FUNCTIONAL GI DISORDERS AHMAD ABUDAYYEH OUTLINE Definition Classification
FUNCTIONAL GI DISORDERS AHMAD ABUDAYYEH
OUTLINE • Definition • Classification • Functional heartburn • Globus • Functional dyspepsia • IBS • Functional diarrhea • Functional constipation
DEFINITION • Disorders in which symptoms occur in the absence of any demonstrable abnormalities in the digestion and absorption of nutrients, fluid and electrolytes and no structural abnormality can be identified in the gastrointestinal tract, although there may be discernible abnormalities in neuromuscular function such as dysmotility and visceral hypersensitivity, which are not routinely investigated • Stigma
DEFINITION – ROME IV • It is a group of disorders classified by GI symptoms related to any combination of the following: motility disturbance, visceral hypersensitivity, altered mucosal and immune function, altered gut microbiota, and altered central nervous system (CNS) processing.


FUNCTIONAL HEARTBURN • Retrosternal burning in the absence of GERD, that meets other essential criteria for the functional esophageal disorders • Heartburn is reported by 20%– 40% of subjects in Western populations, depending on thresholds for a positive response • Studies using both endoscopy and ambulatory p. H monitoring to objectively establish evidence of GERD indicate that functional heartburn represents 10% of patients with heartburn presenting to gastroenterologists.
FUNCTIONAL HEARTBURN – ROME IV • Must include all of the following: 1. Burning retrosternal discomfort or pain 2. Absence of evidence that gastroesophageal acid reflux is the cause of the symptom 3. Absence of histopathology-based esophageal motility disorders * Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis
PATHOPHYSIOLOGY • The prevailing view is to consider disturbed visceral perception as a major factor involved in pathogenesis • Enhanced sensitivity to refluxate having slight p. H alterations from normal may be responsible in some instances • Psychological factors may participate in heart-burn reporting when evidence of a noxious esophageal stimulus is limited.
CLINICAL EVALUATION • Clarification of the nature of the symptom is an essential first step to avoid overlooking extra esophageal symptom sources. • Additional evaluation primarily is oriented toward establishing or excluding the presence of GERD. • Endoscopy that reveals no evidence of esophagitis is insufficient in this regard, especially in those subjects who are evaluated while remaining on or shortly after discontinuing anti reflux therapy • Ambulatory p. H monitoring can better classify patients who have normal findings on endoscopic evaluation, including those whose symptoms persist despite therapy.
TREATMENT • Low-dose tricyclic antidepressants • Other antidepressants • Psychological therapies • Although controlled trials demonstrating efficacy are unavailable
GLOBUS • A sense of a lump, a retained food bolus, or tightness in the throat. • Globus is a common symptom and is reported by up to 46% of apparently healthy individuals, with a peak incidence in middle age. • The symptom is equally prevalent in men and women among healthy individuals in the community, but women are more likely to seek health care for this symptom.
GLOBUS – ROME IV • Must include all of the following: 1. Persistent or intermittent, nonpainful sensation of a lump or foreign body in the throat 2. Occurrence of the sensation between meals 3. Absence of dysphagia or odynophagia 4. Absence of evidence that gastroesophageal reflux is the cause of the symptom 5. Absence of histopathology-based esophageal motility disorders *Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis
PATHOPHYSIOLOGY • Upper esophageal sphincter mechanics do not seem relevant, and the pharyngeal swallow mechanism is normal. • Urge to swallow and increased swallow frequency might contribute to the symptom by periodically causing air entrapment in the proximal esophagus. • Esophageal balloon distention can reproduce globus sensation at low distending thresholds, suggesting some degree of esophageal hypersensitivity. • Up to 96% of subjects with globus report symptom exacerbation during periods of high emotional intensity.
