Figure 17 17 An electrocardiogram ECG tracing Sinoatrial
- Slides: 23
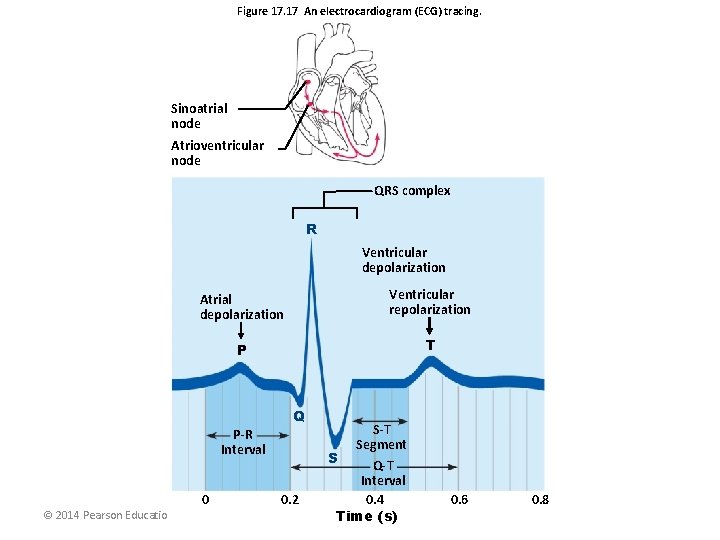
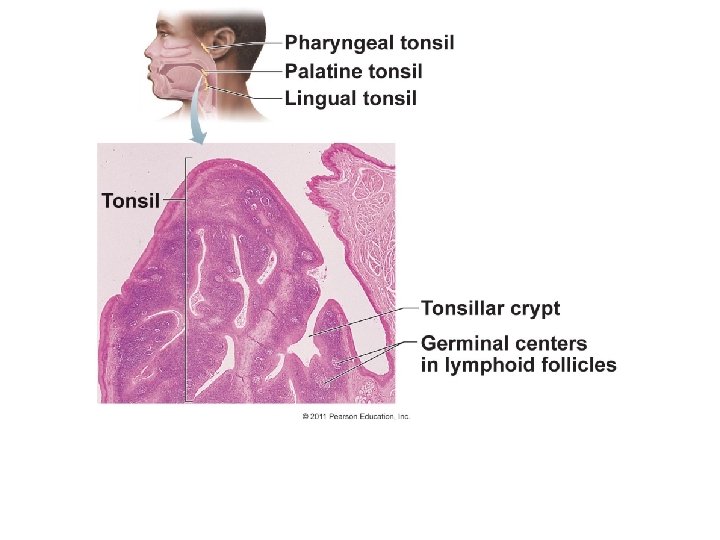
Figure 17. 17 An electrocardiogram (ECG) tracing. Sinoatrial node Atrioventricular node QRS complex R Ventricular depolarization Atrial depolarization Ventricular repolarization P T Q P-R Interval © 2014 Pearson Education, Inc. 0 S 0. 2 S-T Segment Q-T Interval 0. 4 Time (s) 0. 6 0. 8
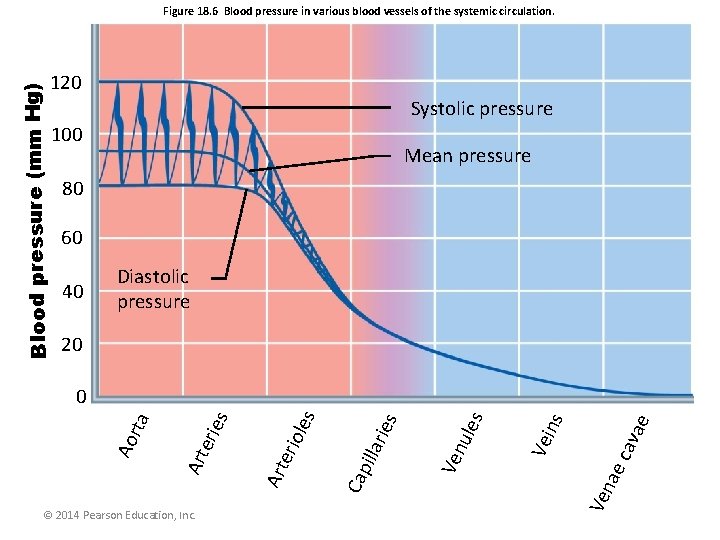
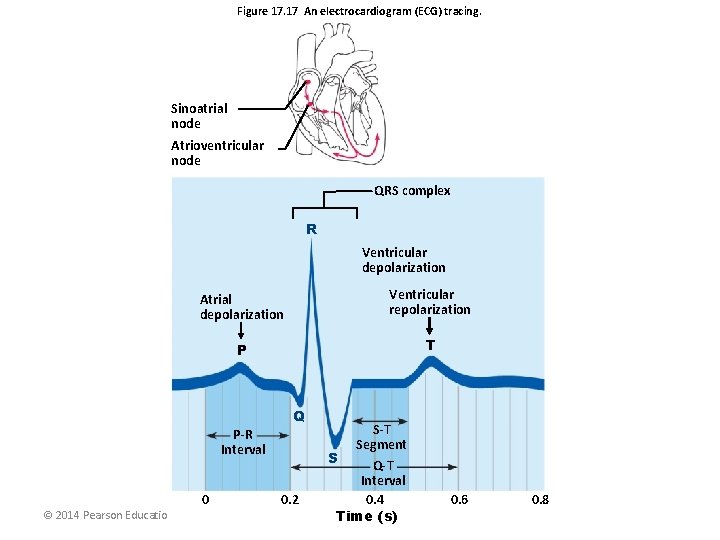
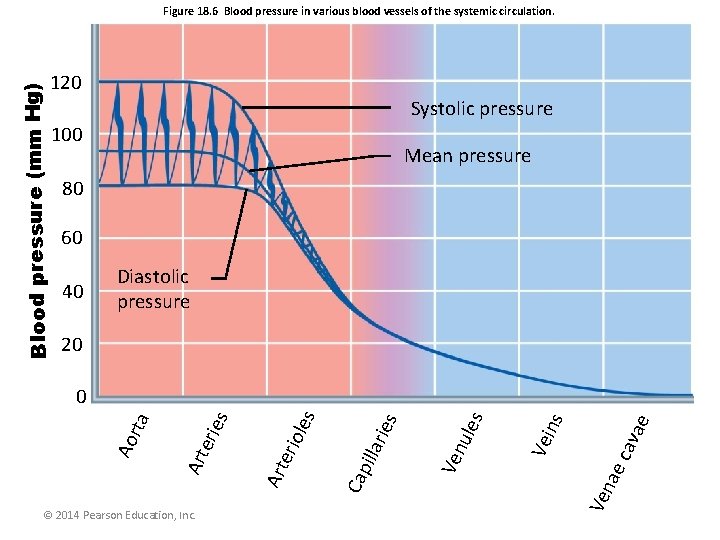
Figure 18. 6 Blood pressure in various blood vessels of the systemic circulation. Blood pressure (mm Hg) 120 Systolic pressure 100 Mean pressure 80 60 40 Diastolic pressure 20 ava e ec ns Vei s ule Ven ies llar les erio Cap i Ven a © 2014 Pearson Education, Inc. Art erie s Art Ao rta 0
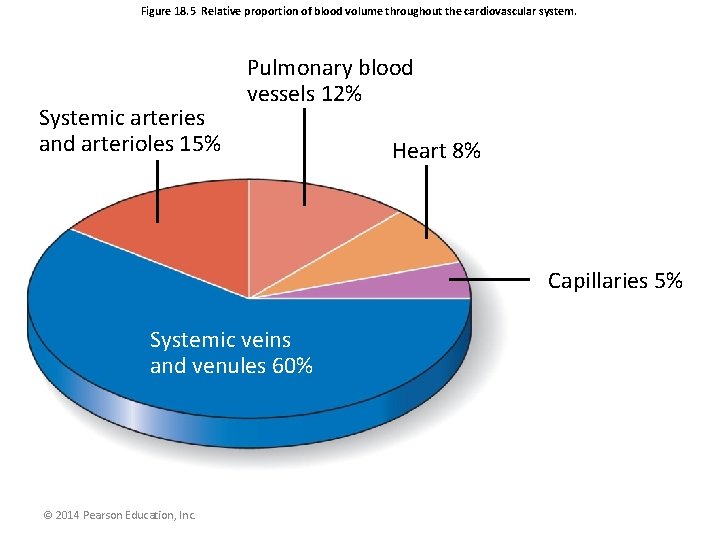
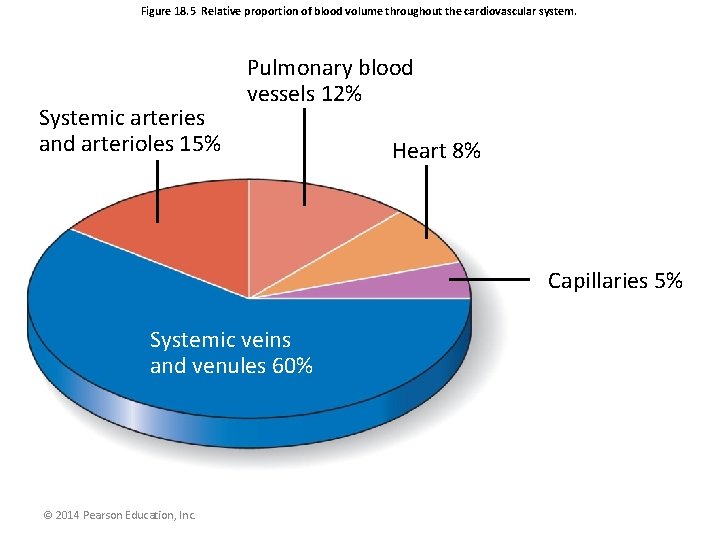
Figure 18. 5 Relative proportion of blood volume throughout the cardiovascular system. Systemic arteries and arterioles 15% Pulmonary blood vessels 12% Heart 8% Capillaries 5% Systemic veins and venules 60% © 2014 Pearson Education, Inc.
