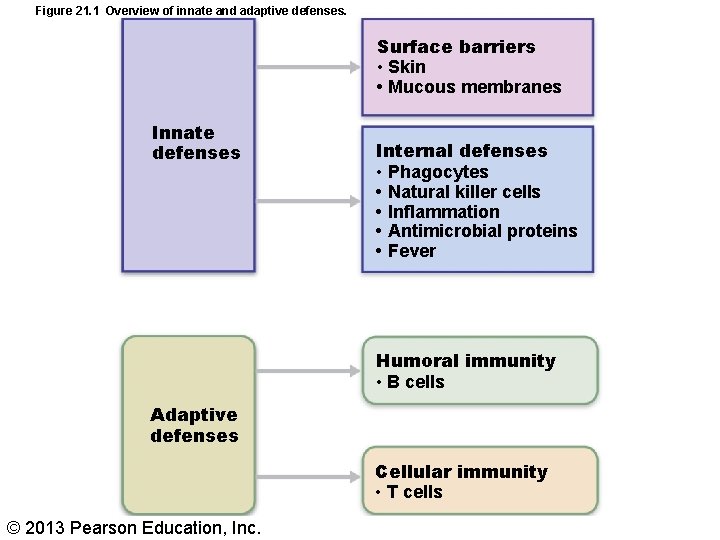
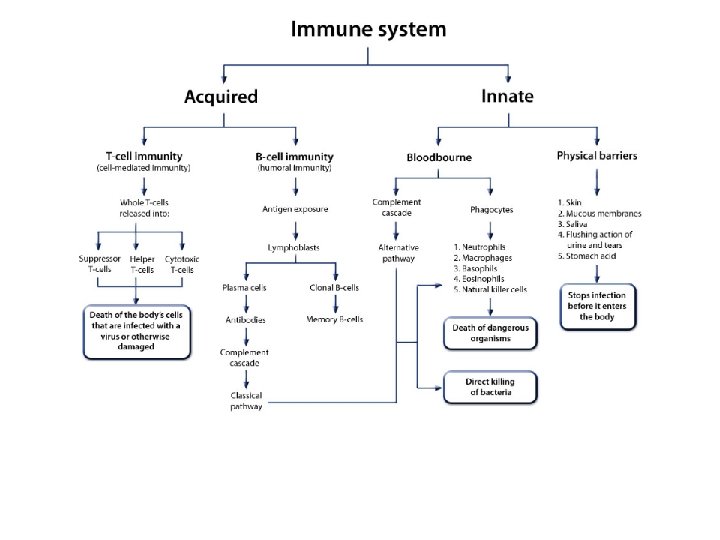
Figure 21 1 Overview of innate and adaptive
- Slides: 28
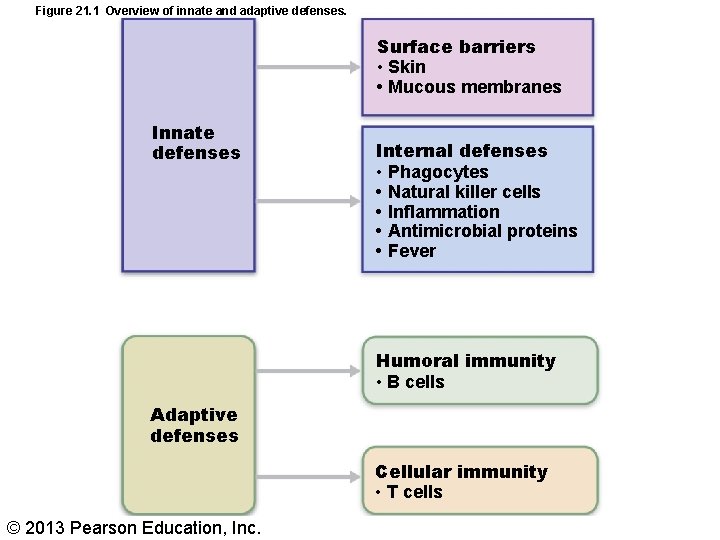
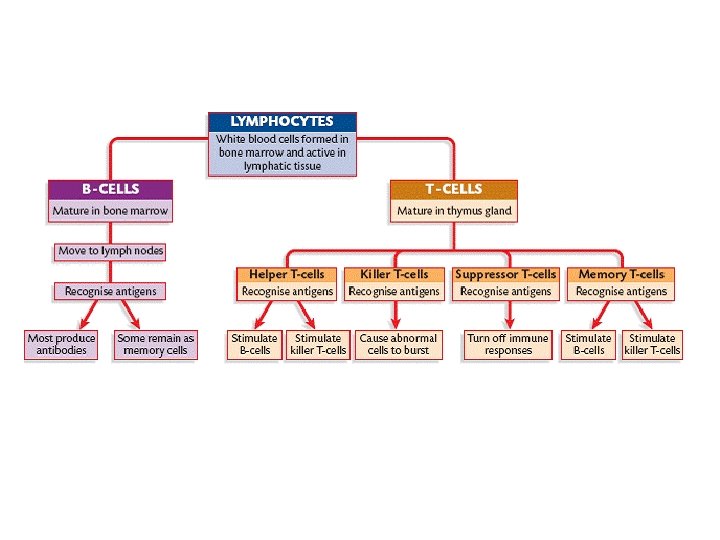
Figure 21. 1 Overview of innate and adaptive defenses. Surface barriers • Skin • Mucous membranes Innate defenses Internal defenses • Phagocytes • Natural killer cells • Inflammation • Antimicrobial proteins • Fever Humoral immunity • B cells Adaptive defenses Cellular immunity • T cells © 2013 Pearson Education, Inc.
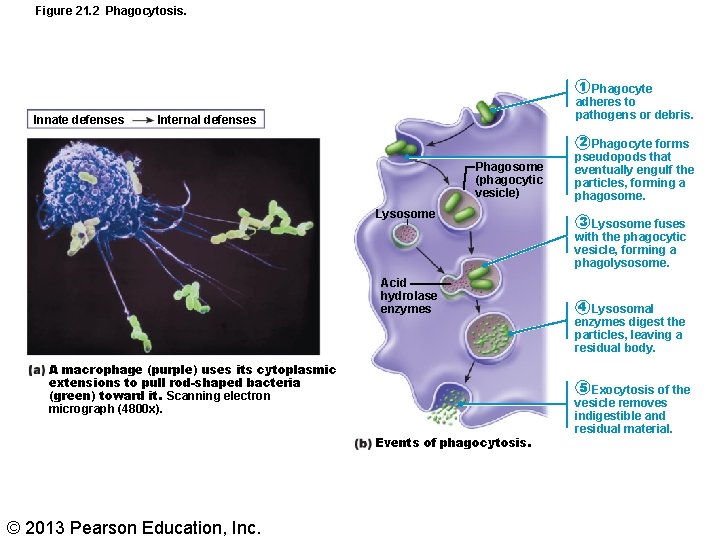
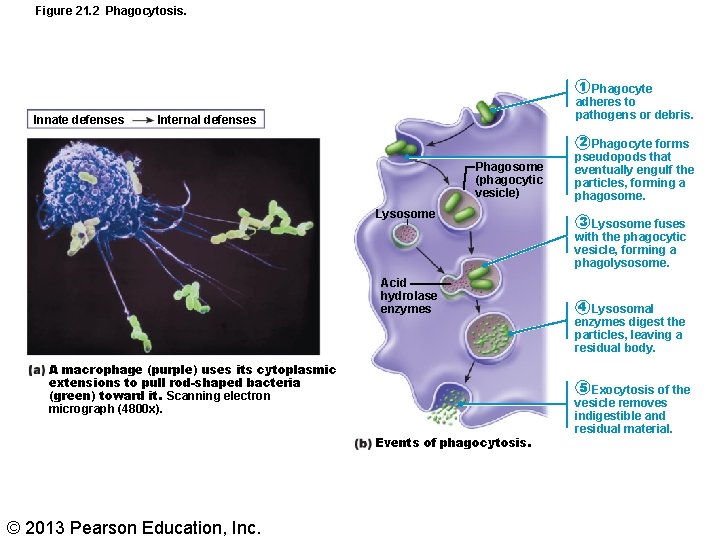
Figure 21. 2 Phagocytosis. Innate defenses 1 Phagocyte adheres to pathogens or debris. Internal defenses Phagosome (phagocytic vesicle) Lysosome Acid hydrolase enzymes A macrophage (purple) uses its cytoplasmic extensions to pull rod-shaped bacteria (green) toward it. Scanning electron micrograph (4800 x). Events of phagocytosis. © 2013 Pearson Education, Inc. 2 Phagocyte forms pseudopods that eventually engulf the particles, forming a phagosome. 3 Lysosome fuses with the phagocytic vesicle, forming a phagolysosome. 4 Lysosomal enzymes digest the particles, leaving a residual body. 5 Exocytosis of the vesicle removes indigestible and residual material.
