Fluid and Electrolyte Balance Myoung Kyu Park MD
Fluid and Electrolyte Balance Myoung Kyu Park MD. Ph. D. Department of Physiology Sungkyunkwan University School of Medicine
Fluid and Electrolyte Balance 1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance and compositions Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance and compositions Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
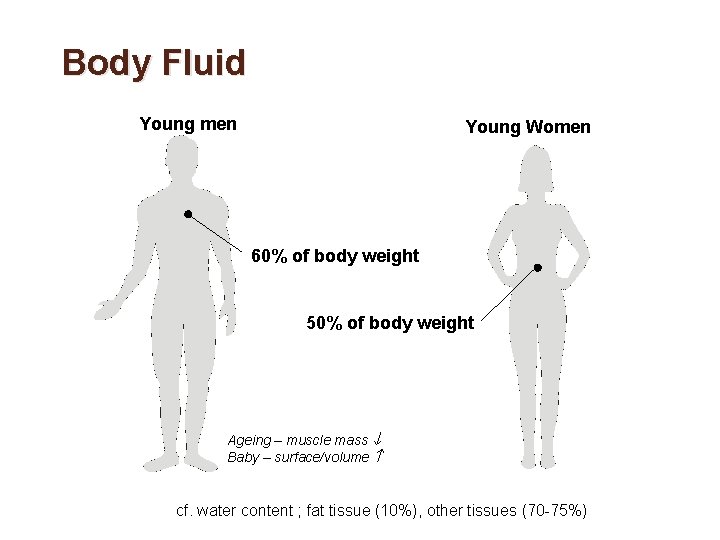
Body Fluid Young men Young Women 60% of body weight 50% of body weight Ageing – muscle mass Baby – surface/volume cf. water content ; fat tissue (10%), other tissues (70 -75%)
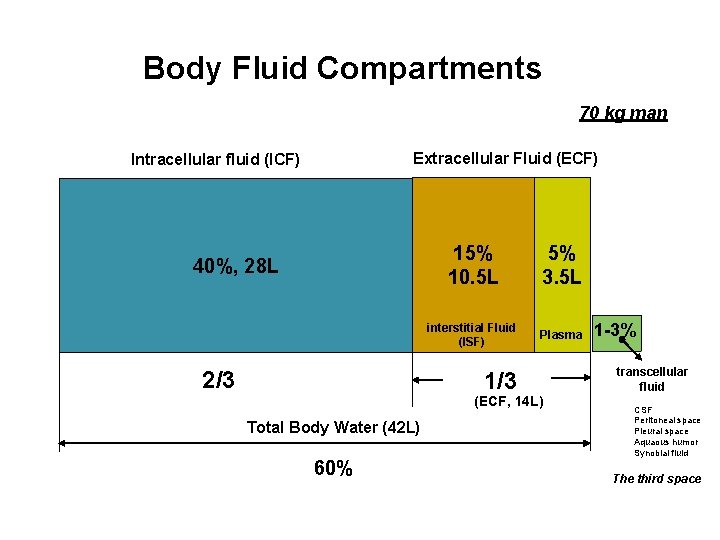
Body Fluid Compartments 70 kg man Extracellular Fluid (ECF) Intracellular fluid (ICF) 40%, 28 L 2/3 15% 10. 5 L 5% 3. 5 L interstitial Fluid (ISF) Plasma 1/3 (ECF, 14 L) Total Body Water (42 L) 60% 1 -3% transcellular fluid CSF Peritoneal space Pleural space Aquaous humor Synobial fluid The third space
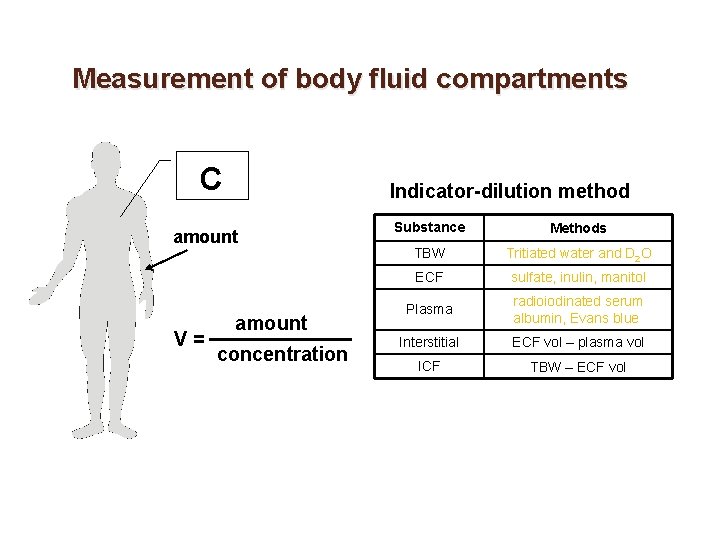
Measurement of body fluid compartments C Indicator-dilution method amount V= amount concentration Substance Methods TBW Tritiated water and D 2 O ECF sulfate, inulin, manitol Plasma radioiodinated serum albumin, Evans blue Interstitial ECF vol – plasma vol ICF TBW – ECF vol
1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance and compositions Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
