FLU The underestimated threat Influenza Virus Types Type




- Slides: 39

FLU The underestimated threat.
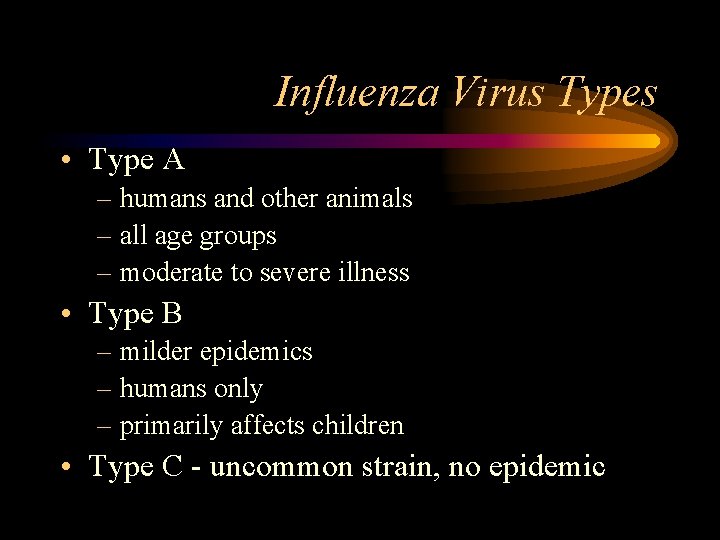
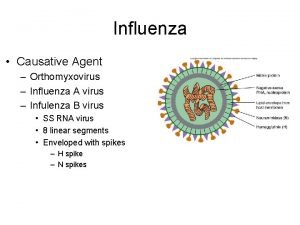
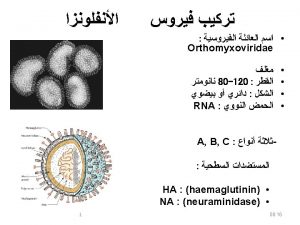
Influenza Virus Types • Type A – humans and other animals – all age groups – moderate to severe illness • Type B – milder epidemics – humans only – primarily affects children • Type C - uncommon strain, no epidemic
Increased Risk • • Age 65 and older Any age with chronic medical conditions Pregnant women Children 6 -23 months
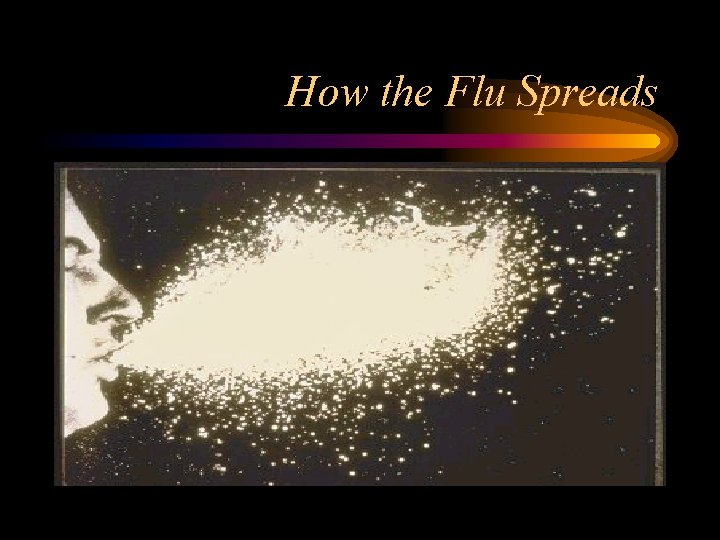
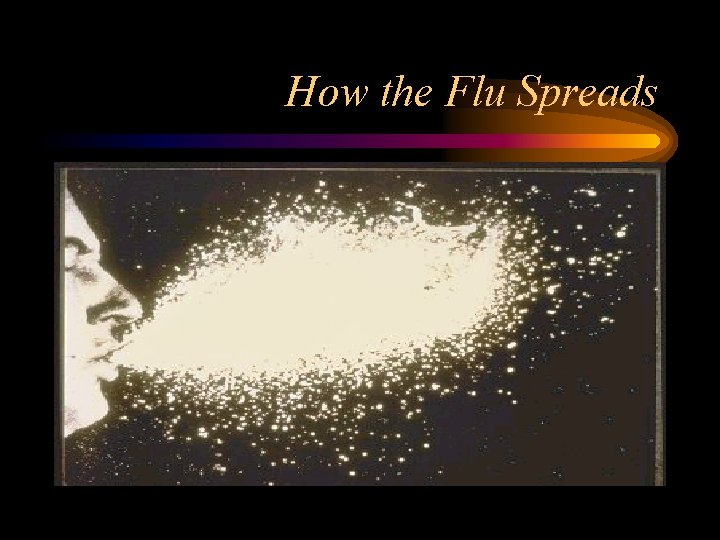
How the Flu Spreads
Spread of Flu • Droplet Spread – from a person’s cough or sneeze – person touches respiratory droplets on another person or object and then touches their own mouth or nose • Incubation period = 1 -4 days
Symptoms • Adults- shed virus 1 day before developing symptoms to 7 days after getting sick • Young children- can shed virus for longer than 7 days
Hospitalization from Influenza • Highest rate among young children and persons >65 yrs • 114, 000 hospitalizations/yr with 57% occurring in ages < 65 yrs • Highest # caused by type A (H 3 N 2) viruses