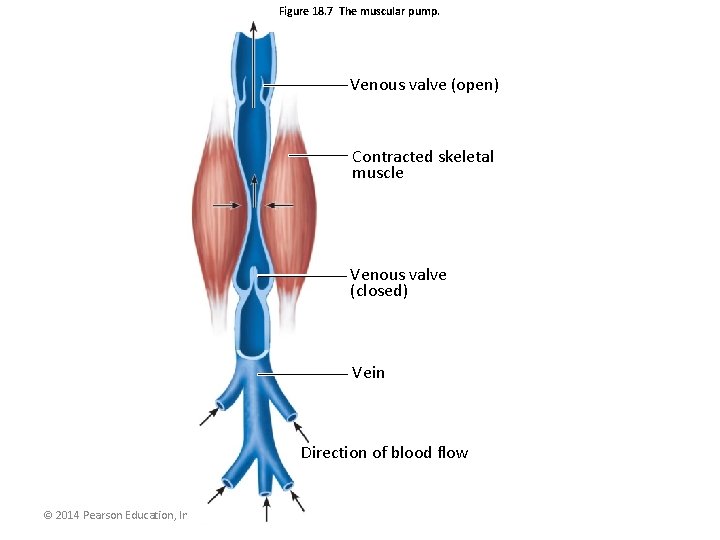
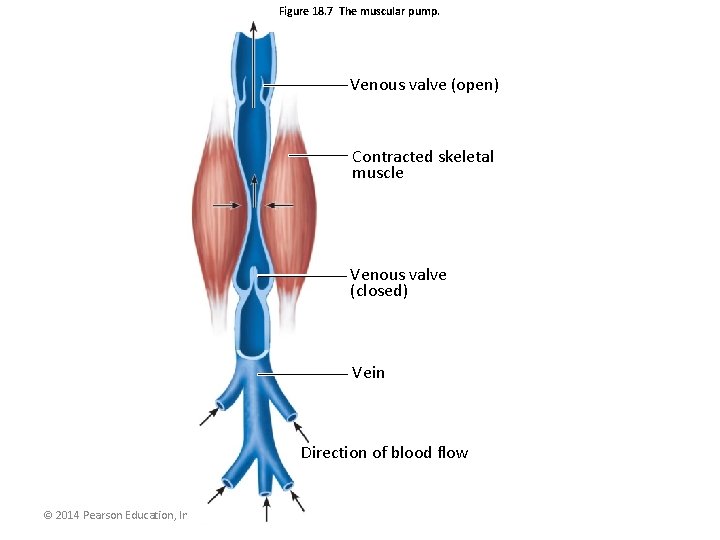
Figure 18. 7 The muscular pump. Venous valve (open) Contracted skeletal muscle Venous valve (closed) Vein Direction of blood flow © 2014 Pearson Education, Inc.
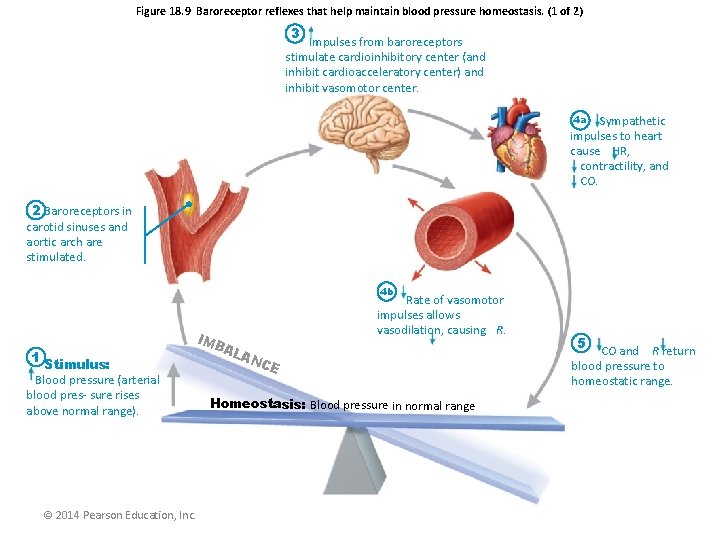
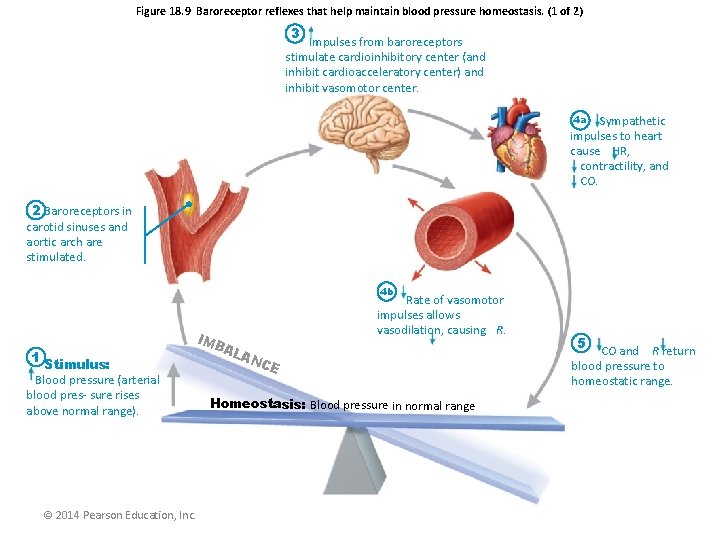
Figure 18. 9 Baroreceptor reflexes that help maintain blood pressure homeostasis. (1 of 2) 3 Impulses from baroreceptors stimulate cardioinhibitory center (and inhibit cardioacceleratory center) and inhibit vasomotor center. 4 a Sympathetic impulses to heart cause HR, contractility, and CO. 2 Baroreceptors in carotid sinuses and aortic arch are stimulated. 4 b IMB Rate of vasomotor impulses allows vasodilation, causing R. 1 Stimulus: Blood pressure (arterial blood pres- sure rises above normal range). © 2014 Pearson Education, Inc. AL AN CE Homeostasis: Blood pressure in normal range 5 CO and R return blood pressure to homeostatic range.
