First Aid Part 1 From Wound Care To





- Slides: 50
First Aid Part 1 From Wound Care To Rabies!

Be Prepared
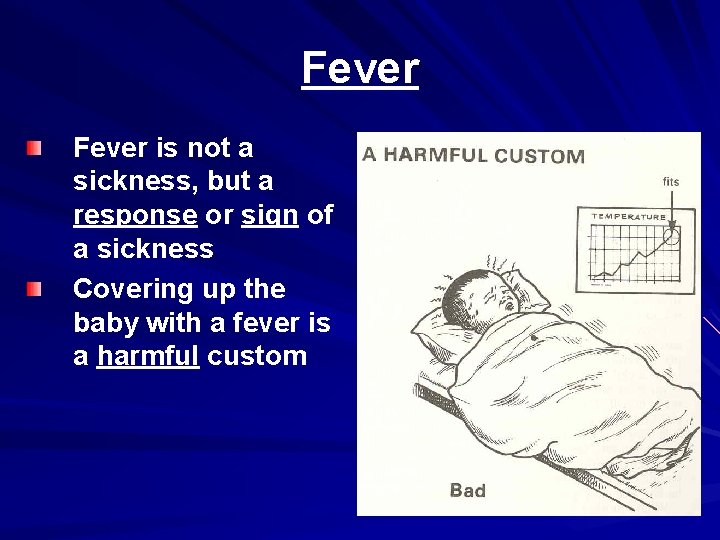
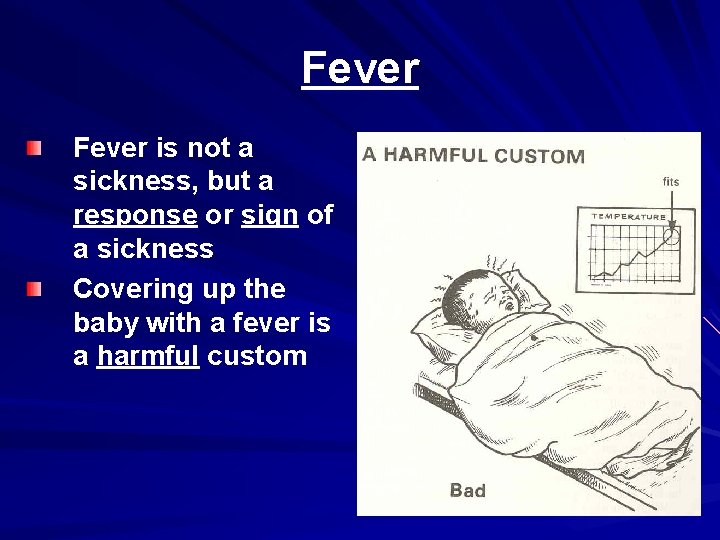
Fever is not a sickness, but a response or sign of a sickness Covering up the baby with a fever is a harmful custom
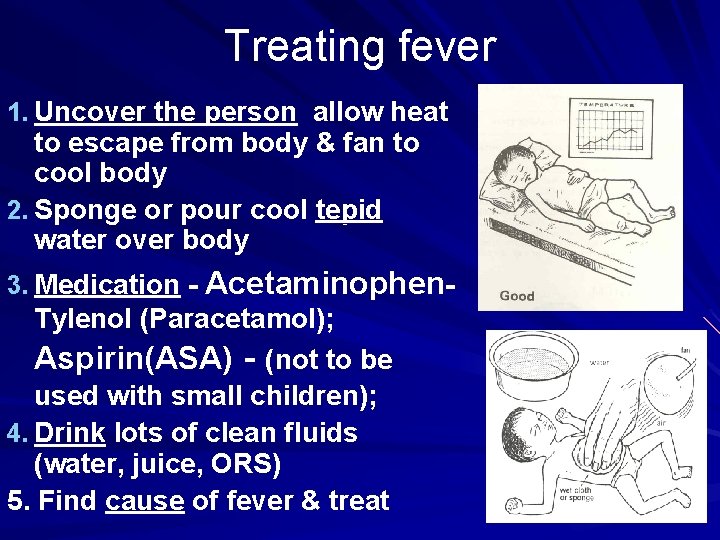
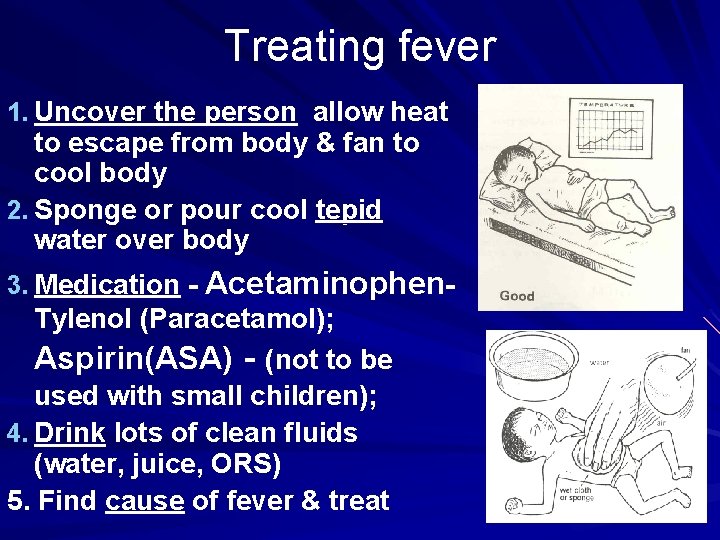
Treating fever 1. Uncover the person allow heat to escape from body & fan to cool body 2. Sponge or pour cool tepid water over body 3. Medication - Acetaminophen- Tylenol (Paracetamol); Aspirin(ASA) - (not to be used with small children); 4. Drink lots of clean fluids (water, juice, ORS) 5. Find cause of fever & treat
Soft tissue injury-Wound Care Two types wounds: Closed Wounds – – Bruise (contusion) Blood & fluid seep into tissue discoloration Open wounds – – Abrasions Lacerations Avulsion Puncture
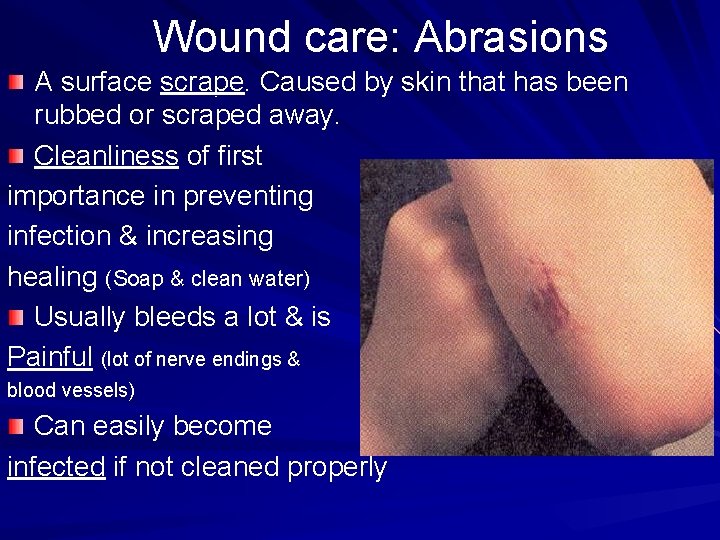
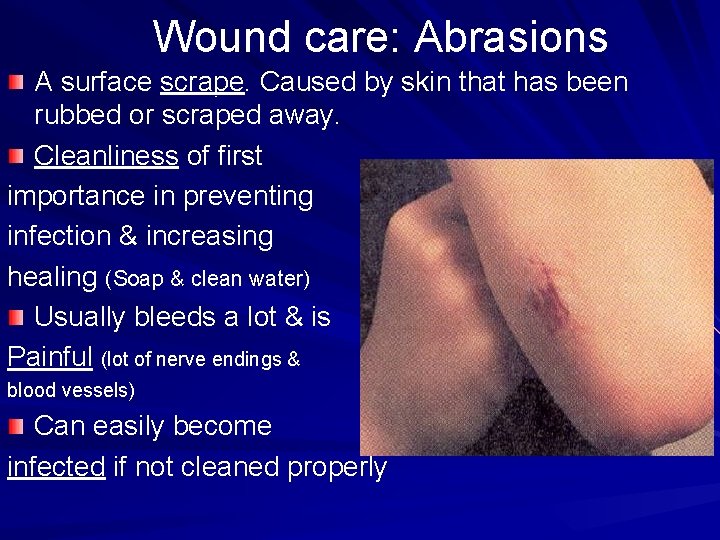
Wound care: Abrasions A surface scrape. Caused by skin that has been rubbed or scraped away. Cleanliness of first importance in preventing infection & increasing healing (Soap & clean water) Usually bleeds a lot & is Painful (lot of nerve endings & blood vessels) Can easily become infected if not cleaned properly
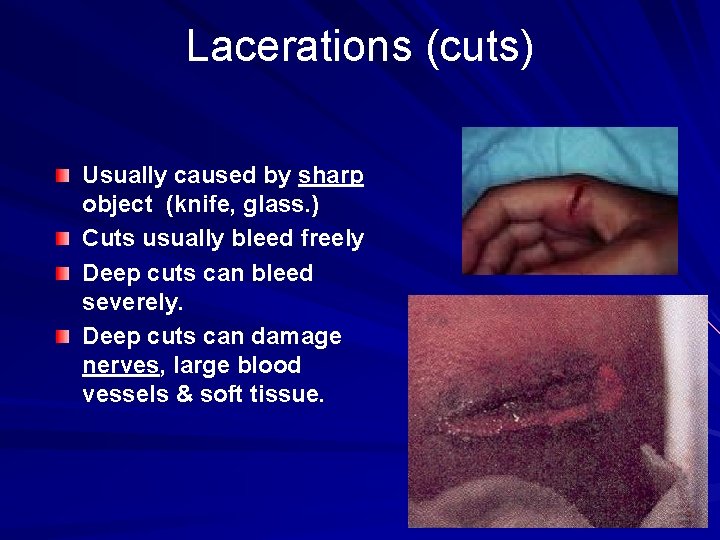
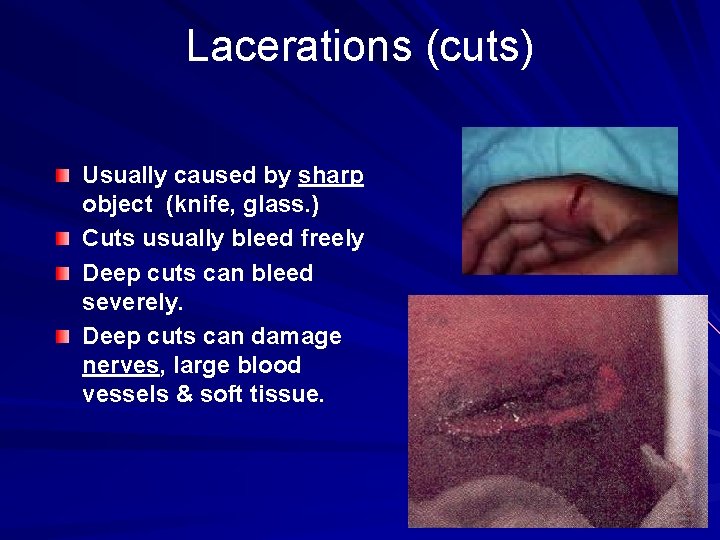
Lacerations (cuts) Usually caused by sharp object (knife, glass. ) Cuts usually bleed freely Deep cuts can bleed severely. Deep cuts can damage nerves, large blood vessels & soft tissue.

