Functional Components of Peripheral Nerves Spinal Nerves General

- Slides: 46

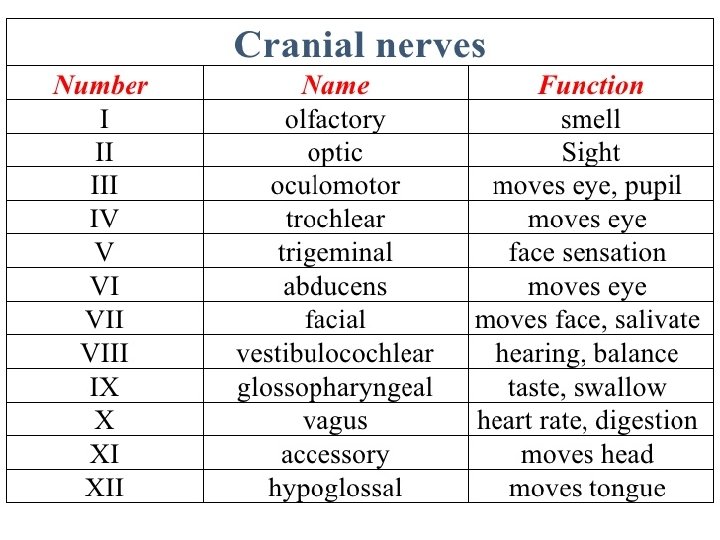
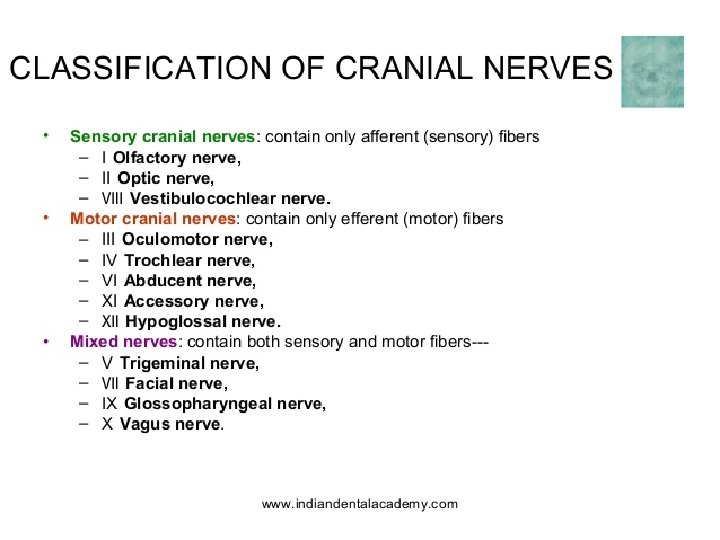
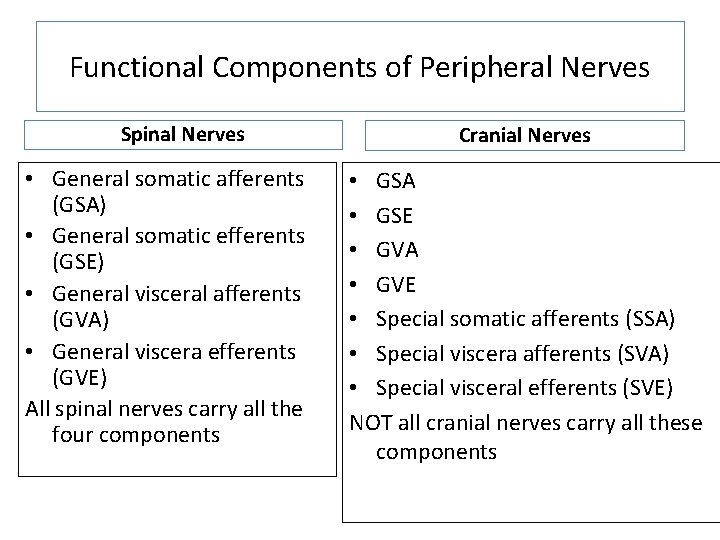
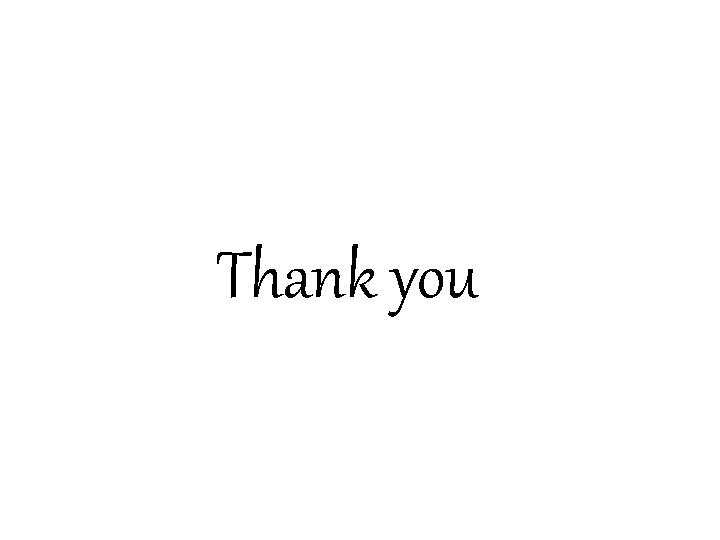
Functional Components of Peripheral Nerves Spinal Nerves • General somatic afferents (GSA) • General somatic efferents (GSE) • General visceral afferents (GVA) • General viscera efferents (GVE) All spinal nerves carry all the four components Cranial Nerves • GSA • GSE • GVA • GVE • Special somatic afferents (SSA) • Special viscera afferents (SVA) • Special visceral efferents (SVE) NOT all cranial nerves carry all these components
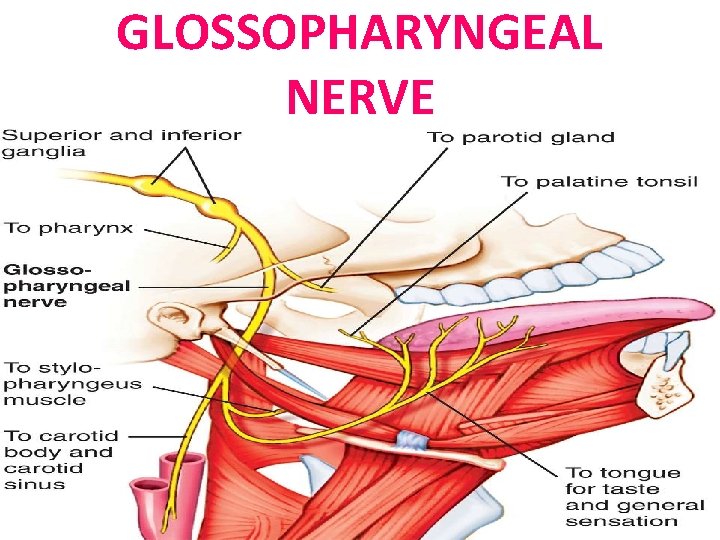
GLOSSOPHARYNGEAL NERVE
Objectives • By the end of the lecture, the student will be able to: • Define the deep origin of Glossopharyngeal Nerves. • Locate the exit of nerve from the brain stem. • Describe the course and distribution of nerve • List the branches of nerves.
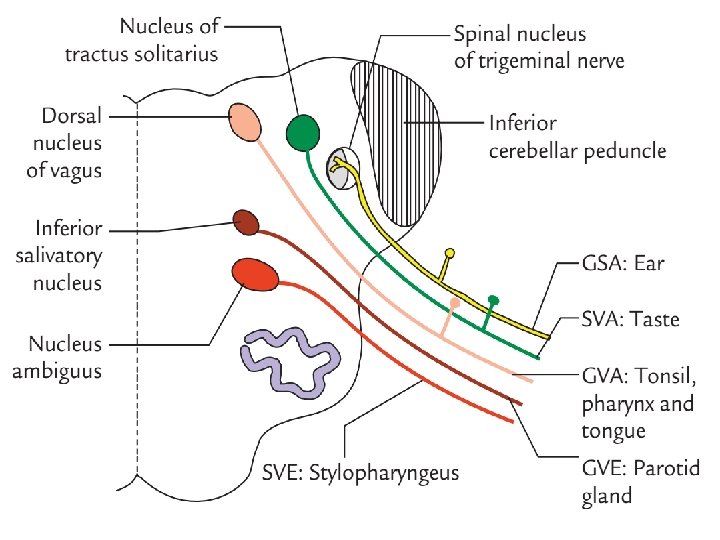
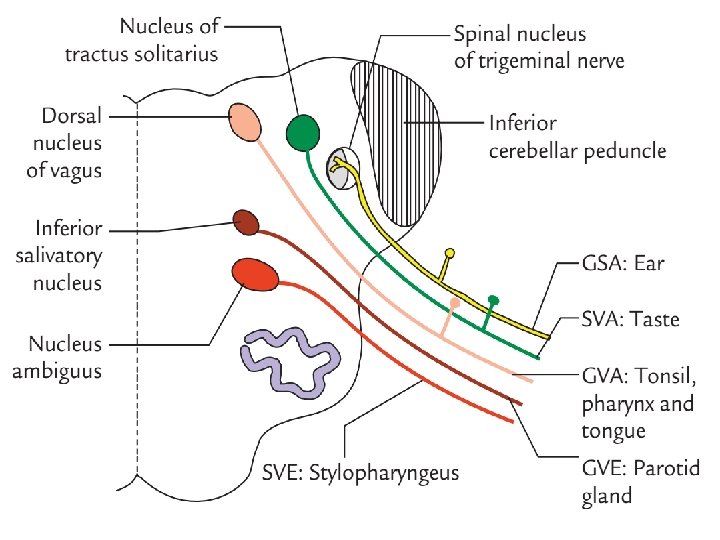
GLOSSOPHARYNGEAL NERVE • It is principally a sensory nerve with preganglionic parasympathetic and few motor fibers. • It has no real nucleus to itself Instead it shares nuclei with VII and X. • The sensory information goes to the solitary nucleus. • The motor fibers; innervations of the stylopharyngeus muscle, comes from the nucleus ambiguus. • The parasympathetic fibers innervate the salivary glands, comes from the inferior salivatory nucleus
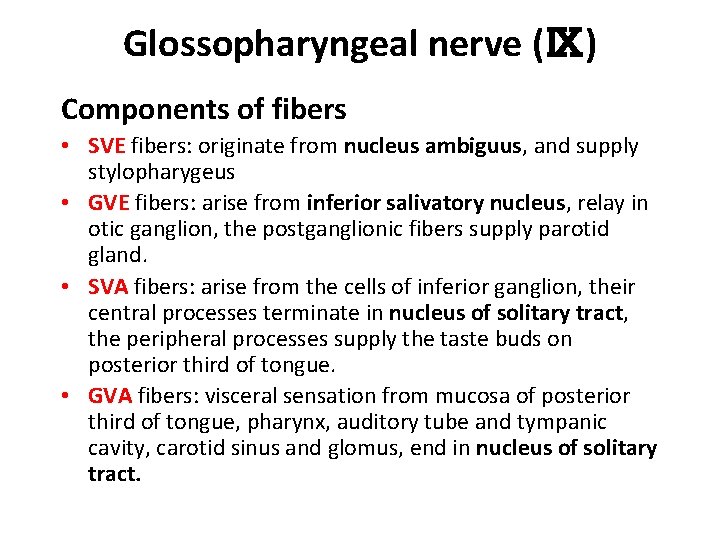
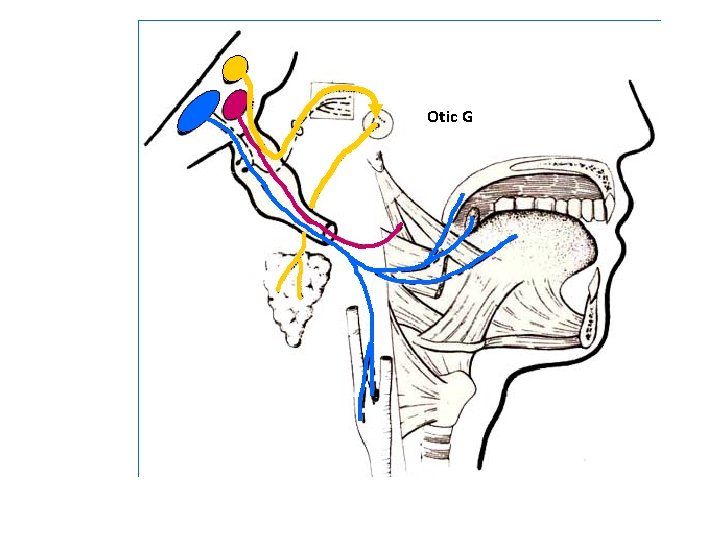
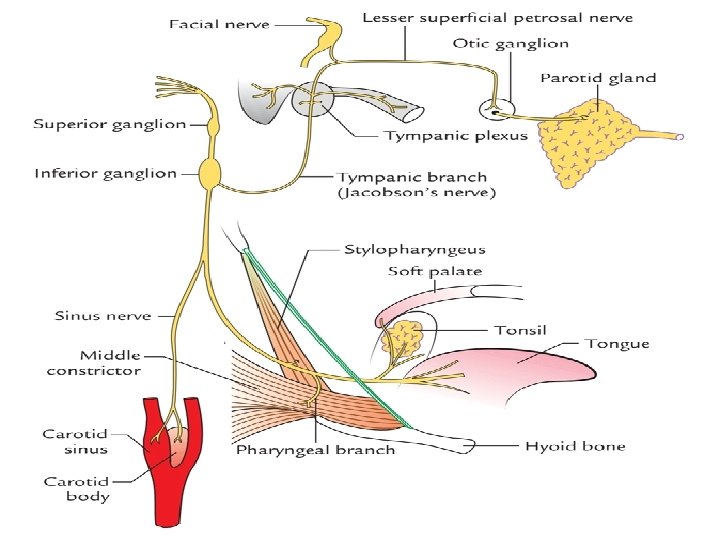
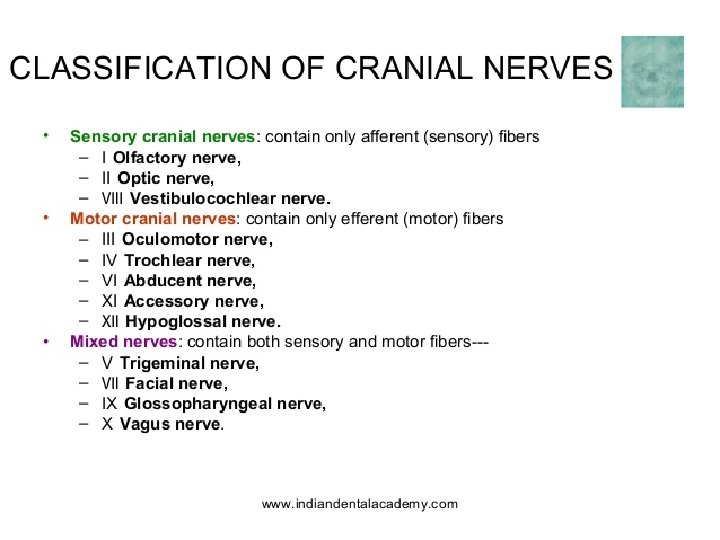
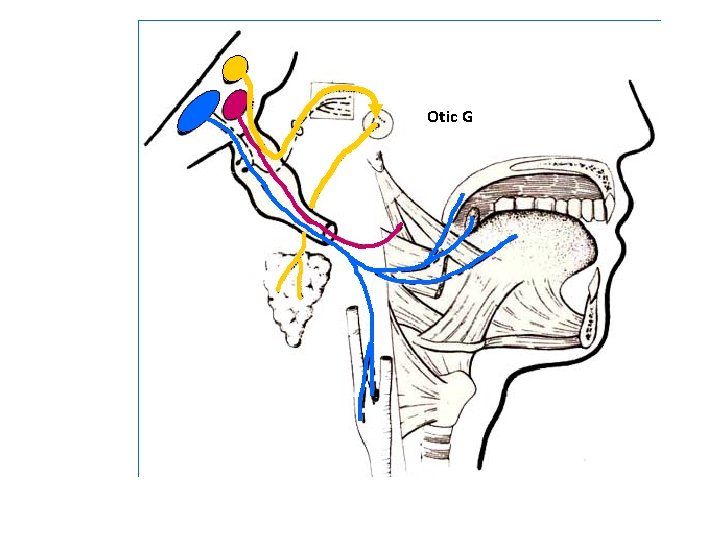
