Fundamentals of Anatomy Physiology Eleventh Edition Chapter 23

- Slides: 175
Fundamentals of Anatomy & Physiology Eleventh Edition Chapter 23 The Respiratory System Lecture Presentation by Deborah A. Hutchinson Seattle University © 2018 Pearson Education, Inc.
Learning outcomes 23 -1 Describe the primary functions and organization of the respiratory system, and explain how the delicate respiratory exchange surfaces are protected from pathogens, debris, and other hazards. 23 -2 Identify the organs of the upper respiratory system, and describe their functions. 23 -3 Describe the structure of the larynx, discuss its roles in normal breathing and in sound production, and identify the structures of the airways. 23 -4 Describe the functional anatomy of alveoli. 23 -5 Describe the superficial anatomy of the lungs and the structure of a pulmonary lobule. 23 -6 Define and compare the processes of external respiration and internal respiration. 2 © 2018 Pearson Education, Inc.
Learning outcomes 23 -7 Summarize the physical principles controlling the movement of air into and out of the lungs, and describe the actions of the respiratory muscles. 23 -8 Summarize the physical principles governing the diffusion of gases into and out of the blood and body tissues. 23 -9 Describe the structure and function of hemoglobin, and the transport of oxygen and carbon dioxide in the blood. 23 -10 List the factors that influence respiration rate, and discuss reflex respiratory activity and the brain centers involved in the control of respiration. 23 -11 Describe age-related changes in the respiratory system. 23 -12 Give examples of interactions between the respiratory system and other organ systems studied so far. 3 © 2018 Pearson Education, Inc.
An Introduction to the Respiratory System § Respiratory system – Cells obtain energy primarily through aerobic metabolism • Requires oxygen and produces carbon dioxide – Oxygen is obtained from air by diffusion across exchange surfaces in lungs – Blood carries oxygen from lungs to peripheral tissues • And carries carbon dioxide from peripheral tissues to lungs 4 © 2018 Pearson Education, Inc.
23 -1 Components of the Respiratory System § Functions of respiratory system – Provide extensive surface area for gas exchange between air and circulating blood – Move air to and from exchange surfaces of lungs – Protect respiratory surfaces from dehydration, temperature changes, and pathogens – Produce sounds – Detect odors with olfactory receptors in nasal cavity 5 © 2018 Pearson Education, Inc.
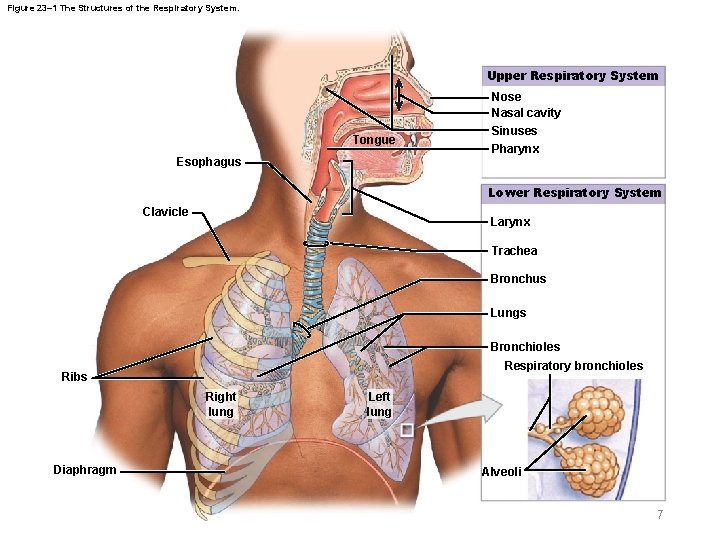
23 -1 Components of the Respiratory System § Organization of respiratory system – Upper respiratory system • Nose, nasal cavity, paranasal sinuses, and pharynx – Lower respiratory system • Larynx, trachea, bronchioles, and alveoli 6 © 2018 Pearson Education, Inc.
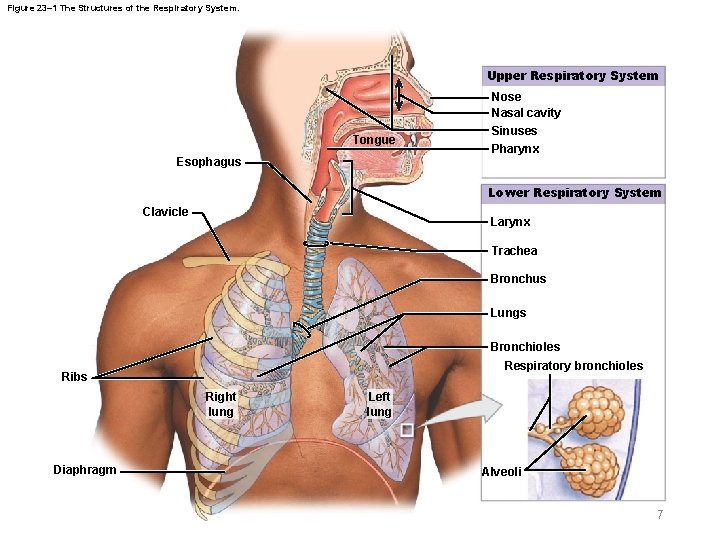
Figure 23– 1 The Structures of the Respiratory System. Upper Respiratory System Tongue Esophagus Nose Nasal cavity Sinuses Pharynx Lower Respiratory System Clavicle Larynx Trachea Bronchus Lungs Bronchioles Respiratory bronchioles Ribs Right lung Diaphragm Left lung Alveoli 7
23 -1 Components of the Respiratory System § Respiratory tract – Conducting portion • From nasal cavity to larger bronchioles – Respiratory portion • Smallest respiratory bronchioles and alveoli – Alveoli • Air-filled pockets within lungs • Where all gas exchange takes place 8 © 2018 Pearson Education, Inc.
23 -1 Components of the Respiratory System § Respiratory mucosa – Lines conducting portion of respiratory system – Consists of • An epithelium • Areolar tissue layer (lamina propria) – Functions in the respiratory defense system • A series of filtration mechanisms • Removes particles and pathogens from inhaled air 9 © 2018 Pearson Education, Inc.
23 -1 Components of the Respiratory System § Lamina propria – In upper respiratory system, trachea, and bronchi • Contains mucous glands that discharge secretions onto epithelial surface – In conducting portion of lower respiratory system • Contains smooth muscle cells that encircle lumen of bronchioles 10 © 2018 Pearson Education, Inc.
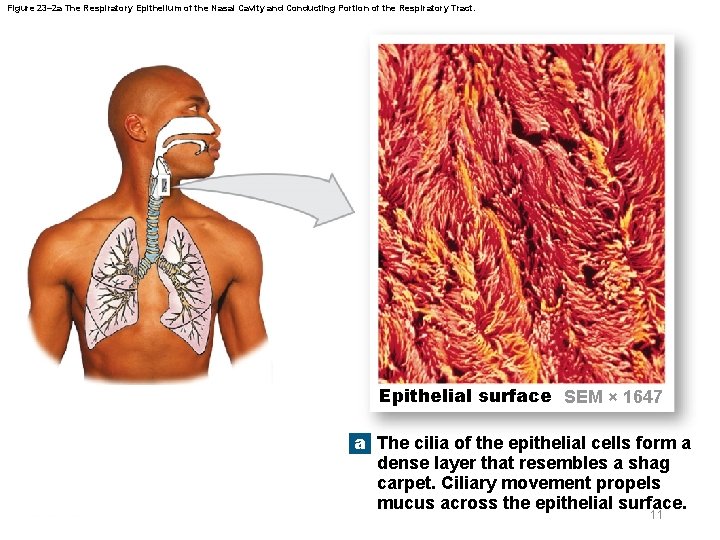
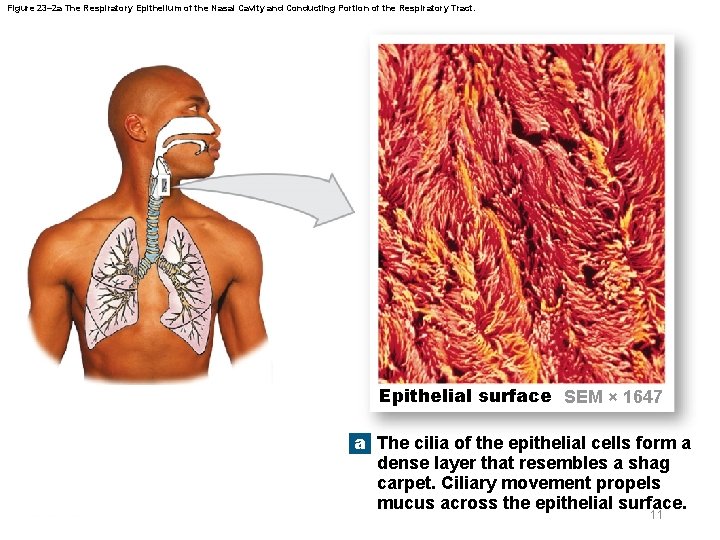
Figure 23– 2 a The Respiratory Epithelium of the Nasal Cavity and Conducting Portion of the Respiratory Tract. Epithelial surface SEM × 1647 a The cilia of the epithelial cells form a dense layer that resembles a shag carpet. Ciliary movement propels mucus across the epithelial surface. 11
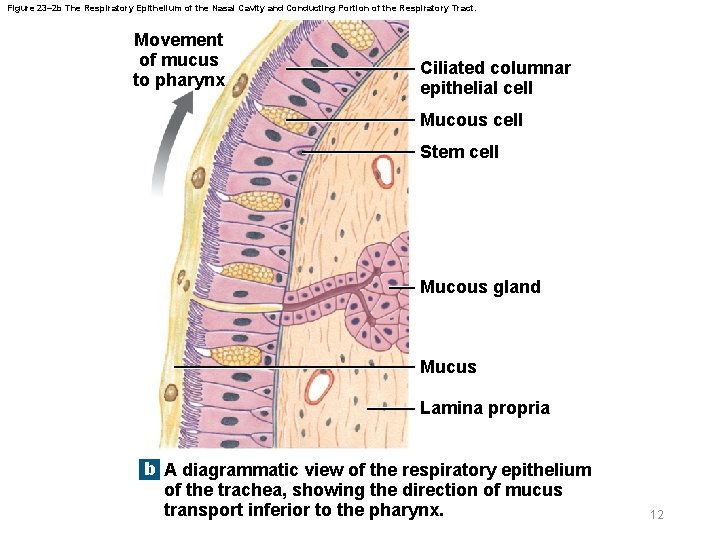
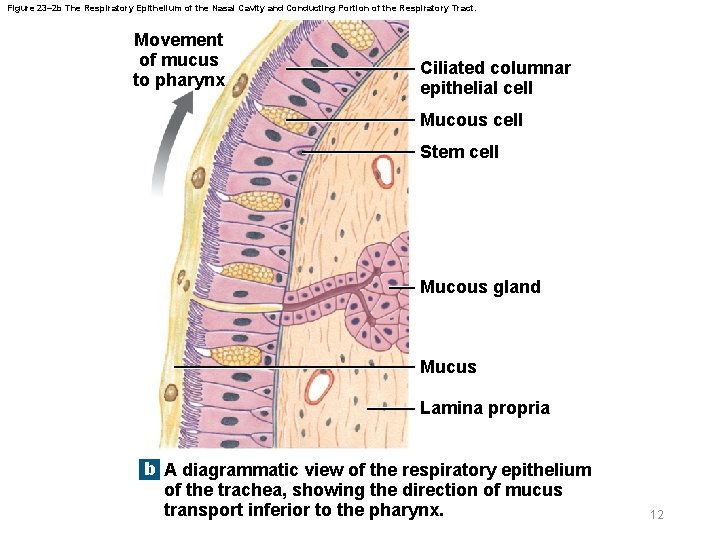
Figure 23– 2 b The Respiratory Epithelium of the Nasal Cavity and Conducting Portion of the Respiratory Tract. Movement of mucus to pharynx Ciliated columnar epithelial cell Mucous cell Stem cell Mucous gland Mucus Lamina propria b A diagrammatic view of the respiratory epithelium of the trachea, showing the direction of mucus transport inferior to the pharynx. 12
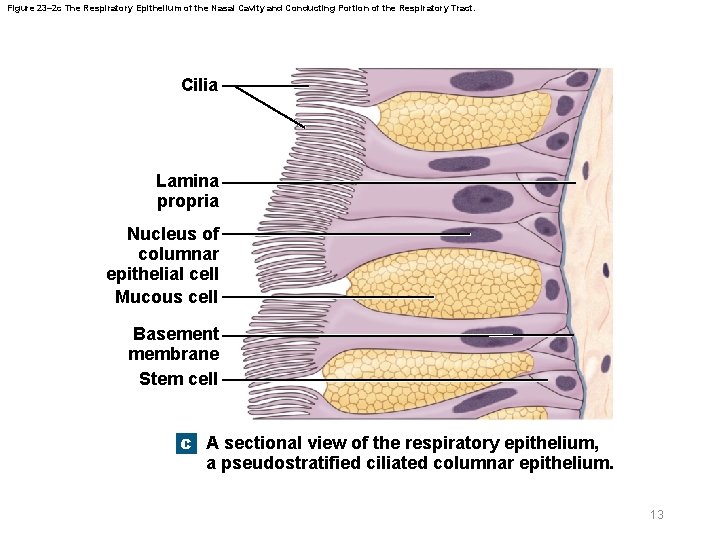
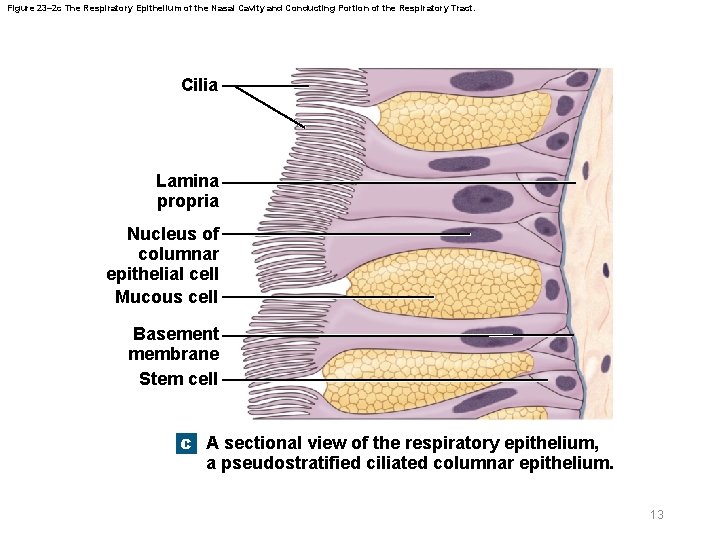
Figure 23– 2 c The Respiratory Epithelium of the Nasal Cavity and Conducting Portion of the Respiratory Tract. Cilia Lamina propria Nucleus of columnar epithelial cell Mucous cell Basement membrane Stem cell c A sectional view of the respiratory epithelium, a pseudostratified ciliated columnar epithelium. 13
23 -1 Components of the Respiratory System § Structure of respiratory epithelium – Nasal cavity and superior portion of pharynx • Pseudostratified ciliated columnar epithelium with numerous mucous cells – Inferior portions of pharynx • Stratified squamous epithelium – Superior portion of lower respiratory system • Pseudostratified ciliated columnar epithelium – Smaller bronchioles • Cuboidal epithelium with scattered cilia 14 © 2018 Pearson Education, Inc.
23 -1 Components of the Respiratory System § Alveolar epithelium – Lines exchange surfaces of alveoli – Very delicate, simple squamous epithelium – Contains scattered, specialized cells 15 © 2018 Pearson Education, Inc.
23 -1 Components of the Respiratory System § Respiratory defense system – Filtration in nasal cavity removes large particles – Mucous cells and mucous glands • Produce mucus that bathes exposed surfaces – Cilia • Sweep mucus and trapped debris and microorganisms toward pharynx to be swallowed – Alveolar macrophages • Engulf small particles that reach lungs 16 © 2018 Pearson Education, Inc.
23 -2 Upper Respiratory System § Nose – Primary passageway for air entering respiratory system – Air enters through nostrils (nares) • Passes into nasal vestibule (space contained within flexible tissues of nose) – Nasal hairs • In epithelium of vestibule • Trap large particles in air 17 © 2018 Pearson Education, Inc.
23 -2 Upper Respiratory System § Nasal cavity – Nasal septum • Divides nasal cavity into left and right sides • Anterior portion (hyaline cartilage) supports dorsum of nose and apex of nose – Superior portion of nasal cavity is olfactory region • Provides sense of smell – Mucus produced in paranasal sinuses and tears • Clean and moisten nasal cavity 18 © 2018 Pearson Education, Inc.
23 -2 Upper Respiratory System § Air flows – From vestibule to choanae (openings of nasal cavity) – Through superior, middle, and inferior nasal meatuses – Meatuses are narrow passageways that produce air turbulence to • Trap particles in mucus • Warm and humidify incoming air • Bring olfactory stimuli to olfactory receptors 19 © 2018 Pearson Education, Inc.
23 -2 Upper Respiratory System § Palates – Hard palate • Forms floor of nasal cavity • Separates nasal and oral cavities – Soft palate • Extends posterior to hard palate • Divides superior nasopharynx from rest of pharynx 20 © 2018 Pearson Education, Inc.
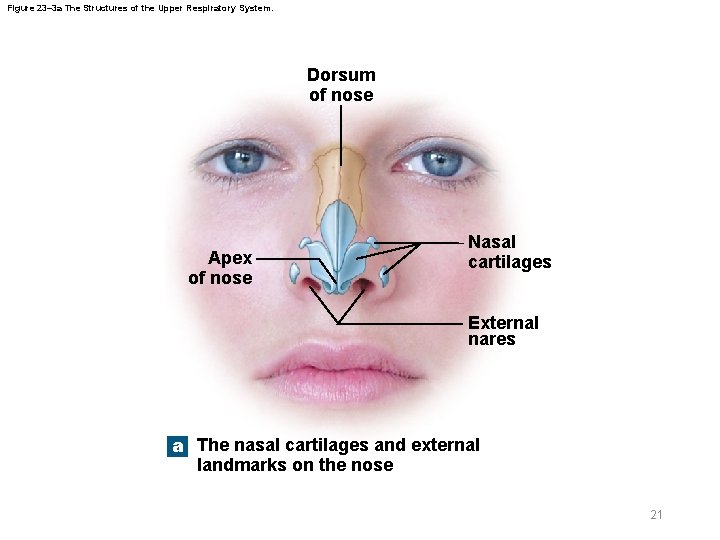
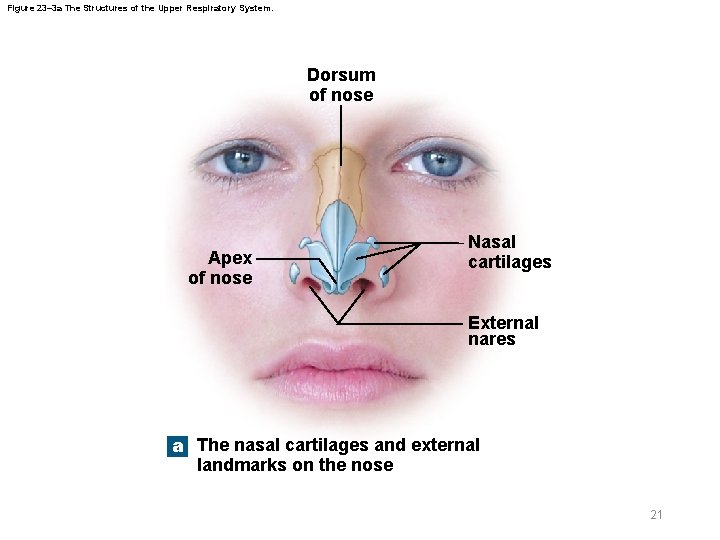
Figure 23– 3 a The Structures of the Upper Respiratory System. Dorsum of nose Apex of nose Nasal cartilages External nares a The nasal cartilages and external landmarks on the nose 21
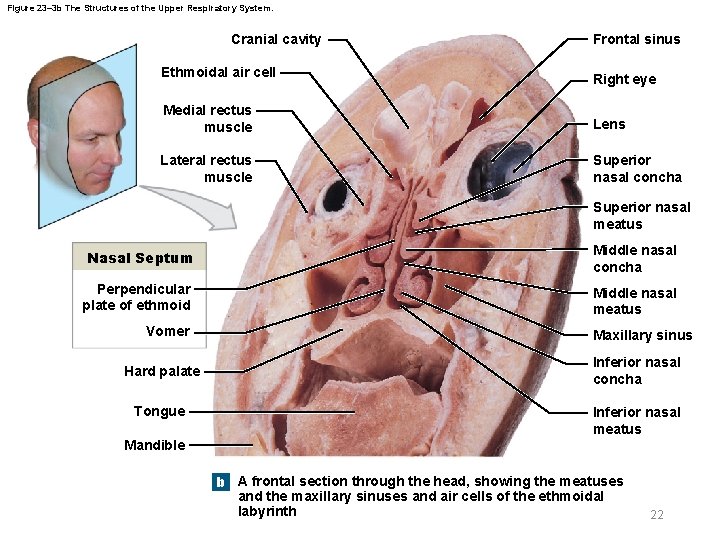
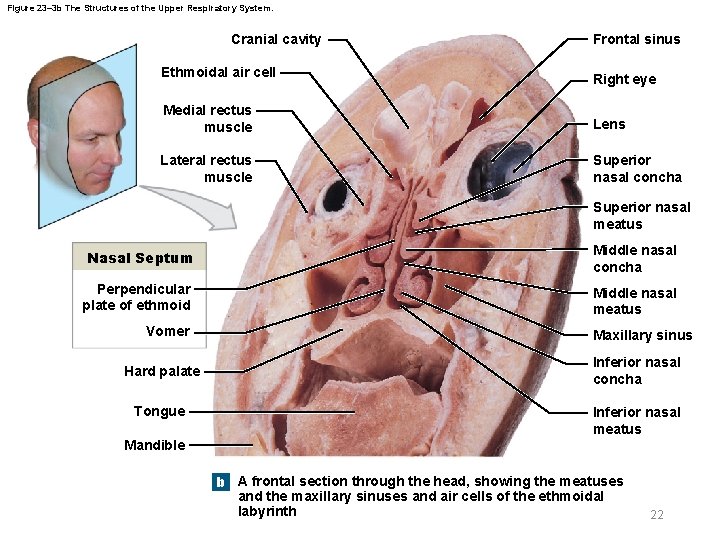
Figure 23– 3 b The Structures of the Upper Respiratory System. Cranial cavity Ethmoidal air cell Frontal sinus Right eye Medial rectus muscle Lens Lateral rectus muscle Superior nasal concha Superior nasal meatus Nasal Septum Middle nasal concha Perpendicular plate of ethmoid Middle nasal meatus Vomer Hard palate Tongue Maxillary sinus Inferior nasal concha Inferior nasal meatus Mandible b A frontal section through the head, showing the meatuses and the maxillary sinuses and air cells of the ethmoidal labyrinth 22
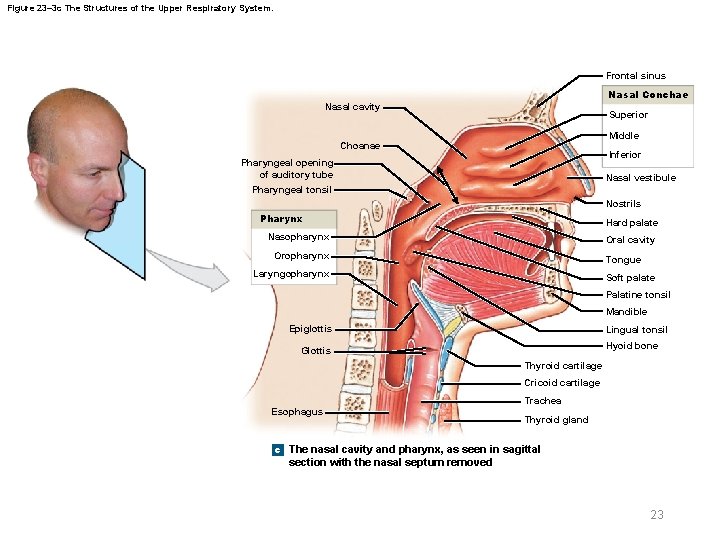
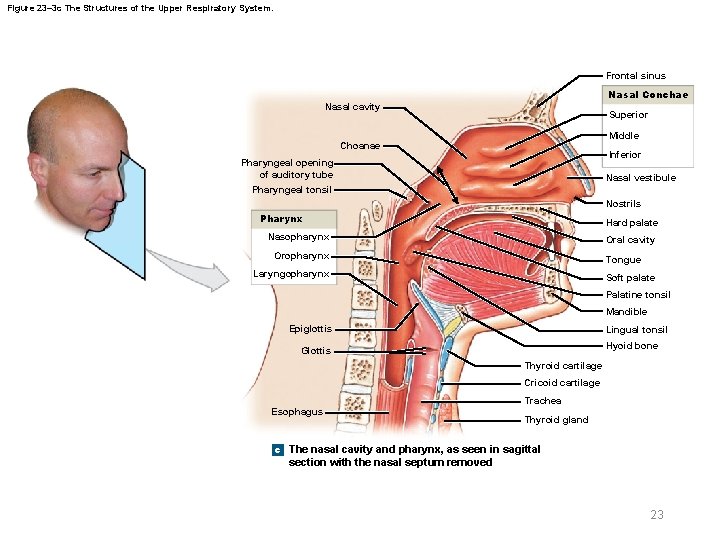
Figure 23– 3 c The Structures of the Upper Respiratory System. Frontal sinus Nasal Conchae Nasal cavity Superior Middle Choanae Inferior Pharyngeal opening of auditory tube Nasal vestibule Pharyngeal tonsil Nostrils Pharynx Hard palate Nasopharynx Oral cavity Oropharynx Tongue Laryngopharynx Soft palate Palatine tonsil Mandible Epiglottis Lingual tonsil Hyoid bone Glottis Thyroid cartilage Cricoid cartilage Esophagus Trachea Thyroid gland c The nasal cavity and pharynx, as seen in sagittal section with the nasal septum removed 23
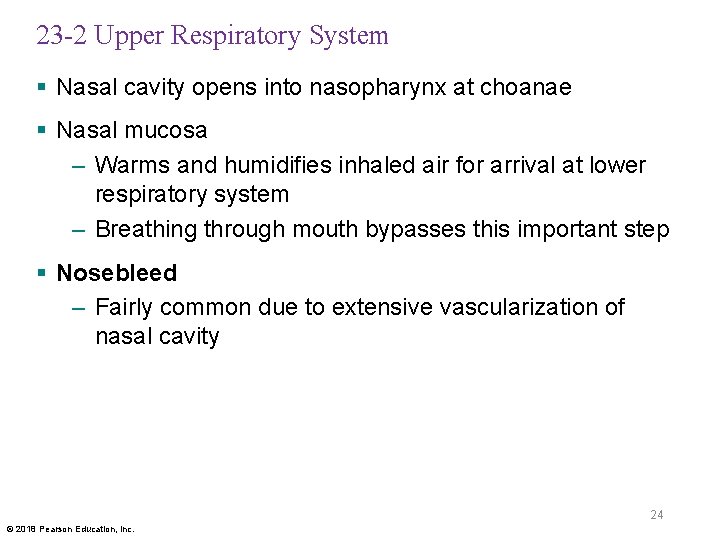
23 -2 Upper Respiratory System § Nasal cavity opens into nasopharynx at choanae § Nasal mucosa – Warms and humidifies inhaled air for arrival at lower respiratory system – Breathing through mouth bypasses this important step § Nosebleed – Fairly common due to extensive vascularization of nasal cavity 24 © 2018 Pearson Education, Inc.
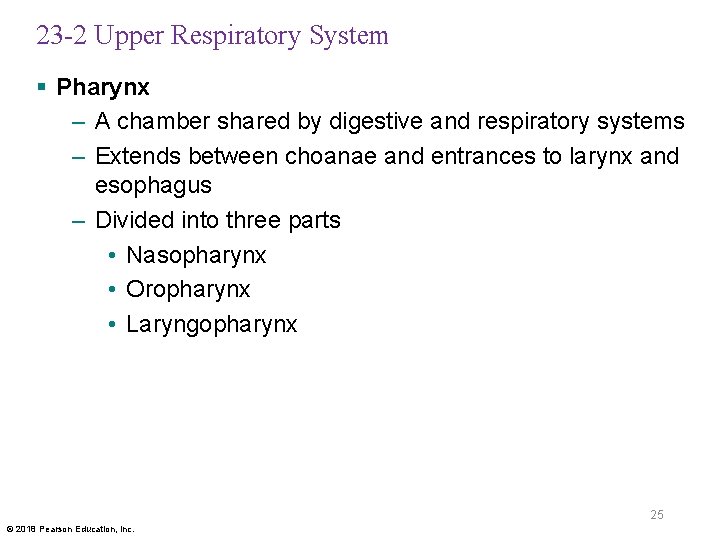
23 -2 Upper Respiratory System § Pharynx – A chamber shared by digestive and respiratory systems – Extends between choanae and entrances to larynx and esophagus – Divided into three parts • Nasopharynx • Oropharynx • Laryngopharynx 25 © 2018 Pearson Education, Inc.
23 -2 Upper Respiratory System § Nasopharynx – Superior portion of pharynx – Contains pharyngeal tonsil and pharyngeal openings of auditory tubes § Oropharynx – Connects directly to oral cavity § Laryngopharynx – Inferior portion of pharynx – Between hyoid bone and entrance to larynx and esophagus 26 © 2018 Pearson Education, Inc.
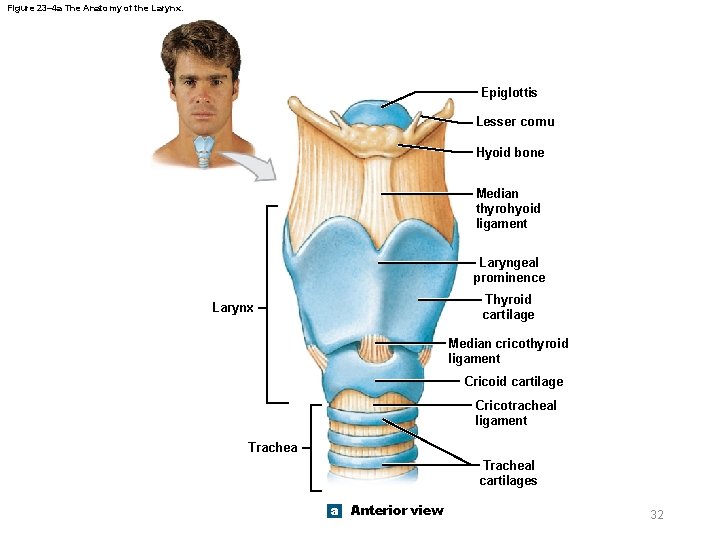
23 -3 Lower Respiratory System § Air flows from pharynx to larynx – Through glottis • Slit-like opening between vocal cords § Three large, unpaired cartilages form the larynx – Thyroid cartilage – Cricoid cartilage – Epiglottis 27 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Thyroid cartilage – Hyaline cartilage – Forms most of anterior and lateral walls of larynx – Anterior surface is called laryngeal prominence, or Adam’s apple – Ligaments attach to hyoid bone, epiglottis, and smaller laryngeal cartilages 28 © 2018 Pearson Education, Inc.
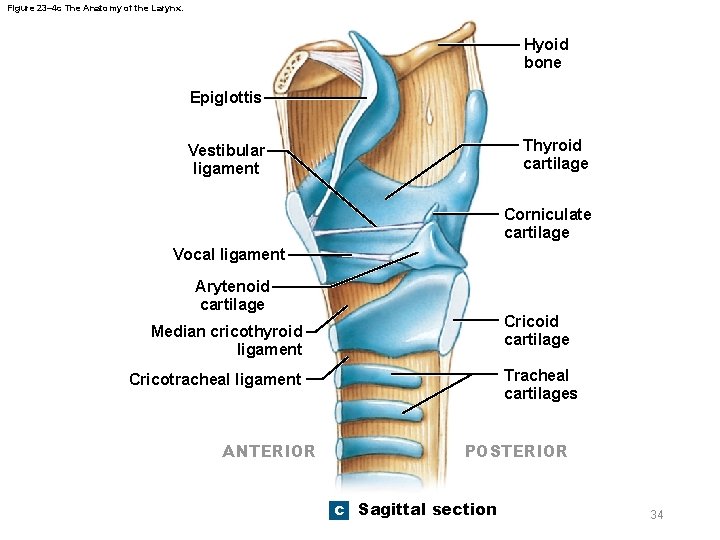
23 -3 Lower Respiratory System § Cricoid cartilage – Hyaline cartilage – Forms posterior portion of larynx – Ligaments attach to first tracheal cartilage – Articulates with arytenoid cartilages § Epiglottis – Elastic cartilage – Covers glottis when swallowing – Ligaments attach to thyroid cartilage and hyoid bone 29 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Thyroid and cricoid cartilages support and protect – Glottis – Entrance to trachea § During swallowing – Larynx is elevated – Epiglottis folds back over glottis • Prevents food and liquids from entering respiratory tract 30 © 2018 Pearson Education, Inc.
