Food borne disease Diarrheal diseases Diarrhea The passage
Food borne disease Diarrheal diseases
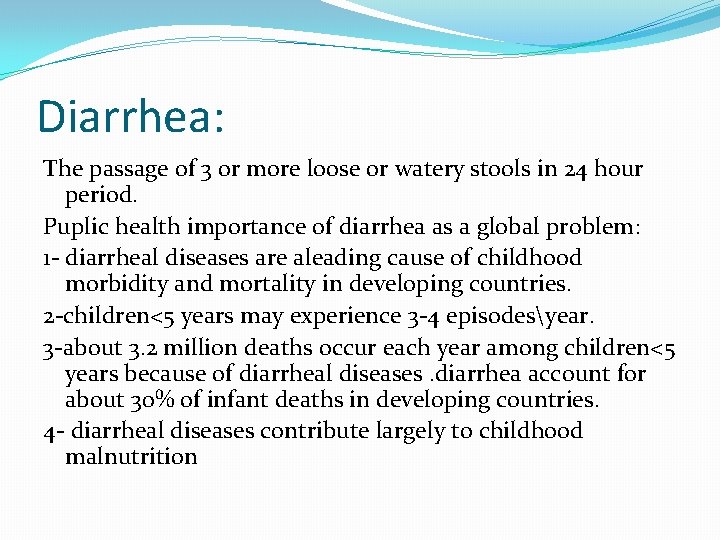
Diarrhea: The passage of 3 or more loose or watery stools in 24 hour period. Puplic health importance of diarrhea as a global problem: 1 - diarrheal diseases are aleading cause of childhood morbidity and mortality in developing countries. 2 -children<5 years may experience 3 -4 episodesyear. 3 -about 3. 2 million deaths occur each year among children<5 years because of diarrheal diseases. diarrhea account for about 30% of infant deaths in developing countries. 4 - diarrheal diseases contribute largely to childhood malnutrition
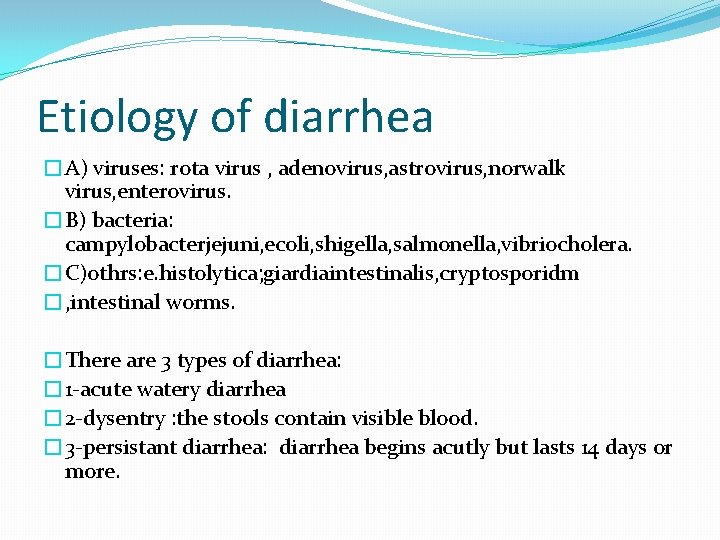
Etiology of diarrhea �A) viruses: rota virus , adenovirus, astrovirus, norwalk virus, enterovirus. �B) bacteria: campylobacterjejuni, ecoli, shigella, salmonella, vibriocholera. �C)othrs: e. histolytica; giardiaintestinalis, cryptosporidm �, intestinal worms. �There are 3 types of diarrhea: � 1 -acute watery diarrhea � 2 -dysentry : the stools contain visible blood. � 3 -persistant diarrhea: diarrhea begins acutly but lasts 14 days or more.