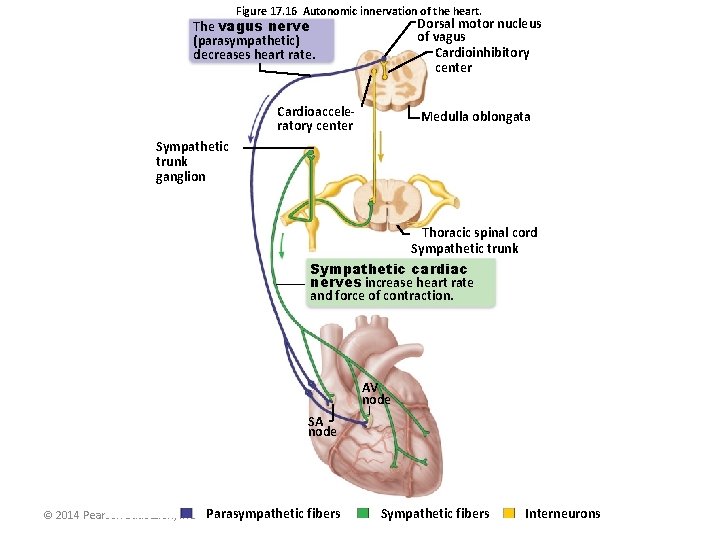
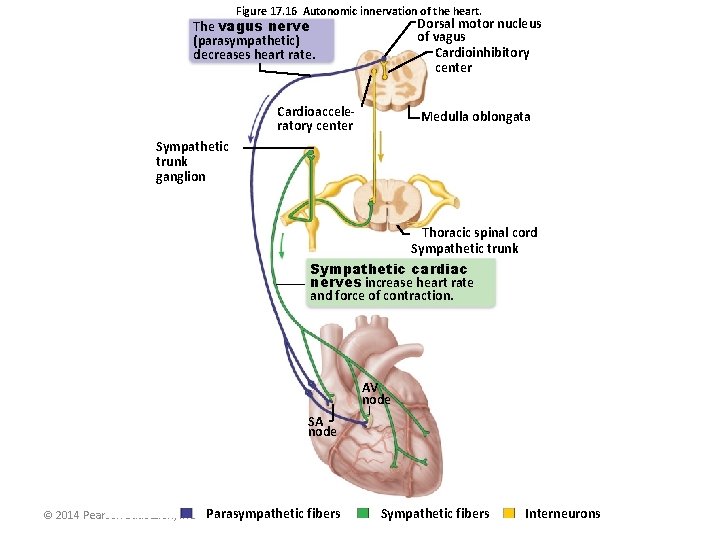
Figure 17. 16 Autonomic innervation of the heart. Dorsal motor nucleus of vagus Cardioinhibitory center The vagus nerve (parasympathetic) decreases heart rate. Cardioacceleratory center Medulla oblongata Sympathetic trunk ganglion Thoracic spinal cord Sympathetic trunk Sympathetic cardiac nerves increase heart rate and force of contraction. AV node SA node © 2014 Pearson Education, Inc. Parasympathetic fibers Sympathetic fibers Interneurons
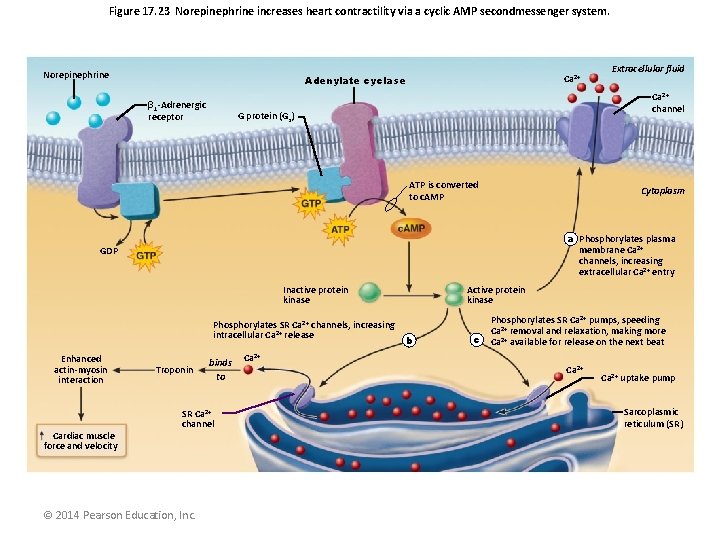
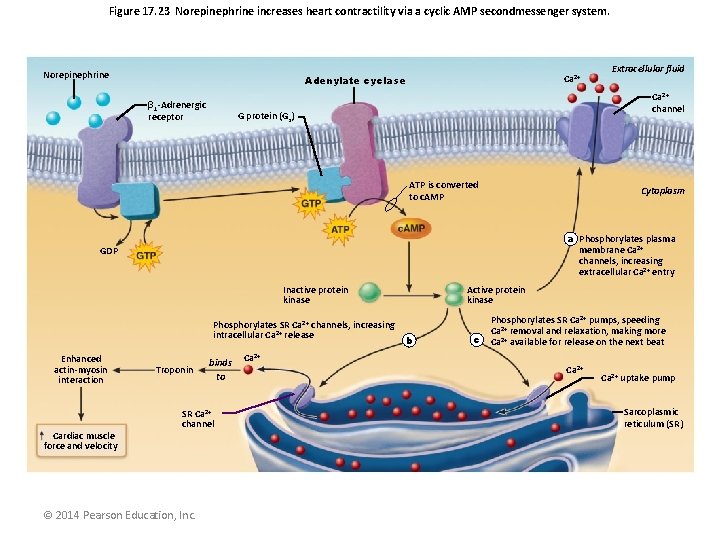
Figure 17. 23 Norepinephrine increases heart contractility via a cyclic AMP secondmessenger system. Norepinephrine Ca 2+ Adenylate cyclase β 1 -Adrenergic receptor Ca 2+ channel G protein (Gs) ATP is converted to c. AMP Cytoplasm a Phosphorylates plasma membrane Ca 2+ channels, increasing extracellular Ca 2+ entry GDP Inactive protein kinase Phosphorylates SR Ca 2+ channels, increasing intracellular Ca 2+ release Enhanced actin-myosin interaction Cardiac muscle force and velocity Extracellular fluid Troponin binds to SR Ca 2+ channel © 2014 Pearson Education, Inc. Ca 2+ Active protein kinase b c Phosphorylates SR Ca 2+ pumps, speeding Ca 2+ removal and relaxation, making more Ca 2+ available for release on the next beat Ca 2+ uptake pump Sarcoplasmic reticulum (SR)
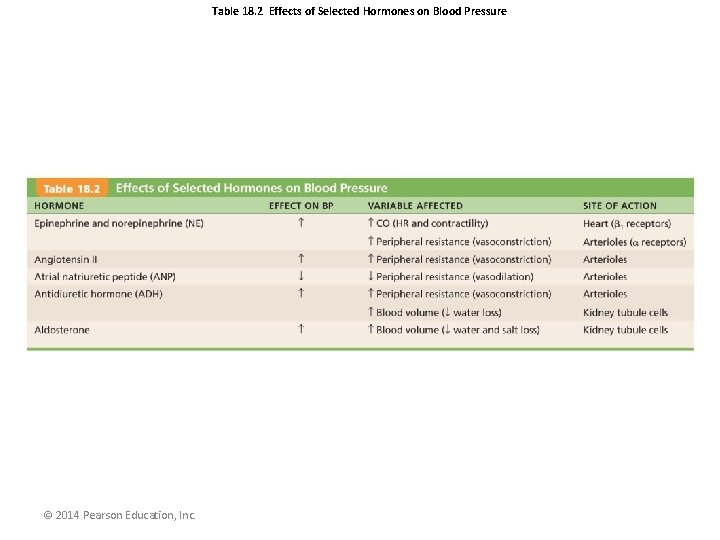
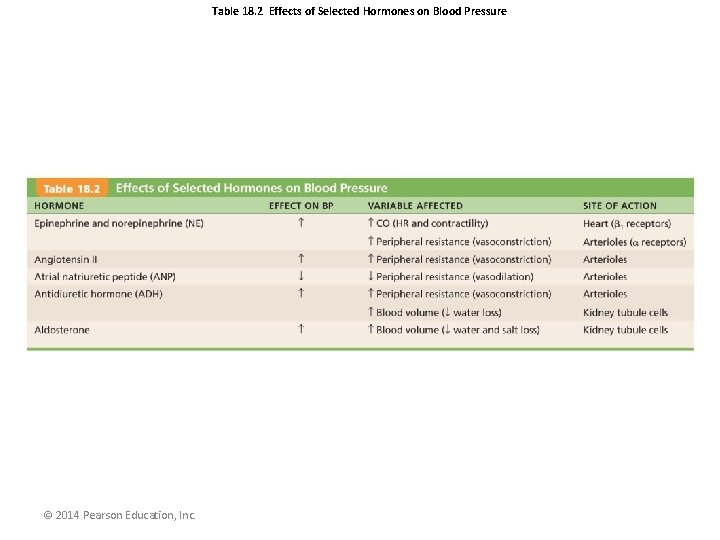
Table 18. 2 Effects of Selected Hormones on Blood Pressure © 2014 Pearson Education, Inc.
