Fever in Pediatrics Emergency medicine APLS PATHOPHYSIOLOGY Defined
- Slides: 24
Fever in Pediatrics 林口急診醫學科 吳孟書 醫師 出處 : Emergency medicine, APLS
PATHOPHYSIOLOGY • Defined as a rise in deep body temperature associated with a resetting of the body’s thermostat. • Exogenous pyrogens • Endogenous pyrogens • Peripheral vasoconstriction • Shivering • Central pooling • Behavioral activity
CLINICAL FEATURES • Temperature more than 38℃ • The higher temperature is, the higher incidence of bacteremia is. • Variation with the body’s circadian rhythm. • Rectal temperature is 0. 6℃ higher than oral temperature. • Oral temperature is 0. 6℃ higher than axillary temperature • Infrared thermometer scan tympanic membrane is mimic with oral tempertrature.
NEWBORN FEVER (1 -3 Mo) • • High risk for life-threatening infection was considered before Serious bacterial infection : 3 -4% noted recently Review of birth history: 1. 2. 3. Length of gestation Use of antibiotics in the mother or infant Any neonatal complication • Organ-specific list of inquiries may be nonspecific in young infants •
NEW BORN FEVER (1 -3 Mo) • Physical Examination: 1. 2. 3. 4. 5. 6. PAT (Pediatric assessment triangle) + ABCDEs Inconsolable crying or increased irritability when handled Fullness of anterior frontanelle Meningeal sings are often absent A complete head-to-toe examination Extensive laboratory septic work-up to detect occult infection UTI is the single most common bacterial infection in this group. 7.
NEWBORN FEVER (1 -3 Mo) • Rochester criteria for low risk for serious bacterial infection: 1. 2. 3. 4. 5. 6. Nontoxic appearance No soft tissue infection WBCs between 5000 -15000/mm 3 Bands <1500/mm 3 Normal urinalysis Stool with less than 5 WBCs/hpf if infants with diarrhea
