Foot Pathologies Traumatic Injuries Pressure Injuries Midfoot Pathologies

- Slides: 33
Foot Pathologies: Traumatic Injuries, Pressure Injuries, Midfoot Pathologies, and Toe Pathologies. To take full advantage of the learning opportunities presented in this resource, Internet access is recommended. Also, view the presentation in “Slide Show” mode. Click on the “Slide Show” tab in your tool bar, then click on the “From the Beginning” tab. As an alternative, you may press the F 5 key as a shortcut to begin the presentation.
Foot Pathologies. Traumatic Injuries: • Plantar Fasciitis; • Turf Toe; • Sprains and Strains.
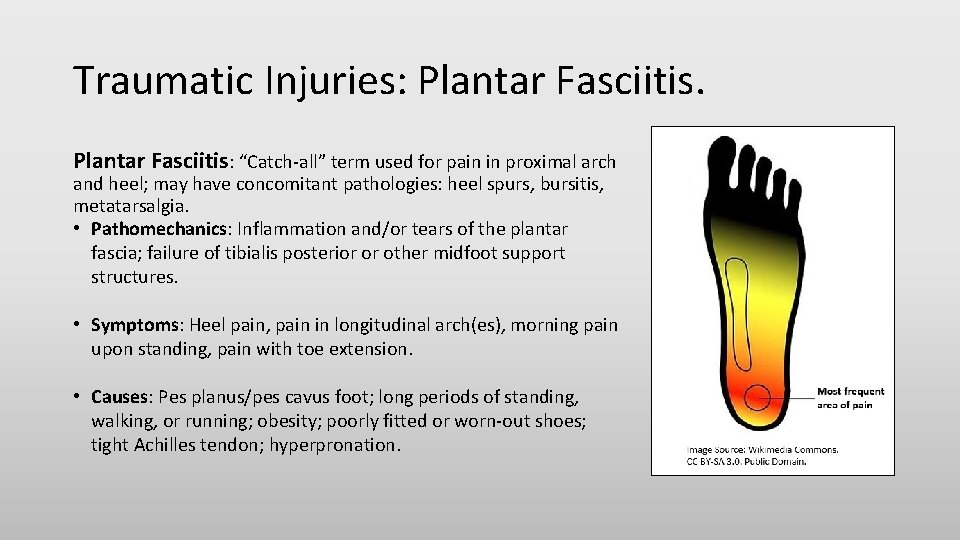
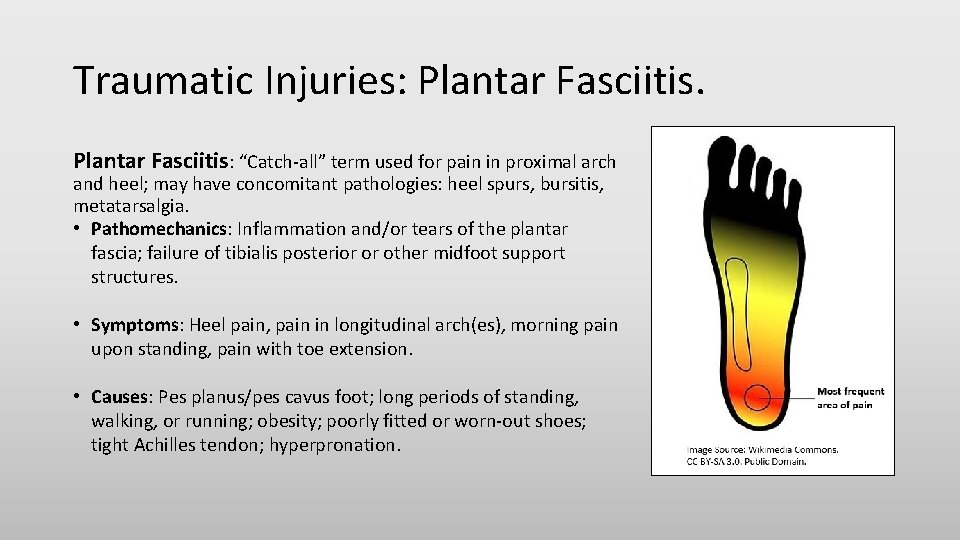
Traumatic Injuries: Plantar Fasciitis: “Catch-all” term used for pain in proximal arch and heel; may have concomitant pathologies: heel spurs, bursitis, metatarsalgia. • Pathomechanics: Inflammation and/or tears of the plantar fascia; failure of tibialis posterior or other midfoot support structures. • Symptoms: Heel pain, pain in longitudinal arch(es), morning pain upon standing, pain with toe extension. • Causes: Pes planus/pes cavus foot; long periods of standing, walking, or running; obesity; poorly fitted or worn-out shoes; tight Achilles tendon; hyperpronation.

Traumatic Injuries: Plantar Fasciitis Video. Watch this video to learn more about Plantar Fasciitis. Click on the following video title: Plantar Fasciitis: Causes, Diagnosis, and Treatment.
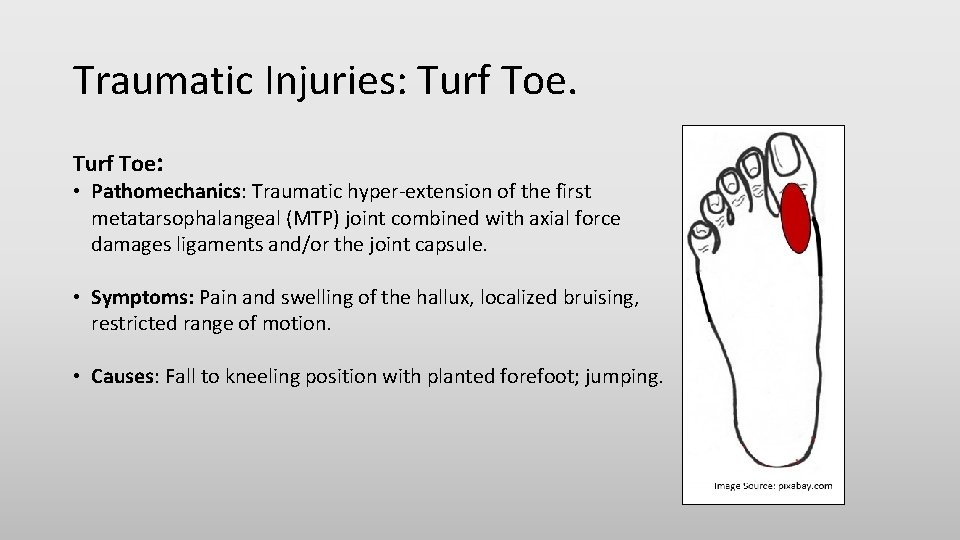
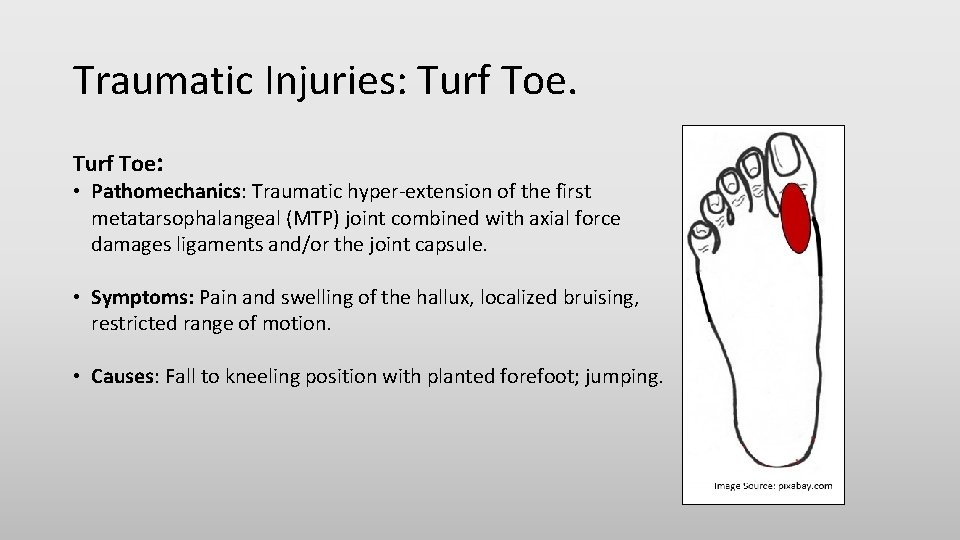
Traumatic Injuries: Turf Toe: • Pathomechanics: Traumatic hyper-extension of the first metatarsophalangeal (MTP) joint combined with axial force damages ligaments and/or the joint capsule. • Symptoms: Pain and swelling of the hallux, localized bruising, restricted range of motion. • Causes: Fall to kneeling position with planted forefoot; jumping.
Traumatic Injuries: Sprains and Strains. Sprains: Occur in ligaments, which are thick bands of cartilage that attach one bone to another. They occur in response to a stretch or tear of a ligament and usually result from traumas like a fall or an external force that displaces the surrounding joint from its normal alignment. Symptoms: Bruising, swelling, instability, and painful movement. Strains: Affect muscles or tendons, which are thick bands that attach muscle to bones. They occur in reaction to a quick tear, twist, or pull of the muscle. They usually result from overstretching or over contraction. Symptoms: Pain, weakness, and muscle spasms.
Foot Pathologies, continued. Pressure Injuries: • Plantar Ulcers; • Heel Spurs; • Retrocalcaneal Bursitis; • Bunion/Hallux Valgus; • Corns and Calluses.