CLINICAL EVALUATION • The diagnosis is made from a compatible clinical history, including clarification that dysphagia is absent. • Physical examination of the neck followed by nasolaryngoscopic examination of the pharynx and larynx are advised (debated) • Further investigation of the simple symptom is not well supported; dysphagia, odynophagia, pain, weight loss, hoarseness, or other alarm symptoms mandate more extensive evaluation • Therapeutic trial of a PPI when uninvestigated patients present with the symptom of globus
TREATMENT • Given the benign nature of the condition, the likelihood of long-term symptom persistence, and the absence of highly effective pharmacotherapy, the mainstay of treatment rests with explanation and reassurance. • Expectations for prompt symptom resolution are low, because symptoms persist in up to 75% of patients at 3 years
FUNCTIONAL DYSPEPSIA • Dyspepsia is a common symptom with an extensive differential diagnosis • Approximately 25% of patients with dyspepsia have an underlying organic cause. However, up to 75% of patients have functional (idiopathic or non-ulcer) dyspepsia with no underlying cause on diagnostic evaluation • The prevalence of functional dyspepsia ranges from 5 to 11% worldwide
PATHOPHYSIOLOGY • The pathophysiology of functional dyspepsia is not well understood. However, several potential mechanisms have been suggested. • Gastric motility and compliance (delayed emptying in 25 -35% rapid in 10%) • Visceral hypersensitivity • Helicobacter pylori infection • Altered gut microbiome • Duodenal inflammation • Psychosocial dysfunction
CLINICAL MANIFESTATIONS • Postprandial fullness, early satiety, and/or epigastric pain/burning. • Symptoms may be severe enough to limit usual activities. • Some patients may have nausea, vomiting, or heartburn, however, these symptoms are usually infrequent.
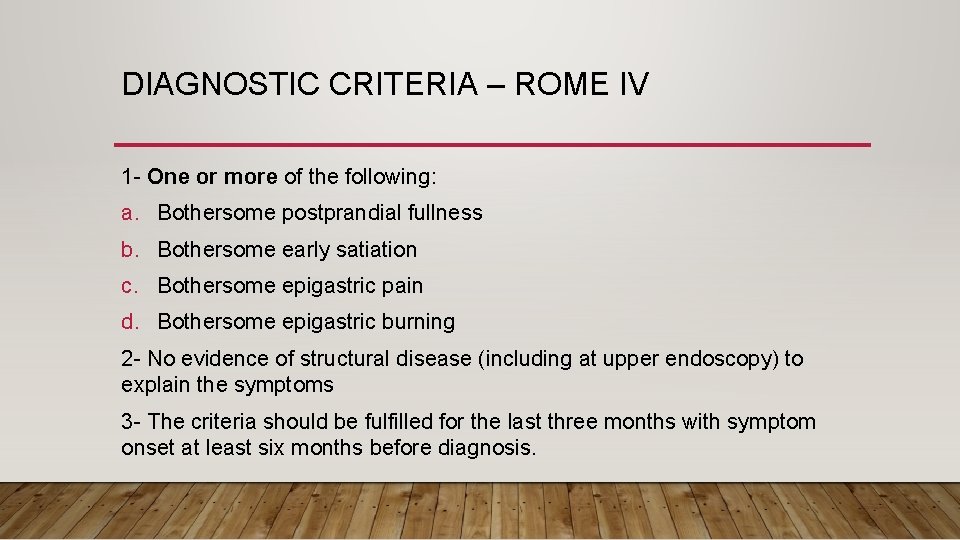
DIAGNOSTIC CRITERIA – ROME IV 1 - One or more of the following: a. Bothersome postprandial fullness b. Bothersome early satiation c. Bothersome epigastric pain d. Bothersome epigastric burning 2 - No evidence of structural disease (including at upper endoscopy) to explain the symptoms 3 - The criteria should be fulfilled for the last three months with symptom onset at least six months before diagnosis.