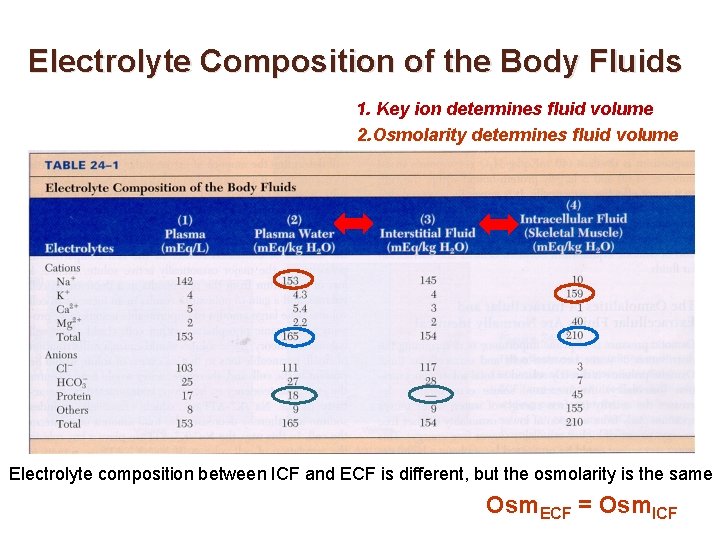
Electrolyte Composition of the Body Fluids 1. Key ion determines fluid volume 2. Osmolarity determines fluid volume Electrolyte composition between ICF and ECF is different, but the osmolarity is the same Osm. ECF = Osm. ICF
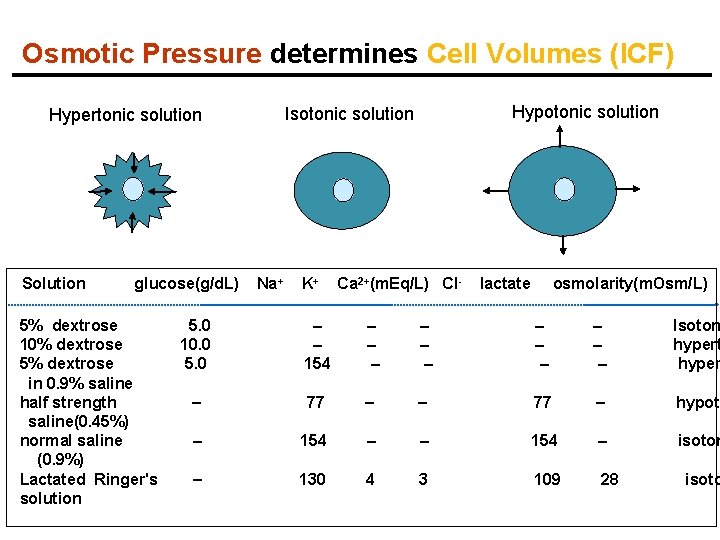
Osmotic Pressure determines Cell Volumes (ICF) Solution glucose(g/d. L) 5% dextrose 10% dextrose 5% dextrose in 0. 9% saline half strength saline(0. 45%) normal saline (0. 9%) Lactated Ringer's solution Hypotonic solution Isotonic solution Hypertonic solution Na+ K+ Ca 2+(m. Eq/L) Cl- lactate osmolarity(m. Osm/L) 5. 0 10. 0 5. 0 154 Isoton hypert hyper 77 hypoto 154 isoton 130 4 3 109 28 isoto
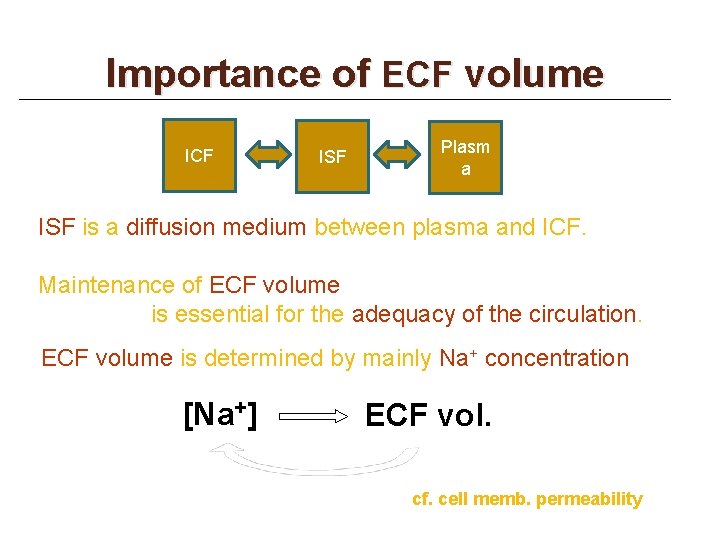
Importance of ECF volume ICF ISF Plasm a ISF is a diffusion medium between plasma and ICF. Maintenance of ECF volume is essential for the adequacy of the circulation. ECF volume is determined by mainly Na+ concentration [Na+] ECF vol. cf. cell memb. permeability
Evolutionary changes sponges jellyfish earthworm
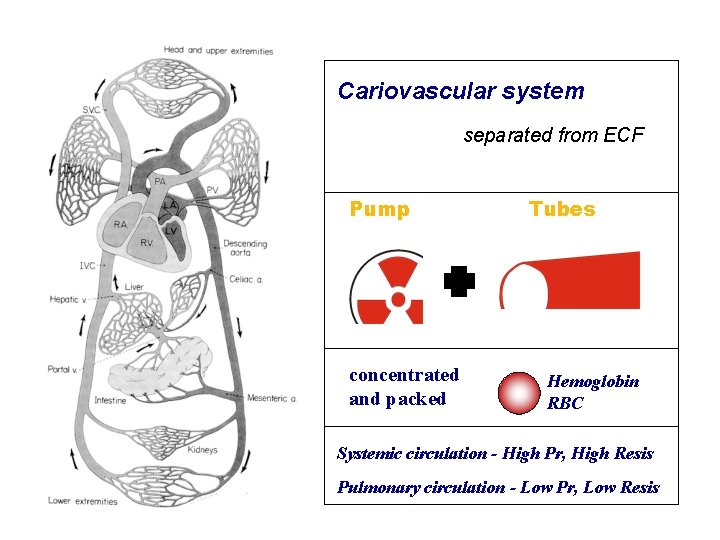
Cariovascular system separated from ECF Pump concentrated and packed Tubes Hemoglobin RBC Systemic circulation - High Pr, High Resis Pulmonary circulation - Low Pr, Low Resis
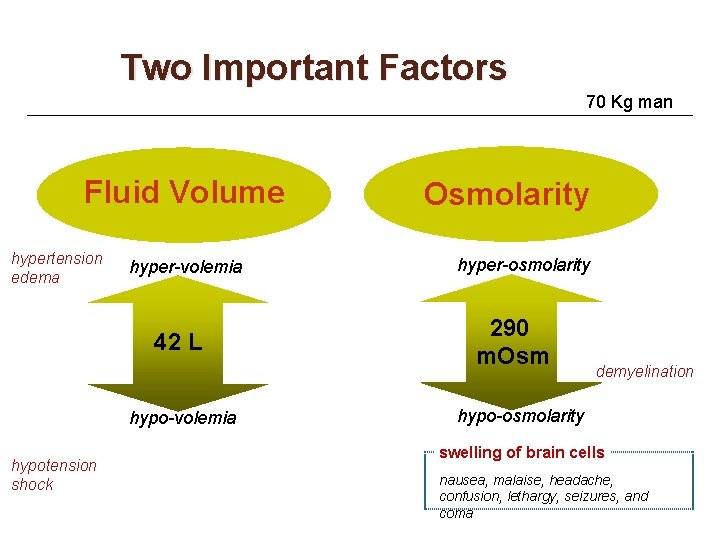
