Functions of Testosterone Secretion Testes produce several male










- Slides: 32
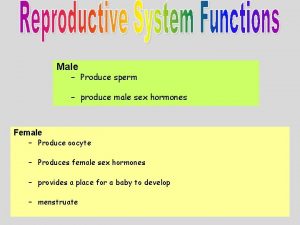
Functions of Testosterone
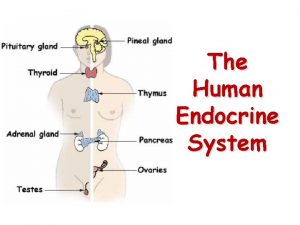
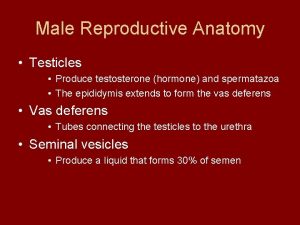
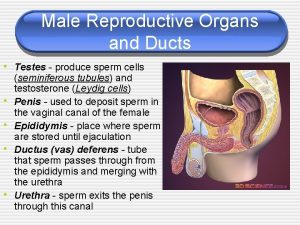
Secretion • Testes produce several male hormones (Androgens) – – – • • • Testosterone Dihydrotestosterone Androstenedione Testosterone – most abundant Dihydrotestosterone is the most active form Most of the testosterone also, is converted into dihydrotestosterone in the tissues Produced in Interstitial cells of Leydig Constitute 20 % of the testicular mass
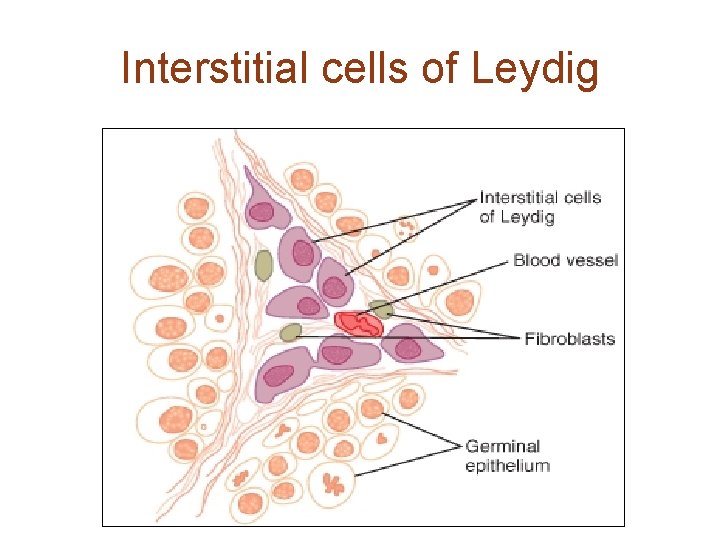
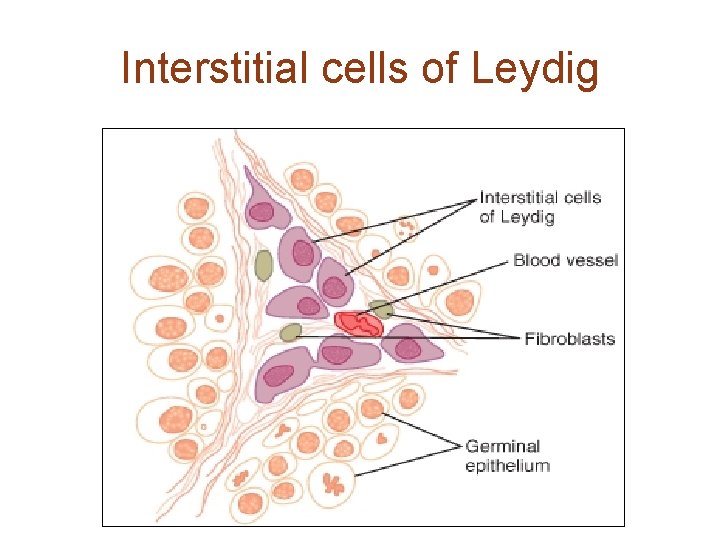
Interstitial cells of Leydig
Interstitial cells of Leydig • Almost nonexistent in childhood – No testosterone secretion throughout childhood because of absence of LH • Numerous in new born babies due to HCGH • If germinal epithelium degenerates due to heat, x-rays etc ICL survive and still produce testosterone.

