From APLS courses to advanced simulation training A




- Slides: 27
From APLS courses to advanced simulation training: A tale of our journey Jos Draaisma & Ester Coolen
Outline • To start with APLS • Teaching pediatric emergencies: Why do we need simulation as an educational tool? • Prerequisites for transfer of training: How can we enhance tranfer of skills into daily clinical practice? • The importance of teaching team skills: How can we train and asses teamskills? - Situational leadership – Followership - Situational awareness • Challanges for our future training program
What is the purpose of APLS courses? • To improve the acute medical care by individual physicians and / or nurses of severly ill or traumatized children by improving • primary assessment / survey • resuscitation • secondary assessment • (sometimes) emergency treatment • definitive treatment
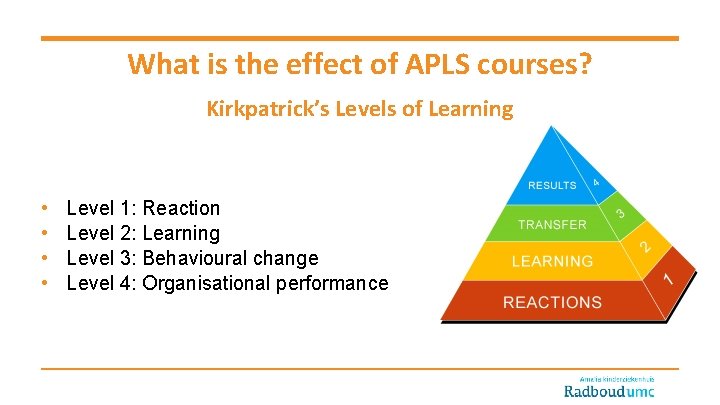
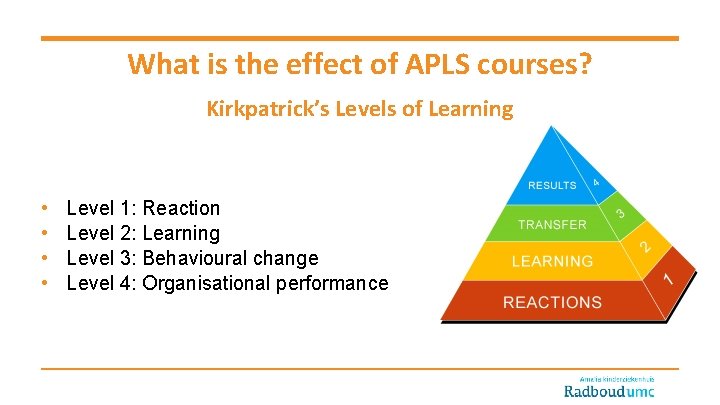
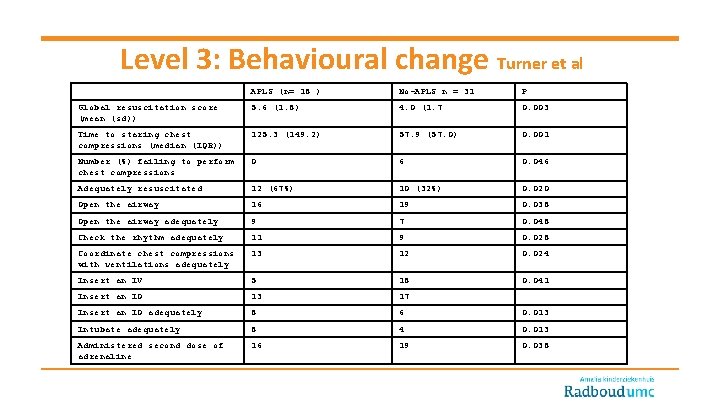
What is the effect of APLS courses? Kirkpatrick’s Levels of Learning • • Level 1: Reaction Level 2: Learning Level 3: Behavioural change Level 4: Organisational performance
Level 1: Self-efficacy Turner et al
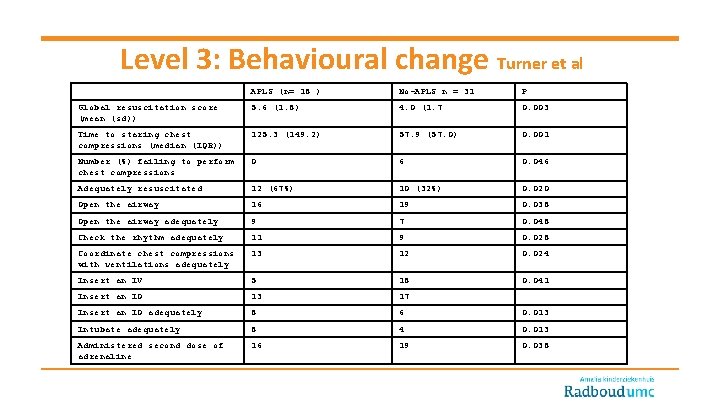
