First Aid for pets Week 2 Introduction This


















































































- Slides: 186

First Aid for pets Week 2
Introduction This course will cover the following first aid scenarios: What is first aid The 3 P’s of first aid The primary assessment ( DR ABC) The Secondary assessment ( History taking and signs and symptoms) Handling and restraint Your first aid kit Common first aid scenarios and treatment: Wounds Burns and scalds Insect bites Fractures Dog attacks Fish hook injuries Heat Stroke (hyperthermia) Hypothermia Epilepsy CPR Cardiopulmonary Resuscitation

What is first aid?

What is first aid? First aid is the assistance given to any animal suffering a sudden illness or injury with care provided to: Preserve Prevent Promote life the condition from worsening, recovery

PRESERVE LIFE Your first aim is to preserve life by carrying out emergency first aid procedures. Preserving life should always be the overall aim of all first aiders
Prevent deterioration Prevent the casualty’s condition from deteriorating any further. In addition, this aim includes preventing further injury. You should attempt to - Make area as safe as possible - Remove any dangers. If removing danger is not possible you should remove the patient from the danger if possible. Always consider yours and others safety when preventing injury.
Promote recovery Arrange prompt emergency medical help. In addition, simple first aid can significantly affect the long-term recovery of an injury

Environmental hazards: poor ventilation temperature control trip, slip and fall hazards grooming environment eg low ceilings, uneven floor, lighting, steps, layout

Limitations of first aid according to Veterinary Surgeons Act (1966) Cannot diagnose Cannot prescribe Cannot administer medication Cannot perform clinical procedures Have no more rights or responsibility than any other member of the public

First aid box List what you think you need in a first aid kit

Essential Scissors Rope or soft length of cloth for use as a muzzle Conforming bandages and cotton wool Non-stick bandages Cohesive bandages Adhesive tape Microporous tape Medium and large dressings Gauze and bandage material for wrapping wounds Sterile gauze swabs Sterile saline solution for flushing wounds and eyes Towels or cloth to stem bleeding A list of emergency phone numbers Medical gloves Round ended scissors Tweezers Alcohol free cleansing wipes Plastic pouches/ plastic bags Foil blanket Tick remover Non-prescription topical treatments

Handling and restraint

Handling and restraint In groups , discuss different ways to retrain the following animals: Small Dogs Large Dogs Cats Birds hedgehogs
How to assess the patient
Warning As animals may be in pain, they may bite or scratch you. Dogs: If it is safe to do so, try and restrain by placing on lead Cats: If it is safe to do so, try and put cat in a basket or a cardboard box
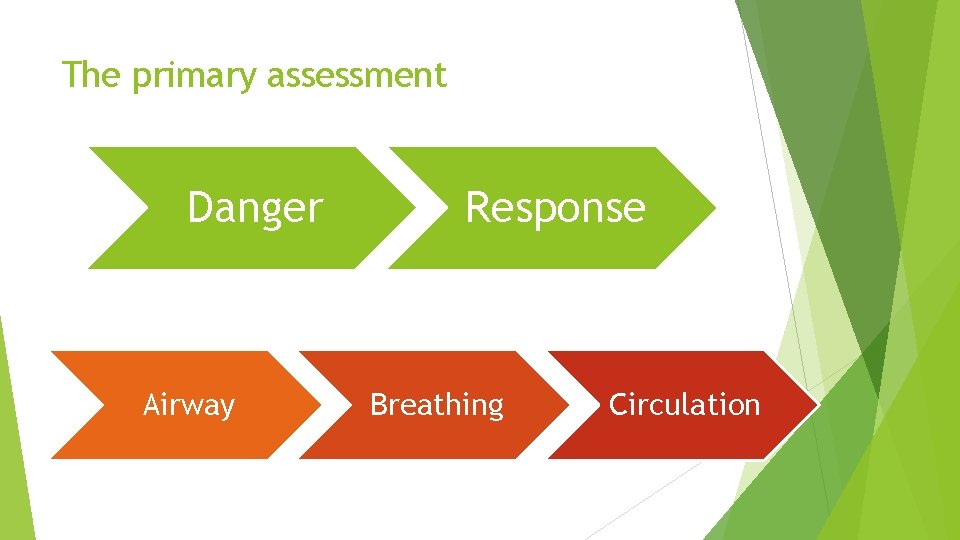
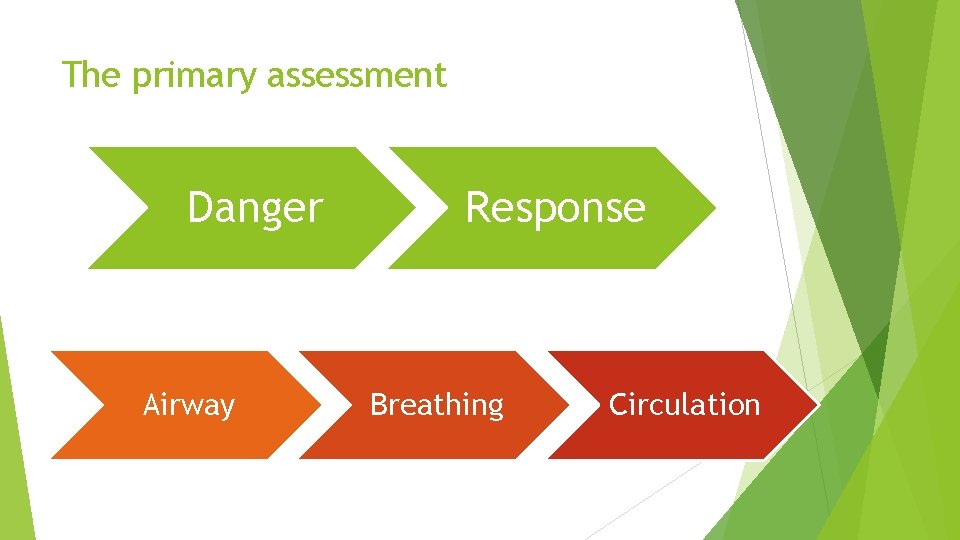
The primary assessment Danger Airway Response Breathing Circulation
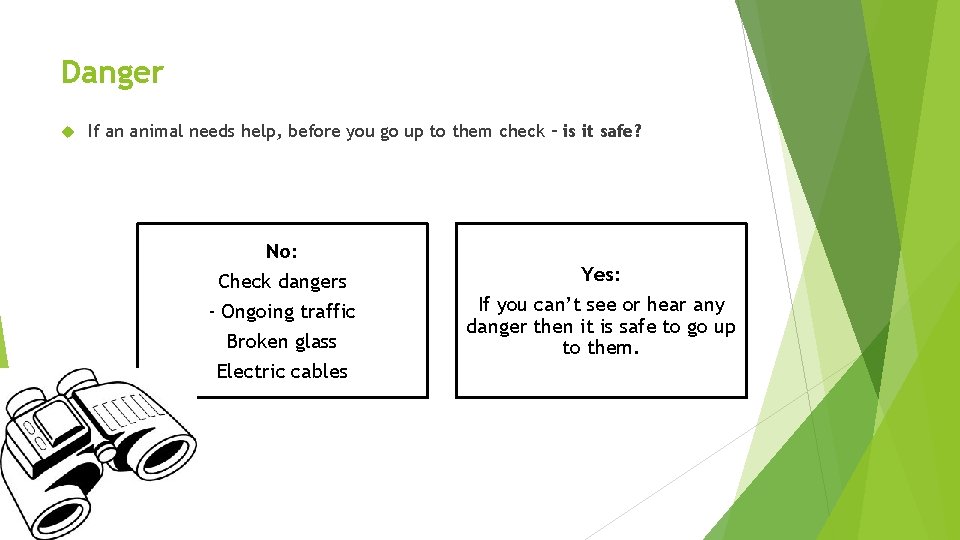
Danger If an animal needs help, before you go up to them check – is it safe? No: Check dangers - Ongoing traffic Broken glass Electric cables Yes: If you can’t see or hear any danger then it is safe to go up to them.

Response Do they respond when you talk to them? Approach slowly, speaking in a reassuring tone of voice No: Yes: If they don’t respond, then gently shake them and call their name. If they respond by making eye contact , wanting to move, or vacalising you can move onto– Airway. Please be aware however that any animal in pain may bite or scratch If they still don’t respond, then you can presume they maybe unconscious and move on to the next stage.

Airway Is their airway open and clear? Yes If their airway is open and clear, move on to the next stage – Breathing. No Unblock their airway, such as choking. Only move on to the next stage – Breathing – once their airway is open and clear.
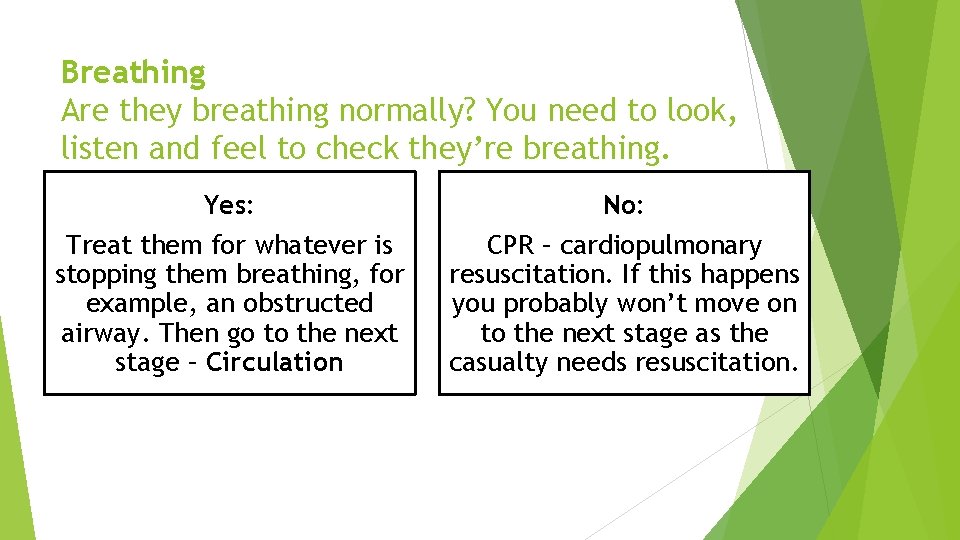
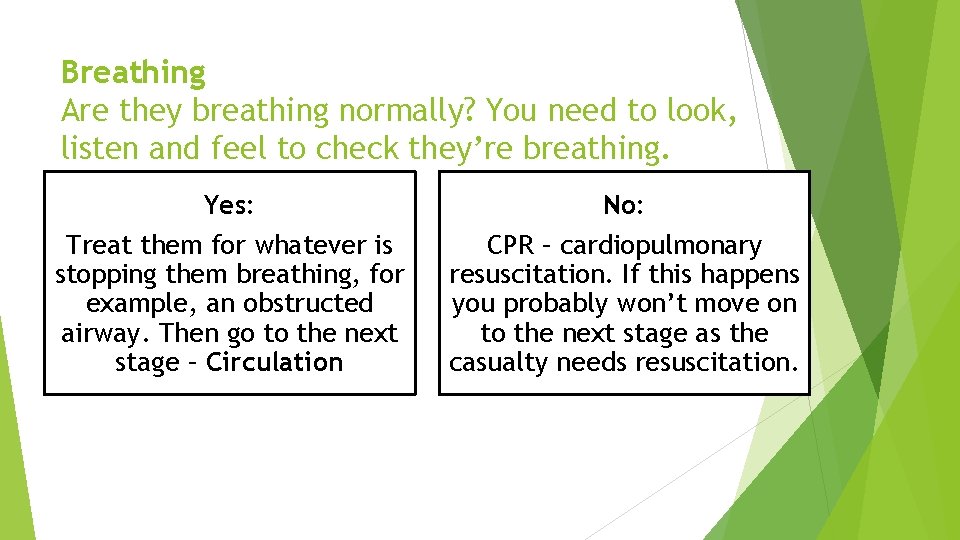
Breathing Are they breathing normally? You need to look, listen and feel to check they’re breathing. Yes: Treat them for whatever is stopping them breathing, for example, an obstructed airway. Then go to the next stage – Circulation No: CPR – cardiopulmonary resuscitation. If this happens you probably won’t move on to the next stage as the casualty needs resuscitation.
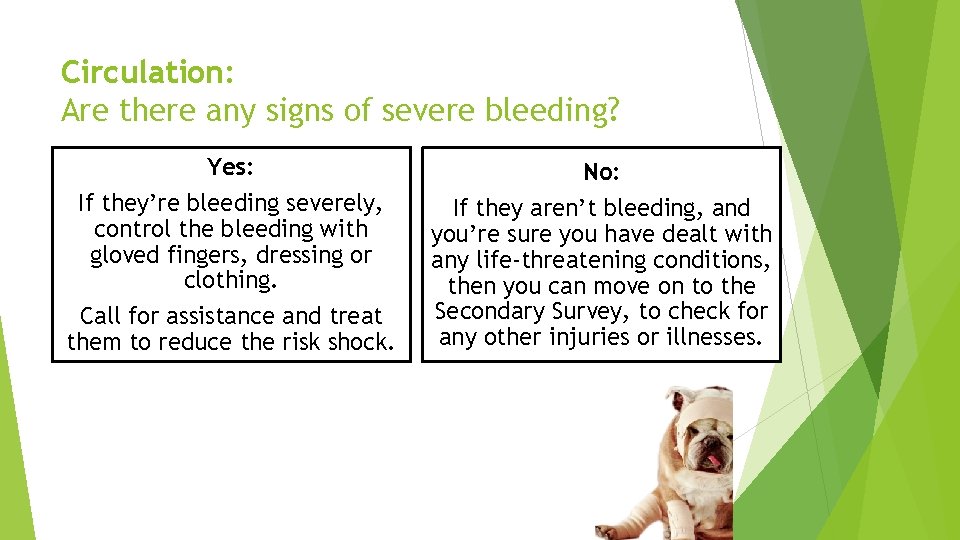
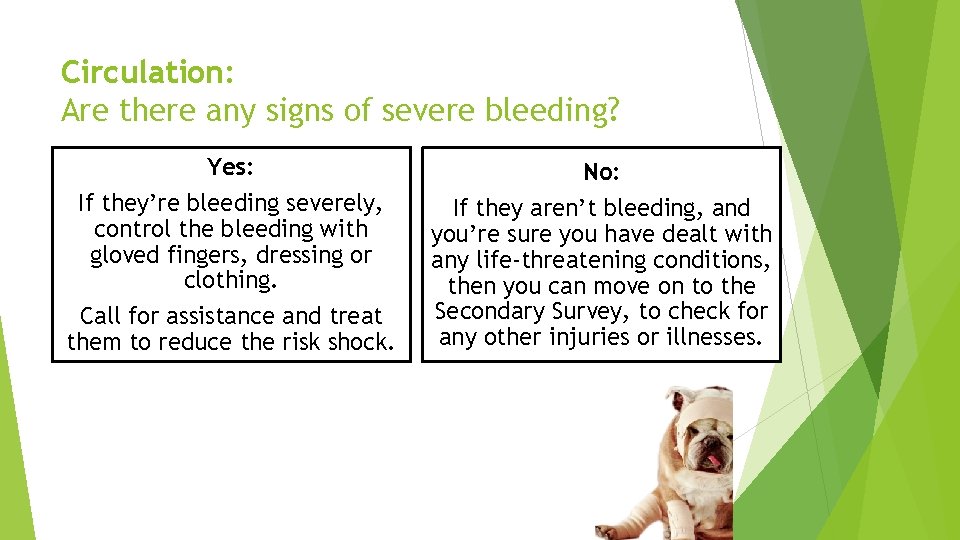
Circulation: Are there any signs of severe bleeding? Yes: No: If they’re bleeding severely, control the bleeding with gloved fingers, dressing or clothing. Call for assistance and treat them to reduce the risk shock. If they aren’t bleeding, and you’re sure you have dealt with any life-threatening conditions, then you can move on to the Secondary Survey, to check for any other injuries or illnesses.
Only move onto the Secondary Survey if you have already done the Primary Survey and succeeded in dealing with any life threatening conditions.

Body Check List Breathing Chest Bleeding Limbs Nose Spine Mouth Abdomen Head Hips Ear Eyes Skin and neck and pelvis