Testosterone • Responsible for distinguishing masculine characteristics • HCGH stimulated intrauterine secretion→ Development of male fetus • No testosterone throughout childhood • Near puberty LH from anterior pituitary → gradually increasing levels of testosterone • Declined secretion after 50 years of age • Secretion continues throughout life

Stages of testosterone secretin

Intrauterine functions • Secreted from genital ridge or developing testes due to HCGH • Y chromosome causes secretion of testosterone from the genital ridge • X chromosome causes secretion of estrogen from the genital ridge • Simply presence or absence is responsible for male or female external genitalia in the fetus.
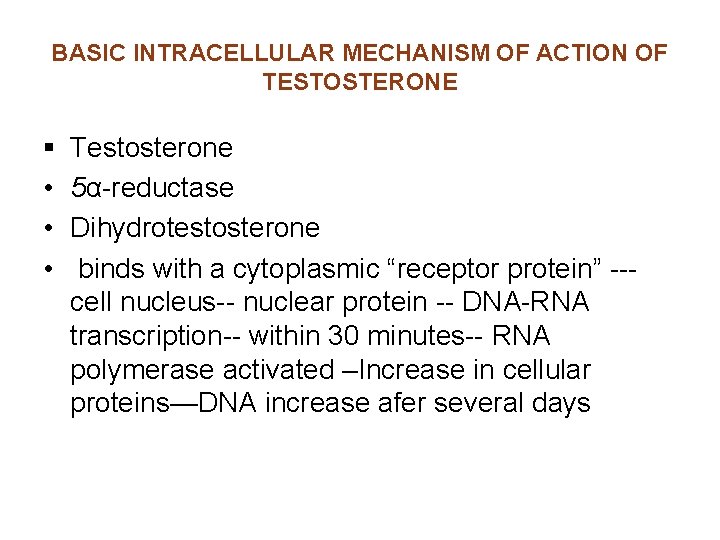
BASIC INTRACELLULAR MECHANISM OF ACTION OF TESTOSTERONE § • • • Testosterone 5α-reductase Dihydrotestosterone binds with a cytoplasmic “receptor protein” --cell nucleus-- nuclear protein -- DNA-RNA transcription-- within 30 minutes-- RNA polymerase activated –Increase in cellular proteins—DNA increase afer several days
Development of male fetus • Intrauterine testosterone responsible for development of – – Penis & Scrotum Prostate gland Seminal vesicles Wolffian duct system give rise to male tubular system • Testosterone suppresses development of female genital organs • Müllerian duct system disappears
Descent of testes • Testes develop from the genital ridge in the genital region • Testes descend into scrotum through inguinal canal • Testosterone required for this descent • Cryptorchidism may be treated with administration of testosterone in neonates

Functions at puberty • Enlargement – Penis – Scrotum – Testes • Development of secondary sex characters of male – Apparent differences of male from female
Distribution of hair • Growth of hair – – On face (beard & mustaches) Over the pubis Along the linea alba Usually on the chest, legs and other parts of the body • Baldness – Genetic back ground – High testosterone level – ↑↑Testosterone even in female can cause baldness Baldness
Voice • Testosterone causes – Enlargement of larynx – Hypertrophy of laryngeal mucosa and vocal cords – Initially cracking voice – Later voice changes into typical masculine voice

