Fractures of the femoral diaphysis including subtrochanteric fracturesmanagement
Fractures of the femoral diaphysis (including subtrochanteric fractures)—management principles AO Trauma Basic Principles Course
Learning objectives • • Elaborate on intramedullary (IM) nailing as the preferred method of stabilization Discuss the need for cephomedullary fixation Understand reaming issues and the implications Consider alternative fixation options to IM nailing
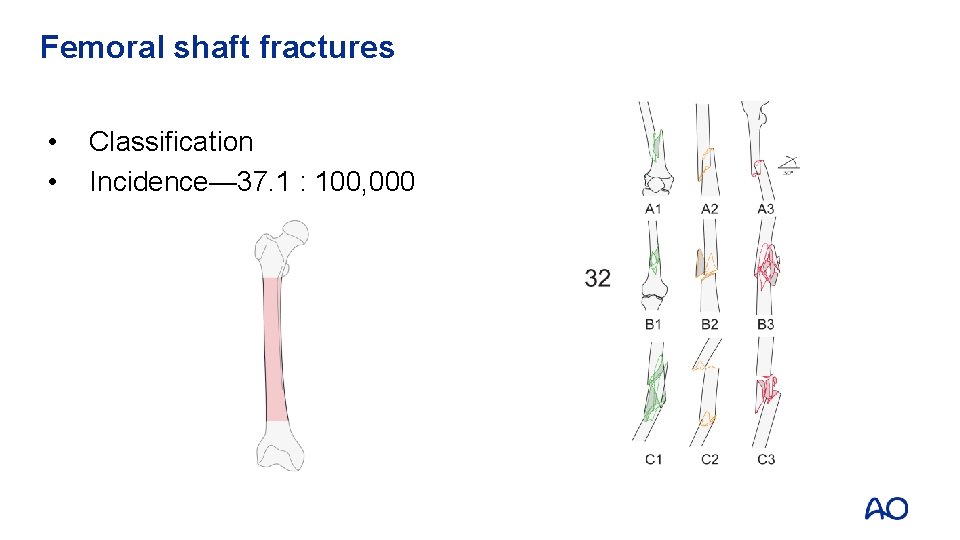
Femoral shaft fractures • • Classification Incidence— 37. 1 : 100, 000
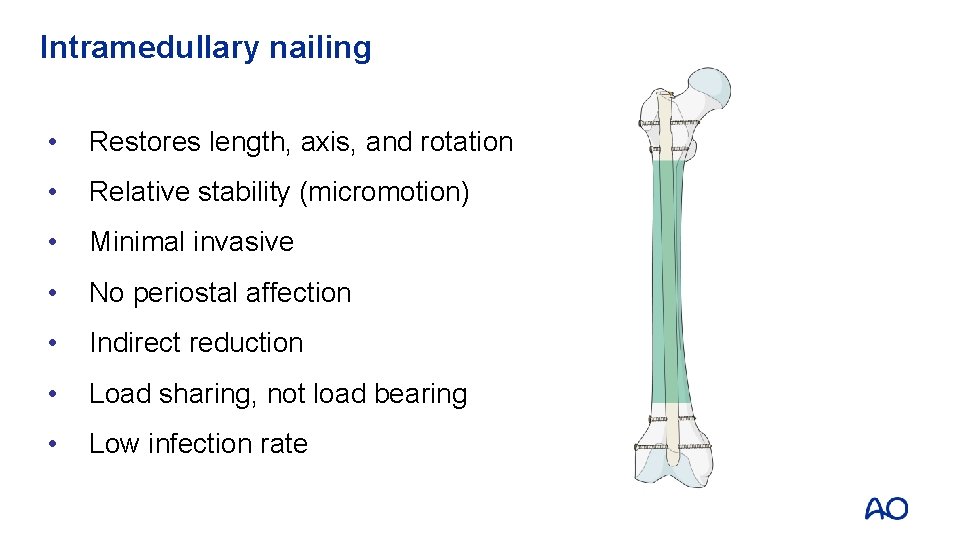
Intramedullary nailing • Restores length, axis, and rotation • Relative stability (micromotion) • Minimal invasive • No periostal affection • Indirect reduction • Load sharing, not load bearing • Low infection rate

