Frozen shoulder Adhesive capsulitis option grid What is
- Slides: 2
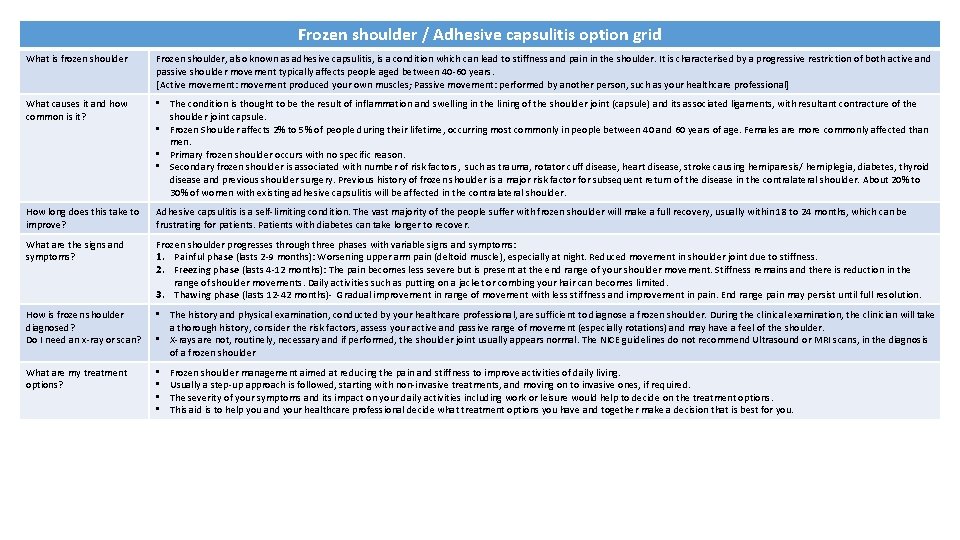
Frozen shoulder / Adhesive capsulitis option grid What is frozen shoulder Frozen shoulder, also known as adhesive capsulitis, is a condition which can lead to stiffness and pain in the shoulder. It is characterised by a progressive restriction of both active and passive shoulder movement typically affects people aged between 40 -60 years. [Active movement: movement produced your own muscles; Passive movement: performed by another person, such as your healthcare professional] What causes it and how common is it? • The condition is thought to be the result of inflammation and swelling in the lining of the shoulder joint (capsule) and its associated ligaments, with resultant contracture of the shoulder joint capsule. • Frozen Shoulder affects 2% to 5% of people during their lifetime, occurring most commonly in people between 40 and 60 years of age. Females are more commonly affected than men. • Primary frozen shoulder occurs with no specific reason. • Secondary frozen shoulder is associated with number of risk factors, such as trauma, rotator cuff disease, heart disease, stroke causing hemiparesis/ hemiplegia, diabetes, thyroid disease and previous shoulder surgery. Previous history of frozen shoulder is a major risk factor for subsequent return of the disease in the contralateral shoulder. About 20% to 30% of women with existing adhesive capsulitis will be affected in the contralateral shoulder. How long does this take to improve? Adhesive capsulitis is a self-limiting condition. The vast majority of the people suffer with frozen shoulder will make a full recovery, usually within 18 to 24 months, which can be frustrating for patients. Patients with diabetes can take longer to recover. What are the signs and symptoms? Frozen shoulder progresses through three phases with variable signs and symptoms: 1. Painful phase (lasts 2 -9 months): Worsening upper arm pain (deltoid muscle), especially at night. Reduced movement in shoulder joint due to stiffness. 2. Freezing phase (lasts 4 -12 months): The pain becomes less severe but is present at the end range of your shoulder movement. Stiffness remains and there is reduction in the range of shoulder movements. Daily activities such as putting on a jacket or combing your hair can becomes limited. 3. Thawing phase (lasts 12 -42 months)- Gradual improvement in range of movement with less stiffness and improvement in pain. End range pain may persist until full resolution. How is frozen shoulder diagnosed? Do I need an x-ray or scan? • The history and physical examination, conducted by your healthcare professional, are sufficient to diagnose a frozen shoulder. During the clinical examination, the clinician will take a thorough history, consider the risk factors, assess your active and passive range of movement (especially rotations) and may have a feel of the shoulder. • X-rays are not, routinely, necessary and if performed, the shoulder joint usually appears normal. The NICE guidelines do not recommend Ultrasound or MRI scans, in the diagnosis of a frozen shoulder What are my treatment options? • • Frozen shoulder management aimed at reducing the pain and stiffness to improve activities of daily living. Usually a step-up approach is followed, starting with non-invasive treatments, and moving on to invasive ones, if required. The severity of your symptoms and its impact on your daily activities including work or leisure would help to decide on the treatment options. This aid is to help you and your healthcare professional decide what treatment options you have and together make a decision that is best for you.