Death rates from influenza-associated pulmonary and circulation deaths/100, 000 persons • • 0 -44 yr: 0. 4 - 0. 6 50 -64 yr: 7. 5 65 yrs: 98. 3 Reasons: – more older people has inc. – Influenza A associated with higher mortality – Influenza A predominates in 90% of seasons from 1990 -99 compared w/57% of seasons 1976 -90
Preventing the Flu • Good Health Habits • Vaccination • Antiviral Medications
Good Health Habits • Avoid close contact • Stay home when you are sick • Cover your mouth • Clean your hand • Avoid touching your eyes, nose or mouth • Get plenty of rest • Drink plenty of liquids • The simplest way to avoid the flu is to avoid crowds. Can’t keep you kids cooped up? Frequent hand washing is the next best thing
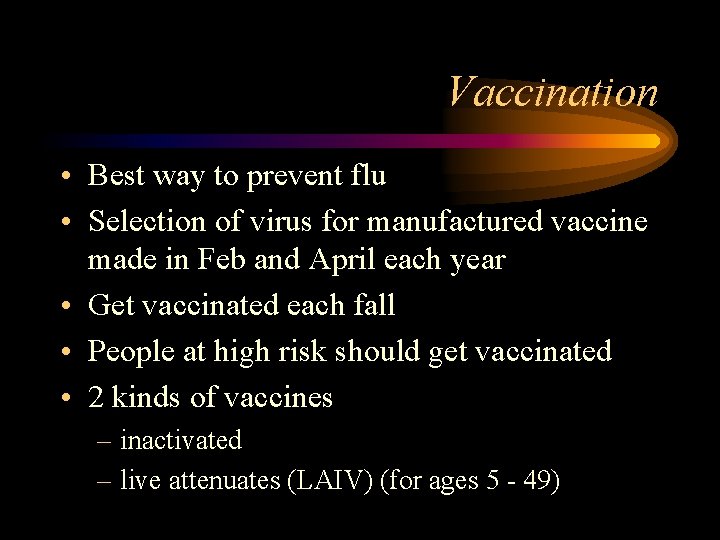
Vaccination
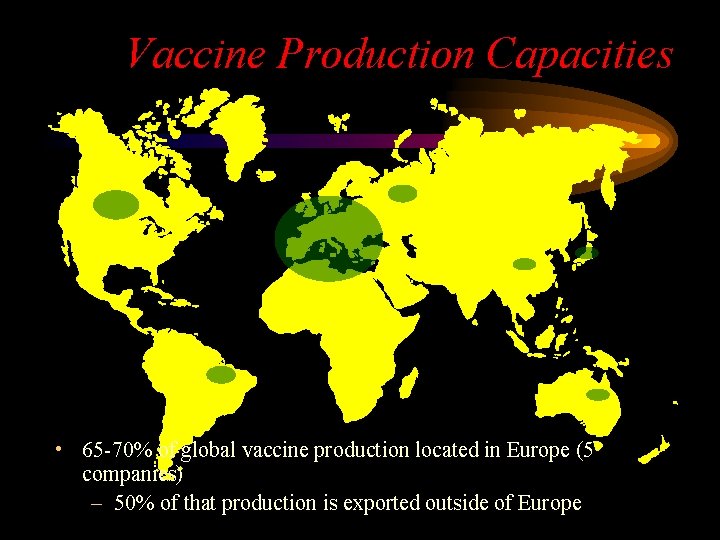
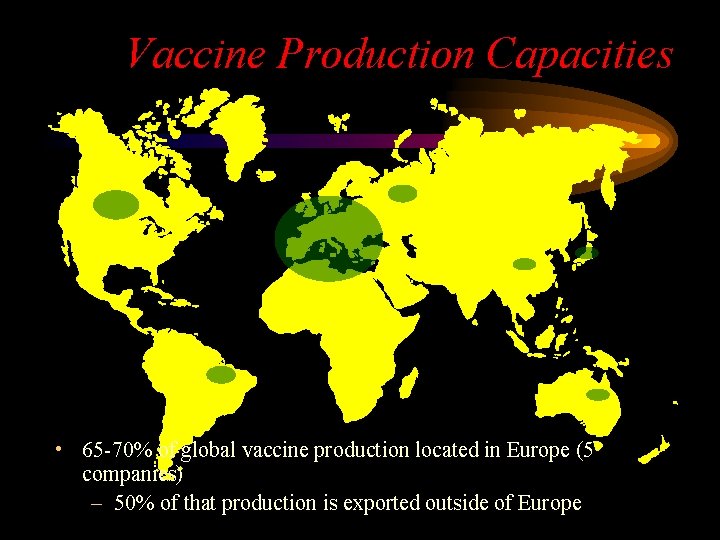
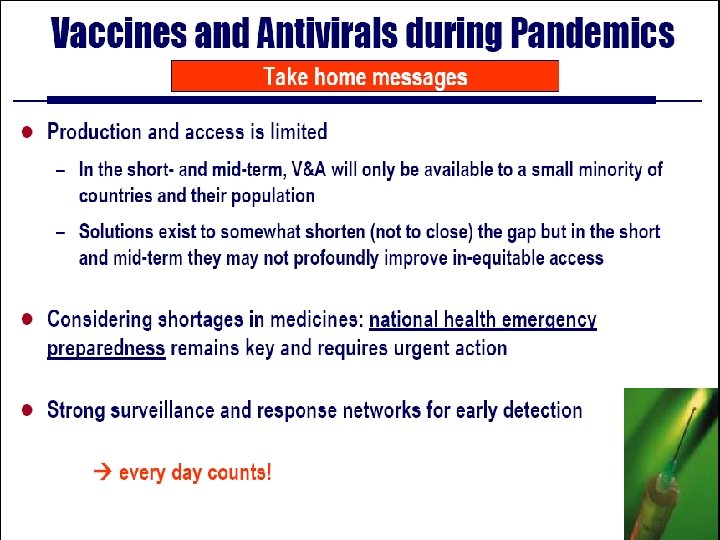
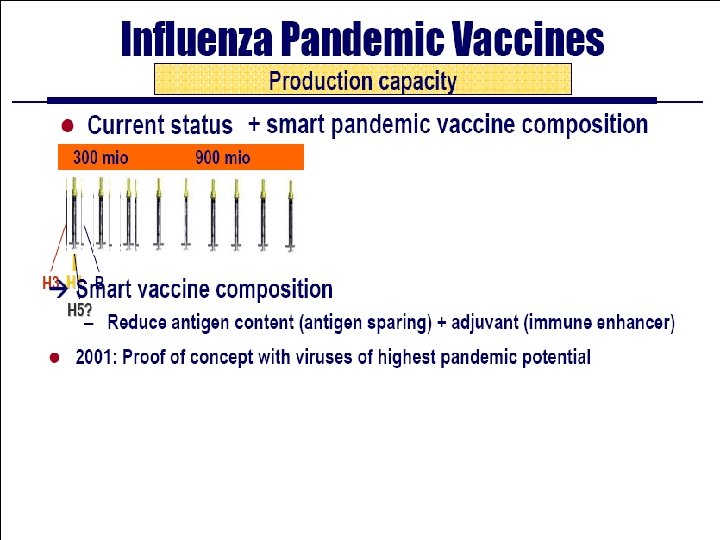
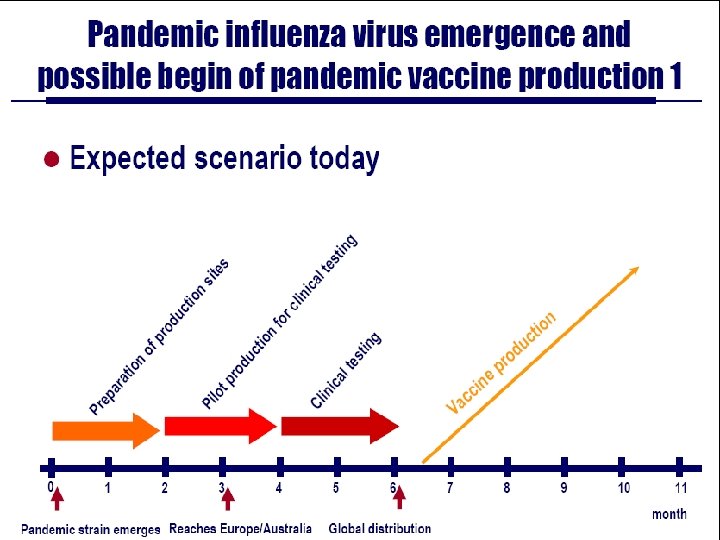
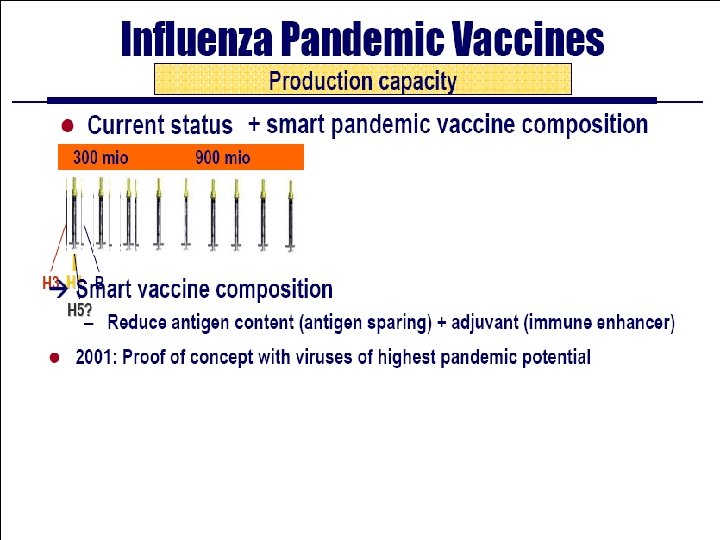
Vaccine Production Capacities • 65 -70% of global vaccine production located in Europe (5 companies) – 50% of that production is exported outside of Europe
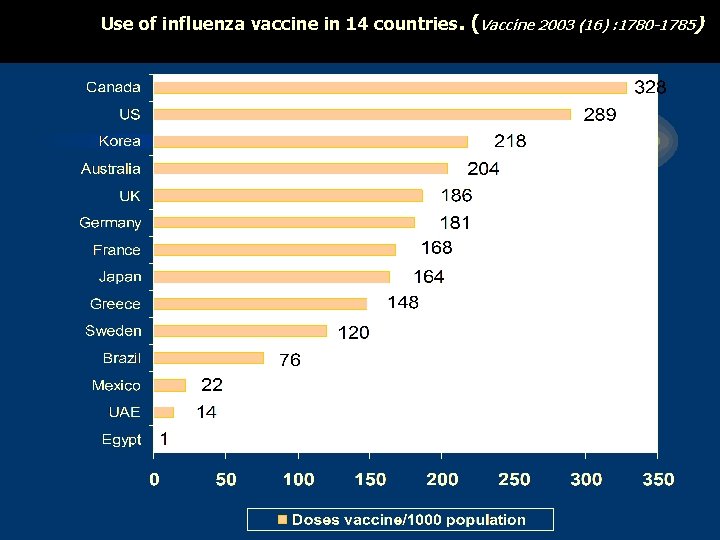