Two Important Factors 70 Kg man Fluid Volume hypertension edema hyper-volemia 42 L hypo-volemia hypotension shock Osmolarity hyper-osmolarity 290 m. Osm demyelination hypo-osmolarity swelling of brain cells nausea, malaise, headache, confusion, lethargy, seizures, and coma

Shifts of water between compartments osmolality pure water 300 Add Normal m. Osm ICF ECF 2/3 (28 L) 1/3 (14 L) volume Darrow-Yannet Diagram
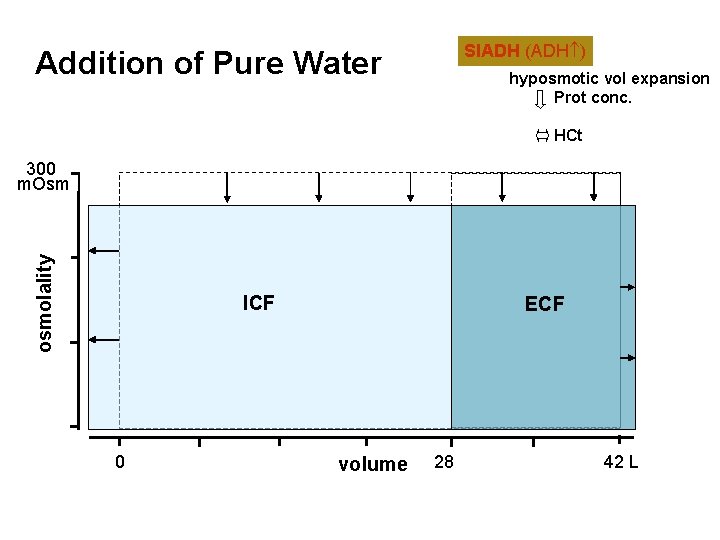
SIADH (ADH ) Addition of Pure Water hyposmotic vol expansion Prot conc. HCt osmolality 300 m. Osm ICF 0 ECF volume 28 42 L
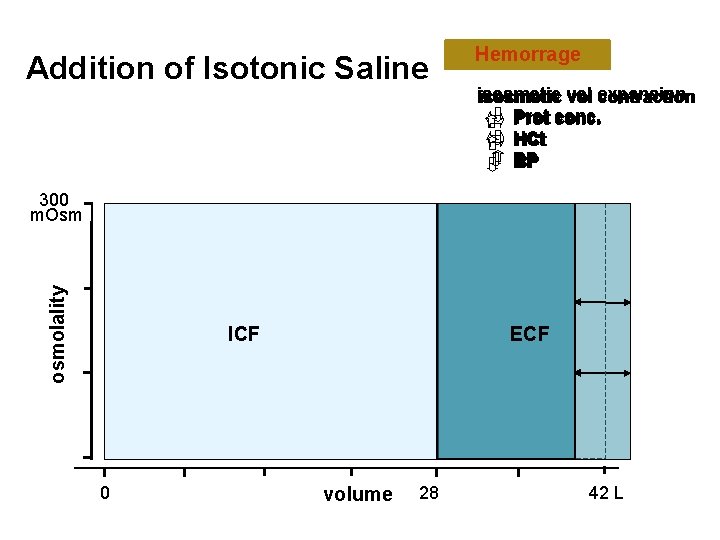
Addition of Isotonic Saline Diarrhea Hemorrage 0. 9% saline IV isosmotic vol expansion contraction Prot conc. HCt BP osmolality 300 m. Osm ICF 0 ECF volume 28 42 L
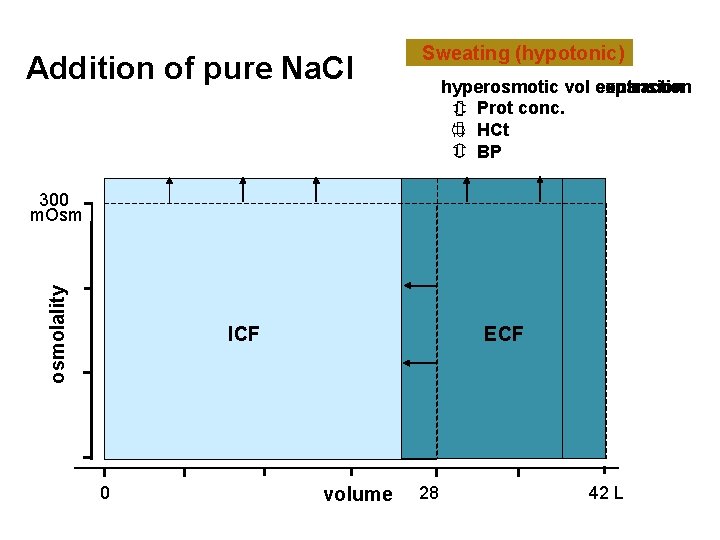
Addition of pure Na. Cl Sweating (hypotonic) Na. Cl addition hyperosmotic vol contraction expansion Prot conc. HCt BP osmolality 300 m. Osm ICF 0 ECF volume 28 42 L
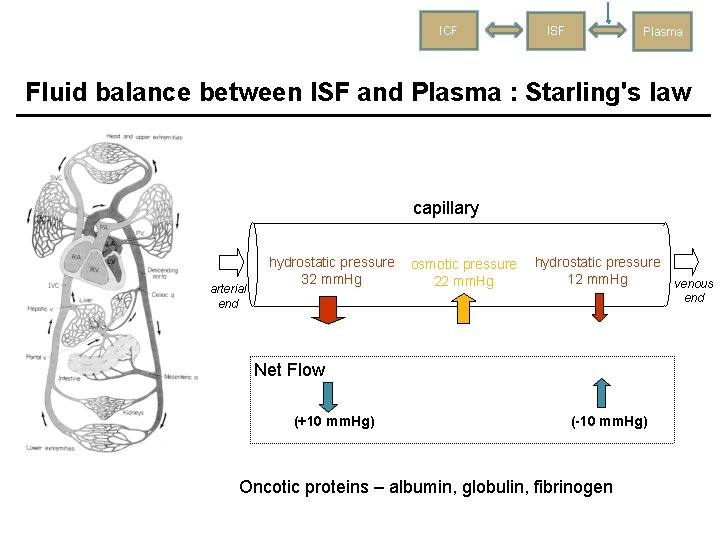
ICF ISF Plasma Fluid balance between ISF and Plasma : Starling's law capillary arterial end hydrostatic pressure 32 mm. Hg osmotic pressure 22 mm. Hg hydrostatic pressure 12 mm. Hg venous end Net Flow (+10 mm. Hg) (-10 mm. Hg) Oncotic proteins – albumin, globulin, fibrinogen
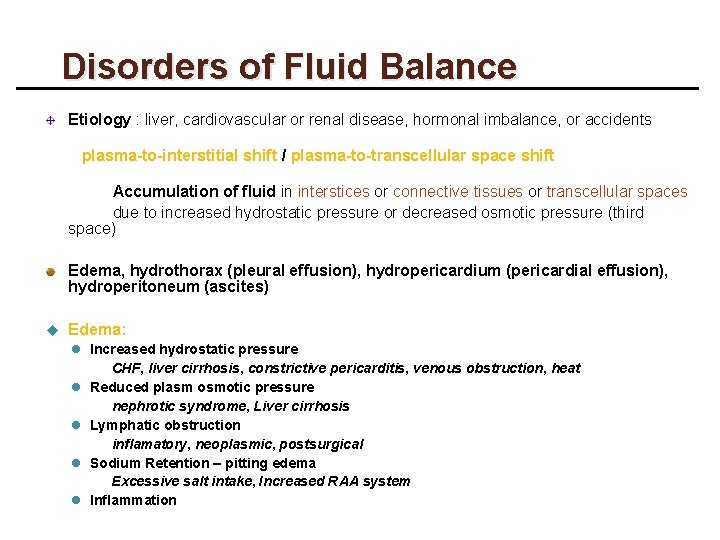
