Frontal Plane Patellofemoral Joint Stability Part 2 RIMT
Frontal Plane Patellofemoral Joint Stability (Part 2) RIMT University Department of Physiotherapy Prepared by: Dr. Navkaran Singh
FRONTAL PLANE STABILITY • The patellofemoral joint is UNIQUE in its potential for frontal plane instability near full knee extension, as well as for degenerative changes resulting from increased patellofemoral joint stresses (in flexion). • This multifaceted problem makes understanding the control of the patella’s frontal plane motion particularly important.
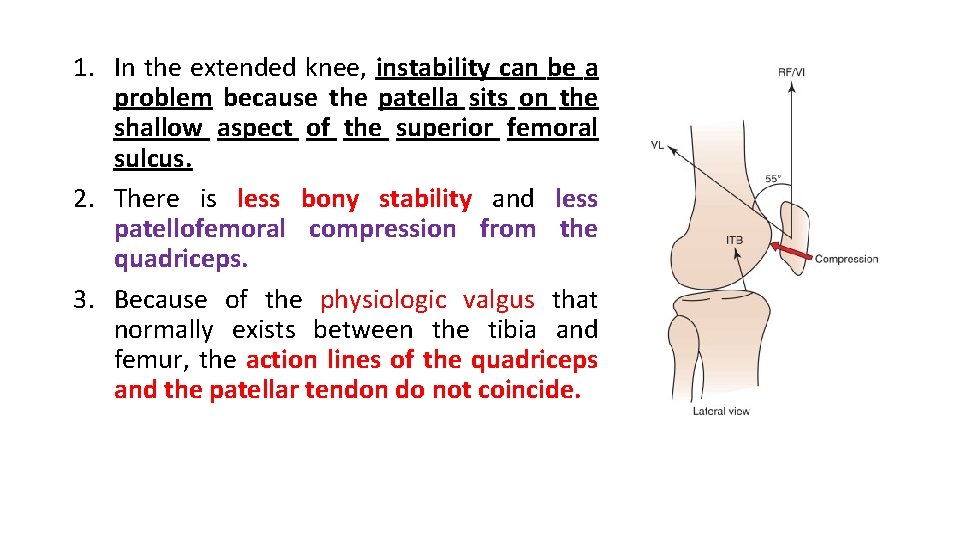
1. In the extended knee, instability can be a problem because the patella sits on the shallow aspect of the superior femoral sulcus. 2. There is less bony stability and less patellofemoral compression from the quadriceps. 3. Because of the physiologic valgus that normally exists between the tibia and femur, the action lines of the quadriceps and the patellar tendon do not coincide.
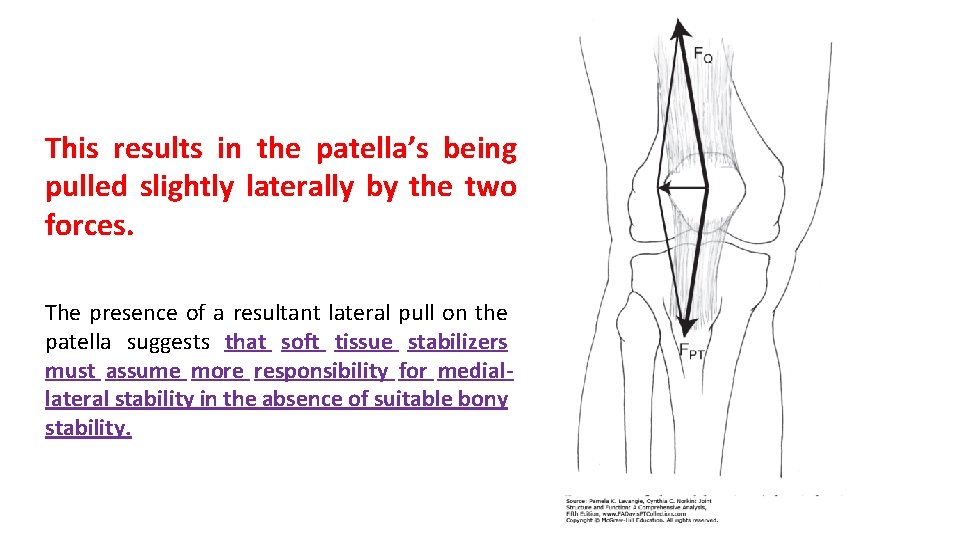
This results in the patella’s being pulled slightly laterally by the two forces. The presence of a resultant lateral pull on the patella suggests that soft tissue stabilizers must assume more responsibility for mediallateral stability in the absence of suitable bony stability.