Skin • • • ↑ thickness of the skin ↑ruggedness of SC tissue ↑ rate of secretion of sebaceous glands ↑ secretion on the face → Acne very common after puberty Acne disappear due to gradual adaptation of sebaceous glands and skin
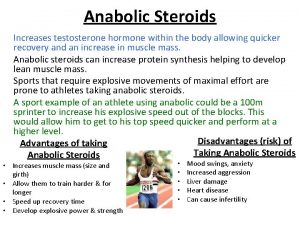
Proteins • Powerful anabolic hormone • Deposition of protein in muscles • Deposition of protein in nonmuscular tissues as well • Male musculature is 50 % more than female • Athletes use synthetic androgens to improve muscular performance • May be used in elderly people to improve muscle strength
Bones • • ↑Deposition of protein in bones ↑matrix as well as calcium deposition ↑ thickness and strength of the bones Male bones are much more stronger than female ↑ growth in length of the bone near puberty Disappearance of epiphyseal cartilage Eunuchs have more height than normal male or female
Special changes in pelvis • • • Narrow pelvic outlet Elongated and Funnel shaped pelvis More load bearing type Female pelvis is broad and ovoid If testosterone is absent the male pelvis is also female like

BMR & RBC count • ↑ BMR • More oxygen consumption in male compared to female • BMR 15 % more than female • May be an indirect effect of protein anabolism caused by testosterone • ↑O 2 consumption → relative hypoxia → renal erythropoietic factor → ↑erythropoiesis • ↑ RBC count may be due to direct effect on erythropoiesis
Water and electrolytes • All the steroid can – ↑ Na+ and other electrolytes reabsorption from the kidney tubules – Secondary reabsorption of water
Regulation of Testosterone secretion and reproductive functions
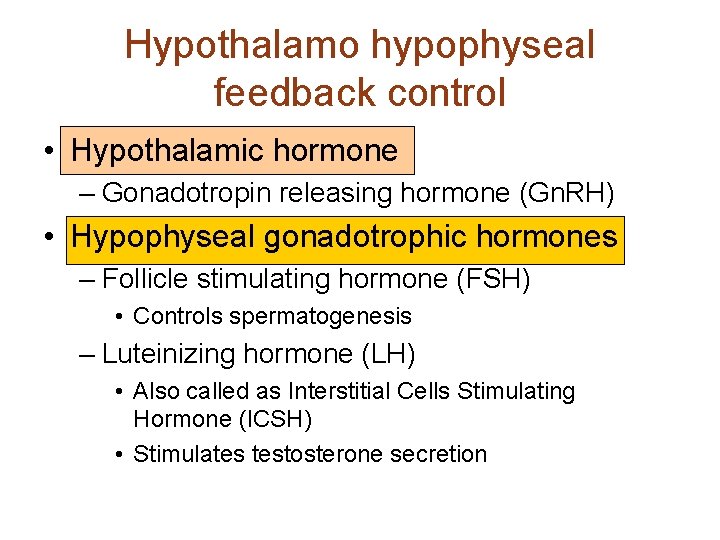
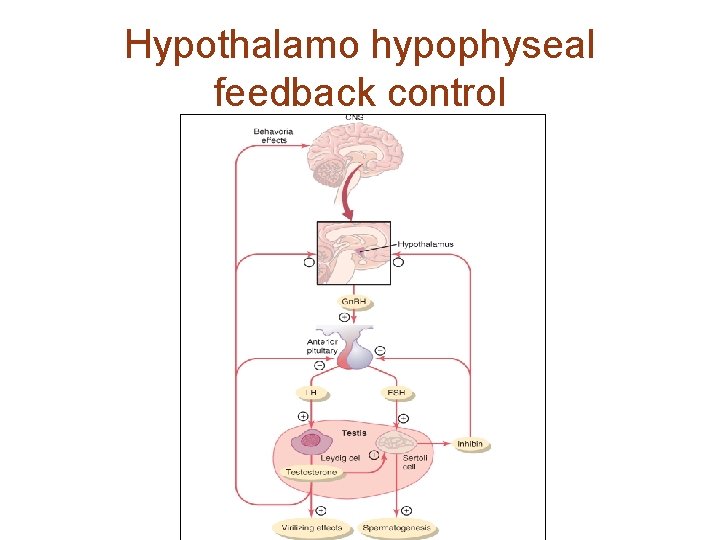
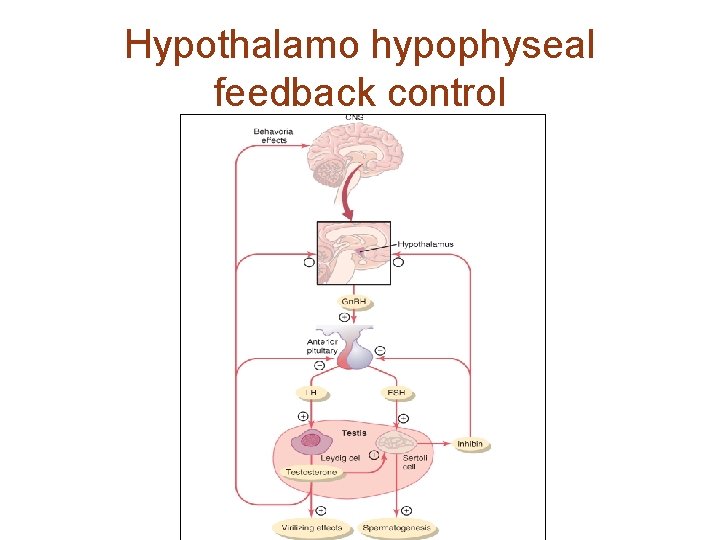
Hypothalamo hypophyseal feedback control • Hypothalamic hormone – Gonadotropin releasing hormone (Gn. RH) • Hypophyseal gonadotrophic hormones – Follicle stimulating hormone (FSH) • Controls spermatogenesis – Luteinizing hormone (LH) • Also called as Interstitial Cells Stimulating Hormone (ICSH) • Stimulates testosterone secretion
Hypothalamo hypophyseal feedback control • Gn. RH – – – 10 AA peptide Arcuate nuclei of hypothalamus Nerve endings in median eminence Hypothalamo-hypophyseal portal vessels Intermittent (cyclic) release of Gn. RH • A few minutes release after every 1 -3 hours • Variations in frequency of release • Variations in quantity released in each cycle – LH secretion has similar cyclic release – LHRH