Glossopharyngeal nerve (Ⅸ) Components of fibers • SVE fibers: originate from nucleus ambiguus, and supply stylopharygeus • GVE fibers: arise from inferior salivatory nucleus, relay in otic ganglion, the postganglionic fibers supply parotid gland. • SVA fibers: arise from the cells of inferior ganglion, their central processes terminate in nucleus of solitary tract, the peripheral processes supply the taste buds on posterior third of tongue. • GVA fibers: visceral sensation from mucosa of posterior third of tongue, pharynx, auditory tube and tympanic cavity, carotid sinus and glomus, end in nucleus of solitary tract.
Otic G
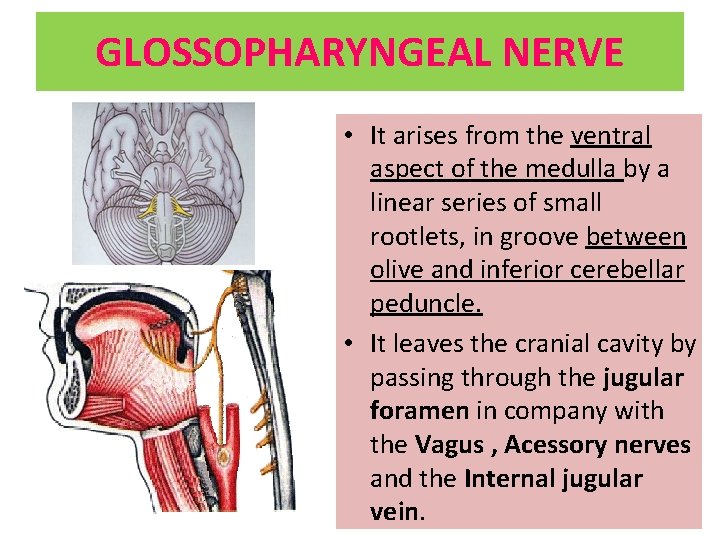
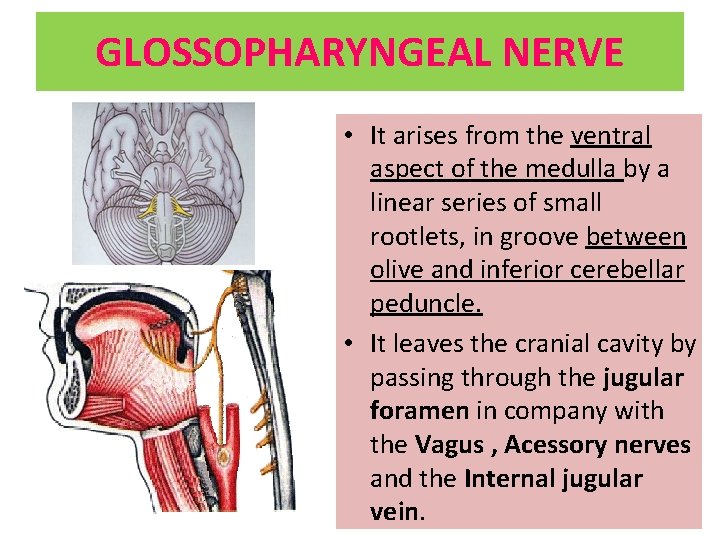
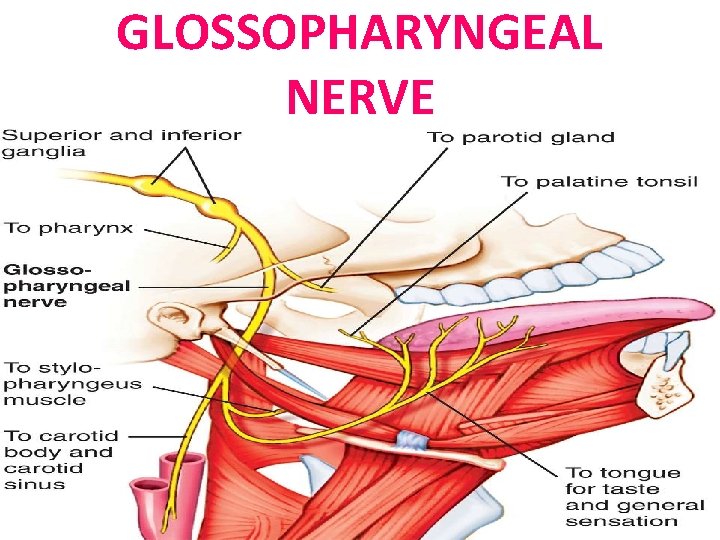
GLOSSOPHARYNGEAL NERVE • It arises from the ventral aspect of the medulla by a linear series of small rootlets, in groove between olive and inferior cerebellar peduncle. • It leaves the cranial cavity by passing through the jugular foramen in company with the Vagus , Acessory nerves and the Internal jugular vein.
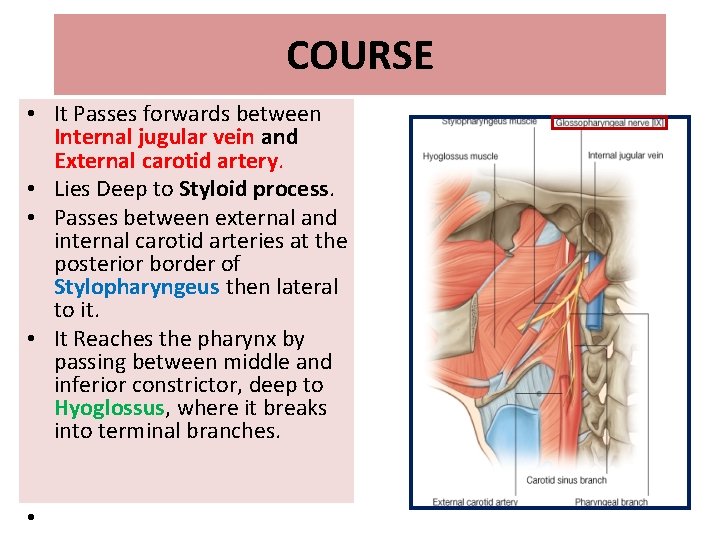
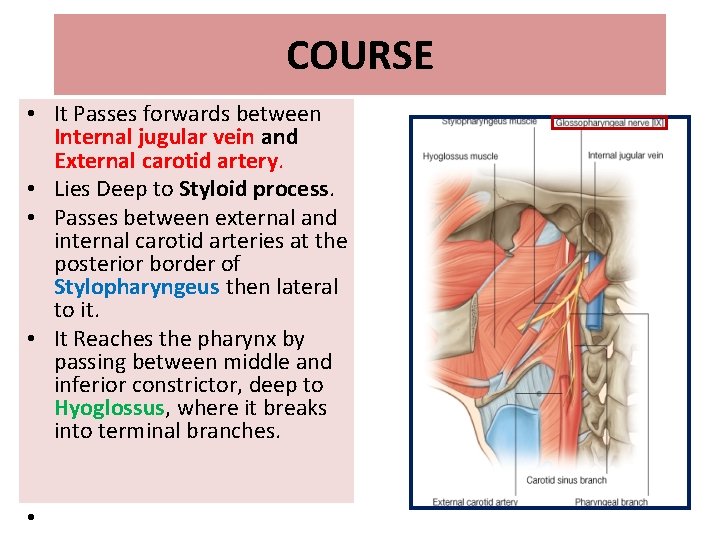
COURSE • It Passes forwards between Internal jugular vein and External carotid artery. • Lies Deep to Styloid process. • Passes between external and internal carotid arteries at the posterior border of Stylopharyngeus then lateral to it. • It Reaches the pharynx by passing between middle and inferior constrictor, deep to Hyoglossus, where it breaks into terminal branches. •
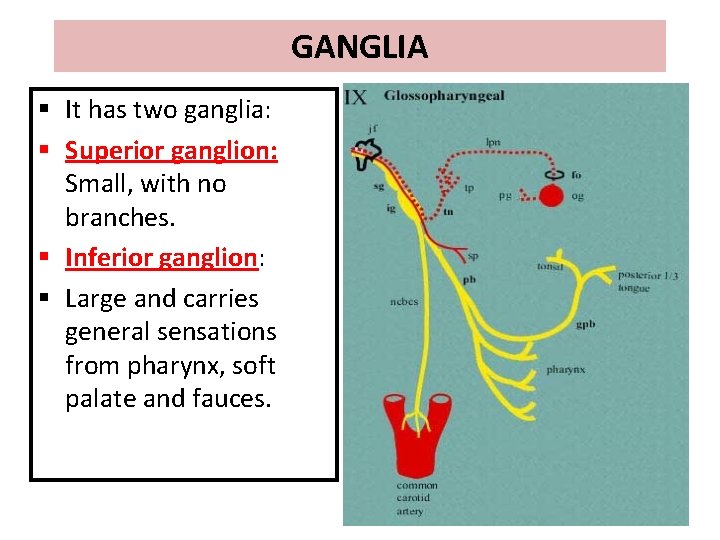
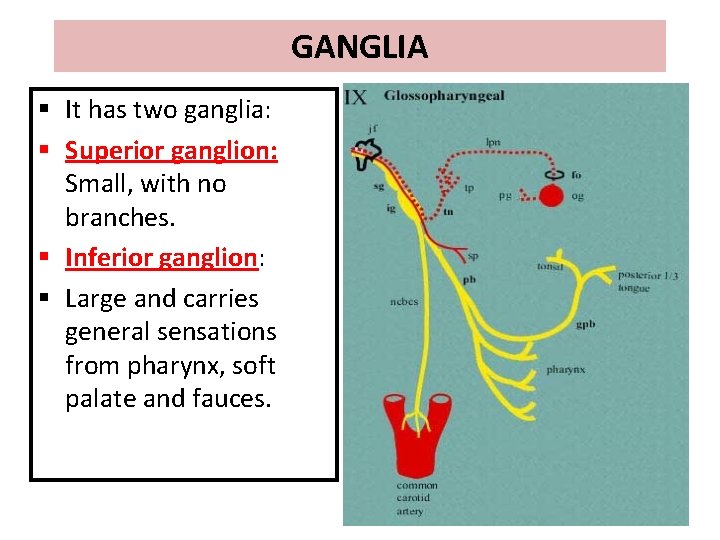
GANGLIA § It has two ganglia: § Superior ganglion: Small, with no branches. § Inferior ganglion: § Large and carries general sensations from pharynx, soft palate and fauces.
