Fluid Bolus Isotonic Lungs Clear 20 mlkg Lungs

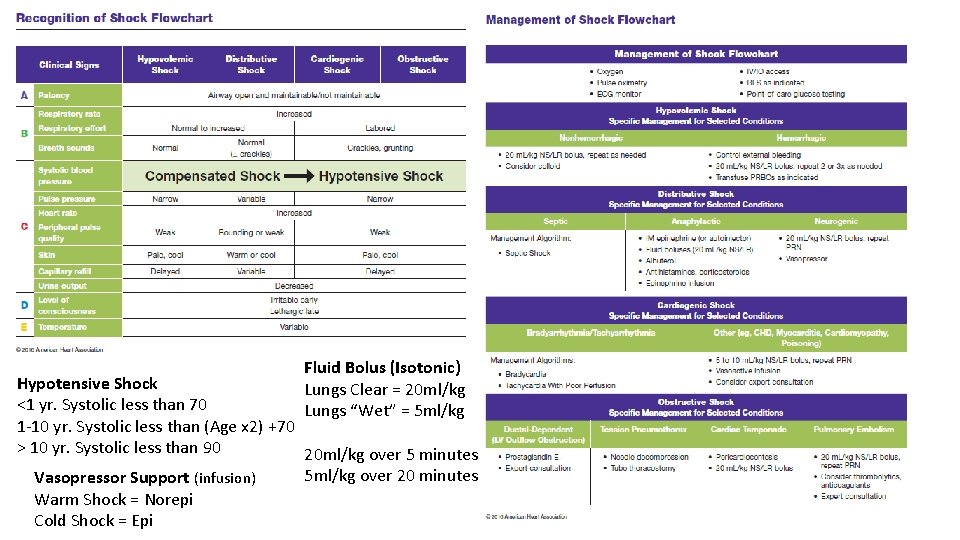
Fluid Bolus (Isotonic) Lungs Clear = 20 ml/kg Lungs “Wet” = 5 ml/kg Hypotensive Shock <1 yr. Systolic less than 70 1 -10 yr. Systolic less than (Age x 2) +70 > 10 yr. Systolic less than 90 20 ml/kg over 5 minutes 5 ml/kg over 20 minutes Vasopressor Support (infusion) Warm Shock = Norepi Cold Shock = Epi

VF/p. VT = Defib Start CPR Defib 2 J/kg 2 minutes of CPR Defib 4 J/kg 2 minutes of CPR & Epi 0. 01 mg/kg Defib 4 -10 J/kg 2 minutes of CPR & Amio 5 mg/kg or Lido 1 mg/kg Asystole/Pulseless Electrical Activity Start CPR, Epi 0. 01 mg/kg ASAP (then every other rhythm check), H + T’s and recheck pulse & rhythm every 2 minutes. PEA = Push Epi Ask why PEA = Push Epi All the time PEA = Push Epi Always PEA = Push Epi Again Post Cardiac Arrest Care 4 H’s to Avoid Hypoxia: Maintain 94 -99% SPO 2 Hypotension: Manage BP for age, use fluids or pressor Hypoglycemia: Treat with D 10 or D 25 Hyperthermia: Don’t confuse with Targeted Temp Management Also. prone to seizures, may monitor with EEG
