Foot Pressure Ulcers In Patients with Peripheral Vascular
- Slides: 30
Foot Pressure Ulcers: In Patients with Peripheral Vascular Disease (PVD)/ Peripheral Artery Disease (PAD) ERIN MOORE CLINICAL PROBLEM SOLVING I
Clinical Question: Is peripheral vascular disease/ peripheral artery disease a valid prognostic factor for determining the healing process of foot pressure ulcers in an 80 year old man?
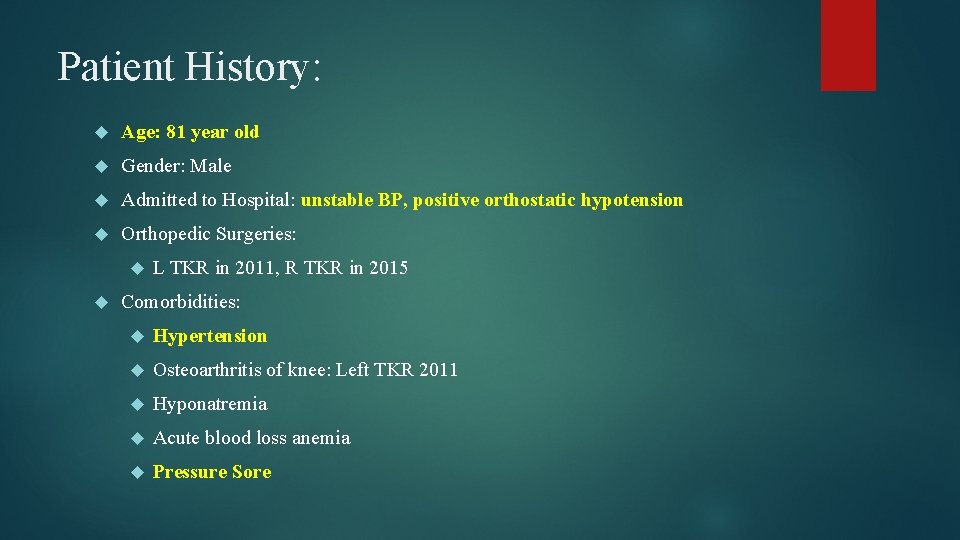
Patient History: Age: 81 year old Gender: Male Admitted to Hospital: unstable BP, positive orthostatic hypotension Orthopedic Surgeries: L TKR in 2011, R TKR in 2015 Comorbidities: Hypertension Osteoarthritis of knee: Left TKR 2011 Hyponatremia Acute blood loss anemia Pressure Sore
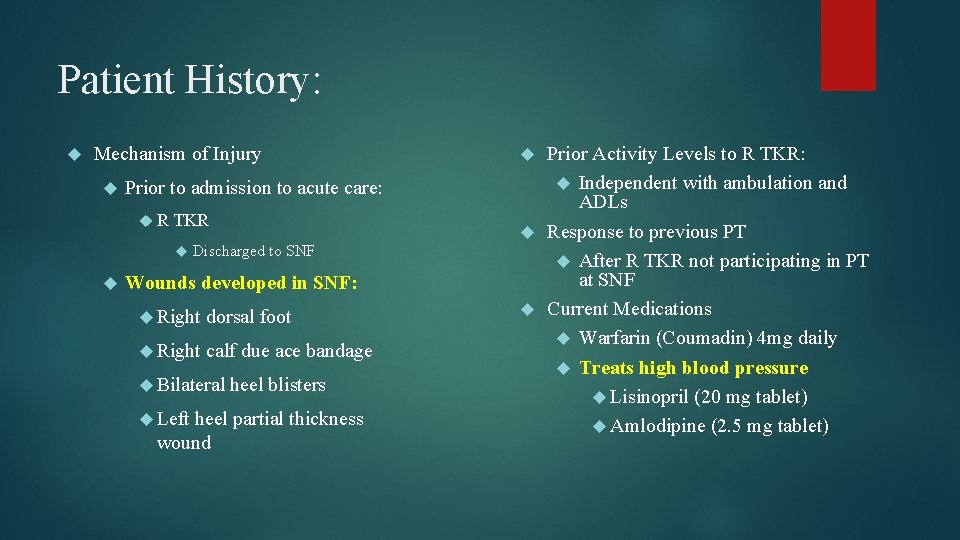
Patient History: Mechanism of Injury Prior to admission to acute care: R TKR Discharged to SNF Wounds developed in SNF: Right dorsal foot Right calf due ace bandage Bilateral Left heel blisters heel partial thickness wound Prior Activity Levels to R TKR: Independent with ambulation and ADLs Response to previous PT After R TKR not participating in PT at SNF Current Medications Warfarin (Coumadin) 4 mg daily Treats high blood pressure Lisinopril (20 mg tablet) Amlodipine (2. 5 mg tablet)
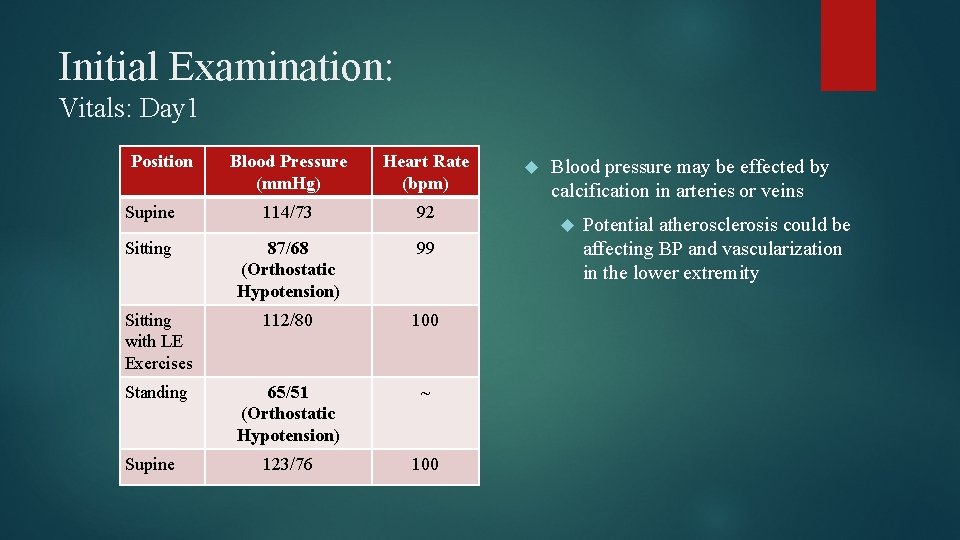
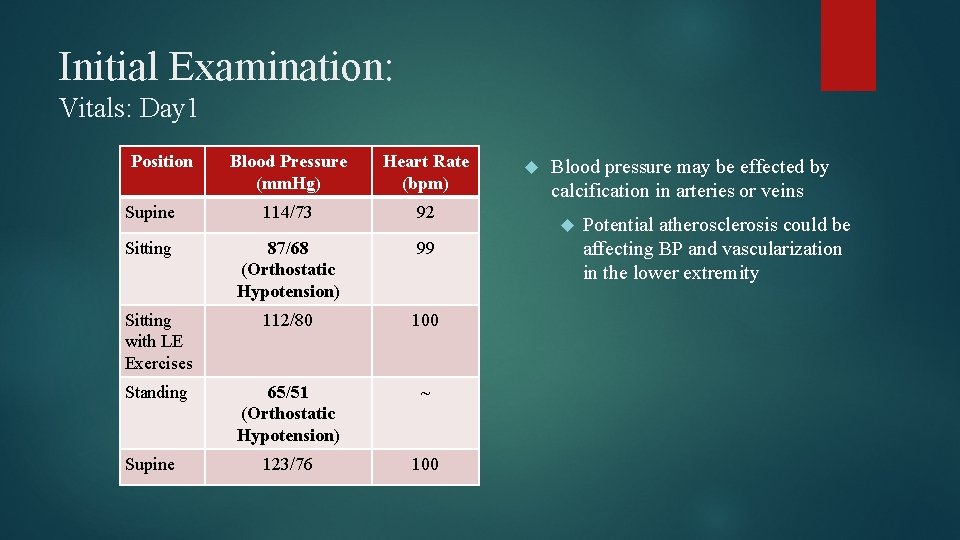