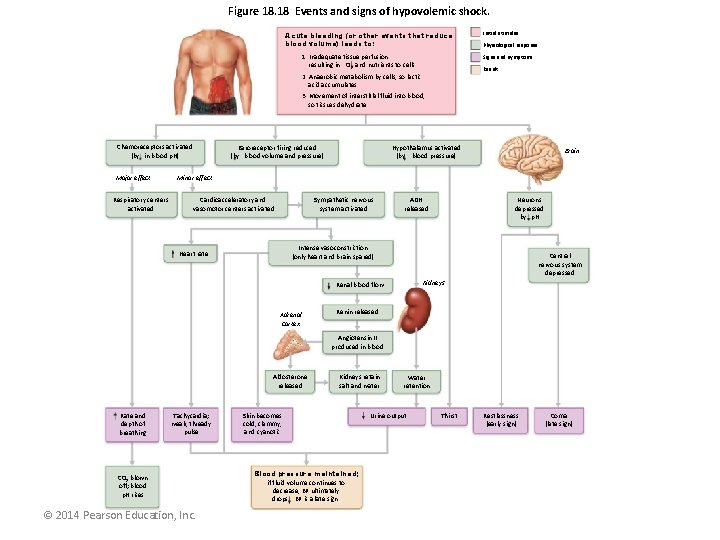
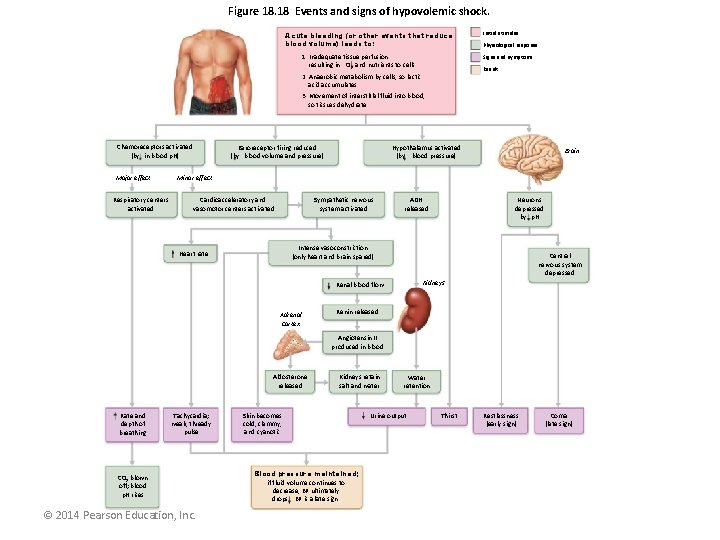
Figure 18. 18 Events and signs of hypovolemic shock. Acute bleeding (or other events that reduce blood volume) leads to: 1. Inadequate tissue perfusion resulting in O 2 and nutrients to cells Initial stimulus Physiological response Signs and symptoms Result 2. Anaerobic metabolism by cells, so lactic acid accumulates 3. Movement of interstitial fluid into blood, so tissues dehydrate Chemoreceptors activated (by in blood p. H) Major effect Respiratory centers activated Baroreceptor firing reduced (by blood volume and pressure) Hypothalamus activated (by blood pressure) Brain Minor effect Cardioacceleratory and vasomotor centers activated Sympathetic nervous system activated ADH released Neurons depressed by p. H Intense vasoconstriction (only heart and brain spared) Heart rate Central nervous system depressed Kidneys Renal blood flow Adrenal cortex Renin released Angiotensin II produced in blood Aldosterone released Rate and depth of breathing Tachycardia; weak, thready pulse CO 2 blown off; blood p. H rises © 2014 Pearson Education, Inc. Kidneys retain salt and water Skin becomes cold, clammy, and cyanotic Blood pressure maintained; if fluid volume continues to decrease, BP ultimately drops. BP is a late sign. Water retention Urine output Thirst Restlessness (early sign) Coma (late sign)
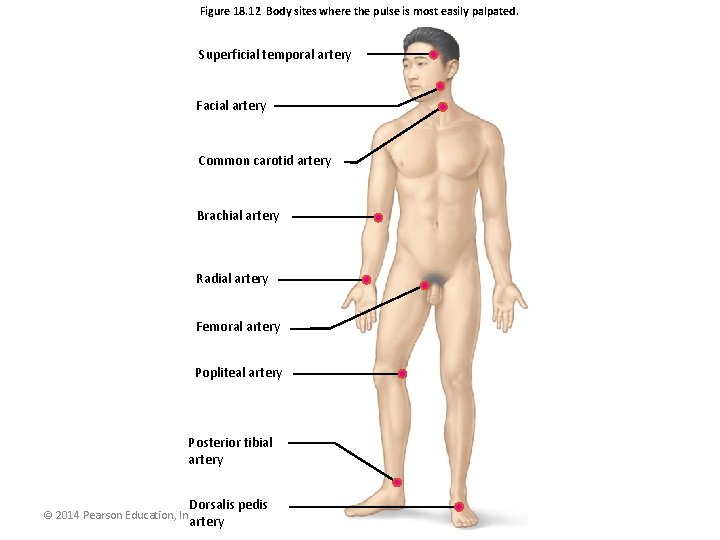
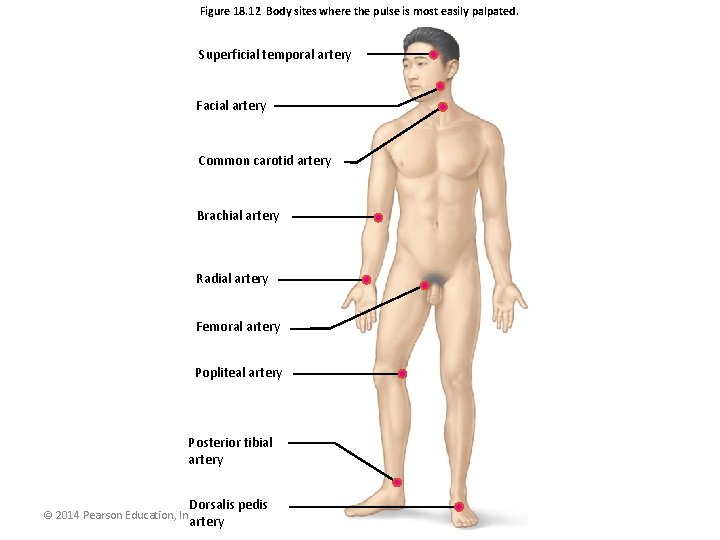
Figure 18. 12 Body sites where the pulse is most easily palpated. Superficial temporal artery Facial artery Common carotid artery Brachial artery Radial artery Femoral artery Popliteal artery Posterior tibial artery Dorsalis pedis artery © 2014 Pearson Education, Inc.