Pulse

What is a PULSE ? A pulse is the movement of blood that passes a valve within a artery The heart is a muscular pump that pushes blood through blood vessels around the body.
Reasons for a change in heart / pulse rate?
Variation in the pulse may be caused by following reasons: 1. Age 2. Size of animal 3. Exercise. 4. Health.
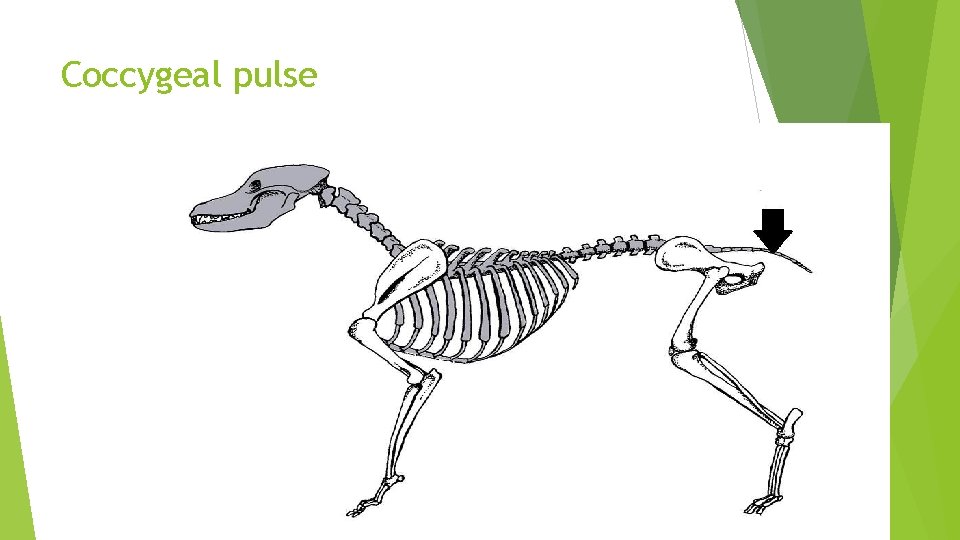
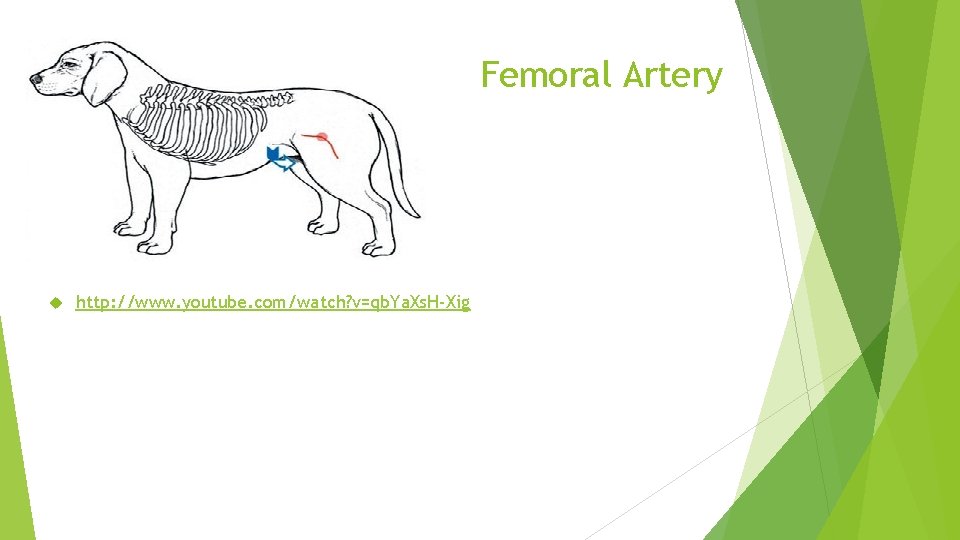
Pulse Rate per Minute: The beating of heart (pulsating) as displayed by expansion and contraction of the arteries is called pulse and the number per minute is called pulse rate. The pulse is felt on any convenient artery. The usual artery is coccygeal, found below the base in the centre of tail. Another common artery to feel is the femoral artery – this is found on the inner (medial) thigh (femur)
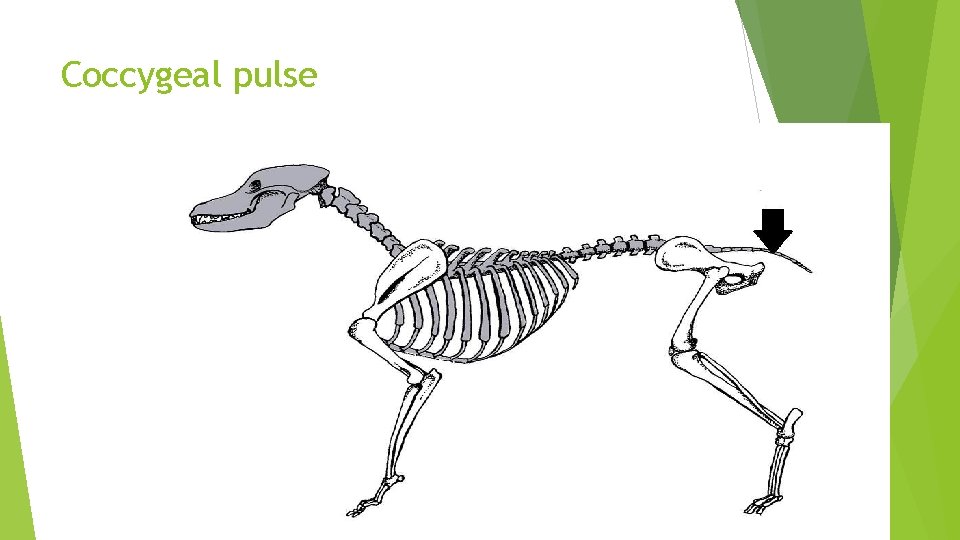
Coccygeal pulse
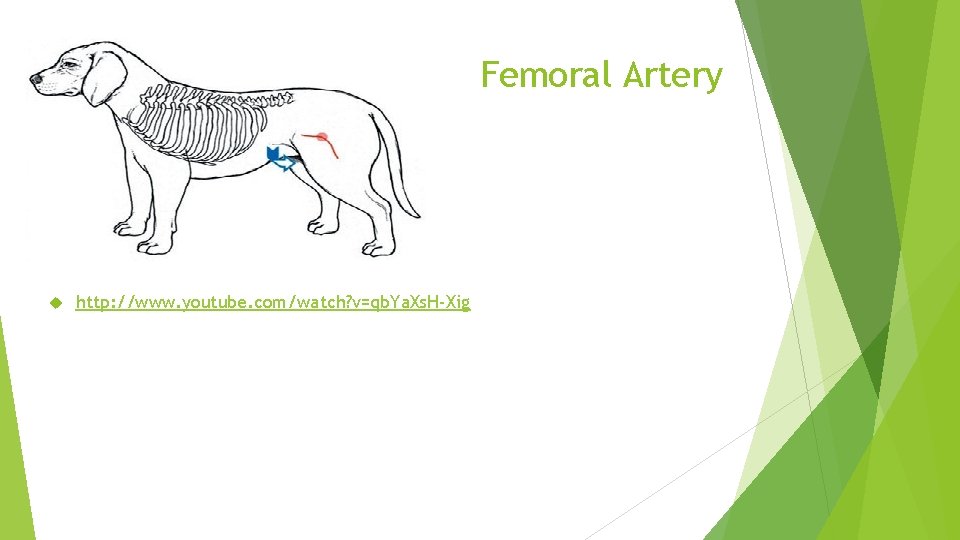
Femoral Artery http: //www. youtube. com/watch? v=qb. Ya. Xs. H-Xig
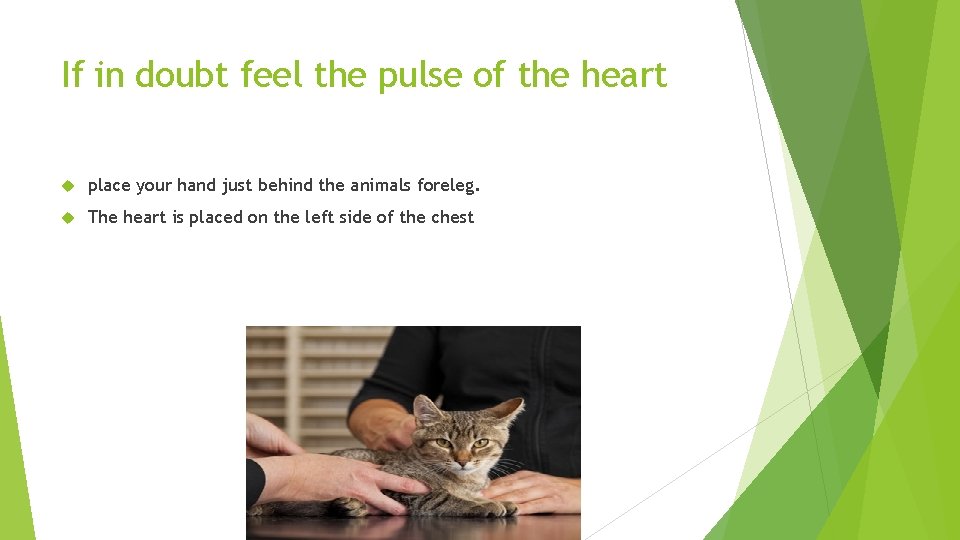
If in doubt feel the pulse of the heart place your hand just behind the animals foreleg. The heart is placed on the left side of the chest

terminology Bradycardia –decreased heart rate Tachycardia – increased heart rate

Respiration
Respiration rate per minute: Respiration is the act of breathing, by which drawn into and expelled from the lungs in animals. The normal respiratory frequency is the number of respirations per minute. It is determined by observing the movements of the air at the nostrils, chest or flanks.

How to count the respiration rate For the respiratory rate, count the number of breaths your pet takes in 15 seconds and then multiply that number by four. watch for each rise of the chest wall
The following factors influence the respiration rate: 1. Exercise. 2. Sleep. 3. Rumination. 4. Season. 5. Pregnancy. 6. Health condition. poisons
terminology Apnoea – without breathe Bardypnoea – slow respiration rate Cyanosis – lack of oxygen – blue mm Dyspnoea – difficulty in breathing Tachypnoea – fast breathing
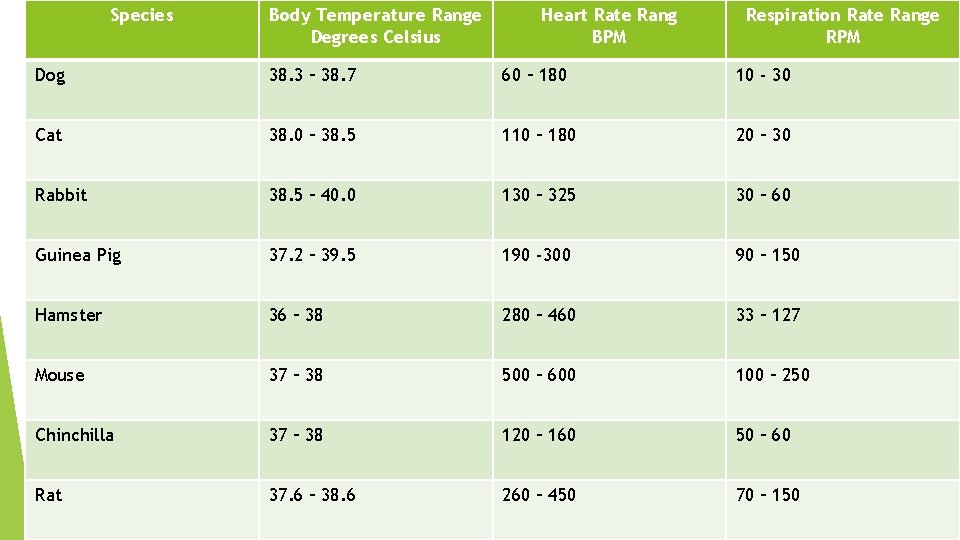
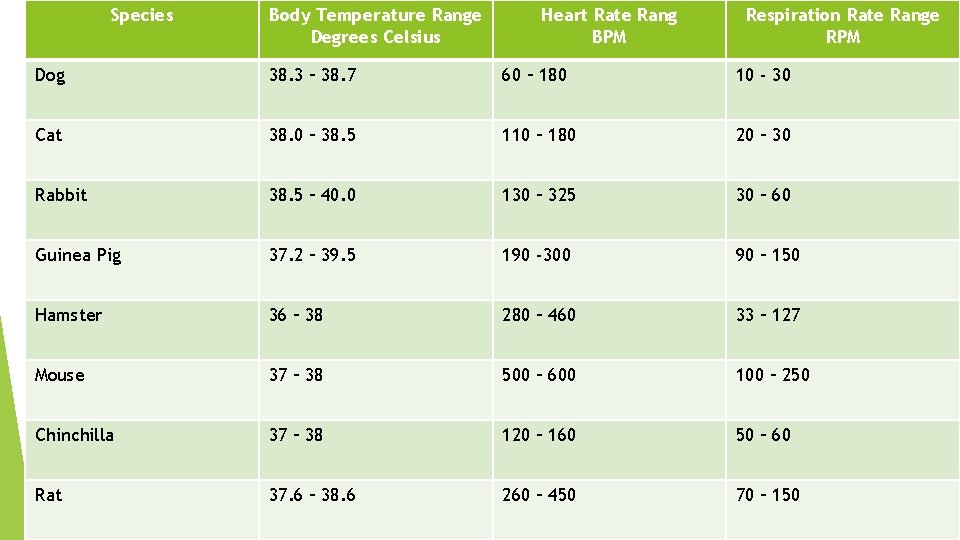
Species Body Temperature Range Degrees Celsius Heart Rate Rang BPM Respiration Rate Range RPM Dog 38. 3 – 38. 7 60 – 180 10 - 30 Cat 38. 0 – 38. 5 110 – 180 20 – 30 Rabbit 38. 5 – 40. 0 130 – 325 30 – 60 Guinea Pig 37. 2 – 39. 5 190 -300 90 – 150 Hamster 36 – 38 280 – 460 33 – 127 Mouse 37 – 38 500 – 600 100 – 250 Chinchilla 37 – 38 120 – 160 50 – 60 Rat 37. 6 – 38. 6 260 – 450 70 – 150
Taking temperature – mercury thermometer Take a firm grip and shake so that thermometer is below ) oc Lubricate end with KY petroleum jelly Insert into rectum , making sure animal has been restrained , using a twisting affect. Make sure that end is touching a membrane and not in faecal matter. After 1 minute, remove from rectum and clean thermometer Read thermometer

Changes in temperature - causes Environmental Infection Pain Exercise
Specific terminology Hyperthermia – high temperature Hypothermia – low temperature Normothermia – normal temperature Pyrexia - fever

Wounds
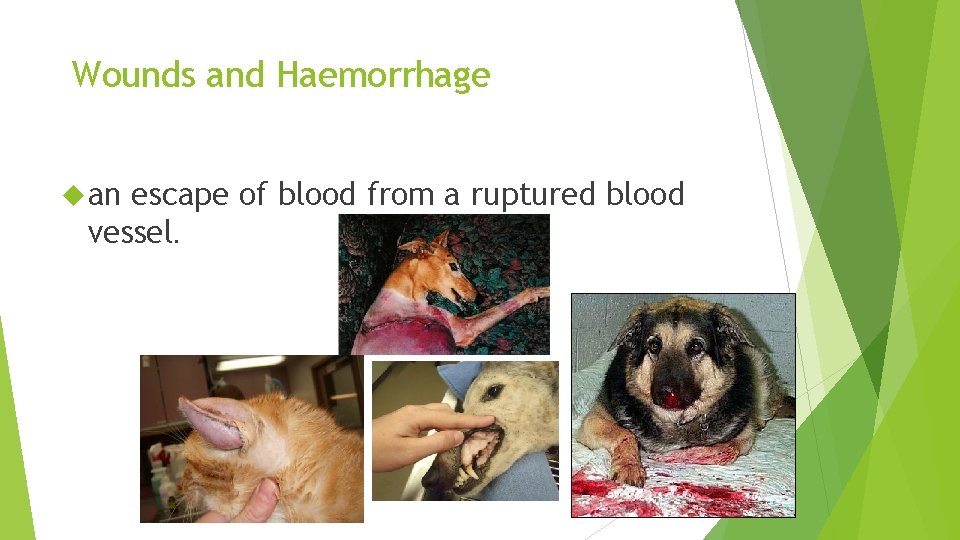
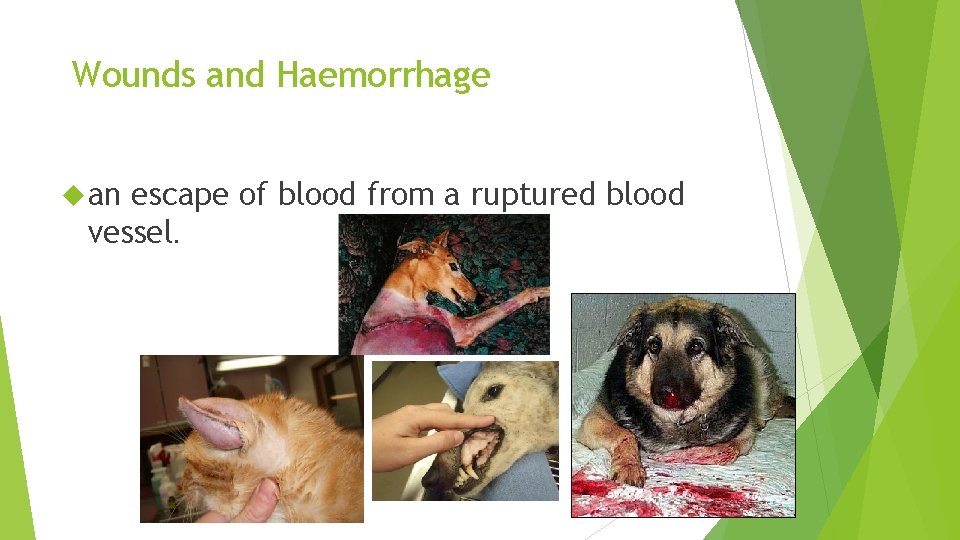
Wounds and Haemorrhage an escape of blood from a ruptured blood vessel.
Haemorrhage Four types of haemorrhage – Arterial – Most serious, forceful and spurting. Bleeding point can usually be detected Venous – Darker in colour, steady stream, bleeding point usually detected Capillary Mixed – Oozes with little force – Usually profuse bleeding from all types of vessel, difficult to locate
Haemorrhage Symptoms Weak Dull and depressed Pale mucous membranes Cold/ low temperature Weak/ thready pulse Visible bleeding / open wounds

