Fever joint pain rash and hyperferritinemia A diagnostic
- Slides: 1
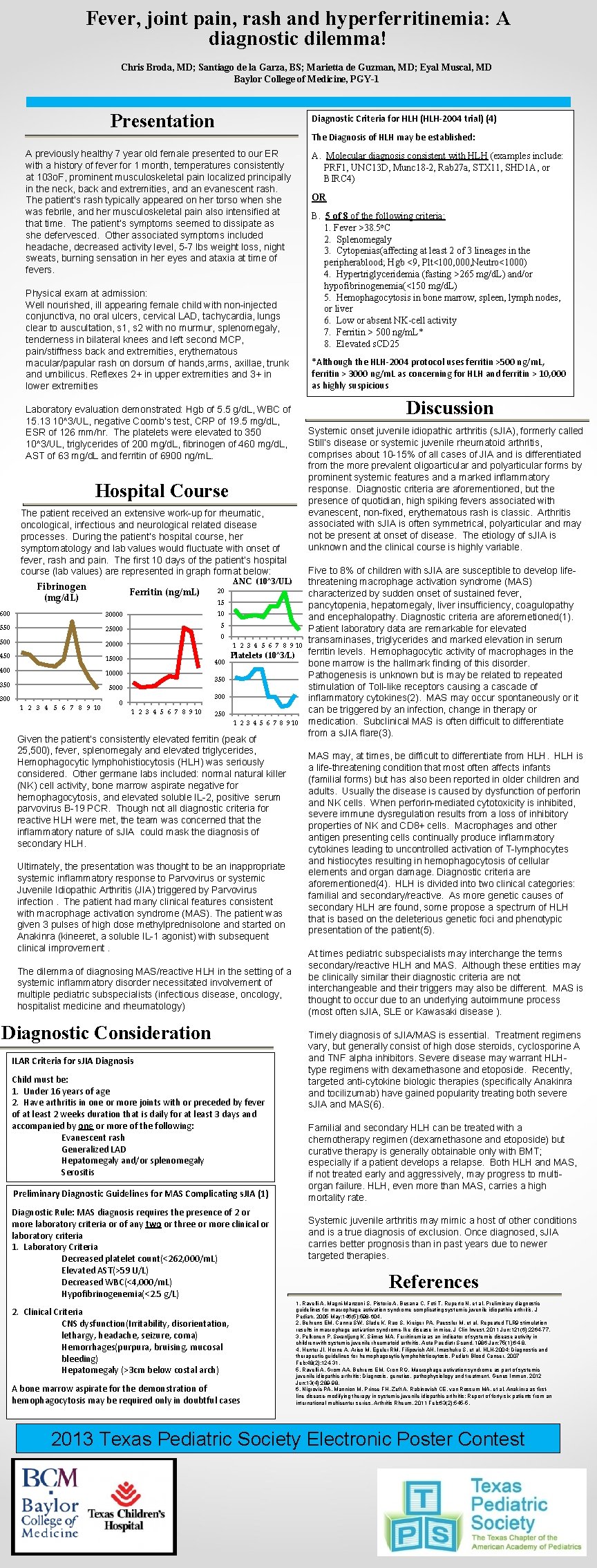
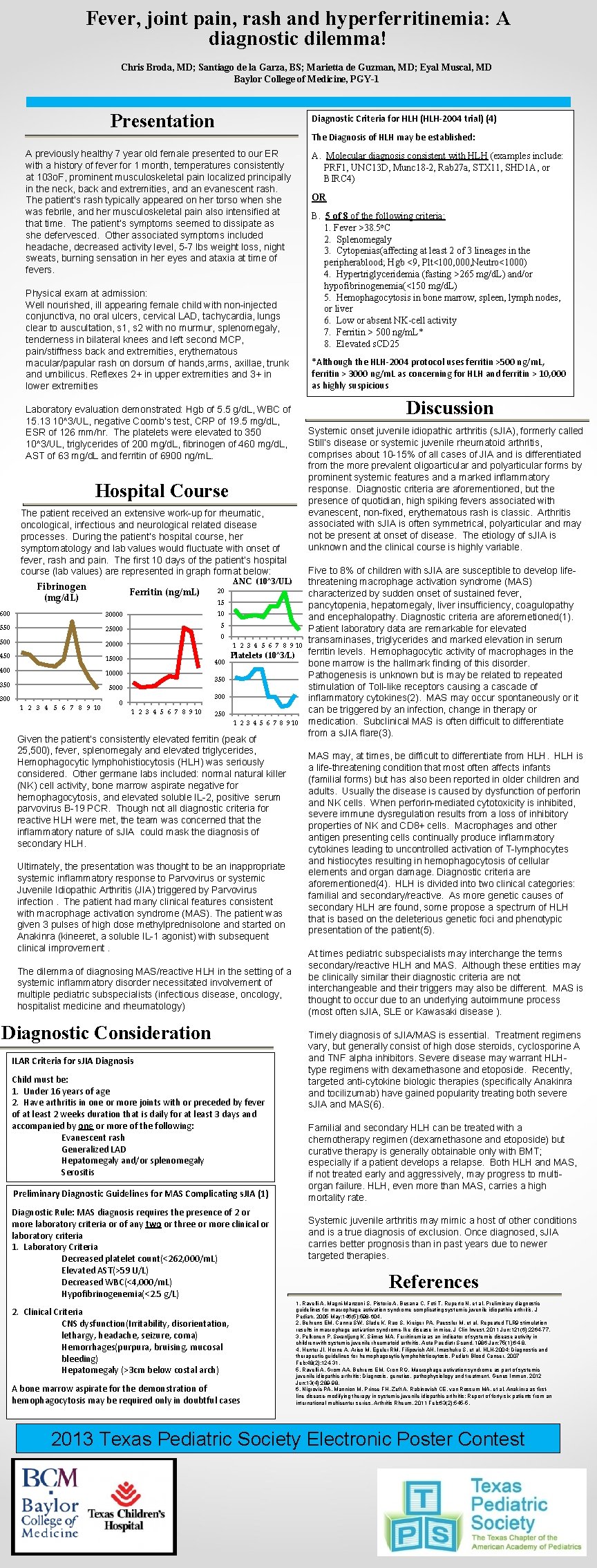
Fever, joint pain, rash and hyperferritinemia: A diagnostic dilemma! Chris Broda, MD; Santiago de la Garza, BS; Marietta de Guzman, MD; Eyal Muscal, MD Baylor College of Medicine, PGY-1 Presentation Diagnostic Criteria for HLH (HLH-2004 trial) (4) The Diagnosis of HLH may be established: A previously healthy 7 year old female presented to our ER with a history of fever for 1 month, temperatures consistently at 103 o. F, prominent musculoskeletal pain localized principally in the neck, back and extremities, and an evanescent rash. The patient’s rash typically appeared on her torso when she was febrile, and her musculoskeletal pain also intensified at that time. The patient’s symptoms seemed to dissipate as she defervesced. Other associated symptoms included headache, decreased activity level, 5 -7 lbs weight loss, night sweats, burning sensation in her eyes and ataxia at time of fevers. A. Molecular diagnosis consistent with HLH (examples include: PRF 1, UNC 13 D, Munc 18 -2, Rab 27 a, STX 11, SHD 1 A, or BIRC 4) OR B. 5 of 8 of the following criteria: 1. Fever >38. 5 o. C 2. Splenomegaly 3. Cytopenias(affecting at least 2 of 3 lineages in the peripherablood; Hgb <9, Plt<100, 000, Neutro<1000) 4. Hypertriglyceridemia (fasting >265 mg/d. L) and/or hypofibrinogenemia(<150 mg/d. L) 5. Hemophagocytosis in bone marrow, spleen, lymph nodes, or liver 6. Low or absent NK-cell activity 7. Ferritin > 500 ng/m. L* 8. Elevated s. CD 25 Physical exam at admission: Well nourished, ill appearing female child with non-injected conjunctiva, no oral ulcers, cervical LAD, tachycardia, lungs clear to auscultation, s 1, s 2 with no murmur, splenomegaly, tenderness in bilateral knees and left second MCP, pain/stiffness back and extremities, erythematous macular/papular rash on dorsum of hands, arms, axillae, trunk and umbilicus. Reflexes 2+ in upper extremities and 3+ in lower extremities *Although the HLH-2004 protocol uses ferritin >500 ng/m. L, ferritin > 3000 ng/m. L as concerning for HLH and ferritin > 10, 000 as highly suspicious Discussion Laboratory evaluation demonstrated: Hgb of 5. 5 g/d. L, WBC of 15. 13 10^3/UL, negative Coomb’s test, CRP of 19. 