Child at the gate of missionary with cut to foot in Malawi, Africa
Puncture wound Wound caused by pointed object (nail, thorn, piece of glass… Usually doesn’t bleed easily infected. If penetrates a major blood vessel - bleeding may be severe. Frequently found on feet from going bare-footed. May need a tetanus injection.
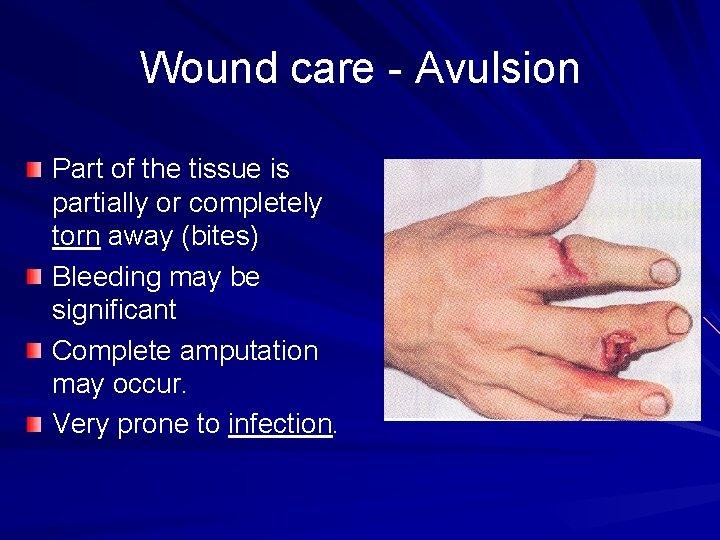
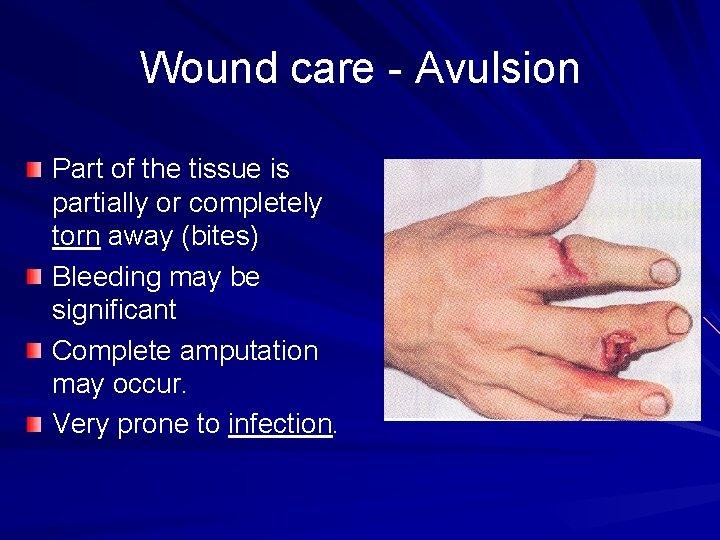
Wound care - Avulsion Part of the tissue is partially or completely torn away (bites) Bleeding may be significant Complete amputation may occur. Very prone to infection.
Wounds: Preventing Infection Cleanliness most important step in preventing infection Wash hands & wound with soap & clean water Pick out dirt and trash from wound Cover with clean gauze or cloth Never put alcohol, iodine or methiolate directly on wound Never use dirty poultice Give Tetanus shot
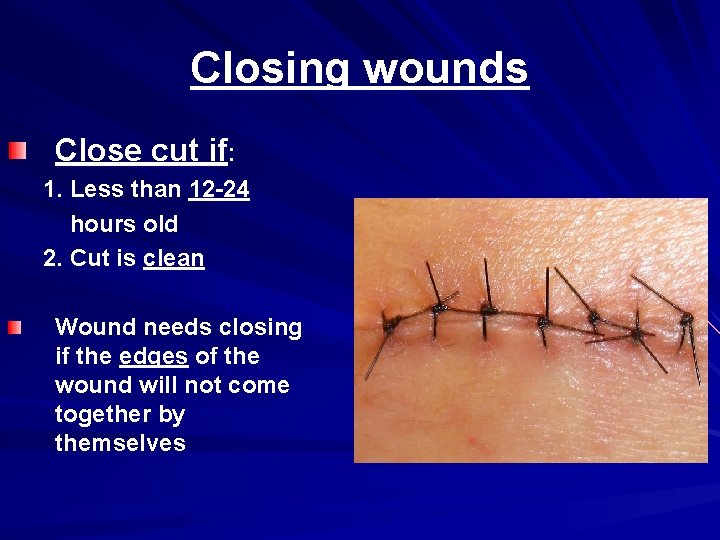
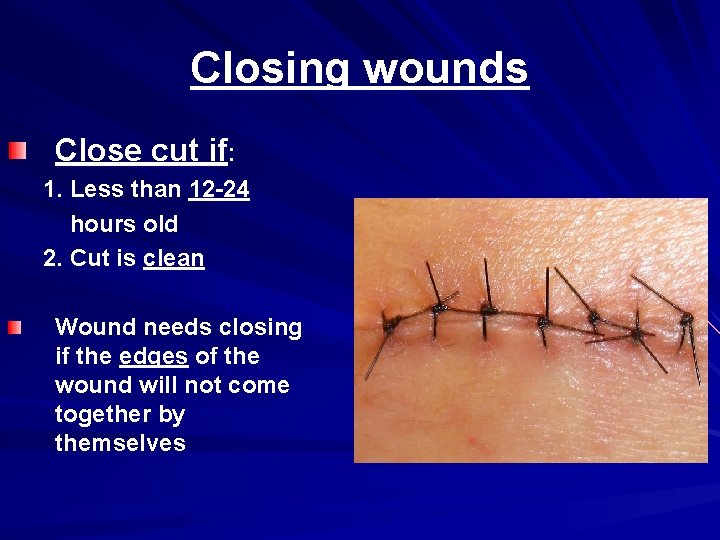
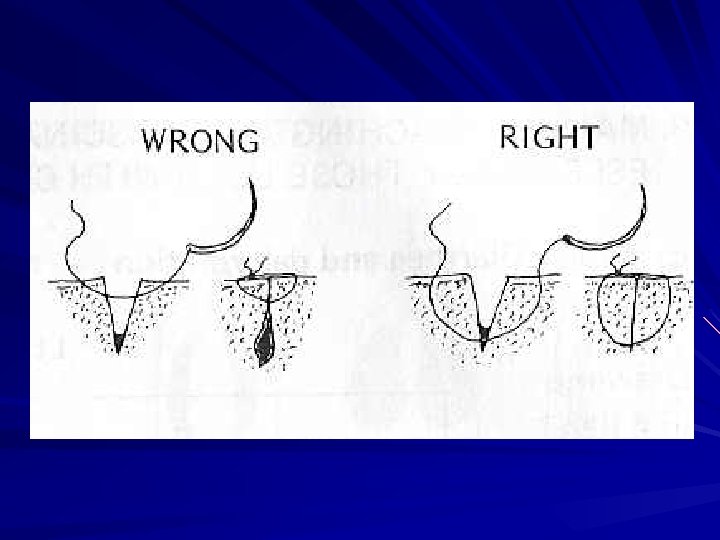
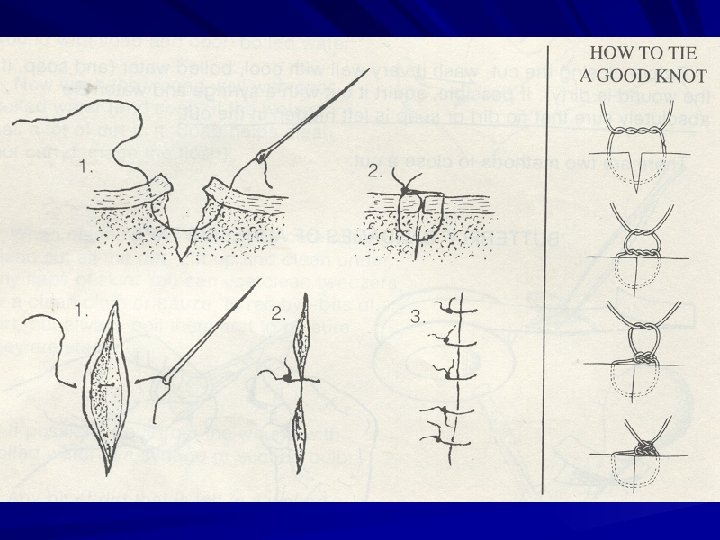
Closing wounds Close cut if: 1. Less than 12 -24 hours old 2. Cut is clean Wound needs closing if the edges of the wound will not come together by themselves
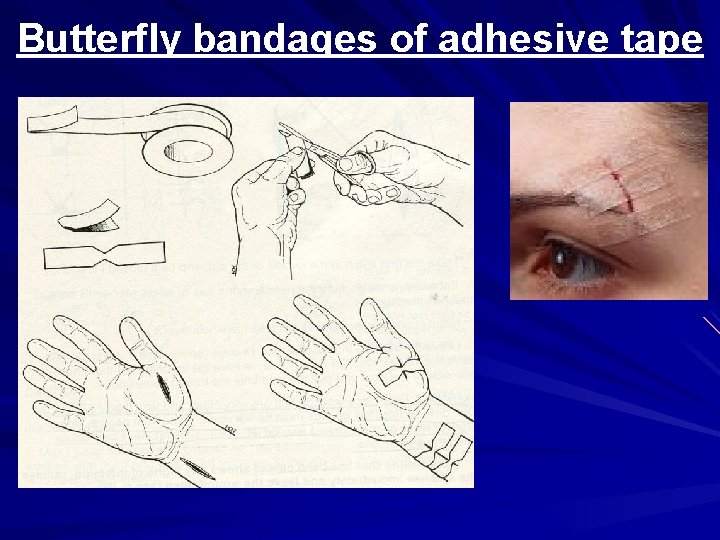
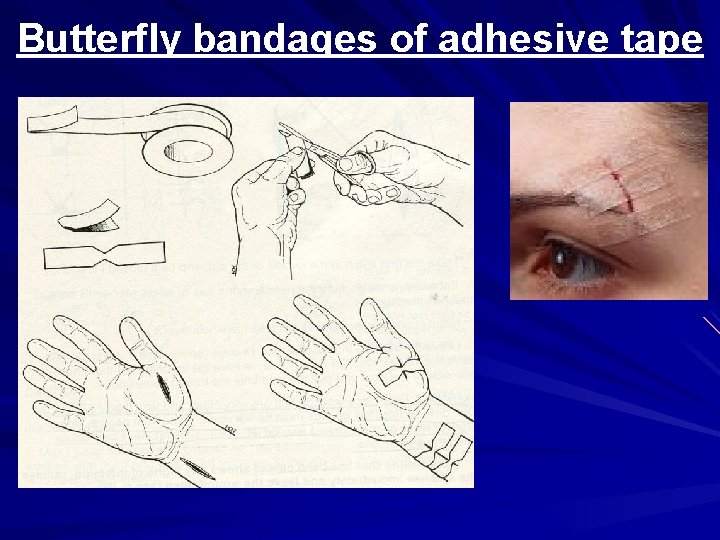
Butterfly bandages of adhesive tape
Sewing or suturing with thread Boil sewing needle & thread (nylon or silk is best) for 20 minutes Wash your hands Wash wound Sew pulling the edges of the tissue together
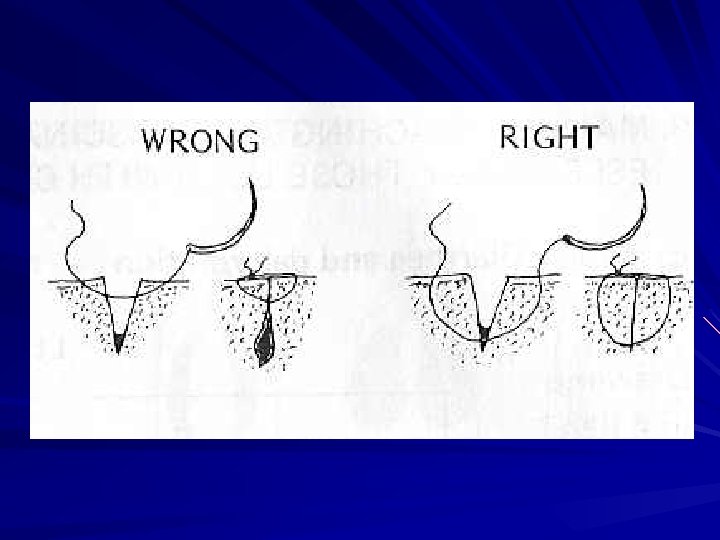
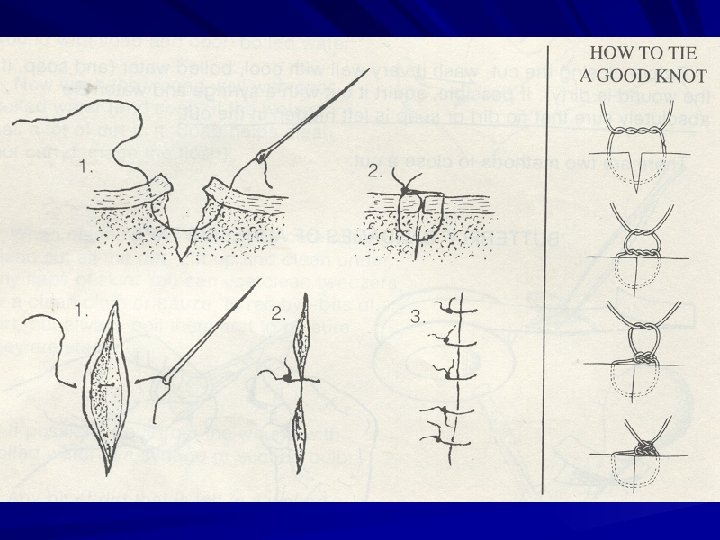