• 28 -year-old man • Fall from 4 meters • AO B 1, C II° Postoperative

Follow-up
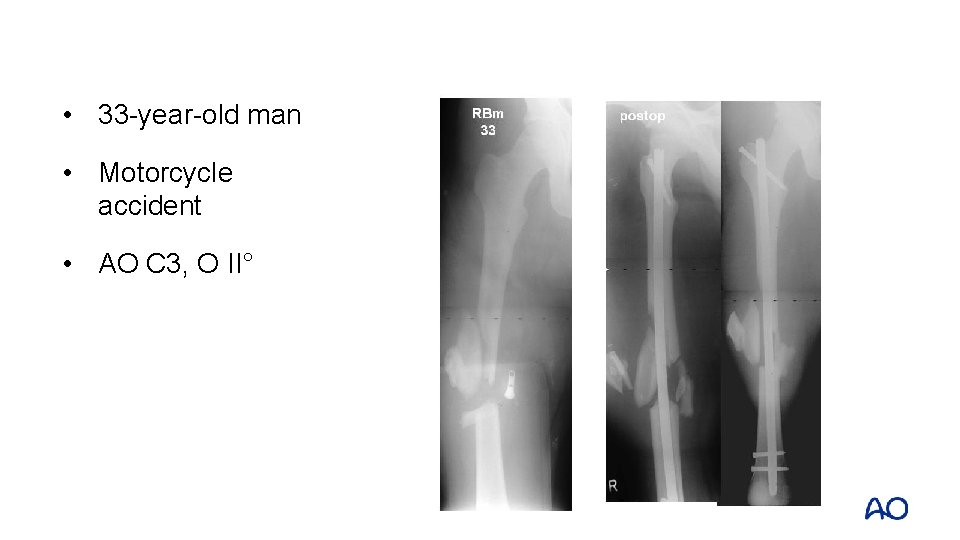
• 33 -year-old man • Motorcycle accident • AO C 3, O II°
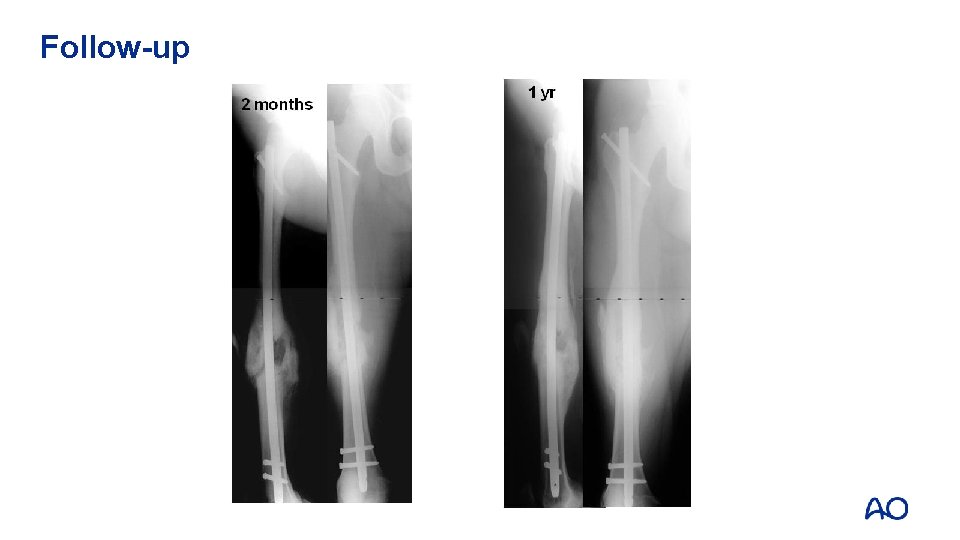
Follow-up
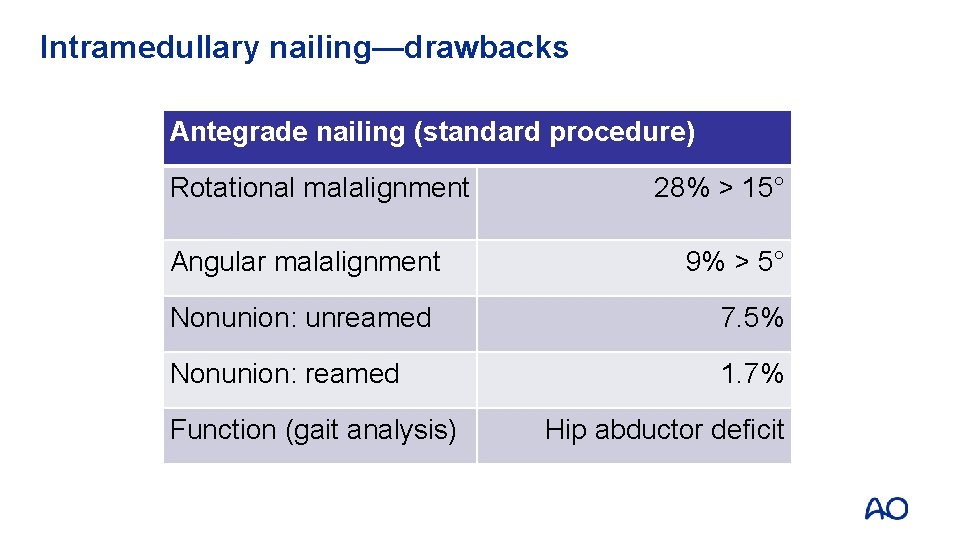
Intramedullary nailing—drawbacks Antegrade nailing (standard procedure) Rotational malalignment Angular malalignment 28% > 15° 9% > 5° Nonunion: unreamed 7. 5% Nonunion: reamed 1. 7% Function (gait analysis) Hip abductor deficit
Reduction of femoral diaphyseal fractures • Distraction, as a principle • Traction table • Distractor • Utilize indirect reduction methods
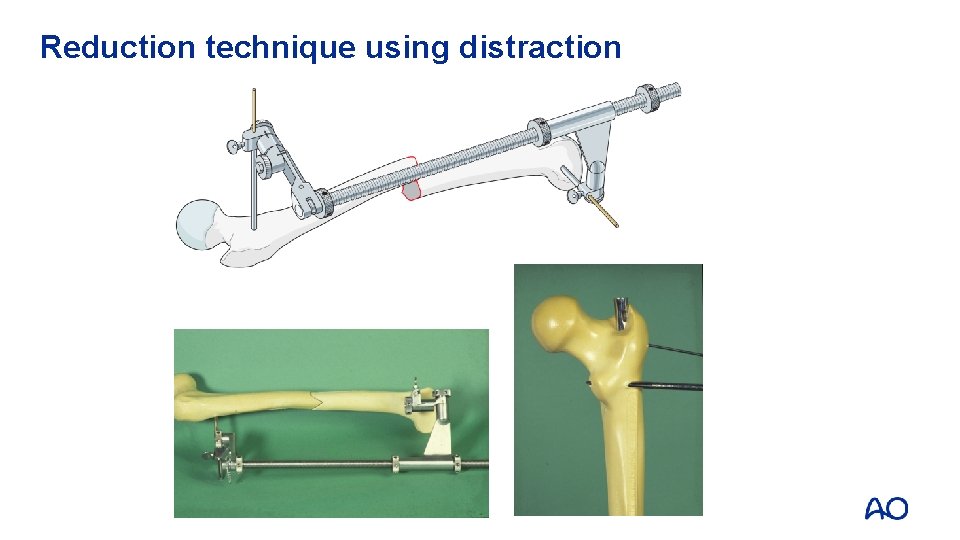
Reduction technique using distraction
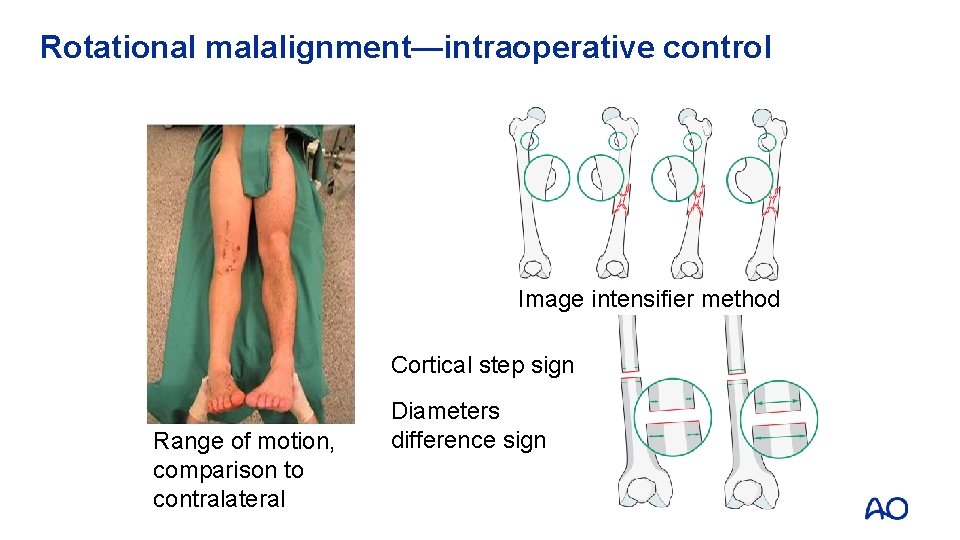