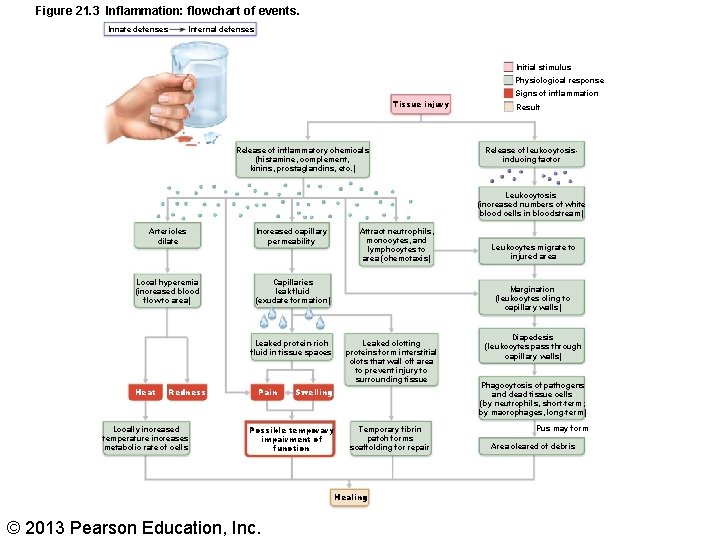
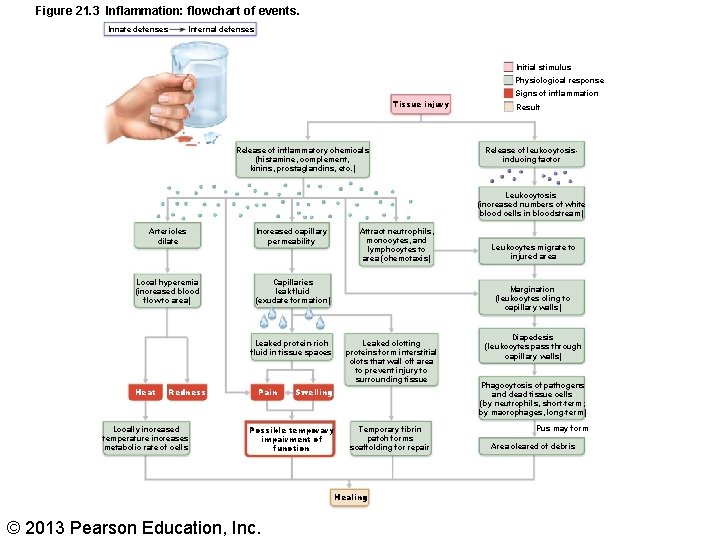
Figure 21. 3 Inflammation: flowchart of events. Innate defenses Internal defenses Initial stimulus Physiological response Tissue injury Release of inflammatory chemicals (histamine, complement, kinins, prostaglandins, etc. ) Signs of inflammation Result Release of leukocytosisinducing factor Leukocytosis (increased numbers of white blood cells in bloodstream) Arterioles dilate Increased capillary permeability Local hyperemia (increased blood flow to area) Capillaries leak fluid (exudate formation) Leaked protein-rich fluid in tissue spaces Heat Redness Locally increased temperature increases metabolic rate of cells Pain Attract neutrophils, monocytes, and lymphocytes to area (chemotaxis) Margination (leukocytes cling to capillary walls) Leaked clotting proteins form interstitial clots that wall off area to prevent injury to surrounding tissue Swelling Possible temporary impairment of function Temporary fibrin patch forms scaffolding for repair Healing © 2013 Pearson Education, Inc. Leukocytes migrate to injured area Diapedesis (leukocytes pass through capillary walls) Phagocytosis of pathogens and dead tissue cells (by neutrophils, short-term; by macrophages, long-term) Pus may form Area cleared of debris
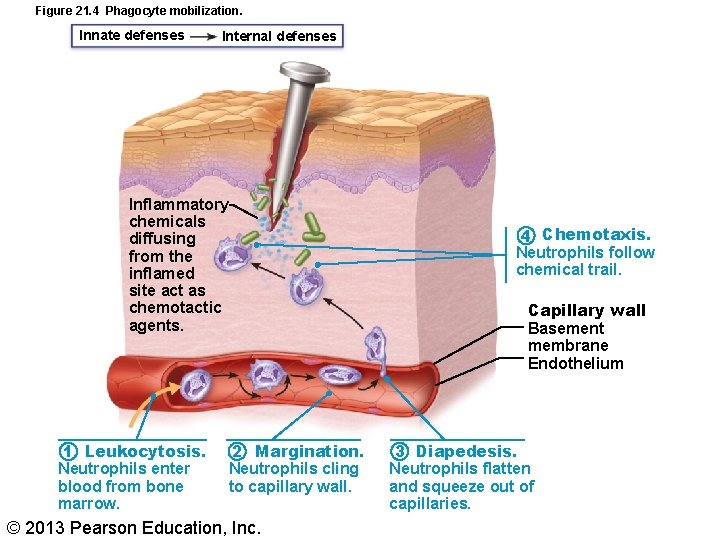
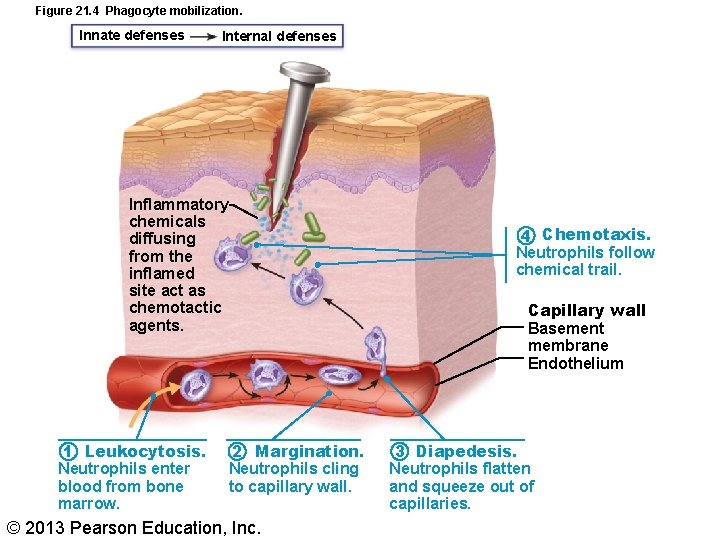
Figure 21. 4 Phagocyte mobilization. Innate defenses Internal defenses Inflammatory chemicals diffusing from the inflamed site act as chemotactic agents. 1 Leukocytosis. Neutrophils enter blood from bone marrow. 2 Margination. Neutrophils cling to capillary wall. © 2013 Pearson Education, Inc. 4 Chemotaxis. Neutrophils follow chemical trail. Capillary wall Basement membrane Endothelium 3 Diapedesis. Neutrophils flatten and squeeze out of capillaries.
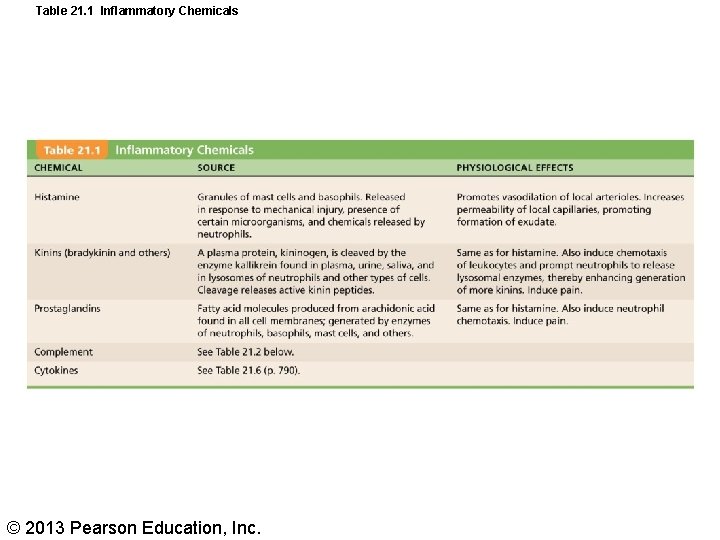
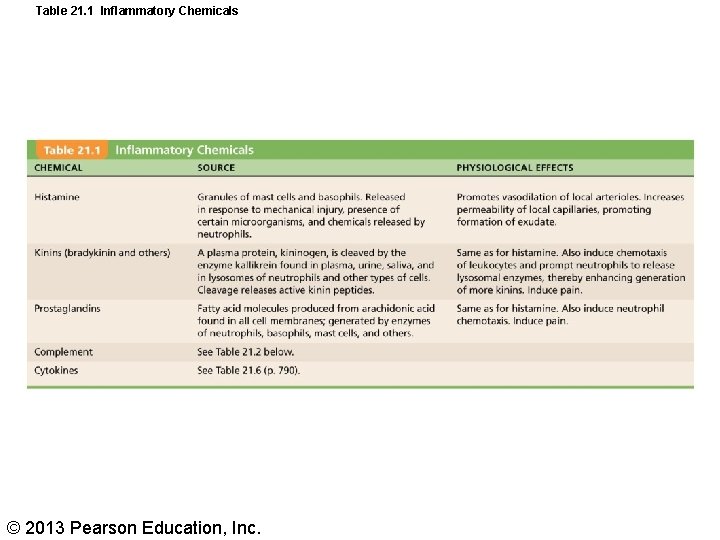
Table 21. 1 Inflammatory Chemicals © 2013 Pearson Education, Inc.
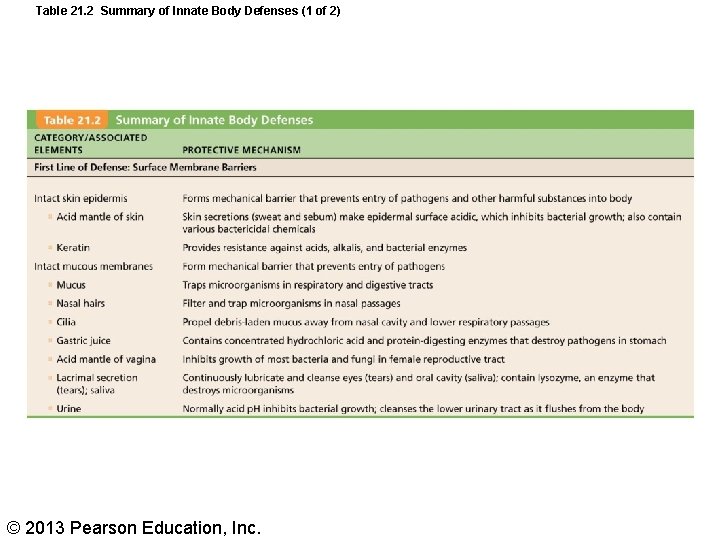
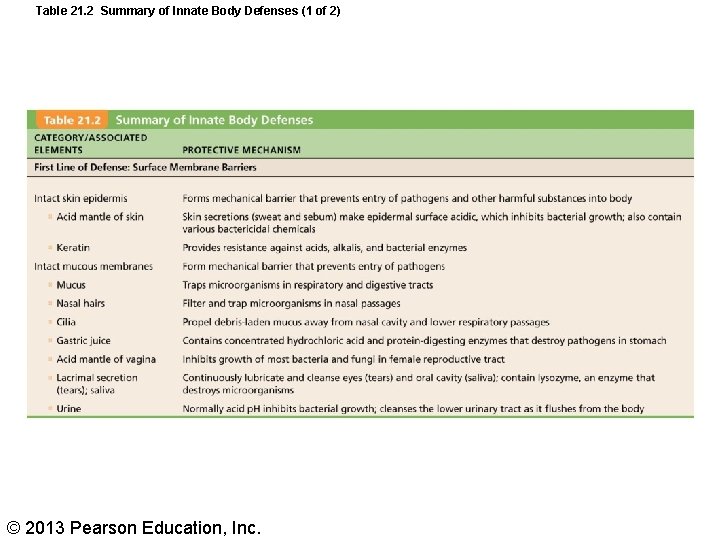
Table 21. 2 Summary of Innate Body Defenses (1 of 2) © 2013 Pearson Education, Inc.