OPEN Incised CLOSED Abrasion Haematoma Contusion
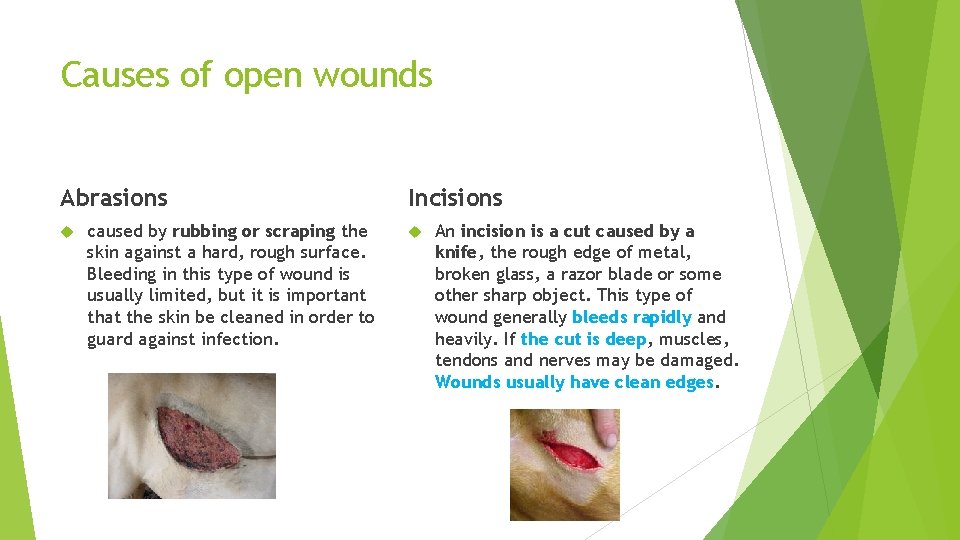
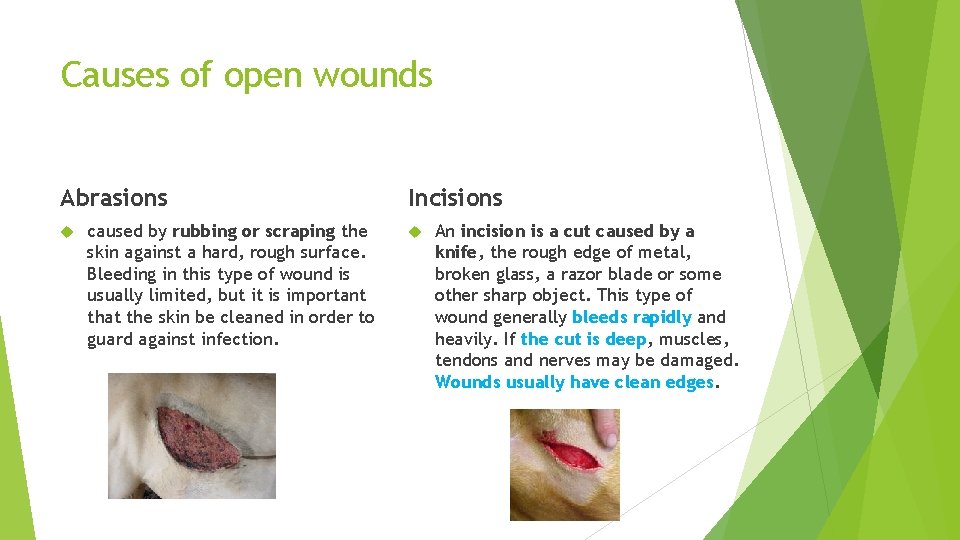
Causes of open wounds Abrasions caused by rubbing or scraping the skin against a hard, rough surface. Bleeding in this type of wound is usually limited, but it is important that the skin be cleaned in order to guard against infection. Incisions An incision is a cut caused by a knife, the rough edge of metal, broken glass, a razor blade or some other sharp object. This type of wound generally bleeds rapidly and heavily. If the cut is deep, muscles, tendons and nerves may be damaged. Wounds usually have clean edges.
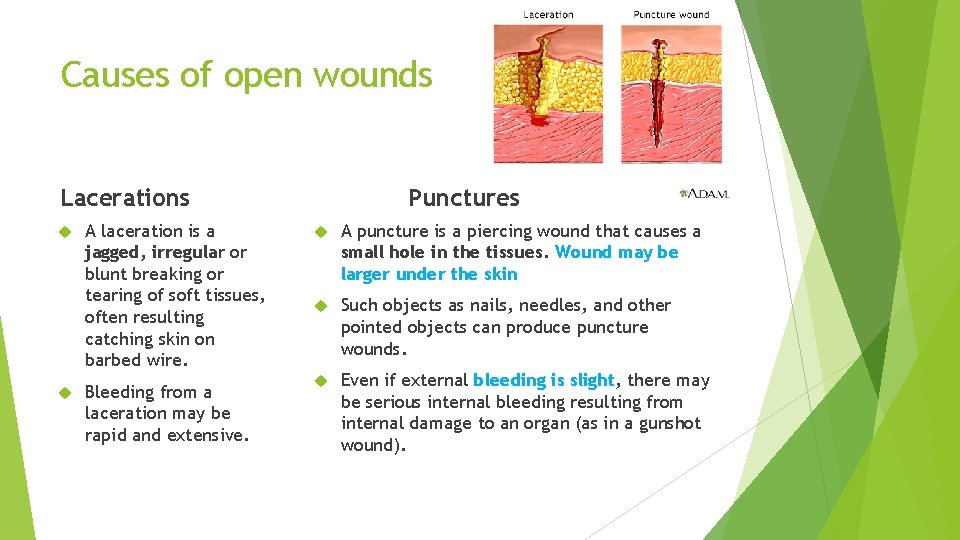
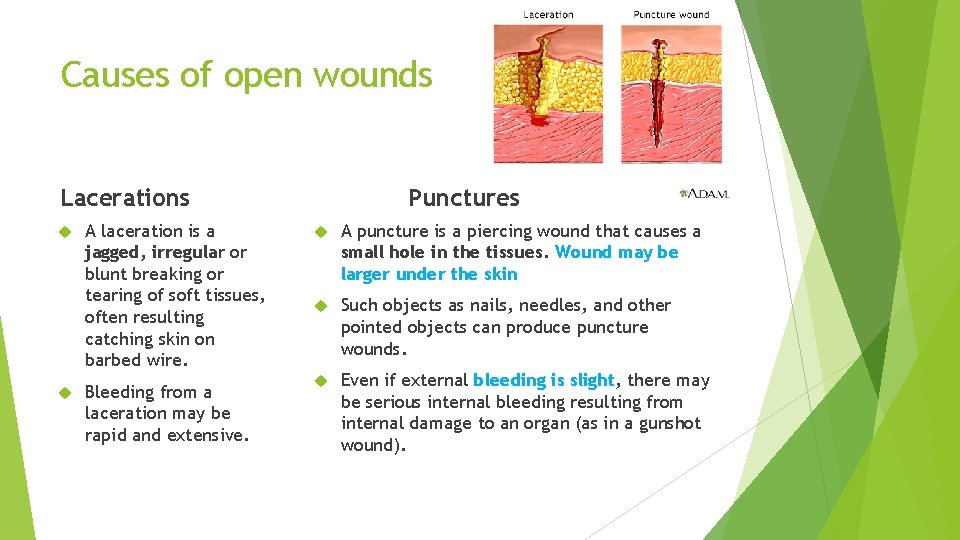
Causes of open wounds Lacerations A laceration is a jagged, irregular or blunt breaking or tearing of soft tissues, often resulting catching skin on barbed wire. Bleeding from a laceration may be rapid and extensive. Punctures A puncture is a piercing wound that causes a small hole in the tissues. Wound may be larger under the skin Such objects as nails, needles, and other pointed objects can produce puncture wounds. Even if external bleeding is slight, there may be serious internal bleeding resulting from internal damage to an organ (as in a gunshot wound).

Puncture Wound
First Aid Treatment for Wounds Open Wounds 1. Make sure the animal is restrained 2. Firstly stop the bleeding by applying pressure –Remove any obvious SMALL foreign bodies that may cause damage. Any protruding FB’s should not be removed however can be shortened 3. Clip hair around wound – avoid contamination of wound site -sterile water soluble gel can be used 4. Clean the wound working from the wound outwards / remove any foreign bodies 5. Apply a light dressing. If wound is large call a vet for assistance (conforming / dressings / sterile swabs / surgical tape). 6. Wound may later need suturing under sedation / anaesthesia. Antibiotics may be needed. Treatment for shock should then be considered.
Closed Wounds Apply cold compress to reduce blood flow to the damaged capillaries 2. A dressing will provide support if needed – abdominal organs Aural haematomas can heal however a surgical procedure will reduce swelling Depending on where the bleed is, this could be classed as an emergency 1.

Deep Wounds Some wounds may be deeper than others. Depending on the site of the wound depends on its severity. Chest wounds – may cause breathing issues. Oxygen therapy may be needed Dressing applied to chest prevent leakage of air Abdominal Wounds – May cause organ damage Abdominal dressing applied to prevent further blood loss and contamination Muscular – may cause nerve paralysis / blood loss Dressing to be applied to prevent contamination
Internal Bleeding Internal bleeding may be caused by trauma or by internal abnormalities: Road Dog traffic accident bites Tumour Poisonings Clotting errors
Presenting characteristics of arterial haemorrhage Bright red blood Gushing. Squirting from wound Oxygenated blood

Presenting characteristics of venous haemorrhage Darker blood Slower seeping from wound

Haemorrhage – Bleeding Wounds Any blood loss can result in a serious outcome and should be treated as an emergency Method Risks Advantages Disadvantages Direct digital pressure What is under the wound? FB Quick, effective , no It is temporary treatment as or fracture other equipment haemorrhage will start once required pressure is released Pressure bandage Dressing cold put pressure on object below wound Easy to apply Some areas of the body are difficult Can be left in place to apply a dressing Indirect pressure Locating a pressure point may be difficult Equipment always available e. g. fingers Response is immediate Temporary treatment tourniquet Cuts of circulation to the limb and tissues start to die – should not be left on for more than 15 mins Quick and easy Damage to tissues

Burns & Scalds
Burns and Scalds A burn is an injury caused by: Dry heat such as fire or contact with hot surface Electricity Excessive cold, including cryosurgery Corrosive chemicals A scald is an injury caused by Boiling Hot tar Hot oil water
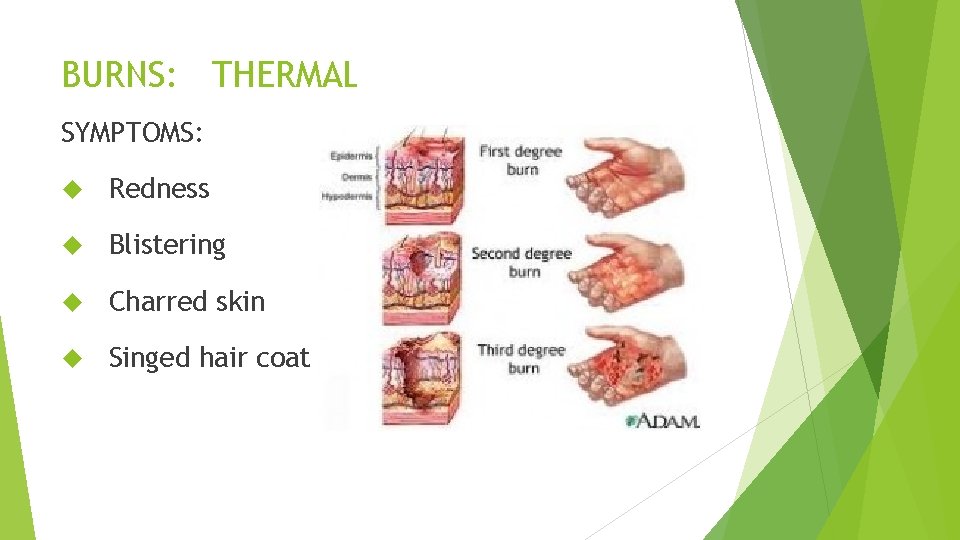
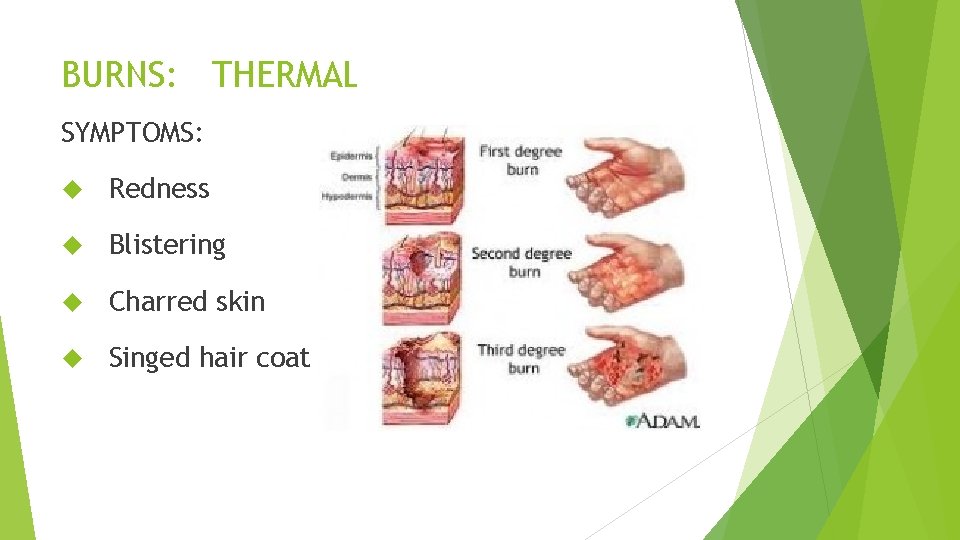
BURNS: THERMAL SYMPTOMS: Redness Blistering Charred skin Singed hair coat

BURNS: THERMAL FIRST AID TREATMENT: If skin is broken and blistered DO *NOT* apply ice, water, or ointment! DO apply sterile non-adherent bandage (second skin) and seek veterinary advice If skin is not broken and blistered, Apply ice packs or cold water compresses and seek veterinary advice
Treatment to burns and scalds 1. Warm the patient – it is important to maintain the animals body temperature so it does not become hypothermic 2. Veterinary treatment may be required : 1. Replace lost fluid by using an intravenous infusion 2. Provide analgesia 3. Treat for shock

ELECTRICAL BURNS **** YOUR SAFETY MUST COME FIRST **** Usually results from chewing electrical cords or being struck by lightening Affects local tissues as well as the heart
Electrical Burns These should be treated in the same way as other burns and scalds. It is vital that you do not touch the animal until the electricity has been disconnected. Use a wooden implement such as a broom handle o move the patient away from the source
ELECTRICAL BURNS SYMPTOMS: May be local tissue (if chewing a cord) of the mouth or may involve deep underlying tissues Full extent of tissue injury may not be evident for several weeks when all of the burned tissue sloughs off May have initial swelling around area May have affected heart rate and rhythm May be unconscious, not breathing, and/or without a heartbeat
Electrical Burns Turn off power supply Use a wooden object to move animal away from source Check vital signs (CPR may be needed) Take to vet as soon as possible
BURNS: CHEMICAL FIRST AID TREATMENT: 1. Flush areas with copious amounts of water (5 minutes!) even if the skin is broken Water dilutes the chemical and helps to flush it away from the skin Pad the area with wet gauze and transport ASAP 2. Try to ID the chemical 3. Do *NOT* apply topical meds 4. Do *NOT* let animal lick the area 1. It can lead to burns of the mouth and throat 5. If burn occurs near or in the eyes, flush with sterile saline (contact lens solution)

Chemical Burn – Petrol
Complications of burns and scalds Shock caused by : Fluid loss Pain Infection after injury Dyspnea – (difficulty in breathing)smoke inhalation Infection – occurs because the moist conditions attract bacteria. This delays healing Poisoning – patient may lick chemical
Paraphimosis The inability to completely retract the penis into the preputial cavity usually occurs after erection
Causes More common causes of this condition can include: chronic licking, sexual or excitement, foreign bodies getting up under the skin. However, there are more serious causes including neurological disease (such as a herniation of a disc in the spinal cord), penis fractures, or muscular issues. Paraphimosis also needs to be differentiated from priapism, which is a state of continuous erection, usually due to a neurological problem.
A diagnosis of paraphimosis is generally based on simple observation of the penis extruded from the prepuce without any physiological reason. Paraphimosis accounts for approximately 7% of penile problems in the dog. Treatment : First, thoroughly clean the exposed penis and inspect it for any foreign material such as foxtails or long fur that is “strangulating” the tissues of the penis. Mix up a “sugar paste” using ordinary white sugar and enough water to make it into a thick slurry. Apply this mixture liberally to the extruded penis. The sugar works as a hyperosmotic agent, “pulling out” fluid from the tissues to help to reduce the swelling and shrink the penis. Wrap up a bag of frozen peas in a light towel and place over the area for 5 minutes at a time, which also helps to reduce swelling of the tissues. Packaged peas work well because they are very moldable around the dog’s anatomy. Lubricants, such as K-Y jelly, should then be applied. Lubrication helps aid in returning the penis back into the sheath. If the swelling does not resolve within 30 minutes, and if the penis does not stay retracted into the prepuce despite the interventions above, then immediate veterinary assistance is needed.

Insect Bites
INSECT BITES Includes bees and hornet type flying bugs, ants, spiders Can cause an allergic reaction, locally or systematically
INSECT BITES FIRST AID TREATMENT: 1. 2. 3. 4. 5. Locate stinger and remove with tweezers Apply ice pack or cold compress Monitor for infection If in doubt, check it out! Monitor breathing and possibility of swelling around the face and neck or possibly hives 6. Benadryl may be given to reduce swelling(speak to your veterinary surgeon before administering medication) 7. Transport ASAP if systemic reaction is occurring
INSECT BITES 8. Watch for symptoms of toxicity over the next few days including: Excess salivation Irritated skin areas Painful areas Fever Rapid or difficult breathing Paleness to gums Vomiting or diarrhea Blood in urine Stiffness or paralysis Allergic reaction
Hives is a severe allergic reaction that usually appears on your dogs skin within thirty minutes and if left to heal on its own can disappear in about twenty four hours. The problem for many pet owners is that hives on dogs are extremely irritating for your pet, and he will stop at nothing to try and bite and scratch those small red bumps until the itching subsides

Causes of Hives Insect stings or bites Vaccines, like rabies or Bordetella (also known as Kennel Cough). Food allergies. A chemical reaction, primarily to insecticides used to treat grass. Plants, including poison ivy or oak.

Hives – Treatment Hives are generally treated with the appropriate dose of antihistamines, such as Benadryl or a steroid- get advice from your vet before administering medication
Ticks
TICKS Ticks embed only their mouth parts into the skin. It is not possible for a tick’s head to get left behind in the animal’s skin but it is possible for the area to become infected or irritated and swollen. Mouth parts may be left in bite area. They are “glued” into the skin when the tick attaches

TICKS LYME DISEASE Is a bacterial infection transmitted to the animal via the deer tick, which is very small, similar in size to the head of a pin SYMPTOMS May Include: Fever, shifting lameness, lethargy, poor appetite, kidney disease

TICKS FIRST AID TREATMENT: **** Best treatment is prevention **** Use flea/tick topical drops or sprays and check the animal over after every trip into the fields or woodlands***** Vaccination is helpful in high risk areas 1. Use a tick hook 2. If available, apply flea and tick spray first 3. Do *NOT* burn or apply any other chemicals to the tick while it is in the animal’s skin 4. Avoid touching the tick with your bare hands and flush it down the toilet 5. Apply antibiotic ointment to the area if you would like

Animal Fights
ANIMAL FIGHTS / BITES AVOID THEM! Keep a close eye on your animal using your collar and lead. Watch for the approach of other animals whose owners are not as watchful. Watch the behaviour of the two animals!
First Step – Take control Separation of the dogs is important – however you should not get bitten in the process Shocking the animals by throwing water over them may help or making loud noises When separated, take control of the dogs so further attacks are prevented BE AWARE – they may be in severe pain and full of adrenaline so may lash out and bite. Muzzles can be used if no breathing conditions
ANIMAL FIGHTS / BITES FIRST AID TREATMENT: 1. Thoroughly go over the animal looking for punctures, tears, or matted fur 2. Clip the hair around the wounds 3. Scrapes and minor abrasions can be cleaned with sterile swabs and saline 4. Anything over 1/2 inch should be seen by Veterinarian 5. Bites on head, limbs, and genitalia or from a larger animal may have more serious “crushing” injuries, which will severely damage underlying tissues 6. Have it checked out! Many vets will prescribe antibiotics
Fractures the cracking or breaking of a hard object or material
FRACTURES Generally associated with trauma Must immediately restrict activity May also involve internal bleeding or other life threatening injuries.