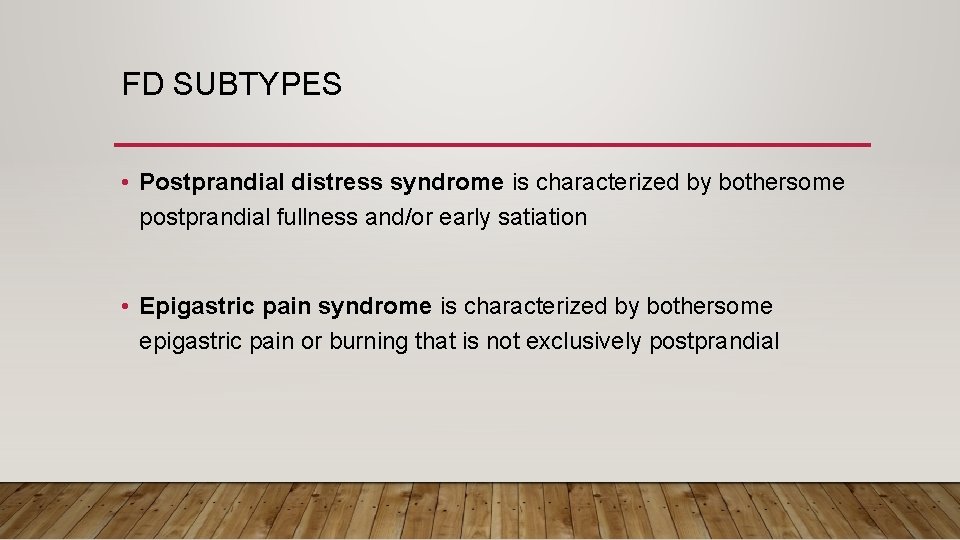
FD SUBTYPES • Postprandial distress syndrome is characterized by bothersome postprandial fullness and/or early satiation • Epigastric pain syndrome is characterized by bothersome epigastric pain or burning that is not exclusively postprandial
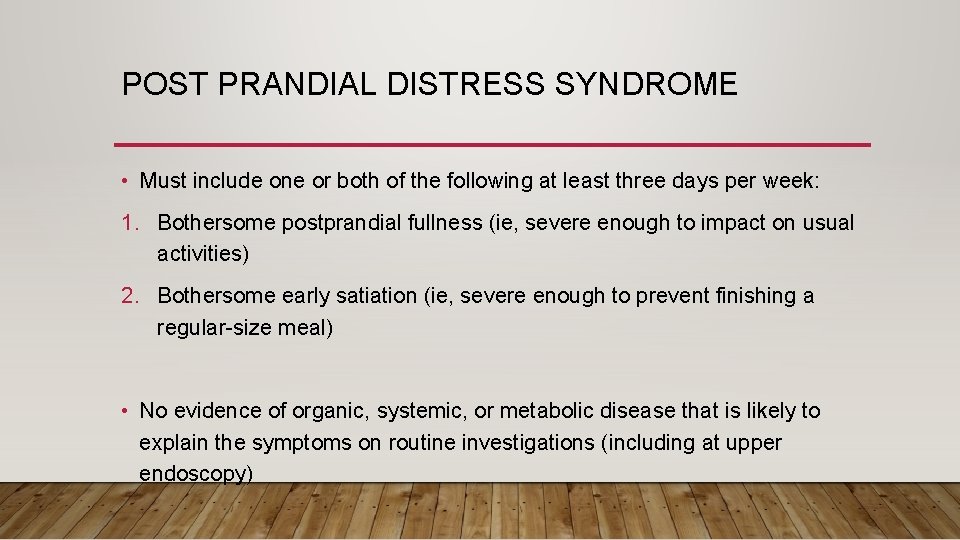
POST PRANDIAL DISTRESS SYNDROME • Must include one or both of the following at least three days per week: 1. Bothersome postprandial fullness (ie, severe enough to impact on usual activities) 2. Bothersome early satiation (ie, severe enough to prevent finishing a regular-size meal) • No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms on routine investigations (including at upper endoscopy)
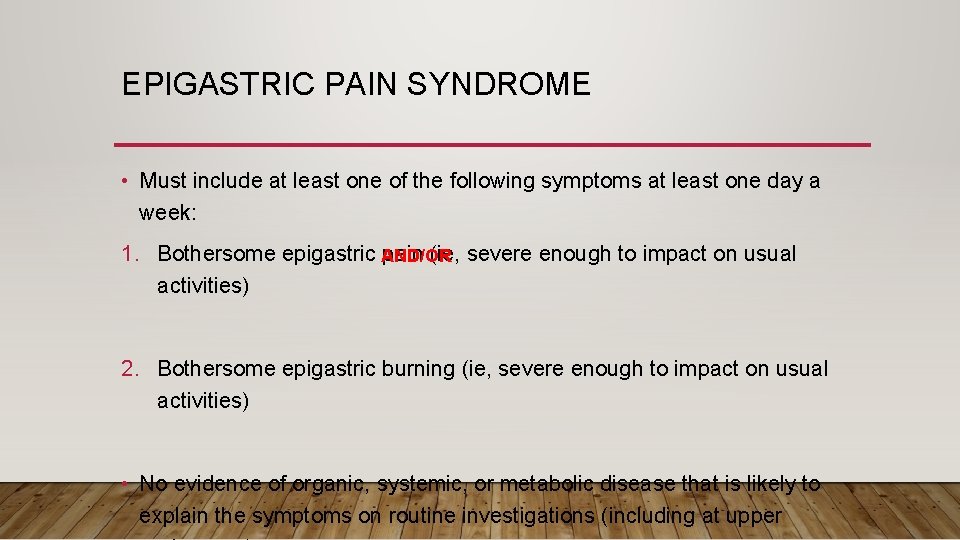
EPIGASTRIC PAIN SYNDROME • Must include at least one of the following symptoms at least one day a week: 1. Bothersome epigastric pain (ie, severe enough to impact on usual AND/OR activities) 2. Bothersome epigastric burning (ie, severe enough to impact on usual activities) • No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms on routine investigations (including at upper

DIFFERENTIAL DIAGNOSIS • PUD • GERD – Can coexist, burning vs epigastric pain and fullness • Gastroparesis – slow gastric emptying but vomiting is the predominant symptom • IBS – 40% overlap, abdominal pain + change in stool form/frequency • Medications (e. g. NSAIDS) • Gastric malignancy
APPROACH
MANAGEMENT • Helicobacter pylori test and treat • Proton pump inhibitors: if negative for H. pylori and those with persistent symptoms four weeks after eradication of H. pylori - Trial for 8 weeks - twice daily PPIs are no better than once daily PPIs for the treatment of functional dyspepsia - H 2 receptor antagonists: better than placebo but the effect in treating FB is small
MANAGEMENT • Antidepressants - If symptoms don’t improve after 8 weeks of PPI trial we stop it and start a TCA - For patients with a partial clinical response to a PPI, a tricyclic antidepressant can be initiated as combination therapy.