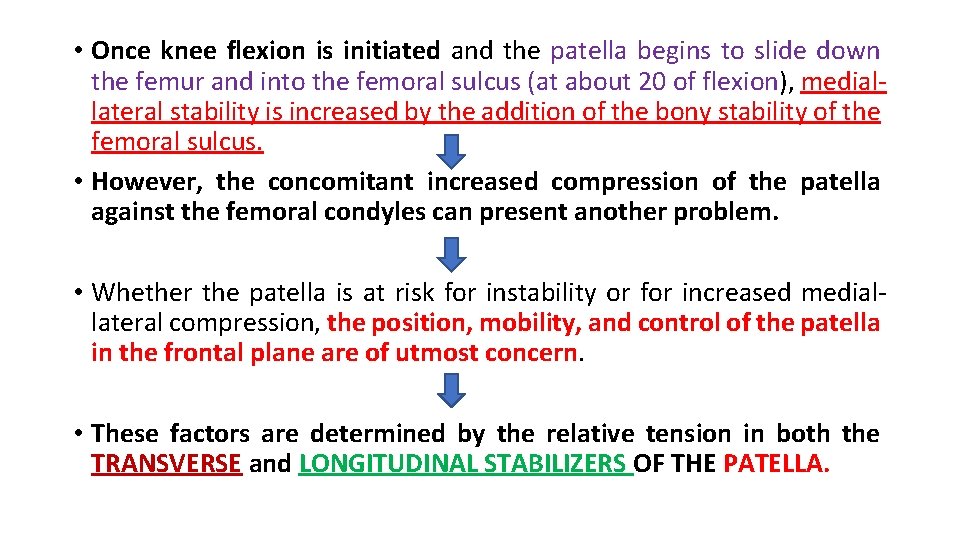
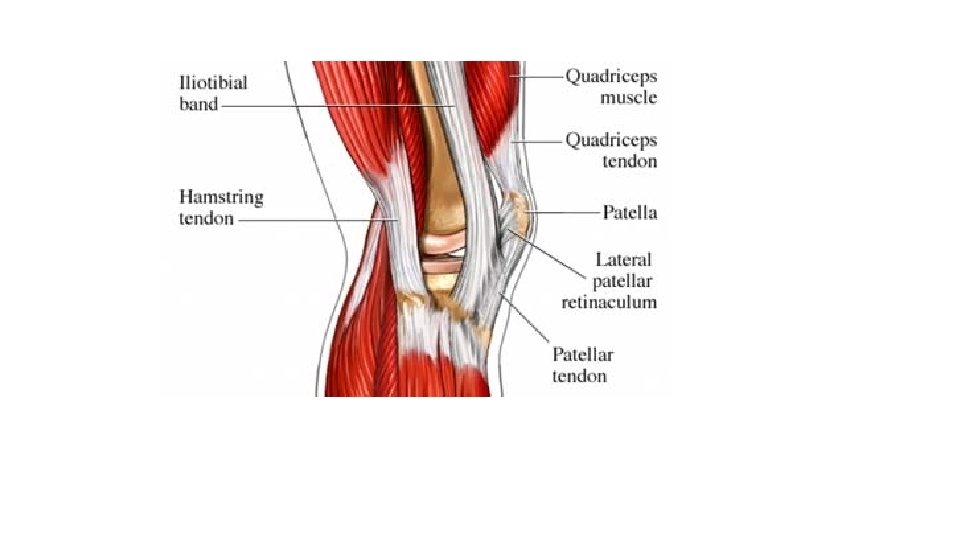
• Once knee flexion is initiated and the patella begins to slide down the femur and into the femoral sulcus (at about 20 of flexion), mediallateral stability is increased by the addition of the bony stability of the femoral sulcus. • However, the concomitant increased compression of the patella against the femoral condyles can present another problem. • Whether the patella is at risk for instability or for increased mediallateral compression, the position, mobility, and control of the patella in the frontal plane are of utmost concern. • These factors are determined by the relative tension in both the TRANSVERSE and LONGITUDINAL STABILIZERS OF THE PATELLA.

