Fracture Fixation Fracture Fixation Casts Wires Pins Screws
- Slides: 36
Fracture Fixation • Fracture Fixation Casts Wires Pins Screws Cortical Bone Plates Maxillofacial Fractures Trabecular Bone Fractures Intramedullary Devices Artificial Bone Mineral • Bone Grafts and Supplementation • Dental Implants Whole Teeth Endosseous Implants Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Classification • Based on morphology of fracture • Results from variations in: - Direction of load - Magnitude and area of application of force - Rate of loading • Fractures can result from: - Direct loads - gun shots, direct blow to bone, crushing - Indirect loads - through muscles or joints Fracture Glossary • Comminuted - multiple fragments • Complex - soft tissue injury (disruption of free ends) • Simple - minimal or no soft tissue injury (no disruption) • Open - bone ends exposed to outside environment • Closed - bone ends covered with skin and soft tissue Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation (1) • Numerous systems have been developed to assist a bone’s natural healing properties - Plates - Screws - Pins - External fixators - Intramedullary nails • Fixation systems are typically compared in terms of stabilization (stiffness) - Axial - Bending - Torsion • Performance of a fracture fixation system will depend on: - Natural stability of fracture - State of contact between fragments Organi Artificiali e Protesi Prof. O. Sbaizero
Goals: Mechanical stability Proper healing Allow general function of limb Minimize healing time Comfortable and attractive Fracture Fixation (2) Constraints: No adverse tissue reactions Low cost Ease of use Minimal tissue damage Patient compliance • Method should take into account mechanisms which enhance bone healing - Loading in compression vs. tension - Weight-bearing vs. non-weight-bearing • However, best loading mechanism for fracture healing is not understood and studies have yielded conflicting results - Typical: apply some load