5 mg/d. L, ESR of 126 mm/hr. The platelets were elevated to 350 10^3/UL, triglycerides of 200 mg/d. L, fibrinogen of 460 mg/d. L, AST of 63 mg/d. L and ferritin of 6900 ng/m. L. Systemic onset juvenile idiopathic arthritis (s. JIA), formerly called Still’s disease or systemic juvenile rheumatoid arthritis, comprises about 10 -15% of all cases of JIA and is differentiated from the more prevalent oligoarticular and polyarticular forms by prominent systemic features and a marked inflammatory response. Diagnostic criteria are aforementioned, but the presence of quotidian, high spiking fevers associated with evanescent, non-fixed, erythematous rash is classic. Arthritis associated with s. JIA is often symmetrical, polyarticular and may not be present at onset of disease. The etiology of s. JIA is unknown and the clinical course is highly variable. Hospital Course The patient received an extensive work-up for rheumatic, oncological, infectious and neurological related disease processes. During the patient’s hospital course, her symptomatology and lab values would fluctuate with onset of fever, rash and pain. The first 10 days of the patient’s hospital course (lab values) are represented in graph format below: Fibrinogen (mg/d. L) Ferritin (ng/m. L) 600 30000 550 25000 500 20000 450 15000 400 10000 350 5000 300 1 2 3 4 5 6 7 8 9 10 0 20 ANC (10^3/UL) 15 10 5 0 400 1 2 3 4 5 6 7 8 9 10 Platelets (10^3/L) 350 300 1 2 3 4 5 6 7 8 9 10 250 1 2 3 4 5 6 7 8 9 10 Given the patient’s consistently elevated ferritin (peak of 25, 500), fever, splenomegaly and elevated triglycerides, Hemophagocytic lymphohistiocytosis (HLH) was seriously considered. Other germane labs included: normal natural killer (NK) cell activity, bone marrow aspirate negative for hemophagocytosis, and elevated soluble IL-2, positive serum parvovirus B-19 PCR. Though not all diagnostic criteria for reactive HLH were met, the team was concerned that the inflammatory nature of s. JIA could mask the diagnosis of secondary HLH. Ultimately, the presentation was thought to be an inappropriate systemic inflammatory response to Parvovirus or systemic Juvenile Idiopathic Arthritis (JIA) triggered by Parvovirus infection. The patient had many clinical features consistent with macrophage activation syndrome (MAS). The patient was given 3 pulses of high dose methylprednisolone and started on Anakinra (kineeret, a soluble IL-1 agonist) with subsequent clinical improvement. The dilemma of diagnosing MAS/reactive HLH in the setting of a systemic inflammatory disorder necessitated involvement of multiple pediatric subspecialists (infectious disease, oncology, hospitalist medicine and rheumatology) Diagnostic Consideration ILAR Criteria for s. JIA Diagnosis Child must be: 1. Under 16 years of age 2. Have arthritis in one or more joints with or preceded by