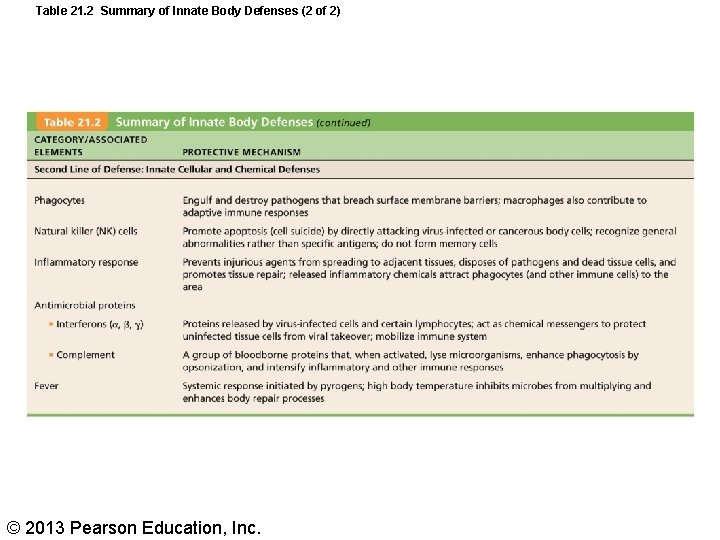
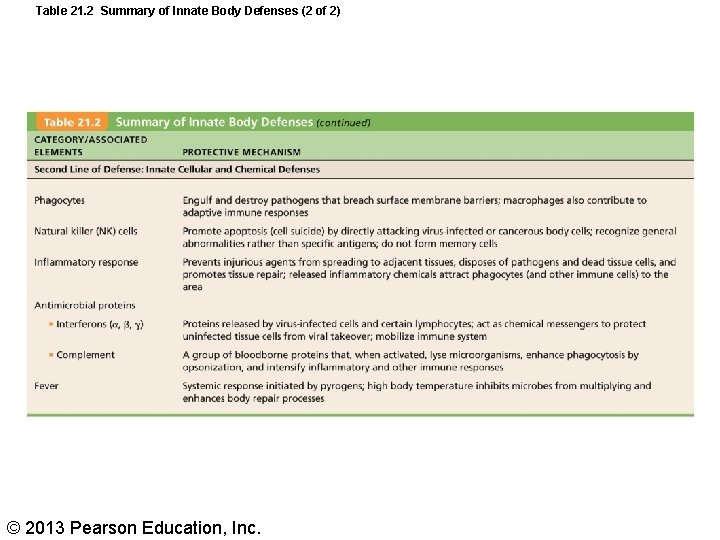
Table 21. 2 Summary of Innate Body Defenses (2 of 2) © 2013 Pearson Education, Inc.
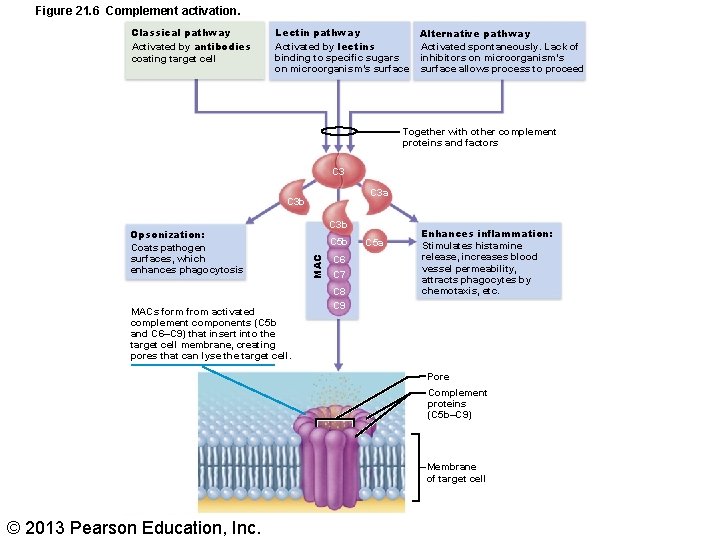
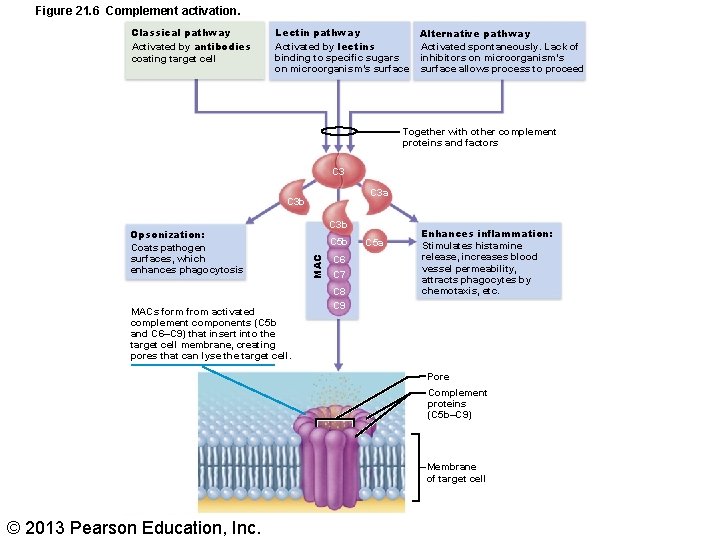
Figure 21. 6 Complement activation. Classical pathway Activated by antibodies coating target cell Lectin pathway Activated by lectins binding to specific sugars on microorganism’s surface Alternative pathway Activated spontaneously. Lack of inhibitors on microorganism’s surface allows process to proceed Together with other complement proteins and factors C 3 a C 3 b MACs form from activated complement components (C 5 b and C 6–C 9) that insert into the target cell membrane, creating pores that can lyse the target cell. C 3 b C 5 b MAC Opsonization: Coats pathogen surfaces, which enhances phagocytosis C 6 C 7 C 8 C 9 C 5 a Enhances inflammation: Stimulates histamine release, increases blood vessel permeability, attracts phagocytes by chemotaxis, etc. Pore Complement proteins (C 5 b–C 9) Membrane of target cell © 2013 Pearson Education, Inc.
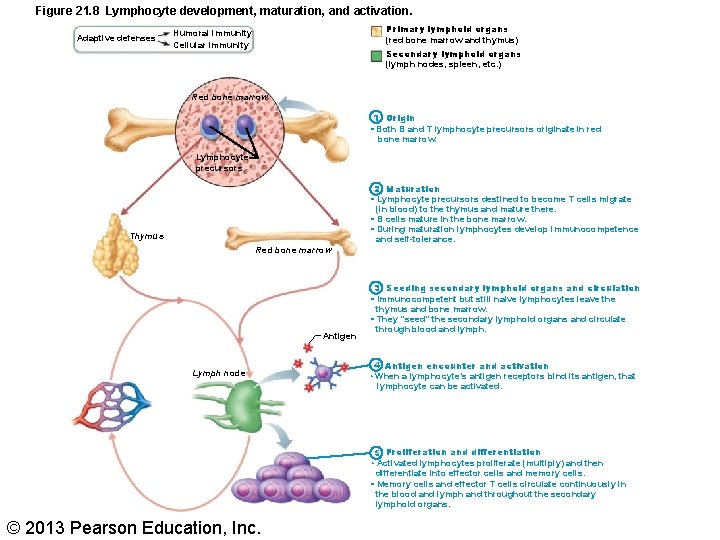
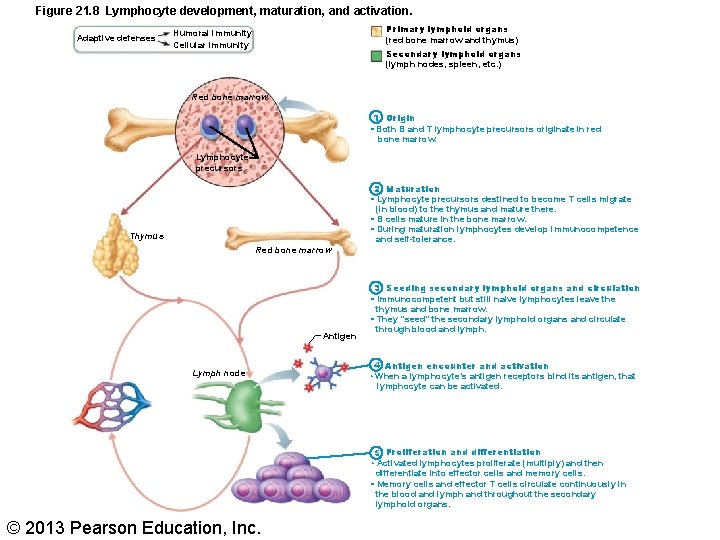
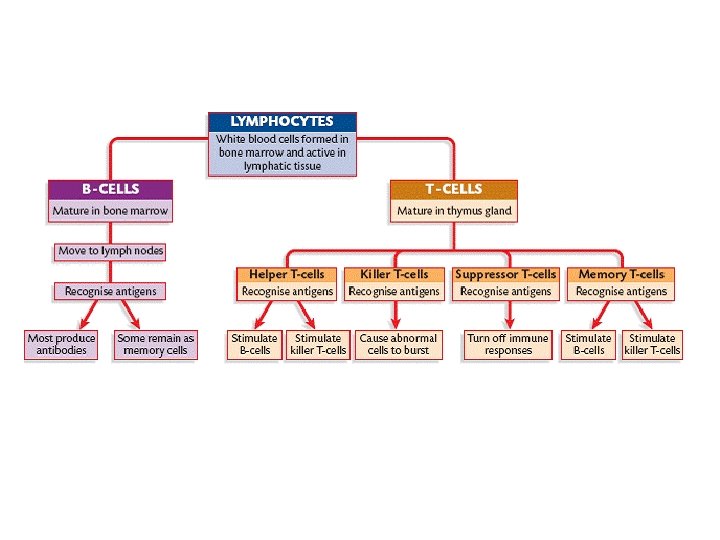
Figure 21. 8 Lymphocyte development, maturation, and activation. Adaptive defenses Primary lymphoid organs (red bone marrow and thymus) Humoral immunity Cellular immunity Secondary lymphoid organs (lymph nodes, spleen, etc. ) Red bone marrow 1 Origin • Both B and T lymphocyte precursors originate in red bone marrow. Lymphocyte precursors 2 Maturation • Lymphocyte precursors destined to become T cells migrate (in blood) to the thymus and mature there. • B cells mature in the bone marrow. • During maturation lymphocytes develop immunocompetence and self-tolerance. Thymus Red bone marrow Antigen Lymph node 3 Seeding secondary lymphoid organs and circulation • Immunocompetent but still naive lymphocytes leave thymus and bone marrow. • They “seed” the secondary lymphoid organs and circulate through blood and lymph. 4 Antigen encounter and activation • When a lymphocyte’s antigen receptors bind its antigen, that lymphocyte can be activated. 5 Proliferation and differentiation • Activated lymphocytes proliferate (multiply) and then differentiate into effector cells and memory cells. • Memory cells and effector T cells circulate continuously in the blood and lymph and throughout the secondary lymphoid organs. © 2013 Pearson Education, Inc.