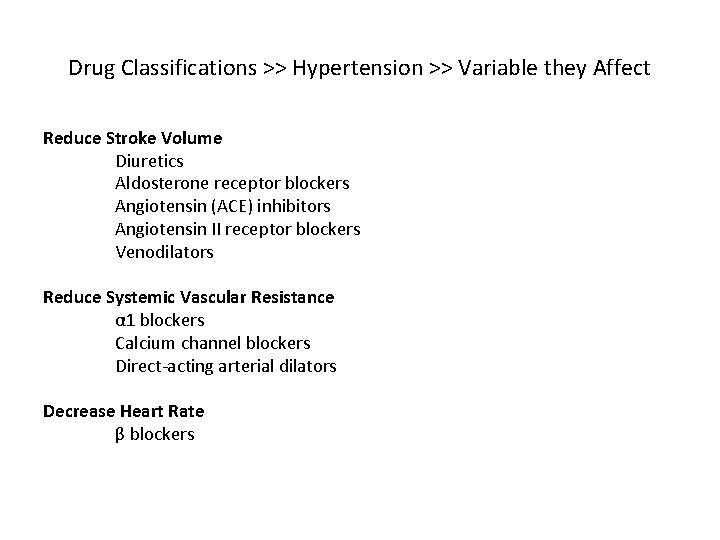
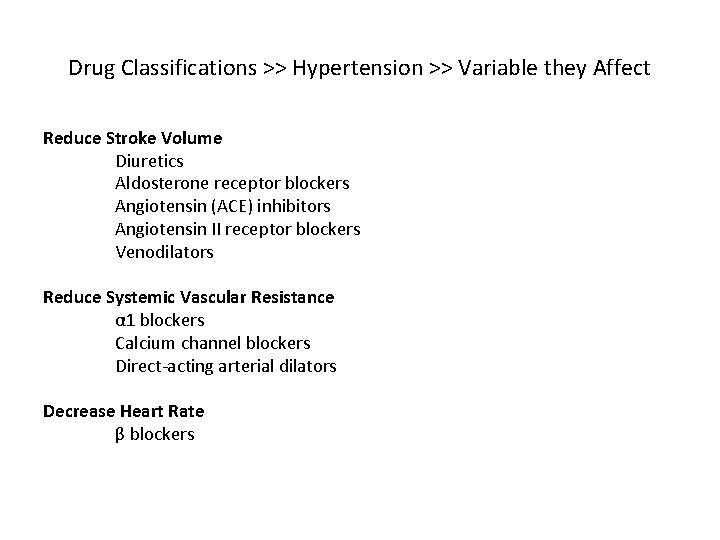
Drug Classifications >> Hypertension >> Variable they Affect Reduce Stroke Volume Diuretics Aldosterone receptor blockers Angiotensin (ACE) inhibitors Angiotensin II receptor blockers Venodilators Reduce Systemic Vascular Resistance α 1 blockers Calcium channel blockers Direct-acting arterial dilators Decrease Heart Rate β blockers
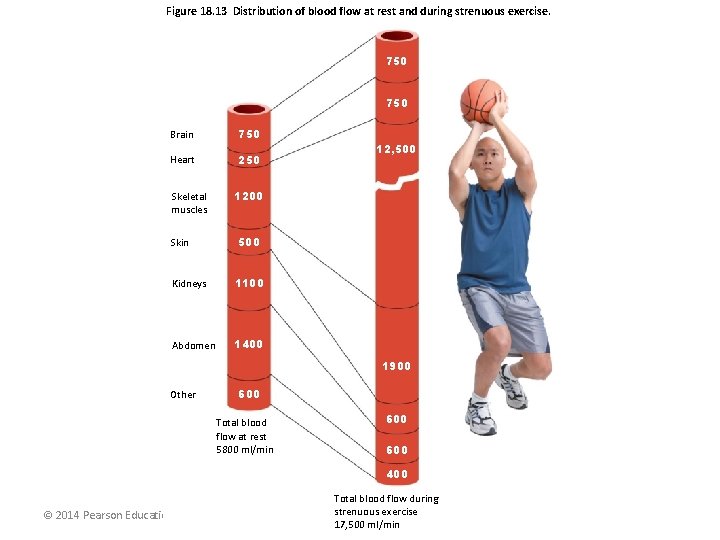
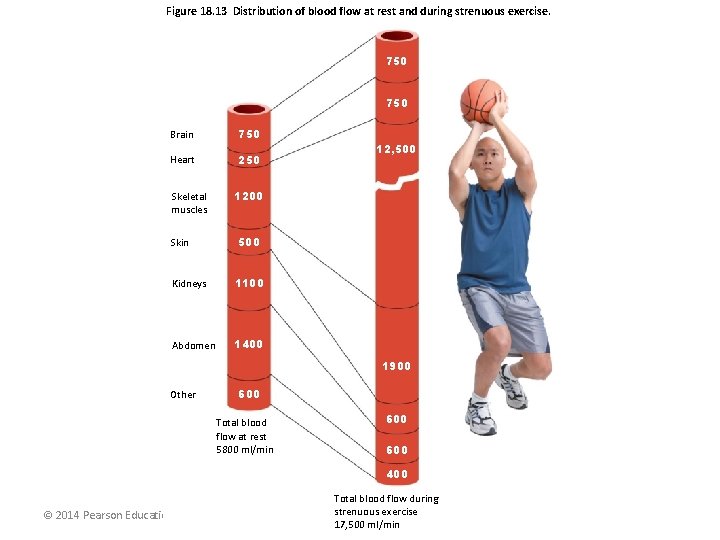
Figure 18. 13 Distribution of blood flow at rest and during strenuous exercise. 750 Brain 750 Heart 250 Skeletal muscles Skin 12, 500 1200 500 Kidneys 1100 Abdomen 1400 1900 Other 600 Total blood flow at rest 5800 ml/min 600 400 © 2014 Pearson Education, Inc. Total blood flow during strenuous exercise 17, 500 ml/min
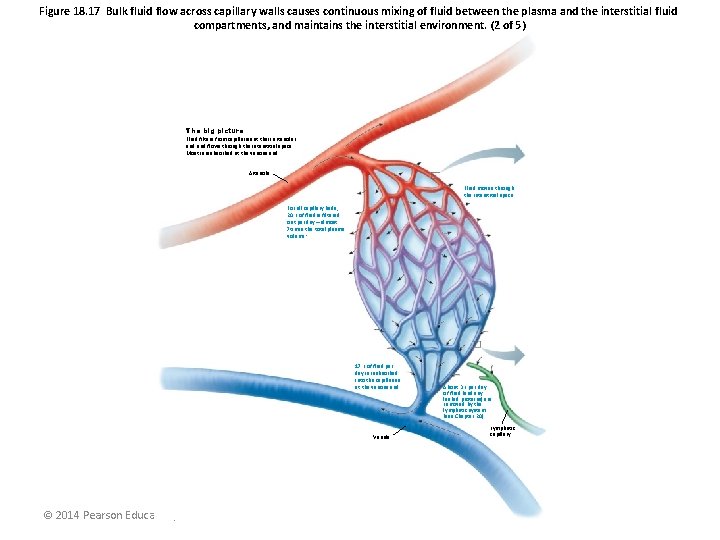
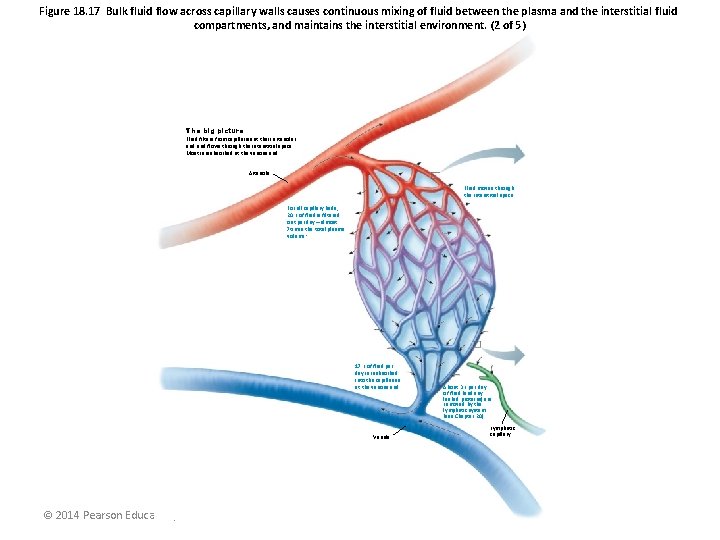
Figure 18. 17 Bulk fluid flow across capillary walls causes continuous mixing of fluid between the plasma and the interstitial fluid compartments, and maintains the interstitial environment. (2 of 5) The big picture Fluid filters from capillaries at their arteriolar end and flows through the interstitial space. Most is reabsorbed at the venous end. Arteriole Fluid moves through the interstitial space. For all capillary beds, 20 L of fluid is filtered out per day—almost 7 times the total plasma volume! 