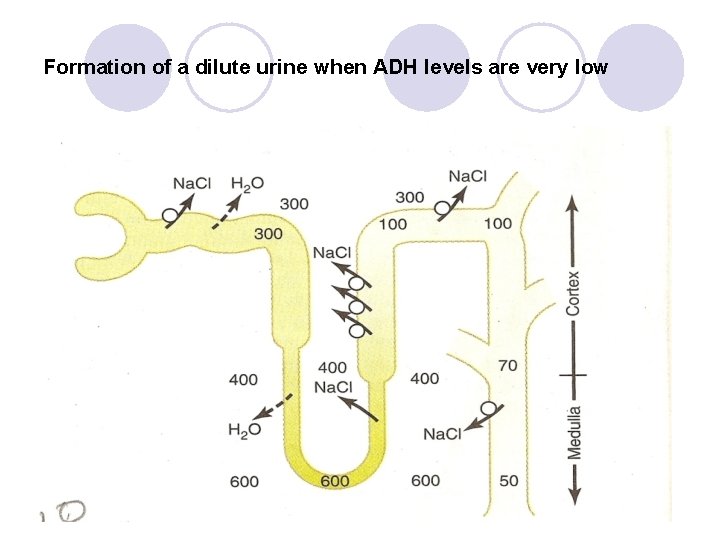
Formation of a dilute urine when ADH levels
- Slides: 24
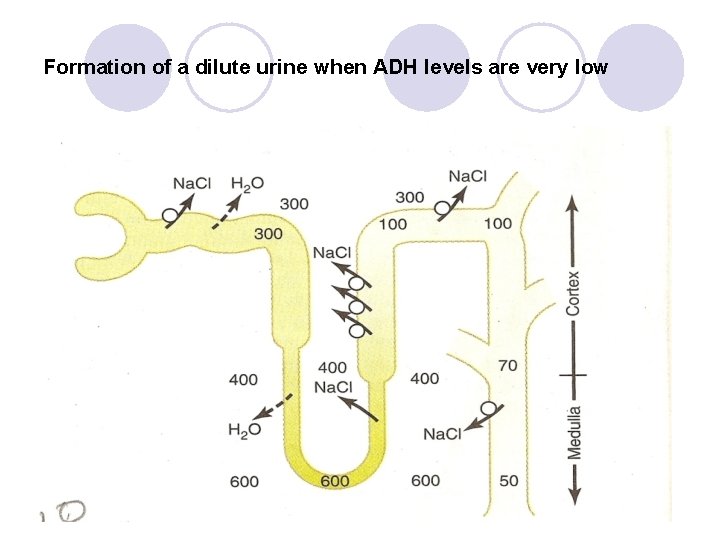
Formation of a dilute urine when ADH levels are very low
Countercurrent mechanism • Prof Rajesh Chandra Sharma
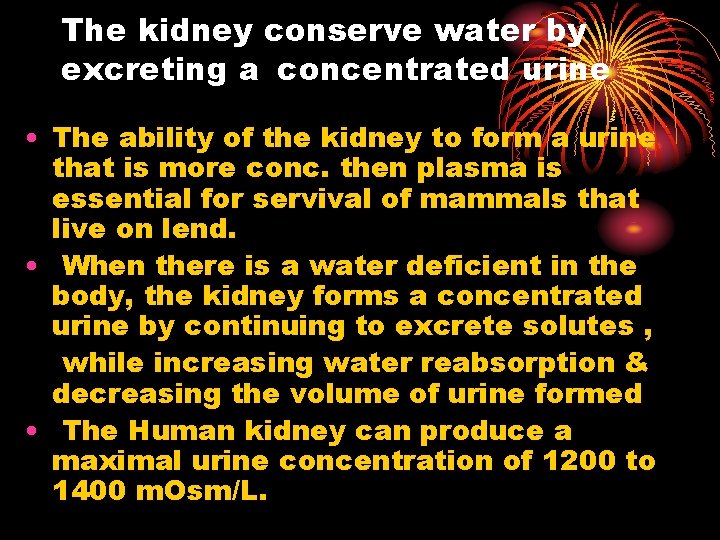
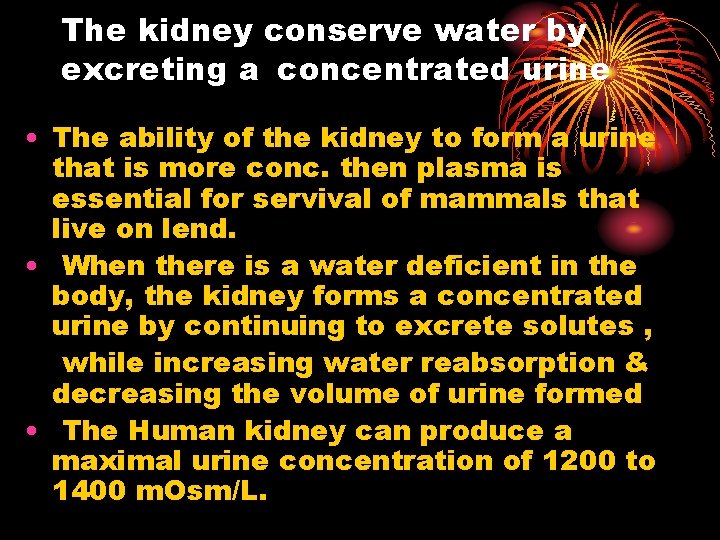
The kidney conserve water by excreting a concentrated urine • The ability of the kidney to form a urine that is more conc. then plasma is essential for servival of mammals that live on lend. • When there is a water deficient in the body, the kidney forms a concentrated urine by continuing to excrete solutes , while increasing water reabsorption & decreasing the volume of urine formed • The Human kidney can produce a maximal urine concentration of 1200 to 1400 m. Osm/L.