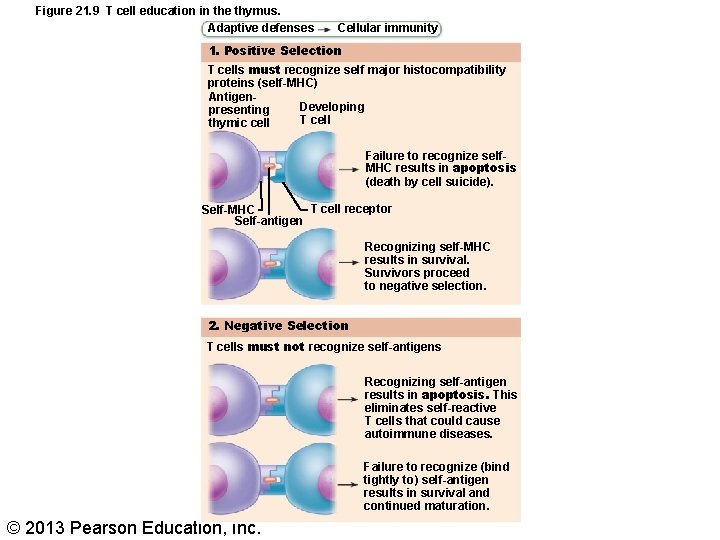
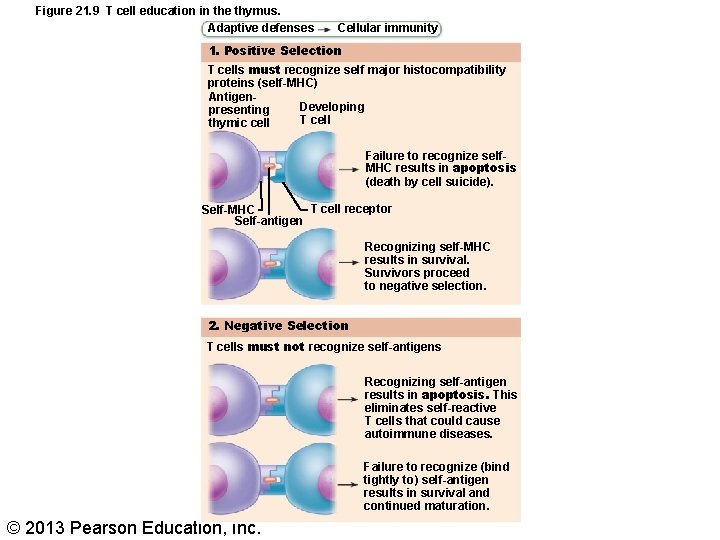
Figure 21. 9 T cell education in the thymus. Adaptive defenses Cellular immunity 1. Positive Selection T cells must recognize self major histocompatibility proteins (self-MHC) Antigen. Developing presenting T cell thymic cell Failure to recognize self. MHC results in apoptosis (death by cell suicide). T cell receptor Self-MHC Self-antigen Recognizing self-MHC results in survival. Survivors proceed to negative selection. 2. Negative Selection T cells must not recognize self-antigens Recognizing self-antigen results in apoptosis. This eliminates self-reactive T cells that could cause autoimmune diseases. Failure to recognize (bind tightly to) self-antigen results in survival and continued maturation. © 2013 Pearson Education, Inc.
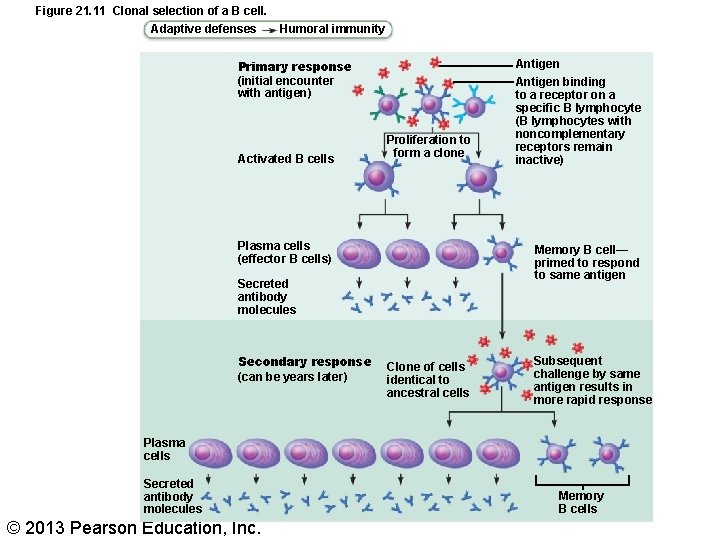
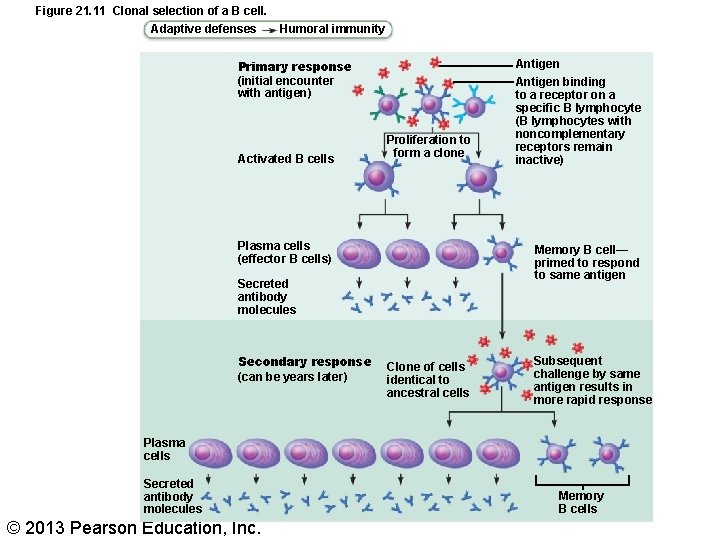
Figure 21. 11 Clonal selection of a B cell. Adaptive defenses Humoral immunity Primary response (initial encounter with antigen) Activated B cells Proliferation to form a clone Plasma cells (effector B cells) Memory B cell— primed to respond to same antigen Secreted antibody molecules Secondary response (can be years later) Antigen binding to a receptor on a specific B lymphocyte (B lymphocytes with noncomplementary receptors remain inactive) Clone of cells identical to ancestral cells Subsequent challenge by same antigen results in more rapid response Plasma cells Secreted antibody molecules © 2013 Pearson Education, Inc. Memory B cells
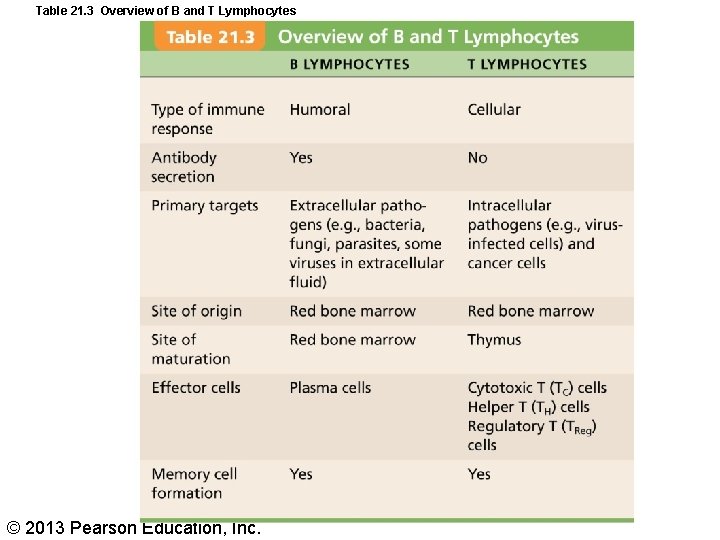
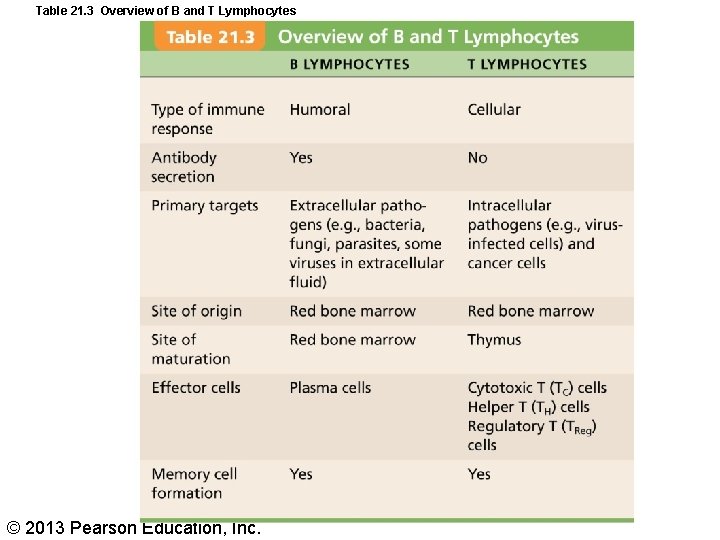
Table 21. 3 Overview of B and T Lymphocytes © 2013 Pearson Education, Inc.