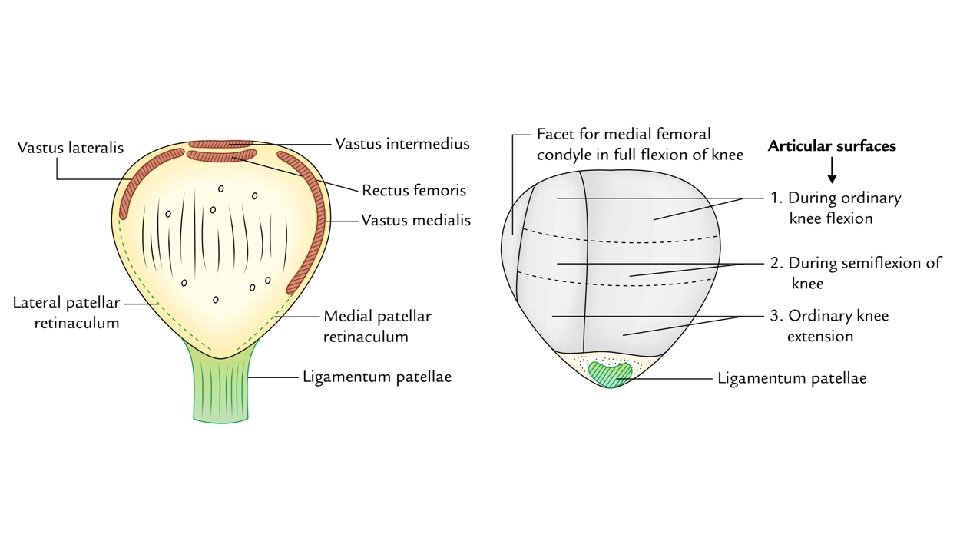
Longitudinal stabilizers • The longitudinal stabilizers of the patella : 1. Patellar tendon inferiorly 2. Quadriceps tendon superiorly • The patellotibial ligaments that are part of the extensor retinaculum and reinforce the capsule also are longitudinal stabilizers. (Fig: A) • The longitudinal stabilizers are capable of providing medial-lateral stability of the patella in knee flexion through increased patellofemoral compression. (Fig: B)