Disorders of Fluid Balance Etiology : liver, cardiovascular or renal disease, hormonal imbalance, or accidents plasma-to-interstitial shift / plasma-to-transcellular space shift Accumulation of fluid in interstices or connective tissues or transcellular spaces due to increased hydrostatic pressure or decreased osmotic pressure (third space) Edema, hydrothorax (pleural effusion), hydropericardium (pericardial effusion), hydroperitoneum (ascites) u Edema: l Increased hydrostatic pressure CHF, liver cirrhosis, constrictive pericarditis, venous obstruction, heat l Reduced plasm osmotic pressure nephrotic syndrome, Liver cirrhosis l Lymphatic obstruction inflamatory, neoplasmic, postsurgical l Sodium Retention – pitting edema Excessive salt intake, Increased RAA system l Inflammation

1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
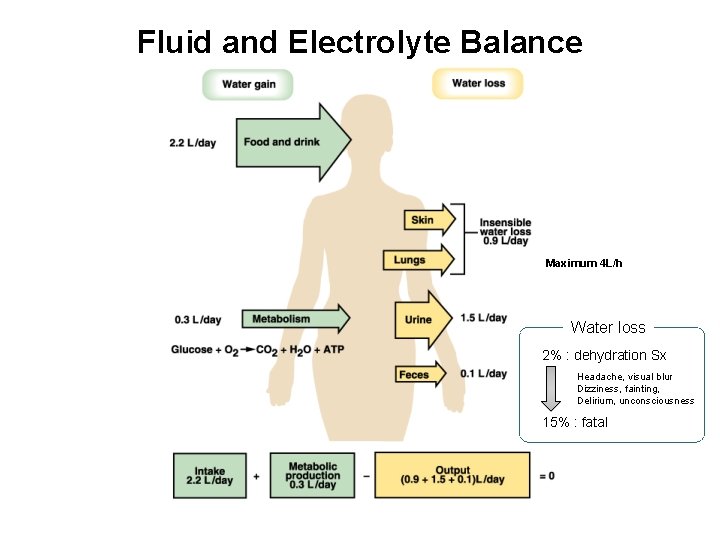
Fluid and Electrolyte Balance Maximum 4 L/h Water loss 2% : dehydration Sx Headache, visual blur Dizziness, fainting, Delirium, unconsciousness 15% : fatal
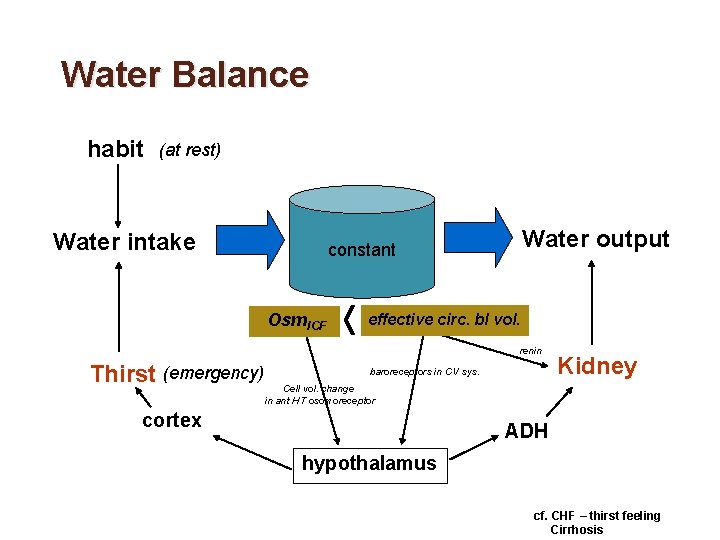
Water Balance habit (at rest) Water intake Water output constant Osm. ICF effective circ. bl vol. renin Thirst (emergency) baroreceptors in CV sys. Kidney Cell vol. change in ant HT osomoreceptor cortex ADH hypothalamus cf. CHF – thirst feeling Cirrhosis
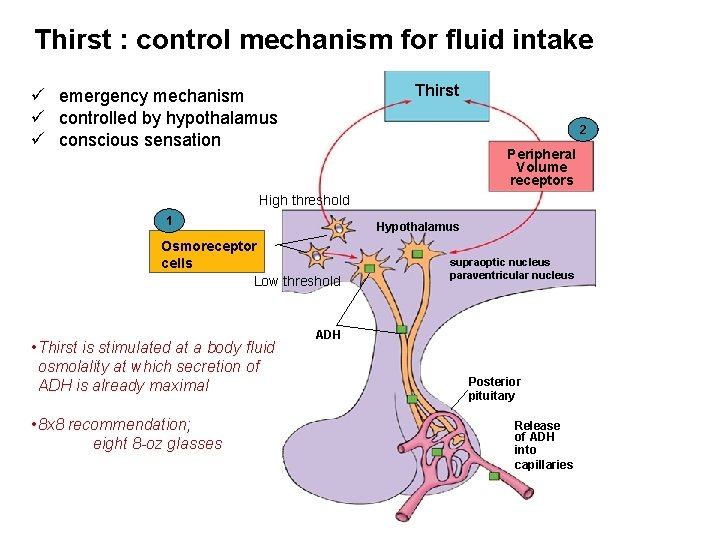