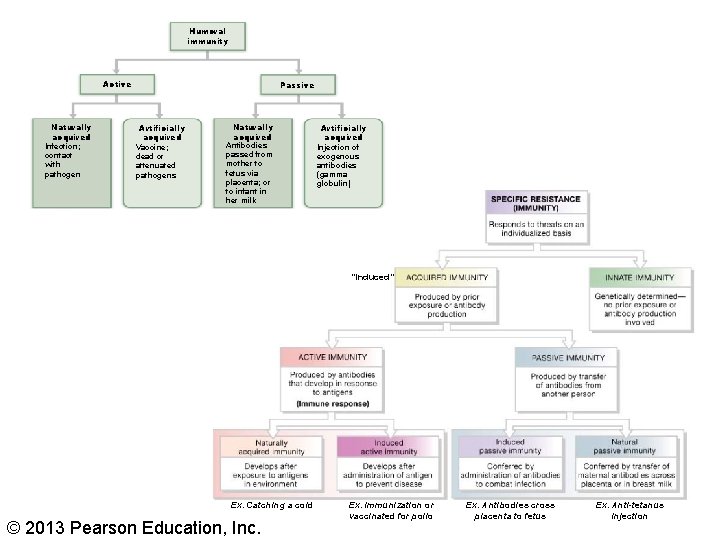
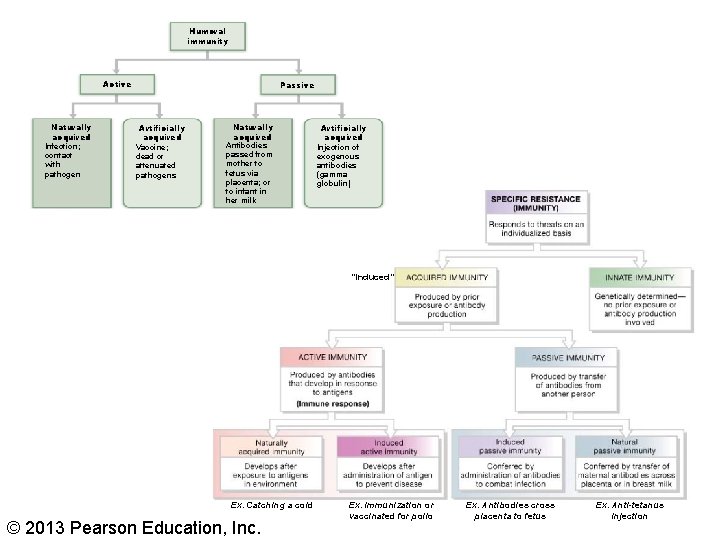
Humoral immunity Active Naturally acquired Infection; contact with pathogen Passive Artificially acquired Vaccine; dead or attenuated pathogens Naturally acquired Antibodies passed from mother to fetus via placenta; or to infant in her milk Artificially acquired Injection of exogenous antibodies (gamma globulin) “Induced” Ex. Catching a cold © 2013 Pearson Education, Inc. Ex. Immunization or vaccinated for polio Ex. Antibodies cross placenta to fetus Ex. Anti-tetanus injection
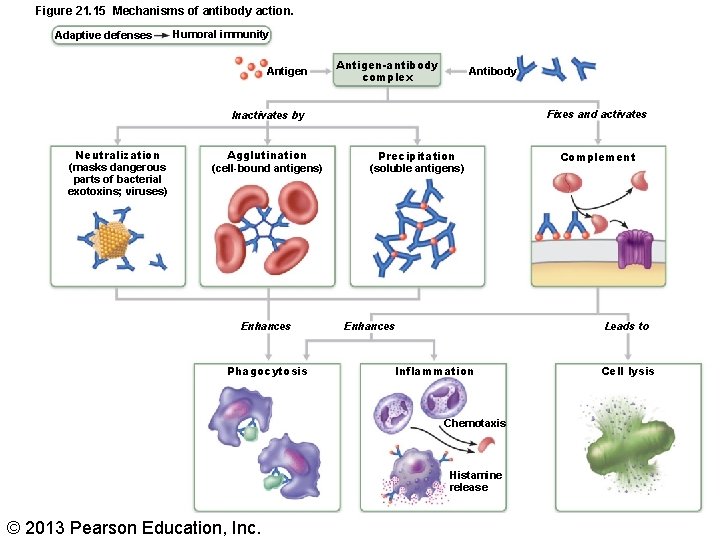
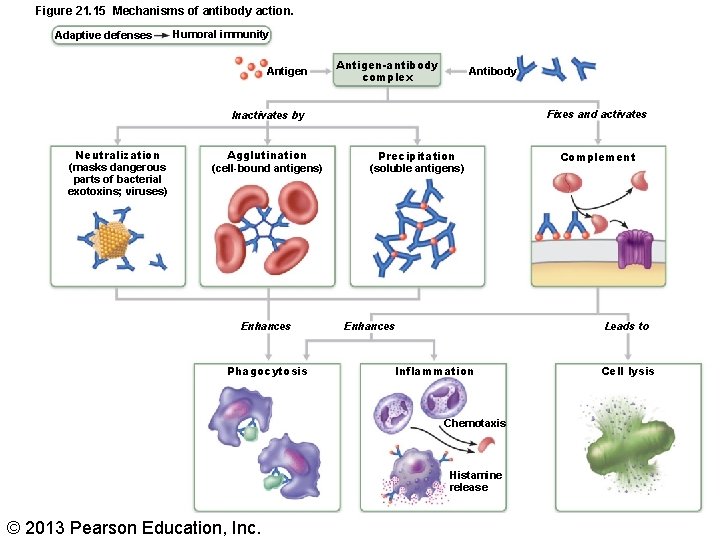
Figure 21. 15 Mechanisms of antibody action. Adaptive defenses Humoral immunity Antigen-antibody complex Antibody Fixes and activates Inactivates by Neutralization (masks dangerous parts of bacterial exotoxins; viruses) Agglutination (cell-bound antigens) Enhances Phagocytosis Precipitation (soluble antigens) Leads to Enhances Inflammation Chemotaxis Histamine release © 2013 Pearson Education, Inc. Complement Cell lysis
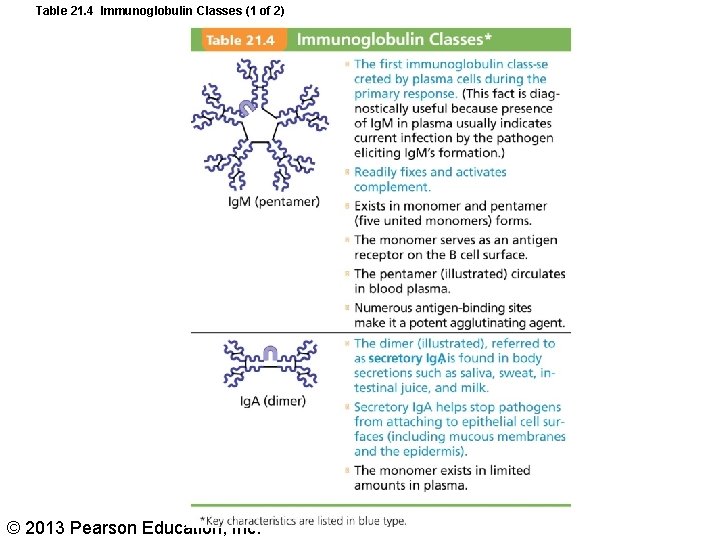
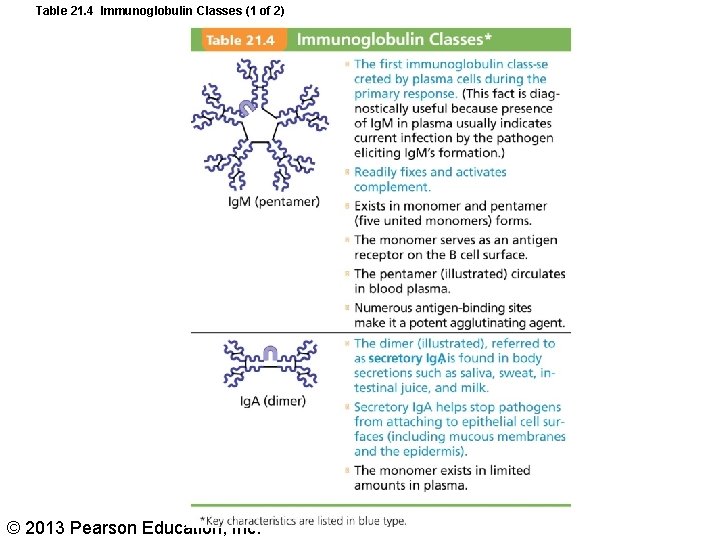
Table 21. 4 Immunoglobulin Classes (1 of 2) © 2013 Pearson Education, Inc.
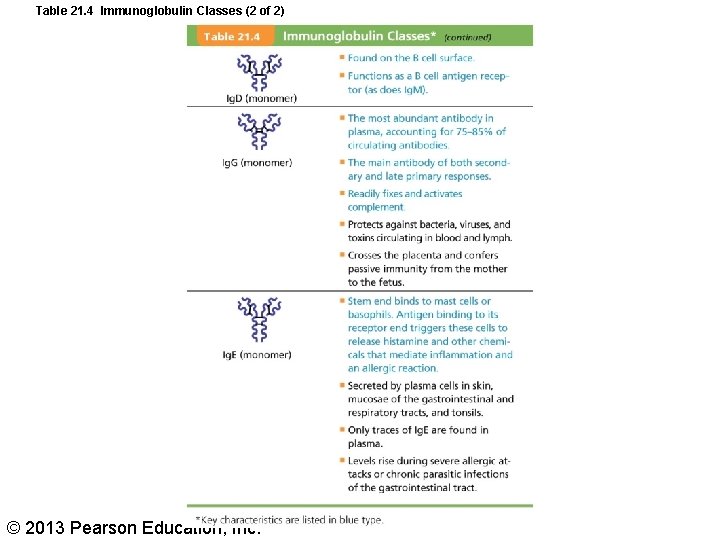
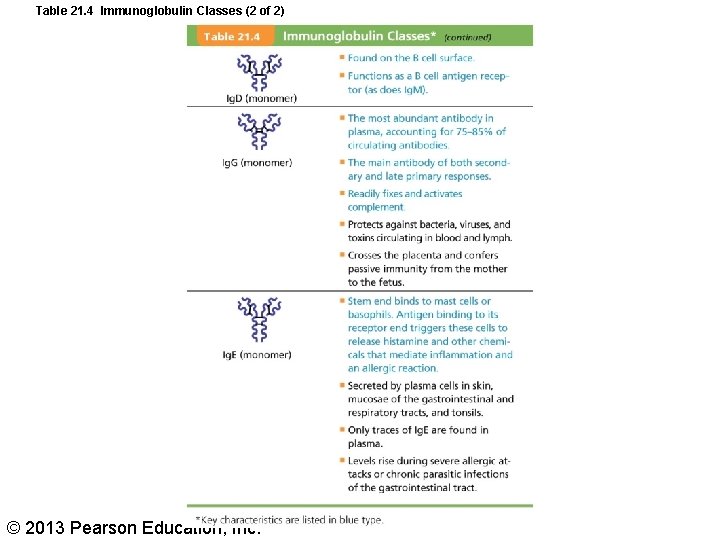
Table 21. 4 Immunoglobulin Classes (2 of 2) © 2013 Pearson Education, Inc.