Sewing or suturing Leave stitches for 5 -14 days depending on where located DO NOT CLOSE old, dirty, infected wounds DO NOT CLOSE bites from humans, dogs, pigs, or other animals – can cause dangerous infections If the wound shows s/s of infection, remove stitches & leave open

When is a wound infected? Red, swollen, hot, & painful May have pus in wound May smell bad Infection is spreading to other parts of body when: – The person has a fever – Red line runs from the wound – Lymph nodes become swollen & tender
Treating an infected wound! Hot compresses for 20 minutes X 4 daily – May hold infected hand or foot in bucket of clean hot water Rest and elevation of infected part Vaccination against tetanus Antibiotic: Penicillin, Ampillicin Complication: gangrene
Wounds likely to become dangerously infected Dirty wounds or wounds made with contaminated objects Puncture wounds that do not bleed well. Wounds made where animals are kept Large wounds with severe crushing or bruising Bites from dogs, people, or pigs
Special care for “Hi-risk” wounds Wash well with boiled water & soap. Remove all dirt, blood clots, damaged flesh If it is deep, a wound may still have dirt in it - use antibiotics. Do NOT close this type wound The danger of tetanus is greater Elevate the wounded part higher than the heart & keep it immobilized.
Bleeding External bleeding: – Arterial: rapid due to ↑pressure, harder to control, bright red in color – Venous: less pressure, steady rate & dark red in color – Capillary: most common, slow, oozes out. Severe external bleeding – Blood spurting from wound – Bleeding that fails to stop after all measures.