Thirst : control mechanism for fluid intake Thirst ü emergency mechanism ü controlled by hypothalamus ü conscious sensation 2 Peripheral Volume receptors High threshold 1 Hypothalamus Osmoreceptor cells Low threshold • Thirst is stimulated at a body fluid osmolality at which secretion of ADH is already maximal • 8 x 8 recommendation; eight 8 -oz glasses supraoptic nucleus paraventricular nucleus ADH Posterior pituitary Release of ADH into capillaries
1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
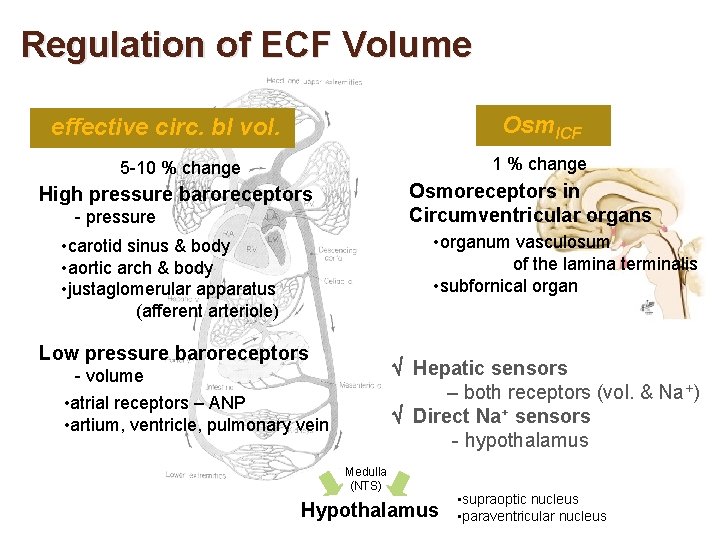
Regulation of ECF Volume Osm. ICF effective circ. bl vol. 1 % change 5 -10 % change Osmoreceptors in Circumventricular organs High pressure baroreceptors - pressure • organum vasculosum of the lamina terminalis • subfornical organ • carotid sinus & body • aortic arch & body • justaglomerular apparatus (afferent arteriole) Low pressure baroreceptors Hepatic sensors – both receptors (vol. & Na+) Direct Na+ sensors - hypothalamus - volume • atrial receptors – ANP • artium, ventricle, pulmonary vein Medulla (NTS) Hypothalamus • supraoptic nucleus • paraventricular nucleus
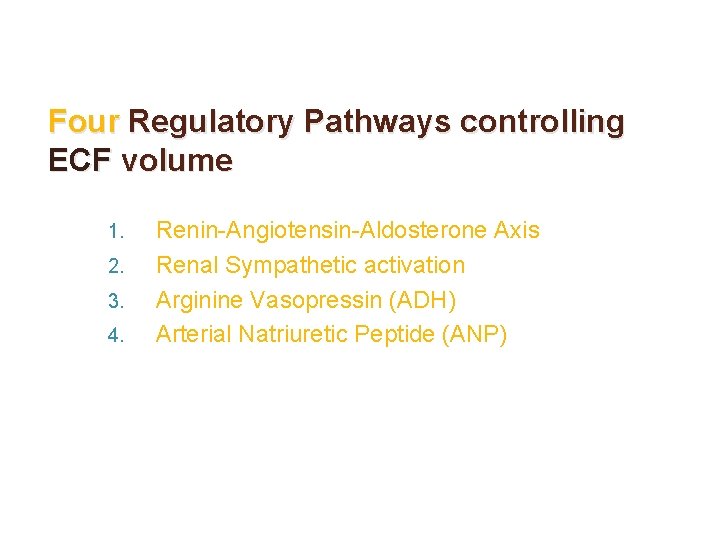
Four Regulatory Pathways controlling ECF volume 1. 2. 3. 4. Renin-Angiotensin-Aldosterone Axis Renal Sympathetic activation Arginine Vasopressin (ADH) Arterial Natriuretic Peptide (ANP)
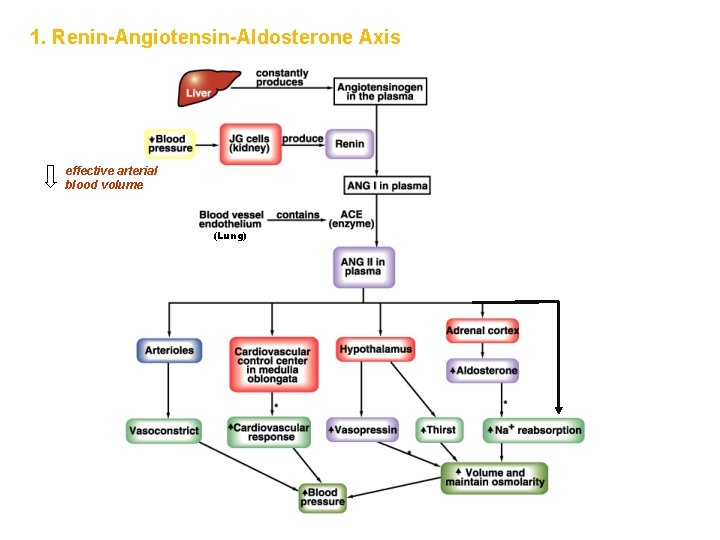
1. Renin-Angiotensin-Aldosterone Axis effective arterial blood volume (Lung)
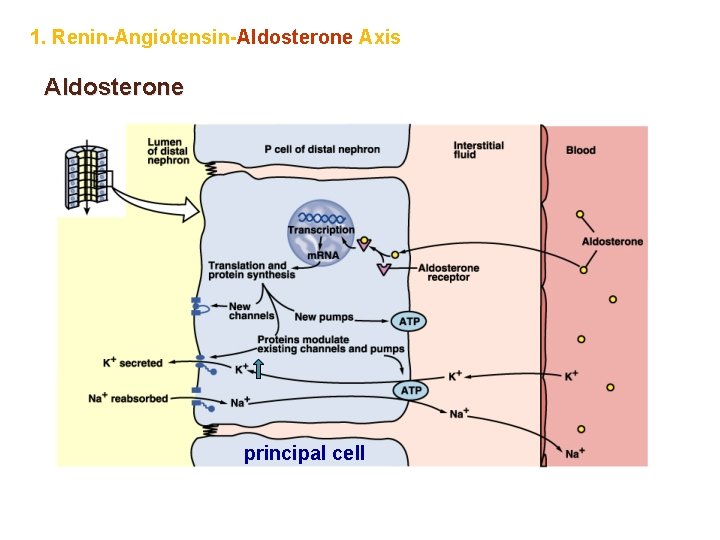