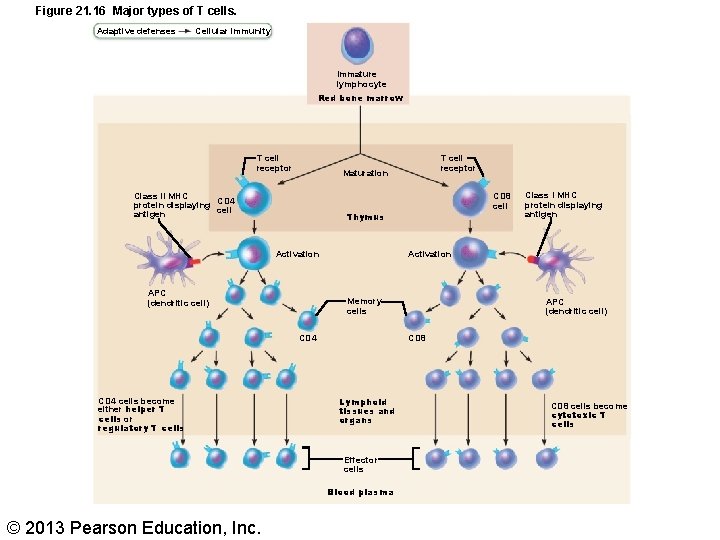
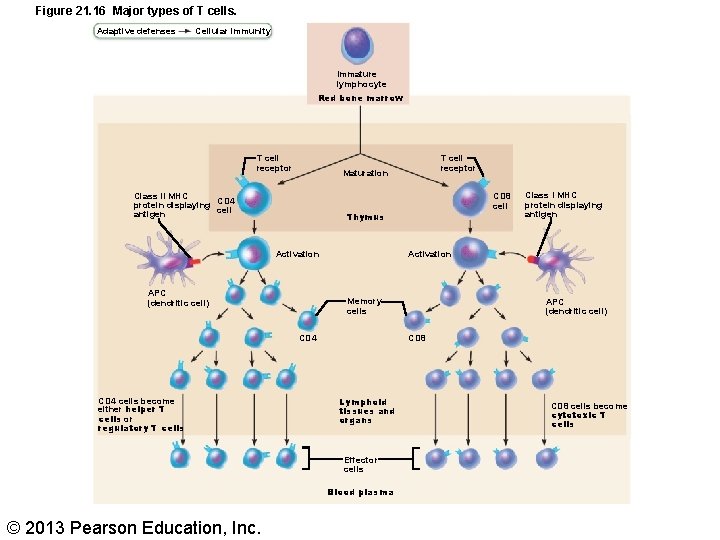
Figure 21. 16 Major types of T cells. Adaptive defenses Cellular immunity Immature lymphocyte Red bone marrow T cell receptor Maturation Class II MHC protein displaying CD 4 cell antigen APC (dendritic cell) Class I MHC protein displaying antigen Activation Memory cells CD 4 APC (dendritic cell) CD 8 Lymphoid tissues and organs Effector cells Blood plasma © 2013 Pearson Education, Inc. CD 8 cell Thymus Activation CD 4 cells become either helper T cells or regulatory T cells T cell receptor CD 8 cells become cytotoxic T cells
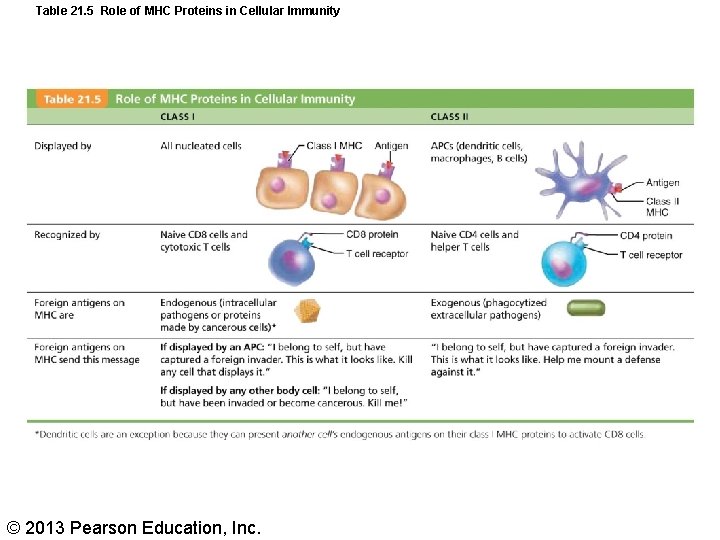
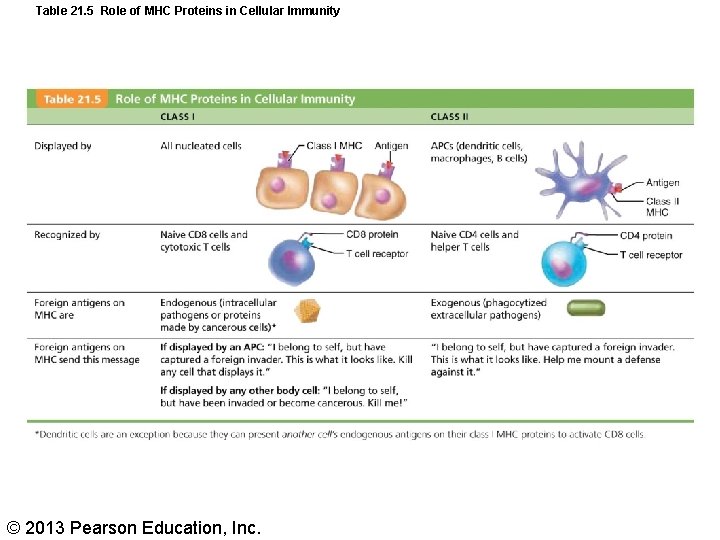
Table 21. 5 Role of MHC Proteins in Cellular Immunity © 2013 Pearson Education, Inc.
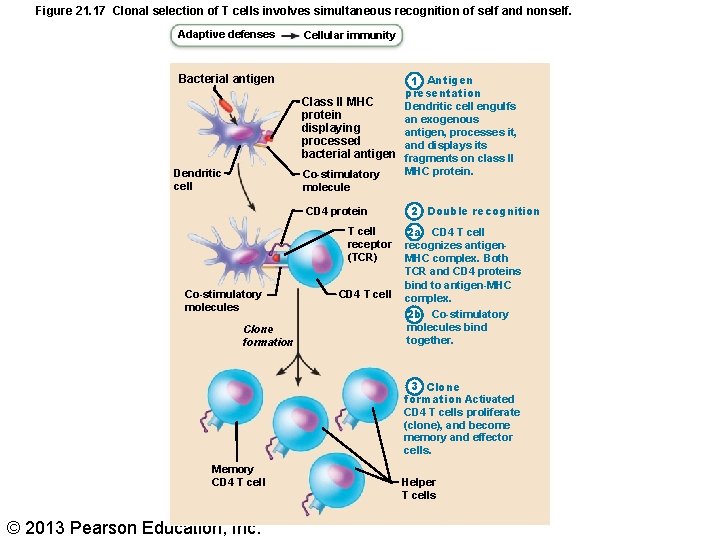
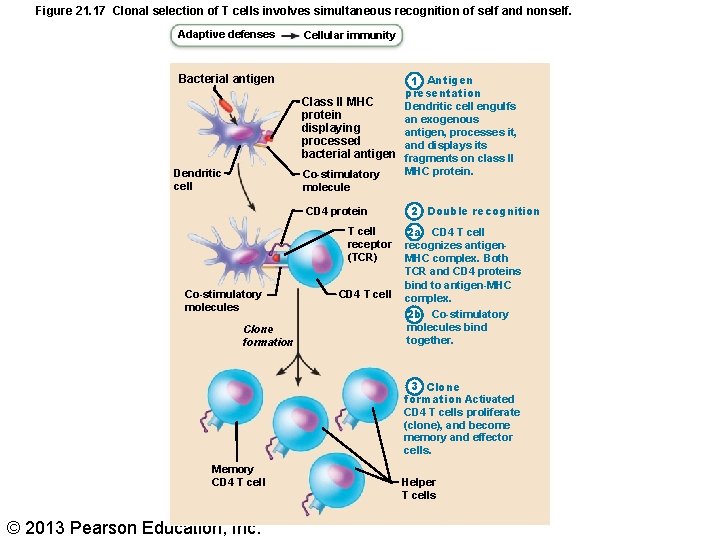
Figure 21. 17 Clonal selection of T cells involves simultaneous recognition of self and nonself. Adaptive defenses Cellular immunity Bacterial antigen 1 Antigen presentation Class l. I MHC Dendritic cell engulfs protein an exogenous displaying antigen, processes it, processed and displays its bacterial antigen fragments on class II MHC protein. Co-stimulatory molecule Dendritic cell CD 4 protein T cell receptor (TCR) Co-stimulatory molecules Clone formation CD 4 T cell 2 Double recognition 2 a CD 4 T cell recognizes antigen. MHC complex. Both TCR and CD 4 proteins bind to antigen-MHC complex. 2 b Co-stimulatory molecules bind together. 3 Clone formation Activated CD 4 T cells proliferate (clone), and become memory and effector cells. Memory CD 4 T cell © 2013 Pearson Education, Inc. Helper T cells
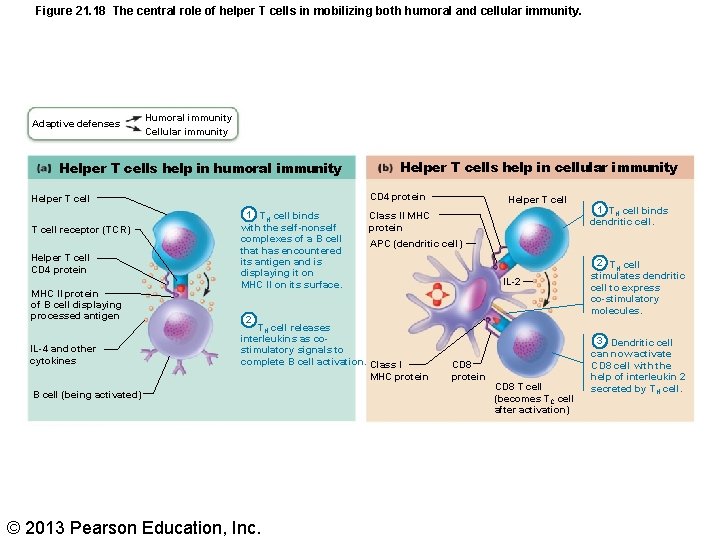
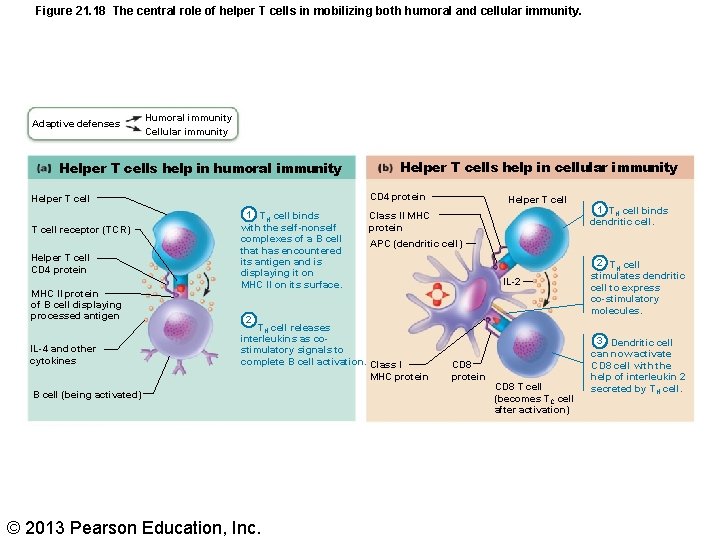
Figure 21. 18 The central role of helper T cells in mobilizing both humoral and cellular immunity. Adaptive defenses Humoral immunity Cellular immunity Helper T cells help in humoral immunity CD 4 protein Helper T cell receptor (TCR) Helper T cell CD 4 protein MHC II protein of B cell displaying processed antigen IL-4 and other cytokines Helper T cells help in cellular immunity 1 TH cell binds with the self-nonself complexes of a B cell that has encountered its antigen and is displaying it on MHC II on its surface. Helper T cell Class II MHC protein APC (dendritic cell) IL-2 2 TH cell releases interleukins as costimulatory signals to complete B cell activation. Class I MHC protein B cell (being activated) © 2013 Pearson Education, Inc. 1 TH cell binds dendritic cell. CD 8 protein CD 8 T cell (becomes TC cell after activation) 2 TH cell stimulates dendritic cell to express co-stimulatory molecules. 3 Dendritic cell can now activate CD 8 cell with the help of interleukin 2 secreted by TH cell.