to damaged tissue to induce growth and prevent resorption, but not too much that it damages bone cells Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Casts Benefits: Cheap Protection from external forces Non-invasive, no tissue damage Easy to use and remove Problems: No direct mechanical fixation Can't get it wet Poor skin reaction Can't cleanse area under cast Good positioning of bone is more difficult non-invasively Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Wires • Simplest and most versatile implant • Less than 3/32 inch diameter for classification as wire (Kirschen wire < 2 mm diameter) • Used to hold fragments of bone together - Facial fractures - "Shattered" bones - Reattachment of greater trochanter in hip replacements if fracture distal to typical osteotomy location - Long oblique or spiral fractures Benefits: Flexible - can be deformed to join pieces in various positions Cheap Easy to use Less damage to tissue than other internal devices Problems: Stress corrosion can occur at bent part of wire Fatigue of thin wire possible due to cyclic loading Not very stable Organi Artificiali e Protesi Prof. O. Sbaizero
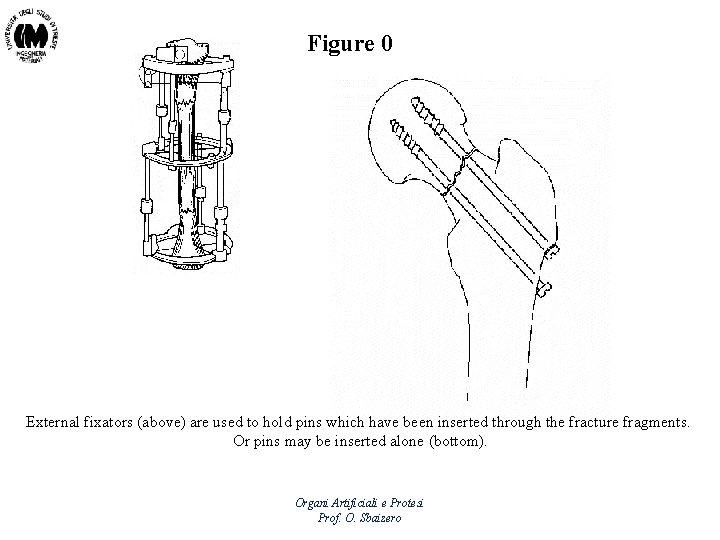
Fracture Fixation - Pins • Diameters greater than 3/32 inch, unthreaded • Used in cases where plating is difficult or o their means of achieving stability are not possible • Pins implanted percutaneously into bone segments and connected/fixed using an external fixator (See Figure 0) • Pins removed after fracture healing has occured Benefits: Relatively easy to use Holds bone in place Less tissue damage and corrosion than plates, nails, etc. Problems: Infection likely due to percutaneous fixation No mechanical hold on pin without external fixation Soft tissue is damaged when pins are removed External fixation is unattractive and awkward Organi Artificiali e Protesi Prof. O. Sbaizero
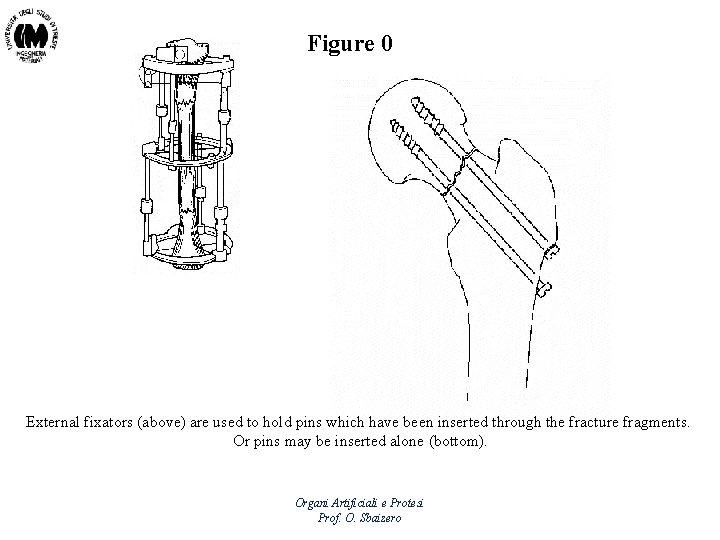