1. Renin-Angiotensin-Aldosterone Axis Aldosterone principal cell
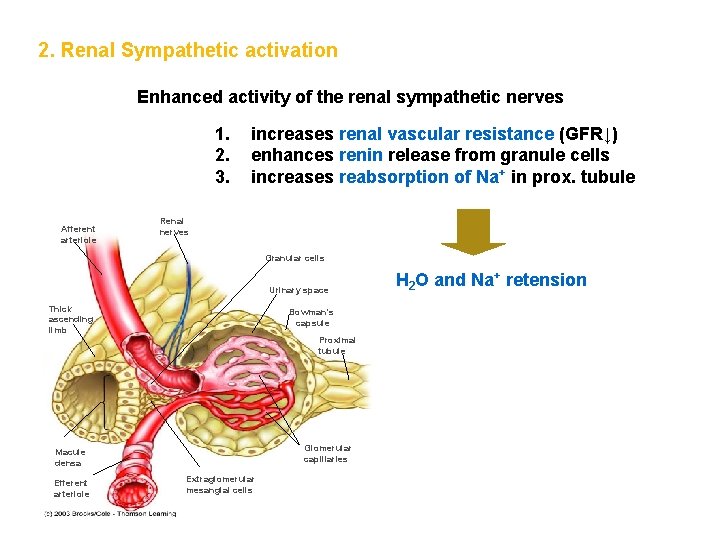
2. Renal Sympathetic activation Enhanced activity of the renal sympathetic nerves 1. 2. 3. Afferent arteriole increases renal vascular resistance (GFR↓) enhances renin release from granule cells increases reabsorption of Na+ in prox. tubule Renal nerves Granular cells Urinary space Thick ascending limb Bowman’s capsule Proximal tubule Glomerular capillaries Macule densa Efferent arteriole Extraglomerular mesangial cells H 2 O and Na+ retension
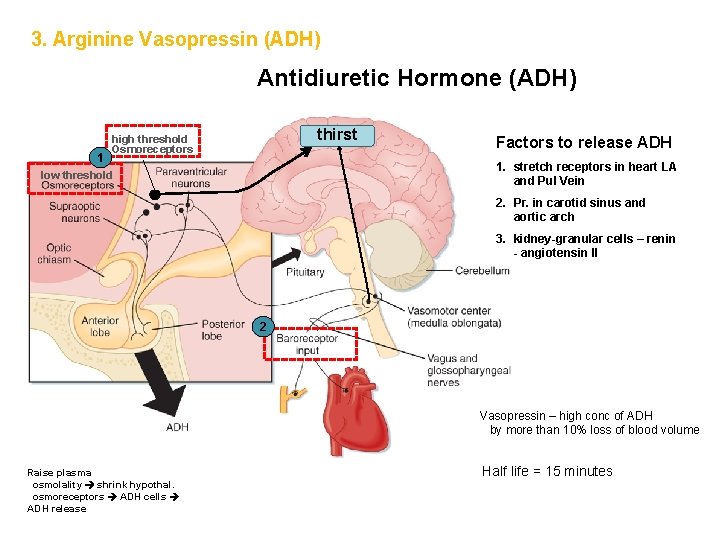
3. Arginine Vasopressin (ADH) Antidiuretic Hormone (ADH) 1 thirst high threshold Osmoreceptors Factors to release ADH 1. stretch receptors in heart LA and Pul Vein low threshold 2. Pr. in carotid sinus and aortic arch 3. kidney-granular cells – renin - angiotensin II 2 Vasopressin – high conc of ADH by more than 10% loss of blood volume Raise plasma osmolality shrink hypothal. osmoreceptors ADH cells ADH release Half life = 15 minutes
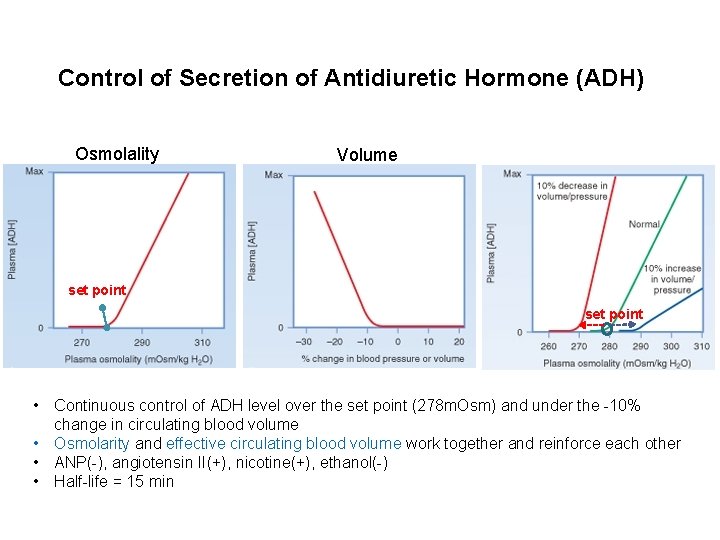
Control of Secretion of Antidiuretic Hormone (ADH) Osmolality Volume set point • Continuous control of ADH level over the set point (278 m. Osm) and under the -10% change in circulating blood volume • Osmolarity and effective circulating blood volume work together and reinforce each other • ANP(-), angiotensin II(+), nicotine(+), ethanol(-) • Half-life = 15 min