Rotational malalignment—intraoperative control Image intensifier method Cortical step sign Range of motion, comparison to contralateral Diameters difference sign
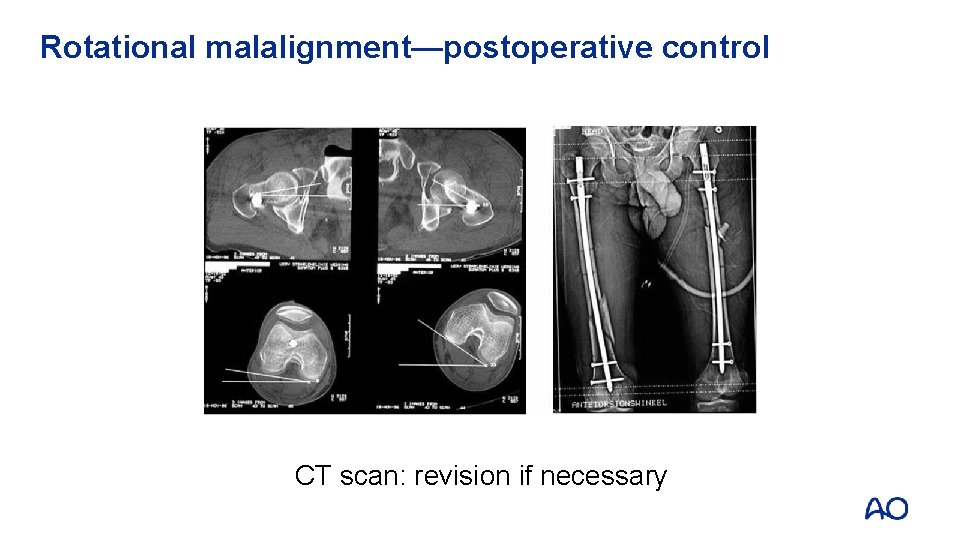
Rotational malalignment—postoperative control CT scan: revision if necessary

Hip abductor weakness—change of entrance point Other advantages: • Easier accessible (especially in obese patients) • No damage to the A. circumflexa media
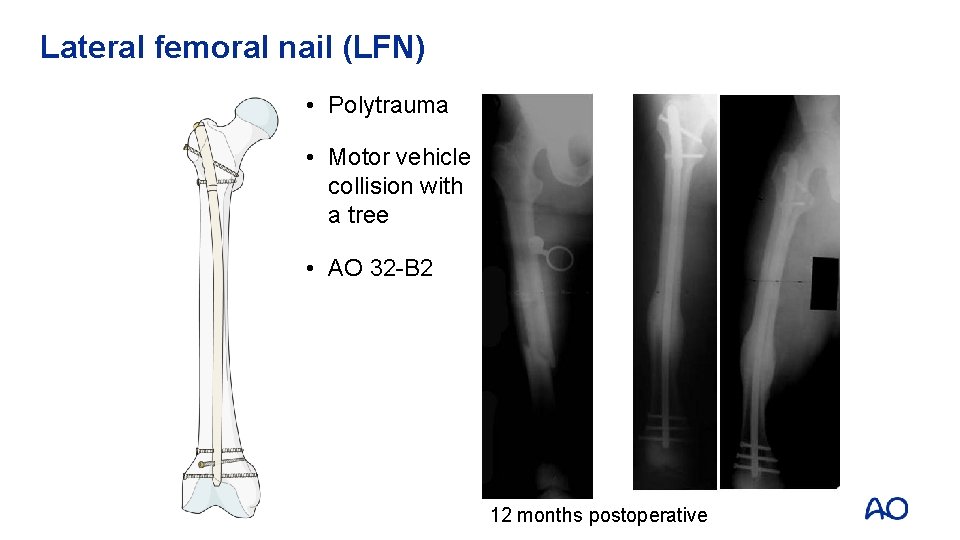
Lateral femoral nail (LFN) • Polytrauma • Motor vehicle collision with a tree • AO 32 -B 2 12 months postoperative
To ream or not to ream? • Reamed • Shorter time to union and higher union rates (nonunion: 1% versus 7. 2%, NNT 16) • Increased risk of pulmonary embolism • Unreamed • Shorter duration of operation • Less blood loss • Bolt breakage, more delayed unions
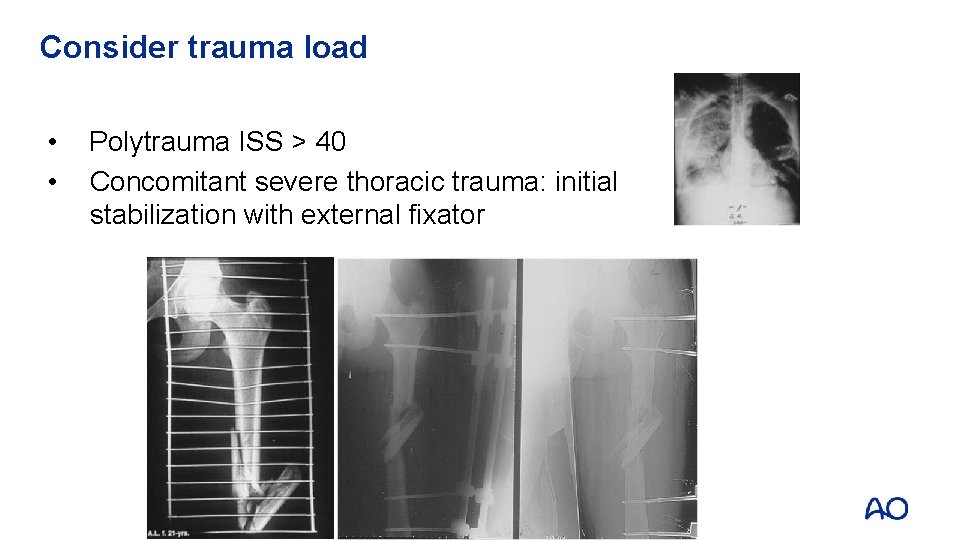