17 L of fluid per day is reabsorbed into the capillaries at the venous end. Venule © 2014 Pearson Education, Inc. About 3 L per day of fluid (and any leaked proteins) are removed by the lymphatic system (see Chapter 20). Lymphatic capillary
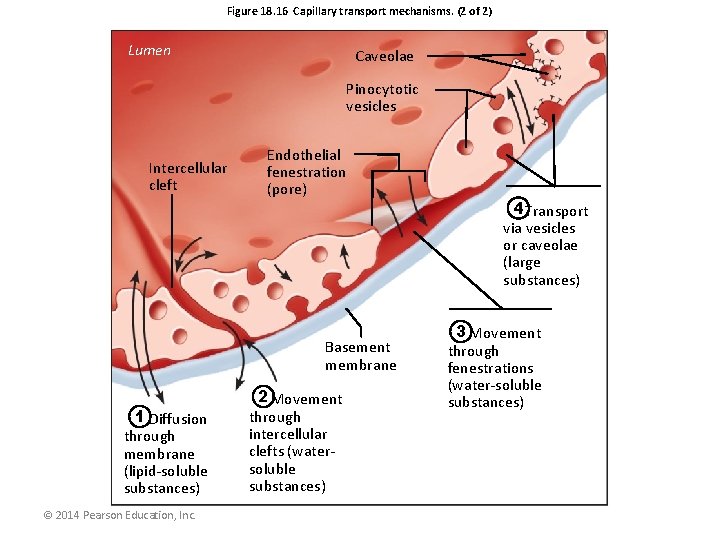
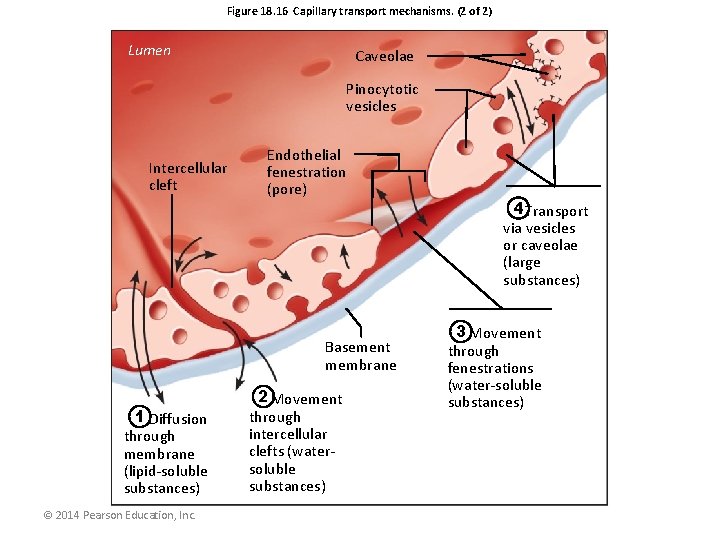
Figure 18. 16 Capillary transport mechanisms. (2 of 2) Lumen Caveolae Pinocytotic vesicles Intercellular cleft Endothelial fenestration (pore) Basement membrane 1 Diffusion through membrane (lipid-soluble substances) © 2014 Pearson Education, Inc. 2 Movement through intercellular clefts (watersoluble substances) 4 Transport via vesicles or caveolae (large substances) 3 Movement through fenestrations (water-soluble substances)
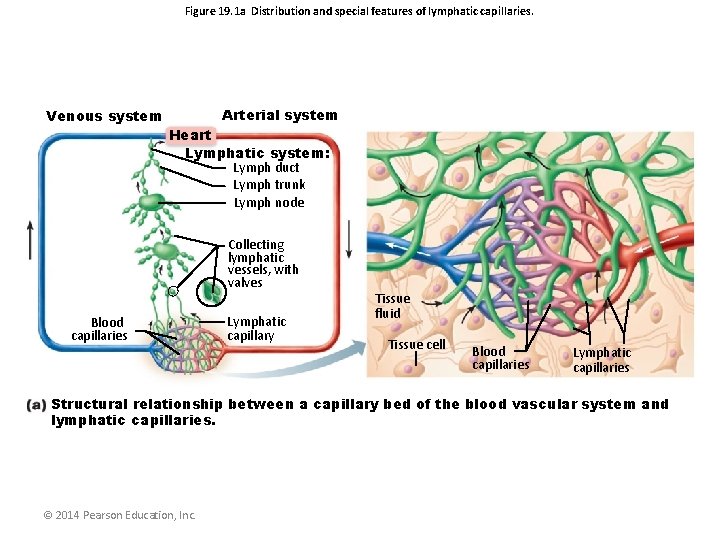
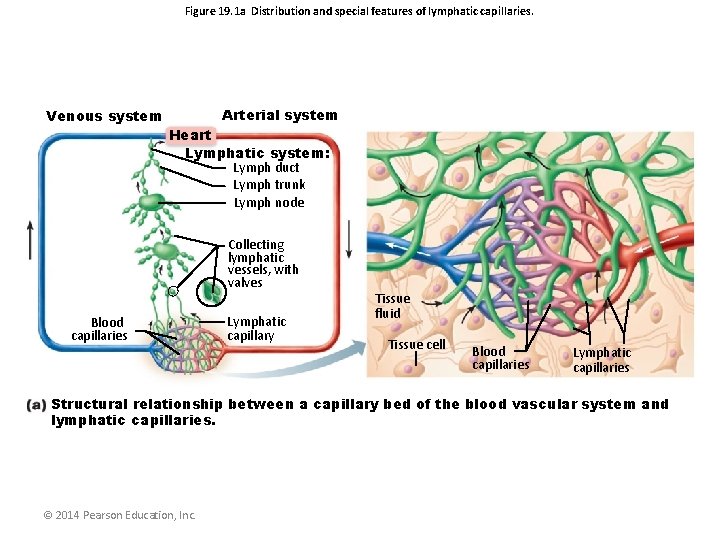
Figure 19. 1 a Distribution and special features of lymphatic capillaries. Venous system Arterial system Heart Lymphatic system: Lymph duct Lymph trunk Lymph node Collecting lymphatic vessels, with valves Blood capillaries Lymphatic capillary Tissue fluid Tissue cell Blood capillaries Lymphatic capillaries Structural relationship between a capillary bed of the blood vascular system and lymphatic capillaries. © 2014 Pearson Education, Inc.