MANAGEMENT • Prokinetic agents - Reserved for when otherapies have failed - Limit their duration to four weeks - If symptoms recur, we repeat a course of therapy - Metoclopramide and domperidone - Serious side effects with long-term use and have limited worldwide availability • Psychological therapy (CBT)
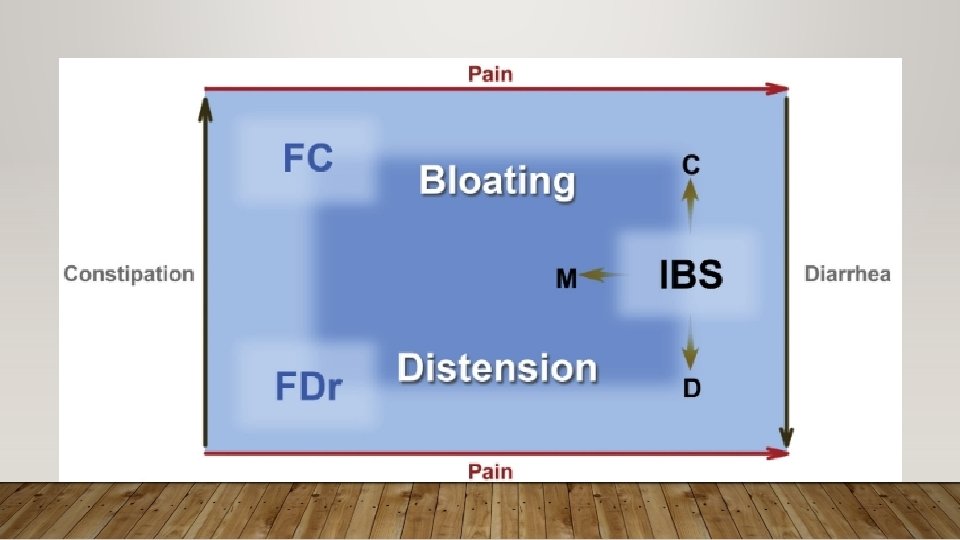
IRRITABLE BOWEL SYNDROME • Functional disorder of the gastrointestinal tract characterized by chronic abdominal pain and altered bowel habits in the absence of any organic cause • Only a small percentage of those affected seek medical attention • The estimated prevalence of IBS globally is approximately 11% with a higher prevalence in younger individuals and in women. • The most common cause of gastrointestinal referral and accounts for frequent absenteeism from work and impaired quality of life
PATHOPHYSIOLOGY • The pathophysiology of IBS remains uncertain. • It is viewed as a disorder resulting from an interaction among a number of factors. • Despite multiple investigations, data have been conflicting and no abnormality has been found to be specific for this disorder.
PATHOPHYSIOLOGY • GASTROINTESTINAL MOTILITY • VISCERAL HYPERSENSITIVITY • INTESTINAL INFLAMMATION • POSTINFECTIOUS (malabsorption, ↑ lymphocytes, antibiotic use) • BACTERIAL OVERGROWTH • GENETICS • PSYCHOSOCIAL DYSFUNCTION
ASSOCIATED CONDITIONS • IBS is associated with other conditions including: - Fibromyalgia - Chronic fatigue syndrome (also known as systemic exertion intolerance disease) - Gastroesophageal reflux disease, - Functional dyspepsia, - Non-cardiac chest pain, - Psychiatric disorders including major depression, anxiety, and somatization
CLINICAL MANIFESTATIONS • Chronic abdominal pain - usually described as a cramping sensation - The location and character of the pain can vary widely - The pain is frequently related to defecation. (relieved/worse) • Diarrhea • Constipation
CLINICAL MANIFESTATIONS • Approximately one-half of all patients with IBS complain of mucus discharge with stools • Large volume diarrhea, bloody stools, nocturnal diarrhea, and greasy stools are not associated with IBS. • Patients may also experience tenesmus even when the rectum is empty.
DIAGNOSIS • IBS should be suspected in patients with chronic abdominal pain and altered bowel habits • A clinical diagnosis of IBS requires the fulfillment of symptom-based diagnostic criteria and a limited evaluation to exclude underlying organic disease • We perform a thorough history with particular attention to the symptoms that are concerning for organic disease. • The physical examination is usually normal in patients with IBS. However, patients may have mild abdominal tenderness to palpation. • Laboratory testing to exclude other diagnoses (CBC, fecal calprotectin)
ROME IV CRITERIA • Recurrent abdominal pain, on average, at least one day per week in the last three months* • Associated with two or more of the following: a. Related to defecation b. change in stool frequency c. change in stool form (appearance) * Criteria fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis.
ADDITIONAL TESTING • In patients who meet diagnostic criteria for IBS and have no alarm features, we do not routinely perform any additional testing beyond the initial evaluation. • In patients with alarm features, we perform additional evaluation to exclude other causes of similar symptoms. The diagnostic evaluation is based on the clinical presentation and usually includes endoscopic evaluation in all patients and imaging in selected cases.