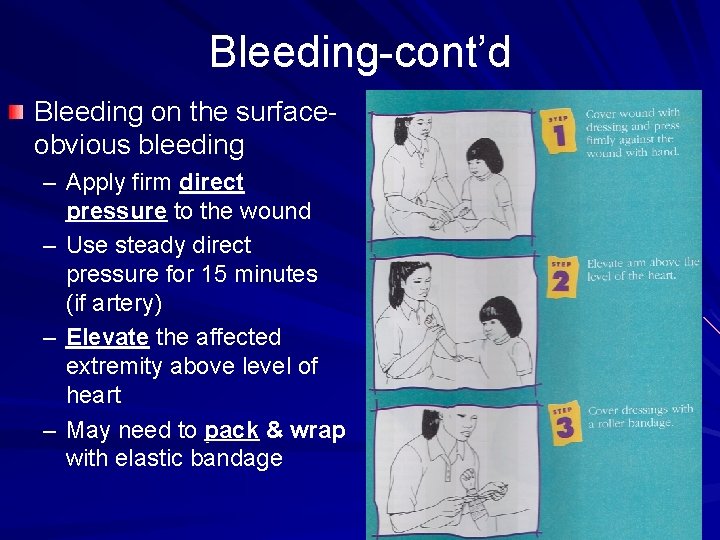
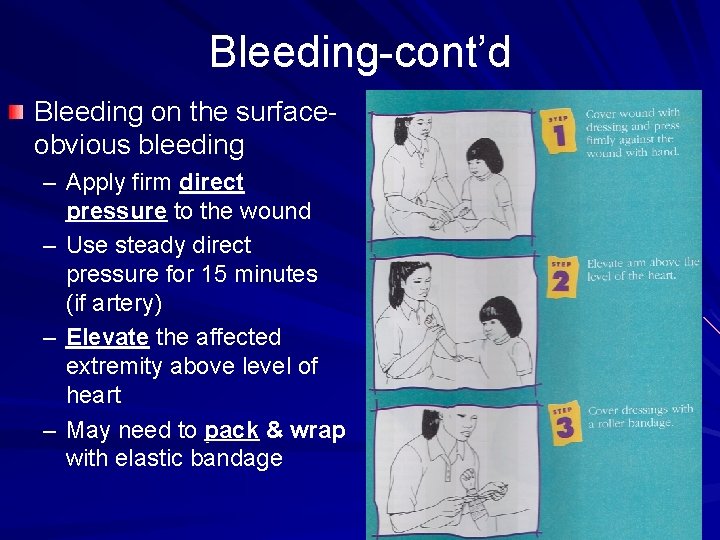
Bleeding-cont’d Bleeding on the surfaceobvious bleeding – Apply firm direct pressure to the wound – Use steady direct pressure for 15 minutes (if artery) – Elevate the affected extremity above level of heart – May need to pack & wrap with elastic bandage
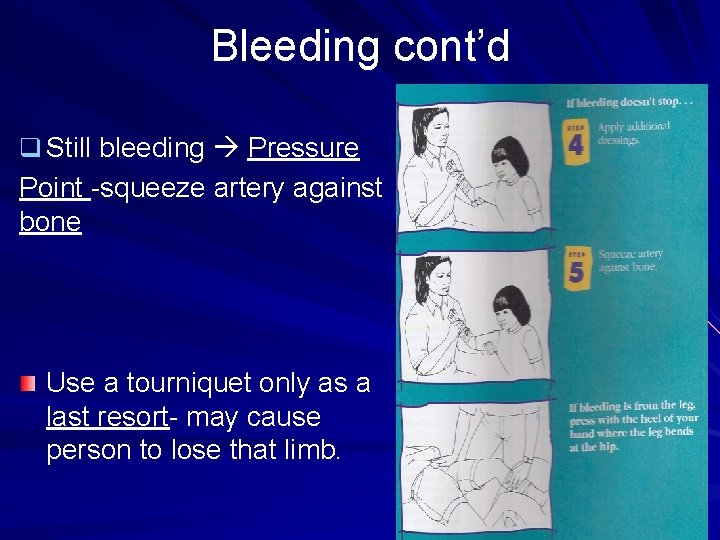
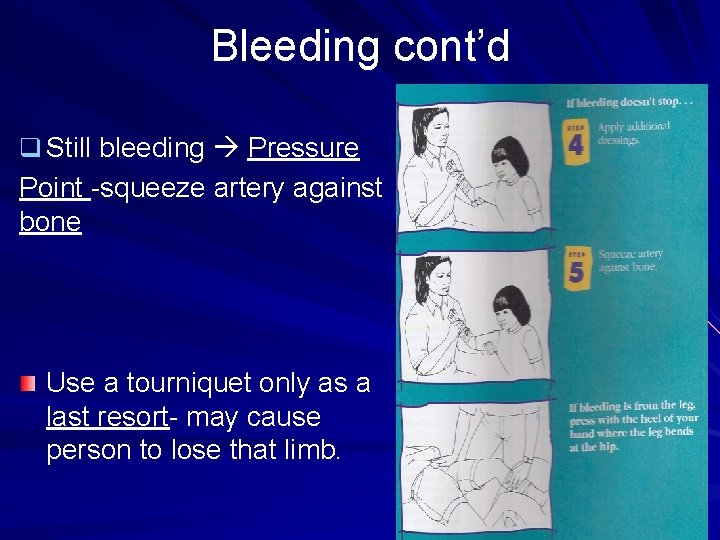
Bleeding cont’d q Still bleeding Pressure Point -squeeze artery against bone Use a tourniquet only as a last resort- may cause person to lose that limb.
Internal Bleeding & Hemorrhage Internal bleeding – Suspect with: blunt force, penetration, fracture – Internal bleeding - how would you know? Person will feel dizzy or faint, will be pale. Pulse will increase & B/P will decrease Skin cool, moist, pale or cyanotic (bluish) Anxiety, restlessness, & rapid breathing Soft tissue-tender, swollen or hard Decreased level of consciousness – Treat for shock immediately. – Transfer patient to the hospital quickly.
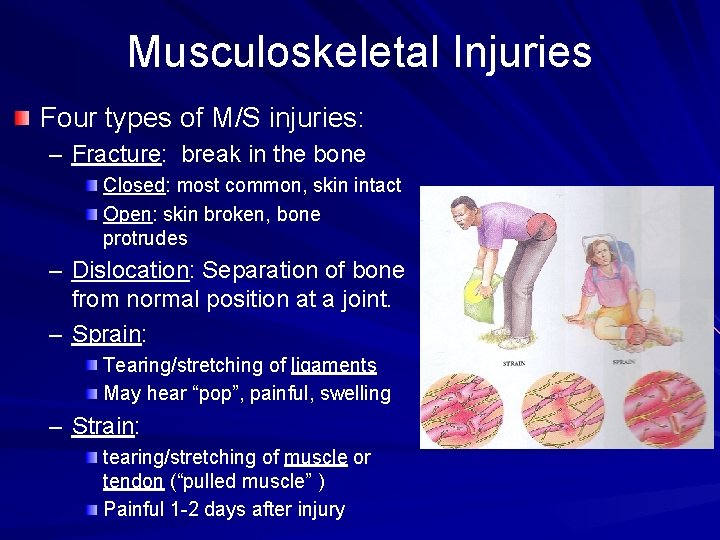
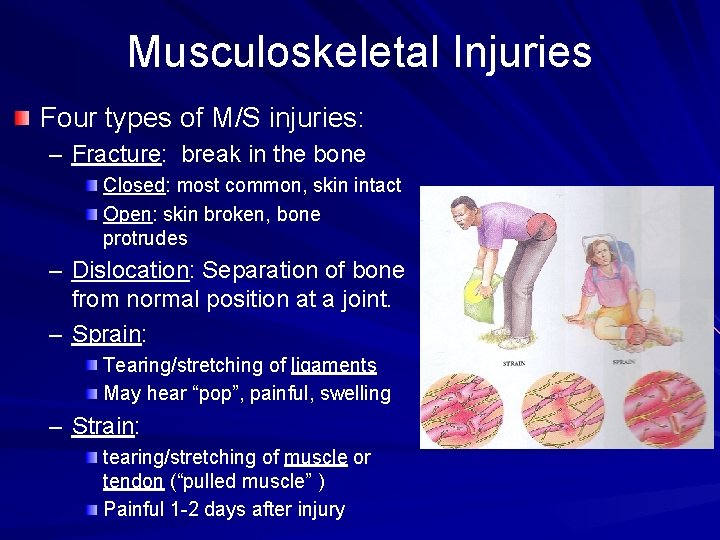
Musculoskeletal Injuries Four types of M/S injuries: – Fracture: break in the bone Closed: most common, skin intact Open: skin broken, bone protrudes – Dislocation: Separation of bone from normal position at a joint. – Sprain: Tearing/stretching of ligaments May hear “pop”, painful, swelling – Strain: tearing/stretching of muscle or tendon (“pulled muscle” ) Painful 1 -2 days after injury
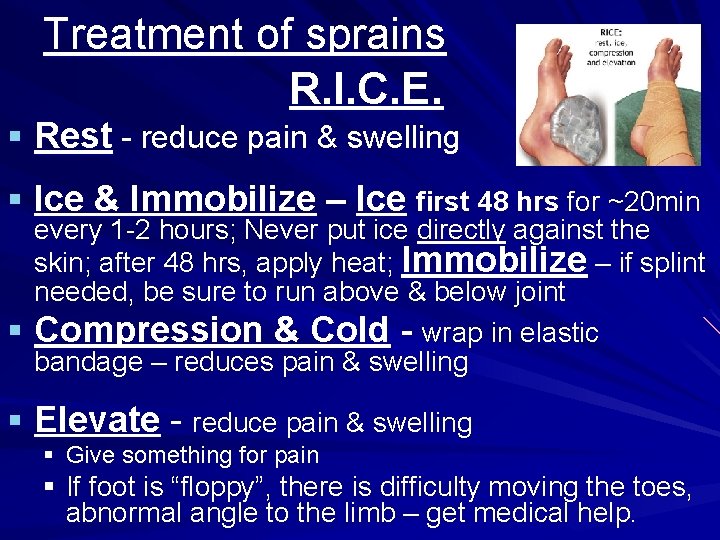
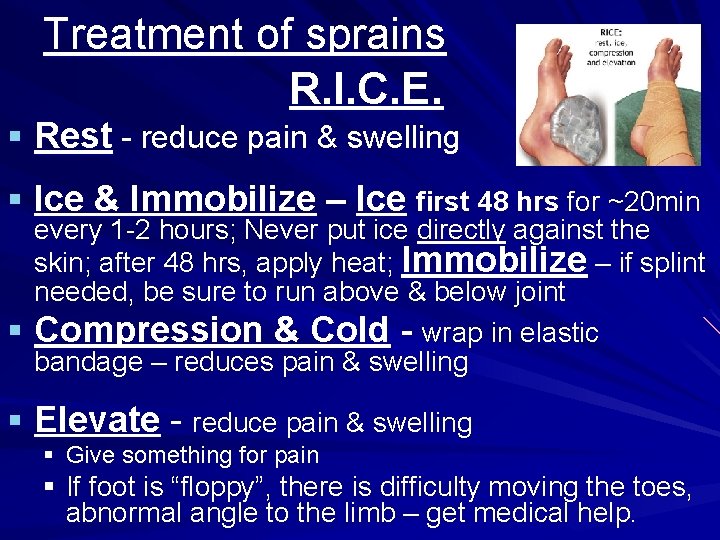
Treatment of sprains R. I. C. E. § Rest - reduce pain & swelling § Ice & Immobilize – Ice first 48 hrs for ~20 min every 1 -2 hours; Never put ice directly against the skin; after 48 hrs, apply heat; Immobilize – if splint needed, be sure to run above & below joint § Compression & Cold - wrap in elastic bandage – reduces pain & swelling § Elevate - reduce pain & swelling § Give something for pain § If foot is “floppy”, there is difficulty moving the toes, abnormal angle to the limb – get medical help.