Figure 0 External fixators (above) are used to hold pins which have been inserted through the fracture fragments. Or pins may be inserted alone (bottom). Organi Artificiali e Protesi Prof. O. Sbaizero
External Fixation • High stresses at the pin-bone interface can be minimized by increasing the bending stiffness of the pins - Increasing diameter - Increasing modulus of material - Reducing separation of side bars of fixator (shorter pins) - Using a full-pin configuration • Half-pin configurations result in high stress in entry cortex - Location of most pin-bone failures • Pins are also a potential site of infection Organi Artificiali e Protesi Prof. O. Sbaizero
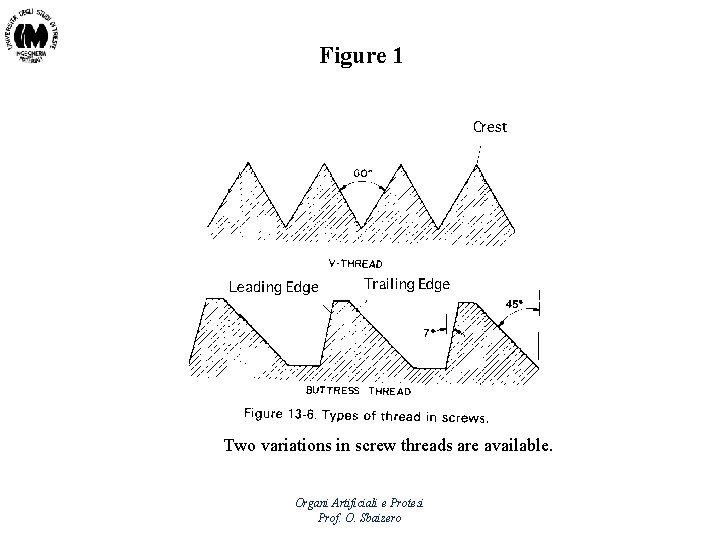
Fracture Fixation - Screws (1) • Used alone to connect bone fragments or in conjunction with plates • Head designs typical of other screw types • Two variations of screw design - Self-tapping: cuts its own threads as it is s crewed in # Similar to a wood screw - Non-self-tapping: requires pre-tapping of hol e - Pull out strengths equal for both designs of screw • Two variations of thread design (See Figure 1)- V-thread and Buttress thread Organi Artificiali e Protesi Prof. O. Sbaizero
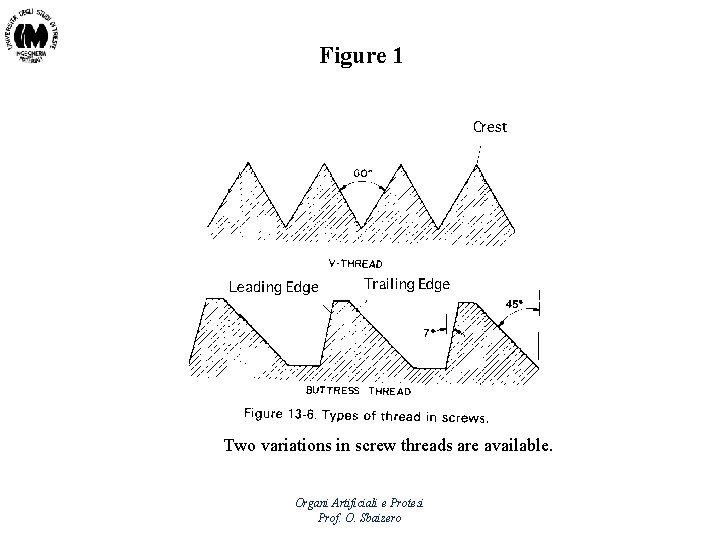
Figure 1 Two variations in screw threads are available. Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Screws (2) • Pull-out strength of screws is directly dependent on the diameter of the screw - Larger screws have a higher pull-out strength - Further design differences have little effect on pull-out strength • Tissue immediately adjacent to screw may necrose and resorb initially - Due to initial trauma of inserting the screw - Once screw is firmly fixed, tissue ingrowth into the threads occurs - If micromotion exists between the screw and t he surrounding bone, a fibrous capsule will form between the two materials # Prevents ingrowth of bone and optimal fixation # Loading of bone should be prevented until firm fixation has occured to prevent micromotion • Screws should be countersunk into a bone or plate to