ALARM FEATURES • Age of onset after age 50 years • Rectal bleeding or melena • Nocturnal diarrhea • Progressive abdominal pain • Unexplained weight loss • Laboratory abnormalities (iron deficiency anemia, elevated Creactive protein or fecal calprotectin) • Family history of IBD or colorectal cancer
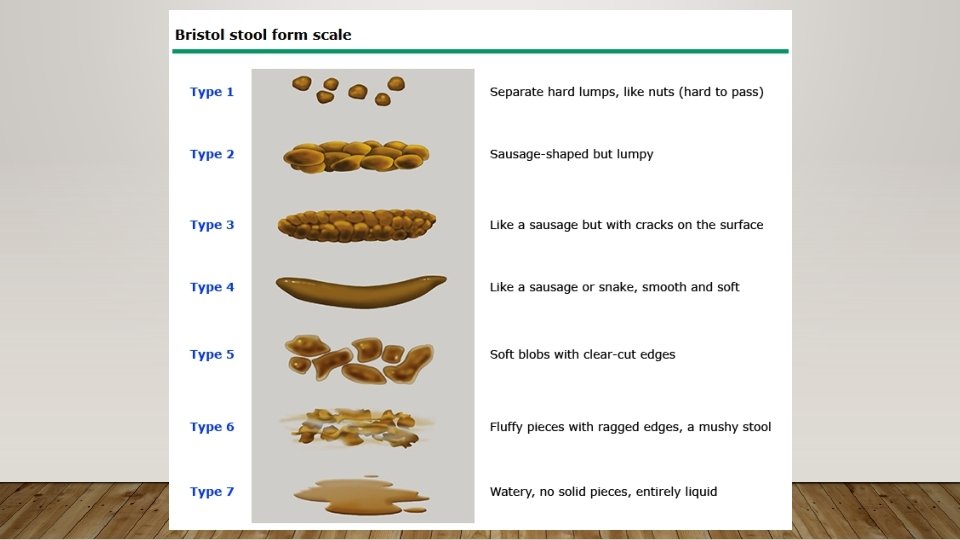
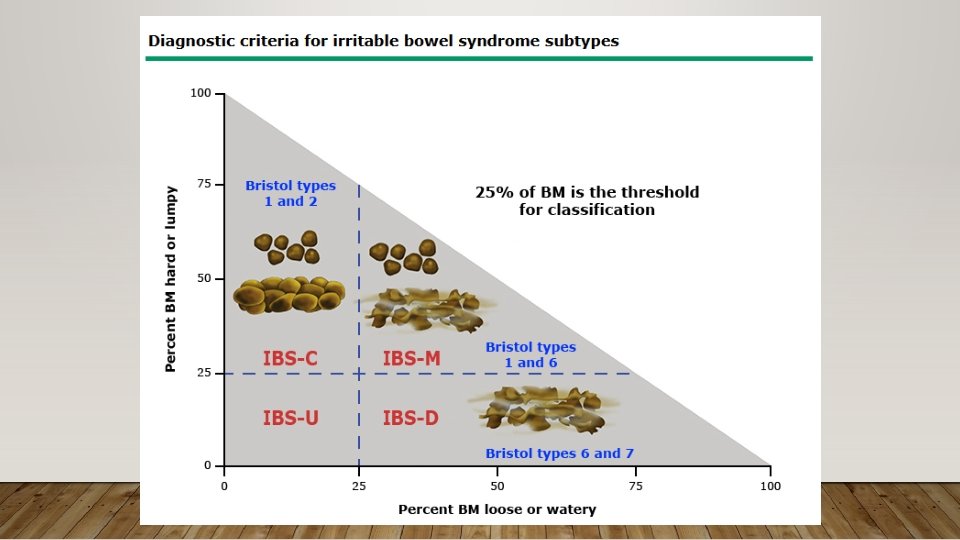
IBS SUBTYPES • Subtypes of IBS are recognized based on the patient's reported predominant bowel habit on days with abnormal bowel movements • The Bristol stool form scale (BSFS) should be used to record stool consistency • Subtypes can only confidently be established when the patient is evaluated off medications used to treat bowel habit abnormalities
IBS SUBTYPES • IBS with predominant constipation: Patient reports that abnormal bowel movements are usually constipation (type 1 and 2 in the BSFS) • IBS with predominant diarrhea: Patient reports that abnormal bowel movements are usually diarrhea (type 6 and 7 in the BSFS) • IBS with mixed bowel habits: Patient reports that abnormal bowel movements are usually both constipation and diarrhea (more than 25% of all the abnormal bowel movements were constipation and more than 25% were diarrhea) • IBS unclassified: Patients who meet diagnostic criteria for IBS but cannot be accurately categorized into one of the other three subtypes.
