Fortification of breast milk Why When With What
Fortification of breast milk, Why? When? With What? KEITH J BA RRINGTO N CHU STE JUS TINE MO NTRÉAL
Conflict of Interest I have no relevant financial relationships to disclose or conflicts of interest to resolve. I will not discuss any unapproved or off‐label, experimental or investigational use of a product, drug or device.
Breast is best, but it’s not good enough The mixed message that we give to parents (mothers) Advantages of breast milk, are they proven in the preterm? Advantages of maternal breast mik, are they certain? Nutritional requirements to achieve good growth (what is that? ) Achieving those requirements
“Breast is best, but it’s not good enough” The mixed message that we give to parents (mothers), try to avoid that implication Advantages of breast milk, are they proven in the preterm? ◦ Clearly, yes Advantages of maternal breast mik, are they certain? ◦ As certain as we can be Nutritional requirements to achieve good growth (what is that? ) ◦ Good growth is not just getting heavier, but getting longer, growing the brain, and without toxicity Achieving those requirements ◦ How to do so with maternal milk as the priority
Nutritional requirements of the preterm infant, enteral Energy : At least 120 kcal/kg/d Protein : 4 (‐ 4. 5) g/kg/d Calcium : 120 (‐ 140) mg/kg/d Phosphorus : 60 (‐ 90) mg/kg/d
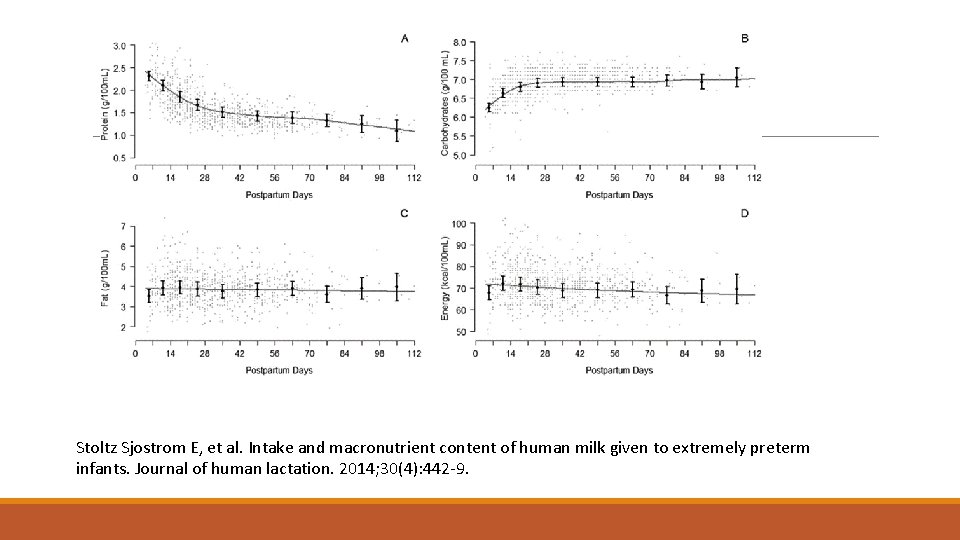
Stoltz Sjostrom E, et al. Intake and macronutrient content of human milk given to extremely preterm infants. Journal of human lactation. 2014; 30(4): 442‐ 9.