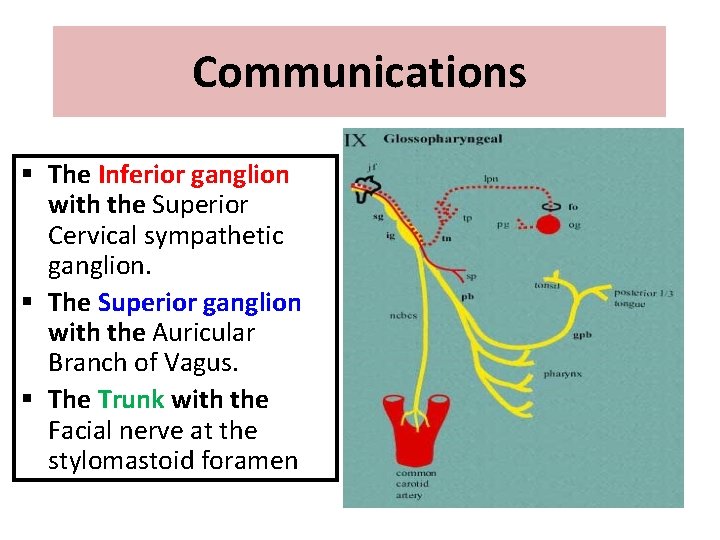
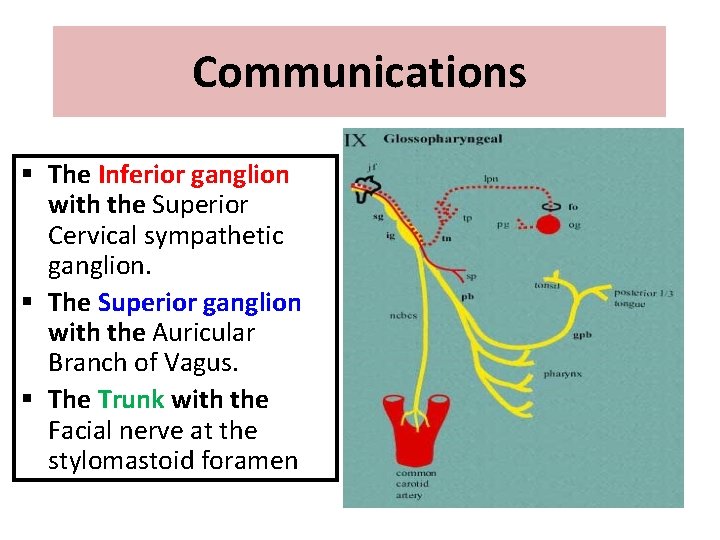
Communications § The Inferior ganglion with the Superior Cervical sympathetic ganglion. § The Superior ganglion with the Auricular Branch of Vagus. § The Trunk with the Facial nerve at the stylomastoid foramen
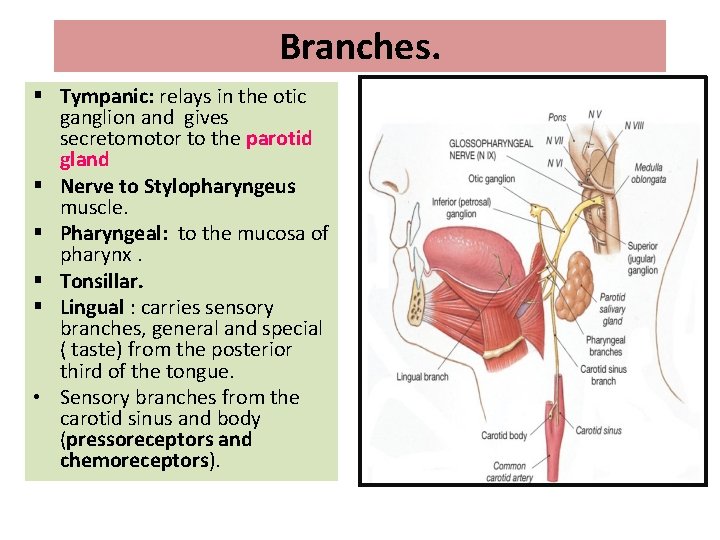
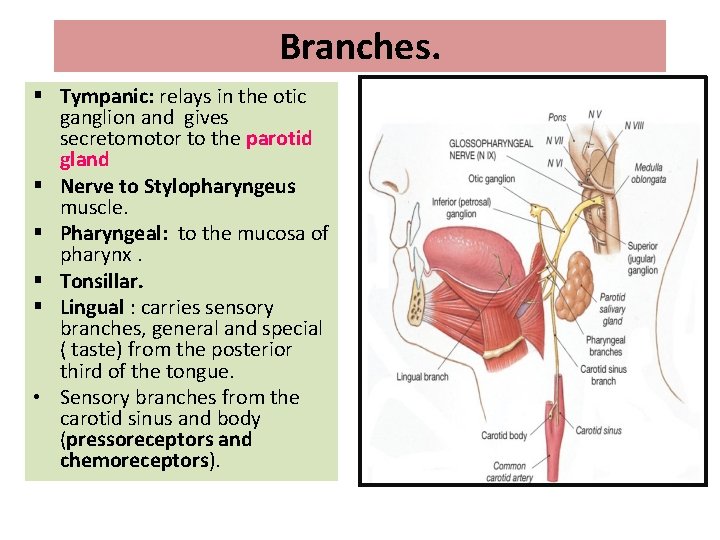
Branches. § Tympanic: relays in the otic ganglion and gives secretomotor to the parotid gland § Nerve to Stylopharyngeus muscle. § Pharyngeal: to the mucosa of pharynx. § Tonsillar. § Lingual : carries sensory branches, general and special ( taste) from the posterior third of the tongue. • Sensory branches from the carotid sinus and body (pressoreceptors and chemoreceptors).
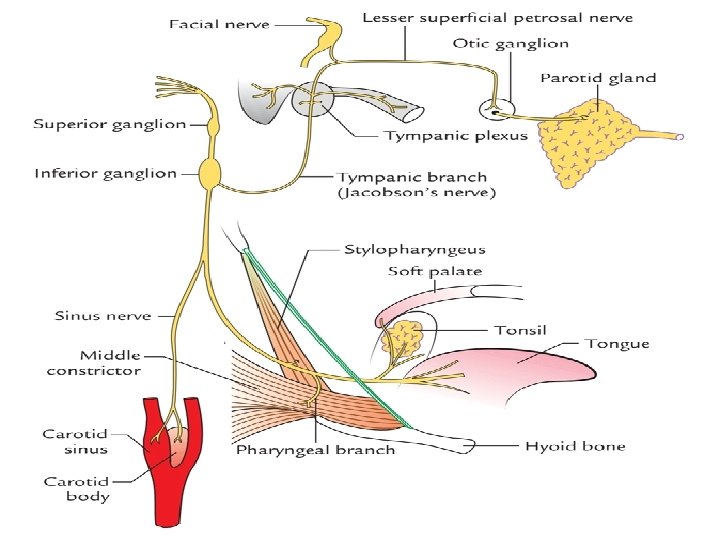
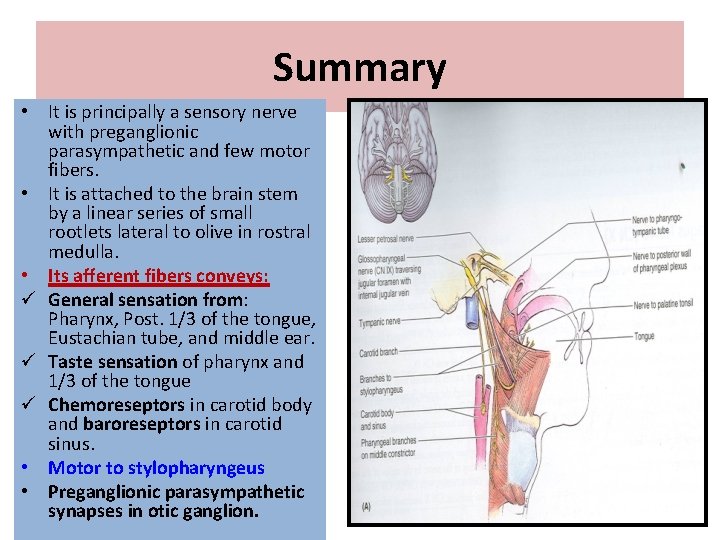
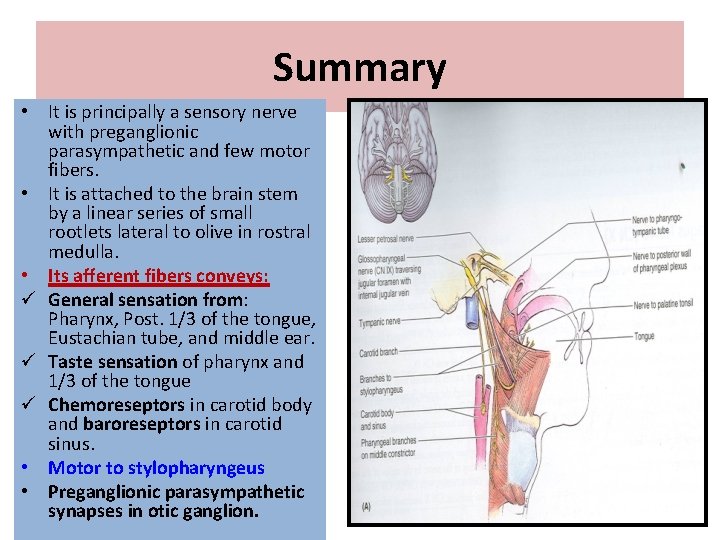
Summary • It is principally a sensory nerve with preganglionic parasympathetic and few motor fibers. • It is attached to the brain stem by a linear series of small rootlets lateral to olive in rostral medulla. • Its afferent fibers conveys: ü General sensation from: Pharynx, Post. 1/3 of the tongue, Eustachian tube, and middle ear. ü Taste sensation of pharynx and 1/3 of the tongue ü Chemoreseptors in carotid body and baroreseptors in carotid sinus. • Motor to stylopharyngeus • Preganglionic parasympathetic synapses in otic ganglion.