DIFFERENTIAL DIAGNOSIS • Celiac disease • Malabsorption • Microscopic colitis • Inflammatory bowel disease
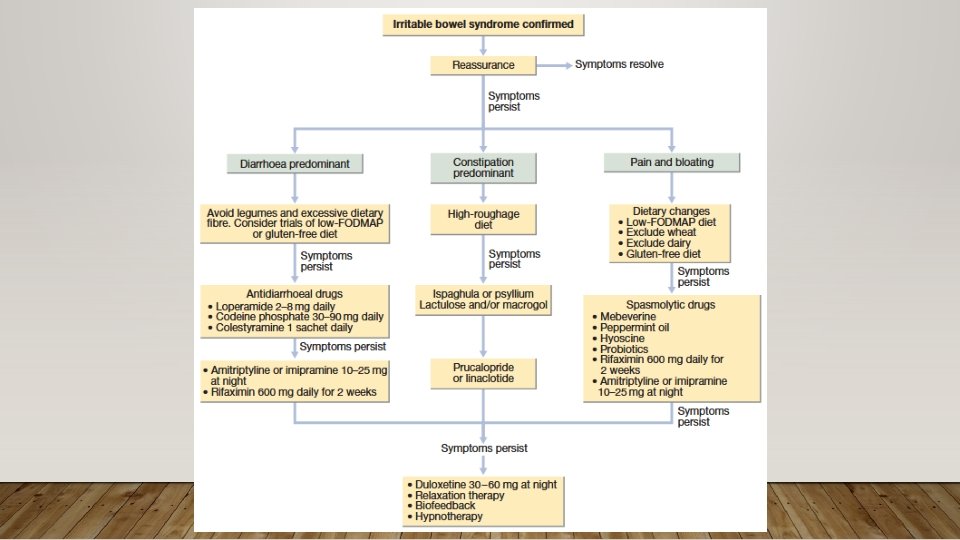
MANAGEMENT • The most important steps are to make a positive diagnosis and reassure the patient. Many people are concerned that they have developed cancer. A cycle of anxiety leading to colonic symptoms, which further heighten anxiety, can be broken by explaining that symptoms are not due to a serious underlying disease but instead are the result of behavioral, psychosocial, physiological and luminal factors.
MANAGEMENT • In patients with mild and intermittent symptoms that do not impair quality of life, we initially start with lifestyle and dietary modification alone rather than specific pharmacologic agents • (eg, exclusion of gas-producing foods; a diet low in fermentable oligo-, di-, and monosaccharides and polyols [FODMAPs]; and in select cases, lactose and gluten avoidance)
MANAGEMENT • In patients with mild to moderate symptoms who fail to respond to lifestyle and dietary modification and in patients with moderate to severe symptoms of IBS that affect quality of life, we use pharmacologic therapy as adjunctive treatment. • Since IBS presents as a complex of symptoms, pharmacologic treatment should be based on the predominant symptom
FUNCTIONAL DIARRHEA – ROME IV • Loose or watery stools, without predominant abdominal pain or bothersome bloating, occurring in >25% of stools. • Criterion fulfilled for the last 3 months with symptom onset at least 6 months before diagnosis • Patients meeting criteria for diarrhea-predominant IBS should be excluded
PATHOPHYSIOLOGY • Multifactorial • Altered GI motility, brain-gut disturbances, environmental factors, prior infections, and psychosocial factors • Genetic studies in FDr patients have not been performed • Similar to IBS, a prior infection can lead to post-infectious FDr.
