Functional Anatomy of the Kidney A A J
- Slides: 28
Functional Anatomy of the Kidney A. A. J. RAJARATNE
Functions: 1. Regulation of Water Balance 2. Regulation of Electrolyte Balance 2. Excretion of Metabolic Waste Products 3. Excretion of Foreign Chemicals & Drugs 4. Regulation of Arterial Blood Pressure 5. Regulation of Erythropoiesis 6. Regulation of Vitamin D 7. Gluconeogenesis
Objectives n Recognize that the functional unit of the kidney is the nephron n List the two different types of nephrons and state the structural differences between them n Describe the process of urine formation
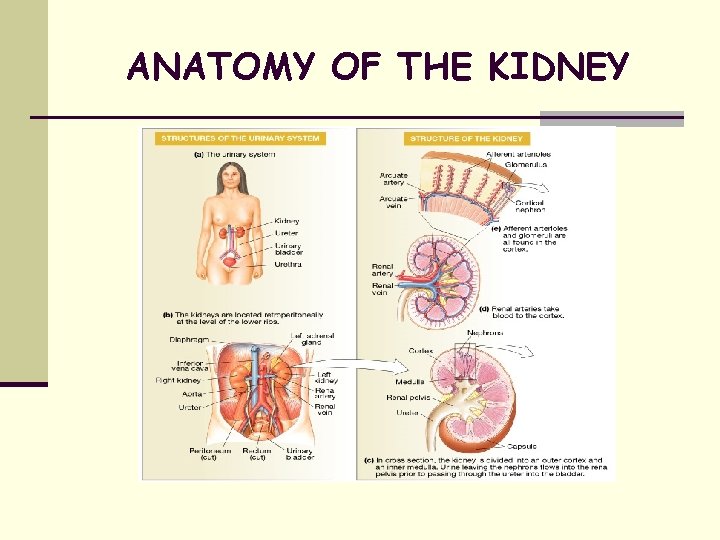
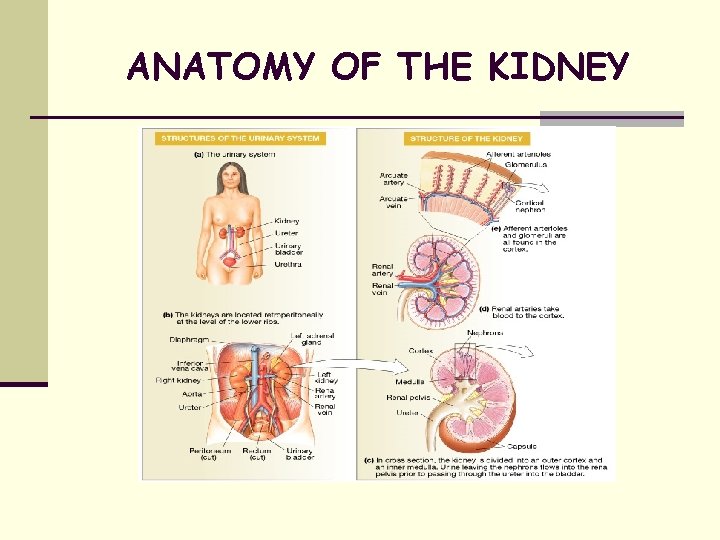
ANATOMY OF THE KIDNEY
Structure of Kidney: The kidneys are paired organs lying in the retroperitoneal space. Medial border = hilum renal pelvis and ureter. The renal pelvis subdivides into major calyces, then minor calyces projecting to a renal pyramid. Divided into outer cortex and inner medulla.