Initial Examination: Vitals: Day 1 Position Blood Pressure (mm. Hg) Heart Rate (bpm) Supine 114/73 92 Sitting 87/68 (Orthostatic Hypotension) 99 Sitting with LE Exercises 112/80 100 Standing 65/51 (Orthostatic Hypotension) ~ 123/76 100 Supine Blood pressure may be effected by calcification in arteries or veins Potential atherosclerosis could be affecting BP and vascularization in the lower extremity
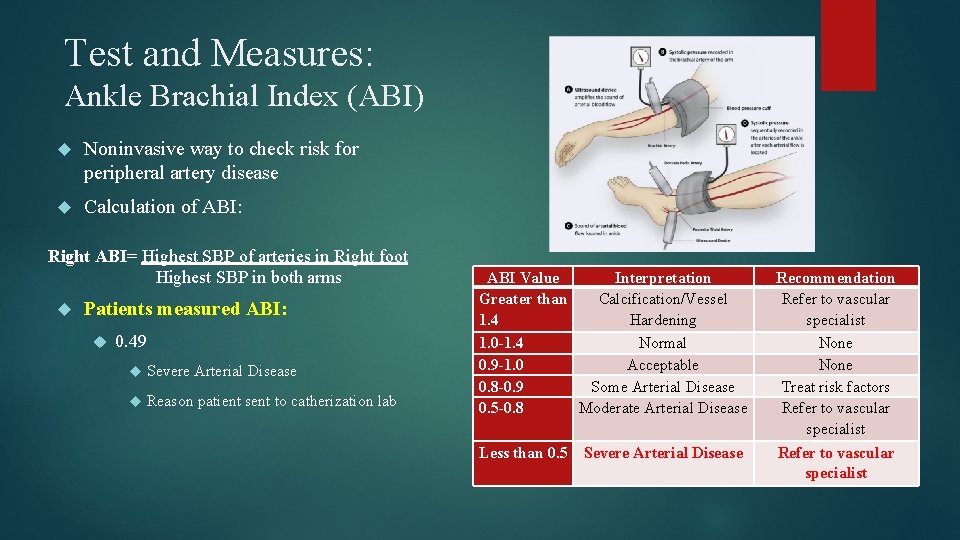
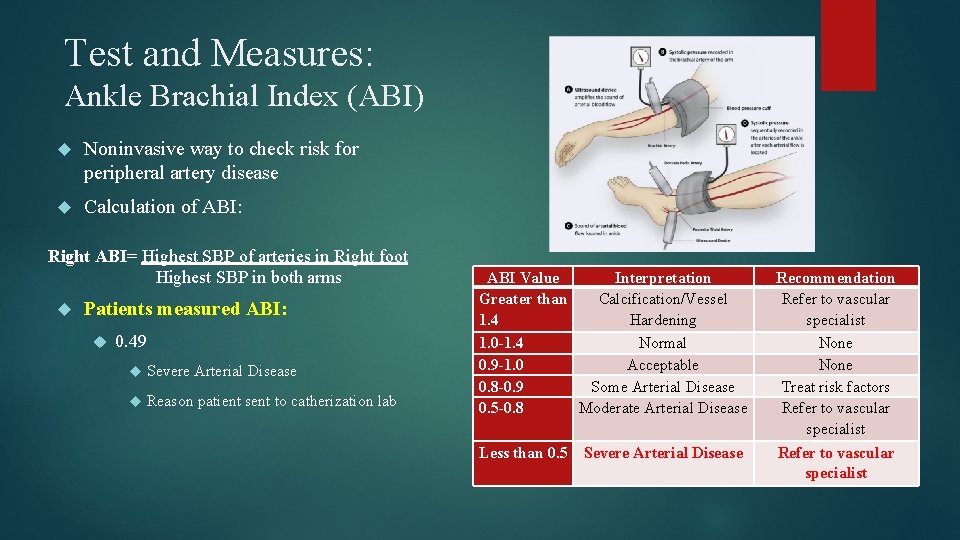
Test and Measures: Ankle Brachial Index (ABI) Noninvasive way to check risk for peripheral artery disease Calculation of ABI: Right ABI= Highest SBP of arteries in Right foot Highest SBP in both arms Patients measured ABI: 0. 49 Severe Arterial Disease Reason patient sent to catherization lab ABI Value Interpretation Greater than Calcification/Vessel 1. 4 Hardening 1. 0 -1. 4 Normal 0. 9 -1. 0 Acceptable 0. 8 -0. 9 Some Arterial Disease 0. 5 -0. 8 Moderate Arterial Disease Less than 0. 5 Severe Arterial Disease Recommendation Refer to vascular specialist None Treat risk factors Refer to vascular specialist
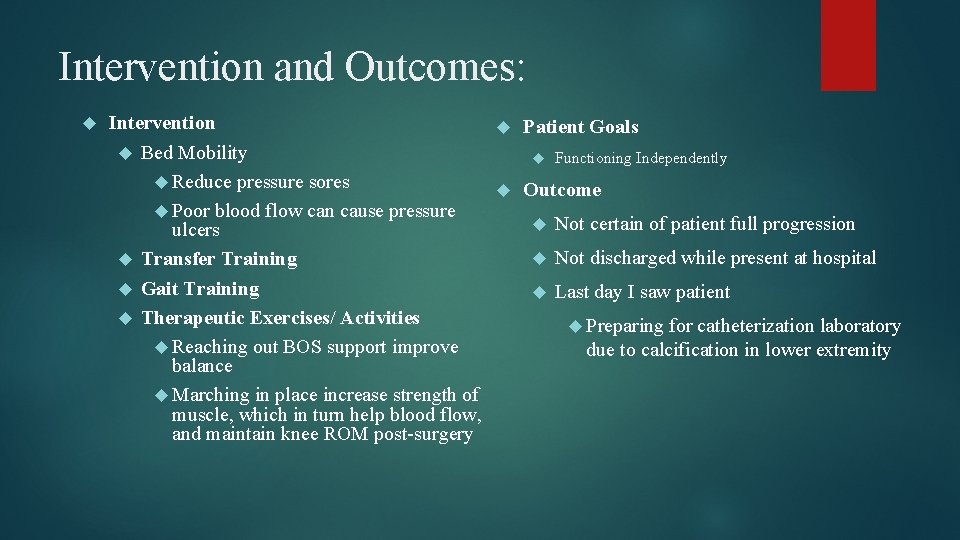
Intervention and Outcomes: Intervention Patient Goals Bed Mobility Functioning Independently Reduce pressure sores Outcome Poor blood flow can cause pressure Not certain of patient full progression ulcers Not discharged while present at hospital Transfer Training Gait Training Last day I saw patient Therapeutic Exercises/ Activities Preparing for