Free Powerpoint Templates Page 1 Fluid and electrolytes
















- Slides: 154

Free Powerpoint Templates Page 1
Fluid and electrolytes balance Unit ten
Body fluid and electrolyte: • About 46 to 6 o % of the average adult weight is water.
• The proportion of water decreases with aging because fat, age and sex effect of total body water. • (Infant 70 – 80%).
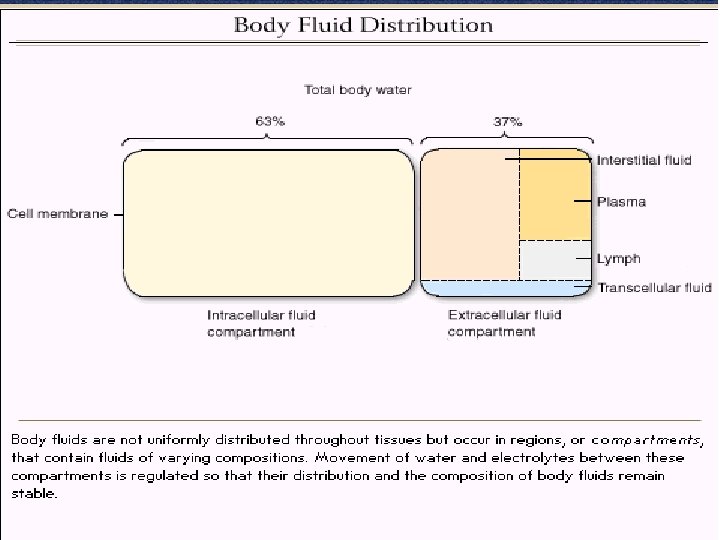
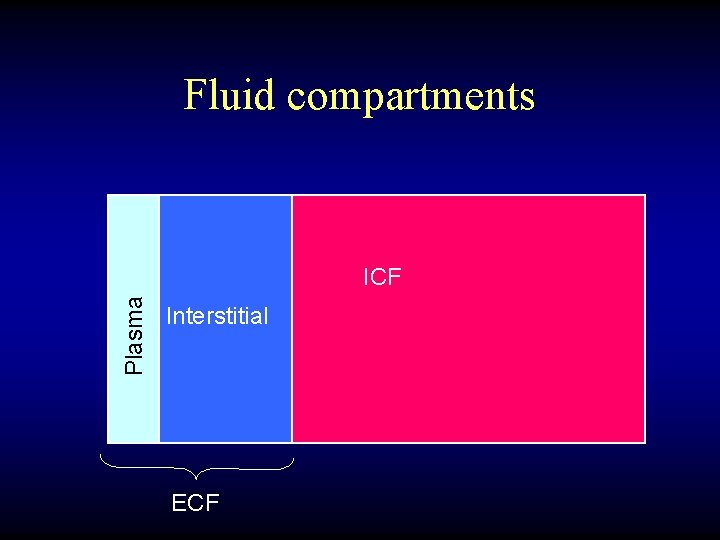
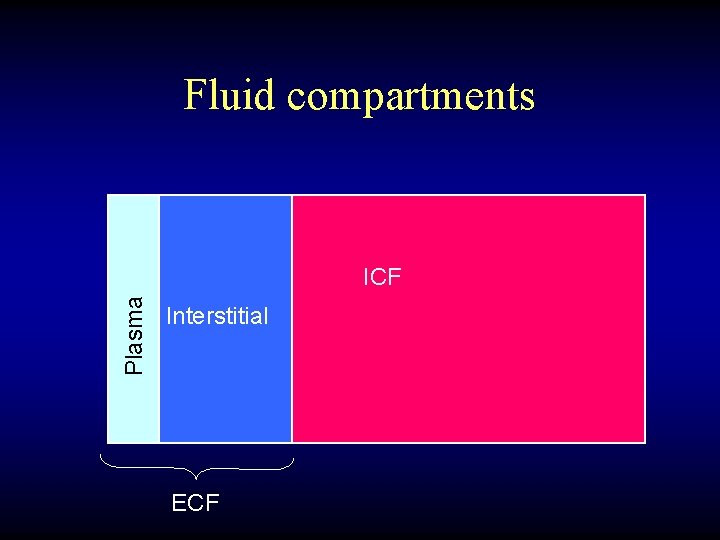
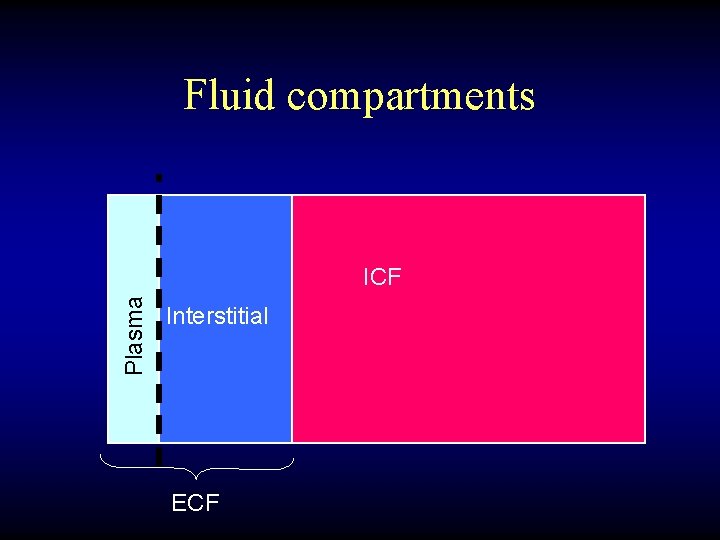
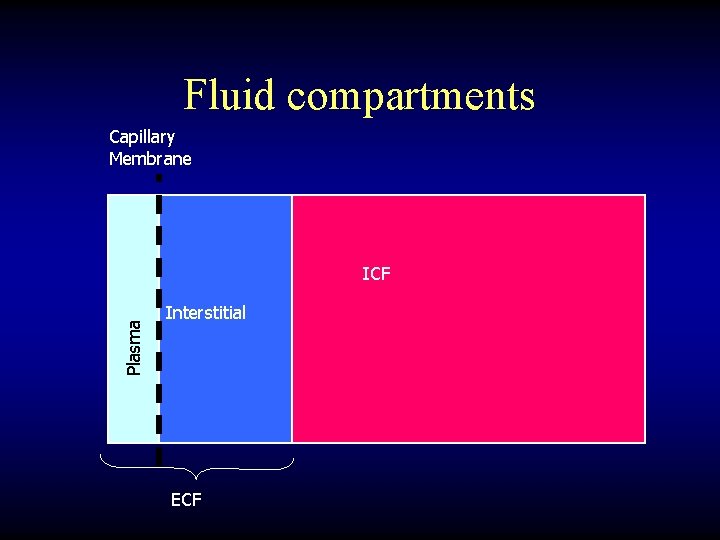
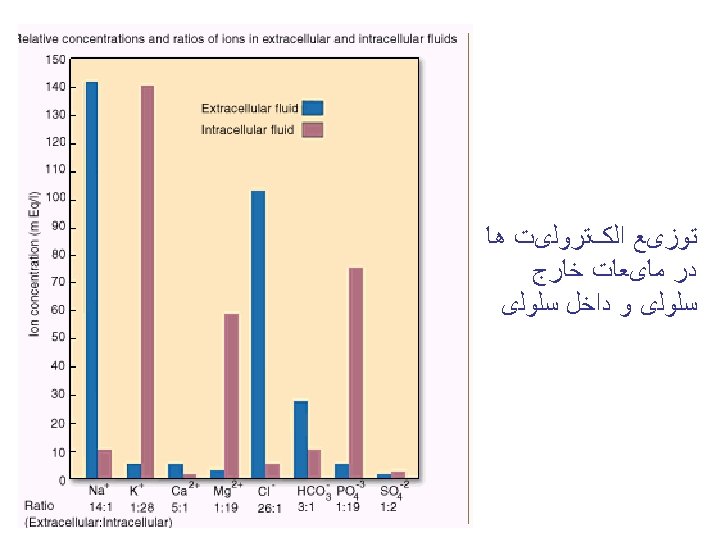
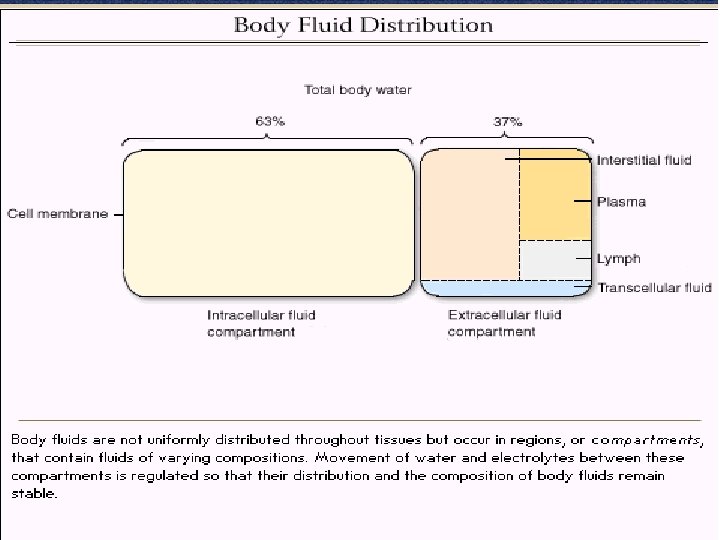
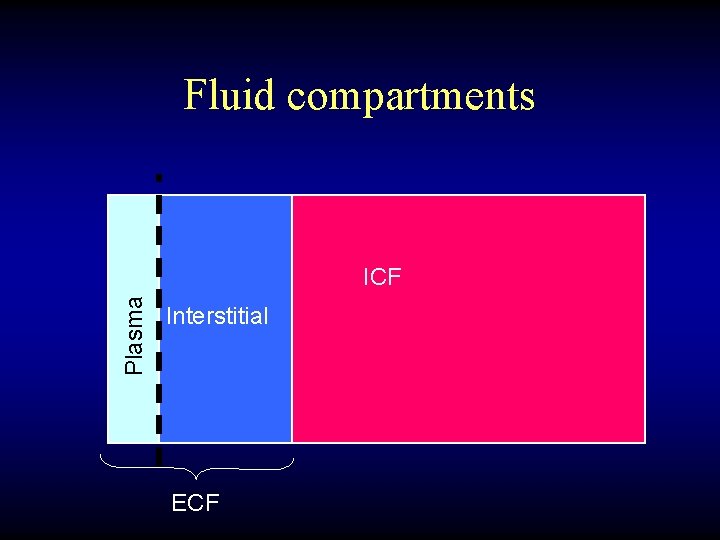
Distribution of body fluids: • The body fluid divided in two major compartments: A) Intracellular fluid (ICF): • Is found in the cells of the body. its constitute 2/3 of the total body fluid in the adult.
b) Extracelluar fluid (ECF): • is found out side of cell and account 1/3 of the total body fluid. • it’s subdivided into three compartments: 1) Intravascular fluid or plasma: is found within vascular system. 2) Interstitial fluid: is found surrounding the cell and includes lymph. 3) Transcellular: includes cerebrospinal fluid, pleural, peritoneal and synovial fluid.

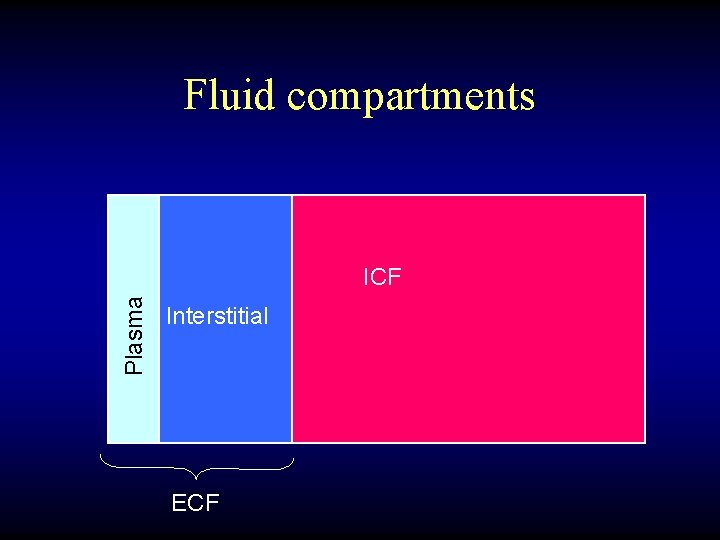
Fluid compartments Plasma ICF Interstitial ECF
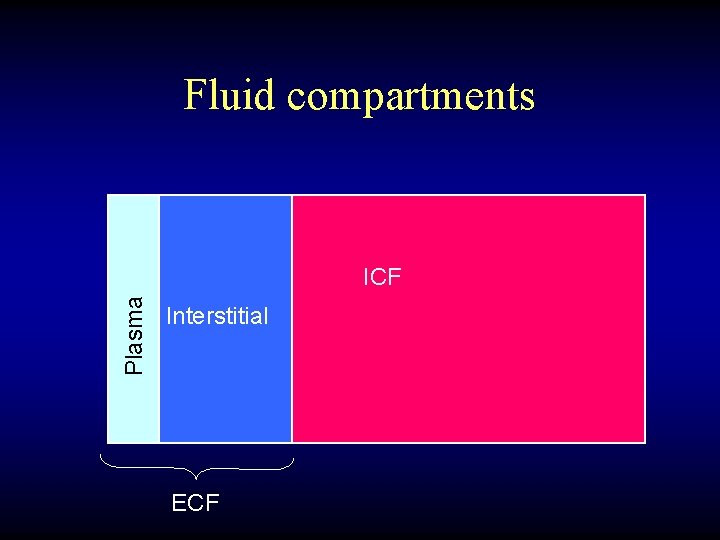
Fluid compartments Plasma ICF Interstitial ECF
Fluid compartments Plasma ICF Interstitial ECF
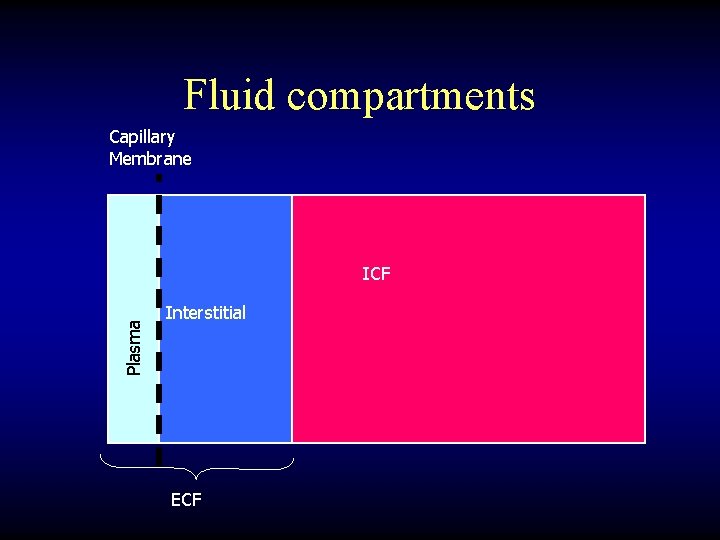
Fluid compartments Capillary Membrane Plasma ICF Interstitial ECF
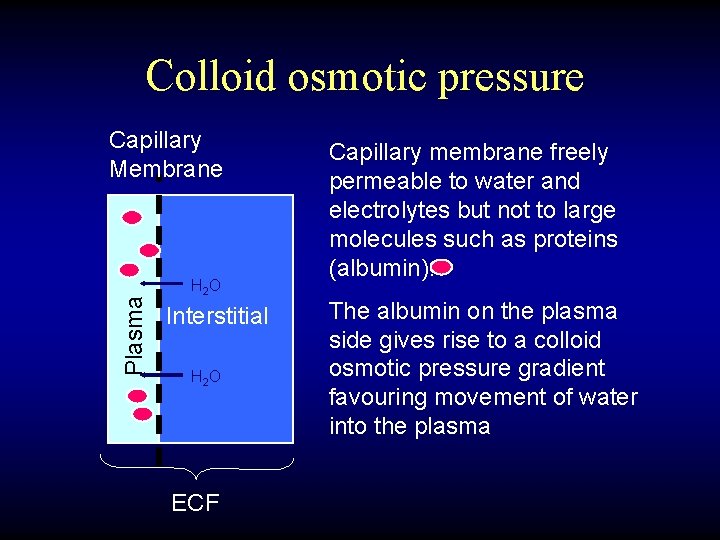
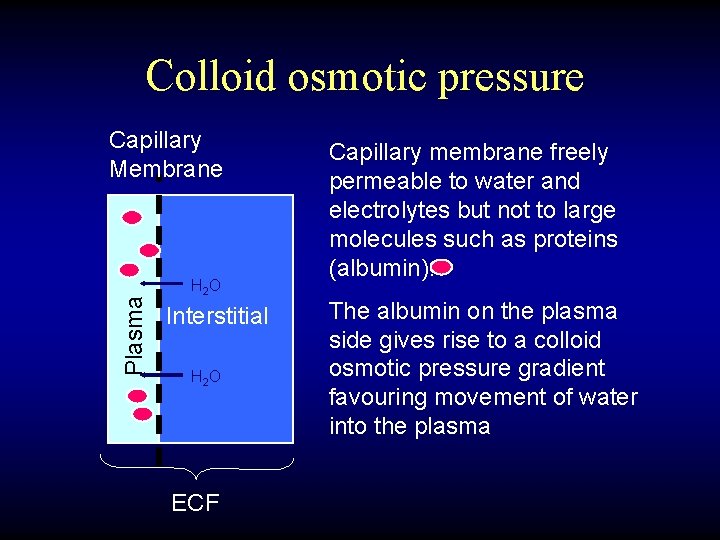
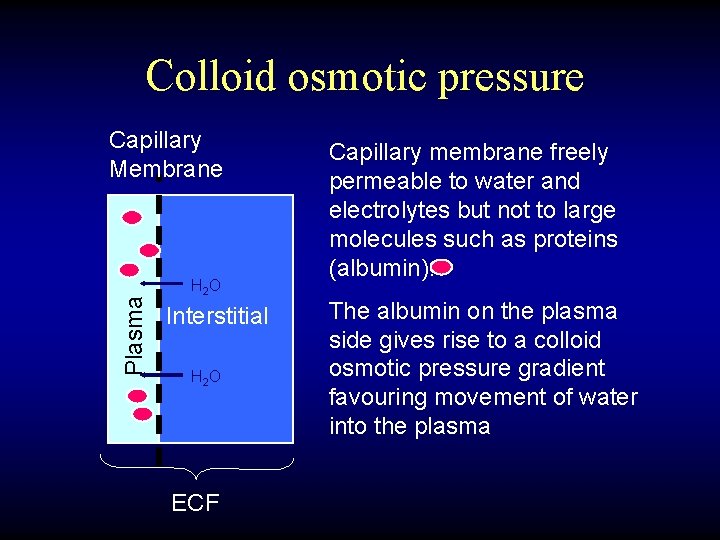
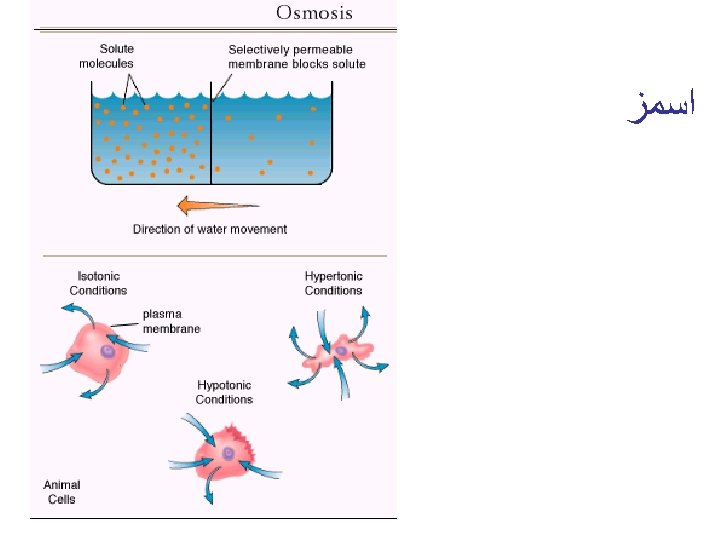
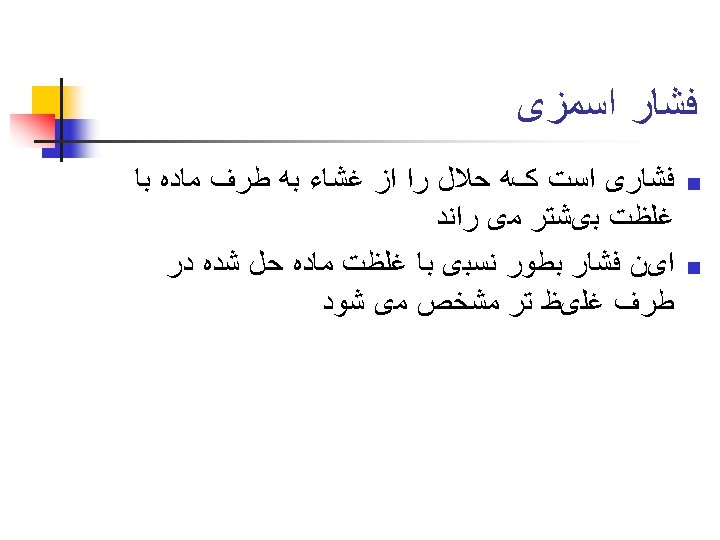
Colloid osmotic pressure Plasma Capillary Membrane H 2 O Interstitial H 2 O ECF Capillary membrane freely permeable to water and electrolytes but not to large molecules such as proteins (albumin). The albumin on the plasma side gives rise to a colloid osmotic pressure gradient favouring movement of water into the plasma
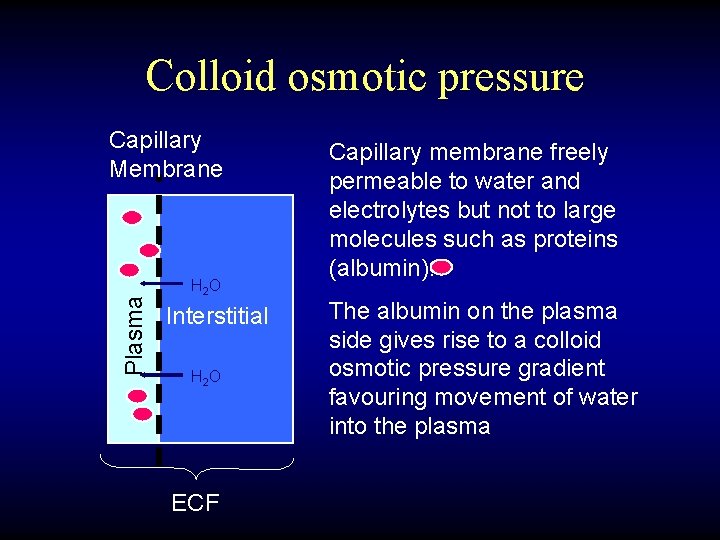
Colloid osmotic pressure Plasma Capillary Membrane H 2 O Interstitial H 2 O ECF Capillary membrane freely permeable to water and electrolytes but not to large molecules such as proteins (albumin). The albumin on the plasma side gives rise to a colloid osmotic pressure gradient favouring movement of water into the plasma