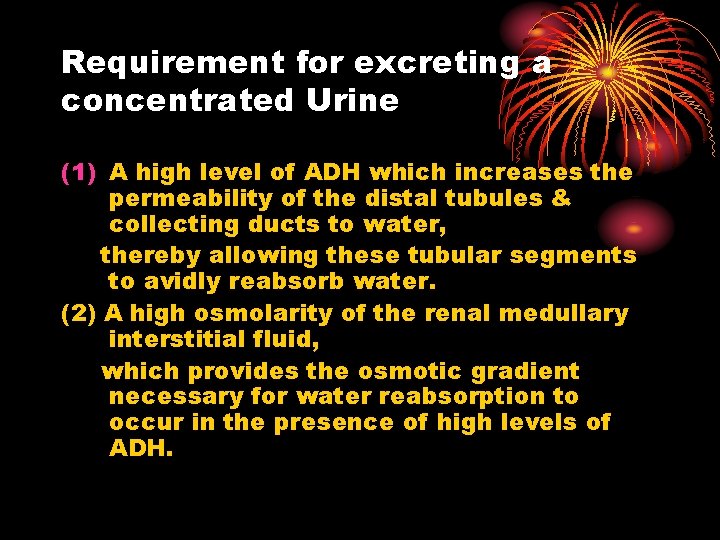
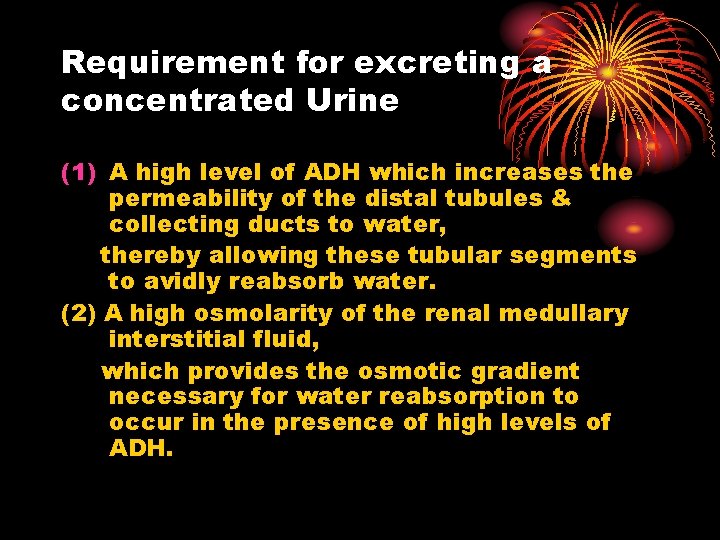
Requirement for excreting a concentrated Urine (1) A high level of ADH which increases the permeability of the distal tubules & collecting ducts to water, thereby allowing these tubular segments to avidly reabsorb water. (2) A high osmolarity of the renal medullary interstitial fluid, which provides the osmotic gradient necessary for water reabsorption to occur in the presence of high levels of ADH.
COUNTER CURRENT MECHANISM • Counter current multiplier mechanism is in • • the loop of Henle. Purpose : - To create a very high osmotic pressure of the medullary interstitial fluid. Depends on typical anatomical arrangement of loop of Henle. normal osmolarity of fluid entering the loop is 300 m. Osm/L. In medullary interstitial fluid – 1200 to 1400 m. Osm/L.
COUNTER CURRENT MECHANISM • The major factors that contribute to the build up of solutes concentration into the renal medulla are: 1) Active transport of sodium & co-transport of potassium , chloride & other ions out of the thick ascending limb into the medullary interstitium. 2) Active transport of ions from collecting ducts into the medullary interstitium. 3) Facilitated diffusion of urea from inner collecting ducts into the medullary interstitium. 4) Diffusion of small amount of water from medullary tubule into the medullary interstitium.
COUNTER CURRENT MECHANISM • Special characteristics of loop of Henle that cause solutes to be trapped in the renal medulla. Ascending limb : Active transport of sodium ions of thick portion of ascending limb. ` • Co-transport of potassium, chloride & other ions. • This movement of salt is not accompanied by water reabsorption so conc. of salt in the ascending limb decreases but conc. In modullary interstitial fluid rises. Descending limb : Is very permeable to water & the tubular fluid osmolarity become equal to the renal medullary osmolarity. • So, water diffuses out of the limb into interstitium & the tubular fluid osmolarity rises as it flow toward the tip of the loop of henle.
