Fluid and Electrolytes Chapter 11 continued Copyright 2014






















- Slides: 92
Fluid and Electrolytes Chapter 11 continued Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Electrolytes • Substances whose molecules dissociate into ions when placed into water • Cations: positively charged • Anions: negatively charged Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Electrolyte Composition • ICF • Prevalent cation is K+ • Prevalent anion is PO 43 - • ECF • Prevalent cation is Na+ • Prevalent anion is Cl. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
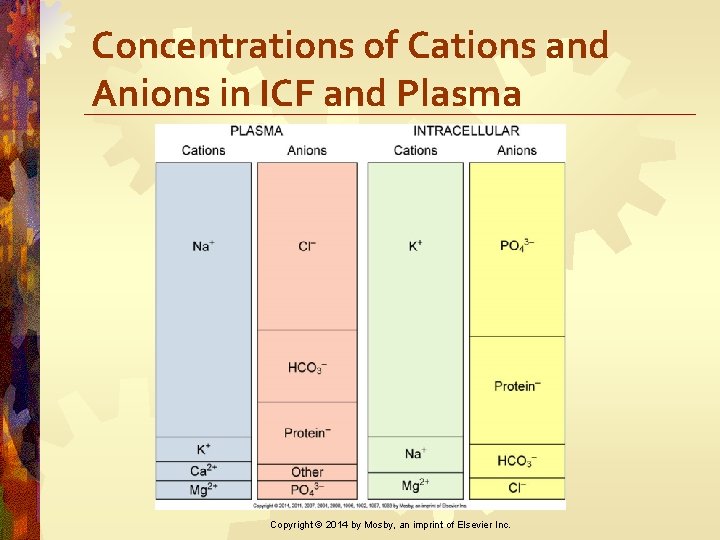
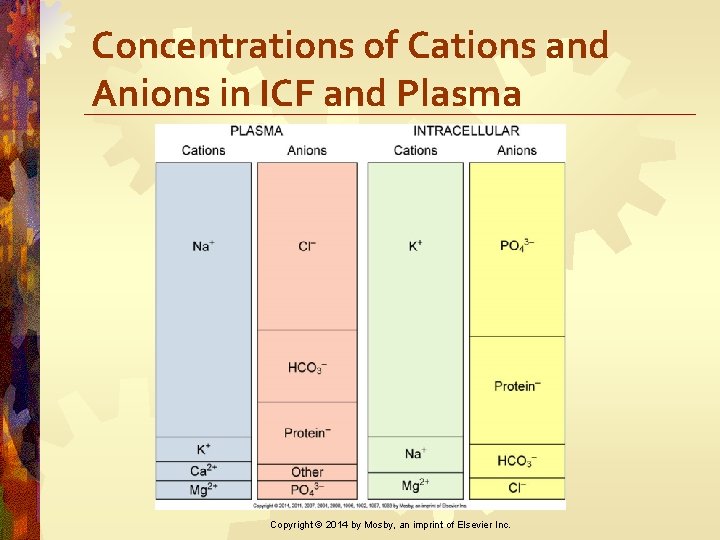
Concentrations of Cations and Anions in ICF and Plasma Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
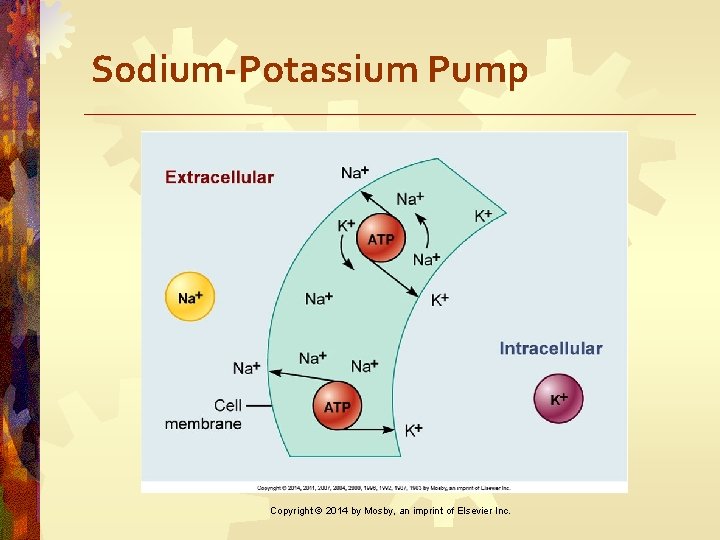
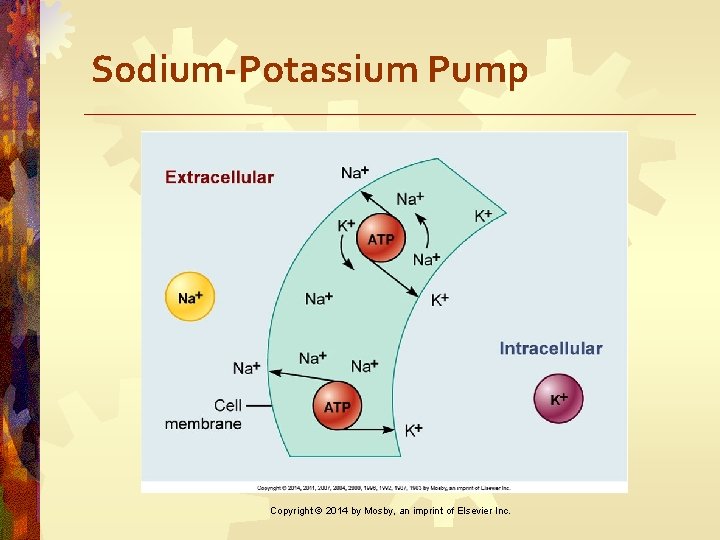
Sodium-Potassium Pump Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
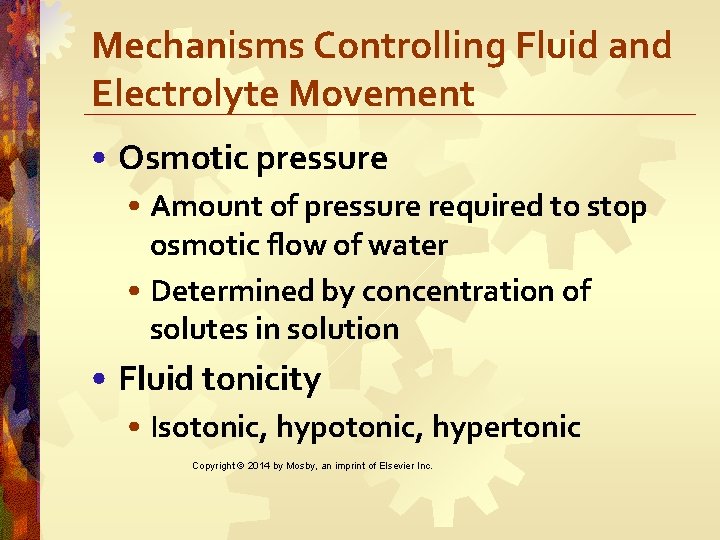
Mechanisms Controlling Fluid and Electrolyte Movement • Osmotic pressure • Amount of pressure required to stop osmotic flow of water • Determined by concentration of solutes in solution • Fluid tonicity • Isotonic, hypertonic Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
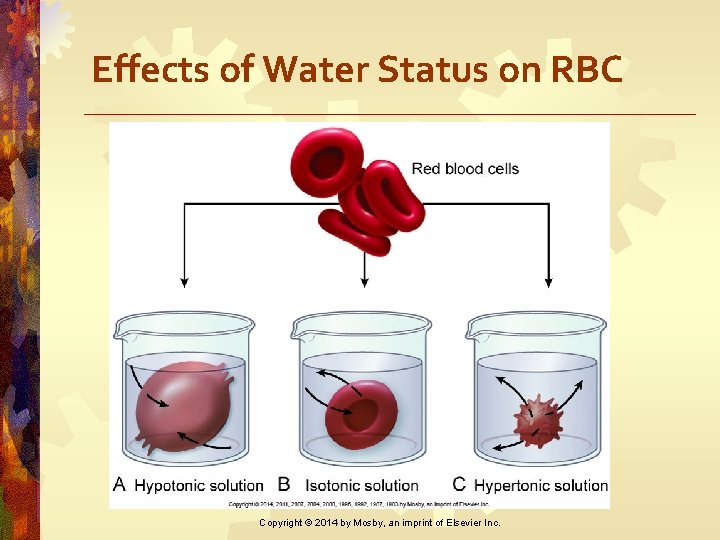
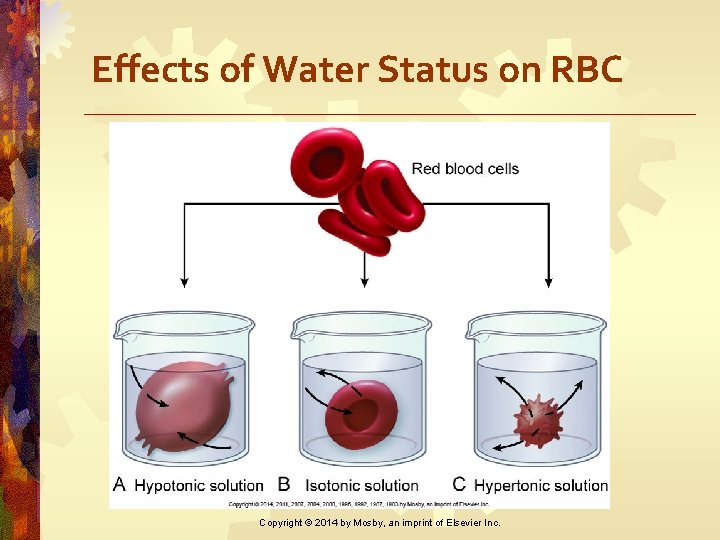
Effects of Water Status on RBC Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
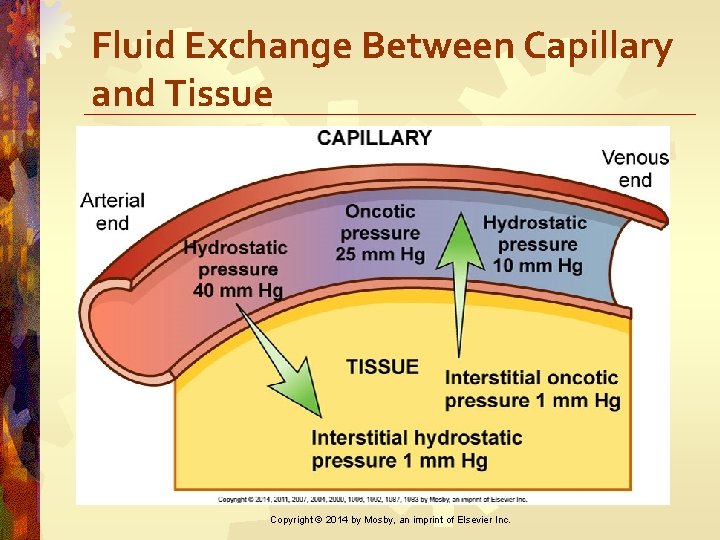
Mechanisms Controlling Fluid and Electrolyte Movement • Hydrostatic pressure • Blood pressure generated by heart contraction • Oncotic pressure • Osmotic pressure caused by plasma proteins Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Fluid Movement in Capillaries • Amount and direction of movement determined by • Capillary hydrostatic pressure • Plasma oncotic pressure • Interstitial hydrostatic pressure • Interstitial oncotic pressure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
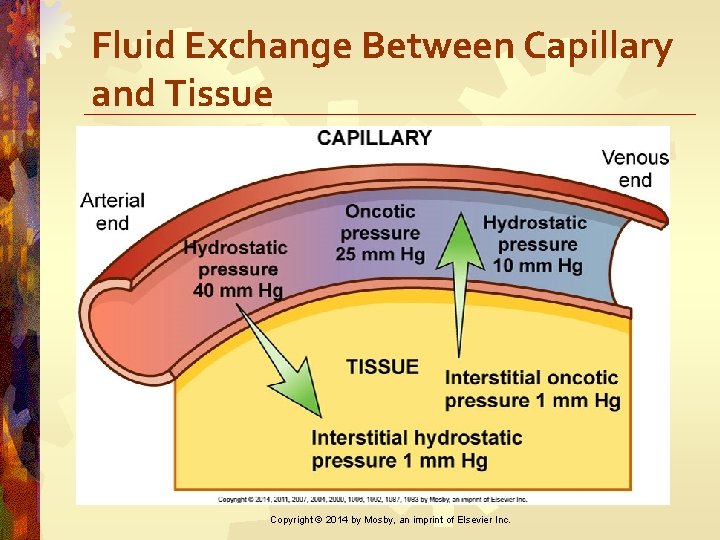
Fluid Exchange Between Capillary and Tissue Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Fluid Shifts • Plasma-to-interstitial fluid shift results in edema • Interstitial fluid to plasma decreases edema Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Fluid Spacing • First spacing • Normal distribution • Second spacing • Abnormal (edema) • Third spacing • Fluid accumulation in part of body where it is not easily exchanged with ECF Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Fluid and Electrolyte Imbalances • Directly caused by illness or disease (burns or heart failure) • Result of therapeutic measures (IV fluid replacement or diuretics) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Extracellular Fluid Volume Imbalances • ECF volume deficit (hypovolemia) • Abnormal loss of normal body fluids, inadequate intake, or