FOCUSED EMERGENCY ULTRASOUND EVALUATION OF THE ABDOMINAL AORTA
FOCUSED EMERGENCY ULTRASOUND: EVALUATION OF THE ABDOMINAL AORTA MARY BETH PHELAN, MD, RDMS DEPARTMENT OF EMERGENCY MEDICINE FOREDTERT MEMORIAL HOSPITAL
Lecture Objectives l Describe clinical role of bedside ultrasound in screening for AAA l Describe the technique of acquiring sonographic images of the aorta l Describe the sonographic appearance of the normal aorta l Describe the sonographic appearance of AAA SAEM 2

Case History A 62 -year-old man comes to the emergency department at 11 PM complaining of left flank pain for approximately 2 hours. He has a history of hypertension. His initial vital signs are: HR 98, RR 24, BP 190/105, Temp 98. 0. SAEM 4
Case History The emergency medicine resident equipped with the latest in emergency medicine ultrasound technology and training, IMMEDIATELY performs an abdominal ultrasound on the patient. This exam reveals the following: SAEM 5

SAEM 6
Case History The patient is taken to the OR after only 30 minutes in the ED. SAEM 7
OVERVIEW l l l l Epidemiology Clinical presentation Anatomy US exam Sonographic anatomy Scanning techniques Pitfalls SAEM 8
Epidemiology l AAA present in 2 -4% of the population > 50 l Incidence increasing l Male > female l 10, 000 deaths/yr l Rupture has a > 80% mortality rate SAEM 9