catheterization laboratory Reaching out BOS support improve due to calcification in lower extremity balance Marching in place increase strength of muscle, which in turn help blood flow, and maintain knee ROM post-surgery
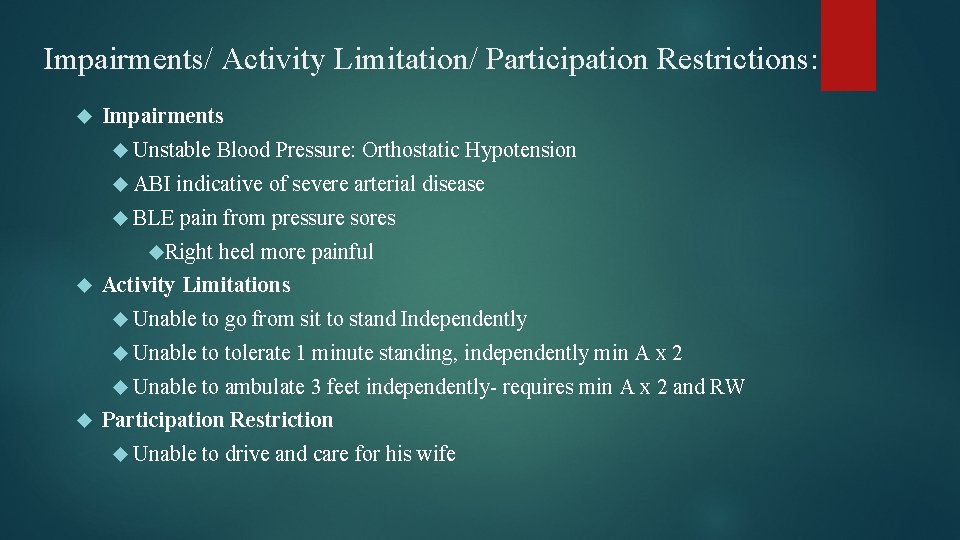
Impairments/ Activity Limitation/ Participation Restrictions: Impairments Unstable ABI indicative of severe arterial disease BLE pain from pressure sores Right Blood Pressure: Orthostatic Hypotension heel more painful Activity Limitations Unable to go from sit to stand Independently Unable to tolerate 1 minute standing, independently min A x 2 Unable to ambulate 3 feet independently- requires min A x 2 and RW Participation Restriction Unable to drive and care for his wife
Factors related to outcome of neuroischemic/ischemic foot ulcer in diabetic patients: Prospective study of individuals with diabetes, foot ulcers, and severe PVD
Methods: Study Population 1151 patients were included Average Age: 75 61% males Patients with diabetes, foot ulcers and severe PVD Followed every patient 5 years after intervention
Methods: Inclusion Criteria Diabetes mellitus and foot ulcer and systolic toe pressure <45 mm Hg, a systolic ankle pressure <80 mm Hg Non-palpable Wagner All foot pulses: grades 4 -5 or pain at rest Grade 4: forefoot gangrene Grade 5: Full foot gangrene patient fulfilled Fontaine grade 4 Ischemic ulcers or gangrene
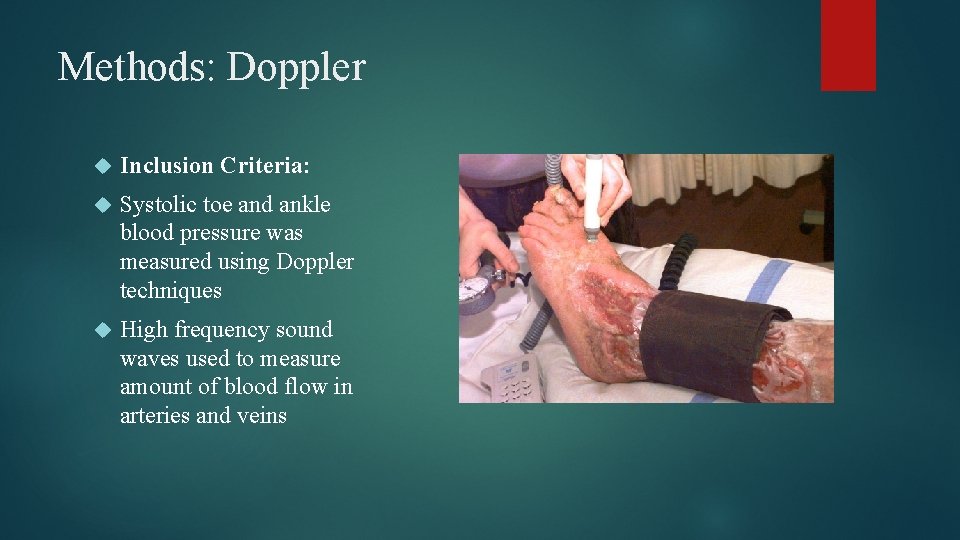