Fracture symptoms?
Symptoms Pain- at the site – this may not occur until the animal moves the affected part of the body Swelling – due to bruising of the surrounding tissues Deformity of limb- the limb is often held at a abnormal angle. Crepitus – grating of bone Loss of Function- may be complete or partial Lameness Unnatural Mobility
FRACTURES FIRST AID TREATMENT: 1. Make sure area is safe 2. Prevent bleeding 3. Restrict movement 4. Restrict limb – use splints 5. Use of a buster colloar? 6. Place dog on a board, crate pan or crate bottom (Vari-Kennel) and transport ASAP
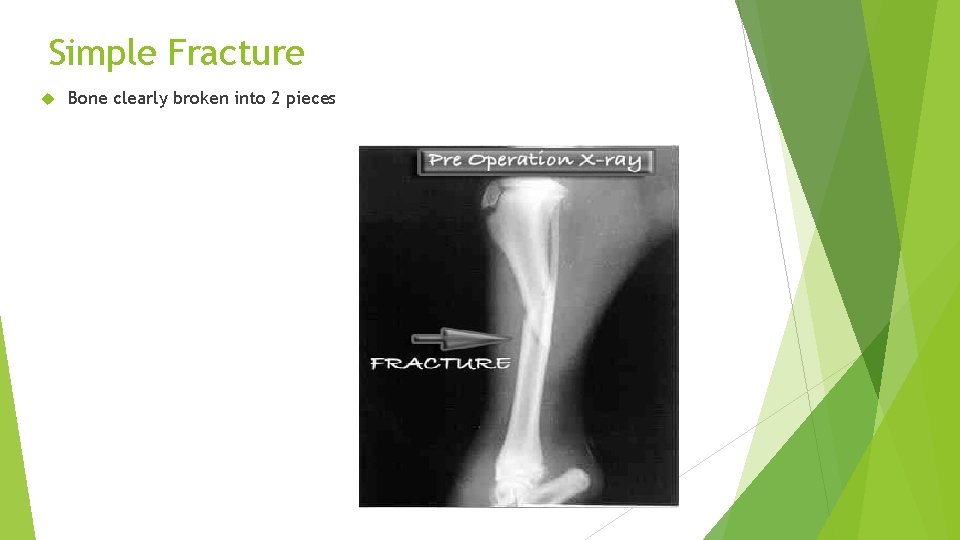
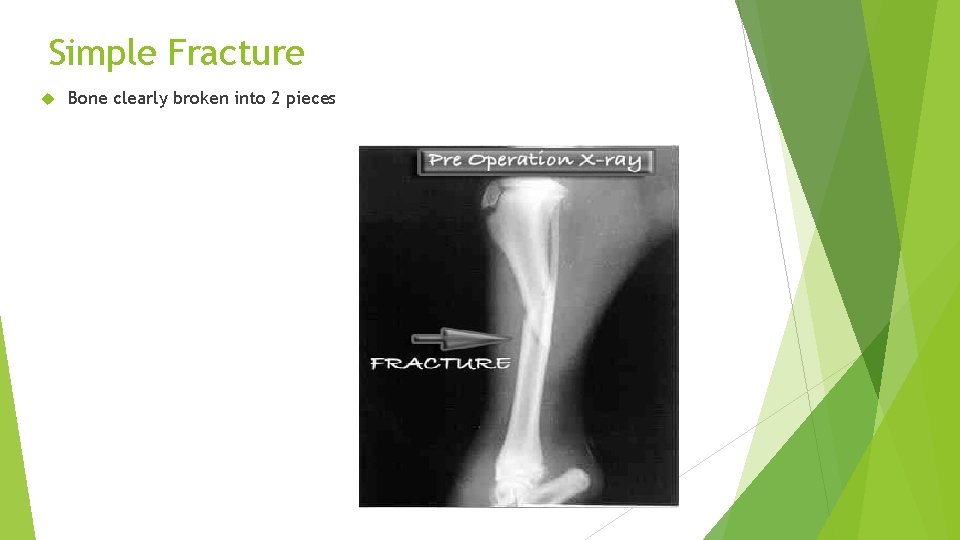
Simple Fracture Bone clearly broken into 2 pieces
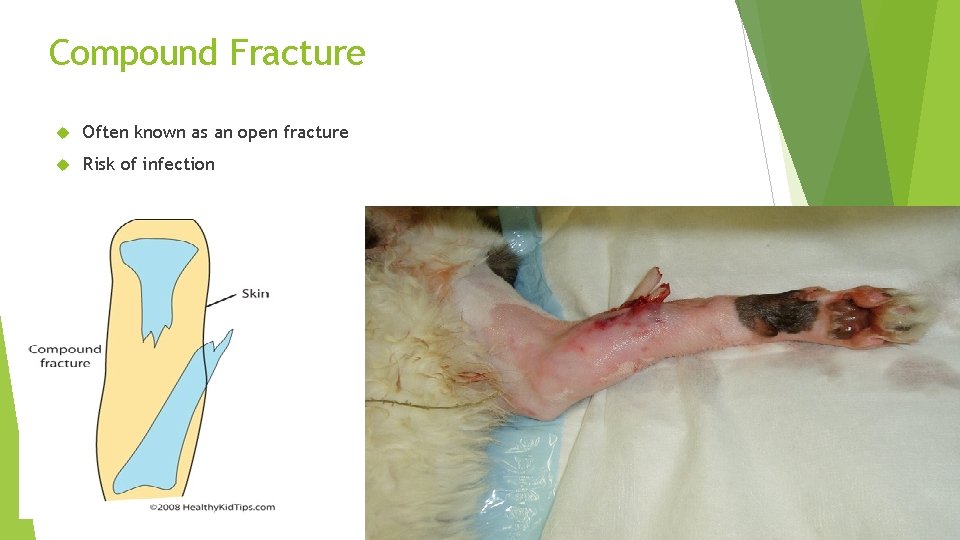
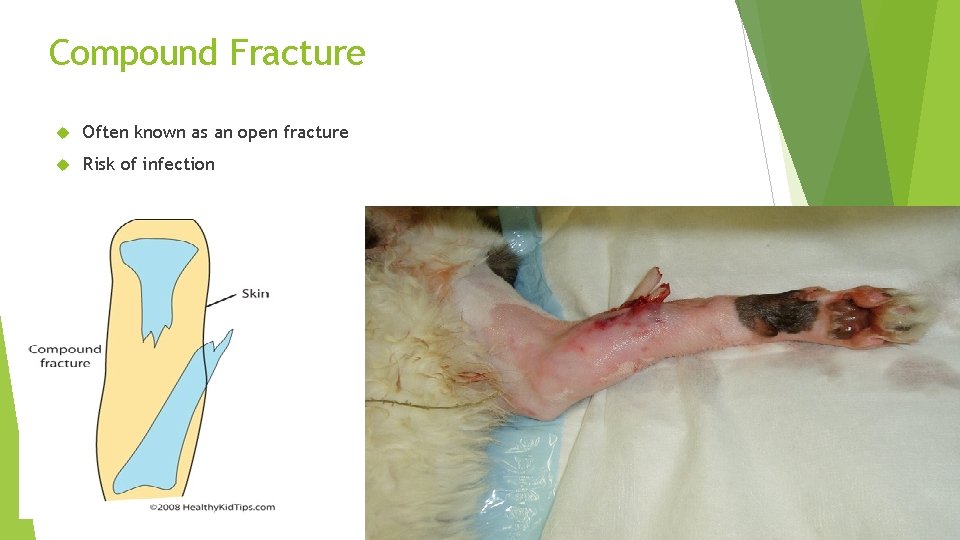
Compound Fracture Often known as an open fracture Risk of infection

Complicated Fracture Vital structures such as nerves and blood vessels involved in the fracture site
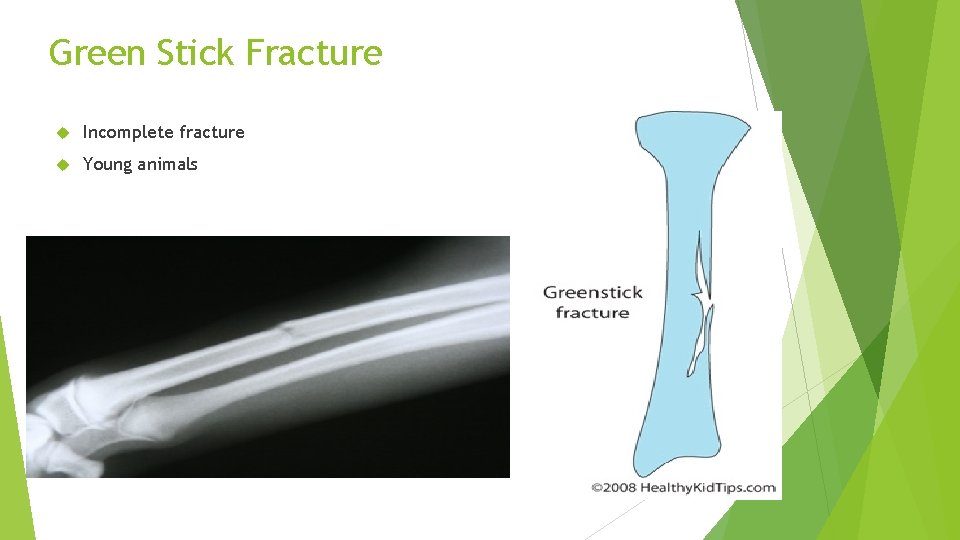
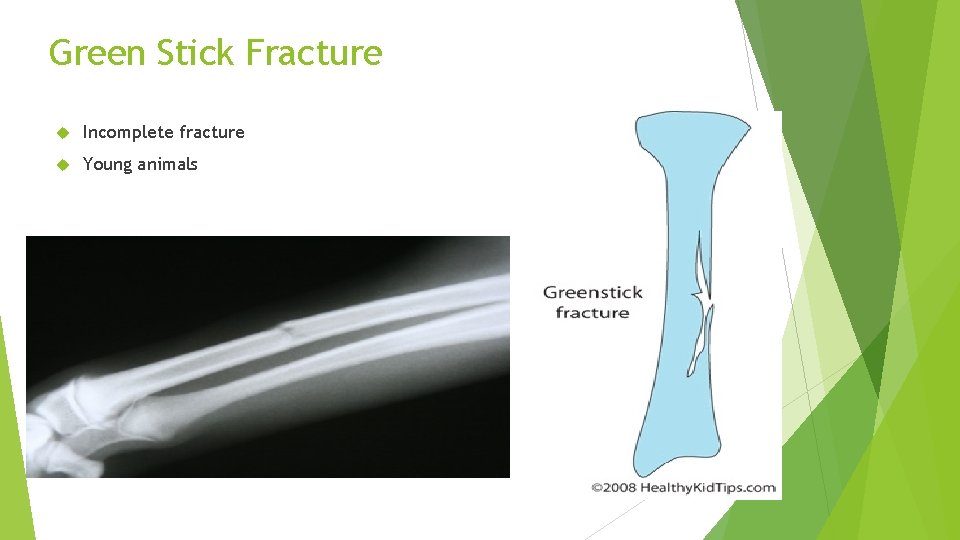
Green Stick Fracture Incomplete fracture Young animals

Comminuted Fracture Bone is shattered

Dislocation The displacement of the surface of bones within a joint Partial or complete

Dislocations – characteristics Pain Swelling Crepitus One limb longer than the other Lameness or limping

Dislocation – treatment Restrict movement Prevent further damage by supporting limb Check for shock keep calm / seek veterinary attention

Head Injuries
Head Injuries The Eye The Ear The nose The mouth The Skull and brain
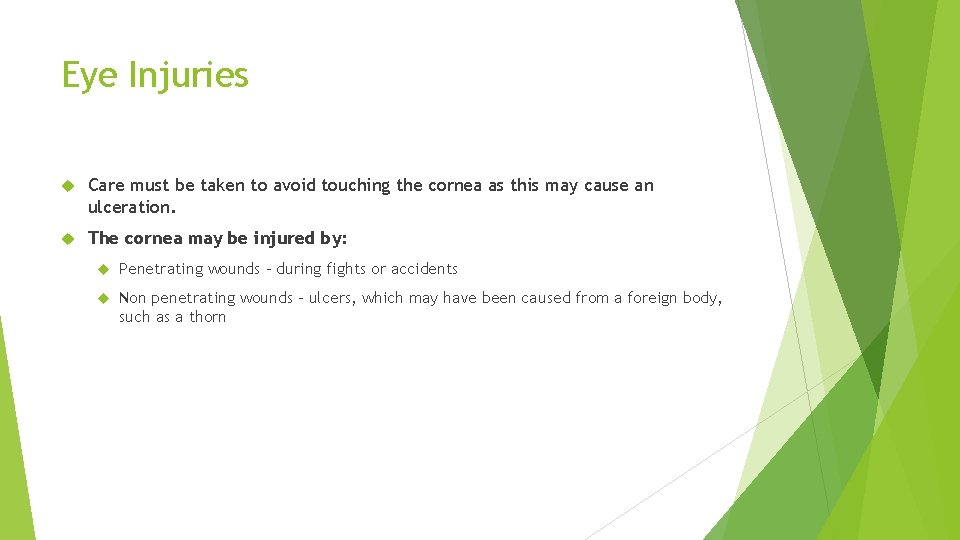
Eye Injuries Care must be taken to avoid touching the cornea as this may cause an ulceration. The cornea may be injured by: Penetrating wounds – during fights or accidents Non penetrating wounds – ulcers, which may have been caused from a foreign body, such as a thorn

Proptosis - Prolapsed of the eye: • The eye becomes dislodged from its socket and it exposed – may have been a cause from fighting • Common in breeds with protruding eyes – Pekinese. • In this state the eye is unprotected and may dry out causing corneal ulceration • Damage may also be caused to the optic nerve Treatment Although it is vital that the eye is replaced as soon as possible, this must not be attempted by anyone other than a veterinary surgeon Lubricate the eye using false tears or contact lens fluid. If neither is available – boiled and cooled water can be used Prevent self trauma to eye

Direct Eye Trauma Causing Haemorrhage in the eye
Fractures of the skull Can cause the eye to be bruised, which is often seen as a red blister on the sclera or the eye may protrude slightly from the socket as a result of haemorrhage in the soft tissues behind the eye.

General Treatment – eye ball injuries Flush with saline to clean area Place sterile gauze swab over the eye and attach loosely in position with adhesive tape Reduce the possibility of self trauma Place patient in a darkened room Keep warm Monitor TPR – signs for shock
Eye lid injuries – Foreign Bodies Foreign bodies – the most common are grass seeds, which become lodged either under the eye lids or beneath the third eye lid. They cause excruciating pain and the patient will keep eye shut making and examination difficult Foreign bodies can be removed however removal should be undertaken if the cornea is penetrated.

Eye Lid Injuries - Wounds Due to trauma such as fights and road traffic accidents Self trauma Wounds should be cleaned to remove any contamination by flushing with warmed saline.
The Ear – External Injuries The most common injuries to the ear are those to the ear pinna This is caused by scratches, bites, stings or self trauma resulting in aural haematoma. Clinical signs Haemorrhage Shaking of head swelling

The Ear – External injuries – Treatment 1. Stop the haemorrhage – apply pressure pad to the wound. Make sure dressing are not too tight around the head 2. Treat for insect sting 3. Icepack may reduce pain 4. Aural haematoma – usually treated surgically

Apply a dressing

The Nose The nose is part of the respiratory system and injury may cause restriction of oxygen supply Injuries to the nose may result in epistaxis (nose bleed) – this may be unilateral or bilateral Causes 1. Trauma 2. Foreign body 3. Infection 4. Tumours

The Nose - Treatment Avoid muzzling if nose is injures Cold compresses can be applied Place patient in dark quiet room Observe – may need oxygen if breathing compromised
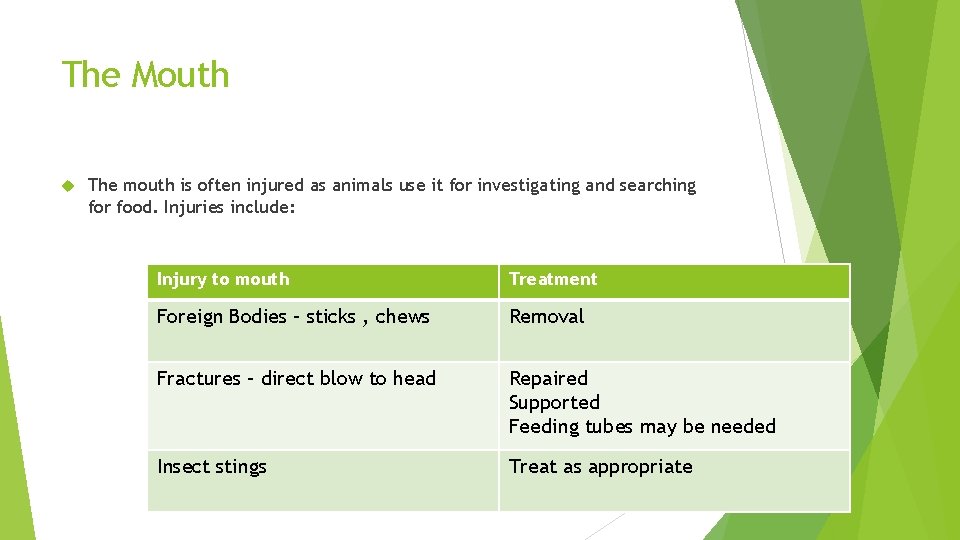
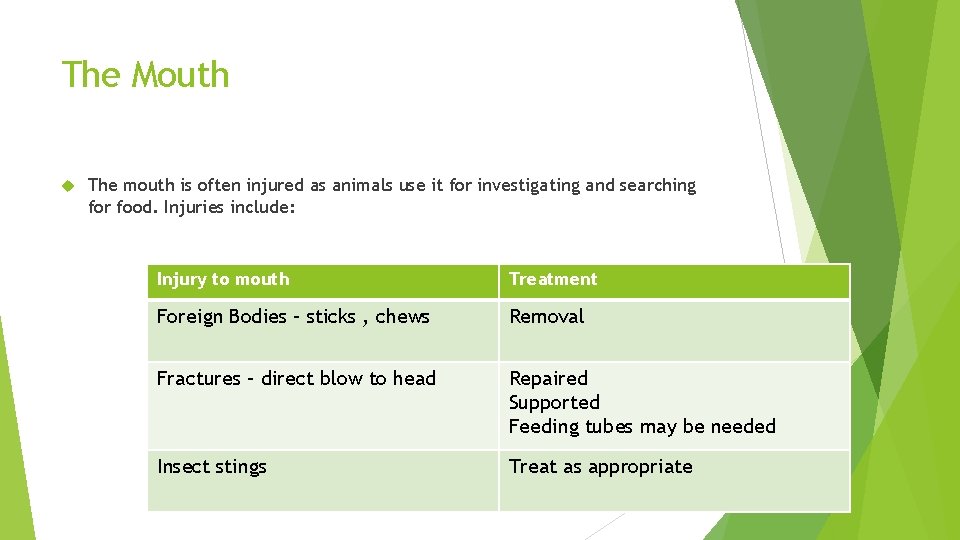
The Mouth The mouth is often injured as animals use it for investigating and searching for food. Injuries include: Injury to mouth Treatment Foreign Bodies – sticks , chews Removal Fractures – direct blow to head Repaired Supported Feeding tubes may be needed Insect stings Treat as appropriate