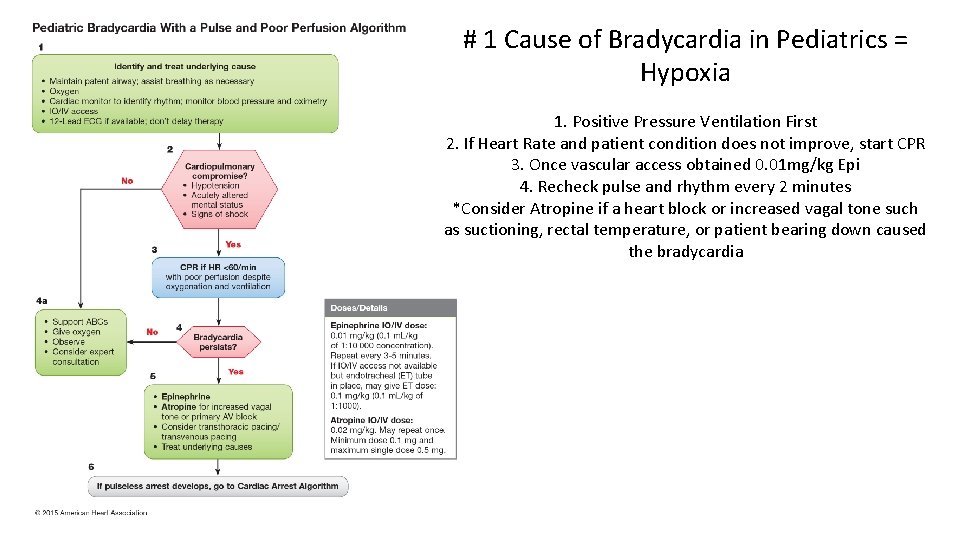
# 1 Cause of Bradycardia in Pediatrics = Hypoxia 1. Positive Pressure Ventilation First 2. If Heart Rate and patient condition does not improve, start CPR 3. Once vascular access obtained 0. 01 mg/kg Epi 4. Recheck pulse and rhythm every 2 minutes *Consider Atropine if a heart block or increased vagal tone such as suctioning, rectal temperature, or patient bearing down caused the bradycardia
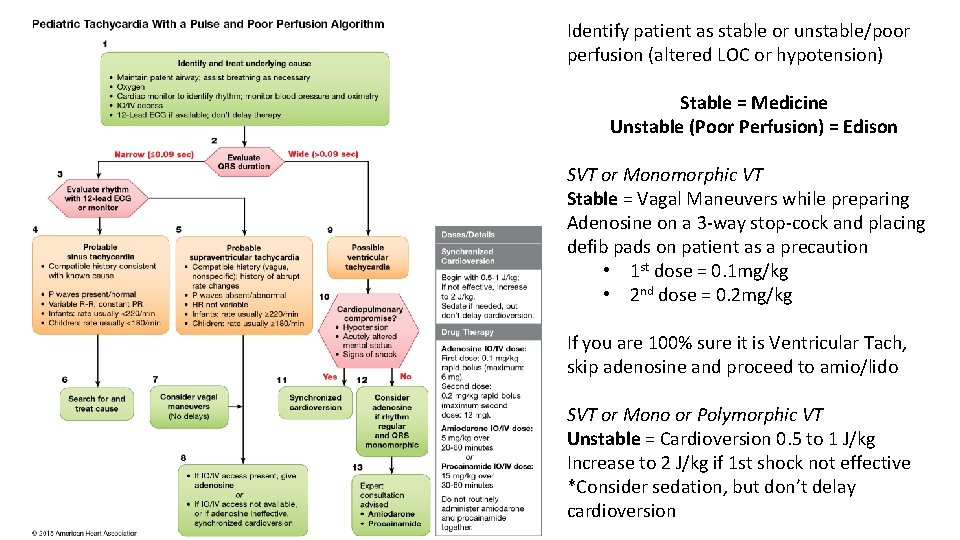
Identify patient as stable or unstable/poor perfusion (altered LOC or hypotension) Stable = Medicine Unstable (Poor Perfusion) = Edison SVT or Monomorphic VT Stable = Vagal Maneuvers while preparing Adenosine on a 3 -way stop-cock and placing defib pads on patient as a precaution • 1 st dose = 0. 1 mg/kg • 2 nd dose = 0. 2 mg/kg If you are 100% sure it is Ventricular Tach, skip adenosine and proceed to amio/lido SVT or Mono or Polymorphic VT Unstable = Cardioversion 0. 5 to 1 J/kg Increase to 2 J/kg if 1 st shock not effective *Consider sedation, but don’t delay cardioversion
- Slides: 6