Epidemiology: Risk Factors l Cardiovascular l Family l Age disease History increases risk 10 -20% > 50 l Smoker SAEM 10
Clinical Perspective Settings in which to perform US in the ED – Abdominal/back/flank pain and hypotension – Stable elderly patient with abdominal or back pain SAEM 11
Clinical Perspective l Rate of expansion variable – 4 -4. 9 cm AAA has a 3. 3% risk of rupture – 5 cm AAA has a 14% risk of rupture – > 5 cm has a 20 -40% risk of rupture SAEM 12
Clinical Perspective l 4 cm or less: annual US examinations l Between l Greater 4 -5 cm: US every 6 months than 5 cm: Elective repair l Mortality rate for elective repair is 5% SAEM 13
Clinical Presentation l Highly variable l Classic triad: – Abdominal/Back pain – Pulsatile mass – Hypotension l Less than 1/3 of patients will have the triad SAEM 14
Clinical Presentation l Diagnosis – A formidable clinical challenge – Notorious for masquerading as renal colic – May be mistaken for: Diverticullitis l GI bleed l MI l Musculoskeletal back pain l SAEM 15
Clinical Presentation l Stable vital signs l Back or flank pain, left side > right l Testicular or leg pain l Hypertension l Mortality rate same as elective repair SAEM 16