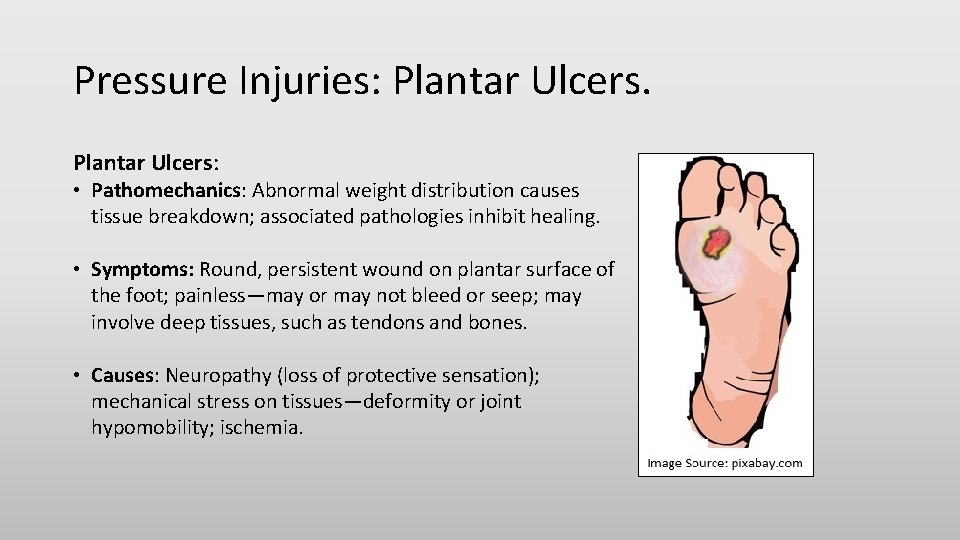
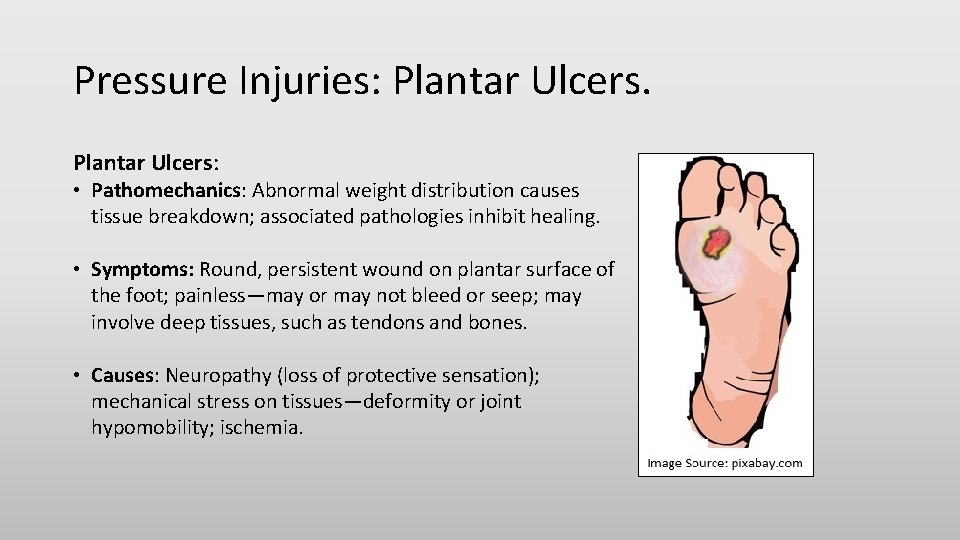
Pressure Injuries: Plantar Ulcers: • Pathomechanics: Abnormal weight distribution causes tissue breakdown; associated pathologies inhibit healing. • Symptoms: Round, persistent wound on plantar surface of the foot; painless—may or may not bleed or seep; may involve deep tissues, such as tendons and bones. • Causes: Neuropathy (loss of protective sensation); mechanical stress on tissues—deformity or joint hypomobility; ischemia.
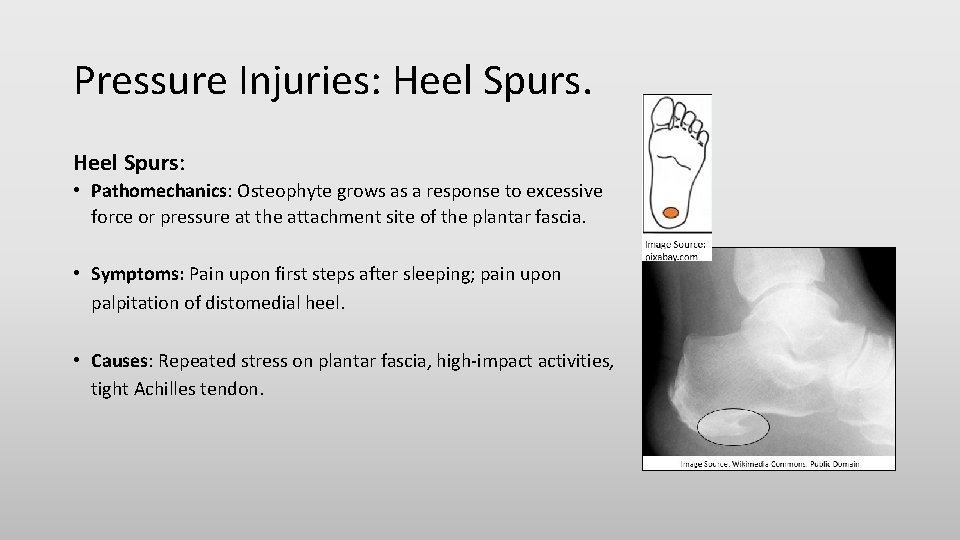
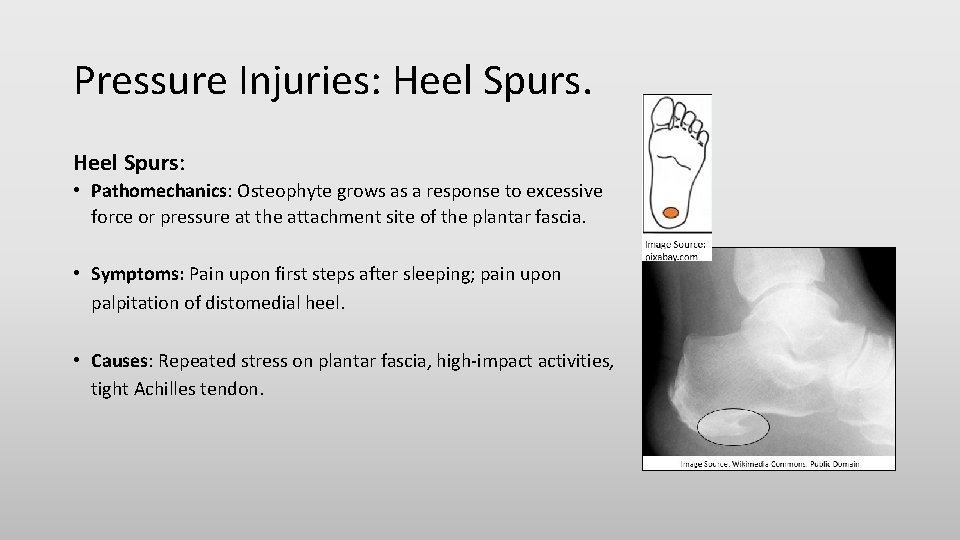
Pressure Injuries: Heel Spurs: • Pathomechanics: Osteophyte grows as a response to excessive force or pressure at the attachment site of the plantar fascia. • Symptoms: Pain upon first steps after sleeping; pain upon palpitation of distomedial heel. • Causes: Repeated stress on plantar fascia, high-impact activities, tight Achilles tendon.
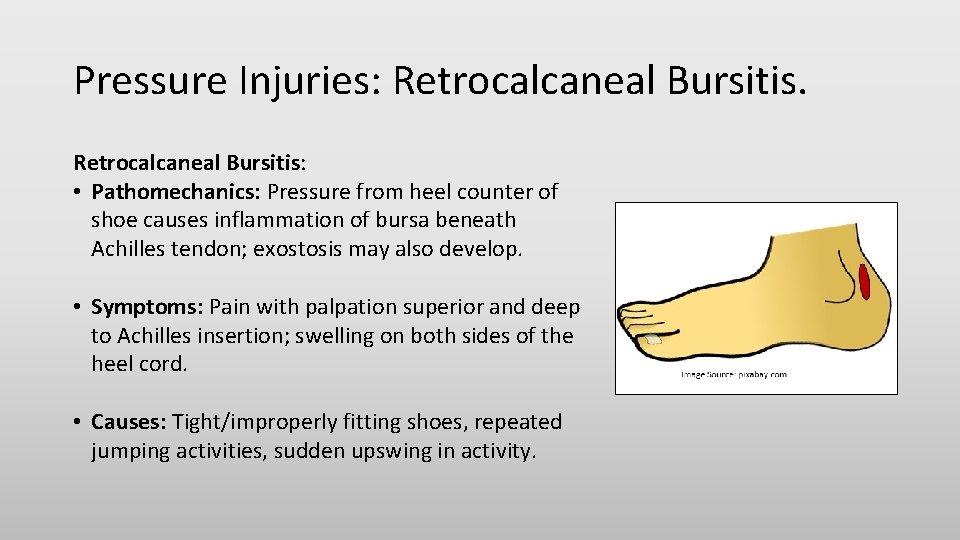
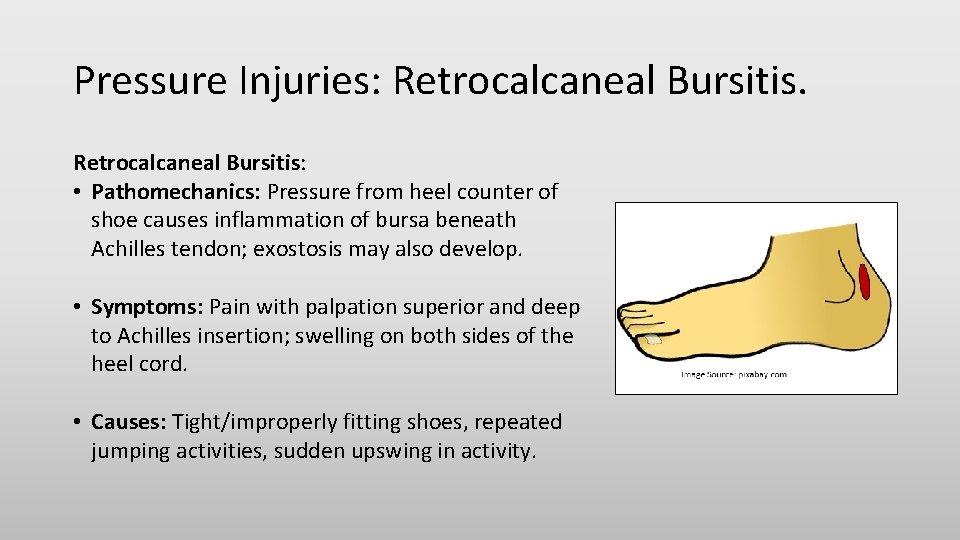
Pressure Injuries: Retrocalcaneal Bursitis: • Pathomechanics: Pressure from heel counter of shoe causes inflammation of bursa beneath Achilles tendon; exostosis may also develop. • Symptoms: Pain with palpation superior and deep to Achilles insertion; swelling on both sides of the heel cord. • Causes: Tight/improperly fitting shoes, repeated jumping activities, sudden upswing in activity.