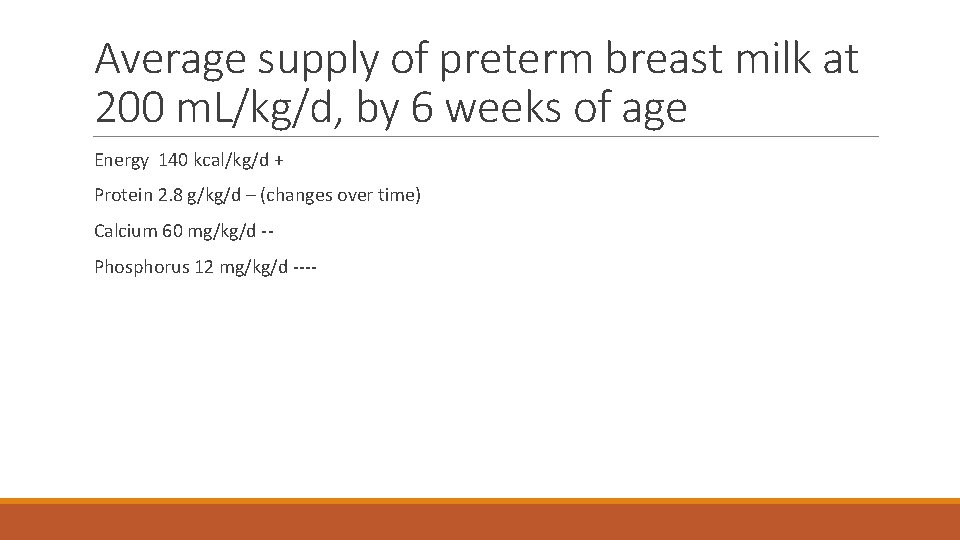
Average supply of preterm breast milk at 200 m. L/kg/d, by 6 weeks of age Energy 140 kcal/kg/d + Protein 2. 8 g/kg/d – (changes over time) Calcium 60 mg/kg/d ‐‐ Phosphorus 12 mg/kg/d ‐‐‐‐
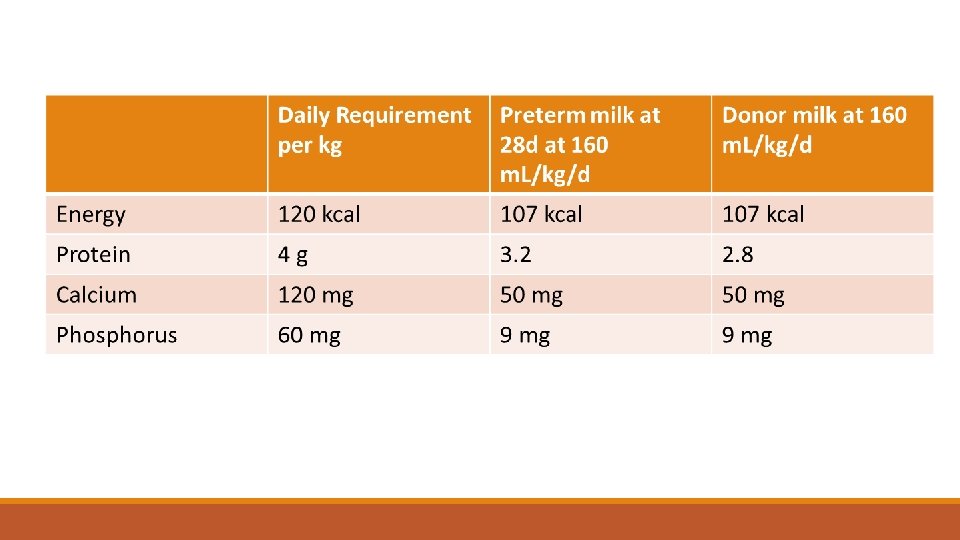
Achieving recommended intakes Without fortifier: Possible for calories Possible for protein in the first week if baby tolerating full feeds at high volumes Deficient for calcium, Grossly deficient for phosphorus
What growth should we be aiming for? Tradition‐ Intra‐uterine growth curves with good bone mineralization Newer‐ Aim for weight, length, and head circumference at 44 weeks that the infant would have had if remained in utero with a well functioning placenta Landau‐Crangle E, et al. Individualized Postnatal Growth Trajectories for Preterm Infants. JPEN Journal of parenteral and enteral nutrition. 2018; 42(6): 1084‐ 92.