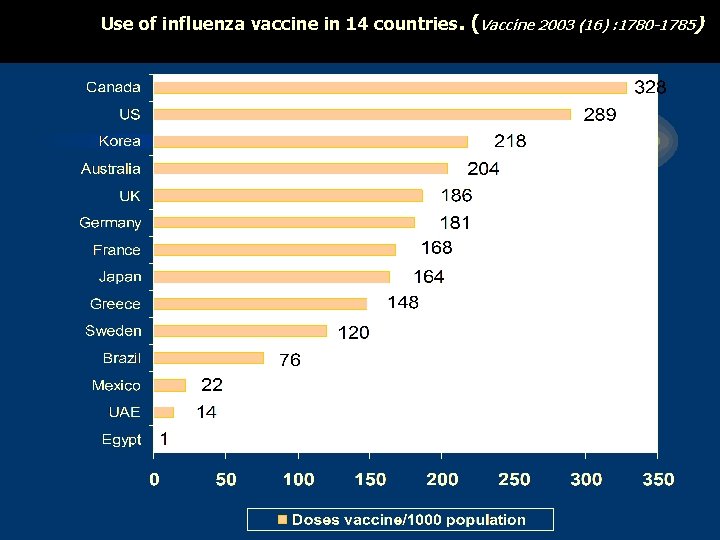
Use of influenza vaccine in 14 countries. (Vaccine 2003 (16) : 1780 -1785)
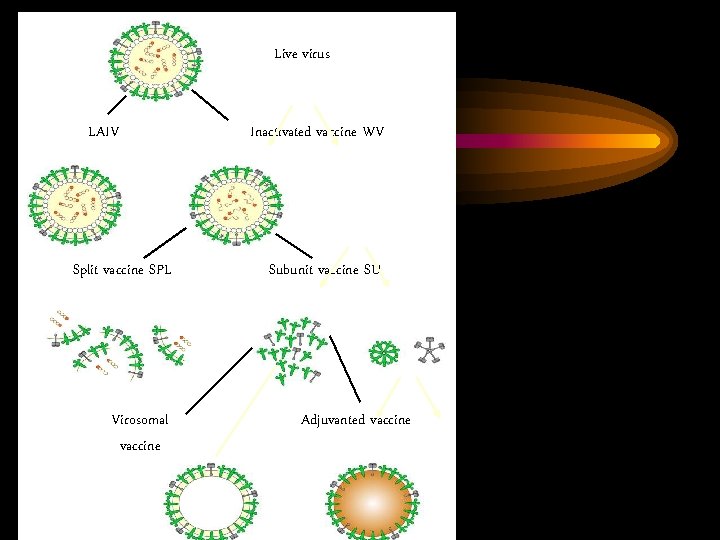
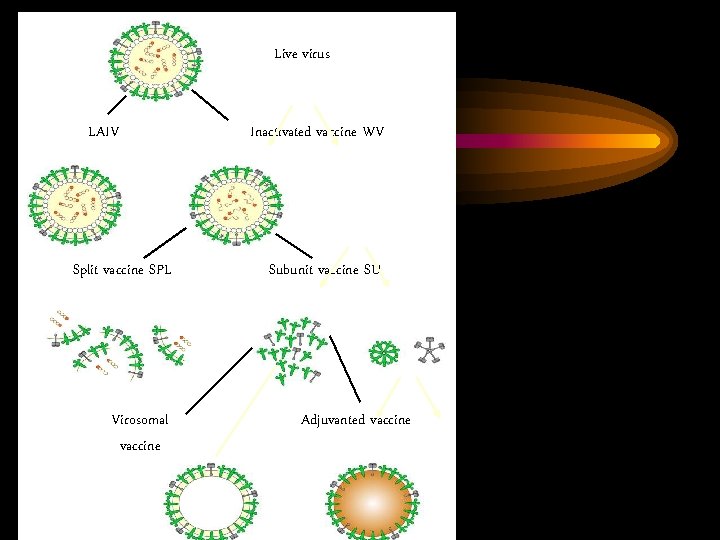
Live virus LAIV Split vaccine SPL Inactivated vaccine WV Subunit vaccine SU rosettes Virosomal vaccine Adjuvanted vaccine
Vaccination • Best way to prevent flu • Selection of virus for manufactured vaccine made in Feb and April each year • Get vaccinated each fall • People at high risk should get vaccinated • 2 kinds of vaccines – inactivated – live attenuates (LAIV) (for ages 5 - 49)
Who Should Not Get Vaccine • Have severe allergy to hen’s eggs (anaphylactic allergic rxn) • People who previously developed Guillian. Barre syndrome (GBS) w/in 6 weeks after getting a flu shot
Influenza Vaccination Strategy • Yearly vaccination of high risk persons is the most effective means of reducing the effect of influenza – persons with increased risk – close contacts and care-givers of persons with increased risk
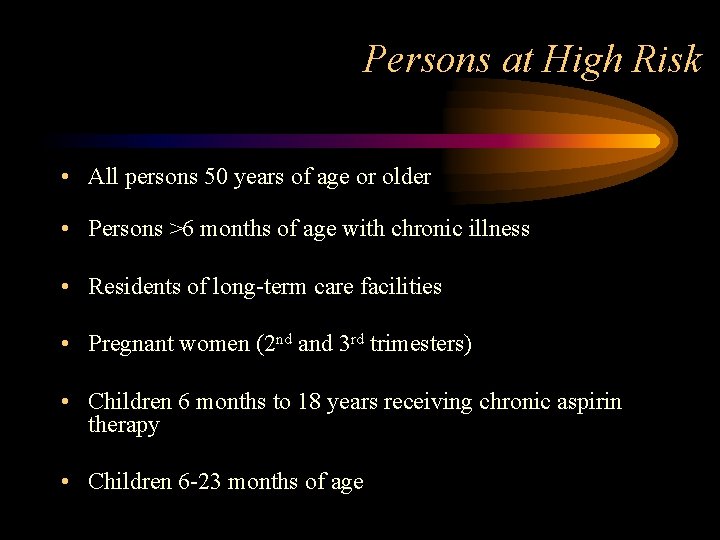