Parts of the nephron glomerulus
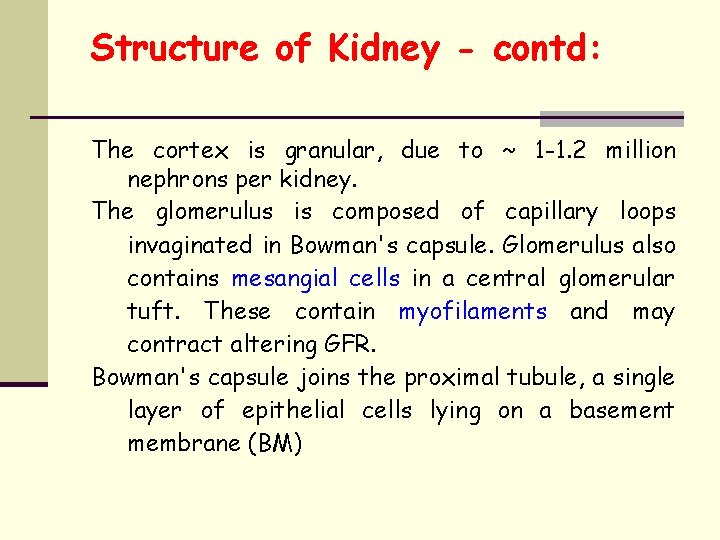
Structure of Kidney - contd: The cortex is granular, due to ~ 1 -1. 2 million nephrons per kidney. The glomerulus is composed of capillary loops invaginated in Bowman's capsule. Glomerulus also contains mesangial cells in a central glomerular tuft. These contain myofilaments and may contract altering GFR. Bowman's capsule joins the proximal tubule, a single layer of epithelial cells lying on a basement membrane (BM)
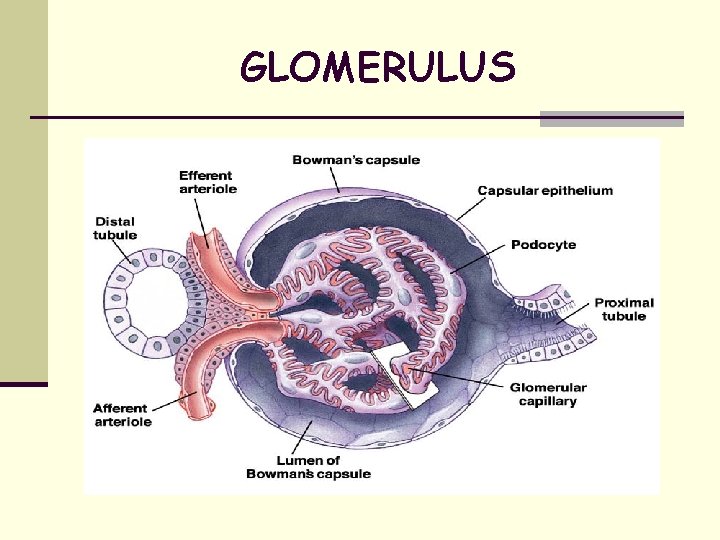
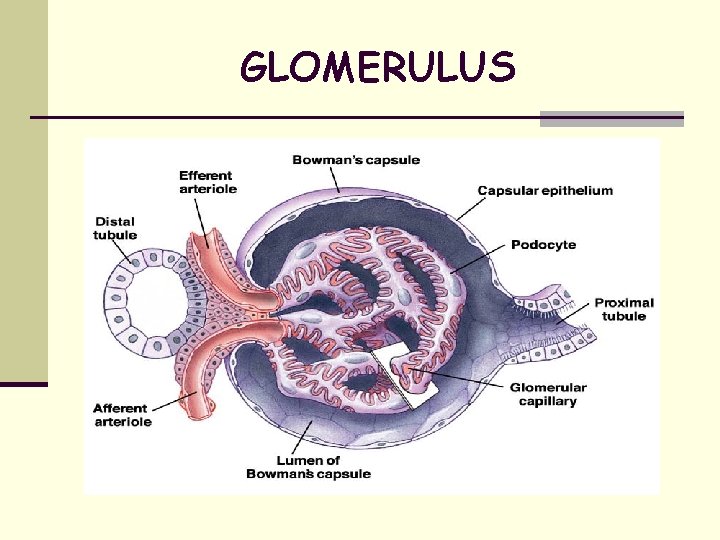
GLOMERULUS
t Glomerulus - 200 m in diameter t Formed by invagination of capillary tuft into blind end of nephron Bowman’s capsule t Afferent and efferent arterioles t Filtration barrier - two layers of cells separating blood from glomerular filtrate