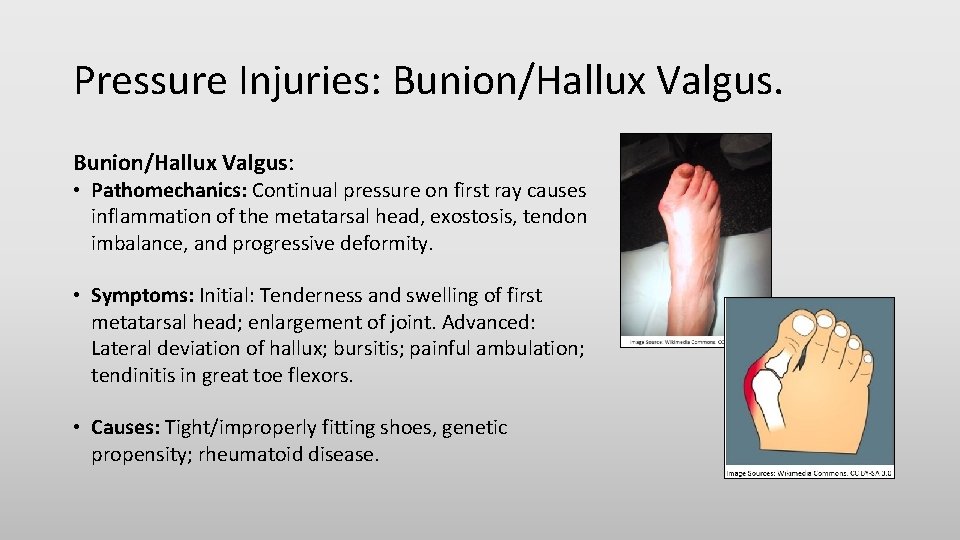
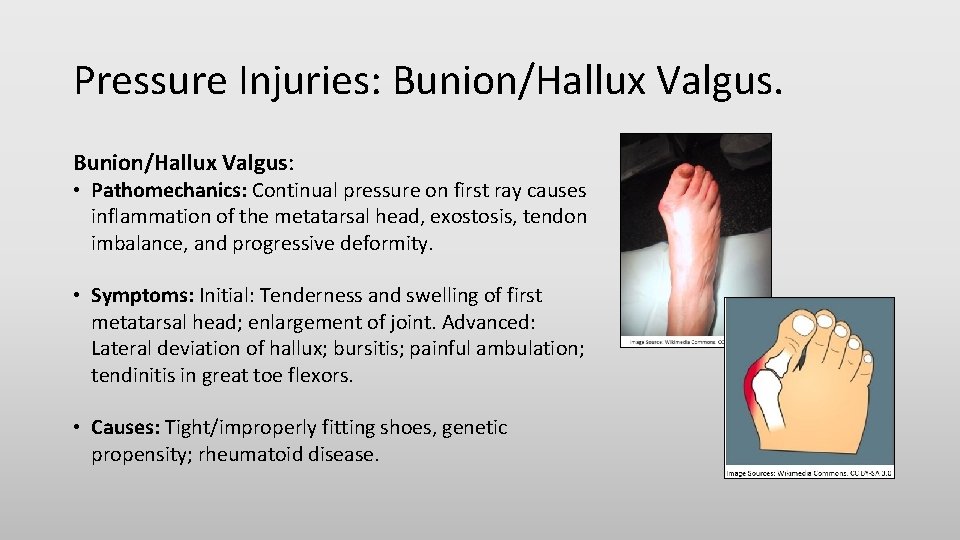
Pressure Injuries: Bunion/Hallux Valgus: • Pathomechanics: Continual pressure on first ray causes inflammation of the metatarsal head, exostosis, tendon imbalance, and progressive deformity. • Symptoms: Initial: Tenderness and swelling of first metatarsal head; enlargement of joint. Advanced: Lateral deviation of hallux; bursitis; painful ambulation; tendinitis in great toe flexors. • Causes: Tight/improperly fitting shoes, genetic propensity; rheumatoid disease.
Pressure Injuries: Corns and Calluses: Thick, hardened layers of skin that develop when the skin tries to protect itself against friction and pressure. For most people, simply eliminating the source of friction or pressure makes corns and calluses disappear. People with diabetes are at greater risk of complications from corns and calluses. Corns are smaller than calluses and have a hard center surrounded by inflamed skin. Corns tend to develop on parts of the feet that don’t bear weight, such as the tops and sides of the toes and even between the toes. They can also be found in weight-bearing areas. Corns can be painful when pressed. Calluses are rarely painful. They usually develop on the soles of the feet, especially under the heels or balls, on the palms, or on the knees. Calluses vary in size and shape, and are often larger than corns.
Foot Pathologies, continued. Midfoot Pathologies: • • • Pes Planus Foot (Acquired); Pes Cavus Foot; Sesamoiditis; Morton’s Neuroma; Metatarsalgia.
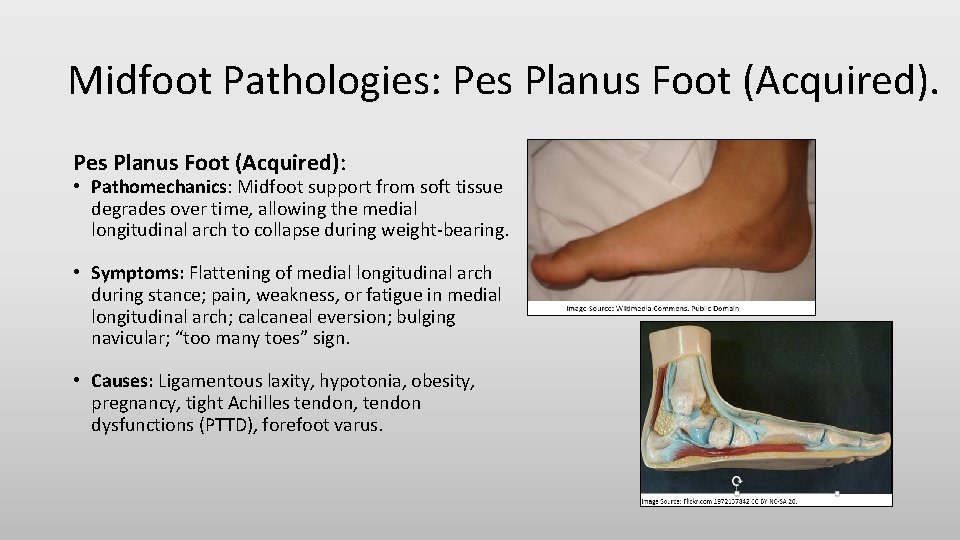
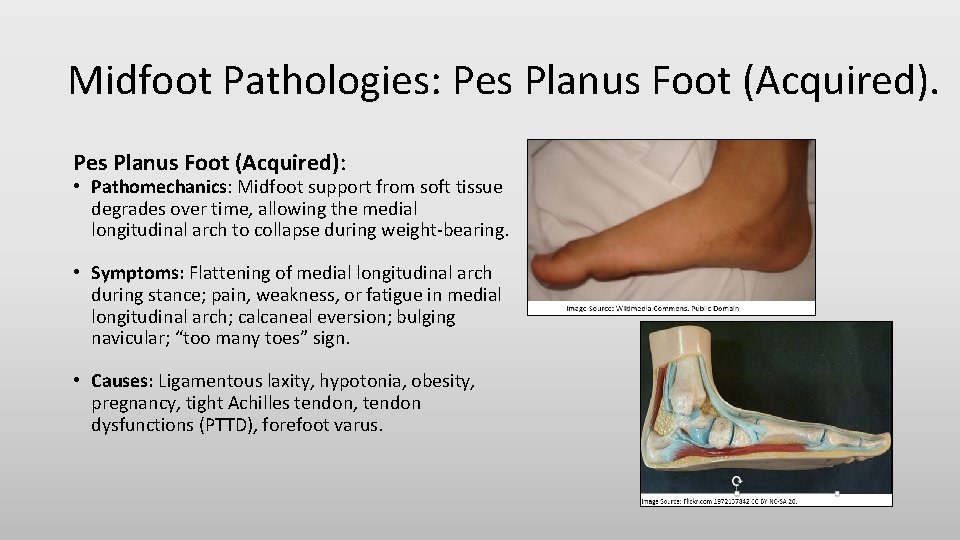
Midfoot Pathologies: Pes Planus Foot (Acquired): • Pathomechanics: Midfoot support from soft tissue degrades over time, allowing the medial longitudinal arch to collapse during weight-bearing. • Symptoms: Flattening of medial longitudinal arch during stance; pain, weakness, or fatigue in medial longitudinal arch; calcaneal eversion; bulging navicular; “too many toes” sign. • Causes: Ligamentous laxity, hypotonia, obesity, pregnancy, tight Achilles tendon, tendon dysfunctions (PTTD), forefoot varus.