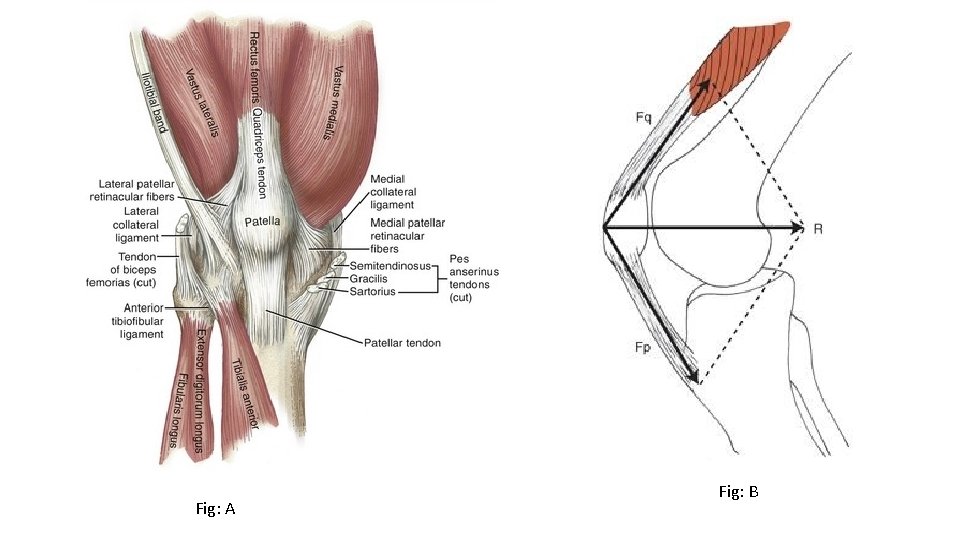
Fig: A Fig: B
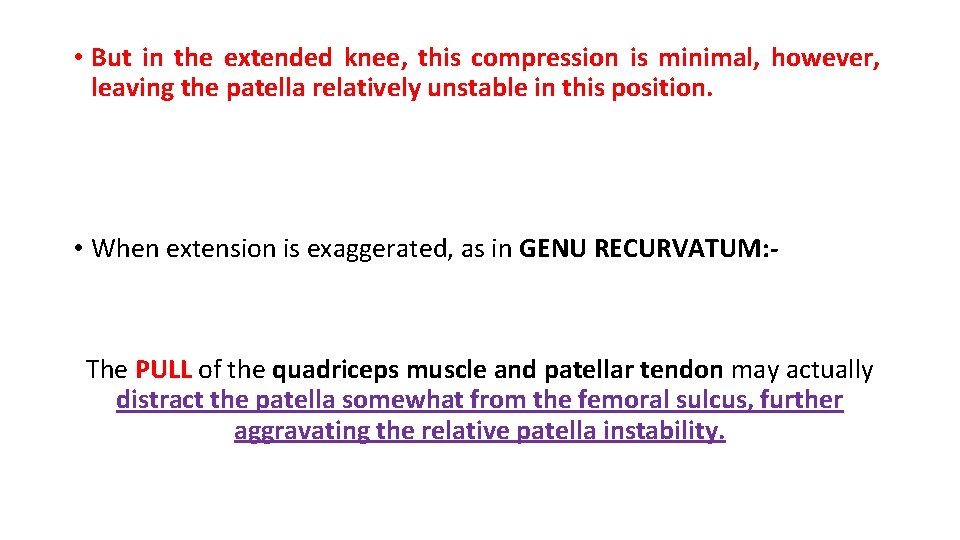
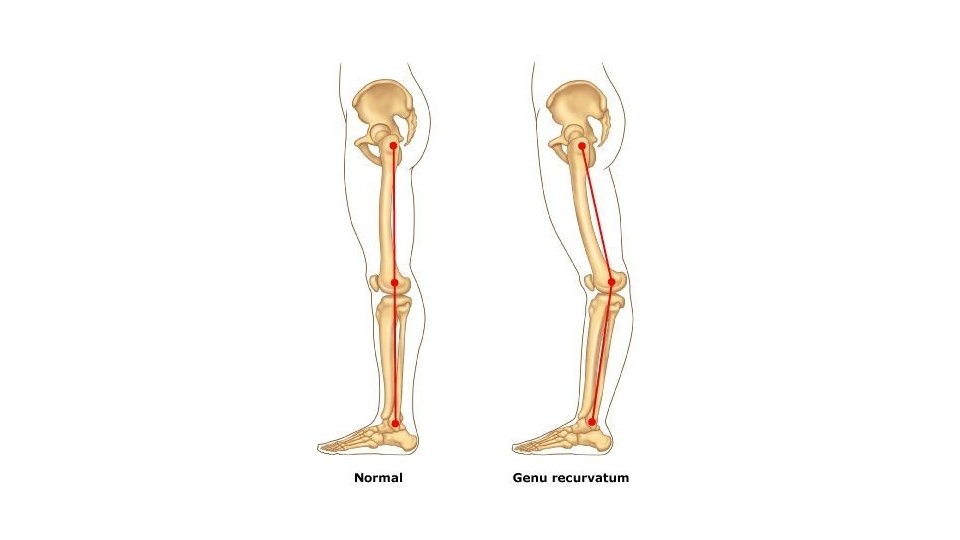
• But in the extended knee, this compression is minimal, however, leaving the patella relatively unstable in this position. • When extension is exaggerated, as in GENU RECURVATUM: - The PULL of the quadriceps muscle and patellar tendon may actually distract the patella somewhat from the femoral sulcus, further aggravating the relative patella instability.