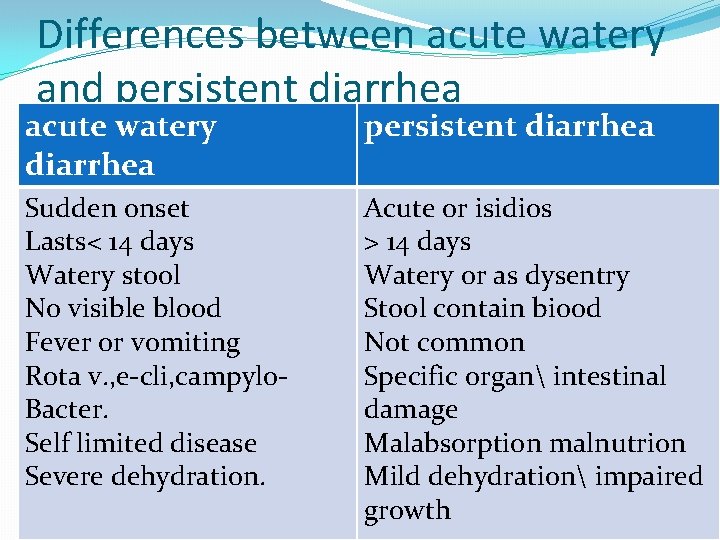
Differences between acute watery and persistent diarrhea acute watery diarrhea persistent diarrhea Sudden onset Lasts< 14 days Watery stool No visible blood Fever or vomiting Rota v. , e-cli, campylo. Bacter. Self limited disease Severe dehydration. Acute or isidios > 14 days Watery or as dysentry Stool contain biood Not common Specific organ intestinal damage Malabsorption malnutrion Mild dehydration impaired growth
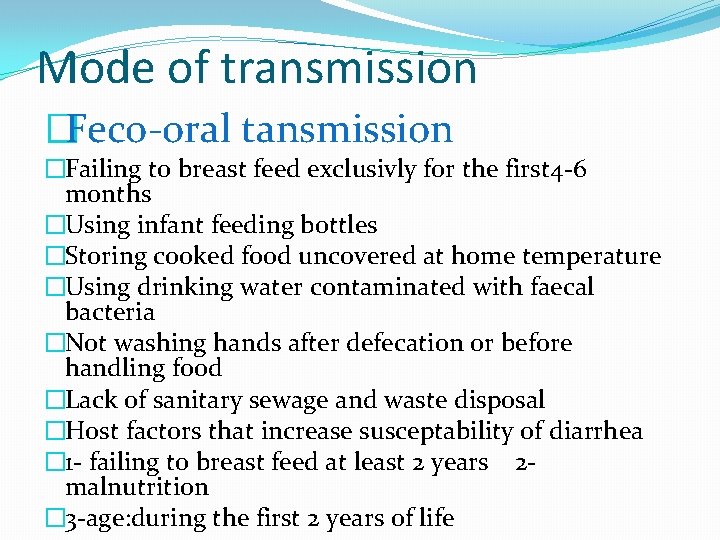
Mode of transmission �Feco-oral tansmission �Failing to breast feed exclusivly for the first 4 -6 months �Using infant feeding bottles �Storing cooked food uncovered at home temperature �Using drinking water contaminated with faecal bacteria �Not washing hands after defecation or before handling food �Lack of sanitary sewage and waste disposal �Host factors that increase susceptability of diarrhea � 1 - failing to breast feed at least 2 years 2 malnutrition � 3 -age: during the first 2 years of life
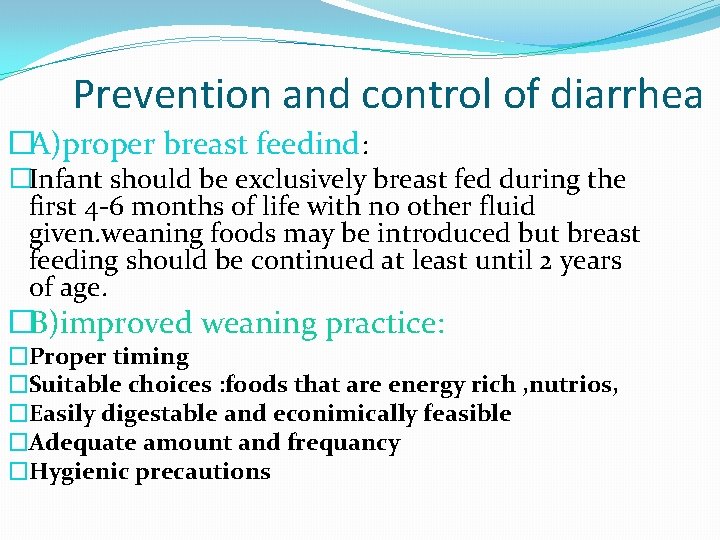
Prevention and control of diarrhea �A)proper breast feedind: �Infant should be exclusively breast fed during the first 4 -6 months of life with no other fluid given. weaning foods may be introduced but breast feeding should be continued at least until 2 years of age. �B)improved weaning practice: �Proper timing �Suitable choices : foods that are energy rich , nutrios, �Easily digestable and econimically feasible �Adequate amount and frequancy �Hygienic precautions
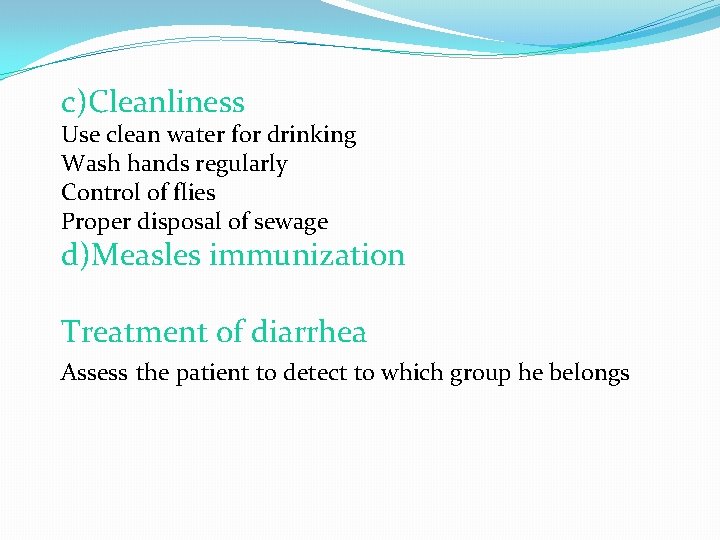
c)Cleanliness Use clean water for drinking Wash hands regularly Control of flies Proper disposal of sewage d)Measles immunization Treatment of diarrhea Assess the patient to detect to which group he belongs
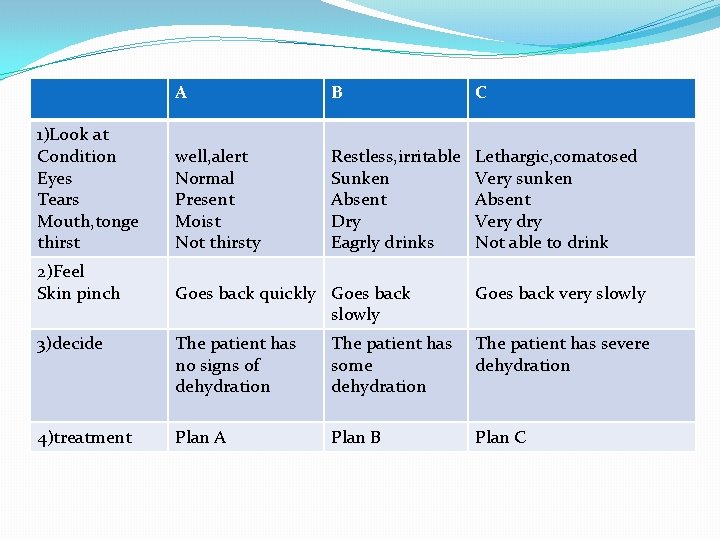