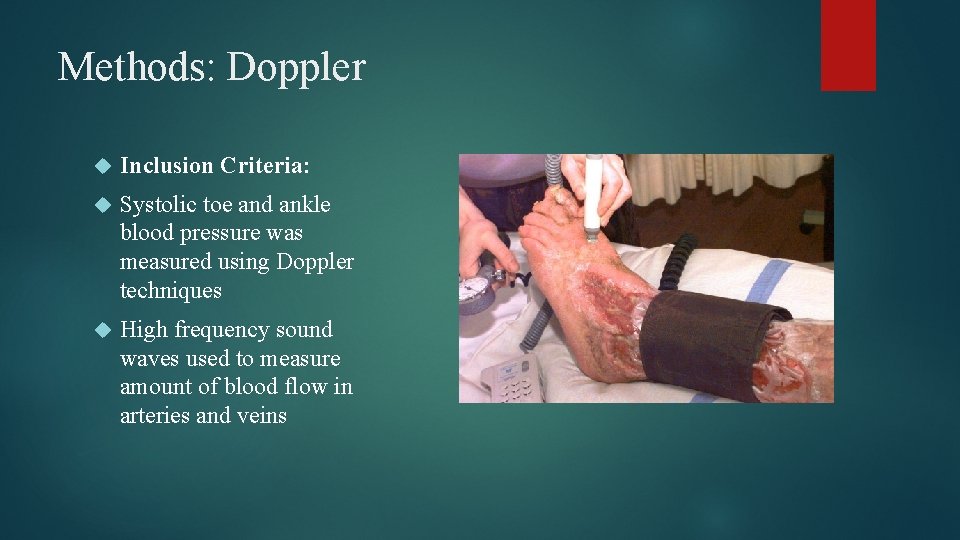
Methods: Doppler Inclusion Criteria: Systolic toe and ankle blood pressure was measured using Doppler techniques High frequency sound waves used to measure amount of blood flow in arteries and veins
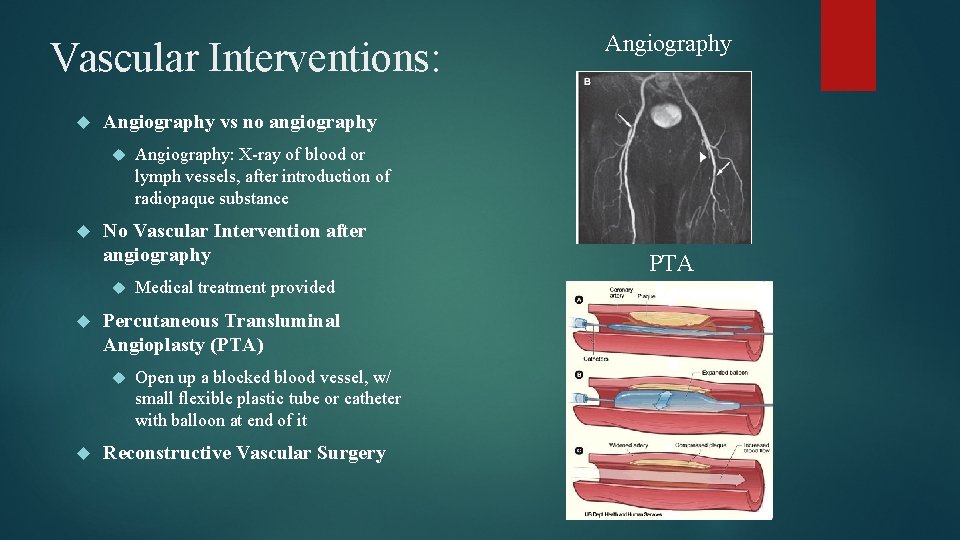
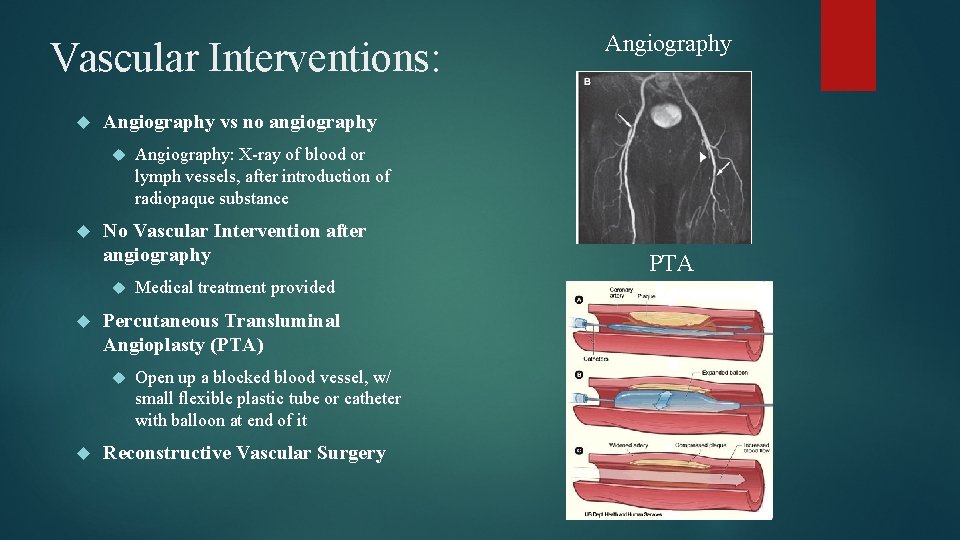
Vascular Interventions: Angiography vs no angiography Medical treatment provided Percutaneous Transluminal Angioplasty (PTA) Angiography: X-ray of blood or lymph vessels, after introduction of radiopaque substance No Vascular Intervention after angiography Angiography Open up a blocked blood vessel, w/ small flexible plastic tube or catheter with balloon at end of it Reconstructive Vascular Surgery PTA
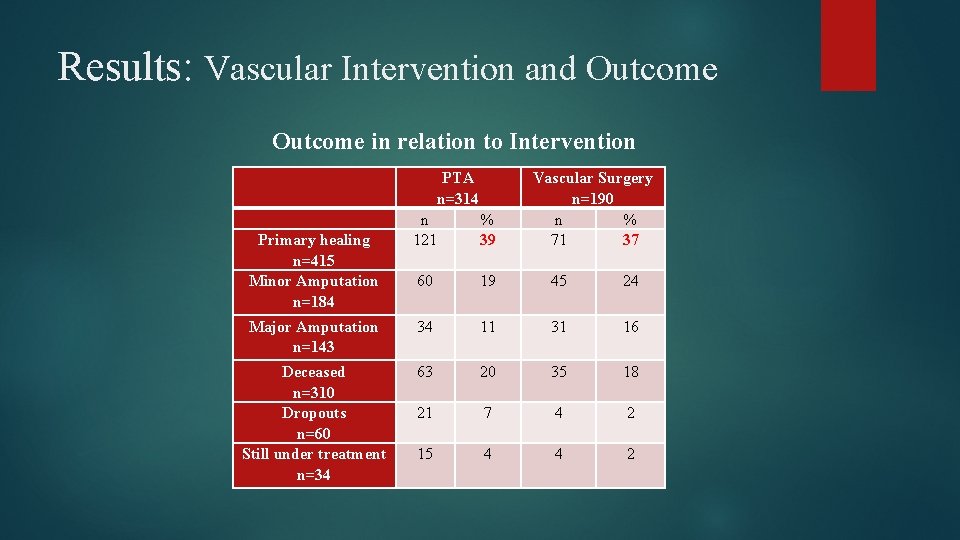
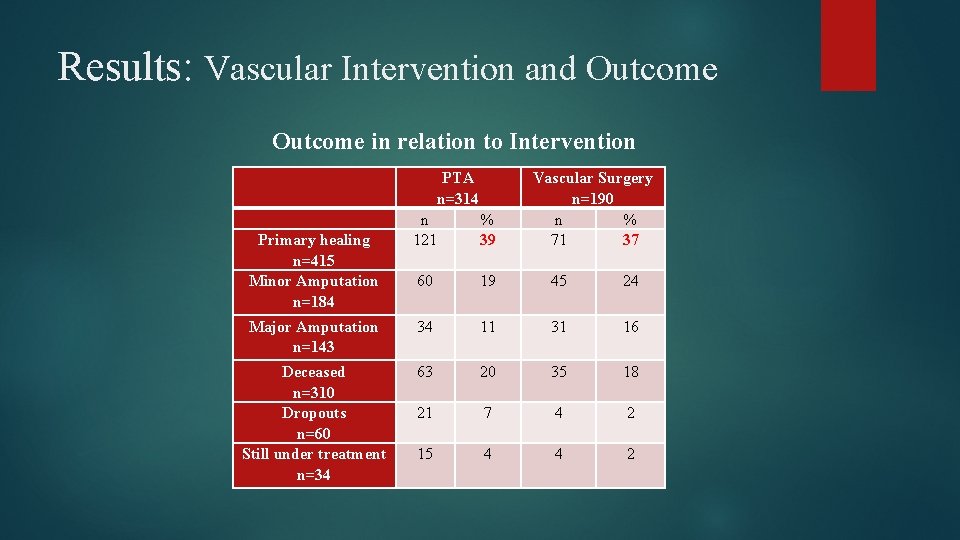
Results: Vascular Intervention and Outcome in relation to Intervention PTA n=314 Vascular Surgery n=190 n % 71 37 n 121 % 39 60 19 45 24 Major Amputation n=143 34 11 31 16 Deceased n=310 Dropouts n=60 Still under treatment n=34 63 20 35 18 21 7 4 2 15 4 4 2 Primary healing n=415 Minor Amputation n=184
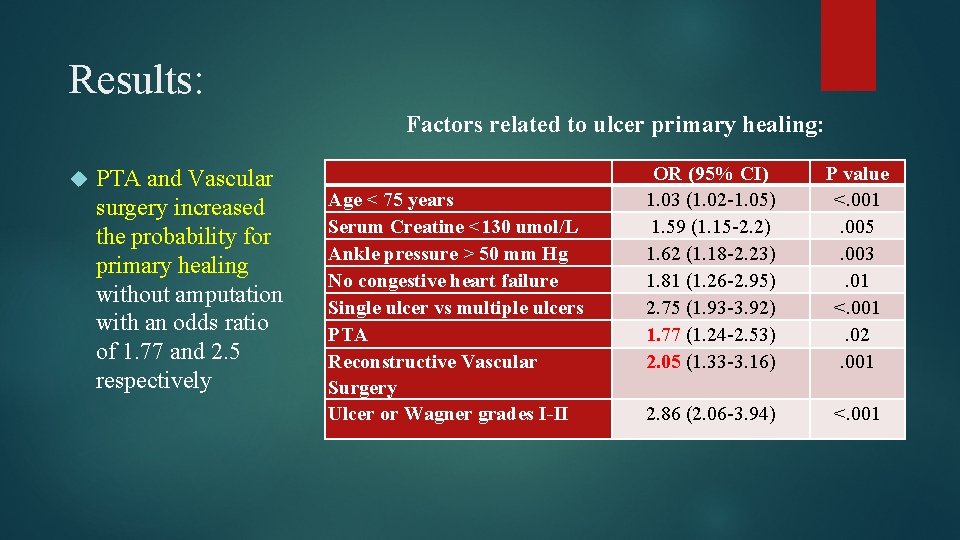
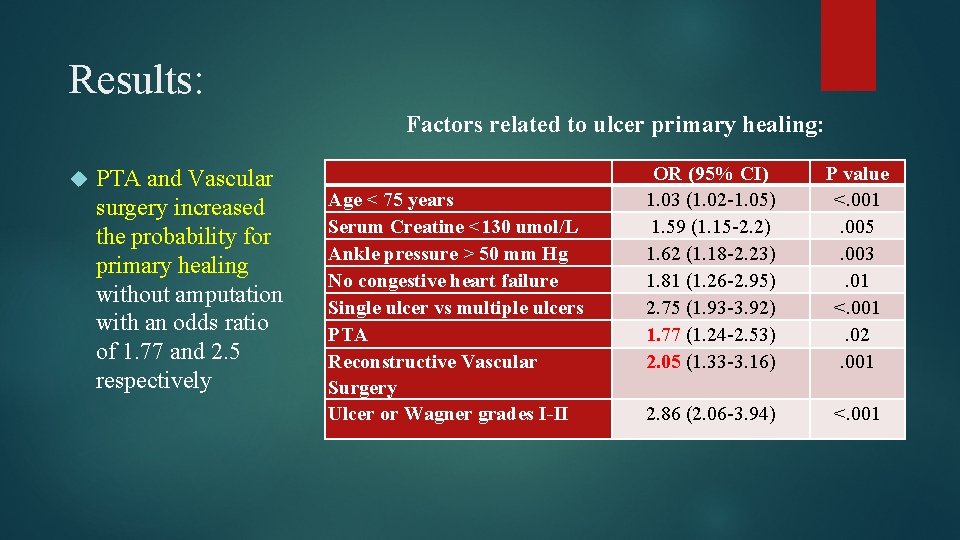