Consider trauma load • • Polytrauma ISS > 40 Concomitant severe thoracic trauma: initial stabilization with external fixator
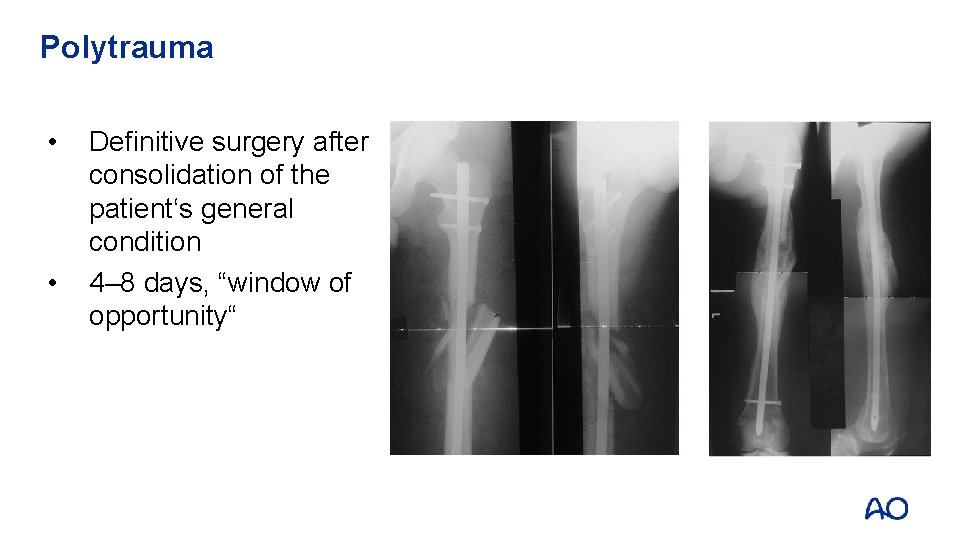
Polytrauma • • Definitive surgery after consolidation of the patient‘s general condition 4– 8 days, “window of opportunity“
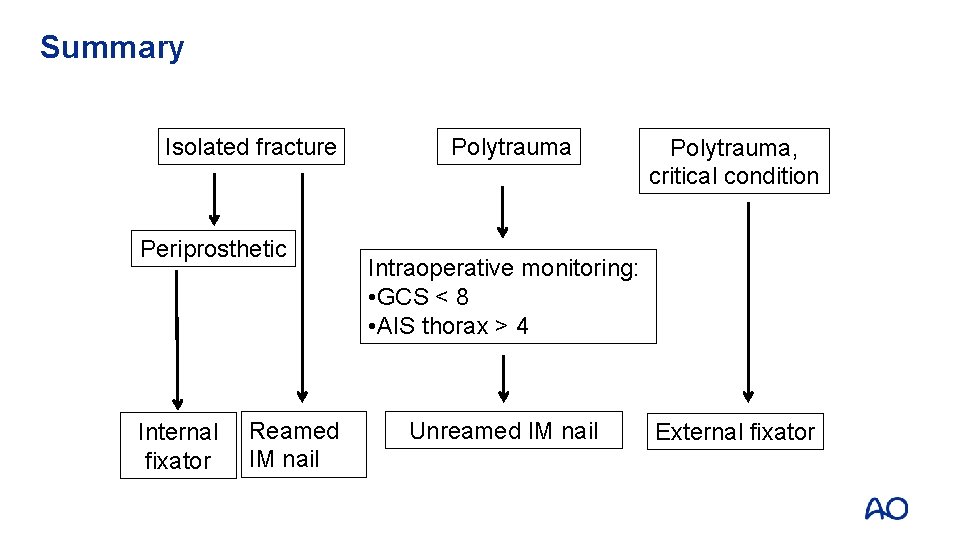
Summary Isolated fracture Periprosthetic Internal fixator Reamed IM nail Polytrauma, critical condition Intraoperative monitoring: • GCS < 8 • AIS thorax > 4 Unreamed IM nail External fixator
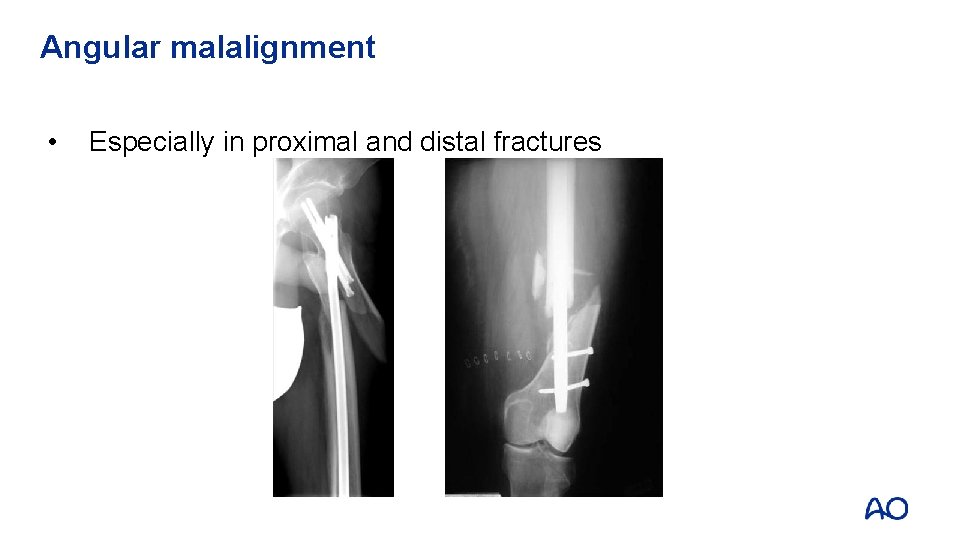
Angular malalignment • Especially in proximal and distal fractures
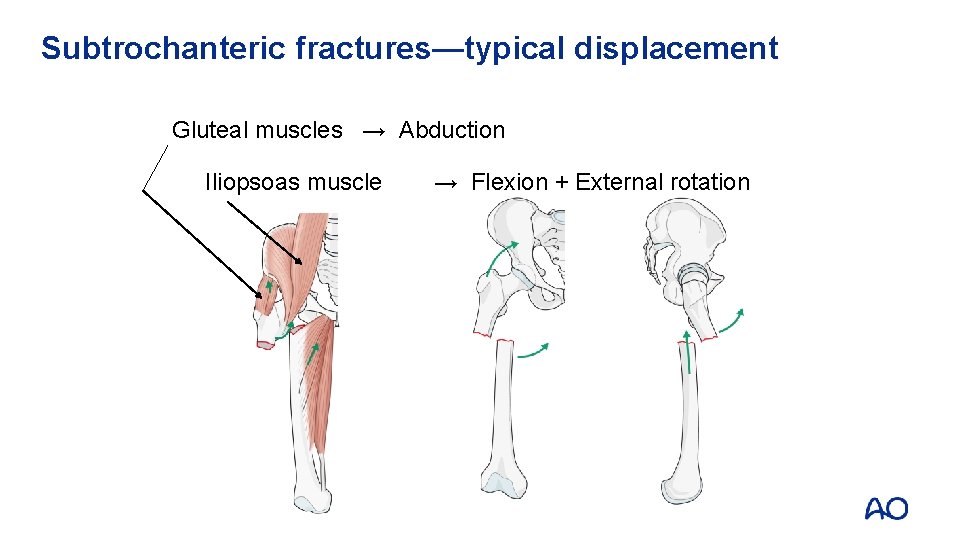
Subtrochanteric fractures—typical displacement Gluteal muscles → Abduction Iliopsoas muscle → Flexion + External rotation
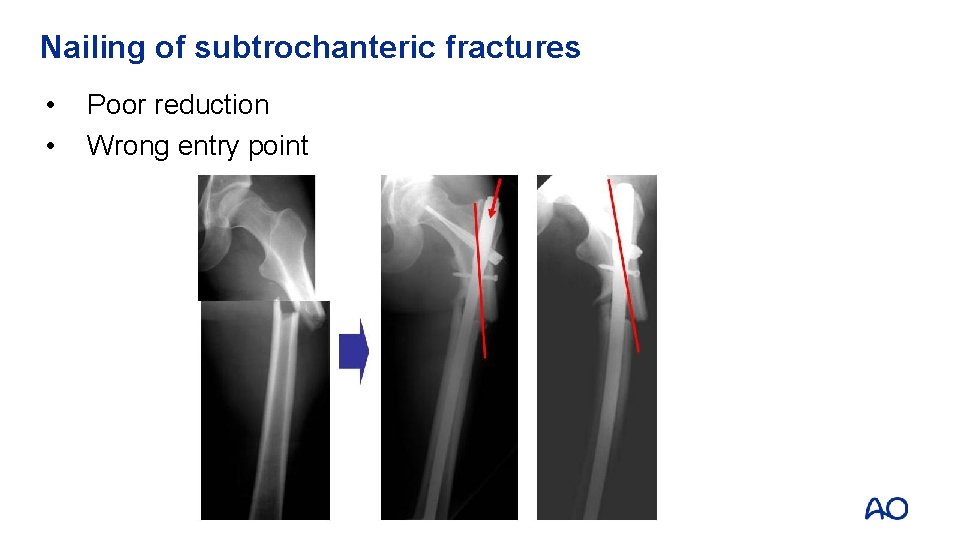