plasma-tointerstitial fluid shift • Clinical manifestations related to loss of vascular volume as well as CNS effects • Treatment: Replace water and electrolytes with balanced IV solutions Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Extracellular Fluid Volume Imbalances • Fluid volume excess (hypervolemia) • Excessive intake of fluids, abnormal retention of fluids, or interstitial-toplasma fluid shift • Clinical manifestations related to excess volume • Treatment: Remove fluid without changing electrolyte composition or osmolality of ECF Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Nursing Management Nursing Diagnoses Hypovolemia • Deficient fluid volume • Decreased cardiac output • Risk for deficient fluid volume • Potential complication: Hypovolemic shock Hypervolemia • Excess fluid volume • Impaired gas exchange • Risk for impaired skin integrity • Activity intolerance • Disturbed body image • Potential complications: Pulmonary edema, ascites Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Sodium • Imbalances typically associated with parallel changes in osmolality • Plays a major role in • ECF volume and concentration • Generation and transmission of nerve impulses • Muscle contractility • Acid-base balance Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypernatremia • Elevated serum sodium occurring with water loss or sodium gain • Causes hyperosmolality leading to cellular dehydration • Primary protection is thirst from hypothalamus Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Differential Assessment of ECF Volume Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypernatremia • Manifestations • Thirst, lethargy, agitation, seizures, and coma • Impaired LOC • Symptoms of fluid volume deficit Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Diagnoses • Risk for injury • Risk for fluid volume deficit • Risk for electrolyte imbalance • Potential complication: Seizures and coma leading to irreversible brain damage Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Implementation • Treat underlying cause • Primary water deficit—replace fluid orally or IV with isotonic or hypotonic fluids • Excess sodium—dilute with sodiumfree IV fluids and promote excretion with diuretics • Monitor carefully Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hyponatremia i. Stockphoto/Thinkstock • M. H. , a 62 -year-old female, was admitted with confusion and lethargy related to hyponatremia. • Her husband tells you that M. H. had c/o diarrhea over the past week and was drinking lots of water to prevent dehydration. • What caused M. H. ’s serum sodium level to fall? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hyponatremia • Results from loss of sodiumcontaining fluids and/or from water excess • Manifestations • Confusion, irritability, headache, seizures, and coma Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hyponatremia i. Stockphoto/Thinkstock • As you admit M. H. to the nursing unit, you develop an individualized plan of care. • Identify appropriate nursing diagnoses for M. H. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Diagnoses • Acute confusion • Risk for injury • Risk for electrolyte imbalance • Potential complication: Severe neurologic changes Copyright © 2014 by Mosby, an imprint of Elsevier Inc.


Case Study Hyponatremia i. Stockphoto/Thinkstock • Identify appropriate nursing interventions to help normalize M. H. ’s serum sodium levels. • How would treatment differ if hyponatremia was more severe? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Implementation • Caused by water excess • Fluid restriction is needed • Severe symptoms (seizures) • Give small amount of IV hypertonic saline solution (3% Na. Cl) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Nursing Management Nursing Implementation • Abnormal fluid loss • Fluid replacement with sodiumcontaining solution • Drugs that block vasopressin (ADH) • Convaptan (Vaprisol) • Tolvaptan (Samsca) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Potassium • Major ICF cation • Necessary for • Transmission and conduction of nerve and muscle impulses • Cellular growth • Maintenance of cardiac rhythms • Acid-base balance Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Potassium • Sources • Fruits and vegetables (bananas and oranges) • Salt substitutes • Potassium medications (PO, IV) • Stored blood • Regulated by kidneys Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hyperkalemia • High serum potassium caused by • Impaired renal excretion • Shift from ICF to ECF • Massive intake • Most common in renal failure Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hyperkalemia • Manifestations • Cramping leg pain • Weak or paralyzed skeletal muscles • Abdominal cramping or diarrhea • Cardiac dysrhythmias Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
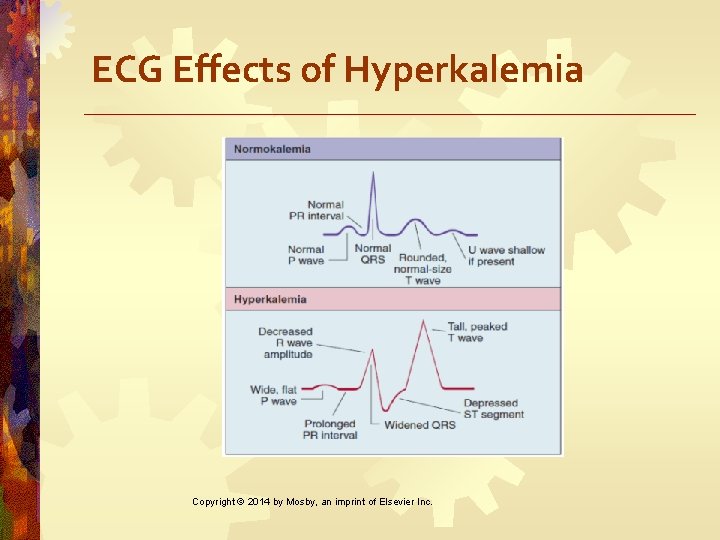
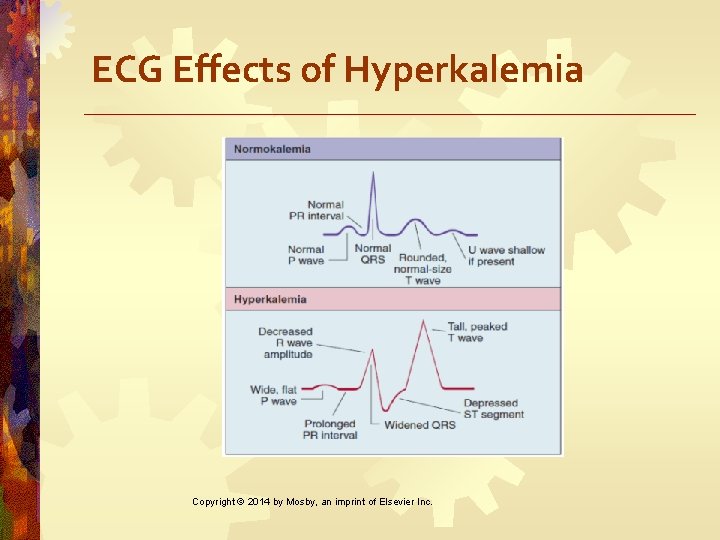
ECG Effects of Hyperkalemia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Diagnoses • Risk for activity intolerance • Risk for electrolyte imbalance • Risk for injury • Potential complication: dysrhythmias Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Implementation • Eliminate oral and parenteral K intake • Increase elimination of K (diuretics, dialysis, Kayexalate) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Nursing Management Nursing Implementation • Force K from ECF to ICF by IV insulin or sodium bicarbonate • Reverse membrane effects of elevated ECF potassium by administering calcium gluconate IV Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hypokalemia • T. M. , a 76 -year-old male, is brought to