Persons at High Risk • All persons 50 years of age or older • Persons >6 months of age with chronic illness • Residents of long-term care facilities • Pregnant women (2 nd and 3 rd trimesters) • Children 6 months to 18 years receiving chronic aspirin therapy • Children 6 -23 months of age
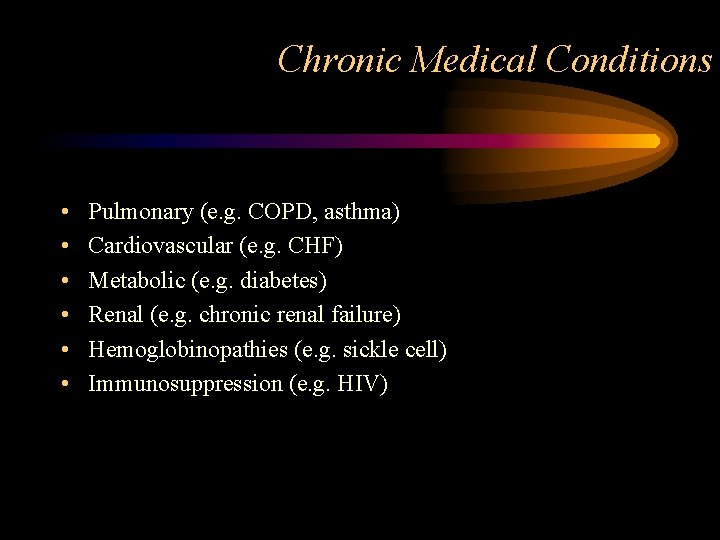
Chronic Medical Conditions • • • Pulmonary (e. g. COPD, asthma) Cardiovascular (e. g. CHF) Metabolic (e. g. diabetes) Renal (e. g. chronic renal failure) Hemoglobinopathies (e. g. sickle cell) Immunosuppression (e. g. HIV)
HIV Infection • Persons with HIV at higher risk for complications of influenza • Vaccine induces protective antibody titers in many HIV-infected persons • Transient increase in HIV replication reported • Vaccine will benefit many HIV-infected persons
Pregnancy and Inactivated Influenza Vaccine • Risk of hospitalization 4 times higher than nonpregnant women • Risk of complications comparable to nonpregnant women with high-risk medical conditions • Vaccination recommended if pregnant during influenza season
Contacts of High-Risk Persons • Household members and caregivers of high-risk persons (including children 0 -23 months) • Health care providers, including home care • Employees of long-term care facilities
