First FRCR Examination in Clinical Radiology Statutory Requirements

- Slides: 83
First FRCR Examination in Clinical Radiology Statutory Requirements and Non-Statutory Recommendations Ionising Radiations Regulations 2017 John Saunderson Radiation Protection Adviser 2018 1
The route to regulations 2
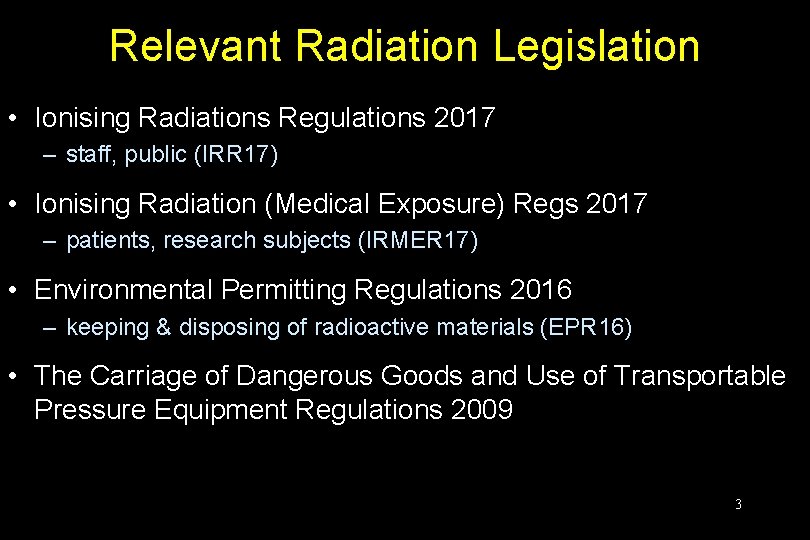
Relevant Radiation Legislation • Ionising Radiations Regulations 2017 – staff, public (IRR 17) • Ionising Radiation (Medical Exposure) Regs 2017 – patients, research subjects (IRMER 17) • Environmental Permitting Regulations 2016 – keeping & disposing of radioactive materials (EPR 16) • The Carriage of Dangerous Goods and Use of Transportable Pressure Equipment Regulations 2009 3
Guidance • • • Approved Code of Practice (ACOP) Guidance Notes odd HSE guidance etc. IPEM, NRPB, RCR, BIR, etc. stuff. 4
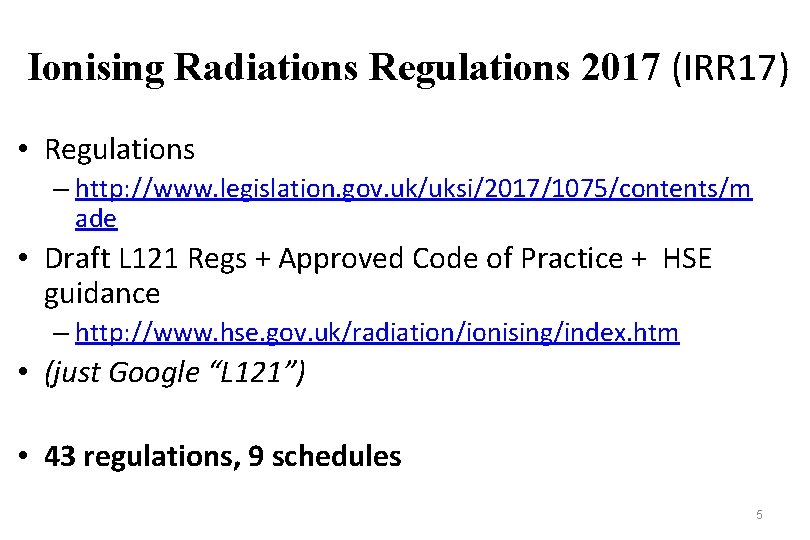
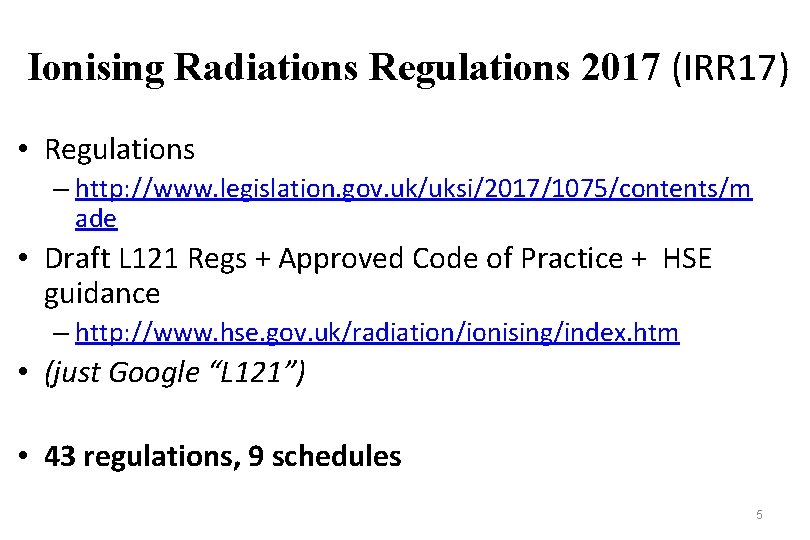
Ionising Radiations Regulations 2017 (IRR 17) • Regulations – http: //www. legislation. gov. uk/uksi/2017/1075/contents/m ade • Draft L 121 Regs + Approved Code of Practice + HSE guidance – http: //www. hse. gov. uk/radiation/ionising/index. htm • (just Google “L 121”) • 43 regulations, 9 schedules 5
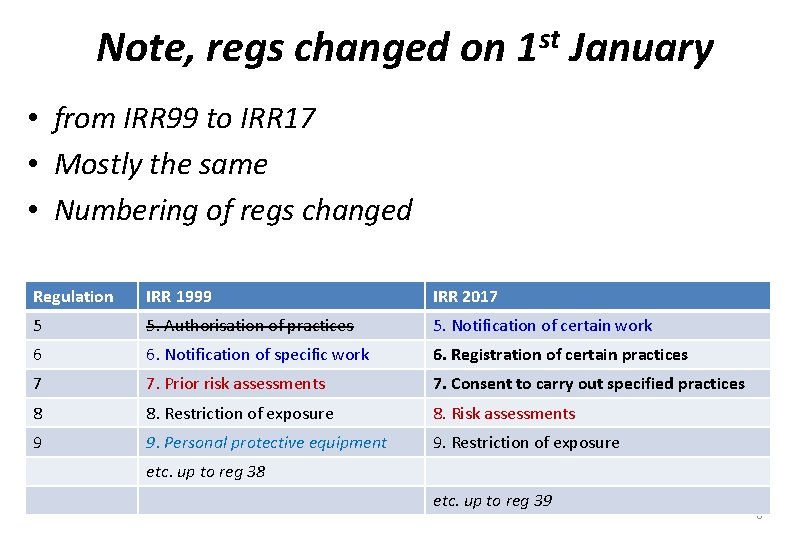
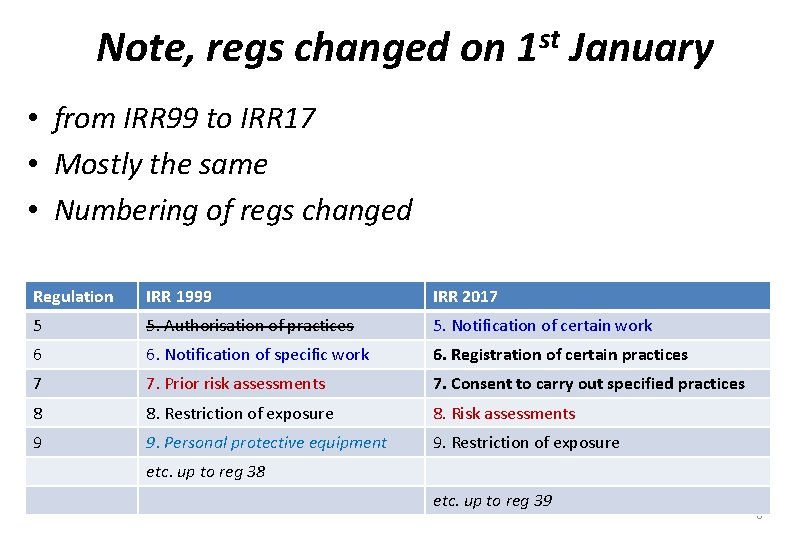
Note, regs changed on st 1 January • from IRR 99 to IRR 17 • Mostly the same • Numbering of regs changed Regulation IRR 1999 IRR 2017 5 5. Authorisation of practices 5. Notification of certain work 6 6. Notification of specific work 6. Registration of certain practices 7 7. Prior risk assessments 7. Consent to carry out specified practices 8 8. Restriction of exposure 8. Risk assessments 9 9. Personal protective equipment 9. Restriction of exposure etc. up to reg 38 etc. up to reg 39 6
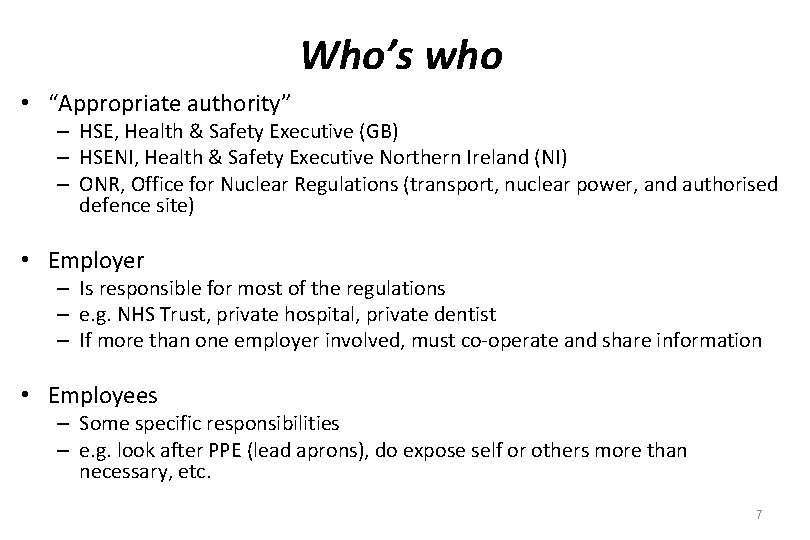
Who’s who • “Appropriate authority” – HSE, Health & Safety Executive (GB) – HSENI, Health & Safety Executive Northern Ireland (NI) – ONR, Office for Nuclear Regulations (transport, nuclear power, and authorised defence site) • Employer – Is responsible for most of the regulations – e. g. NHS Trust, private hospital, private dentist – If more than one employer involved, must co-operate and share information • Employees – Some specific responsibilities – e. g. look after PPE (lead aprons), do expose self or others more than necessary, etc. 7
Ionising Radiations Regulations 2017 (IRR 17) • Regulation 1 Citation & commencement – Came into force 1 st January 2018 • Regulation 2 Interpretation – Defines various terms (e. g. overexposure, dose, controlled area, work with ionising radiation, etc. ) 8
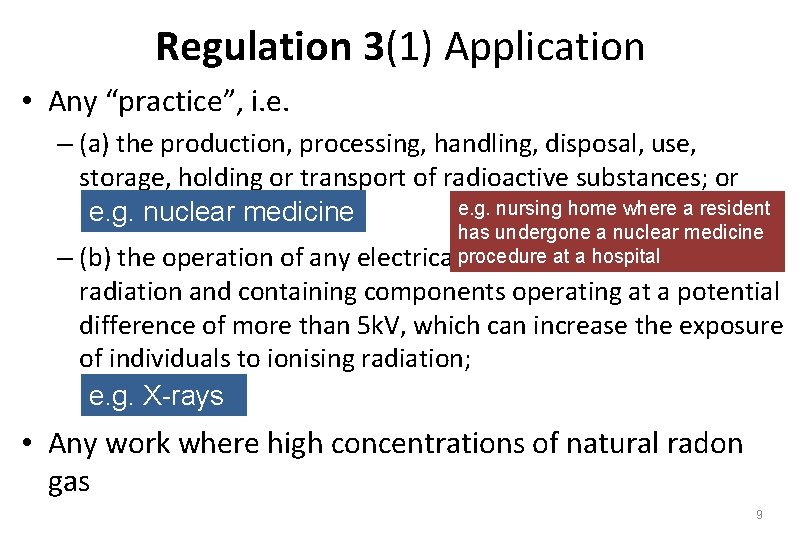
Regulation 3(1) Application • Any “practice”, i. e. – (a) the production, processing, handling, disposal, use, storage, holding or transport of radioactive substances; or e. g. nursing home where a resident e. g. nuclear medicine has undergone a nuclear medicine at a hospital electricalprocedure equipment emitting ionising – (b) the operation of any radiation and containing components operating at a potential difference of more than 5 k. V, which can increase the exposure of individuals to ionising radiation; e. g. X-rays • Any work where high concentrations of natural radon gas 9
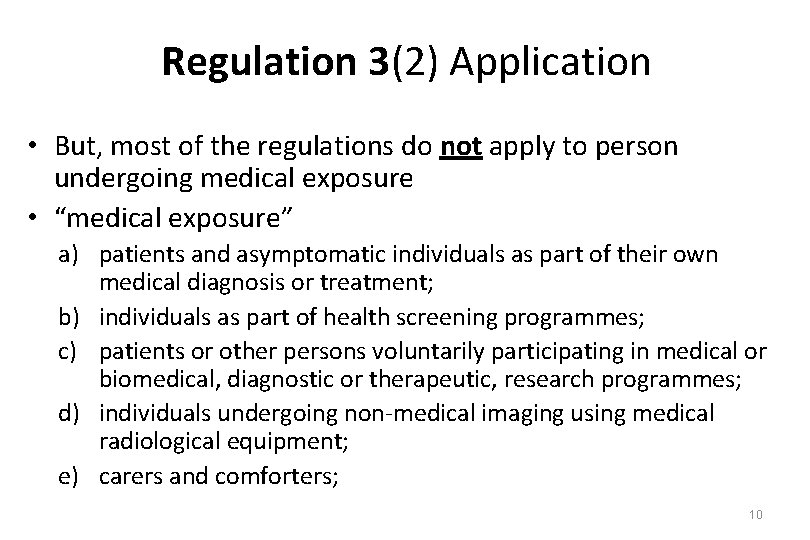
Regulation 3(2) Application • But, most of the regulations do not apply to person undergoing medical exposure • “medical exposure” a) patients and asymptomatic individuals as part of their own medical diagnosis or treatment; b) individuals as part of health screening programmes; c) patients or other persons voluntarily participating in medical or biomedical, diagnostic or therapeutic, research programmes; d) individuals undergoing non-medical imaging using medical radiological equipment; e) carers and comforters; 10
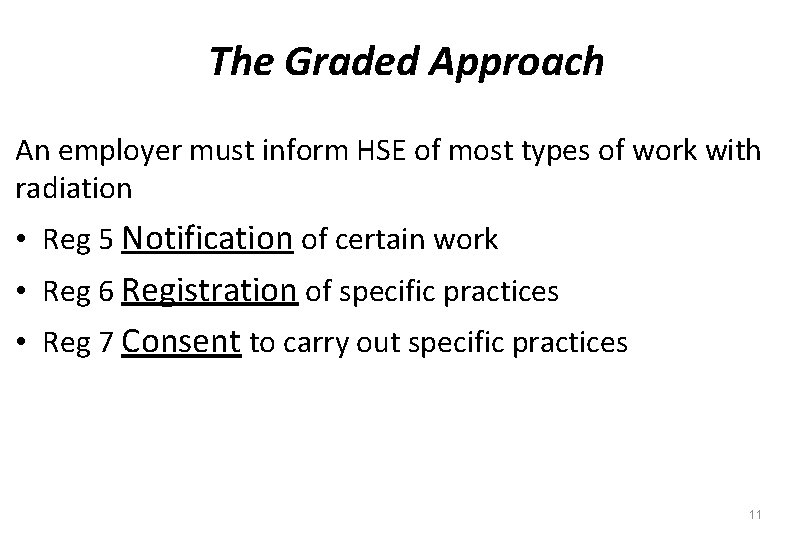
The Graded Approach An employer must inform HSE of most types of work with radiation • Reg 5 Notification of certain work • Reg 6 Registration of specific practices • Reg 7 Consent to carry out specific practices 11
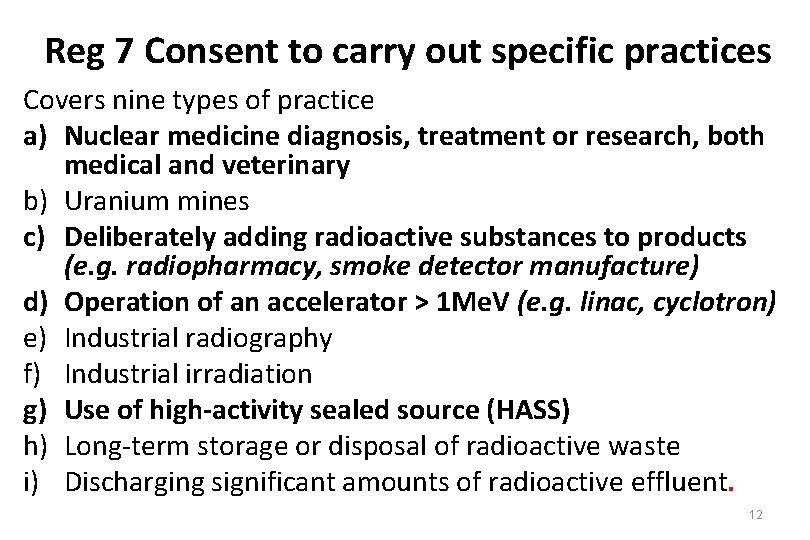
Reg 7 Consent to carry out specific practices Covers nine types of practice a) Nuclear medicine diagnosis, treatment or research, both medical and veterinary b) Uranium mines c) Deliberately adding radioactive substances to products (e. g. radiopharmacy, smoke detector manufacture) d) Operation of an accelerator > 1 Me. V (e. g. linac, cyclotron) e) Industrial radiography f) Industrial irradiation g) Use of high-activity sealed source (HASS) h) Long-term storage or disposal of radioactive waste i) Discharging significant amounts of radioactive effluent. 12
Reg 7 Consent to carry out specific practices • Consent for one of the nine practices covers all such practices by that employer at all sites – e. g. one consent to “operate accelerators” will cover all radiotherapy linacs and proposed cyclotron at CHH • Online service - £ 25 per practice • System is mostly yes/no questions – All “yeses” and consent almost guaranteed – Any “nos” and no consent – Also give maximum likely doses to staff and public. – Consent may or may not be time limited 13