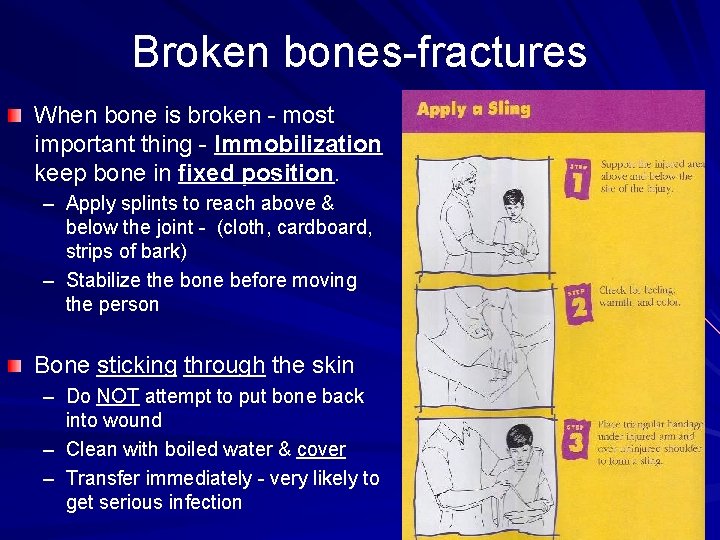
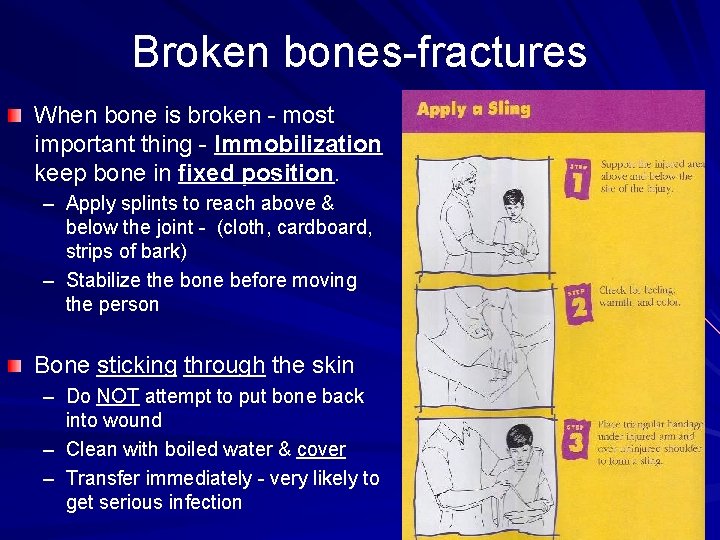
Broken bones-fractures When bone is broken - most important thing - Immobilization keep bone in fixed position. – Apply splints to reach above & below the joint - (cloth, cardboard, strips of bark) – Stabilize the bone before moving the person Bone sticking through the skin – Do NOT attempt to put bone back into wound – Clean with boiled water & cover – Transfer immediately - very likely to get serious infection
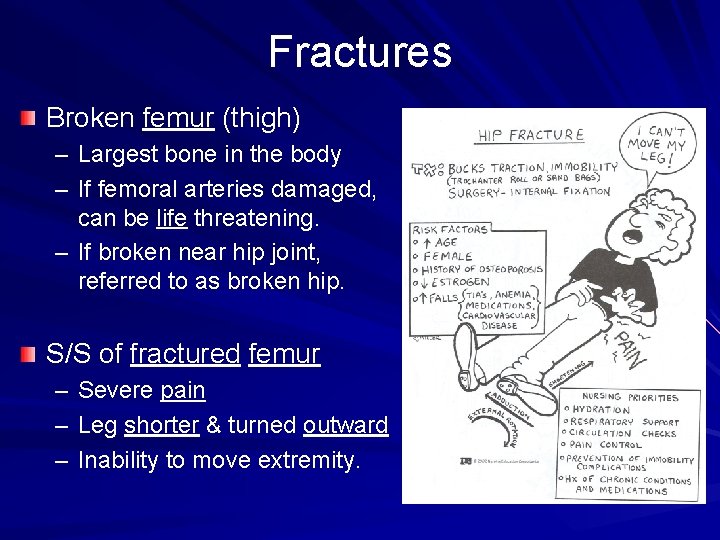
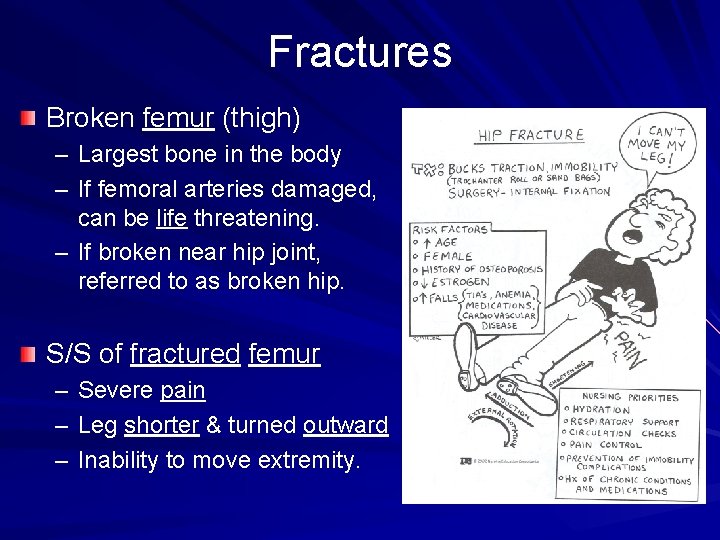
Fractures Broken femur (thigh) – Largest bone in the body – If femoral arteries damaged, can be life threatening. – If broken near hip joint, referred to as broken hip. S/S of fractured femur – – – Severe pain Leg shorter & turned outward Inability to move extremity.
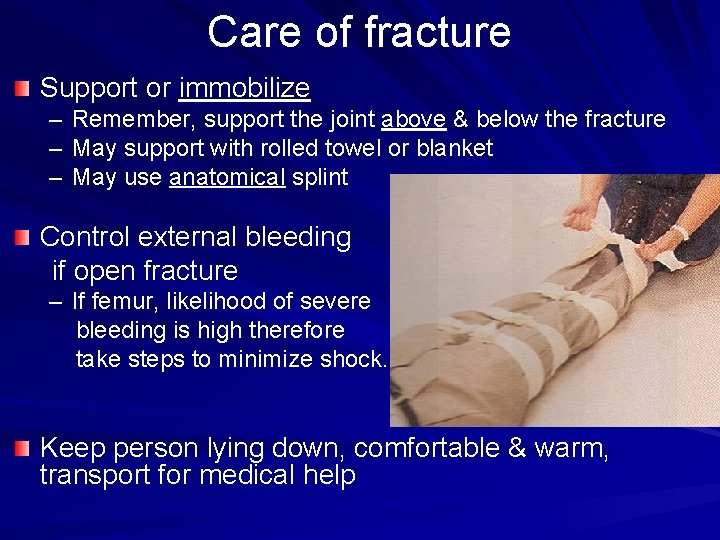
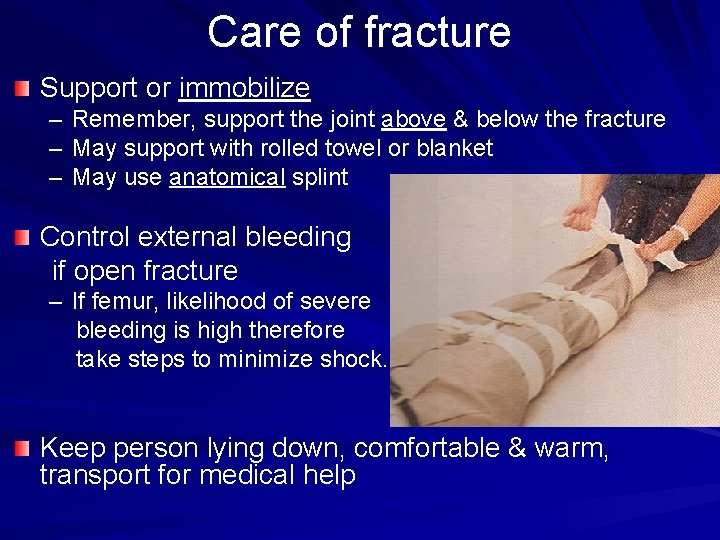
Care of fracture Support or immobilize – – – Remember, support the joint above & below the fracture May support with rolled towel or blanket May use anatomical splint Control external bleeding if open fracture – If femur, likelihood of severe bleeding is high therefore take steps to minimize shock. Keep person lying down, comfortable & warm, transport for medical help
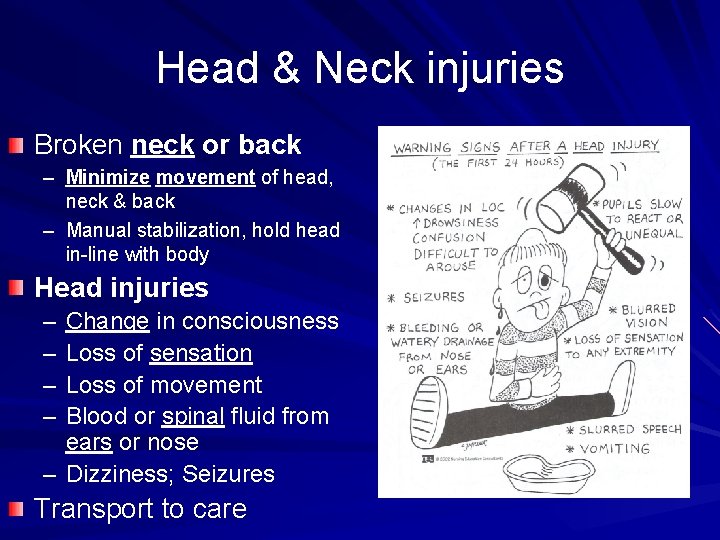
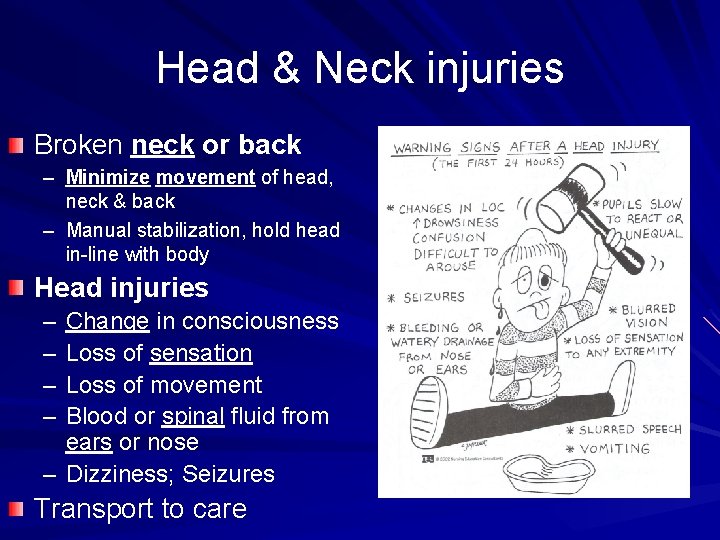
Head & Neck injuries Broken neck or back – Minimize movement of head, neck & back – Manual stabilization, hold head in-line with body Head injuries – – Change in consciousness Loss of sensation Loss of movement Blood or spinal fluid from ears or nose – Dizziness; Seizures Transport to care
Poisoning Four ways poisons enter the body: – Inhalation – Ingestion - Absorption - Injection Inhaled poisons: – Breathing in toxic fumes – Carbon monoxide: colorless, odorless gas Tx: Remove from source Provide oxygen or fresh air
Ingested poisons Bacterial food poisonings – Salmonella often found in poultry, pork, eggs & dairy products. – Botulism, the most deadly food poison (toxin associated with home canning) – Signs/symptoms of food poisoning (4 -6 hrs) Nausea, vomiting & diarrhea (N/V/D) dehydration Abdominal pain Fever Prevention: proper cooking, refrigeration & proper sanitation.