Results: Factors related to ulcer primary healing: PTA and Vascular surgery increased the probability for primary healing without amputation with an odds ratio of 1. 77 and 2. 5 respectively Age < 75 years Serum Creatine <130 umol/L Ankle pressure > 50 mm Hg No congestive heart failure Single ulcer vs multiple ulcers PTA Reconstructive Vascular Surgery Ulcer or Wagner grades I-II OR (95% CI) 1. 03 (1. 02 -1. 05) 1. 59 (1. 15 -2. 2) 1. 62 (1. 18 -2. 23) 1. 81 (1. 26 -2. 95) 2. 75 (1. 93 -3. 92) 1. 77 (1. 24 -2. 53) 2. 05 (1. 33 -3. 16) P value <. 001. 005. 003. 01 <. 001. 02. 001 2. 86 (2. 06 -3. 94) <. 001
Conclusion: Factors that negatively affected the probability of healing. Comorbidity: Severity Extent ulcers congestive heart failure and/or renal disease of PVD: ankle brachial index < 50 mm Hg of tissue involvement: Wagner grades 3 -5 and multiple
Limitation of Study: Unable to compare outcome of PTA or reconstructive surgery Vascular surgery performed in patients not feasible for PTA Negative Selection Bias Patients admitted to university-based foot center Possibility ulcers treated in primary health care without knowledge of foot team
Application to Patient: Median Age in Study: 75 Patient: Increased likelihood of having PTA or vascular reconstructive surgery due to: ABI 81 years old indicative: Severe arterial disease If patient has a procedure such as PTA or vascular reconstructive surgery Prognosis: Odds ratio of primary healing, good
Early Revascularization after Admittance to Diabetic Foot Center Affects the Healing Probability of Ischemic Foot Ulcer in Patients with Diabetes