Fractured Jaw
Abdominal Injuries Some of the organs of the body are essential to life and if they are seriously injured the death of the animal is inevitable.
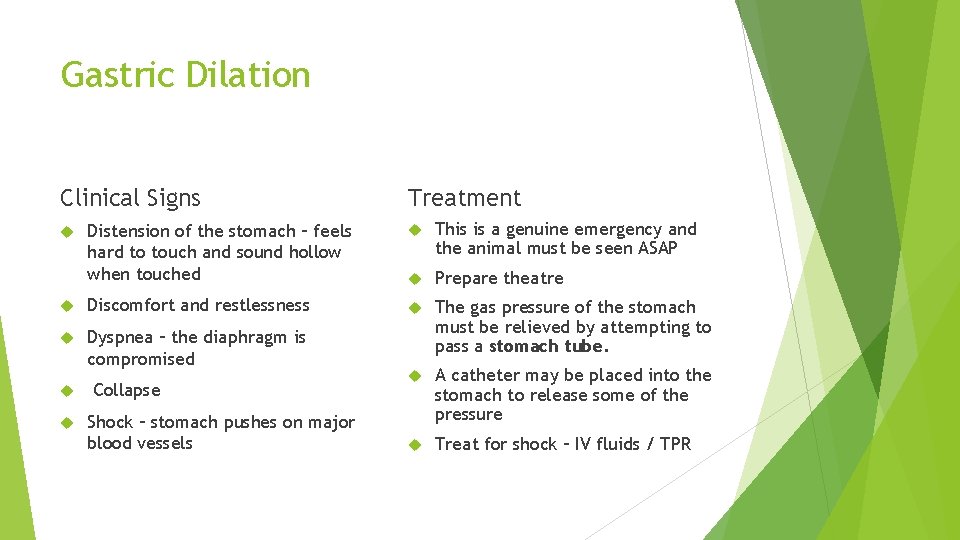
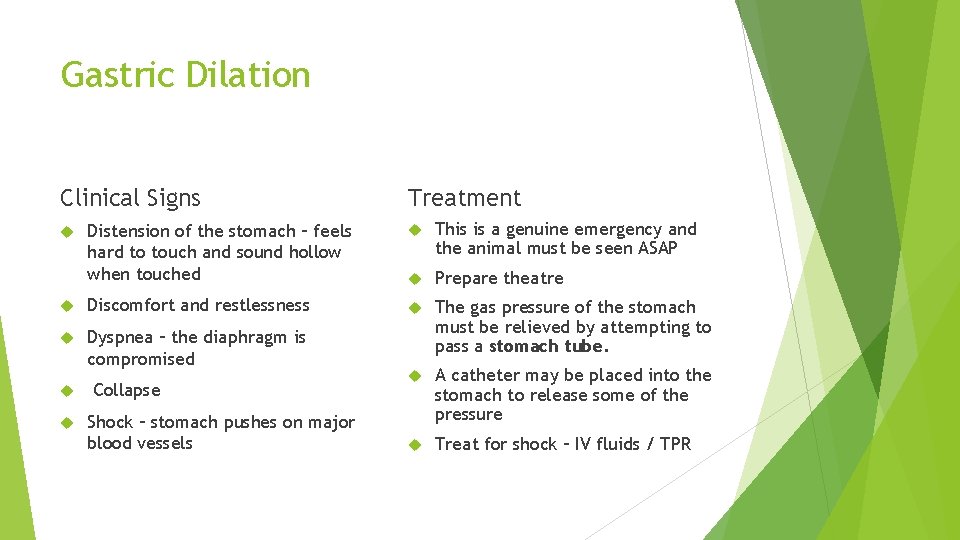
Gastric Dilation Clinical Signs Treatment Distension of the stomach – feels hard to touch and sound hollow when touched This is a genuine emergency and the animal must be seen ASAP Prepare theatre Discomfort and restlessness Dyspnea – the diaphragm is compromised The gas pressure of the stomach must be relieved by attempting to pass a stomach tube. A catheter may be placed into the stomach to release some of the pressure Treat for shock – IV fluids / TPR Collapse Shock – stomach pushes on major blood vessels




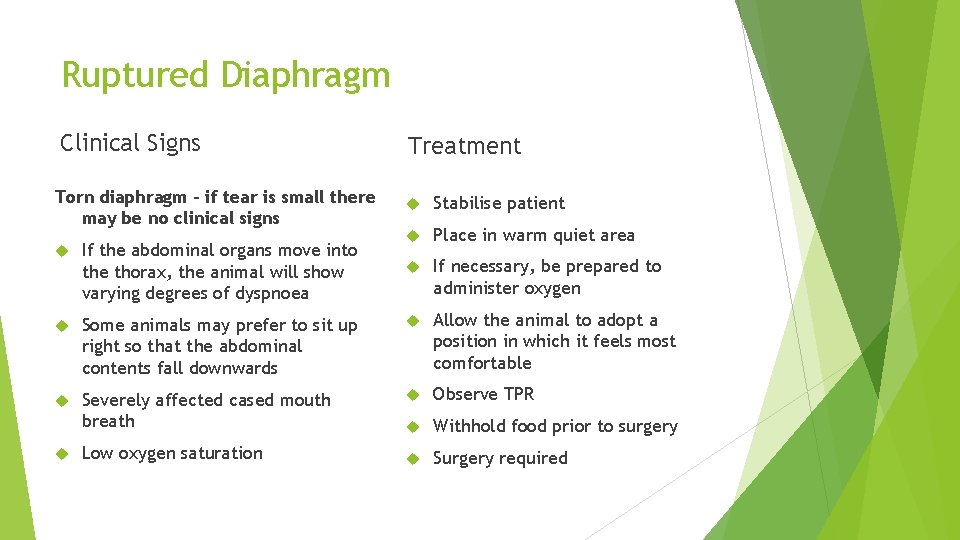
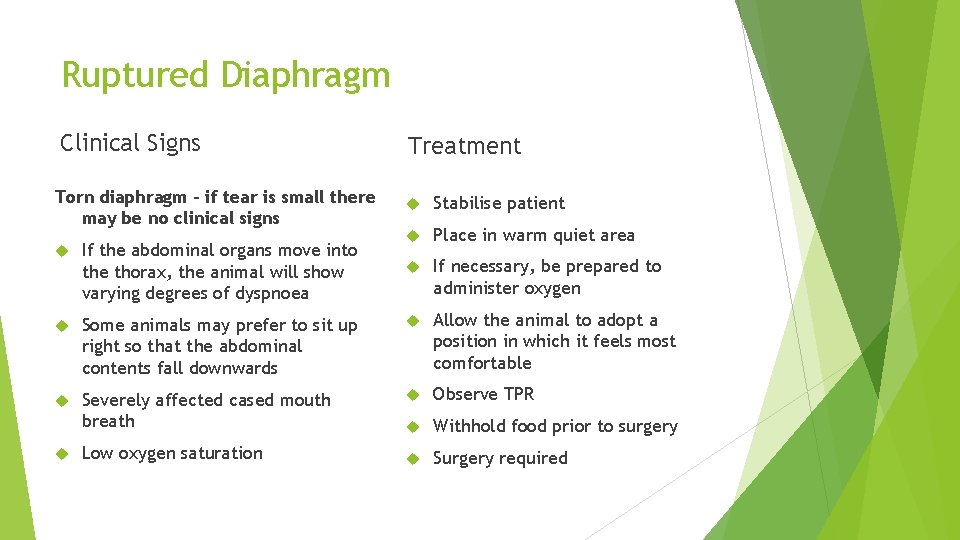
Ruptured Diaphragm Clinical Signs Treatment Torn diaphragm – if tear is small there may be no clinical signs Stabilise patient If the abdominal organs move into the thorax, the animal will show varying degrees of dyspnoea Place in warm quiet area If necessary, be prepared to administer oxygen Some animals may prefer to sit up right so that the abdominal contents fall downwards Allow the animal to adopt a position in which it feels most comfortable Severely affected cased mouth breath Observe TPR Withhold food prior to surgery Surgery required Low oxygen saturation

Diaphragmatic Rupture
Splenic Injuries Clinical Signs The spleen is a blood filled organ capable of profuse haemorrhage. Damage can be caused by tumours / trauma / torsion Sudden collapse Rapid RR Pale MM colour Blood filling in abdominal cavity If torsion – abdomen swollen and hard Treatment In cases where the spleen has ruptured very little can be done and the animal is likely to die of internal bleeding If the animal is able to be treated then treat for shock then surgery.


Splenic Removal

Bladder Injuries Clinical Signs The bladder may become ruptured / bruised Anuria – without Urine Haematuria – Blood in urine Dysuria – difficulty in passing urine Oliguria – reduced amount of urine being passed Treatment Monitor urine output Collect urine sample for analysis Prepare for catheterisation Prepare for radiography

Shock

Causes of Shock?

Shock an acute medical condition associated with a fall in blood pressure, caused by such events as loss of blood (hypovolaemia) , severe burns, allergic reaction, poisons or sudden emotional stress, and marked by cold, pale skin, irregular breathing, rapid pulse, and dilated pupils
Clinical symptoms Weak rapid pulse Pale mucous membranes Cold Eyes dilating Shallow breathing
Treatment for shock DR ABC (assess bleeding / reason for shock) Keep patient warm Seek medical veterinary attention as soon as possible

First aid treatment Keep animal warm Restrict movement Keep animal calm Seek veterinary treatment

Keeping the patient warm
Torn ears and haematomas
TORN EARS AND HEMATOMAS Result from barbed wire, fighting Hematoma = hemorrhage under the skin, usually results from severe head shaking (itchy ears) Torn ears will bleed profusely Head shaking leads to more bleeding
TORN EARS AND HEMATOMAS FIRST AID TREATMENT: 1. Cold wet compresses applied quickly and firmly to ear flap (ice) 2. Bandage up over the head - bandage right around the head and neck (not too tight!) 3. If hematoma, see a Veterinarian for treatment (not an emergency)
FISH HOOK INJURIES Ingested: Do not pull on line! It is likely to get caught and do internal damage. Go to Veterinarian, ASAP In lip, mouth or body. Push hook through skin, cut barb with wire cutters, and back rest of hook out.

Heat Stroke

Heat Stroke (Hyperthermia) Heatstroke occurs when normal body mechanisms cannot keep the body's temperature in a safe range. Animals do not have efficient cooling systems (like humans who sweat) and get overheated easily.
Causes of heat stroke Excessive environmental heat and humidity (may be due to weather conditions, such as a hot day, or to being enclosed in an unventilated room, car, or grooming dryer cage) Upper airway disease that inhibits breathing; the upper airway (also known as the upper respiratory tract) includes the nose, nasal passages, throat (pharynx), and windpipe (trachea) Poisoning; some poisonous compounds, such as strychnine and slug and snail bait, can lead to seizures, which can cause an abnormal increase in body temperature Excessive exercise

Heat Stroke Symptoms Rapid panting Bright red tongue Red or pale gums Thick, sticky saliva Depression Weakness Dizziness Vomiting sometimes with blood Shock leading to coma
What you should do Remove the dog from the hot area immediately. Prior to taking to your veterinarian, lower his temperature by wetting him thoroughly with cool tepid water, then increase air movement around him with a fan. CAUTION: Using very cold water can actually be counterproductive. Cooling too quickly and especially allowing his body temperature to become too low can cause other life-threatening medical conditions. The rectal temperature should be checked every 5 minutes by the veterinary team. Once the body temperature is 103ºF, the cooling measures should be stopped and the dog should be dried thoroughly and covered so he does not continue to lose heat. Even if the dog appears to be recovering, take him to your veterinarian as soon as possible. He should still be examined since he may be dehydrated or have other complications. Allow free access to water should be offered at all time.

Frost Bite
Hypothermia is a condition in which the body temperature becomes too low for normal functioning. It is more common in animals who are shorthaired, small, wet, or have no shelter during periods of cold temperatures.
HYPOTHERMIA, FROSTBITE FIRST AID TREATMENT 1. Wrap animal in blanket, and warm with gentle heat 2. Frostbite. Warm frozen areas with moist heat.

What are the symptoms? Animals with hypothermia often have violent shivering, slow and shallow respiration, and a slower heart rate. Their gums may appear pale or blue. If they are not warmed, they will become listless and eventually will be unresponsive and may die. What are the risks? If the body temperature becomes too low, dogs and cats will not be able to return their body to normal temperature without treatment. Injuries to tissues because of a decrease in the flow of oxygenated blood can occur. The extent of the injuries varies with the body temperature and duration of hypothermia. Hypothermia can be fatal.

What is the treatment? Hypothermic animals should be warmed slowly. There are several ways to do this. The animal can be placed in a warm room and wrapped in warm blankets (run dry blankets or towels through the clothes dryer for a few minutes to warm them). Bottles filled with warm water can be wrapped in a towel and placed next to the animal (plastic soda bottles work well) in the armpit and groin areas where there is less hair. Do NOT place hot water bottles directly in contact with the animal's body since burns could occur even if the bottles do not seem that hot to you. Hair dryers can be helpful, especially if the animal is wet as well as hypothermic. Warm water baths can be used for animals mildly hypothermic animals Contact the veterinary surgery

CPR
Cardiopulmonary resuscitation is the treatment required to save an animal (or human) life when suffering cardiopulmonary arrest. Unlike what we see on television, most patients who suffer from cardiac arrest are unable to be saved, even with CPR. The intent of CPR is to provide sufficient blood flow and oxygen to the brain and vital organs to support life until more advanced medical therapy can be started. In a study from the University of California at Davis, researchers discovered that long-term survival among feline patients is extremely poor. In this study, only 2. 3% of feline patients who received CPR survived to be discharged from the hospital alive. This closely parallels findings of similar studies in human medicine
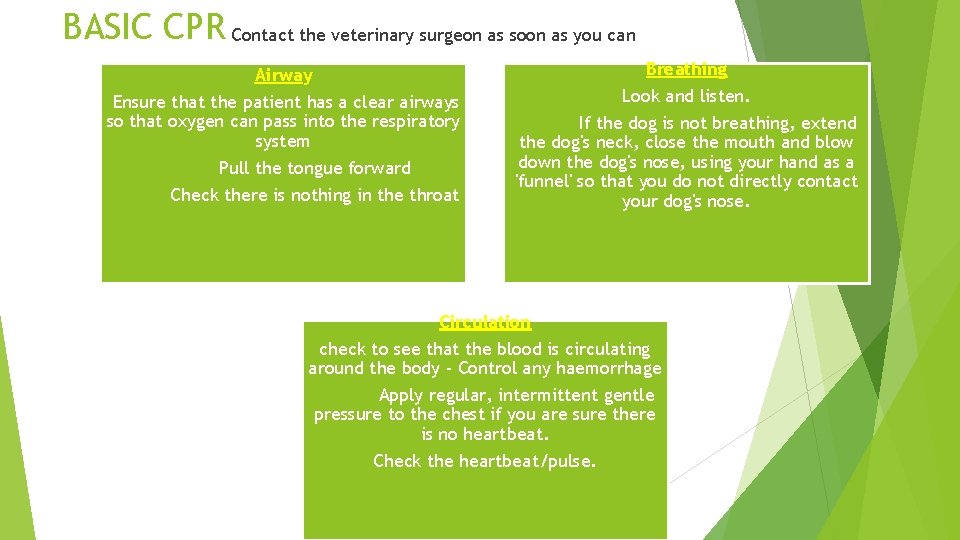
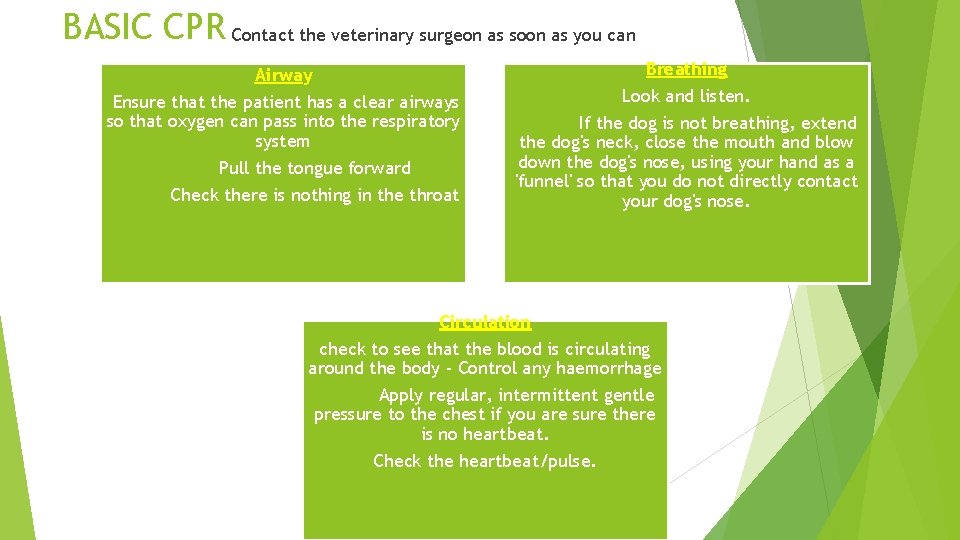
BASIC CPR Contact the veterinary surgeon as soon as you can Airway Breathing Ensure that the patient has a clear airways so that oxygen can pass into the respiratory system Pull the tongue forward Check there is nothing in the throat Look and listen. If the dog is not breathing, extend the dog's neck, close the mouth and blow down the dog's nose, using your hand as a 'funnel' so that you do not directly contact your dog's nose. Circulation check to see that the blood is circulating around the body - Control any haemorrhage Apply regular, intermittent gentle pressure to the chest if you are sure there is no heartbeat. Check the heartbeat/pulse.
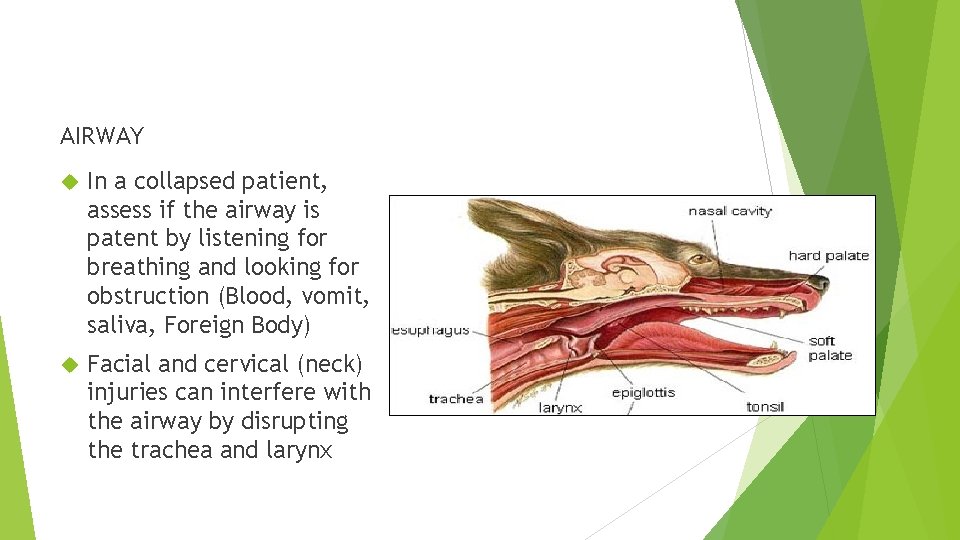
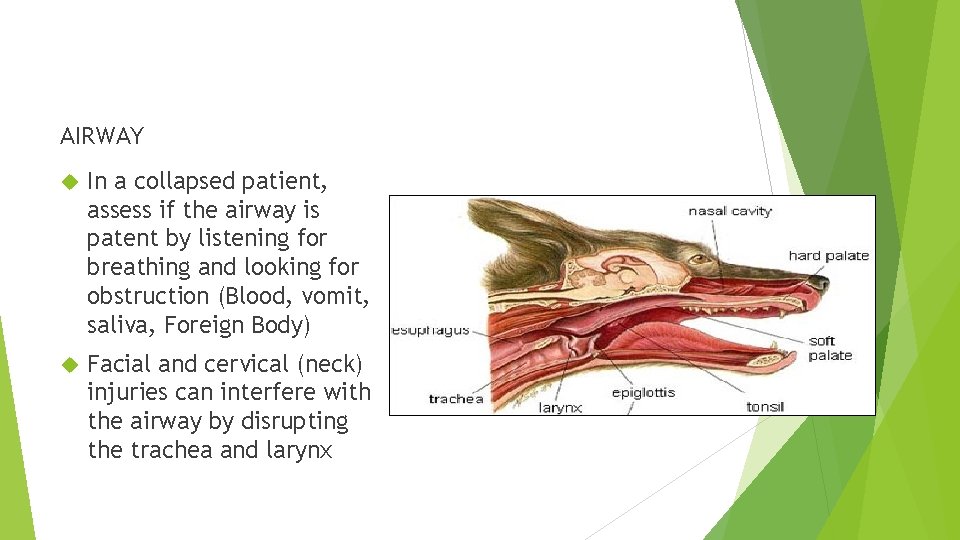
AIRWAY In a collapsed patient, assess if the airway is patent by listening for breathing and looking for obstruction (Blood, vomit, saliva, Foreign Body) Facial and cervical (neck) injuries can interfere with the airway by disrupting the trachea and larynx
Emergencies involving the air way Air Way Obstruction: Other: FB – Ball Heat Bee sting creating inflammatory response Breed (brachio cephalic- short nose dogs) Cancer Choking Structural abnormality (such as elongated soft palate, common in flat faced breeds
B: BREATHING Observation should focus on: - RR, an increased rate is named tachypnoea Normal Respiratory Pattern: - tachypnoea can also be caused by fear and stress Respiratory Effort These animals often alter their body posture to help assist breathing Flared nostrils, extended neck Exaggerated effort Check breathing cycle – time of inspiration is usually the same as expiration Auscultation Listen to chest sounds