Fluids • Crystalloids • Colloids • blood
Which of the following solutions is isotonic? A. D 5 W B. 0. 45% saline C. 0. 9% saline D. D 5 in 0. 9% saline
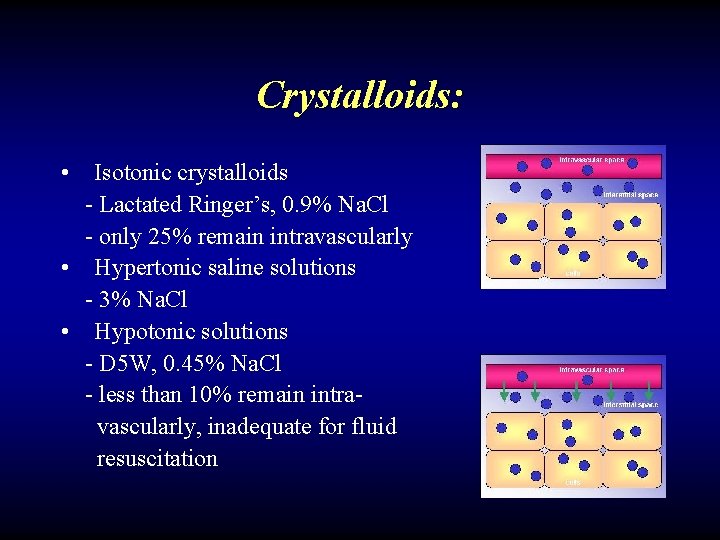
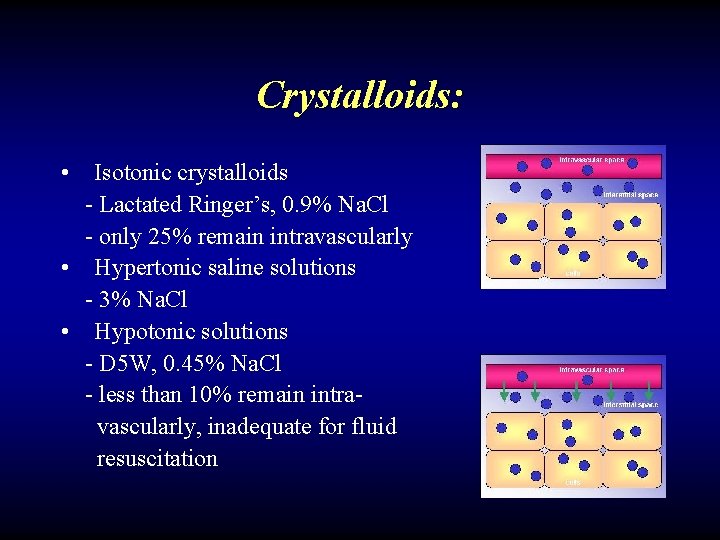
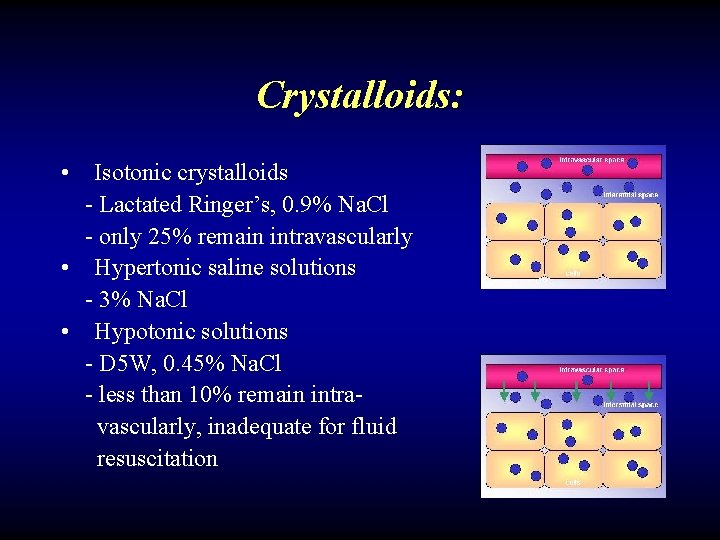
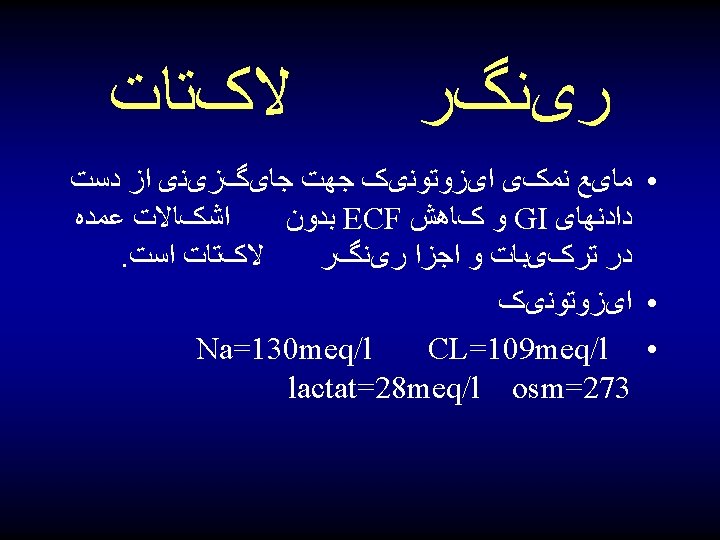
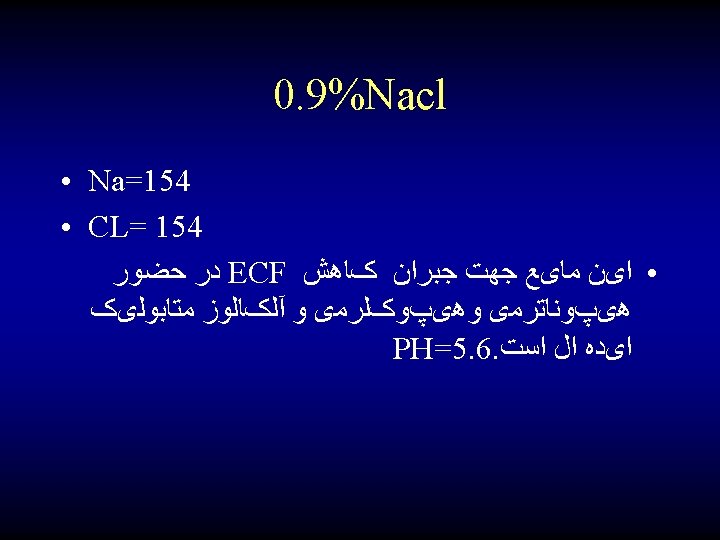
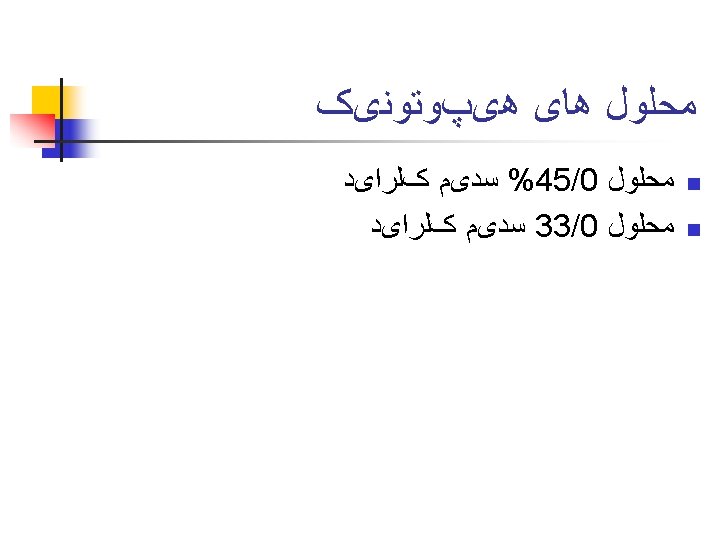
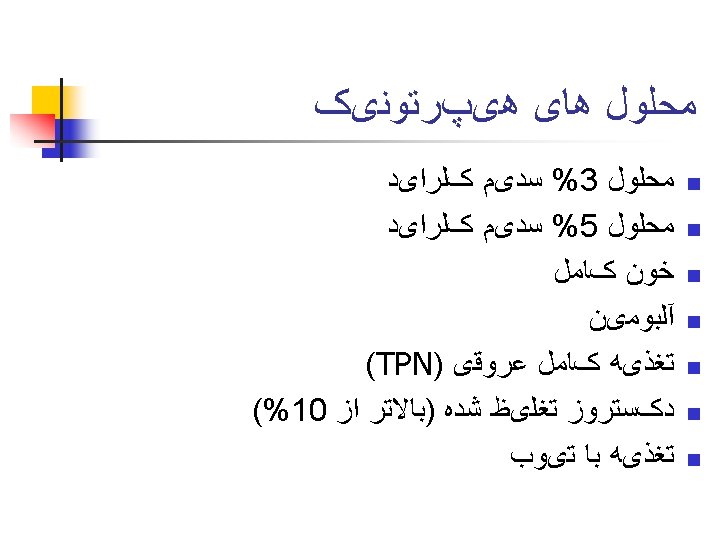
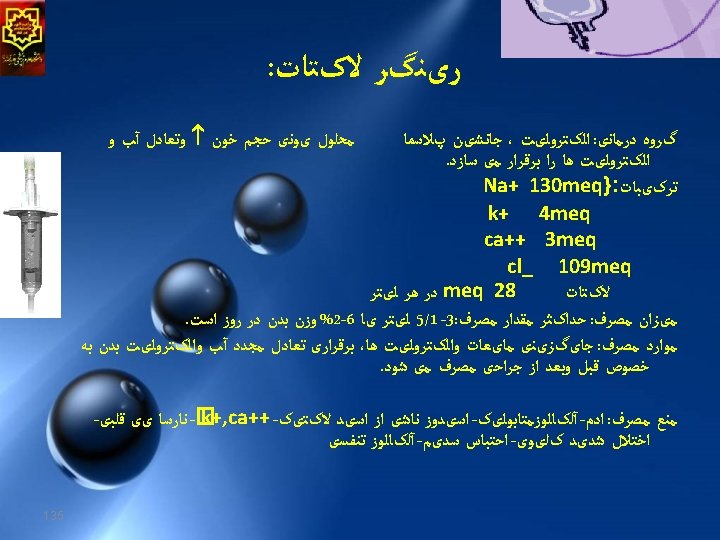
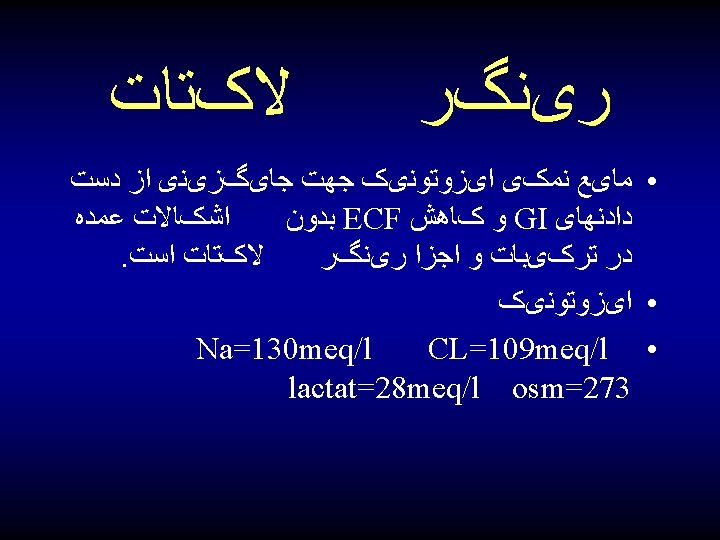
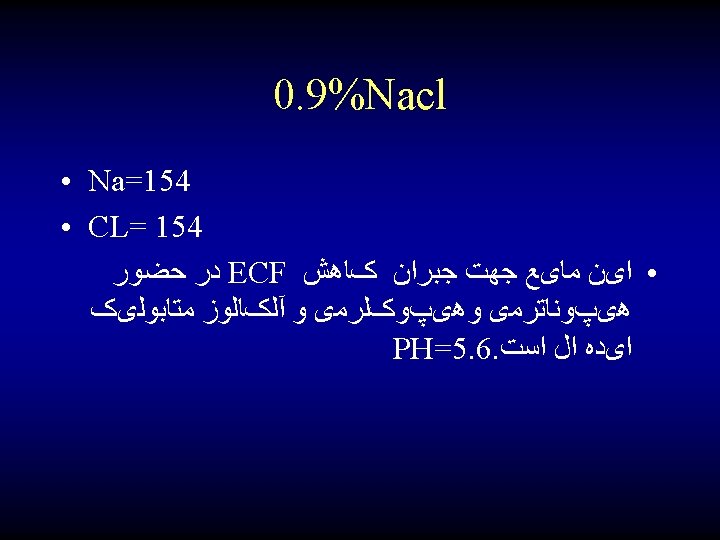
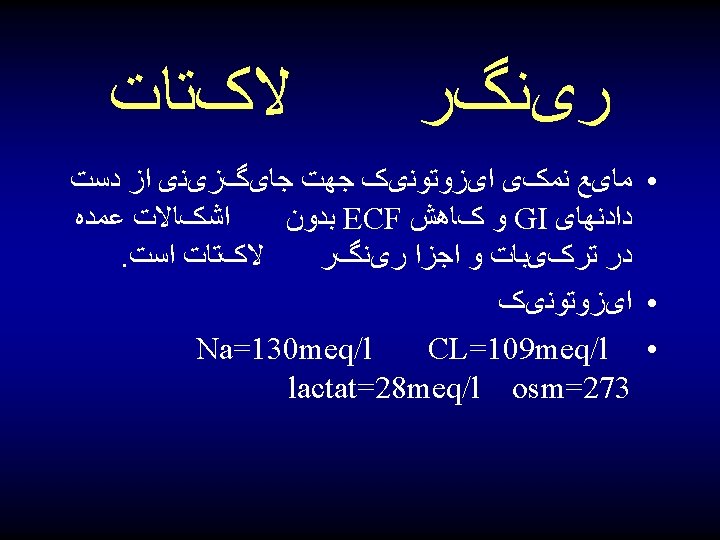
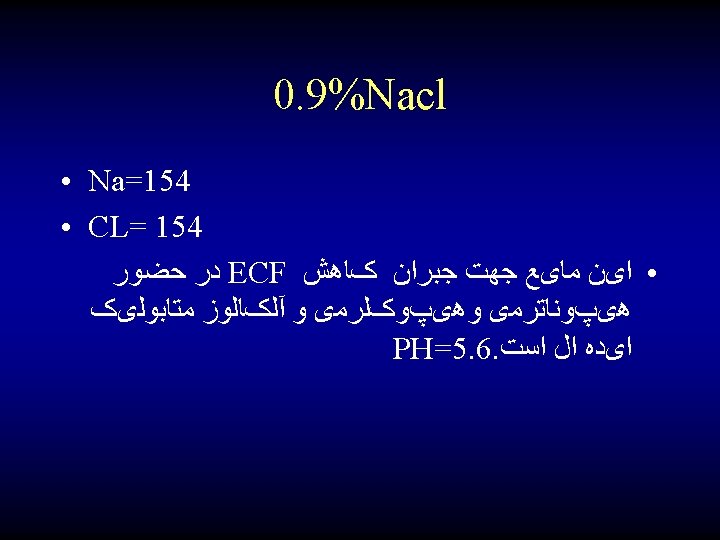
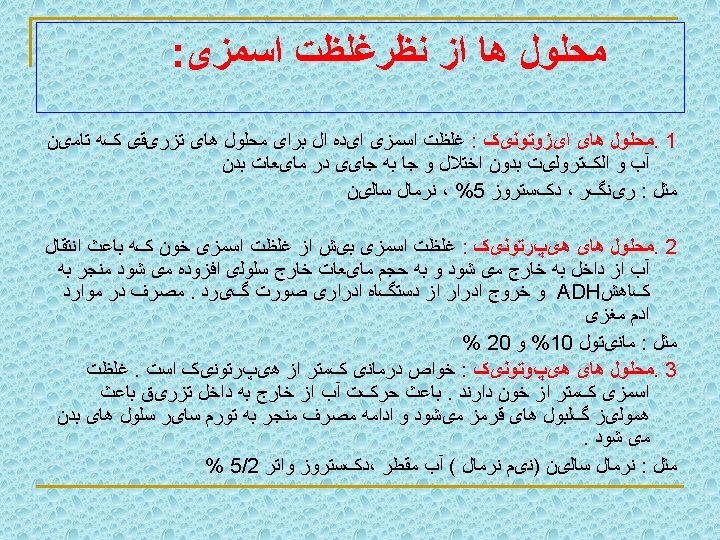
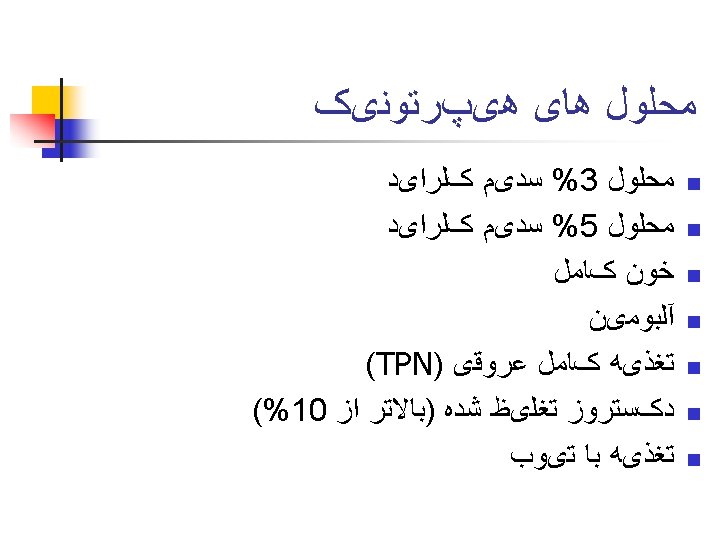
Crystalloids: • Isotonic crystalloids - Lactated Ringer’s, 0. 9% Na. Cl - only 25% remain intravascularly • Hypertonic saline solutions - 3% Na. Cl • Hypotonic solutions - D 5 W, 0. 45% Na. Cl - less than 10% remain intravascularly, inadequate for fluid resuscitation
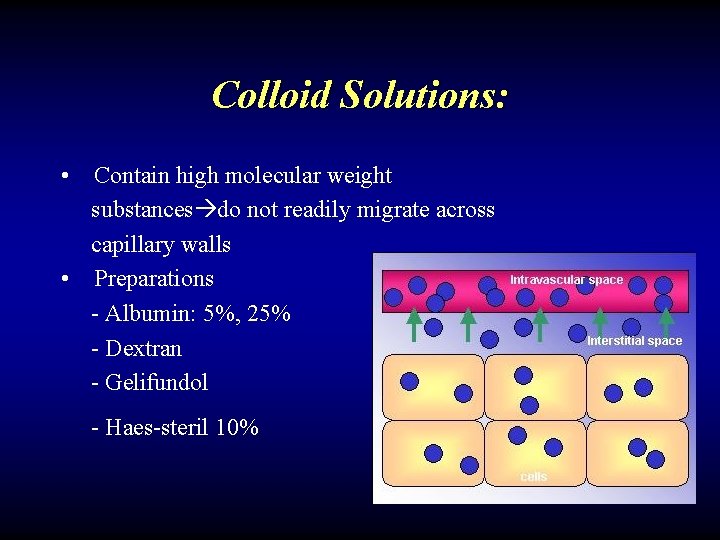
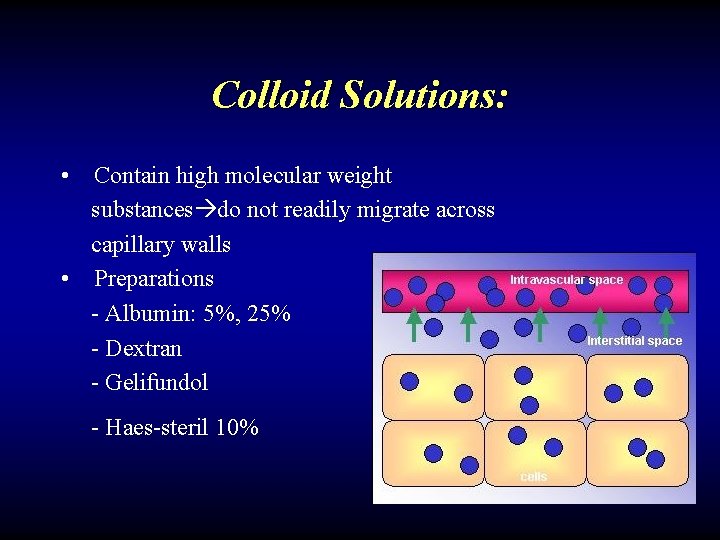
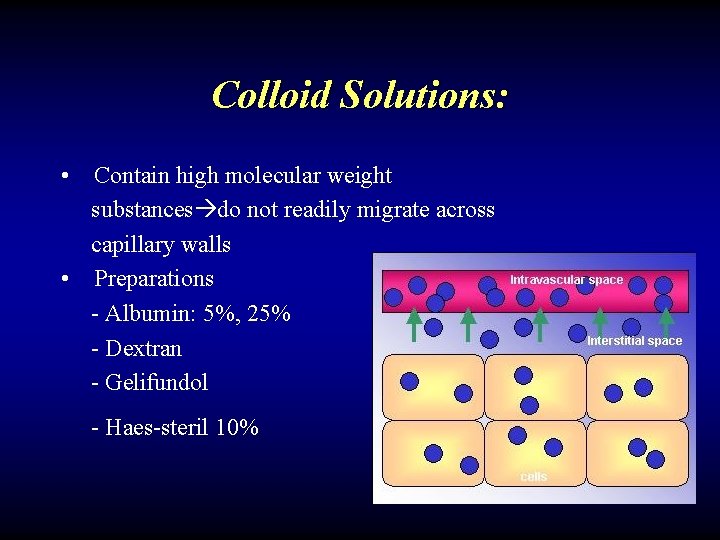
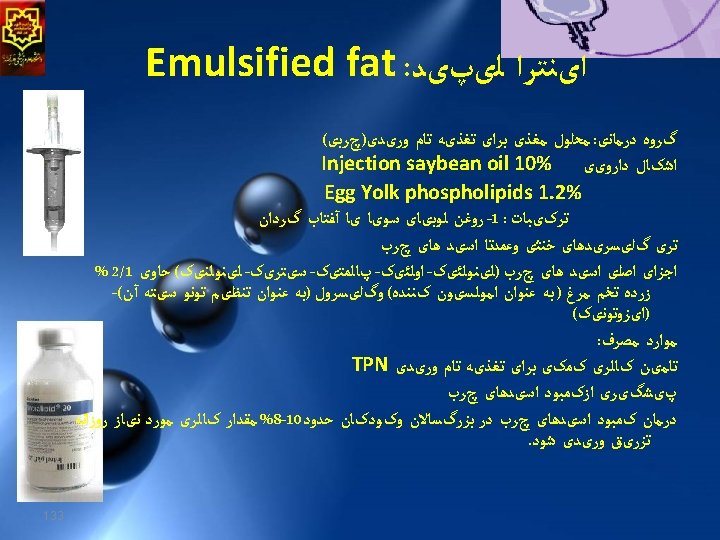
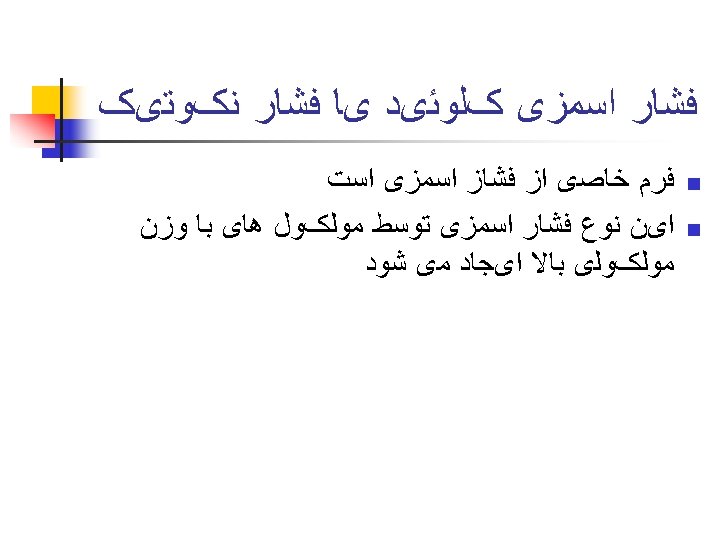
Colloid Solutions: • Contain high molecular weight substances do not readily migrate across capillary walls • Preparations - Albumin: 5%, 25% - Dextran - Gelifundol - Haes-steril 10%
Perioperative management of fluid balance include: 1. Preoperative evaluation 2. Intraoperative maintenance 3. Replacement of fluid losses
Perioperative management of fluid balance include: 1. Preoperative evaluation 2. Intraoperative maintenance 3. Replacement of fluid losses
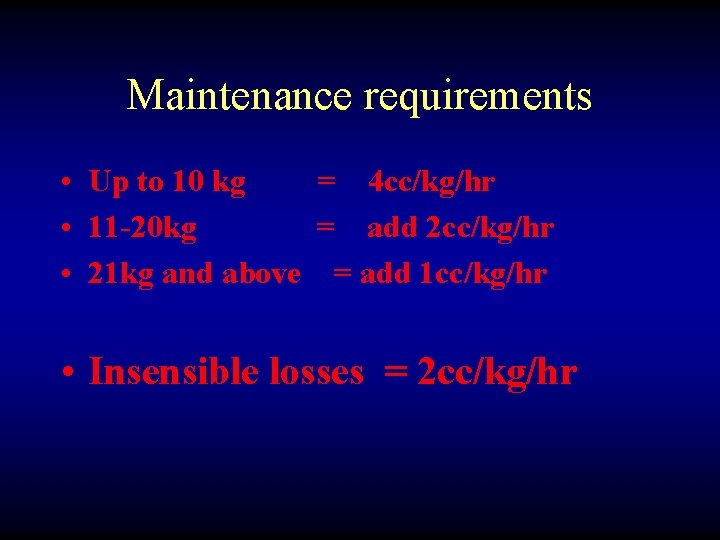
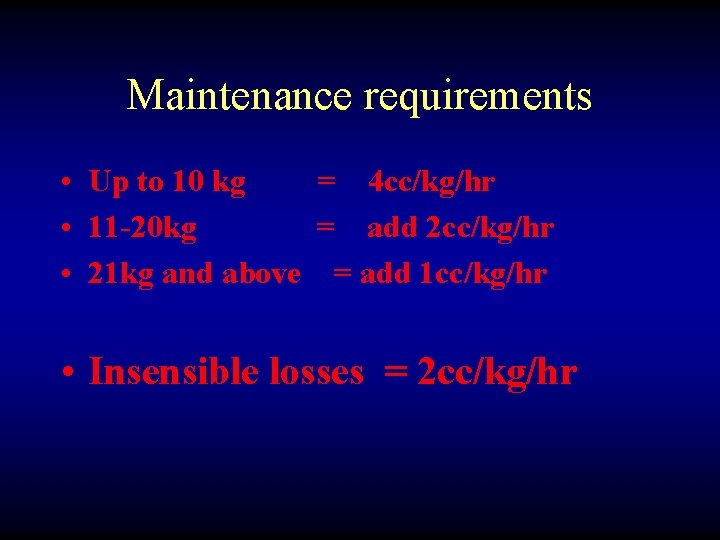
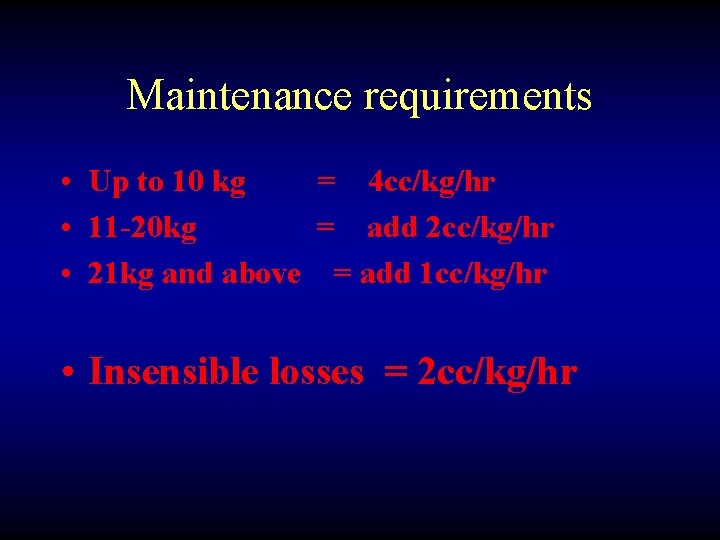
Maintenance requirements • Up to 10 kg = 4 cc/kg/hr • 11 -20 kg = add 2 cc/kg/hr • 21 kg and above = add 1 cc/kg/hr • Insensible losses = 2 cc/kg/hr
Fluids • Crystalloids • Colloids • blood
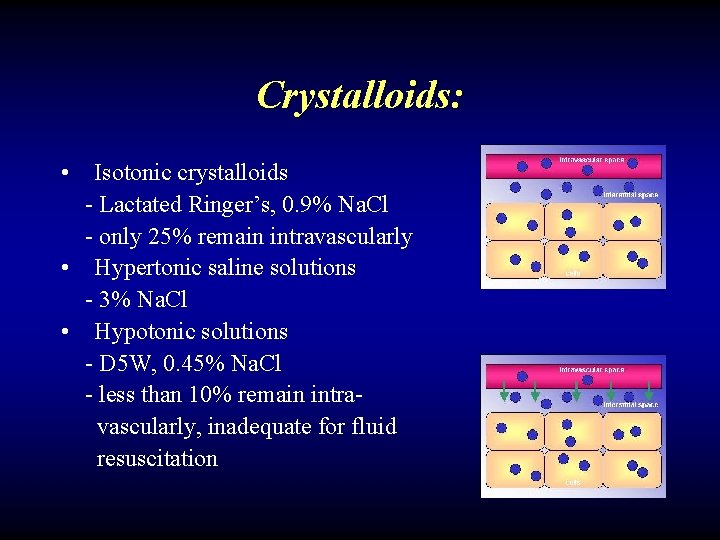
Crystalloids: • Isotonic crystalloids - Lactated Ringer’s, 0. 9% Na. Cl - only 25% remain intravascularly • Hypertonic saline solutions - 3% Na. Cl • Hypotonic solutions - D 5 W, 0. 45% Na. Cl - less than 10% remain intravascularly, inadequate for fluid resuscitation
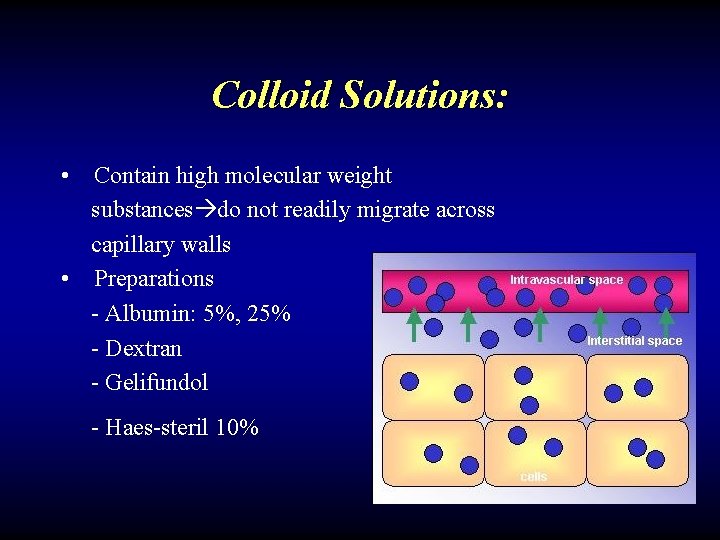
Colloid Solutions: • Contain high molecular weight substances do not readily migrate across capillary walls • Preparations - Albumin: 5%, 25% - Dextran - Gelifundol - Haes-steril 10%