Reg 6 Registration of specific practices Covers a) radiation generators, such as X-ray devices, that are not a specific practice requiring consent, e. g. i. iii. iv. diagnostic X-ray, superficial X-ray therapy, interventional radiology, use of calibration sources b) 1000 kg or over of artificial or naturally occurring radionuclides (“NORM”) that is above the low end of specific concentration levels c) under 1000 kg of artificial or NORM that is above the medium end of specific concentration levels. 14
Reg 6 Registration of specific practices • A practice subject to “consent” does not need to be “registered” • A single registration from an employer covers all their registrable practices at all their sites • Online service - £ 25 per employer • A subset of the consent questions • Must notify immediately HSE if employer ceases to carry out the practice or material change • HSE anticipated around 28, 000 employers registering. 15
Only for trivial quantities of radioactive materials Reg 5 Notification of certain work Covers a) Work with ionising radiation which is i. Not exempt (below schedule 1 limits, e. g. very small amounts of radioactive material) ii. Not registerable iii. Not requiring consent b) i. e. work with under 1, 000 kg of artificial or naturally occurring radionuclides that is: a) between the low and medium end of specific concentration levels b) above specific quantity levels c) And work in a radon atmosphere above an annual average of 300 Bq. m-3 d) Online and free. 16
Reg 8 Radiation risk assessments • Prior risk assessment required before new activity involving radiation can start – must be recorded This regulation does not apply to persons undergoing medical exposures 17

Boston Magistrates’ Court heard today that the male staff member working with a CT scanner at the Boston hospital received more than double the annual dose limit for skin exposure in just over three months. 18 https: //www. bostonstandard. co. uk/news/health/pilgrim-hospital-trust-fined-30 -000 -for-radiation-exposure-1 -5561987
Reg 8 Radiation risk assessments • Prior risk assessment required before new activity involving radiation can start – must be recorded • Must identify measures required to restrict exposure to staff and others (applied to “comforters & carers” but not patients undergoing medical exposures) • Must identify all risks of radiation accidents • Must take all reasonable steps to – prevent accidents – limit consequences – Provide employees information, instruction, training & equipment needed to restrict exposure This regulation does not apply to persons undergoing medical exposures 19
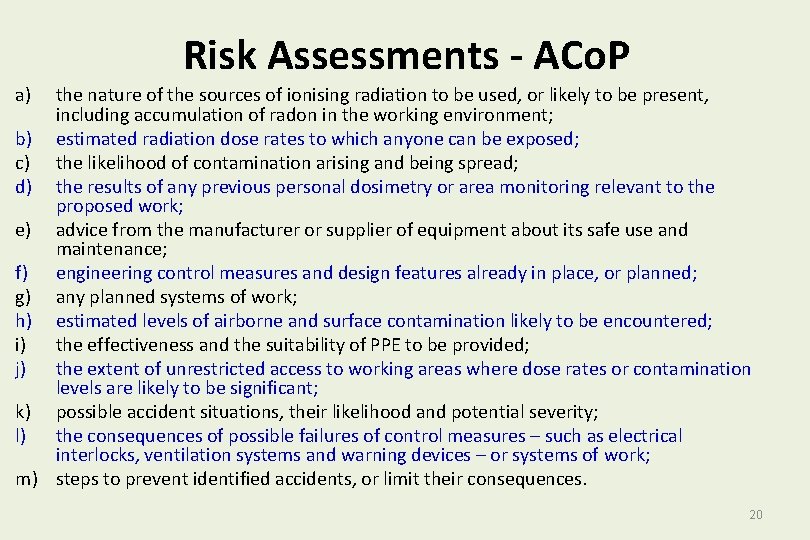
Risk Assessments - ACo. P a) the nature of the sources of ionising radiation to be used, or likely to be present, including accumulation of radon in the working environment; b) estimated radiation dose rates to which anyone can be exposed; c) the likelihood of contamination arising and being spread; d) the results of any previous personal dosimetry or area monitoring relevant to the proposed work; e) advice from the manufacturer or supplier of equipment about its safe use and maintenance; f) engineering control measures and design features already in place, or planned; g) any planned systems of work; h) estimated levels of airborne and surface contamination likely to be encountered; i) the effectiveness and the suitability of PPE to be provided; j) the extent of unrestricted access to working areas where dose rates or contamination levels are likely to be significant; k) possible accident situations, their likelihood and potential severity; l) the consequences of possible failures of control measures – such as electrical interlocks, ventilation systems and warning devices – or systems of work; m) steps to prevent identified accidents, or limit their consequences. 20
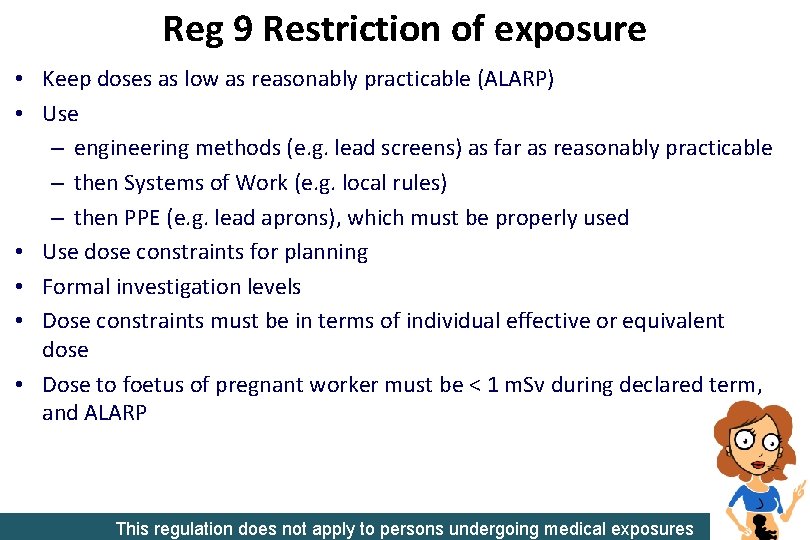
Reg 9 Restriction of exposure • Keep doses as low as reasonably practicable (ALARP) • Use – engineering methods (e. g. lead screens) as far as reasonably practicable – then Systems of Work (e. g. local rules) – then PPE (e. g. lead aprons), which must be properly used • Use dose constraints for planning • Formal investigation levels • Dose constraints must be in terms of individual effective or equivalent dose • Dose to foetus of pregnant worker must be < 1 m. Sv during declared term, and ALARP This regulation does not apply to persons undergoing medical exposures 21
Here on 14/09/2020 22
• Must comply with other PPE regs • Appropriate storage must be provided 23