Level 3: Behavioural change Turner et al APLS (n= 18 ) No-APLS n = 31 P Global resuscitation score (mean (sd)) 5. 6 (1. 8) 4. 0 (1. 7 0. 003 Time to staring chest compressions (median (IQR)) 125. 3 (149. 2) 57. 9 (57. 0) 0. 001 Number (%) failing to perform chest compressions 0 6 0. 046 Adequately resuscitated 12 (67%) 10 (32%) 0. 020 Open the airway 16 19 0. 038 Open the airway adequately 9 7 0. 048 Check the rhythm adequately 11 9 0. 028 Coordinate chest compressions with ventilations adequately 13 12 0. 024 Insert an IV 5 18 0. 041 Insert an IO 13 17 Insert an IO adequately 8 6 0. 013 Intubate adequately 8 4 0. 013 Administered second dose of adrenaline 16 19 0. 038

From a team of experts to an expert team
• • Members of pediatric teams are expected to share a common goal, also called a “shared mental model “ Although team members are sufficiently trained individually; team work skills have traditionally been less emphasized in medical training
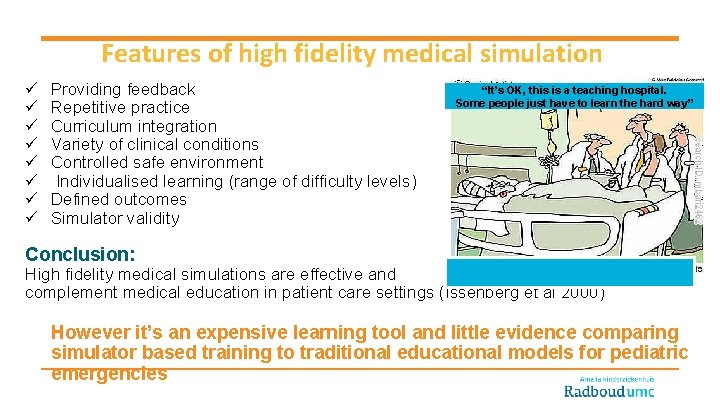
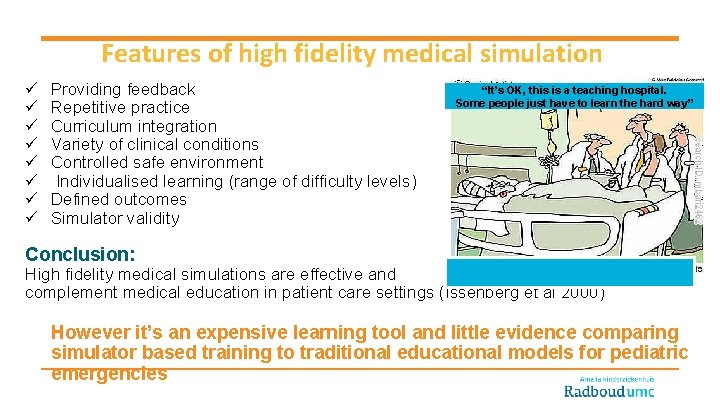
Features of high fidelity medical simulation ü ü ü ü Providing feedback Repetitive practice Curriculum integration Variety of clinical conditions Controlled safe environment Individualised learning (range of difficulty levels) Defined outcomes Simulator validity “It’s OK, this is a teaching hospital. Some people just have to learn the