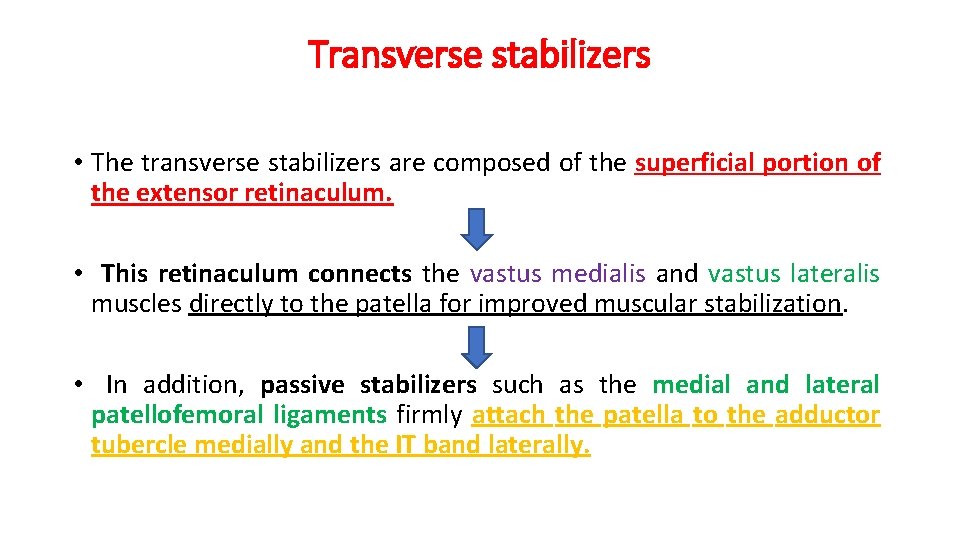
Transverse stabilizers • The transverse stabilizers are composed of the superficial portion of the extensor retinaculum. • This retinaculum connects the vastus medialis and vastus lateralis muscles directly to the patella for improved muscular stabilization. • In addition, passive stabilizers such as the medial and lateral patellofemoral ligaments firmly attach the patella to the adductor tubercle medially and the IT band laterally.