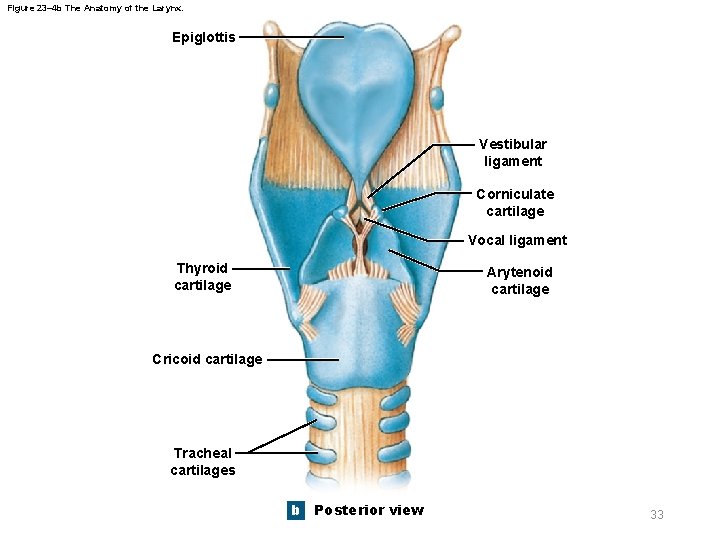
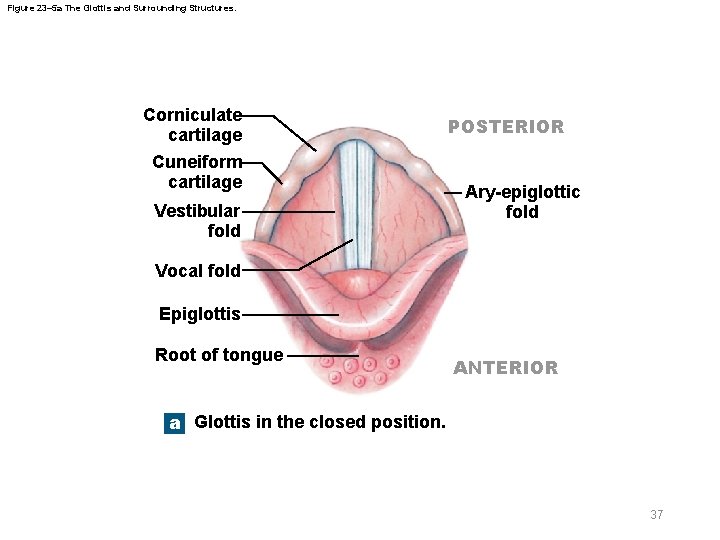
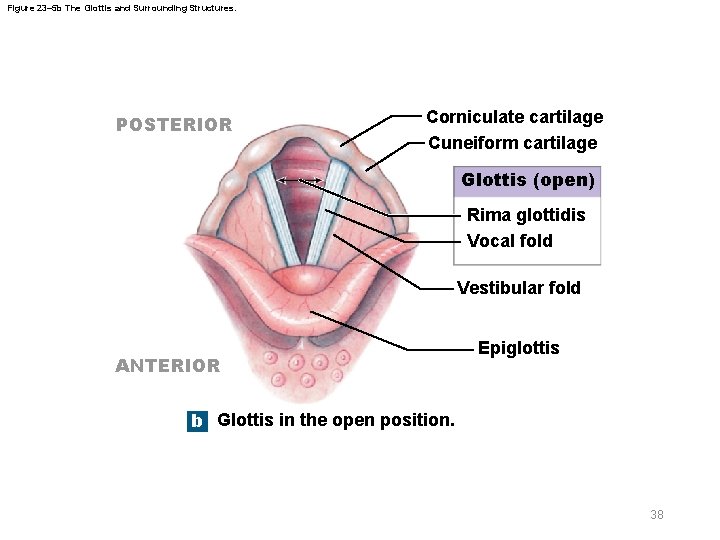
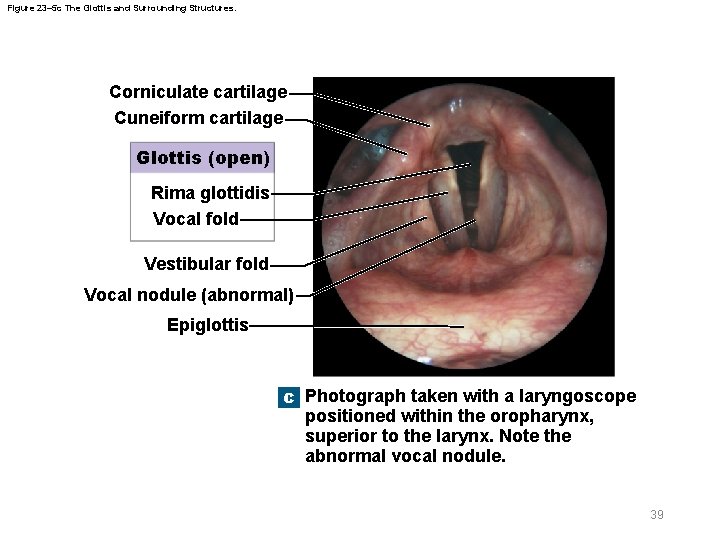
23 -3 Lower Respiratory System § Three pairs of smaller hyaline cartilages in larynx – Arytenoid cartilage – Corniculate cartilage – Cuneiform cartilage § Corniculate and arytenoid cartilages function in – Opening and closing of glottis – Production of sound 31 © 2018 Pearson Education, Inc.
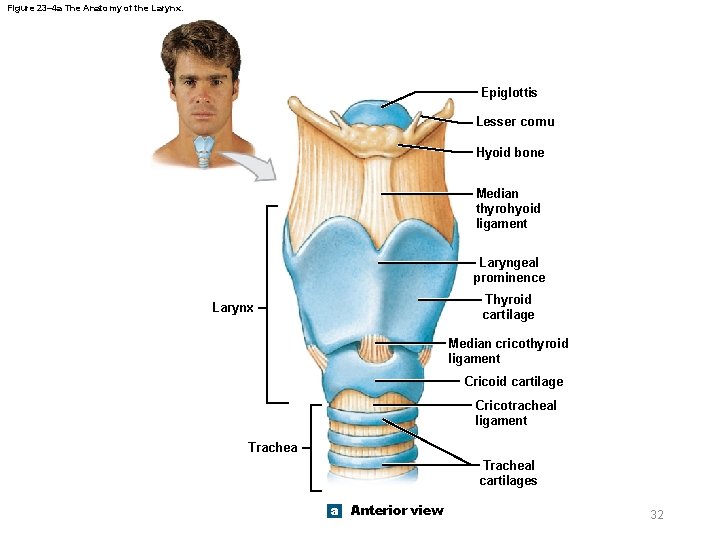
Figure 23– 4 a The Anatomy of the Larynx. Epiglottis Lesser cornu Hyoid bone Median thyrohyoid ligament Laryngeal prominence Thyroid cartilage Larynx Median cricothyroid ligament Cricoid cartilage Cricotracheal ligament Tracheal cartilages a Anterior view 32
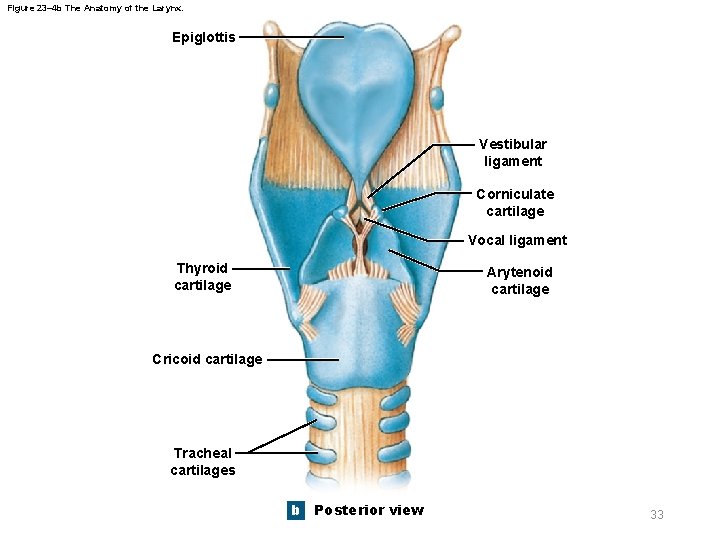
Figure 23– 4 b The Anatomy of the Larynx. Epiglottis Vestibular ligament Corniculate cartilage Vocal ligament Thyroid cartilage Arytenoid cartilage Cricoid cartilage Tracheal cartilages b Posterior view 33
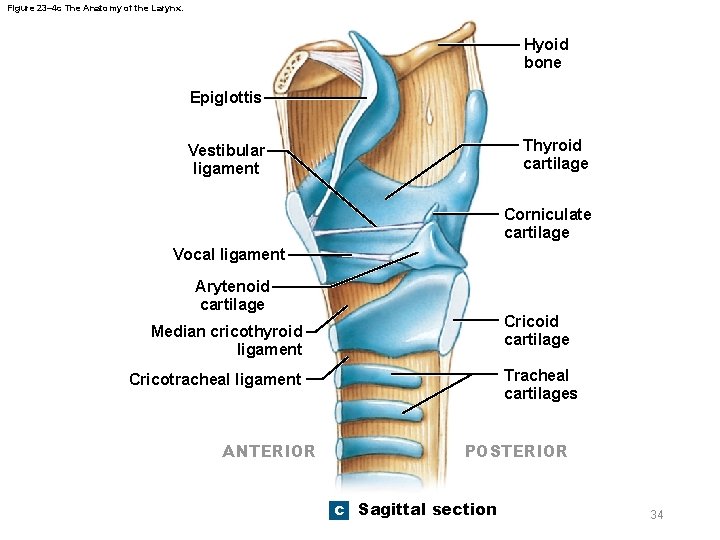
Figure 23– 4 c The Anatomy of the Larynx. Hyoid bone Epiglottis Thyroid cartilage Vestibular ligament Corniculate cartilage Vocal ligament Arytenoid cartilage Cricoid cartilage Median cricothyroid ligament Tracheal cartilages Cricotracheal ligament ANTERIOR POSTERIOR c Sagittal section 34
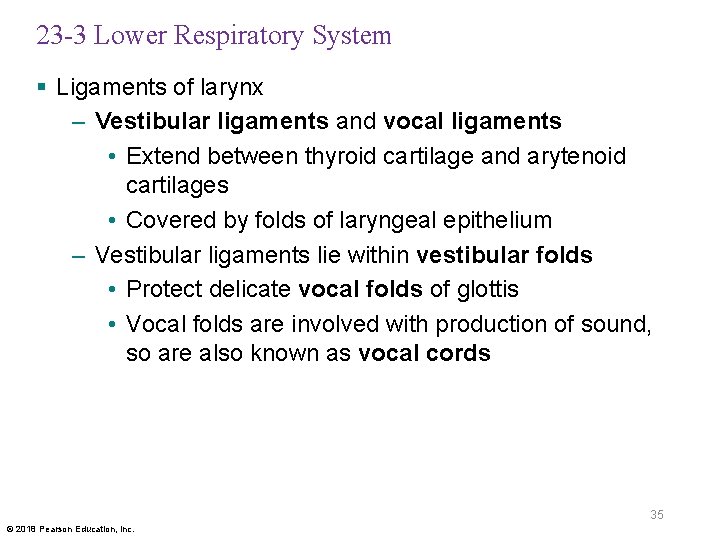
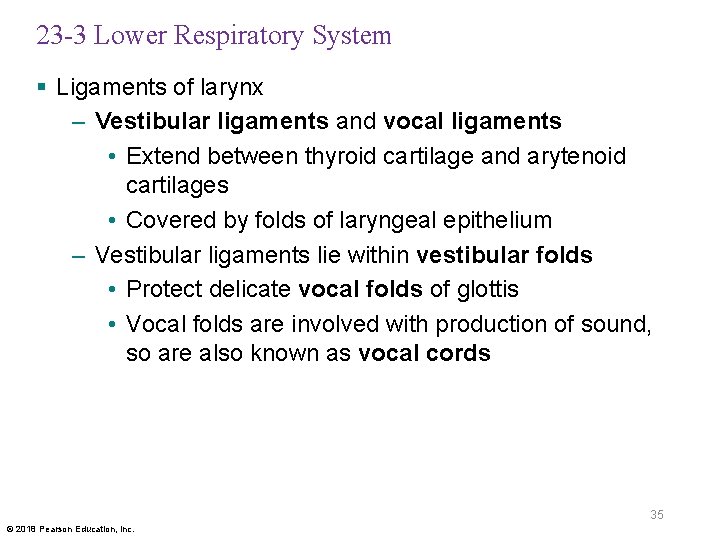
23 -3 Lower Respiratory System § Ligaments of larynx – Vestibular ligaments and vocal ligaments • Extend between thyroid cartilage and arytenoid cartilages • Covered by folds of laryngeal epithelium – Vestibular ligaments lie within vestibular folds • Protect delicate vocal folds of glottis • Vocal folds are involved with production of sound, so are also known as vocal cords 35 © 2018 Pearson Education, Inc.
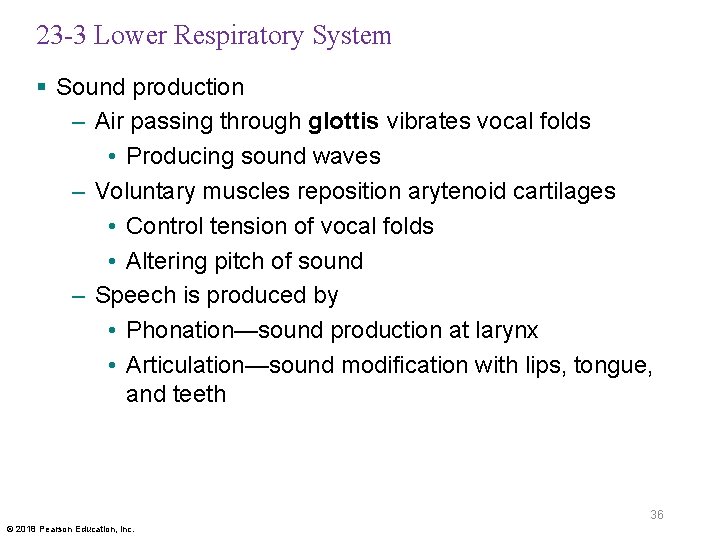
23 -3 Lower Respiratory System § Sound production – Air passing through glottis vibrates vocal folds • Producing sound waves – Voluntary muscles reposition arytenoid cartilages • Control tension of vocal folds • Altering pitch of sound – Speech is produced by • Phonation—sound production at larynx • Articulation—sound modification with lips, tongue, and teeth 36 © 2018 Pearson Education, Inc.
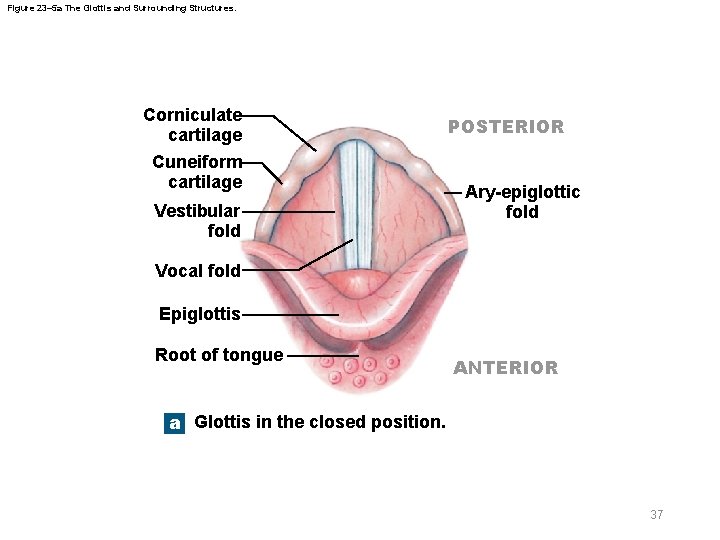
Figure 23– 5 a The Glottis and Surrounding Structures. Corniculate cartilage Cuneiform cartilage Vestibular fold POSTERIOR Ary-epiglottic fold Vocal fold Epiglottis Root of tongue ANTERIOR a Glottis in the closed position. 37
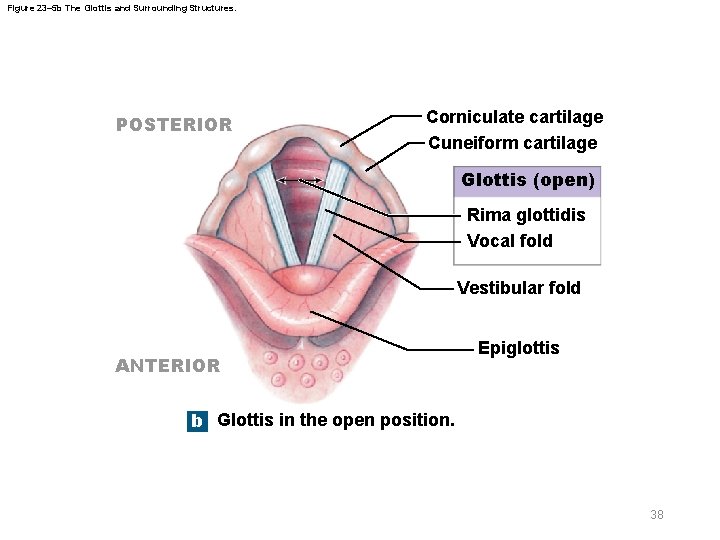
Figure 23– 5 b The Glottis and Surrounding Structures. POSTERIOR Corniculate cartilage Cuneiform cartilage Glottis (open) Rima glottidis Vocal fold Vestibular fold ANTERIOR Epiglottis b Glottis in the open position. 38
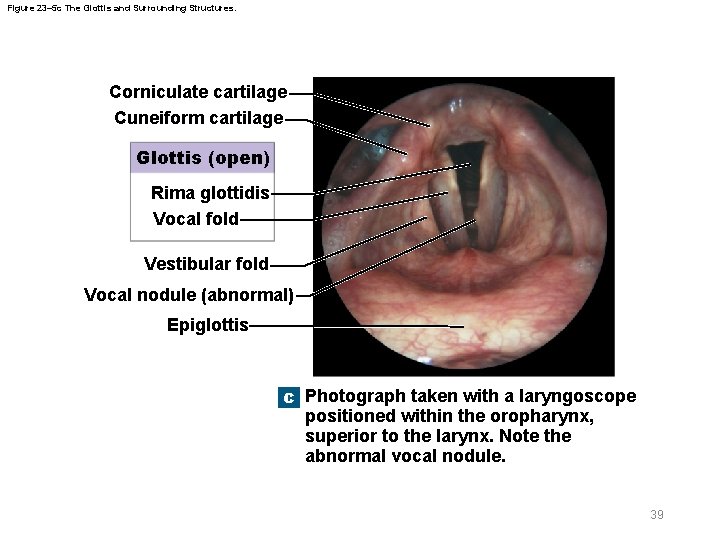
Figure 23– 5 c The Glottis and Surrounding Structures. Corniculate cartilage Cuneiform cartilage Glottis (open) Rima glottidis Vocal fold Vestibular fold Vocal nodule (abnormal) Epiglottis c Photograph taken with a laryngoscope positioned within the oropharynx, superior to the larynx. Note the abnormal vocal nodule. 39
23 -3 Lower Respiratory System § Larynx is associated with two sets of muscles – Muscles of neck and pharynx • Position and stabilize larynx – Smaller intrinsic muscles • Control tension in vocal folds • Open and close glottis 40 © 2018 Pearson Education, Inc.
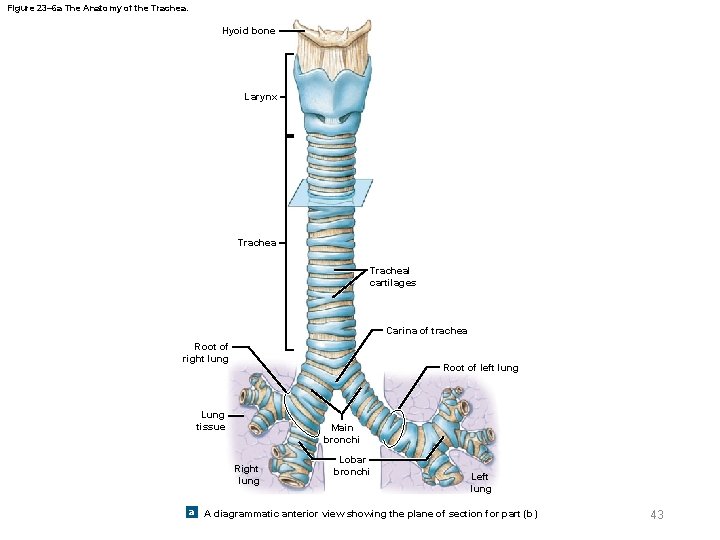
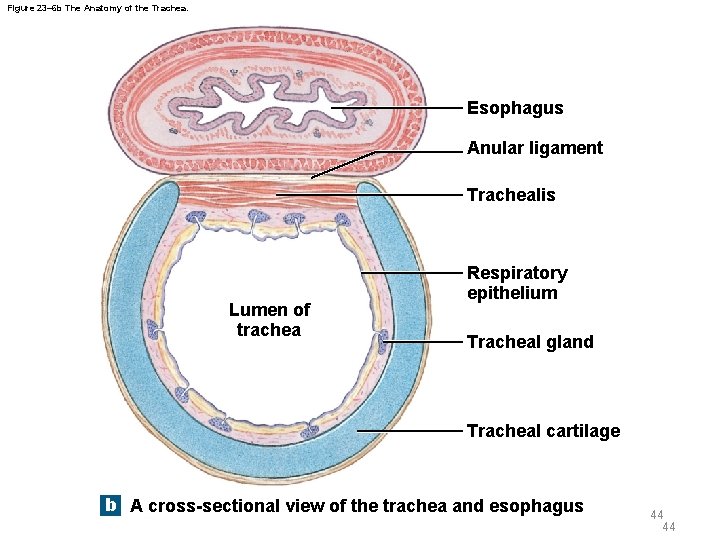
23 -3 Lower Respiratory System § Trachea (windpipe) – Tough, flexible tube – Extends from cricoid cartilage to mediastinum • Branches into right and left main bronchi – Submucosa • Thick layer of connective tissue • Surrounds mucosa • Contains tracheal glands that produce mucous secretions 41 © 2018 Pearson Education, Inc.
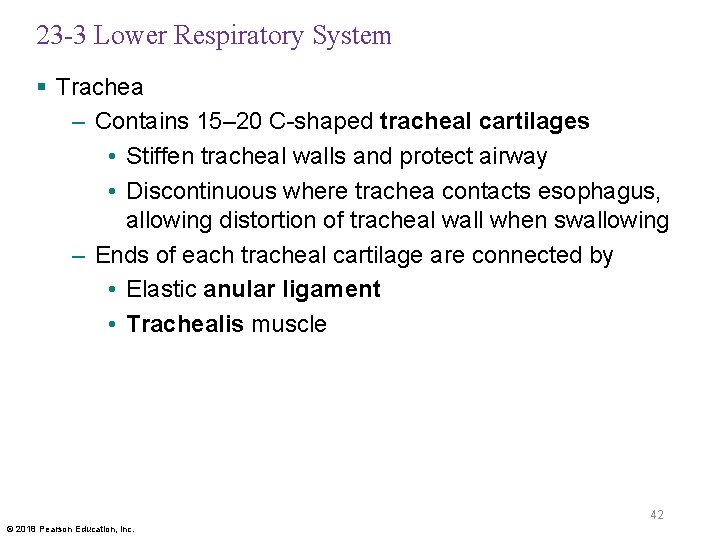
23 -3 Lower Respiratory System § Trachea – Contains 15– 20 C-shaped tracheal cartilages • Stiffen tracheal walls and protect airway • Discontinuous where trachea contacts esophagus, allowing distortion of tracheal wall when swallowing – Ends of each tracheal cartilage are connected by • Elastic anular ligament • Trachealis muscle 42 © 2018 Pearson Education, Inc.
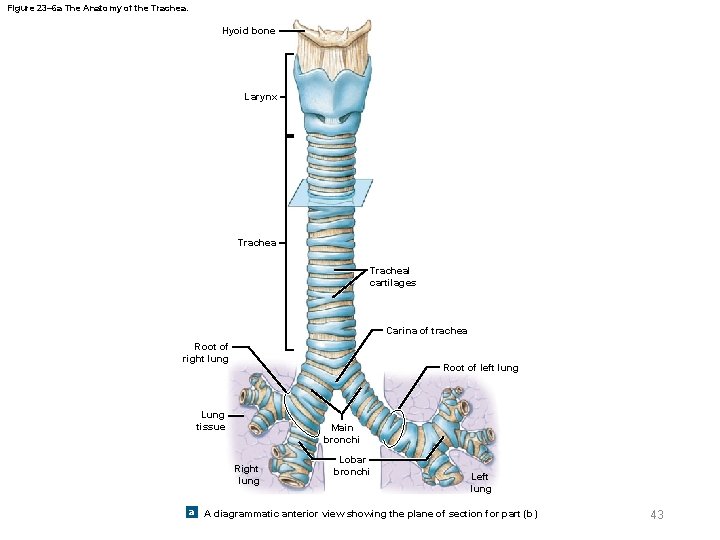
Figure 23– 6 a The Anatomy of the Trachea. Hyoid bone Larynx Tracheal cartilages Carina of trachea Root of right lung Root of left lung Lung tissue Main bronchi Right lung Lobar bronchi Left lung a A diagrammatic anterior view showing the plane of section for part (b) 43
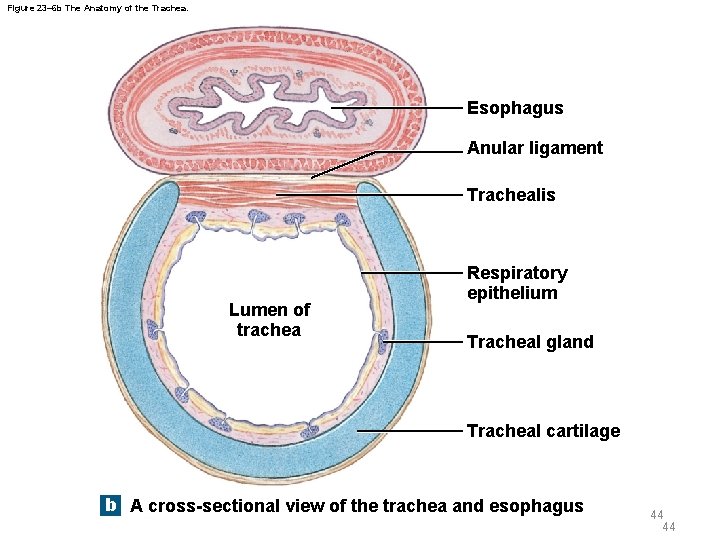
Figure 23– 6 b The Anatomy of the Trachea. Esophagus Anular ligament Trachealis Lumen of trachea Respiratory epithelium Tracheal gland Tracheal cartilage b A cross-sectional view of the trachea and esophagus 44 44
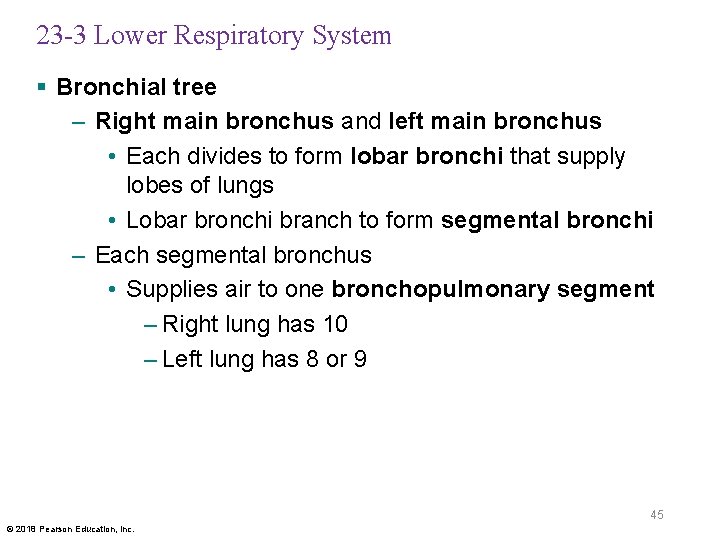
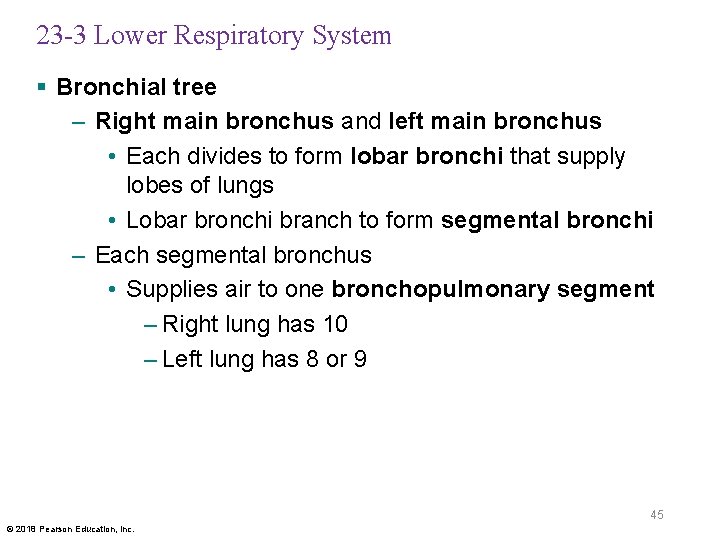
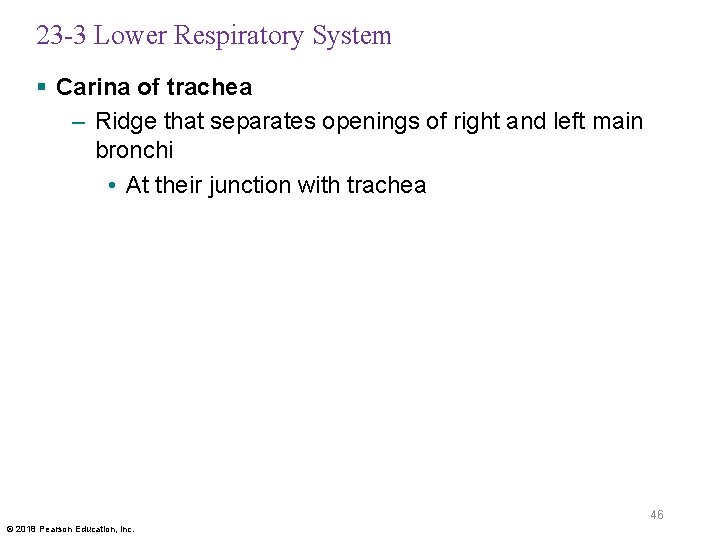
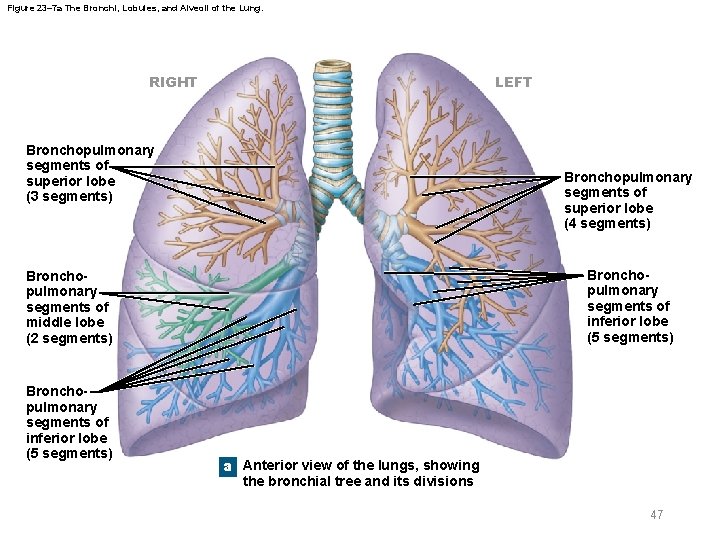
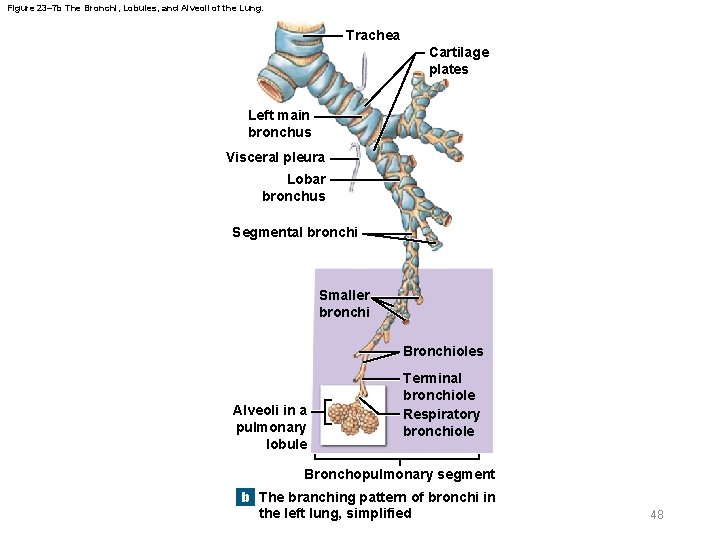
23 -3 Lower Respiratory System § Bronchial tree – Right main bronchus and left main bronchus • Each divides to form lobar bronchi that supply lobes of lungs • Lobar bronchi branch to form segmental bronchi – Each segmental bronchus • Supplies air to one bronchopulmonary segment – Right lung has 10 – Left lung has 8 or 9 45 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Carina of trachea – Ridge that separates openings of right and left main bronchi • At their junction with trachea 46 © 2018 Pearson Education, Inc.