emergency department with confusion and lethargy. • He has a history of hypertension and type 2 diabetes. • Patient doubled his furosemide (Lasix) dose for the last 2 weeks because he felt “puffy. ” i. Stockphoto/Thinkstock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hypokalemia • Low serum potassium caused by • Increased loss of K+ via the kidneys or gastrointestinal tract • Increased shift of K+ from ECF to ICF • Dietary K+ deficiency (rare) • Magnesium deficiency • Metabolic alkalosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hypokalemia • T. M. ’s lab results include serum K+ 2. 8 and Hct 56%. • What is the probable cause of T. M. ’s hypokalemia? • Explain the Hct lab result based on T. M. ’s recent history. • For what clinical manifestations would you assess T. M. ? i. Stockphoto/Thinkstock Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypokalemia • Manifestations • Cardiac most serious • Skeletal muscle weakness (legs) • Weakness of respiratory muscles • Decreased gastrointestinal motility • Impaired regulation of arteriolar blood flow • Hyperglycemia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

ECG Effects of Hyp 0 kalemia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hypokalemia • Assessment of T. M. reveals the following: • Poor skin turgor, c/o leg cramps • Heart rate 135 and irregular • Respiratory rate 26 • BP 110/58 • Identify appropriate nursing diagnoses for T. M. Copyright © 2014 by Mosby, an imprint of Elsevier Inc. i. Stockphoto/Thinkstock

Nursing Management Nursing Diagnoses • Risk for activity intolerance • Risk for electrolyte imbalance • Risk for injury • Potential complication: Dysrhythmias Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hypokalemia i. Stockphoto/Thinkstock • T. M. is started on. 45 Na. Cl and potassium chloride replacement is ordered. • How will you administer the potassium chloride? • Discuss other appropriate nursing interventions for T. M. Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Implementation • KCl supplements orally or IV • Always dilute IV KCL • NEVER give KCL via IV push or as a bolus • Should not exceed 10 m. Eq/hr • To prevent hyperkalemia and cardiac arrest Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Case Study Hypokalemia i. Stockphoto/Thinkstock • T. M. ’s serum electrolytes and fluid volume status return to normal. • What important teaching should be done with T. M. in anticipation of discharge? Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Calcium • Functions • Formation of teeth and bone • Blood clotting • Transmission of nerve impulses • Myocardial contractions • Muscle contractions Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Calcium • Obtained from ingested foods • Need vitamin D to absorb • Present in three forms: Ionized calcium is biologically active • Changes in p. H and serum albumin affect levels Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Calcium • Balance controlled by • Parathyroid hormone • Calcitonin Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hypercalcemia • High levels of serum calcium caused by • Hyperparathyroidism (two thirds of cases) • Malignancy • Prolonged immobilization Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypercalcemia • Manifestations • Lethargy, weakness, stupor, coma • Depressed reflexes • Decreased memory • Confusion, personality changes, psychosis • Anorexia, nausea, vomiting • Bone pain, fractures, nephrolithiasis • Polyuria, dehydration Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Diagnoses • Risk for inactivity intolerance • Risk for electrolyte imbalance • Risk for injury • Potential complication: Dysrhythmias Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Nursing Management Nursing Implementation • Excretion of Ca with loop diuretic • Hydration with isotonic saline infusion • Low calcium diet • Mobilization • Synthetic calcitonin • Bisphonates Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypocalcemia • Low serum Ca levels caused by • Decreased production of PTH • Acute pancreatitis • Multiple blood transfusions • Alkalosis • Increased calcium loss Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypocalcemia • Manifestations • Positive Trousseau’s or Chvostek’s sign • Laryngeal stridor • Dysphagia • Tingling around the mouth or in the extremities • Cardiac dysrhythmias Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Tests for Hypocalcemia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Nursing Management Nursing Diagnoses • Acute pain • Ineffective breathing pattern • Risk for electrolyte imbalance • Risk for injury • Potential complication: Fracture or respiratory arrest Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Nursing Management Nursing Implementation • Treat cause • Oral or IV calcium supplements • Not IM to avoid local reactions • Rebreathe into paper bag • Treat pain and anxiety to prevent hyperventilation-induced respiratory alkalosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Phosphate • Primary anion in ICF • Essential to function of muscle, red blood cells, and nervous system • Involved in acid-base buffering system, ATP production, cellular uptake of glucose, and metabolism of carbohydrates, proteins, and fats Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Phosphate • Serum levels controlled by parathyroid hormone • Maintenance requires adequate renal functioning • Reciprocal relationship with calcium Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hyperphosphatemia • High serum PO 43 - caused by • Acute kidney injury or chronic kidney disease • Chemotherapy • Excessive ingestion of phosphate or vitamin D Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hyperphosphatemia • Manifestations • Neuromuscular irritability and tetany (hypocalcemia) • Calcified deposition in soft tissue such as joints, arteries, skin, kidneys, and corneas (can cause organ dysfunction) Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hyperphosphatemia • Management • Identify and treat underlying cause • Restrict foods and fluids containing phosphorus • Phosphate-binding agents • Adequate hydration and correction of hypocalcemic conditions • Hemodialysis, IV insulin and glucose Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypophosphatemia • Low serum PO 43 - caused by • Malnourishment/malabsorption • Alcohol withdrawal • Use of phosphate-binding antacids • During parenteral nutrition with inadequate replacement Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypophosphatemia • Manifestations • CNS depression • Confusion • Muscle weakness and pain • Dysrhythmias • Cardiomyopathy Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypophosphatemia • Management • Oral supplementation • Ingestion of foods high in phosphorus • IV administration of sodium or potassium phosphate Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Magnesium • Coenzyme in metabolism of protein and carbohydrates • Required for nucleic acid and protein synthesis • Helps maintain calcium and potassium balance • Necessary for sodium-potassium pump Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Magnesium • Acts directly on myoneural junction • Important for normal cardiac function • 50% to 60% contained in bone • Absorbed in GI tract • Excreted by kidneys Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypermagnesemia • High serum Mg caused by • Increased intake or ingestion of products containing magnesium when renal insufficiency or failure is present • Excess intravenous magnesium administration Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hypermagnesemia • Manifestations • Lethargy • Nausea and vomiting • Impaired reflexes • Somnolence • Respiratory and cardiac arrest Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

Hypermagnesemia • Management • Prevention first—restrict magnesium intake in high-risk patients • Emergency treatment • IV Ca. Cl or calcium gluconate • Fluids and IV furosemide to promote urinary excretion • Dialysis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypomagnesemia • Low serum Mg caused by • Prolonged fasting or starvation • Chronic alcoholism • Fluid loss from gastrointestinal tract • Prolonged parenteral nutrition without supplementation • Diuretics • Hyperglycemic osmotic diuresis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypomagnesemia • Manifestations • Confusion • Hyperactive deep tendon reflexes • Muscle cramps • Tremors • Seizures • Cardiac dysrhythmias • Corresponding hypocalcemia and hypokalemia Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Hypomagnesemia • Management • Treat underlying cause • Oral supplements • Increase dietary intake • Parenteral IV or IM magnesium when severe Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