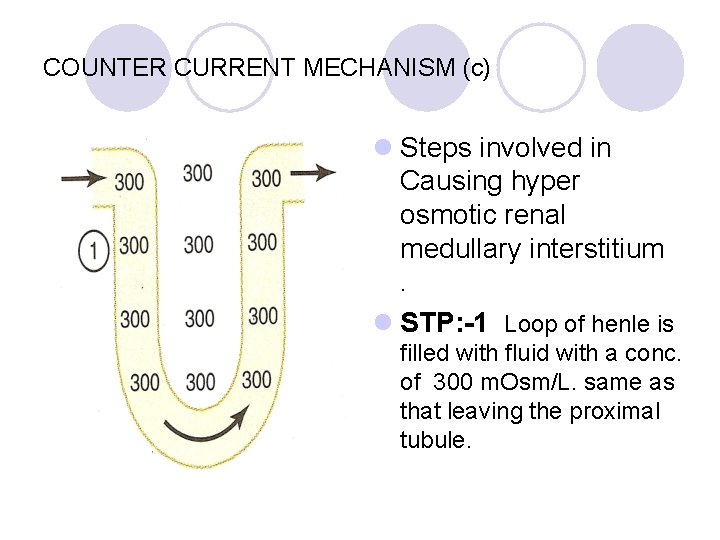
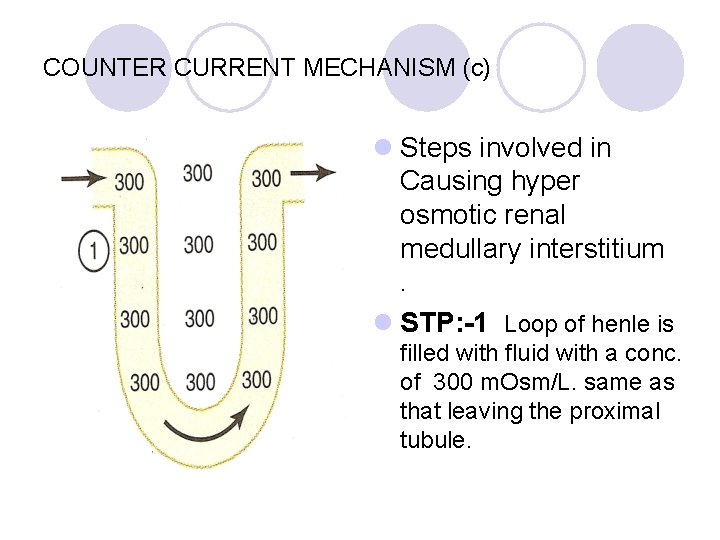
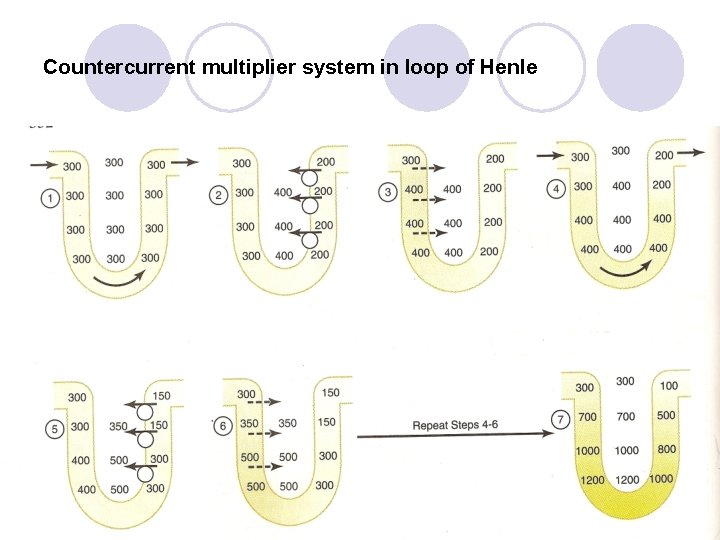
COUNTER CURRENT MECHANISM (c) l Steps involved in Causing hyper osmotic renal medullary interstitium. l STP: -1 Loop of henle is filled with fluid with a conc. of 300 m. Osm/L. same as that leaving the proximal tubule.