Reg 10 Personal protective equipment Reg 11 Maintenance and examination of engineering controls etc and personal protective equipment • Maintain • Test safety features and warning devices at regular intervals • Appropriate storage must be provided for PPE • Examine PPE and keep records for at least 2 years 24
Reg 12 Dose limitation • Employer must ensure dose limits are not exceeded This regulation does not apply to persons undergoing medical exposures 25
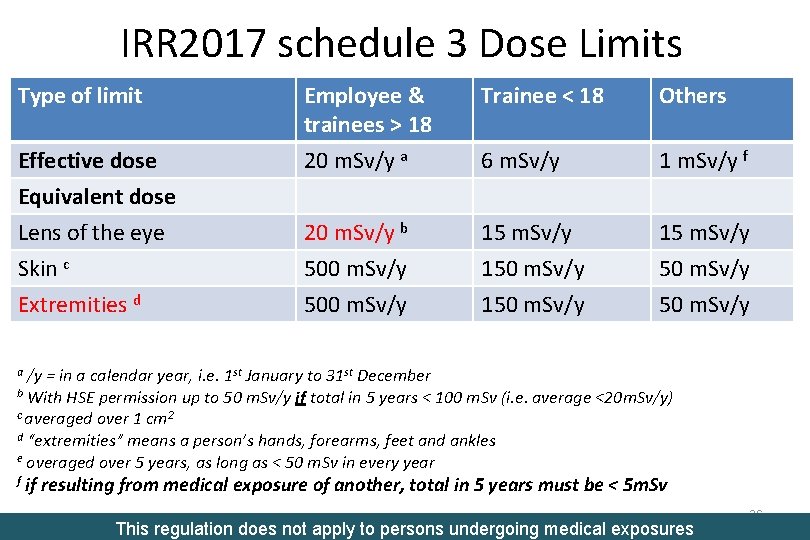
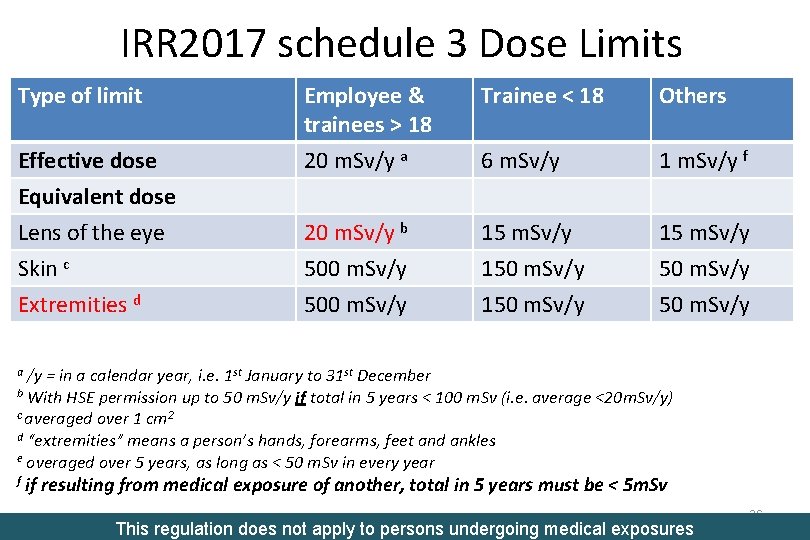
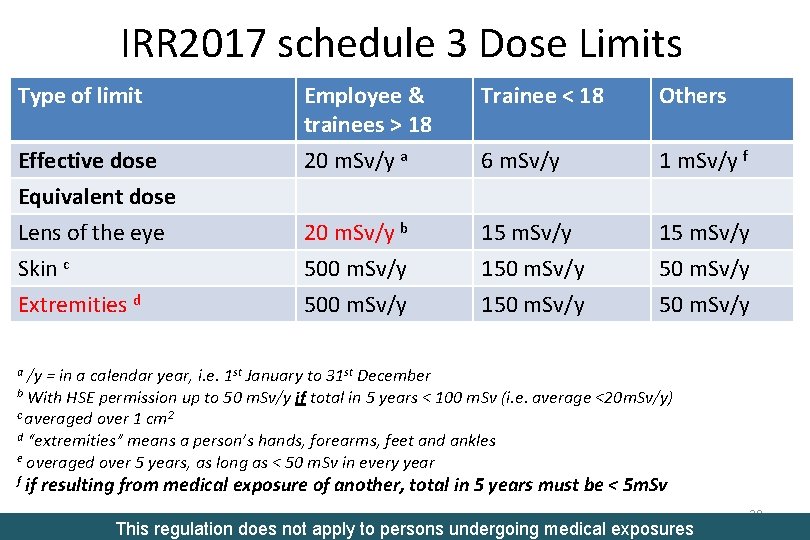
IRR 2017 schedule 3 Dose Limits Type of limit Trainee < 18 Others Effective dose Employee & trainees > 18 20 m. Sv/y a 6 m. Sv/y 1 m. Sv/y f Equivalent dose Lens of the eye Skin c 20 m. Sv/y b 500 m. Sv/y 150 m. Sv/y 15 m. Sv/y 50 m. Sv/y Extremities d 500 m. Sv/y 150 m. Sv/y /y = in a calendar year, i. e. 1 st January to 31 st December b With HSE permission up to 50 m. Sv/y if total in 5 years < 100 m. Sv (i. e. average <20 m. Sv/y) c averaged over 1 cm 2 d “extremities” means a person’s hands, forearms, feet and ankles e overaged over 5 years, as long as < 50 m. Sv in every year a f if resulting from medical exposure of another, total in 5 years must be < 5 m. Sv This regulation does not apply to persons undergoing medical exposures 26
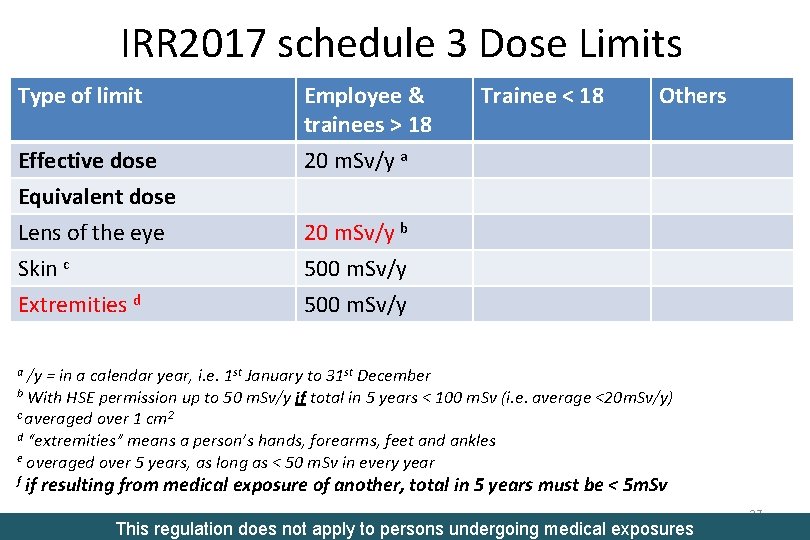
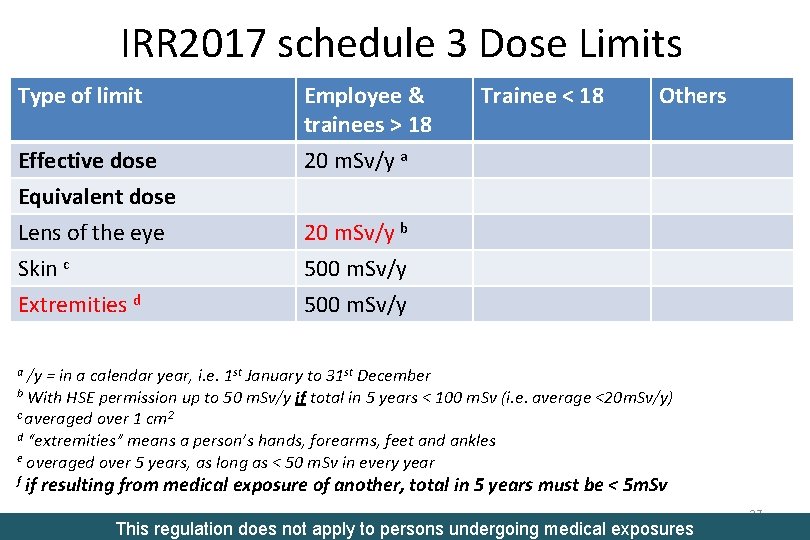
IRR 2017 schedule 3 Dose Limits Type of limit Effective dose Employee & trainees > 18 20 m. Sv/y a Equivalent dose Lens of the eye Skin c 20 m. Sv/y b 500 m. Sv/y Extremities d 500 m. Sv/y Trainee < 18 Others /y = in a calendar year, i. e. 1 st January to 31 st December b With HSE permission up to 50 m. Sv/y if total in 5 years < 100 m. Sv (i. e. average <20 m. Sv/y) c averaged over 1 cm 2 d “extremities” means a person’s hands, forearms, feet and ankles e overaged over 5 years, as long as < 50 m. Sv in every year a f if resulting from medical exposure of another, total in 5 years must be < 5 m. Sv This regulation does not apply to persons undergoing medical exposures 27
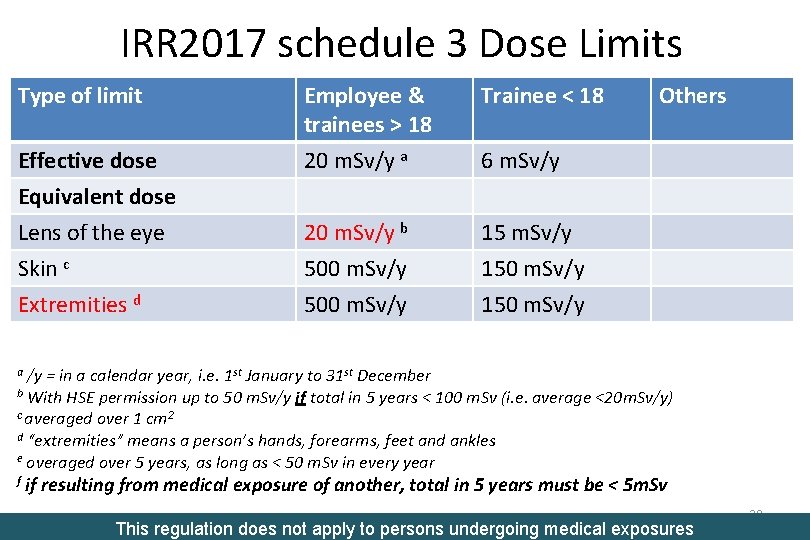
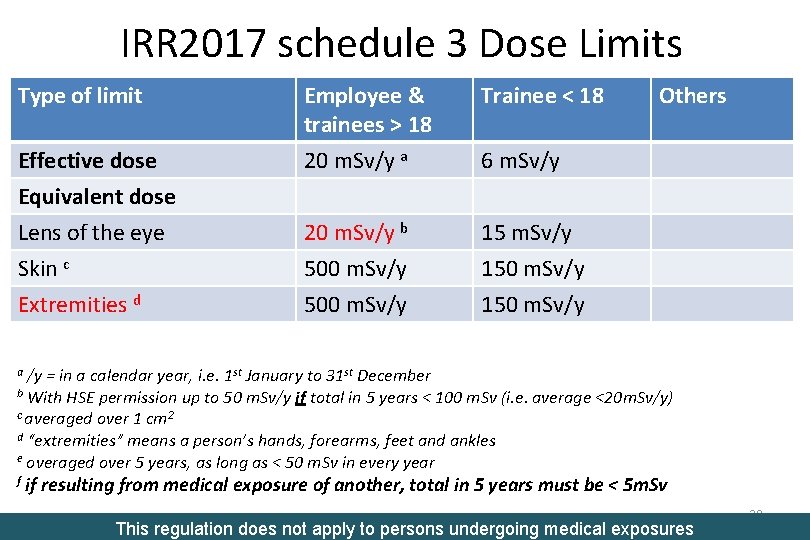
IRR 2017 schedule 3 Dose Limits Type of limit Trainee < 18 Effective dose Employee & trainees > 18 20 m. Sv/y a Equivalent dose Lens of the eye Skin c 20 m. Sv/y b 500 m. Sv/y 150 m. Sv/y Extremities d 500 m. Sv/y 150 m. Sv/y Others 6 m. Sv/y /y = in a calendar year, i. e. 1 st January to 31 st December b With HSE permission up to 50 m. Sv/y if total in 5 years < 100 m. Sv (i. e. average <20 m. Sv/y) c averaged over 1 cm 2 d “extremities” means a person’s hands, forearms, feet and ankles e overaged over 5 years, as long as < 50 m. Sv in every year a f if resulting from medical exposure of another, total in 5 years must be < 5 m. Sv This regulation does not apply to persons undergoing medical exposures 28
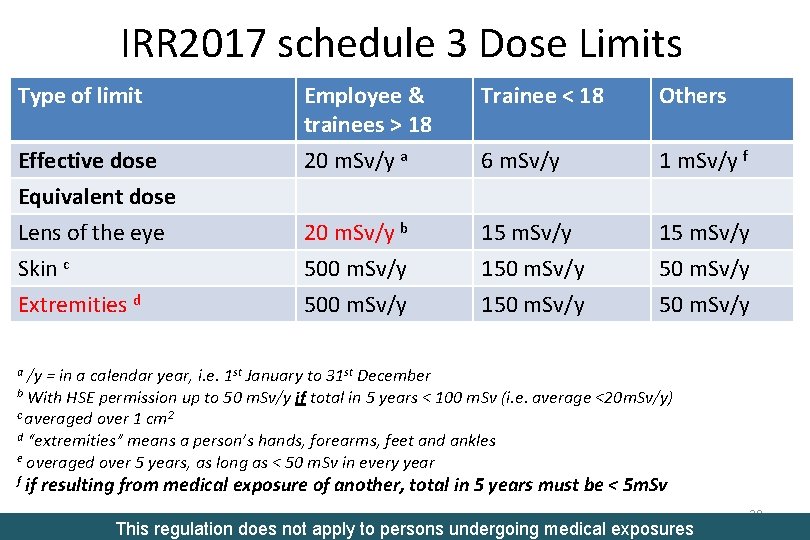
IRR 2017 schedule 3 Dose Limits Type of limit Trainee < 18 Others Effective dose Employee & trainees > 18 20 m. Sv/y a 6 m. Sv/y 1 m. Sv/y f Equivalent dose Lens of the eye Skin c 20 m. Sv/y b 500 m. Sv/y 150 m. Sv/y 15 m. Sv/y 50 m. Sv/y Extremities d 500 m. Sv/y 150 m. Sv/y /y = in a calendar year, i. e. 1 st January to 31 st December b With HSE permission up to 50 m. Sv/y if total in 5 years < 100 m. Sv (i. e. average <20 m. Sv/y) c averaged over 1 cm 2 d “extremities” means a person’s hands, forearms, feet and ankles e overaged over 5 years, as long as < 50 m. Sv in every year a f if resulting from medical exposure of another, total in 5 years must be < 5 m. Sv This regulation does not apply to persons undergoing medical exposures 29
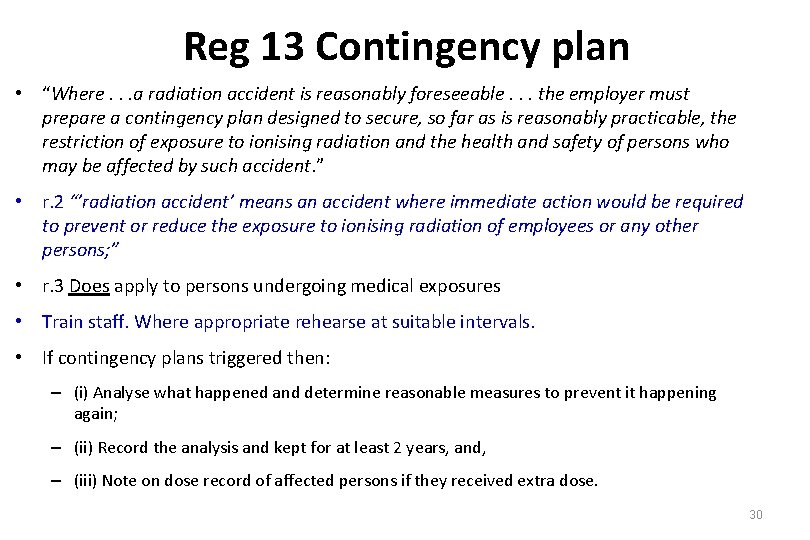
Reg 13 Contingency plan • “Where. . . a radiation accident is reasonably foreseeable. . . the employer must prepare a contingency plan designed to secure, so far as is reasonably practicable, the restriction of exposure to ionising radiation and the health and safety of persons who may be affected by such accident. ” • r. 2 “’radiation accident’ means an accident where immediate action would be required to prevent or reduce the exposure to ionising radiation of employees or any other persons; ” • r. 3 Does apply to persons undergoing medical exposures • Train staff. Where appropriate rehearse at suitable intervals. • If contingency plans triggered then: – (i) Analyse what happened and determine reasonable measures to prevent it happening again; – (ii) Record the analysis and kept for at least 2 years, and, – (iii) Note on dose record of affected persons if they received extra dose. 30
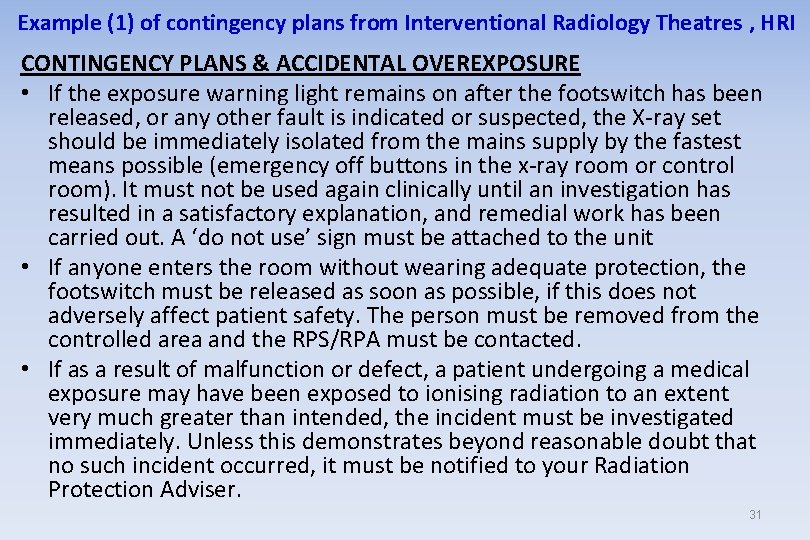