Perioperative management of fluid balance include: 1. Preoperative evaluation 2. Intraoperative maintenance 3. Replacement of fluid losses
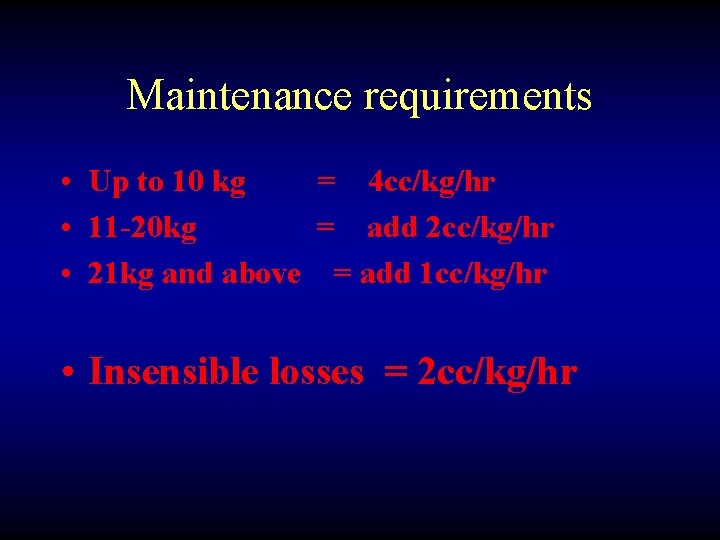
Maintenance requirements • Up to 10 kg = 4 cc/kg/hr • 11 -20 kg = add 2 cc/kg/hr • 21 kg and above = add 1 cc/kg/hr • Insensible losses = 2 cc/kg/hr
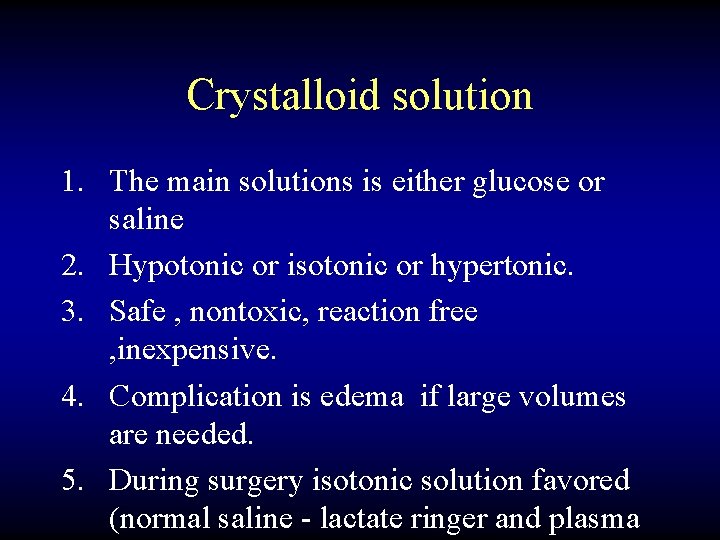
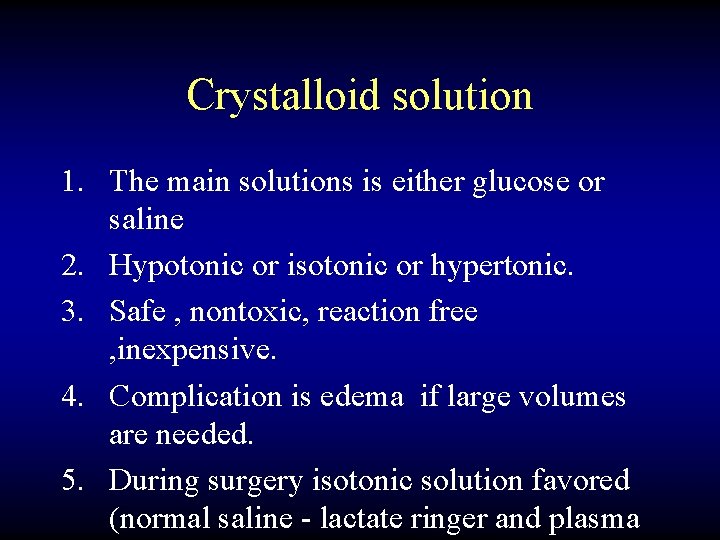
Crystalloid solution 1. The main solutions is either glucose or saline 2. Hypotonic or isotonic or hypertonic. 3. Safe , nontoxic, reaction free , inexpensive. 4. Complication is edema if large volumes are needed. 5. During surgery isotonic solution favored (normal saline - lactate ringer and plasma
Colloids 1. Albumin 2. Hydroxyethyl starch 3. Dextran
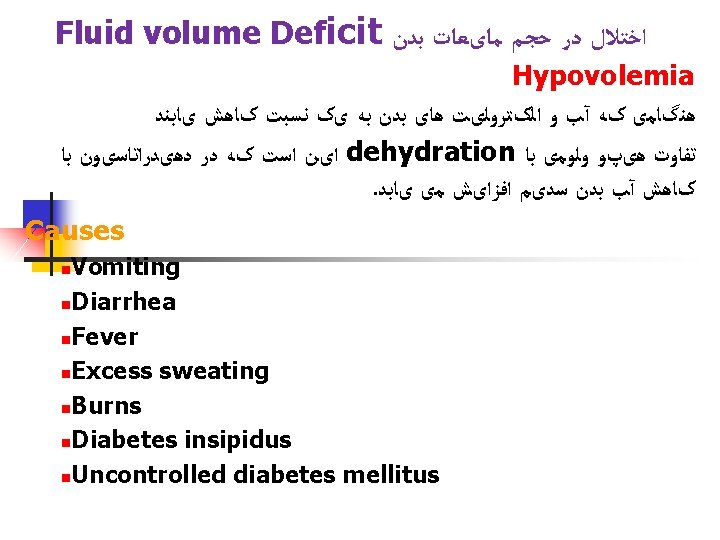
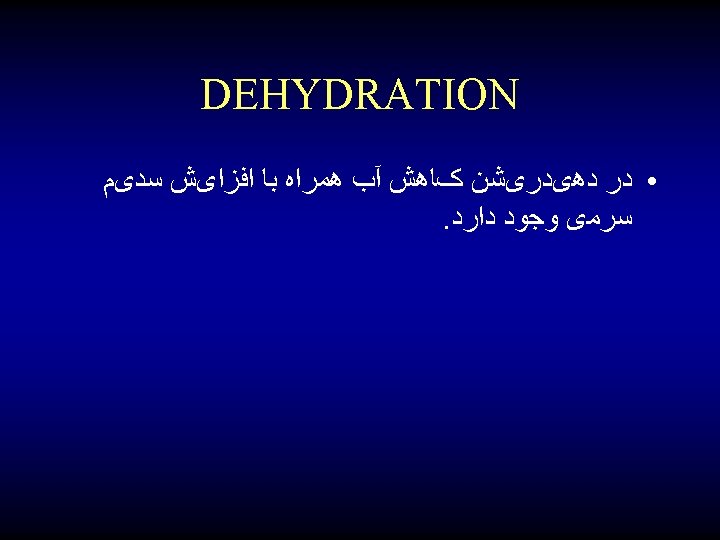
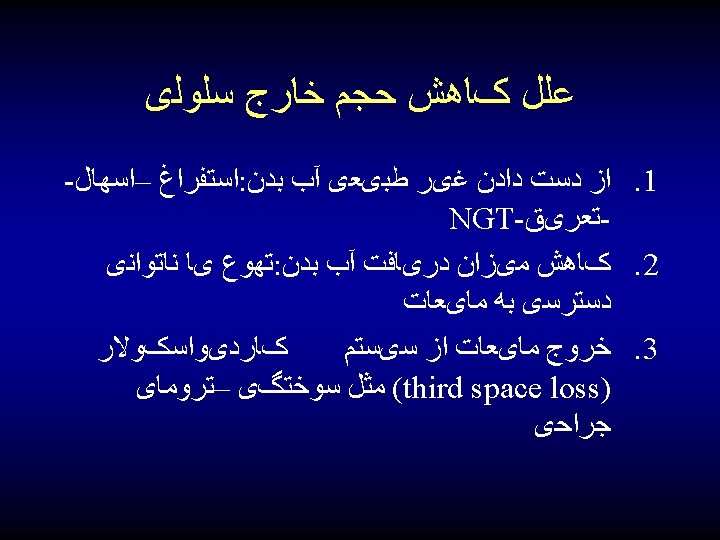
ﺍﺧﺘﻼﻝ ﺩﺭ ﺣﺠﻢ ﻣﺎیﻌﺎﺕ ﺑﺪﻥ 1. Fluid volume deficit 2. Fluid volume excess

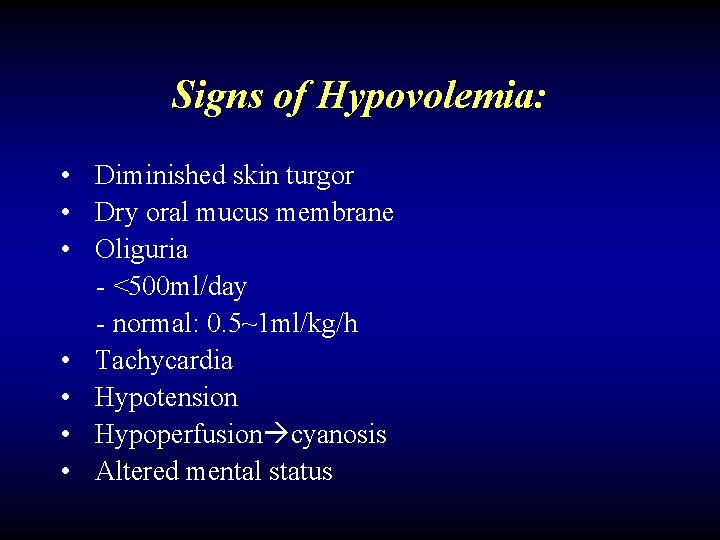
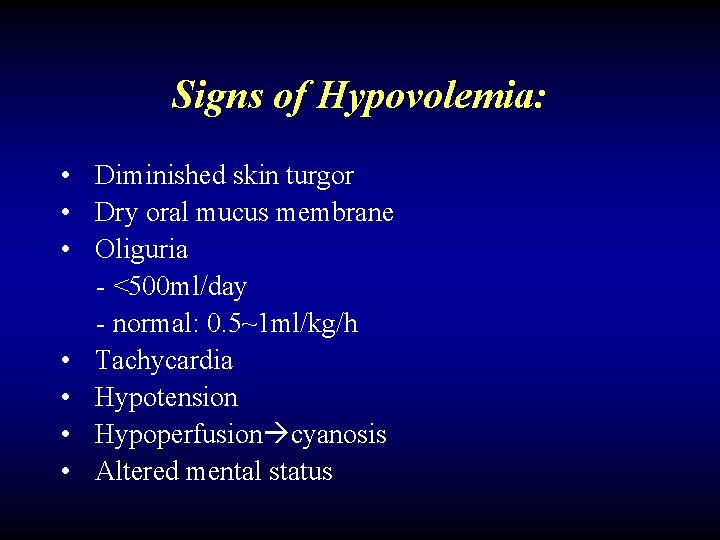
Signs of Hypovolemia: • Diminished skin turgor • Dry oral mucus membrane • Oliguria - <500 ml/day - normal: 0. 5~1 ml/kg/h • Tachycardia • Hypotension • Hypoperfusion cyanosis • Altered mental status
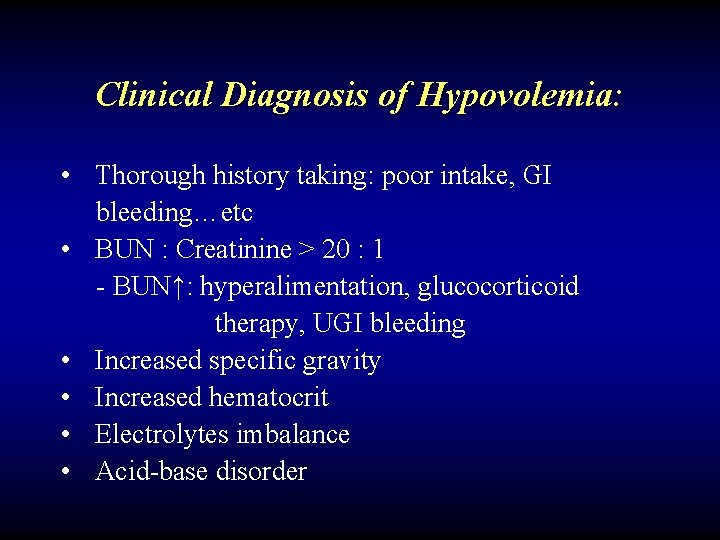
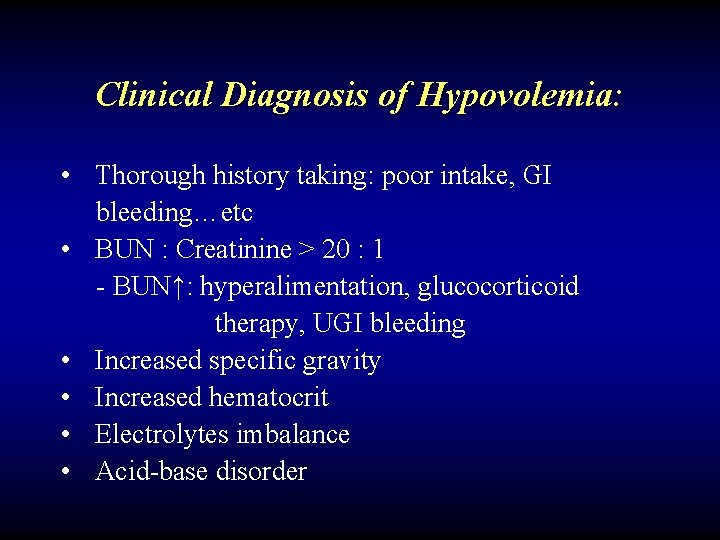
Clinical Diagnosis of Hypovolemia: • Thorough history taking: poor intake, GI bleeding…etc • BUN : Creatinine > 20 : 1 - BUN↑: hyperalimentation, glucocorticoid therapy, UGI bleeding • Increased specific gravity • Increased hematocrit • Electrolytes imbalance • Acid-base disorder
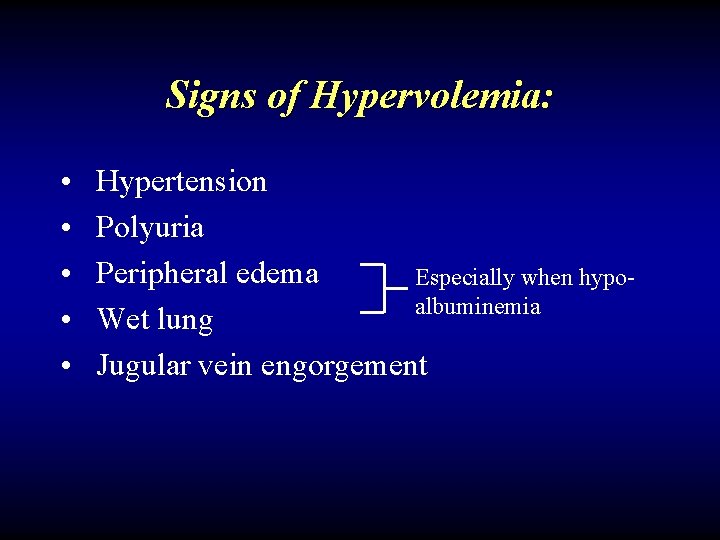
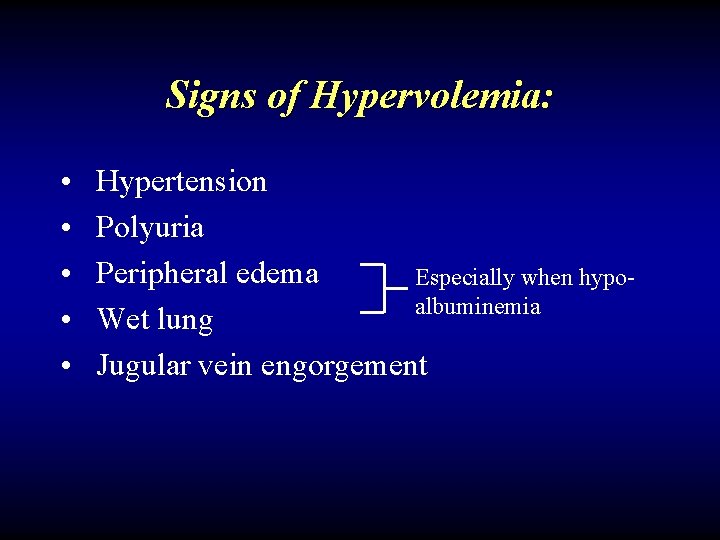
Signs of Hypervolemia: • • • Hypertension Polyuria Peripheral edema Especially when hypoalbuminemia Wet lung Jugular vein engorgement
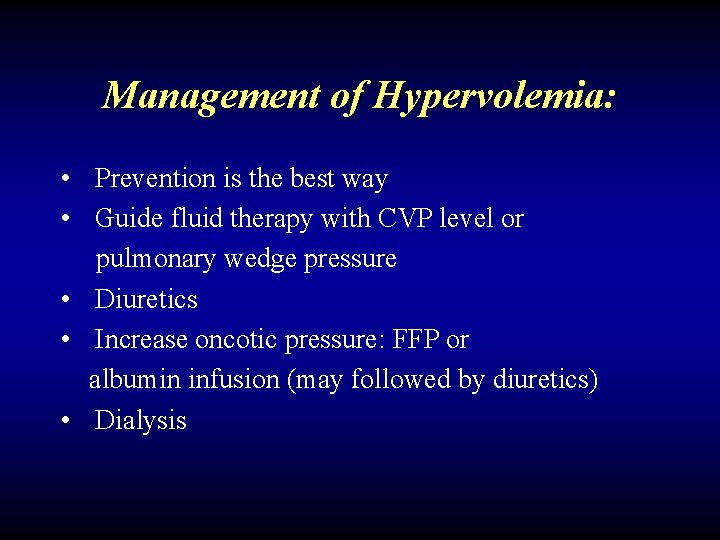
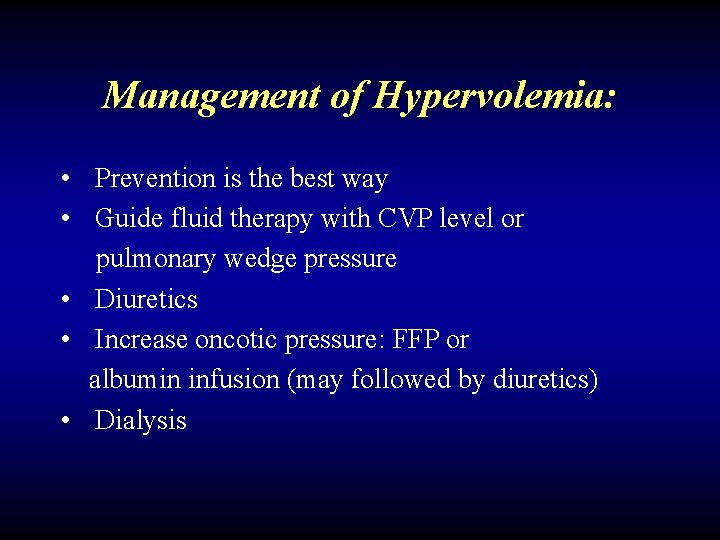
Management of Hypervolemia: • Prevention is the best way • Guide fluid therapy with CVP level or pulmonary wedge pressure • Diuretics • Increase oncotic pressure: FFP or albumin infusion (may followed by diuretics) • Dialysis
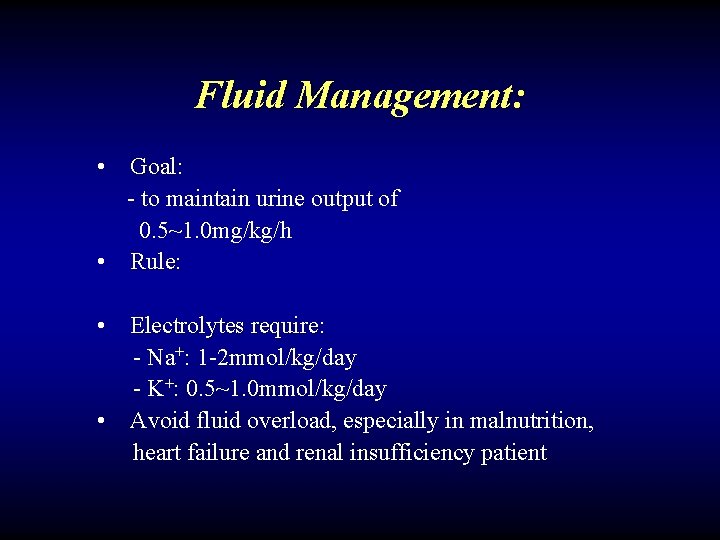
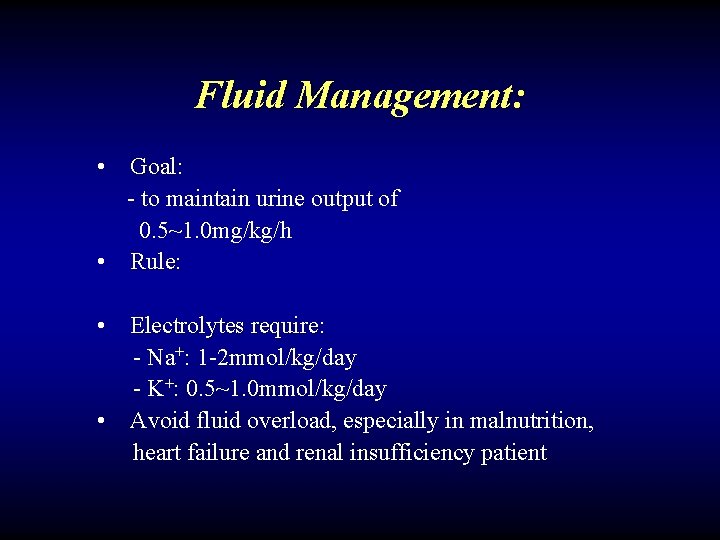
Fluid Management: • Goal: - to maintain urine output of 0. 5~1. 0 mg/kg/h • Rule: • Electrolytes require: - Na+: 1 -2 mmol/kg/day - K+: 0. 5~1. 0 mmol/kg/day • Avoid fluid overload, especially in malnutrition, heart failure and renal insufficiency patient