minimize stress concentrations at the junction of the head and shaft - Can result in corrosion or failure of the screw • Screws may be removed following fracture healing or left in place - Dependent on surgeon and application Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Screws (3) Benefits: Good fixation Allows for plating Can be removed Less stress shielding (when used alone) than for plates Problems: Soft tissue damage Bony tissue damage Corrosion -- especially crevice corrosion in threads Could produce metal particles on insertion Leaves hole on removal, which can cause stress concentrations Organi Artificiali e Protesi Prof. O. Sbaizero
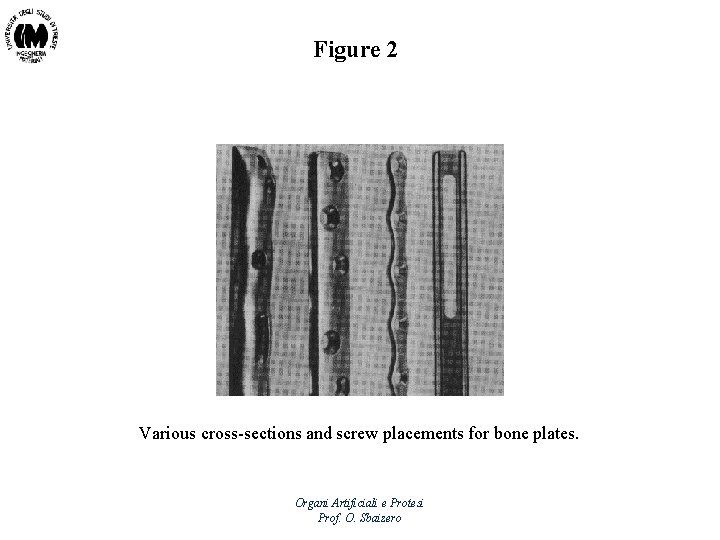
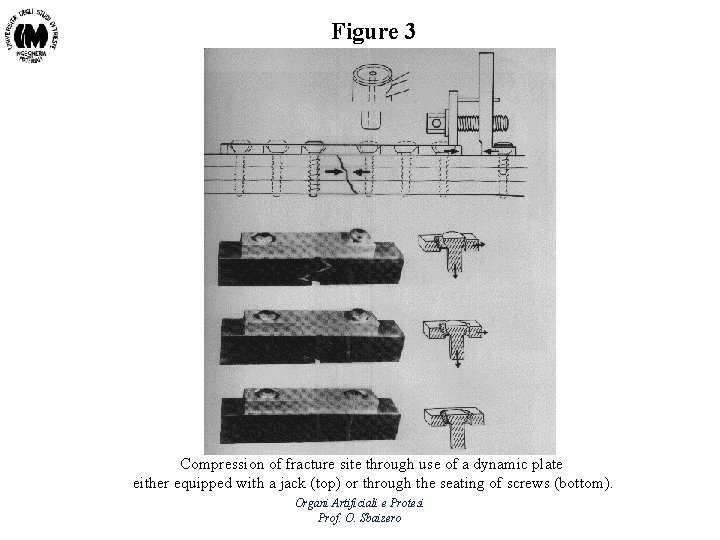
Fracture Fixation - Cortical Bone Plates (1) • Means of internal fixation and direct mechanical stabilization • Allows connection of bone fragments using plates and screws • Many designs with varying screw placement and cross-sectional shape (See Figure 2) - Different designs posess different structural properties, including strength and stiffness • Some plates designed to induce compression of bone segments during fixation (See Figure 3) - May be self-compressing due to seating of screws - Also may involve the use of a "jack" to induce compression before final tightening - Benefit of induced compression is still being debated • Requires more extensive surgery and disruption of periosteum Organi Artificiali e Protesi Prof. O. Sbaizero
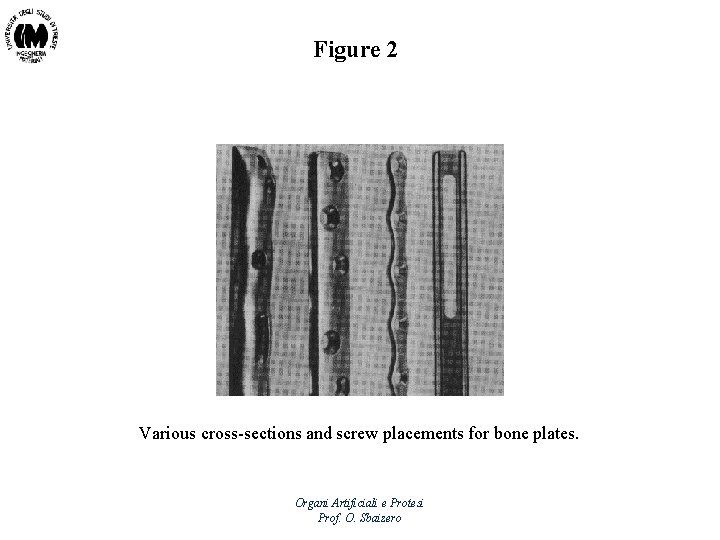
Figure 2 Various cross-sections and screw placements for bone plates. Organi Artificiali e Protesi Prof. O. Sbaizero
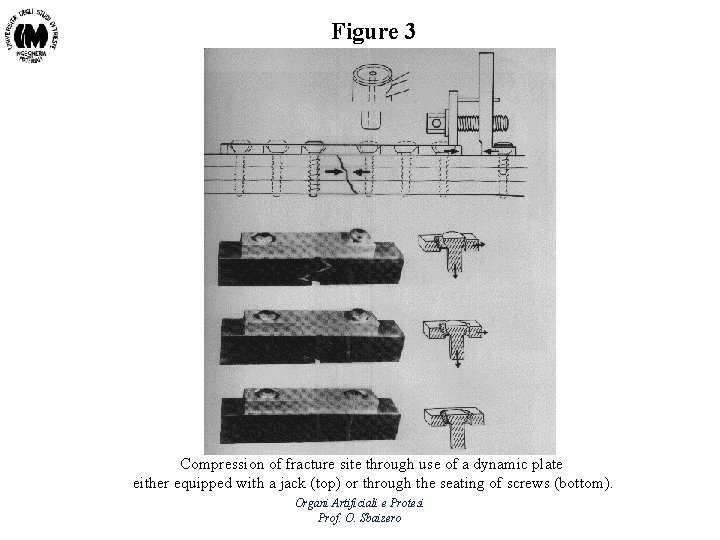
Figure 3 Compression of fracture site through use of a dynamic plate either equipped with a jack (top) or through the seating of screws (bottom). Organi Artificiali e Protesi Prof. O. Sbaizero
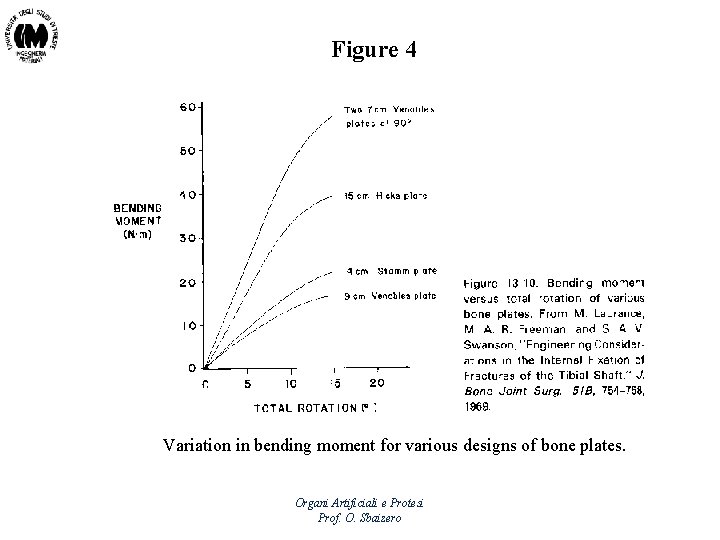
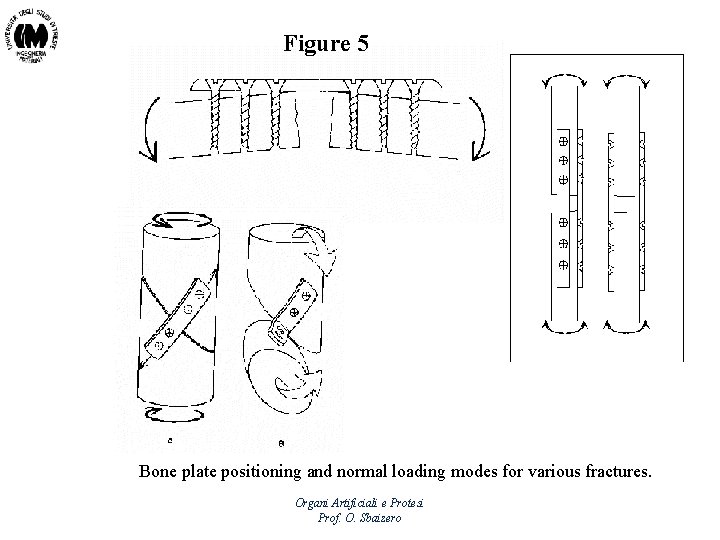