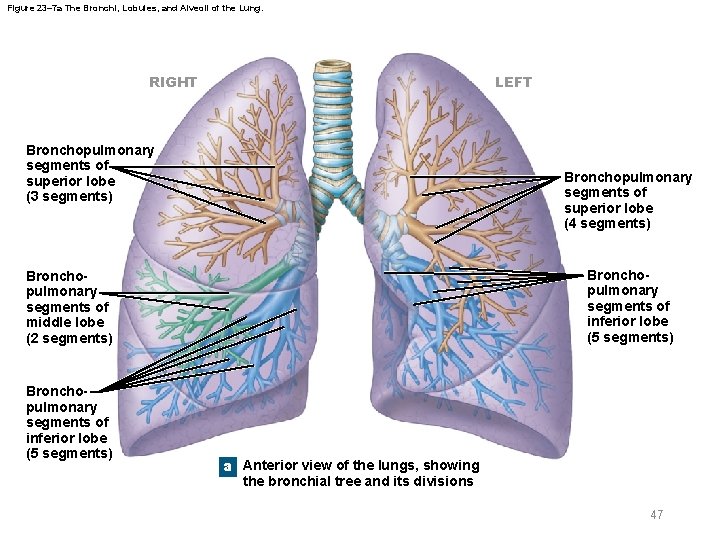
Figure 23– 7 a The Bronchi, Lobules, and Alveoli of the Lung. RIGHT LEFT Bronchopulmonary segments of superior lobe (3 segments) Bronchopulmonary segments of superior lobe (4 segments) Bronchopulmonary segments of inferior lobe (5 segments) Bronchopulmonary segments of middle lobe (2 segments) Bronchopulmonary segments of inferior lobe (5 segments) a Anterior view of the lungs, showing the bronchial tree and its divisions 47
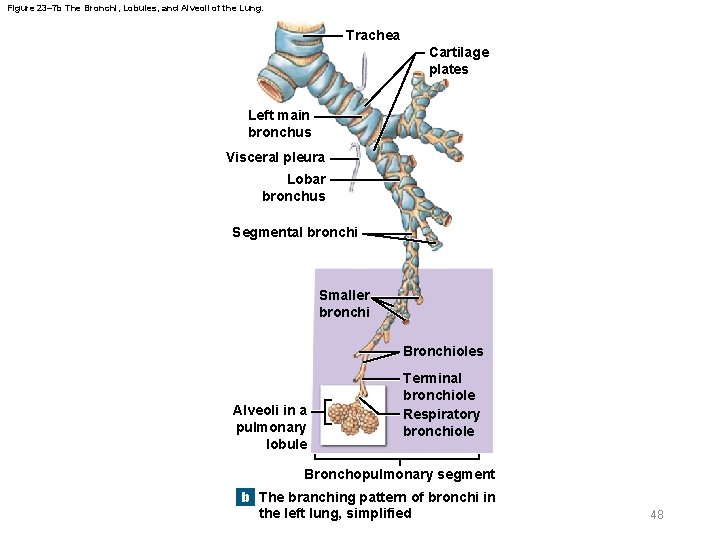
Figure 23– 7 b The Bronchi, Lobules, and Alveoli of the Lung. Trachea Cartilage plates Left main bronchus Visceral pleura Lobar bronchus Segmental bronchi Smaller bronchi Bronchioles Alveoli in a pulmonary lobule Terminal bronchiole Respiratory bronchiole Bronchopulmonary segment b The branching pattern of bronchi in the left lung, simplified 48
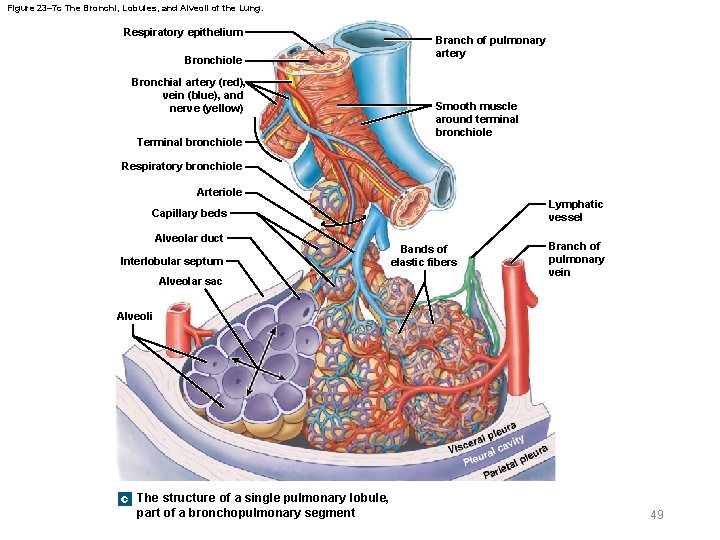
Figure 23– 7 c The Bronchi, Lobules, and Alveoli of the Lung. Respiratory epithelium Bronchiole Bronchial artery (red), vein (blue), and nerve (yellow) Terminal bronchiole Branch of pulmonary artery Smooth muscle around terminal bronchiole Respiratory bronchiole Arteriole Lymphatic vessel Capillary beds Alveolar duct Interlobular septum Alveolar sac Bands of elastic fibers Branch of pulmonary vein Alveoli c The structure of a single pulmonary lobule, part of a bronchopulmonary segment 49
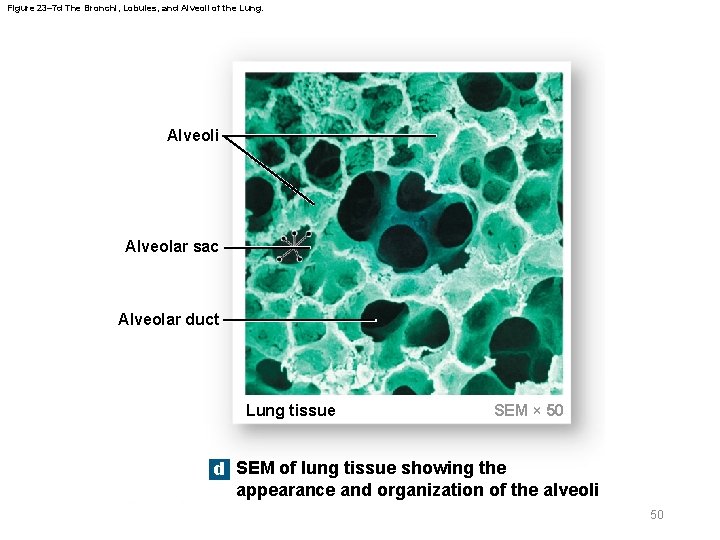
Figure 23– 7 d The Bronchi, Lobules, and Alveoli of the Lung. Alveoli Alveolar sac Alveolar duct Lung tissue SEM × 50 d SEM of lung tissue showing the appearance and organization of the alveoli 50
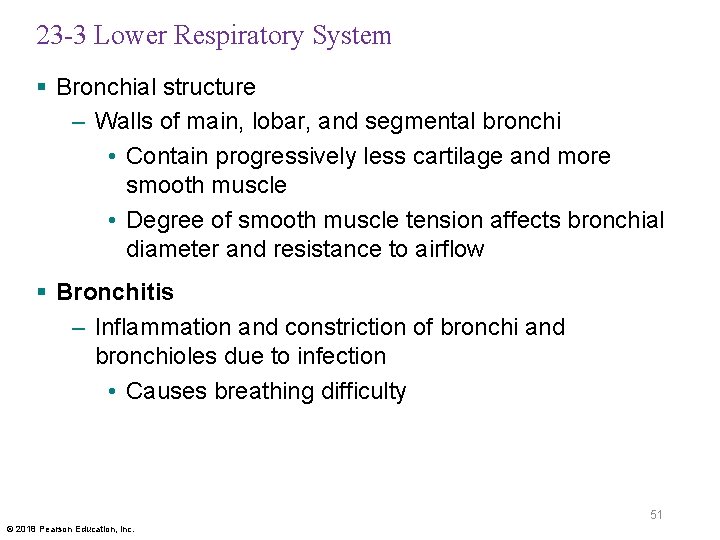
23 -3 Lower Respiratory System § Bronchial structure – Walls of main, lobar, and segmental bronchi • Contain progressively less cartilage and more smooth muscle • Degree of smooth muscle tension affects bronchial diameter and resistance to airflow § Bronchitis – Inflammation and constriction of bronchi and bronchioles due to infection • Causes breathing difficulty 51 © 2018 Pearson Education, Inc.
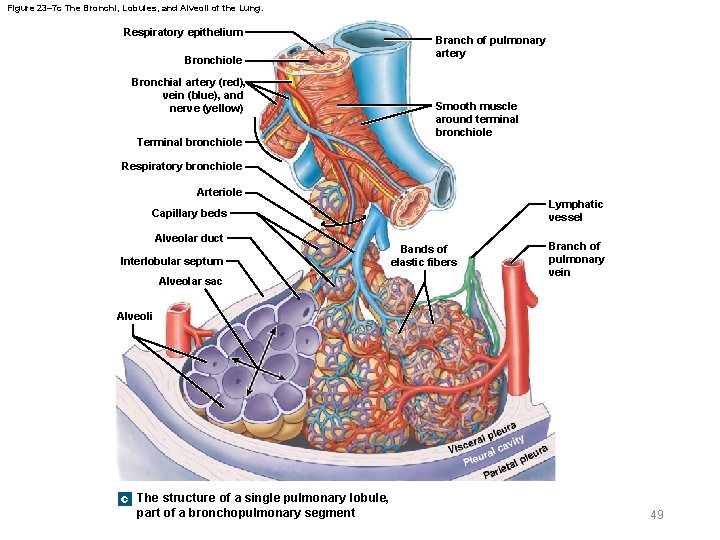
23 -3 Lower Respiratory System § Bronchioles – Each segmental bronchus branches into multiple bronchioles – Bronchioles branch into terminal bronchioles • Each segmental bronchus forms about 6500 terminal bronchioles – Bronchioles have no cartilage • Dominated by smooth muscle 52 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Autonomic nervous system – Controls luminal diameter of bronchioles by regulating smooth muscle – Controls airflow in lungs 53 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Bronchodilation – Caused by sympathetic activation – Enlarges luminal diameter of airway – Reduces resistance to airflow § Bronchoconstriction – Reduces luminal diameter of airway – Caused by • Parasympathetic activation • Histamine release (allergic reactions) 54 © 2018 Pearson Education, Inc.
23 -3 Lower Respiratory System § Asthma – Excessive stimulation of smooth muscles – Causing severe bronchoconstriction • Restricts airflow 55 © 2018 Pearson Education, Inc.
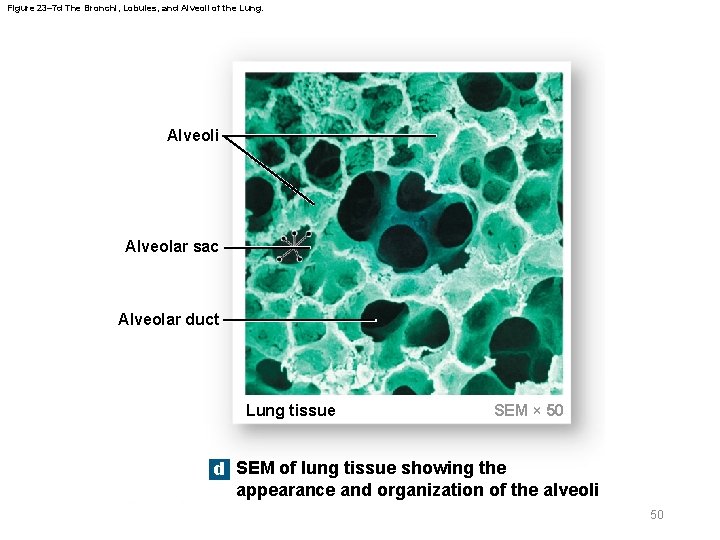
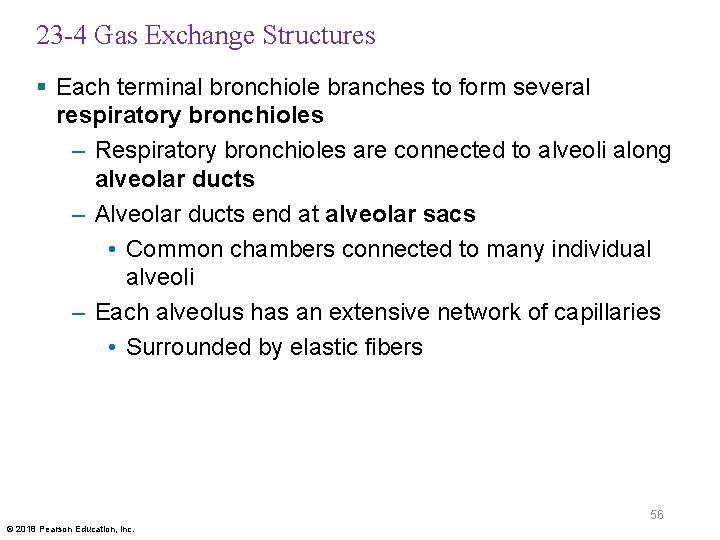
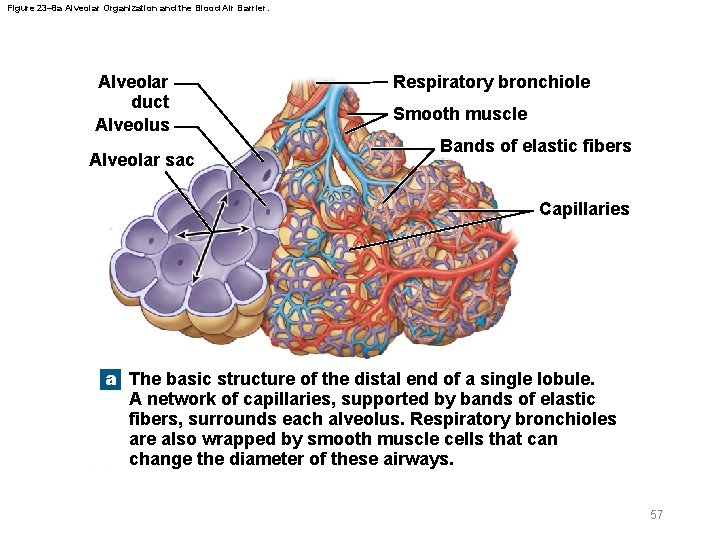
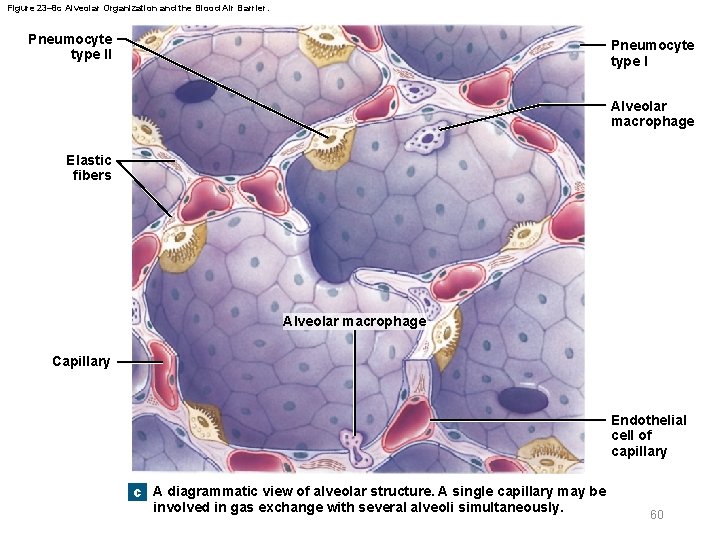
23 -4 Gas Exchange Structures § Each terminal bronchiole branches to form several respiratory bronchioles – Respiratory bronchioles are connected to alveoli along alveolar ducts – Alveolar ducts end at alveolar sacs • Common chambers connected to many individual alveoli – Each alveolus has an extensive network of capillaries • Surrounded by elastic fibers 56 © 2018 Pearson Education, Inc.
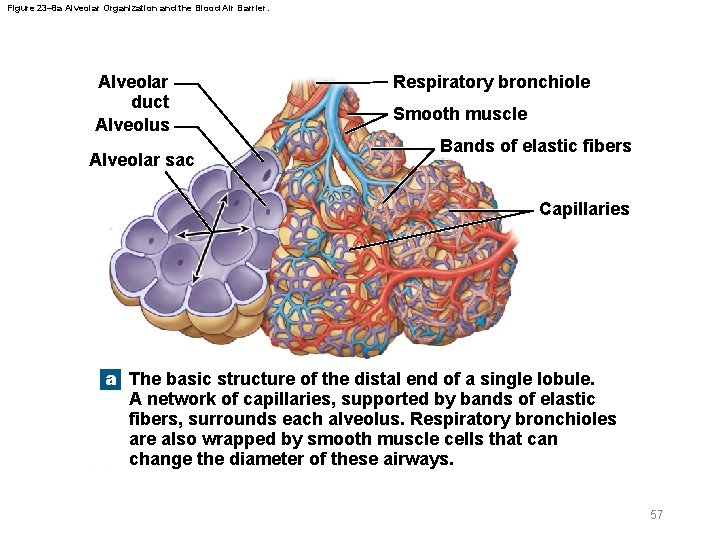
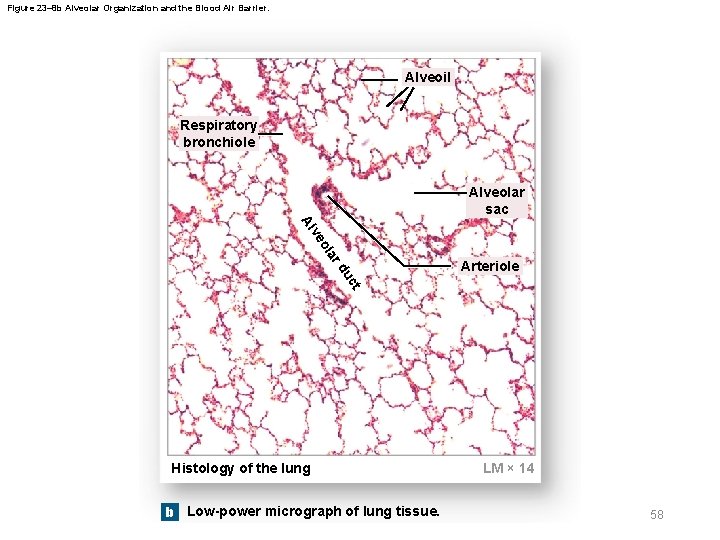
Figure 23– 8 a Alveolar Organization and the Blood Air Barrier. Alveolar duct Alveolus Alveolar sac Respiratory bronchiole Smooth muscle Bands of elastic fibers Capillaries a The basic structure of the distal end of a single lobule. A network of capillaries, supported by bands of elastic fibers, surrounds each alveolus. Respiratory bronchioles are also wrapped by smooth muscle cells that can change the diameter of these airways. 57
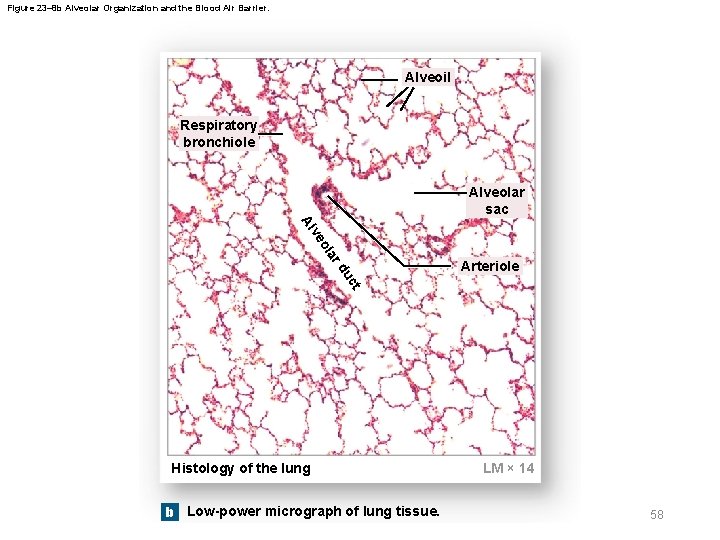
Figure 23– 8 b Alveolar Organization and the Blood Air Barrier. Alveoil Respiratory bronchiole Alveolar sac lar o ve Al ct du Arteriole Histology of the lung b Low-power micrograph of lung tissue. LM × 14 58
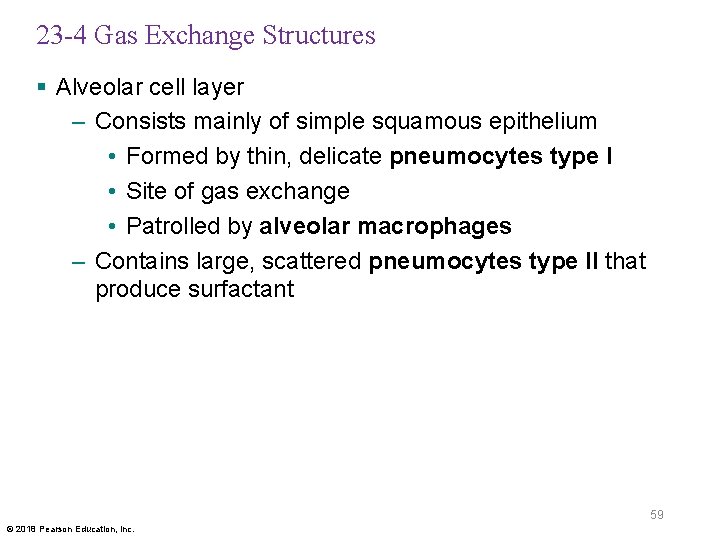
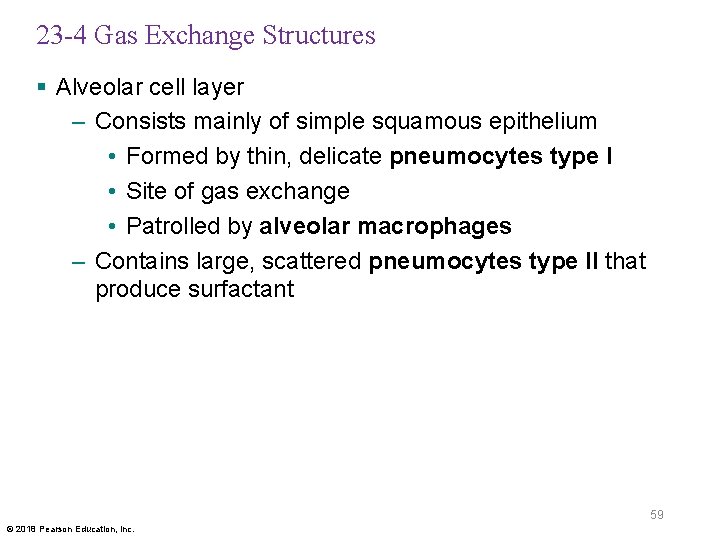
23 -4 Gas Exchange Structures § Alveolar cell layer – Consists mainly of simple squamous epithelium • Formed by thin, delicate pneumocytes type I • Site of gas exchange • Patrolled by alveolar macrophages – Contains large, scattered pneumocytes type II that produce surfactant 59 © 2018 Pearson Education, Inc.
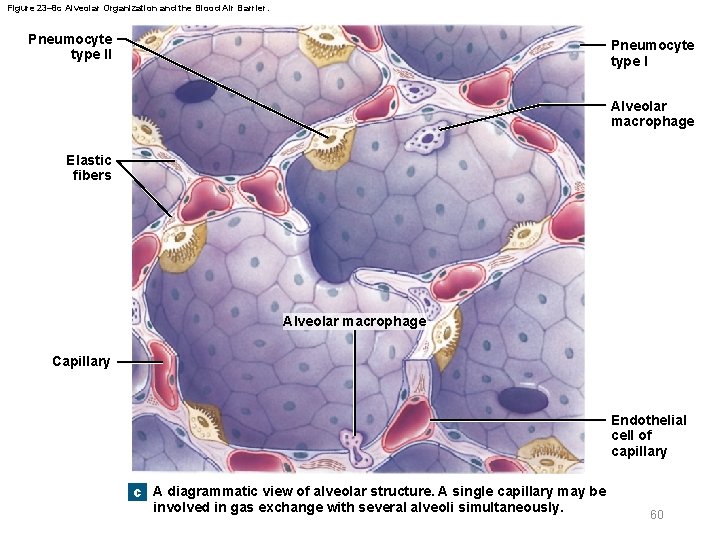
Figure 23– 8 c Alveolar Organization and the Blood Air Barrier. Pneumocyte type II Pneumocyte type I Alveolar macrophage Elastic fibers Alveolar macrophage Capillary Endothelial cell of capillary c A diagrammatic view of alveolar structure. A single capillary may be involved in gas exchange with several alveoli simultaneously. 60
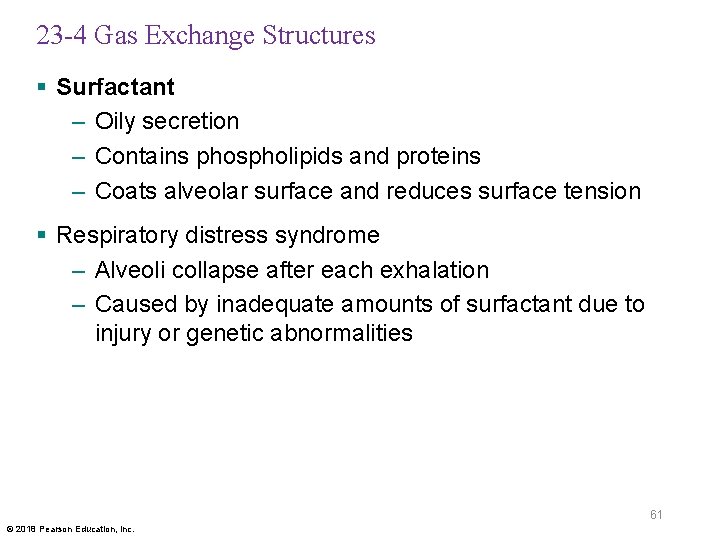
23 -4 Gas Exchange Structures § Surfactant – Oily secretion – Contains phospholipids and proteins – Coats alveolar surface and reduces surface tension § Respiratory distress syndrome – Alveoli collapse after each exhalation – Caused by inadequate amounts of surfactant due to injury or genetic abnormalities 61 © 2018 Pearson Education, Inc.
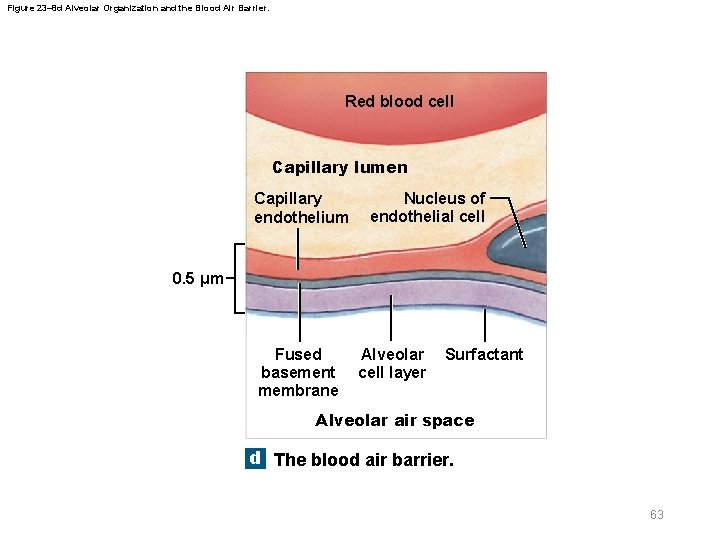
23 -4 Gas Exchange Structures § Gas exchange occurs across blood air barrier of alveoli – Consists of three layers • Alveolar cell layer • Capillary endothelial layer • Fused basement membrane between them 62 © 2018 Pearson Education, Inc.
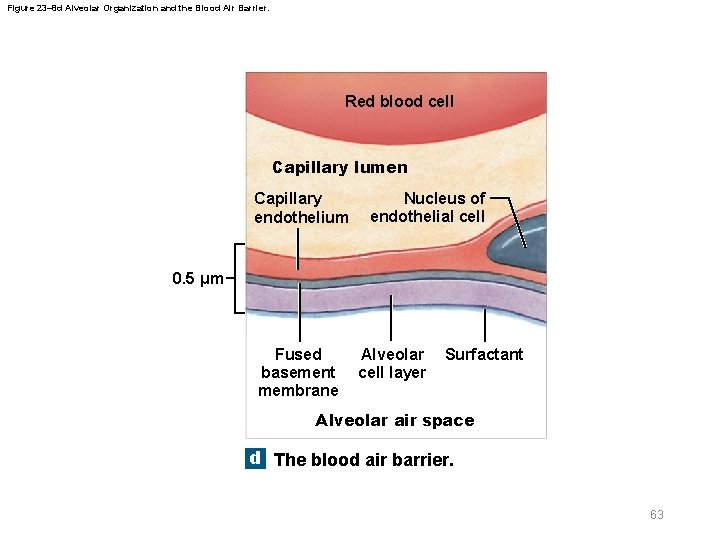
Figure 23– 8 d Alveolar Organization and the Blood Air Barrier. Red blood cell Capillary lumen Capillary endothelium Nucleus of endothelial cell 0. 5 µm Fused basement membrane Alveolar cell layer Surfactant Alveolar air space d The blood air barrier. 63
23 -4 Gas Exchange Structures § Gas exchange across blood air barrier is quick and efficient – Because distance for diffusion is short – And O 2 and CO 2 are small and lipid soluble § Pneumonia – Inflammation of lung tissue – Causes fluid to leak into alveoli – Compromises function of blood air barrier 64 © 2018 Pearson Education, Inc.