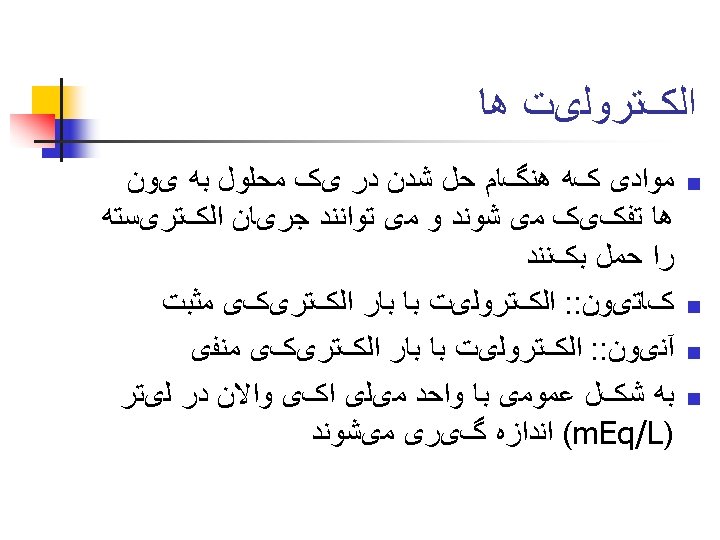
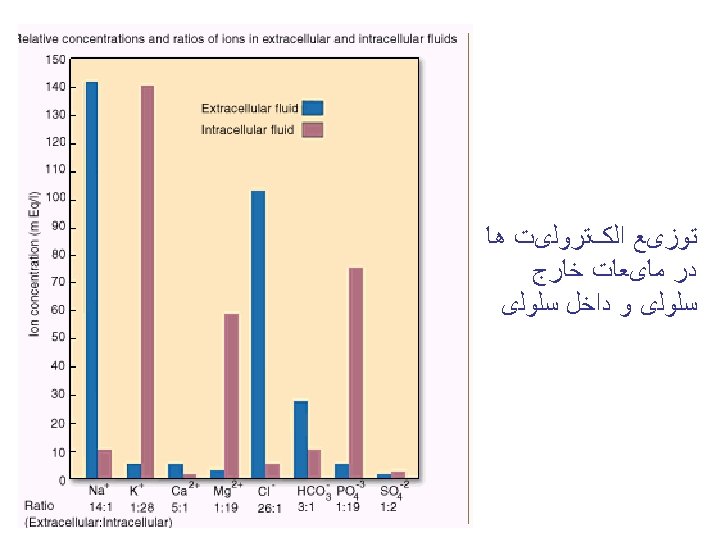
Electrolyte physiology
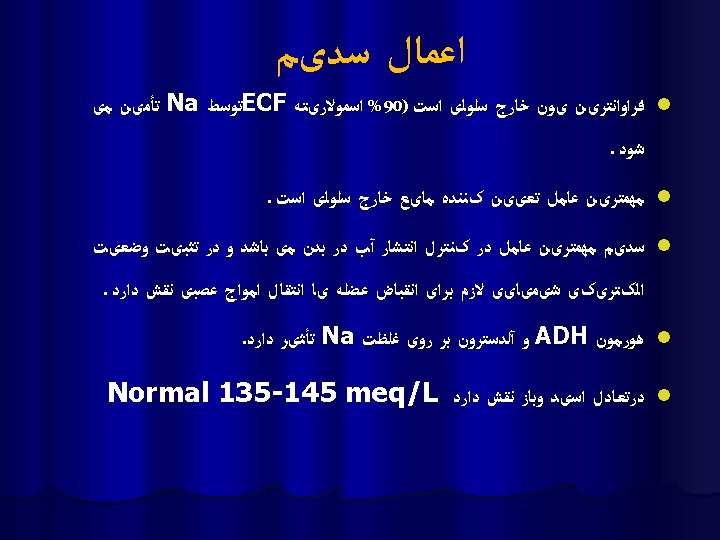
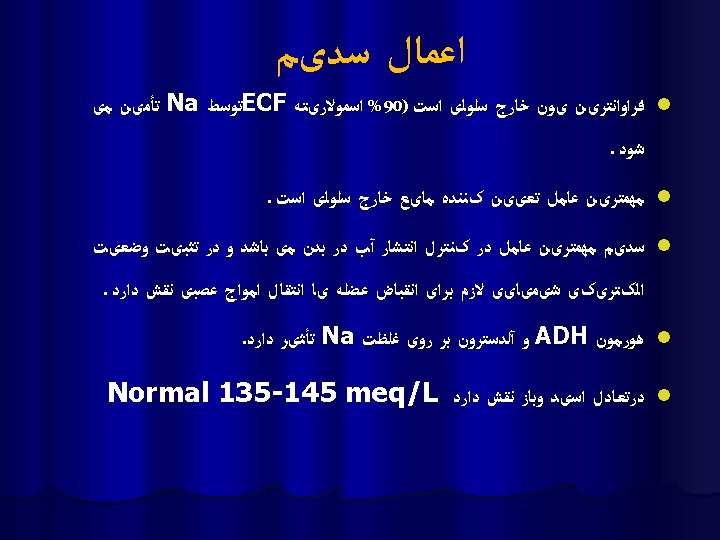
Sodium physiology ü Na is the most abundant positive ion of ECF compartment and is critical in determining the ECF and ICF osmolality. ü Normal amount 135 -145 meq/l
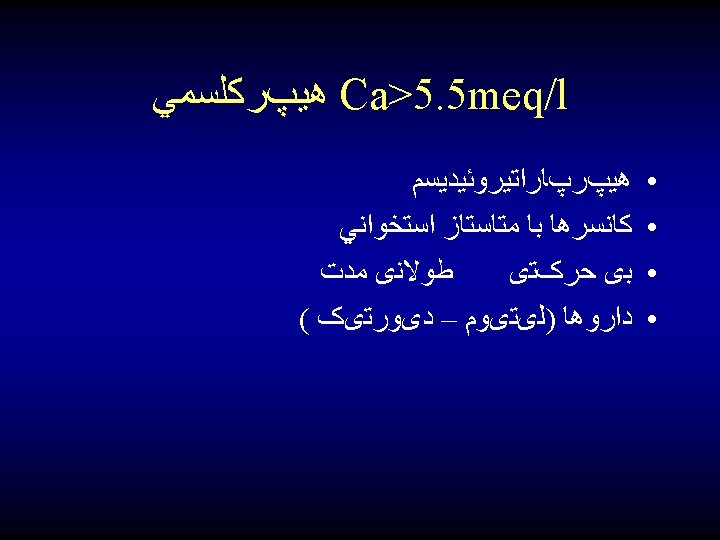
Hypernatremia Serum Na>145 m. Eq/L
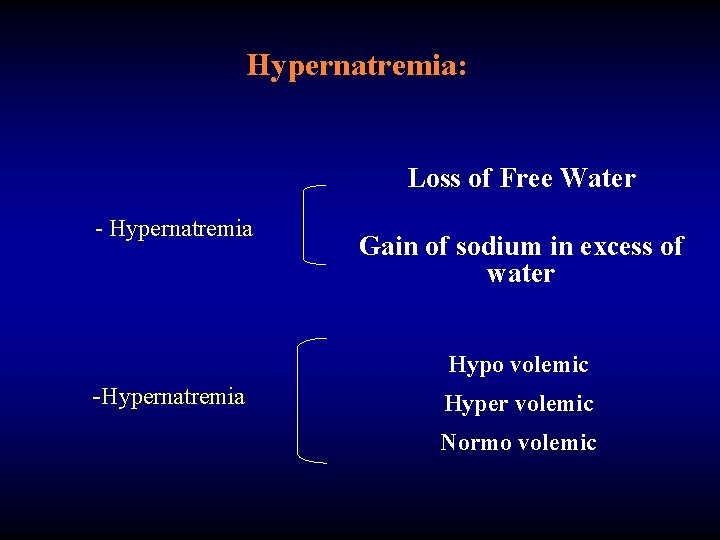
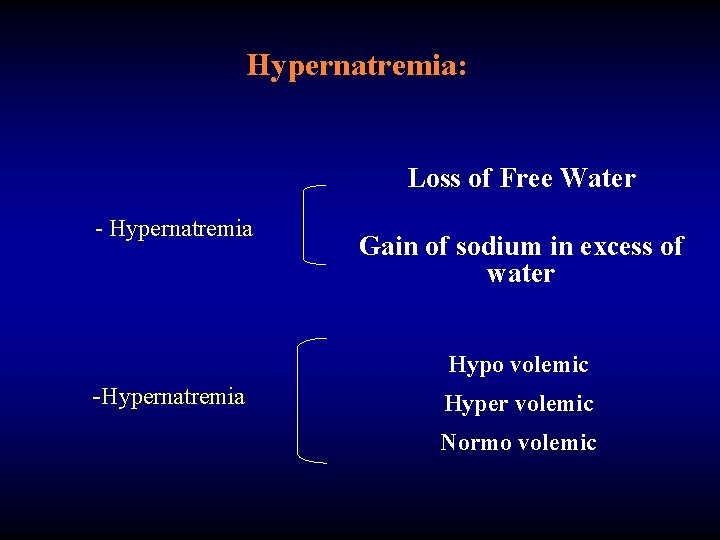
Hypernatremia: Loss of Free Water - Hypernatremia Gain of sodium in excess of water Hypo volemic -Hypernatremia Hyper volemic Normo volemic
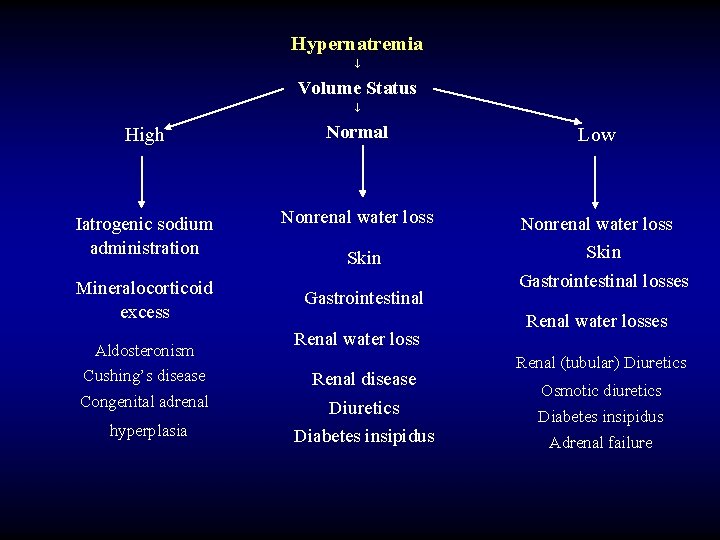
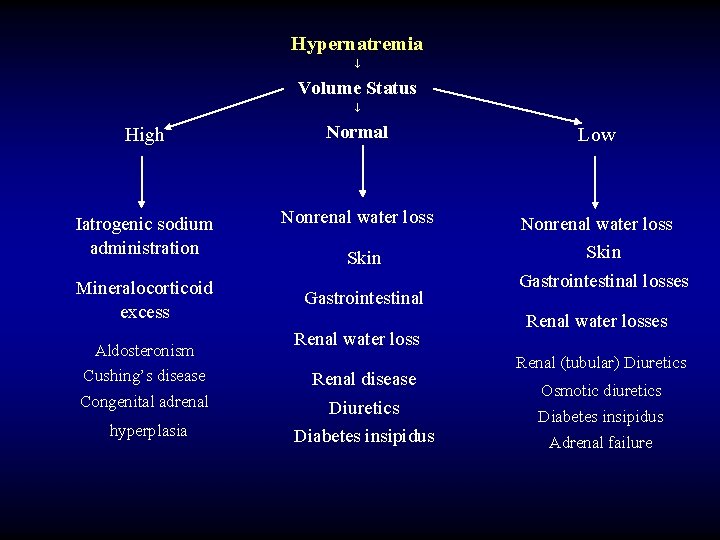
Hypernatremia Volume Status High Normal Iatrogenic sodium administration Nonrenal water loss Mineralocorticoid excess Aldosteronism Cushing’s disease Congenital adrenal hyperplasia Skin Gastrointestinal Renal water loss Renal disease Diuretics Diabetes insipidus Low Nonrenal water loss Skin Gastrointestinal losses Renal water losses Renal (tubular) Diuretics Osmotic diuretics Diabetes insipidus Adrenal failure
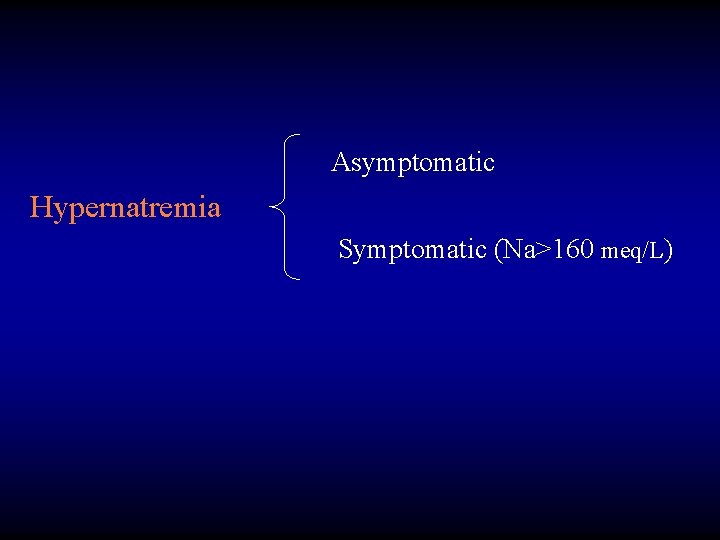
Asymptomatic Hypernatremia Symptomatic (Na>160 meq/L)
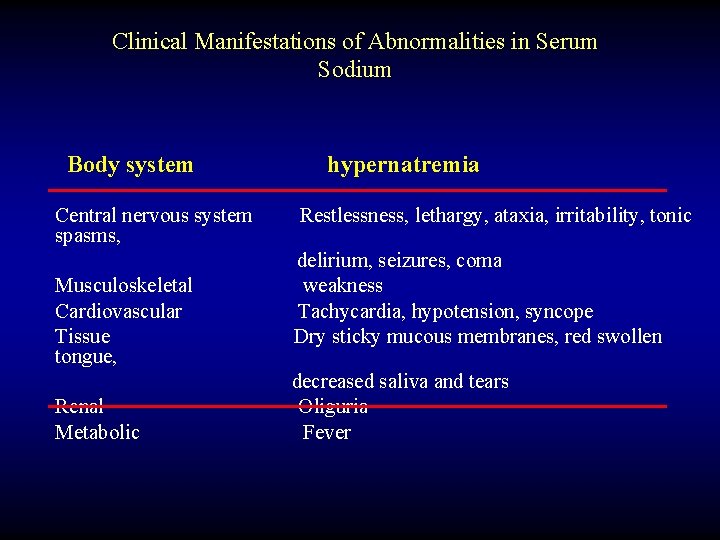
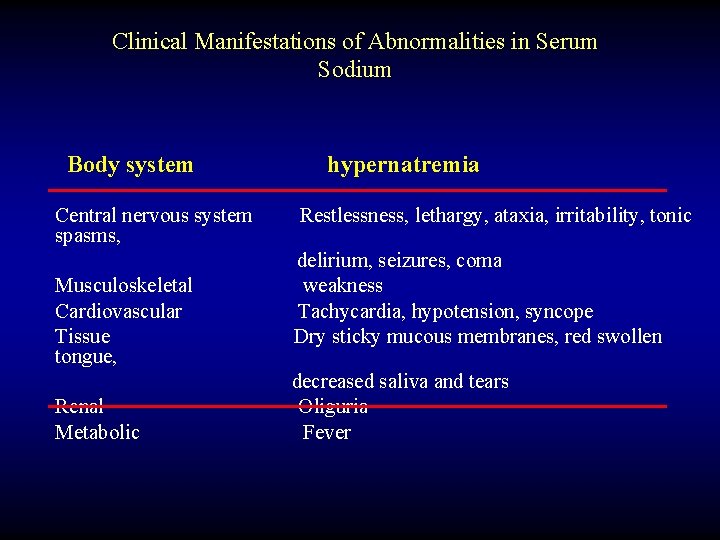
Clinical Manifestations of Abnormalities in Serum Sodium Body system Central nervous system spasms, Musculoskeletal Cardiovascular Tissue tongue, Renal Metabolic hypernatremia Restlessness, lethargy, ataxia, irritability, tonic delirium, seizures, coma weakness Tachycardia, hypotension, syncope Dry sticky mucous membranes, red swollen decreased saliva and tears Oliguria Fever
Treatment Normal saline in hypovolemic patients Hypotonic fluid (D/w 5%, D/W 5% in ¼ or ½ normal saline, or entral water)
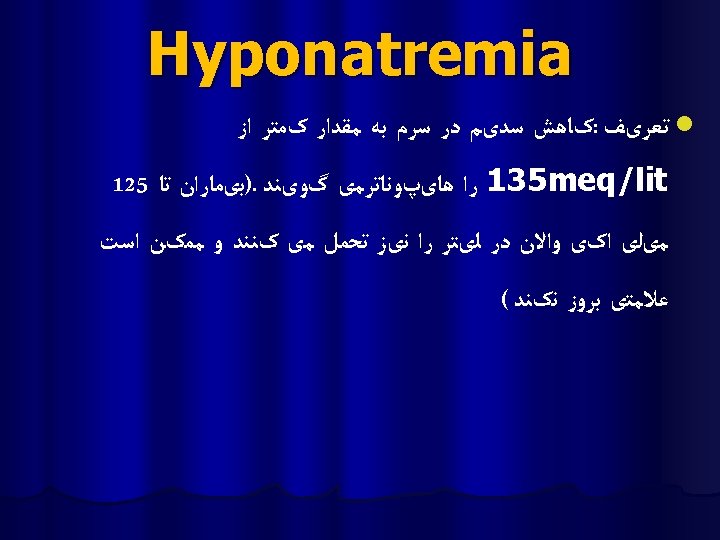
Hyponatremia: Na<135 m. Eq/L Causes : 1. Sodium depletion 2. Sodium dilution
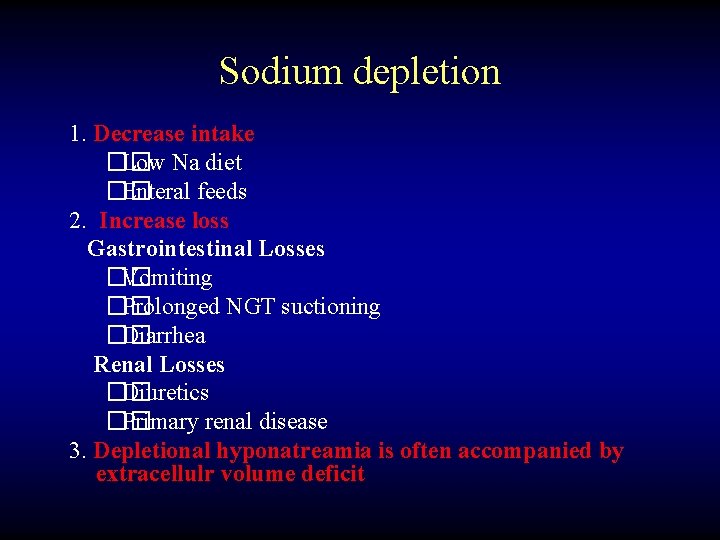
Sodium depletion 1. Decrease intake �� Low Na diet �� Enteral feeds 2. Increase loss Gastrointestinal Losses �� Vomiting �� Prolonged NGT suctioning �� Diarrhea Renal Losses �� Diuretics �� Primary renal disease 3. Depletional hyponatreamia is often accompanied by extracellulr volume deficit
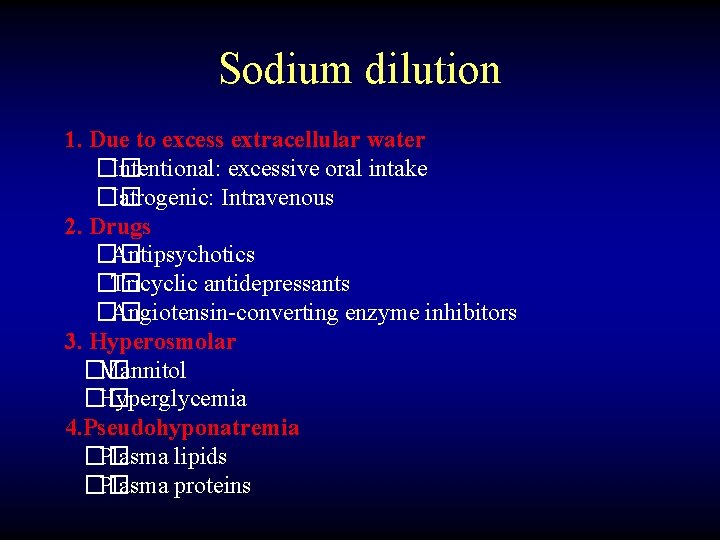
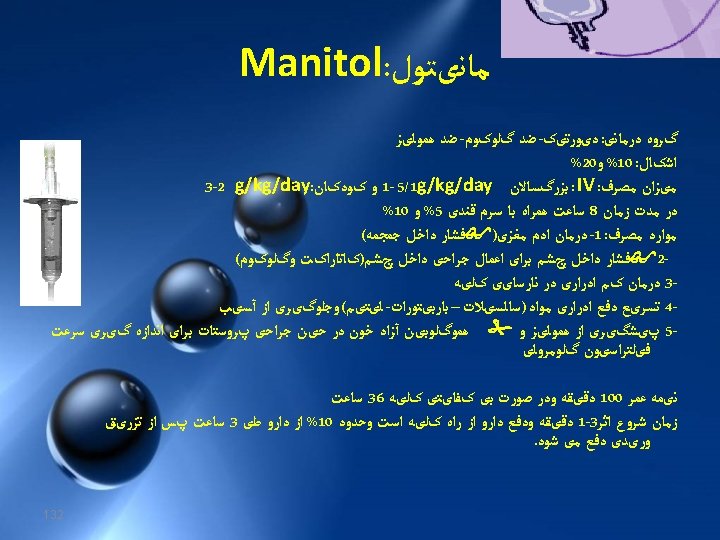
