Forensic Toxicology Toxicology Study harmful effects of toxins












- Slides: 29
Forensic Toxicology
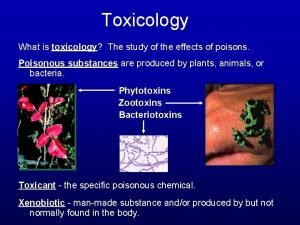
Toxicology Study harmful effects of toxins on animals and plants Many different types: • Environmental (air, water, soil) • “Consumer” (foods, pharmaceuticals, cosmetics) • Medical, clinical, forensic
Clinical vs. Forensic Toxicology • Clinical: –emergency screening (e. g. overdose) –therapeutic drug monitoring (TDM) (limited menu of drugs) Testing only done if likely to affect the management and course of clinical treatment.

Forensic Toxicology Broad based screening and measurement for legal purpose – Postmortem (ME/Coroner) – Criminal (MVA; assault) – Workplace drug testing – Sports (human & animal)
What Do Forensic Toxicologists Do? • Analyze blood and other human fluids or tissues for alcohol, drugs and poisons (analytical toxicology) • Interpret analytical results • Considerable experience required
Analytical Toxicology: What do you need? • Strong Chemistry background – Analytical, organic, physical • • Accuracy and attention to detail Computer skills Troubleshooting skills Willingness to do repetitive work • A “strong stomach” • Common sense, patience

Why? • • Cause of death? Contribution to death? Cause Impairment? Explain Behavior? • Footnote: Drug or alcohol caused deaths almost never show specific signs at autopsy.
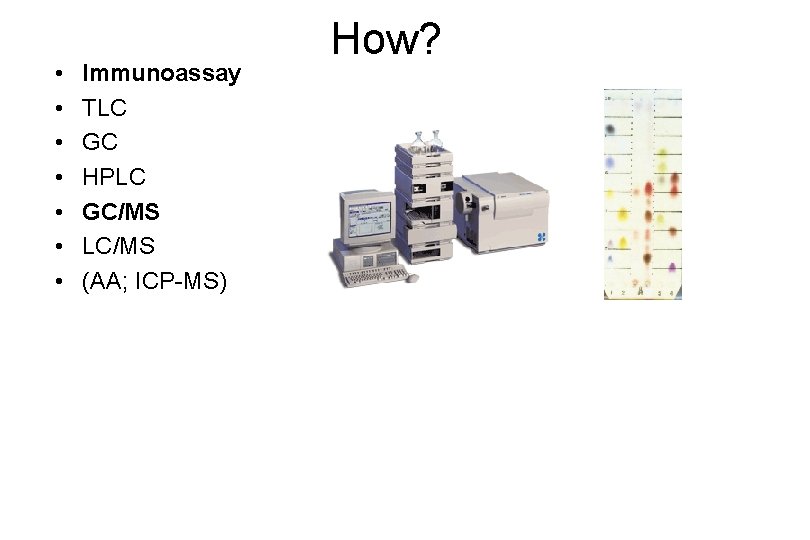
• • Immunoassay TLC GC HPLC GC/MS LC/MS (AA; ICP-MS) How?

Analytical Basis of Toxicology Separation, detection, identification and measurement of drugs in biological specimens • Immunoassay – 10% • Chromatography – 85% • Other – 5%
The Analytical Process • Sample receipt – Chain-of-custody • • Review request and information Decide on testing to be performed Analytical testing Review, evaluate and interpret results

What are the (Analytical) Problems? • 1. Endogenous substances • cholesterol, fats, proteins • putrefactive amines • 2. Enormous range of drug concentrations • therapeutic concentrations range over at least 100, 000 fold • can vary >1000 x even for single class of drugs • 3. Some drugs cannot be readily detected • Analytical conditions may not be appropriate • Drug/poison may be new or very unusual

“Forensic” Alcohol vs. Forensic Clinical
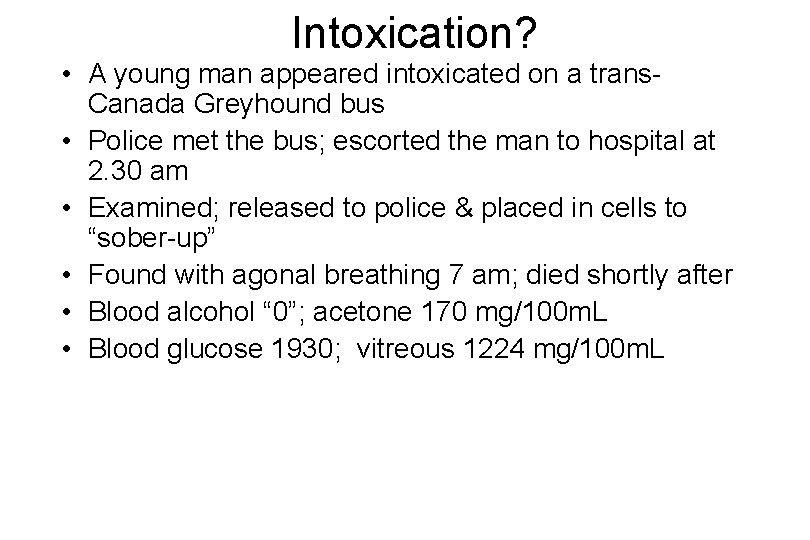
Intoxication? • A young man appeared intoxicated on a trans. Canada Greyhound bus • Police met the bus; escorted the man to hospital at 2. 30 am • Examined; released to police & placed in cells to “sober-up” • Found with agonal breathing 7 am; died shortly after • Blood alcohol “ 0”; acetone 170 mg/100 m. L • Blood glucose 1930; vitreous 1224 mg/100 m. L
Postmortem Fermentation Blood ON ITS OWN is UNRELIABLE as a specimen for assessing the presence of alcohol at the time of death. Blood Vitreous
Postmortem Fermentation • 86 y. o. lady died suddenly from heart disease; autopsy ordered and blood taken for routine toxicology • Blood alcohol 320 mg/100 ml – Urine 0; bile 20 mg/100 ml • No evidence of alcohol abuse • No alcohol in morgue • Meds in blood and urine correlated – Warfarin & digoxin; also blood typing
Methanol Cases… Methanol causes: blindness, acidosis, hypoxic brain damage and death