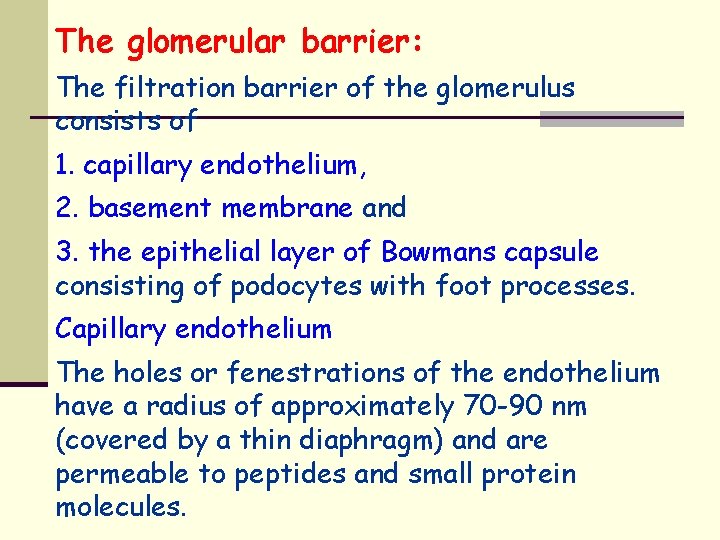
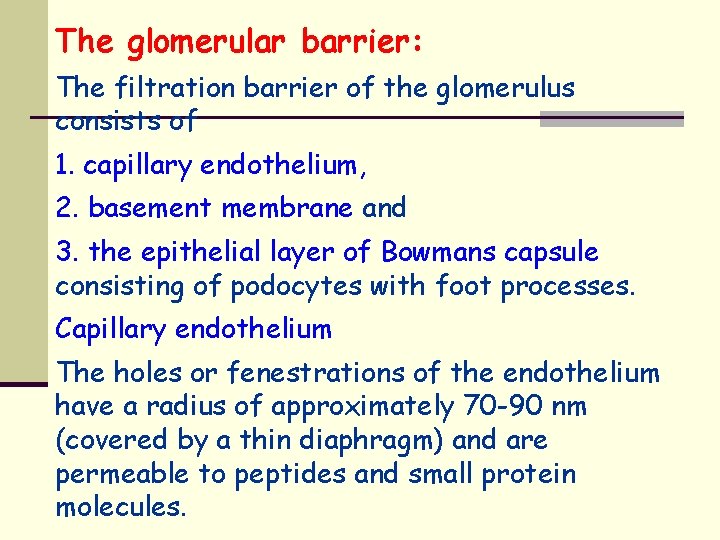
The glomerular barrier: The filtration barrier of the glomerulus consists of 1. capillary endothelium, 2. basement membrane and 3. the epithelial layer of Bowmans capsule consisting of podocytes with foot processes. Capillary endothelium The holes or fenestrations of the endothelium have a radius of approximately 70 -90 nm (covered by a thin diaphragm) and are permeable to peptides and small protein molecules.
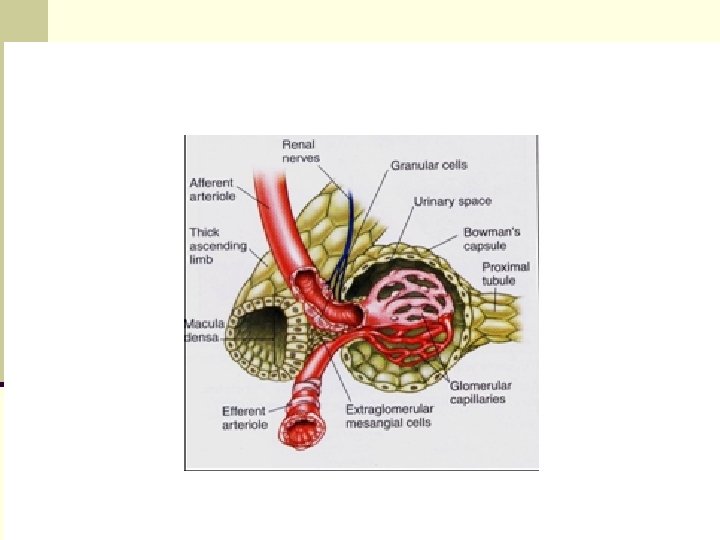
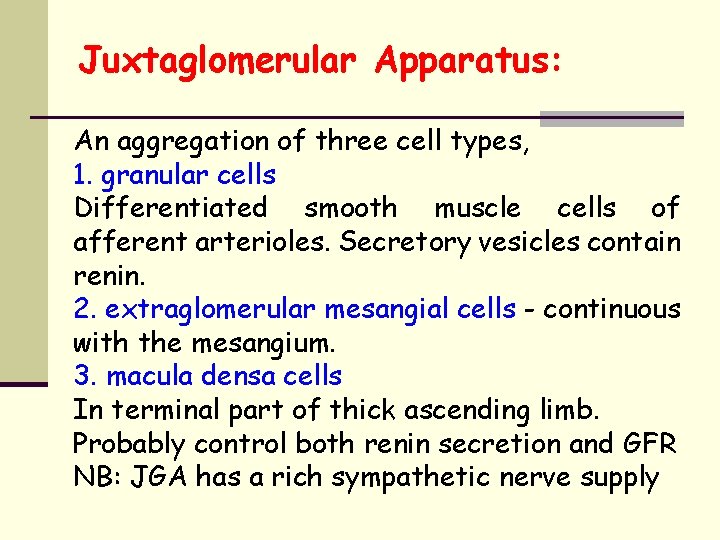
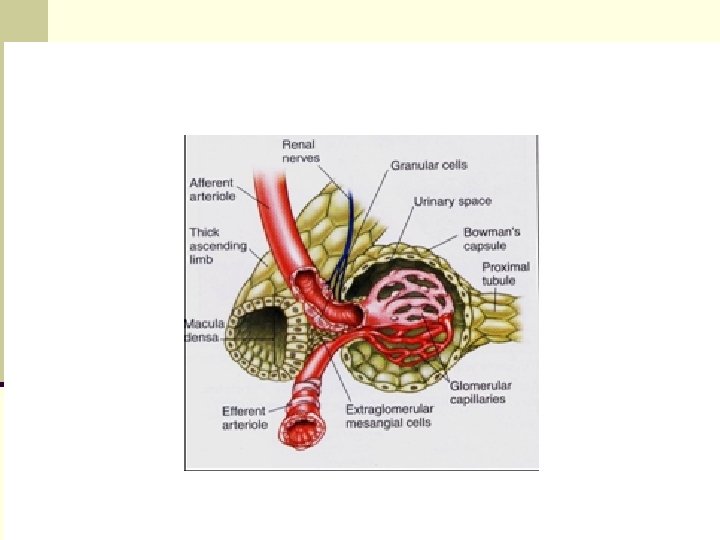
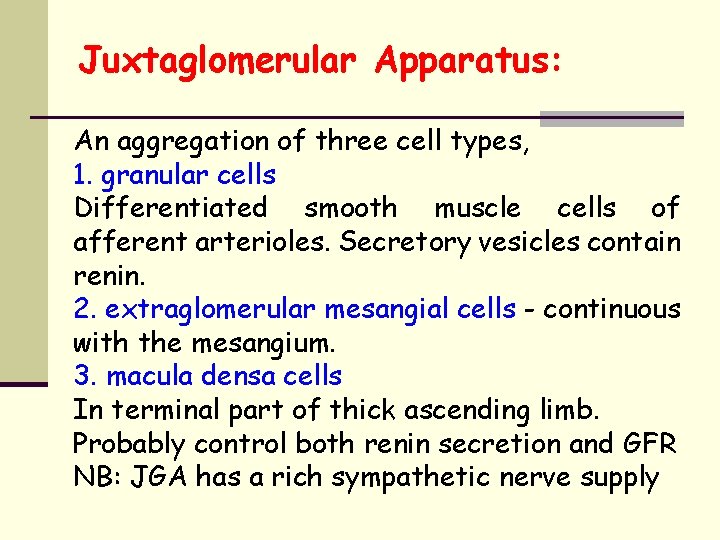