Clinical Presentation l Vast majority are retroperitoneal l 10 -30 % intraperitoneal l GI bleeding most often seen in patients with aortic grafts l Mortality 50% SAEM 17
Does this patient have an abdominal aortic aneurysm? LEDERLE, JAMA 99 l 2 groups l Sensitivity of examination for ruptured AAA l Sensitivity of exam with increasing size of AAA l CONCLUSION: Cannot be relied on to exclude AAA SAEM 18
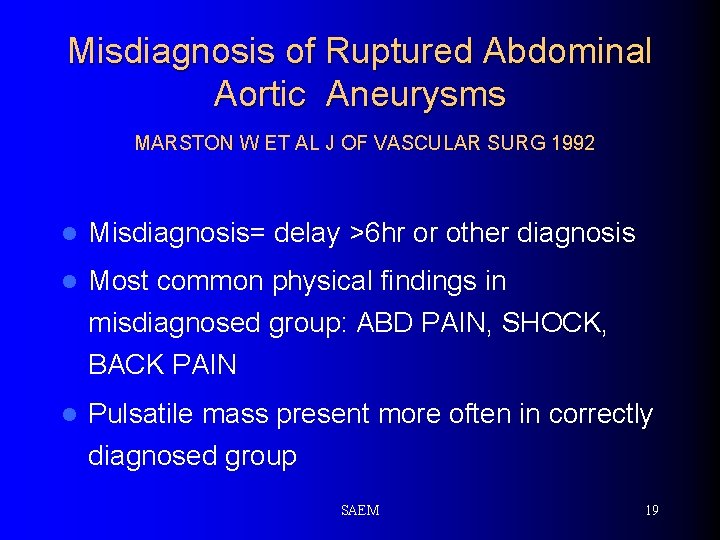
Misdiagnosis of Ruptured Abdominal Aortic Aneurysms MARSTON W ET AL J OF VASCULAR SURG 1992 l Misdiagnosis= delay >6 hr or other diagnosis l Most common physical findings in misdiagnosed group: ABD PAIN, SHOCK, BACK PAIN l Pulsatile mass present more often in correctly diagnosed group SAEM 19
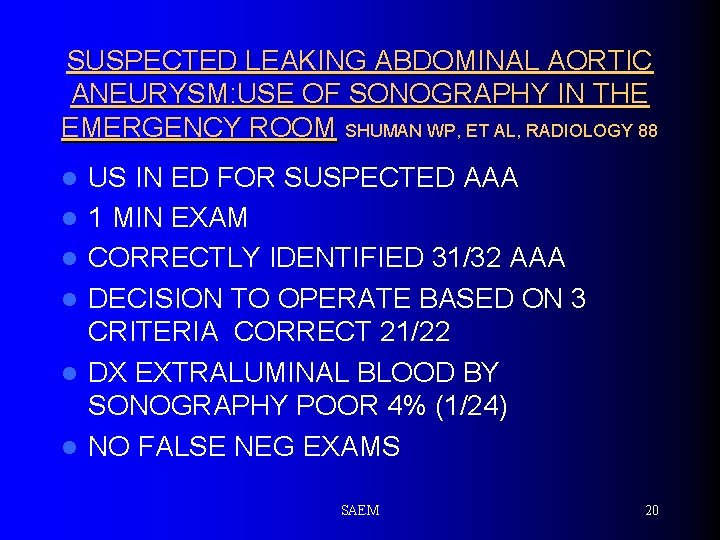
SUSPECTED LEAKING ABDOMINAL AORTIC ANEURYSM: USE OF SONOGRAPHY IN THE EMERGENCY ROOM SHUMAN WP, ET AL, RADIOLOGY 88 l l l US IN ED FOR SUSPECTED AAA 1 MIN EXAM CORRECTLY IDENTIFIED 31/32 AAA DECISION TO OPERATE BASED ON 3 CRITERIA CORRECT 21/22 DX EXTRALUMINAL BLOOD BY SONOGRAPHY POOR 4% (1/24) NO FALSE NEG EXAMS SAEM 20
Diagnosing AAA l Palpation l Plain of the abdomen alone radiographs l Computed tomography l ULTRASOUND SAEM 21
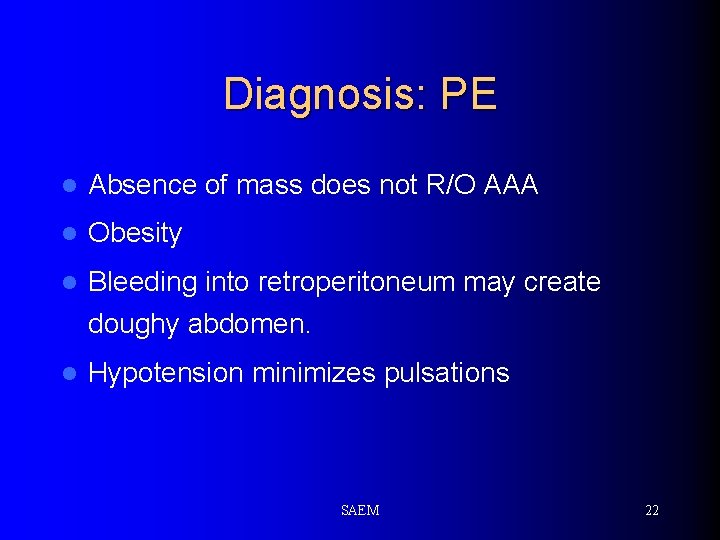