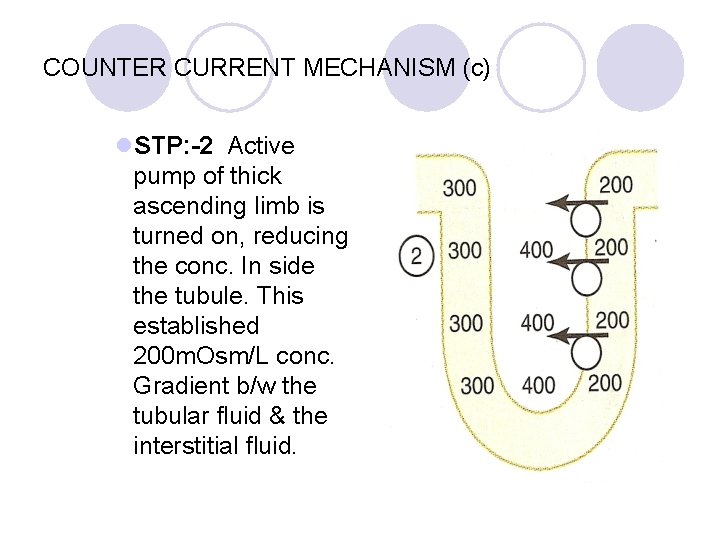
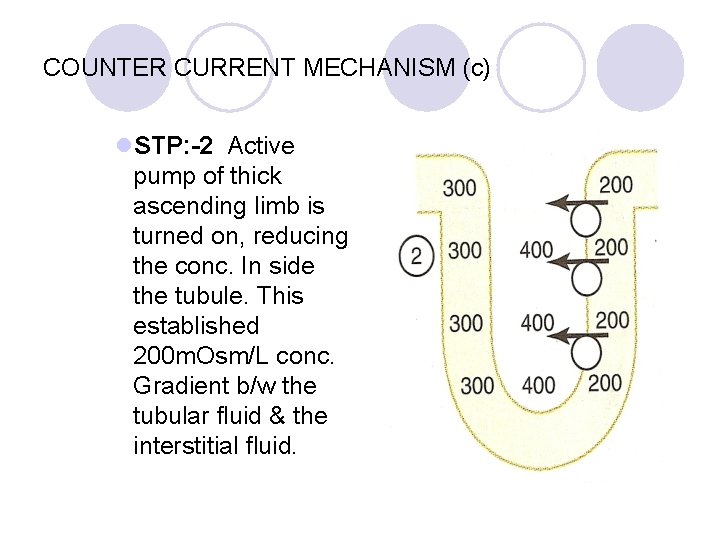
COUNTER CURRENT MECHANISM (c) l. STP: -2 Active pump of thick ascending limb is turned on, reducing the conc. In side the tubule. This established 200 m. Osm/L conc. Gradient b/w the tubular fluid & the interstitial fluid.
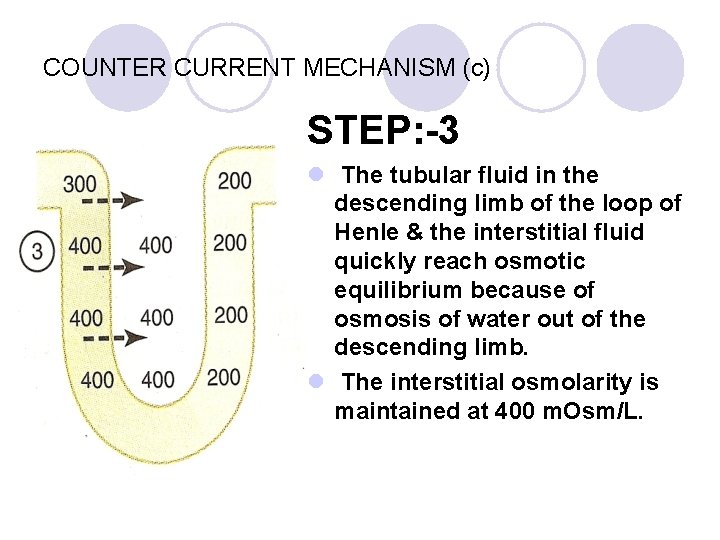
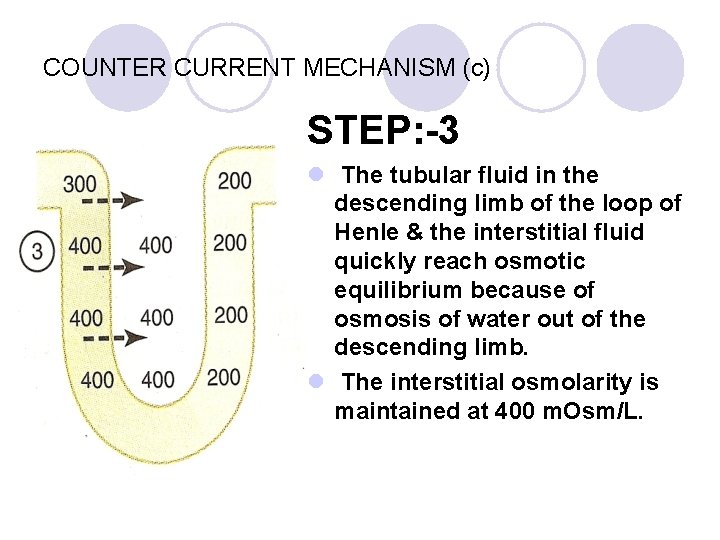
COUNTER CURRENT MECHANISM (c) STEP: -3 l The tubular fluid in the descending limb of the loop of Henle & the interstitial fluid quickly reach osmotic equilibrium because of osmosis of water out of the descending limb. l The interstitial osmolarity is maintained at 400 m. Osm/L.