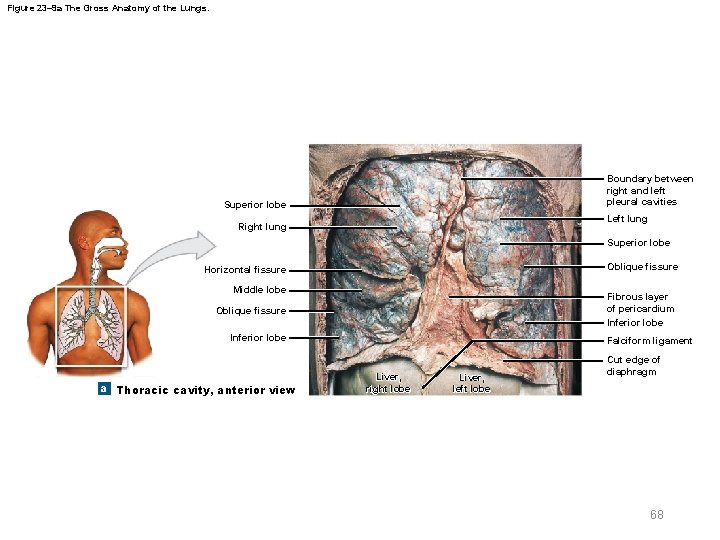
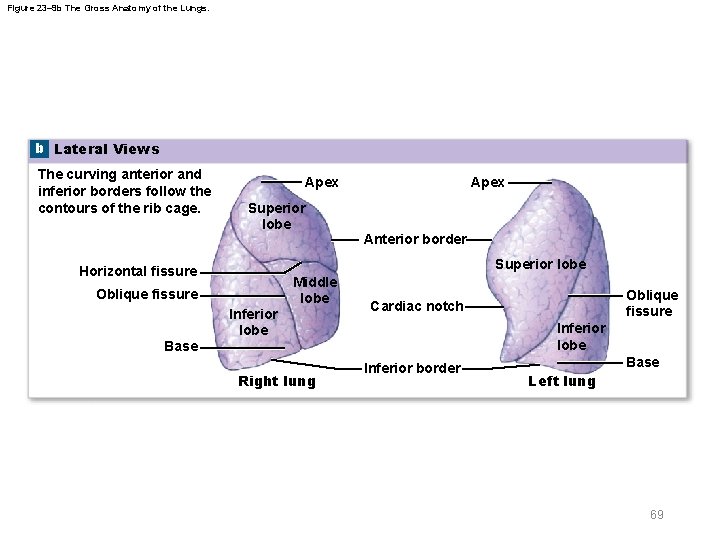
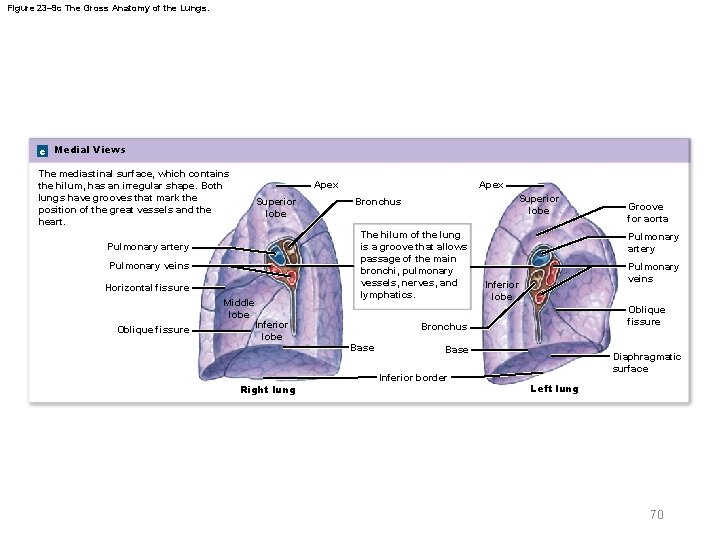
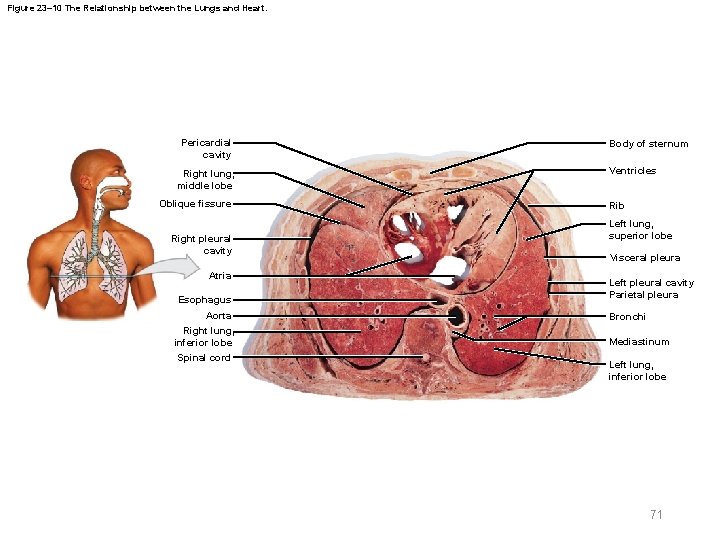
23 -5 The Lungs § Left and right lungs – In left and right pleural cavities – Inferior portion (base) rests on diaphragm § Lobes of lungs are separated by deep fissures – Right lung has three lobes • Superior, middle, and inferior • Separated by horizontal and oblique fissures – Left lung has two lobes • Superior and inferior • Separated by oblique fissure 65 © 2018 Pearson Education, Inc.
23 -5 The Lungs § Right lung – Wider than left lung – Displaced upward by liver § Left lung – Longer than right lung – Indented on medial margin forming cardiac notch 66 © 2018 Pearson Education, Inc.
23 -5 The Lungs § Hilum – Where pulmonary vessels, nerves, and lymphatics enter lung § Root of the lung – Complex of dense connective tissue, nerves, and vessels in hilum • Anchored to mediastinum 67 © 2018 Pearson Education, Inc.
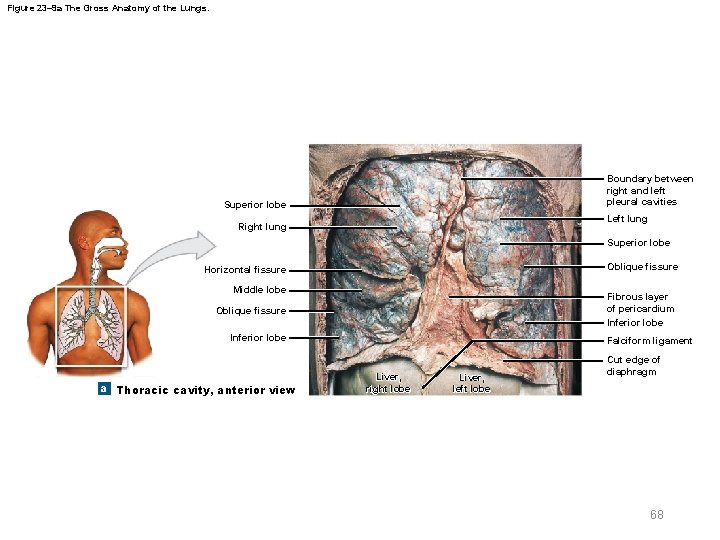
Figure 23– 9 a The Gross Anatomy of the Lungs. Boundary between right and left pleural cavities Superior lobe Left lung Right lung Superior lobe Oblique fissure Horizontal fissure Middle lobe Fibrous layer of pericardium Inferior lobe Oblique fissure Inferior lobe a Thoracic cavity, anterior view Falciform ligament Liver, right lobe Liver, left lobe Cut edge of diaphragm 68
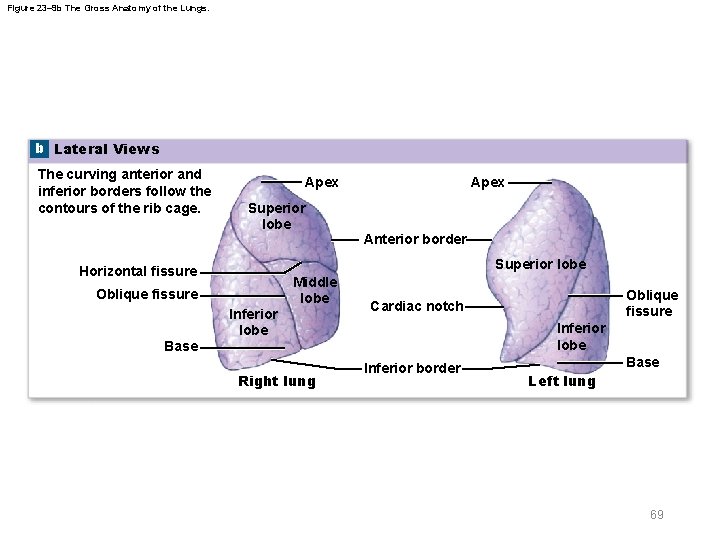
Figure 23– 9 b The Gross Anatomy of the Lungs. b Lateral Views The curving anterior and inferior borders follow the contours of the rib cage. Apex Superior lobe Apex Anterior border Superior lobe Horizontal fissure Oblique fissure Inferior lobe Middle lobe Inferior lobe Base Right lung Oblique fissure Cardiac notch Inferior border Base Left lung 69
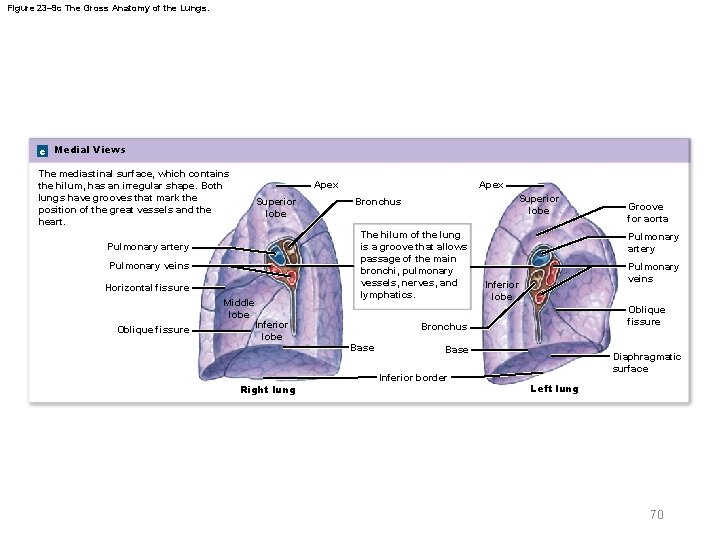
Figure 23– 9 c The Gross Anatomy of the Lungs. c Medial Views The mediastinal surface, which contains the hilum, has an irregular shape. Both lungs have grooves that mark the position of the great vessels and the heart. Apex Superior lobe Pulmonary artery Pulmonary veins Horizontal fissure Oblique fissure Middle lobe Inferior lobe Right lung Apex Superior lobe Bronchus The hilum of the lung is a groove that allows passage of the main bronchi, pulmonary vessels, nerves, and lymphatics. Pulmonary artery Pulmonary veins Inferior lobe Oblique fissure Bronchus Base Inferior border Groove for aorta Diaphragmatic surface Left lung 70
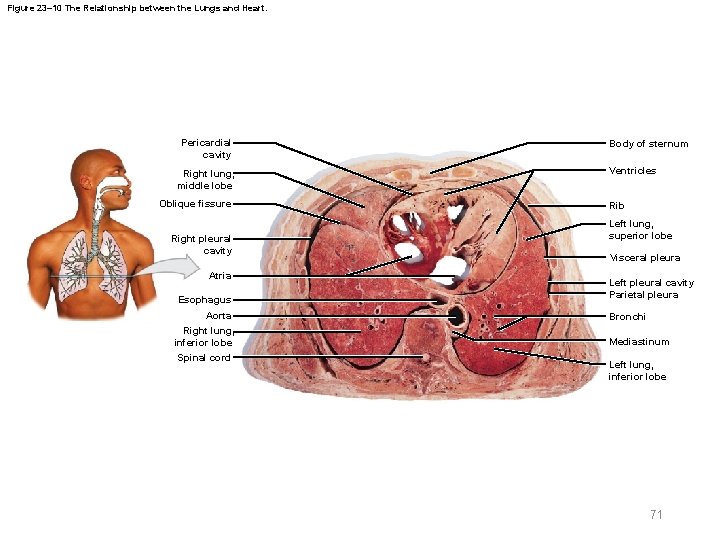
Figure 23– 10 The Relationship between the Lungs and Heart. Pericardial cavity Right lung, middle lobe Oblique fissure Right pleural cavity Atria Esophagus Aorta Right lung, inferior lobe Spinal cord Body of sternum Ventricles Rib Left lung, superior lobe Visceral pleura Left pleural cavity Parietal pleura Bronchi Mediastinum Left lung, inferior lobe 71
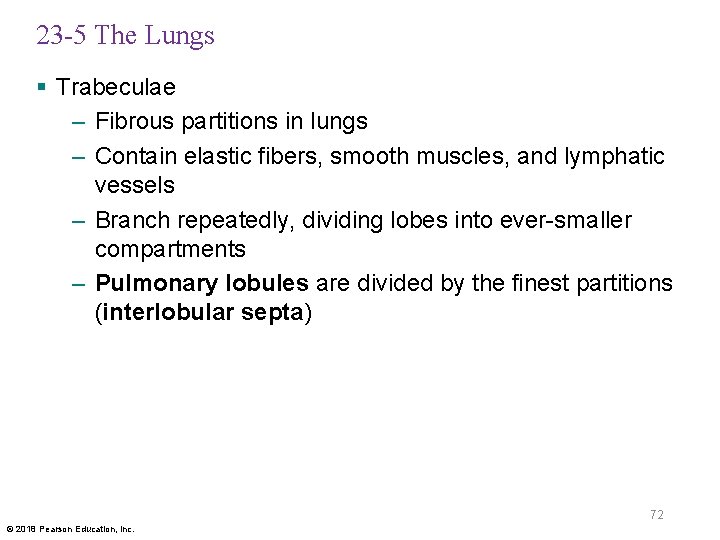
23 -5 The Lungs § Trabeculae – Fibrous partitions in lungs – Contain elastic fibers, smooth muscles, and lymphatic vessels – Branch repeatedly, dividing lobes into ever-smaller compartments – Pulmonary lobules are divided by the finest partitions (interlobular septa) 72 © 2018 Pearson Education, Inc.
23 -5 The Lungs § Blood supply to lungs – Respiratory exchange surfaces receive deoxygenated blood from pulmonary arteries – A capillary network surrounds each alveolus – Oxygen-rich blood from alveolar capillaries is carried through pulmonary veins to left atrium – Capillaries supplied by bronchial arteries provide oxygen and nutrients to conducting passageways 73 © 2018 Pearson Education, Inc.
23 -5 The Lungs § Blood pressure in pulmonary circuit – Lower than that in systemic circuit – Pulmonary vessels are easily blocked by blood clots, fat, or air bubbles – Pulmonary embolism • A blocked branch of pulmonary artery that stops blood flow to lobules or alveoli 74 © 2018 Pearson Education, Inc.
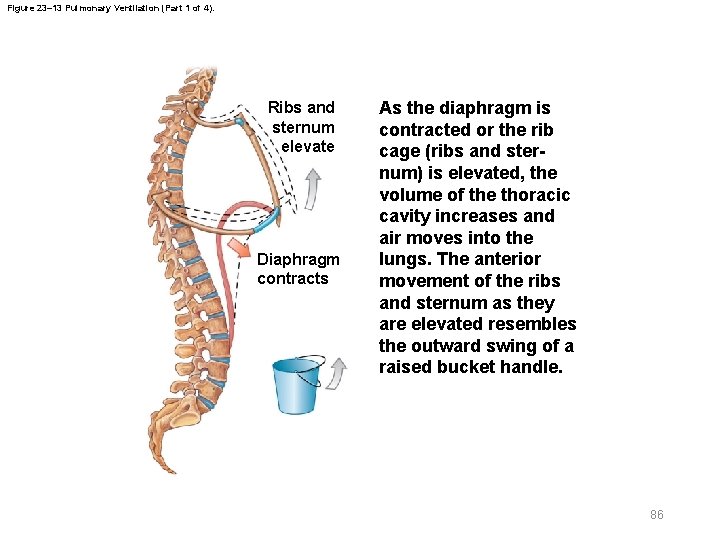
23 -5 The Lungs § Two pleural cavities – Separated by mediastinum – Each pleural cavity contains a lung • Cavity is lined with serous membrane (pleura) § Pleura – Consists of two layers • Parietal pleura (lines inner surface of thoracic wall) • Visceral pleura (covers outer surfaces of lungs) – Pleural fluid • Lubricates space between the two layers 75 © 2018 Pearson Education, Inc.
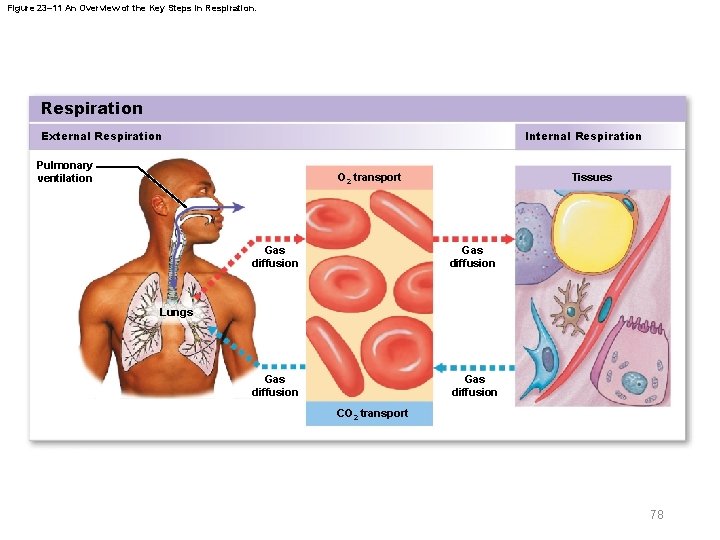
23 -6 External and Internal Respiration § Respiration includes two integrated processes – External respiration • All processes involved in exchange of O 2 and CO 2 with external environment – Internal respiration • Uptake of O 2 and release of CO 2 by cells • Result of cellular respiration 76 © 2018 Pearson Education, Inc.
23 -6 External and Internal Respiration § Integrated steps in external respiration – Pulmonary ventilation (breathing) – Gas diffusion • Across blood air barrier in lungs • Across capillary walls in other tissues – Transport of O 2 and CO 2 • Between alveolar capillaries • Between capillary beds in other tissues 77 © 2018 Pearson Education, Inc.
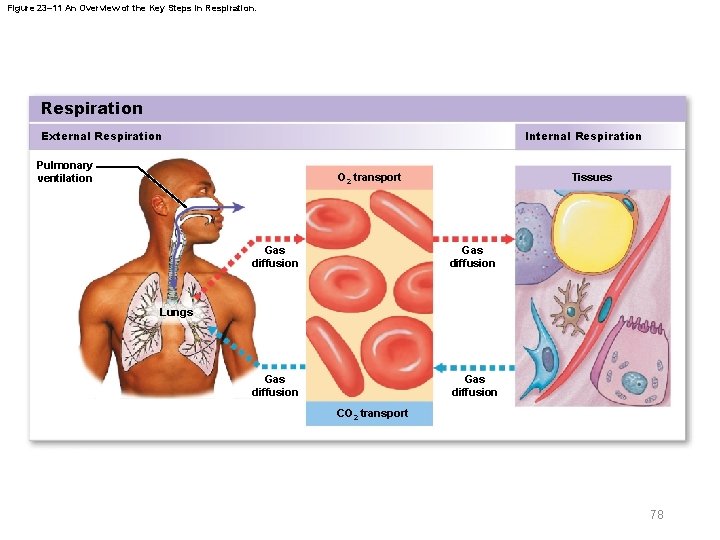
Figure 23– 11 An Overview of the Key Steps in Respiration External Respiration Internal Respiration Pulmonary ventilation Tissues O 2 transport Gas diffusion Lungs CO 2 transport 78
23 -6 External and Internal Respiration § Abnormal external respiration is dangerous – Hypoxia • Low tissue oxygen levels – Anoxia • Complete lack of oxygen in tissues 79 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Pulmonary ventilation (breathing) – Physical movement of air into and out of respiratory tract – Provides alveolar ventilation § Atmospheric pressure (atm) – Weight of Earth’s atmosphere • Has several important physiological effects 80 © 2018 Pearson Education, Inc.
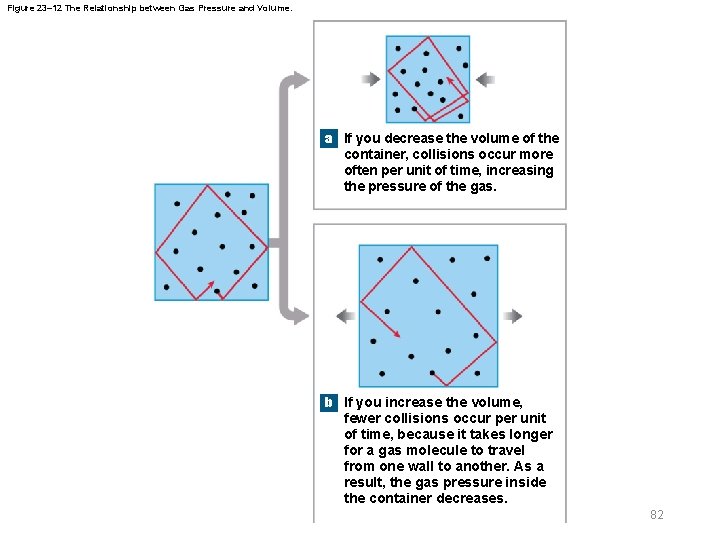
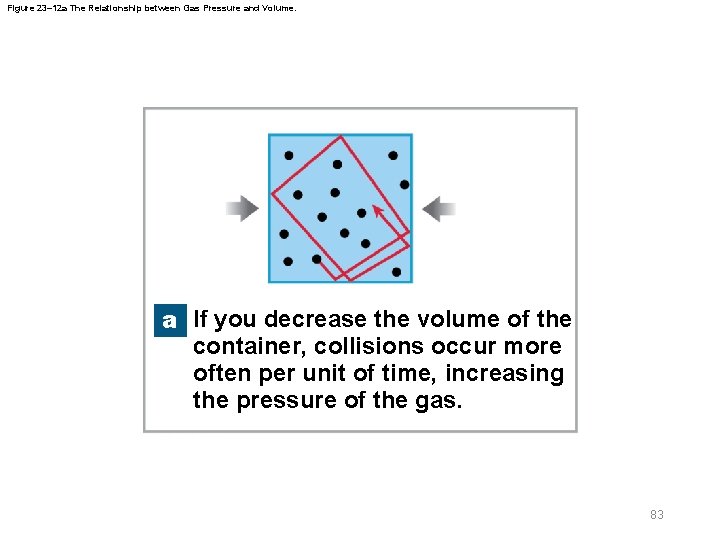
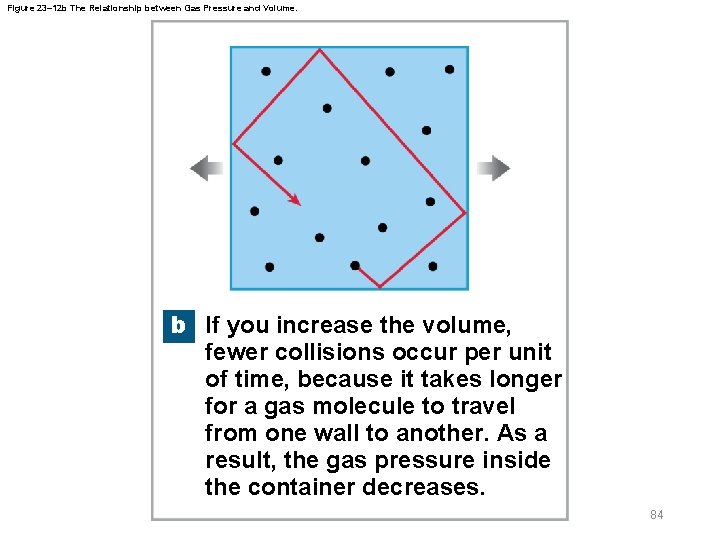
23 -7 Pulmonary Ventilation § Boyle’s law – Defines the relationship between gas pressure and volume P = 1/V – In a contained gas • External pressure forces molecules closer together • Movement of gas molecules exerts pressure on container 81 © 2018 Pearson Education, Inc.
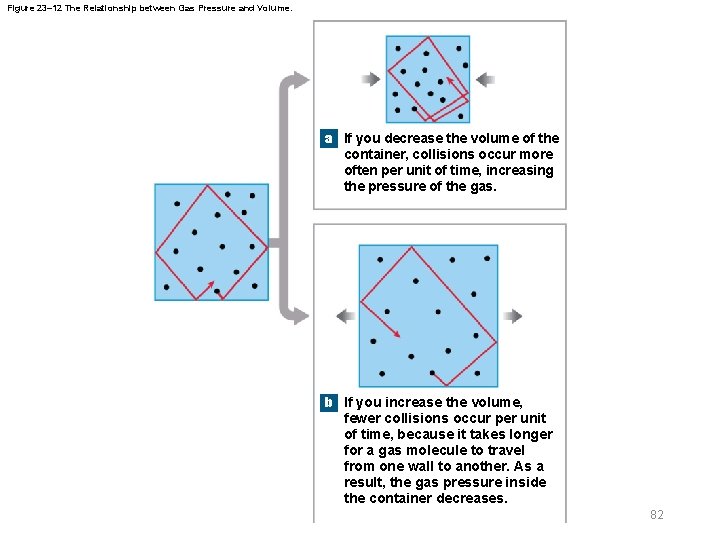
Figure 23– 12 The Relationship between Gas Pressure and Volume. a If you decrease the volume of the container, collisions occur more often per unit of time, increasing the pressure of the gas. b If you increase the volume, fewer collisions occur per unit of time, because it takes longer for a gas molecule to travel from one wall to another. As a result, the gas pressure inside the container decreases. 82
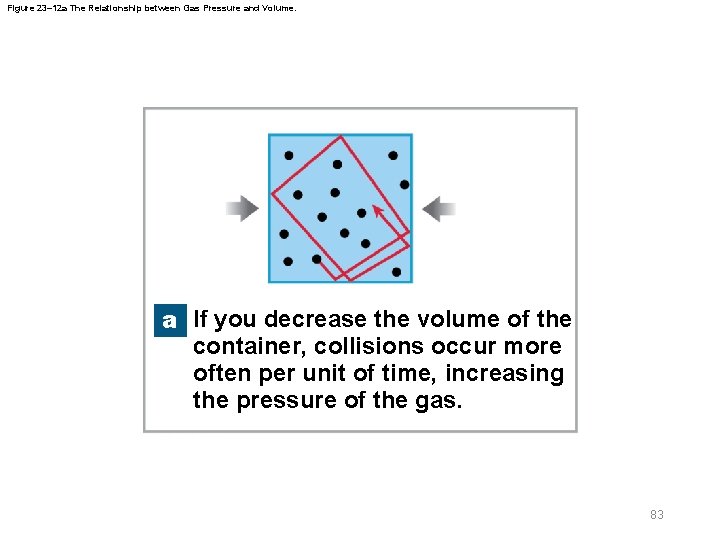
Figure 23– 12 a The Relationship between Gas Pressure and Volume. a If you decrease the volume of the container, collisions occur more often per unit of time, increasing the pressure of the gas. 83
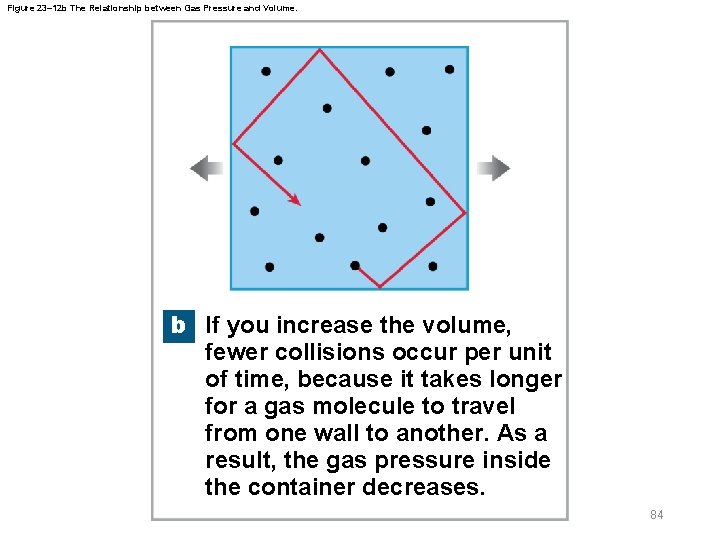
Figure 23– 12 b The Relationship between Gas Pressure and Volume. b If you increase the volume, fewer collisions occur per unit of time, because it takes longer for a gas molecule to travel from one wall to another. As a result, the gas pressure inside the container decreases. 84
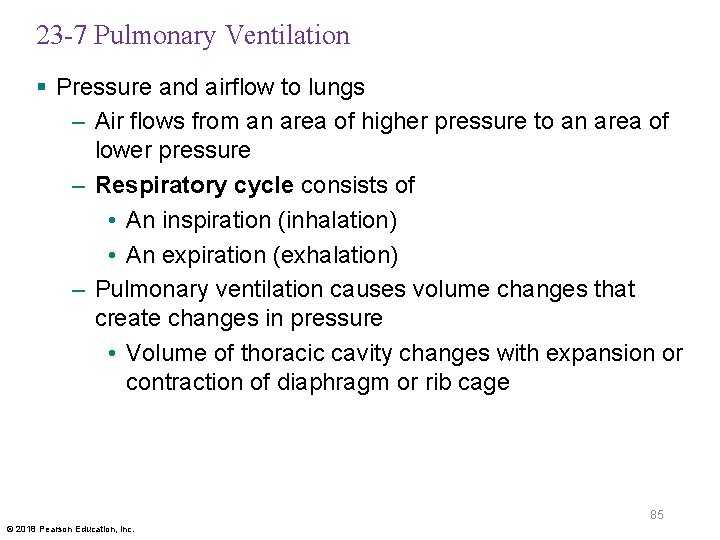
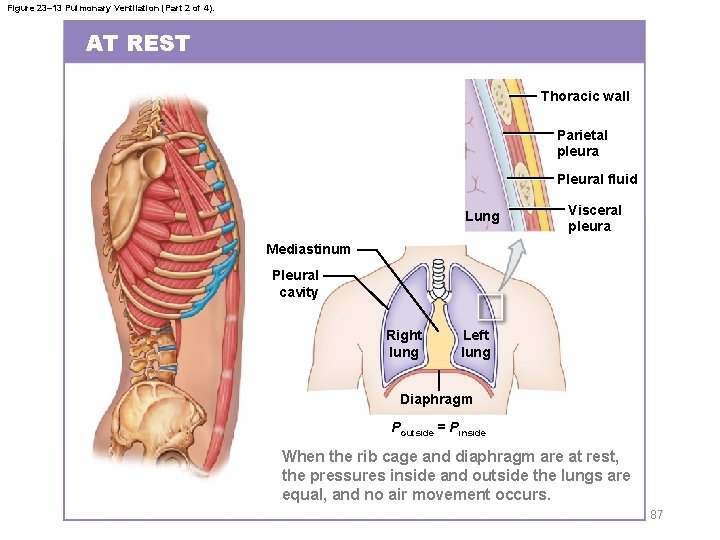
23 -7 Pulmonary Ventilation § Pressure and airflow to lungs – Air flows from an area of higher pressure to an area of lower pressure – Respiratory cycle consists of • An inspiration (inhalation) • An expiration (exhalation) – Pulmonary ventilation causes volume changes that create changes in pressure • Volume of thoracic cavity changes with expansion or contraction of diaphragm or rib cage 85 © 2018 Pearson Education, Inc.