Other Groups • Providers of essential community services • Foreign travelers • Students • Anyone who wishes to reduce the likelihood of becoming ill from influenza
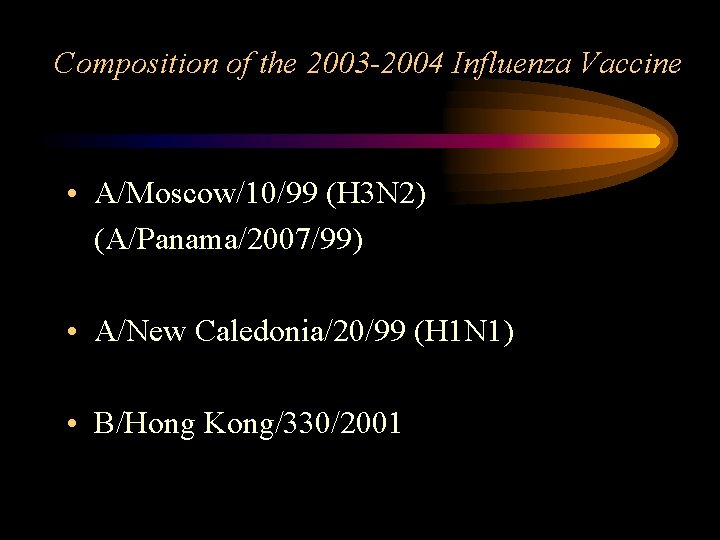
Composition of the 2003 -2004 Influenza Vaccine • A/Moscow/10/99 (H 3 N 2) (A/Panama/2007/99) • A/New Caledonia/20/99 (H 1 N 1) • B/Hong Kong/330/2001

Composition of the 2004 -2005 Influenza Vaccine* • A/Fujian/411/2002 (H 3 N 2) (A/Wyoming/3/2003) • A/New Caledonia/20/99 (H 1 N 1) • B/Shanghai/361/2002 (B/Jilin/20/2003 or B/Jiangsu/10/2003) *strains in (parenthesis) are antigenically identical to the selected strains and may be used in the vaccines
Live Attentuated Intranasal Influenza (LAIV) • Contains weakened live influenza vs killed viruses • Administered by nasal spray • Contains 3 different live (but weakened) viruses, which stimulate body to make antibodies
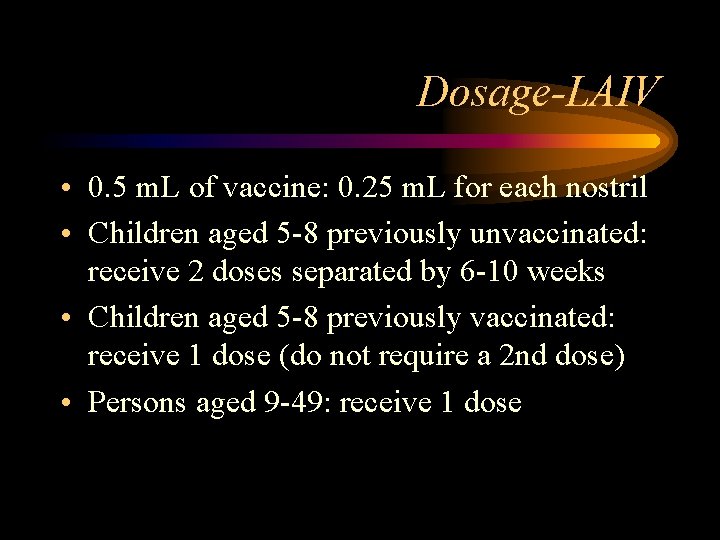
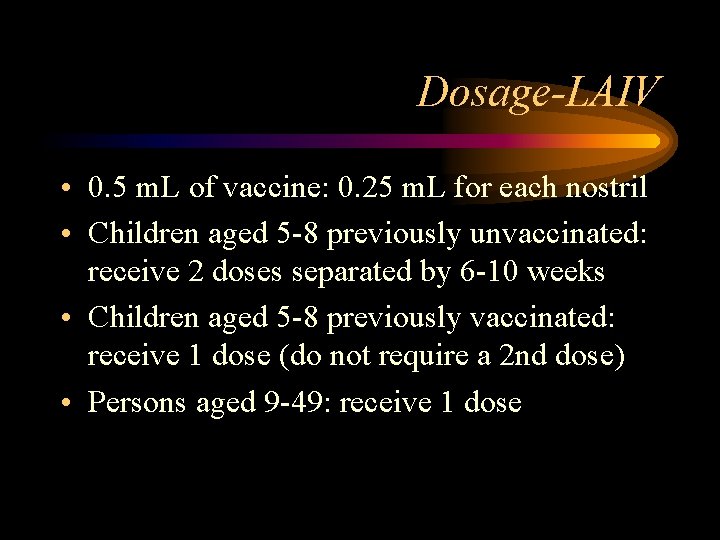
Dosage-LAIV • 0. 5 m. L of vaccine: 0. 25 m. L for each nostril • Children aged 5 -8 previously unvaccinated: receive 2 doses separated by 6 -10 weeks • Children aged 5 -8 previously vaccinated: receive 1 dose (do not require a 2 nd dose) • Persons aged 9 -49: receive 1 dose
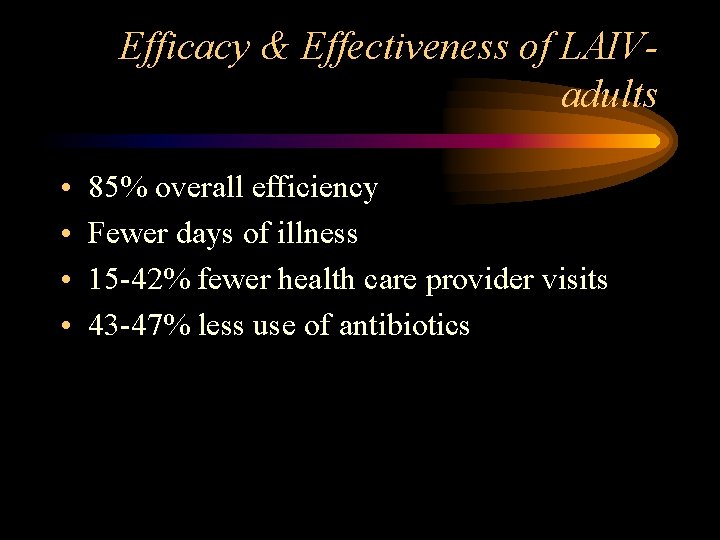