1)Look at Condition Eyes Tears Mouth, tonge thirst 2)Feel Skin pinch A B C well, alert Normal Present Moist Not thirsty Restless, irritable Sunken Absent Dry Eagrly drinks Lethargic, comatosed Very sunken Absent Very dry Not able to drink Goes back quickly Goes back slowly Goes back very slowly 3)decide The patient has no signs of dehydration The patient has some dehydration The patient has severe dehydration 4)treatment Plan A Plan B Plan C

1 - plan A (treatment of diarrhea at home) a) Give the child more fluids than usual as soon as diarrhea start to prevent dehydration with continous breast feeding this fluid as rice water , tea without sugar, soup, youghurt , ORS b)give the child plenty of nutrious food to prevent malnutrition c)Take the child to the health unit if : 1 -child does not get better in 3 days 2 - passage of many water stool 3 -blood in stool 4 -repeated v 0 miting 5 -failure to eat or drink normally 6 -fever
2 -Plan B (management of patient with some dehydration) Children can be treated in a rehydration center A)Estimate the amount of ORS solution to be given during the first 4 hours for initial rehydration according to the weight of the baby b)Show the mother how to give ORS solution c)Continue brest feeding and give other fluid required d)Monitor treatment and manage any difficulty during oral rehydration e)Assess the child periodically untill rehydration is completed F)Give instruction for treatment at home after rehydration is
3 - Plan C (management of patients with severe dehydration) Children with sever dehydration should be treated urgently to avoid death from hypovolemic shock The treatment should be undertaken in hospital by experienced personnel The main tasks of plan C are as follow: 1 -give appropriate amount of Ivfluids 2 -shift to plan B or plan A when the child is no longer severly dehydrated
Indication of Iv fluid therapy 1 - severe dehydration 2 -Failure of ORS 3 -paralytic ileus or sever abdominal distention Indication of antimicrobial therapy in diarrhea 1 -diarrhea caused by specific pathogens such as cholera, shigella and amaebiasis 2 -associated bacterial infections as pneumonia or otitis media
Typhoid and paratyphoid fevers