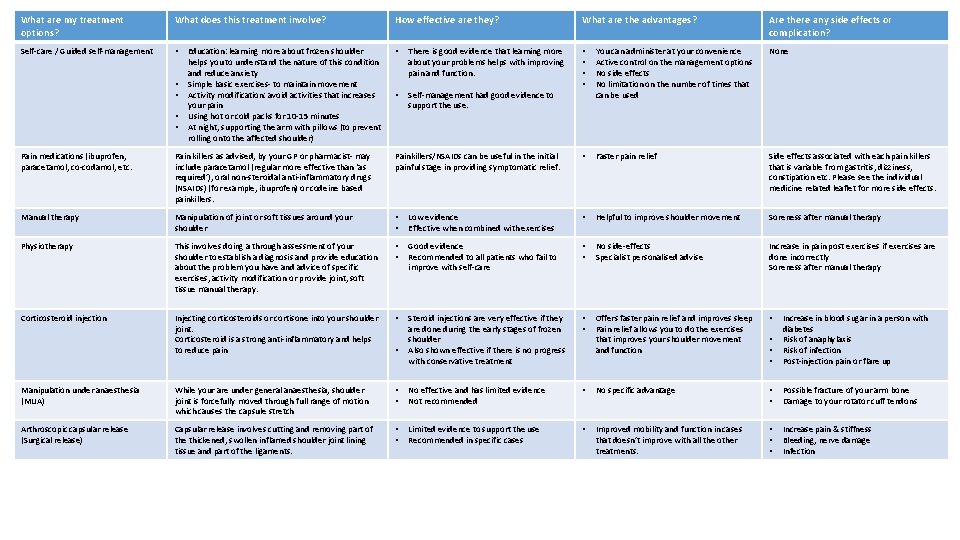
What are my treatment options? What does this treatment involve? How effective are they? What are the advantages? Are there any side effects or complication? Self-care / Guided self-management • • There is good evidence that learning more about your problems helps with improving pain and function. • • None • Self-management had good evidence to support the use. You can administer at your convenience Active control on the management options No side effects No limitation on the number of times that can be used • • Education: learning more about frozen shoulder helps you to understand the nature of this condition and reduce anxiety Simple basic exercises- to maintain movement Activity modification: avoid activities that increases your pain Using hot or cold packs for 10 -15 minutes At night, supporting the arm with pillows (to prevent rolling onto the affected shoulder) Pain medications (ibuprofen, paracetamol, co-codamol, etc. Pain killers as advised, by your GP or pharmacist- may include paracetamol (regular more effective than ‘as required’), oral non-steroidal anti-inflammatory drugs (NSAIDs) (for example, ibuprofen) or codeine based painkillers. Painkillers/NSAIDs can be useful in the initial painful stage in providing symptomatic relief. • Faster pain relief Side effects associated with each pain killers that is variable from gastritis, dizziness, constipation etc. Please see the individual medicine related leaflet for more side effects. Manual therapy Manipulation of joint or soft tissues around your shoulder • • Low evidence Effective when combined with exercises • Helpful to improve shoulder movement Soreness after manual therapy Physiotherapy This involves doing a through assessment of your shoulder to establish a diagnosis and provide education about the problem you have and advice of specific exercises, activity modification or provide joint, soft tissue manual therapy. • • Good evidence Recommended to all patients who fail to improve with self-care • • No side-effects Specialist personalised advise Increase in pain post exercises if exercises are done incorrectly Soreness after manual therapy Corticosteroid injection Injecting corticosteroids or cortisone into your shoulder joint. Corticosteroid is a strong anti-inflammatory and helps to reduce pain • Steroid injections are very effective if they are done during the early stages of frozen shoulder Also shown effective if there is no progress with conservative treatment • • Offers faster pain relief and improves sleep Pain relief allows you to do the exercises that improves your shoulder movement and function • • Increase in blood sugar in a person with diabetes Risk of anaphylaxis Risk of infection Post-injection pain or flare up Manipulation under anaesthesia (MUA) While your are under general anaesthesia, shoulder joint is forcefully moved through full range of motion which causes the capsule stretch • • No effective and has limited evidence Not recommended • No specific advantage • • Possible fracture of your arm bone Damage to your rotator cuff tendons Arthroscopic capsular release (Surgical release) Capsular release involves cutting and removing part of the thickened, swollen inflamed shoulder joint lining tissue and part of the ligaments. • • Limited evidence to support the use Recommended in specific cases • Improved mobility and function in cases that doesn’t improve with all the other treatments. • • • Increase pain & stiffness Bleeding, nerve damage Infection •