Efficacy & Effectiveness of LAIVadults • • 85% overall efficiency Fewer days of illness 15 -42% fewer health care provider visits 43 -47% less use of antibiotics
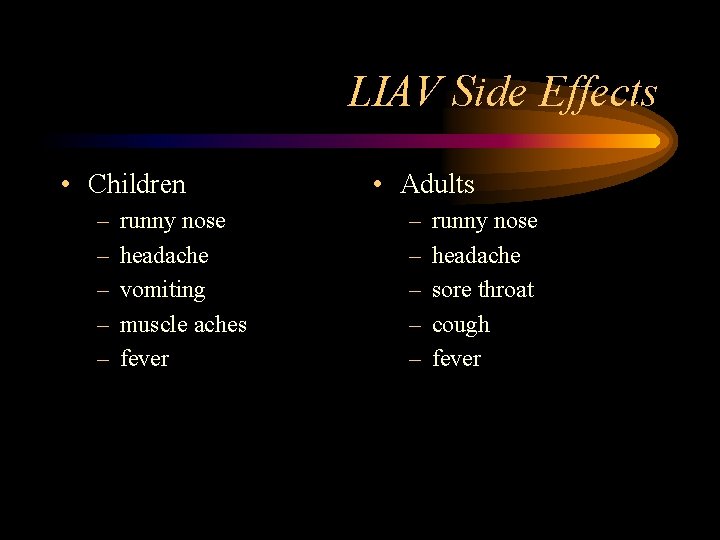
LIAV Side Effects • Children – – – runny nose headache vomiting muscle aches fever • Adults – – – runny nose headache sore throat cough fever
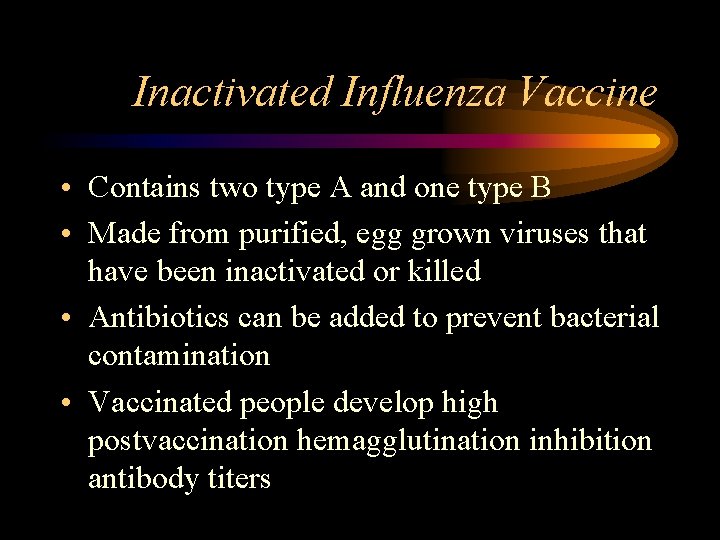
Inactivated Influenza Vaccine • Contains two type A and one type B • Made from purified, egg grown viruses that have been inactivated or killed • Antibiotics can be added to prevent bacterial contamination • Vaccinated people develop high postvaccination hemagglutination inhibition antibody titers

Effectiveness of Inactivated Vaccine- Children • 77% - 91% effective against influenza respiratory illness
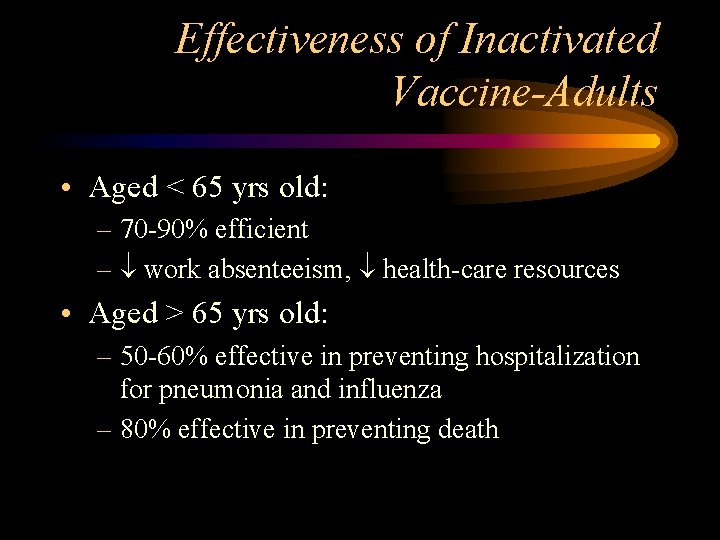
Effectiveness of Inactivated Vaccine-Adults • Aged < 65 yrs old: – 70 -90% efficient – work absenteeism, health-care resources • Aged > 65 yrs old: – 50 -60% effective in preventing hospitalization for pneumonia and influenza – 80% effective in preventing death
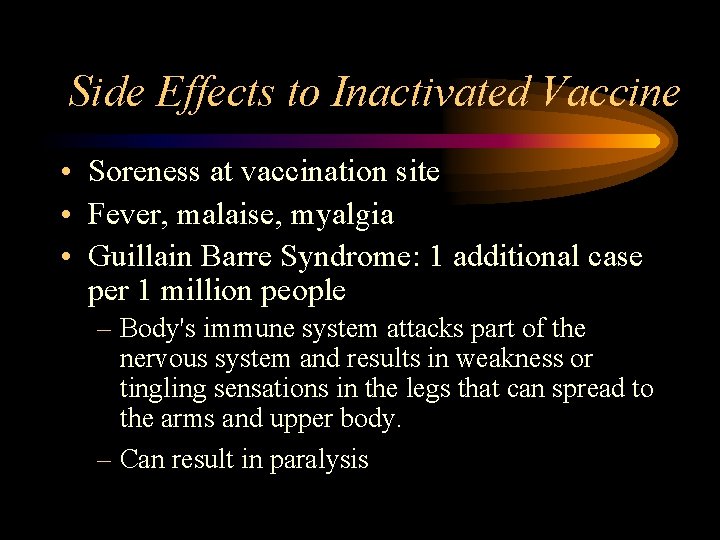
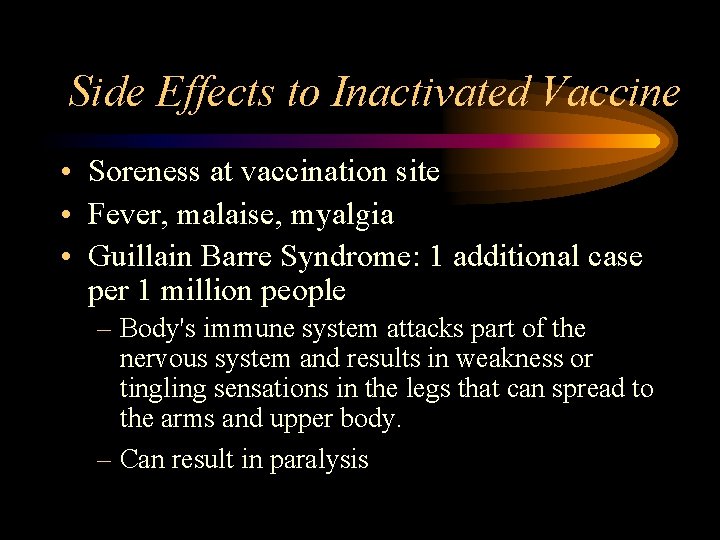