IV Fluids • Purposes • Maintenance • When oral intake is not adequate • Replacement • When losses have occurred • Types of fluids categorized by tonicity Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
IV Fluids • Hypotonic • More water than electrolytes • Pure water lyses RBCs. • Water moves from ECF to ICF by osmosis • Usually maintenance fluids • Monitor for changes in mentation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
IV Fluids • Isotonic • Expands only ECF • No net loss or gain from ICF • Ideal to replace ECF volume deficit Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

IV Fluids • Hypertonic • Initially expands and raises the osmolality of ECF • Require frequent monitoring of • Blood pressure • Lung sounds • Serum sodium levels Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
D 5 W • Isotonic • Provides 170 cal/L • Prevents ketosis associated with starvation Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
D 5 W • Free water • Moves into ICF • Increases renal solute excretion • Used to replace water losses and treat hypernatremia • Does not provide electrolytes Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Normal Saline (NS or NSS) • Isotonic • More Na. Cl than ECF • Expands IV volume • Preferred fluid for immediate response • Risk for fluid overload higher • Also monitor for hyperchloremic acidosis Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Normal Saline (NS or NSS) • No free water • No calories • No additional electrolytes • Blood products • Compatible with most medications Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
Lactated Ringer’s Solution • Isotonic • Similar in composition to plasma except contains no magnesium • Expands ECF—treat burns and GI losses • Contraindicated with hyperkalemia and lactic acidosis • No free water or calories Copyright © 2014 by Mosby, an imprint of Elsevier Inc.

D 5 ½ NS • Hypertonic • Common maintenance fluid • Replaces fluid loss • KCl added for maintenance or replacement Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
D 10 W • Hypertonic • Provides 340 kcal/L • Provides free water but no electrolytes • Limit of dextrose concentration may be infused peripherally Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
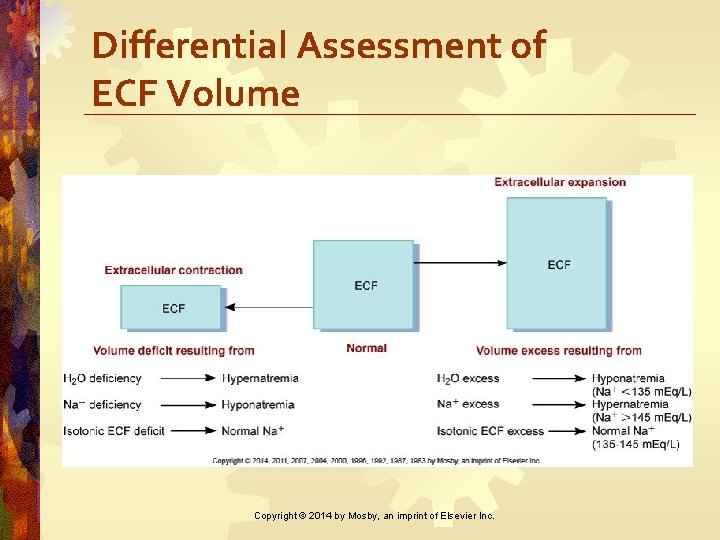
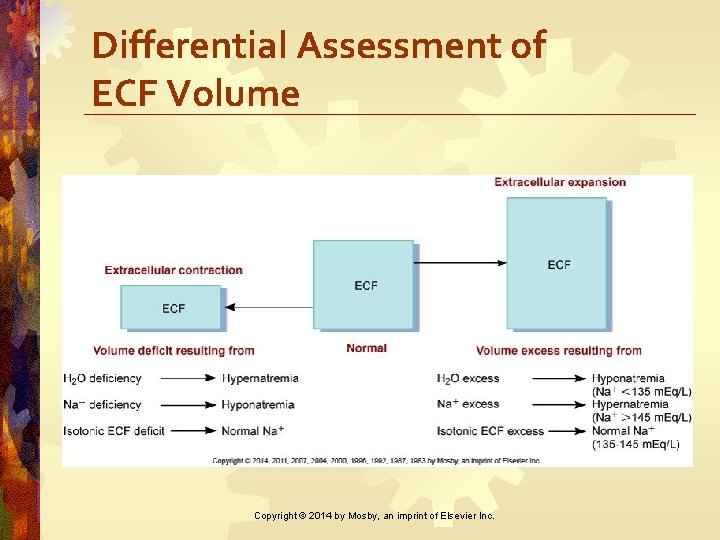
Plasma Expanders • Stay in vascular space and increase osmotic pressure • Colloids (protein solutions) • Plasma, albumin, commercial plasmas • Dextran • Hetastarch • Blood Fig. 17 -12. Differential assessment of extracellular fluid (ECF) volume.