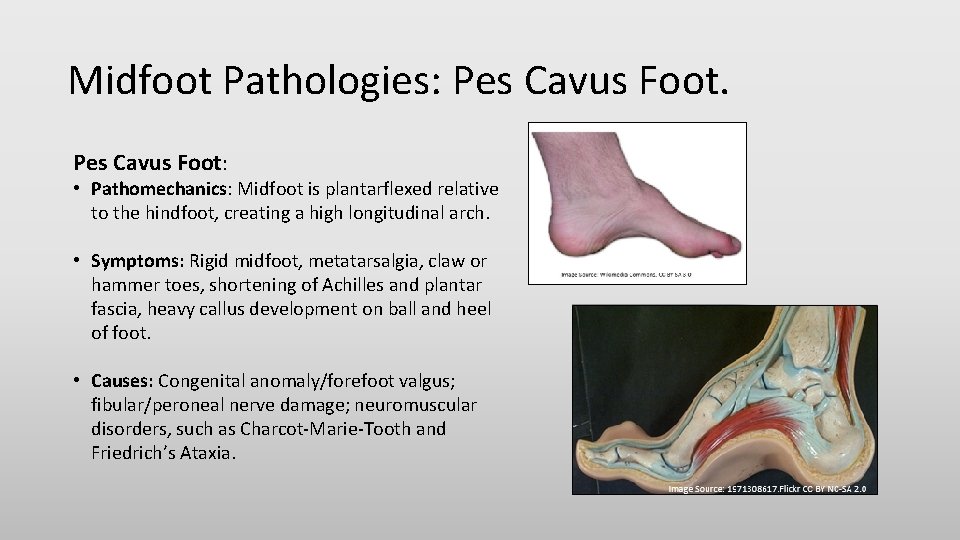
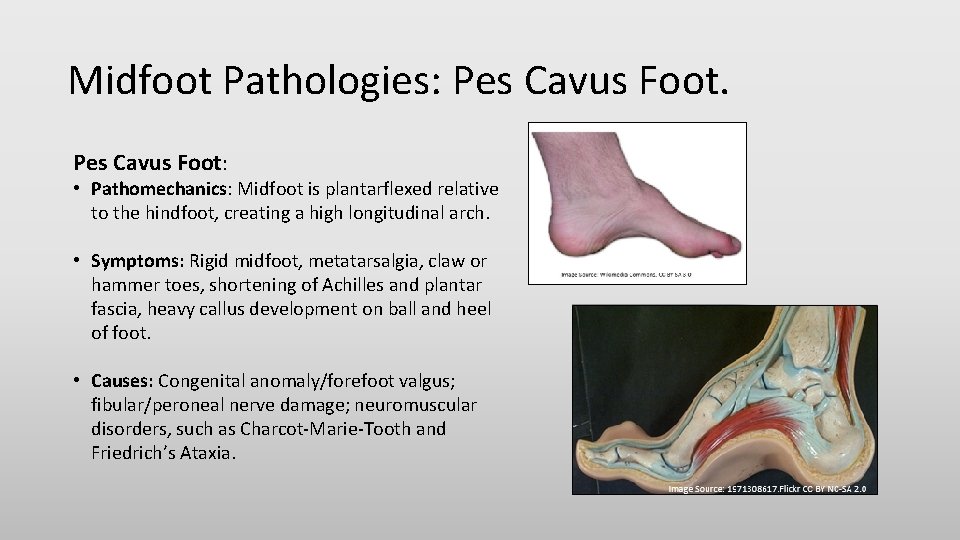
Midfoot Pathologies: Pes Cavus Foot: • Pathomechanics: Midfoot is plantarflexed relative to the hindfoot, creating a high longitudinal arch. • Symptoms: Rigid midfoot, metatarsalgia, claw or hammer toes, shortening of Achilles and plantar fascia, heavy callus development on ball and heel of foot. • Causes: Congenital anomaly/forefoot valgus; fibular/peroneal nerve damage; neuromuscular disorders, such as Charcot-Marie-Tooth and Friedrich’s Ataxia.
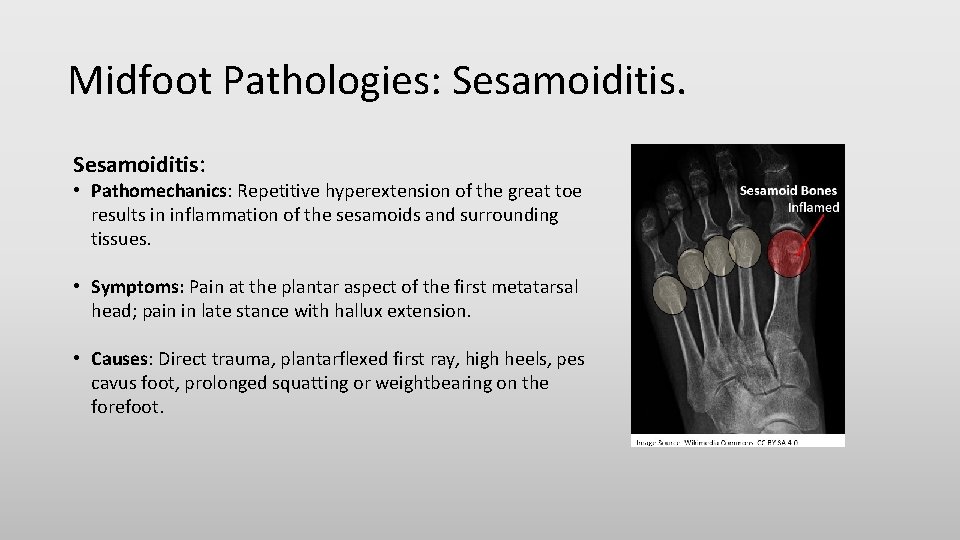
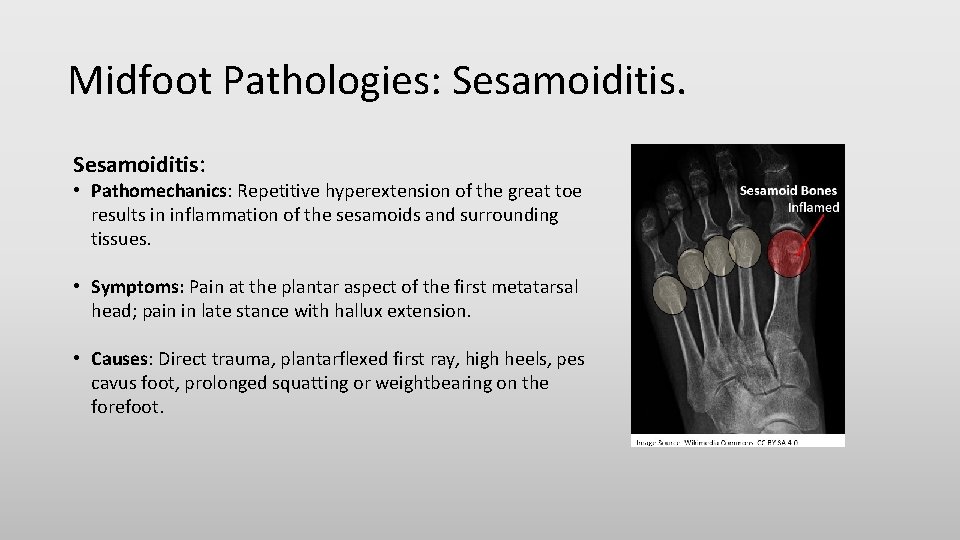
Midfoot Pathologies: Sesamoiditis: • Pathomechanics: Repetitive hyperextension of the great toe results in inflammation of the sesamoids and surrounding tissues. • Symptoms: Pain at the plantar aspect of the first metatarsal head; pain in late stance with hallux extension. • Causes: Direct trauma, plantarflexed first ray, high heels, pes cavus foot, prolonged squatting or weightbearing on the forefoot.