Side Effects to Inactivated Vaccine • Soreness at vaccination site • Fever, malaise, myalgia • Guillain Barre Syndrome: 1 additional case per 1 million people – Body's immune system attacks part of the nervous system and results in weakness or tingling sensations in the legs that can spread to the arms and upper body. – Can result in paralysis
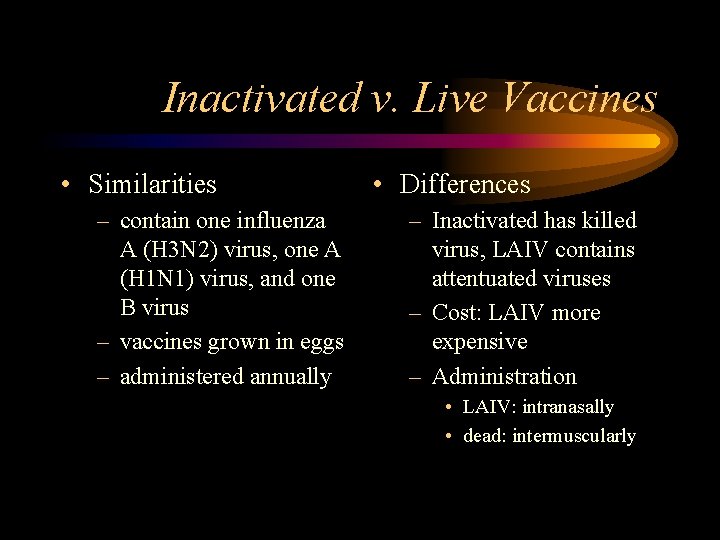
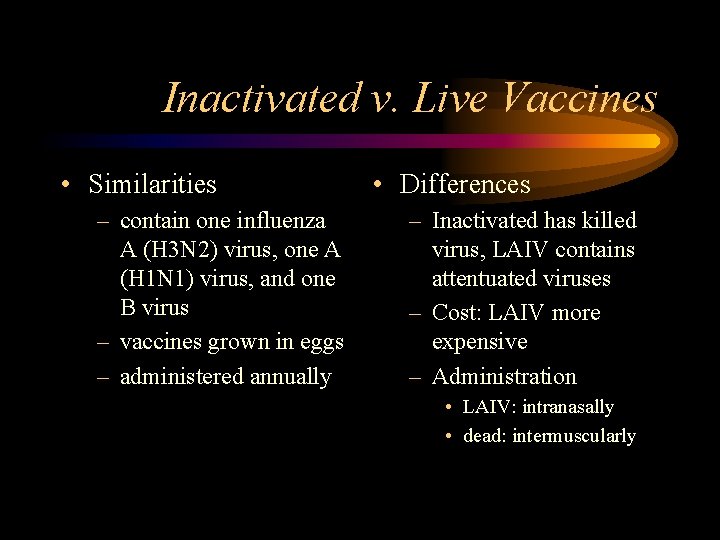
Inactivated v. Live Vaccines • Similarities – contain one influenza A (H 3 N 2) virus, one A (H 1 N 1) virus, and one B virus – vaccines grown in eggs – administered annually • Differences – Inactivated has killed virus, LAIV contains attentuated viruses – Cost: LAIV more expensive – Administration • LAIV: intranasally • dead: intermuscularly

 Stomach flu vs influenza
Stomach flu vs influenza Rimantidina
Rimantidina Influenza virus replication
Influenza virus replication Suppose a student carrying a flu virus
Suppose a student carrying a flu virus Definition of underestimated
Definition of underestimated Blended threat virus
Blended threat virus Spinte metallostatiche
Spinte metallostatiche Causative agent of diseases
Causative agent of diseases The great influenza rhetorical analysis essay