Emergencies involving Respiration Damaged ribs Infection (bacterial, viral, parasitic) Foreign objects Heart failure Anaemia Trauma Allergies Drowning Pain Electrocution Fever Asphyxia Choking Shock Diseases that make the belly enlarged or bloated (such as enlarged liver, stomach filled with air (bloat) or fluid in the belly) Asthma Attack Medications Bleeding Tumours
Symptoms of Respiratory Arrest Collapse Cyanosis No breathing movements Distressed Heart beat present If respiration has stopped for more than 1 minute artificial respiration should begin
Medical terms Dyspnea -this term implies conscious perception of "air hunger" or a sense of shortness of breath. This term is not ideal to use in reference to veterinary patients, as they cannot relay this sense or perception of respiratory difficulty. Tachypnea - greater than normal respiratory rate. Hyperventilation that exceeds metabolic demands; Hypoventilation that does not meet metabolic demands Apnea - cessation of breathing for an indeterminate period.
C: Cardiovascular The aim is to examine the effect of the heart pumping blood to body tissues. Poor perfusion leads to reduced oxygen delivery to body tissues – known as shock Left uncorrected shock can lead to cell death Decreased cardiac output may be due to reduced circulating volume (hypvolaemia) or due to heart failure and arrhythmias. The aim of shock is to preserve core vital organs at the expense of the skin / gastrointestinal/ muscles / kidneys

Causes of cardiac arrest Signs Heart Attack Collapse Heart Failure Cyanosis Electrocution Dilated Pupils Hyperventilating No heart beat Poison Shock / Haemorrhage Blood loss
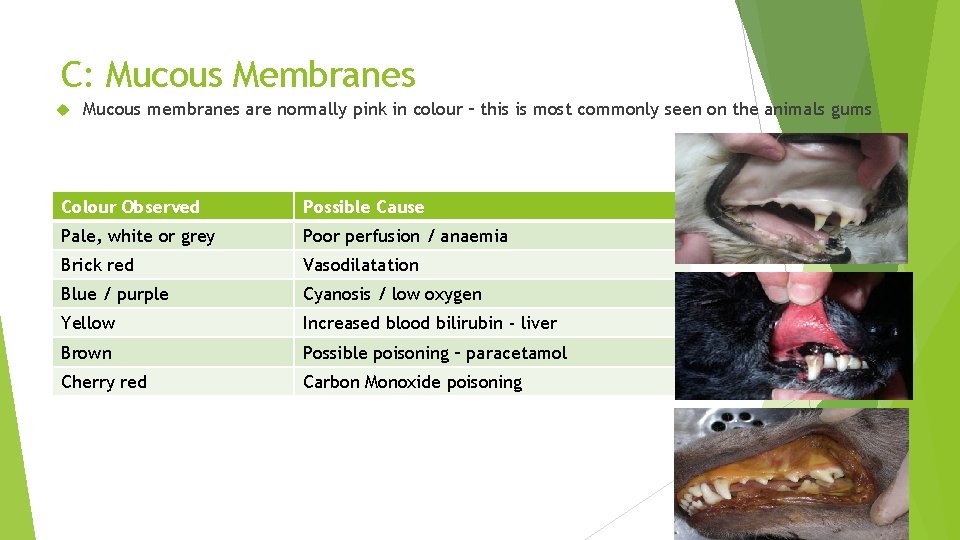
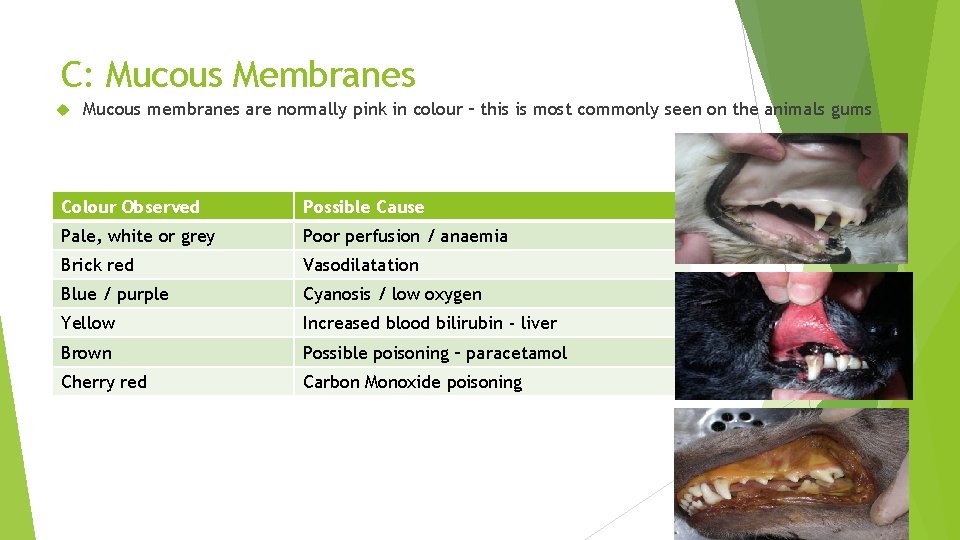
C: Mucous Membranes Mucous membranes are normally pink in colour – this is most commonly seen on the animals gums Colour Observed Possible Cause Pale, white or grey Poor perfusion / anaemia Brick red Vasodilatation Blue / purple Cyanosis / low oxygen Yellow Increased blood bilirubin - liver Brown Possible poisoning – paracetamol Cherry red Carbon Monoxide poisoning
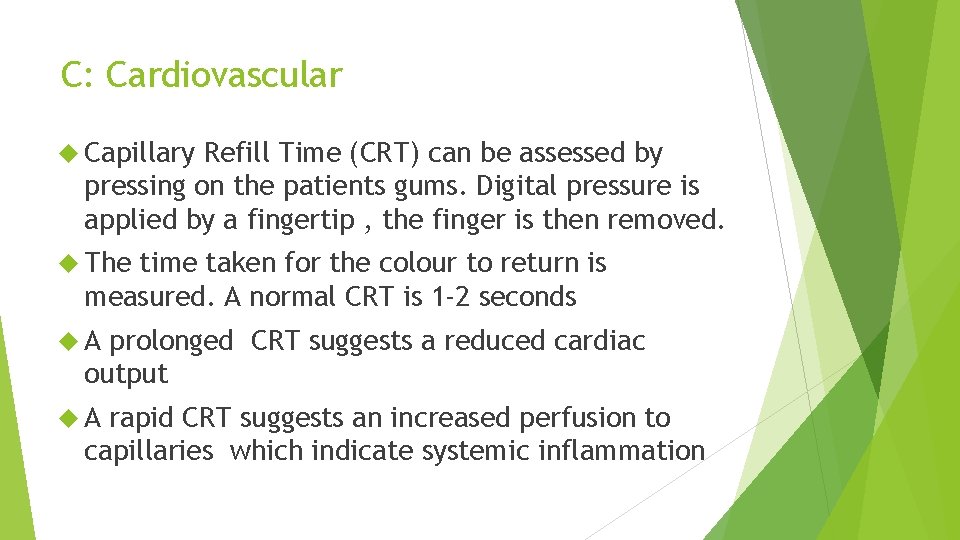
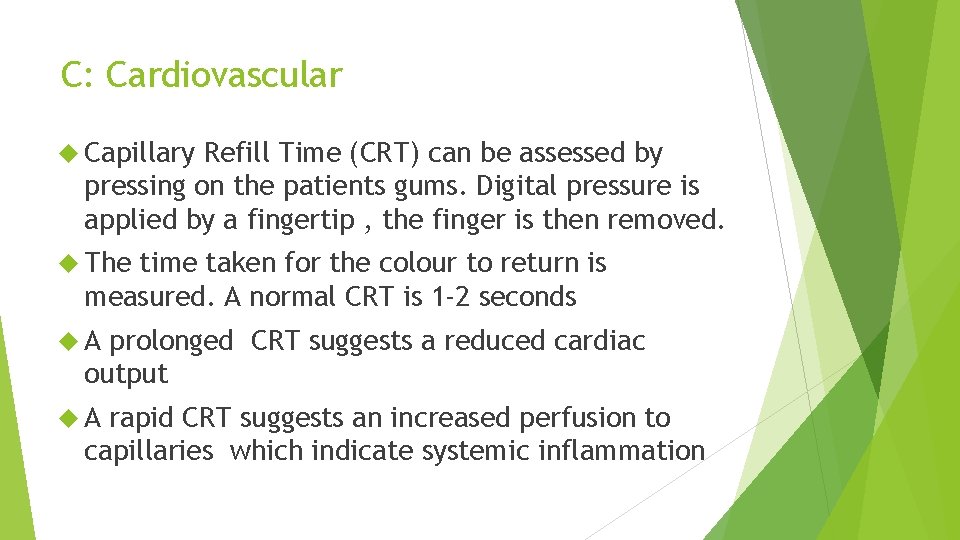
C: Cardiovascular Capillary Refill Time (CRT) can be assessed by pressing on the patients gums. Digital pressure is applied by a fingertip , the finger is then removed. The time taken for the colour to return is measured. A normal CRT is 1 -2 seconds A prolonged CRT suggests a reduced cardiac output A rapid CRT suggests an increased perfusion to capillaries which indicate systemic inflammation

CRT

Pulse Palpation of the femoral pulse will reveal pulse rate and rhythm and gives an impression of stroke volume (the amount of blood pumped with each beat).
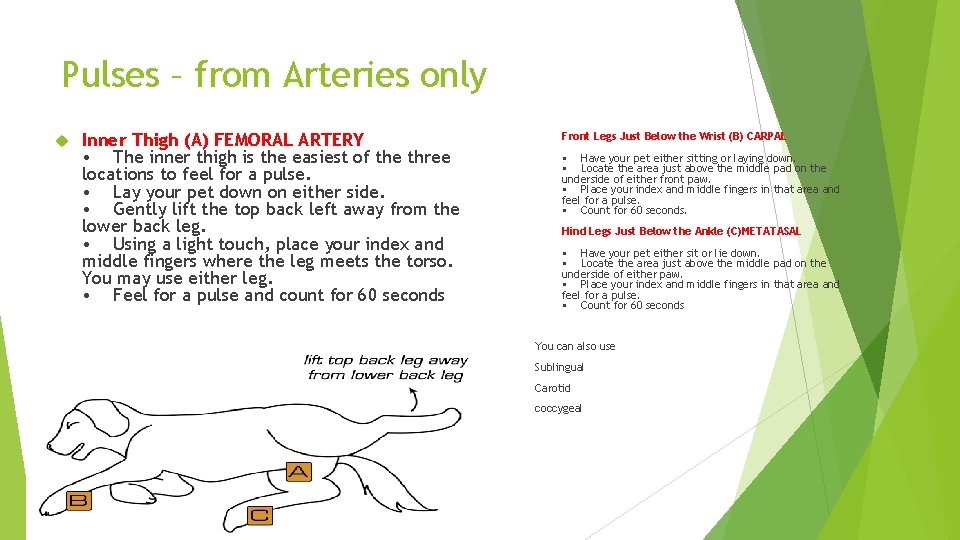
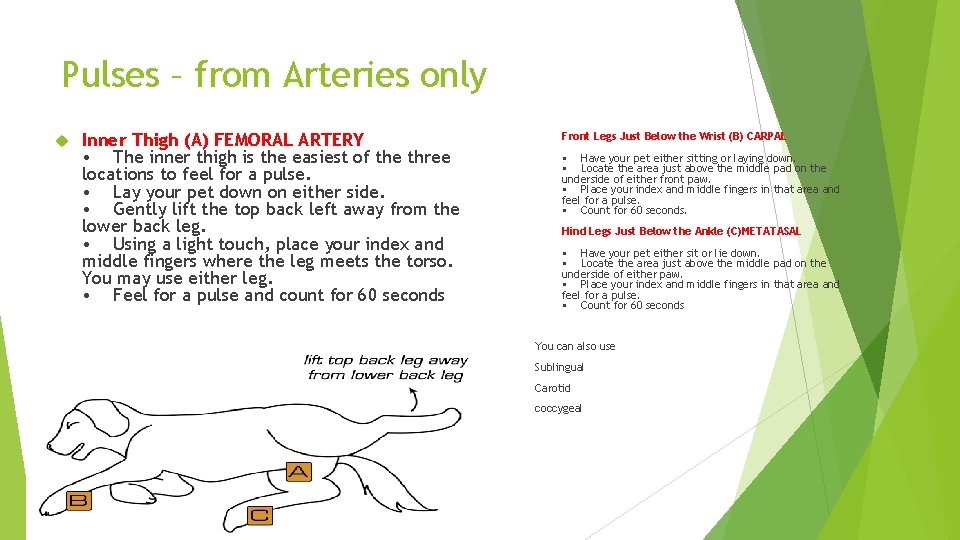
Pulses – from Arteries only Inner Thigh (A) FEMORAL ARTERY • The inner thigh is the easiest of the three locations to feel for a pulse. • Lay your pet down on either side. • Gently lift the top back left away from the lower back leg. • Using a light touch, place your index and middle fingers where the leg meets the torso. You may use either leg. • Feel for a pulse and count for 60 seconds Front Legs Just Below the Wrist (B) CARPAL • Have your pet either sitting or laying down. • Locate the area just above the middle pad on the underside of either front paw. • Place your index and middle fingers in that area and feel for a pulse. • Count for 60 seconds. Hind Legs Just Below the Ankle (C)METATASAL • Have your pet either sit or lie down. • Locate the area just above the middle pad on the underside of either paw. • Place your index and middle fingers in that area and feel for a pulse. • Count for 60 seconds You can also use Sublingual Carotid coccygeal
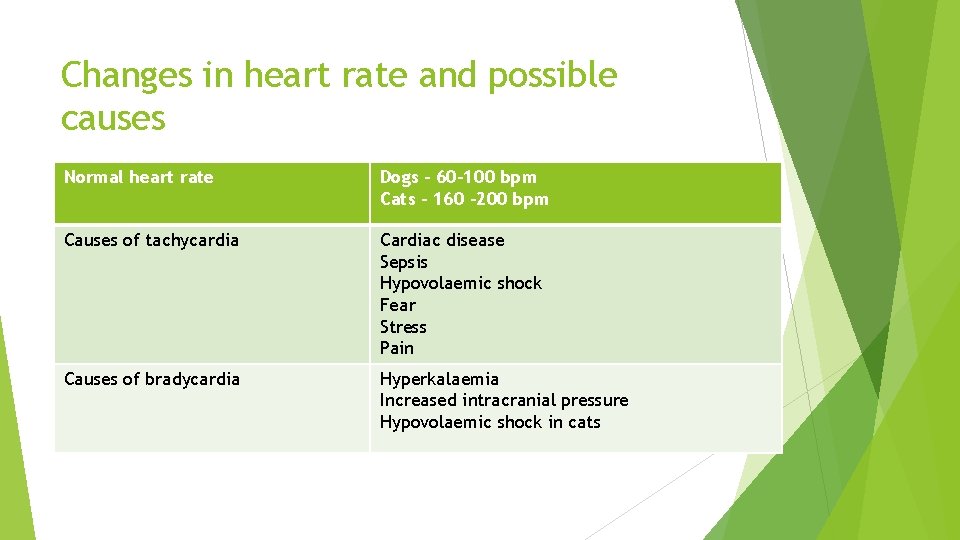
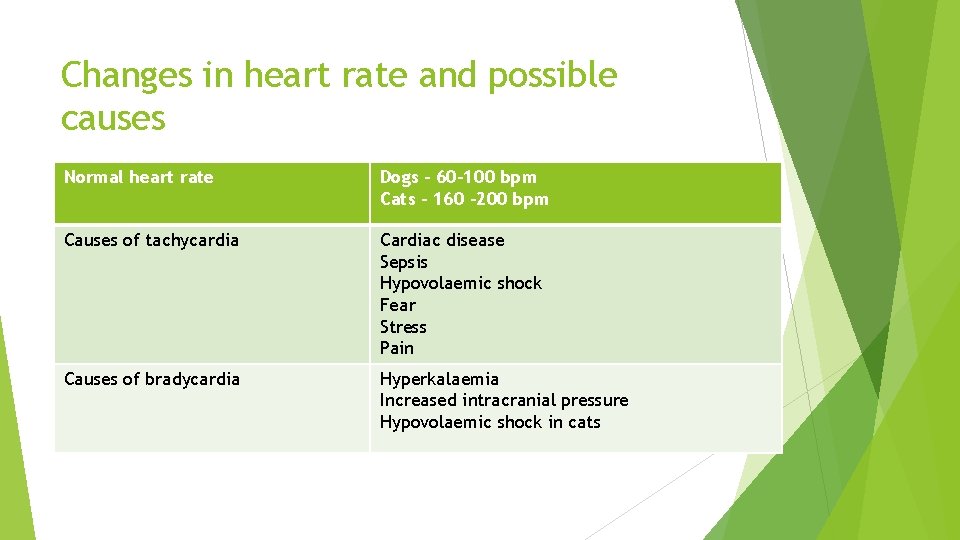
Changes in heart rate and possible causes Normal heart rate Dogs – 60 -100 bpm Cats – 160 -200 bpm Causes of tachycardia Cardiac disease Sepsis Hypovolaemic shock Fear Stress Pain Causes of bradycardia Hyperkalaemia Increased intracranial pressure Hypovolaemic shock in cats