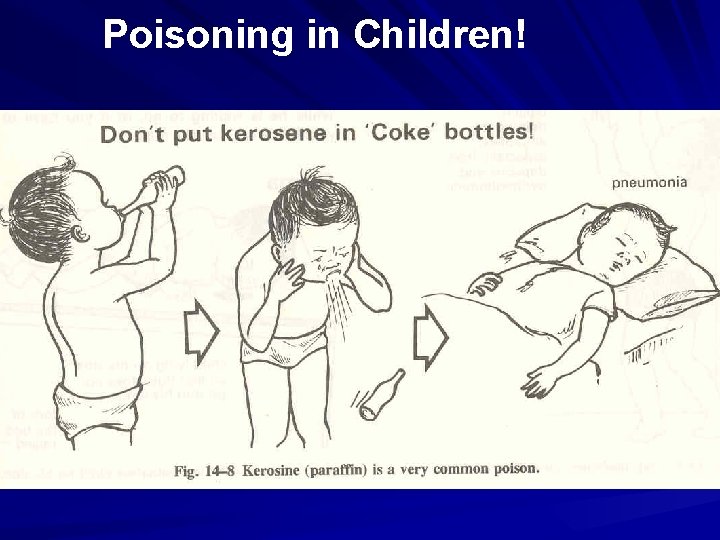
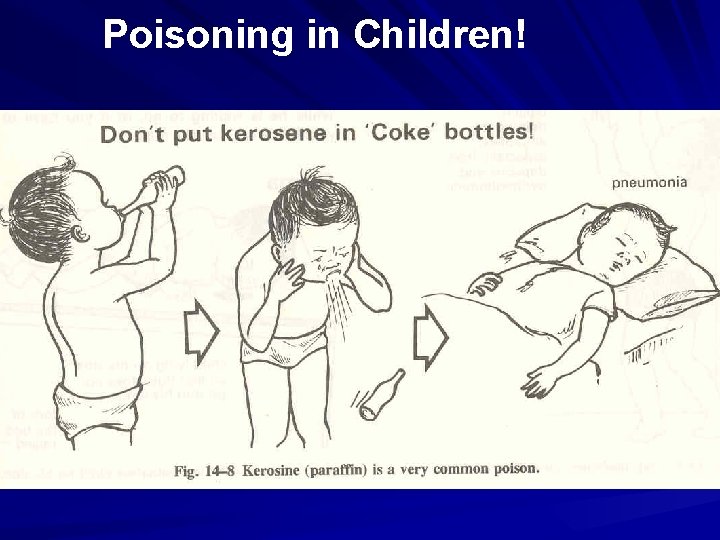
Poisoning in Children!
Poisoning Keep all poisons out of reach of children Never keep kerosene, gasoline, bleach, etc. in coke bottles Some common poisons: – – – rat poison Insecticides medication (Iron, Tylenol) bleach; lye; salt spoiled food Plants
Treatment of Poisonings Determine the product of poisoning If a petroleum product such as gasoline, kerosene, or strong acid or corrosive substance (lye) do not induce vomiting – give water to dilute solution Do the following immediately (if not above) – Induce vomiting with your finger or mild soap or salt solution Medical help if severe
Chemicals in the eye Rinse the eye immediately with water – Must be done very quickly – Must use copious amounts of water – A quart of water/eye is minimum – Rinse from nose side to outside of eye Alkali: drain, toilet bowl & oven cleaners these actually do more damage than acids Acids: damage is usually immediately apparent.
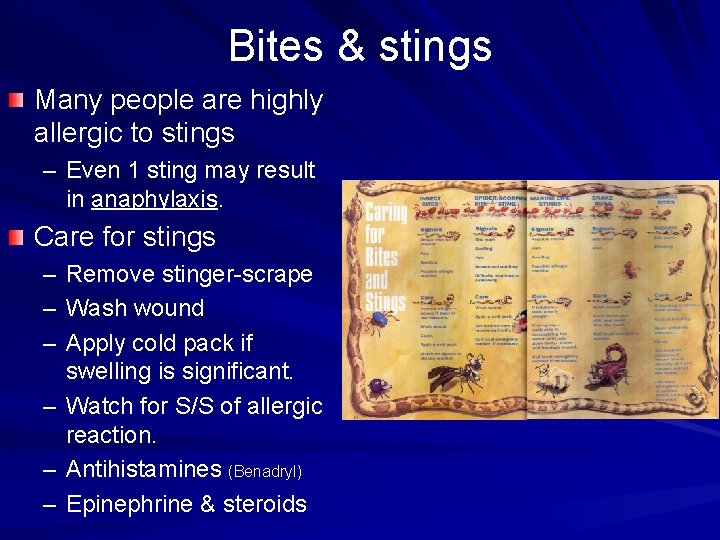
Bites & stings Many people are highly allergic to stings – Even 1 sting may result in anaphylaxis. Care for stings – Remove stinger-scrape – Wash wound – Apply cold pack if swelling is significant. – Watch for S/S of allergic reaction. – Antihistamines (Benadryl) – Epinephrine & steroids
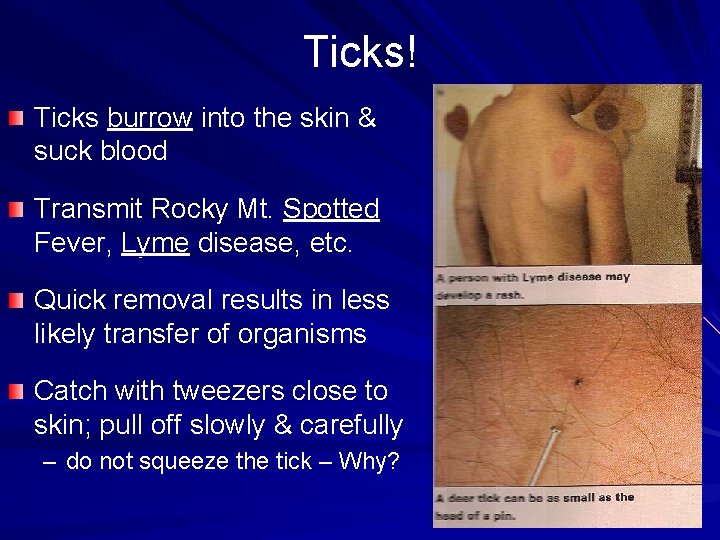
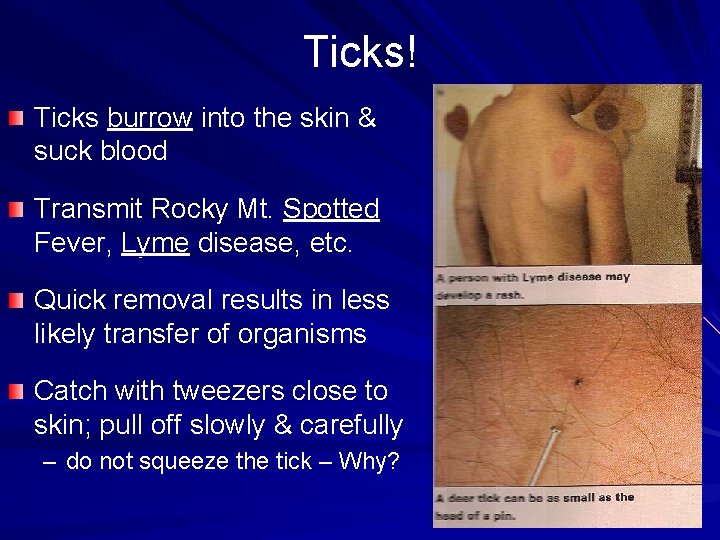
Ticks! Ticks burrow into the skin & suck blood Transmit Rocky Mt. Spotted Fever, Lyme disease, etc. Quick removal results in less likely transfer of organisms Catch with tweezers close to skin; pull off slowly & carefully – do not squeeze the tick – Why?