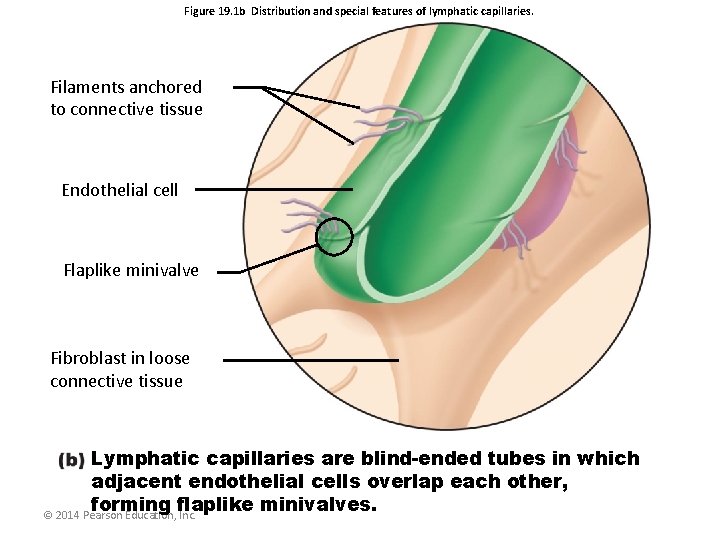
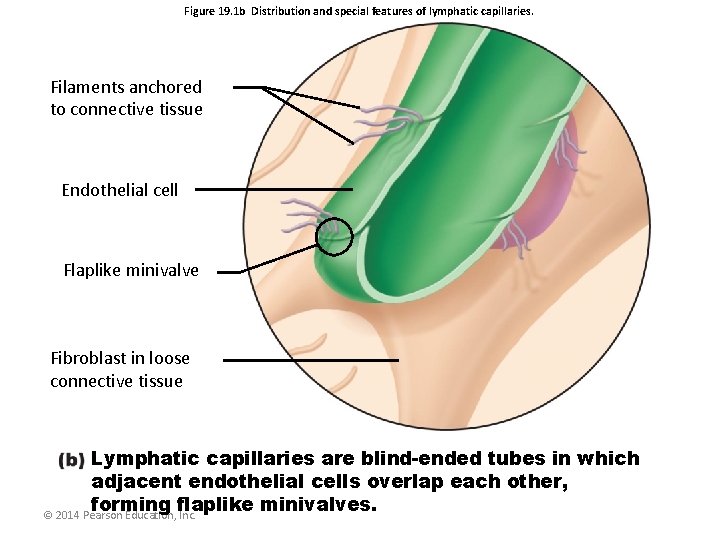
Figure 19. 1 b Distribution and special features of lymphatic capillaries. Filaments anchored to connective tissue Endothelial cell Flaplike minivalve Fibroblast in loose connective tissue Lymphatic capillaries are blind-ended tubes in which adjacent endothelial cells overlap each other, forming flaplike minivalves. © 2014 Pearson Education, Inc.
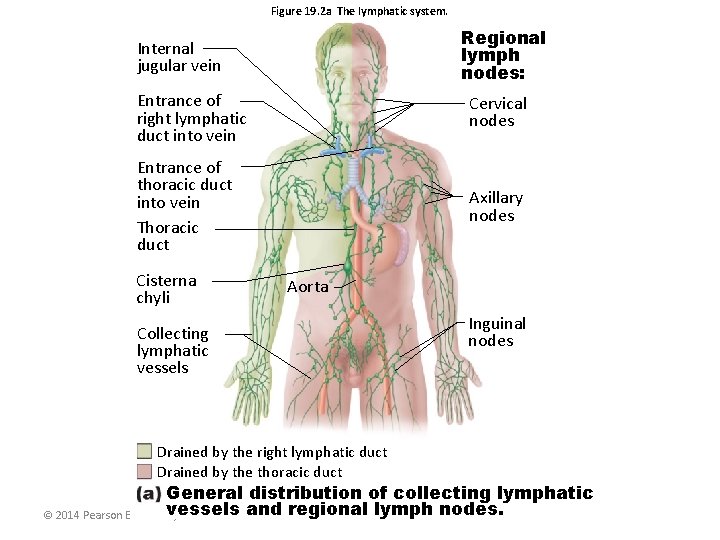
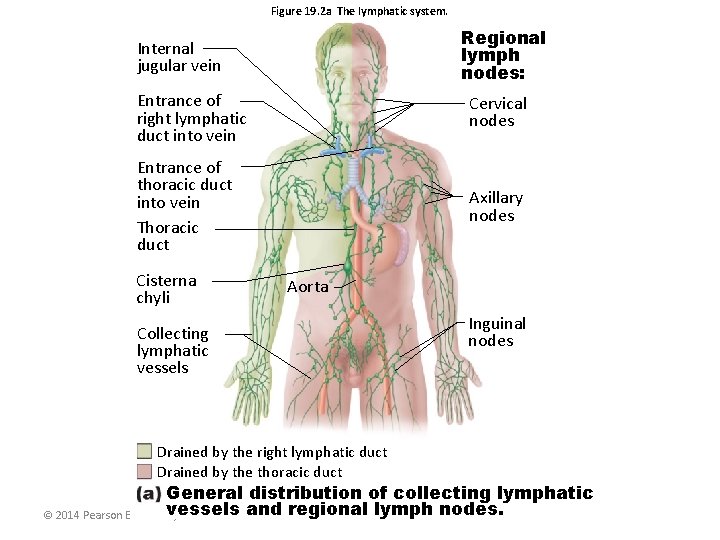
Figure 19. 2 a The lymphatic system. Regional lymph nodes: Internal jugular vein Entrance of right lymphatic duct into vein Cervical nodes Entrance of thoracic duct into vein Thoracic duct Axillary nodes Cisterna chyli Aorta Collecting lymphatic vessels Drained by the right lymphatic duct Drained by the thoracic duct Inguinal nodes General distribution of collecting lymphatic vessels and regional lymph nodes. © 2014 Pearson Education, Inc.
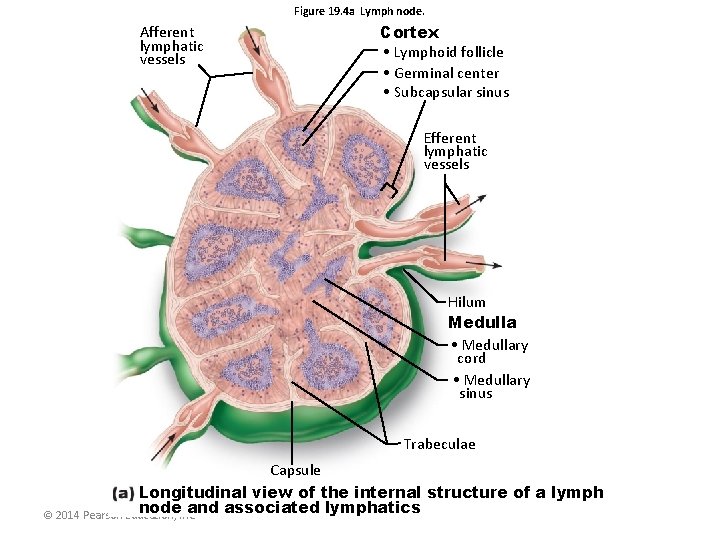
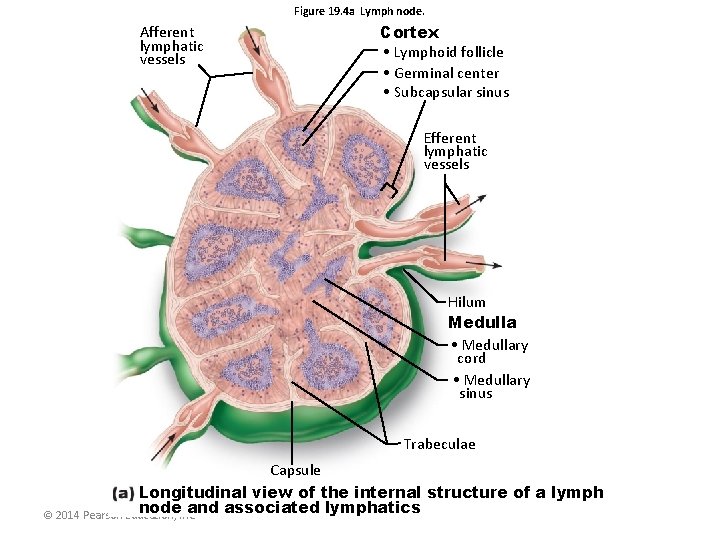
Figure 19. 4 a Lymph node. Afferent lymphatic vessels Cortex • Lymphoid follicle • Germinal center • Subcapsular sinus Efferent lymphatic vessels Hilum Medulla • Medullary cord • Medullary sinus Trabeculae Capsule Longitudinal view of the internal structure of a lymph node. Inc. and associated lymphatics © 2014 Pearson Education,
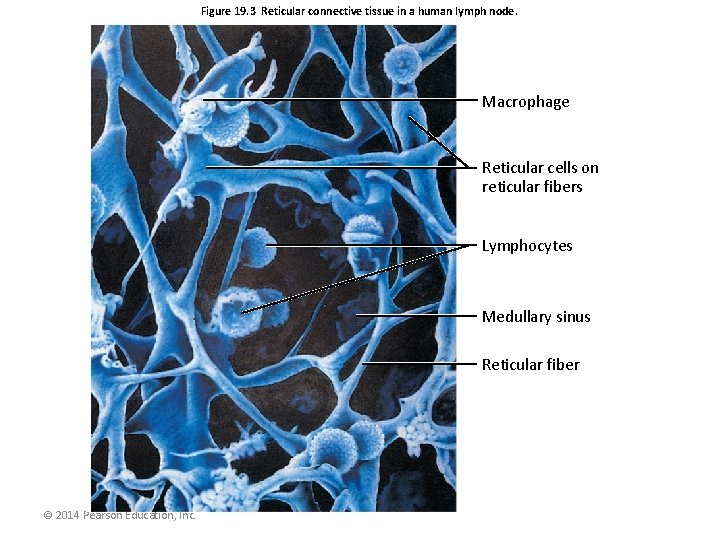
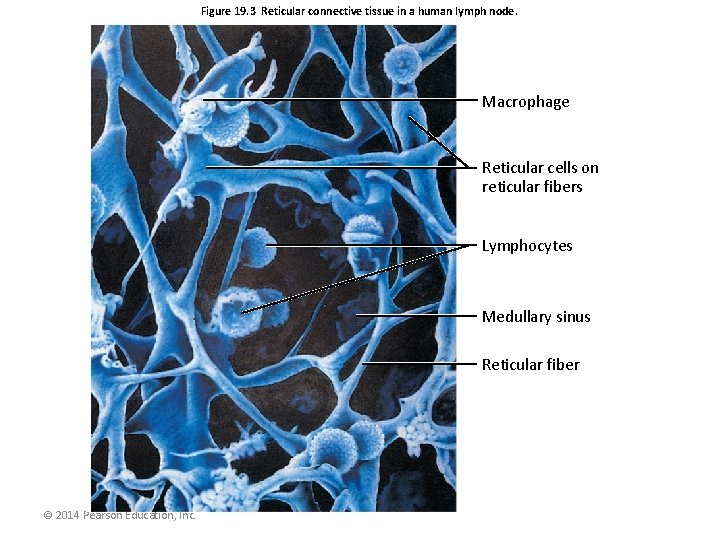
Figure 19. 3 Reticular connective tissue in a human lymph node. Macrophage Reticular cells on reticular fibers Lymphocytes Medullary sinus Reticular fiber © 2014 Pearson Education, Inc.