Example (1) of contingency plans from Interventional Radiology Theatres , HRI CONTINGENCY PLANS & ACCIDENTAL OVEREXPOSURE • If the exposure warning light remains on after the footswitch has been released, or any other fault is indicated or suspected, the X-ray set should be immediately isolated from the mains supply by the fastest means possible (emergency off buttons in the x-ray room or control room). It must not be used again clinically until an investigation has resulted in a satisfactory explanation, and remedial work has been carried out. A ‘do not use’ sign must be attached to the unit • If anyone enters the room without wearing adequate protection, the footswitch must be released as soon as possible, if this does not adversely affect patient safety. The person must be removed from the controlled area and the RPS/RPA must be contacted. • If as a result of malfunction or defect, a patient undergoing a medical exposure may have been exposed to ionising radiation to an extent very much greater than intended, the incident must be investigated immediately. Unless this demonstrates beyond reasonable doubt that no such incident occurred, it must be notified to your Radiation Protection Adviser. 31
Example (1) of contingency plans from Interventional Radiology Theatres , HRI CONTINGENCY PLANS & ACCIDENTAL OVEREXPOSURE • If the exposure warning light remains on after the footswitch has been released, or any other fault is indicated or suspected, the X-ray set Know where the should be immediately isolated from the mains supply by the fastest buttons means possible (emergency off buttons inemergency the x-ray room off or control room). It must not be used again clinically until an investigation has are located resulted in a satisfactory explanation, and remedial work has been carried out. A ‘do not use’ sign must be attached to the unit • If anyone enters the room without wearing adequate protection, the footswitch must be released as soon as possible, if this does not adversely affect patient safety. The person must be removed from the controlled area and the RPS/RPA must be contacted. • If as a result of malfunction or defect, a patient undergoing a medical exposure may have been exposed to ionising radiation to an extent very much greater than intended, the incident must be investigated immediately. Unless this demonstrates beyond reasonable doubt that no such incident occurred, it must be notified to your Radiation Protection Adviser. 32
Example (1) of contingency plans from Interventional Radiology Theatres , HRI CONTINGENCY PLANS & ACCIDENTAL OVEREXPOSURE • If the exposure warning light remains on after the footswitch has been released, or any other fault is indicated or suspected, the X-ray set Know where the should be immediately isolated from the mains supply by the fastest buttons means possible (emergency off buttons inemergency the x-ray room off or control room). It must not be used again clinically until an investigation has are located resulted in a satisfactory explanation, and remedial work has been carried out. A ‘do not use’ sign must be attached to the unit • If anyone enters the room without wearing adequate protection, the footswitch must be released as soon as possible, if this does not adversely affect patient safety. The person must be removed from the controlled area and the RPS/RPA mustabe contacted. If this happens • If as a result of malfunction or defect, a patient undergoing a medical Datix must exposure may have been form exposed to ionising radiation to an extent very much greater be thancompleted intended, the incident must be investigated immediately. Unless this demonstrates beyond reasonable doubt that no such incident occurred, it must be notified to your Radiation Protection Adviser. 33
Example (1) of contingency plans from Interventional Radiology Theatres , HRI CONTINGENCY PLANS & ACCIDENTAL OVEREXPOSURE • If the exposure warning light remains on after the footswitch has been released, or any other fault is indicated or suspected, the X-ray set Know where the should be immediately isolated from the mains supply by the fastest buttons means possible (emergency off buttons inemergency the x-ray room off or control room). It must not be used again clinically until an investigation has are located resulted in a satisfactory explanation, and remedial work has been carried out. A ‘do not use’ sign must be attached to the unit • If anyone enters the room without wearing adequate protection, the If this happens a Datix footswitch must be released as soon as possible, if this does not adversely affect The person must be removed from the formpatient mustsafety. be completed controlled area and the RPS/RPA must be contacted. • If as a result of malfunction or defect, a patient undergoing a medical exposure may have been exposed to ionising radiation to an extent very much greater than intended, the incident must be investigated immediately. Unless this demonstrates beyond reasonable doubt that no such incident occurred, it must be notified to your Radiation Protection Adviser. 34
Example (2) of contingency plans from Nuclear Medicine, HRI & CHH A lot longer than for X-ray, as risk from liquid radioactive substances, includes • Emergency telephone numbers for staff and authorities • Spills and contamination – Clothing, skin, hair – Open would/needlestick – Ingestion or inhalation – Surfaces • • • Missing, stolen sources Fire Delivery of wrong radioactive material Transport accidents Annual rehearsal 35