Fracture Fixation - Cortical Bone Plates (2) • Bending moments experienced by bones, due to muscle forces, generally greater than the bending strength of bone plates - Greatest resistible bending moment measured at proximal femur ranges from 25 - 130 N*m - Immobilization required until sufficient healing has occurred to allow the bone to bear a portion of the load - Bending strength can vary significantly based on plate design (See Figure 4) • The effect of screw holes on stress concentrations within the plate must be considered • The placement of a plate on a bone is critical in regards to the load-bearing capabilities of the system (See Figure 5) - Fractured bones can withstand compressive loading but not tensile - Plates should be positioned to provide tensile support to the bone during normal loading conditions • Bone plates are often removed after fracture fixation Organi Artificiali e Protesi Prof. O. Sbaizero
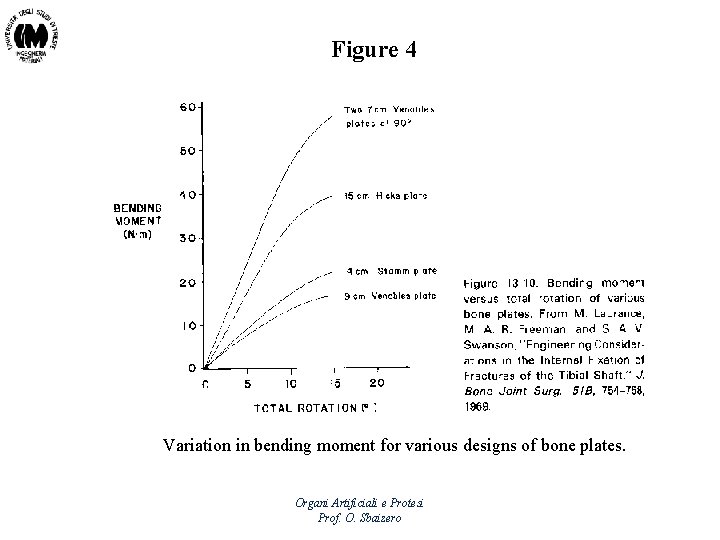
Figure 4 Variation in bending moment for various designs of bone plates. Organi Artificiali e Protesi Prof. O. Sbaizero
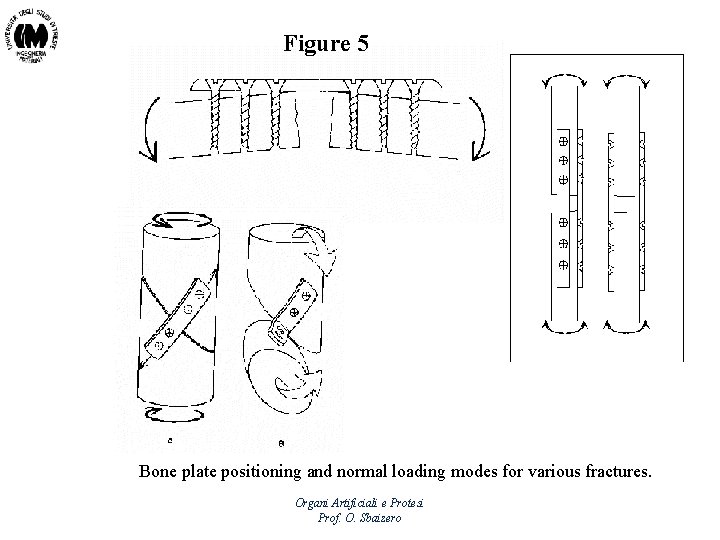
Figure 5 Bone plate positioning and normal loading modes for various fractures. Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Cortical Bone Plates (3) Benefits: Good fixation Provide mechanical support in tension and torsion Can induce compressive loading at fracture site Can be used for multiple fracture fragments Problems: Cause stress shielding (loss of bone under plate) Requires major surgery If they are removed, it results in extra cost, tissue damage, and surgical risks Possibility of corrosion # Especially due to existence of screw and plate Ideas Biodegradable plates Better timing for plate removal Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Maxillofacial Fractures • Variations on plates can also be sued to fix maxillofacial fractures which often involve thinner segments of bone - Titanium mini-plates with non-linear geometries or more flexible meshes can be used (See Figure 6) Organi Artificiali e Protesi Prof. O. Sbaizero