Sodium dilution 1. Due to excess extracellular water �� Intentional: excessive oral intake �� Iatrogenic: Intravenous 2. Drugs �� Antipsychotics �� Tricyclic antidepressants �� Angiotensin-converting enzyme inhibitors 3. Hyperosmolar �� Mannitol �� Hyperglycemia 4. Pseudohyponatremia �� Plasma lipids �� Plasma proteins
Sign and symptoms • CNS symptom when Na<123 meq/l • Cardiac symptom when Na<100 meq/l
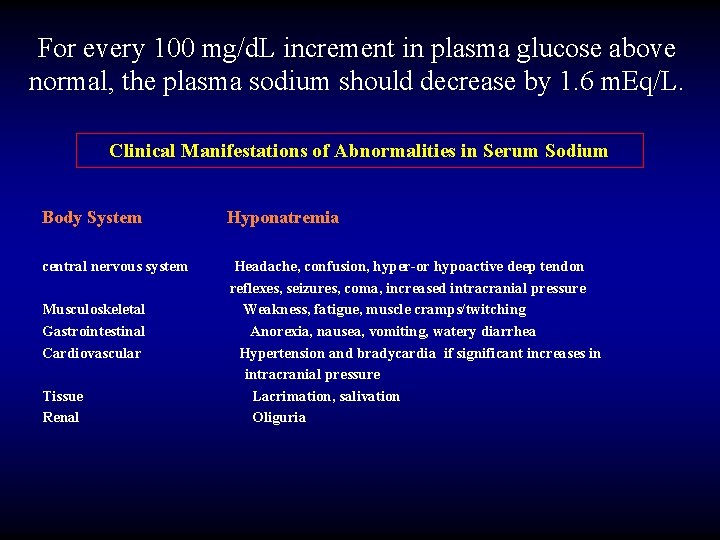
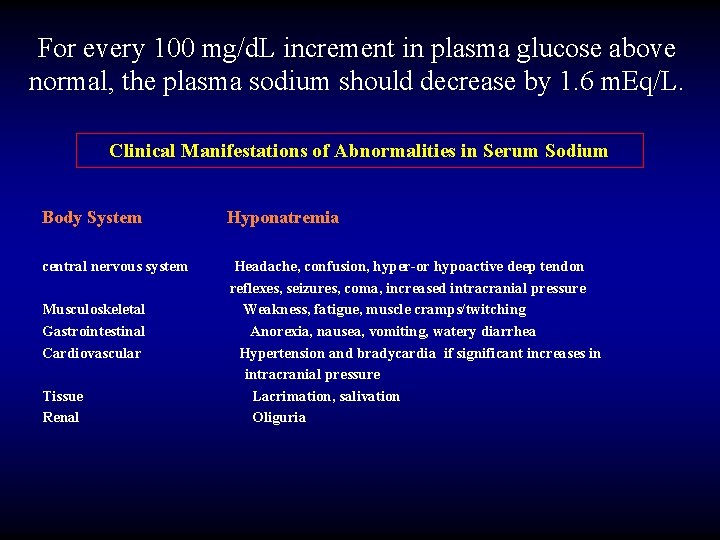
For every 100 mg/d. L increment in plasma glucose above normal, the plasma sodium should decrease by 1. 6 m. Eq/L. Clinical Manifestations of Abnormalities in Serum Sodium Body System Hyponatremia central nervous system Headache, confusion, hyper-or hypoactive deep tendon reflexes, seizures, coma, increased intracranial pressure Weakness, fatigue, muscle cramps/twitching Anorexia, nausea, vomiting, watery diarrhea Hypertension and bradycardia if significant increases in intracranial pressure Lacrimation, salivation Oliguria Musculoskeletal Gastrointestinal Cardiovascular Tissue Renal
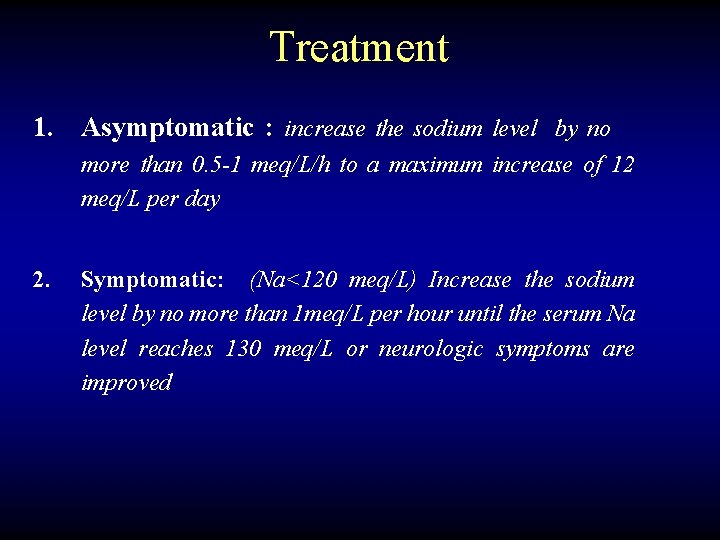
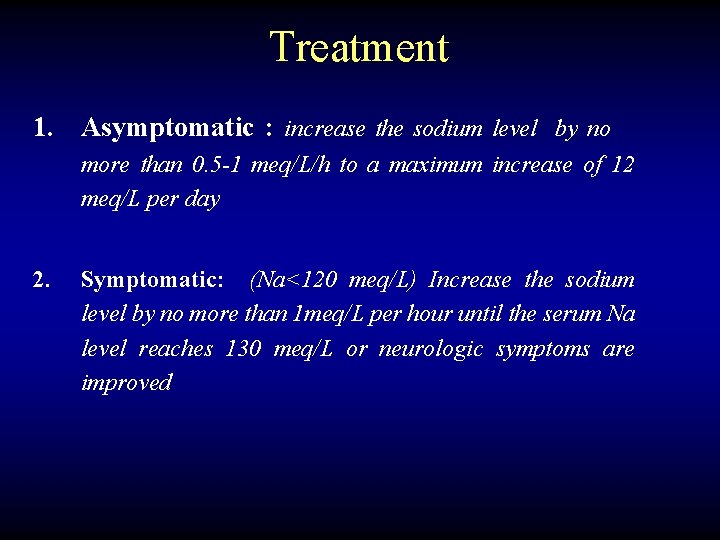
Treatment 1. Asymptomatic : increase the sodium level by no more than 0. 5 -1 meq/L/h to a maximum increase of 12 meq/L per day 2. Symptomatic: (Na<120 meq/L) Increase the sodium level by no more than 1 meq/L per hour until the serum Na level reaches 130 meq/L or neurologic symptoms are improved
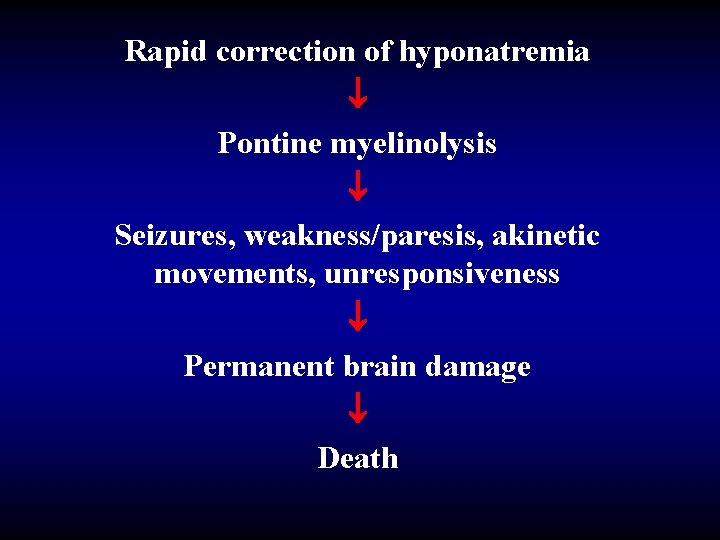
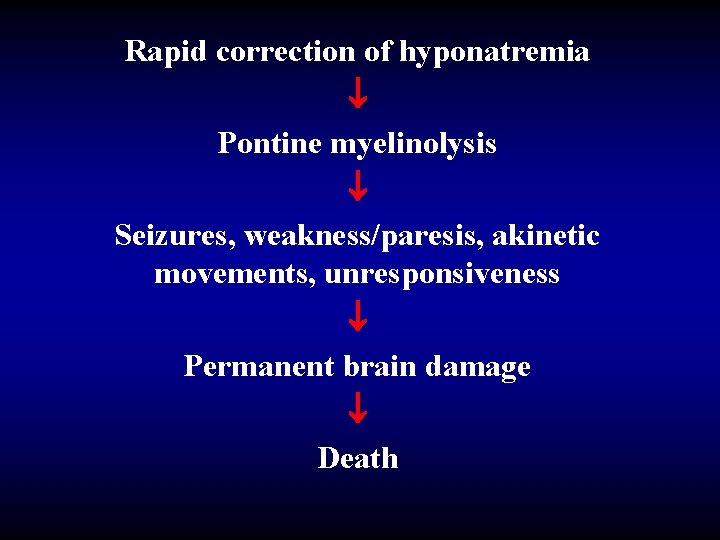
Rapid correction of hyponatremia Pontine myelinolysis Seizures, weakness/paresis, akinetic movements, unresponsiveness Permanent brain damage Death
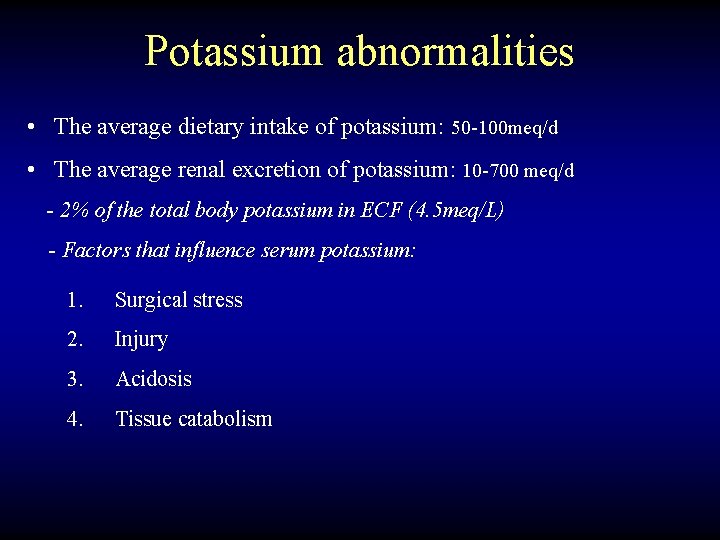
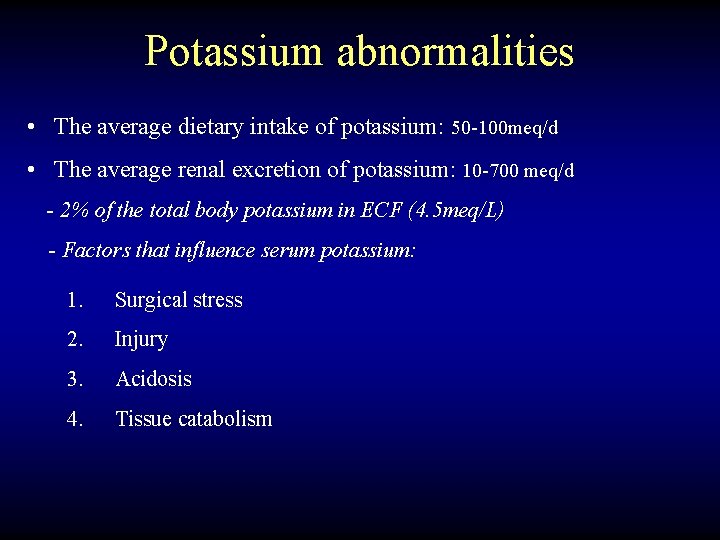
Potassium abnormalities • The average dietary intake of potassium: 50 -100 meq/d • The average renal excretion of potassium: 10 -700 meq/d - 2% of the total body potassium in ECF (4. 5 meq/L) - Factors that influence serum potassium: 1. Surgical stress 2. Injury 3. Acidosis 4. Tissue catabolism
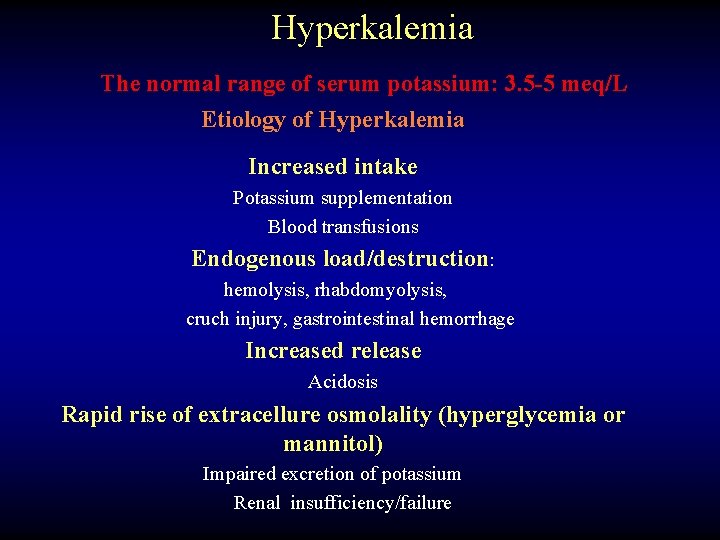
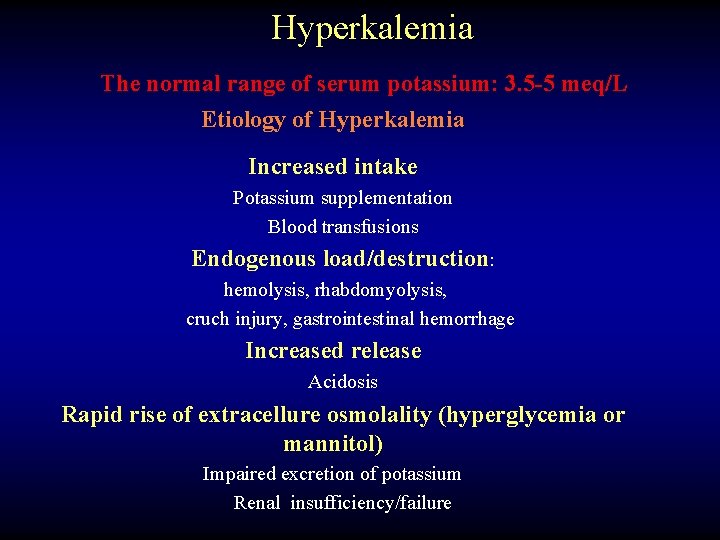
Hyperkalemia The normal range of serum potassium: 3. 5 -5 meq/L Etiology of Hyperkalemia Increased intake Potassium supplementation Blood transfusions Endogenous load/destruction: hemolysis, rhabdomyolysis, cruch injury, gastrointestinal hemorrhage Increased release Acidosis Rapid rise of extracellure osmolality (hyperglycemia or mannitol) Impaired excretion of potassium Renal insufficiency/failure