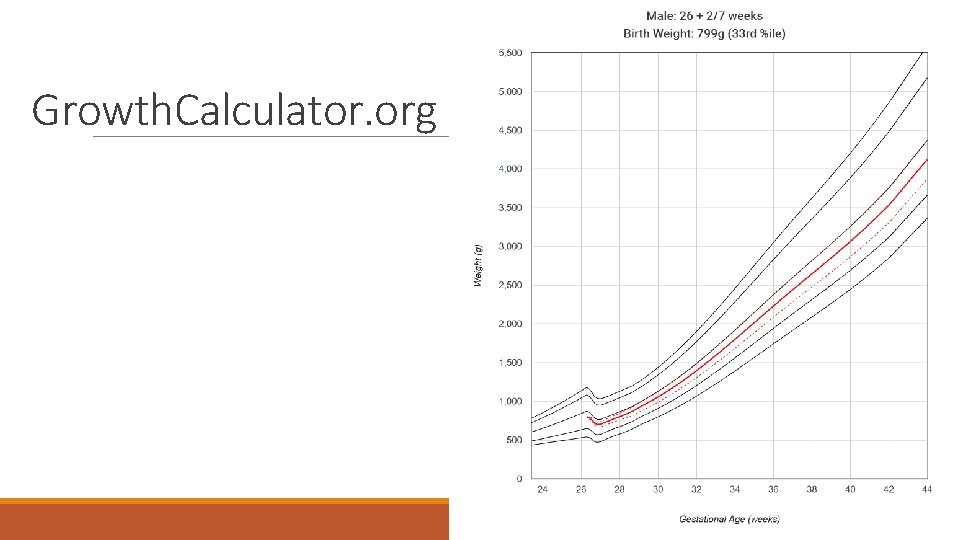
Growth. Calculator. org

Adding fortifiers All derived from cows’ milk until recently Not identical Powders/Liquids Different sources of calories and protein concentrations Differing p. H and other details of composition
What is the evidence about efficacy and safety? Randomized trials of fortification vs no fortification with Bovine Protein Fortifiers ◦ Not isoenergetic/isoproteinic ◦ Not blinded Growth better (weight and head circumference) No evidence of adverse impacts, specifically no evidence of increase in NEC or other GI complications ◦ Confidence intervals relatively wide
Systematic reviews Comparing no fortifier to a multicomponent fortifier Cochrane review ◦ Only powdered fortifiers studied ◦ Most studies pre 2000 ◦ Most studies very small