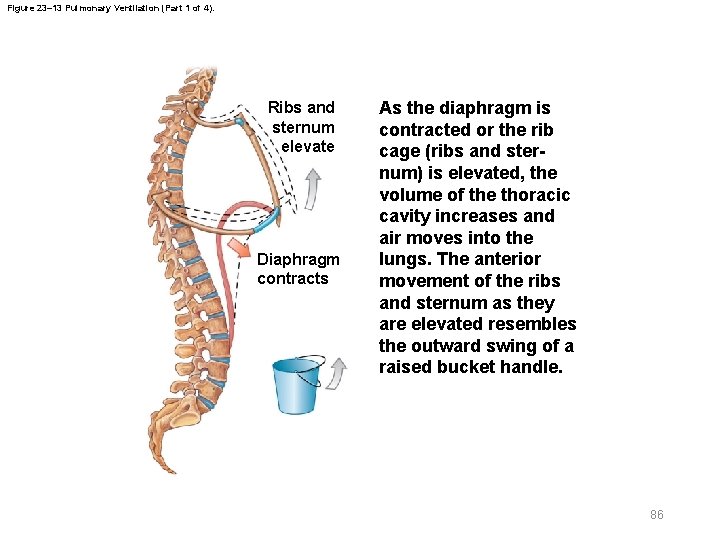
Figure 23– 13 Pulmonary Ventilation (Part 1 of 4). Ribs and sternum elevate Diaphragm contracts As the diaphragm is contracted or the rib cage (ribs and sternum) is elevated, the volume of the thoracic cavity increases and air moves into the lungs. The anterior movement of the ribs and sternum as they are elevated resembles the outward swing of a raised bucket handle. 86
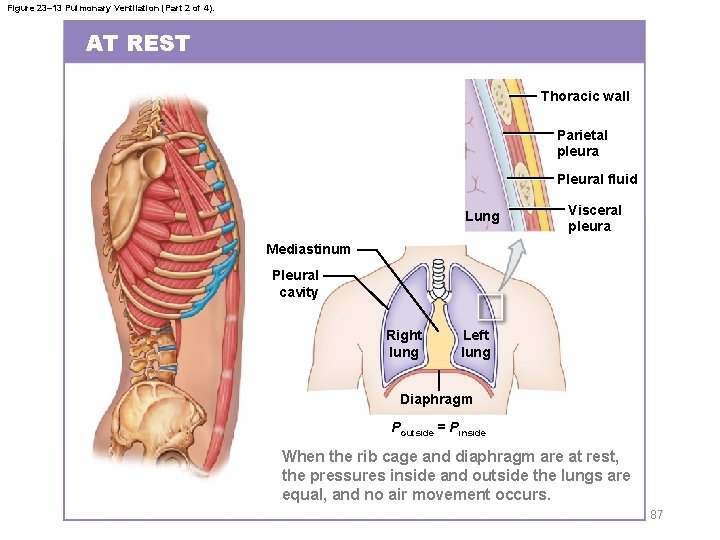
Figure 23– 13 Pulmonary Ventilation (Part 2 of 4). AT REST Thoracic wall Parietal pleura Pleural fluid Lung Visceral pleura Mediastinum Pleural cavity Right lung Left lung Diaphragm Poutside = Pinside When the rib cage and diaphragm are at rest, the pressures inside and outside the lungs are equal, and no air movement occurs. 87
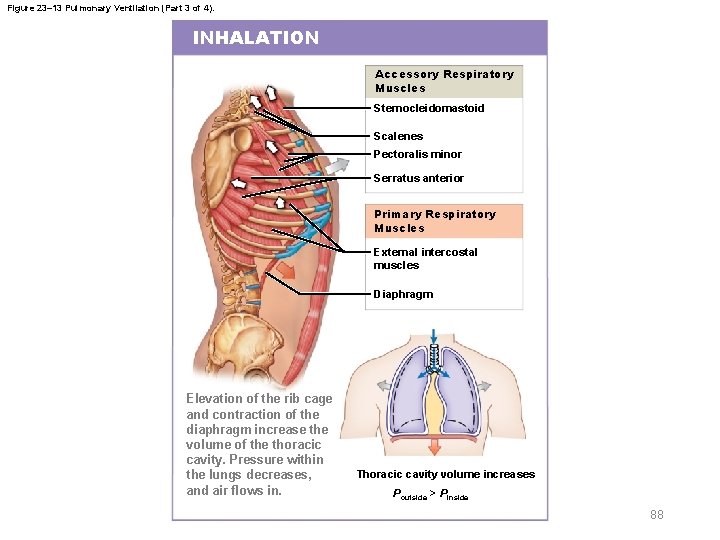
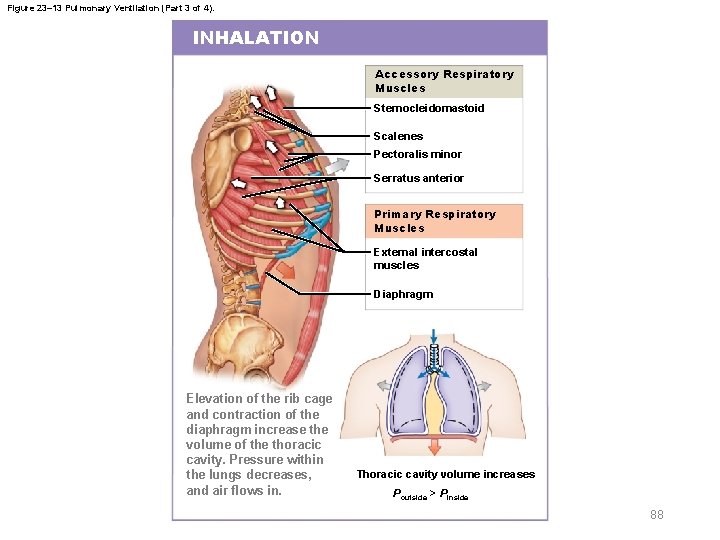
Figure 23– 13 Pulmonary Ventilation (Part 3 of 4). INHALATION Accessory Respiratory Muscles Sternocleidomastoid Scalenes Pectoralis minor Serratus anterior Primary Respiratory Muscles External intercostal muscles Diaphragm Elevation of the rib cage and contraction of the diaphragm increase the volume of the thoracic cavity. Pressure within the lungs decreases, and air flows in. Thoracic cavity volume increases Poutside > Pinside 88
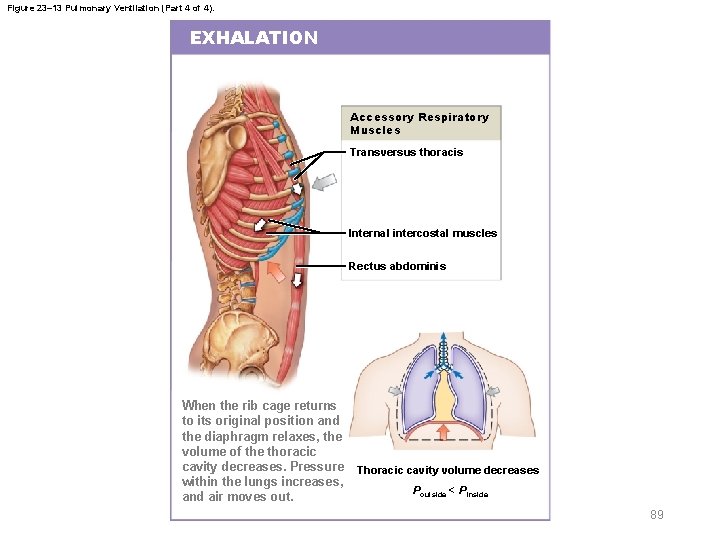
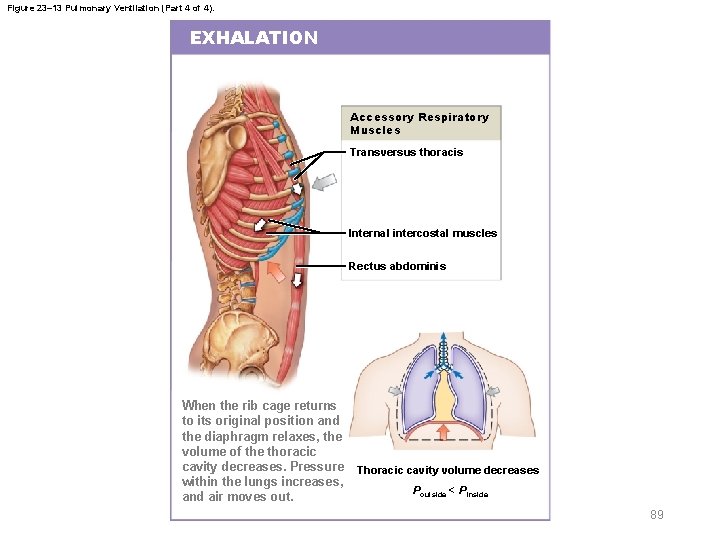
Figure 23– 13 Pulmonary Ventilation (Part 4 of 4). EXHALATION Accessory Respiratory Muscles Transversus thoracis Internal intercostal muscles Rectus abdominis When the rib cage returns to its original position and the diaphragm relaxes, the volume of the thoracic cavity decreases. Pressure within the lungs increases, and air moves out. Thoracic cavity volume decreases Poutside < Pinside 89
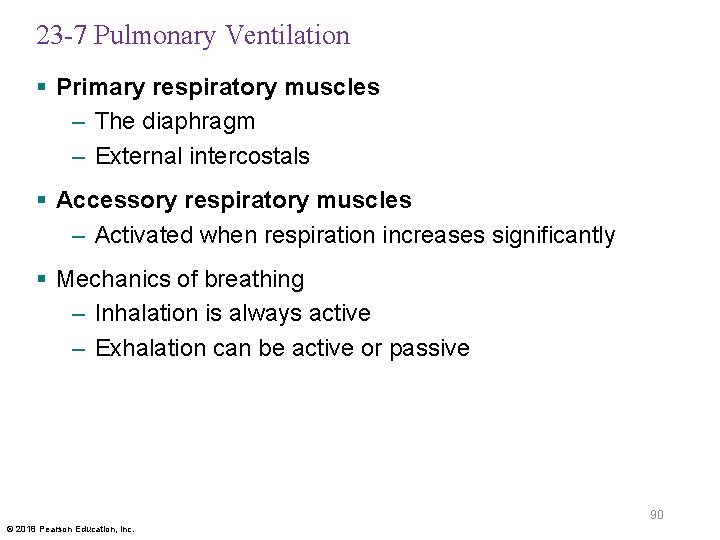
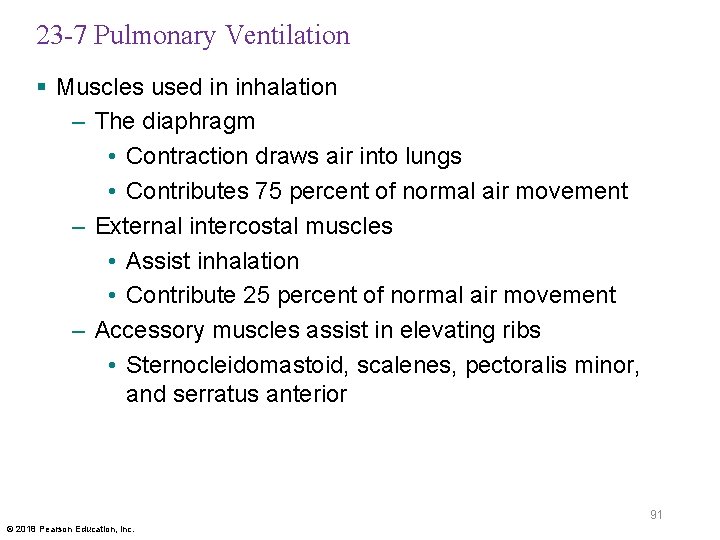
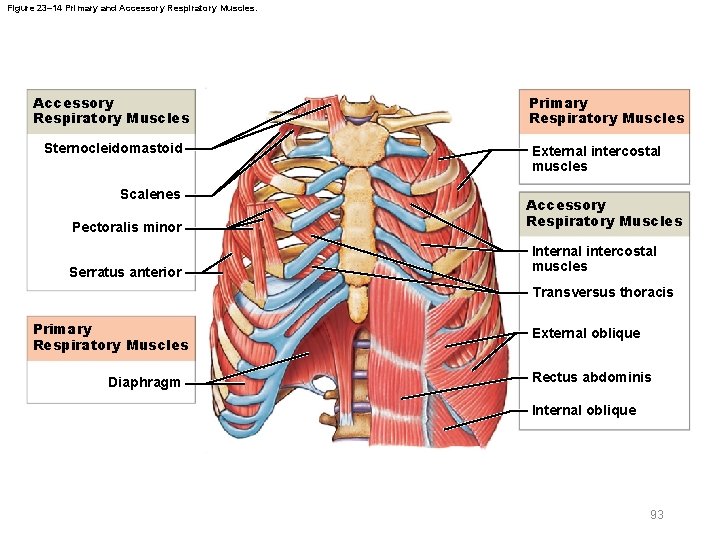
23 -7 Pulmonary Ventilation § Primary respiratory muscles – The diaphragm – External intercostals § Accessory respiratory muscles – Activated when respiration increases significantly § Mechanics of breathing – Inhalation is always active – Exhalation can be active or passive 90 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Muscles used in inhalation – The diaphragm • Contraction draws air into lungs • Contributes 75 percent of normal air movement – External intercostal muscles • Assist inhalation • Contribute 25 percent of normal air movement – Accessory muscles assist in elevating ribs • Sternocleidomastoid, scalenes, pectoralis minor, and serratus anterior 91 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Muscles used in exhalation – Internal intercostal muscle and transversus thoracis • Depress the ribs – Abdominal muscles • Compress abdomen • Force diaphragm upward 92 © 2018 Pearson Education, Inc.
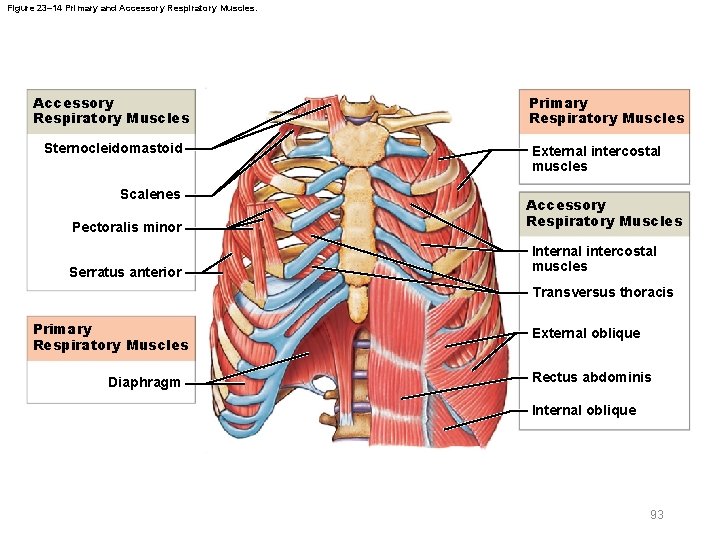
Figure 23– 14 Primary and Accessory Respiratory Muscles Sternocleidomastoid Scalenes Pectoralis minor Serratus anterior Primary Respiratory Muscles External intercostal muscles Accessory Respiratory Muscles Internal intercostal muscles Transversus thoracis Primary Respiratory Muscles Diaphragm External oblique Rectus abdominis Internal oblique 93
23 -7 Pulmonary Ventilation § Respiratory movements are classified by pattern of muscle activity – Quiet breathing – Forced breathing § Forced breathing (hyperpnea) – Involves active inhalation and exhalation – Assisted by accessory muscles 94 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Quiet breathing (eupnea) – Involves active inhalation and passive exhalation – Diaphragmatic breathing or deep breathing • Dominated by diaphragm – Costal breathing or shallow breathing • Dominated by rib cage movements § Elastic rebound – When muscles of inhalation relax • Elastic components of tissues recoil • Diaphragm and rib cage return to original positions 95 © 2018 Pearson Education, Inc.
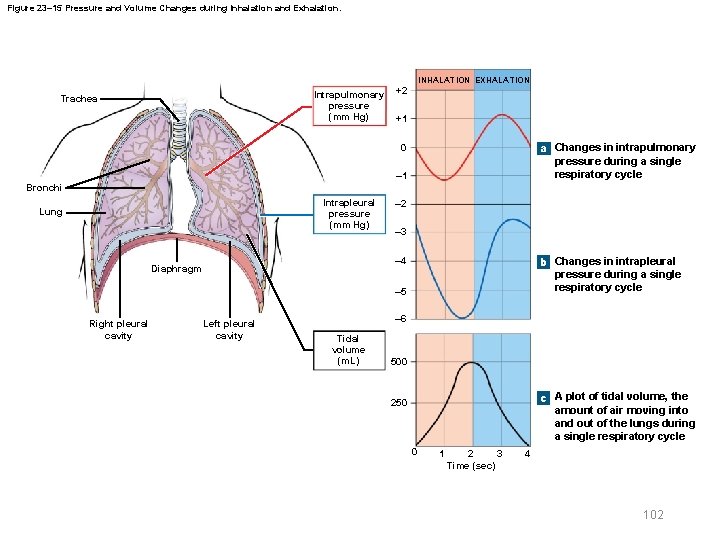
23 -7 Pulmonary Ventilation § Pressure changes during inhalation and exhalation – Can be measured inside or outside lungs – Normal atmospheric pressure • 1 atmosphere (atm) = 760 mm Hg 96 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Intrapulmonary pressure – Also called intra-alveolar pressure – Difference from atmospheric pressure determines direction of airflow – In relaxed breathing, pressure differential is small • – 1 mm Hg on inhalation or +1 mm Hg on exhalation – Breathing at maximum capacity (e. g. , when lifting weights) can increase pressure gradient • From – 30 mm Hg during inhalation to +100 mm Hg while straining with glottis closed 97 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Intrapleural pressure – Pressure in space between parietal and visceral pleurae – Averages – 4 mm Hg • Maximum of – 18 mm Hg during powerful inhalation – Remains below atmospheric pressure throughout respiratory cycle – Cyclical changes in intrapleural pressure create respiratory pump • Assists in venous return to heart 98 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Pneumothorax – Air enters pleural cavity – Due to injury to chest wall or rupture of alveoli – Results in atelectasis (collapsed lung) 99 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Resistance – Adjusted with bronchodilation and bronchoconstriction § Compliance – A measure of expandability – Lower compliance requires greater force to fill lungs – Factors that affect compliance • Connective tissue of lungs • Level of surfactant production • Mobility of thoracic cage 100 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Respiratory rates and volumes – Respiratory system adapts to changing oxygen demands by varying • Number of breaths per minute (respiratory rate) • Amount of air moved per breath (tidal volume, VT) – Respiratory minute volume (VE) • Amount of air moved per minute • Calculated as: respiratory rate × tidal volume • Measures pulmonary ventilation 101 © 2018 Pearson Education, Inc.
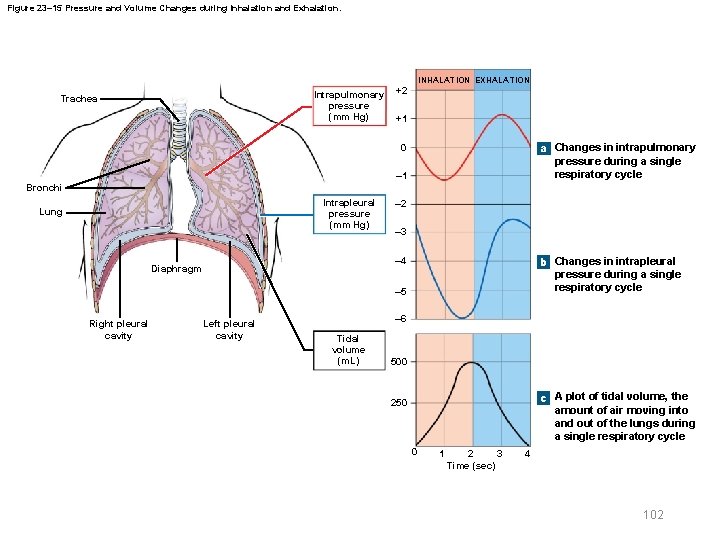
Figure 23– 15 Pressure and Volume Changes during Inhalation and Exhalation. INHALATION EXHALATION Intrapulmonary pressure (mm Hg) Trachea +2 +1 a Changes in intrapulmonary pressure during a single respiratory cycle 0 – 1 Bronchi Intrapleural pressure (mm Hg) Lung – 2 – 3 b Changes in intrapleural pressure during a single respiratory cycle – 4 Diaphragm – 5 Right pleural cavity Left pleural cavity – 6 Tidal volume (m. L) 500 c A plot of tidal volume, the amount of air moving into and out of the lungs during a single respiratory cycle 250 0 1 2 3 Time (sec) 4 102
23 -7 Pulmonary Ventilation § Only some inhaled air reaches alveolar exchange surfaces – Volume of air remaining in conducting passages is anatomic dead space (VD) § Alveolar ventilation – Amount of air reaching alveoli each minute – Calculated as respiratory rate × (tidal volume – anatomic dead space) – Alveoli contain less O 2 than atmospheric air because inhaled air mixes with “used” air 103 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Relationships among VT, and – For a given respiratory rate, • Increasing tidal volume increases alveolar ventilation rate – For a given tidal volume, • Increasing respiratory rate increases alveolar ventilation rate 104 © 2018 Pearson Education, Inc.
23 -7 Pulmonary Ventilation § Respiratory performance and volume relationships – Pulmonary function tests • Measure rates and volumes of air movements – Total lung volume is divided into a series of volumes and capacities • Measured with a spirometer 105 © 2018 Pearson Education, Inc.
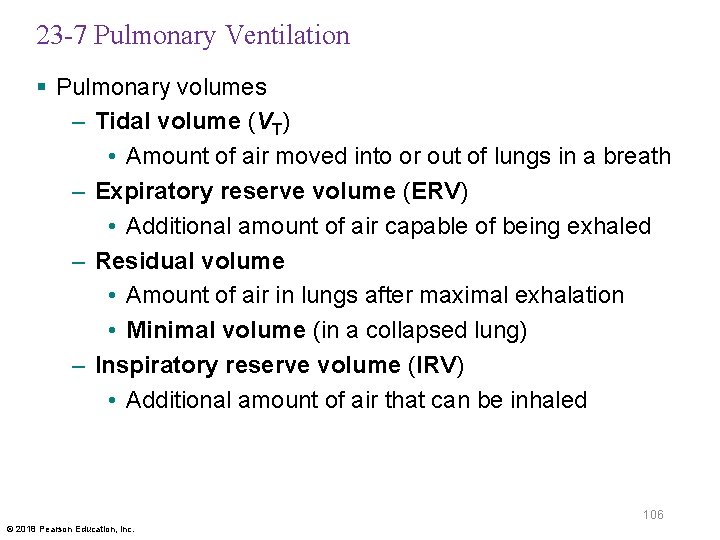
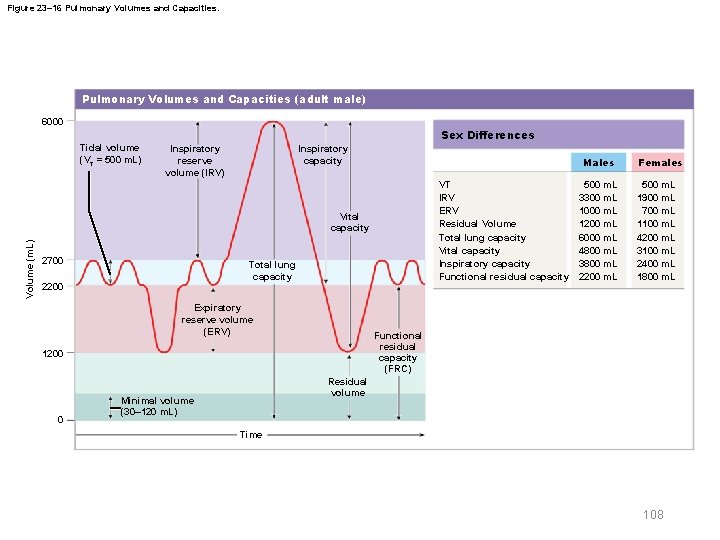
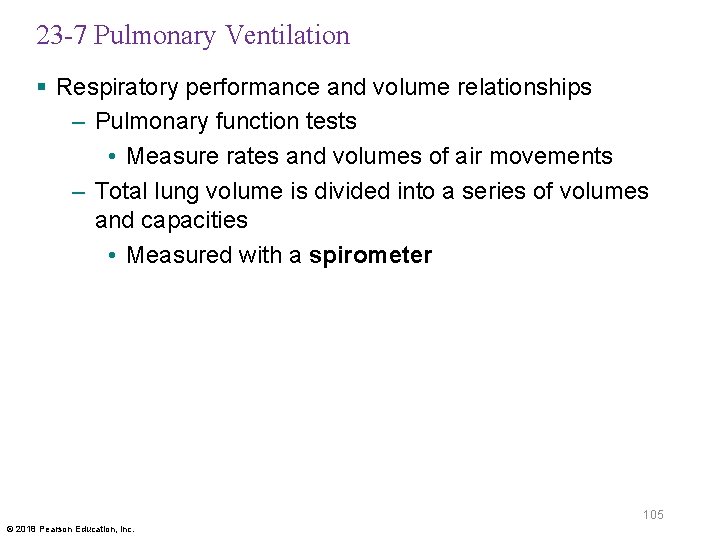
23 -7 Pulmonary Ventilation § Pulmonary volumes – Tidal volume (VT) • Amount of air moved into or out of lungs in a breath – Expiratory reserve volume (ERV) • Additional amount of air capable of being exhaled – Residual volume • Amount of air in lungs after maximal exhalation • Minimal volume (in a collapsed lung) – Inspiratory reserve volume (IRV) • Additional amount of air that can be inhaled 106 © 2018 Pearson Education, Inc.
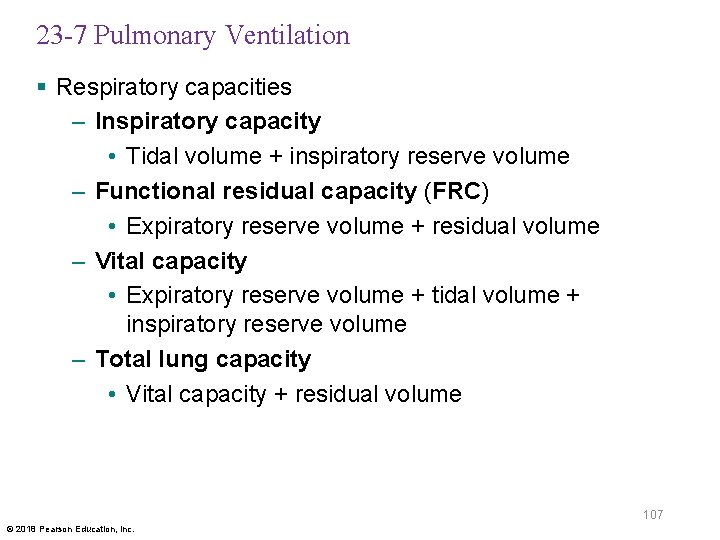
23 -7 Pulmonary Ventilation § Respiratory capacities – Inspiratory capacity • Tidal volume + inspiratory reserve volume – Functional residual capacity (FRC) • Expiratory reserve volume + residual volume – Vital capacity • Expiratory reserve volume + tidal volume + inspiratory reserve volume – Total lung capacity • Vital capacity + residual volume 107 © 2018 Pearson Education, Inc.
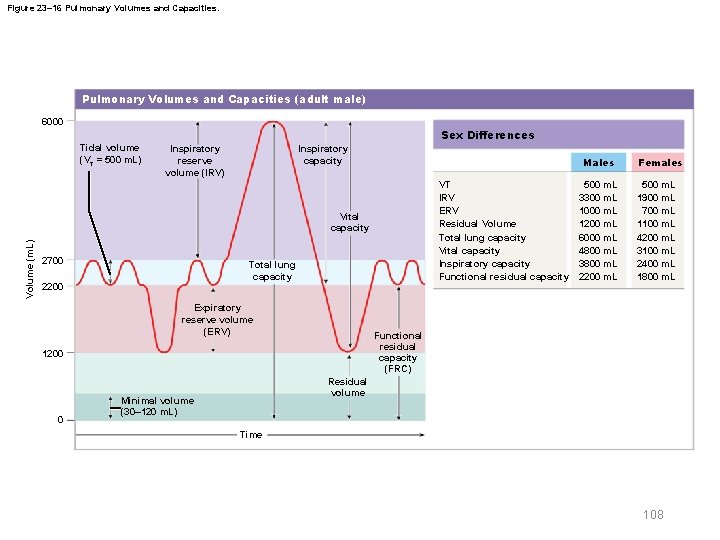
Figure 23– 16 Pulmonary Volumes and Capacities (adult male) 6000 Sex Differences Tidal volume (VT = 500 m. L) Inspiratory capacity Inspiratory reserve volume (IRV) Males VT IRV ERV Residual Volume Total lung capacity Vital capacity Inspiratory capacity Functional residual capacity Volume (m. L) Vital capacity 2700 Total lung capacity 2200 Expiratory reserve volume (ERV) 500 m. L 1900 m. L 700 m. L 1100 m. L 4200 m. L 3100 m. L 2400 m. L 1800 m. L Functional residual capacity (FRC) 1200 0 500 m. L 3300 m. L 1000 m. L 1200 m. L 6000 m. L 4800 m. L 3800 m. L 2200 m. L Females Residual volume Minimal volume (30– 120 m. L) Time 108
23 -8 Gas Exchange § Gas exchange – Occurs between blood and alveolar air – Across blood air barrier § Depends on – Partial pressures of gases involved – Diffusion of molecules between gas and liquid 109 © 2018 Pearson Education, Inc.
23 -8 Gas Exchange § Diffusion of gases – Occurs in response to concentration gradients – Rate of diffusion depends on physical principles, or gas laws • Example: Boyle’s law 110 © 2018 Pearson Education, Inc.
23 -8 Gas Exchange § Dalton’s law – Each gas contributes to total pressure in proportion to its relative abundance § Partial pressure – Pressure contributed by a single gas in a mixture – In atmospheric air (760 mm Hg) • Nitrogen (N 2) is 78. 6 percent (597 mm Hg) • Oxygen (O 2) is 20. 9 percent (159 mm Hg) • Water vapor (H 2 O) is 0. 5 percent (3. 7 mm Hg) • Carbon dioxide (CO 2) is 0. 04 percent (0. 3 mm Hg) 111 © 2018 Pearson Education, Inc.
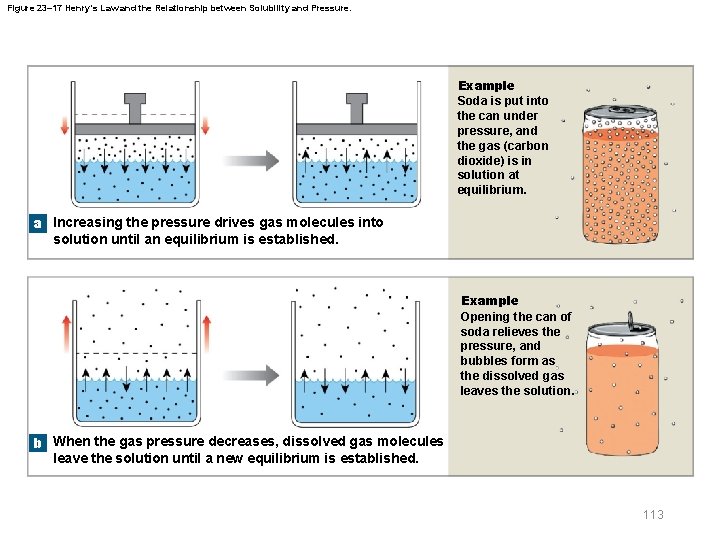
23 -8 Gas Exchange § Diffusion between liquids and gases – Henry’s law • At a given temperature, amount of a gas in solution is proportional to partial pressure of that gas • When gas under pressure contacts a liquid, pressure forces gas molecules into solution • At equilibrium – Gas molecules diffuse out of liquid as quickly as they enter it – Number of gas molecules in solution is constant 112 © 2018 Pearson Education, Inc.
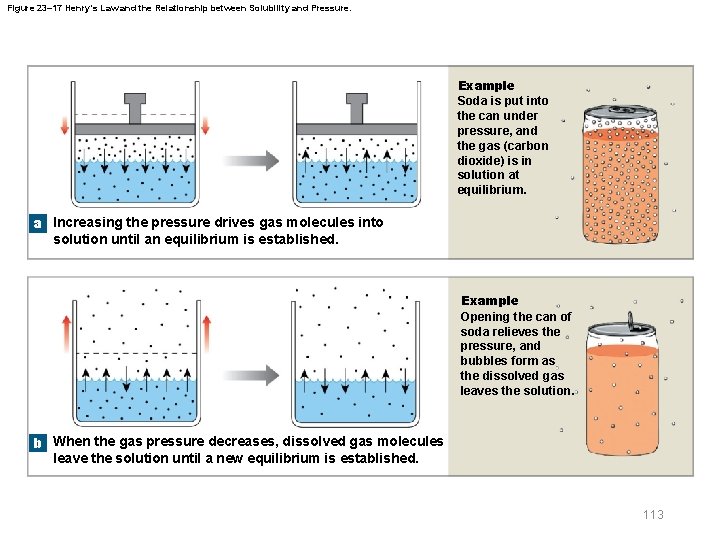
Figure 23– 17 Henry’s Law and the Relationship between Solubility and Pressure. Example Soda is put into the can under pressure, and the gas (carbon dioxide) is in solution at equilibrium. a Increasing the pressure drives gas molecules into solution until an equilibrium is established. Example Opening the can of soda relieves the pressure, and bubbles form as the dissolved gas leaves the solution. b When the gas pressure decreases, dissolved gas molecules leave the solution until a new equilibrium is established. 113
23 -8 Gas Exchange § Solubility of gases in body fluids – CO 2 is highly soluble – O 2 is somewhat less soluble – N 2 has very limited solubility § Partial pressures in plasma of pulmonary vein – PCO 2 = 40 mm Hg – PO 2 = 100 mm Hg – PN 2 = 573 mm Hg 114 © 2018 Pearson Education, Inc.
23 -8 Gas Exchange § Diffusion of gases across blood air barrier – Direction and rate of diffusion are determined by differing partial pressures and solubilities 115 © 2018 Pearson Education, Inc.
23 -8 Gas Exchange § Reasons for efficiency of gas exchange – Differences in partial pressure across blood air barrier are substantial – Distances involved in gas exchange are short – O 2 and CO 2 are lipid soluble – Total surface area is large – Blood flow and airflow are coordinated 116 © 2018 Pearson Education, Inc.