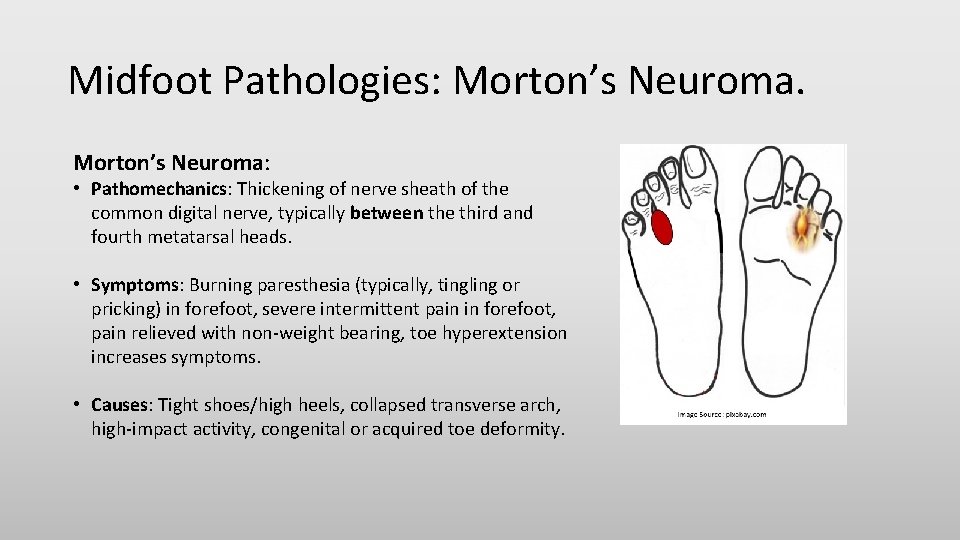
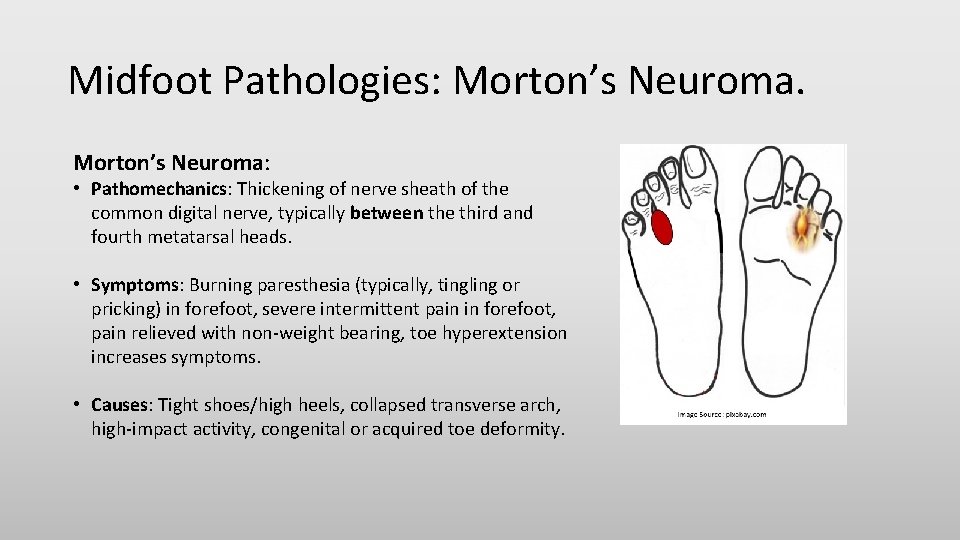
Midfoot Pathologies: Morton’s Neuroma: • Pathomechanics: Thickening of nerve sheath of the common digital nerve, typically between the third and fourth metatarsal heads. • Symptoms: Burning paresthesia (typically, tingling or pricking) in forefoot, severe intermittent pain in forefoot, pain relieved with non-weight bearing, toe hyperextension increases symptoms. • Causes: Tight shoes/high heels, collapsed transverse arch, high-impact activity, congenital or acquired toe deformity.
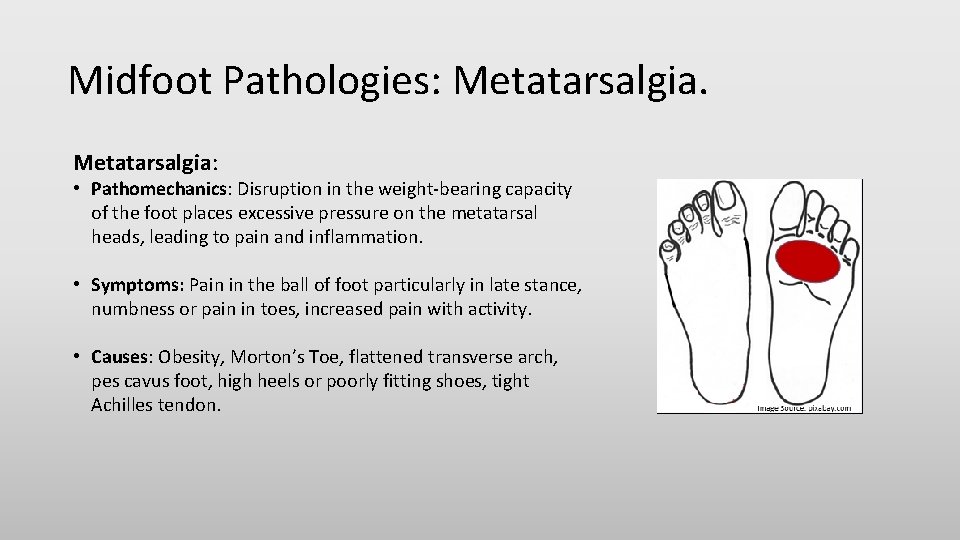
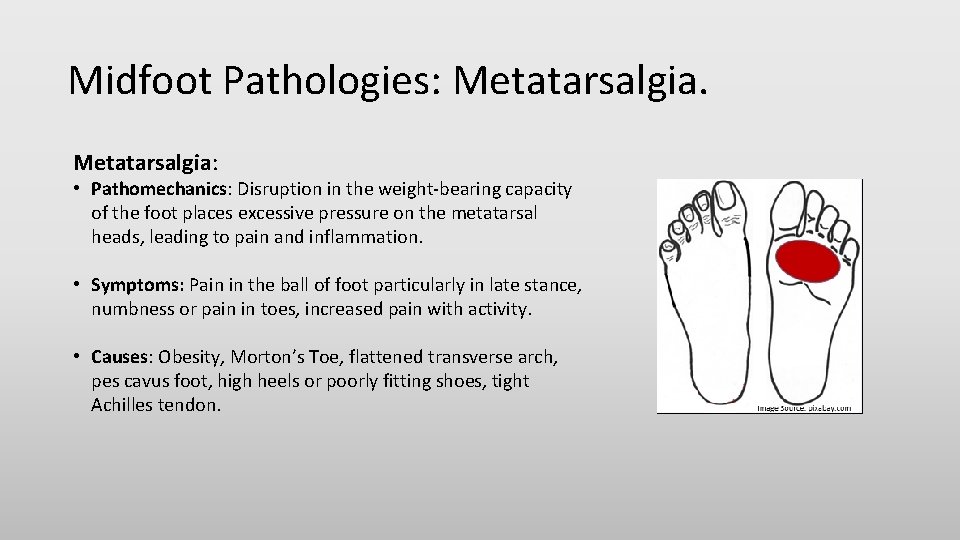
Midfoot Pathologies: Metatarsalgia: • Pathomechanics: Disruption in the weight-bearing capacity of the foot places excessive pressure on the metatarsal heads, leading to pain and inflammation. • Symptoms: Pain in the ball of foot particularly in late stance, numbness or pain in toes, increased pain with activity. • Causes: Obesity, Morton’s Toe, flattened transverse arch, pes cavus foot, high heels or poorly fitting shoes, tight Achilles tendon.
Foot Pathologies. Toe Pathologies: • Hallux Limitus/Rigidus; • Morton’s Toe; • Mallet, Hammer, and Claw Toes.
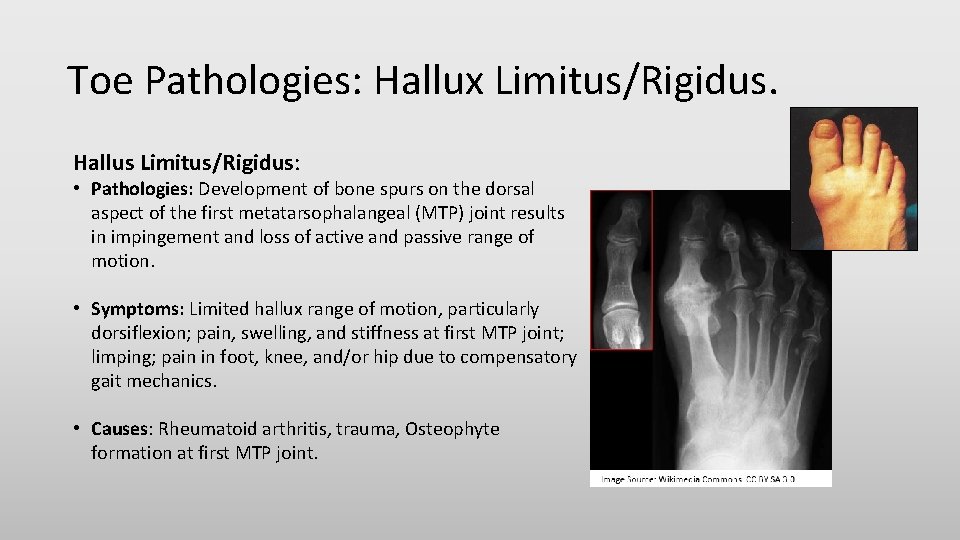
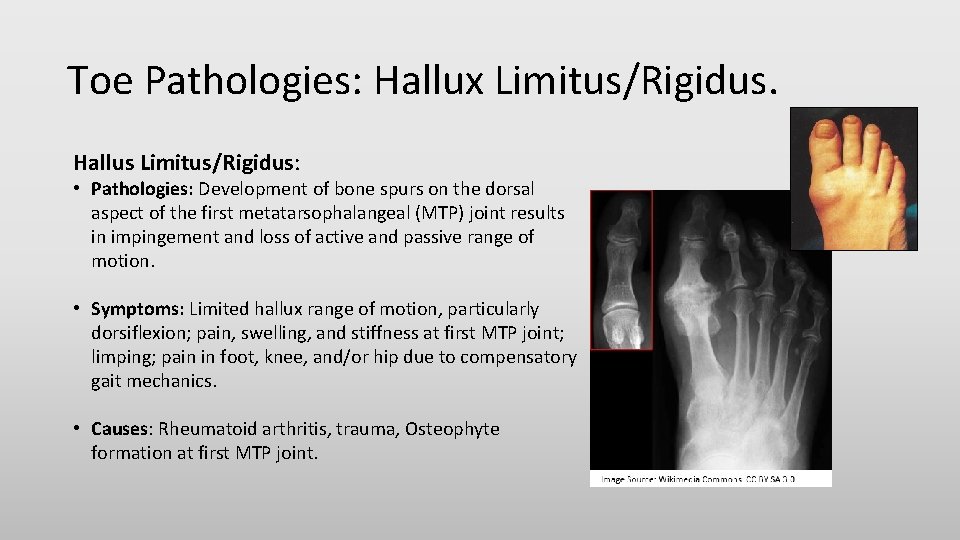
Toe Pathologies: Hallux Limitus/Rigidus. Hallus Limitus/Rigidus: • Pathologies: Development of bone spurs on the dorsal aspect of the first metatarsophalangeal (MTP) joint results in impingement and loss of active and passive range of motion. • Symptoms: Limited hallux range of motion, particularly dorsiflexion; pain, swelling, and stiffness at first MTP joint; limping; pain in foot, knee, and/or hip due to compensatory gait mechanics. • Causes: Rheumatoid arthritis, trauma, Osteophyte formation at first MTP joint.