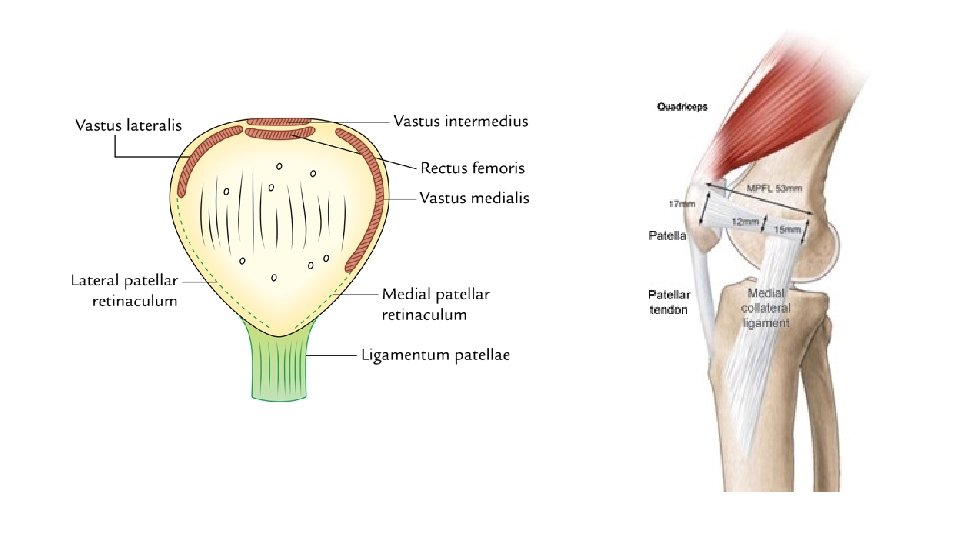
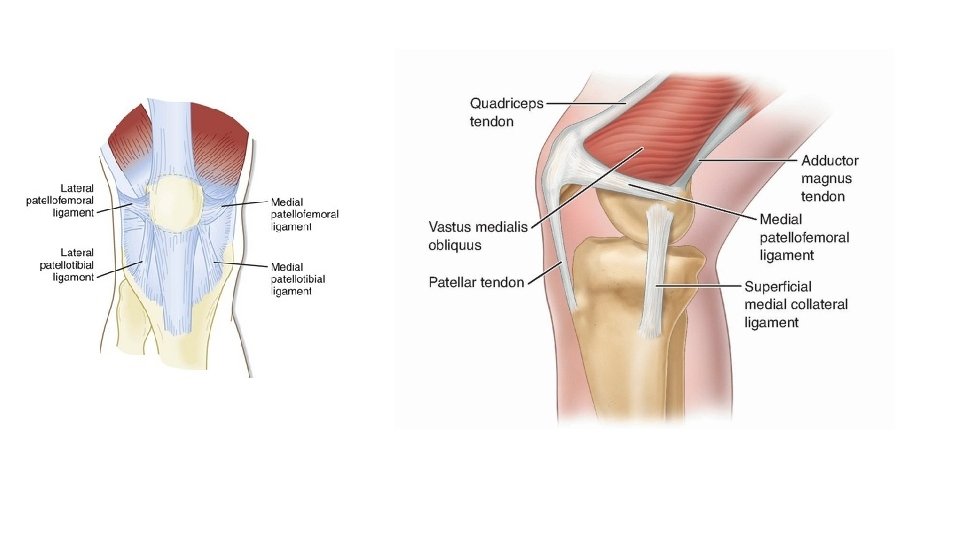
• The role of the medial patellofemoral ligament in assisting normal patellar tracking should not be understated. • As the thickest portion of the medial retinaculum, the medial patellofemoral ligament alone provides approximately 60% of the passive restraining force against lateral translation (lateral shift) of the patella.
