of body fluids • Urinary system • Integumentary system • Respiratory system • Digestive system 149 © 2018 Pearson Education, Inc.

Figure 26– 21 Integration of the URINARY system with the other body systems presented so far. Integumentary System • The Integumentary System prevents excessive fluid loss through skin surface; produces vitamin D 3, important for the renal production of calcitriol; sweat glands assist in elimination of water and solutes • The urinary system excretes nitrogenous wastes; maintains fluid, electrolyte, and acid–base balance of blood that nourishes the skin Respiratory System • The Respiratory System assists in the regulation of p. H by eliminating carbon dioxide • The urinary system assists in the excretion of carbon dioxide; provides bicarbonate buffers that assist in p. H regulation Cardiovascular System • The Cardiovascular System delivers blood to glomerular capillaries, where filtration occurs; accepts fluids and solutes reabsorbed during urine production • The urinary system releases renin to elevate blood pressure and erythropoietin to accelerate red blood cell production Skeletal System • The Skeletal System provides some protection for kidneys and ureters with its axial divison; pelvis protects urinary bladder and proximal portion of urethra • The urinary system conserves calcium and phosphate needed for bone growth Muscular System • The Muscular System controls urination by closing urethral sphincters. Muscle layers of trunk provide some protection for urinary organs • The urinary system excretes waste products of muscle and protein metabolism; assists in regulation of calcium and phosphate concentrations © 2018 Pearson Education, Inc. Nervous System • The Nervous System adjusts renal blood pressure; monitors distension of urinary bladder and controls urination • The urinary system eliminates nitrogenous wastes; maintains fluid, electrolyte, and acid–base balance of blood, which is critical for neural function Endocrine System • The Endocrine System produces aldosterone and antidiuretic hormone (ADH), which adjust rates of fluid and electrolyte reabsorption by kidneys • The urinary system releases renin when local blood pressure drops and erythropoietin (EPO) when renal oxygen levels fall Lymphatic System • The Lymphatic System provides adaptive (specific) defense against urinary tract infections • The urinary system excretes toxins and wastes generated by cellular activities; acid p. H of urine provides innate (nonspecific) defense against urinary tract infections Digestive System • The Digestive System absorbs water needed to excrete wastes at kidneys; absorbs ions needed to maintain normal body fluid concentrations; liver removes bilirubin • The urinary system excretes toxins absorbed by the digestive epithelium; excretes bilirubin and nitrogenous wastes from the liver; calcitriol production by kidneys aids calcium and phosphate absorption Urinary System The urinary system excretes metabolic wastes and maintains normal body fluid p. H and ion composition. It: • regulates blood volume and blood pressure • regulates plasma concentrations of sodium, potassium, chloride, and other ions • helps to stabilize blood p. H • conserves valuable nutrients 150
 Eleventh edition management
Eleventh edition management Eleventh edition management
Eleventh edition management Management eleventh edition
Management eleventh edition Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Uterus perimetrium
Uterus perimetrium The central sulcus divides which two lobes? (figure 14-13)
The central sulcus divides which two lobes? (figure 14-13) Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Chapter 7:9 lymphatic system
Chapter 7:9 lymphatic system Chapter 14 the digestive system and body metabolism
Chapter 14 the digestive system and body metabolism Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Necessary life functions anatomy and physiology
Necessary life functions anatomy and physiology Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Gi tract histology
Gi tract histology Anterior posterior distal proximal
Anterior posterior distal proximal Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Anatomy and physiology chapter 8 skeletal system
Anatomy and physiology chapter 8 skeletal system Chapter 6 general anatomy and physiology
Chapter 6 general anatomy and physiology Anterior posterior ventral dorsal
Anterior posterior ventral dorsal Chadha committee
Chadha committee Eleventh 5 year plan
Eleventh 5 year plan Eleventh plan
Eleventh plan For his eleventh birthday elvis presley
For his eleventh birthday elvis presley Physiology of sport and exercise 5th edition
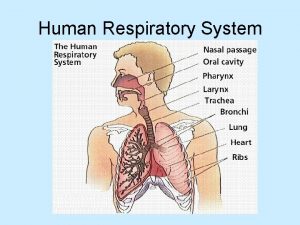
Physiology of sport and exercise 5th edition Upper respiratory system labeled
Upper respiratory system labeled Tattoo anatomy and physiology
Tattoo anatomy and physiology Science olympiad anatomy and physiology
Science olympiad anatomy and physiology Perfect vs imperfect flower
Perfect vs imperfect flower Anatomy and physiology bone
Anatomy and physiology bone Ulcer anatomy
Ulcer anatomy Liver hilus
Liver hilus Epigastric region
Epigastric region Difference between anatomy and physiology
Difference between anatomy and physiology Cytoplasmic granules
Cytoplasmic granules Http://anatomy and physiology
Http://anatomy and physiology Anatomy and physiology of appendicitis
Anatomy and physiology of appendicitis Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 2
Aohs foundations of anatomy and physiology 2 Anatomical planes
Anatomical planes Unit 26 self evaluation answers
Unit 26 self evaluation answers Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Stomach anatomy corpus
Stomach anatomy corpus Anatomy and physiology of pancreas in diabetes