Nailing of subtrochanteric fractures • • Poor reduction Wrong entry point
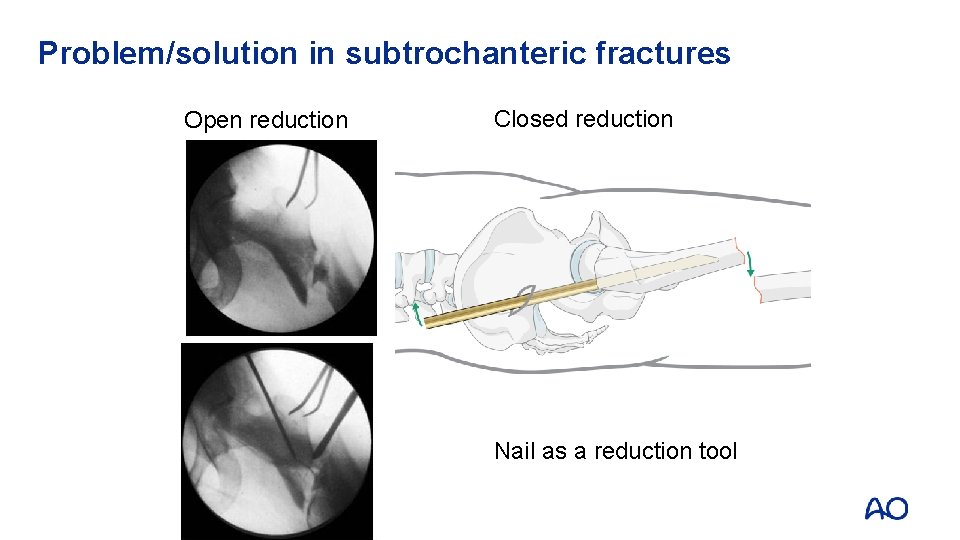
Problem/solution in subtrochanteric fractures Open reduction Closed reduction Nail as a reduction tool
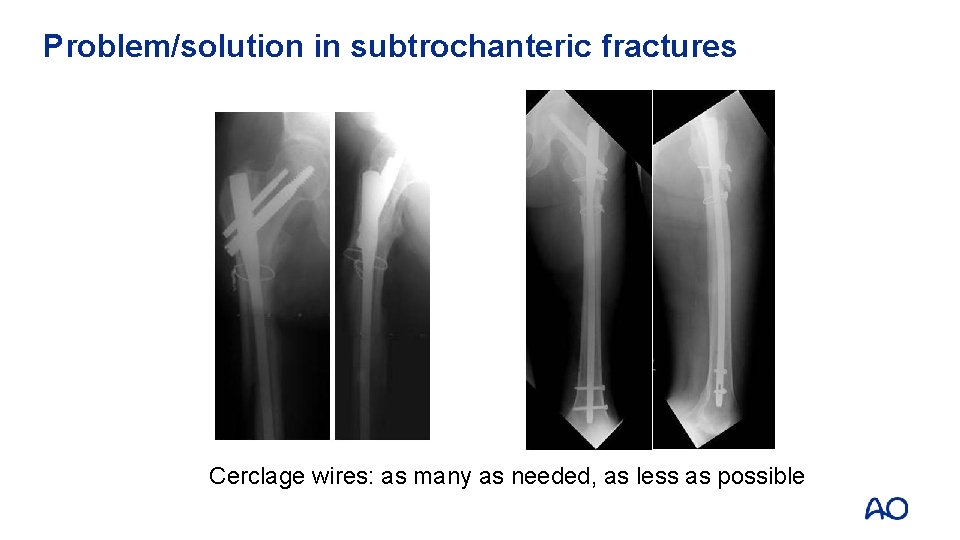
Problem/solution in subtrochanteric fractures Cerclage wires: as many as needed, as less as possible
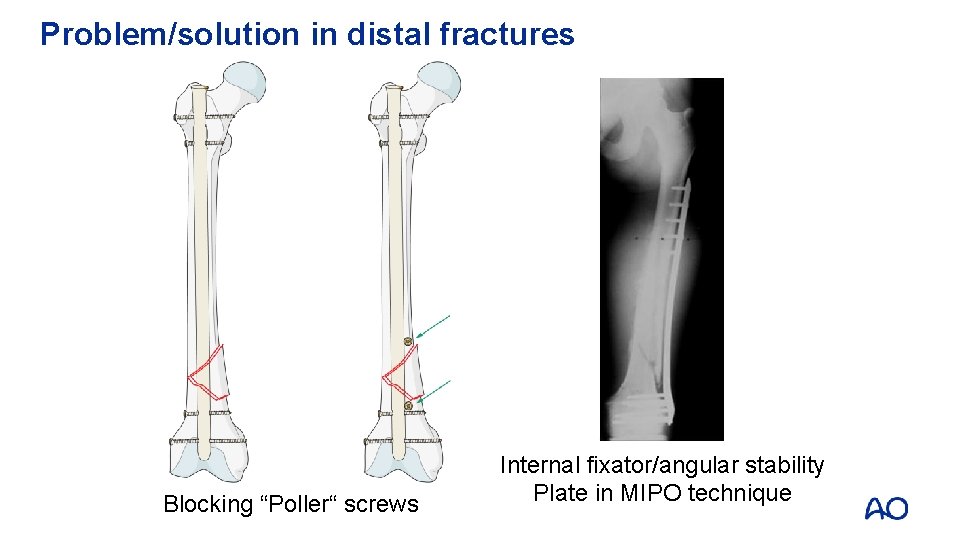
Problem/solution in distal fractures Blocking “Poller“ screws Internal fixator/angular stability Plate in MIPO technique
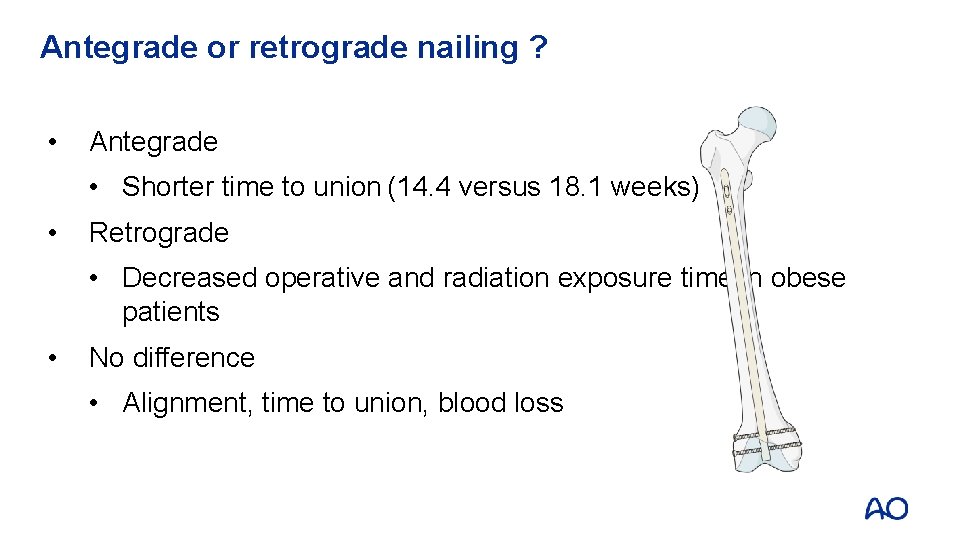
Antegrade or retrograde nailing ? • Antegrade • Shorter time to union (14. 4 versus 18. 1 weeks) • Retrograde • Decreased operative and radiation exposure time in obese patients • No difference • Alignment, time to union, blood loss
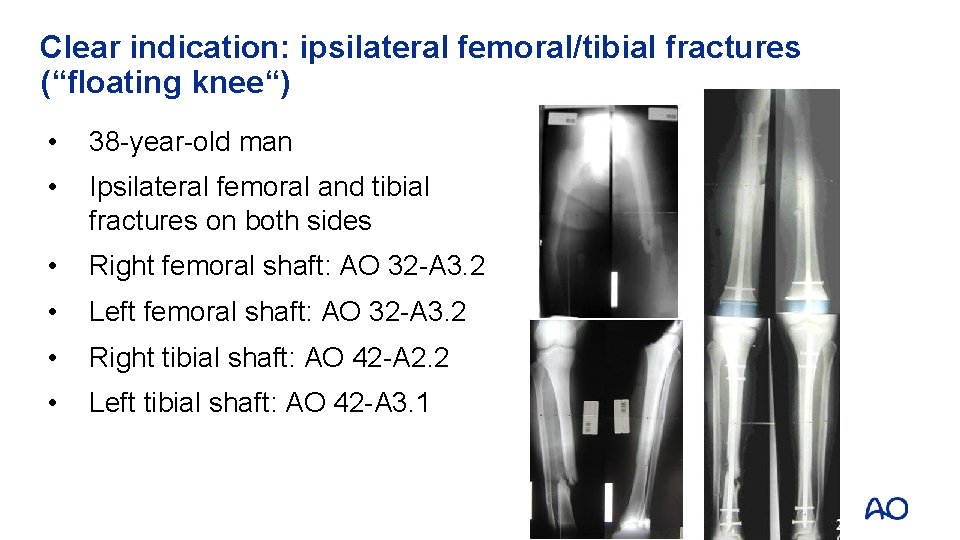