Rabies Cause: Rabies virus Uniformly fatal infection once S/S appear – Can prevent death with post-exposure vaccine injections Animal reservoir of rabies USA: Domestic - cat most commonly; then wild animals raccoons, skunks, bats, foxes… – Worldwide most common domestic reservoir – dogs Animal exposure source to rabies USA: bats; worldwide: dogs Transmission: – viral laden saliva of rabid animal contact with skin or mucus membranes – Inhalation in bat filled caves – Transplantation of organs Occurrence: – >55, 000 deaths/yr, almost all in developing countries –Asia, Africa – No post-exposure vaccine available in many countries

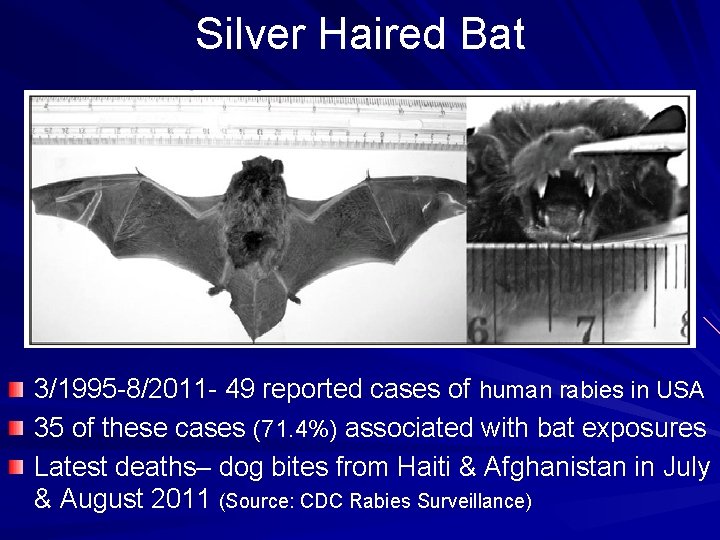
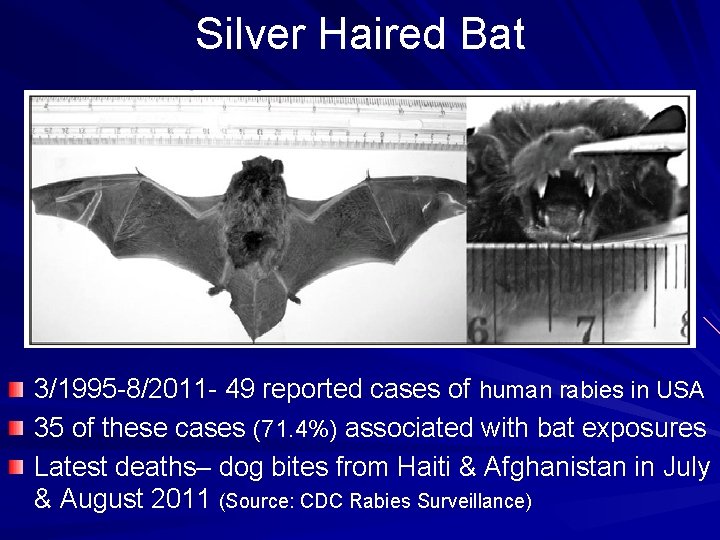
Silver Haired Bat 3/1995 -8/2011 - 49 reported cases of human rabies in USA 35 of these cases (71. 4%) associated with bat exposures Latest deaths– dog bites from Haiti & Afghanistan in July & August 2011 (Source: CDC Rabies Surveillance)
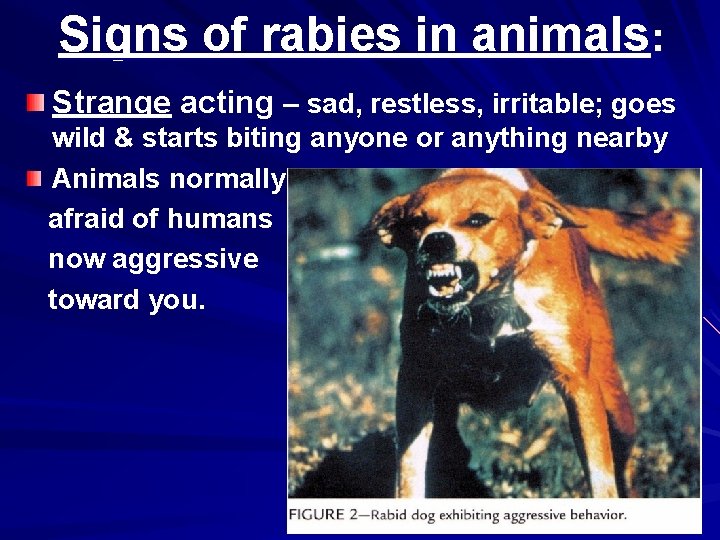
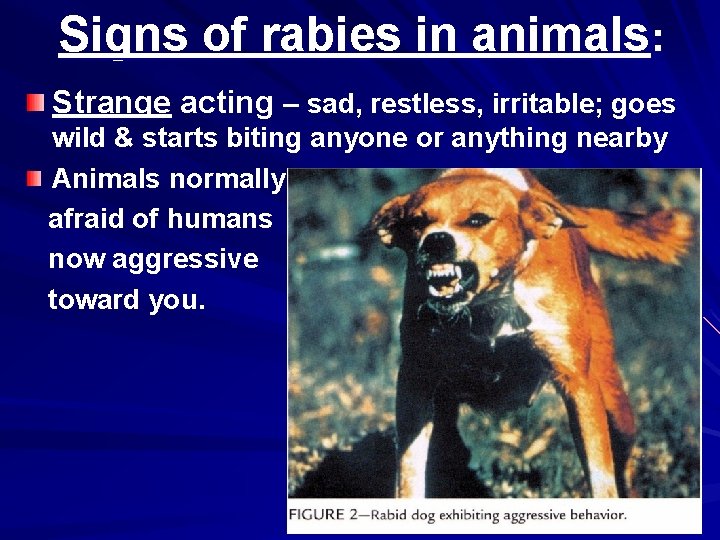
Signs of rabies in animals: Strange acting – sad, restless, irritable; goes wild & starts biting anyone or anything nearby Animals normally afraid of humans now aggressive toward you.
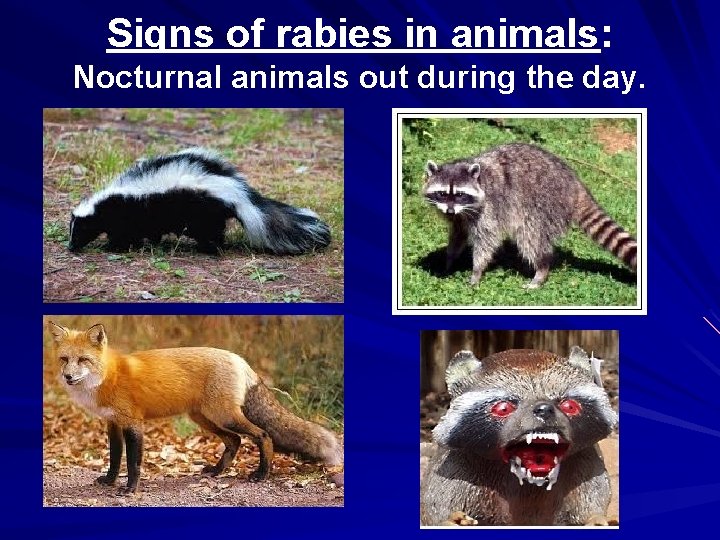
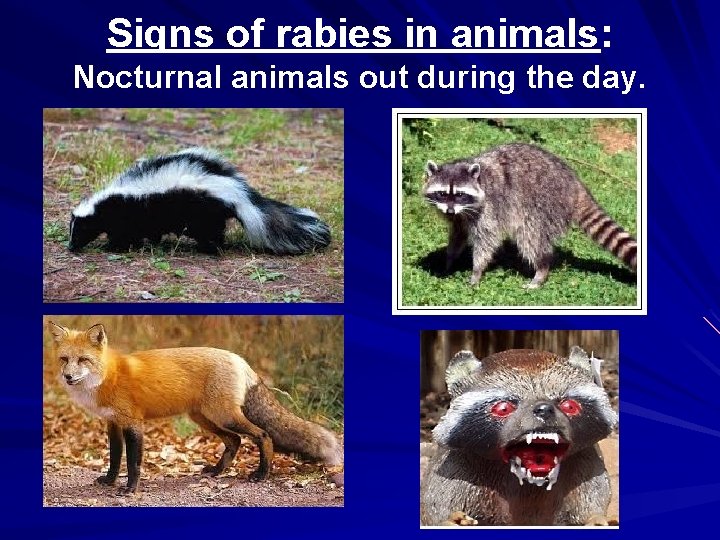
Signs of rabies in animals: Nocturnal animals out during the day.