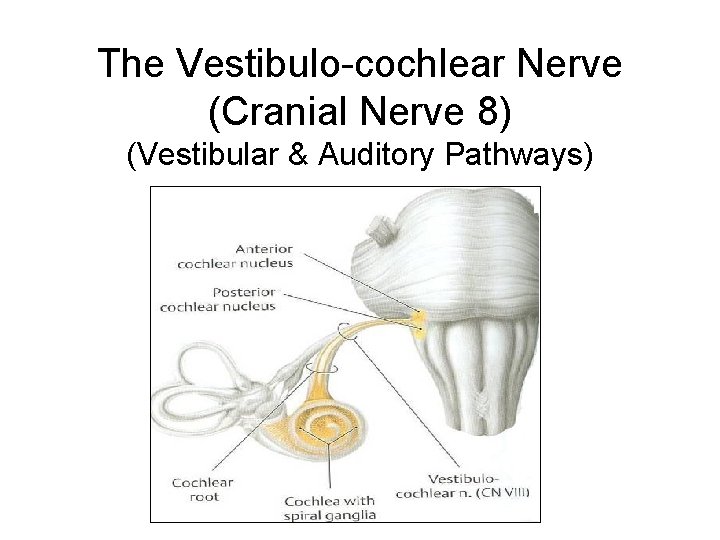
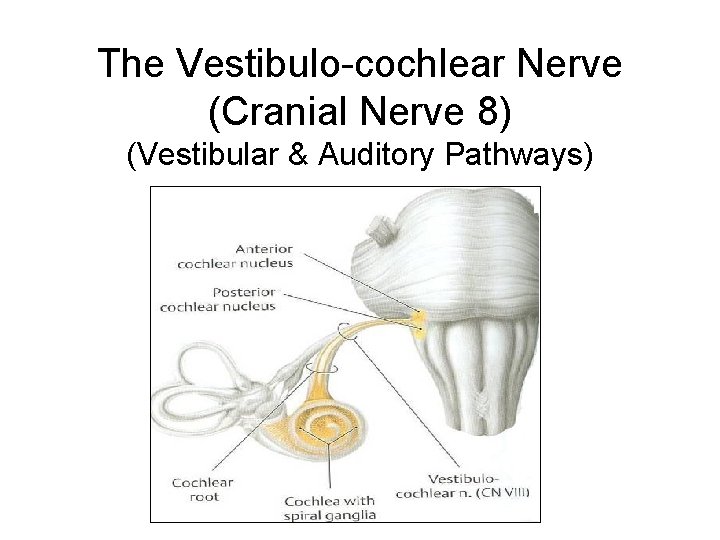
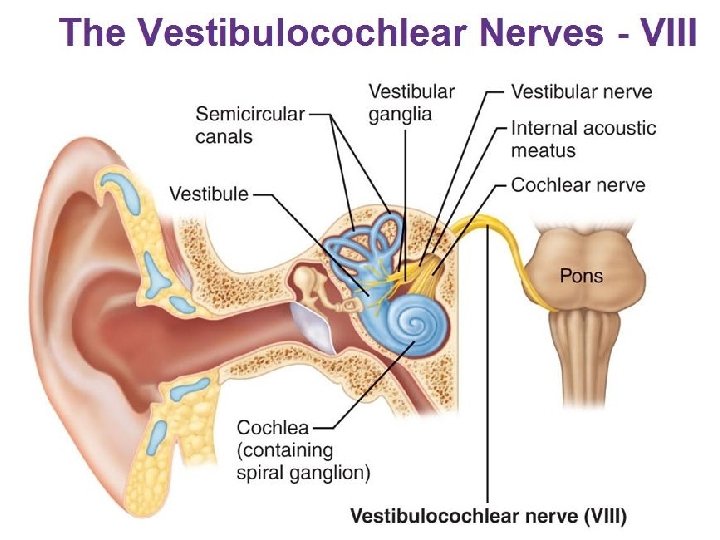
The Vestibulo-cochlear Nerve (Cranial Nerve 8) (Vestibular & Auditory Pathways)
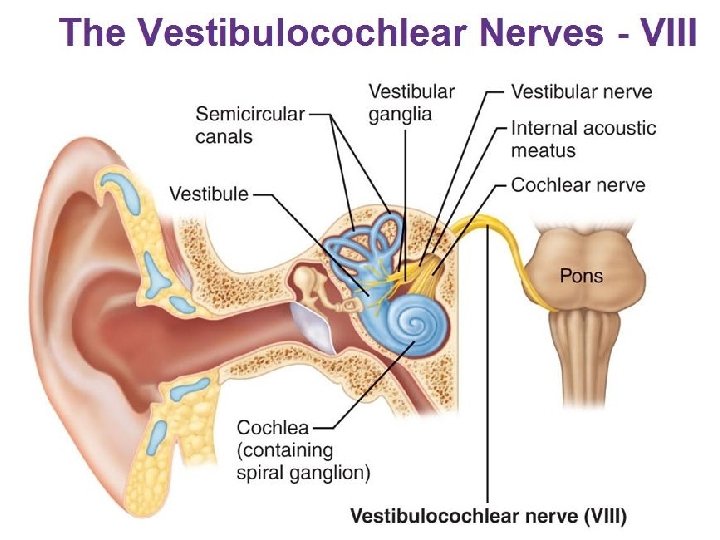
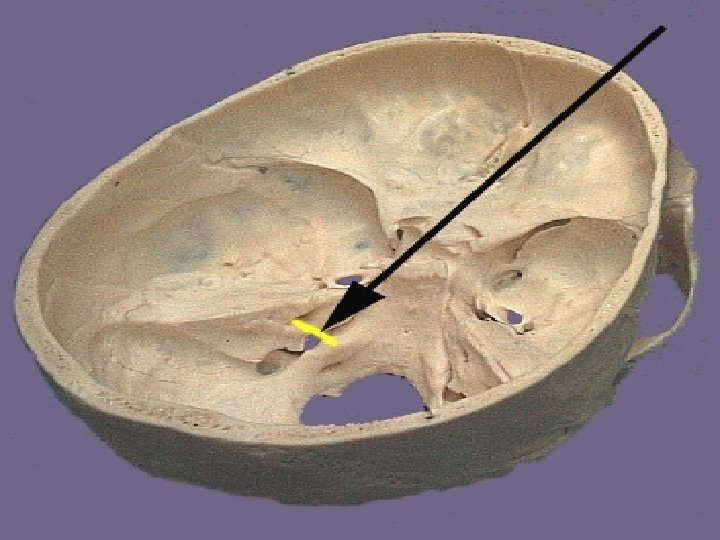
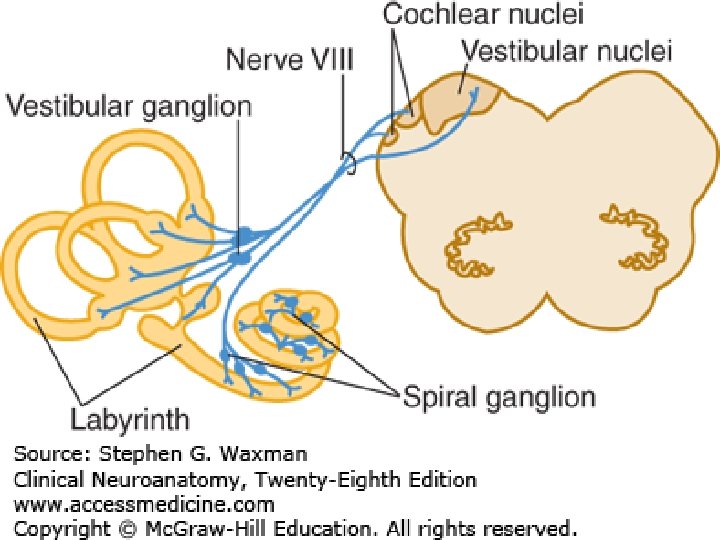
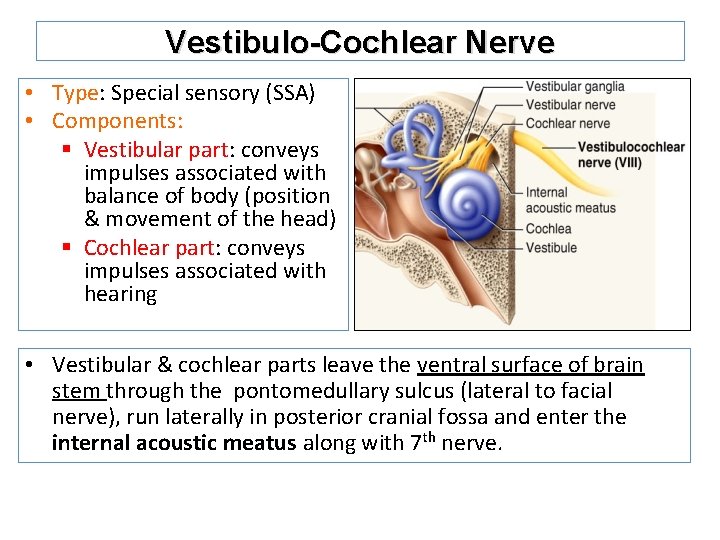
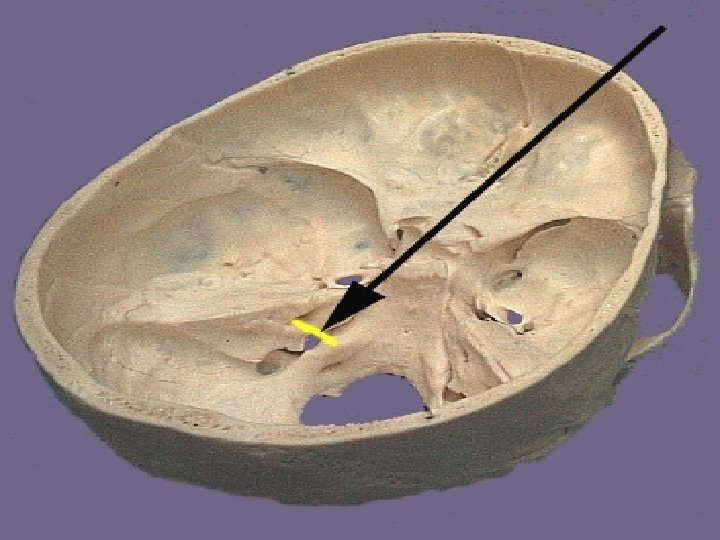
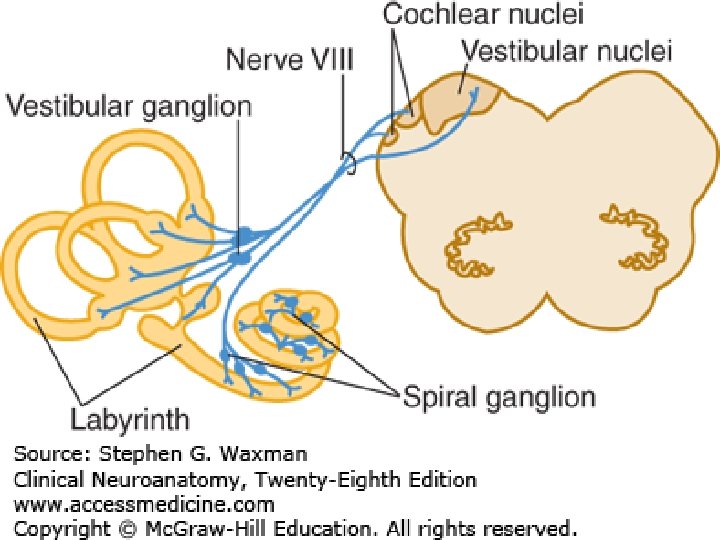
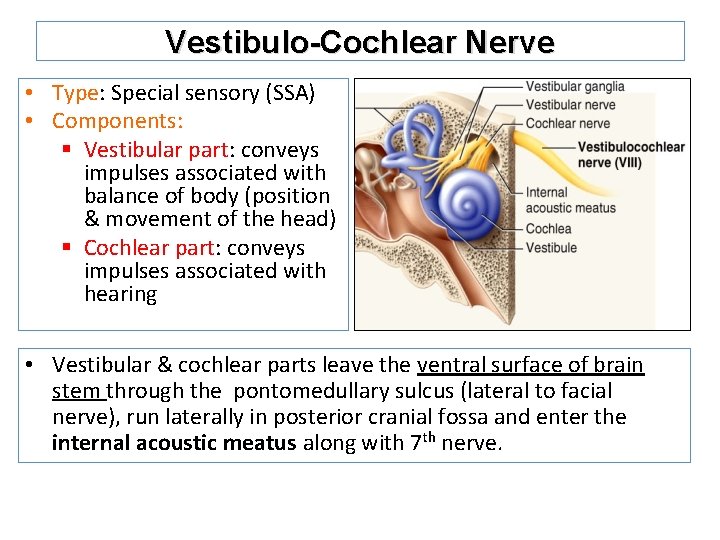
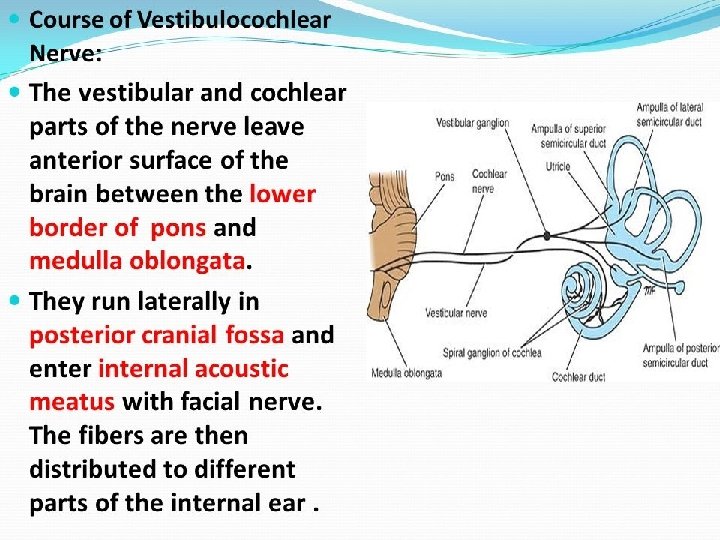
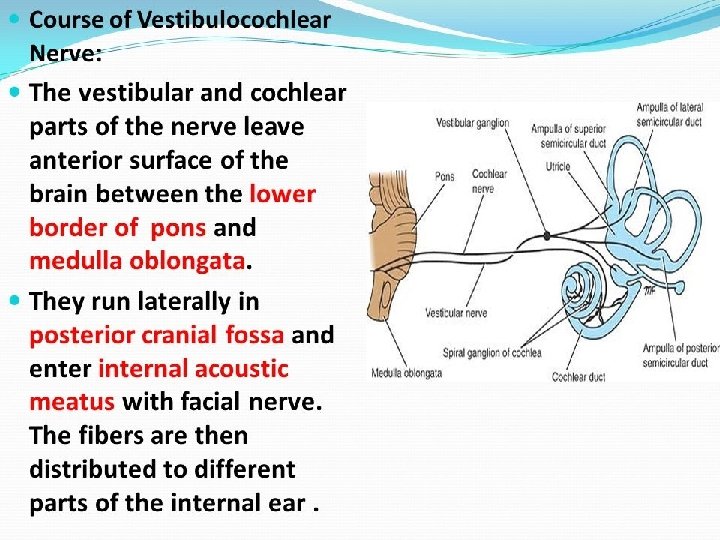
Vestibulo-Cochlear Nerve • Type: Special sensory (SSA) • Components: § Vestibular part: conveys impulses associated with balance of body (position & movement of the head) § Cochlear part: conveys impulses associated with hearing • Vestibular & cochlear parts leave the ventral surface of brain stem through the pontomedullary sulcus (lateral to facial nerve), run laterally in posterior cranial fossa and enter the internal acoustic meatus along with 7 th nerve.