NEWBORN FEVER (1 -3 Mo) • Management: 1. Hospitalize febrile infants, especially for infants younger than age one month Ceftriaxone 50 mg/kg for low risk infants with caretaker telephone in outpatient management Infants could be discharged if cultures were negative after 24 h observation. 2. 3.
INFANTS OF 3 -24 MONTHS • At high risk for occult bacteremia • Clinical judgment appears to be more reliable: PAT + ABCDEs • Eye contact • Playfulness and positive response to interaction • Negative response to noxious stimuli • Alertness and consolability
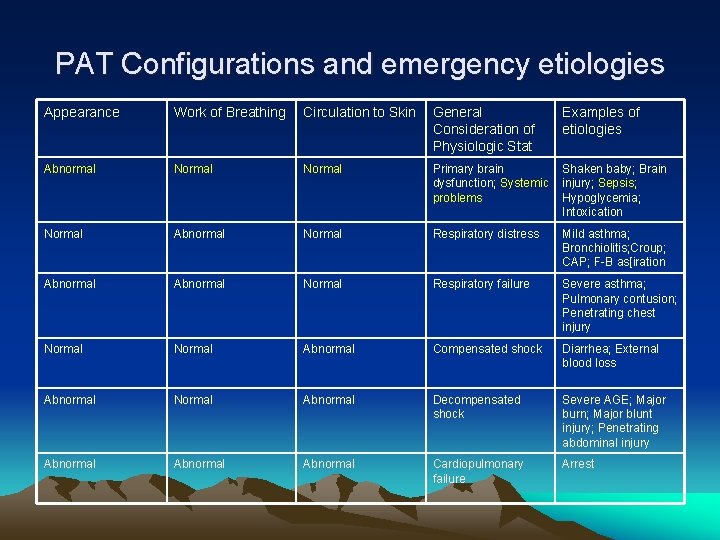
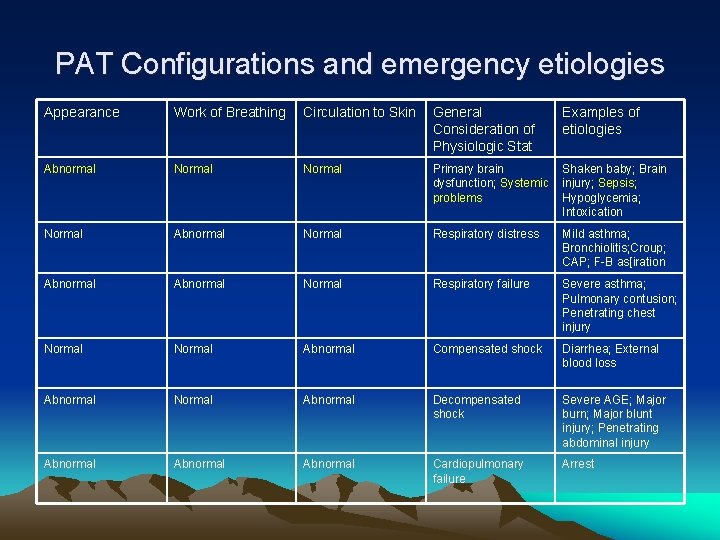
PAT Configurations and emergency etiologies Appearance Work of Breathing Circulation to Skin General Consideration of Physiologic Stat Examples of etiologies Abnormal Normal Primary brain dysfunction; Systemic problems Shaken baby; Brain injury; Sepsis; Hypoglycemia; Intoxication Normal Abnormal Normal Respiratory distress Mild asthma; Bronchiolitis; Croup; CAP; F-B as[iration Abnormal Normal Respiratory failure Severe asthma; Pulmonary contusion; Penetrating chest injury Normal Abnormal Compensated shock Diarrhea; External blood loss Abnormal Normal Abnormal Decompensated shock Severe AGE; Major burn; Major blunt injury; Penetrating abdominal injury Abnormal Cardiopulmonary failure Arrest
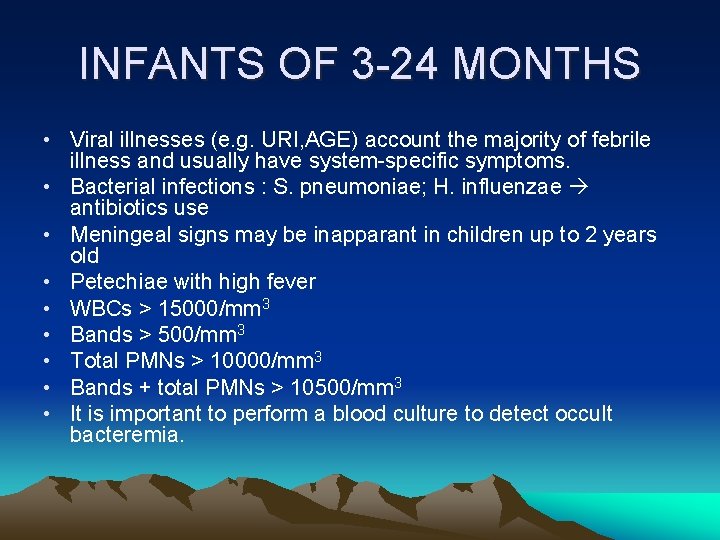
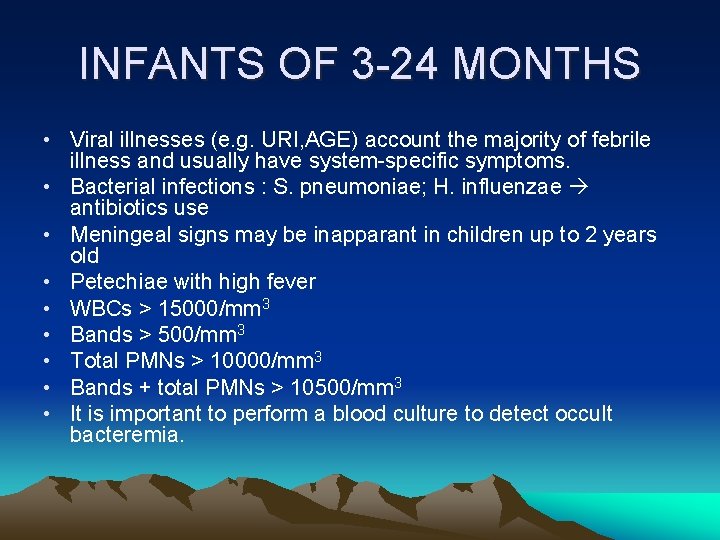
INFANTS OF 3 -24 MONTHS • Viral illnesses (e. g. URI, AGE) account the majority of febrile illness and usually have system-specific symptoms. • Bacterial infections : S. pneumoniae; H. influenzae antibiotics use • Meningeal signs may be inapparant in children up to 2 years old • Petechiae with high fever • WBCs > 15000/mm 3 • Bands > 500/mm 3 • Total PMNs > 10000/mm 3 • Bands + total PMNs > 10500/mm 3 • It is important to perform a blood culture to detect occult bacteremia.