Clear indication: ipsilateral femoral/tibial fractures (“floating knee“) • 38 -year-old man • Ipsilateral femoral and tibial fractures on both sides • Right femoral shaft: AO 32 -A 3. 2 • Left femoral shaft: AO 32 -A 3. 2 • Right tibial shaft: AO 42 -A 2. 2 • Left tibial shaft: AO 42 -A 3. 1
Intramedullary nailing—indications • Unreamed nailing: • Acute fractures • Reamed nailing: • Nonunions • Revisional operations • Retrograde nailing: • “Floating knee“ • Obese patients • Distal shaft fractures
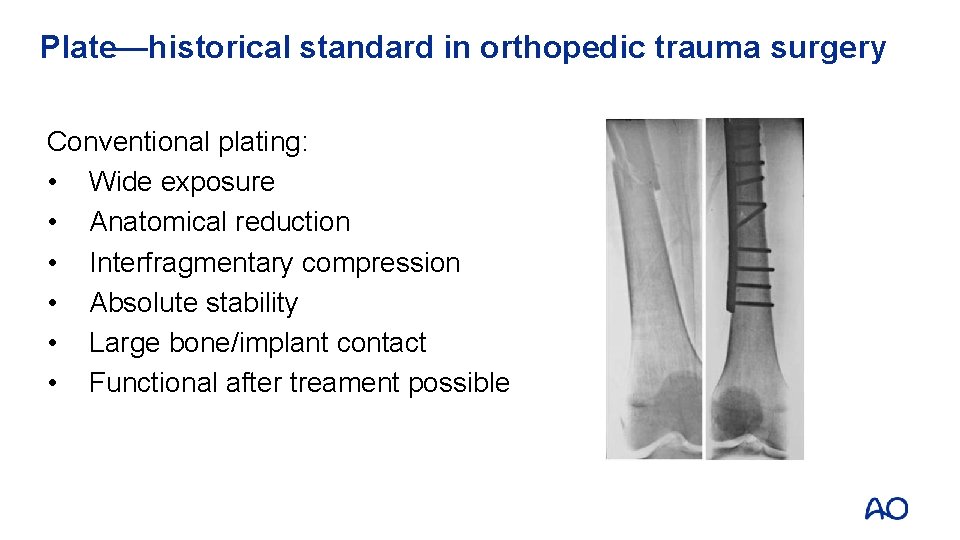
Plate—historical standard in orthopedic trauma surgery Conventional plating: • Wide exposure • Anatomical reduction • Interfragmentary compression • Absolute stability • Large bone/implant contact • Functional after treament possible
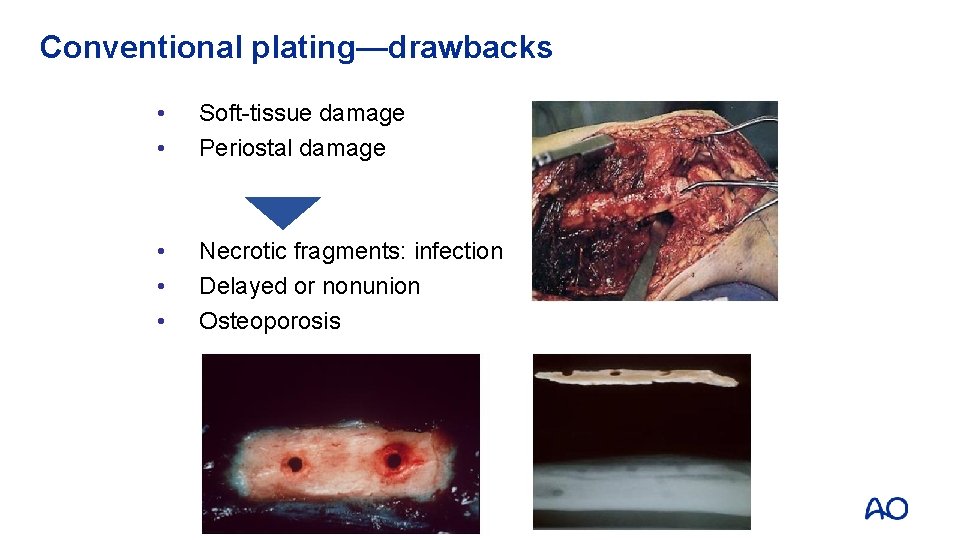