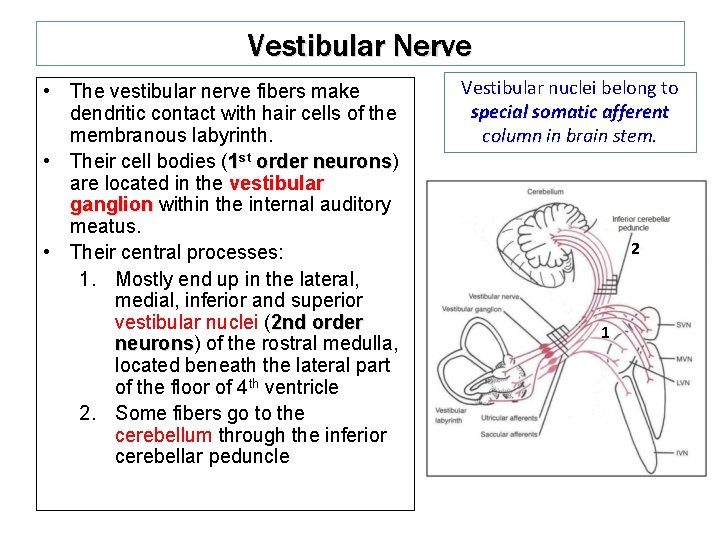
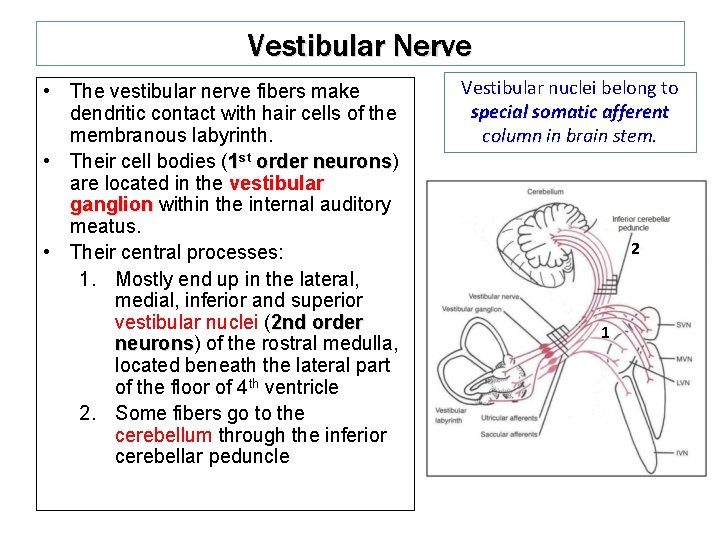
Vestibular Nerve • The vestibular nerve fibers make dendritic contact with hair cells of the membranous labyrinth. • Their cell bodies (1 st order neurons) neurons are located in the vestibular ganglion within the internal auditory meatus. • Their central processes: 1. Mostly end up in the lateral, medial, inferior and superior vestibular nuclei (2 nd order neurons) neurons of the rostral medulla, located beneath the lateral part of the floor of 4 th ventricle 2. Some fibers go to the cerebellum through the inferior cerebellar peduncle Vestibular nuclei belong to special somatic afferent column in brain stem. 2 1
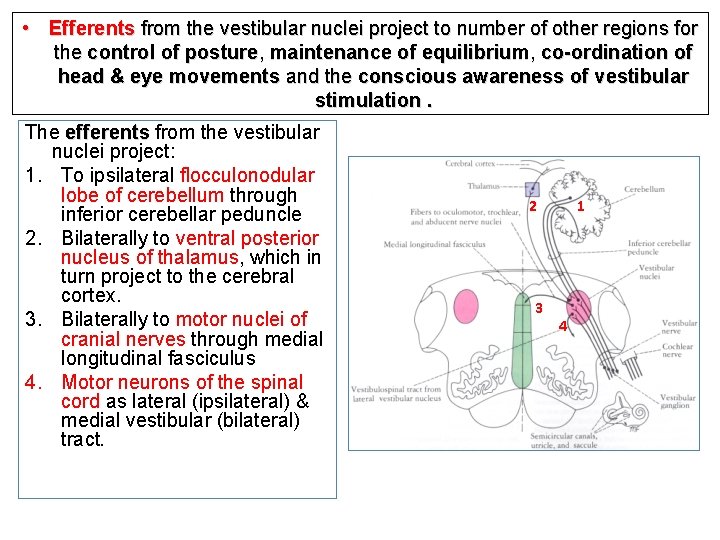
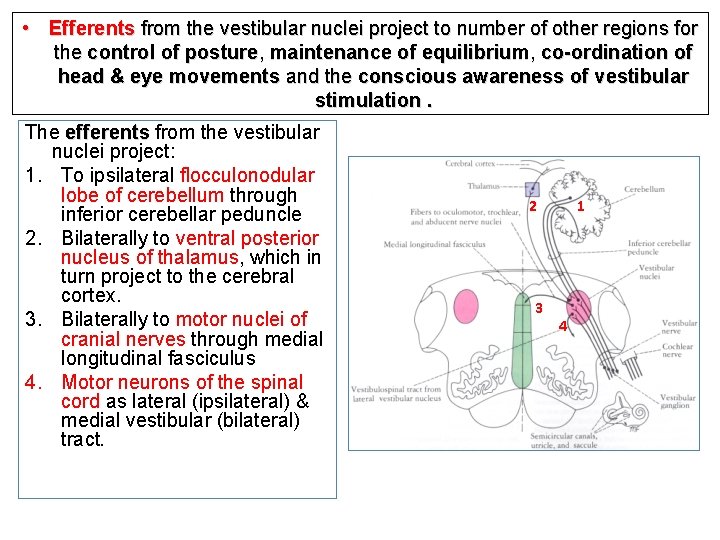
• Efferents from the vestibular nuclei project to number of other regions for the control of posture, maintenance of equilibrium, co-ordination of head & eye movements and the conscious awareness of vestibular stimulation. The efferents from the vestibular nuclei project: 1. To ipsilateral flocculonodular lobe of cerebellum through inferior cerebellar peduncle 2. Bilaterally to ventral posterior nucleus of thalamus, which in turn project to the cerebral cortex. 3. Bilaterally to motor nuclei of cranial nerves through medial longitudinal fasciculus 4. Motor neurons of the spinal cord as lateral (ipsilateral) & medial vestibular (bilateral) tract. 2 3 1 4
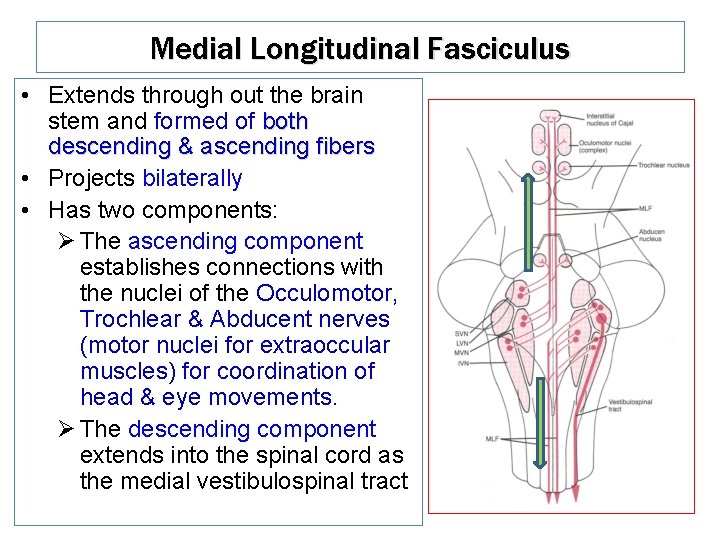
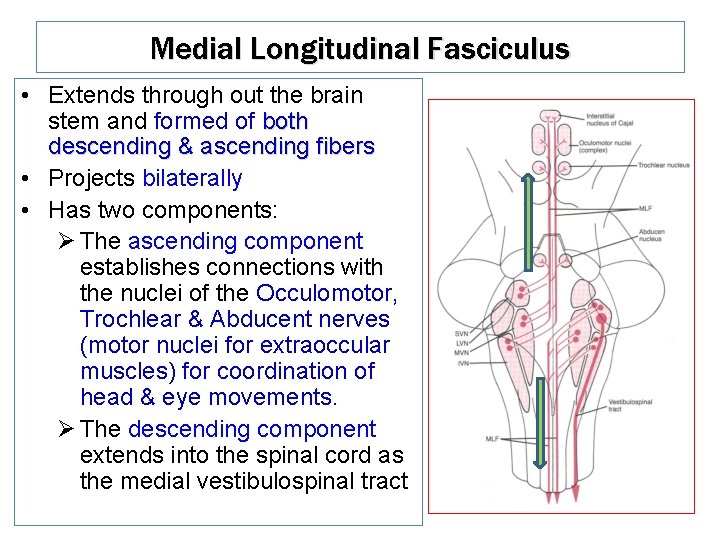
Medial Longitudinal Fasciculus • Extends through out the brain stem and formed of both descending & ascending fibers • Projects bilaterally • Has two components: Ø The ascending component establishes connections with the nuclei of the Occulomotor, Trochlear & Abducent nerves (motor nuclei for extraoccular muscles) for coordination of head & eye movements. Ø The descending component extends into the spinal cord as the medial vestibulospinal tract
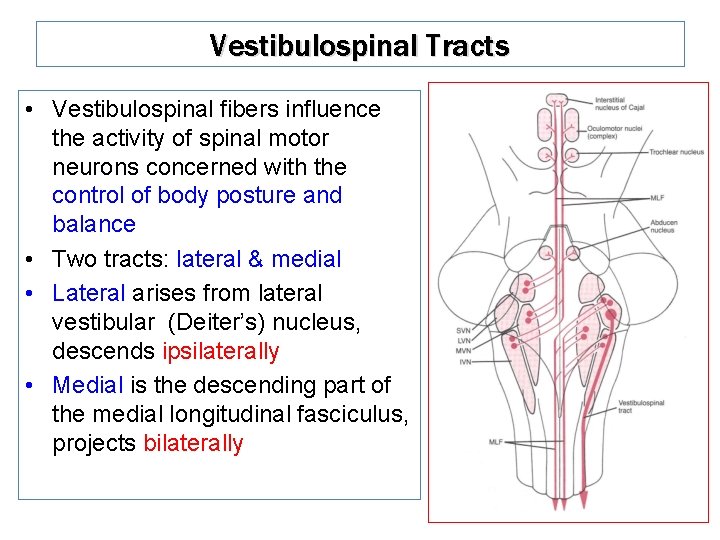
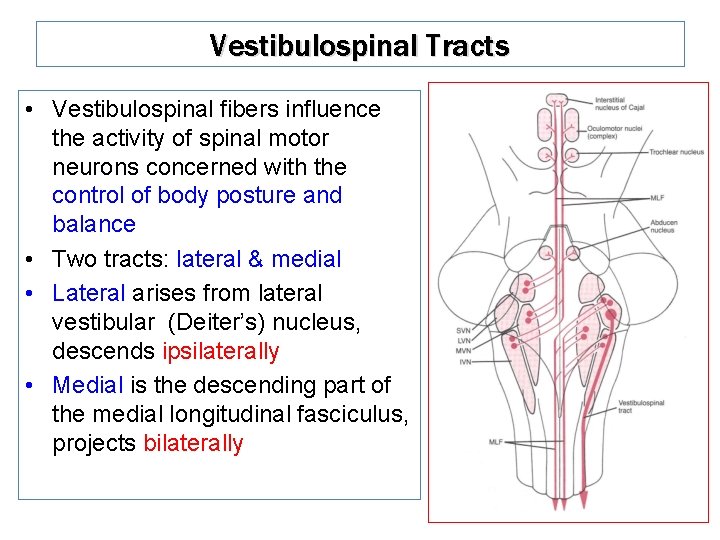
Vestibulospinal Tracts • Vestibulospinal fibers influence the activity of spinal motor neurons concerned with the control of body posture and balance • Two tracts: lateral & medial • Lateral arises from lateral vestibular (Deiter’s) nucleus, descends ipsilaterally • Medial is the descending part of the medial longitudinal fasciculus, projects bilaterally
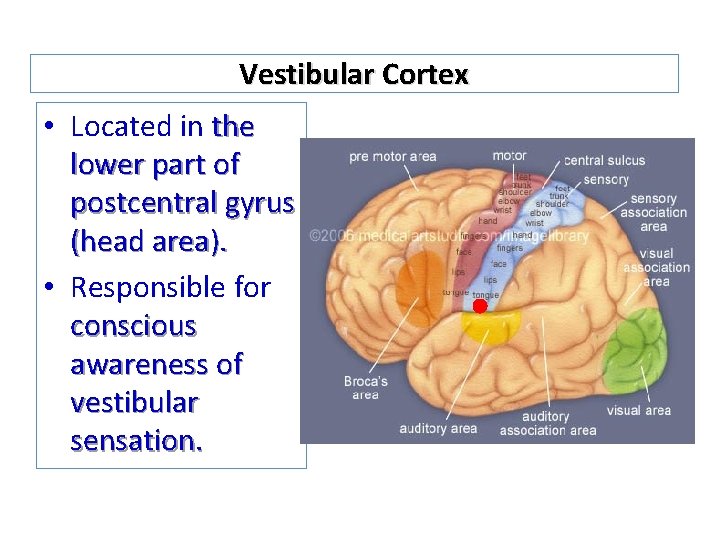
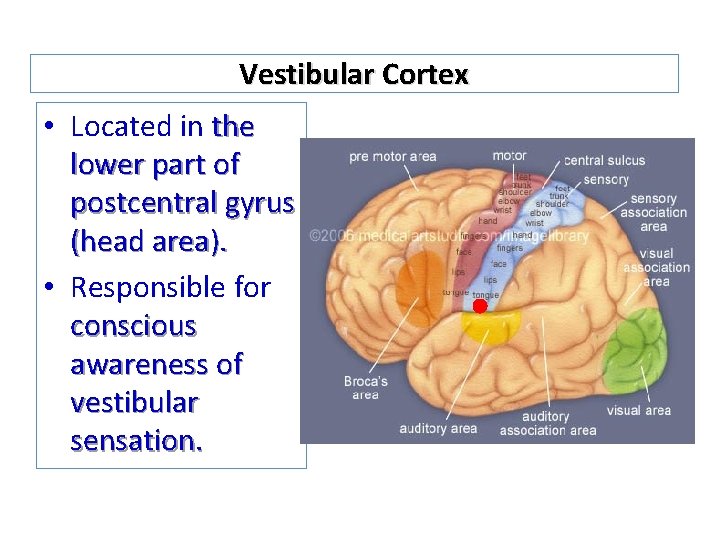
Vestibular Cortex • Located in the lower part of postcentral gyrus (head area). • Responsible for conscious awareness of vestibular sensation.