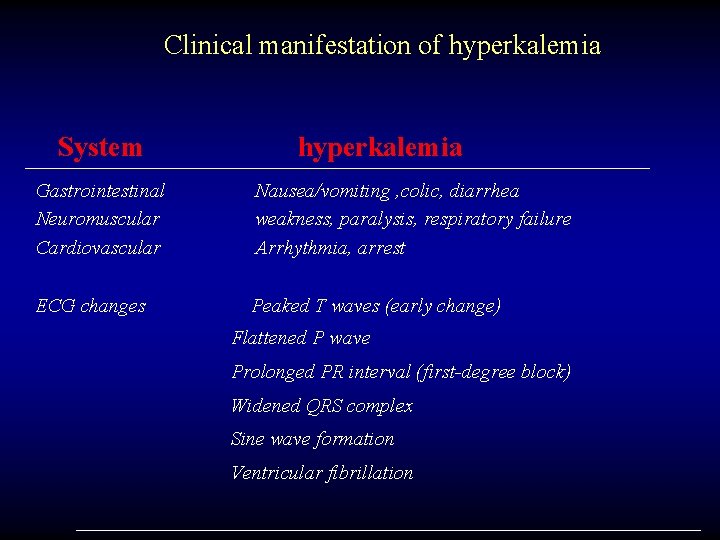
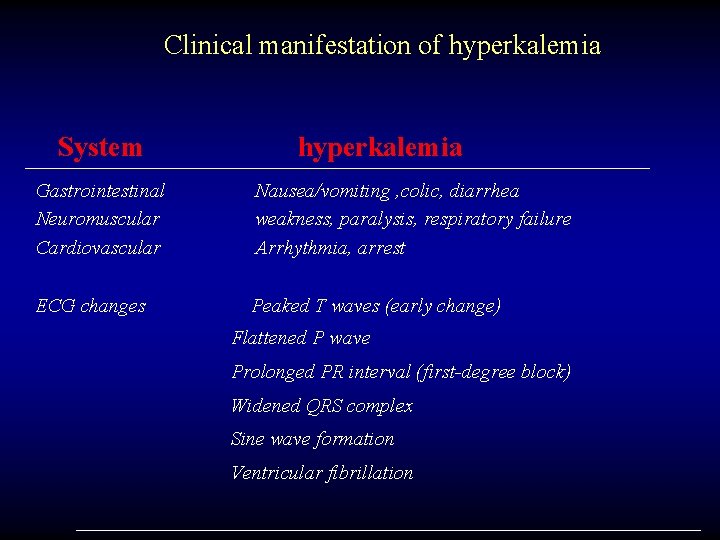
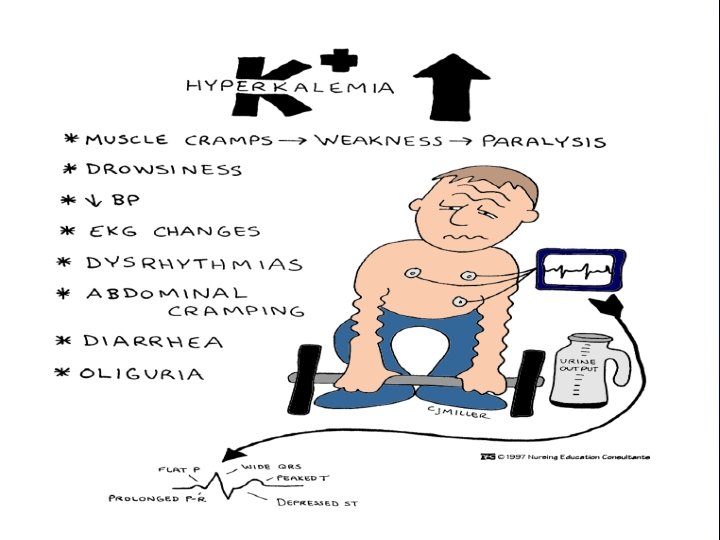
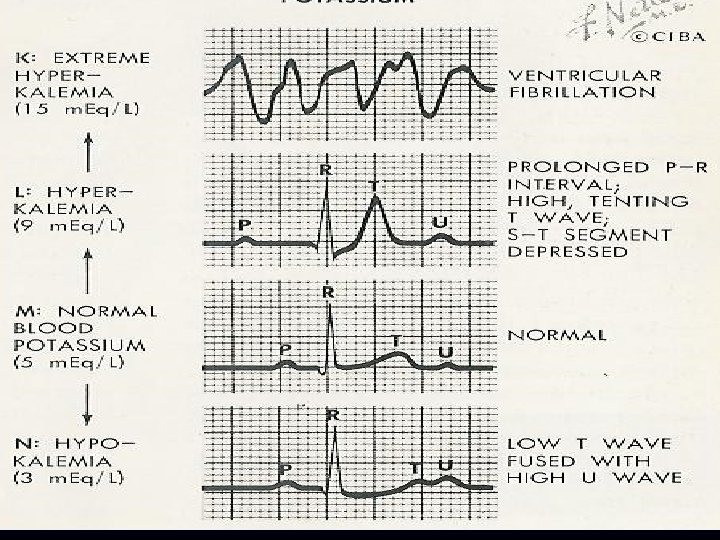
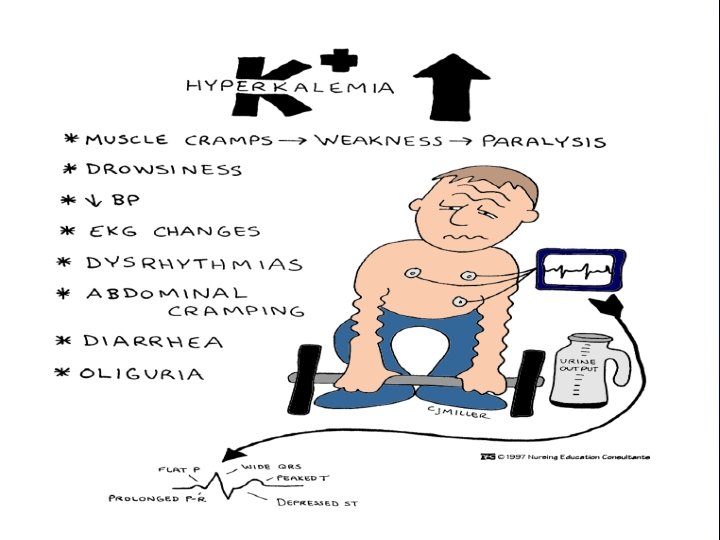
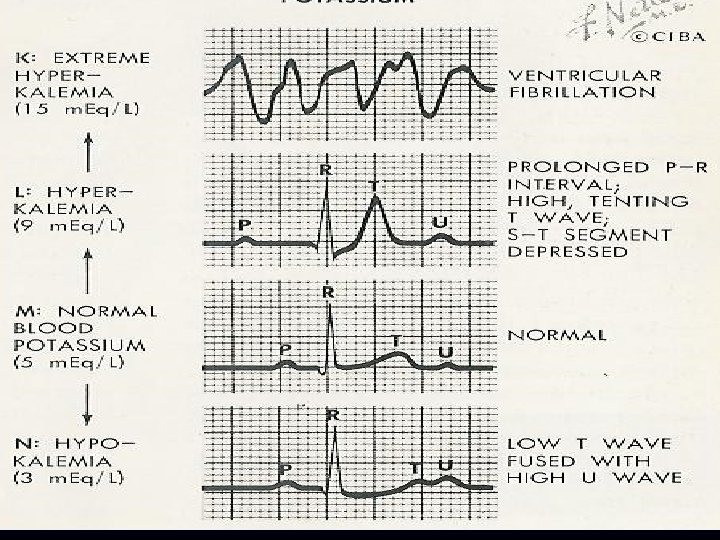
Clinical manifestation of hyperkalemia System hyperkalemia Gastrointestinal Neuromuscular Cardiovascular Nausea/vomiting , colic, diarrhea weakness, paralysis, respiratory failure Arrhythmia, arrest ECG changes Peaked T waves (early change) Flattened P wave Prolonged PR interval (first-degree block) Widened QRS complex Sine wave formation Ventricular fibrillation
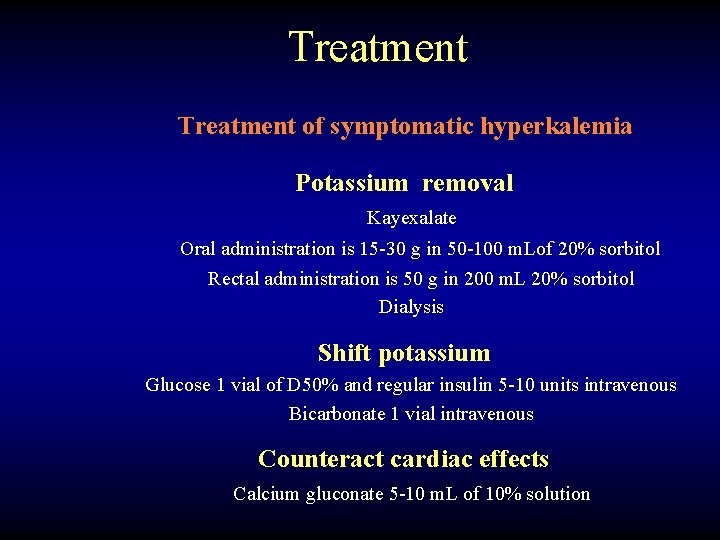
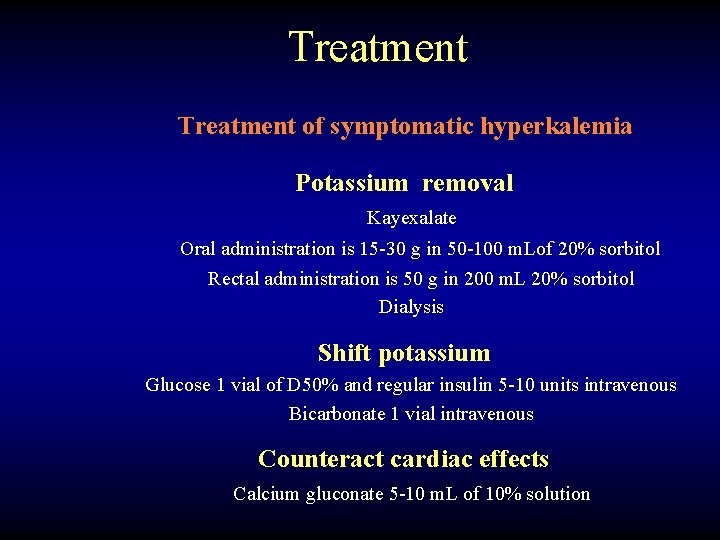
Treatment of symptomatic hyperkalemia Potassium removal Kayexalate Oral administration is 15 -30 g in 50 -100 m. Lof 20% sorbitol Rectal administration is 50 g in 200 m. L 20% sorbitol Dialysis Shift potassium Glucose 1 vial of D 50% and regular insulin 5 -10 units intravenous Bicarbonate 1 vial intravenous Counteract cardiac effects Calcium gluconate 5 -10 m. L of 10% solution
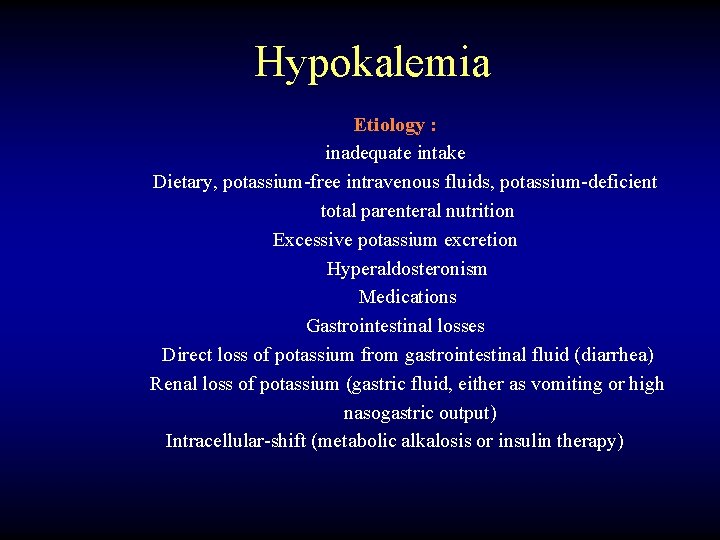
Hypokalemia Etiology : inadequate intake Dietary, potassium-free intravenous fluids, potassium-deficient total parenteral nutrition Excessive potassium excretion Hyperaldosteronism Medications Gastrointestinal losses Direct loss of potassium from gastrointestinal fluid (diarrhea) Renal loss of potassium (gastric fluid, either as vomiting or high nasogastric output) Intracellular-shift (metabolic alkalosis or insulin therapy)
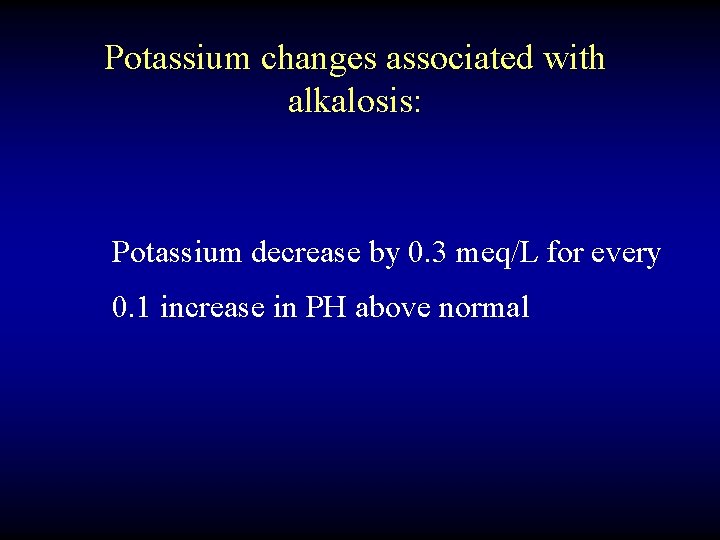
Potassium changes associated with alkalosis: Potassium decrease by 0. 3 meq/L for every 0. 1 increase in PH above normal
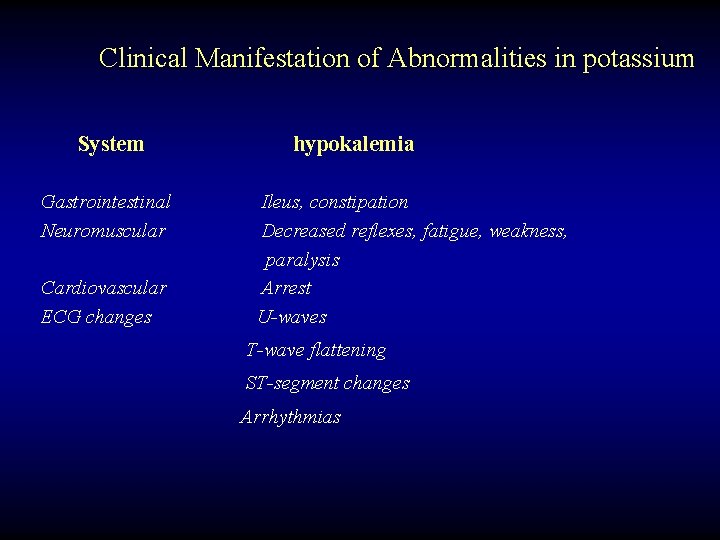
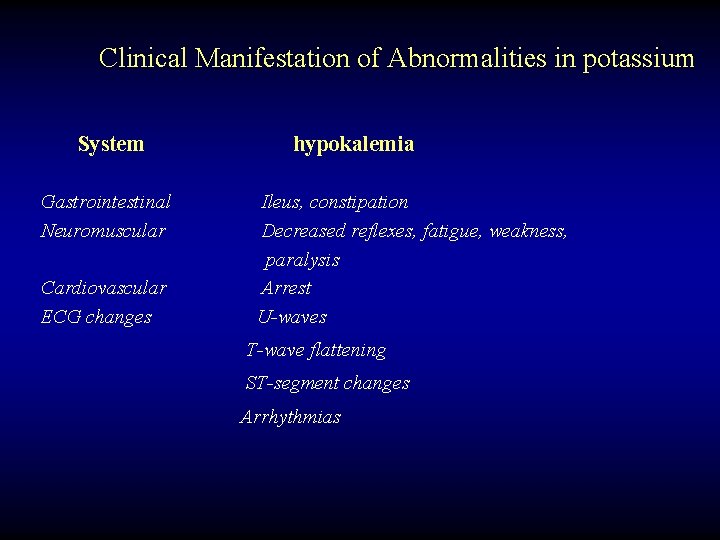
Clinical Manifestation of Abnormalities in potassium System Gastrointestinal Neuromuscular Cardiovascular ECG changes hypokalemia Ileus, constipation Decreased reflexes, fatigue, weakness, paralysis Arrest U-waves T-wave flattening ST-segment changes Arrhythmias
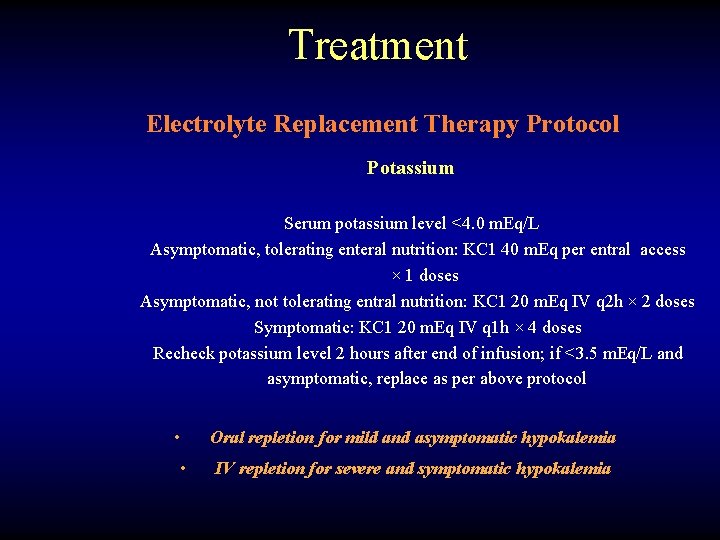
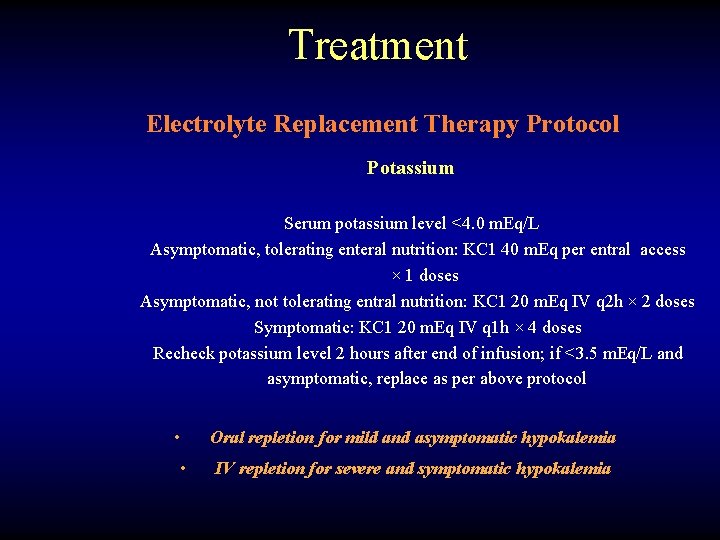
Treatment Electrolyte Replacement Therapy Protocol Potassium Serum potassium level <4. 0 m. Eq/L Asymptomatic, tolerating enteral nutrition: KC 1 40 m. Eq per entral access × 1 doses Asymptomatic, not tolerating entral nutrition: KC 1 20 m. Eq IV q 2 h × 2 doses Symptomatic: KC 1 20 m. Eq IV q 1 h × 4 doses Recheck potassium level 2 hours after end of infusion; if <3. 5 m. Eq/L and asymptomatic, replace as per above protocol • • Oral repletion for mild and asymptomatic hypokalemia IV repletion for severe and symptomatic hypokalemia