CPR step by step plan
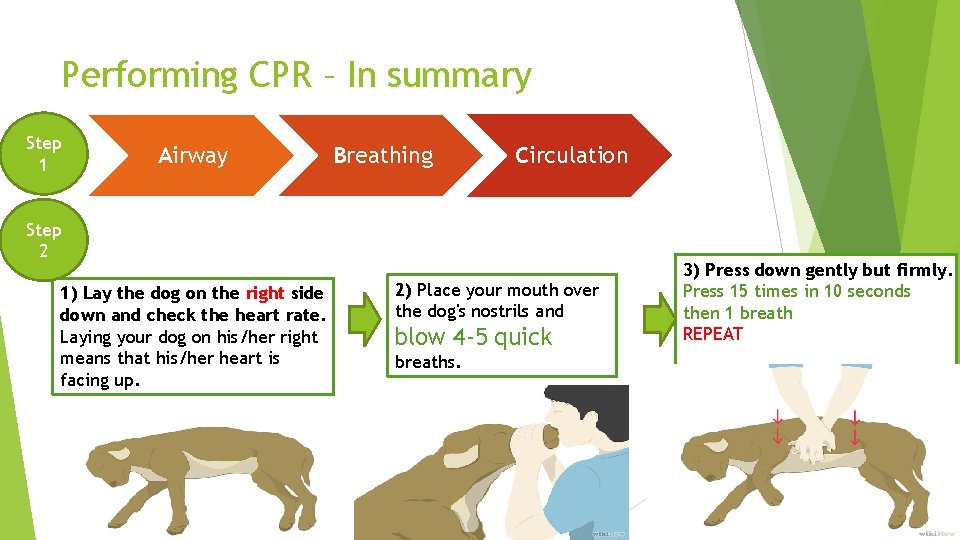
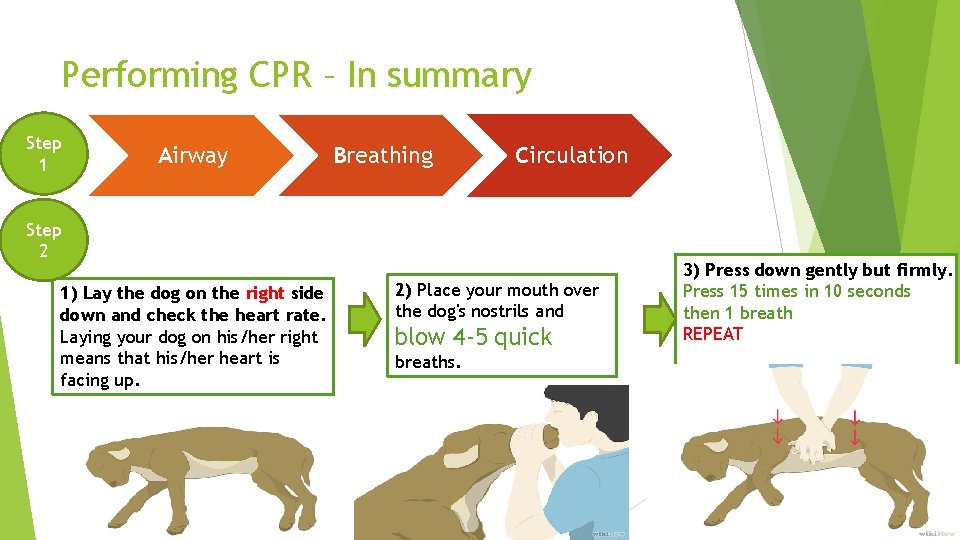
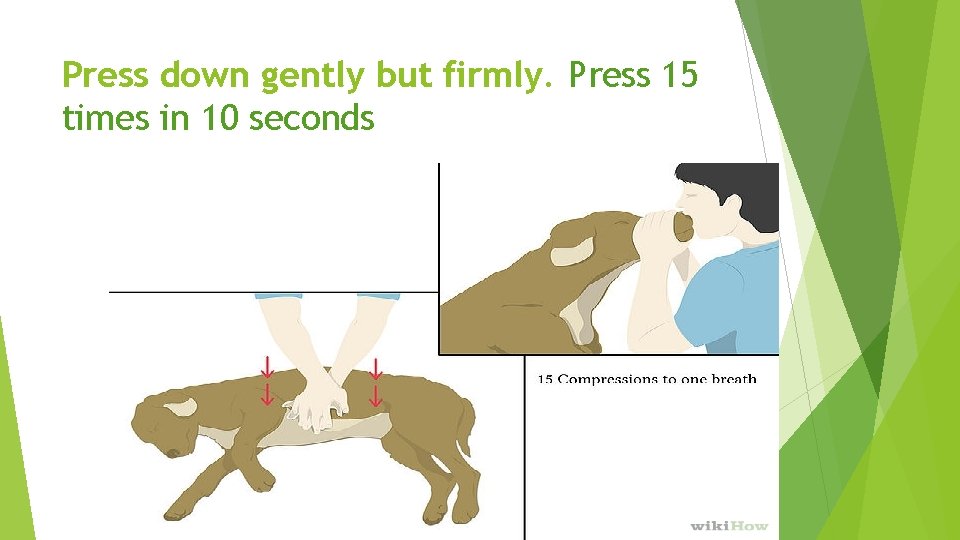
Performing CPR – In summary Step 1 Airway Breathing Circulation Step 2 1) Lay the dog on the right side down and check the heart rate. Laying your dog on his/her right means that his/her heart is facing up. 2) Place your mouth over the dog's nostrils and blow 4 -5 quick breaths. 3) Press down gently but firmly. Press 15 times in 10 seconds then 1 breath REPEAT

Check your dog's vital signs. Talk to and rub your dog to see if he/she responds. If he/she offers no response, CPR will be helpful. Your dog has fallen unconscious and has stopped breathing; and/or Has no heartbeat
Contact emergency help immediately. Call your vet, to let them know.
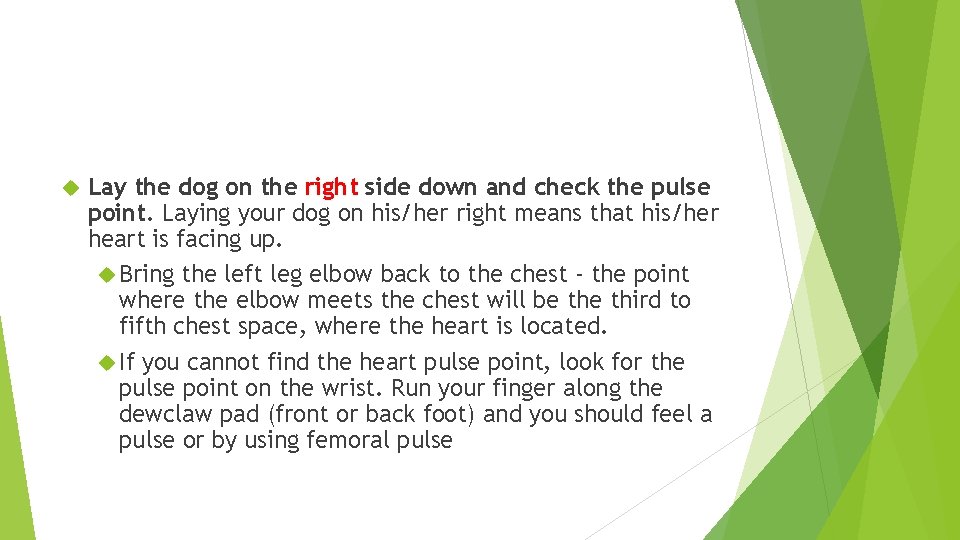
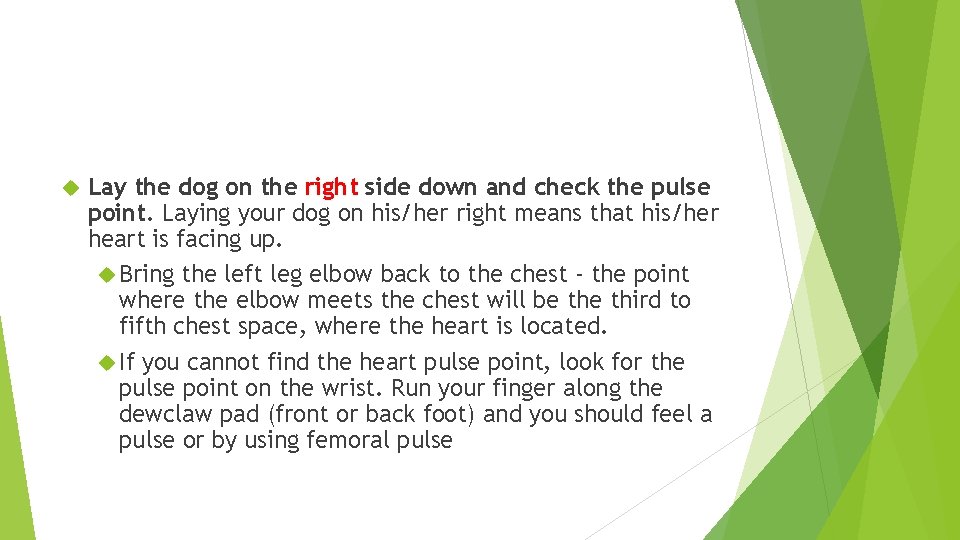
Lay the dog on the right side down and check the pulse point. Laying your dog on his/her right means that his/her heart is facing up. Bring the left leg elbow back to the chest - the point where the elbow meets the chest will be third to fifth chest space, where the heart is located. If you cannot find the heart pulse point, look for the pulse point on the wrist. Run your finger along the dewclaw pad (front or back foot) and you should feel a pulse or by using femoral pulse
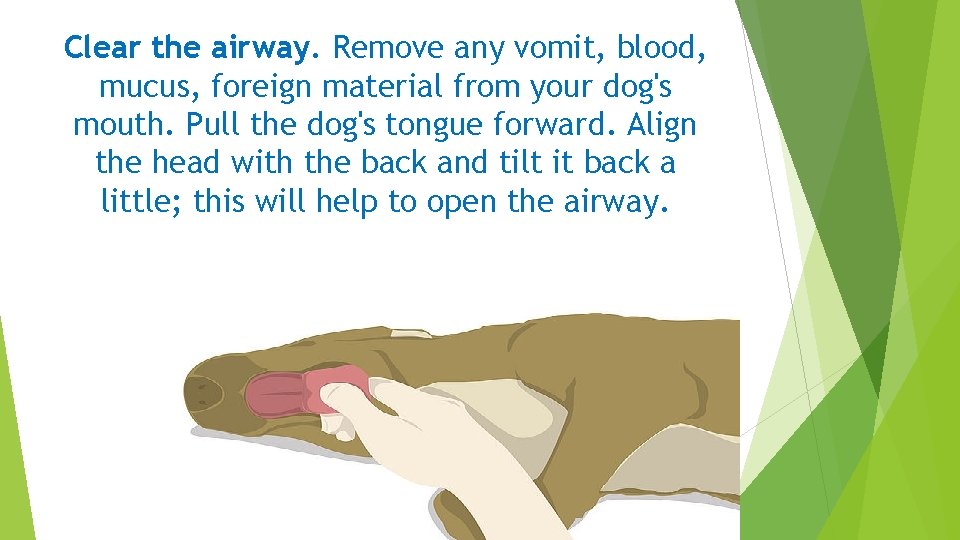
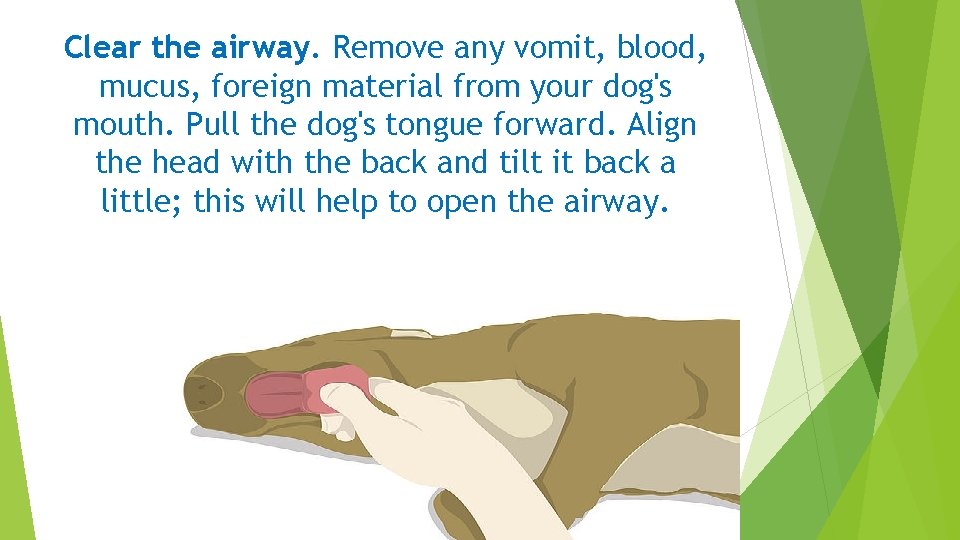
Clear the airway. Remove any vomit, blood, mucus, foreign material from your dog's mouth. Pull the dog's tongue forward. Align the head with the back and tilt it back a little; this will help to open the airway.
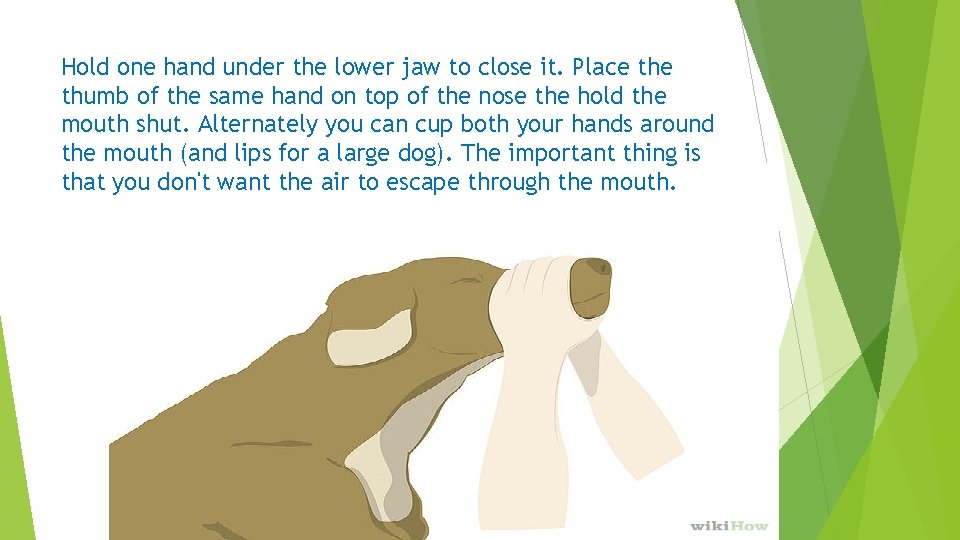
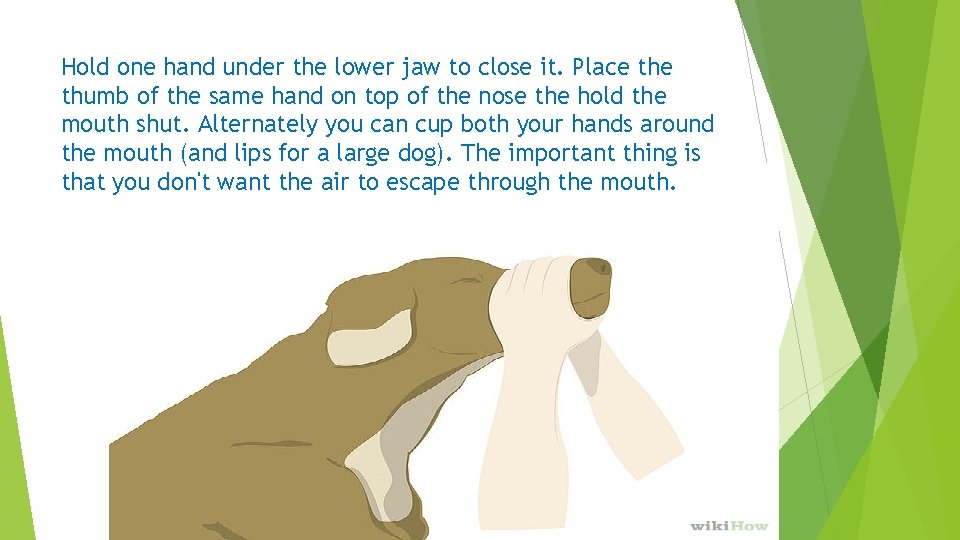
Hold one hand under the lower jaw to close it. Place thumb of the same hand on top of the nose the hold the mouth shut. Alternately you can cup both your hands around the mouth (and lips for a large dog). The important thing is that you don't want the air to escape through the mouth.
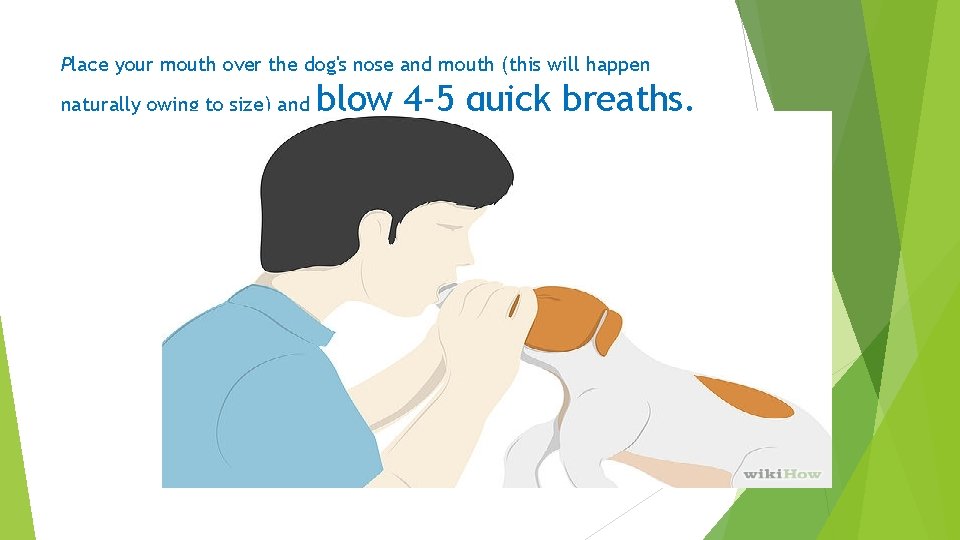
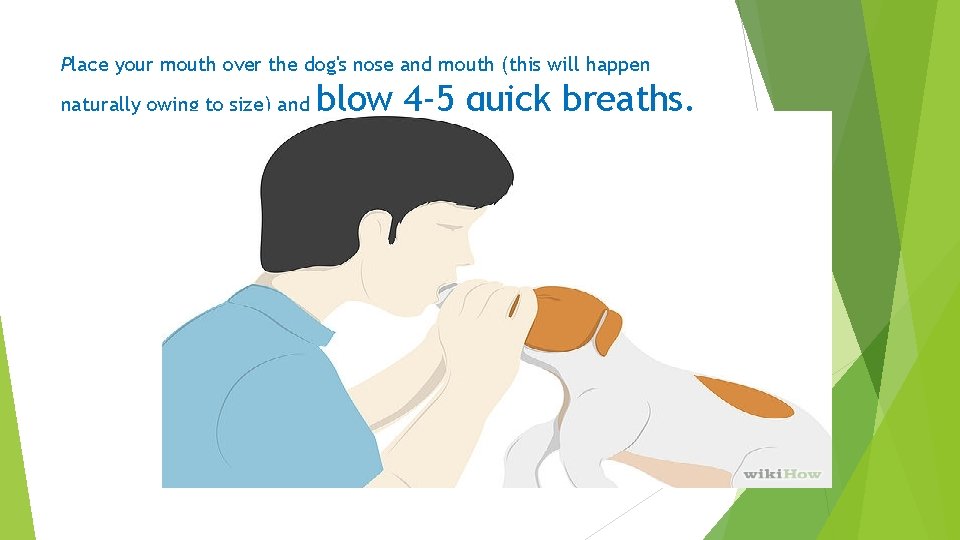
Place your mouth over the dog's nose and mouth (this will happen naturally owing to size) and blow 4 -5 quick breaths.