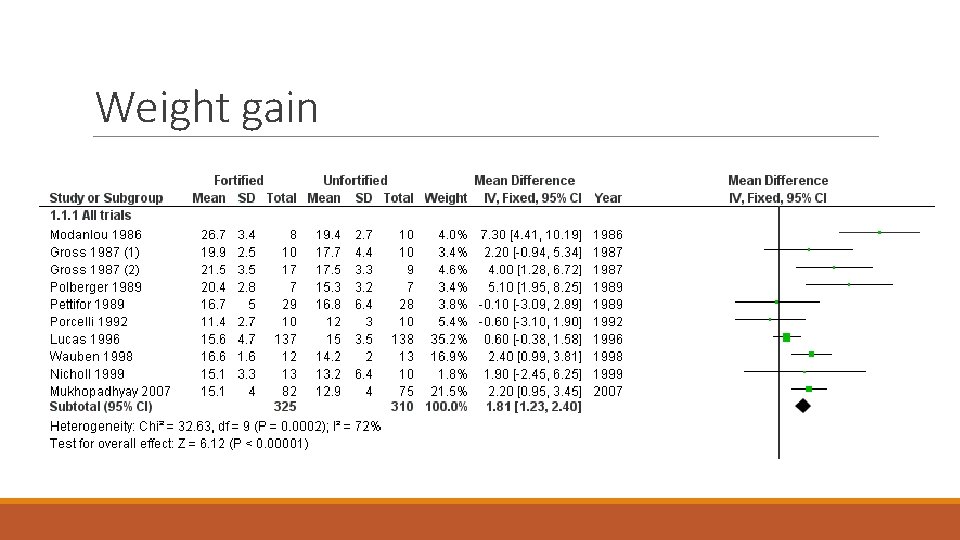
Weight gain
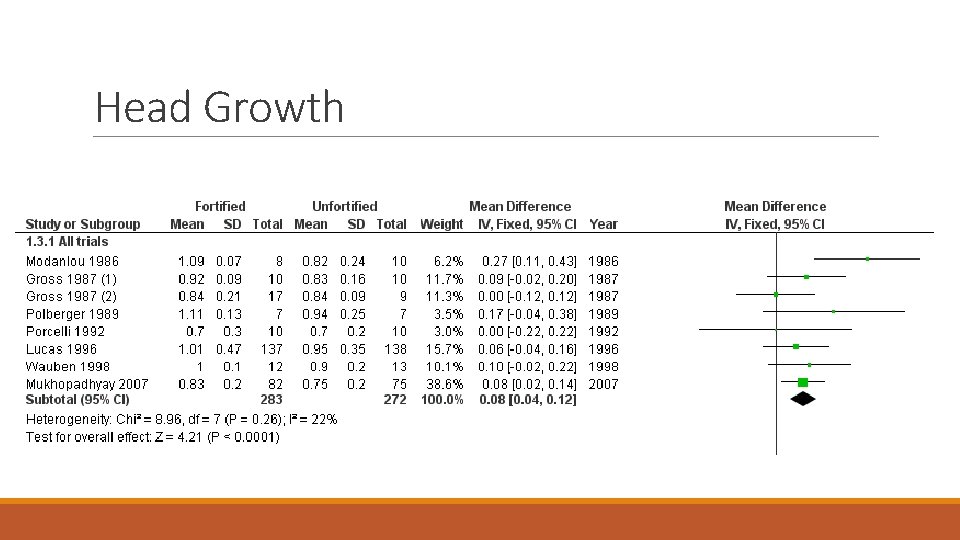
Head Growth
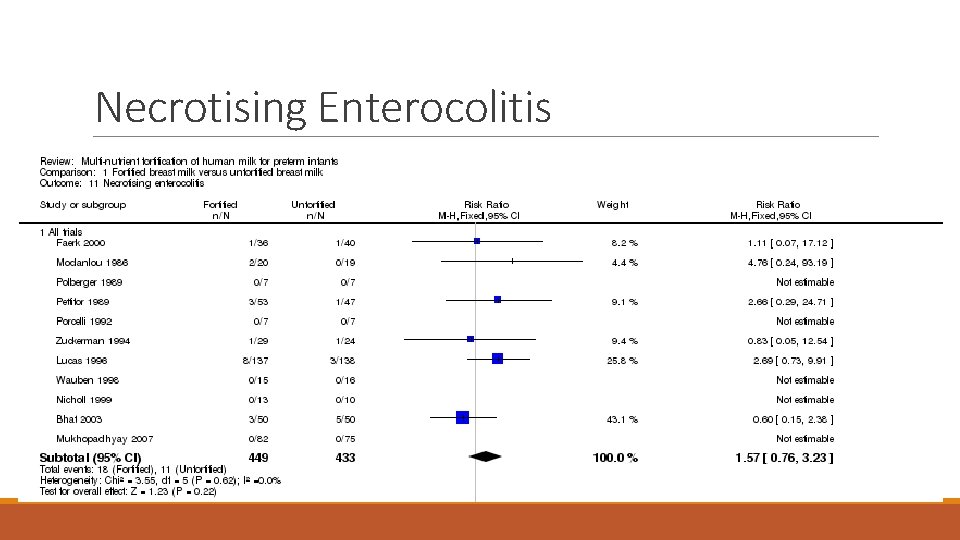
Necrotising Enterocolitis
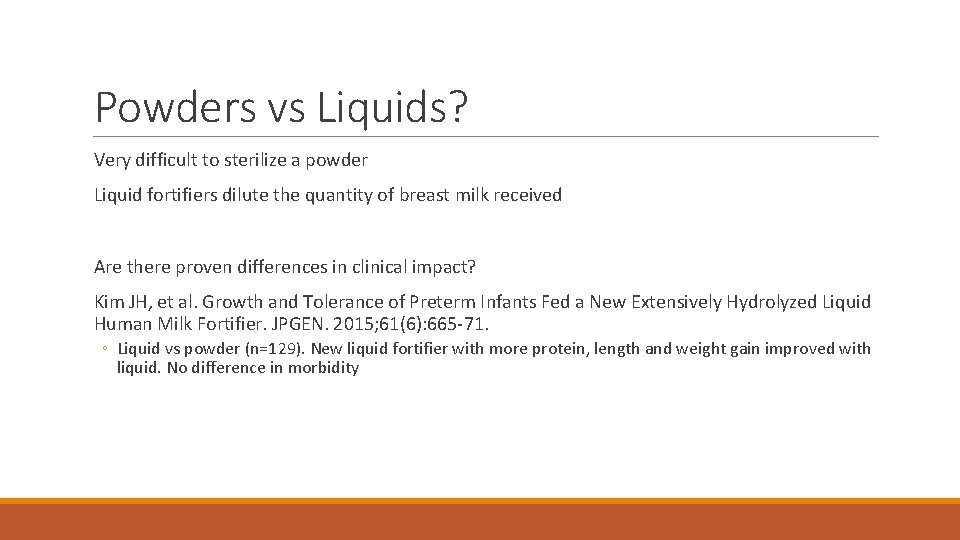
Powders vs Liquids? Very difficult to sterilize a powder Liquid fortifiers dilute the quantity of breast milk received Are there proven differences in clinical impact? Kim JH, et al. Growth and Tolerance of Preterm Infants Fed a New Extensively Hydrolyzed Liquid Human Milk Fortifier. JPGEN. 2015; 61(6): 665‐ 71. ◦ Liquid vs powder (n=129). New liquid fortifier with more protein, length and weight gain improved with liquid. No difference in morbidity
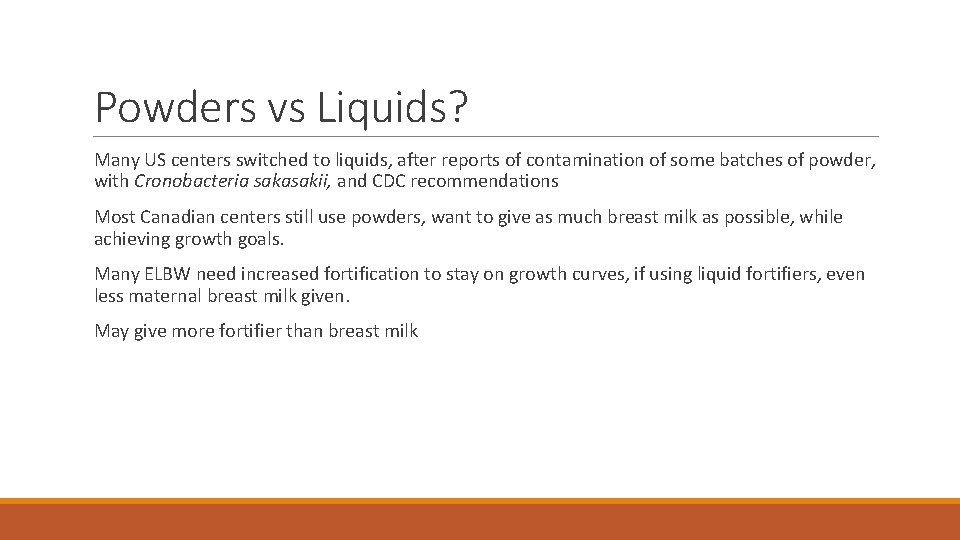
Powders vs Liquids? Many US centers switched to liquids, after reports of contamination of some batches of powder, with Cronobacteria sakasakii, and CDC recommendations Most Canadian centers still use powders, want to give as much breast milk as possible, while achieving growth goals. Many ELBW need increased fortification to stay on growth curves, if using liquid fortifiers, even less maternal breast milk given. May give more fortifier than breast milk
Human vs Bovine (or Donkey) Human milk (fortified) as a supplement for insufficient maternal supply compared to artifical formula Human based fortifier added to mother’s milk compared to bovine based fortifier Human based fortifier added to donor milk compared to bovine based fortifier ◦ Bertino E, et al. A Novel Donkey Milk‐derived Human Milk Fortifier in Feeding Preterm Infants: A Randomized Controlled Trial. Journal of pediatric gastroenterology and nutrition. 2019; 68(1): 116‐ 23.