fever of at least 2 weeks duration that is daily for at least 3 days and accompanied by one or more of the following: Evanescent rash Generalized LAD Hepatomegaly and/or splenomegaly Serositis Preliminary Diagnostic Guidelines for MAS Complicating s. JIA (1) Diagnostic Rule: MAS diagnosis requires the presence of 2 or more laboratory criteria or of any two or three or more clinical or laboratory criteria 1. Laboratory Criteria Decreased platelet count(<262, 000/m. L) Elevated AST(>59 U/L) Decreased WBC(<4, 000/m. L) Hypofibrinogenemia(<2. 5 g/L) 2. Clinical Criteria CNS dysfunction(Irritability, disorientation, lethargy, headache, seizure, coma) Hemorrhages(purpura, bruising, mucosal bleeding) Hepatomegaly (>3 cm below costal arch) A bone marrow aspirate for the demonstration of hemophagocytosis may be required only in doubtful cases Five to 8% of children with s. JIA are susceptible to develop lifethreatening macrophage activation syndrome (MAS) characterized by sudden onset of sustained fever, pancytopenia, hepatomegaly, liver insufficiency, coagulopathy and encephalopathy. Diagnostic criteria are aforemetioned(1). Patient laboratory data are remarkable for elevated transaminases, triglycerides and marked elevation in serum ferritin levels. Hemophagocytic activity of macrophages in the bone marrow is the hallmark finding of this disorder. Pathogenesis is unknown but is may be related to repeated stimulation of Toll-like receptors causing a cascade of inflammatory cytokines(2). MAS may occur spontaneously or it can be triggered by an infection, change in therapy or medication. Subclinical MAS is often difficult to differentiate from a s. JIA flare(3). MAS may, at times, be difficult to differentiate from HLH is a life-threatening condition that most often affects infants (familial forms) but has also been reported in older children and adults. Usually the disease is caused by dysfunction of perforin and NK cells. When perforin-mediated cytotoxicity is inhibited, severe immune dysregulation results from a loss of inhibitory properties of NK and CD 8+ cells. Macrophages and other antigen presenting cells continually produce inflammatory cytokines leading to uncontrolled activation of T-lymphocytes and histiocytes resulting in hemophagocytosis of cellular elements and organ damage. Diagnostic criteria are aforementioned(4). HLH is divided into two clinical categories: familial and secondary/reactive. As more genetic causes of secondary HLH are found, some propose a spectrum of HLH that is based on the deleterious genetic foci and phenotypic