FUNCTIONAL DIARRHEA • Chronic diarrhea without pain is caused by many diseases indistinguishable by history from functional diarrhea. • Features atypical for a functional disorder (e. g. large-volume stools, rectal bleeding, nutritional deficiency and weight loss) call for more extensive investigations • Treatment of functional diarrhea is with loperamide often combined with a tricyclic antidepressant prescribed at night
FUNCTIONAL CONSTIPATION 1. Must include 2 or more of the following: a. Straining during more than one-fourth (25%) of defecations b. Lumpy or hard stools (BSFS 1 -2) in more than one-fourth (25%) of defecations c. Sensation of incomplete evacuation more than one-fourth (25%) of defecations d. Sensation of anorectal obstruction/blockage more than one-fourth (25%) of defecations e. Manual maneuvers to facilitate more than one-fourth (25%) of defecations (eg, digital evacuation, support of the pelvic floor) f. Fewer than 3 spontaneous bowel movements per week
FUNCTIONAL CONSTIPATION 2. Loose stools are rarely present without the use of laxatives 3. Insufficient criteria for irritable bowel syndrome *Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis.
FUNCTIONAL CONSTIPATION • The diagnosis of FC should be made using the following 4 key features: - Clinical history - Physical examination (CNS, abdominal, rectal), - Minimal laboratory tests (CBC, TSH, Ca) - Colonoscopy or other tests (if clinically indicated and available)
MANAGEMENT • Begin by educating the patient about FC • The patient should maintain a diet that contains an adequate amount of fiber, scheduling routine bathroom time after the morning or evening meal, and elevating the feet with a foot stool or using a toilet that is lower to the ground. • If symptoms persist, empiric therapy can be initiated in the absence of warning signs
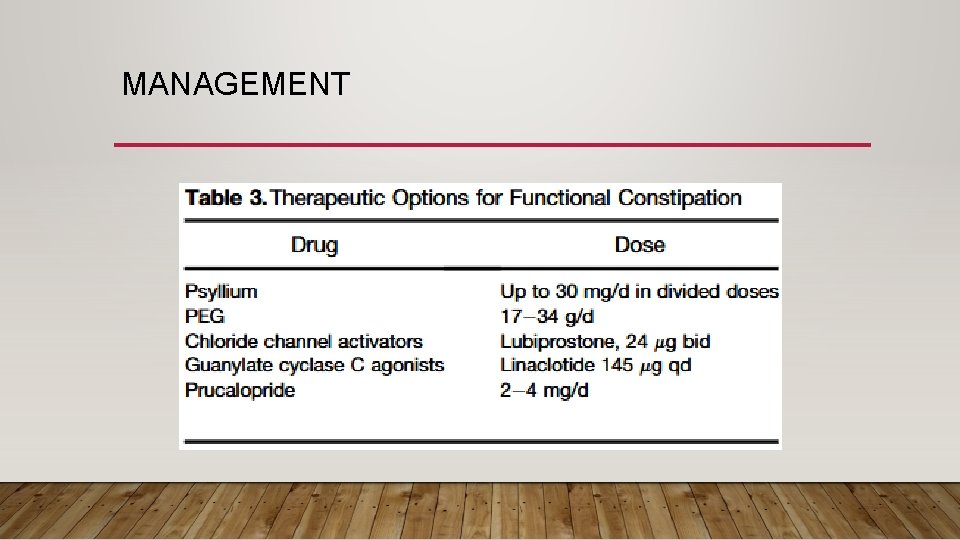
MANAGEMENT

THANK YOU
- Slides: 56