Size of the problem and public health importance Worldwide the annual incidence is about 16 million cases with about 600000 deaths In Egypt , the incidence rate is 50100000 Agents : salmonella group They are strong resistant organisms, they can live outside the body particularly in milk , shellfish and Water. they can survive in the frozen condition for up to 1 year. Chlorinated Water and pasteurization of milk can destroy it. Salmonella have the following antigens: O antigen(body antigen) H antigen (flagellar antigen) Vi antigen
Reservoir : humans case and carrier Source of infection : faeces and urine of cases and carriers Mode of transmission : fecal oral route Incubation period : 1 -3 weeks for typhoid 1 -10 days for paratyphoid Host factors : Age : any age specially < 15 years sex : male to female ratio is 3 : 2 seasonal : all over the year with certain seasonal effect. Its peak in August susceptibility : general , common in preschool and school children (an attack gives a specific immunity for about 5 years ) Period of communicability : as long as bacilli appear in the excreta of the patient or chronic carrier
Diagnosis : Clinical manifestations : Stepladder fever for 3 -4 weeks constipation Relative bradycardia marked constitutional Headache symptoms Intestinal hemorrhage in late untreated cases Investigations : 1 st week : blood culture 2 nd week : Widal test 3 rd week : stool specimens Prevention : Cutting the link between the agent and susceptible host through the environment does prevention.
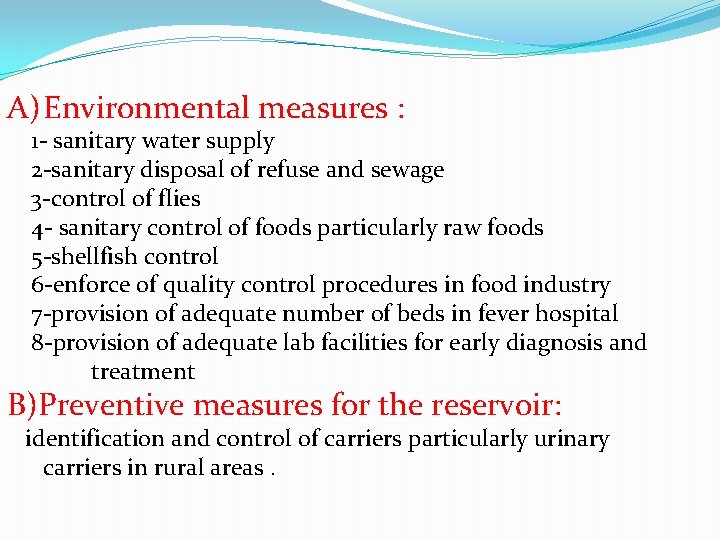
A) Environmental measures : 1 - sanitary water supply 2 -sanitary disposal of refuse and sewage 3 -control of flies 4 - sanitary control of foods particularly raw foods 5 -shellfish control 6 -enforce of quality control procedures in food industry 7 -provision of adequate number of beds in fever hospital 8 -provision of adequate lab facilities for early diagnosis and treatment B)Preventive measures for the reservoir: identification and control of carriers particularly urinary carriers in rural areas.