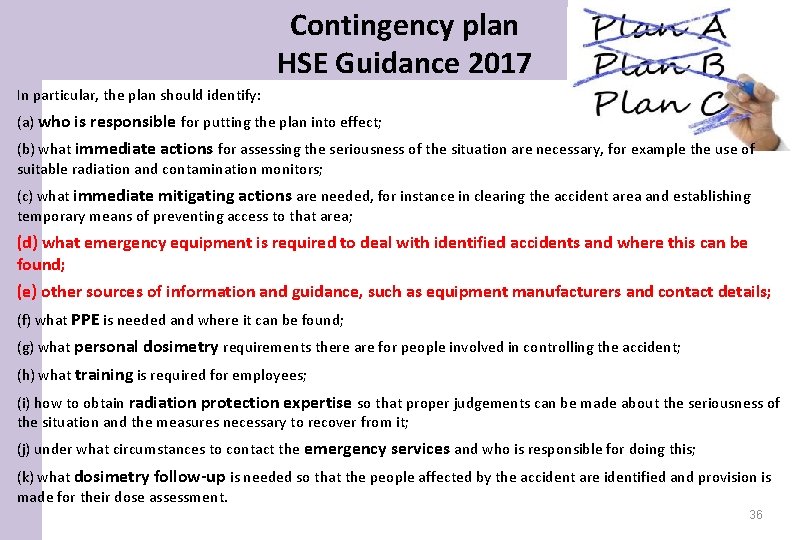
Contingency plan HSE Guidance 2017 In particular, the plan should identify: (a) who is responsible for putting the plan into effect; (b) what immediate actions for assessing the seriousness of the situation are necessary, for example the use of suitable radiation and contamination monitors; (c) what immediate mitigating actions are needed, for instance in clearing the accident area and establishing temporary means of preventing access to that area; (d) what emergency equipment is required to deal with identified accidents and where this can be found; (e) other sources of information and guidance, such as equipment manufacturers and contact details; (f) what PPE is needed and where it can be found; (g) what personal dosimetry requirements there are for people involved in controlling the accident; (h) what training is required for employees; (i) how to obtain radiation protection expertise so that proper judgements can be made about the seriousness of the situation and the measures necessary to recover from it; (j) under what circumstances to contact the emergency services and who is responsible for doing this; (k) what dosimetry follow-up is needed so that the people affected by the accident are identified and provision is made for their dose assessment. 36
Reg 14 Radiation Protection Adviser (RPA) • Must have qualification approved by HSE (e. g. RPA 2000 certificate) • Must be appointed in writing, • Must provide RPA with adequate information & facilities • Must be consulted on –controlled and supervised areas –prior examination of plans –regular calibration of dose monitoring equipment –periodic testing of safety features and warning devices –risk assessment of new radiation work –incidents where more then 6 m. Sv has been received –critical examination of safety features of new radiation equipment –and as necessary for advice on observing IRR 17 –(Unless schedule 1 work only - i. e. trivial exempt work)
Reg 15 Education, training and provision of information • Radiation workers must be adequately trained, including general and specific risks and safety procedures • Adequate information to others directly concerned • Female workers informed of risk to foetus and importance of informing employer if pregnant/breast feeding • Training must be specific to the controlled area they work in • Repeat training at suitable intervals and document • If HASS used training in specific requirement 38
Reg 15 & HASS training (2) In addition to the requirements in paragraph (1), every employer who is engaged in work with ionising radiation involving a high-activity sealed source must ensure that the information and training given to employees involved in such work includes— (a) specific requirements for the safe management and control of highactivity sealed sources for the purpose of preparing such employees for any events which may affect their radiation protection; (b) particular emphasis on the necessary safety requirements in connection with high-activity sealed sources; and (c) specific information on the possible consequences of the loss of adequate control of high-activity sealed sources. 39
Reg 16 Cooperation between employers “Where work with ionising radiation undertaken by one employer is likely to give rise to the exposure to ionising radiation of the employee of another employer, the employers concerned must co-operate by the exchange of information or otherwise to the extent necessary to ensure that each such employer – (a) has access to information on the possible exposure of their employees to ionising radiation; and (b) is enabled to comply with the requirements of these Regulations in so far as their ability to comply depends upon such co-operation. 40
Reg 16 Cooperation between employers “Where work with ionising radiation undertaken by one e. g. is likely to give rise to the exposure to ionising employer radiation of thein employee of Trusts another employer, the • Working two NHS employers concerned must co-operate by the exchange of • Working in privatetohospital and NHS hospital information or otherwise the extent necessary to ensure that such employer – • each Company rep helping train in use of or set up (a) has access to information on the possible exposure of their new equipment employees to ionising radiation; and cleaners in NHS hospital (b) • is Private enabled to comply with the requirements of these Regulations so faretc. as their ability to comply Note, dose in limits, apply to the sum ofdepends doses upon such co-operation. from all work undertaken by an individual person. 41