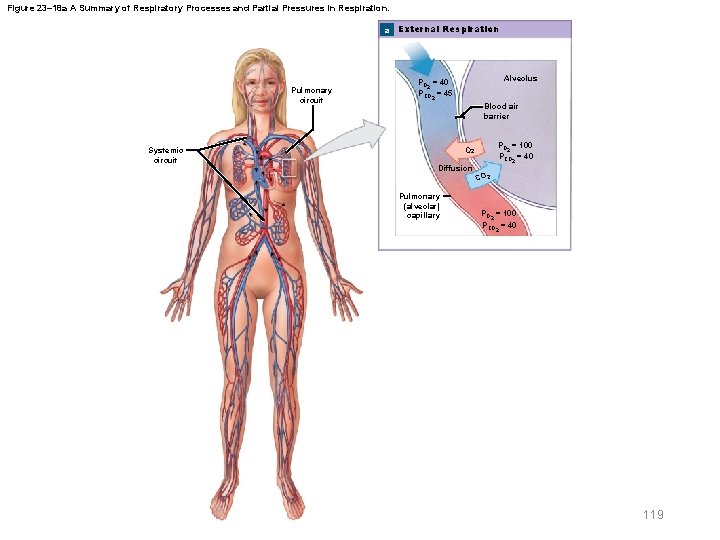
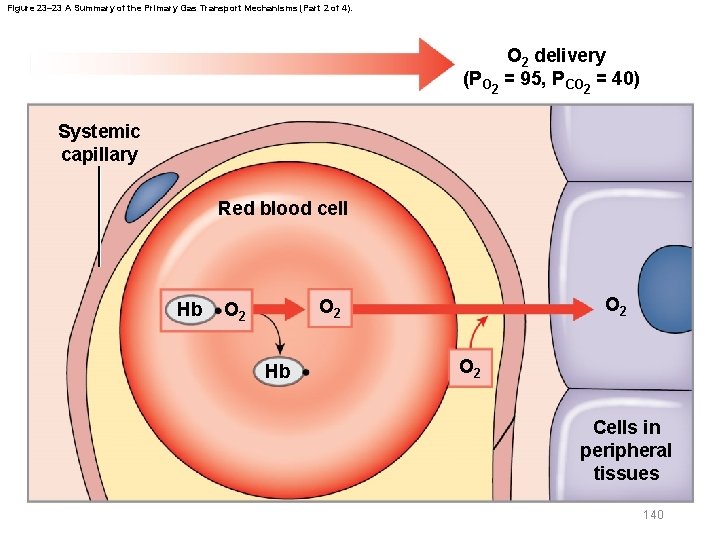
23 -8 Gas Exchange § External respiration – Blood arriving in pulmonary arteries has • Low PO 2 • High PCO 2 – Concentration gradient causes • O 2 to enter blood • CO 2 to leave blood – Rapid exchange allows blood and alveolar air to reach equilibrium 117 © 2018 Pearson Education, Inc.
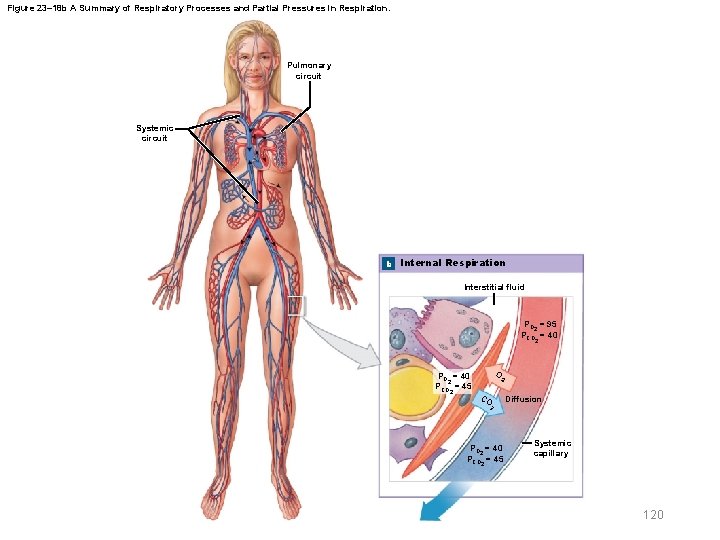
23 -8 Gas Exchange § Internal respiration – Oxygenated blood mixes with deoxygenated blood from conducting passageways – Lowers PO 2 of blood entering systemic circuit to about 95 mm Hg – Interstitial fluid • PO 2 40 mm Hg, PCO 2 45 mm Hg – Concentration gradient in peripheral capillaries is opposite of lungs • CO 2 diffuses into blood, O 2 diffuses out of blood 118 © 2018 Pearson Education, Inc.
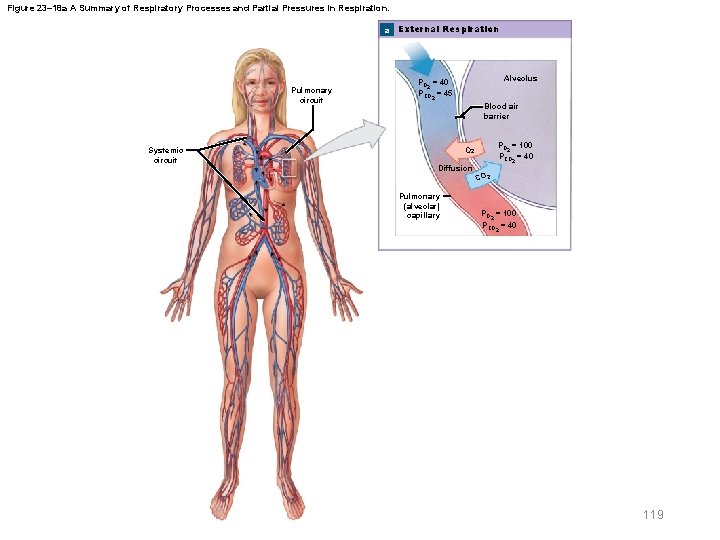
Figure 23– 18 a A Summary of Respiratory Processes and Partial Pressures in Respiration. a External Respiration Pulmonary circuit Systemic circuit Alveolus PO = 40 2 PCO = 45 2 Blood air barrier PO = 100 2 PCO = 40 O 2 Diffusion Pulmonary (alveolar) capillary 2 CO 2 PO = 100 2 PCO = 40 2 119
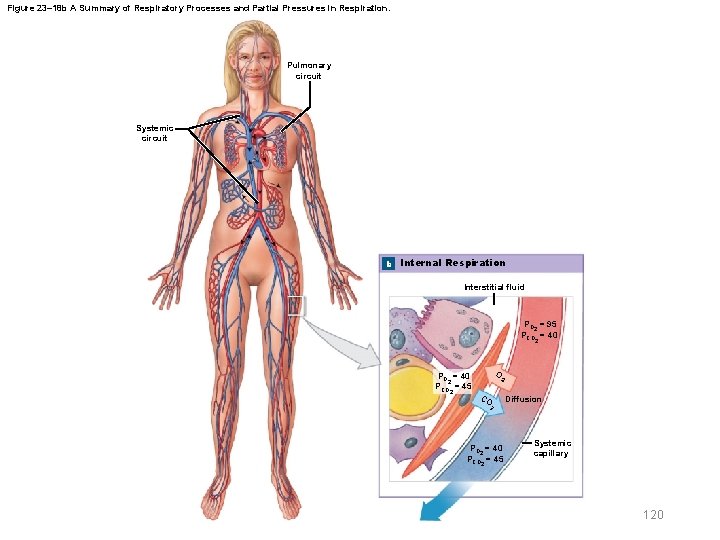
Figure 23– 18 b A Summary of Respiratory Processes and Partial Pressures in Respiration. Pulmonary circuit Systemic circuit b Internal Respiration Interstitial fluid PO 2 = 95 PCO 2 = 40 PCO 2 = 45 O 2 CO 2 PO 2 = 40 PCO 2 = 45 Diffusion Systemic capillary 120
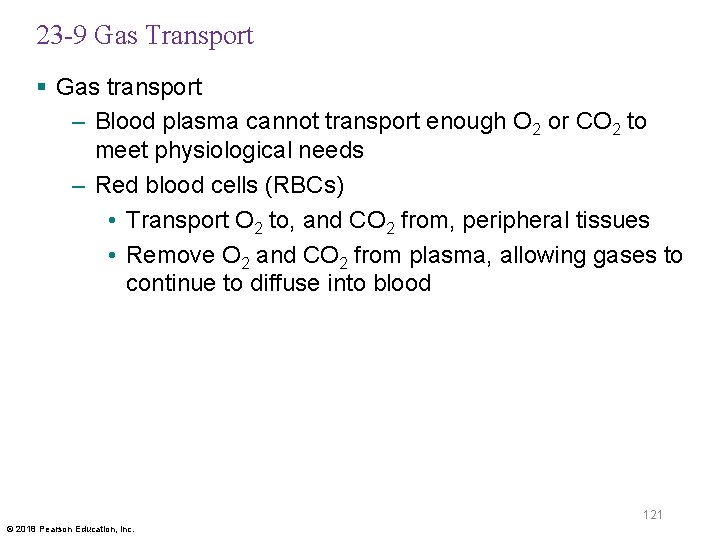
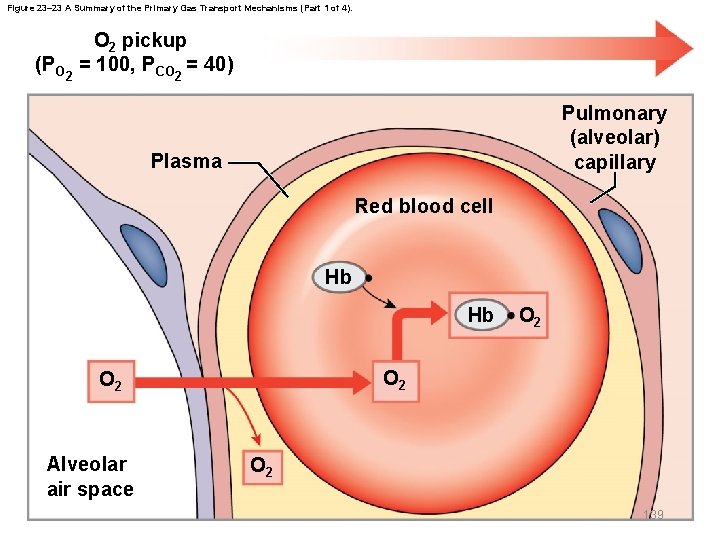
23 -9 Gas Transport § Gas transport – Blood plasma cannot transport enough O 2 or CO 2 to meet physiological needs – Red blood cells (RBCs) • Transport O 2 to, and CO 2 from, peripheral tissues • Remove O 2 and CO 2 from plasma, allowing gases to continue to diffuse into blood 121 © 2018 Pearson Education, Inc.
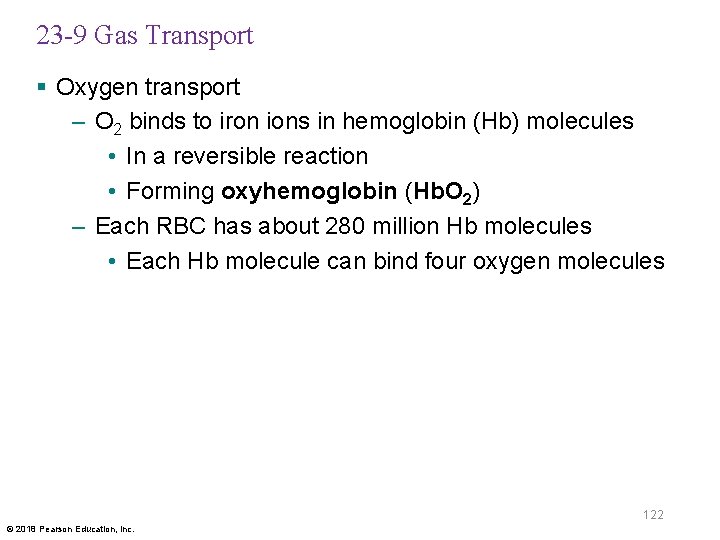
23 -9 Gas Transport § Oxygen transport – O 2 binds to iron ions in hemoglobin (Hb) molecules • In a reversible reaction • Forming oxyhemoglobin (Hb. O 2) – Each RBC has about 280 million Hb molecules • Each Hb molecule can bind four oxygen molecules 122 © 2018 Pearson Education, Inc.
23 -9 Gas Transport § Hemoglobin saturation – Percentage of heme units containing bound oxygen at any given moment § Factors affecting Hb saturation – PO 2 of blood – Blood p. H – Temperature – Metabolic activity within RBCs 123 © 2018 Pearson Education, Inc.
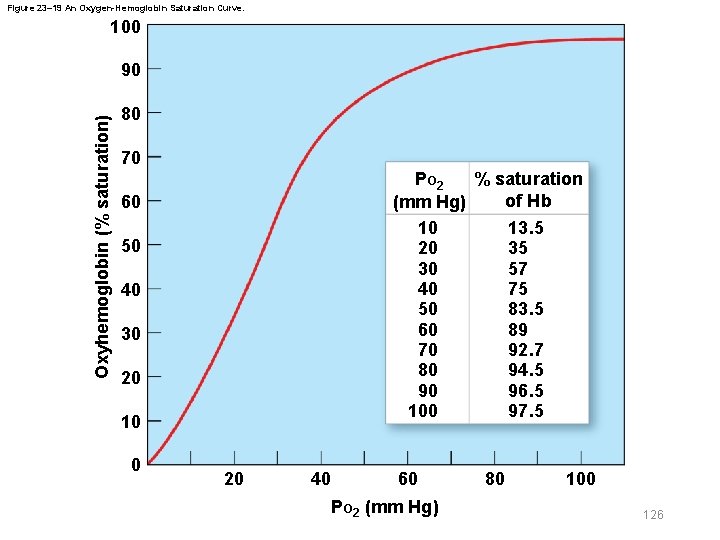
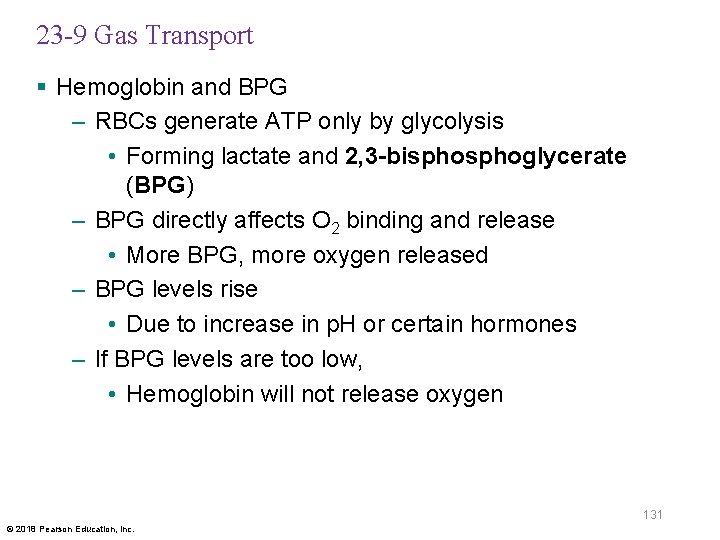
23 -9 Gas Transport § Oxygen–hemoglobin saturation curve – A graph relating hemoglobin saturation to partial pressure of oxygen • Higher PO 2 results in greater Hb saturation – Curve rather than a straight line because Hb changes shape each time a molecule of O 2 binds • Each O 2 bound makes next O 2 bind more easily 124 © 2018 Pearson Education, Inc.
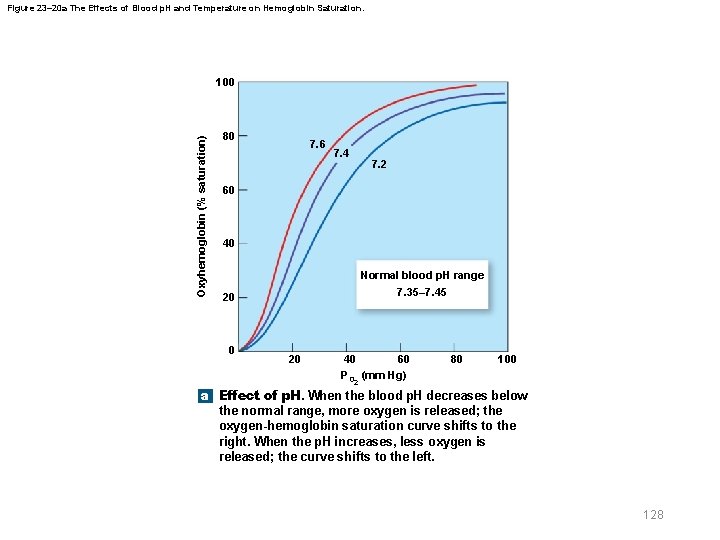
23 -9 Gas Transport § Oxygen–hemoglobin saturation curve – Standardized for normal conditions (p. H 7. 4, 37ºC) – When p. H drops or temperature rises • More oxygen is released • Curve shifts to right – When p. H rises or temperature drops • Less oxygen is released • Curve shifts to left 125 © 2018 Pearson Education, Inc.
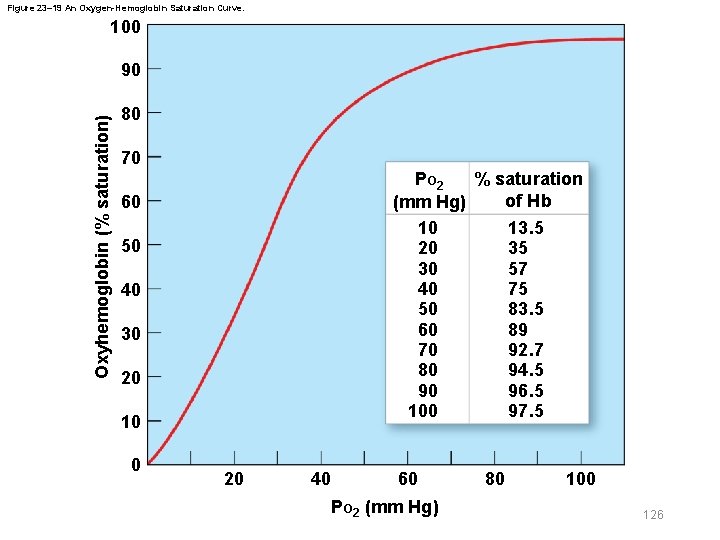
Figure 23– 19 An Oxygen-Hemoglobin Saturation Curve. 100 Oxyhemoglobin (% saturation) 90 80 70 % saturation PO 2 of Hb (mm Hg) 10 13. 5 20 35 30 57 40 75 50 83. 5 60 89 70 92. 7 80 94. 5 90 96. 5 100 97. 5 60 50 40 30 20 10 0 20 40 60 PO 2 (mm Hg) 80 100 126
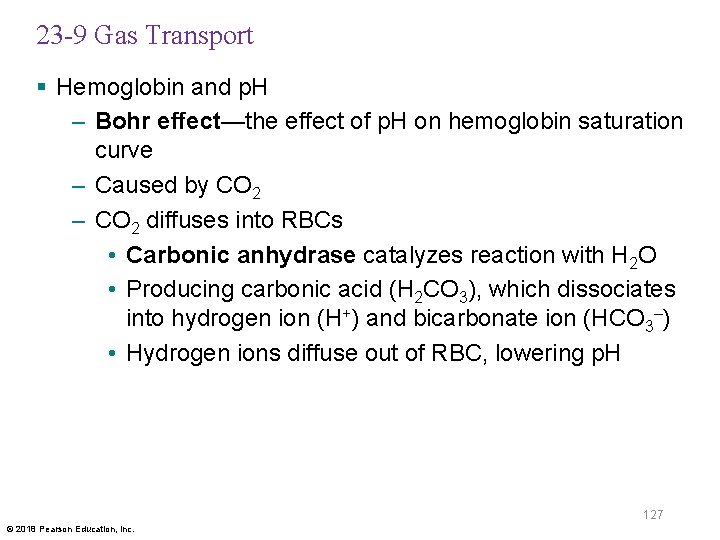
23 -9 Gas Transport § Hemoglobin and p. H – Bohr effect—the effect of p. H on hemoglobin saturation curve – Caused by CO 2 – CO 2 diffuses into RBCs • Carbonic anhydrase catalyzes reaction with H 2 O • Producing carbonic acid (H 2 CO 3), which dissociates into hydrogen ion (H+) and bicarbonate ion (HCO 3–) • Hydrogen ions diffuse out of RBC, lowering p. H 127 © 2018 Pearson Education, Inc.
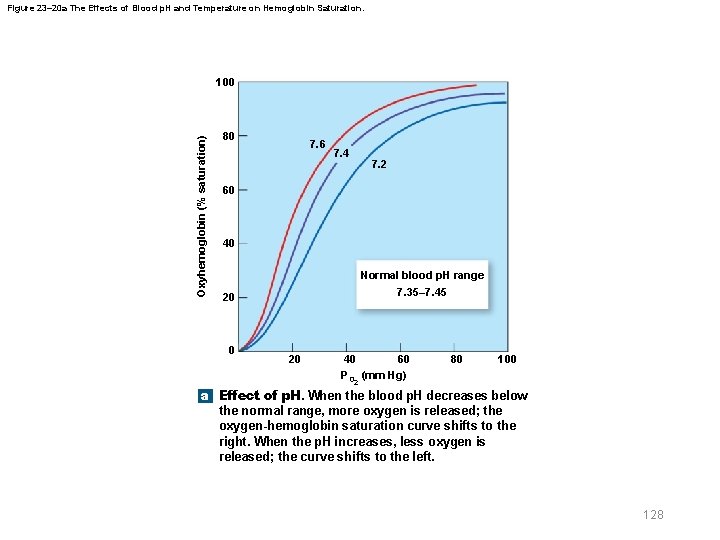
Figure 23– 20 a The Effects of Blood p. H and Temperature on Hemoglobin Saturation. Oxyhemoglobin (% saturation) 100 80 7. 6 7. 4 7. 2 60 40 Normal blood p. H range 7. 35– 7. 45 20 0 20 40 60 PO 2 (mm Hg) 80 100 a Effect of p. H. When the blood p. H decreases below the normal range, more oxygen is released; the oxygen-hemoglobin saturation curve shifts to the right. When the p. H increases, less oxygen is released; the curve shifts to the left. 128
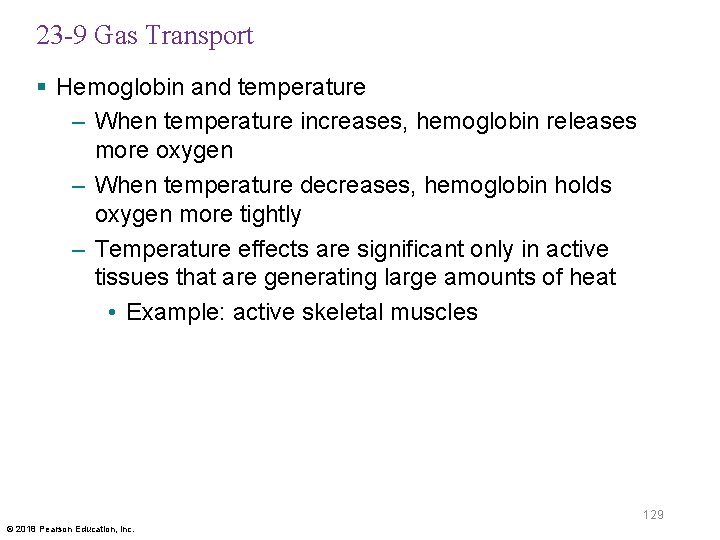
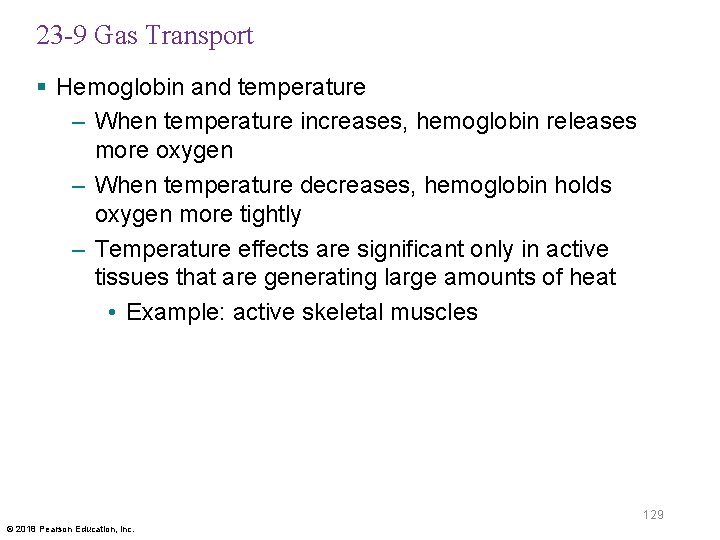
23 -9 Gas Transport § Hemoglobin and temperature – When temperature increases, hemoglobin releases more oxygen – When temperature decreases, hemoglobin holds oxygen more tightly – Temperature effects are significant only in active tissues that are generating large amounts of heat • Example: active skeletal muscles 129 © 2018 Pearson Education, Inc.
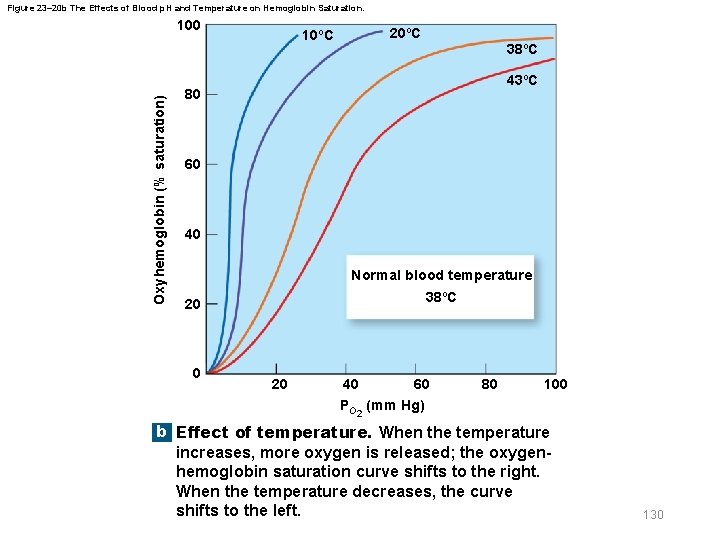
Figure 23– 20 b The Effects of Blood p. H and Temperature on Hemoglobin Saturation. Oxyhemoglobin (% saturation) 100 10ºC 20ºC 38ºC 43ºC 80 60 40 Normal blood temperature 38ºC 20 0 20 40 60 PO 2 (mm Hg) 80 100 b Effect of temperature. When the temperature increases, more oxygen is released; the oxygenhemoglobin saturation curve shifts to the right. When the temperature decreases, the curve shifts to the left. 130
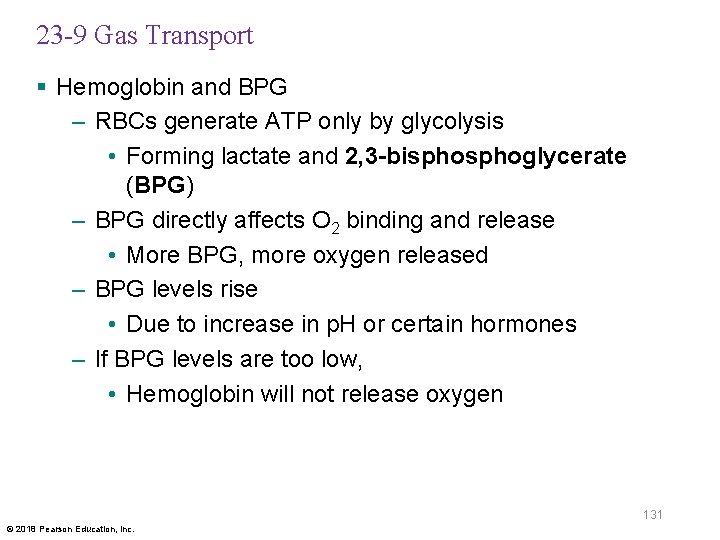
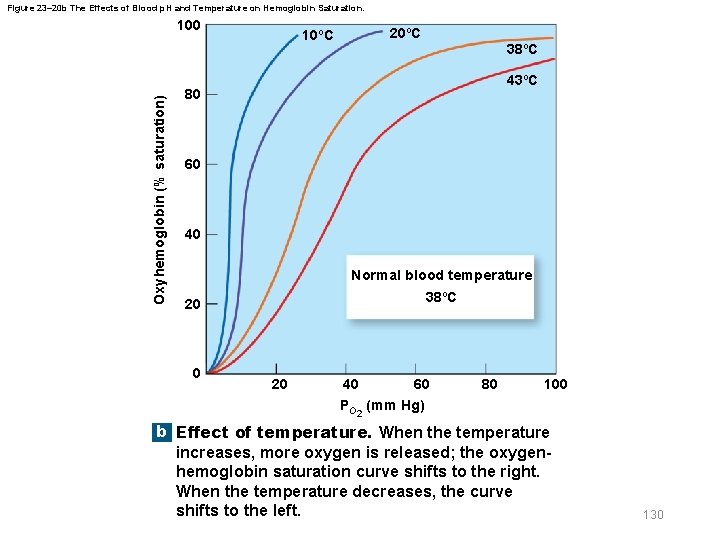
23 -9 Gas Transport § Hemoglobin and BPG – RBCs generate ATP only by glycolysis • Forming lactate and 2, 3 -bisphoglycerate (BPG) – BPG directly affects O 2 binding and release • More BPG, more oxygen released – BPG levels rise • Due to increase in p. H or certain hormones – If BPG levels are too low, • Hemoglobin will not release oxygen 131 © 2018 Pearson Education, Inc.
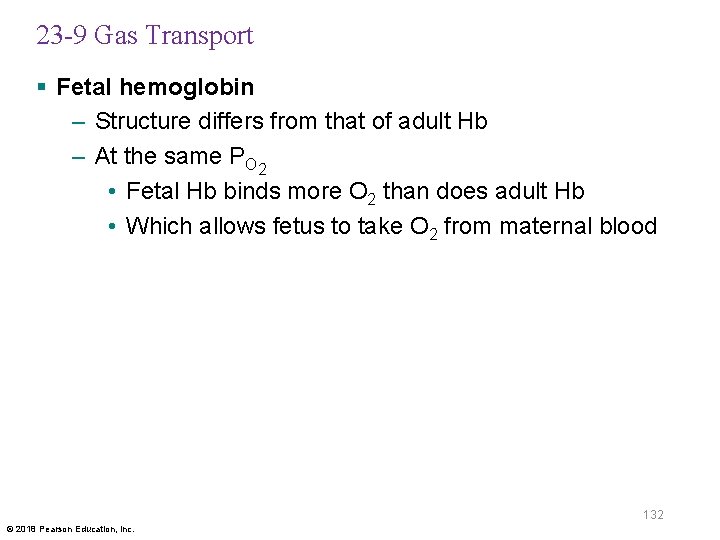
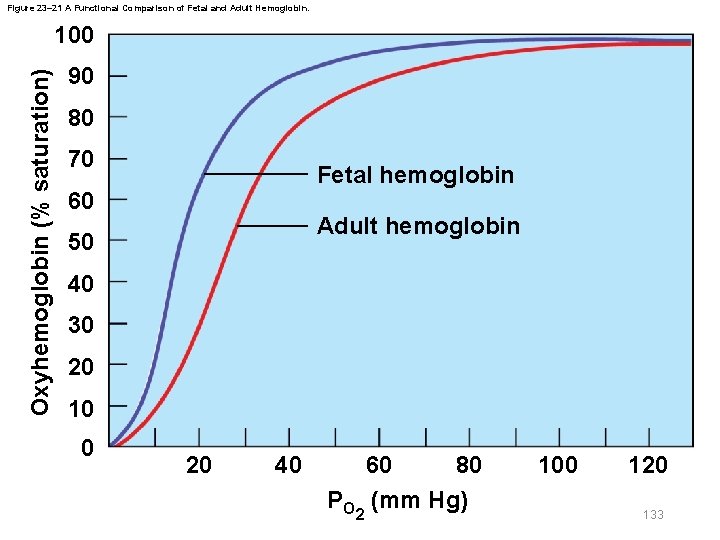
23 -9 Gas Transport § Fetal hemoglobin – Structure differs from that of adult Hb – At the same PO 2 • Fetal Hb binds more O 2 than does adult Hb • Which allows fetus to take O 2 from maternal blood 132 © 2018 Pearson Education, Inc.
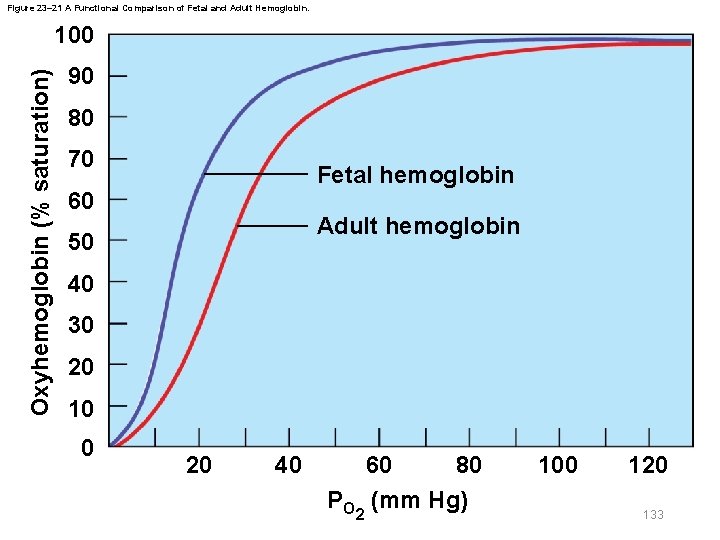
Figure 23– 21 A Functional Comparison of Fetal and Adult Hemoglobin. Oxyhemoglobin (% saturation) 100 90 80 70 Fetal hemoglobin 60 Adult hemoglobin 50 40 30 20 10 0 20 40 60 80 PO 2 (mm Hg) 100 120 133
23 -9 Gas Transport § Carbon monoxide (CO) – From petroleum-burning engines – Binds strongly to hemoglobin – Takes the place of O 2 – Can result in carbon monoxide poisoning 134 © 2018 Pearson Education, Inc.