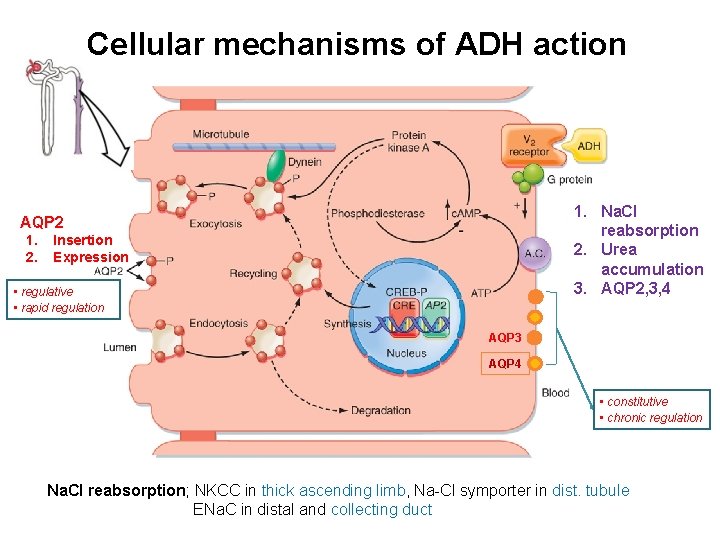
Cellular mechanisms of ADH action 1. Na. Cl reabsorption 2. Urea accumulation 3. AQP 2, 3, 4 AQP 2 1. 2. Insertion Expression • regulative • rapid regulation AQP 3 AQP 4 • constitutive • chronic regulation Na. Cl reabsorption; NKCC in thick ascending limb, Na-Cl symporter in dist. tubule ENa. C in distal and collecting duct
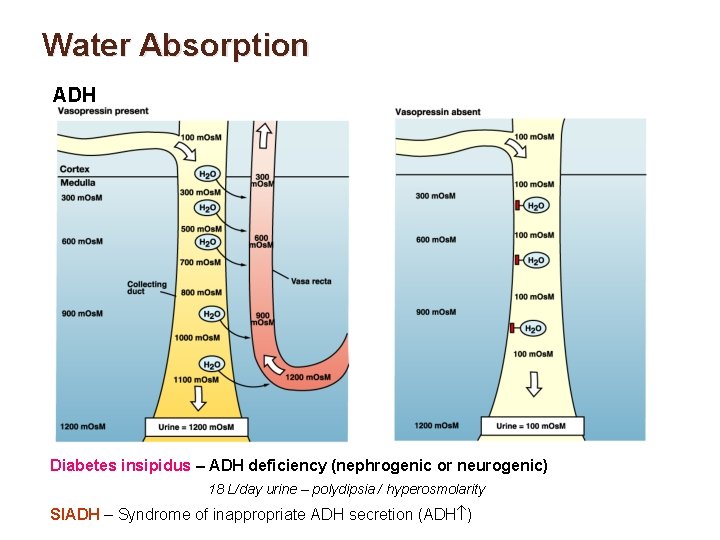
Water Absorption ADH Diabetes insipidus – ADH deficiency (nephrogenic or neurogenic) 18 L/day urine – polydipsia / hyperosmolarity SIADH – Syndrome of inappropriate ADH secretion (ADH )
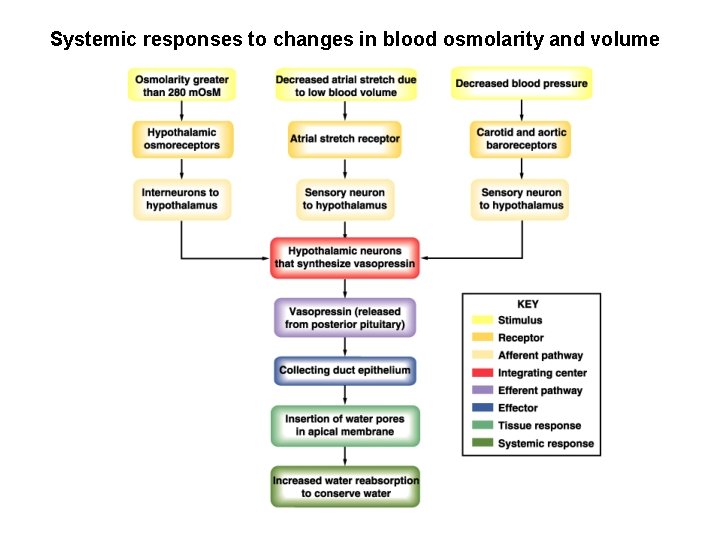
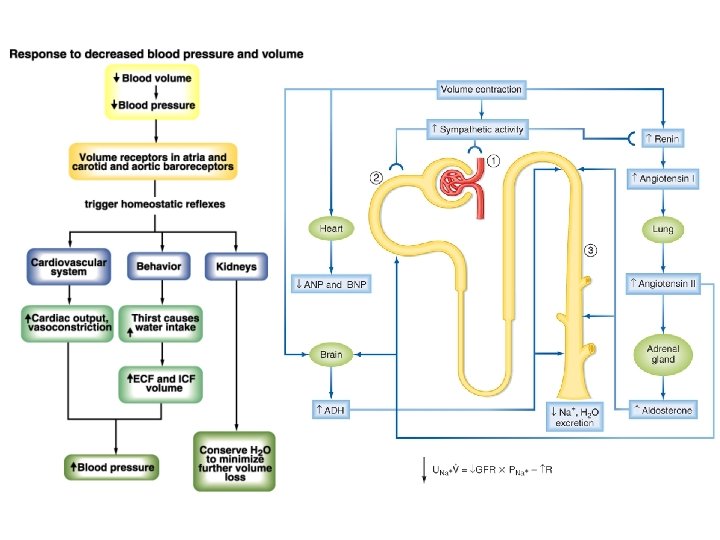
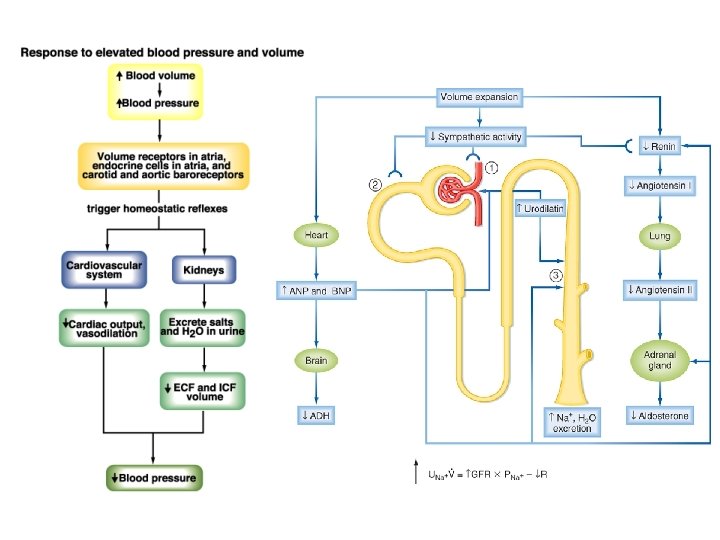
Systemic responses to changes in blood osmolarity and volume
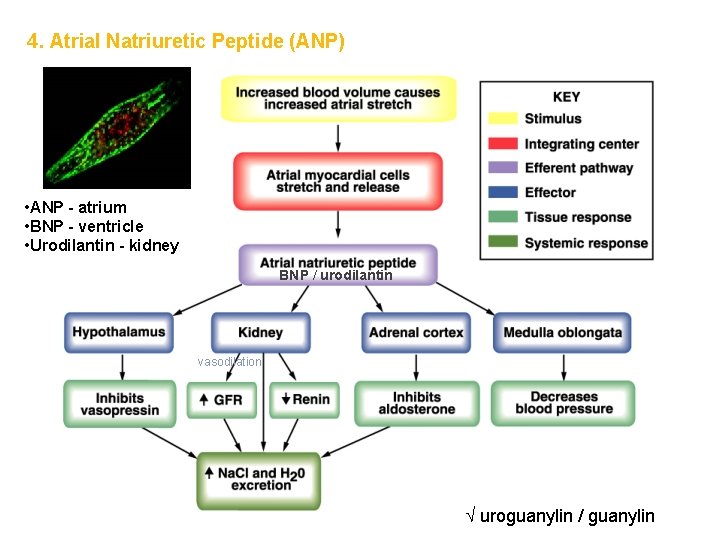
4. Atrial Natriuretic Peptide (ANP) • ANP - atrium • BNP - ventricle • Urodilantin - kidney BNP / urodilantin vasodilation uroguanylin / guanylin
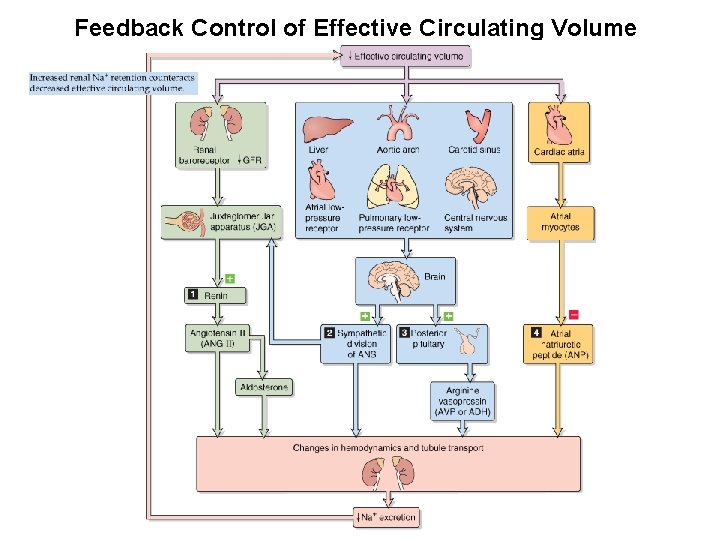
Feedback Control of Effective Circulating Volume
1. 2. 3. 4. 5. Distribution and measurement of body fluid compartments Compartmental fluid balance Systemic fluid balance : water intake & output Regulation mechanism of extracellular fluid volume Electrolytes balance
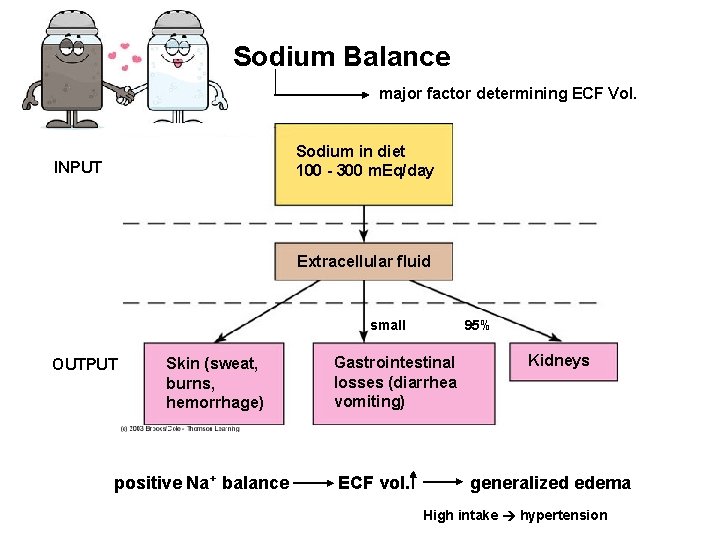