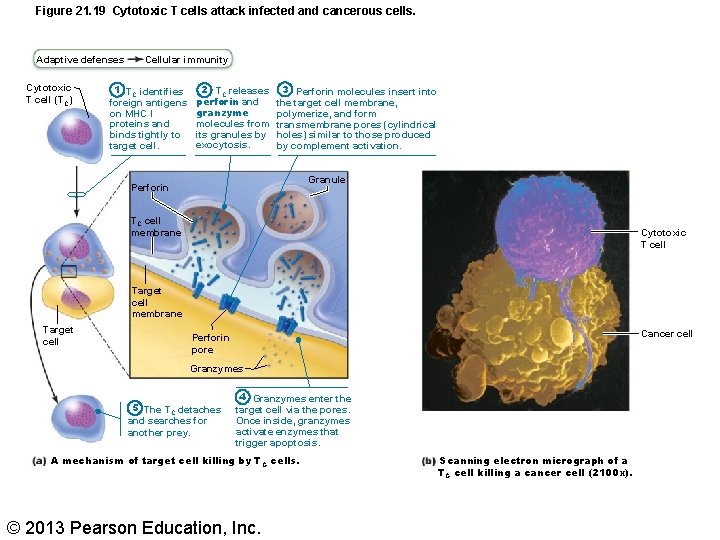
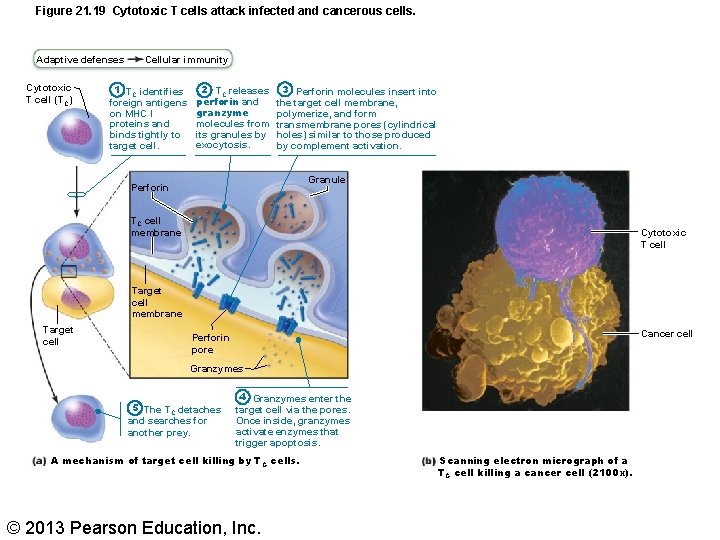
Figure 21. 19 Cytotoxic T cells attack infected and cancerous cells. Adaptive defenses Cytotoxic T cell (TC) Cellular immunity 1 TC identifies foreign antigens on MHC I proteins and binds tightly to target cell. 2 TC releases perforin and granzyme molecules from its granules by exocytosis. 3 Perforin molecules insert into the target cell membrane, polymerize, and form transmembrane pores (cylindrical holes) similar to those produced by complement activation. Granule Perforin TC cell membrane Cytotoxic T cell Target cell membrane Target cell Cancer cell Perforin pore Granzymes 5 The TC detaches and searches for another prey. 4 Granzymes enter the target cell via the pores. Once inside, granzymes activate enzymes that trigger apoptosis. A mechanism of target cell killing by T C cells. © 2013 Pearson Education, Inc. Scanning electron micrograph of a TC cell killing a cancer cell (2100 x).
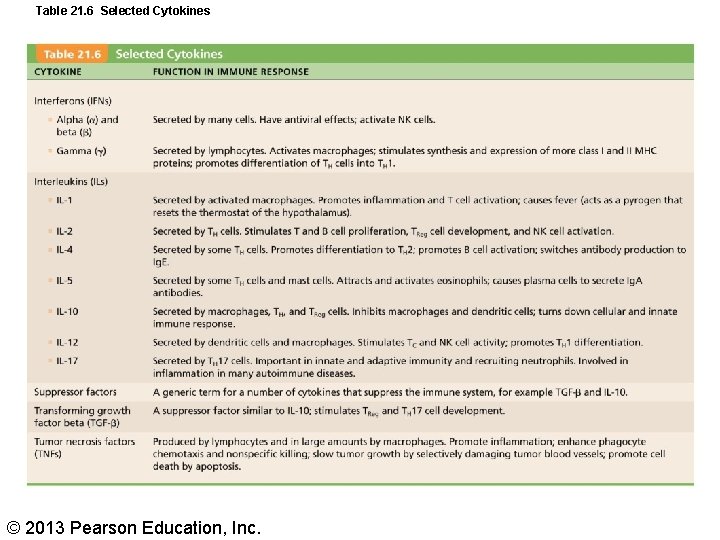
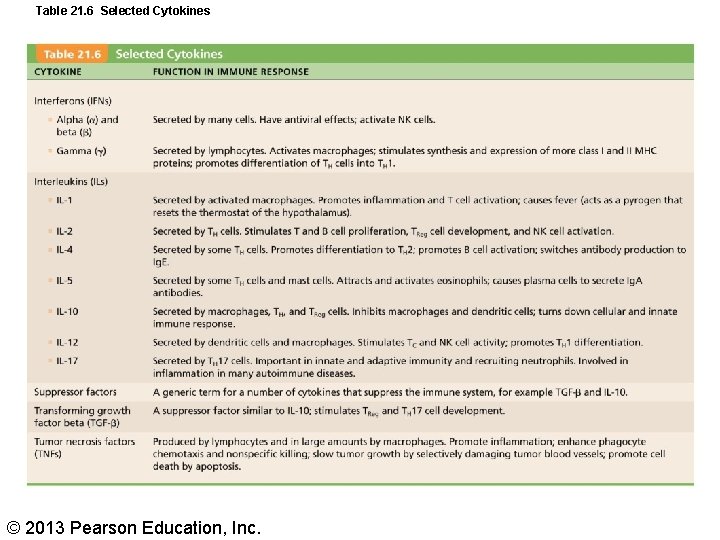
Table 21. 6 Selected Cytokines © 2013 Pearson Education, Inc.
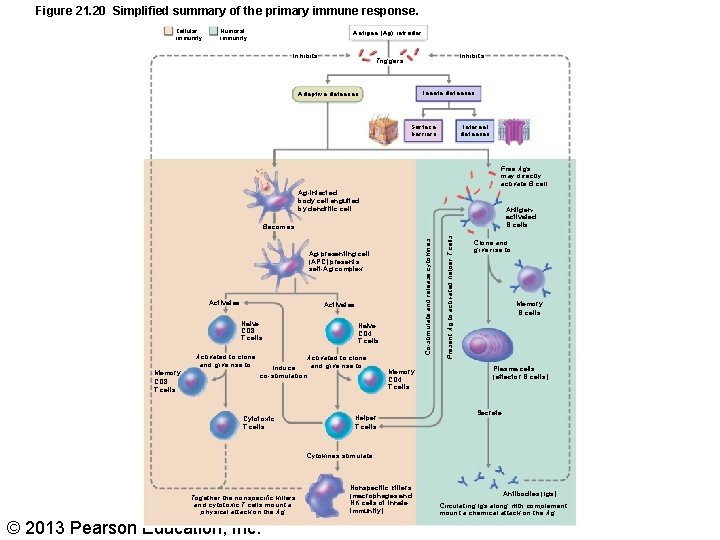
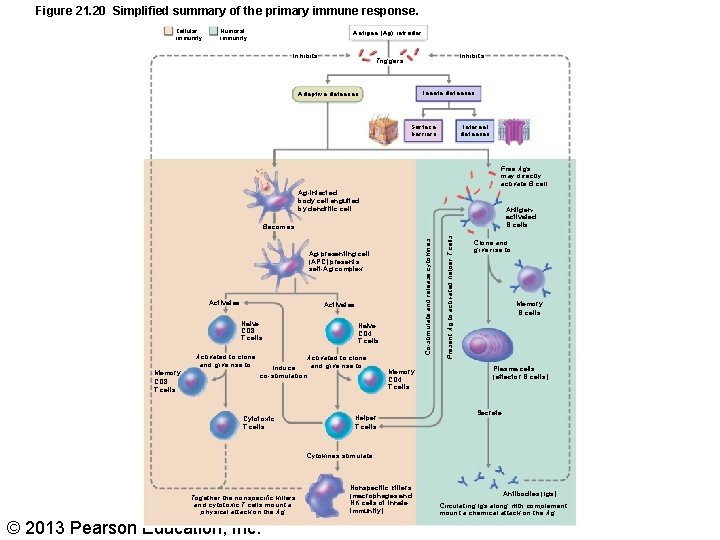
Figure 21. 20 Simplified summary of the primary immune response. Cellular immunity Humoral immunity Antigen (Ag) intruder Inhibits Triggers Innate defenses Adaptive defenses Internal defenses Surface barriers Free Ags may directly activate B cell Ag-infected body cell engulfed by dendritic cell Antigenactivated B cells Ag-presenting cell (APC) presents self-Ag complex Activates Naive CD 8 T cells Activated to clone and give rise to Memory CD 8 T cells Naive CD 4 T cells Activated to clone and give rise to Induce co-stimulation Cytotoxic T cells Memory CD 4 T cells Helper T cells Present Ag to activated helper T cells Co-stimulate and release cytokines Becomes Clone and give rise to Memory B cells Plasma cells (effector B cells) Secrete Cytokines stimulate Together the nonspecific killers and cytotoxic T cells mount a physical attack on the Ag © 2013 Pearson Education, Inc. Nonspecific killers (macrophages and NK cells of innate immunity) Antibodies (Igs) Circulating lgs along with complement mount a chemical attack on the Ag
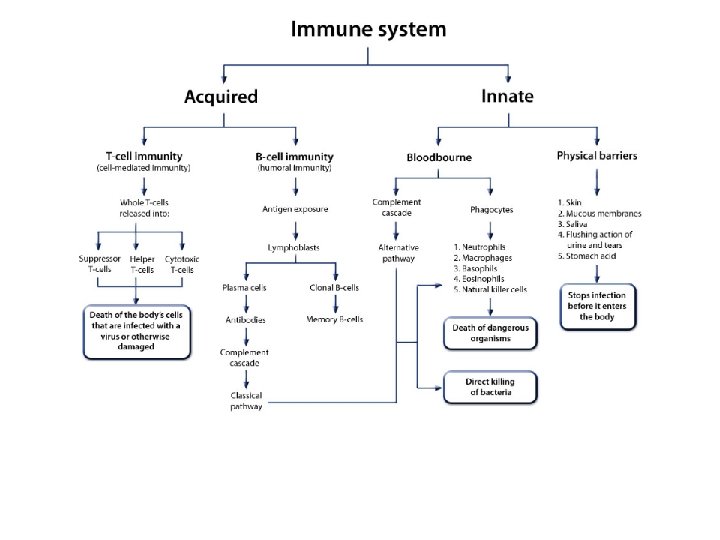
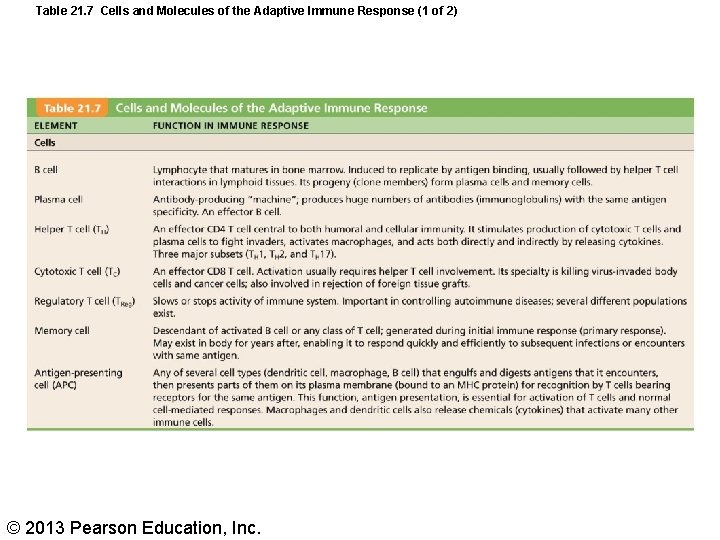
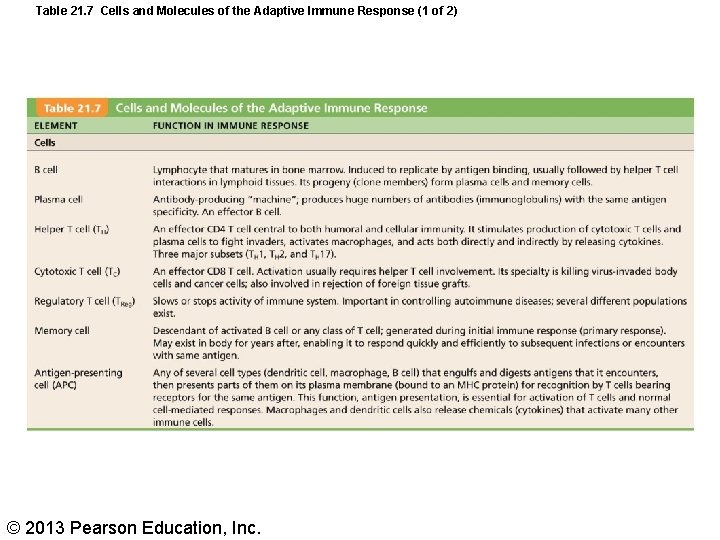
Table 21. 7 Cells and Molecules of the Adaptive Immune Response (1 of 2) © 2013 Pearson Education, Inc.
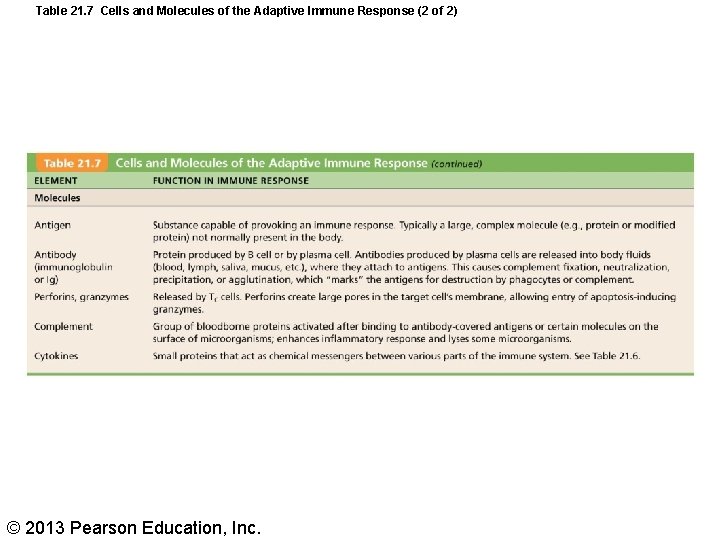
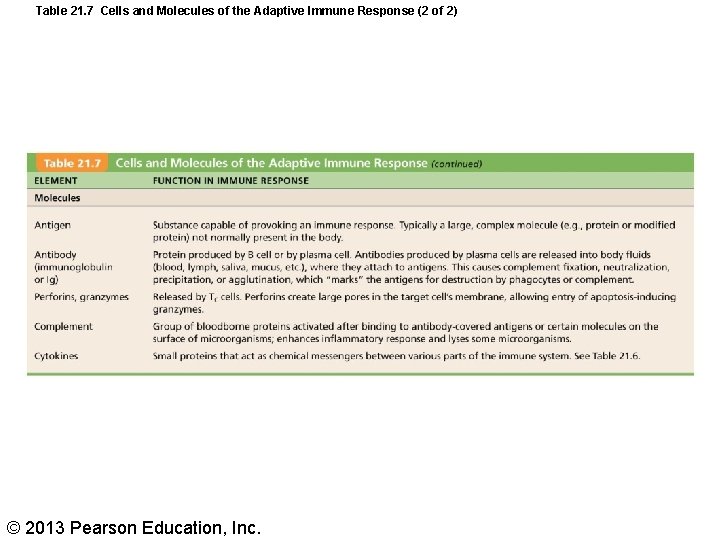
Table 21. 7 Cells and Molecules of the Adaptive Immune Response (2 of 2) © 2013 Pearson Education, Inc.
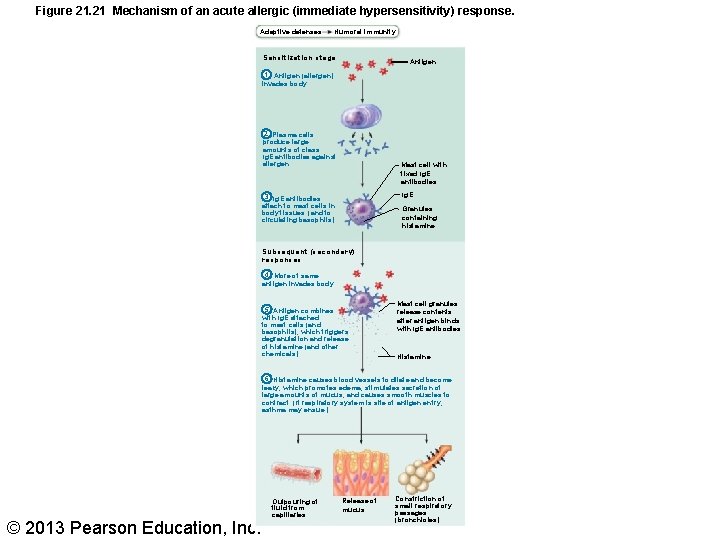
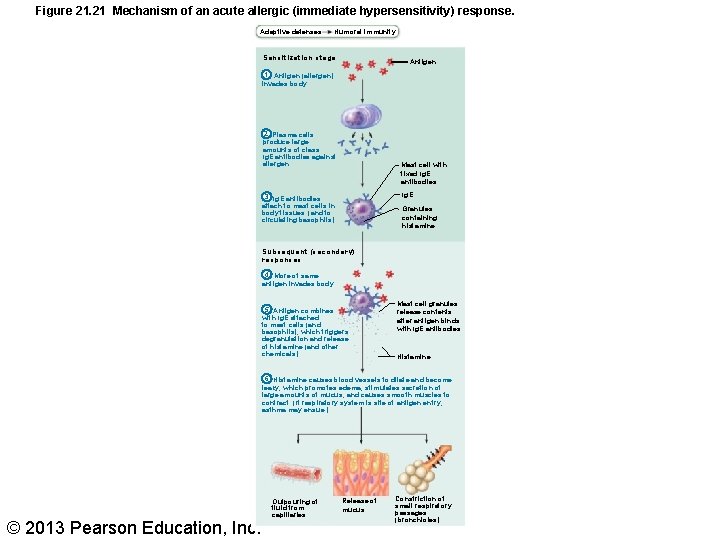
Figure 21. 21 Mechanism of an acute allergic (immediate hypersensitivity) response. Adaptive defenses Humoral immunity Sensitization stage Antigen 1 Antigen (allergen) invades body. 2 Plasma cells produce large amounts of class Ig. E antibodies against allergen. Mast cell with fixed Ig. E antibodies Ig. E 3 Ig. E antibodies attach to mast cells in body tissues (and to circulating basophils). Granules containing histamine Subsequent (secondary) responses 4 More of same antigen invades body. 5 Antigen combines with Ig. E attached to mast cells (and basophils), which triggers degranulation and release of histamine (and other chemicals). Mast cell granules release contents after antigen binds with Ig. E antibodies Histamine 6 Histamine causes blood vessels to dilate and become leaky, which promotes edema; stimulates secretion of large amounts of mucus; and causes smooth muscles to contract. (If respiratory system is site of antigen entry, asthma may ensue. ) © 2013 Pearson Education, Inc. Outpouring of fluid from capillaries Release of mucus Constriction of small respiratory passages (bronchioles)