Reg 16 Cooperation between employers “Where work with ionising radiation undertaken by one employer is likely to give rise to the exposure to ionising radiation of the employee of another employer, the employers concerned must co-operate by the exchange of information or otherwise to the extent necessary to ensure that each such employer – (a) has access to information on the possible exposure of their employees to ionising radiation; and (b) is enabled to comply with the requirements of these Regulations in so far as their ability to comply depends upon such co-operation. 42
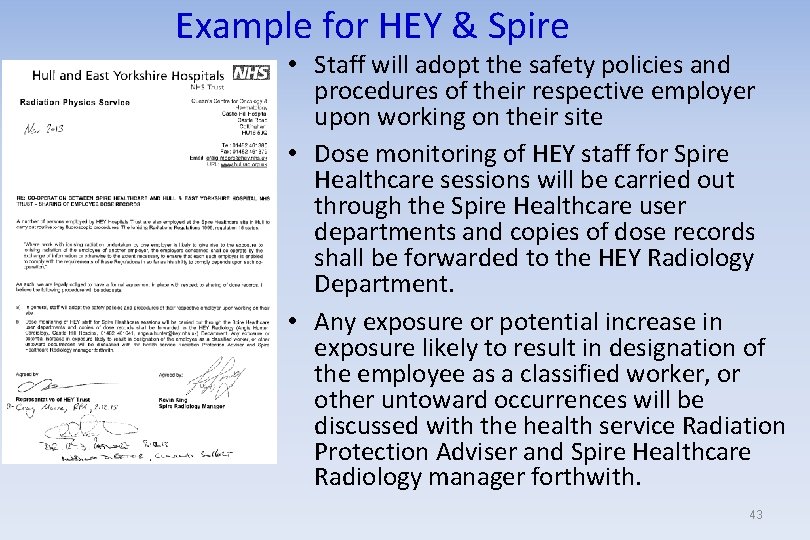
Example for HEY & Spire • Staff will adopt the safety policies and procedures of their respective employer upon working on their site • Dose monitoring of HEY staff for Spire Healthcare sessions will be carried out through the Spire Healthcare user departments and copies of dose records shall be forwarded to the HEY Radiology Department. • Any exposure or potential increase in exposure likely to result in designation of the employee as a classified worker, or other untoward occurrences will be discussed with the health service Radiation Protection Adviser and Spire Healthcare Radiology manager forthwith. 43
Reg 17 Designation of controlled or supervised areas Controlled Area must be designated for • any area where it is necessary to follow special procedures to restrict significant exposure, or • any area where it is likely that annual – E > 6 m. Sv, – Hlens > 15 m. Sv, or – Hskin> 150 m. Sv • (ACo. P gives further advice on where special procedures will be necessary) This regulation does not apply to persons undergoing medical exposures 44
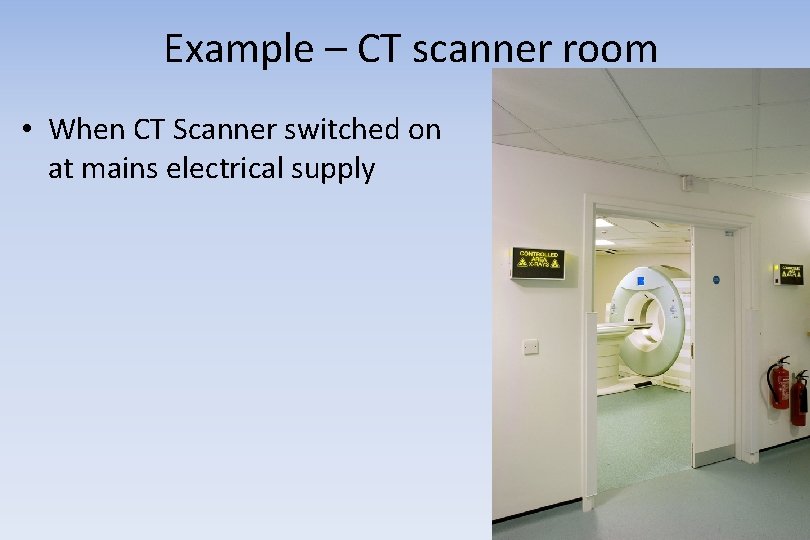
Example – CT scanner room • When CT Scanner switched on at mains electrical supply 45
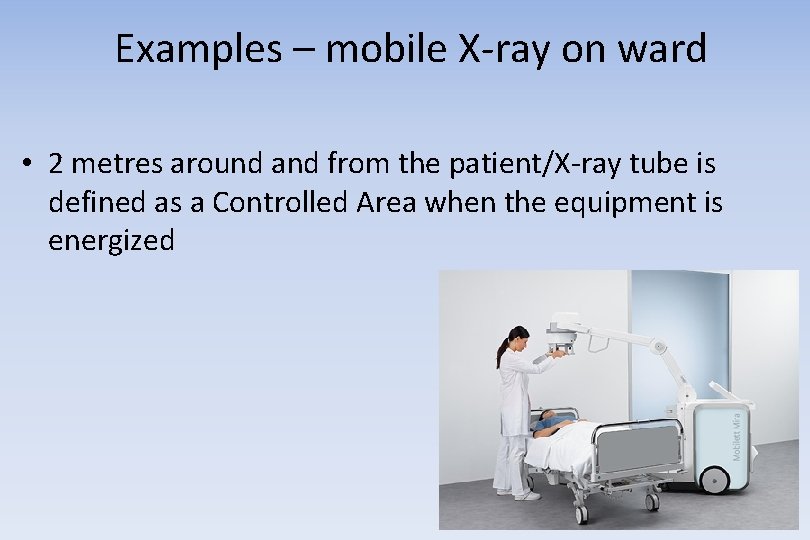
Examples – mobile X-ray on ward • 2 metres around and from the patient/X-ray tube is defined as a Controlled Area when the equipment is energized 46
Example – mobile fluoroscopy in theatre • the operating theatre is the controlled area when the set is energized. 47
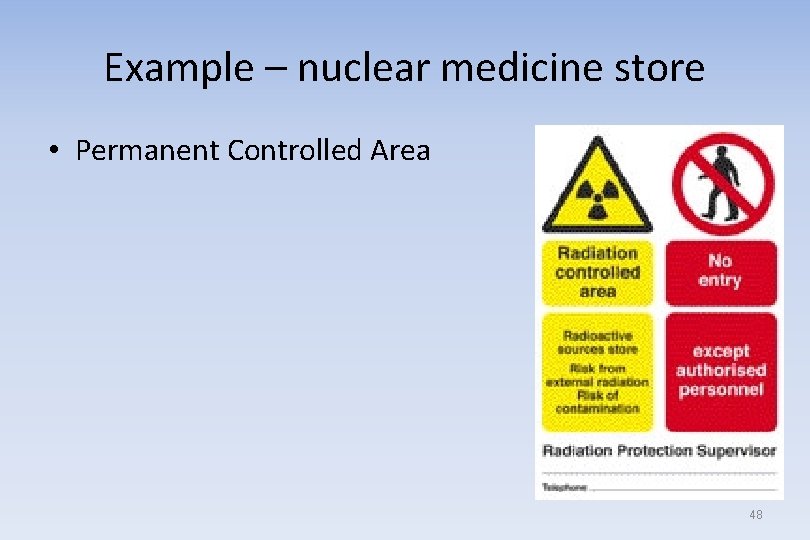
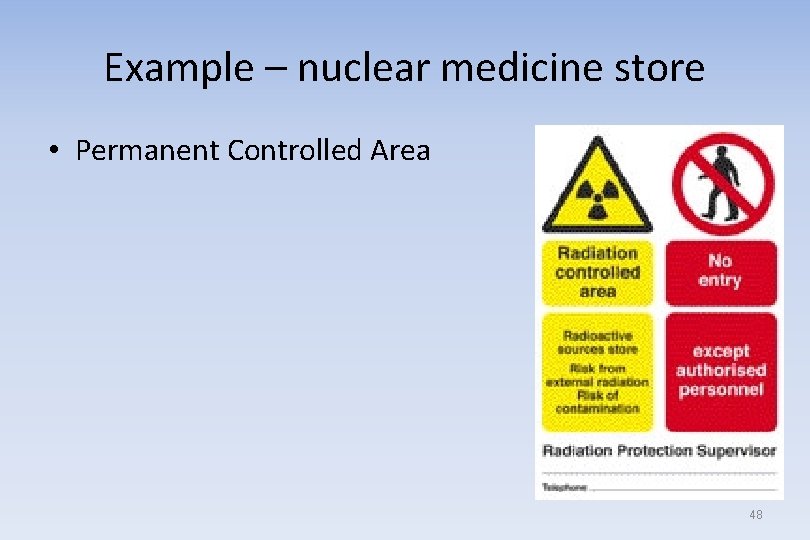
Example – nuclear medicine store • Permanent Controlled Area 48
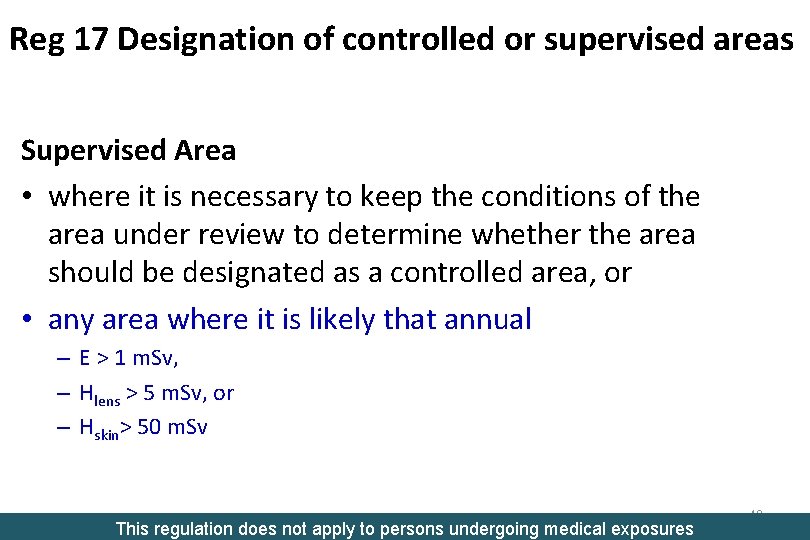
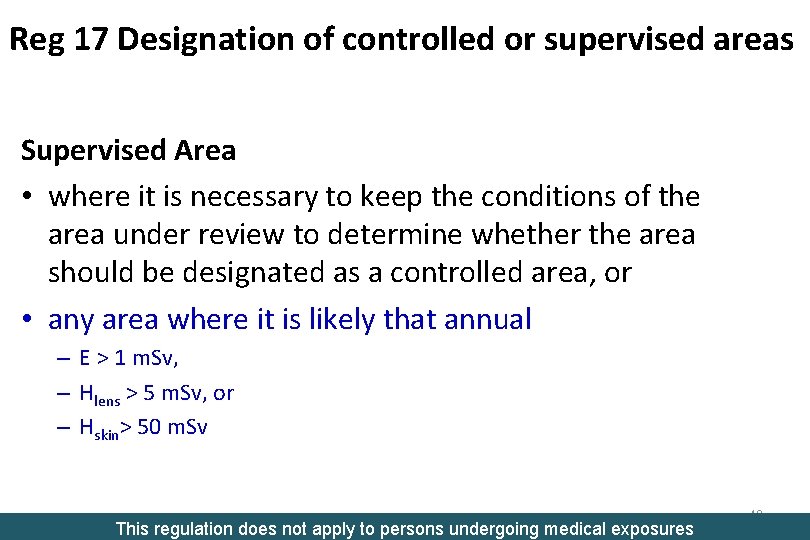
Reg 17 Designation of controlled or supervised areas Supervised Area • where it is necessary to keep the conditions of the area under review to determine whether the area should be designated as a controlled area, or • any area where it is likely that annual – E > 1 m. Sv, – Hlens > 5 m. Sv, or – Hskin> 50 m. Sv This regulation does not apply to persons undergoing medical exposures 49
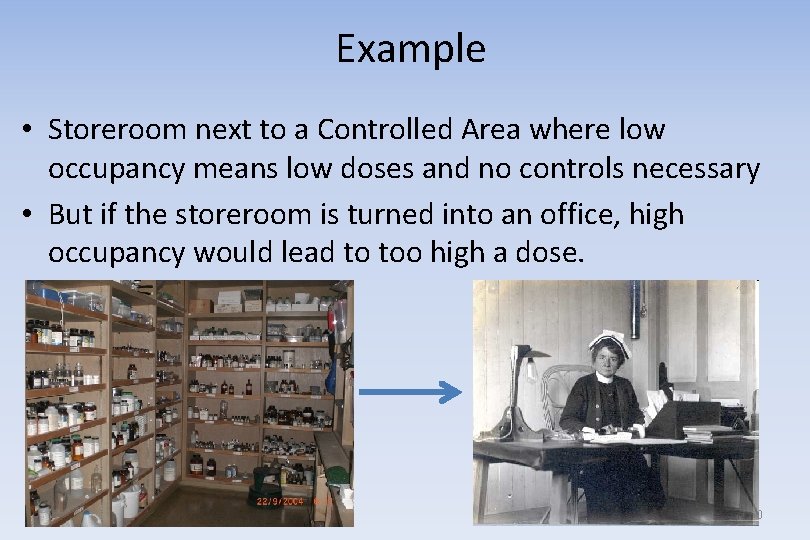
Example • Storeroom next to a Controlled Area where low occupancy means low doses and no controls necessary • But if the storeroom is turned into an office, high occupancy would lead to too high a dose. 50
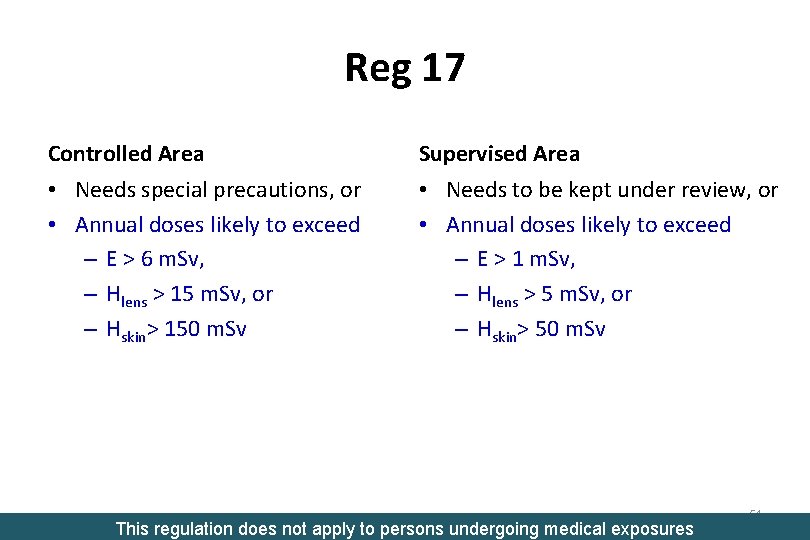
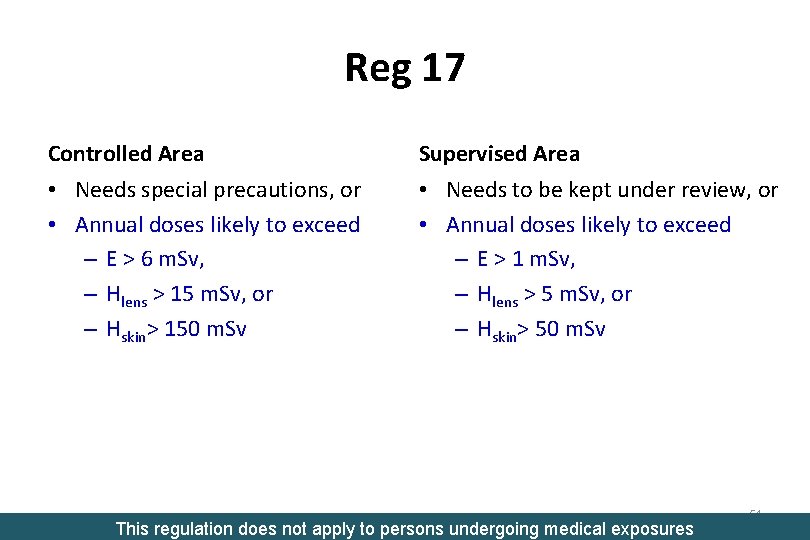
Reg 17 Controlled Area Supervised Area • Needs special precautions, or • Annual doses likely to exceed – E > 6 m. Sv, – Hlens > 15 m. Sv, or – Hskin> 150 m. Sv • Needs to be kept under review, or • Annual doses likely to exceed – E > 1 m. Sv, – Hlens > 5 m. Sv, or – Hskin> 50 m. Sv This regulation does not apply to persons undergoing medical exposures 51
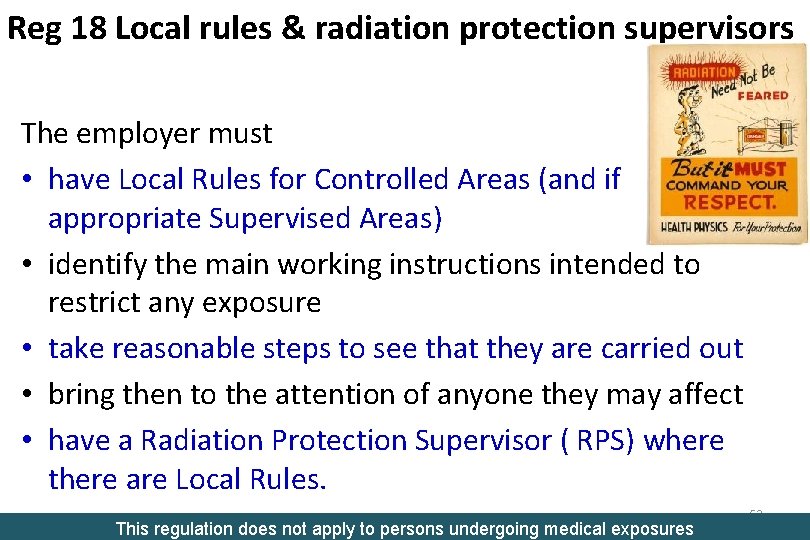
Reg 18 Local rules & radiation protection supervisors The employer must • have Local Rules for Controlled Areas (and if appropriate Supervised Areas) • identify the main working instructions intended to restrict any exposure • take reasonable steps to see that they are carried out • bring then to the attention of anyone they may affect • have a Radiation Protection Supervisor ( RPS) where there are Local Rules. This regulation does not apply to persons undergoing medical exposures 52
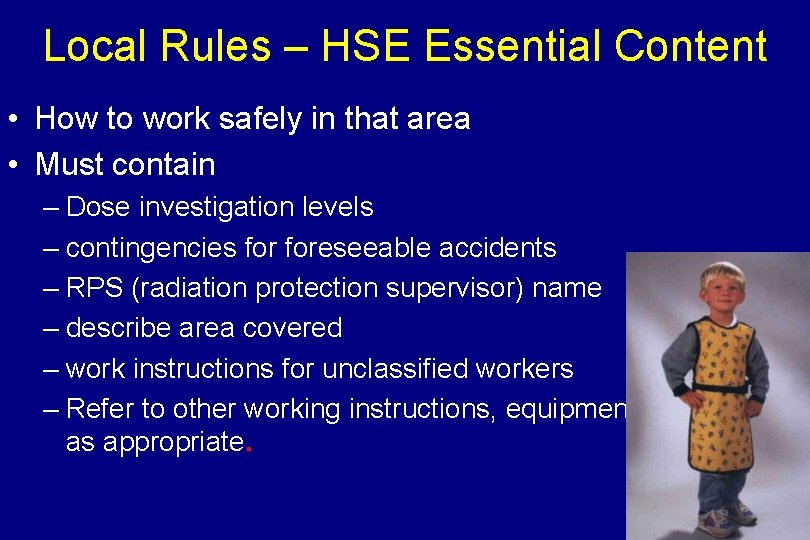
Local Rules – HSE Essential Content • How to work safely in that area • Must contain – Dose investigation levels – contingencies foreseeable accidents – RPS (radiation protection supervisor) name – describe area covered – work instructions for unclassified workers – Refer to other working instructions, equipment manuals, etc. as appropriate. 53
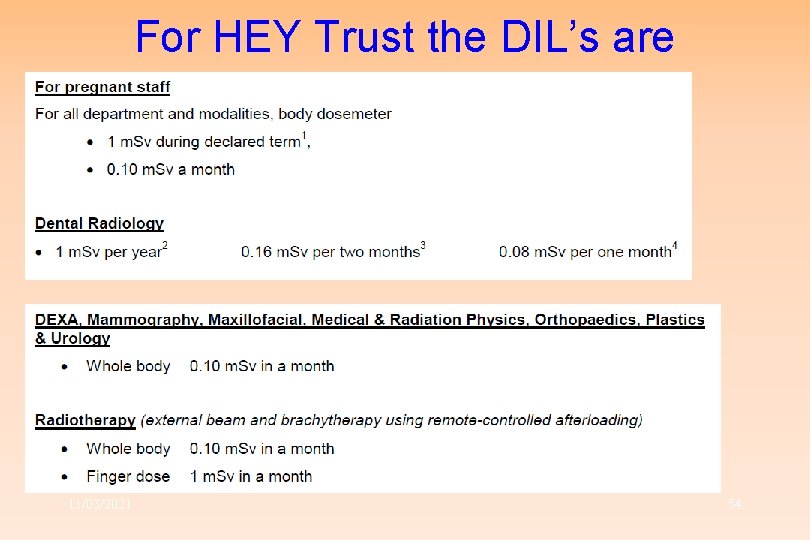
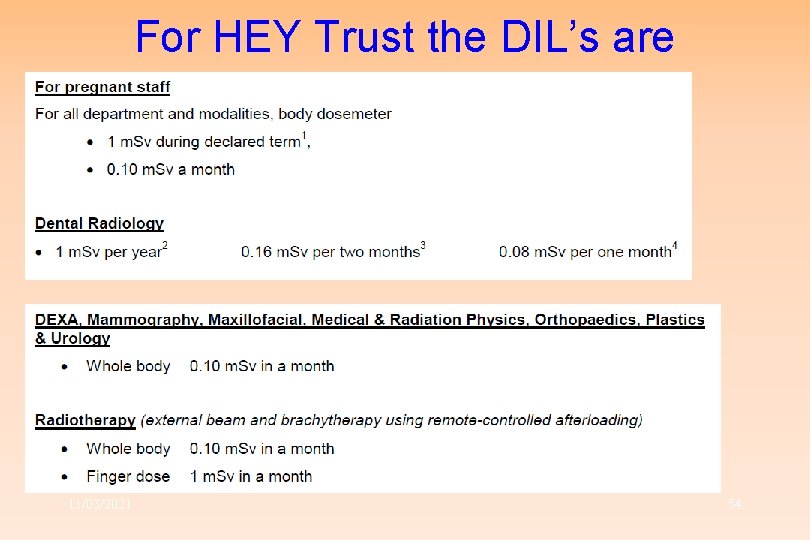
For HEY Trust the DIL’s are 11/03/2021 54
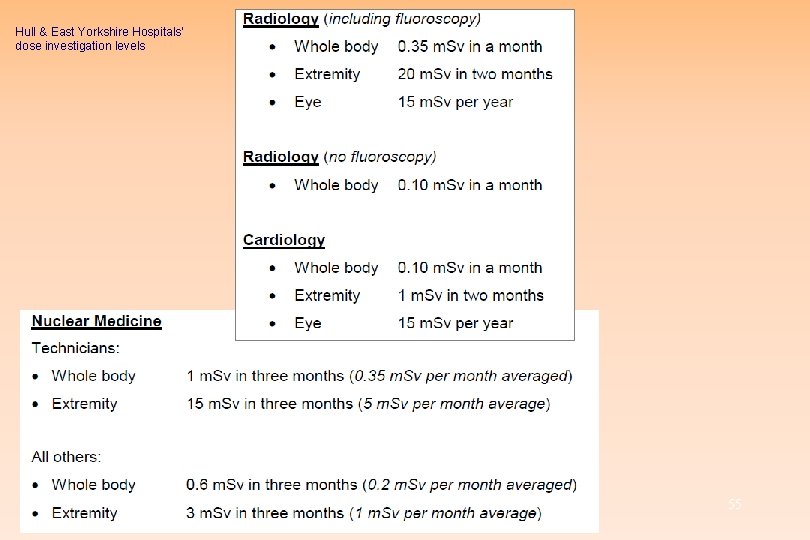
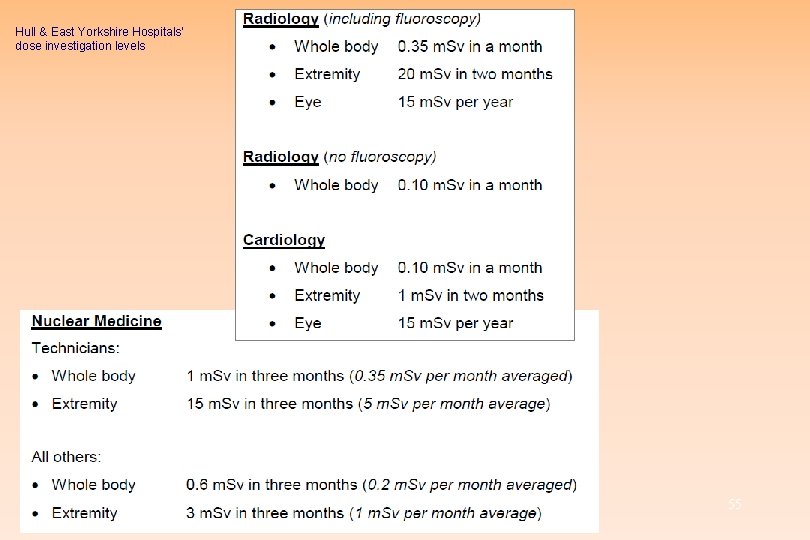
Hull & East Yorkshire Hospitals’ dose investigation levels Radiation Protection Adviser 11/03/2021 55
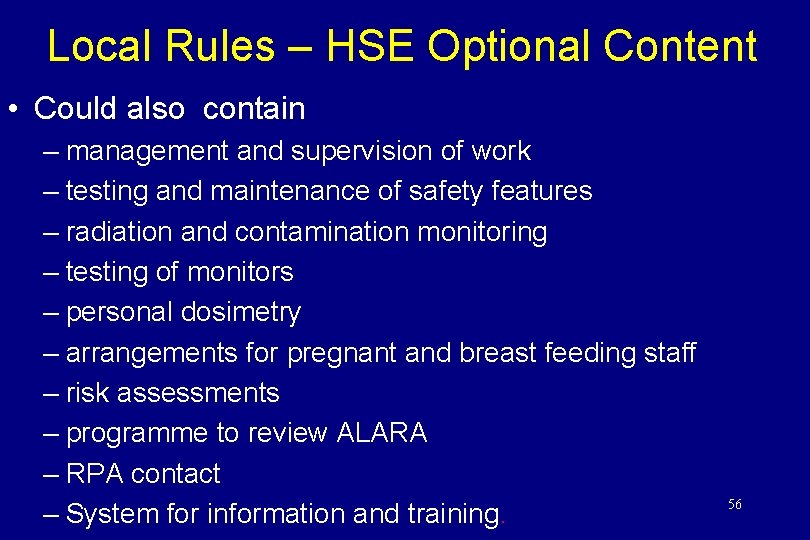
Local Rules – HSE Optional Content • Could also contain – management and supervision of work – testing and maintenance of safety features – radiation and contamination monitoring – testing of monitors – personal dosimetry – arrangements for pregnant and breast feeding staff – risk assessments – programme to review ALARA – RPA contact – System for information and training. 56