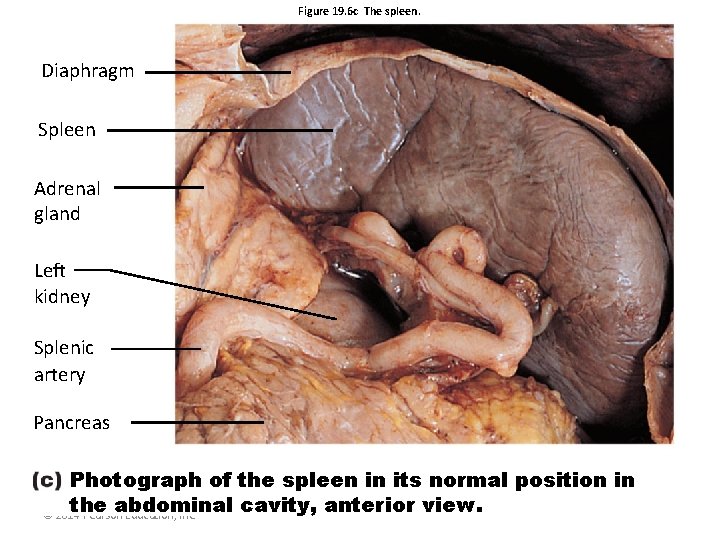
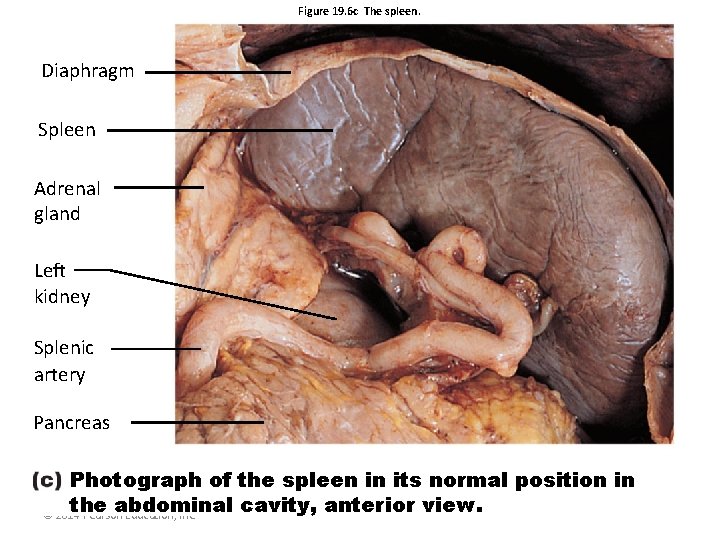
Figure 19. 6 c The spleen. Diaphragm Spleen Adrenal gland Left kidney Splenic artery Pancreas Photograph of the spleen in its normal position in the abdominal cavity, anterior view. © 2014 Pearson Education, Inc.
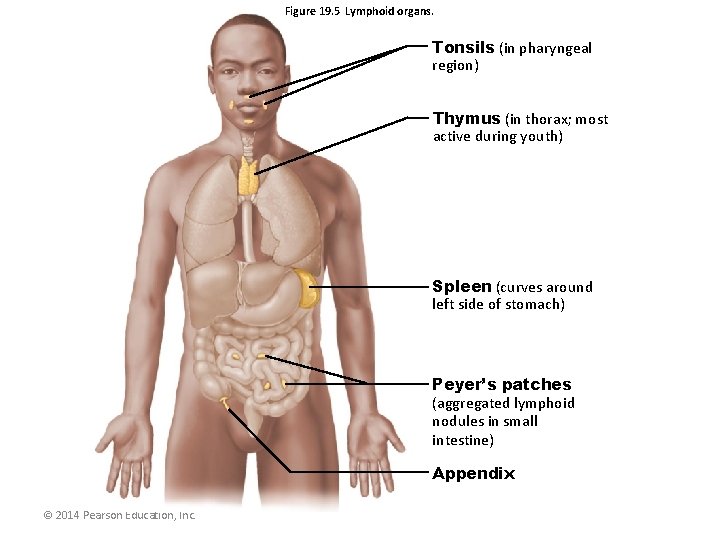
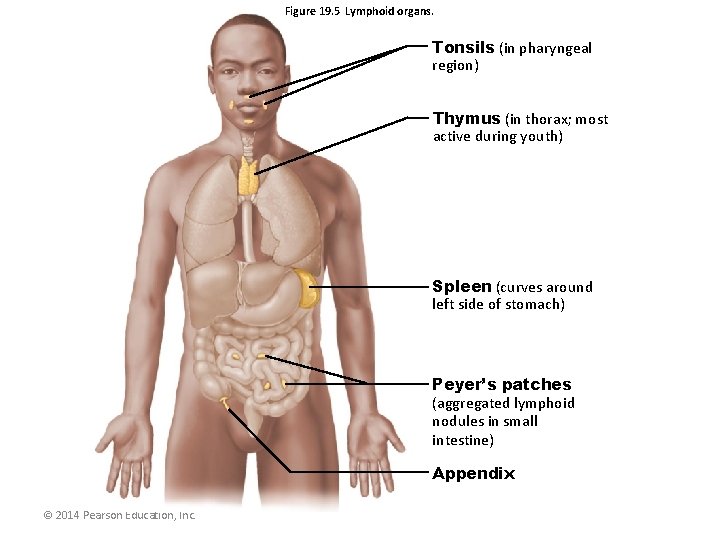
Figure 19. 5 Lymphoid organs. Tonsils (in pharyngeal region) Thymus (in thorax; most active during youth) Spleen (curves around left side of stomach) Peyer’s patches (aggregated lymphoid nodules in small intestine) Appendix © 2014 Pearson Education, Inc.