Juxtaglomerular Apparatus: An aggregation of three cell types, 1. granular cells Differentiated smooth muscle cells of afferent arterioles. Secretory vesicles contain renin. 2. extraglomerular mesangial cells - continuous with the mesangium. 3. macula densa cells In terminal part of thick ascending limb. Probably control both renin secretion and GFR NB: JGA has a rich sympathetic nerve supply
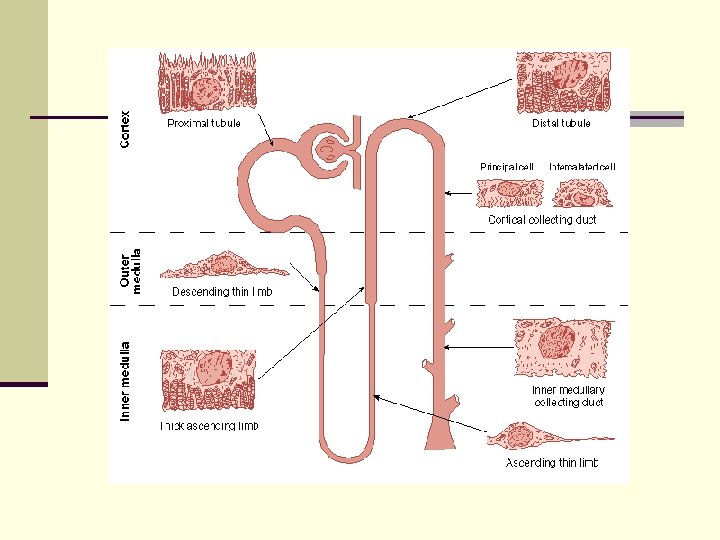
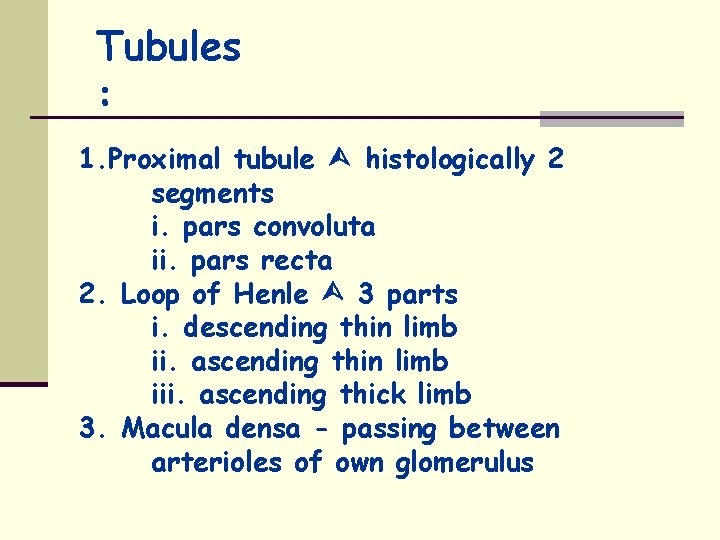
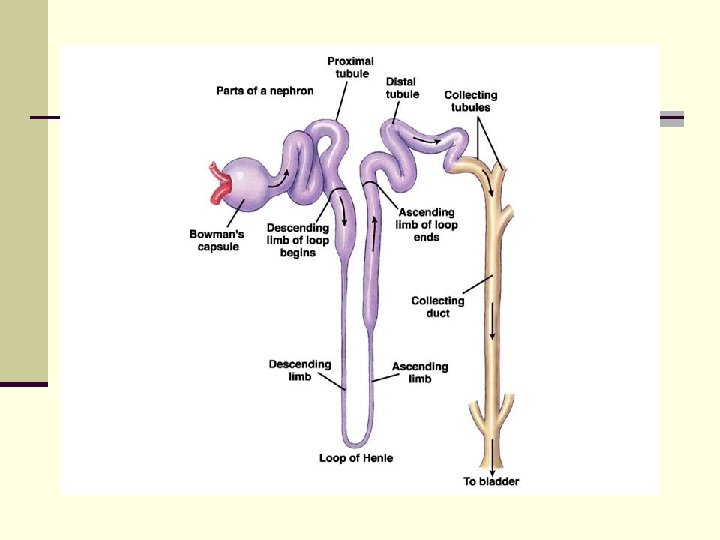
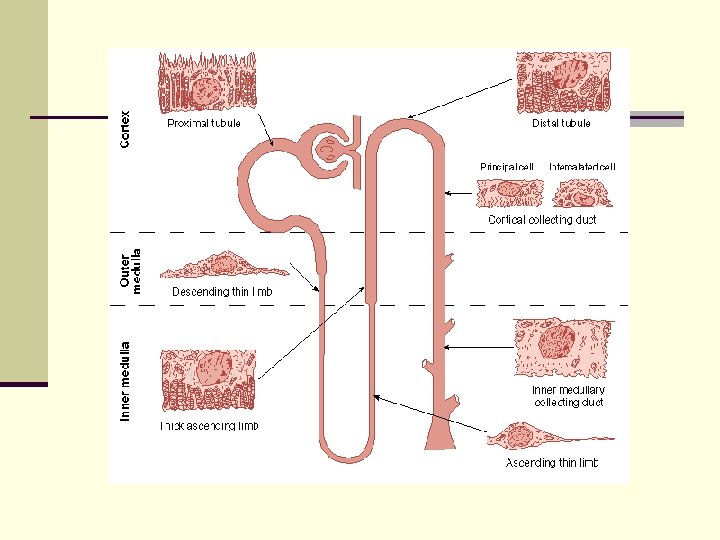
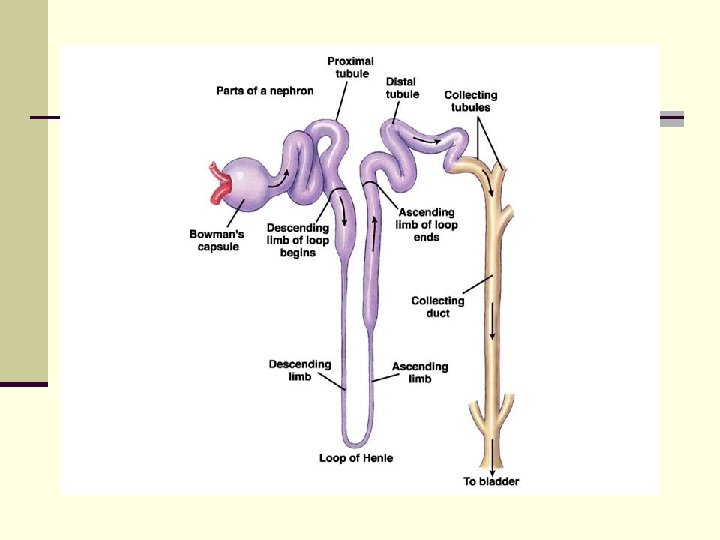
Tubules : 1. Proximal tubule histologically 2 segments i. pars convoluta ii. pars recta 2. Loop of Henle 3 parts i. descending thin limb