Toe Pathologies: Hallux Limitus/Rigidus: Video. Watch this video to learn more about Hallux Rigidus. Click on the following video title: Hallux Rigidus: Causes, Diagnosis, and Treatment.
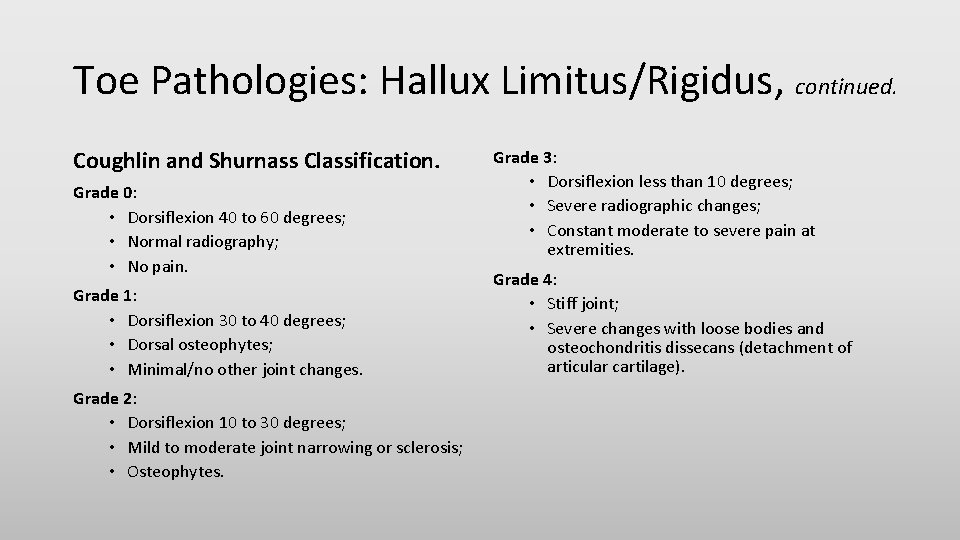
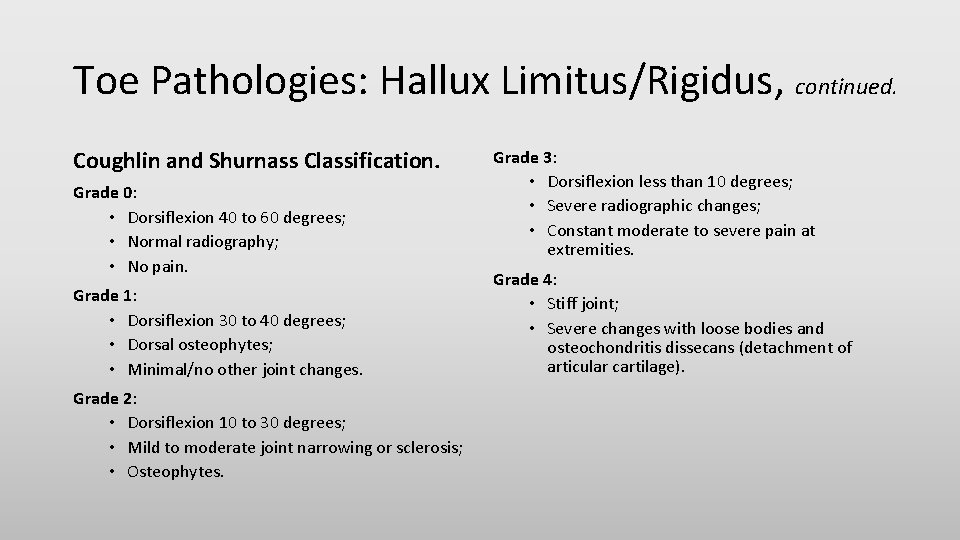
Toe Pathologies: Hallux Limitus/Rigidus, continued. Coughlin and Shurnass Classification. Grade 0: • Dorsiflexion 40 to 60 degrees; • Normal radiography; • No pain. Grade 1: • Dorsiflexion 30 to 40 degrees; • Dorsal osteophytes; • Minimal/no other joint changes. Grade 2: • Dorsiflexion 10 to 30 degrees; • Mild to moderate joint narrowing or sclerosis; • Osteophytes. Grade 3: • Dorsiflexion less than 10 degrees; • Severe radiographic changes; • Constant moderate to severe pain at extremities. Grade 4: • Stiff joint; • Severe changes with loose bodies and osteochondritis dissecans (detachment of articular cartilage).
Toe Pathologies: Morton’s Toe: • Pathomechanics: Excessive weight-bearing on the second ray in late stance leads to pain in the metatarsal heads. • Symptoms: Pain during and after activity, point tenderness on second metatarsal head, callus development under second metatarsal head. • Causes: Hallux hypoplasia, hypermobile first ray.
Toe Pathologies: Mallet, Hammer, and Claw Toe: Tight shoes are the most common cause of these toe problems. Wearing tight shoes can cause the toe muscles to get out of balance. If a shoe forces a toe to stay in a bent position for too long, the muscles tighten and the tendons shorten, or contract. Over time, the toe muscles can’t straighten the toe. Symptoms: Pain, toes rub against footwear; calluses or corns may appear where a bent toe presses against another toe or where a toe’s tip touches the ground. • MALLET TOE: Flexion contracture of the distal interphalangeal (DIP) joint. • HAMMER TOE: Flexion contracture of the proximal interphalangeal (PIP) joint. • CLAW TOE: Flexion contracture of the PIP/DIP joints with hyperextension at the metatarsophalangeal (MTP) joint. Watch this video to learn more about Mallet, Hammer, and Claw Toe. Click on the following video title: Hammer Toe Surgery Explained Podiatry Claw Toe Mallet Toe.
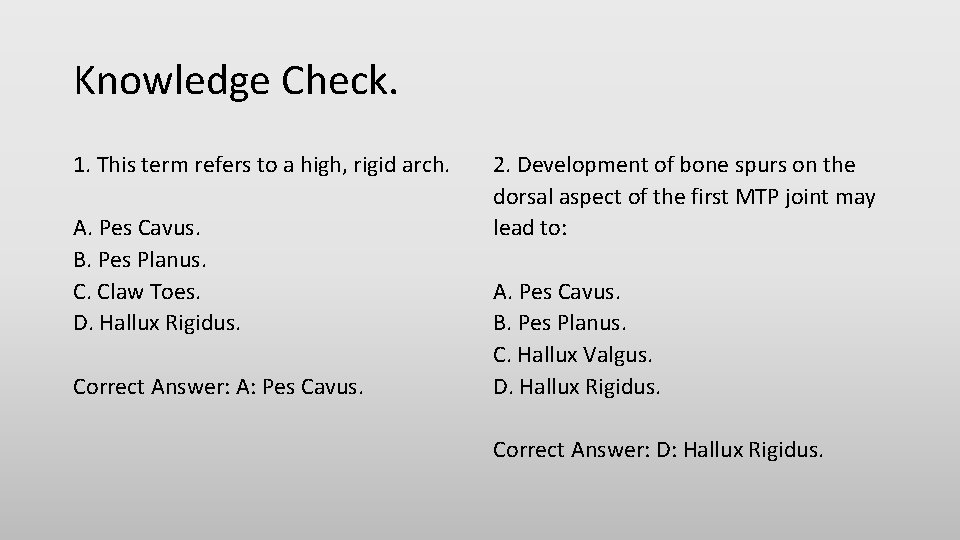
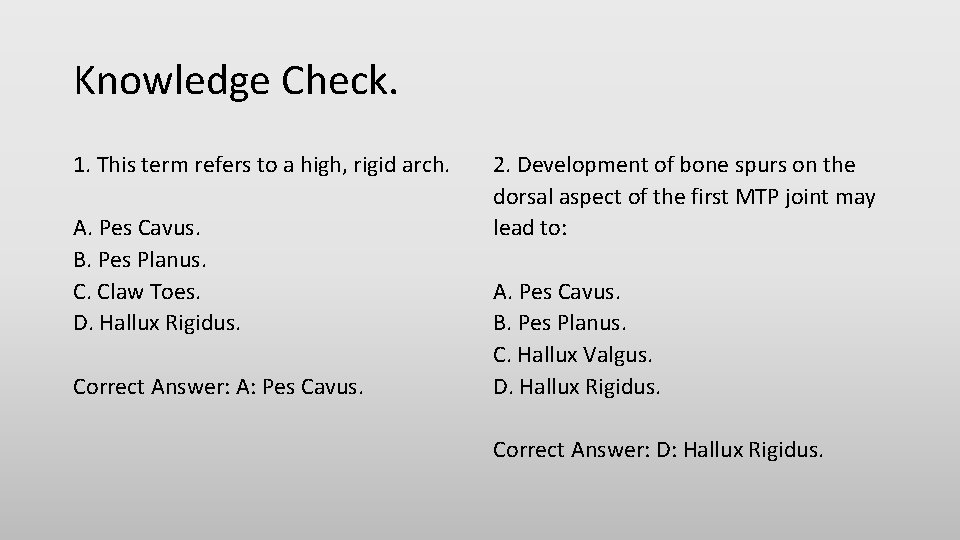
Knowledge Check. 1. This term refers to a high, rigid arch. A. Pes Cavus. B. Pes Planus. C. Claw Toes. D. Hallux Rigidus. Correct Answer: A: Pes Cavus. 2. Development of bone spurs on the dorsal aspect of the first MTP joint may lead to: A. Pes Cavus. B. Pes Planus. C. Hallux Valgus. D. Hallux Rigidus. Correct Answer: D: Hallux Rigidus.