Figure 6 Fixation of an orbital fracture with a titanium mesh. Organi Artificiali e Protesi Prof. O. Sbaizero
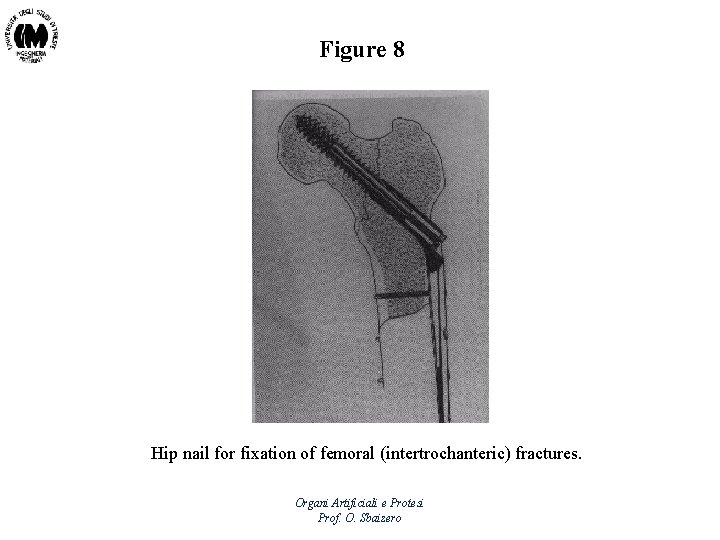
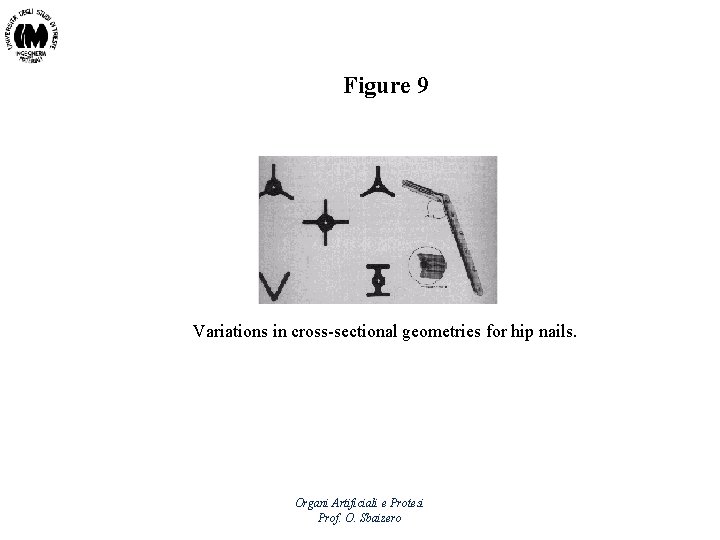
Fracture Fixation - Trabecular Bone (1) • More difficult to provide mechanical stability in fracture locations that are highly trabecular - Because trabecular bone is less dense and less stiff, so it is more difficult to obtain good fixation of an implanted fixation device • Generally fixed with a combination of plates, screws, bolts, and nuts (See Figure 7) - Large amount of material required for fixation • Fixation of trabecular bone with nails alone may be possible if the trabecular bone is sufficiently dense • Fixation of a femoral neck or intertrochanteric (lower) bone fracture may be accomplished with a hip nail - Combined with a plate to provide better stability (See Figure 8) - Cross-sectional shapes of the nail vary, but are designed to prevent rotation of the nail (See Figure 9) - Hip nails generally involve a mechanism to induce compression at the fracture zone by tightening a screw Organi Artificiali e Protesi Prof. O. Sbaizero
Figure 7 Fixation of a metaphysial fracture through a highly cancellous region with a combination of plates, bolts, and screws Organi Artificiali e Protesi Prof. O. Sbaizero
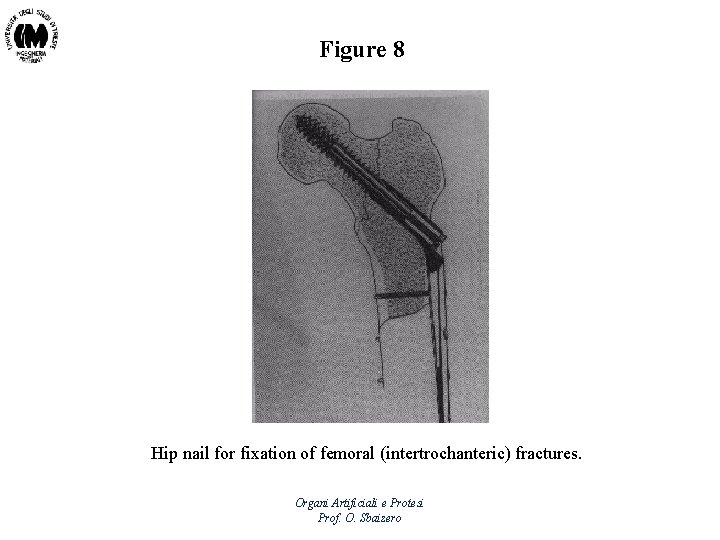
Figure 8 Hip nail for fixation of femoral (intertrochanteric) fractures. Organi Artificiali e Protesi Prof. O. Sbaizero
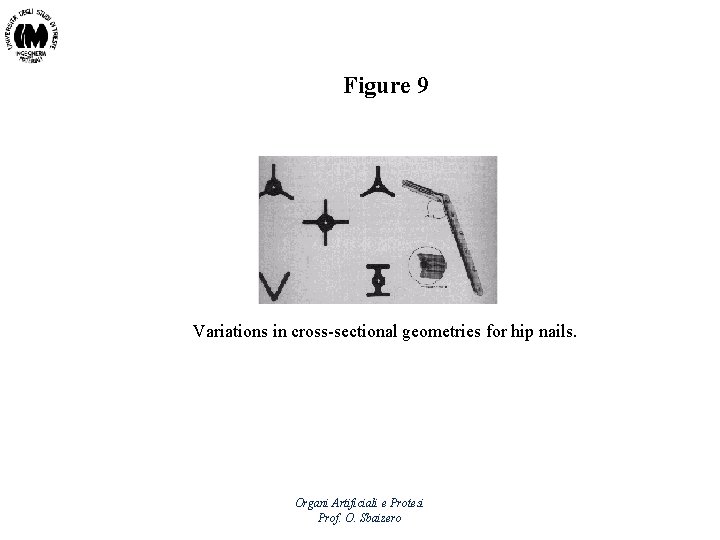
Figure 9 Variations in cross-sectional geometries for hip nails. Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Trabecular Bone (2) Benefits: Able to repair the fracture!! Problems: Tissue damage due to large device Corrosion due to multiple metallic parts and large amount of metal Major surgery is required Damages bone on removal Organi Artificiali e Protesi Prof. O. Sbaizero
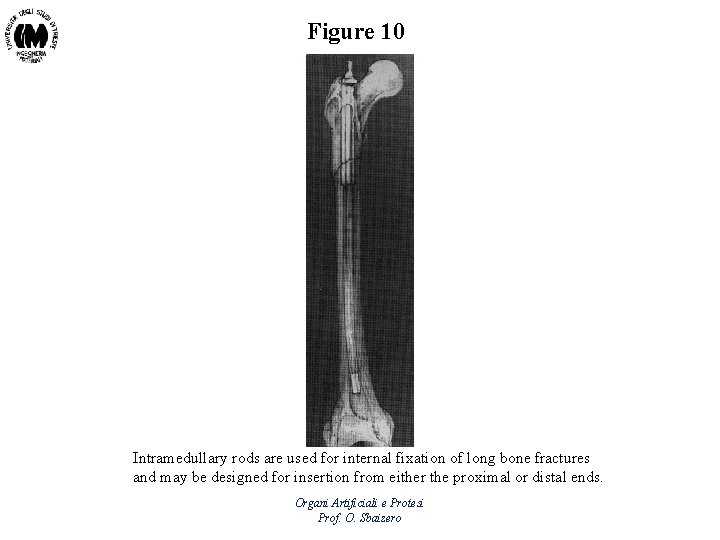