Hypothalamo hypophyseal feedback control • LH and FSH – Glycoprotein in nature – Produced by gonadotropes in adenohypophysis – LH cyclic release according to cyclic fluctuations of Gn. RH- exactly follows – FSH also increases or decreases with the fluctuations in Gn. RH- more slowly – Gn. RH also called as LH-releasing hormone (LHRH) – Without Gn. RH no secretion of LH & FSH
Regulation of testosterone secretion • • • Interstitial cells of Leydig LH stimulates secretion of testosterone ICL present in new born babies Absent throughout childhood At puberty when LH secretion starts ICL develop again • Testosterone has negative feed back effect on LH secretion

Negative feedback control • ↑Testosterone inhibits – Hypothalamus – arcuate nuclei →↓ Gn. RH – Adenohypophysis – gonadotropes →↓ LH & FSH • ↓ Testosterone stimulates – Hypothalamus – arcuate nuclei → ↑ Gn. RH – Adenohypophysis – gonadotropes →↑ LH & FSH

Regulation of spermatogenesis • FSH –receptors in Sertoli cells – Cells enlarge – Produce substances necessary for spermatogenesis – Testosterone also increases spermatogenic activity – Sertoli cells produce hormone “Inhibin” • A glycoprotein • Has been extracted from the Sertoli cells – Inhibin inhibits FSH and Gn. RH
Hypothalamo hypophyseal feedback control
Psychic element • Different signals from different part of the brain affect Hypothalamic release of Gn. RH • Psychic factors from limbic system greatly affect the hypothalamic secretion of Gn. RH – Hence secretion of LH and FSH
Puberty • Gradual onset of secretion of sex hormones and the reproductive life • Before puberty – – No secretion of Gn. RH No secretion of LH & FSH No testosterone and spermatogenesis Hypothalamus is hypersensitive to smallest amount of circulating sex hormones – This hypersensitivity gradually reduces – Or maturation process of limbic system or hypothalamus → onset of puberty
Adult sexual life and male climacteric • After puberty LH & FSH are produced throughout life • After late 40 s or 50 s there is reduction in testosterone level • The decrease in sexual functions in elderly male is called male climacteric. • Sometimes symptoms like female menopause (hot flushes, psychic sensation of dyspnea, irritability, fatigue, anxiety etc) may need treatment with testosterone

Thank-you Questions ? ?
 In males, fsh prods these organs to produce testosterone.
In males, fsh prods these organs to produce testosterone. What hormone does the testes produce
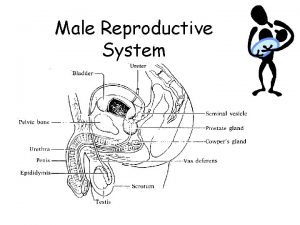
What hormone does the testes produce Bull reproductive system parts and functions
Bull reproductive system parts and functions Dating serves several important functions that include:
Dating serves several important functions that include: Dating serves several important functions that include
Dating serves several important functions that include Dating serves several important functions that include:
Dating serves several important functions that include: Hormone secretion
Hormone secretion Produces testosterone
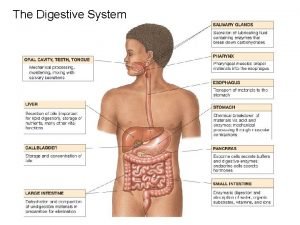
Produces testosterone Secretion of gastric juice
Secretion of gastric juice Estrogen effect
Estrogen effect Pseudostratified columnar epithelium
Pseudostratified columnar epithelium Thyroid hormone secretion
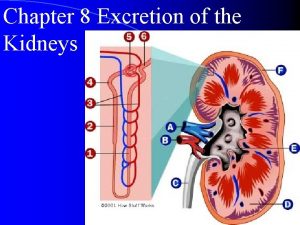
Thyroid hormone secretion H+ secretion in proximal tubule
H+ secretion in proximal tubule Secretion of bicarbonate ions
Secretion of bicarbonate ions Embryology of git
Embryology of git Serous acinus
Serous acinus Contents of gastric juice
Contents of gastric juice Dr claude chauchard
Dr claude chauchard Where does secretion occur in nephron
Where does secretion occur in nephron Trib3 precio
Trib3 precio Atrial natriuretic peptide
Atrial natriuretic peptide Anabolic steroids
Anabolic steroids Holocrine secretion
Holocrine secretion Nephron reabsorption and secretion
Nephron reabsorption and secretion Function of body in stomach
Function of body in stomach Produces testosterone
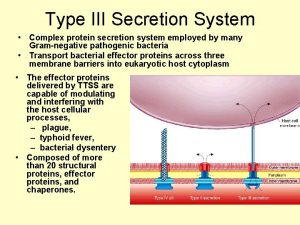
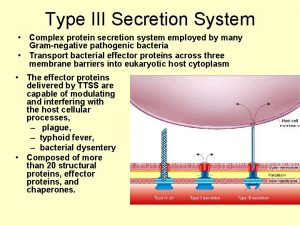
Produces testosterone Type 3 secretion system
Type 3 secretion system Erythropin
Erythropin Parietal cell of stomach secrete
Parietal cell of stomach secrete Hydrogen secretion in kidney
Hydrogen secretion in kidney Bile and pancreatic juices are secreted in the
Bile and pancreatic juices are secreted in the Nebido effectiveness
Nebido effectiveness Tubular reabsorption and secretion
Tubular reabsorption and secretion