Diagnosis: PE l Absence of mass does not R/O AAA l Obesity l Bleeding into retroperitoneum may create doughy abdomen. l Hypotension minimizes pulsations SAEM 22
Diagnosis: Plain Radiographs l AAA can be seen in 60 -75% of cases l Calcification of aortic wall l Paravertebral mass l Cross table lateral most helpful view l Negative study not helpful SAEM 23
Diagnosis: CT Scan Near 100% accuracy l Better demonstration of extent of aneurysm l Will detect complications of the aneurysm l – Retroperitoneal blood – Dissection l Drawbacks – Contrast – Patient has to leave the ED – Delays time to diagnosis SAEM 24
Diagnosis: US l Ultrasound – Best test for detection of AAA in the ED – Sensitivity 97% to 100% – Small percentage can not be imaged due to bowel gas l 6% in one study SAEM 25
Diagnosis: US l Ultrasound – In some studies as accurate as CT – Measurements within 3 mm of surgical specimens – Angiography may underestimate AAA diameter SAEM 26
Diagnosis: US Emergency department ultrasound scanning for abdominal aortic aneurysm: accessible, accurate and advantageous Kuhn et al. Ann Emerg Med 2000 “Relative neophytes can perform aortic ultrasound scans accurately. These scans appear useful as a screening measure in high-risk emergency patients; they may also aide in rapidly verifying the diagnosis in patients who require immediate surgical intervention” SAEM 27