ii. ascending thin limb iii. ascending thick limb 3. Macula densa - passing between arterioles of own glomerulus
4. Distal tubule - also termed the late distal tubule i. distal convoluted tubule ii. connecting segment iii. initial collecting tubule 5. Collecting System: 1. Cortical collecting tubule 2. Medullary collecting tubule 3. Papillary collecting ducts These drain into a calyx of the renal pelvis, then to the ureter & bladder.
Proximal convoluted tubule (pars convoluta): t Size - 15 mm long and 55 m in diameter. t Wall - single layer of cells united by apical tight junctions. t Bases - lateral intercellular spaces t Luminal edges - have brush border with innumerable microvilli
Loop of Henle: PCT drains into straight portion (pars recta) - forms first part of loop of Henle. Loop of Henle - epithelium of flat attenuated cells Total length of thin segment varies from 2 - 14 mm. Ends in thick segment 12 mm long. Cells are cuboidal , numerous mitochondria. Modified to form macula densa, which, together with its own afferent and efferent arterioles - forms Juxtaglomerular apparatus. Regional differences are present.
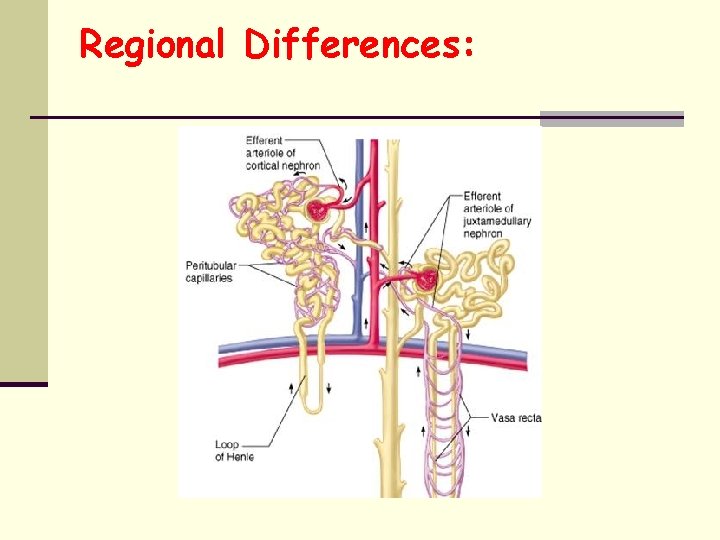
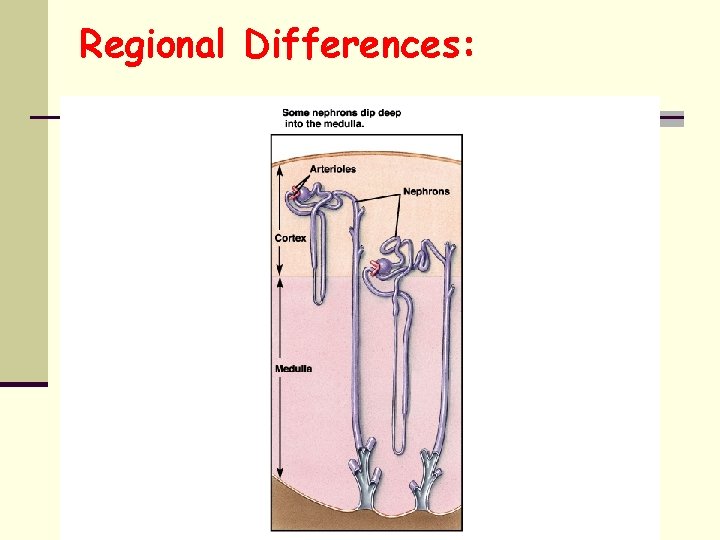
Regional Differences: Nephrons are not homogeneous and vary according to the location of the glomerulus in the cortex. a. Superficial cortical nephrons - all short looped b. Midcortical nephrons - mixture c. Juxtamedullary nephrons (15% in man) all long looped.