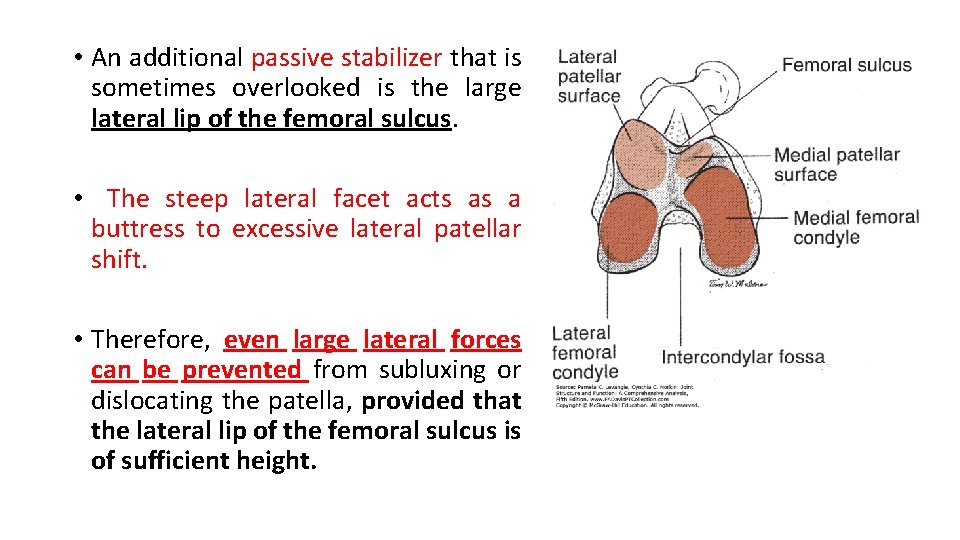
• An additional passive stabilizer that is sometimes overlooked is the large lateral lip of the femoral sulcus. • The steep lateral facet acts as a buttress to excessive lateral patellar shift. • Therefore, even large lateral forces can be prevented from subluxing or dislocating the patella, provided that the lateral lip of the femoral sulcus is of sufficient height.
• In the case of TROCHLEAR DYSPLASIA: relatively small lateral forces imposed on the patella can cause the patella to sublux or fully dislocate. • Both the transverse and the longitudinal structures will influence the medial-lateral positioning of the patella within the femoral sulcus, as well as influence patellar tracking as the patella slides down the femoral condyles and into the intercondylar groove.

Continued……. • The passive mobility of the patella and its medial- lateral positioning are largely governed by the passive and dynamic pulls of the structures surrounding it. • This is important because the presence of hypermobility could result in patellar subluxations or dislocations, whereas hypomobility could yield greater patellofemoral stresses. • Passive mobility of the patella is maximal when the knee is fully extended and the musculature is relaxed.
• An imbalance in the passive tension or a change in the line of pull of the dynamic structures will substantially influence the orientation of the patella. This is predominantly true when the knee joint is in extension and the patella sits on the relatively shallow superior femoral sulcus. • Abnormal forces, however, may influence the excursion of the patella even in its more secure location within the intercondylar groove with the knee in flexion.
• As already noted, tension in the active and/or stretched quadriceps muscle helps create compression between the patella and the femur to increase patellofemoral stability. • The force on the patella is determined by the resultant pull of the four muscles that constitute the quadriceps and by the pull of the patellar tendon. • Each of the segments of the quadriceps can make some contribution to frontal plane mobility and stability.