Audience Response Question In a patient with prolonged vomiting, the nurse monitors for fluid volume deficit because vomiting results in a. Fluid movement from the cells into the interstitial space and the blood vessels b. Excretion of large amounts of interstitial fluid with depletion of extracellular fluids c. An overload of extracellular fluid with a significant increase in intracellular fluid volume d. Fluid movement from the vascular system into the cells, causing cellular swelling and rupture Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
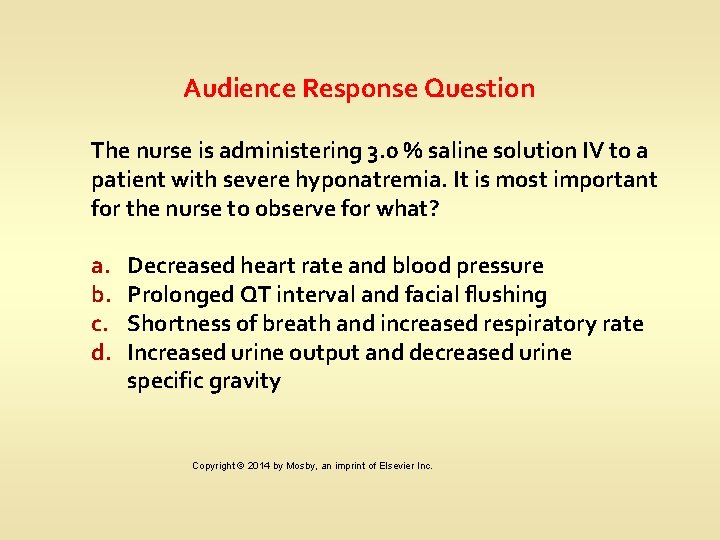
Audience Response Question The nurse is administering 3. 0 % saline solution IV to a patient with severe hyponatremia. It is most important for the nurse to observe for what? a. b. c. d. Decreased heart rate and blood pressure Prolonged QT interval and facial flushing Shortness of breath and increased respiratory rate Increased urine output and decreased urine specific gravity Copyright © 2014 by Mosby, an imprint of Elsevier Inc.
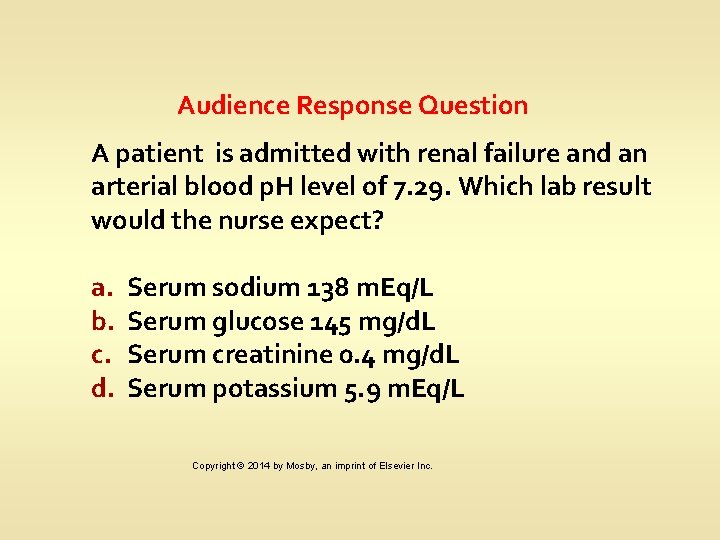
Audience Response Question A patient is admitted with renal failure and an arterial blood p. H level of 7. 29. Which lab result would the nurse expect? a. b. c. d. Serum sodium 138 m. Eq/L Serum glucose 145 mg/d. L Serum creatinine 0. 4 mg/d. L Serum potassium 5. 9 m. Eq/L Copyright © 2014 by Mosby, an imprint of Elsevier Inc.