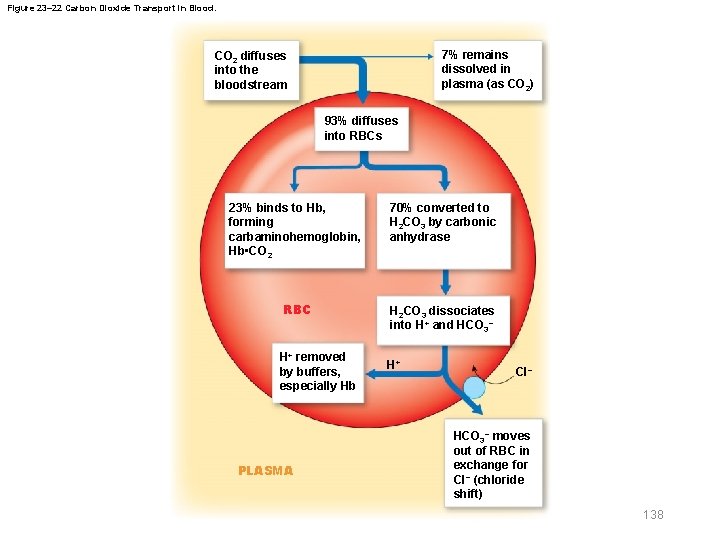
23 -9 Gas Transport § Carbon dioxide transport – CO 2 is generated by aerobic metabolism – CO 2 in bloodstream can be carried three ways • Converted to carbonic acid • Bound to hemoglobin within red blood cells • Dissolved in plasma 135 © 2018 Pearson Education, Inc.

23 -9 Gas Transport § 70 percent of CO 2 is transported as bicarbonate ions (HCO 3–) – Most CO 2 entering bloodstream diffuses into RBCs • CO 2 is converted to carbonic acid (H 2 CO 3) • Dissociates into H+ and bicarbonate (HCO 3–) – Hydrogen ions bind to hemoglobin in RBCs – Bicarbonate ions move into plasma • In exchange for Cl– ions (chloride shift) 136 © 2018 Pearson Education, Inc.
23 -9 Gas Transport § Transport of CO 2 – 23 percent is bound to protein portions of Hb molecules in RBCs • Forming carbaminohemoglobin – 7 percent of CO 2 is transported as dissolved gas molecules in plasma 137 © 2018 Pearson Education, Inc.
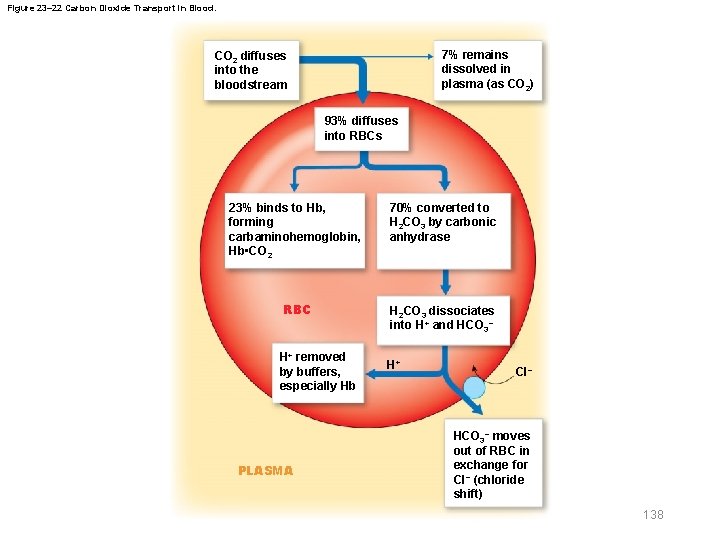
Figure 23– 22 Carbon Dioxide Transport in Blood. 7% remains dissolved in plasma (as CO 2) CO 2 diffuses into the bloodstream 93% diffuses into RBCs 23% binds to Hb, forming carbaminohemoglobin, Hb • CO 2 70% converted to H 2 CO 3 by carbonic anhydrase RBC H 2 CO 3 dissociates into H+ and HCO 3− H+ removed by buffers, especially Hb PLASMA H+ Cl− HCO 3− moves out of RBC in exchange for CI− (chloride shift) 138
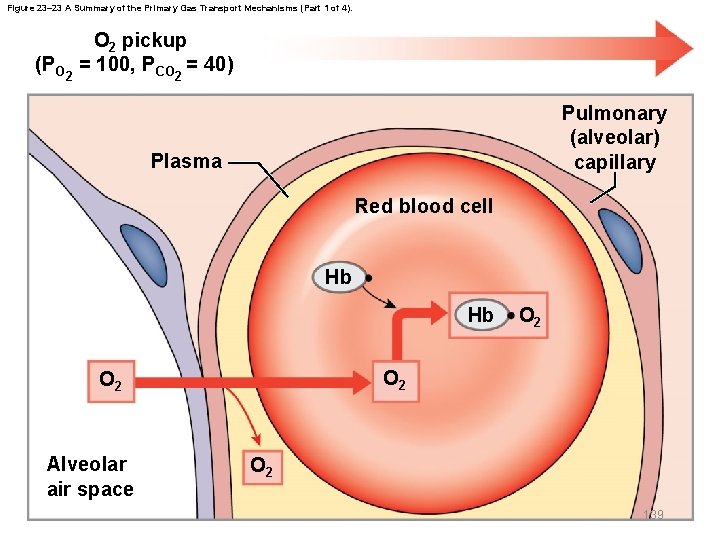
Figure 23– 23 A Summary of the Primary Gas Transport Mechanisms (Part 1 of 4). (PO 2 pickup = 100, PCO = 40) 2 Pulmonary (alveolar) capillary Plasma Red blood cell Hb Hb O 2 Alveolar air space O 2 139
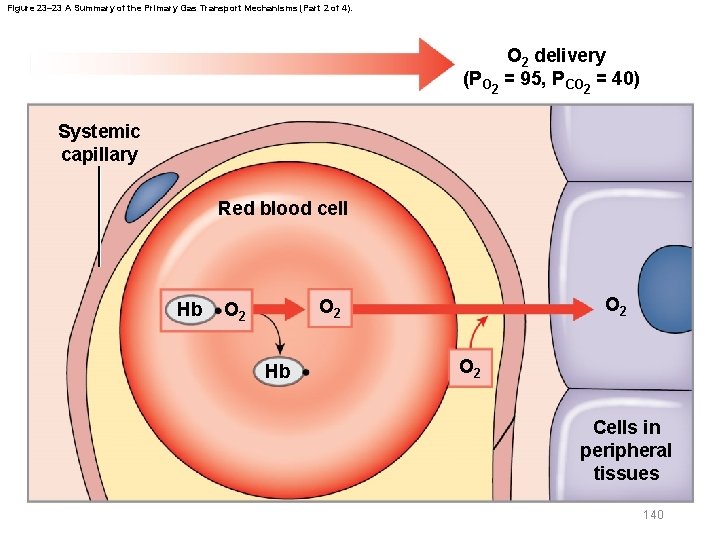
Figure 23– 23 A Summary of the Primary Gas Transport Mechanisms (Part 2 of 4). O 2 delivery (PO 2 = 95, PCO 2 = 40) Systemic capillary Red blood cell Hb O 2 O 2 Hb O 2 Cells in peripheral tissues 140
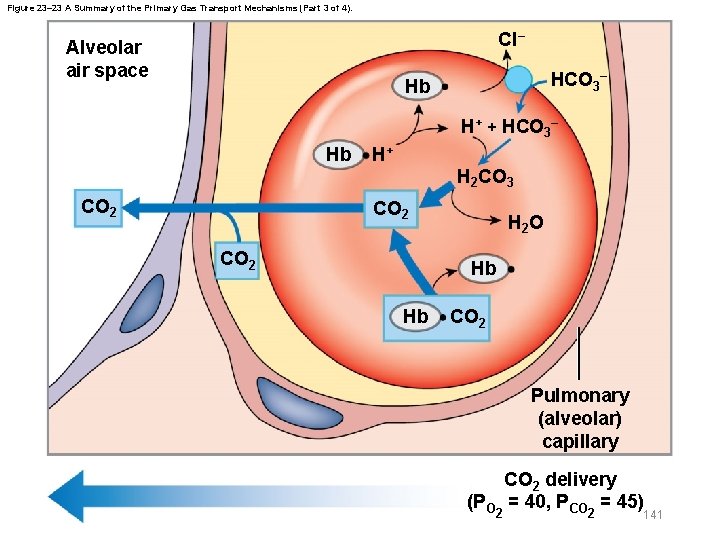
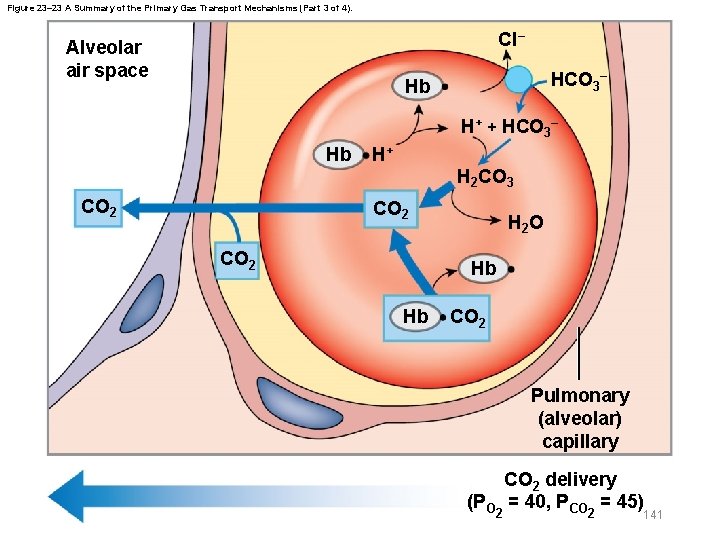
Figure 23– 23 A Summary of the Primary Gas Transport Mechanisms (Part 3 of 4). Cl– Alveolar air space HCO 3– Hb H+ + HCO 3– Hb H+ H 2 CO 3 CO 2 H 2 O Hb Hb CO 2 Pulmonary (alveolar) capillary CO 2 delivery (PO = 40, PCO = 45) 2 2 141
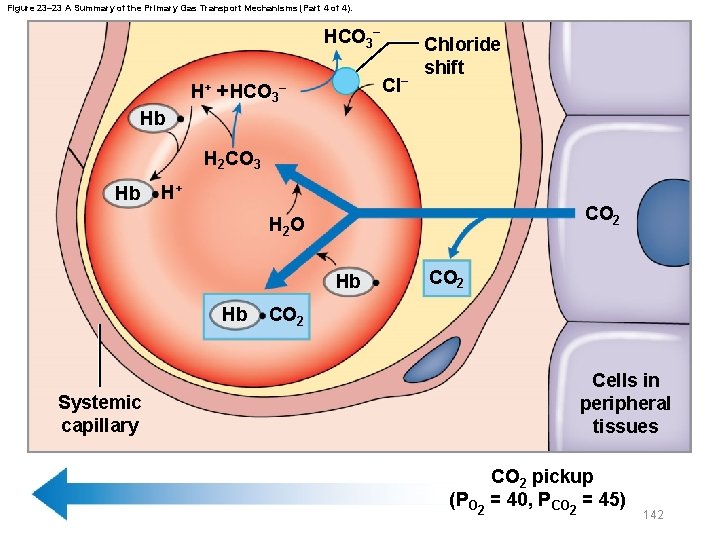
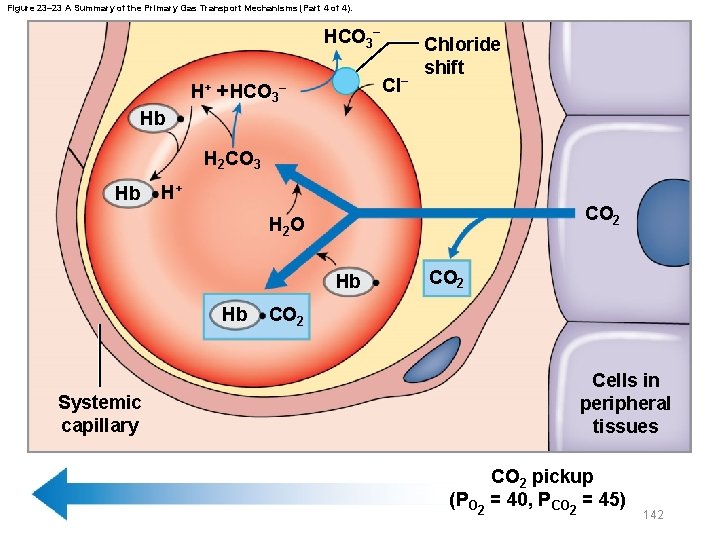
Figure 23– 23 A Summary of the Primary Gas Transport Mechanisms (Part 4 of 4). HCO 3− Cl− H+ + HCO 3– Chloride shift Hb H 2 CO 3 Hb H+ CO 2 H 2 O Hb Hb Systemic capillary CO 2 Cells in peripheral tissues CO 2 pickup (PO 2 = 40, PCO 2 = 45) 142
23 -10 Control of Respiration § Peripheral and alveolar capillaries – Maintain equilibrium of diffusion rates via • Local changes in oxygen delivery to peripheral tissues and in ventilation-to-perfusion ratio in lungs • Changes in depth and rate of respiration under control of brain’s respiratory centers 143 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Local regulation of respiration – Rising PCO 2 levels • Relax smooth muscle in arterioles and capillaries • Increasing blood flow – Ventilation-to-perfusion ratio (V/Q ratio) coordinates • Lung perfusion (blood flow to alveoli) with • Alveolar ventilation (airflow) – PCO 2 levels • Control bronchoconstriction and bronchodilation 144 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Respiratory centers of brain – When oxygen demand rises, respiratory rates increase under neural control • Has voluntary and involuntary components 145 © 2018 Pearson Education, Inc.
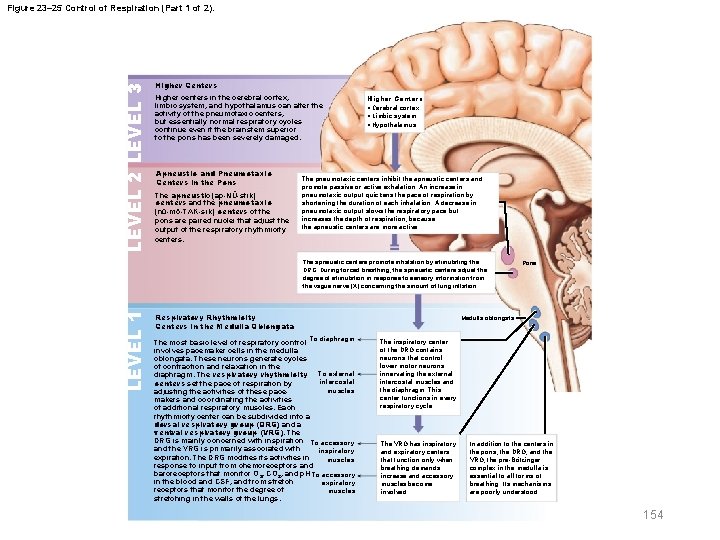
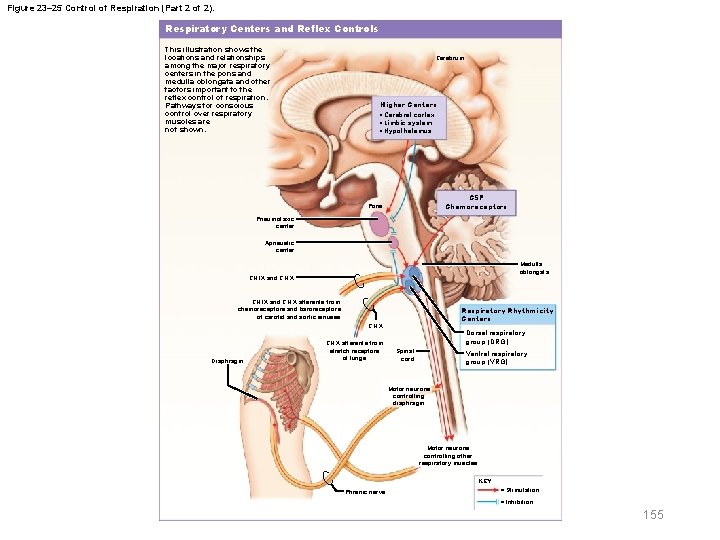
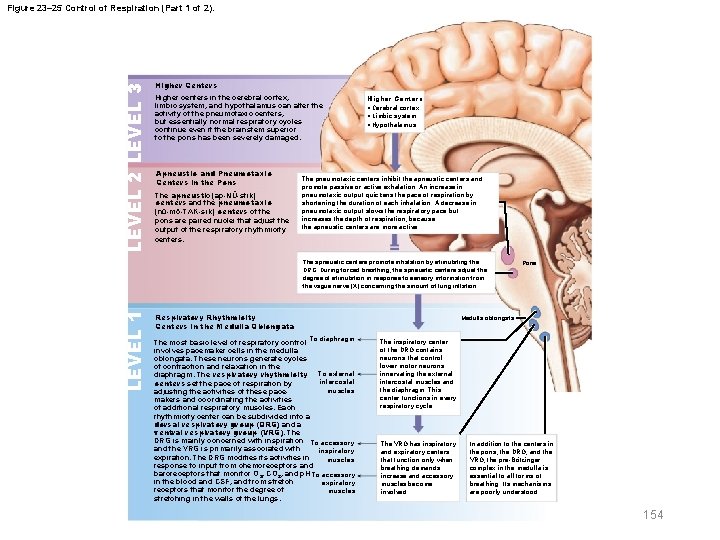
23 -10 Control of Respiration § Respiratory centers of brain – Voluntary centers in cerebral cortex affect • Respiratory centers of pons and medulla oblongata • Motor neurons that control respiratory muscles – Respiratory centers • Three pairs of nuclei in reticular formation of medulla oblongata and pons • Regulate frequency and depth of pulmonary ventilation in response to sensory information 146 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Respiratory rhythmicity centers – In medulla oblongata – Establish respiratory rate and rhythm – Each center is divided into • Dorsal respiratory group (DRG) • Ventral respiratory group (VRG) 147 © 2018 Pearson Education, Inc.
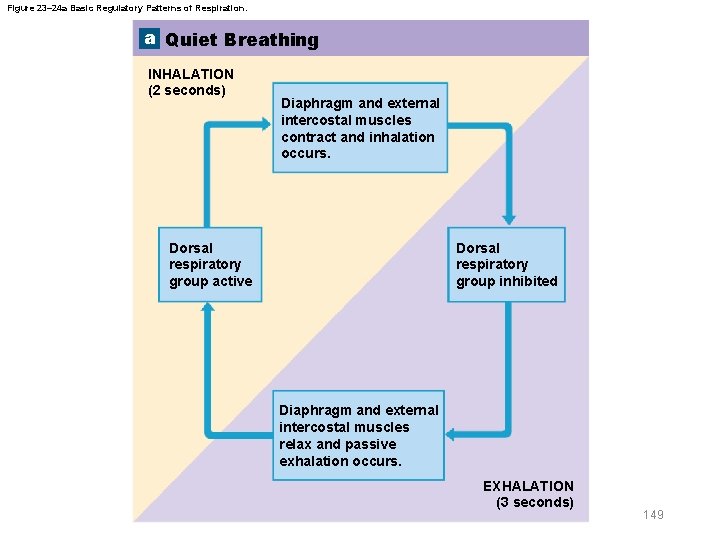
23 -10 Control of Respiration § Dorsal respiratory group (DRG) – Inspiratory center – Functions in quiet and forced breathing – In quiet breathing • Brief activity in DRG stimulates inspiratory muscles • DRG neurons become inactive allowing passive exhalation 148 © 2018 Pearson Education, Inc.
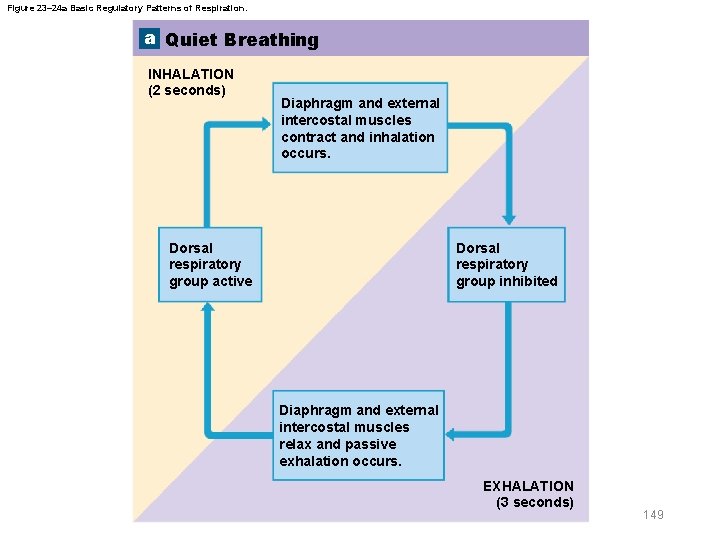
Figure 23– 24 a Basic Regulatory Patterns of Respiration. a Quiet Breathing INHALATION (2 seconds) Diaphragm and external intercostal muscles contract and inhalation occurs. Dorsal respiratory group active Dorsal respiratory group inhibited Diaphragm and external intercostal muscles relax and passive exhalation occurs. EXHALATION (3 seconds) 149
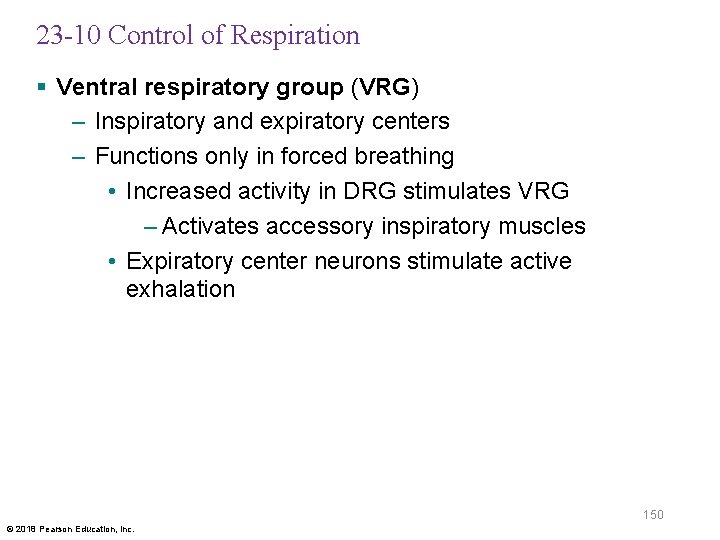
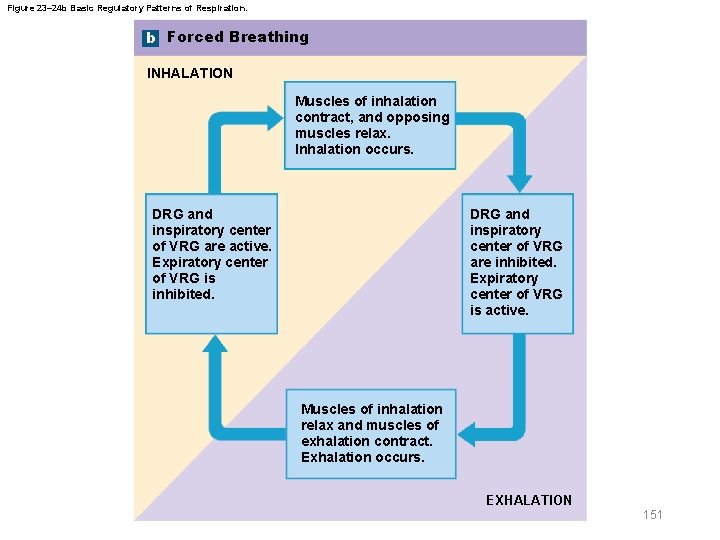
23 -10 Control of Respiration § Ventral respiratory group (VRG) – Inspiratory and expiratory centers – Functions only in forced breathing • Increased activity in DRG stimulates VRG – Activates accessory inspiratory muscles • Expiratory center neurons stimulate active exhalation 150 © 2018 Pearson Education, Inc.
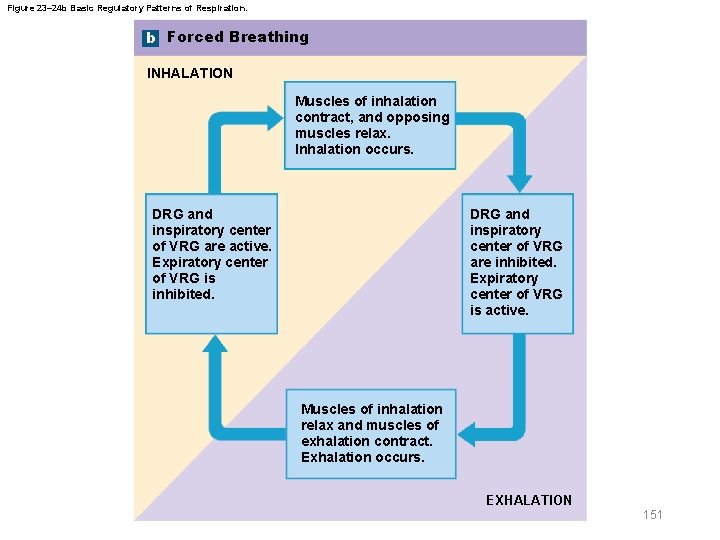
Figure 23– 24 b Basic Regulatory Patterns of Respiration. b Forced Breathing INHALATION Muscles of inhalation contract, and opposing muscles relax. Inhalation occurs. DRG and inspiratory center of VRG are active. Expiratory center of VRG is inhibited. DRG and inspiratory center of VRG are inhibited. Expiratory center of VRG is active. Muscles of inhalation relax and muscles of exhalation contract. Exhalation occurs. EXHALATION 151
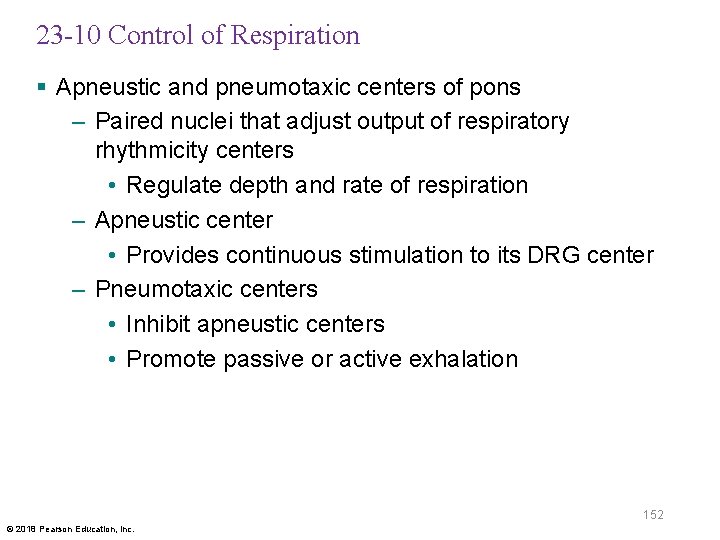
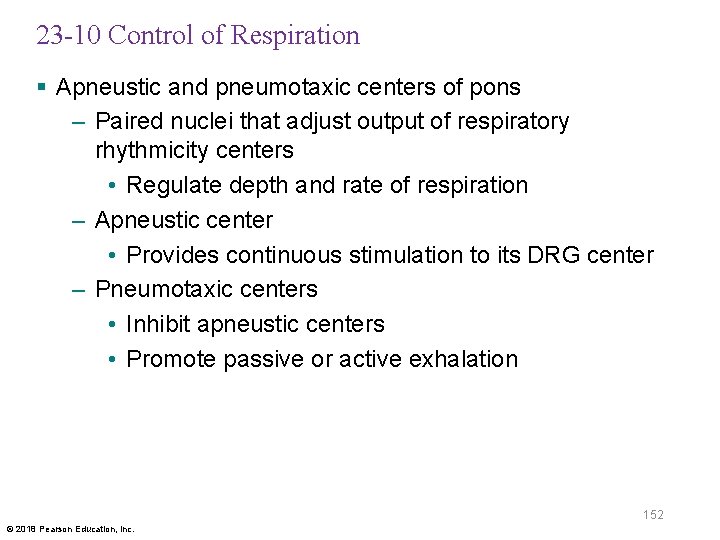
23 -10 Control of Respiration § Apneustic and pneumotaxic centers of pons – Paired nuclei that adjust output of respiratory rhythmicity centers • Regulate depth and rate of respiration – Apneustic center • Provides continuous stimulation to its DRG center – Pneumotaxic centers • Inhibit apneustic centers • Promote passive or active exhalation 152 © 2018 Pearson Education, Inc.
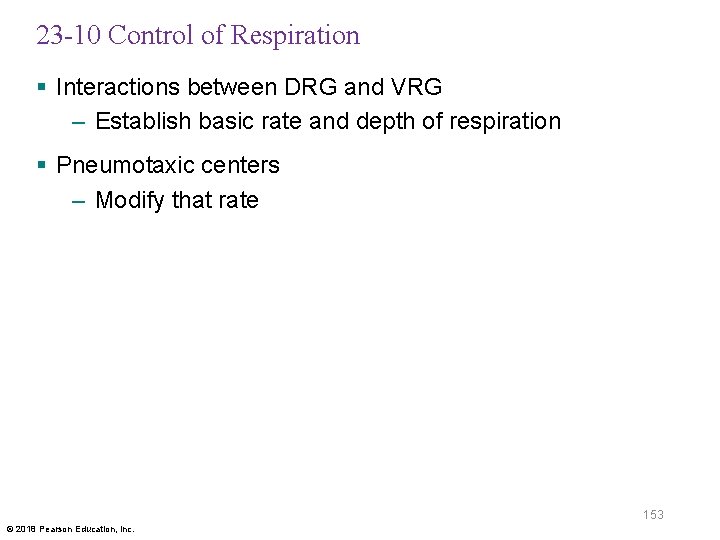
23 -10 Control of Respiration § Interactions between DRG and VRG – Establish basic rate and depth of respiration § Pneumotaxic centers – Modify that rate 153 © 2018 Pearson Education, Inc.