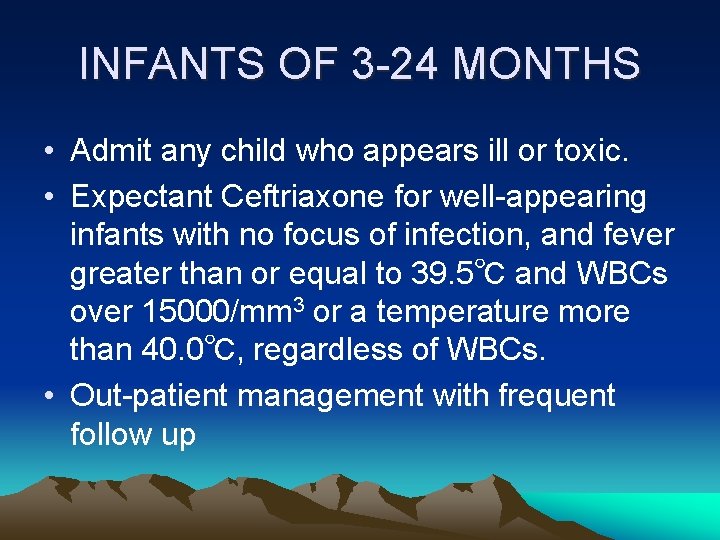
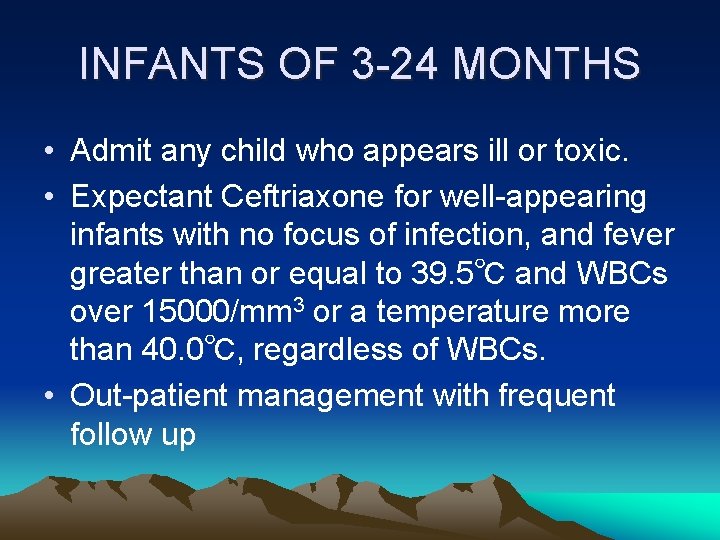
INFANTS OF 3 -24 MONTHS • Admit any child who appears ill or toxic. • Expectant Ceftriaxone for well-appearing infants with no focus of infection, and fever greater than or equal to 39. 5℃ and WBCs over 15000/mm 3 or a temperature more than 40. 0℃, regardless of WBCs. • Out-patient management with frequent follow up
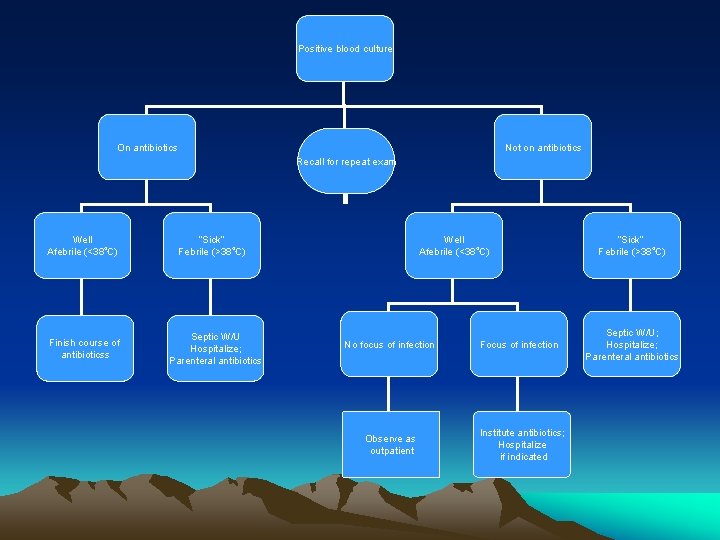
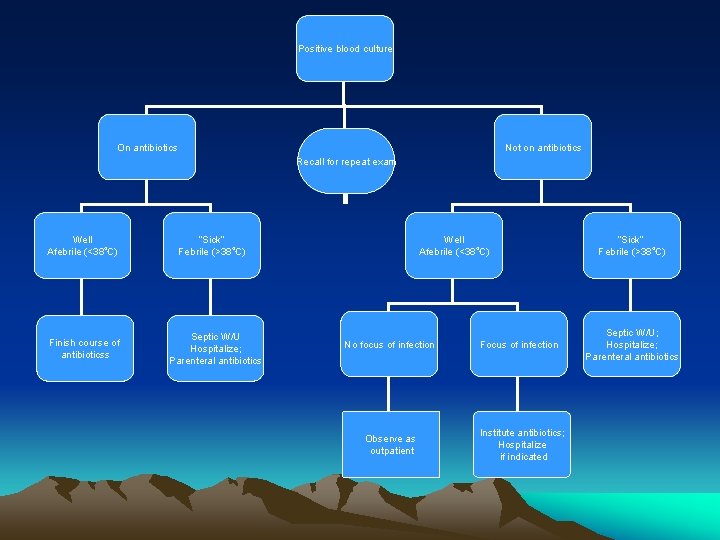
Positive blood culture On antibiotics Not on antibiotics Recall for repeat exam Well Afebrile (<38℃) Finish course of antibioticss “Sick” Febrile (>38℃) Septic W/U Hospitalize; Parenteral antibiotics Well Afebrile (<38℃) No focus of infection Observe as outpatient Focus of infection Institute antibiotics; Hospitalize if indicated “Sick” Febrile (>38℃) Septic W/U; Hospitalize; Parenteral antibiotics
OLDER FEBRILE CHILDREN • Easier to evaluate • Lower risk of bacteremia, but higher incidence of streptococcal pharyngitis in 510 years aged cildren • Infectious mononucleosis: fever, tonsillar hypertrophy with exudate, LAP, and hepatosplenomegaly. • Mycoplasma pneumoniae marcrolid