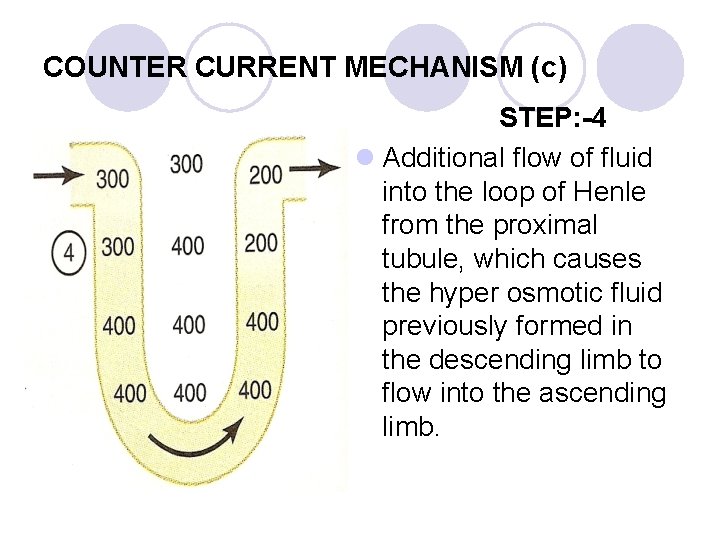
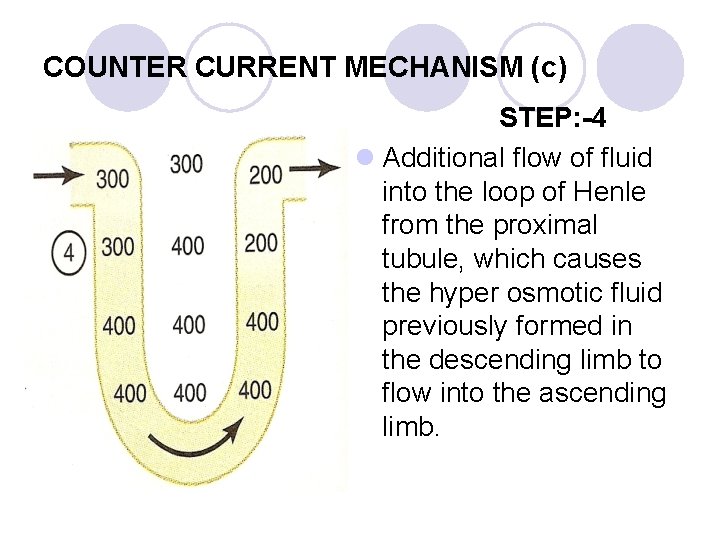
COUNTER CURRENT MECHANISM (c) STEP: -4 l Additional flow of fluid into the loop of Henle from the proximal tubule, which causes the hyper osmotic fluid previously formed in the descending limb to flow into the ascending limb.
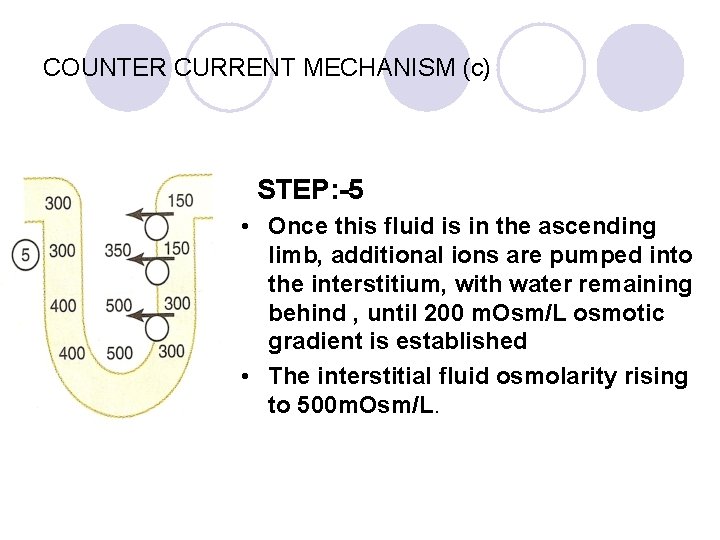
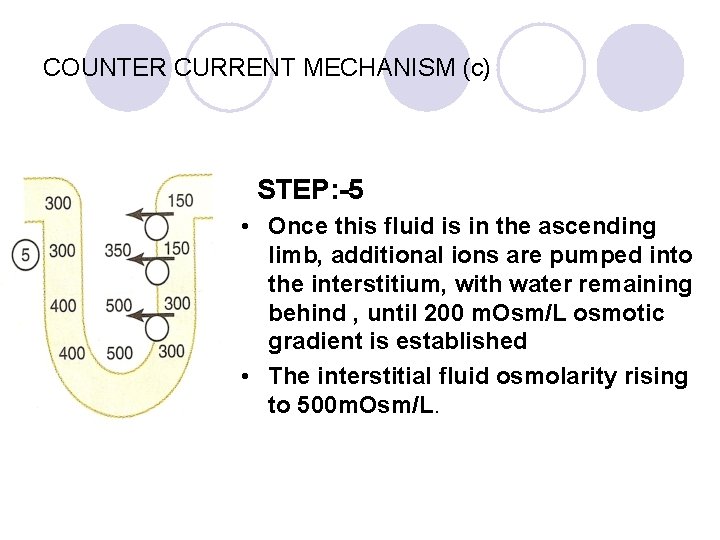
COUNTER CURRENT MECHANISM (c) STEP: -5 • Once this fluid is in the ascending limb, additional ions are pumped into the interstitium, with water remaining behind , until 200 m. Osm/L osmotic gradient is established • The interstitial fluid osmolarity rising to 500 m. Osm/L.