Anatomy and physiology of pancreas in diabetes Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Anatomy and physiology
Anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Physiology exam 1
Physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Anatomy and physiology of the foot
Anatomy and physiology of the foot Integumentary system psoriasis
Integumentary system psoriasis Pse4u
Pse4u Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Organ orientation
Organ orientation Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Thyroid anatomy
Thyroid anatomy Dorsifelxion
Dorsifelxion Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 10-1 blood
Figure 10-1 blood Anatomy histology
Anatomy histology Anatomy and physiology of eye
Anatomy and physiology of eye Oblongata
Oblongata Irn.org anatomy and physiology
Irn.org anatomy and physiology Anatomy and physiology body parts
Anatomy and physiology body parts Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition The digestive system and body metabolism
The digestive system and body metabolism Anatomy and physiology of the retina
Anatomy and physiology of the retina Anatomy and physiology
Anatomy and physiology Anatomy and physiology of meningitis ppt
Anatomy and physiology of meningitis ppt Jeopardy anatomy and physiology game
Jeopardy anatomy and physiology game Homeostasis
Homeostasis Anatomy and physiology
Anatomy and physiology Human.respiratory.system
Human.respiratory.system Anatomy and physiology trivia
Anatomy and physiology trivia Superior mouth fish
Superior mouth fish Brain anatomy and physiology
Brain anatomy and physiology Anatomy and physiology
Anatomy and physiology Long axis of body
Long axis of body 2012 pearson education inc anatomy and physiology
2012 pearson education inc anatomy and physiology Palatopharyngeal folds
Palatopharyngeal folds Fish anatomy and physiology
Fish anatomy and physiology Cengage anatomy and physiology
Cengage anatomy and physiology Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition No slip condition
No slip condition Digital fundamentals floyd
Digital fundamentals floyd Machining fundamentals 10th edition
Machining fundamentals 10th edition Fundamentals of organizational communication 9th edition
Fundamentals of organizational communication 9th edition Fundamentals of organizational communication 9th edition
Fundamentals of organizational communication 9th edition Sujata madan
Sujata madan Digital fundamentals 10th edition
Digital fundamentals 10th edition Digital fundamentals by floyd
Digital fundamentals by floyd Dc/ac fundamentals 1st edition
Dc/ac fundamentals 1st edition Computer security fundamentals 4th edition
Computer security fundamentals 4th edition Management fundamentals 8th edition
Management fundamentals 8th edition Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Fundamentals of corporate finance third canadian edition
Fundamentals of corporate finance third canadian edition Fundamentals of corporate finance fifth edition
Fundamentals of corporate finance fifth edition Fundamentals of corporate finance 6th edition
Fundamentals of corporate finance 6th edition Abnormal psychology comer 9th edition
Abnormal psychology comer 9th edition Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Thermal resistance formula
Thermal resistance formula The fundamentals of political science research 2nd edition
The fundamentals of political science research 2nd edition Mis chapter 6
Mis chapter 6 Report
Report Brunnstrom's clinical kinesiology 7th edition
Brunnstrom's clinical kinesiology 7th edition Clinical kinesiology and anatomy 6th edition
Clinical kinesiology and anatomy 6th edition Human anatomy fifth edition
Human anatomy fifth edition Human anatomy fifth edition
Human anatomy fifth edition Fundamentals chapter 1
Fundamentals chapter 1 Fundamentals of electric circuits chapter 4 solutions
Fundamentals of electric circuits chapter 4 solutions Fundamentals of corporate finance chapter 6 solutions
Fundamentals of corporate finance chapter 6 solutions Digital fundamentals chapter 4
Digital fundamentals chapter 4 Conceptual physics magnetism
Conceptual physics magnetism Chapter 73 tire wheel and wheel bearing fundamentals
Chapter 73 tire wheel and wheel bearing fundamentals Understanding your health and wellness
Understanding your health and wellness Fundamentals of electric circuits chapter 9 solutions
Fundamentals of electric circuits chapter 9 solutions Fundamentals of electric circuits chapter 7 solutions
Fundamentals of electric circuits chapter 7 solutions Fundamentals of building construction chapter summaries
Fundamentals of building construction chapter summaries Computer fundamentals chapter 1
Computer fundamentals chapter 1 Examples of agency problems
Examples of agency problems Fundamentals of thermal-fluidsciences chapter 1 problem 13p
Fundamentals of thermal-fluidsciences chapter 1 problem 13p White-collar workers คือ
White-collar workers คือ Fundamentals of information system
Fundamentals of information system Fundamentals of nursing chapter 17 vital signs
Fundamentals of nursing chapter 17 vital signs Chapter 6 fingerprints
Chapter 6 fingerprints Fundamentals in lodging operations chapter 2
Fundamentals in lodging operations chapter 2 Chapter 2 lab java fundamentals
Chapter 2 lab java fundamentals Back channeling nursing
Back channeling nursing Examples of the respiratory system
Examples of the respiratory system Chapter 39 electrical fundamentals
Chapter 39 electrical fundamentals Fundamentals of thermal-fluidsciences chapter 2 problem 19p
Fundamentals of thermal-fluidsciences chapter 2 problem 19p Fundamentals of thermal-fluidsciences chapter 2 problem 58p
Fundamentals of thermal-fluidsciences chapter 2 problem 58p Chapter 15 critical thinking in nursing practice
Chapter 15 critical thinking in nursing practice