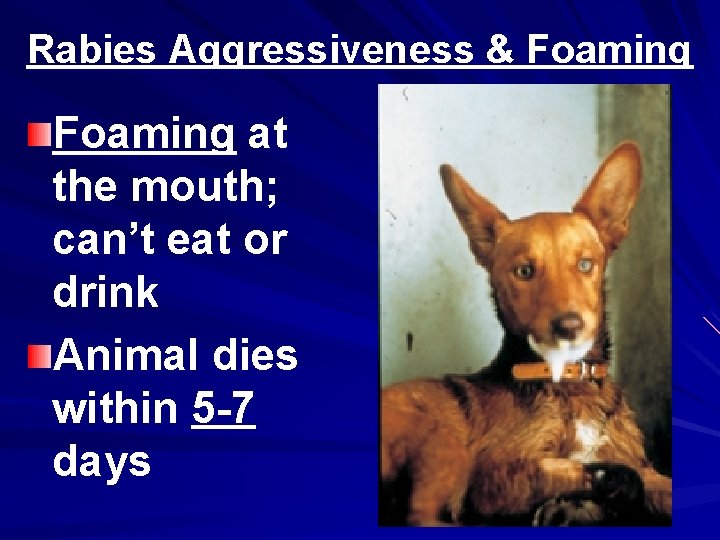
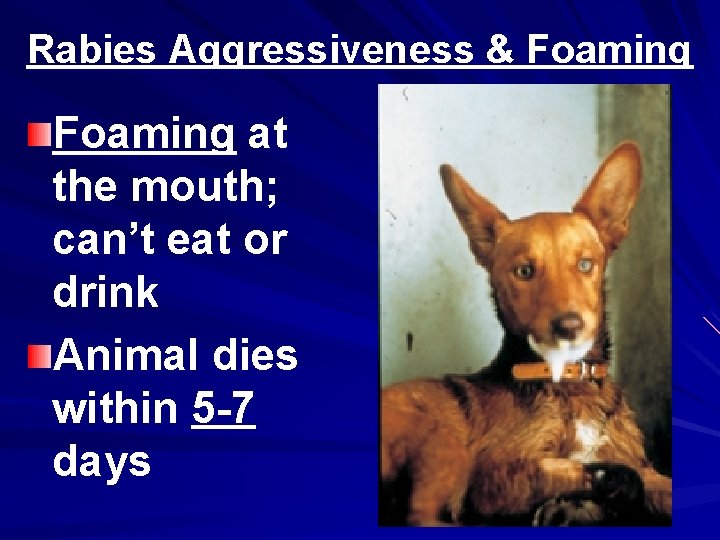
Rabies Aggressiveness & Foaming at the mouth; can’t eat or drink Animal dies within 5 -7 days
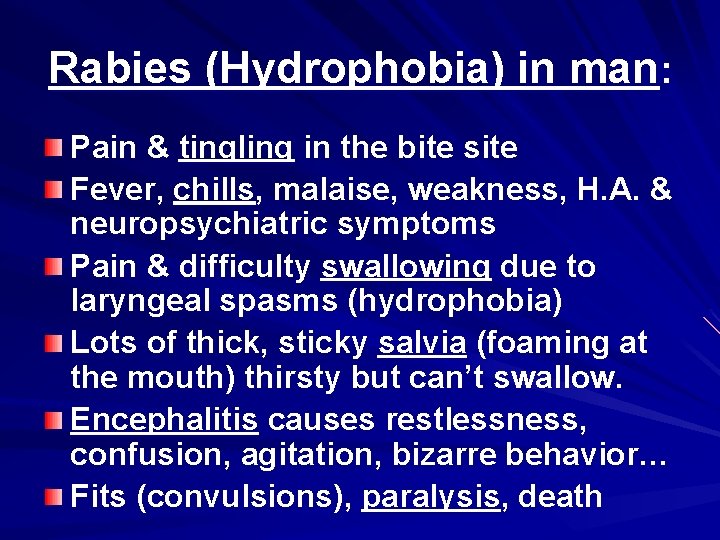
Rabies (Hydrophobia) in man: Pain & tingling in the bite site Fever, chills, malaise, weakness, H. A. & neuropsychiatric symptoms Pain & difficulty swallowing due to laryngeal spasms (hydrophobia) Lots of thick, sticky salvia (foaming at the mouth) thirsty but can’t swallow. Encephalitis causes restlessness, confusion, agitation, bizarre behavior… Fits (convulsions), paralysis, death
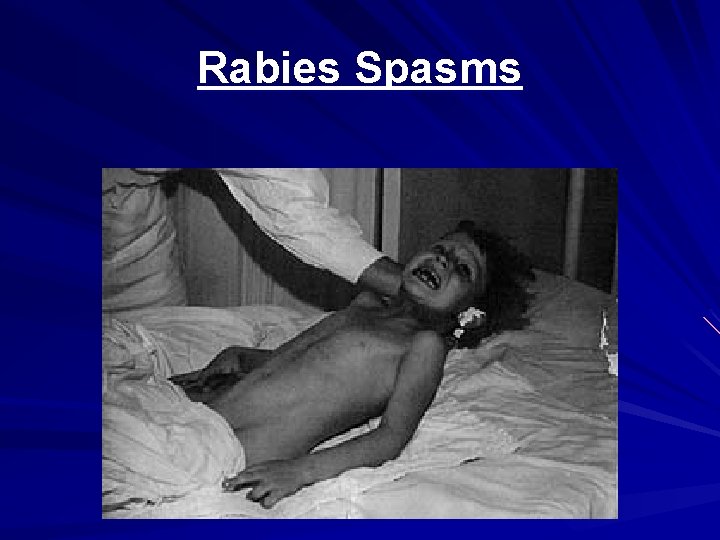
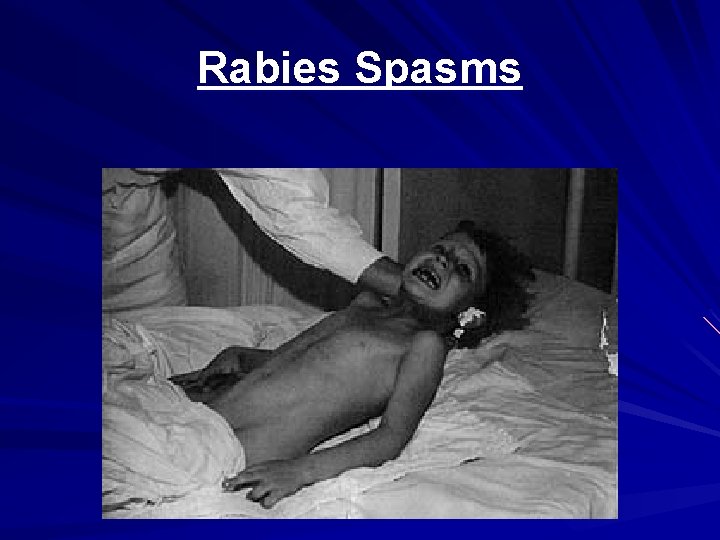
Rabies Spasms

Rabies Effects on Brain & Neurological System
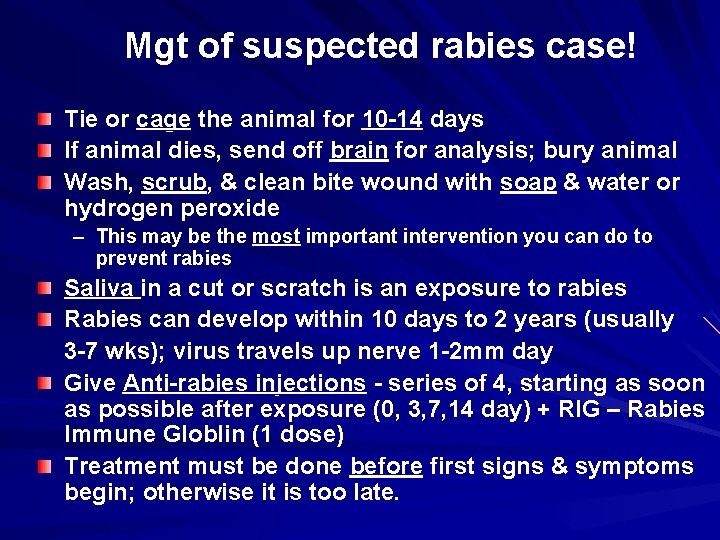
Mgt of suspected rabies case! Tie or cage the animal for 10 -14 days If animal dies, send off brain for analysis; bury animal Wash, scrub, & clean bite wound with soap & water or hydrogen peroxide – This may be the most important intervention you can do to prevent rabies Saliva in a cut or scratch is an exposure to rabies Rabies can develop within 10 days to 2 years (usually 3 -7 wks); virus travels up nerve 1 -2 mm day Give Anti-rabies injections - series of 4, starting as soon as possible after exposure (0, 3, 7, 14 day) + RIG – Rabies Immune Globlin (1 dose) Treatment must be done before first signs & symptoms begin; otherwise it is too late.
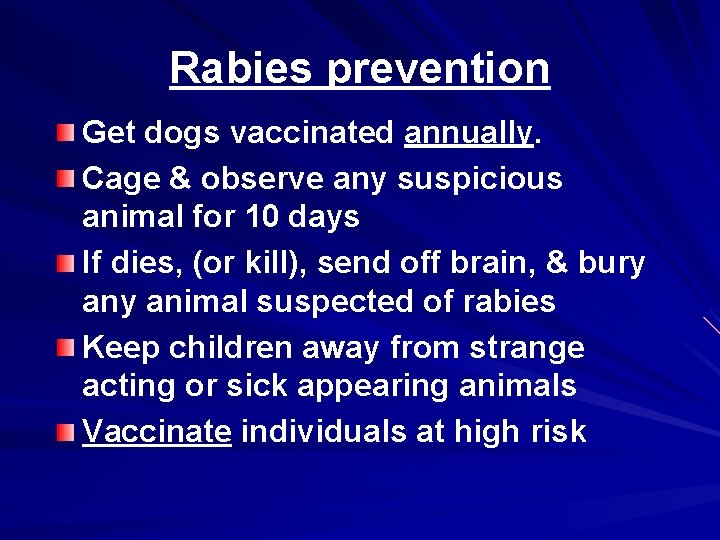
Rabies prevention Get dogs vaccinated annually. Cage & observe any suspicious animal for 10 days If dies, (or kill), send off brain, & bury animal suspected of rabies Keep children away from strange acting or sick appearing animals Vaccinate individuals at high risk