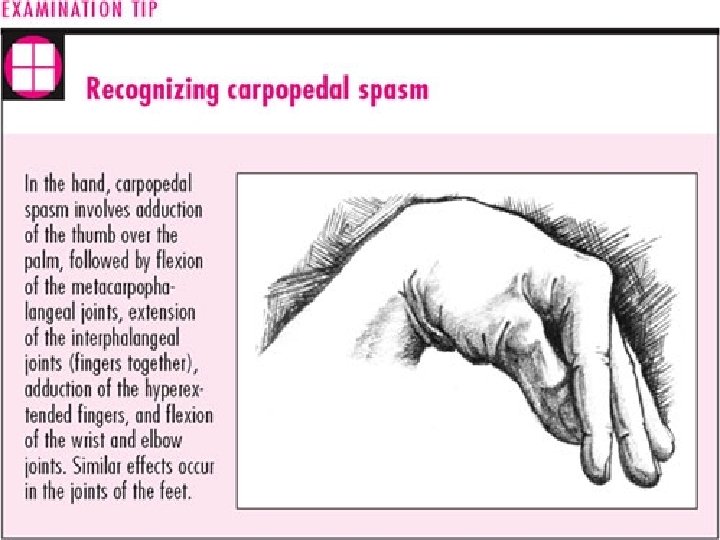

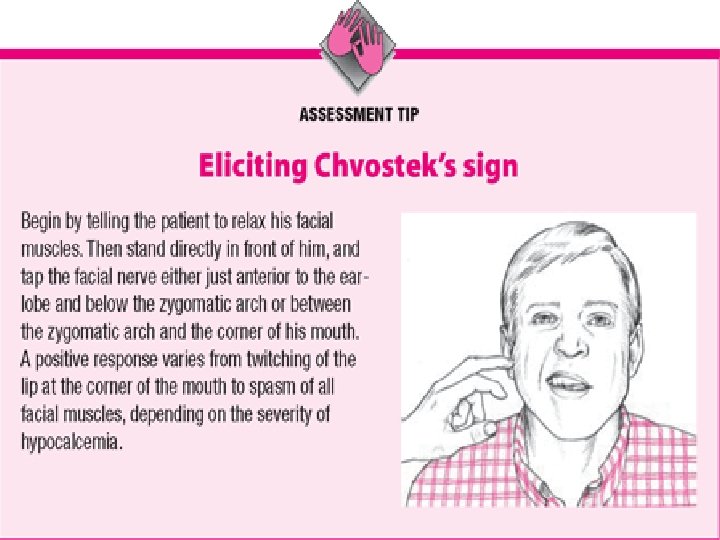
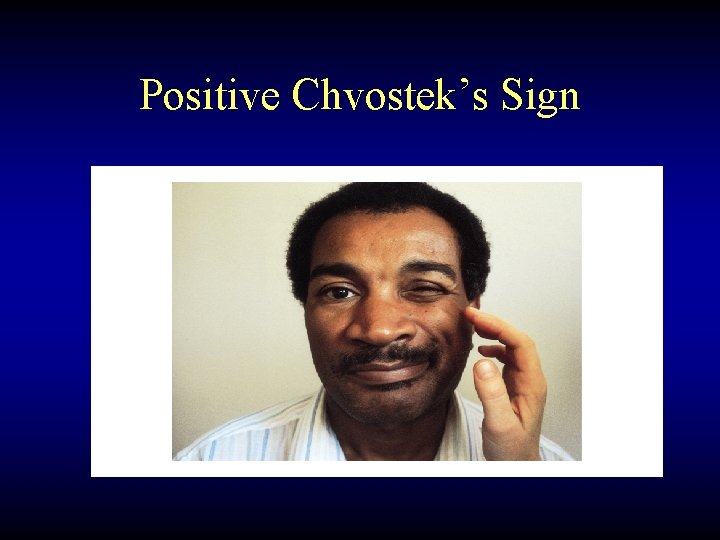
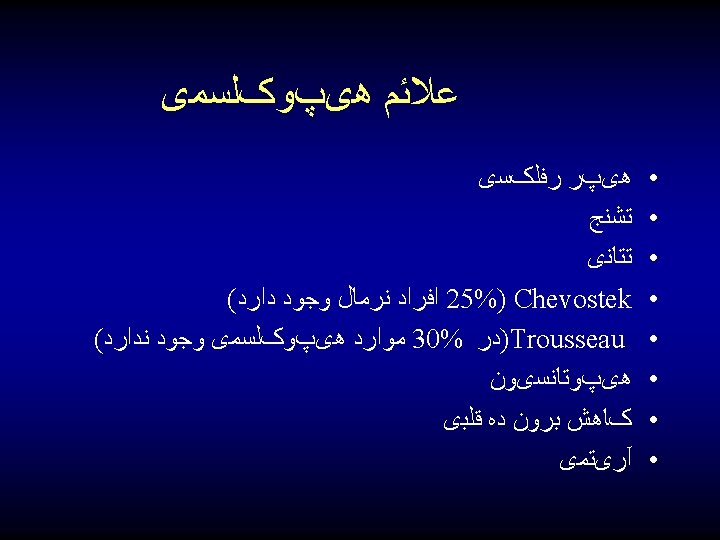
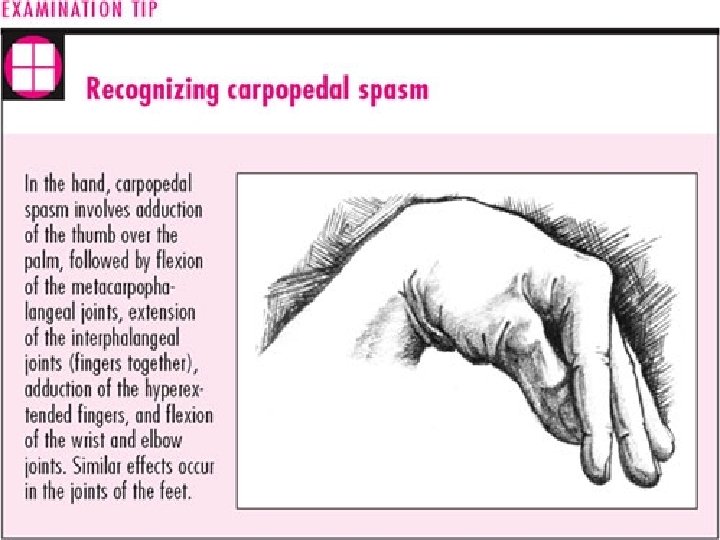
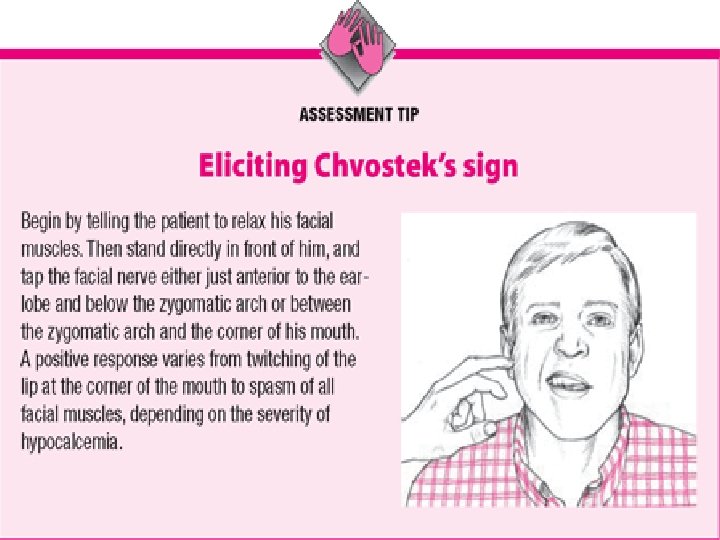
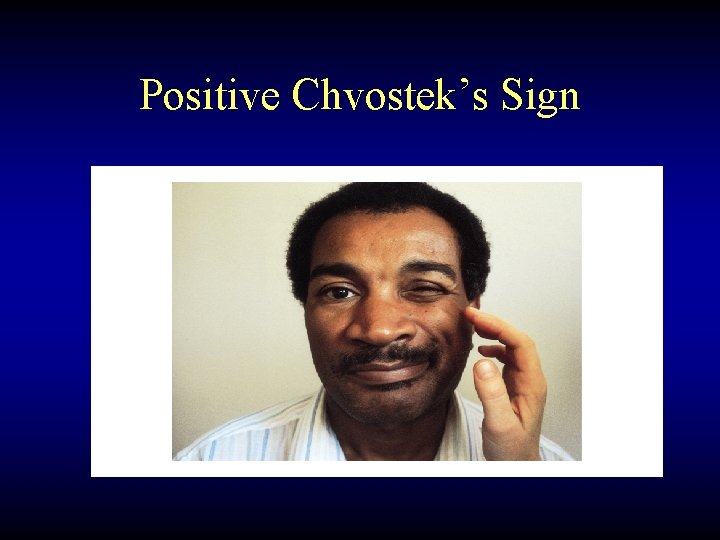
Positive Chvostek’s Sign
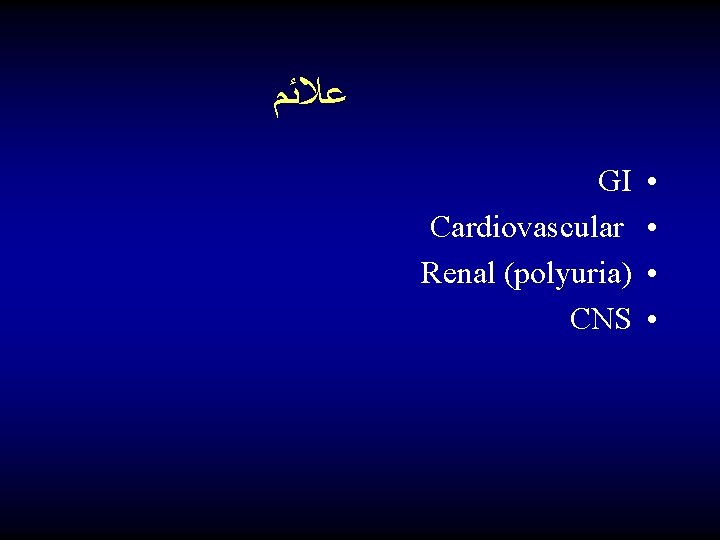
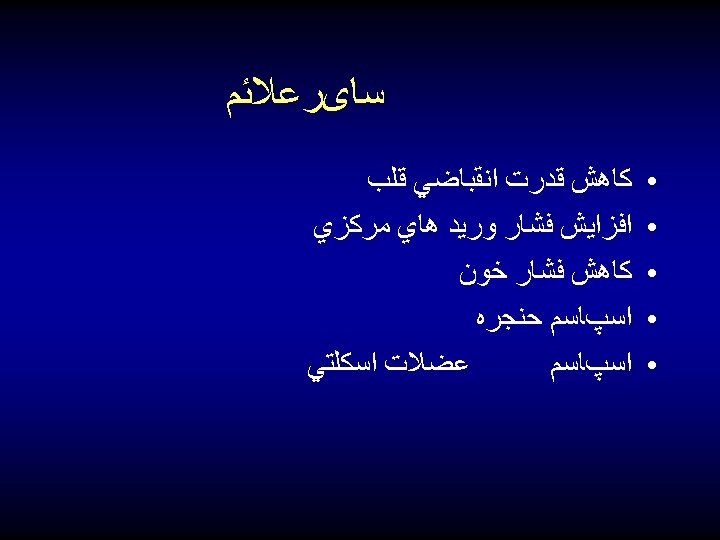
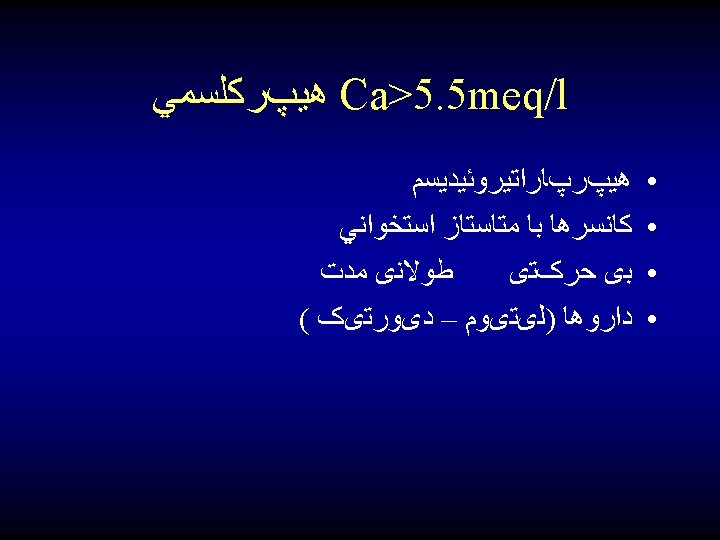
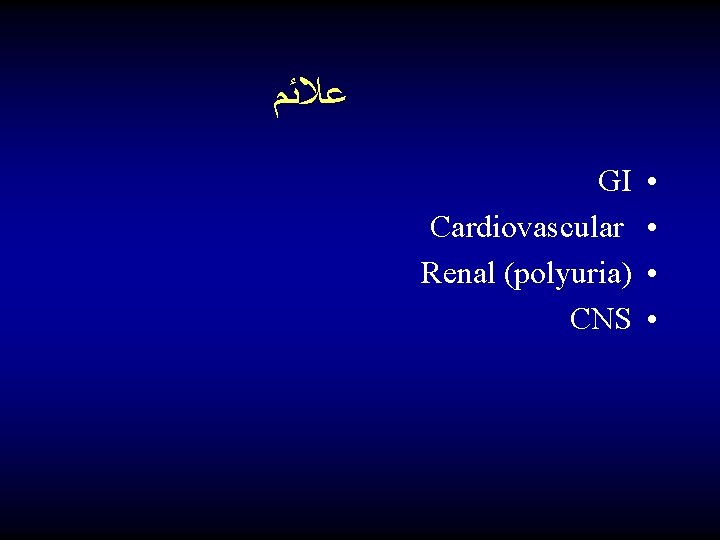
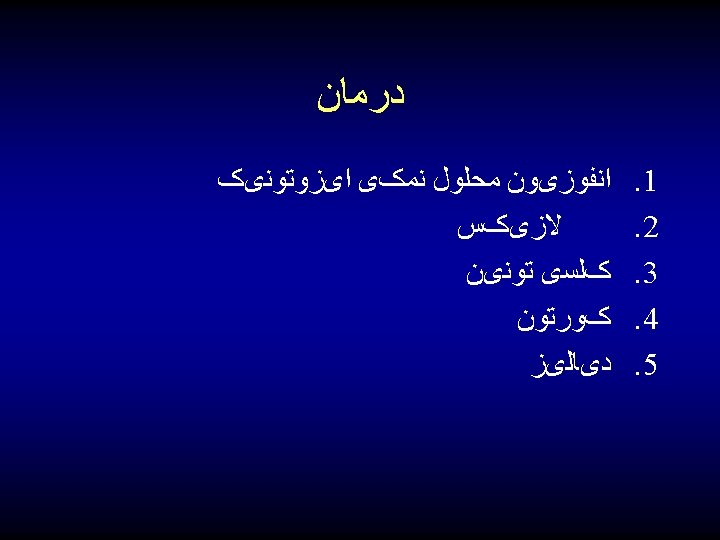
ﻋﻼﺋﻢ GI Cardiovascular Renal (polyuria) CNS • •


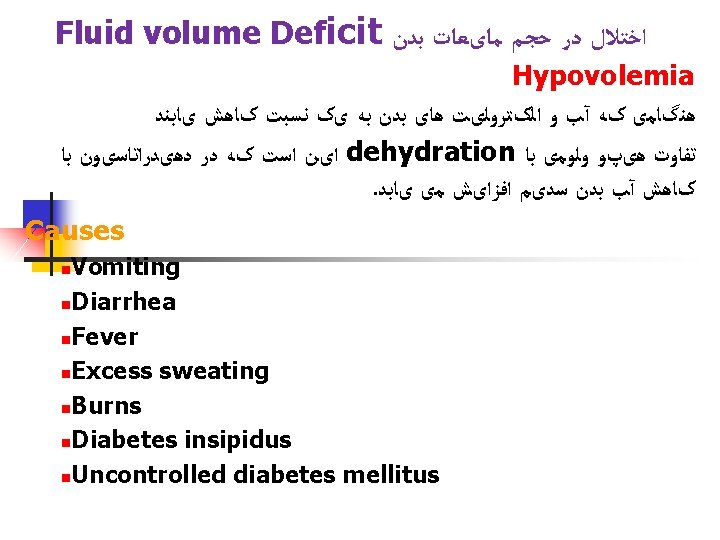
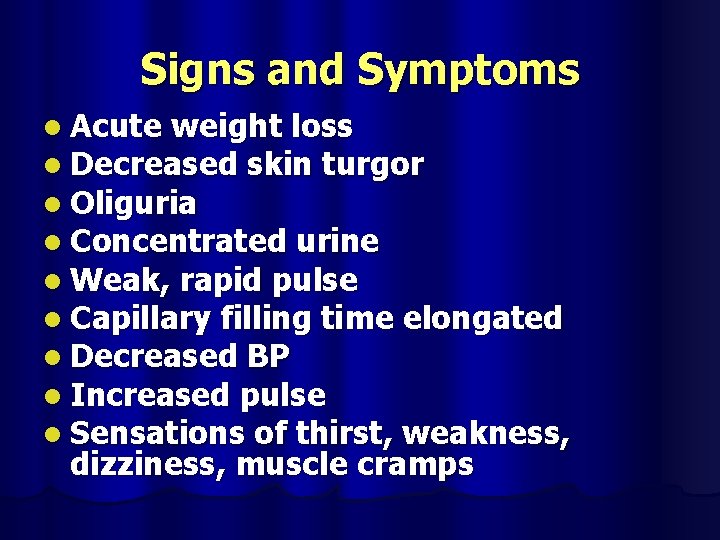
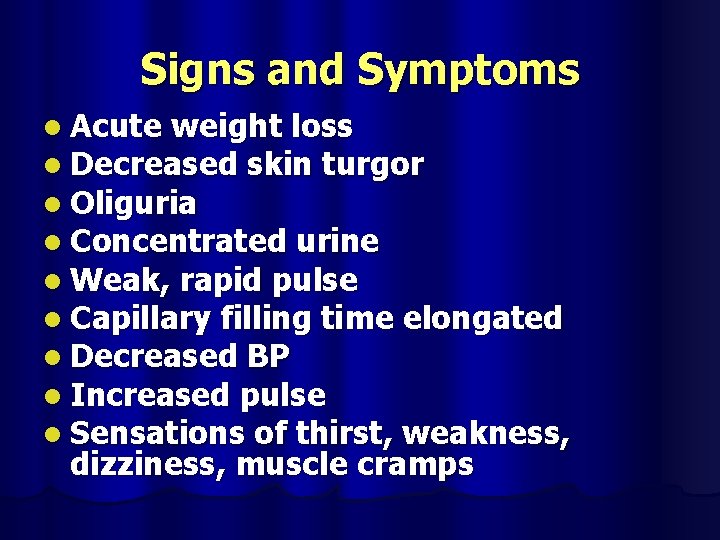
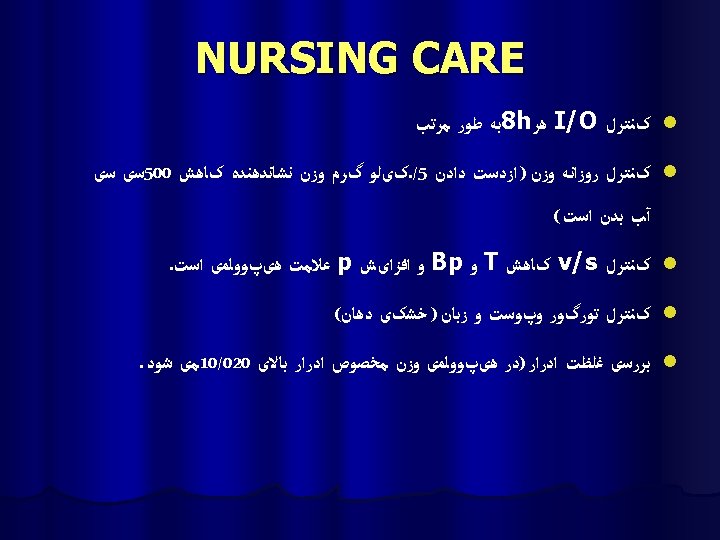
Signs and Symptoms l Acute weight loss l Decreased skin turgor l Oliguria l Concentrated urine l Weak, rapid pulse l Capillary filling time elongated l Decreased BP l Increased pulse l Sensations of thirst, weakness, dizziness, muscle cramps
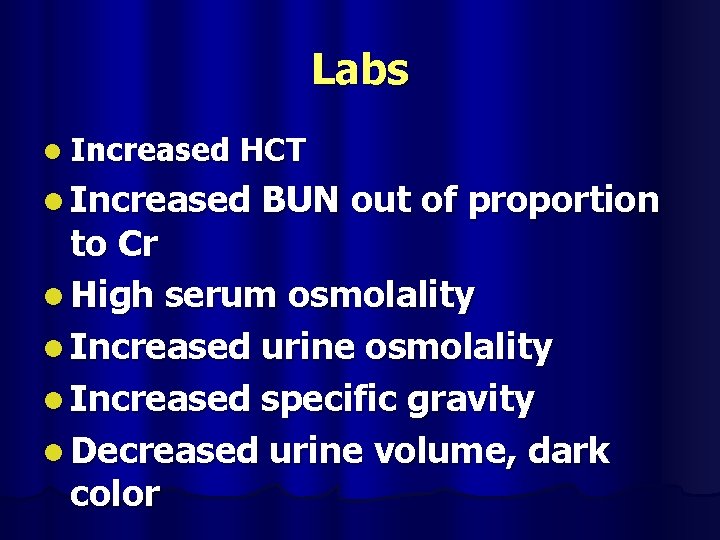
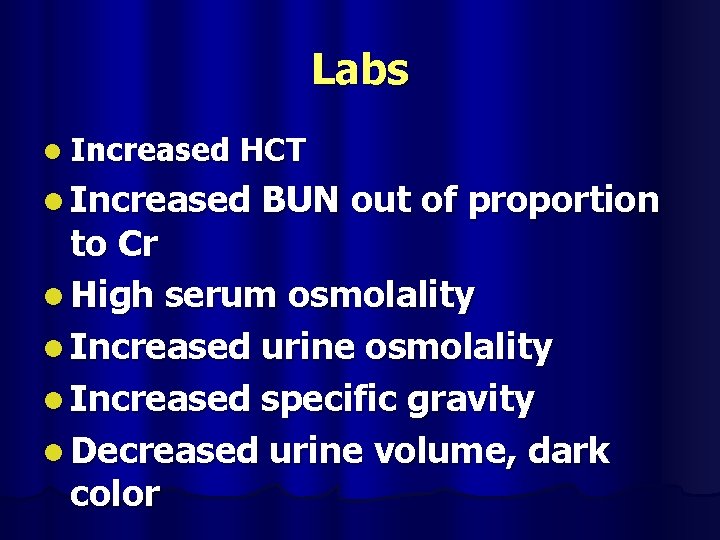
Labs l Increased HCT l Increased BUN out of proportion to Cr l High serum osmolality l Increased urine osmolality l Increased specific gravity l Decreased urine volume, dark color
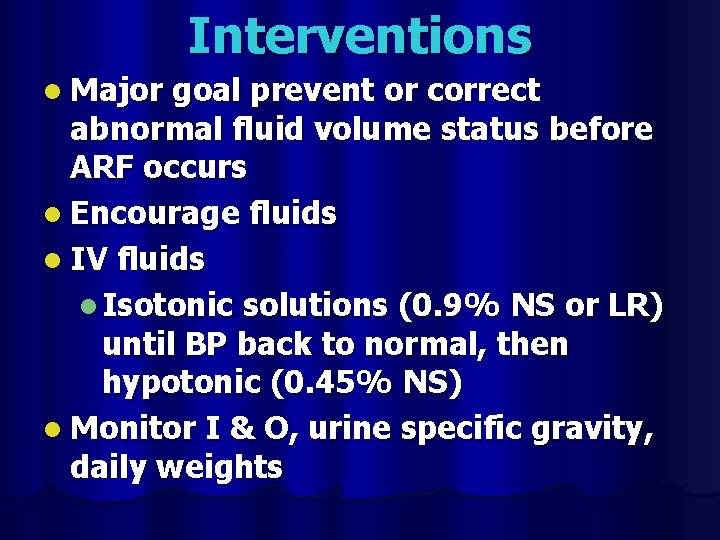
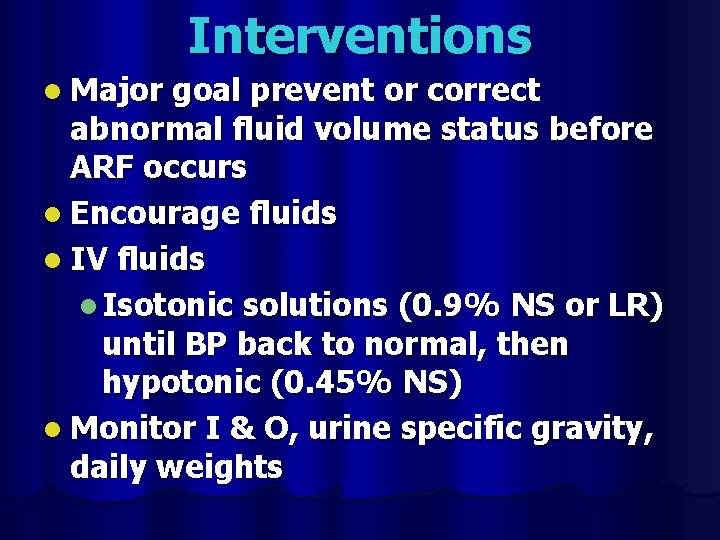
Interventions l Major goal prevent or correct abnormal fluid volume status before ARF occurs l Encourage fluids l IV fluids l Isotonic solutions (0. 9% NS or LR) until BP back to normal, then hypotonic (0. 45% NS) l Monitor I & O, urine specific gravity, daily weights

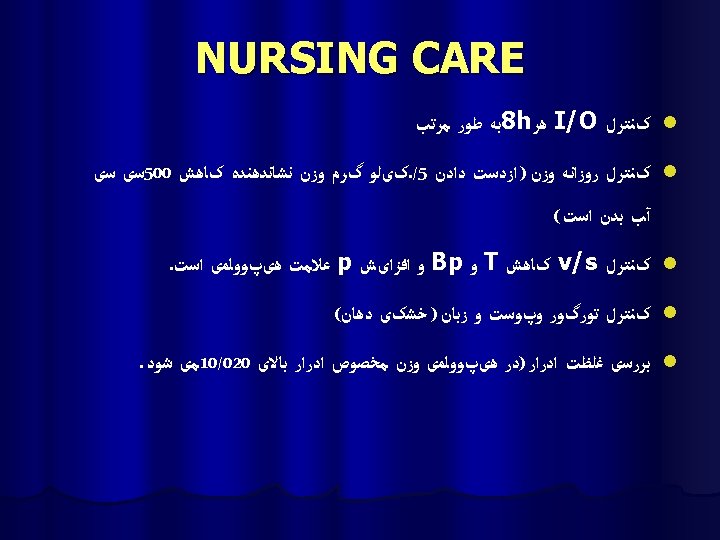
l Monitor skin turgor l Monitor VS and mental status
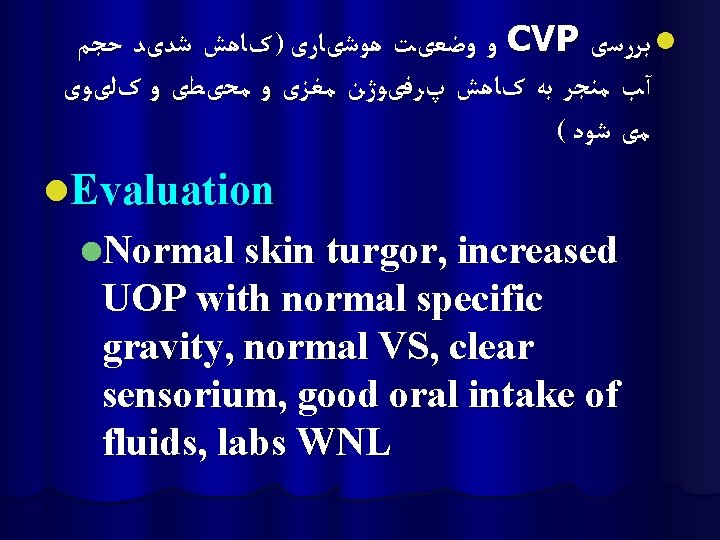
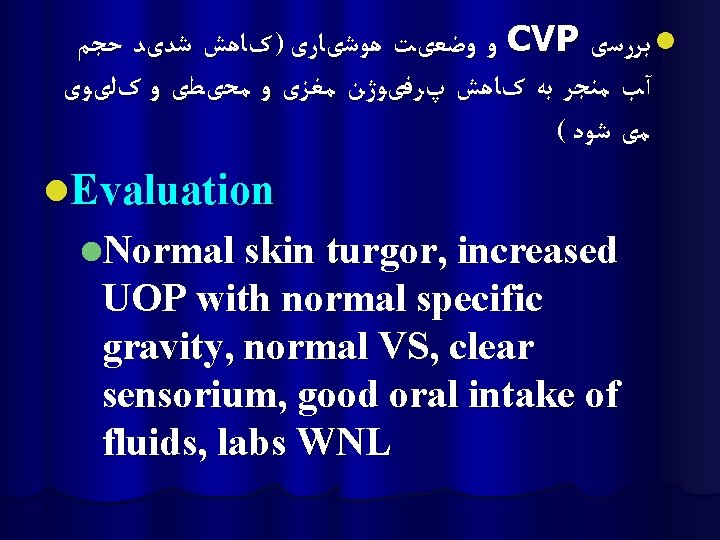
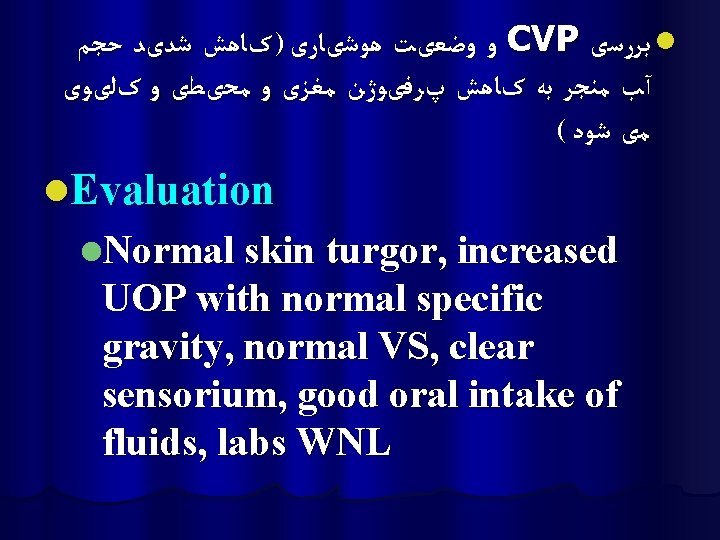
ﻭ ﻭﺿﻌیﺖ ﻫﻮﺷیﺎﺭی ) کﺎﻫﺶ ﺷﺪیﺪ ﺣﺠﻢ CVP ﺑﺮﺭﺳی l آﺐ ﻣﻨﺠﺮ ﺑﻪ کﺎﻫﺶ پﺮﻓیﻮژﻦ ﻣﻐﺰی ﻭ ﻣﺤیﻄی ﻭ کﻠیﻮی ( ﻣی ﺷﻮﺩ l. Evaluation l. Normal skin turgor, increased UOP with normal specific gravity, normal VS, clear sensorium, good oral intake of fluids, labs WNL
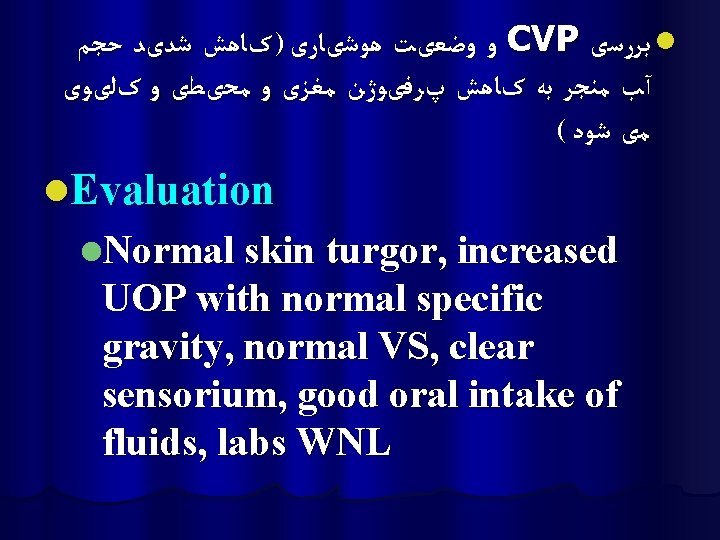
ﻭ ﻭﺿﻌیﺖ ﻫﻮﺷیﺎﺭی ) کﺎﻫﺶ ﺷﺪیﺪ ﺣﺠﻢ CVP ﺑﺮﺭﺳی l آﺐ ﻣﻨﺠﺮ ﺑﻪ کﺎﻫﺶ پﺮﻓیﻮژﻦ ﻣﻐﺰی ﻭ ﻣﺤیﻄی ﻭ کﻠیﻮی ( ﻣی ﺷﻮﺩ l. Evaluation l. Normal skin turgor, increased UOP with normal specific gravity, normal VS, clear sensorium, good oral intake of fluids, labs WNL