Sodium Balance major factor determining ECF Vol. Sodium in diet 100 - 300 m. Eq/day INPUT Extracellular fluid small OUTPUT Skin (sweat, burns, hemorrhage) positive Na+ balance 95% Gastrointestinal losses (diarrhea vomiting) ECF vol. Kidneys generalized edema High intake hypertension
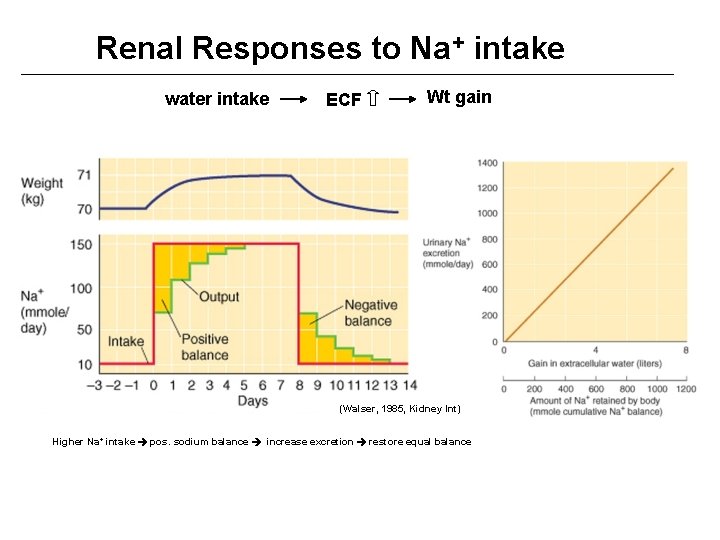
Renal Responses to Na+ intake water intake ECF Wt gain (Walser, 1985, Kidney Int) Higher Na+ intake pos. sodium balance increase excretion restore equal balance
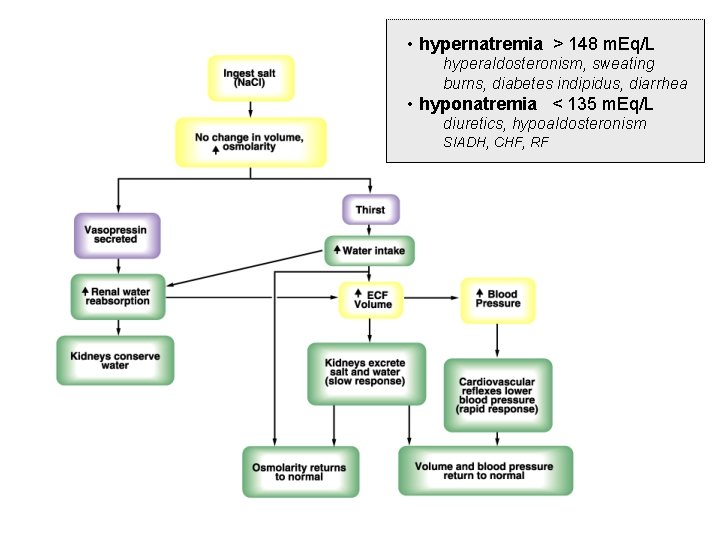
• hypernatremia > 148 m. Eq/L hyperaldosteronism, sweating burns, diabetes indipidus, diarrhea • hyponatremia < 135 m. Eq/L diuretics, hypoaldosteronism SIADH, CHF, RF
Kidney Failure Uremia (urine in blood) u Lack of erythropoietin anemia u Plasma urea creatinine and uric acid azotemia u Lack of vitamin D activation bone disease u Increased ECF hypertension u Decreased H+ secretion metabolic acidosis u decreased GFR hyperkalemia ESRD: End State Renal Disease, GFR <10% of Normal Diabetes, hypertension, glomerulonephritis, polycytic kidney disease
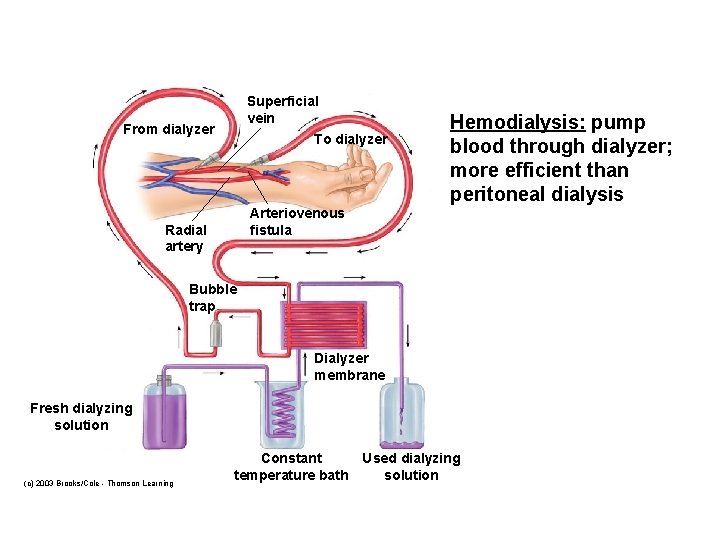
Superficial vein From dialyzer To dialyzer Hemodialysis: pump blood through dialyzer; more efficient than peritoneal dialysis Arteriovenous fistula Radial artery Bubble trap Dialyzer membrane Fresh dialyzing solution (c) 2003 Brooks/Cole - Thomson Learning Constant temperature bath Used dialyzing solution
- Slides: 45