Auditory Pathway • It is a multisynaptic pathway • There are several locations between medulla and the thalamus where axons may synapse and not all the fibers behave in the same manner. • Representation of cochlea is bilateral at all levels above cochlear nuclei.
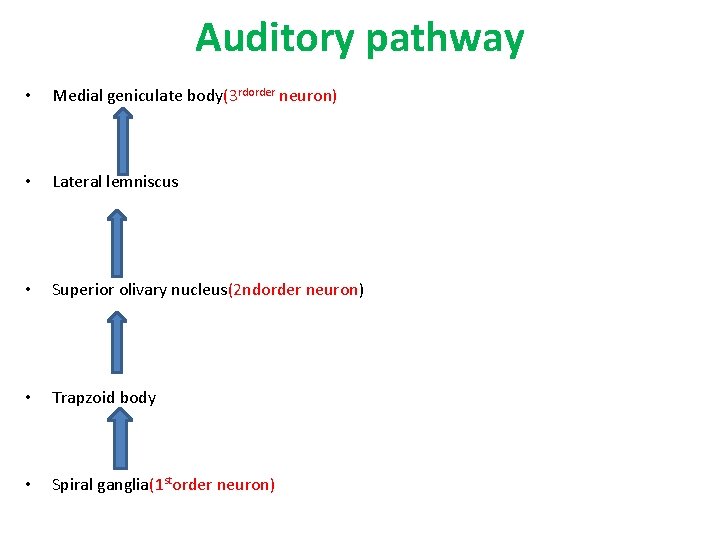
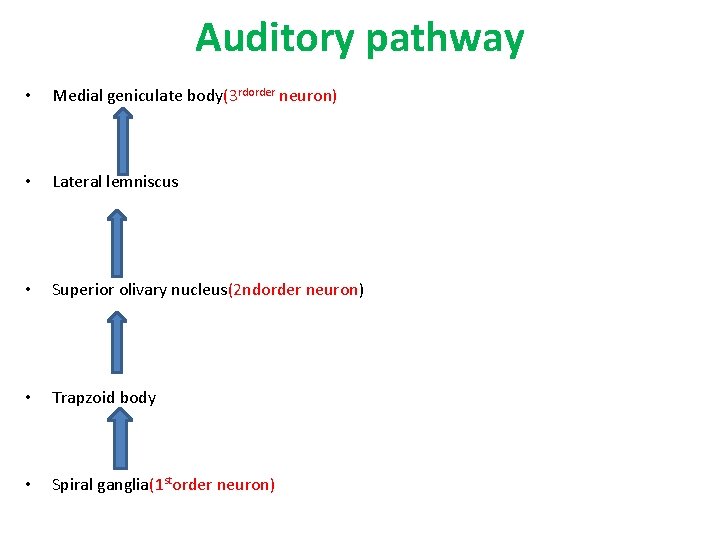
Auditory pathway • Medial geniculate body(3 rdorder neuron) • Lateral lemniscus • Superior olivary nucleus(2 ndorder neuron) • Trapzoid body • Spiral ganglia(1 storder neuron)
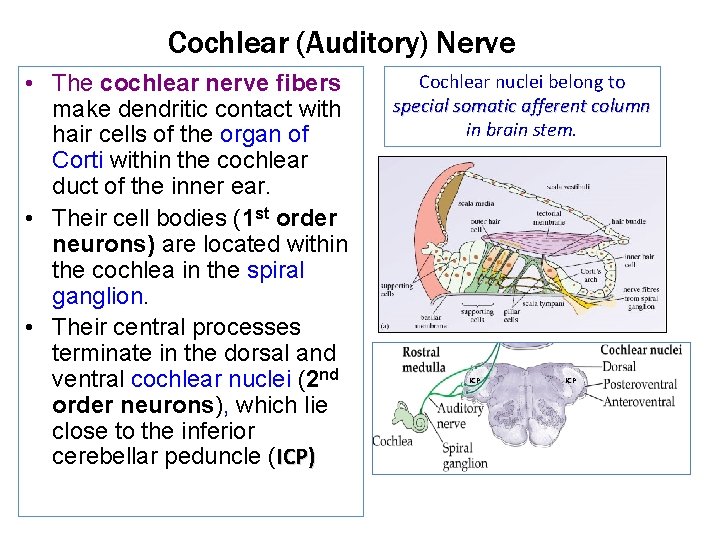
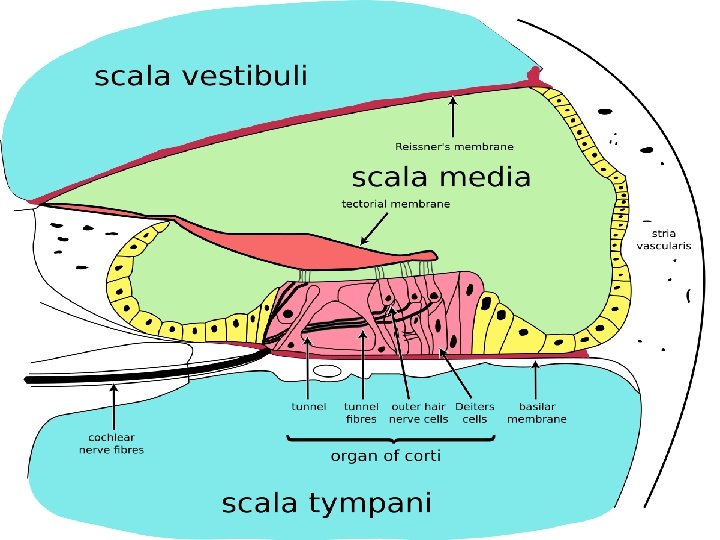
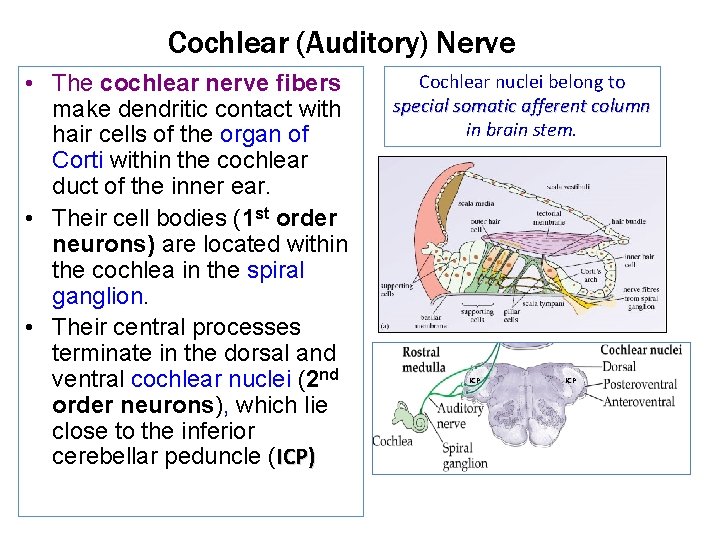
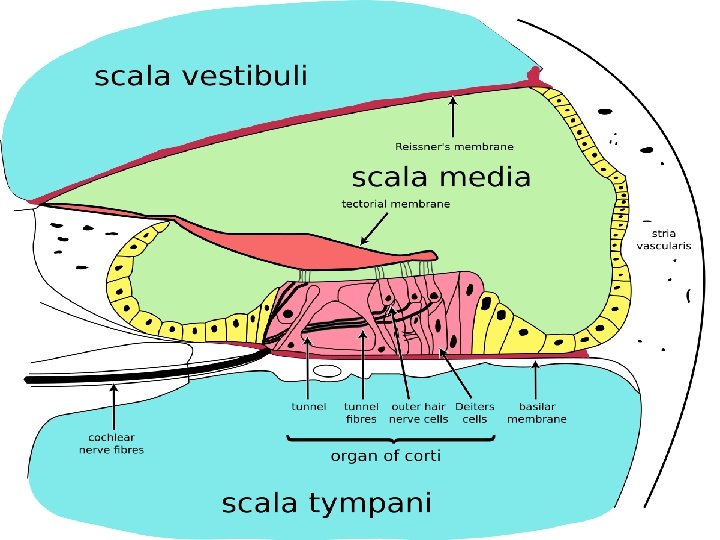
Cochlear (Auditory) Nerve • The cochlear nerve fibers make dendritic contact with hair cells of the organ of Corti within the cochlear duct of the inner ear. • Their cell bodies (1 st order neurons) are located within the cochlea in the spiral ganglion. • Their central processes terminate in the dorsal and ventral cochlear nuclei (2 nd order neurons), which lie close to the inferior cerebellar peduncle (ICP) Cochlear nuclei belong to special somatic afferent column in brain stem. ICP
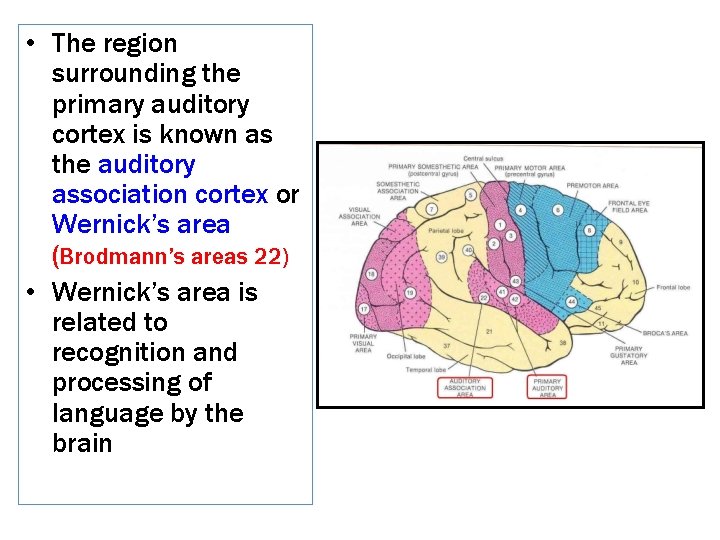
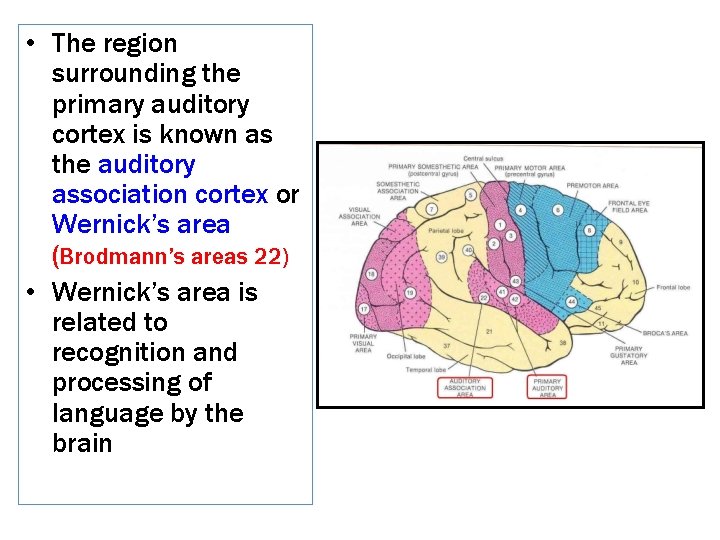
• The region surrounding the primary auditory cortex is known as the auditory association cortex or Wernick’s area (Brodmann’s areas 22) • Wernick’s area is related to recognition and processing of language by the brain
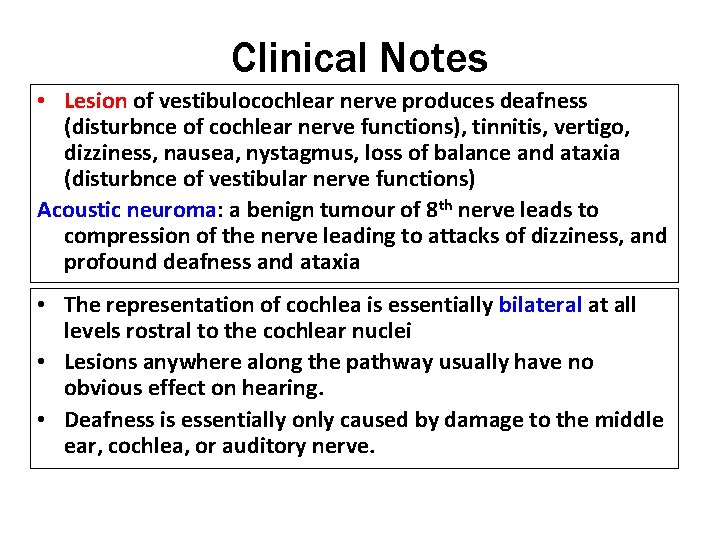
Clinical Notes • Lesion of vestibulocochlear nerve produces deafness (disturbnce of cochlear nerve functions), tinnitis, vertigo, dizziness, nausea, nystagmus, loss of balance and ataxia (disturbnce of vestibular nerve functions) Acoustic neuroma: a benign tumour of 8 th nerve leads to compression of the nerve leading to attacks of dizziness, and profound deafness and ataxia • The representation of cochlea is essentially bilateral at all levels rostral to the cochlear nuclei • Lesions anywhere along the pathway usually have no obvious effect on hearing. • Deafness is essentially only caused by damage to the middle ear, cochlea, or auditory nerve.
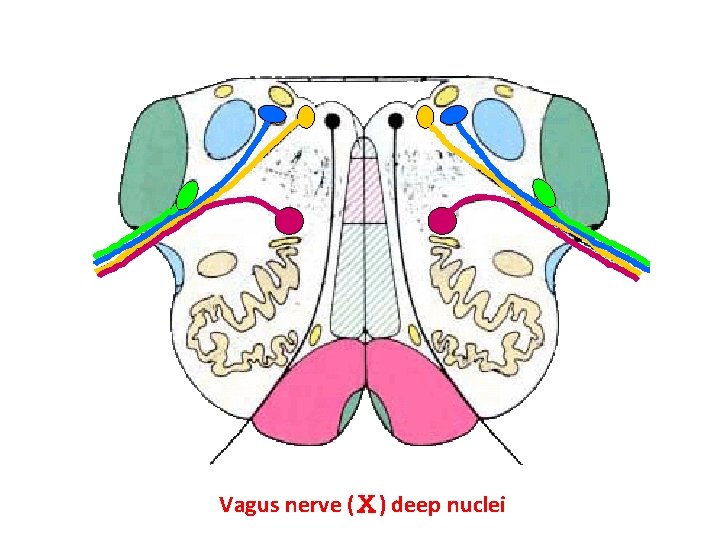
VAGUS NERVE (Ⅹ) • • • Deep nucleoli ; Nucleus ambiguus; Dorsal nucleus Nucleus solitarius Spinal tract of trigeminal
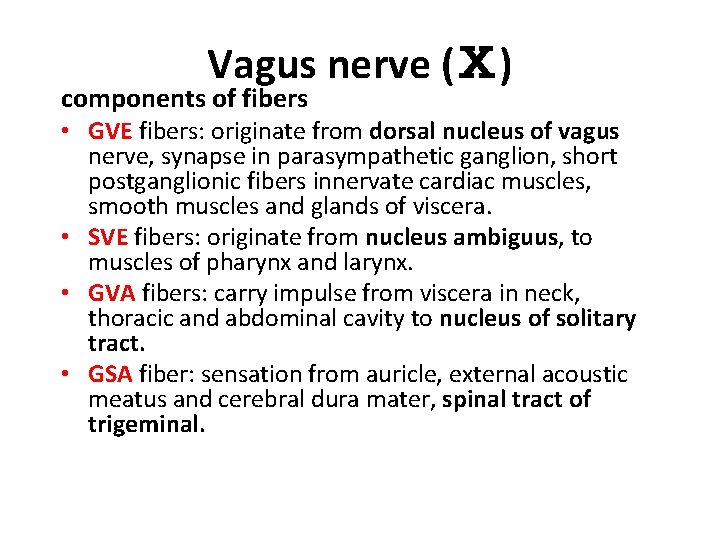
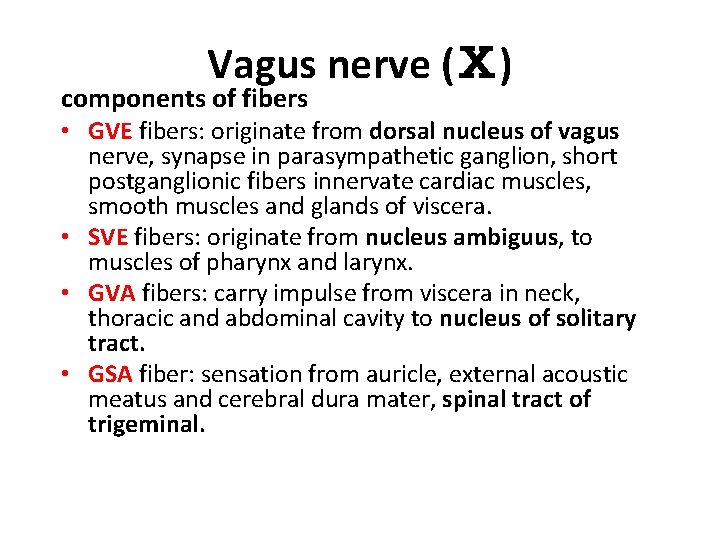
Vagus nerve (Ⅹ) components of fibers • GVE fibers: originate from dorsal nucleus of vagus nerve, synapse in parasympathetic ganglion, short postganglionic fibers innervate cardiac muscles, smooth muscles and glands of viscera. • SVE fibers: originate from nucleus ambiguus, to muscles of pharynx and larynx. • GVA fibers: carry impulse from viscera in neck, thoracic and abdominal cavity to nucleus of solitary tract. • GSA fiber: sensation from auricle, external acoustic meatus and cerebral dura mater, spinal tract of trigeminal.
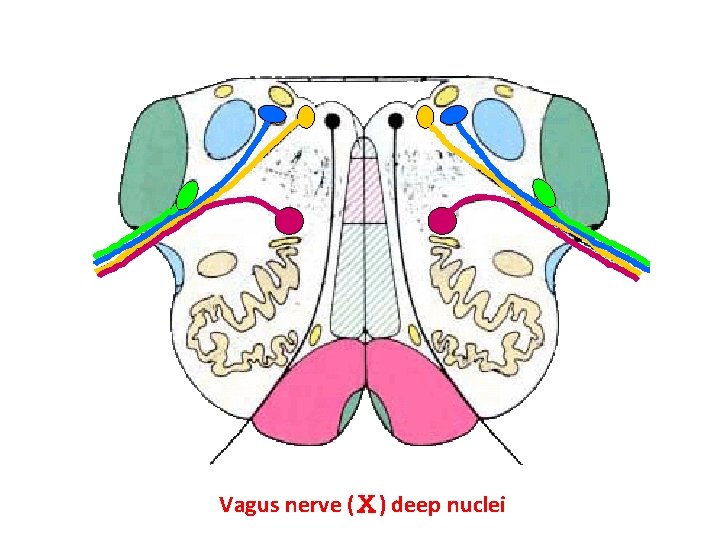
Vagus nerve (Ⅹ) deep nuclei
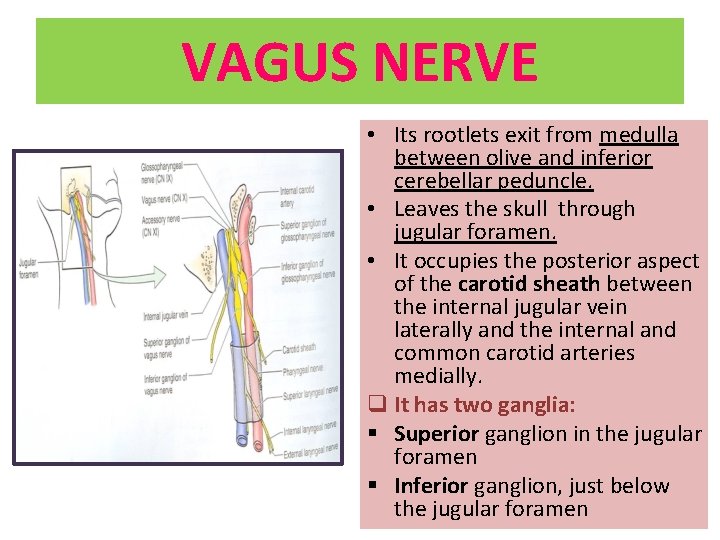
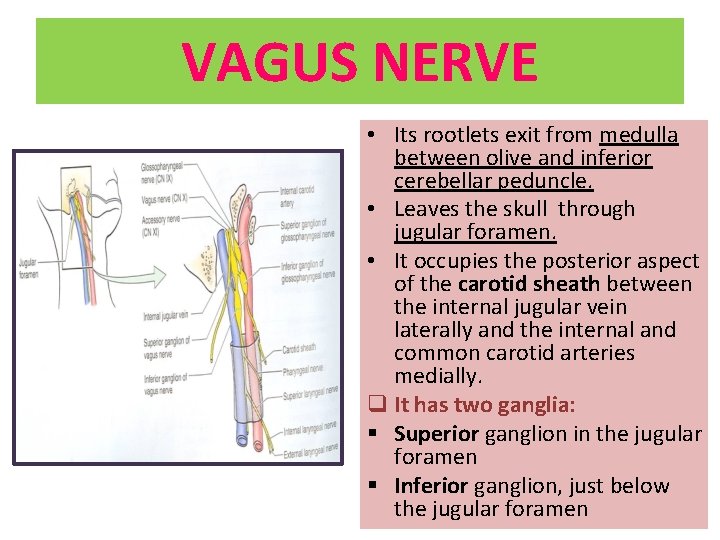
VAGUS NERVE • Its rootlets exit from medulla between olive and inferior cerebellar peduncle. • Leaves the skull through jugular foramen. • It occupies the posterior aspect of the carotid sheath between the internal jugular vein laterally and the internal and common carotid arteries medially. q It has two ganglia: § Superior ganglion in the jugular foramen § Inferior ganglion, just below the jugular foramen
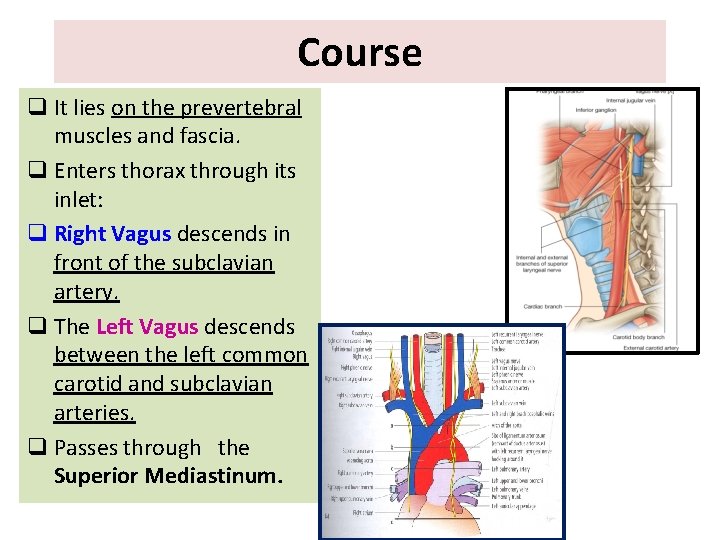
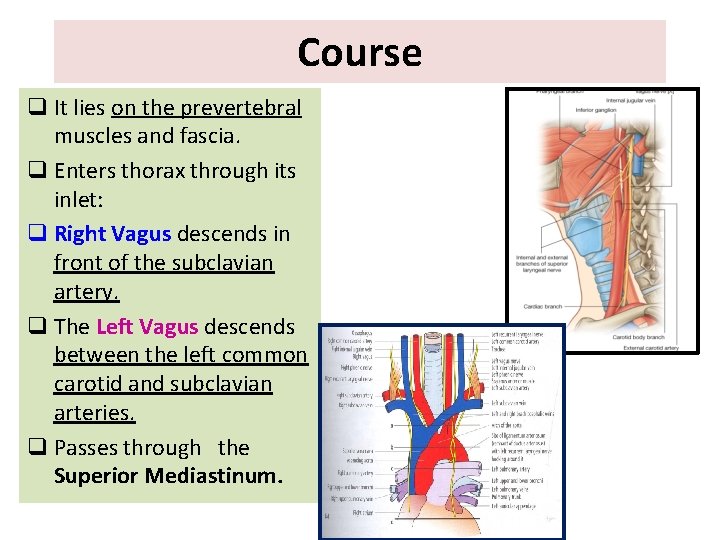
Course q It lies on the prevertebral muscles and fascia. q Enters thorax through its inlet: q Right Vagus descends in front of the subclavian artery. q The Left Vagus descends between the left common carotid and subclavian arteries. q Passes through the Superior Mediastinum.