hard way” Conclusion: High fidelity medical simulations are effective and complement medical education in patient care settings (Issenberg et al 2000) However it’s an expensive learning tool and little evidence comparing simulator based training to traditional educational models for pediatric emergencies

Additional value of VARS model over traditional educational models PBL EPLS Effectiveness of high fidelity video-assisted real-time simulation: a comparison of three training methods for acute pediatric emergencies. Coolen EH & Draaisma JM, et al. -Scores on the post-intervention scenarios were significantly higher for all groups -The VARS-group showed significantly (p<0. 05) higher scores on both post-intervention scenario’s in structure and timely achievement of critial actions VARS
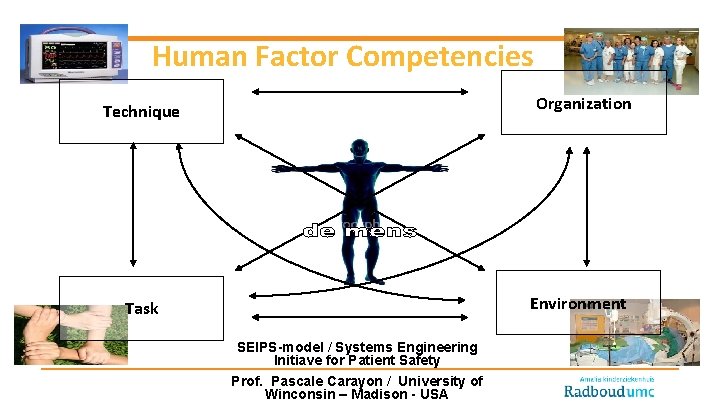
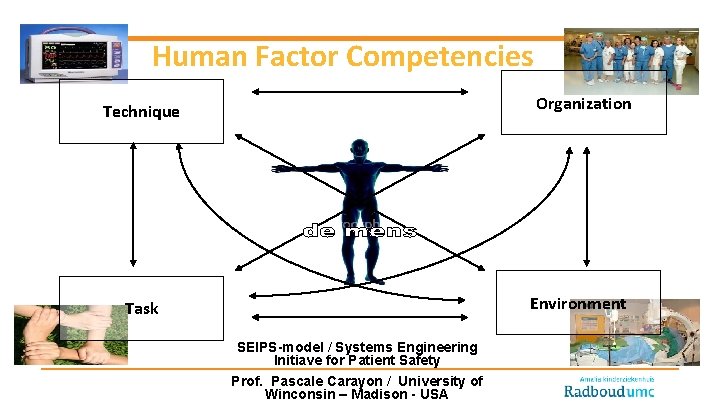
Human Factor Competencies Organization Technique Environment Task SEIPS-model / Systems Engineering Initiave for Patient Safety Prof. Pascale Carayon / University of Winconsin – Madison - USA
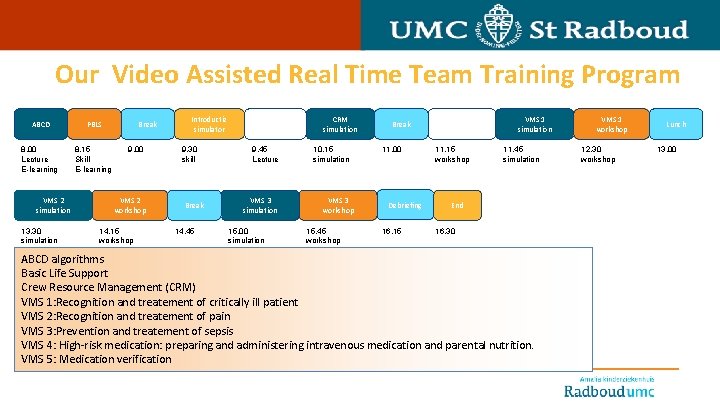
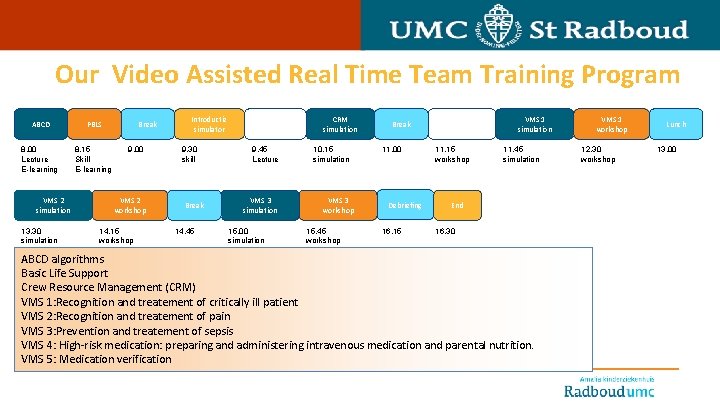