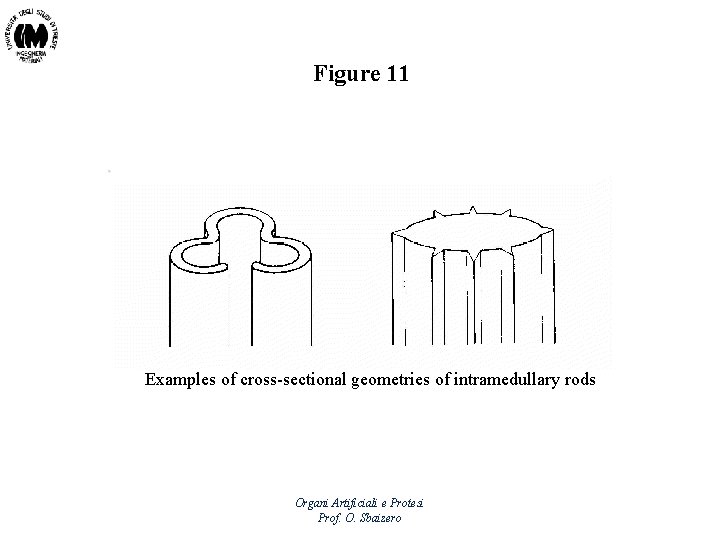
Fracture Fixation - Intramedullary Devices (1) • Used for fractures of long bones (introduced in 1940) • Inserted into the medullary canal (See Figure 10) - Should fit snugly and have some elastic recoil to prevent rotation and slippage • More resistant to bending than cortical bone plates, but more susceptible to torsional loading • May destroy intramedullary blood supply, but does not affect periosteal supply • Can be inserted through a small incision near the proximal or distal end of the bone - Can be locked with screws at distal and proximal end of bone - Induces axial alignment • Device designs vary predominantly in their cross-sectional shape (See Figure 11) - Clover-leaf, diamond, cross - Shapes have varying resistances to bending an d torsion for a given length and "diameter" - All stiffnesses less than that of the bone itself Organi Artificiali e Protesi Prof. O. Sbaizero
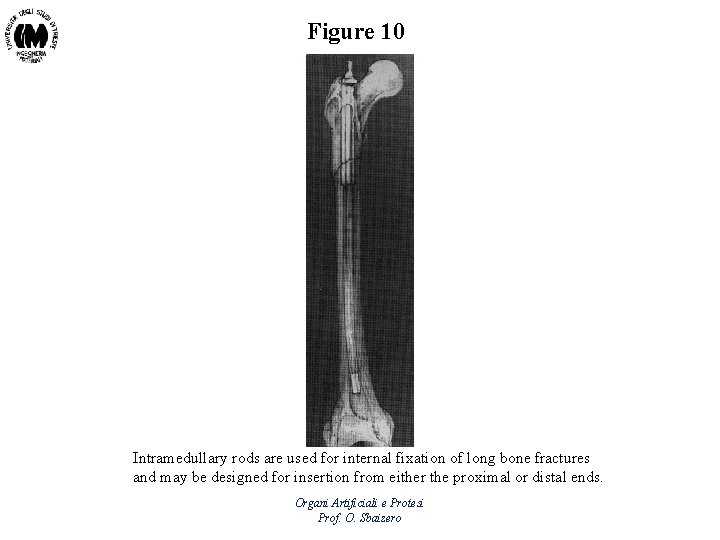
Figure 10 Intramedullary rods are used for internal fixation of long bone fractures and may be designed for insertion from either the proximal or distal ends. Organi Artificiali e Protesi Prof. O. Sbaizero
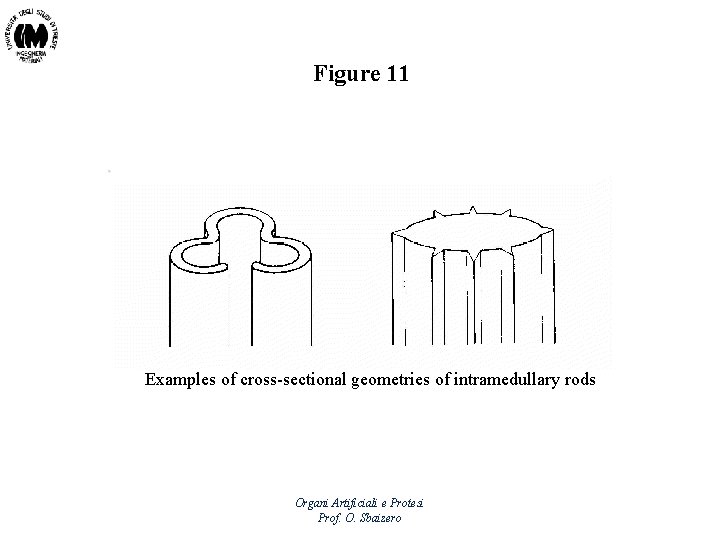
Figure 11 Examples of cross-sectional geometries of intramedullary rods Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Intramedullary Devices (2) Benefits: Provides good fixation and stabilization Requires only a small incision Allows early protected weight bearing due to location of neutral axis along axis of bone # better than plates where early weight bearing without partial union may cause failure of plate Problems: Damage to intramedullary blood supply Large metal piece is subject to corrosion Can cause stress shielding Removal is difficult Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Artificial Bone Mineral (1) New, experimental technique published in Science in 1995 • Mixture of mono- and tri-calcium phosphates, calcium carbonate, and