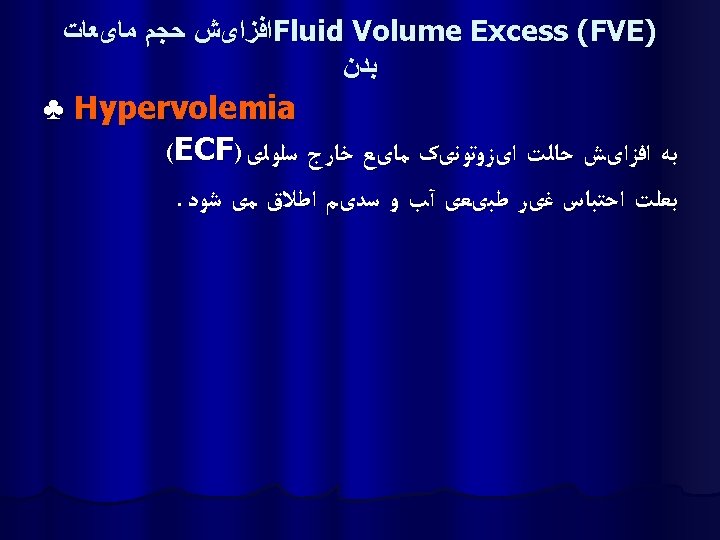
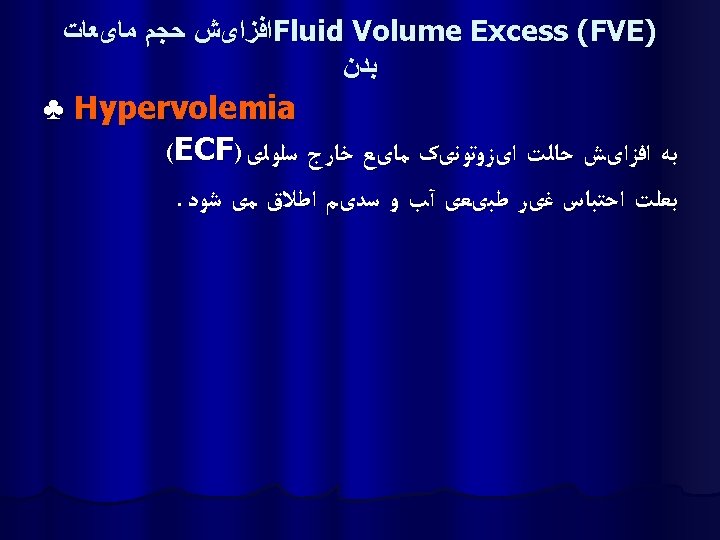
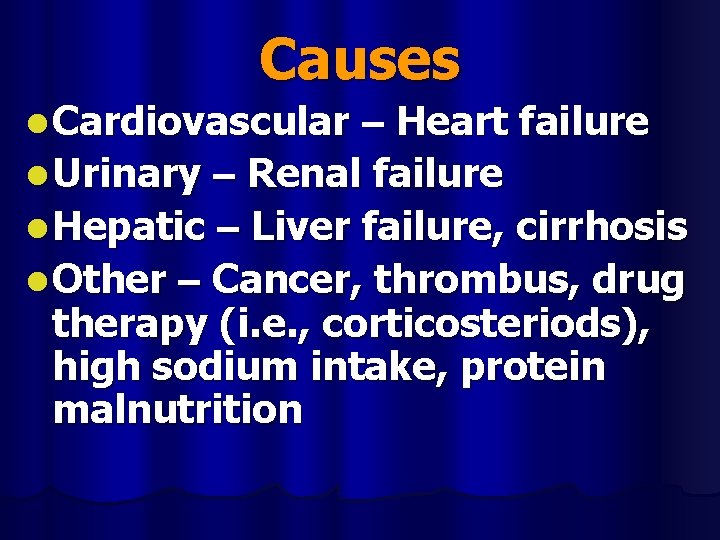
Causes l Cardiovascular – Heart failure l Urinary – Renal failure l Hepatic – Liver failure, cirrhosis l Other – Cancer, thrombus, drug therapy (i. e. , corticosteriods), high sodium intake, protein malnutrition
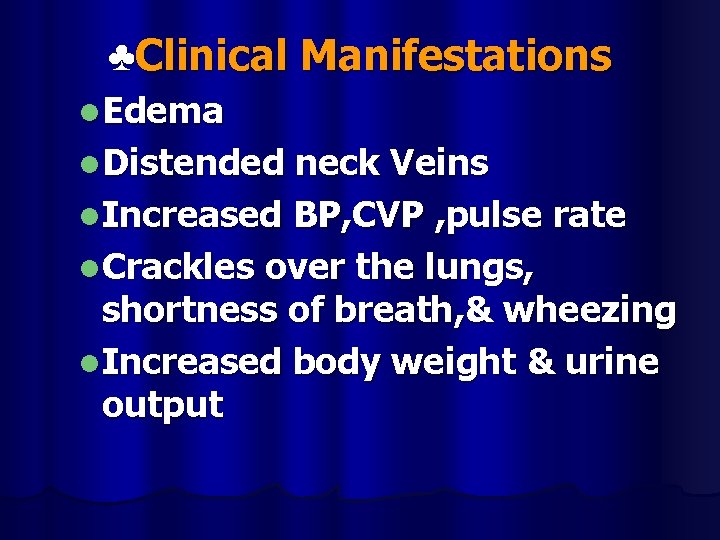
♣Clinical Manifestations l. Edema l. Distended neck Veins l. Increased BP, CVP , pulse rate l. Crackles over the lungs, shortness of breath, & wheezing l. Increased body weight & urine output
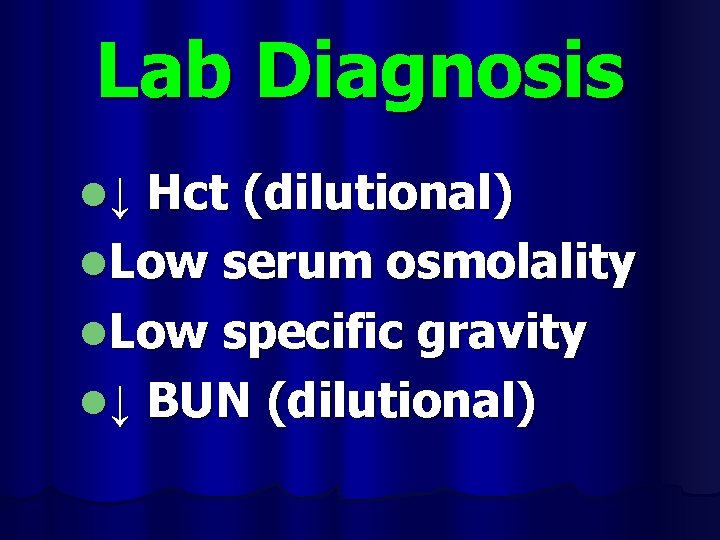
Lab Diagnosis Hct (dilutional) l. Low serum osmolality l. Low specific gravity l↓ BUN (dilutional) l↓
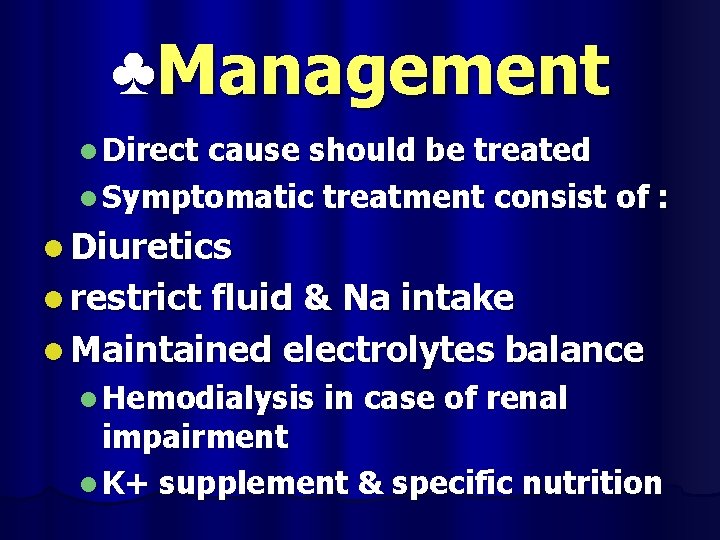
♣Management l Direct cause should be treated l Symptomatic treatment consist of : l Diuretics l restrict fluid & Na intake l Maintained electrolytes balance l Hemodialysis in case of renal impairment l K+ supplement & specific nutrition
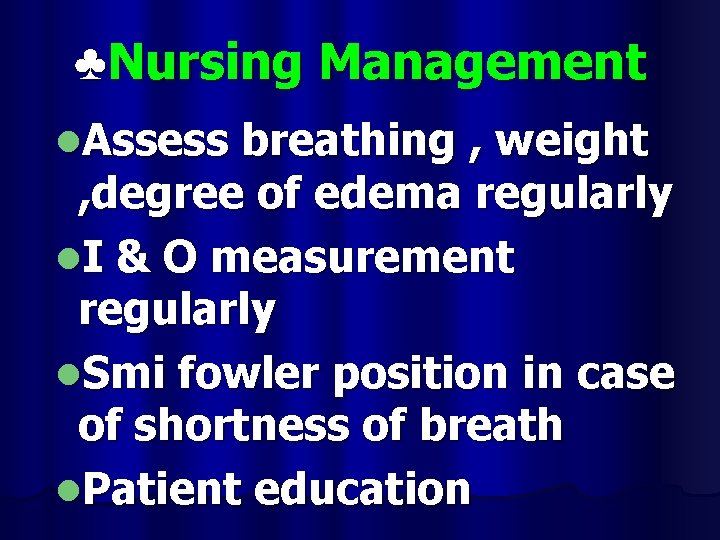
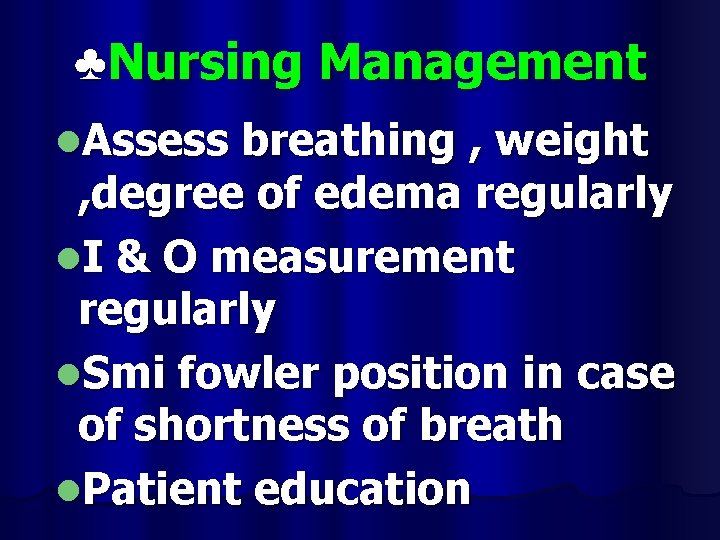
♣Nursing Management l. Assess breathing , weight , degree of edema regularly l. I & O measurement regularly l. Smi fowler position in case of shortness of breath l. Patient education

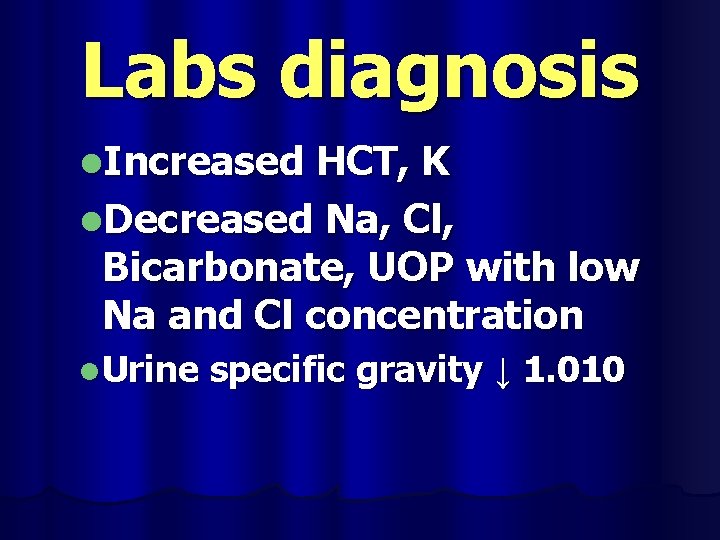
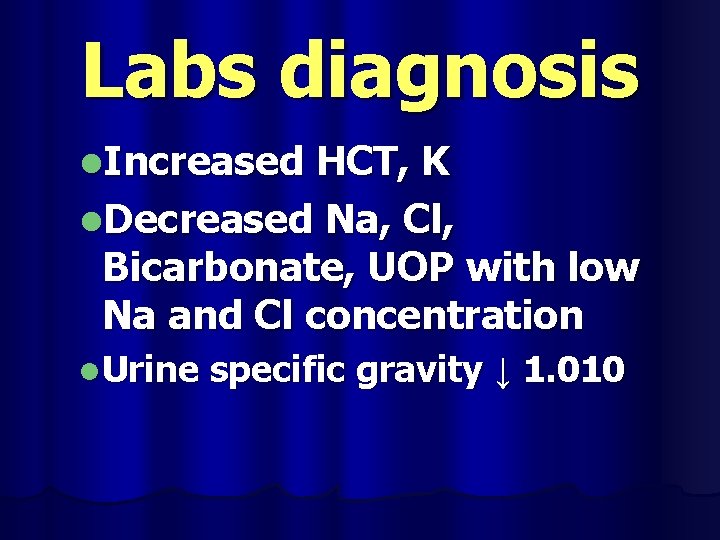
Labs diagnosis l. Increased HCT, K l. Decreased Na, Cl, Bicarbonate, UOP with low Na and Cl concentration l. Urine specific gravity ↓ 1. 010

Clinical Manifestations BP l Anorexia l lethargy l muscle cramps l seizures l exhaustion l decreased l Poor skin turgor muscle tone l dry mucosa/skin l muscle tremors l Confusion l vomiting l headache l diarrhea l↓
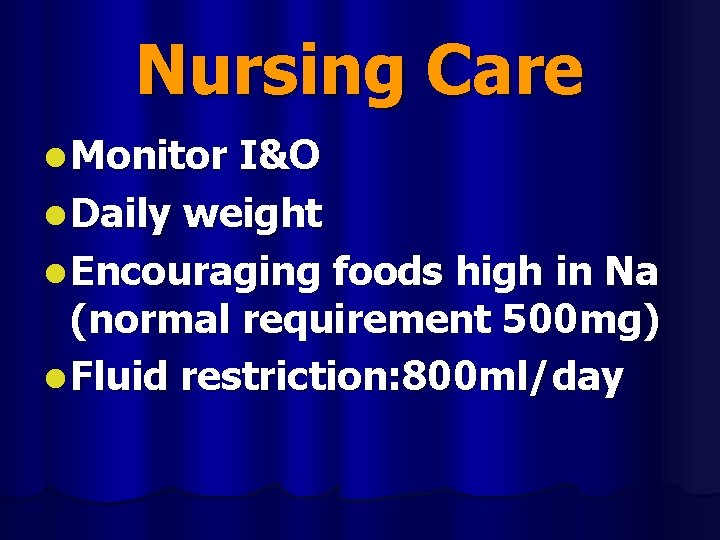
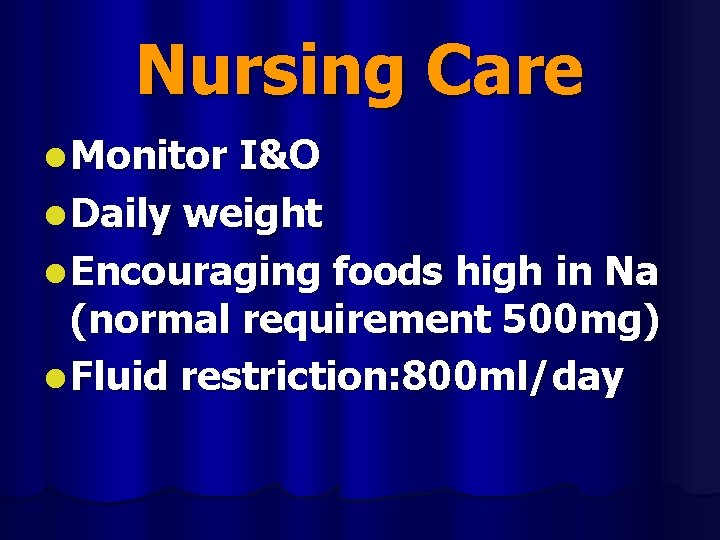
Nursing Care l Monitor I&O l Daily weight l Encouraging foods high in Na (normal requirement 500 mg) l Fluid restriction: 800 ml/day





Free Powerpoint Templates Page 142
Thanks for attention Free Powerpoint Templates Page 143
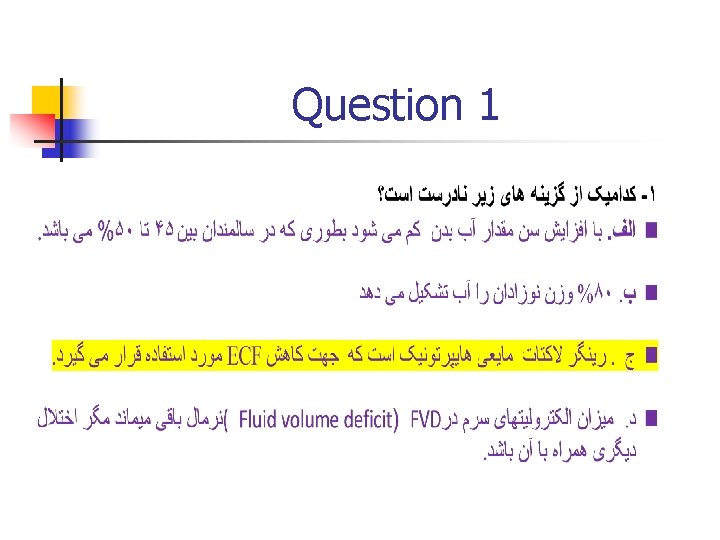
Question 1
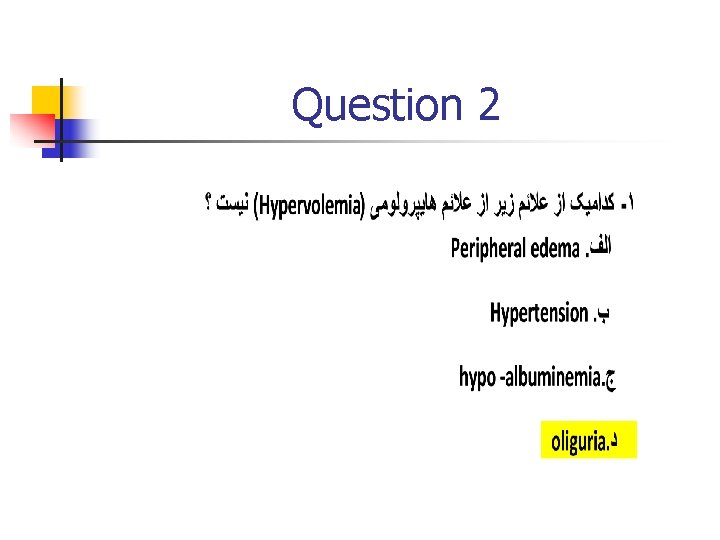
Question 2
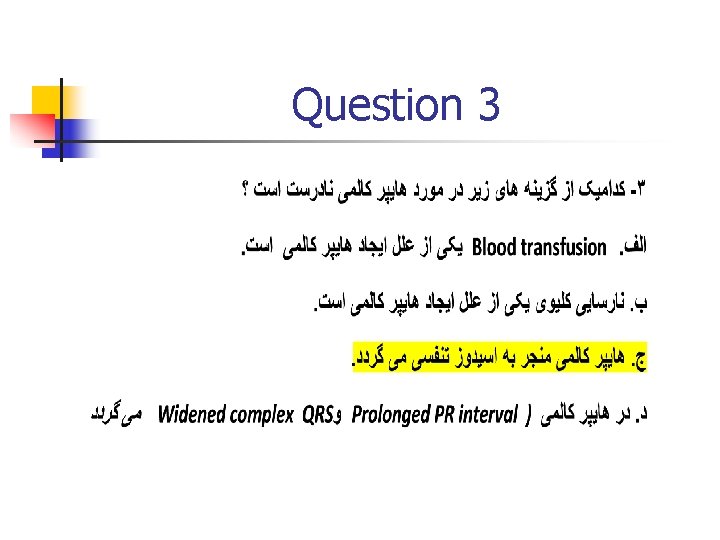
Question 3
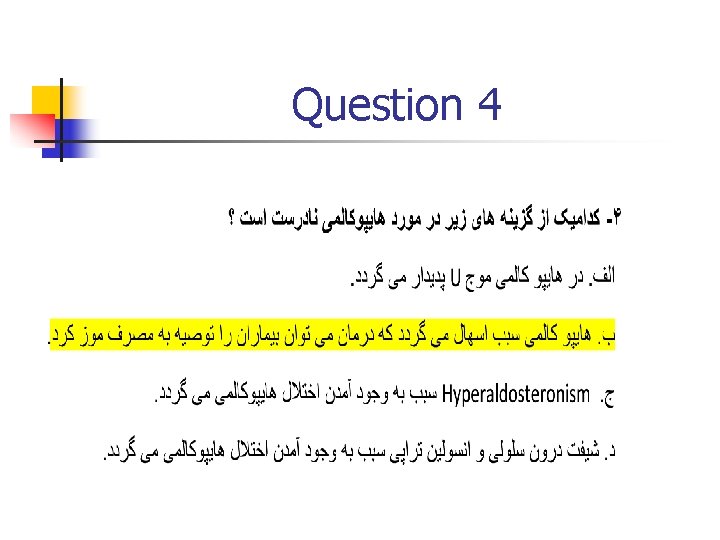
Question 4
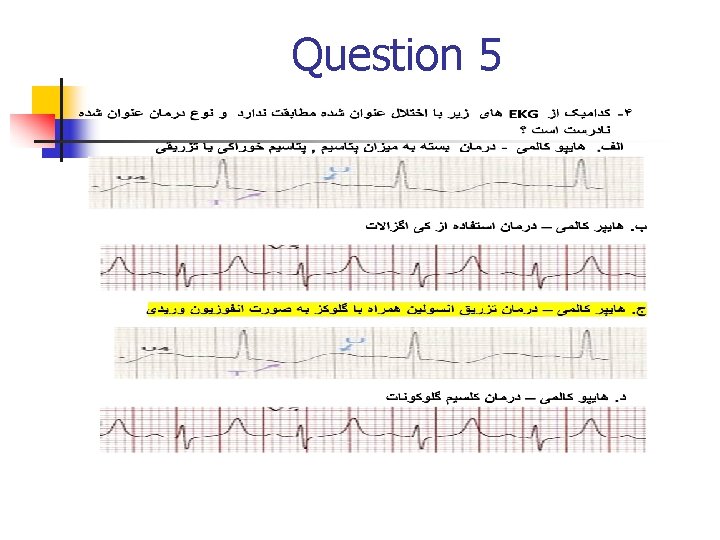
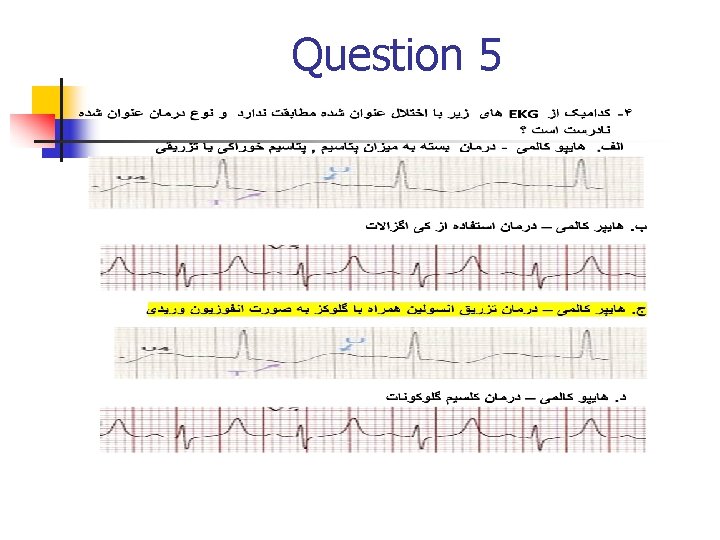
Question 5
Question 6
Question 7
Question 8
Question 9
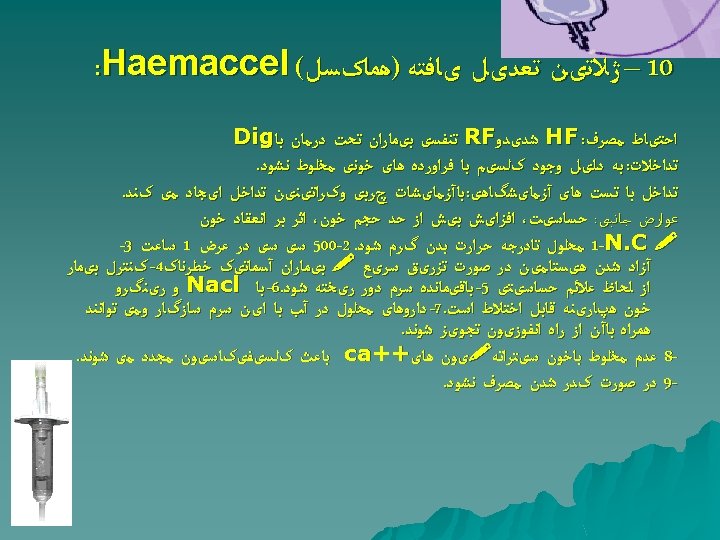
Question 10