Our Video Assisted Real Time Team Training Program ABCD PBLS 8. 00 Lecture E-learning 8. 15 Skill E-learning VMS 2 simulation 13. 30 simulation Break 9. 00 VMS 2 workshop 14. 15 workshop Introductie simulator 9. 30 skill Break 14. 45 CRM principes 9. 45 Lecture VMS 3 simulation 15. 00 simulation CRM simulation 10. 15 simulation VMS 3 workshop 15. 45 workshop Break 11. 00 Debriefing 16. 15 CRM workshop 11. 15 workshop VMS 1 simulation 11. 45 simulation End 16. 30 ABCD algorithms Basic Life Support Crew Resource Management (CRM) VMS 1: Recognition and treatement of critically ill patient VMS 2: Recognition and treatement of pain VMS 3: Prevention and treatement of sepsis VMS 4: High-risk medication: preparing and administering intravenous medication and parental nutrition. VMS 5: Medication verification VMS 1 workshop 12. 30 workshop Lunch 13. 00

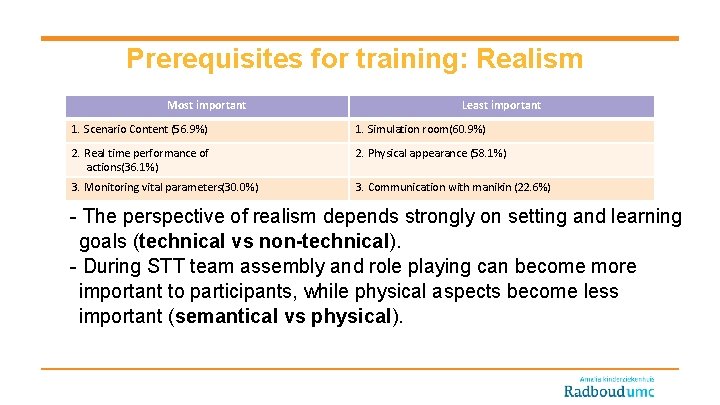
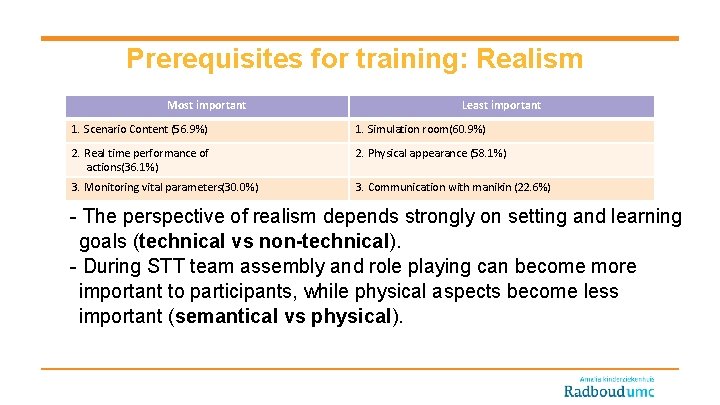
Prerequisites for training: Realism Most important Least important 1. Scenario Content (56. 9%) 1. Simulation room(60. 9%) 2. Real time performance of actions(36. 1%) 2. Physical appearance (58. 1%) 3. Monitoring vital parameters(30. 0%) 3. Communication with manikin (22. 6%) - The perspective of realism depends strongly on setting and learning goals (technical vs non-technical). - During STT team assembly and role playing can become more important to participants, while physical aspects become less important (semantical vs physical).