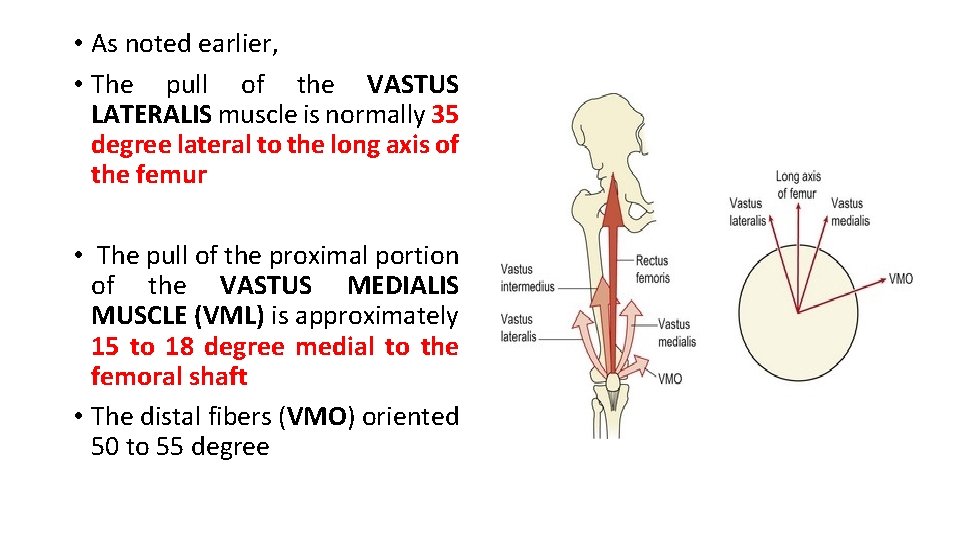
• As noted earlier, • The pull of the VASTUS LATERALIS muscle is normally 35 degree lateral to the long axis of the femur • The pull of the proximal portion of the VASTUS MEDIALIS MUSCLE (VML) is approximately 15 to 18 degree medial to the femoral shaft • The distal fibers (VMO) oriented 50 to 55 degree
• So the vastus medialis and vastus lateralis muscles not only pull on the quadriceps tendon but also exert a pull on the patella through their RETINACULAR CONNECTIONS, complementary function is critical. • Relative weakness of the vastus medialis muscle may substantially increase the resultant lateral forces on the patella. • The individual pulls of each respective portion of the quadriceps is impossible to measure in vivo, however.
• Although measurements of muscular force cannot be made, the literature supports the contention that muscle activity of the two portions of the vastus medialis (VMO and VML) and the vastus lateralis muscles are NOT selectively altered in patients with patellofemoral pain. • Anatomic variations may contribute to asymmetrical pulls on the patella. • In general, the VMO inserts into the superomedial aspect of the patella about one third to one half of the way down on the medial border.
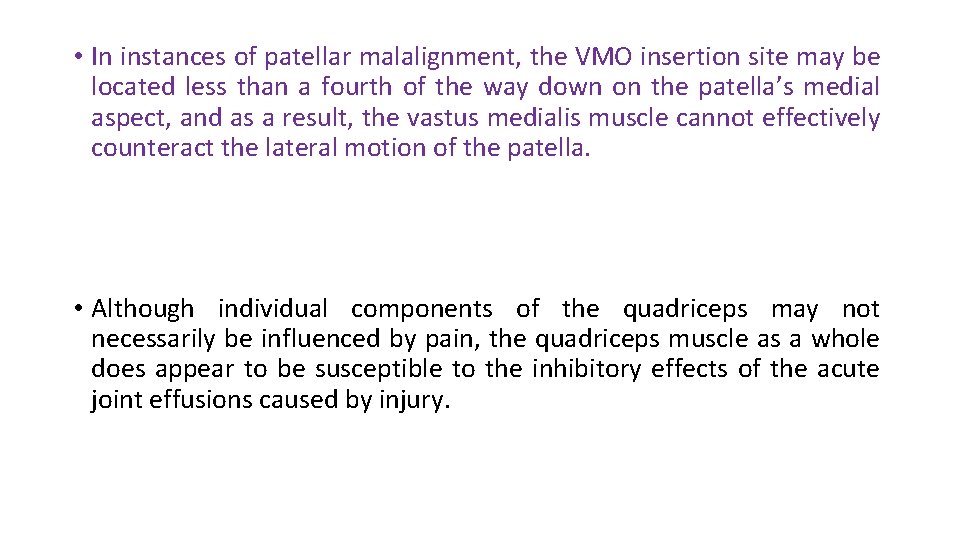
• In instances of patellar malalignment, the VMO insertion site may be located less than a fourth of the way down on the patella’s medial aspect, and as a result, the vastus medialis muscle cannot effectively counteract the lateral motion of the patella. • Although individual components of the quadriceps may not necessarily be influenced by pain, the quadriceps muscle as a whole does appear to be susceptible to the inhibitory effects of the acute joint effusions caused by injury.
• This inhibition can result in hypotonia and atrophy, minimizing the compressive role of the quadriceps and thus altering the resultant pull on the patella.
Thank you
- Slides: 26