Human milk as a supplement cf Formula Moderately good evidence supplementation with fortified human donor milk rather than formula leads to ◦ lower weight gain, ◦ lower longitudinal growth, ◦ less gain in head circumference Incidence of Necrotising Enterocolitis Decreased by donor BF ◦ Relative risk with formula 1. 9 (95% CI : 1. 23, 2. 85) ◦ Quigley M, et al. Formula versus donor breast milk for feeding preterm or low birth weight infants. Cochrane database of systematic reviews (Online). 2018; 6: CD 002971. Little evidence of impact on sepsis
More recent data Trang S, et al. Cost‐Effectiveness of Supplemental Donor Milk Versus Formula for Very Low Birth Weight Infants. Pediatrics. 2018; 141(3). Randomized 363 VLBW, mothers intending to breast feed, supplements with either donor BM or formula, all BM fortified with bovine protein based fortifier (powder) NEC (grade ≥ 1) 11% with formula supplements, 4% with donor BM NEC (grade ≥ 2) 6. 6% vs 1. 7% (n=12 vs 2)
“Exclusive Human Milk Diet” Cristofalo EA, et al. Randomized Trial of Exclusive Human Milk versus Preterm Formula Diets in Extremely Premature Infants. The Journal of pediatrics. 2013. Donor BM with human‐milk‐based fortifier was compared to preterm formula. Small study (n=53) very high frequency of NEC with formula (21%, n=5), lower frequency with donor BM (3%, n=1). Sullivan S, et al. An Exclusively Human Milk‐Based Diet Is Associated with a Lower Rate of Necrotizing Enterocolitis than a Diet of Human Milk and Bovine Milk‐Based Products. The Journal of pediatrics. 2010; 156(4): 562‐ 7. e 1. 3 group trial (n=207) Maternal BM (supplements of donor BM as required) and fortification with human‐milk‐based fortifier starting at 40 m. L/kg/d, or at 100 m. L/kg/d. 3 rd group : maternal BM (supplements of artificial formula as required) BM fortified with bovine fortifier introduced at 100 m. L/kg/d. Higher frequency of NEC in the formula supplements/bovine fortifier group, who received on average 20% of their milk as artificial formula.
The advantages of the “Exclusive Human Milk Diet” have been suggested only in comparison to 1. Preterm formula 2. Supplementing maternal BM with formula (and fortifying with bovine protein based fortifier) What about supplementing maternal BM with donor BM, and fortifying both with bovine based fortifier? ◦ Commonest recipe in Canada
Human milk fortifier (or bovine) to fortify maternal breast milk O'Connor DL, et al. Nutrient enrichment of human milk with human and bovine milk‐based fortifiers for infants born weighing <1250 g: a randomized clinical trial. Am J Clin Nutr. 2018; 108(1): 108‐ 16. Randomized 127 VLBW infants All received maternal BM, when insufficient, donor BM Compared human milk based fortifier to bovine based fortifier (powder containing non‐ hydrolyzed bovine proteins) No differences in feeding tolerance, or NEC (3 per group : stage 2)