Radiation Protection Supervisor R. P. S. • Must be appointed “for the purpose of securing compliance with these Regulations” in controlled or supervised areas • Name must be in Local Rules • It is recommended that – know & understand regs. and local rules – command sufficient authority – understand necessary precautions – know what to do in an emergency. 57
Reg 19 Additional requirements for designated areas Controlled and Supervised Areas must • be adequately described in Local Rules • have suitable & sufficient warning signs • be physically demarcated where reasonably practicable, or by some other means This regulation does not apply to persons undergoing medical exposures 58
Reg 19 Additional requirements for designated areas The employer must not permit a person to enter their Controlled Area unless • They are one of their “Classified Persons”, or • They are a “classified outside worker” (i. e. another employer’s “Classified Person”) who has been suitably trained, is dose assessed and certified fit to do the job, or • enter in accordance with suitable written arrangements (i. e. “Local Rules”) This regulation does not apply to persons undergoing medical exposures 59
Reg 19 Additional requirements for designated areas The written arrangements must ensure • Non-classified persons will not get a dose above a classification trigger level, and • Classified persons do not go above dose limits This regulation does not apply to persons undergoing medical exposures 60
Reg 19 Additional requirements for designated areas • Non-classified outside worker must be provided with PPE and training • No person can enter Controlled Area unless “personal dose monitoring or other suitable measurements” shown dose limits (or classification levels for unclassified staff) will not be exceeded • Results must be kept for at least 2 years • Results must be available to those monitored on request This regulation does not apply to persons undergoing medical exposures 61
Reg 19 Additional requirements for designated areas For “classified outside workers” • Arrangement needed for estimating dose • When finished dose to go in worker’s radiation passbook This regulation does not apply to persons undergoing medical exposures 62
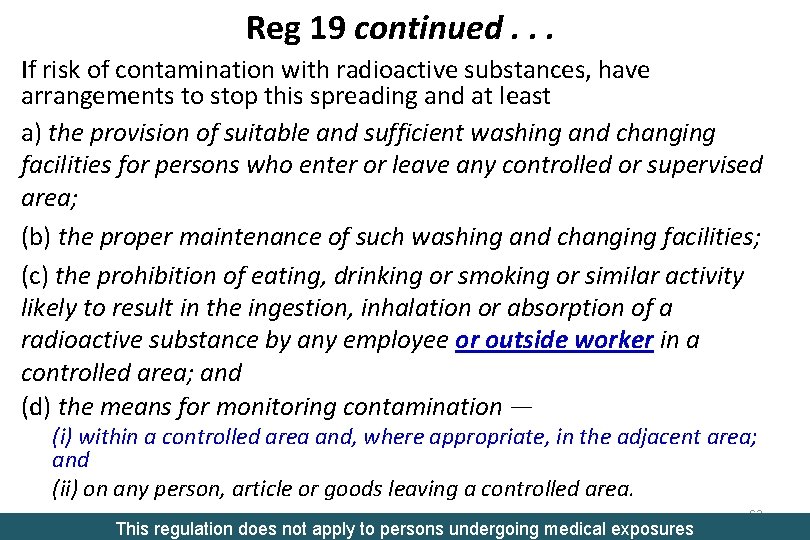
Reg 19 continued. . . If risk of contamination with radioactive substances, have arrangements to stop this spreading and at least a) the provision of suitable and sufficient washing and changing facilities for persons who enter or leave any controlled or supervised area; (b) the proper maintenance of such washing and changing facilities; (c) the prohibition of eating, drinking or smoking or similar activity likely to result in the ingestion, inhalation or absorption of a radioactive substance by any employee or outside worker in a controlled area; and (d) the means for monitoring contamination — (i) within a controlled area and, where appropriate, in the adjacent area; and (ii) on any person, article or goods leaving a controlled area. This regulation does not apply to persons undergoing medical exposures 63
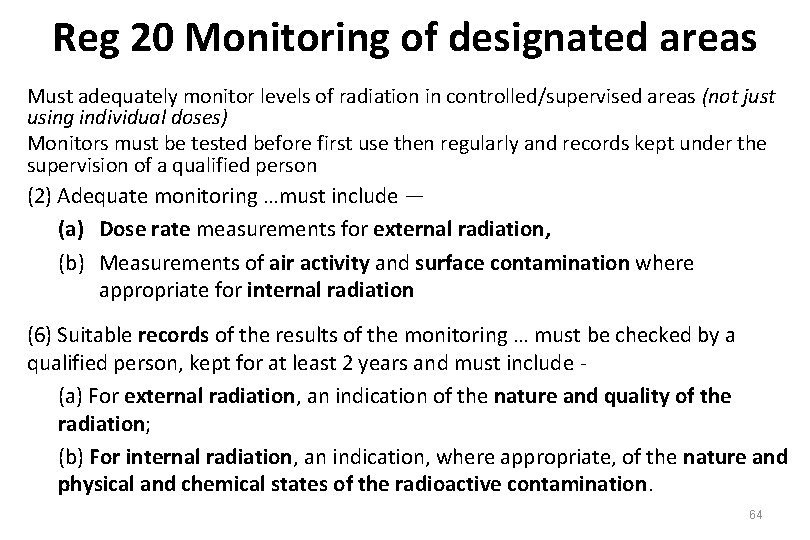
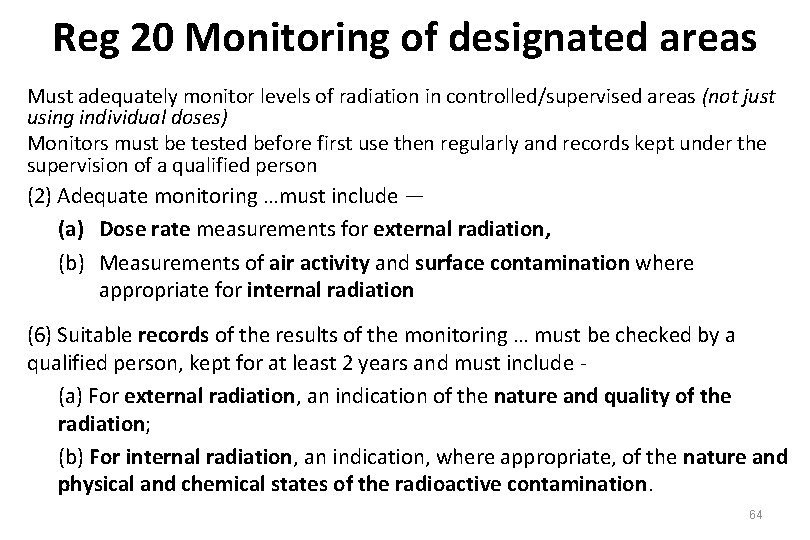
Reg 20 Monitoring of designated areas Must adequately monitor levels of radiation in controlled/supervised areas (not just using individual doses) Monitors must be tested before first use then regularly and records kept under the supervision of a qualified person (2) Adequate monitoring …must include — (a) Dose rate measurements for external radiation, (b) Measurements of air activity and surface contamination where appropriate for internal radiation (6) Suitable records of the results of the monitoring … must be checked by a qualified person, kept for at least 2 years and must include (a) For external radiation, an indication of the nature and quality of the radiation; (b) For internal radiation, an indication, where appropriate, of the nature and physical and chemical states of the radioactive contamination. 64
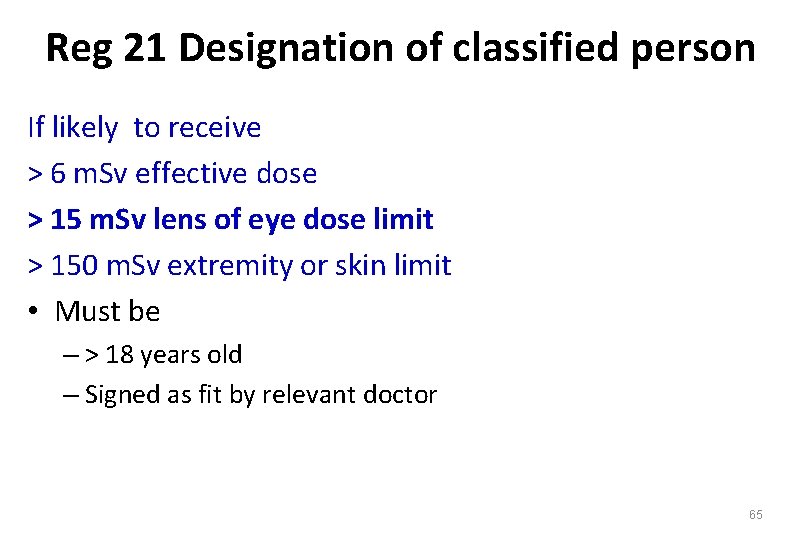
Reg 21 Designation of classified person If likely to receive > 6 m. Sv effective dose > 15 m. Sv lens of eye dose limit > 150 m. Sv extremity or skin limit • Must be – > 18 years old – Signed as fit by relevant doctor 65
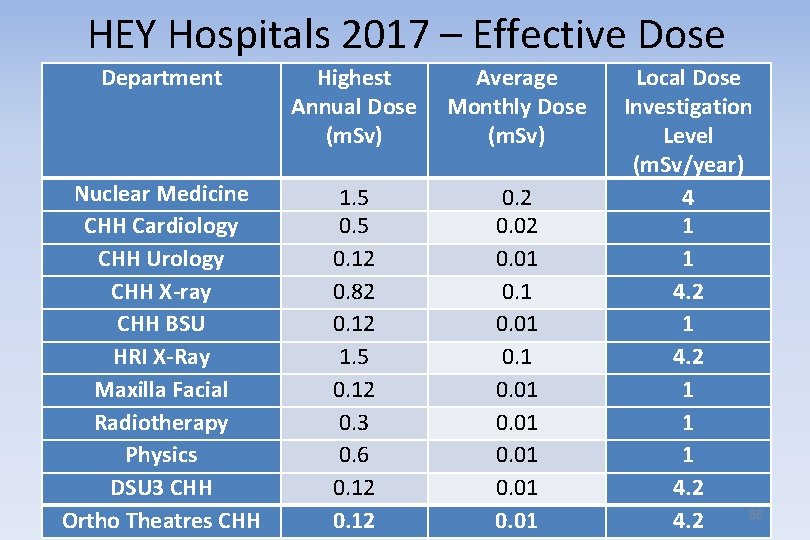
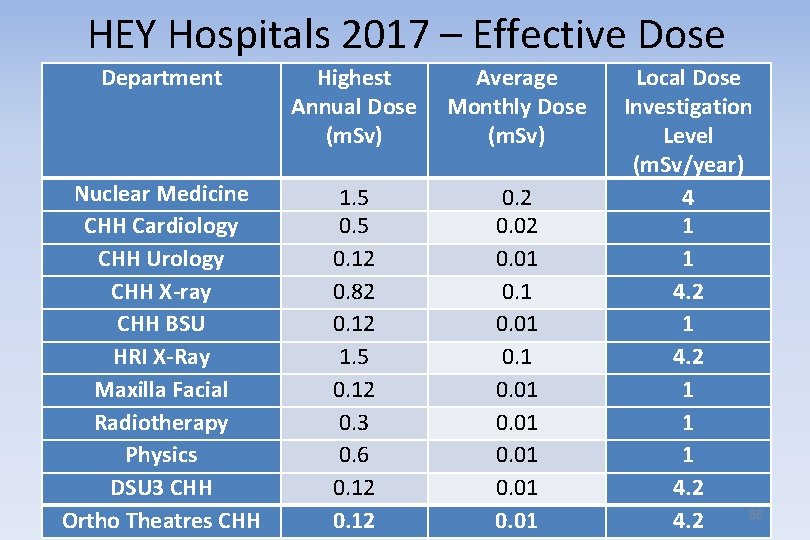
HEY Hospitals 2017 – Effective Dose Department Highest Annual Dose (m. Sv) Average Monthly Dose (m. Sv) Nuclear Medicine CHH Cardiology CHH Urology CHH X-ray CHH BSU HRI X-Ray Maxilla Facial Radiotherapy Physics DSU 3 CHH Ortho Theatres CHH 1. 5 0. 12 0. 82 0. 12 1. 5 0. 12 0. 3 0. 6 0. 12 0. 01 0. 01 Local Dose Investigation Level (m. Sv/year) 4 1 1 4. 2 1 1 1 4. 2 66 4. 2
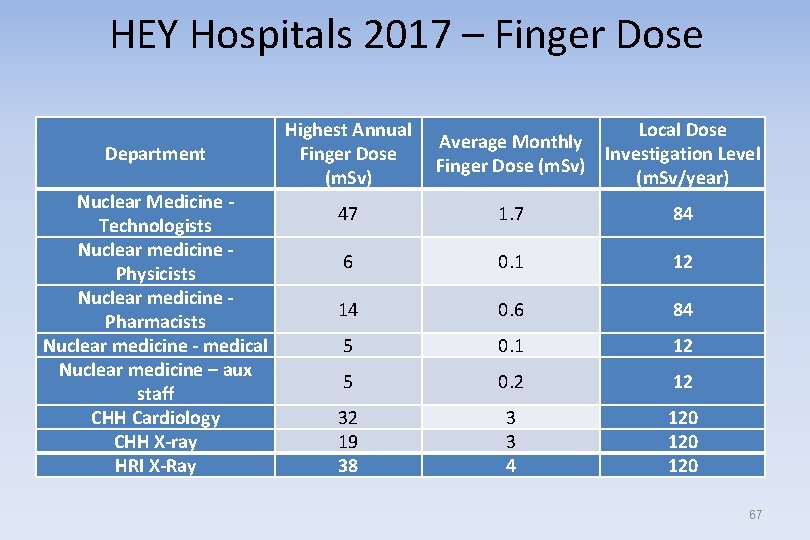
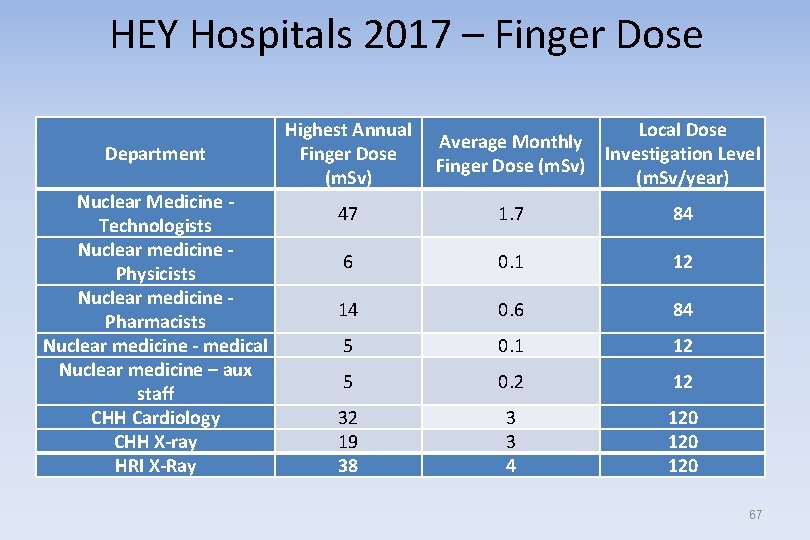