Methods: Study Population 478 patients prospectively included Diabetes, foot ulcers, and severe PAD Average age: 74 yo Male: 60% Treated and followed by a multidisciplinary foot team Continuous follow up until healing or death
Methods: Inclusion Criteria Patients with diabetes mellitus, foot ulcer and a systolic toe pressure <45 mm Hg and or systolic ankle pressure < 80 mm Hg (Doppler techniques) Non-palpable foot pulses with an ulcer Wagner grade 4 -5 or pain at rest Rest pain: Severe persistent pain localized to foot and relieved by dependency All patients were Fontaine grade 4 Exclusion Criteria Patients who did not have invasive revascularization
Methods: Study Design Either had percutaneous transluminal angioplasty (PTA) or reconstructive surgery PTA not feasible, surgery next option Time to revascularization calculated First visit to diabetic foot center
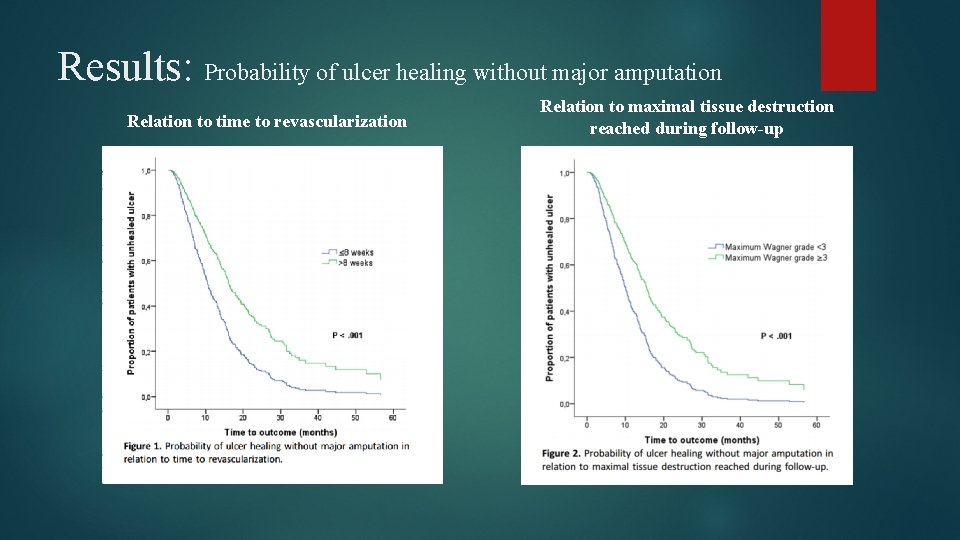
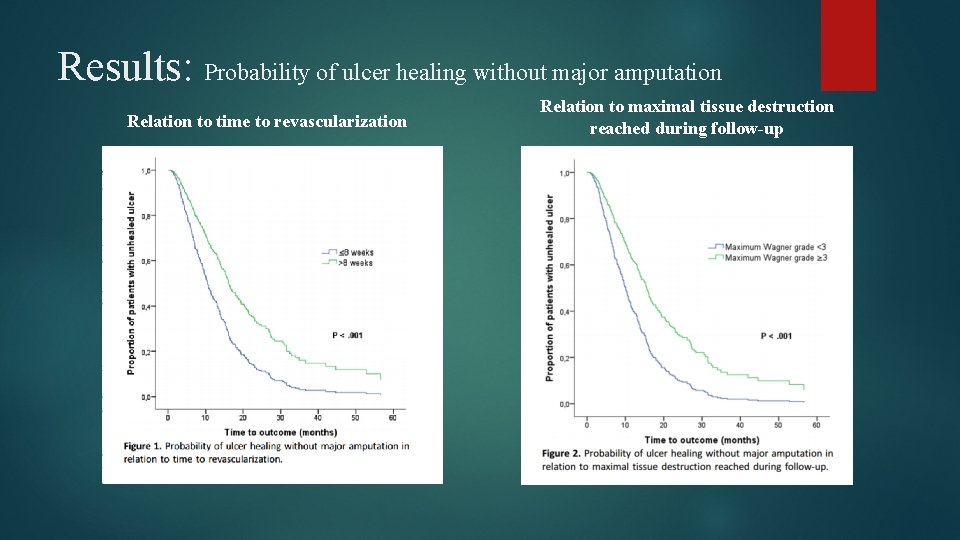
Results: Probability of ulcer healing without major amputation Relation to time to revascularization Relation to maximal tissue destruction reached during follow-up
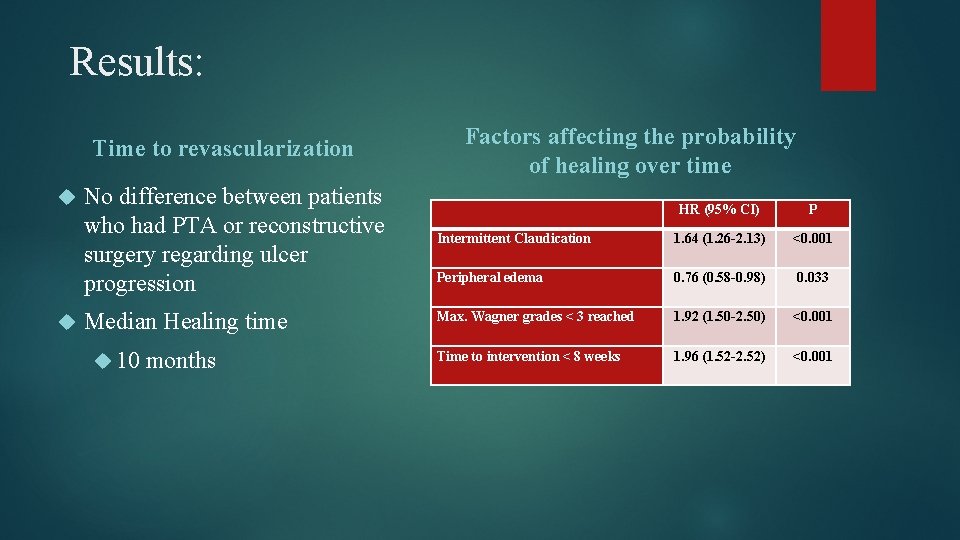
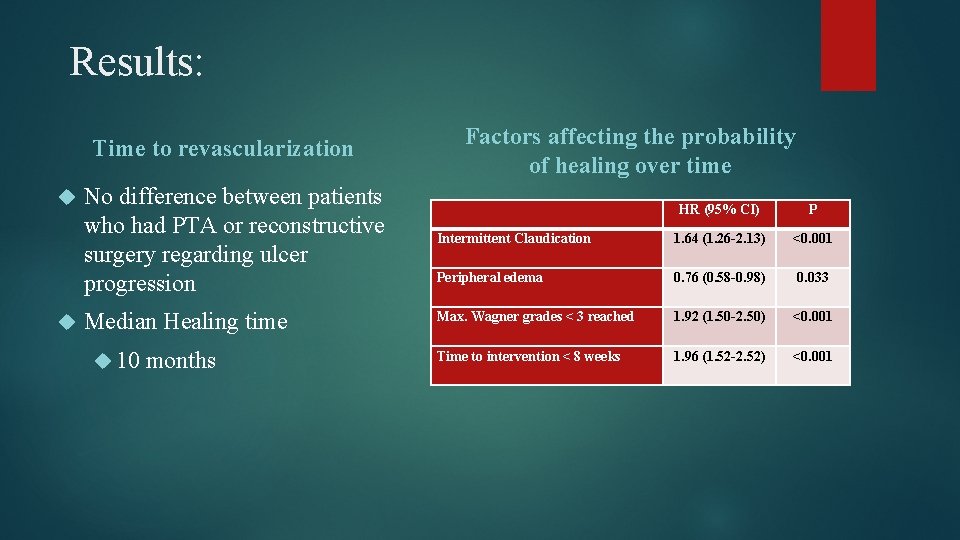
Results: Factors affecting the probability of healing over time Time to revascularization No difference between patients who had PTA or reconstructive surgery regarding ulcer progression Median Healing time 10 months HR (95% CI) P Intermittent Claudication 1. 