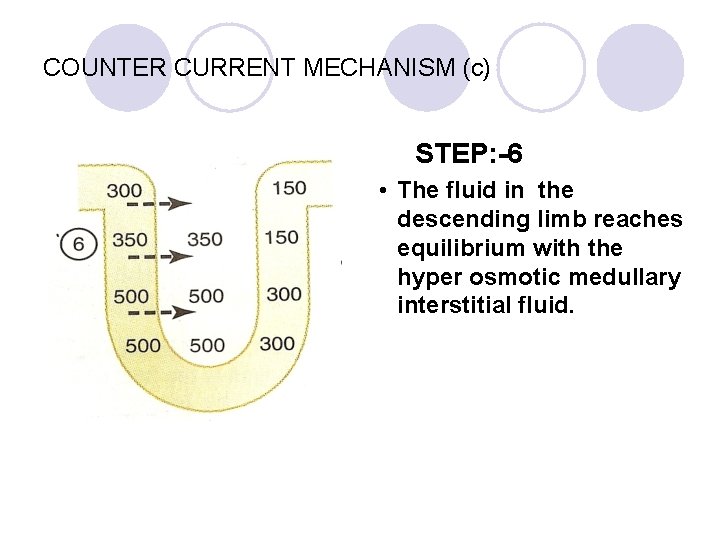
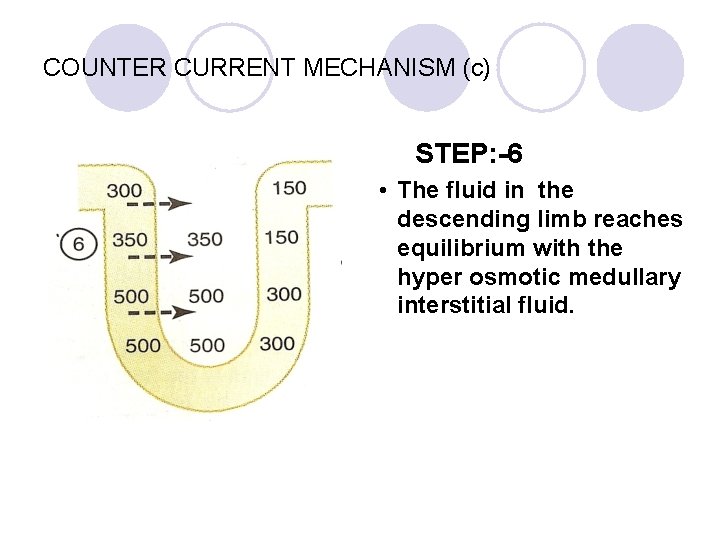
COUNTER CURRENT MECHANISM (c) STEP: -6 • The fluid in the descending limb reaches equilibrium with the hyper osmotic medullary interstitial fluid.
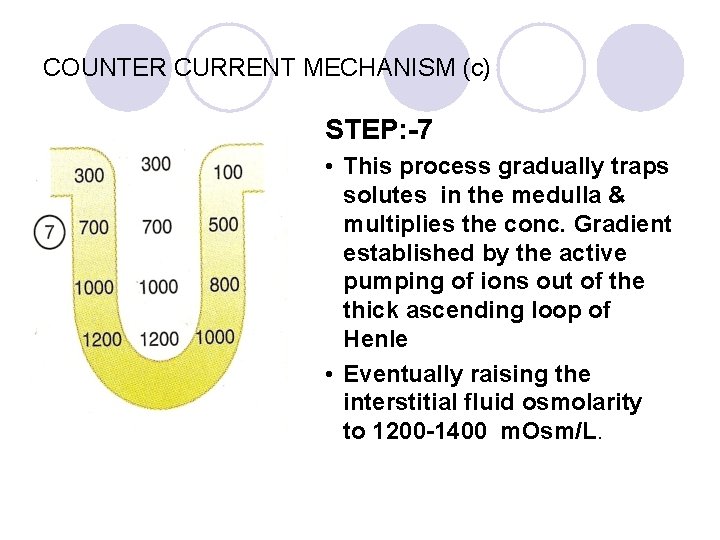
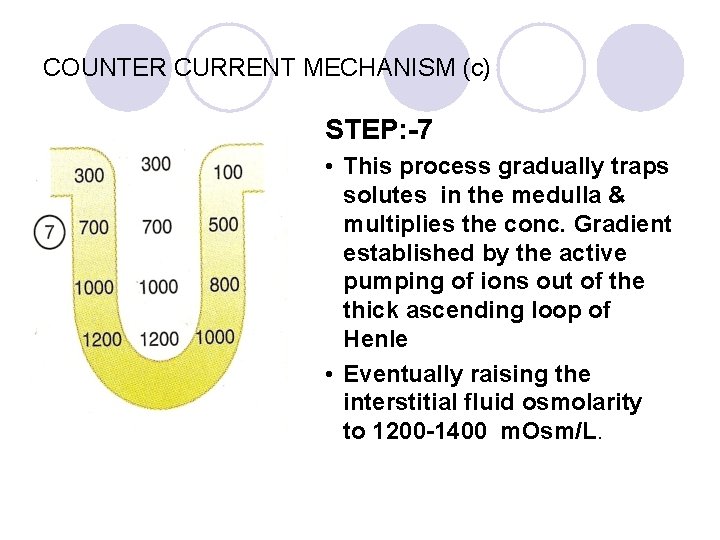
COUNTER CURRENT MECHANISM (c) STEP: -7 • This process gradually traps solutes in the medulla & multiplies the conc. Gradient established by the active pumping of ions out of the thick ascending loop of Henle • Eventually raising the interstitial fluid osmolarity to 1200 -1400 m. Osm/L.