Diagnosis: US ED Ultrasound Improves Time to Diagnosis and Survival in Ruptured AAA Plummer D, et al: Abstract at 1998 SAEM, Chicago, IL. • Average time to diagnosis by bedside US = 5. 4 minutes • Average time to diagnosis by CT = 83 minutes • Average time to OR for diagnosis by US = 12 minutes • Average time to OR for diagnosis by CT = 90 minutes SAEM 28
US EXAM l Transducer is 2. 5 -3. 0 MHz curvilinear l Place the transducer in the subxiphoid area, using the left lobe of the liver as an acoustic window l Pressure must be applied to displace bowel gas l The aorta must be examined in both the longitudinal and transverse planes SAEM 29
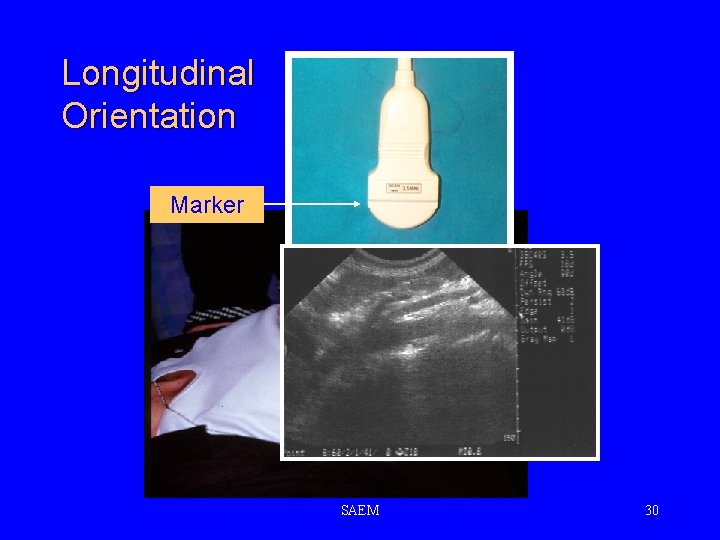
Longitudinal Orientation Marker SAEM 30
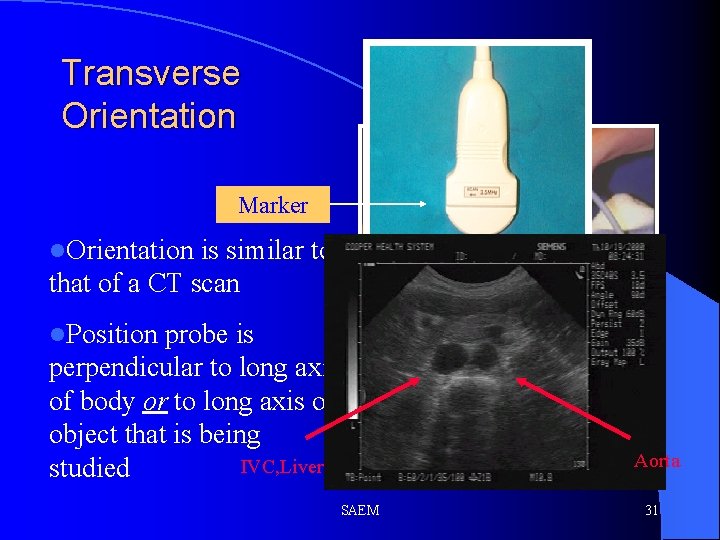
Transverse Orientation Marker l. Orientation is similar to that of a CT scan l. Position probe is perpendicular to long axis of body or to long axis of object that is being IVC, Liver studied Aorta SAEM 31
US EXAM The aorta appears as an anechoic, pulsatile tubular structure to the left of the spine l After the longitudinal scan, the transducer is rotated 90 degrees to the aorta to obtain transverse views. l The key landmark in the transverse view is to locate the spinal column as a hypoechoic area at the bottom of the screen. l The aorta is located above and to the left of the spine l SAEM 32