64 (1. 26 -2. 13) <0. 001 Peripheral edema 0. 76 (0. 58 -0. 98) 0. 033 Max. Wagner grades < 3 reached 1. 92 (1. 50 -2. 50) <0. 001 Time to intervention < 8 weeks 1. 96 (1. 52 -2. 52) <0. 001
Conclusion: Factors affecting probability of healing without major amputation Shorter Extent time to revascularization of tissue destruction Peripheral edema Intermittent claudication
Limitations to Study: Decision for vascular intervention at the discretion of vascular surgeon No control group Either received PTA or reconstructive vascular surgery Time to revascularization calculated from first visit with foot team Foot ulcer onset is usually unknown
Application to patient: Average Age 74 yo Patient: 81 yo After catheterization lab results? Depending on degree of calcification may determine whether patient needs PTA or reconstructive vascular surgery Median healing time 10 months Prognosis: Fair due to length of healing time Patient does have son that is available 24/7 Patient motivated
Conclusion: Is peripheral vascular disease/ peripheral artery disease a valid prognostic factor for determining the healing process of foot pressure ulcers in an 80 year old man? Why is this important to PT? As clinicians able to perform ABI Analyze Make Clinical Question? PAD and PVD negative impact on healing process of foot ulcer Healing time potentially 10 months results physician