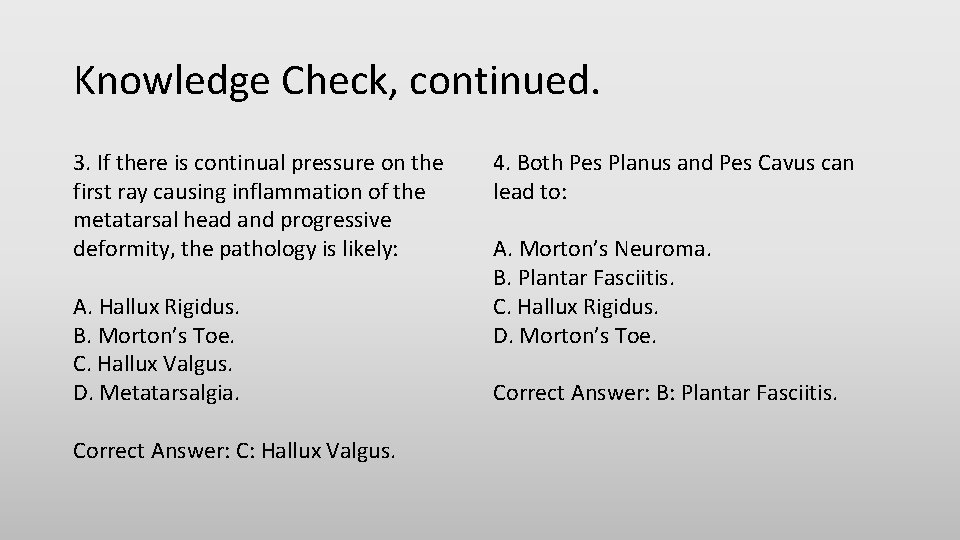
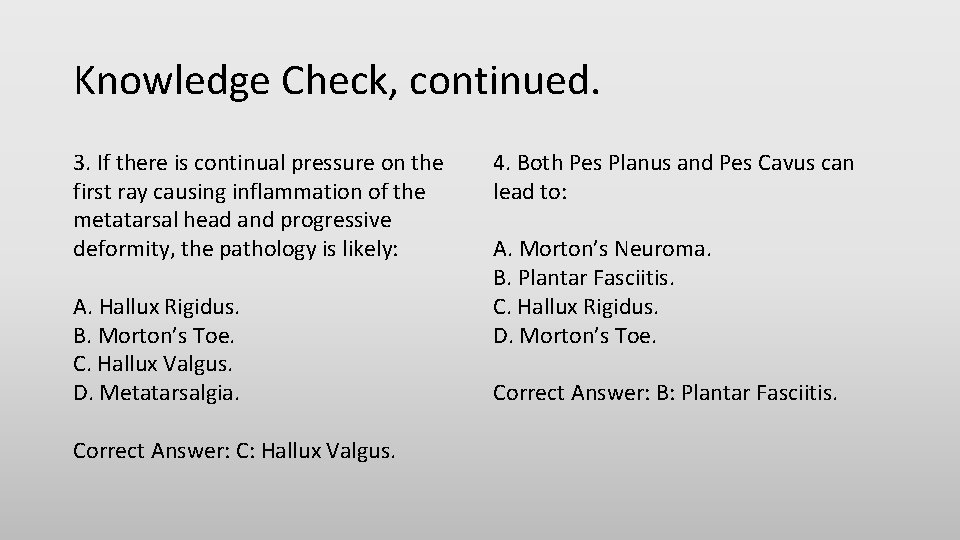
Knowledge Check, continued. 3. If there is continual pressure on the first ray causing inflammation of the metatarsal head and progressive deformity, the pathology is likely: A. Hallux Rigidus. B. Morton’s Toe. C. Hallux Valgus. D. Metatarsalgia. Correct Answer: C: Hallux Valgus. 4. Both Pes Planus and Pes Cavus can lead to: A. Morton’s Neuroma. B. Plantar Fasciitis. C. Hallux Rigidus. D. Morton’s Toe. Correct Answer: B: Plantar Fasciitis.
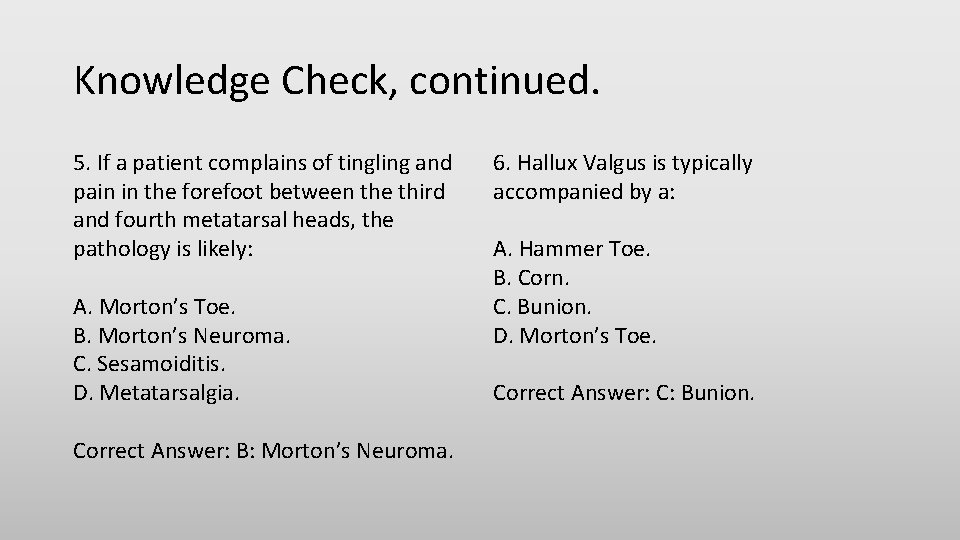
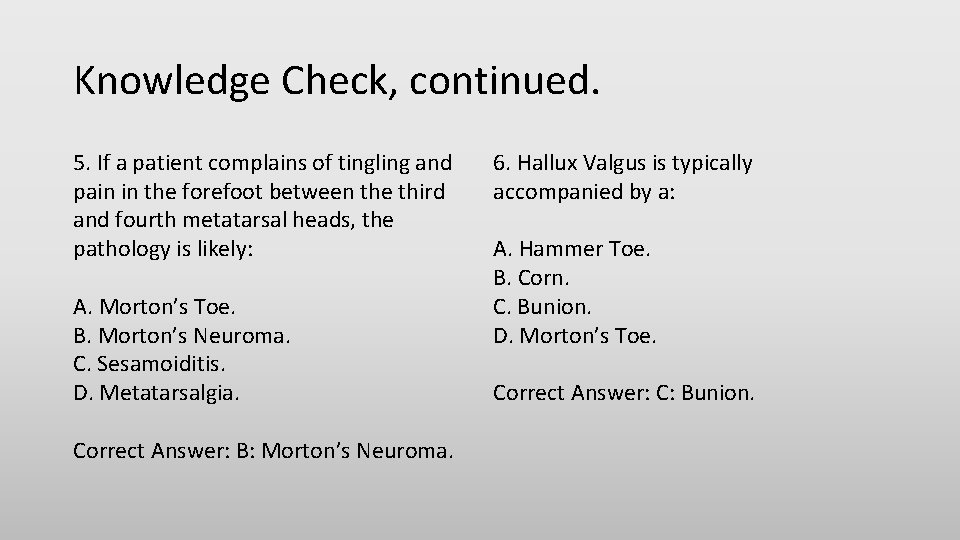
Knowledge Check, continued. 5. If a patient complains of tingling and pain in the forefoot between the third and fourth metatarsal heads, the pathology is likely: A. Morton’s Toe. B. Morton’s Neuroma. C. Sesamoiditis. D. Metatarsalgia. Correct Answer: B: Morton’s Neuroma. 6. Hallux Valgus is typically accompanied by a: A. Hammer Toe. B. Corn. C. Bunion. D. Morton’s Toe. Correct Answer: C: Bunion.