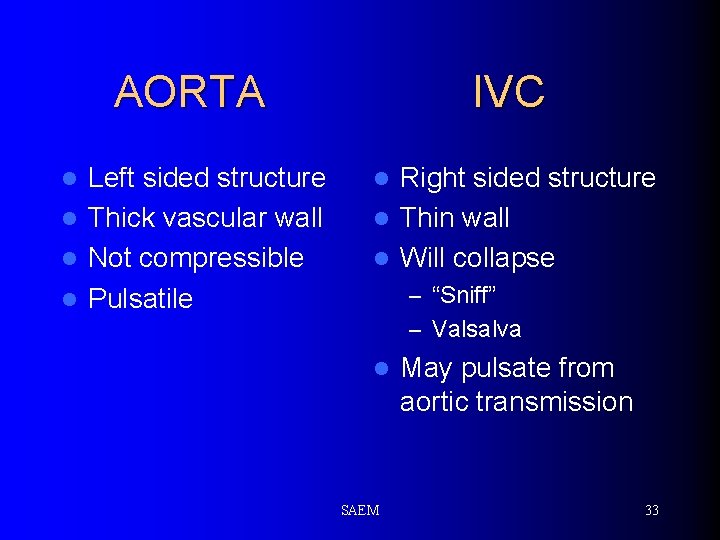
AORTA Left sided structure l Thick vascular wall l Not compressible l Pulsatile l IVC Right sided structure l Thin wall l Will collapse l – “Sniff” – Valsalva l SAEM May pulsate from aortic transmission 33
US EXAM l Measure from outside wall to outside wall l An aneurysm is identified as any measurement of 3 cm or greater l Measure at: – Epigastric region – Take off of SMA – 3 -4 cm intervals to bifurcation l Measure any aneurysm SAEM 34
US EXAM l l l Obesity or excessive bowel gas may obscure the aorta A coronal view of the aorta may be a reasonable alternative The patient is supine The transducer is placed in the mid-axillary line (probe indicator toward the patient’s head) The aorta is visualized adjacent to the vena cava SAEM 35
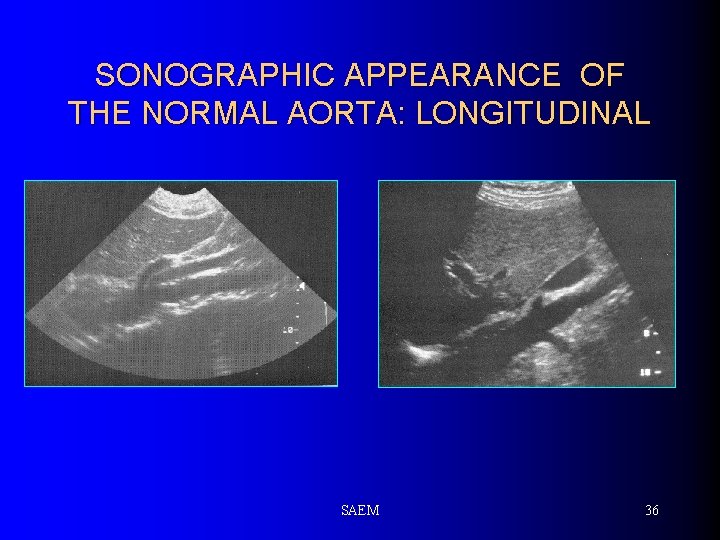
SONOGRAPHIC APPEARANCE OF THE NORMAL AORTA: LONGITUDINAL SAEM 36
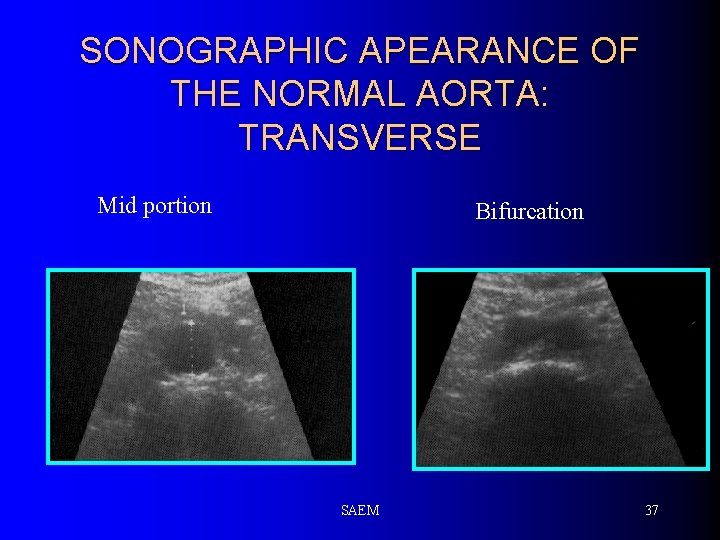
SONOGRAPHIC APEARANCE OF THE NORMAL AORTA: TRANSVERSE Mid portion Bifurcation SAEM 37
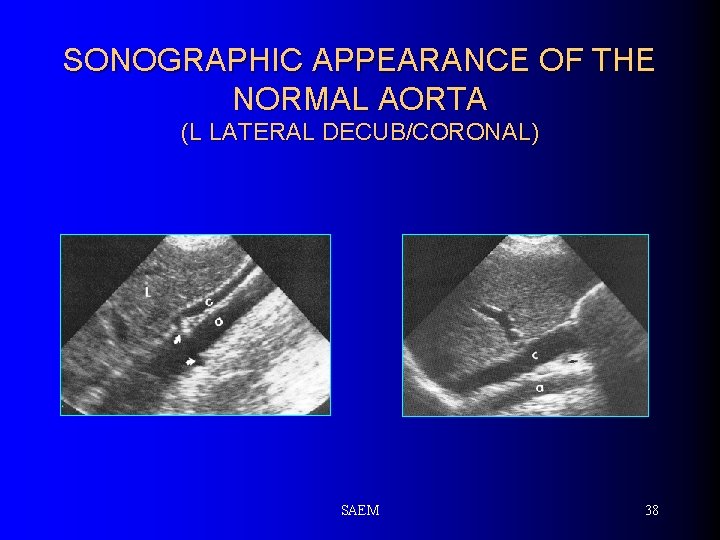
SONOGRAPHIC APPEARANCE OF THE NORMAL AORTA (L LATERAL DECUB/CORONAL) SAEM 38