aware of results motivation Severe arterial disease Effects progress of pressure ulcer healing May deter patient from ambulation, due to pain Perform on ulcer exercise that avoid pressure of patient? Once patient has surgery the importance of mobility to increase blood flow
Resources: Apelqvist, J. , Elgzyri, T. , Larsson, J. , Londahl, M. , Nyberg, P. , Thorne, J. (2011). Factors related to outcome of neuroischmeic/ischemic foot ulcer in diabetic patients. Journal of Vascular Surgery, 53(9), 1582 -1588. Retrieved from http: //www. sciencedirect. com/science/article/pii/S 0741521411002990 Apelqvist, J. , Elgzyri, T. , Eriksson, K. , Larsson, J. , Nyberg, P. , Thorne, J. (2014). Early Revascularization after Admittance to a Diabetic Foot Center Affects the Healing Probability of Ischemic Foot Ulcer in Patients with Diabetes. European Journal of Vascular and Endovascular Surgery, 48 (7), 440 -446. Retrieved from http: //www. sciencedirect. com/science/article/pii/S 1078588414003876 Images http: //www. southpalmcardiovascular. com/florida-vein-specialists-explain-the-ankle-brachial-index-test-and-how-it-is-used-todetect-vascular-disease/ http: //www. worldwidewounds. com/2001/march/Vowden/Doppler-assessment-and-ABPI. html https: //www. drmcdougall. com/misc/2006 nl/sept/angio. htm (Angiography) http: //www. nature. com/nrcardio/journal/v 4/n 12/fig_tab/ncpcardio 1035_F 6. html (PTA)
Questions?