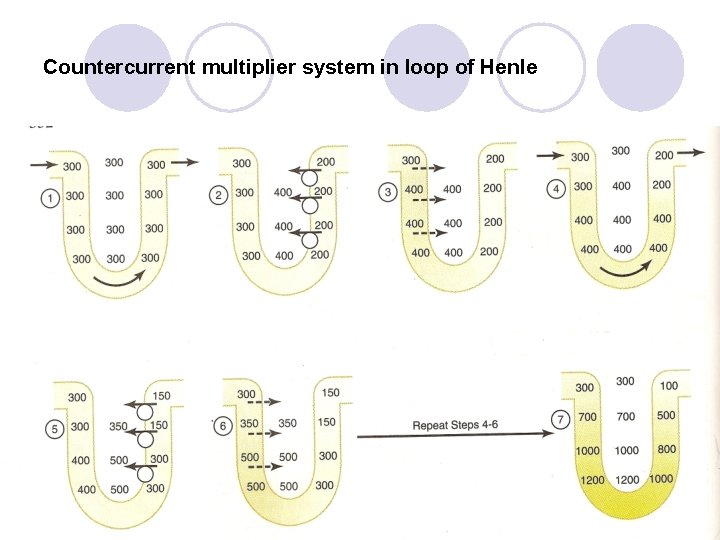
Countercurrent multiplier system in loop of Henle
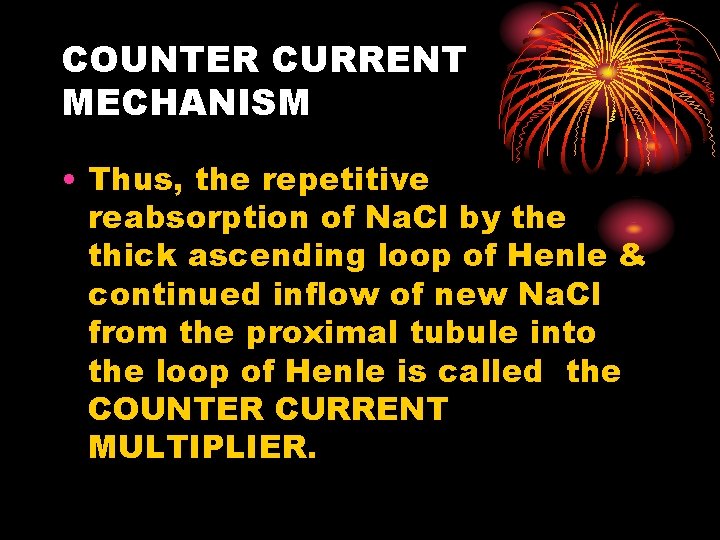
COUNTER CURRENT MECHANISM • Thus, the repetitive reabsorption of Na. Cl by the thick ascending loop of Henle & continued inflow of new Na. Cl from the proximal tubule into the loop of Henle is called the COUNTER CURRENT MULTIPLIER.
Role of distal tubule & collecting ducts in Excreting a concentrated unit • When the tubular fluid flows in to the distal convoluted tubule in the renal cortex, osmolarity of only about 100 m. Osm/L. • In the distal tubule, actively transport of Na. Cl out of tubule but impermeable to water. • In collecting tubule, the amount of water reabsorbed is dependent on the plasma concentration of ADH.