Managing the Fever • 1. 2. 3. 4. 5. 6. • • • Aside from febrile convulsion, fever is not known to produce any harmful effects in children. Unwrapping a bundled child Rehydrating a dehydratded child Sponging with tepid water slowly Acetaminophen : 10 -15 mg/kg, po, q 4 -6 h Ibuprofen : 5 -10 mg/kg, po, q 6 -8 h Aspirin : 10 -15 mg/kg, po, q 4 -6 h Equally effective in reducing fever between antipyretics Sponging and antipyretics used together are more effective. Administration of these antipyretics simultaneously produce a longer duration of reducing fever Avoid aspirin in children with chicken pox or influenza-like illness – Reye syndrome Antibiotics for system-specific infection
Fever in Children at Risk for Sepsis • Fever in the immunosuppressed children • Fever in very young infants • Fever with petechiae
Fever in the immunosuppressed children • Often benign illness, but 20% of SBI • Absolute neutrophil count (ANC) < 500 • Low lymphocyte count, especially a low CD 4 lymphocyte count in children with HIV • Acute deterioration • Catheter infection • Other infection site as normal children • Several viral infection may disseminate
Fever in the immunosuppressed children • CBC/DC – compared with previous data • Blood culture – from catheter and other peripheral site • U/A and U/C • Other laboratory test and radiologic studies as indicate
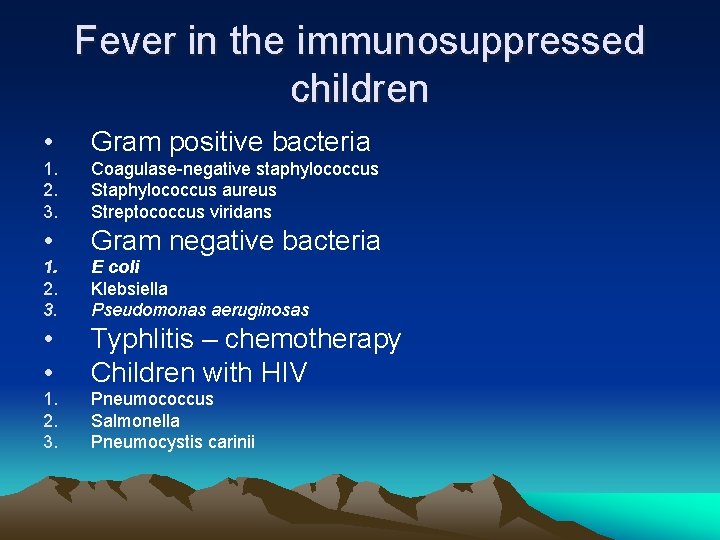
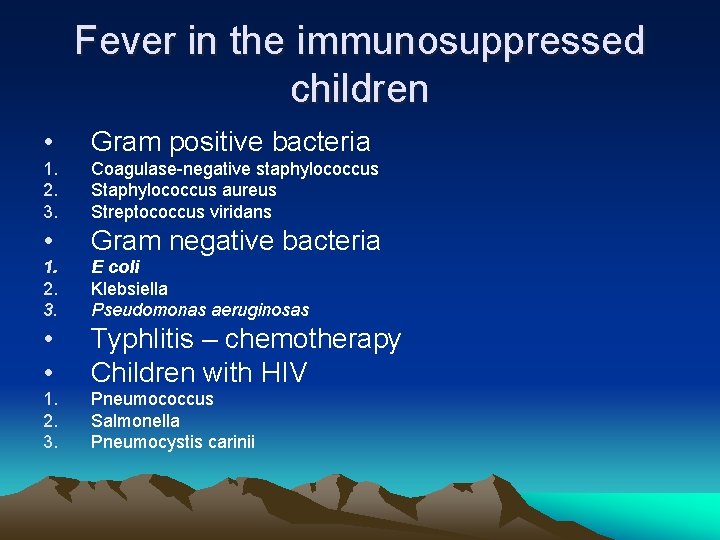
Fever in the immunosuppressed children • Gram positive bacteria 1. 2. 3. Coagulase-negative staphylococcus Staphylococcus aureus Streptococcus viridans • Gram negative bacteria 1. 2. 3. E coli Klebsiella Pseudomonas aeruginosas • • Typhlitis – chemotherapy Children with HIV 1. 2. 3. Pneumococcus Salmonella Pneumocystis carinii
Fever in the immunosuppressed children • Access and treat respiratory distress and failure • Obtain IV access and begin fluid resuscitation for signs of shock • Obtain laboratory studies as indicated • Begin empiric antibiotics treatment including ceftazidime (antipseudomonal antibiotics) and gentamicin, plus vancomycin if there are catheter-related infections or a severe infection. • Admit for inpatient care.