The great influenza rhetorical analysis essay Influenza
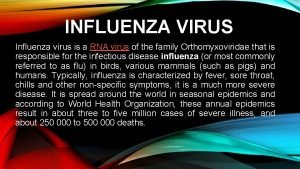
Influenza Influenza
Influenza Is influenza a airborne disease
Is influenza a airborne disease Influenza vaccine dosage chart 2019-2020
Influenza vaccine dosage chart 2019-2020 Influenza ww1
Influenza ww1 Low pathogenic avian influenza
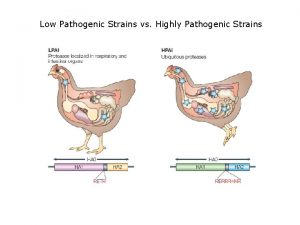
Low pathogenic avian influenza Flu root word definition
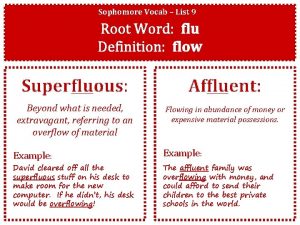
Flu root word definition Oraciones con xa xe xi xo xu
Oraciones con xa xe xi xo xu Oraciones con fla fle fli flo flu
Oraciones con fla fle fli flo flu Flu definition
Flu definition Decoding the flu case study answers
Decoding the flu case study answers Texto con fla fle fli flo flu
Texto con fla fle fli flo flu Spanish flu
Spanish flu Homophones watch
Homophones watch Spanish flu
Spanish flu Spanish flu
Spanish flu Mec flu
Mec flu Diane gould
Diane gould Flu timeline
Flu timeline Flu produit chimique
Flu produit chimique Flu watch canada
Flu watch canada Virus herpes simplex de type 2
Virus herpes simplex de type 2 Trmatoda
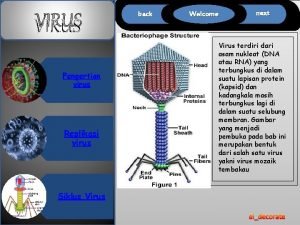
Trmatoda T4 page virus
T4 page virus Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia