Fluid and Electrolyte Abnormalities Hypovolemia l l l
Fluid and Electrolyte Abnormalities
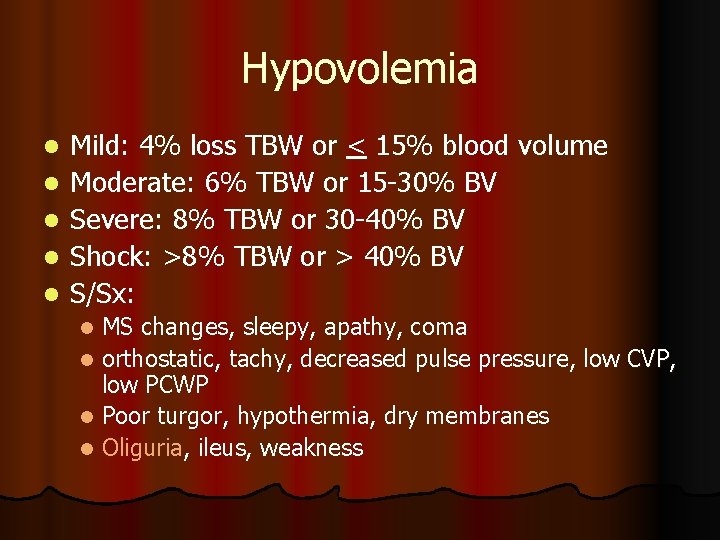
Hypovolemia l l l Mild: 4% loss TBW or < 15% blood volume Moderate: 6% TBW or 15 -30% BV Severe: 8% TBW or 30 -40% BV Shock: >8% TBW or > 40% BV S/Sx: MS changes, sleepy, apathy, coma l orthostatic, tachy, decreased pulse pressure, low CVP, low PCWP l Poor turgor, hypothermia, dry membranes l Oliguria, ileus, weakness l
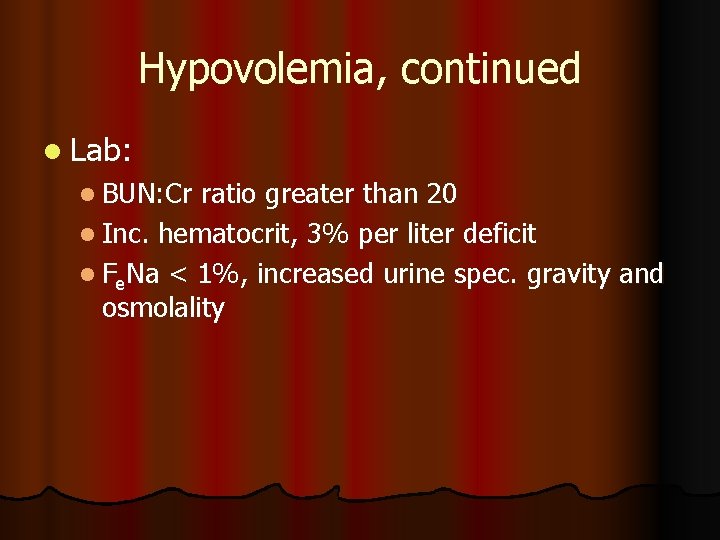
Hypovolemia, continued l Lab: l BUN: Cr ratio greater than 20 l Inc. hematocrit, 3% per liter deficit l Fe. Na < 1%, increased urine spec. gravity and osmolality
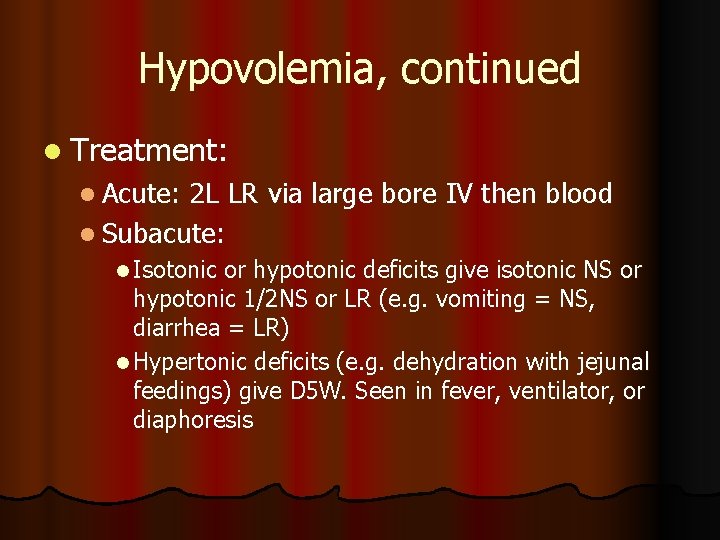
Hypovolemia, continued l Treatment: l Acute: 2 L LR via large bore IV then blood l Subacute: l Isotonic or hypotonic deficits give isotonic NS or hypotonic 1/2 NS or LR (e. g. vomiting = NS, diarrhea = LR) l Hypertonic deficits (e. g. dehydration with jejunal feedings) give D 5 W. Seen in fever, ventilator, or diaphoresis
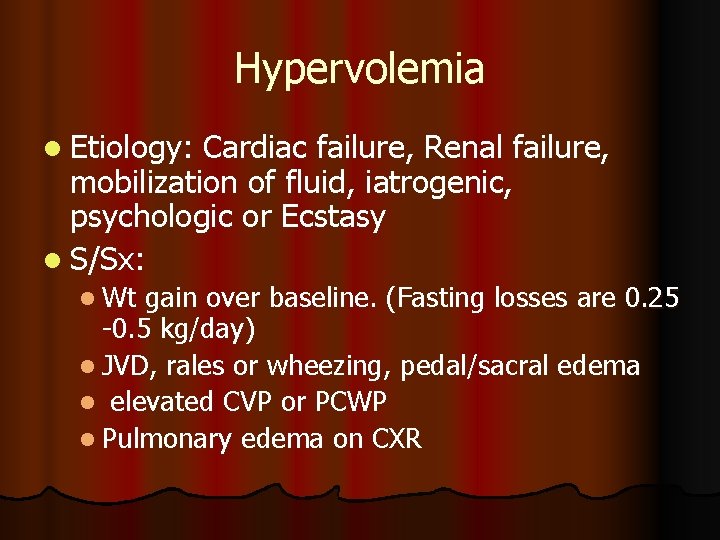
Hypervolemia l Etiology: Cardiac failure, Renal failure, mobilization of fluid, iatrogenic, psychologic or Ecstasy l S/Sx: l Wt gain over baseline. (Fasting losses are 0. 25 -0. 5 kg/day) l JVD, rales or wheezing, pedal/sacral edema l elevated CVP or PCWP l Pulmonary edema on CXR
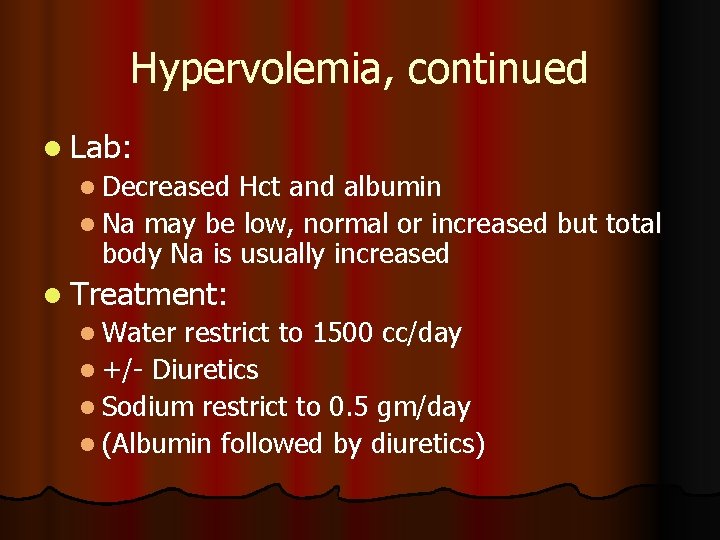
Hypervolemia, continued l Lab: l Decreased Hct and albumin l Na may be low, normal or increased but total body Na is usually increased l Treatment: l Water restrict to 1500 cc/day l +/- Diuretics l Sodium restrict to 0. 5 gm/day l (Albumin followed by diuretics)
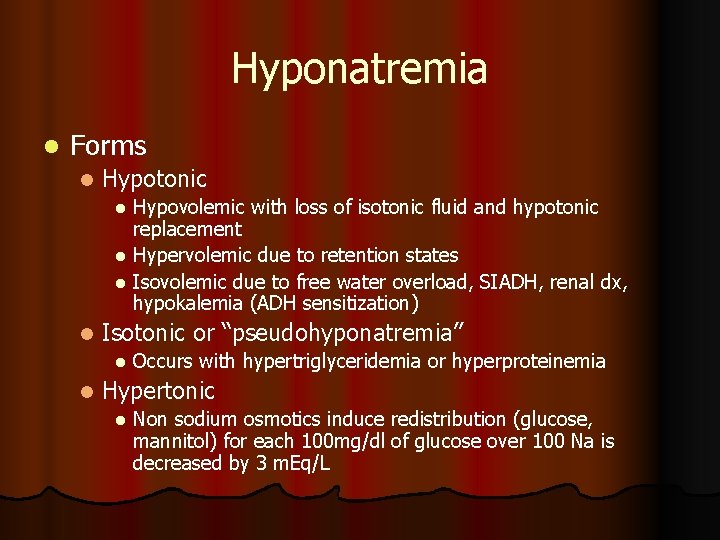
Hyponatremia l Forms l Hypotonic Hypovolemic with loss of isotonic fluid and hypotonic replacement l Hypervolemic due to retention states l Isovolemic due to free water overload, SIADH, renal dx, hypokalemia (ADH sensitization) l l Isotonic or “pseudohyponatremia” l l Occurs with hypertriglyceridemia or hyperproteinemia Hypertonic l Non sodium osmotics induce redistribution (glucose, mannitol) for each 100 mg/dl of glucose over 100 Na is decreased by 3 m. Eq/L
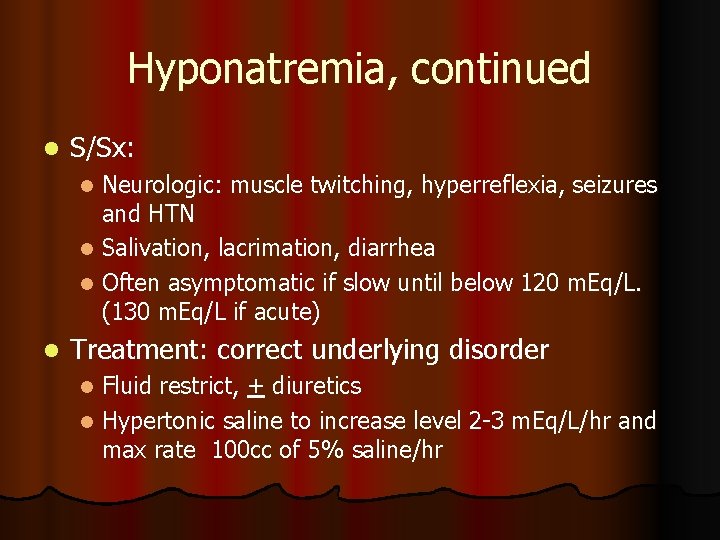
Hyponatremia, continued l S/Sx: Neurologic: muscle twitching, hyperreflexia, seizures and HTN l Salivation, lacrimation, diarrhea l Often asymptomatic if slow until below 120 m. Eq/L. (130 m. Eq/L if acute) l l Treatment: correct underlying disorder Fluid restrict, + diuretics l Hypertonic saline to increase level 2 -3 m. Eq/L/hr and max rate 100 cc of 5% saline/hr l
Hypernatremia l Free water deficit or water loss greater than salt loss. Always assoc with hyper osmolar state. l Forms: l Hypervolemic: loss of hypotonic fluids with inadequate replacement with hypertonic fluids l Isovolemic is subclinical hypovolemia seen in diabetes insipidus l Hypervolemic usually iatrogenic, also Cushing’s, Conn’s, CAH
Hypernatremia, continued l S/Sx: Neurologic: restless, seizure, coma, delirium and mania l Sticky mucus membranes, poor salivation/lacrimation, hyperpyrexia, Red swollen tongue l THIRST, weakness l l Treatment: correct underlying disorder l Free water replacement: (0. 6 * kg BW) * ((Na/140) – 1). Slow infusion of D 5 W give ½ over first 8 hrs then rest over next 16 -24 hrs to avoid cerebral edema.
Hypokalemia l Etiology: Intracellular uptake with redistribution seen in acute alkalosis, inmsulin therapy, and anabolism l Depletion due to GI losses, renal/diuretics, steroids, and renal tubular acidosis l l S/Sx: Clinical: muscle weakness/fatigue, decreased DTR’s, ileus. Insulin resistance in DM l EKG: low, flat T-waves, ST depression, and U waves l
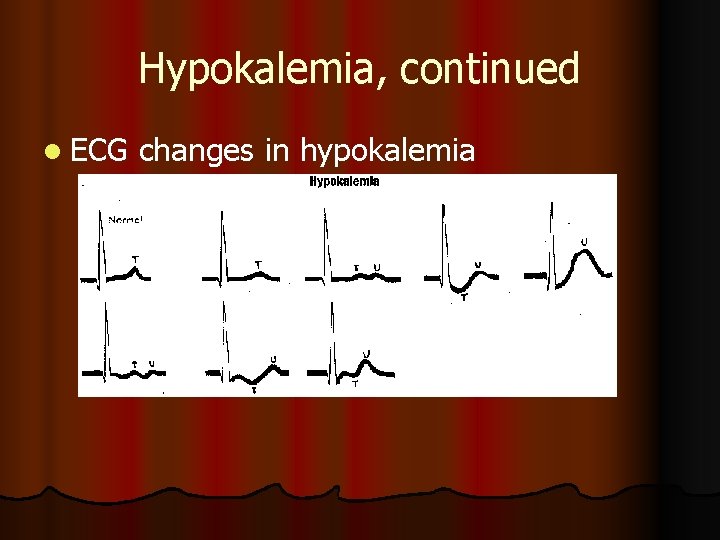
Hypokalemia, continued l ECG changes in hypokalemia
Hypokalemia, continued l Treatment: l Check renal function l Treat alkalosis, decrease sodium intake l PO with 20 -40 m. Eq doses l IV: peripheral 7. 5 m. Eq/hr, central 20 m. Eq/hr and increase K+ in maintenance fluids.
Hyperkalemia l Etiology: l Psuedohyperkalemia in leukocytosis, hemolysis and thrombocytosis l Redistribution in acidosis, hypoinsulinism, tissue necrosis, digoxin poisoning l Renal insufficiency, mineralocorticoid deficiency, DM, spironolactone use
Hyperkalemia, continued l S/Sx: l Clinical: nausea/vomiting, colic, weakness diarrhea l EKG: early – peaked T waves then flat P waves, depressed ST segment, widened QRS progressing to sine wave and V fib. l Cardiac arrest occurs in diastole
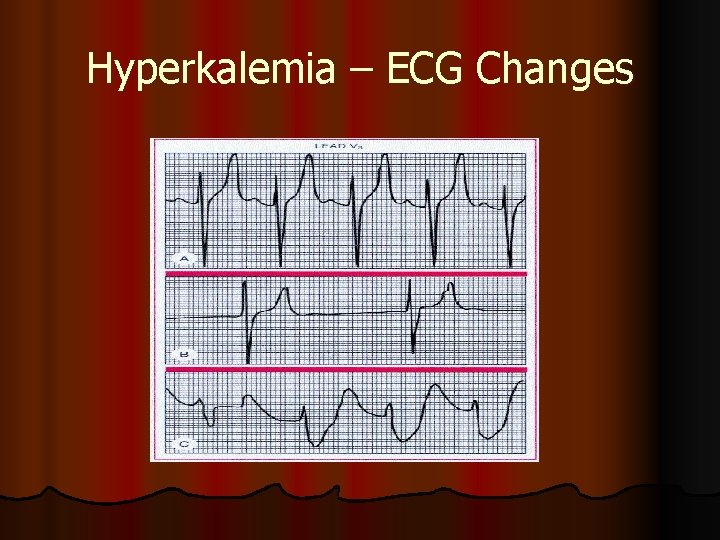
Hyperkalemia – ECG Changes
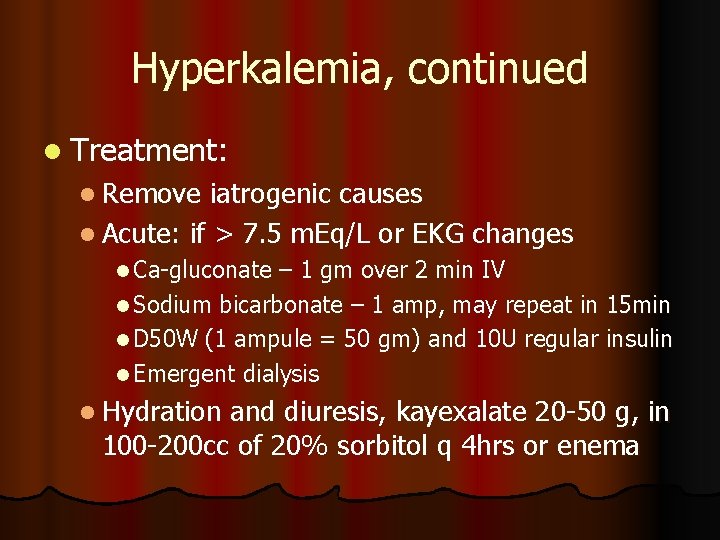
Hyperkalemia, continued l Treatment: l Remove iatrogenic causes l Acute: if > 7. 5 m. Eq/L or EKG changes l Ca-gluconate – 1 gm over 2 min IV l Sodium bicarbonate – 1 amp, may repeat in 15 min l D 50 W (1 ampule = 50 gm) and 10 U regular insulin l Emergent dialysis l Hydration and diuresis, kayexalate 20 -50 g, in 100 -200 cc of 20% sorbitol q 4 hrs or enema