presentation of the patient(5). At times pediatric subspecialists may interchange the terms secondary/reactive HLH and MAS. Although these entities may be clinically similar their diagnostic criteria are not interchangeable and their triggers may also be different. MAS is thought to occur due to an underlying autoimmune process (most often s. JIA, SLE or Kawasaki disease ). Timely diagnosis of s. JIA/MAS is essential. Treatment regimens vary, but generally consist of high dose steroids, cyclosporine A and TNF alpha inhibitors. Severe disease may warrant HLHtype regimens with dexamethasone and etoposide. Recently, targeted anti-cytokine biologic therapies (specifically Anakinra and tocilizumab) have gained popularity treating both severe s. JIA and MAS(6). Familial and secondary HLH can be treated with a chemotherapy regimen (dexamethasone and etoposide) but curative therapy is generally obtainable only with BMT; especially if a patient develops a relapse. Both HLH and MAS, if not treated early and aggressively, may progress to multiorgan failure. HLH, even more than MAS, carries a high mortality rate. Systemic juvenile arthritis may mimic a host of other conditions and is a true diagnosis of exclusion. Once diagnosed, s. JIA carries better prognosis than in past years due to newer targeted therapies. References 1. Ravelli A, Magni-Manzoni S, Pistorio A, Besana C, Foti T, Ruperto N, et al. Preliminary diagnostic guidelines for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Pediatr. 2005 May; 146(5): 598 -604. 2. Behrens EM, Canna SW, Slade K, Rao S, Kreiger PA, Paessler M, et al. Repeated TLR 9 stimulation results in macrophage activation syndrome-like disease in mice. J Clin Invest. 2011 Jun; 121(6): 2264 -77. 3. Pelkonen P, Swanljung K, Siimes MA. Ferritinemia as an indicator of systemic disease activity in children with systemic juvenile rheumatoid arthritis. Acta Paediatr Scand. 1986 Jan; 75(1): 64 -8. 4. Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007 Feb; 48(2): 124 -31. 5. Ravelli A, Grom AA, Behrens EM, Cron RQ. Macrophage activation syndrome as part of systemic juvenile idiopathic arthritis: Diagnosis, genetics, pathophysiology and treatment. Genes Immun. 2012 Jun; 13(4): 289 -98. 6. Nigrovic PA, Mannion M, Prince FH, Zeft A, Rabinovich CE, van Rossum MA, et al. Anakinra as firstline disease-modifying therapy in systemic juvenile idiopathic arthritis: Report of forty-six patients from an international multicenter series. Arthritis Rheum. 2011 Feb; 63(2): 545 -5. 2013 Texas Pediatric Society Electronic Poster Contest