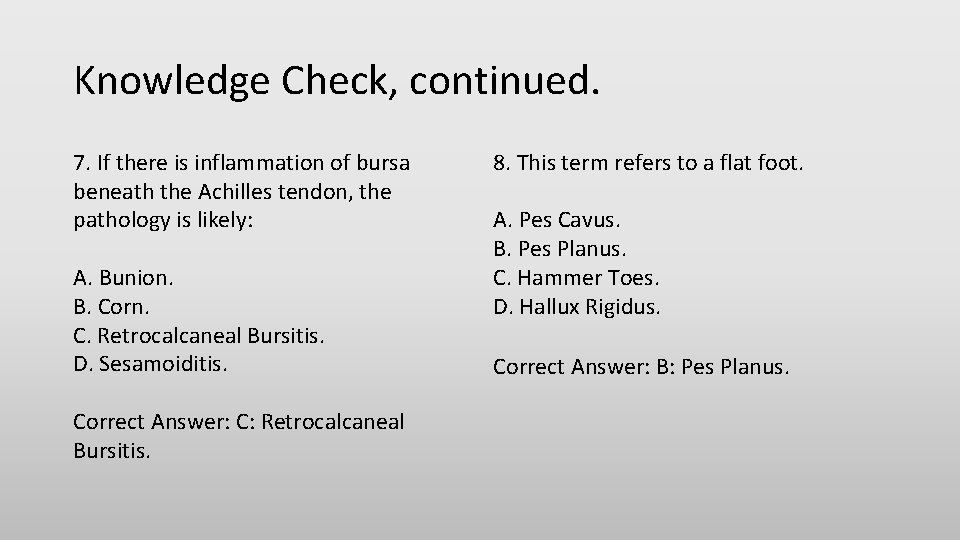
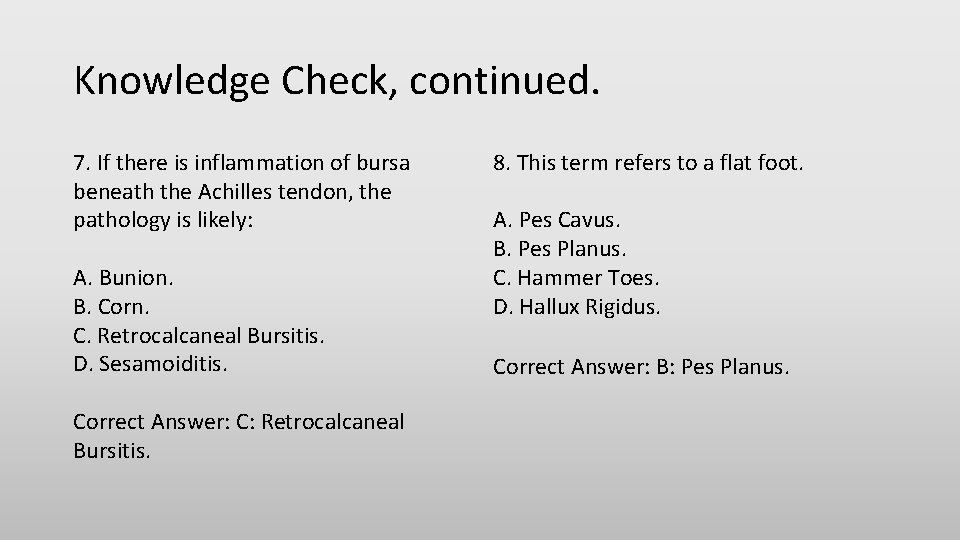
Knowledge Check, continued. 7. If there is inflammation of bursa beneath the Achilles tendon, the pathology is likely: A. Bunion. B. Corn. C. Retrocalcaneal Bursitis. D. Sesamoiditis. Correct Answer: C: Retrocalcaneal Bursitis. 8. This term refers to a flat foot. A. Pes Cavus. B. Pes Planus. C. Hammer Toes. D. Hallux Rigidus. Correct Answer: B: Pes Planus.
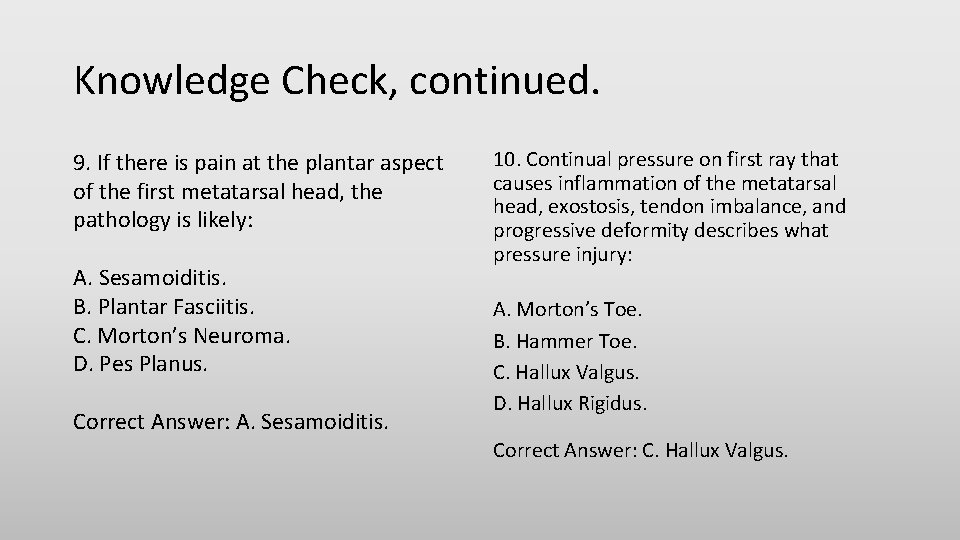
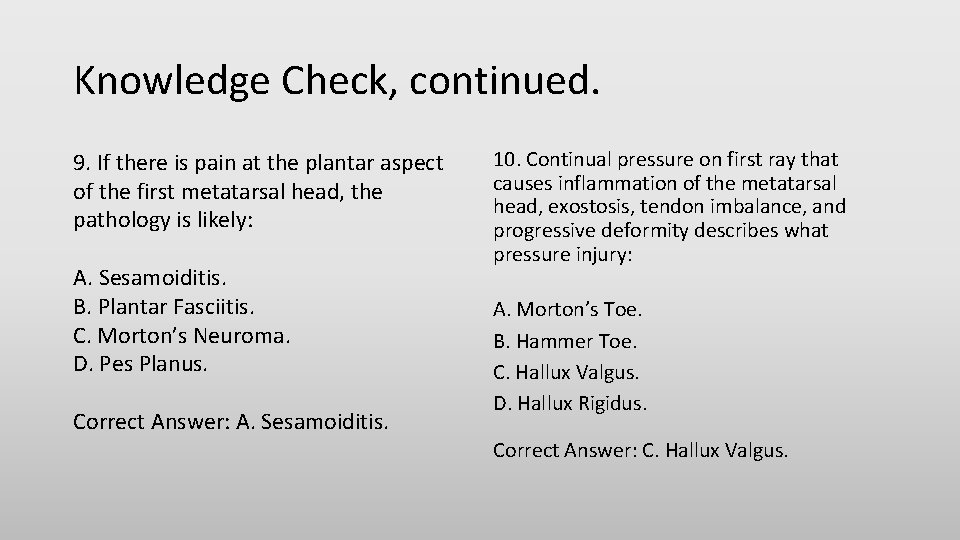
Knowledge Check, continued. 9. If there is pain at the plantar aspect of the first metatarsal head, the pathology is likely: A. Sesamoiditis. B. Plantar Fasciitis. C. Morton’s Neuroma. D. Pes Planus. Correct Answer: A. Sesamoiditis. 10. Continual pressure on first ray that causes inflammation of the metatarsal head, exostosis, tendon imbalance, and progressive deformity describes what pressure injury: A. Morton’s Toe. B. Hammer Toe. C. Hallux Valgus. D. Hallux Rigidus. Correct Answer: C. Hallux Valgus.
Knowledge Check, continued. 11. (Blank) is caused by pes planus/pes cavus foot; long periods of standing, walking, or running; obesity; poorly fitted or worn-out shoes; tight Achilles tendon; hyperpronation. A. Metatarsalgia. B. Sesamoiditis. C. Plantar Fasciitis. D. Morton’s Neuroma. Correct Answer: C. Plantar Fasciitis. 12. A round, persistent wound on the plantar surface of the foot; painless—may or may not bleed or seep, and may involve deep tissues, such as tendons and bones, best describes: A. Metatarsalgia. B. Retrocalcaneal Bursitis. C. Plantar Fasciitis. D. Plantar Ulcer. Correct Answer: D. Plantar Ulcer.
Knowledge Check, continued. 13. Repeated stress on plantar fascia, highimpact activities, and/or a tight Achilles tendon cause: A. Pes Cavus. B. Plantar Ulcer. C. Morton’s Neuroma. D. Heel Spur. Correct Answer: D. Heel Spur. 14. Midfoot support from soft tissue degrades over time, allowing the medial longitudinal arch to collapse during weightbearing describes what midfoot pathology: A. Heel Spurs. B. Retrocalcaneal Bursitis. C. Morton’s Neuroma. D. Pes Planus. Correct Answer: D. Pes Planus.
Knowledge Check, continued. 15. When the midfoot is plantarflexed relative to the hindfoot, creating a high longitudinal arch, the midfoot pathology is: A. Heel Spurs. B. Retrocalcaneal Bursitis. C. Pes Cavus. D. Morton’s Neuroma. Correct Answer: C. Pes Cavus.
Foot Pathologies. This workforce product was funded by a grant awarded by the U. S. Department of Labor’s Employment and Training Administration. The product was created by the grantee and does not necessarily reflect the official position of the U. S. Department of Labor. The U. S. Department of Labor makes no guarantees, warranties, or assurances of any kind, express or implied, with respect to such information, including any information on linked sites and including, but not limited to, accuracy of the information or its completeness, timeliness, usefulness, adequacy, continued availability, or ownership. Produced 2016. HOPE Careers Consortium is a partnership of five institutions of higher education that is building exciting new programs that will provide valuable career education and training in the Orthotics, Prosthetics, and Pedorthics (O&P) sector. The five institutions are: Baker College—Flint, Michigan; Century College—White Bear Lake, Minnesota; Oklahoma State University Institute of Technology— Okmulgee, Oklahoma; Spokane Falls Community College—Spokane, Washington; and St. Petersburg College—St. Petersburg, Florida. Although the authoring institution of this educational resource has made every effort to ensure that the information presented is correct, the institution assumes no liability to any party for any loss, damage, or disruption caused by errors or omissions. Except where otherwise noted (images from Pixabay and Wikimedia), this work by Oklahoma State University Institute of Technology (OSUIT) is licensed under the Creative Commons Attribution 4. 0 International License. To view a copy of this license, click on the following link: Creative Commons Licenses 4. 0.