Methanol Intoxication? Ø Severe MVA Ø Ethanol not detected, but… Ø Urine Me. OH 530 mg% Ø Liver 190, 300 mg% Ø Spleen 20, 70 mg% Ø Explanation?

Carbon Monoxide Deaths Some are obvious… Carbon monoxide binds to hemoglobin 200 x stronger than oxygen!

Carbon Monoxide Deaths Some sources are less obvious…

Postmortem Redistribution Ø False Premise • Blood levels of drugs after autopsy reflect those at the time of death Ø Reality • Many drug levels increase after death; some 2– 10 fold • Many mechanisms • Some drug levels decrease after death (e. g. cocaine)
Other Interpretation Issues • Combined Drug Deaths – additive or synergistic toxicity • Tolerance – need to increase dose for same effect • Genetically Impaired Metabolism – 7 -10% Caucasians are slow metabolizers • Drug-Drug Interactions – can cause synergistic or fatal toxicity
Other Interpretation Issues • Drug Accumulation – caused by decreased metabolism or clearance • Medical Artifacts – intravenous lines; incomplete distribution • Delayed deaths – drug toxicity causes physiological damage; drugs levels may fall to near zero before death occurs
Alcohol Specifics (Route) • Alcohol in stomach (20% absorbed) and intestine • Absorbed within minutes into bloodstream – Timing affected by: – Time taken to consume drink – Alcohol content – Amount consumed – Stomach contents
Alcohol Specifics (Route) • Alcohol distributed to watery parts of body via blood • Liver, 1 st stop- Begin detoxification (0. 015% w/v per hour • Heart • Lungs-Alcohol vapors out with breath – Using Henry’s Law can relate amount of alcohol in breath to amount in blood • Brain-impair neuron transmission

Breath Test Instruments • Breathalyzer – Blow 52. 5 ml of alveolar air into machine – Added to potassium dichromate, silver nitrate, sulfuric acid and water – Alcohol converts dichromate to acetic acid – Dichromate amount reduced-measured via a spectrophotometer in machine (must be calibrated! and chemicals pure)

Breathalyzer
Alcohol and NYS Law • 0 Tolerance Law – Less than 21 – Drive after drinking – Blood alcohol. 02 -. 07 violation of DWAI – Suspend license – Fine – Increased insurance rate – jail

Alcohol and NYS Law • Everyone else: – DWAI at. 08 blood alcohol level – 1 st Offence=15 days jail, $300 -500 fine, 90 day license and registration suspension, surcharge, victim panel – 2 nd Offence=30 days, $500 -750 fine, 6 month license and registration suspension, surcharge, victim panel – Future=Felony
What’s your blood alcohol level? • http: //www. ou. edu/oupd/bac. htm
 Useful and harmful materials in house
Useful and harmful materials in house Important people in forensics
Important people in forensics A breath test reflects the alcohol concentration in the
A breath test reflects the alcohol concentration in the A breath test reflects the alcohol concentration where
A breath test reflects the alcohol concentration where Definition of forensic toxicology
Definition of forensic toxicology Forensic toxicology lab activity
Forensic toxicology lab activity Forensic toxicology vocabulary
Forensic toxicology vocabulary Types of snake toxins
Types of snake toxins Mbvbn
Mbvbn Unit 4: toxins lesson 73 worksheet answers
Unit 4: toxins lesson 73 worksheet answers Human pathogens and toxins act
Human pathogens and toxins act Toxicology study
Toxicology study Toxicology effects
Toxicology effects Toxicology effects
Toxicology effects Nst 110
Nst 110 Dumbi sitti
Dumbi sitti Pathologist and anthropologist
Pathologist and anthropologist Forensic psychiatry vs forensic psychology
Forensic psychiatry vs forensic psychology Forensic odontology
Forensic odontology Effects of internet use and study habits
Effects of internet use and study habits Toxicology excellence for risk assessment
Toxicology excellence for risk assessment Definition of environmental toxicology
Definition of environmental toxicology Chapter 8 toxicology poisons and alcohol
Chapter 8 toxicology poisons and alcohol Chapter 8 toxicology test
Chapter 8 toxicology test Toxicology management
Toxicology management Washington state patrol toxicology lab
Washington state patrol toxicology lab Toxicology definition
Toxicology definition Toxicology and applied pharmacology
Toxicology and applied pharmacology Nc ocme
Nc ocme Toxicology
Toxicology