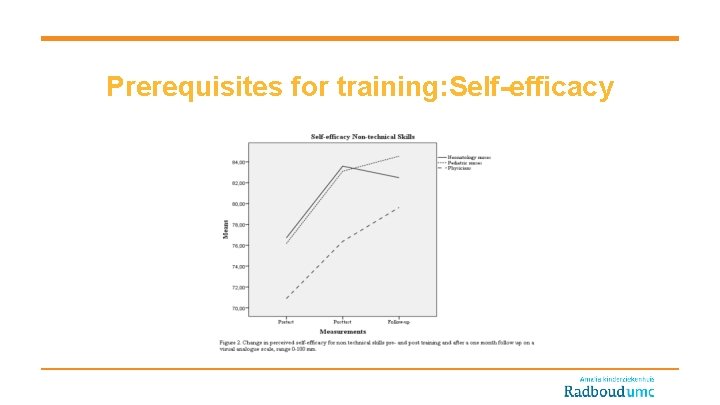
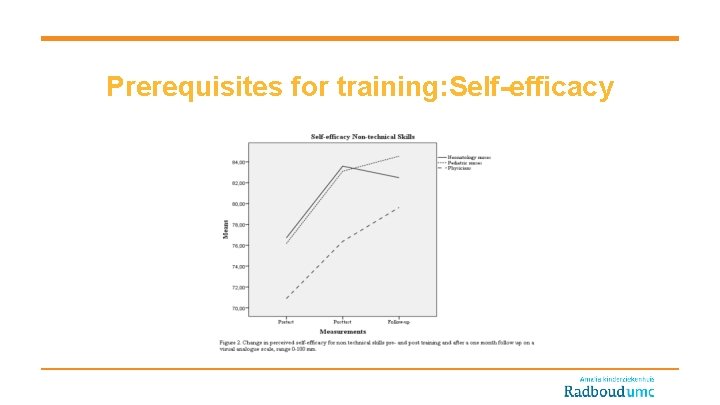
Prerequisites for training: Self-efficacy
Leadership skills
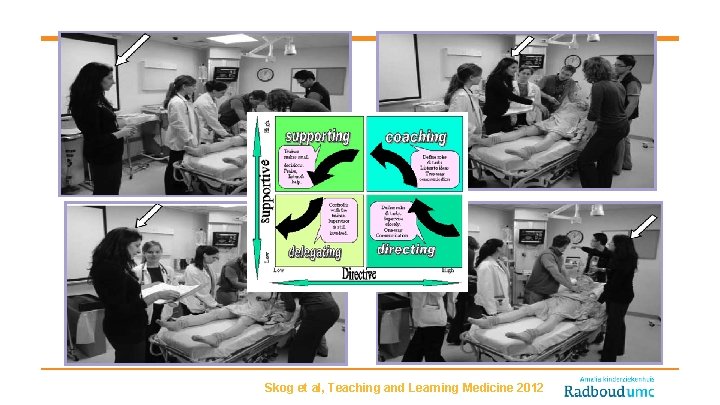
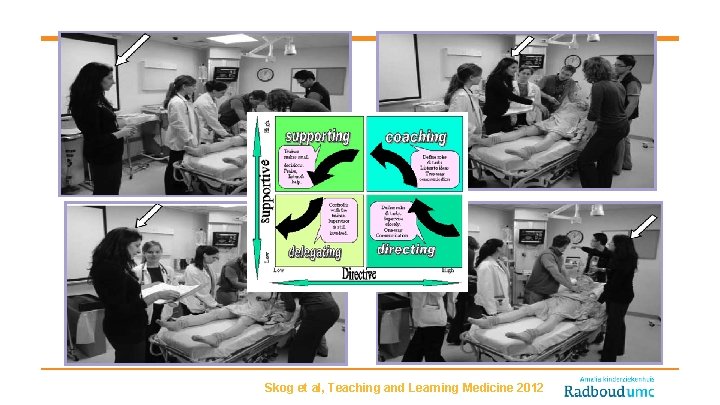
Skog et al, Teaching and Learning Medicine 2012
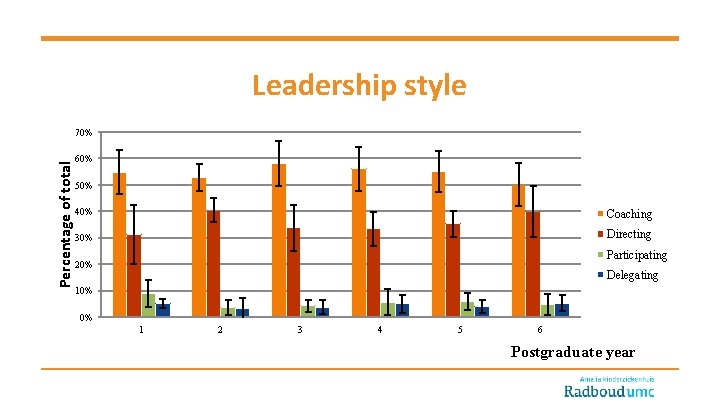
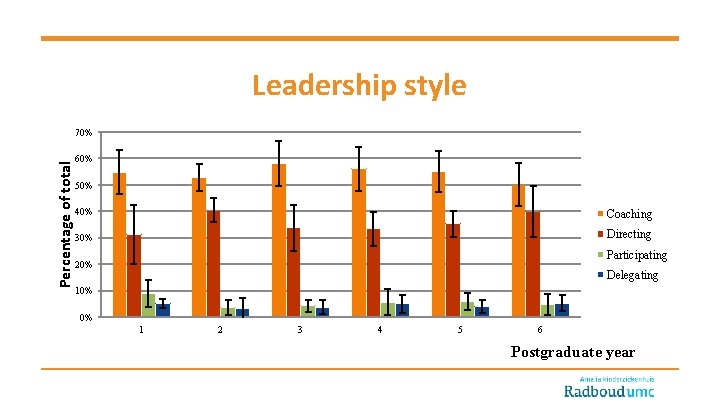
Leadership style Percentage of total 70% 60% 50% 40% Coaching 30% Directing Participating 20% Delegating 10% 0% 1 2 3 4 5 6 Postgraduate year
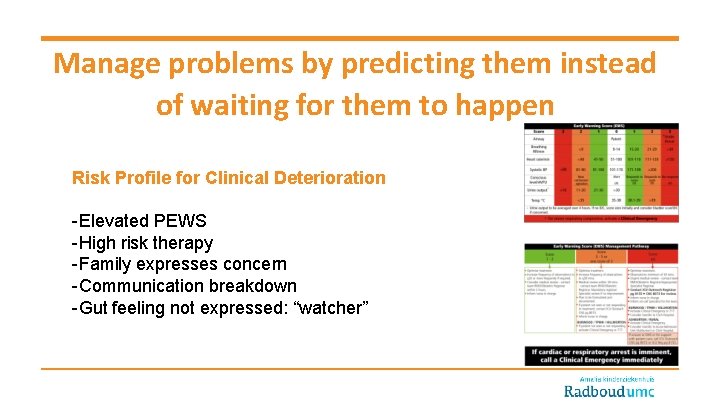
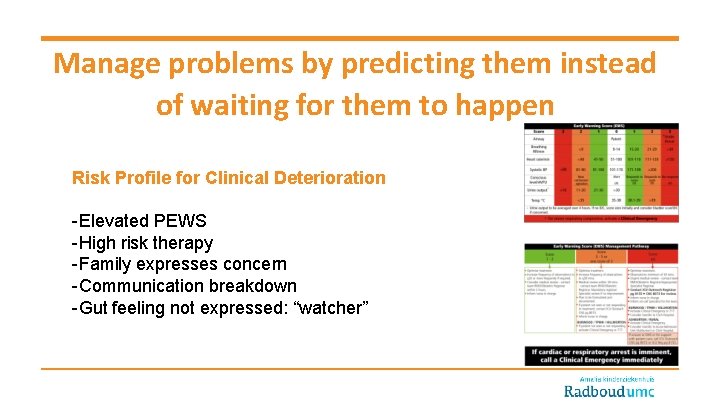
Manage problems by predicting them instead of waiting for them to happen Risk Profile for Clinical Deterioration -Elevated PEWS -High risk therapy -Family expresses concern -Communication breakdown -Gut feeling not expressed: “watcher”