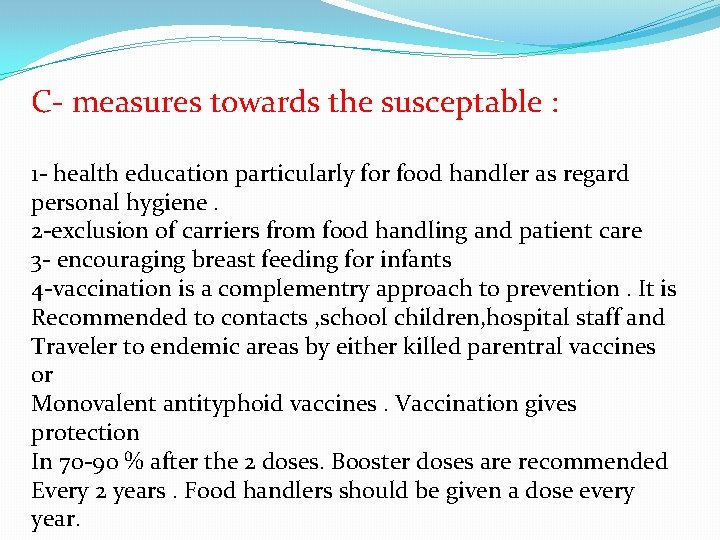
C- measures towards the susceptable : 1 - health education particularly for food handler as regard personal hygiene. 2 -exclusion of carriers from food handling and patient care 3 - encouraging breast feeding for infants 4 -vaccination is a complementry approach to prevention. It is Recommended to contacts , school children, hospital staff and Traveler to endemic areas by either killed parentral vaccines or Monovalent antityphoid vaccines. Vaccination gives protection In 70 -90 % after the 2 doses. Booster doses are recommended Every 2 years. Food handlers should be given a dose every year.
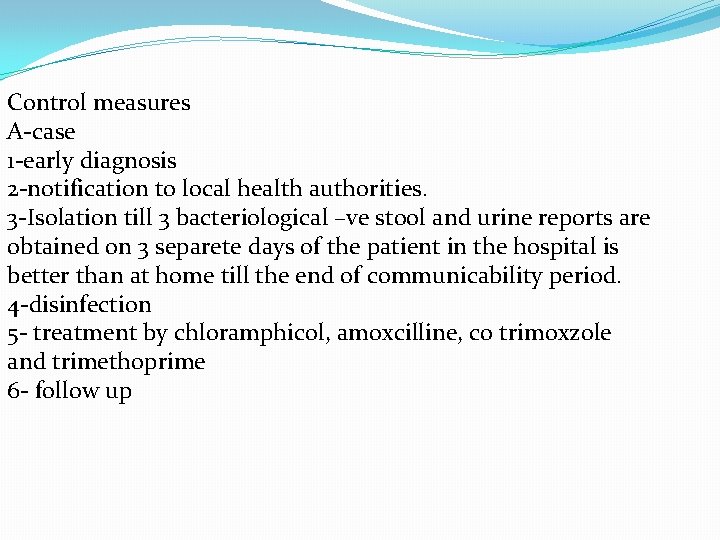
Control measures A-case 1 -early diagnosis 2 -notification to local health authorities. 3 -Isolation till 3 bacteriological –ve stool and urine reports are obtained on 3 separete days of the patient in the hospital is better than at home till the end of communicability period. 4 -disinfection 5 - treatment by chloramphicol, amoxcilline, co trimoxzole and trimethoprime 6 - follow up
Poliomylitis
It is an acute viral infection with severity ranging from inapparent infection to a non paralytic febrile illness and possible death Agent : Polio viruses are members of entero viruses Reservoir : only man Modes of transmission : Feco-oral transmission : Host factors : Age: 6 months – 5 years Susceptability: general Immunity : is type specific and of life long immunity Period of communicability: cases are more infectious during the first days after onset cf symptoms Prevention: the main preventive measure is vaccination Vaccination: 3 main types 1 -Inactivated polio virus vaccine 2 -live oral polio vaccine 3 -enhanced IPV
Global polio eradication Objectives of global polio eradication are: 1 -to interrupt transmission of wild polio virus as soon as possible 2 -to achieve certification of global polio eradication 3 -to contribute to health systems development and strengthening routine immunization and surveillance for communicable diseases in a systematic way. Strategies There are 4 core strategies to stop transmission of wild polio virus 1 -high infant immunization coverage with 4 doses of oral polio vaccine (OPV)in the 1 st year of life 2 -supplementary doses of OPV to all children under 5 years of age 3 -surveillance for wild polio virus through reporting and laboratory testing of all acute flaccid paralysis cases among children under 15 years of age 4 -targeted campaigns once wild polio virus transmission is limited to a specific focal area
Cholera