Watch for the gentle rise of the chest
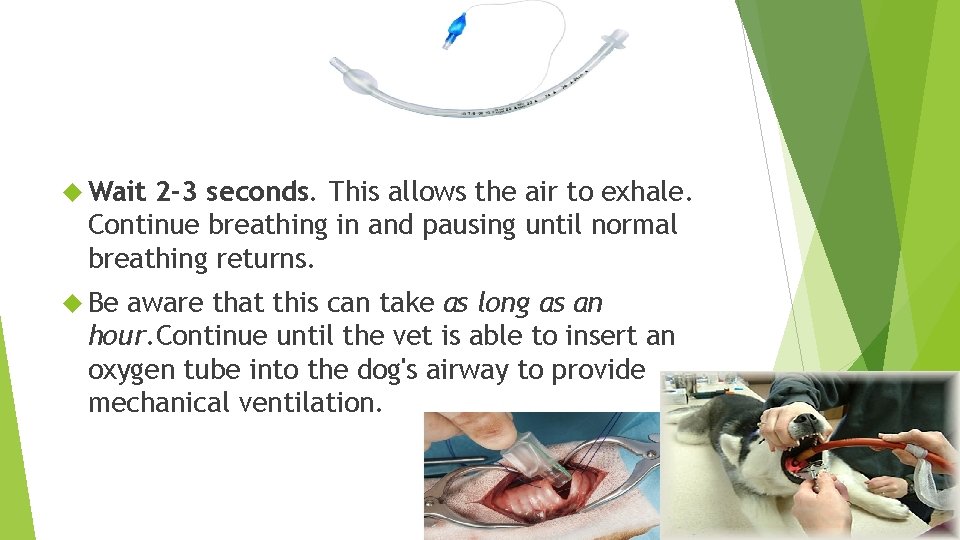
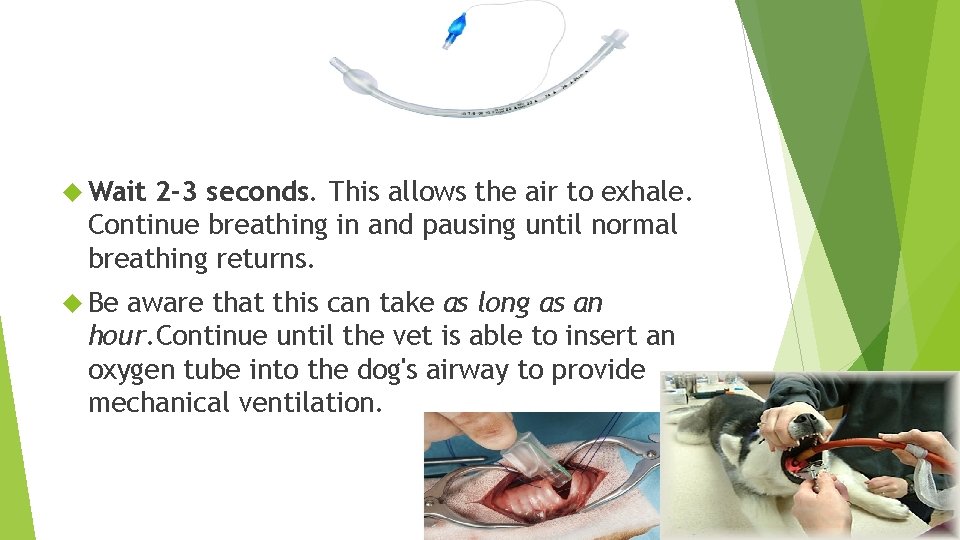
Wait 2 -3 seconds. This allows the air to exhale. Continue breathing in and pausing until normal breathing returns. Be aware that this can take as long as an hour. Continue until the vet is able to insert an oxygen tube into the dog's airway to provide mechanical ventilation.
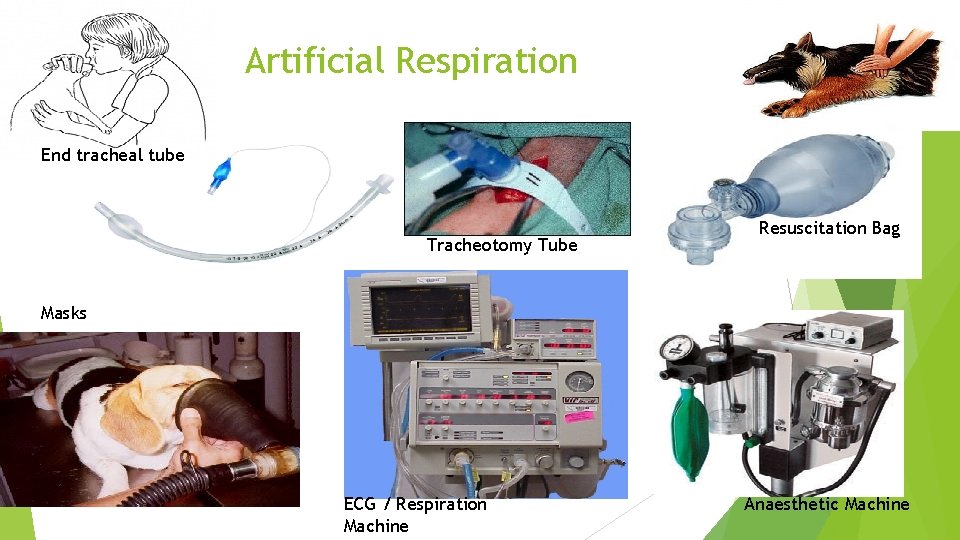
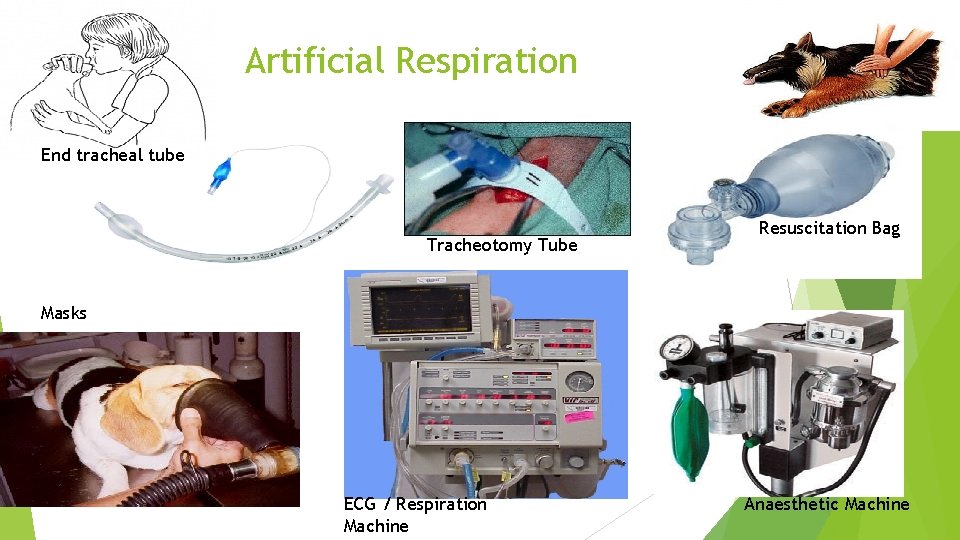
Artificial Respiration End tracheal tube Tracheotomy Tube Resuscitation Bag Masks ECG / Respiration Machine Anaesthetic Machine
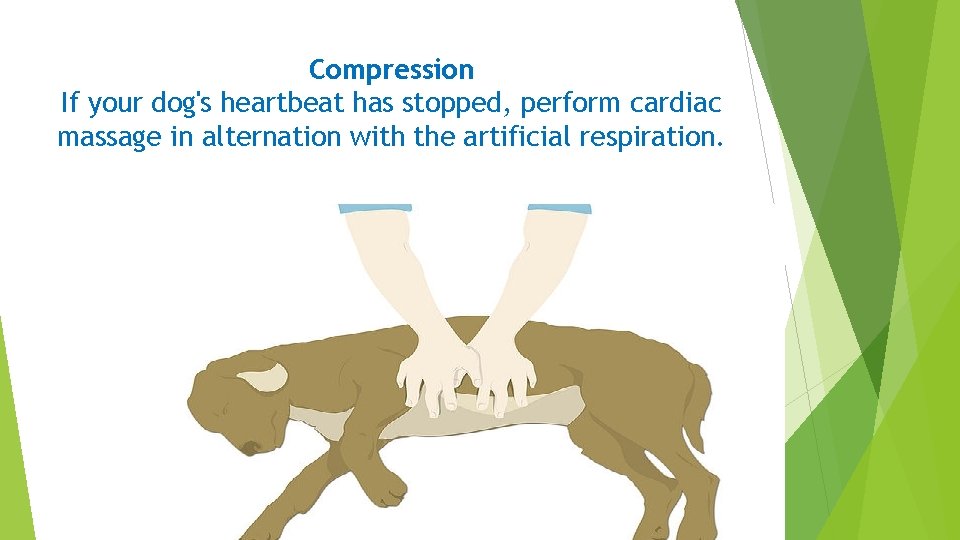
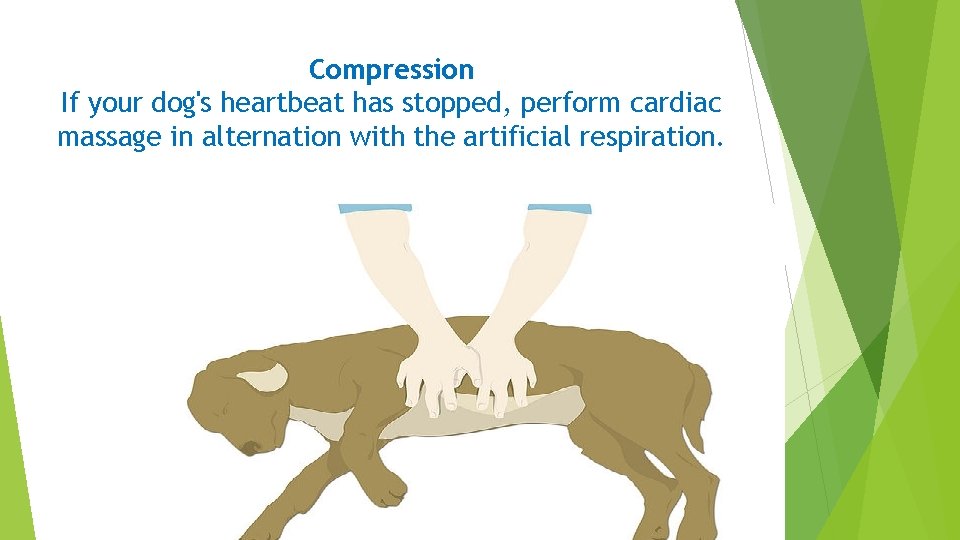
Compression If your dog's heartbeat has stopped, perform cardiac massage in alternation with the artificial respiration.

Place your hand on his/her chest behind her front leg "elbow".

Lock your fingers together and lock your elbows
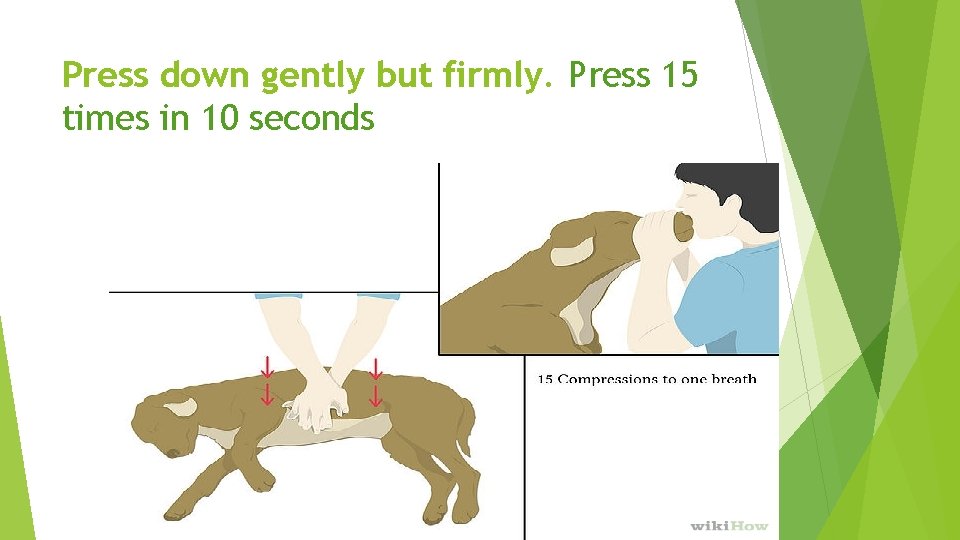
Press down gently but firmly. Press 15 times in 10 seconds

Performing CPR – In summary Step 1 Airway Breathing Circulation Step 2 1) Lay the dog on the right side down and check the heart rate. Laying your dog on his/her right means that his/her heart is facing up. 2) Place your mouth over the dog's nostrils and blow 4 -5 quick breaths. 3) Press down gently but firmly. Press 15 times in 10 seconds then 1 breath
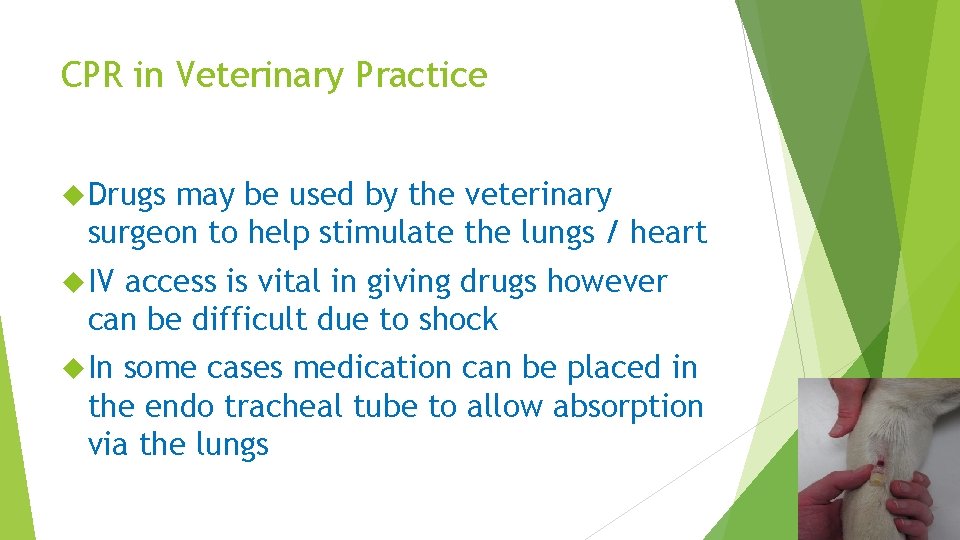
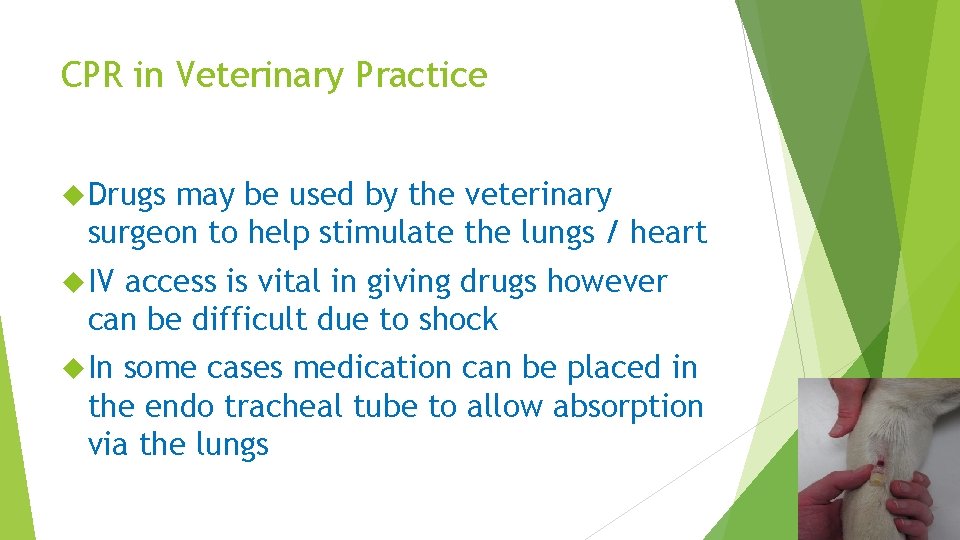
CPR in Veterinary Practice Drugs may be used by the veterinary surgeon to help stimulate the lungs / heart IV access is vital in giving drugs however can be difficult due to shock In some cases medication can be placed in the endo tracheal tube to allow absorption via the lungs
http: //www. youtube. com/watch? v=0 AFr Ui. RIe. Vo&feature=player_embedded

End