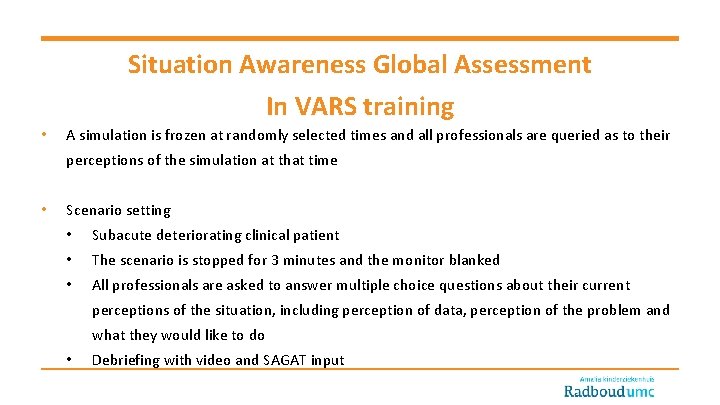
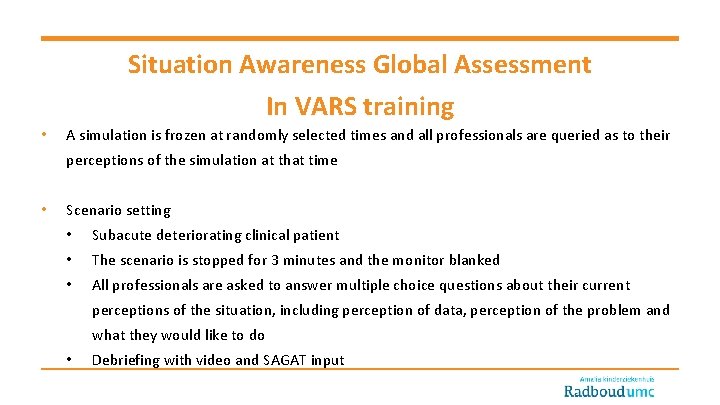
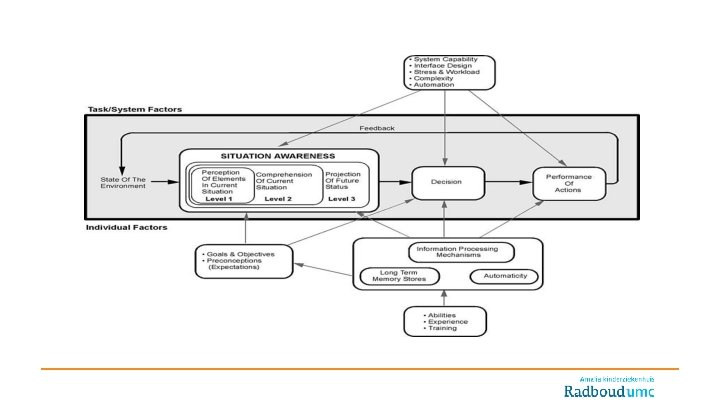
Situation Awareness Global Assessment In VARS training • A simulation is frozen at randomly selected times and all professionals are queried as to their perceptions of the simulation at that time • Scenario setting • Subacute deteriorating clinical patient • The scenario is stopped for 3 minutes and the monitor blanked • All professionals are asked to answer multiple choice questions about their current perceptions of the situation, including perception of data, perception of the problem and what they would like to do • Debriefing with video and SAGAT input
Experiences with SAGA • The disturbance by “freeze” is minimal: time-out can increase individual SA • Complementary SA of nurses may lead to miscommunication • Perception of leadership differs between nusrses and physicians • The mark for teamwork is mainly given as a consequence of the perception of importance of everybody’s own task
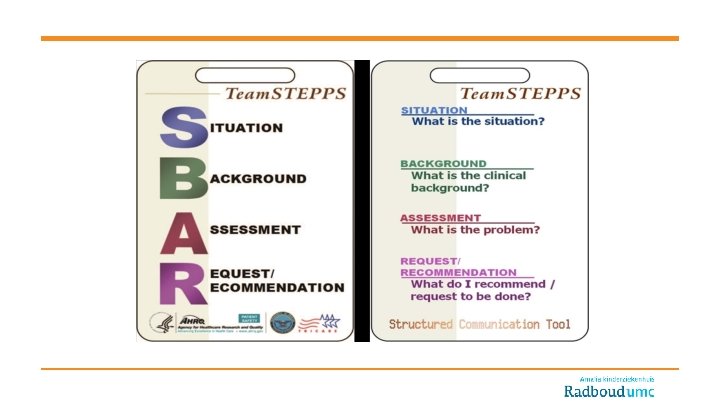
For effective team work: • Explicitely improve speak-up • Leadership may be composed of two tasks: hands-on (management) and hands-off (overview) • Leadership is not only the allocation of tasks, but also the evaluation and correction of individual and teamtasks • Share alternatives with the team
Challenges for our future training program • Measuring Situational Awareness during Clinical Practice • Training inter-professional teams: e. g. gynecologists, emergency physicians, pediatric surgeons • Competition with other patient safety programs / government obligations • Time and Money

Thank you for your attention