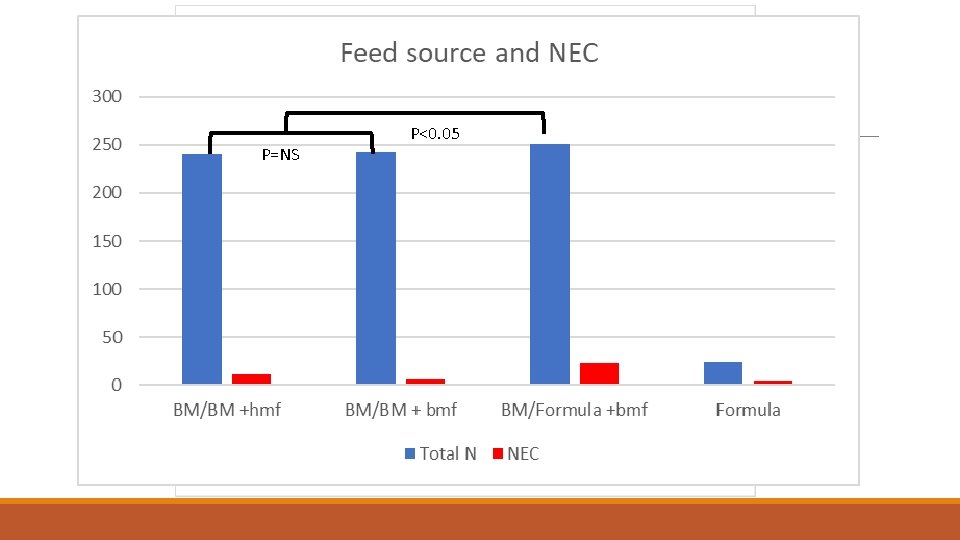
P=NS P<0. 05
Individualized fortification? Breast milk is very variable, and growth can be affected by variations in calorie and protein content Individualized fortification is an attractive option BUT : Breast milk varies within mothers, by day, by time, between foremilk and hindmilk Effective individualized fortification‐labour intensive
Individualized fortification? Trials of routine individualized fortification have shown little impact ◦ Mc. Leod G, et al. Comparing different methods of human breast milk fortification: a randomised controlled trial. Br J Nutr. 2016; 115(3): 431‐ 9. ◦ Only 40 babies included, no impact on growth. Required 1870 analyses. ◦ Arslanoglu S, et al. Adjustable fortification of human milk fed to preterm infants: does it make a difference? J Perinatol. 2006; 26(10): 614‐ 21. ◦ Only 32 babies included, individualized group grew better, received more protein Most preterms grow well with routine fortification, and routine increases in fortifier in case of problems ◦ E. G. start with ‘ 24 calorie’ for maternal BM, or ‘ 26 calorie’ for donor BM. Concentrate on nutrition each day, increase fortification if any growth faltering Trials of individualized fortification only including babies with growth problems not available.
Fortification of donor milk Higher protein content of preterm delivered mothers’ milk ‐ many centers routinely start fortification of donor milk with higher concentrations of fortifier We start with 6 sachets per 100 m. L for donor milk ◦ compared to 4 sachets per 100 m. L for maternal milk. We call this “donor milk at 26 kcal, and maternal milk at 24 kcal”
When to start? Many centers start fortification after substantial enteral feeding tolerance achieved, or at full feeds Some start earlier, we start at 25 m. L total per day ◦ 3 observational studies, no adverse impacts Prospective controlled data? 2 small trials, larger n=100, RCT of fortification starting at 20 m. L/kg/d or 100 m. L/kg/d. ◦ Shah SD, et al. Early versus Delayed Human Milk Fortification in Very Low Birth Weight Infants‐A Randomized Controlled Trial. The Journal of pediatrics. 2016; 174: 126‐ 31 e 1. No adverse effects, better nutrition with earlier fortification
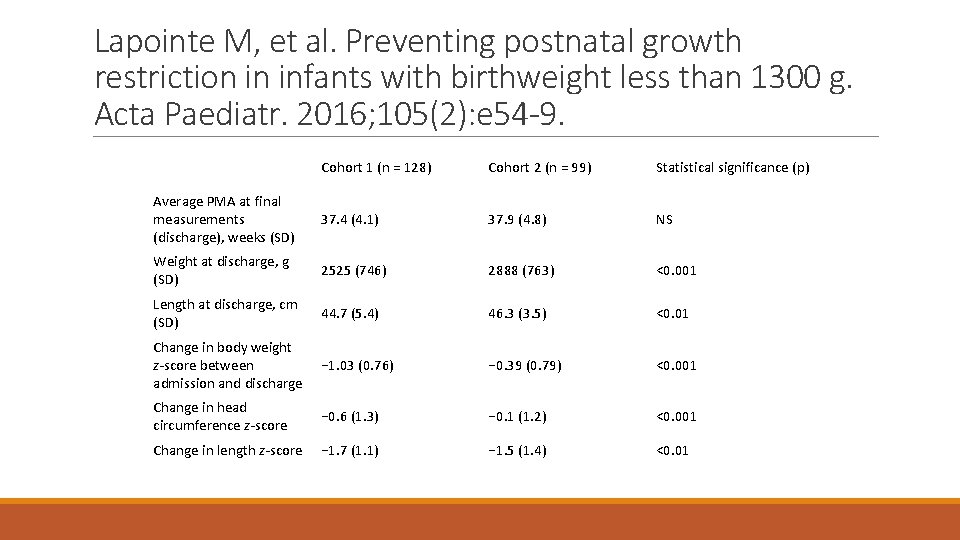