ABDOMINAL AORTIC ANEURYSM 90% of AAA are infra-renal l 70% involve the renal vessels l Thrombus is common, and usually forms on the antero-lateral walls of the aneurysm l Two forms l – Sacular – Fusiform – most common SAEM 39
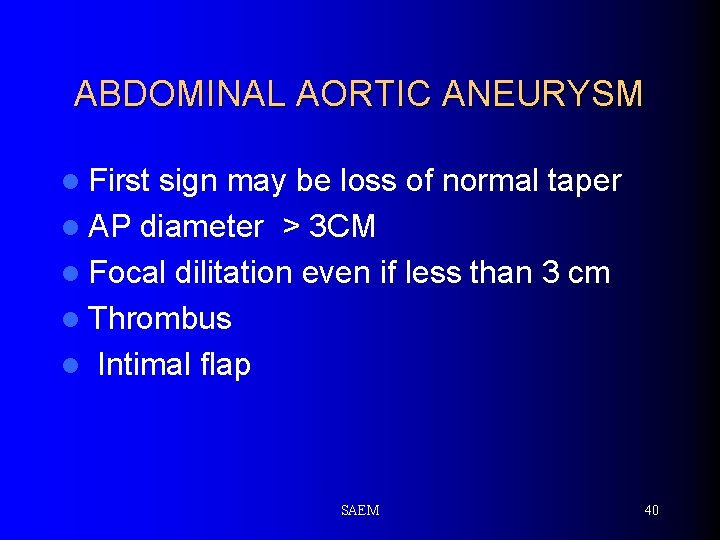
ABDOMINAL AORTIC ANEURYSM l First sign may be loss of normal taper l AP diameter > 3 CM l Focal dilitation even if less than 3 cm l Thrombus l Intimal flap SAEM 40
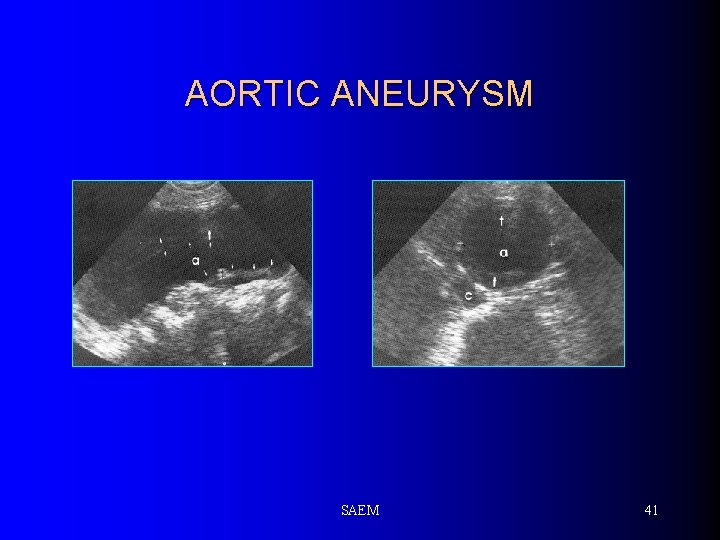
AORTIC ANEURYSM SAEM 41
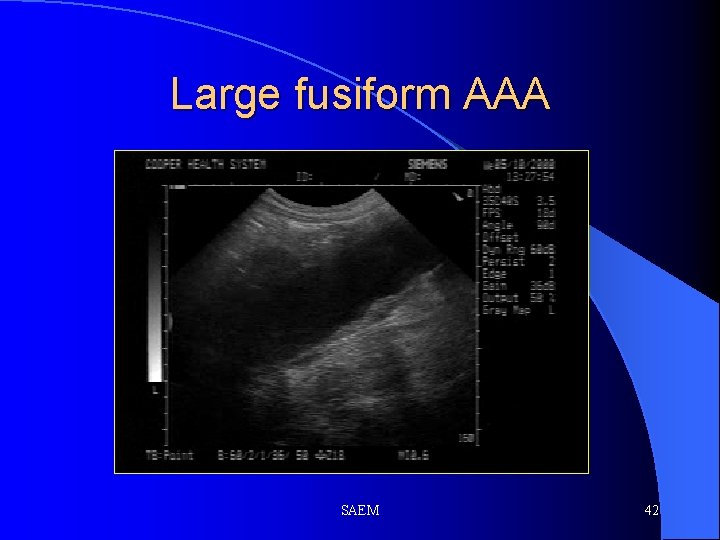
Large fusiform AAA SAEM 42
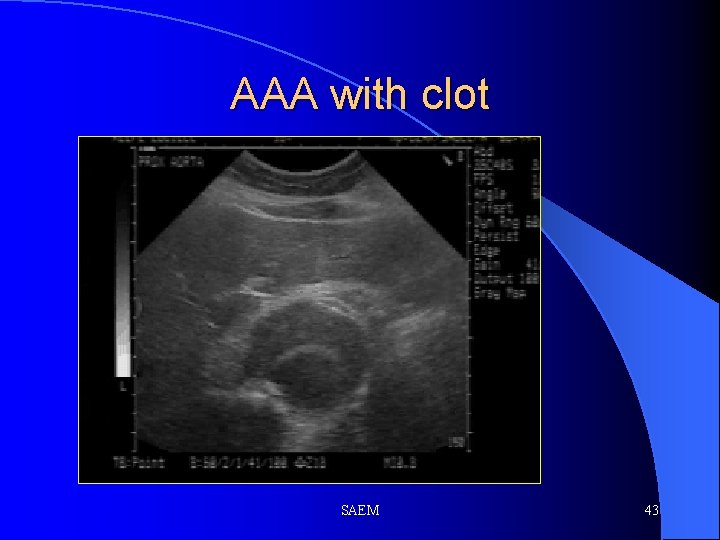
AAA with clot SAEM 43
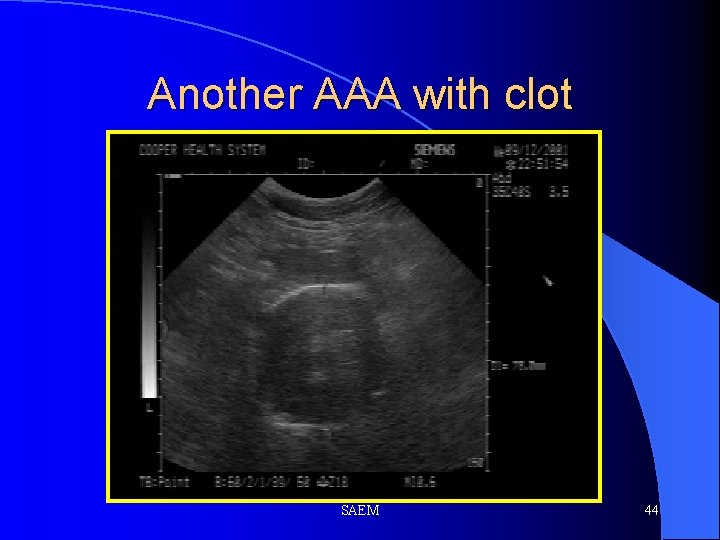
Another AAA with clot SAEM 44
ULTRASOUND EXAM: PITFALLS l Bowel gas can be a major problem – Apply pressure – Roll the patient on their left side ( use the liver as an acoustic window) l Does not detect complications of AAA – Retroperitoneal rupture – Dissection l CT/MRI/angiography for stable patients is still recommended SAEM 45
Pitfalls in Technique l l l Failure to acquire high resolution images due to bowel gas Inaccurate measurements – do not measure what you cannot see! Distinguishing the IVC from the aorta Not identifying extraluminal fluid Failing to distinguish the normal “tortuous” aorta from an abdominal aortic aneurysm. SAEM 46
- Slides: 46