Fever in very young infants • As above at page 4 -7
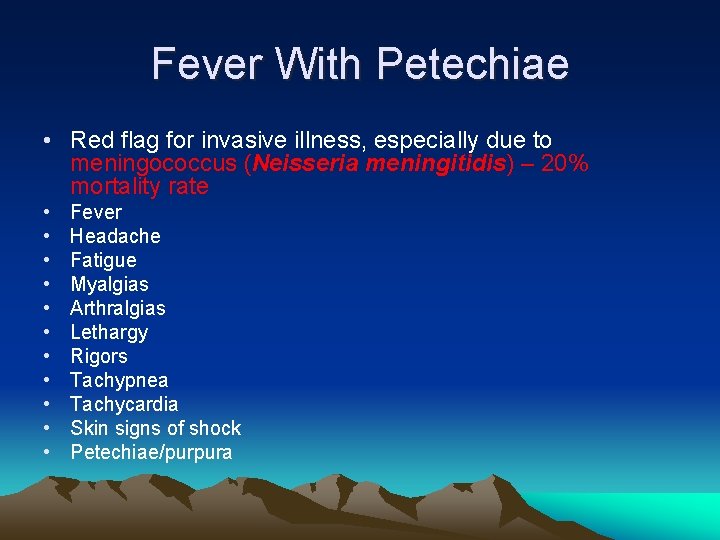
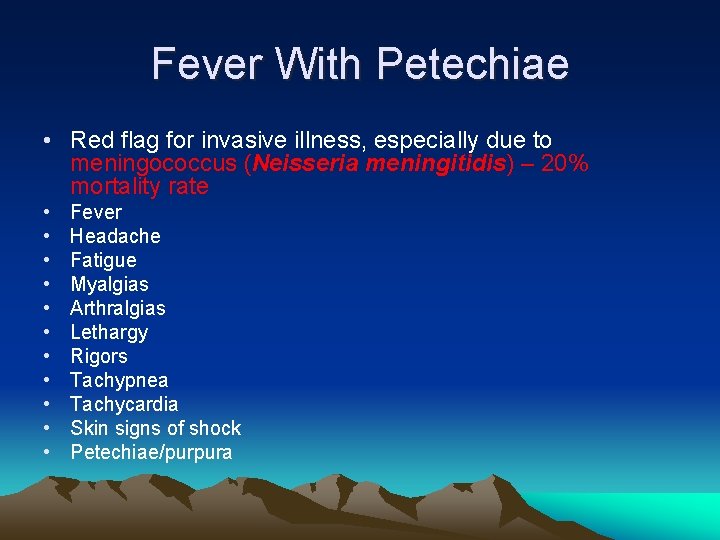
Fever With Petechiae • Red flag for invasive illness, especially due to meningococcus (Neisseria meningitidis) – 20% mortality rate • • • Fever Headache Fatigue Myalgias Arthralgias Lethargy Rigors Tachypnea Tachycardia Skin signs of shock Petechiae/purpura
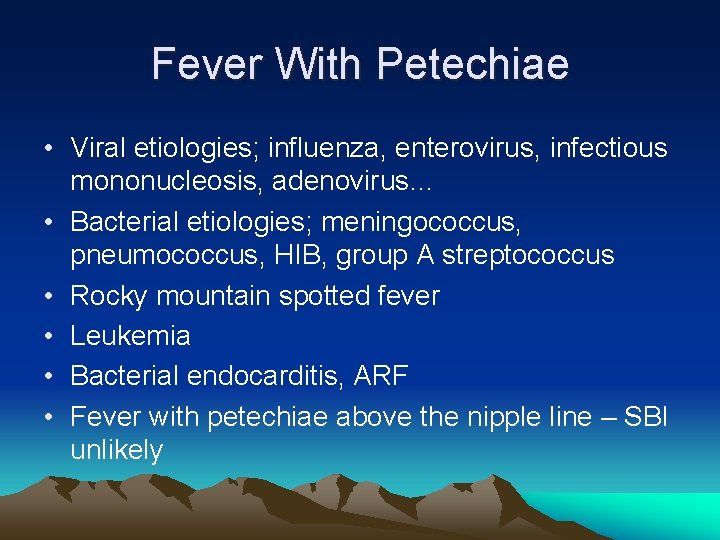
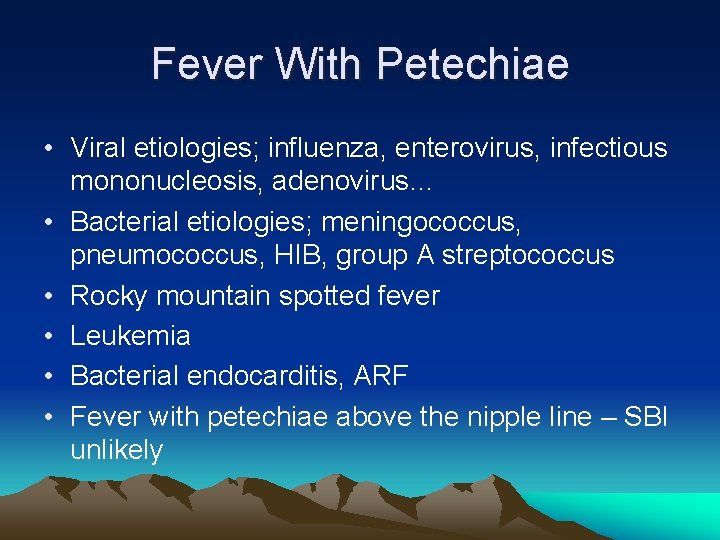
Fever With Petechiae • Viral etiologies; influenza, enterovirus, infectious mononucleosis, adenovirus… • Bacterial etiologies; meningococcus, pneumococcus, HIB, group