HEY Hospitals 2017 – Finger Dose Department Nuclear Medicine Technologists Nuclear medicine Physicists Nuclear medicine Pharmacists Nuclear medicine - medical Nuclear medicine – aux staff CHH Cardiology CHH X-ray HRI X-Ray Highest Annual Finger Dose (m. Sv) Local Dose Average Monthly Investigation Level Finger Dose (m. Sv) (m. Sv/year) 47 1. 7 84 6 0. 1 12 14 0. 6 84 5 0. 1 12 5 0. 2 12 32 19 38 3 3 4 120 120 67
Regulation 22 Dose assessment and recording Applied to classified persons only • Dose monitored and recorded to age 75 and at least for 30 years with an HSE Approved Dosimetry Service results to HSE • Radiation passbook for “outside workers” • Adequate (at least yearly) medical surveillance - record to 75 and at least for 30 y 68
Reg 23 Estimated and notional doses and special entries • What to do if classified person’s dose badge – lost or damaged – is clearly wrong 69
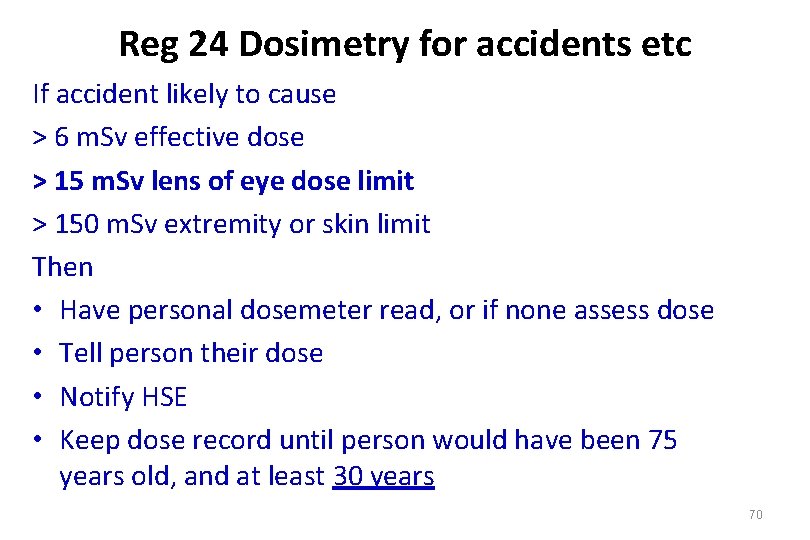
Reg 24 Dosimetry for accidents etc If accident likely to cause > 6 m. Sv effective dose > 15 m. Sv lens of eye dose limit > 150 m. Sv extremity or skin limit Then • Have personal dosemeter read, or if none assess dose • Tell person their dose • Notify HSE • Keep dose record until person would have been 75 years old, and at least 30 years 70
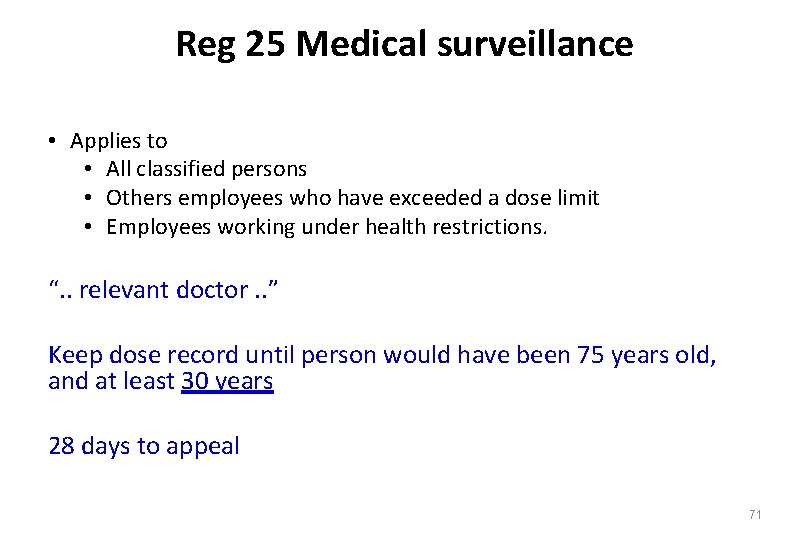
Reg 25 Medical surveillance • Applies to • All classified persons • Others employees who have exceeded a dose limit • Employees working under health restrictions. “. . relevant doctor. . ” Keep dose record until person would have been 75 years old, and at least 30 years 28 days to appeal 71
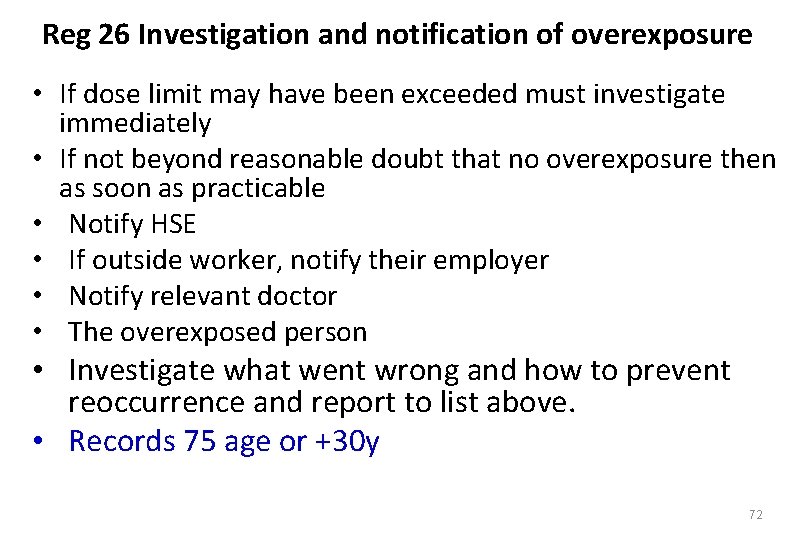
Reg 26 Investigation and notification of overexposure • If dose limit may have been exceeded must investigate immediately • If not beyond reasonable doubt that no overexposure then as soon as practicable • Notify HSE • If outside worker, notify their employer • Notify relevant doctor • The overexposed person • Investigate what went wrong and how to prevent reoccurrence and report to list above. • Records 75 age or +30 y 72
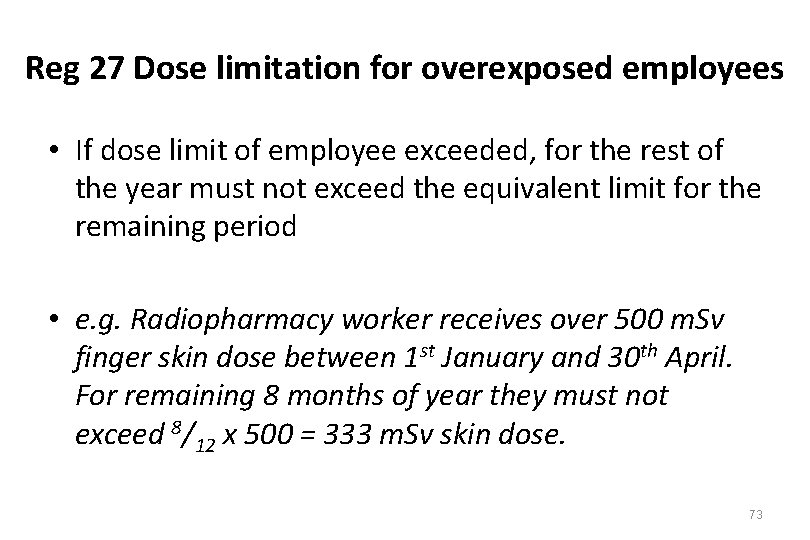
Reg 27 Dose limitation for overexposed employees • If dose limit of employee exceeded, for the rest of the year must not exceed the equivalent limit for the remaining period • e. g. Radiopharmacy worker receives over 500 m. Sv finger skin dose between 1 st January and 30 th April. For remaining 8 months of year they must not exceed 8/12 x 500 = 333 m. Sv skin dose. 73
Reg 28 Sealed sources and articles containing or embodying radioactive substances • Use sealed sources when reasonably practicable • Design and maintain them so they don’t leak • Undertake suitable leak testing and keep records for at least 2 years after disposal of source or until next leak test 74
Reg 29 Accounting for radioactive substances • Audit sources and keep records for 2 years and at least 2 years after disposal. 75
Reg 30 Keeping and moving of radioactive substances • Keep sources in suitable receptacles in suitable stores when not being moved • When being moved, transport in a suitable, labelled receptacle • Doesn’t apply if source inside a live body or corpse of a human being 76
Reg 31 Notification of certain occurrences • Notify HSE if spill or release of more than Schedule 7 Part 1 column 5 level (e. g. 10, 000 GBq 99 Tcm) • Notify HSE if lost or stolen more than Schedule 7 Part 1 column 6 level (e. g. 0. 1 GBq 99 Tcm) • Investigate immediately, make report and keep for 50 years (2 years if investigation shows no spill above levels) 77
Reg 32 Duties of manufacturers etc of articles for use in work with ionising radiation • Installers must undertake a Critical Examination of safety features and warning devices to ensure they work and are sufficient. They must consult an RPA. • articles must be designed to keep doses ALARP • Installer must provide adequate info to user on proper use, testing and maintenance. This regulation does not apply to persons undergoing medical exposures 78
Reg 33 Equipment used for medical exposure 79
Reg 34 Misuse of or interference with sources of ionising radiation “No person may intentionally or recklessly misuse or without reasonable excuse interfere with any radioactive substance or any electrical equipment to which these Regulations apply. ” • Applies to employees and public, and not just employers. 80
Reg 35 Duties of employees • Employees must not knowingly expose themselves or others to a dose greater than reasonably necessary (does not apply to those undergoing medical exposures) • If medical surveillance required, must undergo • Report suspected overexposures • Employees and outside workers must use PPE provided, report any defects and return after use to accommodation provided This regulation does not apply to persons undergoing medical exposures 81
IRR 1999/2017 • Reg 37 Approval of dosimetry services – Now includes emergency dosimetry • Reg 37 Defence on contravention – e. g. if it is completely someone else’s fault • Reg 38 Exemption certificates – At HSE discretion • Reg 39 Extension outside Great Britain – e. g North Sea oil rigs, etc. • etc. 82
Here on 17/9/2020 83