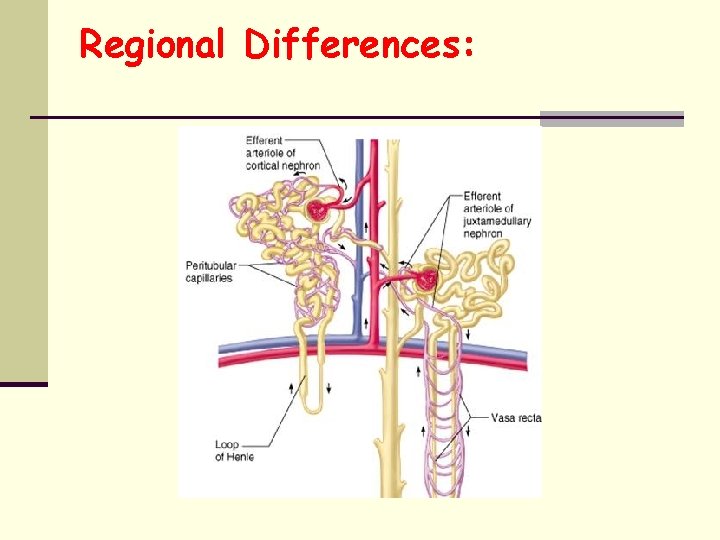
Regional Differences:
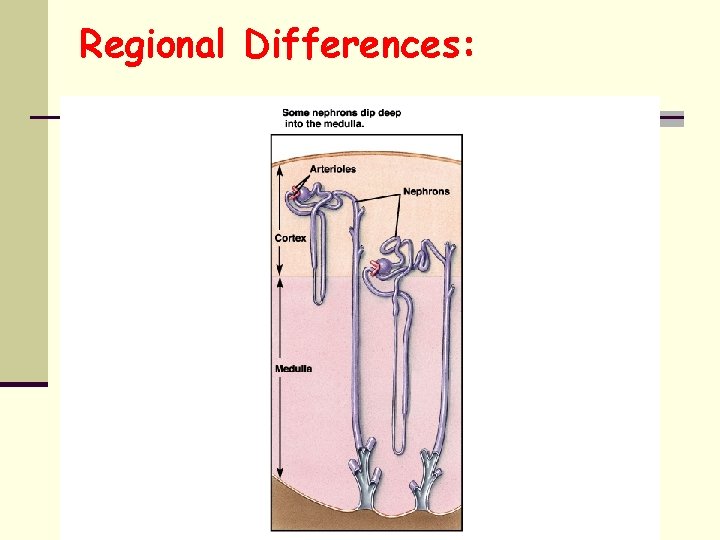
Regional Differences:
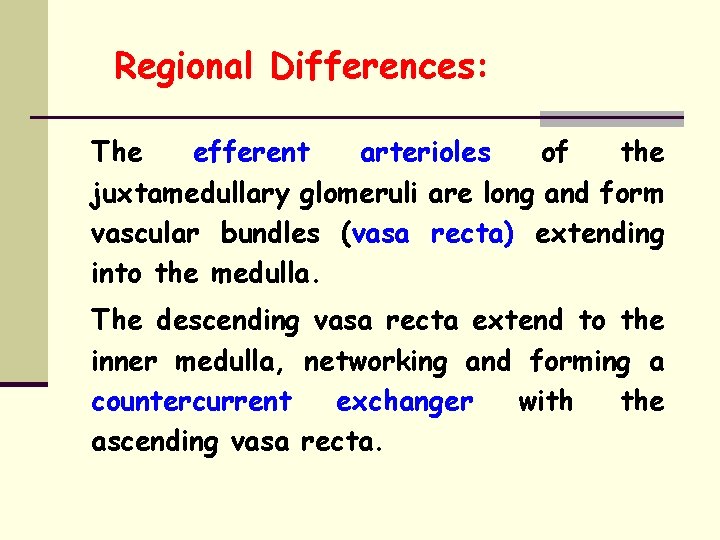
Regional Differences: The efferent arterioles of the juxtamedullary glomeruli are long and form vascular bundles (vasa recta) extending into the medulla. The descending vasa recta extend to the inner medulla, networking and forming a countercurrent exchanger with the ascending vasa recta.
Distal convoluted tubule: 5 mm long. Epithelium - flatter than microvilli, no brush border. PCT, few Join together to form collecting ducts - 20 mm long, pass through cortex and medulla to empty into renal pyramids at medullary pyramids.
Collecting ducts: Epithelium made up of a. Principal cells (P cells) - Na+ reabsorption - ADH induced H 2 O reabsorption b. Intercalated cells (I cells) - more microvilli, vesicles, mitochondria - Acid secretion, HCO 3 transport
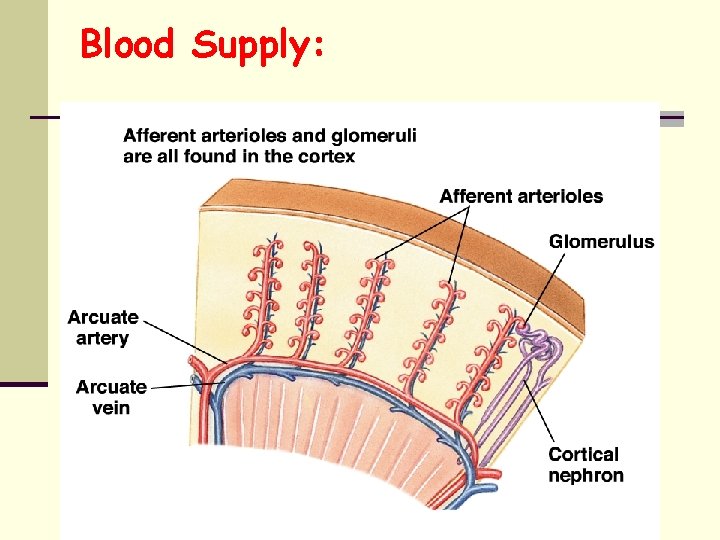
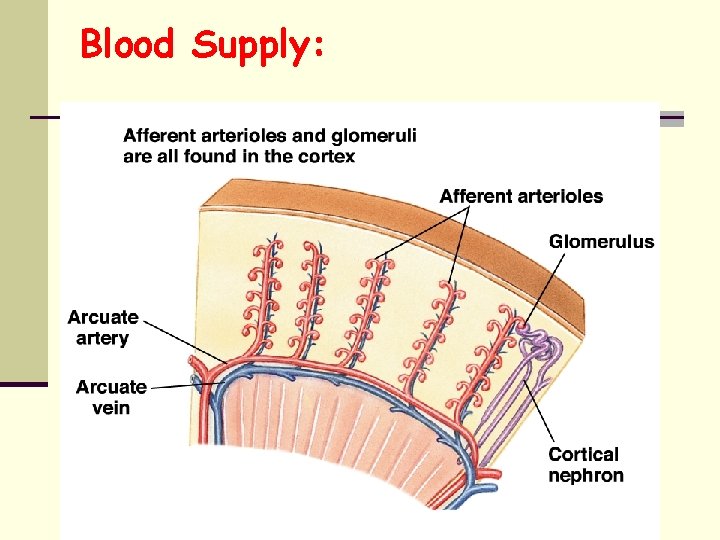
Blood Supply:
Blood Supply: 1. Renal artery 2. Interlobar arteries 3. Arcuate arteries 4. Interlobular arteries 5. Afferent arterioles - parallel series from each interlobular artery 6. Glomerular capillaries 7. Efferent arterioles 8. Peritubular capillaries - nonspecific NB: Interlobular, arcuate, interlobar and renal veins parallel arteries.
Innervation: Renal nerves a. PG sympathetic to afferent and efferent arterioles, PCT and DCT, juxtaglomerular cells b. Sensory nociceptive afferents