A streptococcus • Rocky mountain spotted fever • Leukemia • Bacterial endocarditis, ARF • Fever with petechiae above the nipple line – SBI unlikely
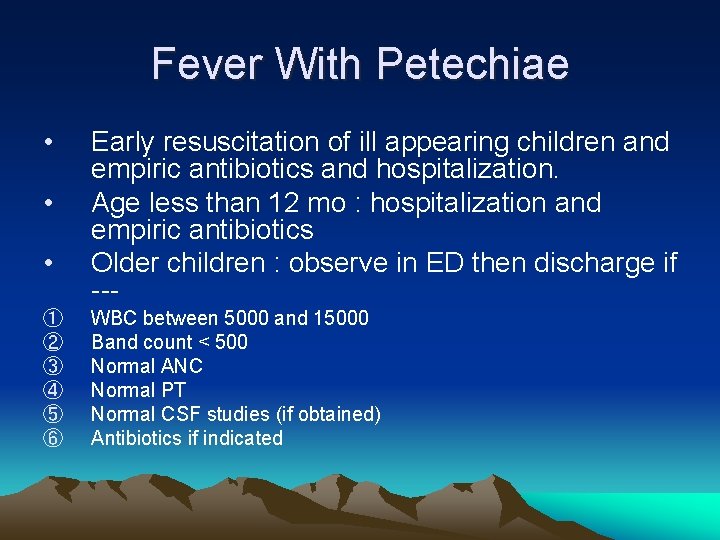
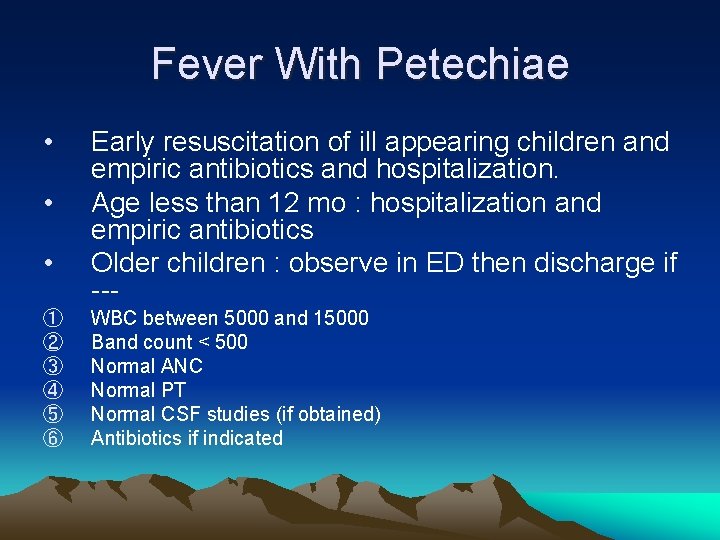
Fever With Petechiae • • • ① ② ③ ④ ⑤ ⑥ Early resuscitation of ill appearing children and empiric antibiotics and hospitalization. Age less than 12 mo : hospitalization and empiric antibiotics Older children : observe in ED then discharge if --WBC between 5000 and 15000 Band count < 500 Normal ANC Normal PT Normal CSF studies (if obtained) Antibiotics if indicated
Thanks for your attention!!