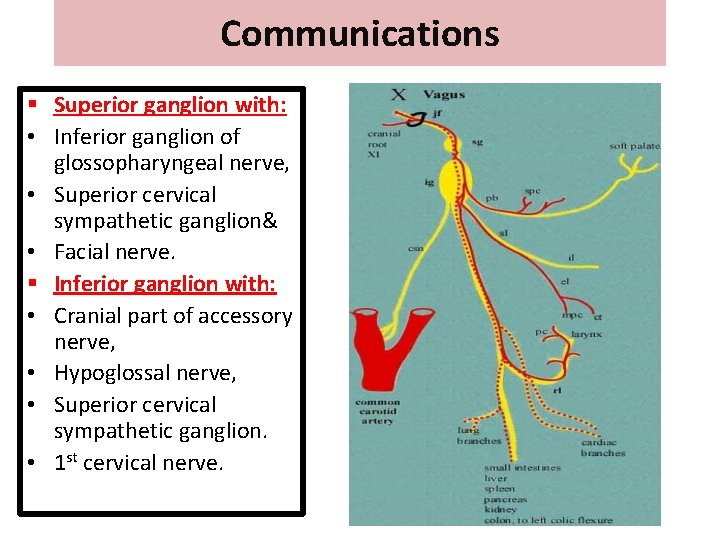
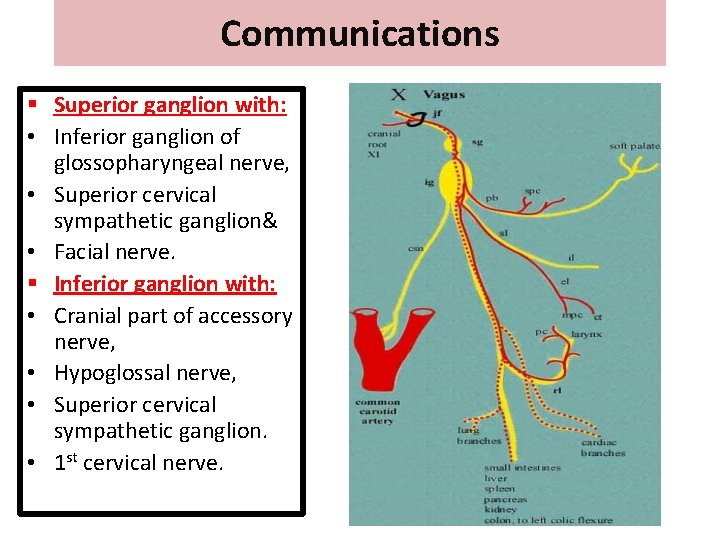
Communications § Superior ganglion with: • Inferior ganglion of glossopharyngeal nerve, • Superior cervical sympathetic ganglion& • Facial nerve. § Inferior ganglion with: • Cranial part of accessory nerve, • Hypoglossal nerve, • Superior cervical sympathetic ganglion. • 1 st cervical nerve.
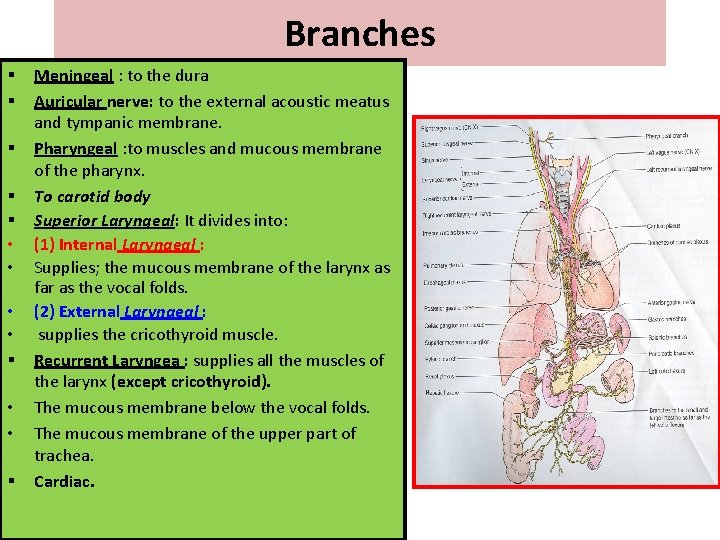
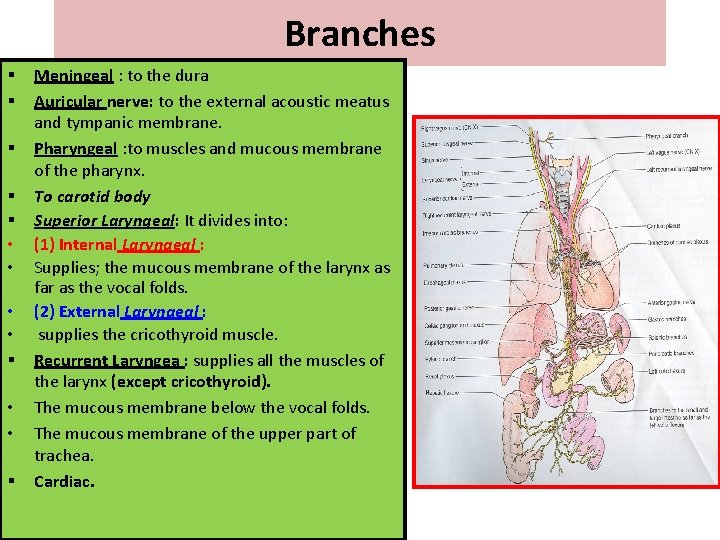
Branches § § § • • § Meningeal : to the dura Auricular nerve: to the external acoustic meatus and tympanic membrane. Pharyngeal : to muscles and mucous membrane of the pharynx. To carotid body Superior Laryngeal: It divides into: (1) Internal Laryngeal : Supplies; the mucous membrane of the larynx as far as the vocal folds. (2) External Laryngeal : supplies the cricothyroid muscle. Recurrent Laryngea : supplies all the muscles of the larynx (except cricothyroid). The mucous membrane below the vocal folds. The mucous membrane of the upper part of trachea. Cardiac.
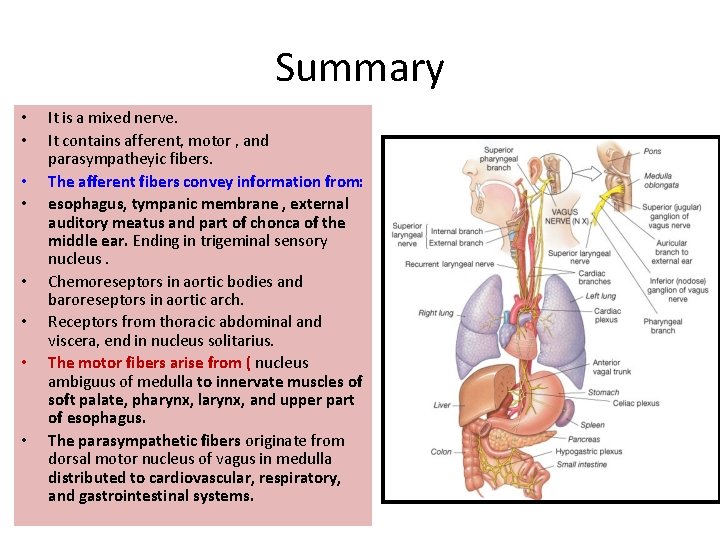
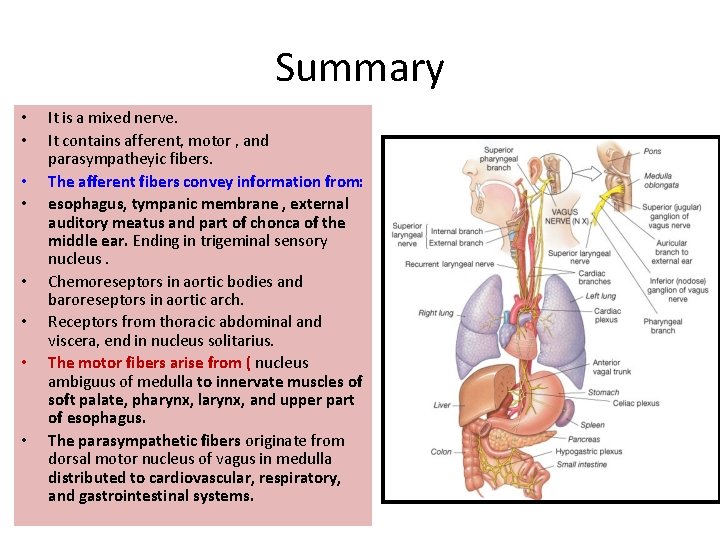
Summary • • It is a mixed nerve. It contains afferent, motor , and parasympatheyic fibers. The afferent fibers convey information from: esophagus, tympanic membrane , external auditory meatus and part of chonca of the middle ear. Ending in trigeminal sensory nucleus. Chemoreseptors in aortic bodies and baroreseptors in aortic arch. Receptors from thoracic abdominal and viscera, end in nucleus solitarius. The motor fibers arise from ( nucleus ambiguus of medulla to innervate muscles of soft palate, pharynx, larynx, and upper part of esophagus. The parasympathetic fibers originate from dorsal motor nucleus of vagus in medulla distributed to cardiovascular, respiratory, and gastrointestinal systems.
Clinical Tests Glossopharyngeal & Vagus nerves – The person is asked to swallow. – The person is asked to say ‘ah-h-h’ to check the movements of palate and uvula. – The ‘gag reflex’ is tested by touching the back of the throat by the tongue depressor. – The person is asked to speak to check the voice for hoarseness.
Clinical anatomy • Moto neuron disease ; is a degenerative disorder seen over 50 years • Tumors compressing the cranial nerves in their exiting foramina from the cranium via the skull base. • Glossopharyngeal nerve lesion is characterized by dysphonia, dysphagia and absence of the gag reflex. • Vagus nerve damage; causes hoarseness or loss of voice, impaired swallowing, GI dysfunction, blood pressure anomalies (with CN IX), fatal if both are damaged.
Thank you