Cholera is an acute intestinal infection with watery diarrhea, rapid dehydration, acidosis and collapse. Agent: vibrio cholera Ogroup 1 and El Tor biotypes Resevoir : man case or carrier Mode of transmission : 1 - Ingestion of water contaminated with feces or vomitus of patients. 2 -Food contaminated by feces, soiled hands Incubation period: few hours to 5 days Susceptability : variable , gastric achlorhydria increases risk of disease Period of communicability : for the duration of stool positive stage The carrier state may persist for several months Effective antibiotics , e. g tetracycline , shorten the period of communicability. Chronic biliry infection , is associated with intermittent sheding of
vibrios in stool Clinical picture: watery diarrea , , rapid dehydration, acidosis and collapse Investigations: 1 - stool culture or vomitus 2 -Visualizing characteristic vibrio motility by dark field microscoby Which is inhibited by specific antiserum 3 -Demonstrating a significant rise in titer of antitoxic antibodies, Agglutinating or vibriocidal antibodies. Prevention and control: 1 - preventive measures: -Strict environmental measures -active immunization is of no practical value in epidemic control or in management of contacts of cases 2 - Control Patient : -Report to local health authority.
-Isolation : hospitalization is desirable for severly ill patients But strict isolation is not necessary Quarantine : none -Specific treatment : electrolyte solutions to correct dehydration, acidosis and hypokalemia (either oral or intravenous) and tetracycline -Contacts: -Surveillance of contacts -Chemoprophylaxis with tetracycline -Investigation of contacts and source of infection 3 - Epidemic measures : -provide effective treatment facilities -Assure a safe water supply by chlorination or boiling -Sanitary sewage disposal -Careful supervision of food and drink
-Control flies -Vaccine is inappropriate in epidemic situation 4 -International measures : -Notification of WHO of the first case -International travelers: immunization usually not required
Viral hepatitis
�Agent : hepatitis A �Public health importance : Major health problem in all parts of the world reservoir : human Mode of spread : 1 - faecal oral route 2 - contaminated water 3 - contaminated food and milk 4 - raw vegetables 5 - other route : parenteral (very rare)
�IP: 1 month �Host factor ** age : 5 -14 developing countries adult in developed countries ** susceptibility : general ** communicability : second half of inculpation period
Diagnosis � 1 - asymptomatic � 2 -cholestatic hepatitis : jaundice - +ve serum Ig. M anti HAV � 3 - recurrent hepatitis and fulminating ( rare )
Investigation � 1 - Ig. M (recent infection) � 2 - Ig. G (immunity) � 3 - SGOT (during IP) � 4 - radioimmunoassay – ELISA
Control and prevention �Isolation is not useful because virus is present in stool 2 weeks before appearance of jaundice �General : 1 - personal hygiene 2 -food and milk sanitation 3 -water sanitation 4 - sanitary disposal of sewage
�Specific : 1 - formalin inactivated vaccine 2 - havrix
- Slides: 35