Conventional plating—drawbacks • • Soft-tissue damage Periostal damage • • • Necrotic fragments: infection Delayed or nonunion Osteoporosis
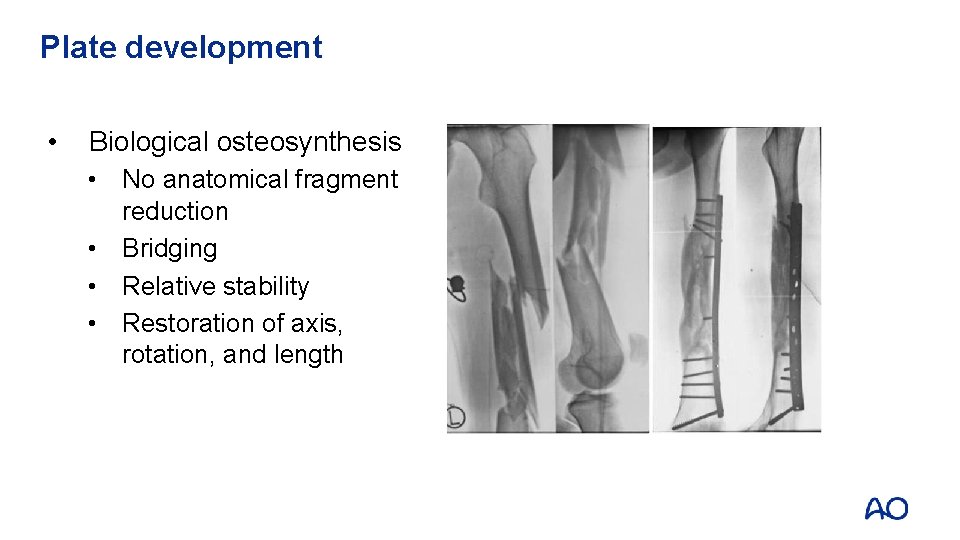
Plate development • Biological osteosynthesis • No anatomical fragment reduction • Bridging • Relative stability • Restoration of axis, rotation, and length
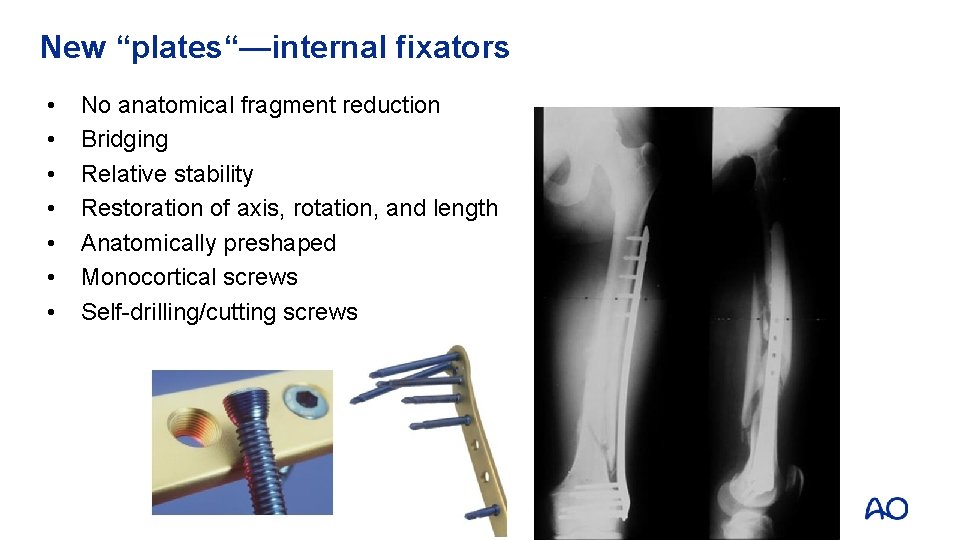
New “plates“—internal fixators • • No anatomical fragment reduction Bridging Relative stability Restoration of axis, rotation, and length Anatomically preshaped Monocortical screws Self-drilling/cutting screws
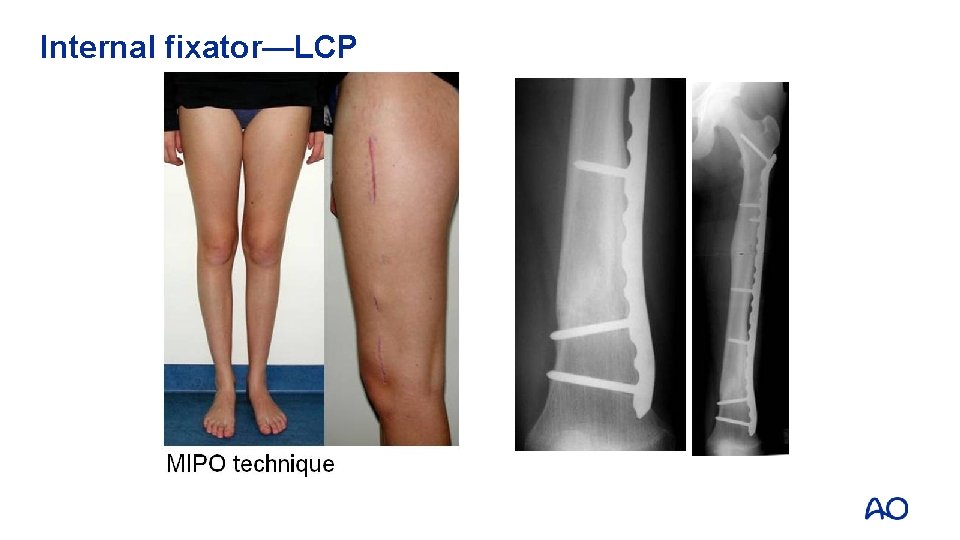
Internal fixator—LCP
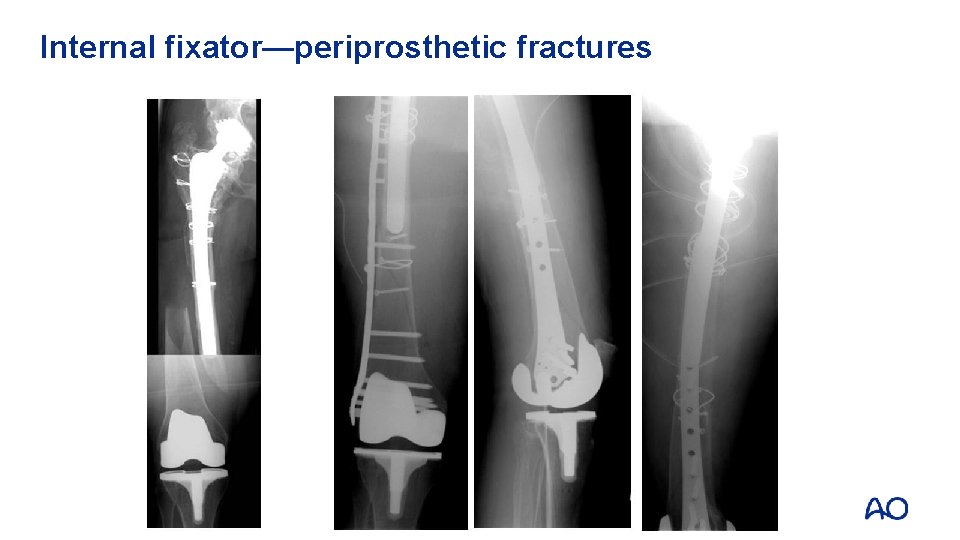
Internal fixator—periprosthetic fractures
Plate (internal fixator)—indications Principally each femoral shaft fracture especially: • Associated injuries (acetabular fractures, open growth plates, vascular injuries) • Preconditions for nailing logistically and anatomically not fulfilled • Periprosthetic and peri-implant fractures
External fixator • Indirect reduction • Relative stability • Minimally invasive • No significant periostal or endostal affection • Patient discomfort
External fixator Indications • Temporary: damage control in multiple-injured patients • Temporary: open fractures • Definitely: children • Definitely: infection
Take-home messages • • • Nailing is the gold standard Reaming is recommended Metaphyseal fractures require consideration of: • Cephalomedullary stabilization • Alternative plating • • Plating implies bridging and use of locked screws External fixation is indicated as temporary stabilization and for special situations
- Slides: 38