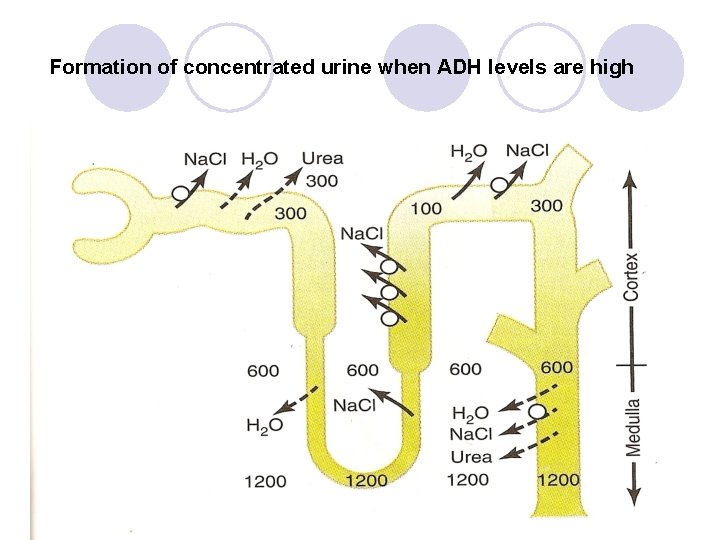
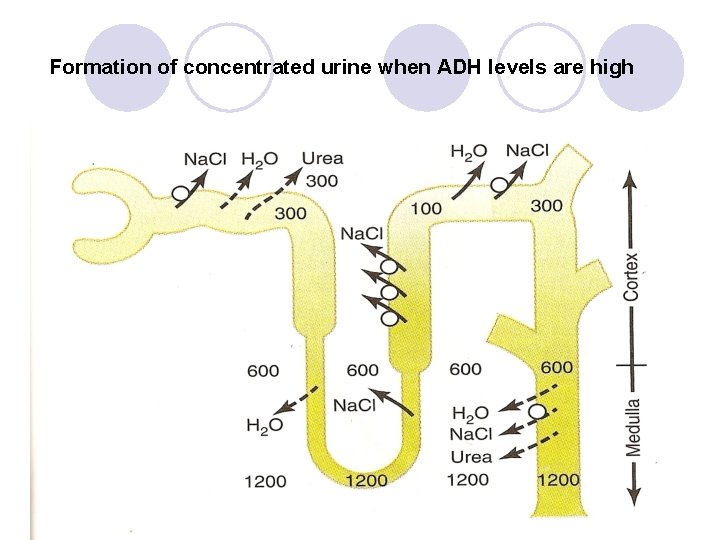
Formation of concentrated urine when ADH levels are high
COUNTER CURRENT EXCHANGE IN THE VASA RECTA PRESERVES HYPEROSMOLARITY OF THE RENAL MEDULLA • This mechanism is responsible for maintaining hyperosmolality of interstitial fluid. • Vasa recta are loop shaped vessels paralleling loop of Henle. They also loop down from cortex to medulla & then back into the cortex of the kidney.
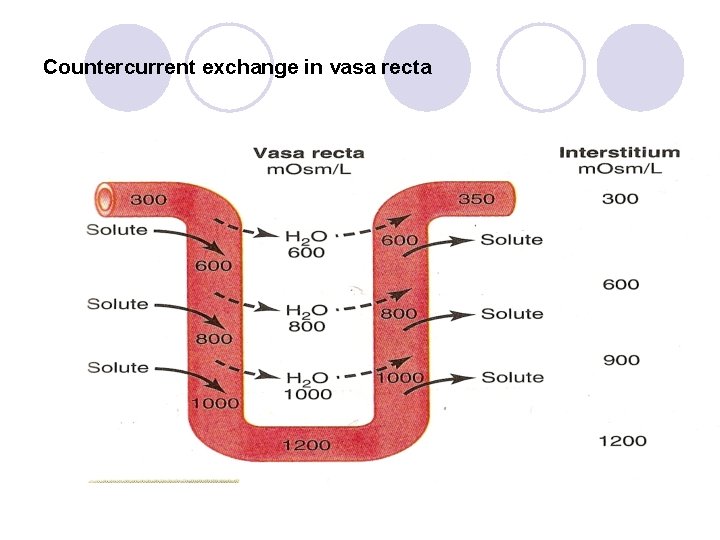
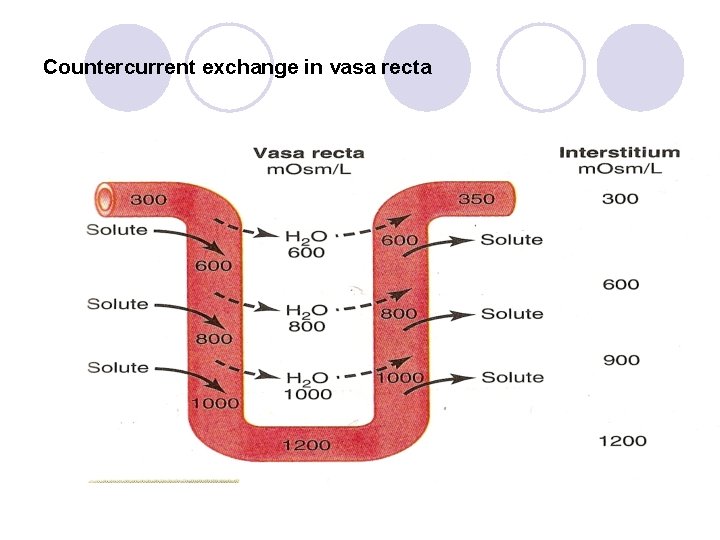
Countercurrent exchange in vasa recta
COUNTER CURRENT EXCHANGE IN THE VASA RECTA • mechanism of counter current exchange works as follow: 1) Inner medullary blood flow is very slight b/z flow is sluggish, removal of solutes in minimized 2) vasa recta serve as counter current exchanger minimizing wash out of solutes from the medullary interstitium.
COUNTER CURRENT EXCHANGE IN THE VASA RECTA • Plasma flowing down the descending limb of the vasa recta becomes more hyper osmotic b/z of diffusion of water out of the blood & diffusion of Na. Cl & urea in to the blood • In the ascending limb of vasa recta solutes diffuse back into the interstitial fluid & water diffuse back into the vasa recta. • Thus large amount of solutes retained in renal medulla due to ‘U’ shape of the vasa recta capillaries.
Thank you