sodium phosphate • Can be injected into fracture sites to provide some mechanical stabilization - Bone fragments or segments can be held in place to allow for traditional casting - Reduces or eliminates necessity of using implanted fixation devices - Especially good for trabecular fractures - Is gradually resorbed and replaced with healthy tissue • Mineral paste hardens to provide initial fixation in 10 minutes - Compressive strength approximately 10 MPa • Within 12 hours, mineral is fully cured - Compressive strength 55 MPa - Tensile strength 2. 1 MPa • Also good for filling bony defects resulting from surgery, implant revision, implant removal (ie. screws), etc. Organi Artificiali e Protesi Prof. O. Sbaizero
Fracture Fixation - Artificial Bone Mineral (2) Benefits: - Removal is not required - Provides quick fixation - Minimizes stress shielding - Is resorbed - Does not corrode - No tissue damage Problems: - Long term effects unknown - Short surgery time due to quick setting time allows no mistakes Organi Artificiali e Protesi Prof. O. Sbaizero
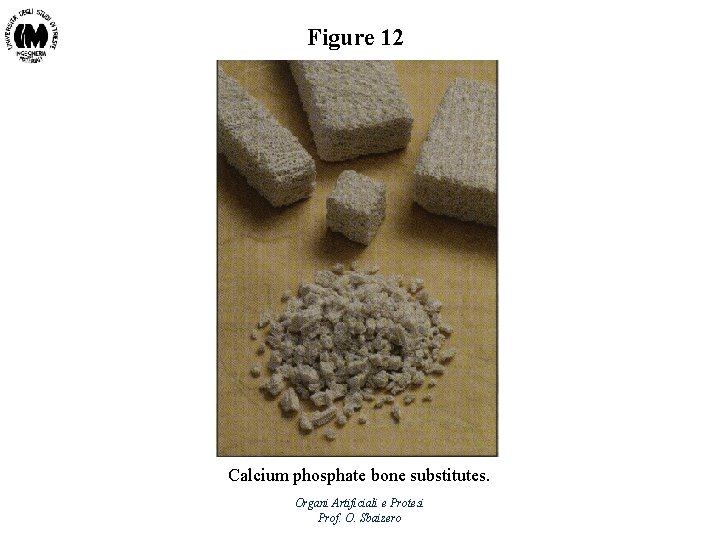
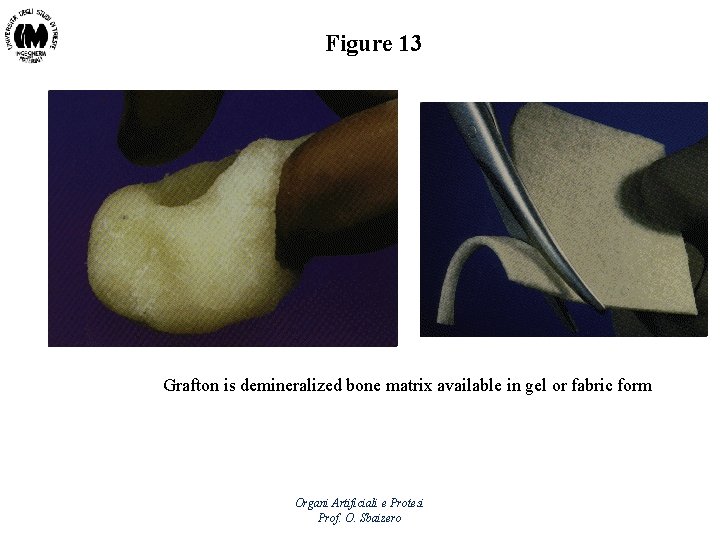
Bone Grafts and Supplementation • Used to fill gaps in native bone due to surgery or injury • Can be chips of trabecular bone or segments/strips of cortical bone (See Figure 12) • A new material known as Grafton is demineralized bone matrix, either in gel or fabric form - Gel can be used to fill in the gaps that exist when using bone chips (See Figure 13) # Forms continuous interface between composite graft and host bone - Fabric can be applied in non-load bearing situations to act as inductive surface Organi Artificiali e Protesi Prof. O. Sbaizero
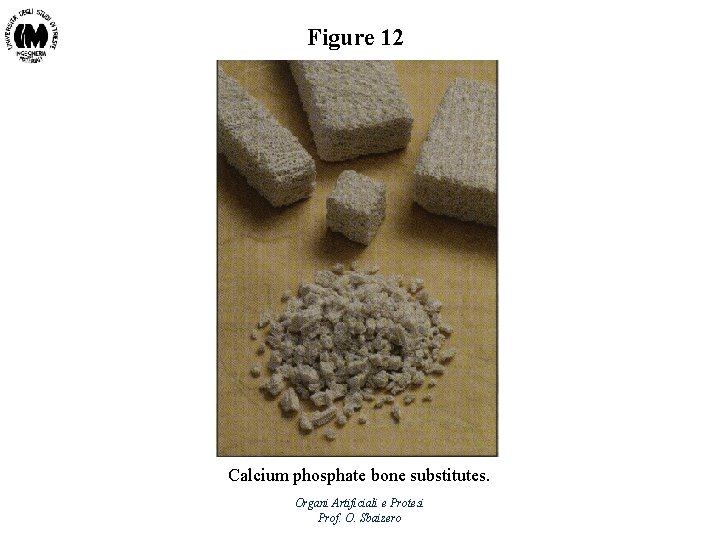
Figure 12 Calcium phosphate bone substitutes. Organi Artificiali e Protesi Prof. O. Sbaizero
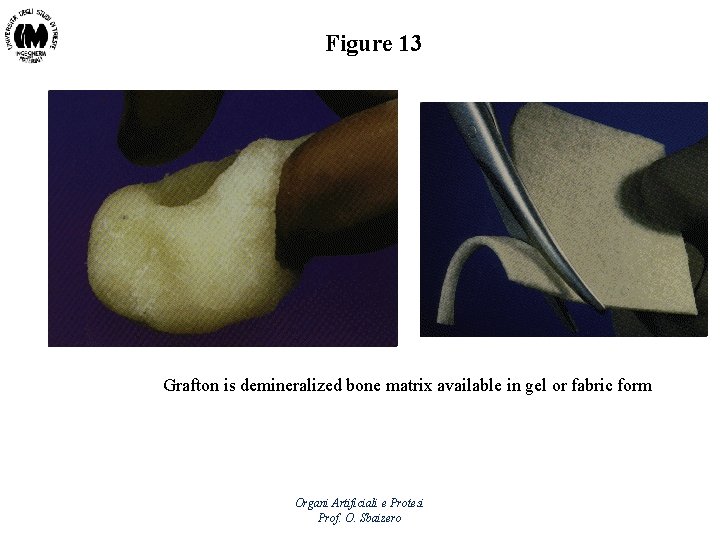
Figure 13 Grafton is demineralized bone matrix available in gel or fabric form Organi Artificiali e Protesi Prof. O. Sbaizero