Lapointe M, et al. Preventing postnatal growth restriction in infants with birthweight less than 1300 g. Acta Paediatr. 2016; 105(2): e 54 -9. Cohort 1 (n = 128) Cohort 2 (n = 99) Statistical significance (p) Average PMA at final measurements (discharge), weeks (SD) 37. 4 (4. 1) 37. 9 (4. 8) NS Weight at discharge, g (SD) 2525 (746) 2888 (763) <0. 001 Length at discharge, cm (SD) 44. 7 (5. 4) 46. 3 (3. 5) <0. 01 Change in body weight − 1. 03 (0. 76) z‐score between admission and discharge − 0. 39 (0. 79) <0. 001 Change in head circumference z‐score − 0. 6 (1. 3) − 0. 1 (1. 2) <0. 001 Change in length z‐score − 1. 7 (1. 1) − 1. 5 (1. 4) <0. 01
When to start? Transitioning from TPN to enteral feeds, Low calorie, protein, and mineral density of EBM can initially be addressed by adjusting intravenous intakes. As feeds progress : progressively more difficult/impossible

Summary of the data Among very preterm or very low birth weight infants : Growth and bone mineralization approaching desired standards can only be achieved by fortifying BM Commercial bovine or human multicomponent fortifers have become the standard of care Desired growth can be achieved with maternal BM and fortification, or donor BM and fortification, if enough attention paid to growth Donor BM has less protein (and sligtly fewer calories) than preterm maternal BM, for a few weeks, and requires higher supplementation
Summary of Data Supplementing insufficient maternal BM with formula increases NEC compared to donor BM (Older and recent studies, moderate to good quality data) Multicomponent fortification not shown to affect NEC compared to no fortification (poor to moderate quality data, wide confidence intervals) Multicomponent fortification from different sources not shown to have impact on NEC, (moderate quality data, wide confidence intervals)
Summary of Data Individualized fortification using BM analysis not shown to improve clinically important outcomes compared to adjustment according to growth (poor quality data, small studies, wide confidence intervals) Early introduction of fortifiers not shown to adversely impact clinical outcomes or complications compared to >100 m. L/kg/d (poor quality data)
Evidence based fortification protocol For infants at risk of NEC: Promote maternal breast milk as much as possible, early expression, lactation consultants, pumps freely available everywhere… When MBM insufficient, always use donor BM, until risk of NEC passed (34 weeks? ) Fortify as soon as TPN can not meet requirements of the infant (± 50 m. L/kg/d) Standard fortification at higher dose for donor BM ◦ Use powder or liquid fortifier ◦ Use bovine or human‐based fortifier Increase fortification if growth < target for 2 wk, at ≥ 160 m. L/kg/d re‐assess frequently
- Slides: 37