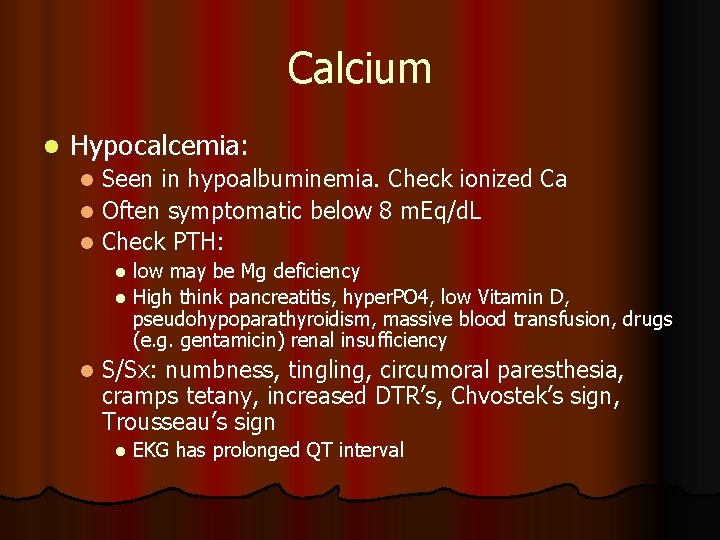
Calcium l Hypocalcemia: Seen in hypoalbuminemia. Check ionized Ca l Often symptomatic below 8 m. Eq/d. L l Check PTH: l low may be Mg deficiency l High think pancreatitis, hyper. PO 4, low Vitamin D, pseudohypoparathyroidism, massive blood transfusion, drugs (e. g. gentamicin) renal insufficiency l l S/Sx: numbness, tingling, circumoral paresthesia, cramps tetany, increased DTR’s, Chvostek’s sign, Trousseau’s sign l EKG has prolonged QT interval
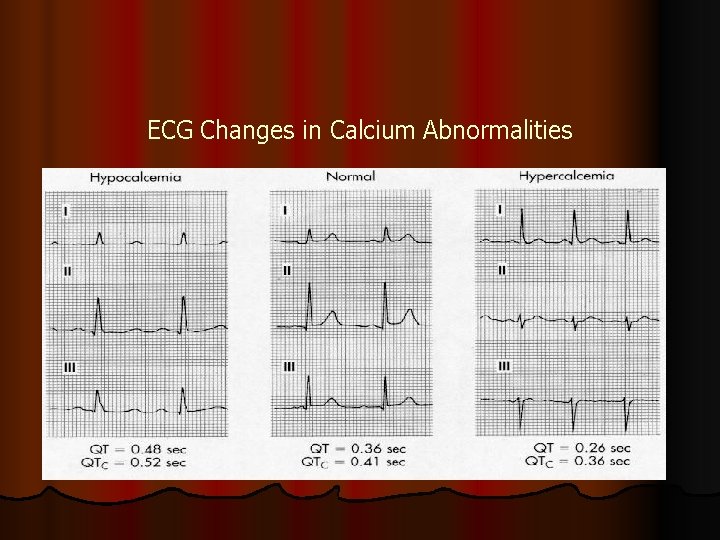
ECG Changes in Calcium Abnormalities
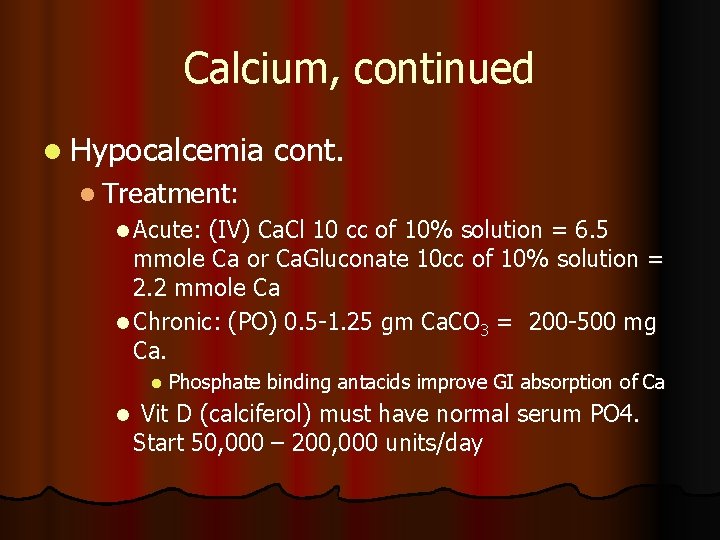
Calcium, continued l Hypocalcemia cont. l Treatment: l Acute: (IV) Ca. Cl 10 cc of 10% solution = 6. 5 mmole Ca or Ca. Gluconate 10 cc of 10% solution = 2. 2 mmole Ca l Chronic: (PO) 0. 5 -1. 25 gm Ca. CO 3 = 200 -500 mg Ca. l l Phosphate binding antacids improve GI absorption of Ca Vit D (calciferol) must have normal serum PO 4. Start 50, 000 – 200, 000 units/day
Calcium, continued l Hypercalcemia Usually secondary to hyperparathyroidism or malignancy. Other causes are thiazides, milk-alkali syndrome, granulomatous disease, acute adrenal insufficiency l Acute crisis is serum Ca> 12 mg/d. L. Critical at 1620 mg/d. L l S/Sx: N/V, anorexia, abdominal pain, confusion, lethargy MS changes= “Bones, stone, abdominal groans and psychic overtones. ” l
Calcium, continued l Treatment: Hydration with NS then loop diuretic. Steroids for lymphoma, multiple myeloma, adrenal insufficiency, bone mets, Vit D intoxication. May need Hemodialysis. l Mithramycin for malignancy induced hyper. Ca refractory to other treatment. Give 15 -25 mcg/kg IVP l Calcitonin in malignant PTH syndromes