LEVEL 2 LEVEL 3 Figure 23– 25 Control of Respiration (Part 1 of 2). Higher Centers Higher centers in the cerebral cortex, limbic system, and hypothalamus can alter the activity of the pneumotaxic centers, but essentially normal respiratory cycles continue even if the brainstem superior to the pons has been severely damaged. Apneustic and Pneumotaxic Centers in the Pons The apneustic (ap-NŪ-stik) centers and the pneumotaxic (nū-mō-TAK-sik) centers of the pons are paired nuclei that adjust the output of the respiratory rhythmicity centers. Higher Centers • Cerebral cortex • Limbic system • Hypothalamus The pneumotaxic centers inhibit the apneustic centers and promote passive or active exhalation. An increase in pneumotaxic output quickens the pace of respiration by shortening the duration of each inhalation. A decrease in pneumotaxic output slows the respiratory pace but increases the depth of respiration, because the apneustic centers are more active. LEVEL 1 The apneustic centers promote inhalation by stimulating the DRG. During forced breathing, the apneustic centers adjust the degree of stimulation in response to sensory information from the vagus nerve (X) concerning the amount of lung inflation. Respiratory Rhythmicity Centers in the Medulla Oblongata Pons Medulla oblongata To diaphragm The most basic level of respiratory control involves pacemaker cells in the medulla oblongata. These neurons generate cycles of contraction and relaxation in the diaphragm. The respiratory rhythmicity To external intercostal centers set the pace of respiration by muscles adjusting the activities of these pacemakers and coordinating the activities of additional respiratory muscles. Each rhythmicity center can be subdivided into a dorsal respiratory group (DRG) and a ventral respiratory group (VRG). The DRG is mainly concerned with inspiration To accessory and the VRG is primarily associated with inspiratory expiration. The DRG modifies its activities in muscles response to input from chemoreceptors and baroreceptors that monitor O 2, CO 2, and p. H To accessory in the blood and CSF, and from stretch expiratory receptors that monitor the degree of muscles stretching in the walls of the lungs. The inspiratory center of the DRG contains neurons that control lower motor neurons innervating the external intercostal muscles and the diaphragm. This center functions in every respiratory cycle. The VRG has inspiratory and expiratory centers that function only when breathing demands increase and accessory muscles become involved. In addition to the centers in the pons, the DRG, and the VRG, the pre-Bötzinger complex in the medulla is essential to all forms of breathing. Its mechanisms are poorly understood. 154
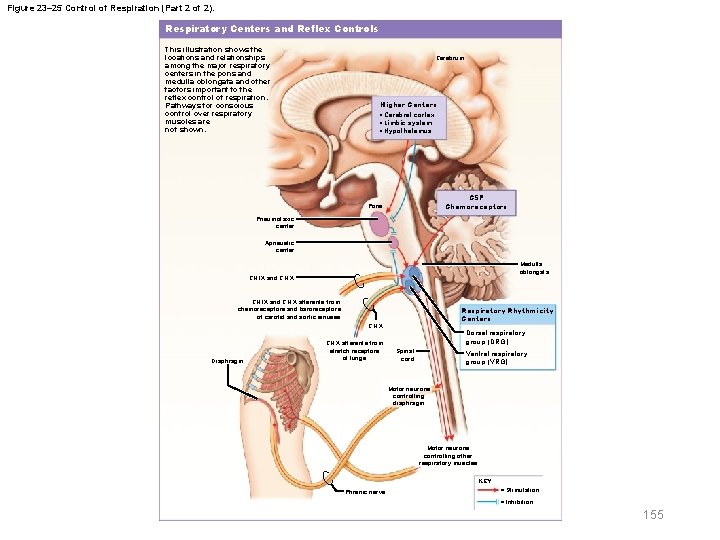
Figure 23– 25 Control of Respiration (Part 2 of 2). Respiratory Centers and Reflex Controls This illustration shows the locations and relationships among the major respiratory centers in the pons and medulla oblongata and other factors important to the reflex control of respiration. Pathways for conscious control over respiratory muscles are not shown. Cerebrum Higher Centers • Cerebral cortex • Limbic system • Hypothalamus CSF Chemoreceptors Pons Pneumotaxic center Apneustic center Medulla oblongata CN IX and CN X afferents from chemoreceptors and baroreceptors of carotid and aortic sinuses Respiratory Rhythmicity Centers CN X Diaphragm CN X afferents from stretch receptors of lungs Dorsal respiratory group (DRG) Spinal cord Ventral respiratory group (VRG) Motor neurons controlling diaphragm Motor neurons controlling other respiratory muscles KEY Phrenic nerve = Stimulation = Inhibition 155
23 -10 Control of Respiration § Sudden infant death syndrome (SIDS) – Disruption in normal respiratory reflex pattern – May result from connection problems between pacemaker complex and respiratory centers with other portions of brain 156 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Respiratory centers respond to sensory information – Chemoreceptors sensitive to PCO 2, PO 2, or p. H of blood or cerebrospinal fluid – Baroreceptors in aortic or carotid sinuses sensitive to changes in blood pressure – Stretch receptors respond to changes in lung volume – Irritating physical or chemical stimuli in nasal cavity, larynx, or bronchial tree – Other sensations including pain, changes in body temperature, and abnormal visceral sensations 157 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Respiratory centers are strongly influenced by chemoreceptor input from – Glossopharyngeal nerves (IX) • Changes in blood p. H or PO 2 at carotid bodies – Vagus nerves (X) • Changes in blood p. H or PO 2 at aortic bodies – Central chemoreceptors that monitor CSF • On ventrolateral surface of medulla oblongata • Respond to PCO 2 and p. H of CSF 158 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Chemoreceptor stimulation – Leads to increased depth and rate of respiration – Subject to adaptation • Decreased sensitivity due to chronic stimulation 159 © 2018 Pearson Education, Inc.
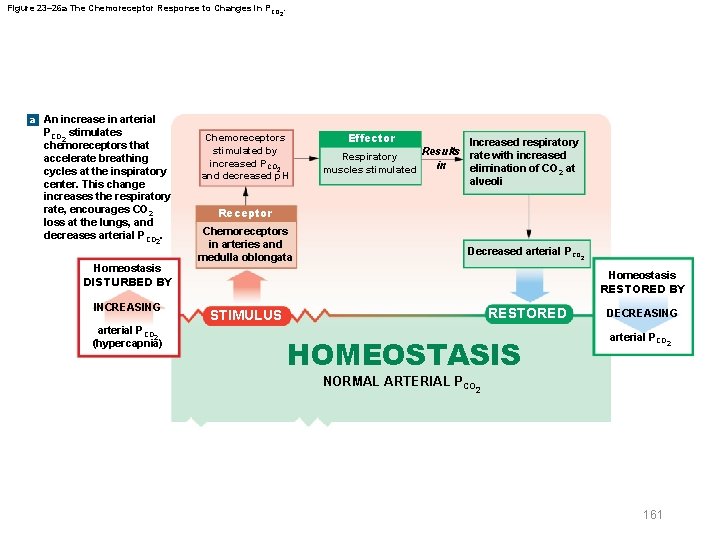
23 -10 Control of Respiration § Hypercapnia – An increase in arterial PCO 2 – Caused by abnormally low respiratory rate (hypoventilation) – Chemoreceptors stimulate respiratory centers to increase rate and depth of respiration 160 © 2018 Pearson Education, Inc.
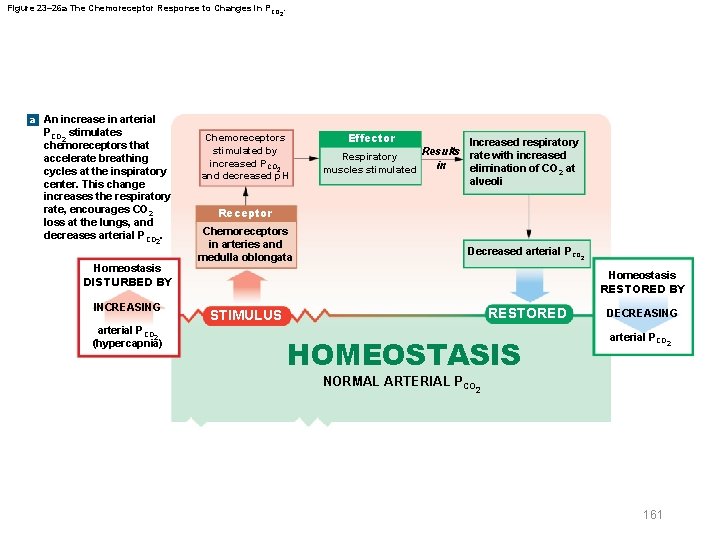
Figure 23– 26 a The Chemoreceptor Response to Changes in PCO 2. a An increase in arterial PCO 2 stimulates chemoreceptors that accelerate breathing cycles at the inspiratory center. This change increases the respiratory rate, encourages CO 2 loss at the lungs, and decreases arterial P CO. 2 Homeostasis DISTURBED BY INCREASING arterial PCO 2 (hypercapnia) Chemoreceptors stimulated by increased PCO 2 and decreased p. H Effector Increased respiratory Results rate with increased Respiratory in elimination of CO 2 at muscles stimulated alveoli Receptor Chemoreceptors in arteries and medulla oblongata Decreased arterial PCO 2 Homeostasis RESTORED BY RESTORED STIMULUS HOMEOSTASIS DECREASING arterial PCO 2 NORMAL ARTERIAL PCO 2 161
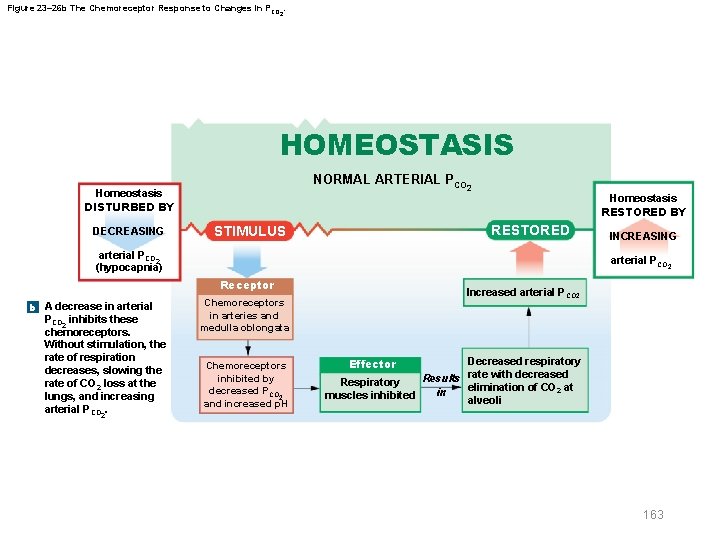
23 -10 Control of Respiration § Hypocapnia – Abnormally low PCO 2 – Caused by excessive ventilation (hyperventilation) – Chemoreceptor activity decreases and respiratory rate falls 162 © 2018 Pearson Education, Inc.
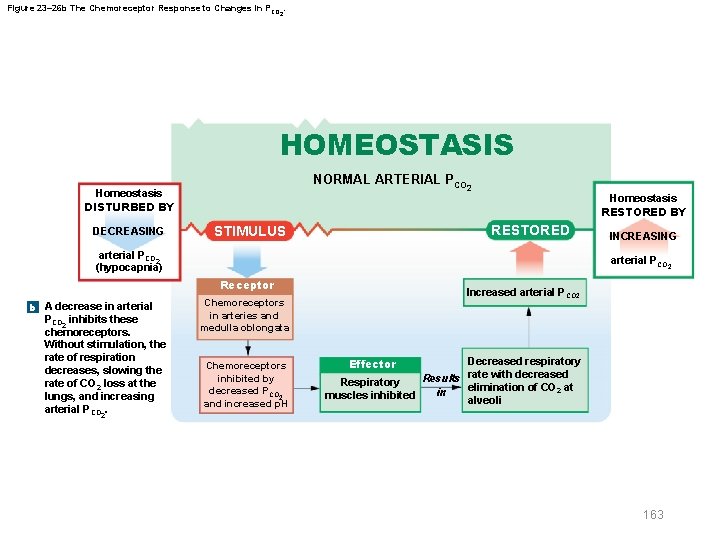
Figure 23– 26 b The Chemoreceptor Response to Changes in PCO 2. HOMEOSTASIS NORMAL ARTERIAL PCO 2 Homeostasis DISTURBED BY DECREASING Homeostasis RESTORED BY RESTORED STIMULUS arterial PCO 2 (hypocapnia) arterial PCO 2 Receptor b A decrease in arterial PCO 2 inhibits these chemoreceptors. Without stimulation, the rate of respiration decreases, slowing the rate of CO 2 loss at the lungs, and increasing arterial PCO. INCREASING Increased arterial P CO 2 Chemoreceptors in arteries and medulla oblongata Chemoreceptors inhibited by decreased PCO 2 and increased p. H Decreased respiratory Results rate with decreased Respiratory elimination of CO 2 at in muscles inhibited alveoli Effector 2 163
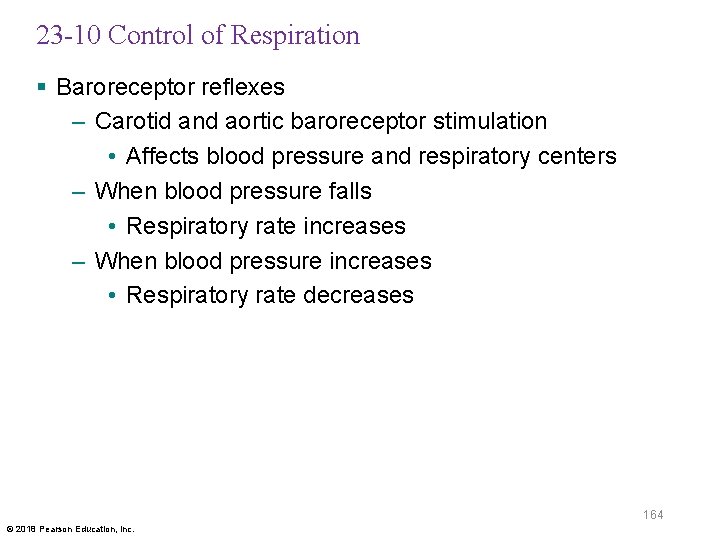
23 -10 Control of Respiration § Baroreceptor reflexes – Carotid and aortic baroreceptor stimulation • Affects blood pressure and respiratory centers – When blood pressure falls • Respiratory rate increases – When blood pressure increases • Respiratory rate decreases 164 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Hering Breuer reflexes – Two reflexes involved in forced breathing • Inflation reflex – Prevents overexpansion of lungs • Deflation reflex – Inhibits expiratory centers – Stimulates inspiratory centers during lung deflation 165 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Protective reflexes – Triggered by receptors in epithelium of respiratory tract when exposed to • Toxic vapors • Chemical irritants • Mechanical stimulation – Examples include sneezing, coughing, and laryngeal spasm 166 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Apnea – A period of suspended respiration – Normally followed by forceful expulsion of air to remove offending stimulus – Involved in sneezing and coughing § Laryngeal spasm – Temporarily closes airway • To prevent foreign objects, chemical irritants, or fluids from entering 167 © 2018 Pearson Education, Inc.
23 -10 Control of Respiration § Voluntary control of respiration – Strong emotions can stimulate respiratory centers in hypothalamus – Emotional states can activate sympathetic or parasympathetic division of ANS • Causing bronchodilation or bronchoconstriction – Anticipation of exercise can increase respiratory rate and cardiac output by sympathetic stimulation 168 © 2018 Pearson Education, Inc.
23 -11 Age-Related Changes in Respiration § Changes in respiratory system in newborns – Before birth • Pulmonary vessels are collapsed • Lungs contain no air – During delivery • Placental connection is lost • Blood PO 2 falls • PCO 2 rises 169 © 2018 Pearson Education, Inc.
23 -11 Age-Related Changes in Respiration § At birth, – Newborn overcomes surface tension to inflate bronchial tree and alveoli and take first breath – Large drop in pressure • Pulls blood into pulmonary circulation • Closing foramen ovale and ductus arteriosus • Redirecting fetal blood circulation patterns – Subsequent breaths fully inflate alveoli 170 © 2018 Pearson Education, Inc.
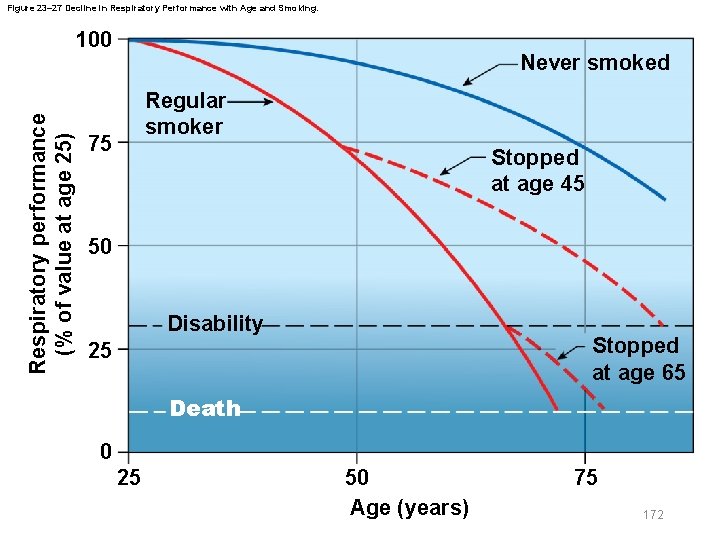
23 -11 Age-Related Changes in Respiration § Effects of aging on respiratory system – Elastic tissue deteriorates • Altering lung compliance and lowering vital capacity – Arthritic changes • Restrict chest movements • Limit respiratory minute volume – Emphysema • Affects individuals over age 50 • Extent depends on exposure to respiratory irritants (e. g. , cigarette smoke) 171 © 2018 Pearson Education, Inc.
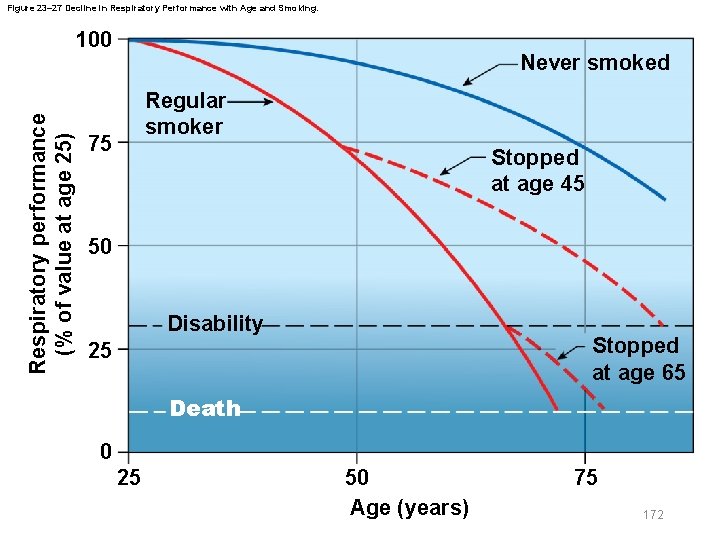
Figure 23– 27 Decline in Respiratory Performance with Age and Smoking. Respiratory performance (% of value at age 25) 100 Never smoked Regular smoker 75 Stopped at age 45 50 Disability Stopped at age 65 25 Death 0 25 50 Age (years) 75 172
23 -12 Respiratory System Integration § Goal of respiratory activity – To maintain homeostatic O 2 and CO 2 levels in peripheral tissues • Requires coordination between respiratory and cardiovascular systems 173 © 2018 Pearson Education, Inc.
23 -12 Respiratory System Integration § Integration of respiratory and cardiovascular systems – Improves efficiency of gas exchange by controlling lung perfusion – Increases respiratory rate and blood pressure through chemoreceptor stimulation – Raises cardiac output and blood flow through baroreceptor stimulation 174 © 2018 Pearson Education, Inc.
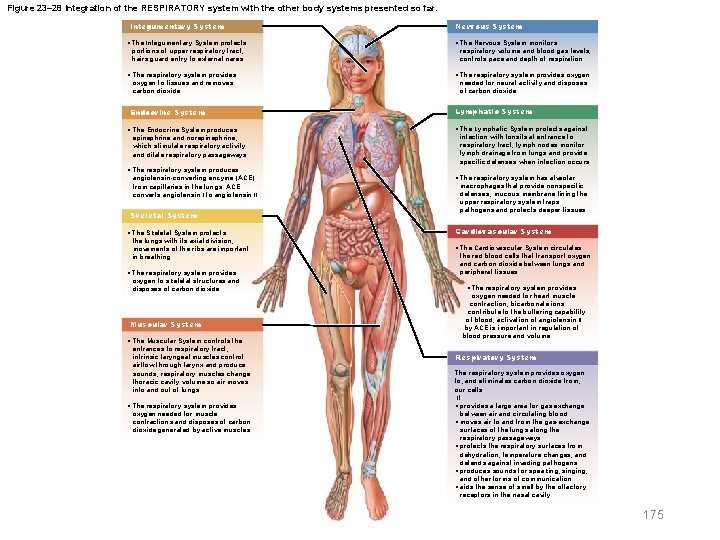
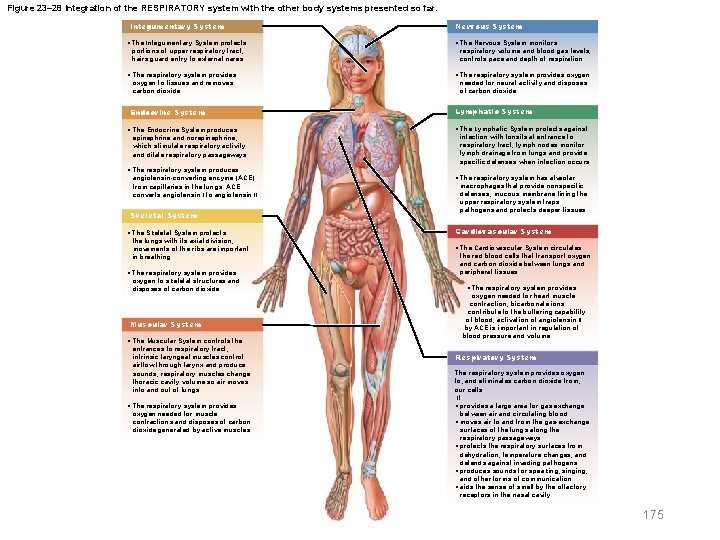
Figure 23– 28 Integration of the RESPIRATORY system with the other body systems presented so far. Integumentary System Nervous System • The Integumentary System protects portions of upper respiratory tract; hairs guard entry to external nares • The Nervous System monitors respiratory volume and blood gas levels; controls pace and depth of respiration • The respiratory system provides oxygen to tissues and removes carbon dioxide • The respiratory system provides oxygen needed for neural activity and disposes of carbon dioxide Endocrine System Lymphatic System • The Endocrine System produces epinephrine and norepinephrine, which stimulate respiratory activity and dilate respiratory passageways • The Lymphatic System protects against infection with tonsils at entrance to respiratory tract; lymph nodes monitor lymph drainage from lungs and provide specific defenses when infection occurs • The respiratory system produces angiotensin-converting enzyme (ACE) from capillaries in the lungs. ACE converts angiotensin I to angiotensin II Skeletal System • The Skeletal System protects the lungs with its axial division; movements of the ribs are important in breathing. • The respiratory system provides oxygen to skeletal structures and disposes of carbon dioxide Muscular System • The Muscular System controls the entrances to respiratory tract; intrinsic laryngeal muscles control airflow through larynx and produce sounds; respiratory muscles change thoracic cavity volume so air moves into and out of lungs • The respiratory system provides oxygen needed for muscle contractions and disposes of carbon dioxide generated by active muscles • The respiratory system has alveolar macrophages that provide nonspecific defenses; mucous membrane lining the upper respiratory system traps pathogens and protects deeper tissues Cardiovascular System • The Cardiovascular System circulates the red blood cells that transport oxygen and carbon dioxide between lungs and peripheral tissues • The respiratory system provides oxygen needed for heart muscle contraction; bicarbonate ions contribute to the buffering capability of blood; activation of angiotensin II by ACE is important in regulation of blood pressure and volume Respiratory System The respiratory system provides oxygen to, and eliminates carbon dioxide from, our cells. It: • provides a large area for gas exchange between air and circulating blood • moves air to and from the gas-exchange surfaces of the lungs along the respiratory passageways • protects the respiratory surfaces from dehydration, temperature changes, and defends against invading pathogens • produces sounds for speaking, singing, and other forms of communication • aids the sense of smell by the olfactory receptors in the nasal cavity 175
 Eleventh edition management
Eleventh edition management Management eleventh edition
Management eleventh edition Management eleventh edition
Management eleventh edition Management eleventh edition stephen p robbins
Management eleventh edition stephen p robbins Human anatomy and physiology seventh edition marieb
Human anatomy and physiology seventh edition marieb Human anatomy & physiology edition 9
Human anatomy & physiology edition 9 Human anatomy and physiology 10th edition
Human anatomy and physiology 10th edition The central sulcus divides which two lobes? (figure 14-13)
The central sulcus divides which two lobes? (figure 14-13) Chapter 1 introduction to human anatomy and physiology
Chapter 1 introduction to human anatomy and physiology Anatomy and physiology chapter 8 special senses
Anatomy and physiology chapter 8 special senses Chapter 13 anatomy and physiology of pregnancy
Chapter 13 anatomy and physiology of pregnancy Anatomy and physiology chapter 2
Anatomy and physiology chapter 2 Chapter 7:9 lymphatic system
Chapter 7:9 lymphatic system Anatomy and physiology coloring workbook chapter 14
Anatomy and physiology coloring workbook chapter 14 Chapter 10 blood anatomy and physiology
Chapter 10 blood anatomy and physiology Anatomy and physiology chapter 15
Anatomy and physiology chapter 15 Anatomy and physiology chapter 1
Anatomy and physiology chapter 1 Holes anatomy and physiology chapter 1
Holes anatomy and physiology chapter 1 Gi tract histology
Gi tract histology Medial lateral distal proximal
Medial lateral distal proximal Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Pectoral girdle acetabulum
Pectoral girdle acetabulum Chapter 6 general anatomy and physiology
Chapter 6 general anatomy and physiology Cranial cephalic
Cranial cephalic Eleventh 5 year plan
Eleventh 5 year plan Eleventh 5 year plan
Eleventh 5 year plan 11th five year plan
11th five year plan For his eleventh birthday elvis presley
For his eleventh birthday elvis presley Physiology of sport and exercise 5th edition
Physiology of sport and exercise 5th edition Pulmonary tract
Pulmonary tract Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad Woody stem parts
Woody stem parts Anatomy and physiology of bone
Anatomy and physiology of bone Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Liver hilus
Liver hilus Epigastric region
Epigastric region Wpigastric region
Wpigastric region Rbc anatomy and physiology
Rbc anatomy and physiology Http://anatomy and physiology
Http://anatomy and physiology Physiology of appendix
Physiology of appendix Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology of swine
Anatomy and physiology of swine Unit 26 self evaluation answers
Unit 26 self evaluation answers Science olympiad anatomy and physiology 2020 cheat sheet
Science olympiad anatomy and physiology 2020 cheat sheet Anatomy and physiology of stomach ppt
Anatomy and physiology of stomach ppt Pancreas anatomy and physiology
Pancreas anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Anatomy and physiology
Anatomy and physiology Cornell notes for anatomy and physiology
Cornell notes for anatomy and physiology Holes essential of human anatomy and physiology
Holes essential of human anatomy and physiology Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Anatomy and physiology
Anatomy and physiology Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Aohs foundations of anatomy and physiology 1
Aohs foundations of anatomy and physiology 1 Physiology exam 1
Physiology exam 1 Welcome to anatomy and physiology
Welcome to anatomy and physiology Physiology of the foot and ankle
Physiology of the foot and ankle Skin cancer
Skin cancer Pse 4
Pse 4 Pancreas anatomy and physiology
Pancreas anatomy and physiology Anatomy and physiology vocabulary
Anatomy and physiology vocabulary Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Figure 11-8 arteries
Figure 11-8 arteries Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy and physiology
Anatomy and physiology Anatomy histology
Anatomy histology Anatomy and physiology of eye
Anatomy and physiology of eye Oblongata
Oblongata Irn.org anatomy and physiology
Irn.org anatomy and physiology Anatomy and physiology body parts
Anatomy and physiology body parts Unit 26 animal anatomy physiology and nutrition
Unit 26 animal anatomy physiology and nutrition The digestive system and body metabolism
The digestive system and body metabolism Anatomy and physiology of the retina
Anatomy and physiology of the retina Animal tissue
Animal tissue Anatomy and physiology of meningitis ppt
Anatomy and physiology of meningitis ppt Jeopardy anatomy and physiology game
Jeopardy anatomy and physiology game Definition of homeostasis
Definition of homeostasis Anatomy and physiology
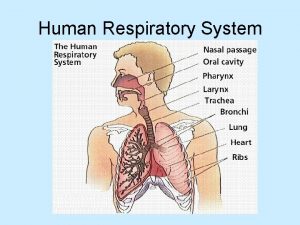
Anatomy and physiology Picture of human respiratory system
Picture of human respiratory system Physiology trivia
Physiology trivia Fish anatomy and physiology
Fish anatomy and physiology Brain anatomy and physiology
Brain anatomy and physiology Anatomy and physiology
Anatomy and physiology Unit 5 anatomy and physiology
Unit 5 anatomy and physiology 2012 pearson education inc anatomy and physiology
2012 pearson education inc anatomy and physiology Physiology of esophagus
Physiology of esophagus Fish anatomy and physiology
Fish anatomy and physiology Cengage anatomy and physiology
Cengage anatomy and physiology Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Fluid mechanics fundamentals and applications
Fluid mechanics fundamentals and applications Digital fundamentals tenth edition floyd
Digital fundamentals tenth edition floyd Machining fundamentals 10th edition
Machining fundamentals 10th edition Fundamentals of organizational communication
Fundamentals of organizational communication Fundamentals of organizational communication 9th edition
Fundamentals of organizational communication 9th edition Fundamentals of corporate finance 3rd canadian edition
Fundamentals of corporate finance 3rd canadian edition Digital fundamentals by floyd 10th edition
Digital fundamentals by floyd 10th edition Floyd digital fundamentals 10th edition pdf
Floyd digital fundamentals 10th edition pdf Electronics fundamentals a systems approach
Electronics fundamentals a systems approach Computer security fundamentals 4th edition
Computer security fundamentals 4th edition Management fundamentals 8th edition
Management fundamentals 8th edition Fundamentals of information systems
Fundamentals of information systems Fundamentals of corporate finance canadian edition
Fundamentals of corporate finance canadian edition Fundamentals of corporate finance fifth edition
Fundamentals of corporate finance fifth edition Corporate finance 6th edition
Corporate finance 6th edition Abnormal psychology comer 9th edition
Abnormal psychology comer 9th edition Fundamentals of information systems 9th edition
Fundamentals of information systems 9th edition Thermal conduction resistance
Thermal conduction resistance The fundamentals of political science research 2nd edition
The fundamentals of political science research 2nd edition Mis chapter 6
Mis chapter 6 Mis
Mis Clinical kinesiology and anatomy 6th edition
Clinical kinesiology and anatomy 6th edition Clinical kinesiology and anatomy 6th edition
Clinical kinesiology and anatomy 6th edition Human anatomy fifth edition
Human anatomy fifth edition Human anatomy fifth edition
Human anatomy fifth edition Fundamental of nursing chapter 1
Fundamental of nursing chapter 1 Fundamentals of electric circuits chapter 4 solutions
Fundamentals of electric circuits chapter 4 solutions Fundamentals of corporate finance chapter 6 solutions
Fundamentals of corporate finance chapter 6 solutions Digital fundamentals chapter 4
Digital fundamentals chapter 4 Conceptual physics magnetism
Conceptual physics magnetism Tire wheel and wheel bearing fundamentals
Tire wheel and wheel bearing fundamentals Chapter 1 understanding health and wellness answer key
Chapter 1 understanding health and wellness answer key The circuit chapter 9
The circuit chapter 9 Fundamentals of electric circuits chapter 7 solutions
Fundamentals of electric circuits chapter 7 solutions Building the right foundations/fundamentals
Building the right foundations/fundamentals Computer fundamentals chapter 1
Computer fundamentals chapter 1 Fundamentals of corporate management
Fundamentals of corporate management Fundamentals of thermal-fluidsciences chapter 1 problem 24p
Fundamentals of thermal-fluidsciences chapter 1 problem 24p Introduction to information systems 6th edition
Introduction to information systems 6th edition Fundamentals of information systems
Fundamentals of information systems Fundamentals of nursing chapter 17 vital signs
Fundamentals of nursing chapter 17 vital signs Chapter 6 fingerprints
Chapter 6 fingerprints Lodging operation in hospitality industry
Lodging operation in hospitality industry Chapter 2 lab java fundamentals
Chapter 2 lab java fundamentals Back channeling nursing
Back channeling nursing Examples of the respiratory system
Examples of the respiratory system Chapter 39 electrical fundamentals
Chapter 39 electrical fundamentals Fundamentals of thermal-fluidsciences chapter 1 problem 1p
Fundamentals of thermal-fluidsciences chapter 1 problem 1p Fundamentals of thermal-fluidsciences chapter 2 problem 58p
Fundamentals of thermal-fluidsciences chapter 2 problem 58p Fundamentals of nursing chapter 15 critical thinking
Fundamentals of nursing chapter 15 critical thinking Chapter 1 lesson 1 your total health
Chapter 1 lesson 1 your total health Fundamentals of thermal-fluidsciences chapter 1 problem 18p
Fundamentals of thermal-fluidsciences chapter 1 problem 18p Fundamentals of thermal-fluidsciences chapter 1 problem 16p
Fundamentals of thermal-fluidsciences chapter 1 problem 16p Fundamentals of nursing chapter 16
Fundamentals of nursing chapter 16 Grashof number
Grashof number Fundamentals of corporate finance, chapter 1
Fundamentals of corporate finance, chapter 1 Fundamentals of thermal-fluidsciences chapter 2 problem 30p
Fundamentals of thermal-fluidsciences chapter 2 problem 30p Fundamentals of thermal-fluidsciences chapter 2 problem 27p
Fundamentals of thermal-fluidsciences chapter 2 problem 27p Chapter 23 computer system fundamentals
Chapter 23 computer system fundamentals Organizational behavior 18th edition chapter 1
Organizational behavior 18th edition chapter 1 Organic chemistry (3rd) edition chapter 1 problem 16s
Organic chemistry (3rd) edition chapter 1 problem 16s Mechanics of materials chapter 10
Mechanics of materials chapter 10 Chapter 7 mechanics of materials solutions
Chapter 7 mechanics of materials solutions Mechanics of materials 6th edition beer solution chapter 6
Mechanics of materials 6th edition beer solution chapter 6 Mechanics of materials 6th edition beer solution chapter 5
Mechanics of materials 6th edition beer solution chapter 5 Mechanics of materials
Mechanics of materials Everything's an argument chapter 1 questions
Everything's an argument chapter 1 questions Ifsta 7th edition chapter 6
Ifsta 7th edition chapter 6 Engineering economy 16th edition chapter 5 solutions
Engineering economy 16th edition chapter 5 solutions Engineering economy 16th edition chapter 4 solutions
Engineering economy 16th edition chapter 4 solutions Business essentials 12th edition chapter 1
Business essentials 12th edition chapter 1 Lazarus's appraisal theory
Lazarus's appraisal theory Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Group cohesiveness and performance
Group cohesiveness and performance Organic chemistry third edition david klein
Organic chemistry third edition david klein