Magnesium l Hypomagnesemia l Malnutrition, burns, pancreatitis, SIADH, parathyroidectomy, primary hyperaldosteronism l S/Sx: weakness, fatigue, MS changes, hyperreflexia, seizure, arrhythmia l Treatment: IV replacement of 2 -4 gm of Mg. SO 4 per day or oral replacement
Magnesium, continued l Hypermagnesemia l Renal insufficiency, antacid abuse, adrenal insufficiency, hypothyroidism, iatrogenic l S/Sx: N/V, weakness, MS changes, hyporeflexia, paralysis of voluntary muscles, EKG has AV block and prolonged QT interval. l Treatment: Discontinue source, IV Ca. Gluconate for acute Rx, Dialysis
Phosphate l Hypophosphatemia l Seen in hyperalimentation, after starvation, DKA, malabsorption, phosphate binding antacids, alkalosis, hemodialysis, hyperparathyroidism l S/Sx: myocardial depression due to low ATP, shift of oxyhemoglobin curve to left due to low 2, 3 DPG, anorexia, bone pain, hemolysis, cardiac arrest
Phosphate l Treatment: PO replacement (Neutraphos) or IV KPhos or Na. Phos 0. 08 -0. 20 m. M/kg over 6 hrs l Hyperphosphatemia l Renal insufficiency, hypoparathyroidism, may produce metastatic calcification l Treat with restriction and phosphate-binding antacid (Amphogel)
Zinc l l l 1 -2 gm in body (brain, pancreas, liver, kidney, prostate and testis) Enzyme activator and cofactor Deficiency in malabsorption, trauma, IBD, refeeding syndrome, cancer or diarrhea Absorbed in terminal ileum S/Sx: “ 4 D’s” – diarrhea, depression, dermatitis, dementia l l Also alopecia, nyctalopia, tremor, loss of taste Treat with zinc sulfate 3 -6 mg/day if with (normal number of stools)
- Slides: 27